User login
AAGL Global Congress of Minimally Invasive Gynecology 2012
Hysterectomy Trendelenburg position: Less may be more
LAS VEGAS – Significantly reducing the degree of Trendelenburg position during robotic-assisted hysterectomy did not increase operative time and cut blood loss in half in a small retrospective analysis.
Surgeons spent an average of 66.5 minutes (range, 38-110 minutes) at the console when patients were placed in a minimum Trendelenburg position, compared with 79 minutes (range, 30-180 minutes) with a steep Trendelenburg position.
The difference in this primary outcome failed to achieve statistical significance (P = .105); however, the use of a minimum Trendelenburg position significantly reduced the average estimated blood loss from 101.3 mL to 50 mL (P = .007), Dr. Kelli Sasada reported at the 41st AAGL Global Congress.
A minimum degree of Trendelenburg position can be as effective as a steep Trendelenburg position in achieving adequate surgical exposure, thereby allowing safe completion of hysterectomy without increasing operative time, she said.
A steep Trendelenburg position, defined as at least 20 degrees in the anesthesia literature, improves the view of the surgical area during pelvic surgery by taking advantage of gravity to retract the bowels. It is common practice to use this approach during robotic-assisted hysterectomy because the patient’s position cannot conveniently be adjusted once the robot is docked, Dr. Sasada explained.
A steep Trendelenburg position, however, is often fraught with complications that can be severe and permanent, such as neural and retinal injuries, the patient moving or sliding off the table, ventilation concerns including airway access for the anesthesia provider, poor cardiopulmonary status, and alopecia, she added.
To explore the minimum degree of Trendelenburg necessary to complete the surgery safely, Dr. Sasada and her associate, Dr. Linda Mihalov, at Virginia Mason Medical Center in Seattle, took advantage of a new iPad app called clinometer HD (by plaincode) among 50 women undergoing da Vinci robotic-assisted benign total laparoscopic hysterectomy with or without bilateral salpingo-oophorectomy. Patients were secured in the dorsal lithotomy position, the abdomen was entered laparoscopically, and a brief survey was conducted to assess the size, position, and accessibility of the pelvic organs. The degree of Trendelenburg was determined by the surgeon and the iPad clinometer HD placed on the bed rail to measure the table tilt. The robot was then docked parallel to the patient’s side, and the surgery completed.
A steep Trendelenburg, defined as 30 degrees, was used in 38 women, and a minimum degree of Trendelenburg averaging 16.6 degrees (range, 13.8-19 degrees) used in 12 women, said Dr. Sasada, now with United Hospital System, St. Catherine’s Medical Center in Pleasant Prairie, Wis.
The average uterine weight was not significantly different between the steep and minimum Trendelenburg groups (215.4 g vs. 173.6 g; P = .21).
Body mass index also was similar at 28.5 kg/m2 vs. 25 kg/m2 (P = .071), with a wide range in both groups, she said.
There was one case of intraoperative bleeding (500 cc) and no postoperative complications in the steep Trendelenburg group, and one case of postoperative urinary retention and no intraoperative complications in the minimum Trendelenburg group.
During a discussion of the study, Dr. Sasada said it’s possible that the lower blood loss with the minimum Trendelenburg position could be due to chance, but that both surgeries were completed with the same four incisions and without bowel prep.
Dr. Sasada currently uses a minimum Trendelenburg position and an iPad when performing robotic-assisted hysterectomy and other pelvic surgeries, but not in all cases, as some OR beds have built-in clinometers. The advantage of the iPad technology is that it offers "ease of use in the OR by anesthesia or nursing staff, and reproducibility between OR beds," she said in an interview.
Dr. Sasada and Dr. Mihalov reported no relevant financial disclosures.
LAS VEGAS – Significantly reducing the degree of Trendelenburg position during robotic-assisted hysterectomy did not increase operative time and cut blood loss in half in a small retrospective analysis.
Surgeons spent an average of 66.5 minutes (range, 38-110 minutes) at the console when patients were placed in a minimum Trendelenburg position, compared with 79 minutes (range, 30-180 minutes) with a steep Trendelenburg position.
The difference in this primary outcome failed to achieve statistical significance (P = .105); however, the use of a minimum Trendelenburg position significantly reduced the average estimated blood loss from 101.3 mL to 50 mL (P = .007), Dr. Kelli Sasada reported at the 41st AAGL Global Congress.
A minimum degree of Trendelenburg position can be as effective as a steep Trendelenburg position in achieving adequate surgical exposure, thereby allowing safe completion of hysterectomy without increasing operative time, she said.
A steep Trendelenburg position, defined as at least 20 degrees in the anesthesia literature, improves the view of the surgical area during pelvic surgery by taking advantage of gravity to retract the bowels. It is common practice to use this approach during robotic-assisted hysterectomy because the patient’s position cannot conveniently be adjusted once the robot is docked, Dr. Sasada explained.
A steep Trendelenburg position, however, is often fraught with complications that can be severe and permanent, such as neural and retinal injuries, the patient moving or sliding off the table, ventilation concerns including airway access for the anesthesia provider, poor cardiopulmonary status, and alopecia, she added.
To explore the minimum degree of Trendelenburg necessary to complete the surgery safely, Dr. Sasada and her associate, Dr. Linda Mihalov, at Virginia Mason Medical Center in Seattle, took advantage of a new iPad app called clinometer HD (by plaincode) among 50 women undergoing da Vinci robotic-assisted benign total laparoscopic hysterectomy with or without bilateral salpingo-oophorectomy. Patients were secured in the dorsal lithotomy position, the abdomen was entered laparoscopically, and a brief survey was conducted to assess the size, position, and accessibility of the pelvic organs. The degree of Trendelenburg was determined by the surgeon and the iPad clinometer HD placed on the bed rail to measure the table tilt. The robot was then docked parallel to the patient’s side, and the surgery completed.
A steep Trendelenburg, defined as 30 degrees, was used in 38 women, and a minimum degree of Trendelenburg averaging 16.6 degrees (range, 13.8-19 degrees) used in 12 women, said Dr. Sasada, now with United Hospital System, St. Catherine’s Medical Center in Pleasant Prairie, Wis.
