User login
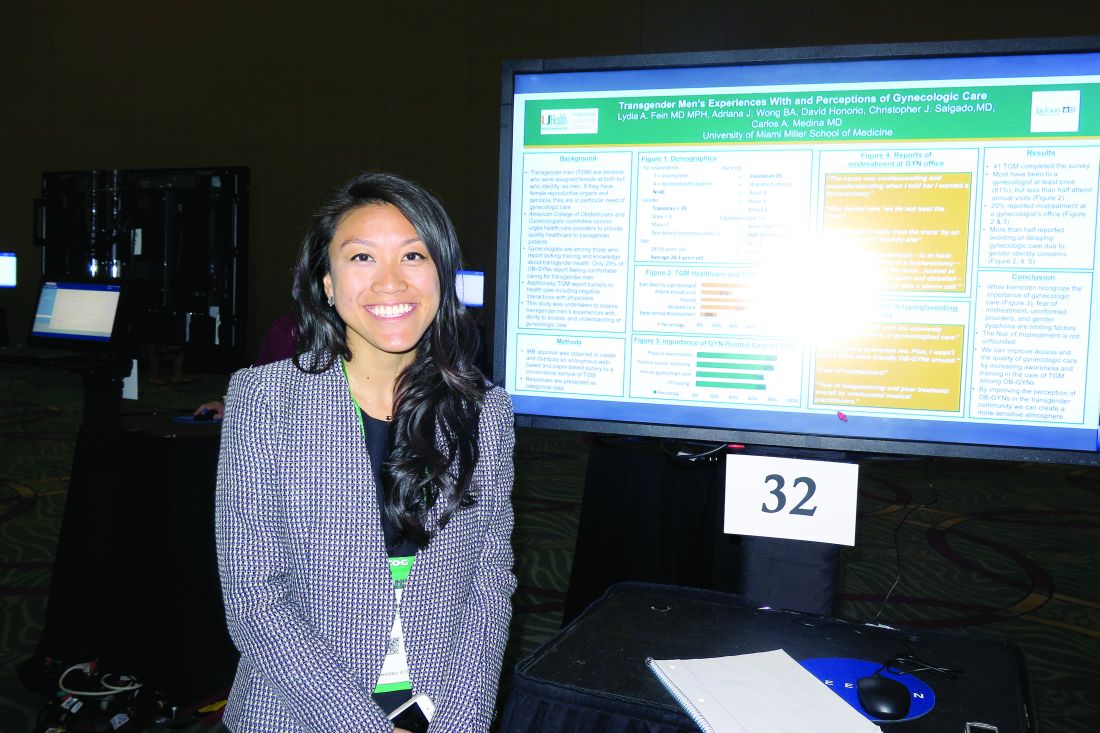
Survey highlights care gaps for transgender men
SAN DIEGO – Most transgender men have visited a gynecologist’s office at least once, but just 37% attend annual visits, results from a small survey showed.
“We’re seeing a large need and lack of access to gynecologic care,” Adriana J. Wong, the study author, said in an interview at the annual meeting of the American College of Obstetricians and Gynecologists. “Some barriers that we’ve identified are fear of mistreatment, a perceived lack of informed providers, and gender dysphoria.”
In an effort to assess transgender men’s experiences with, ability to access, and understanding of gynecologic care, Ms. Wong and her associates distributed an anonymous Web-based and paper-based survey to a convenience sample of transgender men in the Miami area. The mean age of the 41 respondents was 28 years, 56% were white, 41% had a high school diploma, 27% had a college degree, and 17% had a graduate degree.
The majority of survey participants (78%) reported having been to a gynecologist, 37% attended annual visits, 78% had health insurance, 56% delayed care because of gender identity concerns, and 20% experienced mistreatment at a gynecologist’s office.
Respondents reported delaying or avoiding care because they “felt uncomfortable with the extremely gendered experience of [gynecologic] care,” “fear of mistreatment,” and “my dysphoria prevented me. Plus, I wasn’t sure if there were friendly ob.gyns. around.”
“One of the most distinctive things to me is that we had a pretty well-insured population in our sample, and they were mostly Caucasian,” said Ms. Wong, a second-year medical student at the University of Miami. “Even though almost 80% were insured, [fewer] than 40% were receiving annual visits. This is the population that would potentially have the best possibility of receiving care, but they’re not seeking it out.”