The average uterine weight was not significantly different between the steep and minimum Trendelenburg groups (215.4 g vs. 173.6 g; P = .21).
Body mass index also was similar at 28.5 kg/m2 vs. 25 kg/m2 (P = .071), with a wide range in both groups, she said.
There was one case of intraoperative bleeding (500 cc) and no postoperative complications in the steep Trendelenburg group, and one case of postoperative urinary retention and no intraoperative complications in the minimum Trendelenburg group.
During a discussion of the study, Dr. Sasada said it’s possible that the lower blood loss with the minimum Trendelenburg position could be due to chance, but that both surgeries were completed with the same four incisions and without bowel prep.
Dr. Sasada currently uses a minimum Trendelenburg position and an iPad when performing robotic-assisted hysterectomy and other pelvic surgeries, but not in all cases, as some OR beds have built-in clinometers. The advantage of the iPad technology is that it offers "ease of use in the OR by anesthesia or nursing staff, and reproducibility between OR beds," she said in an interview.
Dr. Sasada and Dr. Mihalov reported no relevant financial disclosures.
LAS VEGAS – Significantly reducing the degree of Trendelenburg position during robotic-assisted hysterectomy did not increase operative time and cut blood loss in half in a small retrospective analysis.
Surgeons spent an average of 66.5 minutes (range, 38-110 minutes) at the console when patients were placed in a minimum Trendelenburg position, compared with 79 minutes (range, 30-180 minutes) with a steep Trendelenburg position.
The difference in this primary outcome failed to achieve statistical significance (P = .105); however, the use of a minimum Trendelenburg position significantly reduced the average estimated blood loss from 101.3 mL to 50 mL (P = .007), Dr. Kelli Sasada reported at the 41st AAGL Global Congress.
A minimum degree of Trendelenburg position can be as effective as a steep Trendelenburg position in achieving adequate surgical exposure, thereby allowing safe completion of hysterectomy without increasing operative time, she said.
A steep Trendelenburg position, defined as at least 20 degrees in the anesthesia literature, improves the view of the surgical area during pelvic surgery by taking advantage of gravity to retract the bowels. It is common practice to use this approach during robotic-assisted hysterectomy because the patient’s position cannot conveniently be adjusted once the robot is docked, Dr. Sasada explained.
A steep Trendelenburg position, however, is often fraught with complications that can be severe and permanent, such as neural and retinal injuries, the patient moving or sliding off the table, ventilation concerns including airway access for the anesthesia provider, poor cardiopulmonary status, and alopecia, she added.
To explore the minimum degree of Trendelenburg necessary to complete the surgery safely, Dr. Sasada and her associate, Dr. Linda Mihalov, at Virginia Mason Medical Center in Seattle, took advantage of a new iPad app called clinometer HD (by plaincode) among 50 women undergoing da Vinci robotic-assisted benign total laparoscopic hysterectomy with or without bilateral salpingo-oophorectomy. Patients were secured in the dorsal lithotomy position, the abdomen was entered laparoscopically, and a brief survey was conducted to assess the size, position, and accessibility of the pelvic organs. The degree of Trendelenburg was determined by the surgeon and the iPad clinometer HD placed on the bed rail to measure the table tilt. The robot was then docked parallel to the patient’s side, and the surgery completed.
A steep Trendelenburg, defined as 30 degrees, was used in 38 women, and a minimum degree of Trendelenburg averaging 16.6 degrees (range, 13.8-19 degrees) used in 12 women, said Dr. Sasada, now with United Hospital System, St. Catherine’s Medical Center in Pleasant Prairie, Wis.
The average uterine weight was not significantly different between the steep and minimum Trendelenburg groups (215.4 g vs. 173.6 g; P = .21).
Body mass index also was similar at 28.5 kg/m2 vs. 25 kg/m2 (P = .071), with a wide range in both groups, she said.
There was one case of intraoperative bleeding (500 cc) and no postoperative complications in the steep Trendelenburg group, and one case of postoperative urinary retention and no intraoperative complications in the minimum Trendelenburg group.
During a discussion of the study, Dr. Sasada said it’s possible that the lower blood loss with the minimum Trendelenburg position could be due to chance, but that both surgeries were completed with the same four incisions and without bowel prep.
Dr. Sasada currently uses a minimum Trendelenburg position and an iPad when performing robotic-assisted hysterectomy and other pelvic surgeries, but not in all cases, as some OR beds have built-in clinometers. The advantage of the iPad technology is that it offers "ease of use in the OR by anesthesia or nursing staff, and reproducibility between OR beds," she said in an interview.
Dr. Sasada and Dr. Mihalov reported no relevant financial disclosures.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: Average estimated blood loss was 101.3 mL with the steep Trendelenburg position vs. 50 mL with the minimum Trendelenburg (P = .007).
Data Source: Retrospective chart study of 50 women undergoing robotic-assisted hysterectomy.
Disclosures: Dr. Sasada and Dr. Mihalov reported no relevant financial disclosures.
Simple technique facilitates laparoscopic port closure
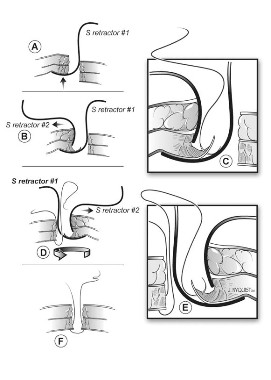
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
LAS VEGAS – Surgeons have developed a simple new suture technique using two S-retractors to close laparoscopic and robotic surgery ports without sacrificing visualization.
"This method involves minimal training and surgical skill, is quick to perform, and requires no additional instrumentation and no additional cost to the institution, surgeon, or patient," Dr. Homayara Aziz said at the 41st AAGL Global Congress.
No fewer than 29 original methods have been described in the literature for fascial closure, but many use assistance from inside the abdomen or extracorporeal assistance, and require additional ports. Others can be performed without an additional port, but may or may not provide direct visualization when securing the abdominal wall fascia and peritoneum.
With the new technique, devised at the State University of New York at Buffalo, the needle does not enter the peritoneal cavity blindly, where the bowel or other visceral organs may be present, Dr. Aziz said. Instead, the S-retractor functions as a barrier to protect the contents of the abdominal cavity, reducing the risk of visceral injuries.
The S-retractor also provides direct visualization of the different abdominal layers, exposing the needle tip during its course through the fascia. Because there is no needle tip in the intraperitoneal cavity, the procedure is safer, she said.
The two-step process starts with the surgeon inserting an S-retractor through the incision into the peritoneal cavity and then lifting the abdominal layers with the bottom of the retractor, creating a barrier between the fascia and the visceral contents. The assistant uses a second S-retractor to retract the skin, fat, and muscle in the opposite direction to expose the fascia. The surgeon then uses a needle suture to grasp the fascia, Dr. Aziz explained.
The first retractor is then rotated 180 degrees in the peritoneum by the surgeon to allow for work on the opposite side of the fascia. The second retractor, used by the assistant, is also moved to the opposite side of the abdominal wall layers to expose the fascia.
The surgeon again continues to grasp the opposite side of the fascia with the suture. The two ends are tied and the fascia is closed. If the fascial defect is greater than 10 mm, the surgeon may continue the same technique for another interrupted suture, figure of 8, or running closure, said Dr. Aziz, now a clinical instructor of obstetrics, gynecology, and reproductive science at the University of Maryland, Baltimore.
She reported on a prospective, consecutive case series involving 100 private and clinic patients in which this method was used over a 3-year period for fascial closure of total laparoscopic hysterectomies; bilateral or unilateral salpingo-oophorectomy where the port site was more than 12 mm to remove the specimen using an endocatch bag; and any robotic surgery where the ports are generally more than 8 mm.
There were no intraoperative incidents, nor was there added operative time or need to access costly instruments, she said.
No bowel injuries or port-site hernias were reported during a mean follow-up of 6 weeks post surgery and at 12-month annual follow-up.
"Closure of the fascia should remain simple, easy, cost-effective, and quick to apply," Dr. Aziz said. "It should also be safe and without any complications, and this technique described here fulfills all of these criteria."
The technique takes 5 minutes or less to learn, and has been used on at least 200 additional patients at both institutions since the current analysis was performed, Dr. Aziz said in an interview. "Many of my attendings at SUNY Buffalo call it ‘the Aziz technique’ and [it] has gained much popularity."
Dr. Aziz reported no relevant conflicts of interest.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: There were no intraoperative incidents, and no bowel injuries or port site hernias, during a mean follow-up of 6 weeks post surgery and at 12 months follow-up.
Data Source: Prospective, consecutive case series of 100 patients.
Disclosures: Dr. Aziz reported no relevant conflicts of interest.
Study: Uterus Preservation Feasible with Mesh POP Repair System
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
AT THE 41st AAGL GLOBAL CONGRESS
Major Finding: For the apical compartment, success at 24 months was reported in 93.5% of patients with a prior hysterectomy (29 patients), 94.4% of those with a concomitant hysterectomy (17), and 100% with no hysterectomy (24). For the anterior compartment, success was 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17), and 89% with uterine preservation (41).
Data Source: This was a prospective, international study of 142 women treated with the Elevate Anterior and Apical Prolapse Repair System.
Disclosures: Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
Older Docs Still Balking at Minimally Invasive Hysterectomy
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P value = .03).
Data Source: Data are from a mixed-mode, cross-sectional survey sent to 802 ACOG fellows; 52% responded.
Disclosures: Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
Suture Method Linked to Vaginal Cuff Complications
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: One case of evisceration and 4 cases of dehiscence occurred with the intracorporeal continuous suture vs. 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P value = .02)
Data Source: Data are from a retrospective, single-center analysis involving 604 women undergoing six types of hysterectomies.
Disclosures: Dr. Kim reported no relevant financial disclosures.
Are Hysterectomies Really on the Decline?
LAS VEGAS – The number of hysterectomies in the United States appears to be on the decline, despite a 10% increase in minimally invasive cases.
Based on updated surveillance data, an estimated 479,229 hysterectomies were performed in the United States in 2009, of which 24% used a laparoscopic approach.
By comparison, there were 518,828 hysterectomies in 2005, 14% of which were laparoscopic: 64% were abdominal and 22% were vaginal (Obstet. Gynecol. 2009;114:1041-8).
Whether this represents a real decline in hysterectomies is unclear, Dr. Sarah Cohen of Brigham and Women’s Hospital in Boston said at the 41st AAGL Global Congress.
The current analysis included oncologic cases, whereas the 2005 analysis looked only at gynecologic hysterectomies for benign disease.
On the other hand, both analyses are based on the Nationwide Inpatient Sample (NIS), which represents a 20% stratified random sample of discharges from all community hospitals in the United States. It is the largest national all-payer database of hospital discharges, but that’s where it stops.
"It’s possible that there are a number of nonsurgical options being offered to patients; however, I do think this also represents the increase in outpatient surgeries being offered, and the Nationwide Inpatient Sample databases aren’t able to account for those," she said. "Particularly, we may be underestimating laparoscopic and vaginal procedures that are being done in ambulatory settings."
Hysterectomy is the most common nonobstetric surgical procedure among women, with 600,000 typically cited as the annual number of procedures.
Dr. Cohen and her colleagues sought to verify this number using ICD-9 codes in the 2009 NIS – the most recent year available – to abstract information about any patient who underwent a hysterectomy during her hospitalization, including oncologic cases. Obstetric hysterectomies were excluded. The data were then weighted to give national estimates.
The mean patient age was 48 years, and the predominant indications were uterine fibroids (47%) and menstrual disorders (45%). Adnexal surgery occurred in 57% of cases.
Abdominal hysterectomy made up 58% of cases and vaginal hysterectomy 17% in the updated analysis, compared with 64% and 22% in the 2005 NIS, Dr. Cohen said.