The researchers reported having no relevant financial disclosures.
SAN DIEGO – Most transgender men have visited a gynecologist’s office at least once, but just 37% attend annual visits, results from a small survey showed.
“We’re seeing a large need and lack of access to gynecologic care,” Adriana J. Wong, the study author, said in an interview at the annual meeting of the American College of Obstetricians and Gynecologists. “Some barriers that we’ve identified are fear of mistreatment, a perceived lack of informed providers, and gender dysphoria.”
In an effort to assess transgender men’s experiences with, ability to access, and understanding of gynecologic care, Ms. Wong and her associates distributed an anonymous Web-based and paper-based survey to a convenience sample of transgender men in the Miami area. The mean age of the 41 respondents was 28 years, 56% were white, 41% had a high school diploma, 27% had a college degree, and 17% had a graduate degree.
The majority of survey participants (78%) reported having been to a gynecologist, 37% attended annual visits, 78% had health insurance, 56% delayed care because of gender identity concerns, and 20% experienced mistreatment at a gynecologist’s office.
Respondents reported delaying or avoiding care because they “felt uncomfortable with the extremely gendered experience of [gynecologic] care,” “fear of mistreatment,” and “my dysphoria prevented me. Plus, I wasn’t sure if there were friendly ob.gyns. around.”
“One of the most distinctive things to me is that we had a pretty well-insured population in our sample, and they were mostly Caucasian,” said Ms. Wong, a second-year medical student at the University of Miami. “Even though almost 80% were insured, [fewer] than 40% were receiving annual visits. This is the population that would potentially have the best possibility of receiving care, but they’re not seeking it out.”
The researchers reported having no relevant financial disclosures.
SAN DIEGO – Most transgender men have visited a gynecologist’s office at least once, but just 37% attend annual visits, results from a small survey showed.
“We’re seeing a large need and lack of access to gynecologic care,” Adriana J. Wong, the study author, said in an interview at the annual meeting of the American College of Obstetricians and Gynecologists. “Some barriers that we’ve identified are fear of mistreatment, a perceived lack of informed providers, and gender dysphoria.”
In an effort to assess transgender men’s experiences with, ability to access, and understanding of gynecologic care, Ms. Wong and her associates distributed an anonymous Web-based and paper-based survey to a convenience sample of transgender men in the Miami area. The mean age of the 41 respondents was 28 years, 56% were white, 41% had a high school diploma, 27% had a college degree, and 17% had a graduate degree.
The majority of survey participants (78%) reported having been to a gynecologist, 37% attended annual visits, 78% had health insurance, 56% delayed care because of gender identity concerns, and 20% experienced mistreatment at a gynecologist’s office.
Respondents reported delaying or avoiding care because they “felt uncomfortable with the extremely gendered experience of [gynecologic] care,” “fear of mistreatment,” and “my dysphoria prevented me. Plus, I wasn’t sure if there were friendly ob.gyns. around.”
“One of the most distinctive things to me is that we had a pretty well-insured population in our sample, and they were mostly Caucasian,” said Ms. Wong, a second-year medical student at the University of Miami. “Even though almost 80% were insured, [fewer] than 40% were receiving annual visits. This is the population that would potentially have the best possibility of receiving care, but they’re not seeking it out.”
The researchers reported having no relevant financial disclosures.
AT ACOG 2017
Key clinical point:
Major finding: Most transgender men (78%) have been to a gynecologist at least once, but just 37% attend annual visits.
Data source: Responses from a survey of 41 transgender men in the Miami area.
Disclosures: The researchers reported having no relevant financial disclosures.