In regression analysis, factors associated with laparoscopic surgery compared with abdominal surgery were younger age, white race, an indication of prolapse, menstrual disorder or endometriosis, living in an urban area, having a high income, having private insurance, and living in the Western United States.
When the regressions were repeated to compare laparoscopic with vaginal surgery, factors favoring the laparoscopic approach were age 40-49, black race, any nonprolapse indication, concomitant adnexal surgery, living in an urban area, having a high income, having private insurance, and living in the Northeastern United States.
Based on a systematic review of the literature, seven articles have been published in the past 5 years regarding hysterectomy surveillance, Dr. Cohen observed.
Although the NIS database may be incomplete, the bidirectional trends of falling overall numbers and rising laparoscopic procedures appear to be holding. An analysis of the 2003 NIS revealed 602,457 hysterectomies, with the abdominal route the most common at 66%, followed by the vaginal (22%) and laparoscopic (12%) routes (Obstet. Gynecol. 2007;110:1091-5).
Dr. Cohen said it’s critical to continue evaluating trends in hysterectomy performance, particularly with increasing outpatient minimally invasive procedures, and that he and his colleagues plan to incorporate state-level ambulatory surgery databases to capture outpatient procedures. They also will perform subgroup analyses of benign and oncologic cases, and look at factors associated with concomitant adnexal procedures.
Dr. Cohen reported no relevant financial disclosures.
LAS VEGAS – The number of hysterectomies in the United States appears to be on the decline, despite a 10% increase in minimally invasive cases.
Based on updated surveillance data, an estimated 479,229 hysterectomies were performed in the United States in 2009, of which 24% used a laparoscopic approach.
By comparison, there were 518,828 hysterectomies in 2005, 14% of which were laparoscopic: 64% were abdominal and 22% were vaginal (Obstet. Gynecol. 2009;114:1041-8).
Whether this represents a real decline in hysterectomies is unclear, Dr. Sarah Cohen of Brigham and Women’s Hospital in Boston said at the 41st AAGL Global Congress.
The current analysis included oncologic cases, whereas the 2005 analysis looked only at gynecologic hysterectomies for benign disease.
On the other hand, both analyses are based on the Nationwide Inpatient Sample (NIS), which represents a 20% stratified random sample of discharges from all community hospitals in the United States. It is the largest national all-payer database of hospital discharges, but that’s where it stops.
"It’s possible that there are a number of nonsurgical options being offered to patients; however, I do think this also represents the increase in outpatient surgeries being offered, and the Nationwide Inpatient Sample databases aren’t able to account for those," she said. "Particularly, we may be underestimating laparoscopic and vaginal procedures that are being done in ambulatory settings."
Hysterectomy is the most common nonobstetric surgical procedure among women, with 600,000 typically cited as the annual number of procedures.
Dr. Cohen and her colleagues sought to verify this number using ICD-9 codes in the 2009 NIS – the most recent year available – to abstract information about any patient who underwent a hysterectomy during her hospitalization, including oncologic cases. Obstetric hysterectomies were excluded. The data were then weighted to give national estimates.
The mean patient age was 48 years, and the predominant indications were uterine fibroids (47%) and menstrual disorders (45%). Adnexal surgery occurred in 57% of cases.
Abdominal hysterectomy made up 58% of cases and vaginal hysterectomy 17% in the updated analysis, compared with 64% and 22% in the 2005 NIS, Dr. Cohen said.
In regression analysis, factors associated with laparoscopic surgery compared with abdominal surgery were younger age, white race, an indication of prolapse, menstrual disorder or endometriosis, living in an urban area, having a high income, having private insurance, and living in the Western United States.
When the regressions were repeated to compare laparoscopic with vaginal surgery, factors favoring the laparoscopic approach were age 40-49, black race, any nonprolapse indication, concomitant adnexal surgery, living in an urban area, having a high income, having private insurance, and living in the Northeastern United States.
Based on a systematic review of the literature, seven articles have been published in the past 5 years regarding hysterectomy surveillance, Dr. Cohen observed.
Although the NIS database may be incomplete, the bidirectional trends of falling overall numbers and rising laparoscopic procedures appear to be holding. An analysis of the 2003 NIS revealed 602,457 hysterectomies, with the abdominal route the most common at 66%, followed by the vaginal (22%) and laparoscopic (12%) routes (Obstet. Gynecol. 2007;110:1091-5).
Dr. Cohen said it’s critical to continue evaluating trends in hysterectomy performance, particularly with increasing outpatient minimally invasive procedures, and that he and his colleagues plan to incorporate state-level ambulatory surgery databases to capture outpatient procedures. They also will perform subgroup analyses of benign and oncologic cases, and look at factors associated with concomitant adnexal procedures.
Dr. Cohen reported no relevant financial disclosures.
LAS VEGAS – The number of hysterectomies in the United States appears to be on the decline, despite a 10% increase in minimally invasive cases.
Based on updated surveillance data, an estimated 479,229 hysterectomies were performed in the United States in 2009, of which 24% used a laparoscopic approach.
By comparison, there were 518,828 hysterectomies in 2005, 14% of which were laparoscopic: 64% were abdominal and 22% were vaginal (Obstet. Gynecol. 2009;114:1041-8).
Whether this represents a real decline in hysterectomies is unclear, Dr. Sarah Cohen of Brigham and Women’s Hospital in Boston said at the 41st AAGL Global Congress.
The current analysis included oncologic cases, whereas the 2005 analysis looked only at gynecologic hysterectomies for benign disease.
On the other hand, both analyses are based on the Nationwide Inpatient Sample (NIS), which represents a 20% stratified random sample of discharges from all community hospitals in the United States. It is the largest national all-payer database of hospital discharges, but that’s where it stops.
"It’s possible that there are a number of nonsurgical options being offered to patients; however, I do think this also represents the increase in outpatient surgeries being offered, and the Nationwide Inpatient Sample databases aren’t able to account for those," she said. "Particularly, we may be underestimating laparoscopic and vaginal procedures that are being done in ambulatory settings."
Hysterectomy is the most common nonobstetric surgical procedure among women, with 600,000 typically cited as the annual number of procedures.
Dr. Cohen and her colleagues sought to verify this number using ICD-9 codes in the 2009 NIS – the most recent year available – to abstract information about any patient who underwent a hysterectomy during her hospitalization, including oncologic cases. Obstetric hysterectomies were excluded. The data were then weighted to give national estimates.
The mean patient age was 48 years, and the predominant indications were uterine fibroids (47%) and menstrual disorders (45%). Adnexal surgery occurred in 57% of cases.
Abdominal hysterectomy made up 58% of cases and vaginal hysterectomy 17% in the updated analysis, compared with 64% and 22% in the 2005 NIS, Dr. Cohen said.
In regression analysis, factors associated with laparoscopic surgery compared with abdominal surgery were younger age, white race, an indication of prolapse, menstrual disorder or endometriosis, living in an urban area, having a high income, having private insurance, and living in the Western United States.
When the regressions were repeated to compare laparoscopic with vaginal surgery, factors favoring the laparoscopic approach were age 40-49, black race, any nonprolapse indication, concomitant adnexal surgery, living in an urban area, having a high income, having private insurance, and living in the Northeastern United States.
Based on a systematic review of the literature, seven articles have been published in the past 5 years regarding hysterectomy surveillance, Dr. Cohen observed.
Although the NIS database may be incomplete, the bidirectional trends of falling overall numbers and rising laparoscopic procedures appear to be holding. An analysis of the 2003 NIS revealed 602,457 hysterectomies, with the abdominal route the most common at 66%, followed by the vaginal (22%) and laparoscopic (12%) routes (Obstet. Gynecol. 2007;110:1091-5).
Dr. Cohen said it’s critical to continue evaluating trends in hysterectomy performance, particularly with increasing outpatient minimally invasive procedures, and that he and his colleagues plan to incorporate state-level ambulatory surgery databases to capture outpatient procedures. They also will perform subgroup analyses of benign and oncologic cases, and look at factors associated with concomitant adnexal procedures.
Dr. Cohen reported no relevant financial disclosures.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: An estimated 479,229 hysterectomies were performed in 2009, compared with 518,828 in 2005.
Data Source: Data are from an analysis of the 2009 Nationwide Inpatient Sample.
Disclosures: Dr. Cohen reported no relevant financial disclosures.
Radiofrequency Ablation: A Possible Game Changer for Uterine Fibroids
LAS VEGAS – Ultrasound-guided radiofrequency ablation offers women a new, noninvasive treatment option for painful uterine fibroids.
"I actually think this changes the entire outlook," Dr. Scott Chudnoff said at the AAGL Global Congress. "The beauty of this is the simplicity. The risk is so low.
"I’ve been coming to AAGL for years and what I love about it is seeing the new technology on the horizon, and this is the first one in a few years that is a real game changer for the organization and for gynecology in general," he said in an interview.
He presented data from an international, phase III, single-arm study evaluating the safety and efficacy of the Acessa system to treat moderate to severe bleeding in 135 consecutive women, ages 30-54 years, with symptomatic fibroids.
The results prompted the Food and Drug Administration to clear Acessa for the treatment of uterine leiomyoma on Nov. 6, 2012, just as the AAGL Congress kicked off.
Acessa is already in use in Canada and Europe, and shrinks fibroids using radiofrequency energy delivered via an electrode array inserted into the fibroid under intra-abdominal laparoscopic ultrasound guidance.
One in five women may have fibroids during their childbearing years, and they are present in half of all women by aged 50 years. Many are asymptomatic, but fibroids are also one of the leading causes of hysterectomy.
The last time there was a change in fibroid treatment options was more than 5 years ago with the arrival of MRI-guided focused ultrasound ablation, but the data on this have been somewhat disappointing, said Dr. Chudnoff, director of obstetrics and gynecology and women’s health at Montefiore Medical Center in New York.
There are a range of medical therapies, but they primarily target the symptomatology and not the fibroid itself. Uterine artery embolization is a fantastic procedure, but it’s a global destruction process of the entire uterus, and there are concerns regarding future fertility, he observed. Hysteroscopic fibroid resection is useful for submucosal fibroids, but access is often difficult and women typically have other types of fibroids as well.
Finally, there’s myomectomy, "a bloody, invasive procedure that more often than not dooms the patient to having a Cesarean section and carries a recurrence rate of about 80%," Dr. Chudnoff said.
"So what do you tell your 35-year-old patient that comes into your office and says, ‘What can you do for me?’ " Dr. Chudnoff said. "That’s where I think this comes in. It is that opportunity to get in there early before patients become extremely symptomatic and treat these fibroids with fibroid-directed therapy.
"If in 5 or 10 years they get new fibroids, I can treat them again, but there’s a big difference between doing this and doing a myomectomy again or having to do a hysterectomy in a post-myomectomy patient. Those are disasters," he said.
Women in the trial had clinical menorrhagia (160-500 cc of menstrual blood loss per cycle), no more than six fibroids (mean, five), and a total uterine volume of 300 cc or less. Fibroid types were 193 subserosals, 347 intramurals, 39 transmurals, and 164 submucosals. The trial did not include pedunculated fibroids or type 0 fibroids because of concerns that ablation near the base of the stalk could result in secondary potential complications such as superinfections, he said.
In all, 674 fibroids were treated with Acessa, 96.2% on an outpatient basis. Patients returned to normal activity in an average of 7-10 days, and went back to work at a median of 9 days (range 0-29 days).
Patient-reported symptom severity scores on the validated Uterine Fibroid Symptom and Quality-of-Life (UFS-QOL) questionnaire decreased from a mean of 61.4 at baseline to 28.7 at 3 months, 28.6 at 6 months, and was significant at 26.4 at 12 months (P value less than .001), Dr. Chudnoff reported.
At the same time, mean quality of life scores on the UFS-QOL improved from 37.1 at baseline to 75.2, 78.1, and 80 (P less than .0001 at 12 months).
"What’s important to note is that patients continue to improve and [this] persists at high levels," he said.