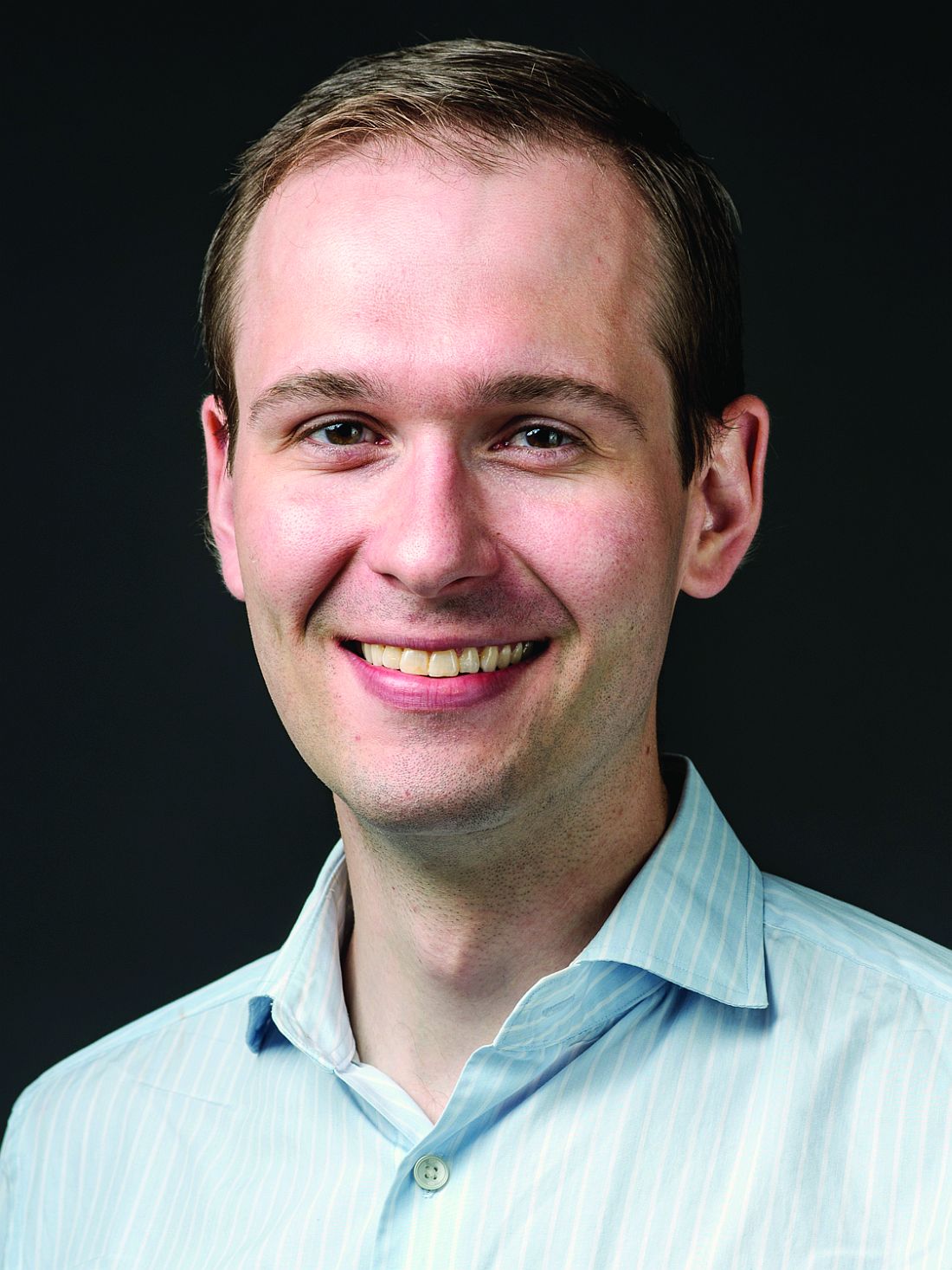
Using telemedicine to improve maternal safety
SAN DIEGO – Utah hospitals reported improved implementation of an obstetrics hemorrhage bundle following a series of teleconferencing sessions.
“There is an increasing body of evidence to support the use of protocols and bundles in obstetrics to improve outcomes for pregnant women and their babies,” Brett D. Einerson, MD, MPH, lead study author, said in an interview. “In Utah and throughout the Mountain West, we face the unique challenge of disseminating information and education on the latest evidence-based treatments to smaller rural hospitals that still need to be prepared for events like severe postpartum hemorrhage but do not have the volume, or sometime the resources, to be adequately prepared.”
“Telehealth allowed us to reach providers who otherwise could not travel the distance to attend frequent training sessions and gave the whole state access to expertise at the region’s large tertiary care hospitals,” Dr. Einerson said. “As far as we know, this is one of the first uses of telehealth as a tool for disseminating patient safety and quality improvement education for health care providers on a statewide scale.”
Dr. Einerson and his associates invited all Utah hospitals to participate in the Obstetric Hemorrhage Collaborative, an evidence-based educational program aimed at facilitating implementation of the obstetric hemorrhage bundle. The program involved two in-person training meetings and twice-monthly teleconferencing with expert mentorship over 6 months. In-person sessions consisted of hands-on training and strategy building, while telehealth sessions were led by regional and national leaders in the field of obstetric hemorrhage.