Mean scores on the EuroQoL-5 dimensions (EQ-5D) measure also increased from 70.7 at baseline to 84.9 at 3 months, 84.6 at 6 months, and were significant at 85.7 at 12 months (P less than .0001).
There were five (3.7%) device-related adverse events: lower abdominal pain, pelvic abscess, two superficial uterine serosal burns, and post-treatment bleeding.
One patient underwent uterine artery embolization after withdrawing from the trial before her 6-month follow-up visit, resulting in a reintervention rate of 0.7%.
In separate presentations at the meeting, fellow Acessa investigators reported significant decreases at 3 and 12 months in mean uterine volume of 16% and 25% and in mean fibroid volume of 38% and 44.3%. Clinically significant reductions in menstrual bleeding were observed in 69% of women (mean 101.6 cc).
Reductions in alkaline hematin levels were associated with fibroid shrinkage. The mean alkaline hematin level was 271.5 mL at baseline, decreasing by 31% at 3 months, 41% at 6 months, and 38% at 12 months (all P less than .0001).
During a discussion of the study, Dr. Chudnoff said quality of life was not directly related to the size of fibroid shrinkage, but observed that all women who experienced fibroid shrinkage had symptom relief.
Finally, when asked about the overall effectiveness of the procedure, 98% of patients said they would recommend Acessa to a friend, 95% said they were satisfied with the treatment, and 94% thought it was effective, he reported.
Dr. Chudnoff and his coauthors reported serving as principal investigators for Halt Medical, which sponsored the study. One coauthor is also a consultant for Halt.
Although Dr. Chudnoff and his coauthors’ prospective, single-arm industry study of Acessa use of targeted radiofrequency ablation for uterine fibroids – which reports on only its first 12 months of follow-up – shows results that are promising, I would caution readers before adopting the technology wholeheartedly.
Dr.. Patrick J. Woodman |
We have seen similar impressive results with targeted vascular embolization of uterine fibroids. The decision to enthusiastically adopt uterine artery embolization lined a good number of radiologists’ pockets, while leaving unhappy gynecologists to deal with the inevitable complications of pain and bleeding.
Equally concerning are the authors’ claims that "the risk is so low." Although I expect that the "intra-abdominal" ultrasound guidance to evolve so that it could be done transvaginally, the approach still resulted in a 1.5% chance of "superficial uterine serosal burns." This could represent the risk of bowel injury in a patient without laparoscopic-ultrasound guidance.
It is reassuring that the Food and Drug Administration has approved the technology, and we have the American registration study and those from Canada and Europe from which to extrapolate safety and efficacy. Dr. Chudnoff’s study also boasts high subjective "satisfaction" and "effectiveness" scores on patient questionnaires. However, with such a short follow-up, it is hard to predict how many subjects will develop recurrence or ultimately require hysterectomy.
Finally, I caution readers to pay attention to the difference between "statistically significant differences" and "clinically significant differences." Although the UFS-QOL and the EuroQoL are validated fibroid questionnaires, my perusal of published literature did not turn up what would be considered the "minimal clinically significant difference" for each measure. A 50% reduction in severity or improvement in QoL score means nothing if the symptoms are not severe, or if the "bother" is very low. Just because there was a numerical difference in the subjects between pre- and post-treatment does not mean that difference necessarily matters.
Patrick J. Woodman, D.O., is a urogynecologist, associate professor of obstetrics and gynecology, and is chief of specialty care at Marian University College of Osteopathic Medicine in Indianapolis. He said that he has no disclosures pertinent to the story.
Although Dr. Chudnoff and his coauthors’ prospective, single-arm industry study of Acessa use of targeted radiofrequency ablation for uterine fibroids – which reports on only its first 12 months of follow-up – shows results that are promising, I would caution readers before adopting the technology wholeheartedly.
Dr.. Patrick J. Woodman |
We have seen similar impressive results with targeted vascular embolization of uterine fibroids. The decision to enthusiastically adopt uterine artery embolization lined a good number of radiologists’ pockets, while leaving unhappy gynecologists to deal with the inevitable complications of pain and bleeding.
Equally concerning are the authors’ claims that "the risk is so low." Although I expect that the "intra-abdominal" ultrasound guidance to evolve so that it could be done transvaginally, the approach still resulted in a 1.5% chance of "superficial uterine serosal burns." This could represent the risk of bowel injury in a patient without laparoscopic-ultrasound guidance.
It is reassuring that the Food and Drug Administration has approved the technology, and we have the American registration study and those from Canada and Europe from which to extrapolate safety and efficacy. Dr. Chudnoff’s study also boasts high subjective "satisfaction" and "effectiveness" scores on patient questionnaires. However, with such a short follow-up, it is hard to predict how many subjects will develop recurrence or ultimately require hysterectomy.
Finally, I caution readers to pay attention to the difference between "statistically significant differences" and "clinically significant differences." Although the UFS-QOL and the EuroQoL are validated fibroid questionnaires, my perusal of published literature did not turn up what would be considered the "minimal clinically significant difference" for each measure. A 50% reduction in severity or improvement in QoL score means nothing if the symptoms are not severe, or if the "bother" is very low. Just because there was a numerical difference in the subjects between pre- and post-treatment does not mean that difference necessarily matters.
Patrick J. Woodman, D.O., is a urogynecologist, associate professor of obstetrics and gynecology, and is chief of specialty care at Marian University College of Osteopathic Medicine in Indianapolis. He said that he has no disclosures pertinent to the story.
Although Dr. Chudnoff and his coauthors’ prospective, single-arm industry study of Acessa use of targeted radiofrequency ablation for uterine fibroids – which reports on only its first 12 months of follow-up – shows results that are promising, I would caution readers before adopting the technology wholeheartedly.
Dr.. Patrick J. Woodman |
We have seen similar impressive results with targeted vascular embolization of uterine fibroids. The decision to enthusiastically adopt uterine artery embolization lined a good number of radiologists’ pockets, while leaving unhappy gynecologists to deal with the inevitable complications of pain and bleeding.
Equally concerning are the authors’ claims that "the risk is so low." Although I expect that the "intra-abdominal" ultrasound guidance to evolve so that it could be done transvaginally, the approach still resulted in a 1.5% chance of "superficial uterine serosal burns." This could represent the risk of bowel injury in a patient without laparoscopic-ultrasound guidance.
It is reassuring that the Food and Drug Administration has approved the technology, and we have the American registration study and those from Canada and Europe from which to extrapolate safety and efficacy. Dr. Chudnoff’s study also boasts high subjective "satisfaction" and "effectiveness" scores on patient questionnaires. However, with such a short follow-up, it is hard to predict how many subjects will develop recurrence or ultimately require hysterectomy.
Finally, I caution readers to pay attention to the difference between "statistically significant differences" and "clinically significant differences." Although the UFS-QOL and the EuroQoL are validated fibroid questionnaires, my perusal of published literature did not turn up what would be considered the "minimal clinically significant difference" for each measure. A 50% reduction in severity or improvement in QoL score means nothing if the symptoms are not severe, or if the "bother" is very low. Just because there was a numerical difference in the subjects between pre- and post-treatment does not mean that difference necessarily matters.
Patrick J. Woodman, D.O., is a urogynecologist, associate professor of obstetrics and gynecology, and is chief of specialty care at Marian University College of Osteopathic Medicine in Indianapolis. He said that he has no disclosures pertinent to the story.
LAS VEGAS – Ultrasound-guided radiofrequency ablation offers women a new, noninvasive treatment option for painful uterine fibroids.
"I actually think this changes the entire outlook," Dr. Scott Chudnoff said at the AAGL Global Congress. "The beauty of this is the simplicity. The risk is so low.
"I’ve been coming to AAGL for years and what I love about it is seeing the new technology on the horizon, and this is the first one in a few years that is a real game changer for the organization and for gynecology in general," he said in an interview.
He presented data from an international, phase III, single-arm study evaluating the safety and efficacy of the Acessa system to treat moderate to severe bleeding in 135 consecutive women, ages 30-54 years, with symptomatic fibroids.
The results prompted the Food and Drug Administration to clear Acessa for the treatment of uterine leiomyoma on Nov. 6, 2012, just as the AAGL Congress kicked off.
Acessa is already in use in Canada and Europe, and shrinks fibroids using radiofrequency energy delivered via an electrode array inserted into the fibroid under intra-abdominal laparoscopic ultrasound guidance.
One in five women may have fibroids during their childbearing years, and they are present in half of all women by aged 50 years. Many are asymptomatic, but fibroids are also one of the leading causes of hysterectomy.
The last time there was a change in fibroid treatment options was more than 5 years ago with the arrival of MRI-guided focused ultrasound ablation, but the data on this have been somewhat disappointing, said Dr. Chudnoff, director of obstetrics and gynecology and women’s health at Montefiore Medical Center in New York.
There are a range of medical therapies, but they primarily target the symptomatology and not the fibroid itself. Uterine artery embolization is a fantastic procedure, but it’s a global destruction process of the entire uterus, and there are concerns regarding future fertility, he observed. Hysteroscopic fibroid resection is useful for submucosal fibroids, but access is often difficult and women typically have other types of fibroids as well.
Finally, there’s myomectomy, "a bloody, invasive procedure that more often than not dooms the patient to having a Cesarean section and carries a recurrence rate of about 80%," Dr. Chudnoff said.
"So what do you tell your 35-year-old patient that comes into your office and says, ‘What can you do for me?’ " Dr. Chudnoff said. "That’s where I think this comes in. It is that opportunity to get in there early before patients become extremely symptomatic and treat these fibroids with fibroid-directed therapy.
"If in 5 or 10 years they get new fibroids, I can treat them again, but there’s a big difference between doing this and doing a myomectomy again or having to do a hysterectomy in a post-myomectomy patient. Those are disasters," he said.
Women in the trial had clinical menorrhagia (160-500 cc of menstrual blood loss per cycle), no more than six fibroids (mean, five), and a total uterine volume of 300 cc or less. Fibroid types were 193 subserosals, 347 intramurals, 39 transmurals, and 164 submucosals. The trial did not include pedunculated fibroids or type 0 fibroids because of concerns that ablation near the base of the stalk could result in secondary potential complications such as superinfections, he said.
In all, 674 fibroids were treated with Acessa, 96.2% on an outpatient basis. Patients returned to normal activity in an average of 7-10 days, and went back to work at a median of 9 days (range 0-29 days).
Patient-reported symptom severity scores on the validated Uterine Fibroid Symptom and Quality-of-Life (UFS-QOL) questionnaire decreased from a mean of 61.4 at baseline to 28.7 at 3 months, 28.6 at 6 months, and was significant at 26.4 at 12 months (P value less than .001), Dr. Chudnoff reported.
At the same time, mean quality of life scores on the UFS-QOL improved from 37.1 at baseline to 75.2, 78.1, and 80 (P less than .0001 at 12 months).
"What’s important to note is that patients continue to improve and [this] persists at high levels," he said.
Mean scores on the EuroQoL-5 dimensions (EQ-5D) measure also increased from 70.7 at baseline to 84.9 at 3 months, 84.6 at 6 months, and were significant at 85.7 at 12 months (P less than .0001).
There were five (3.7%) device-related adverse events: lower abdominal pain, pelvic abscess, two superficial uterine serosal burns, and post-treatment bleeding.
One patient underwent uterine artery embolization after withdrawing from the trial before her 6-month follow-up visit, resulting in a reintervention rate of 0.7%.
In separate presentations at the meeting, fellow Acessa investigators reported significant decreases at 3 and 12 months in mean uterine volume of 16% and 25% and in mean fibroid volume of 38% and 44.3%. Clinically significant reductions in menstrual bleeding were observed in 69% of women (mean 101.6 cc).
Reductions in alkaline hematin levels were associated with fibroid shrinkage. The mean alkaline hematin level was 271.5 mL at baseline, decreasing by 31% at 3 months, 41% at 6 months, and 38% at 12 months (all P less than .0001).
During a discussion of the study, Dr. Chudnoff said quality of life was not directly related to the size of fibroid shrinkage, but observed that all women who experienced fibroid shrinkage had symptom relief.