A statewide self-assessment survey of 38 bundle elements was administered before initiation of the project and after completion. The researchers used modified Likert scales to describe participant responses. Means and proportions were compared before and after the training.
Of Utah’s obstetric hospitals, representing every hospital system in the state, 27 (61%) completed the needs-assessment survey, and 15 (34%) participated in the Obstetric Hemorrhage Collaborative, which included four bundle domains:
- Recognition and Prevention: Conducting a risk assessment and active management of the Third Stage of labor.
- Response: Creating a checklist and a rapid response team.
- Readiness: Establishing a blood bank, hemorrhage cart, and conducting simulation/team drills.
- Reporting and Learning: Fostering a culture of debriefing, conducting a multidisciplinary review, and measuring outcomes and processes.
Hospitals reported implementation, or progress toward implementation, of significantly more elements of the bundle after the educational program, compared with before the collaborative (a mean of 33.3 vs. 19 bundle elements; P less than 0.001). Hospitals reported increased implementation of elements in all four bundle domains. All participants (100%) reported that teleconferencing sessions were “very helpful,” and 14 (93%) said that they were “very satisfied” with the collaborative.
“Hospitals in the state of Utah generally had the right tools to treat and prevent obstetric hemorrhage but did not have the systems in place to be sure that the tools were used correctly,” Dr. Einerson said. “For instance, 80% of hospitals had access to a cart with supplies for treating bleeding, but less than 15% were systematically measuring blood loss after delivery. What surprised me most, however, was that most hospitals did not track their rates of postpartum bleeding. In my mind, you can’t set goals for treatment until you know how good – or bad – you are doing. Knowing your baseline rate of outcomes can help set goals and measure progress toward achieving them. Before training, less than 50% of Utah hospitals knew their own rate of hemorrhage, but all participating hospitals reported tracking their rates after the intervention.”
He acknowledged certain limitations of the study, including the fact that it did not measure obstetric outcomes. “We are in the process of measuring the effectiveness of our telehealth intervention by monitoring hemorrhage rates and complications over time,” Dr. Einerson said. “This survey of participants in the statewide telehealth bundle program is the first step.”
Dr. Einerson reported having no financial disclosures.
SAN DIEGO – Utah hospitals reported improved implementation of an obstetrics hemorrhage bundle following a series of teleconferencing sessions.
“There is an increasing body of evidence to support the use of protocols and bundles in obstetrics to improve outcomes for pregnant women and their babies,” Brett D. Einerson, MD, MPH, lead study author, said in an interview. “In Utah and throughout the Mountain West, we face the unique challenge of disseminating information and education on the latest evidence-based treatments to smaller rural hospitals that still need to be prepared for events like severe postpartum hemorrhage but do not have the volume, or sometime the resources, to be adequately prepared.”
“Telehealth allowed us to reach providers who otherwise could not travel the distance to attend frequent training sessions and gave the whole state access to expertise at the region’s large tertiary care hospitals,” Dr. Einerson said. “As far as we know, this is one of the first uses of telehealth as a tool for disseminating patient safety and quality improvement education for health care providers on a statewide scale.”
Dr. Einerson and his associates invited all Utah hospitals to participate in the Obstetric Hemorrhage Collaborative, an evidence-based educational program aimed at facilitating implementation of the obstetric hemorrhage bundle. The program involved two in-person training meetings and twice-monthly teleconferencing with expert mentorship over 6 months. In-person sessions consisted of hands-on training and strategy building, while telehealth sessions were led by regional and national leaders in the field of obstetric hemorrhage.
A statewide self-assessment survey of 38 bundle elements was administered before initiation of the project and after completion. The researchers used modified Likert scales to describe participant responses. Means and proportions were compared before and after the training.
Of Utah’s obstetric hospitals, representing every hospital system in the state, 27 (61%) completed the needs-assessment survey, and 15 (34%) participated in the Obstetric Hemorrhage Collaborative, which included four bundle domains:
- Recognition and Prevention: Conducting a risk assessment and active management of the Third Stage of labor.
- Response: Creating a checklist and a rapid response team.
- Readiness: Establishing a blood bank, hemorrhage cart, and conducting simulation/team drills.
- Reporting and Learning: Fostering a culture of debriefing, conducting a multidisciplinary review, and measuring outcomes and processes.
Hospitals reported implementation, or progress toward implementation, of significantly more elements of the bundle after the educational program, compared with before the collaborative (a mean of 33.3 vs. 19 bundle elements; P less than 0.001). Hospitals reported increased implementation of elements in all four bundle domains. All participants (100%) reported that teleconferencing sessions were “very helpful,” and 14 (93%) said that they were “very satisfied” with the collaborative.
“Hospitals in the state of Utah generally had the right tools to treat and prevent obstetric hemorrhage but did not have the systems in place to be sure that the tools were used correctly,” Dr. Einerson said. “For instance, 80% of hospitals had access to a cart with supplies for treating bleeding, but less than 15% were systematically measuring blood loss after delivery. What surprised me most, however, was that most hospitals did not track their rates of postpartum bleeding. In my mind, you can’t set goals for treatment until you know how good – or bad – you are doing. Knowing your baseline rate of outcomes can help set goals and measure progress toward achieving them. Before training, less than 50% of Utah hospitals knew their own rate of hemorrhage, but all participating hospitals reported tracking their rates after the intervention.”
He acknowledged certain limitations of the study, including the fact that it did not measure obstetric outcomes. “We are in the process of measuring the effectiveness of our telehealth intervention by monitoring hemorrhage rates and complications over time,” Dr. Einerson said. “This survey of participants in the statewide telehealth bundle program is the first step.”
Dr. Einerson reported having no financial disclosures.
SAN DIEGO – Utah hospitals reported improved implementation of an obstetrics hemorrhage bundle following a series of teleconferencing sessions.
“There is an increasing body of evidence to support the use of protocols and bundles in obstetrics to improve outcomes for pregnant women and their babies,” Brett D. Einerson, MD, MPH, lead study author, said in an interview. “In Utah and throughout the Mountain West, we face the unique challenge of disseminating information and education on the latest evidence-based treatments to smaller rural hospitals that still need to be prepared for events like severe postpartum hemorrhage but do not have the volume, or sometime the resources, to be adequately prepared.”
“Telehealth allowed us to reach providers who otherwise could not travel the distance to attend frequent training sessions and gave the whole state access to expertise at the region’s large tertiary care hospitals,” Dr. Einerson said. “As far as we know, this is one of the first uses of telehealth as a tool for disseminating patient safety and quality improvement education for health care providers on a statewide scale.”
Dr. Einerson and his associates invited all Utah hospitals to participate in the Obstetric Hemorrhage Collaborative, an evidence-based educational program aimed at facilitating implementation of the obstetric hemorrhage bundle. The program involved two in-person training meetings and twice-monthly teleconferencing with expert mentorship over 6 months. In-person sessions consisted of hands-on training and strategy building, while telehealth sessions were led by regional and national leaders in the field of obstetric hemorrhage.
A statewide self-assessment survey of 38 bundle elements was administered before initiation of the project and after completion. The researchers used modified Likert scales to describe participant responses. Means and proportions were compared before and after the training.
Of Utah’s obstetric hospitals, representing every hospital system in the state, 27 (61%) completed the needs-assessment survey, and 15 (34%) participated in the Obstetric Hemorrhage Collaborative, which included four bundle domains:
- Recognition and Prevention: Conducting a risk assessment and active management of the Third Stage of labor.
- Response: Creating a checklist and a rapid response team.
- Readiness: Establishing a blood bank, hemorrhage cart, and conducting simulation/team drills.
- Reporting and Learning: Fostering a culture of debriefing, conducting a multidisciplinary review, and measuring outcomes and processes.
Hospitals reported implementation, or progress toward implementation, of significantly more elements of the bundle after the educational program, compared with before the collaborative (a mean of 33.3 vs. 19 bundle elements; P less than 0.001). Hospitals reported increased implementation of elements in all four bundle domains. All participants (100%) reported that teleconferencing sessions were “very helpful,” and 14 (93%) said that they were “very satisfied” with the collaborative.