Finally, when asked about the overall effectiveness of the procedure, 98% of patients said they would recommend Acessa to a friend, 95% said they were satisfied with the treatment, and 94% thought it was effective, he reported.
Dr. Chudnoff and his coauthors reported serving as principal investigators for Halt Medical, which sponsored the study. One coauthor is also a consultant for Halt.
LAS VEGAS – Ultrasound-guided radiofrequency ablation offers women a new, noninvasive treatment option for painful uterine fibroids.
"I actually think this changes the entire outlook," Dr. Scott Chudnoff said at the AAGL Global Congress. "The beauty of this is the simplicity. The risk is so low.
"I’ve been coming to AAGL for years and what I love about it is seeing the new technology on the horizon, and this is the first one in a few years that is a real game changer for the organization and for gynecology in general," he said in an interview.
He presented data from an international, phase III, single-arm study evaluating the safety and efficacy of the Acessa system to treat moderate to severe bleeding in 135 consecutive women, ages 30-54 years, with symptomatic fibroids.
The results prompted the Food and Drug Administration to clear Acessa for the treatment of uterine leiomyoma on Nov. 6, 2012, just as the AAGL Congress kicked off.
Acessa is already in use in Canada and Europe, and shrinks fibroids using radiofrequency energy delivered via an electrode array inserted into the fibroid under intra-abdominal laparoscopic ultrasound guidance.
One in five women may have fibroids during their childbearing years, and they are present in half of all women by aged 50 years. Many are asymptomatic, but fibroids are also one of the leading causes of hysterectomy.
The last time there was a change in fibroid treatment options was more than 5 years ago with the arrival of MRI-guided focused ultrasound ablation, but the data on this have been somewhat disappointing, said Dr. Chudnoff, director of obstetrics and gynecology and women’s health at Montefiore Medical Center in New York.
There are a range of medical therapies, but they primarily target the symptomatology and not the fibroid itself. Uterine artery embolization is a fantastic procedure, but it’s a global destruction process of the entire uterus, and there are concerns regarding future fertility, he observed. Hysteroscopic fibroid resection is useful for submucosal fibroids, but access is often difficult and women typically have other types of fibroids as well.
Finally, there’s myomectomy, "a bloody, invasive procedure that more often than not dooms the patient to having a Cesarean section and carries a recurrence rate of about 80%," Dr. Chudnoff said.
"So what do you tell your 35-year-old patient that comes into your office and says, ‘What can you do for me?’ " Dr. Chudnoff said. "That’s where I think this comes in. It is that opportunity to get in there early before patients become extremely symptomatic and treat these fibroids with fibroid-directed therapy.
"If in 5 or 10 years they get new fibroids, I can treat them again, but there’s a big difference between doing this and doing a myomectomy again or having to do a hysterectomy in a post-myomectomy patient. Those are disasters," he said.
Women in the trial had clinical menorrhagia (160-500 cc of menstrual blood loss per cycle), no more than six fibroids (mean, five), and a total uterine volume of 300 cc or less. Fibroid types were 193 subserosals, 347 intramurals, 39 transmurals, and 164 submucosals. The trial did not include pedunculated fibroids or type 0 fibroids because of concerns that ablation near the base of the stalk could result in secondary potential complications such as superinfections, he said.
In all, 674 fibroids were treated with Acessa, 96.2% on an outpatient basis. Patients returned to normal activity in an average of 7-10 days, and went back to work at a median of 9 days (range 0-29 days).
Patient-reported symptom severity scores on the validated Uterine Fibroid Symptom and Quality-of-Life (UFS-QOL) questionnaire decreased from a mean of 61.4 at baseline to 28.7 at 3 months, 28.6 at 6 months, and was significant at 26.4 at 12 months (P value less than .001), Dr. Chudnoff reported.
At the same time, mean quality of life scores on the UFS-QOL improved from 37.1 at baseline to 75.2, 78.1, and 80 (P less than .0001 at 12 months).
"What’s important to note is that patients continue to improve and [this] persists at high levels," he said.
Mean scores on the EuroQoL-5 dimensions (EQ-5D) measure also increased from 70.7 at baseline to 84.9 at 3 months, 84.6 at 6 months, and were significant at 85.7 at 12 months (P less than .0001).
There were five (3.7%) device-related adverse events: lower abdominal pain, pelvic abscess, two superficial uterine serosal burns, and post-treatment bleeding.
One patient underwent uterine artery embolization after withdrawing from the trial before her 6-month follow-up visit, resulting in a reintervention rate of 0.7%.
In separate presentations at the meeting, fellow Acessa investigators reported significant decreases at 3 and 12 months in mean uterine volume of 16% and 25% and in mean fibroid volume of 38% and 44.3%. Clinically significant reductions in menstrual bleeding were observed in 69% of women (mean 101.6 cc).
Reductions in alkaline hematin levels were associated with fibroid shrinkage. The mean alkaline hematin level was 271.5 mL at baseline, decreasing by 31% at 3 months, 41% at 6 months, and 38% at 12 months (all P less than .0001).
During a discussion of the study, Dr. Chudnoff said quality of life was not directly related to the size of fibroid shrinkage, but observed that all women who experienced fibroid shrinkage had symptom relief.
Finally, when asked about the overall effectiveness of the procedure, 98% of patients said they would recommend Acessa to a friend, 95% said they were satisfied with the treatment, and 94% thought it was effective, he reported.
Dr. Chudnoff and his coauthors reported serving as principal investigators for Halt Medical, which sponsored the study. One coauthor is also a consultant for Halt.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: Symptom severity scores decreased significantly from a mean of 61.4 at baseline to 28.7 at 3 months, 28.6 at 6 months and 26.4 at 12 months (P value less than .001).
Data Source: This was a prospective, multicenter phase III, single-arm study of 135 women with moderate to severe bleeding and symptomatic fibroids.
Disclosures: Dr. Chudnoff and his coauthors report serving as principal investigators for Halt Medical, which sponsored the study. One coauthor is also a consultant for Halt.