“Hospitals in the state of Utah generally had the right tools to treat and prevent obstetric hemorrhage but did not have the systems in place to be sure that the tools were used correctly,” Dr. Einerson said. “For instance, 80% of hospitals had access to a cart with supplies for treating bleeding, but less than 15% were systematically measuring blood loss after delivery. What surprised me most, however, was that most hospitals did not track their rates of postpartum bleeding. In my mind, you can’t set goals for treatment until you know how good – or bad – you are doing. Knowing your baseline rate of outcomes can help set goals and measure progress toward achieving them. Before training, less than 50% of Utah hospitals knew their own rate of hemorrhage, but all participating hospitals reported tracking their rates after the intervention.”
He acknowledged certain limitations of the study, including the fact that it did not measure obstetric outcomes. “We are in the process of measuring the effectiveness of our telehealth intervention by monitoring hemorrhage rates and complications over time,” Dr. Einerson said. “This survey of participants in the statewide telehealth bundle program is the first step.”
Dr. Einerson reported having no financial disclosures.
AT ACOG 2017
Key clinical point:
Major finding: Hospitals reported implementation, or progress toward implementation, of significantly more elements of the bundle after the educational program, compared with before the collaborative (a mean of 33.3 vs. 19 bundle elements; P less than 0.001).
Data source: Results from 15 Utah hospitals that participated in the Obstetric Hemorrhage Collaborative.
Disclosures: The researchers reported having no financial disclosures.
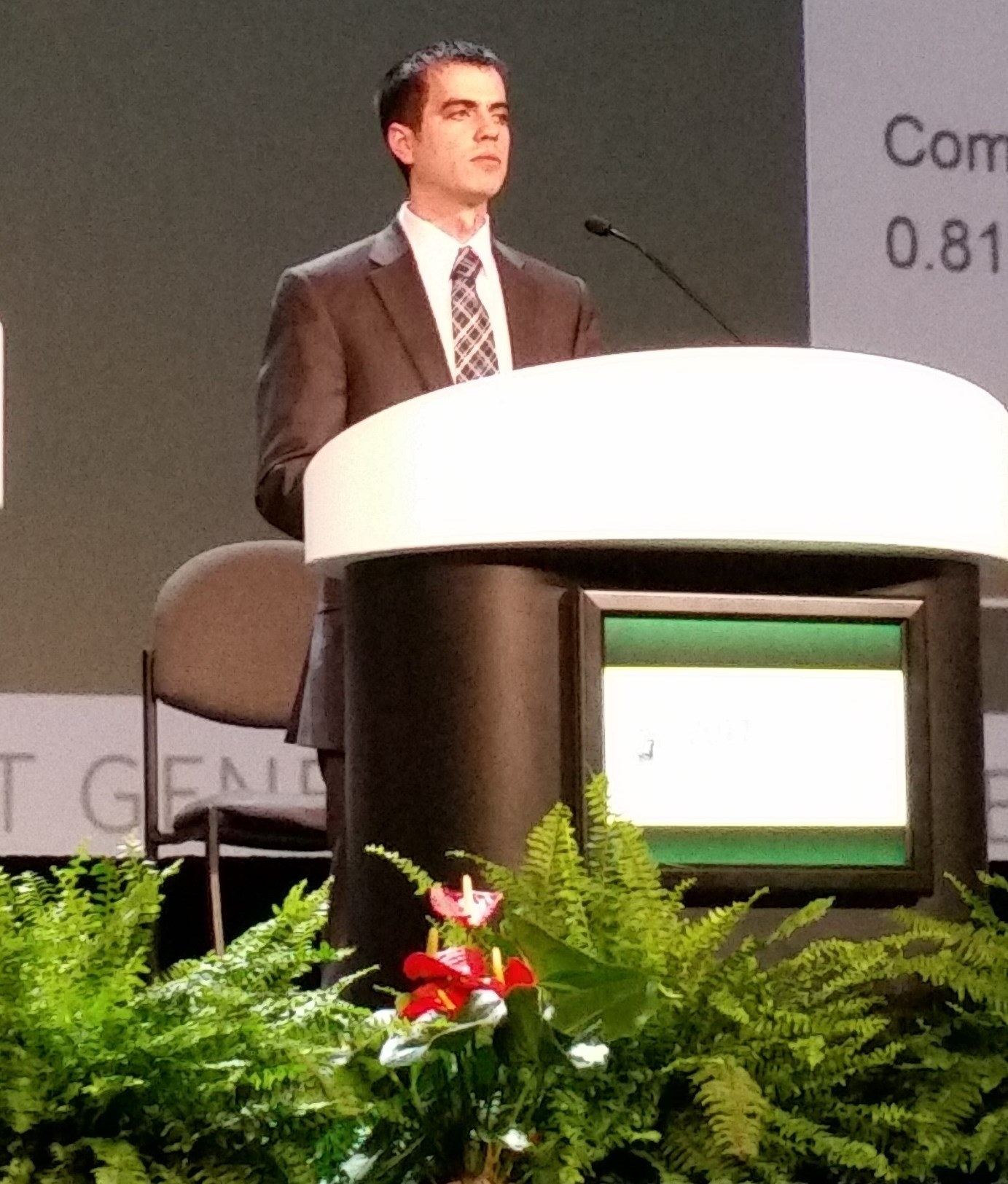
More than one-third of genetic tests misordered, study finds
SAN DIEGO – A review of genetic tests ordered during a 3-month period found that more than one-third were misordered, leading to more than $20,000 in unnecessary health care costs, results from a single-center quality improvement project showed.
“We know there is an ever-expanding number of genetic tests available for clinicians to order, and there is more direct marketing to the patient,” Kathleen Ruzzo, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “It can be difficult to stay on top of that as we have so many different clinical responsibilities.”
Of genetic tests ordered for the 114 patients, 44 (39%) were deemed to be misordered based on published clinical practice guidelines. Of the rest, 24 tests were misordered/not indicated, 8 tests were misordered/false reassurance, and 12 tests were misordered/inadequate.
The costs of ordered genetic testing totaled approximately $75,000, while the cost of recommended testing following the chart review was approximately $54,000, a difference of more than $20,000.
When Dr. Ruzzo shared results of the study with her colleagues at Naval Medical Center San Diego, “I think it opened a lot of people’s eyes … to be more meticulous about [genetic] testing and to ask for help when you need help,” she said. “Having trained individuals, reviewing genetic tests could save money in the health care system more broadly. We could also approve the appropriate testing for the patient.”
She acknowledged certain limitations of the study, including the fact that it “reviewed a very narrow scope of [genetic] tests for a short amount of time, so we think we underestimated the appropriate health care expenditures. Additionally, we didn’t focus on the clinical ramifications of the misordering for patients.”
Study coauthor Monica A. Lutgendorf, MD, a maternal-fetal medicine physician at the medical center, characterized the study findings as “a call to action in general for ob.gyns. to get additional training and resources to handle the ever-expanding number of [genetic] tests,” she said. “I don’t think that this is unique to any specific institution. I think this is part of the new environment of practice that we’re in.”
Physicians can learn more about genetic testing from ACOG and from the Perinatal Quality Foundation, Dr. Lutgendorf said. The study won first prize among oral abstracts presented at the ACOG meeting. The researchers reported having no financial disclosures.
SAN DIEGO – A review of genetic tests ordered during a 3-month period found that more than one-third were misordered, leading to more than $20,000 in unnecessary health care costs, results from a single-center quality improvement project showed.
“We know there is an ever-expanding number of genetic tests available for clinicians to order, and there is more direct marketing to the patient,” Kathleen Ruzzo, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “It can be difficult to stay on top of that as we have so many different clinical responsibilities.”
Of genetic tests ordered for the 114 patients, 44 (39%) were deemed to be misordered based on published clinical practice guidelines. Of the rest, 24 tests were misordered/not indicated, 8 tests were misordered/false reassurance, and 12 tests were misordered/inadequate.
The costs of ordered genetic testing totaled approximately $75,000, while the cost of recommended testing following the chart review was approximately $54,000, a difference of more than $20,000.
When Dr. Ruzzo shared results of the study with her colleagues at Naval Medical Center San Diego, “I think it opened a lot of people’s eyes … to be more meticulous about [genetic] testing and to ask for help when you need help,” she said. “Having trained individuals, reviewing genetic tests could save money in the health care system more broadly. We could also approve the appropriate testing for the patient.”
She acknowledged certain limitations of the study, including the fact that it “reviewed a very narrow scope of [genetic] tests for a short amount of time, so we think we underestimated the appropriate health care expenditures. Additionally, we didn’t focus on the clinical ramifications of the misordering for patients.”
Study coauthor Monica A. Lutgendorf, MD, a maternal-fetal medicine physician at the medical center, characterized the study findings as “a call to action in general for ob.gyns. to get additional training and resources to handle the ever-expanding number of [genetic] tests,” she said. “I don’t think that this is unique to any specific institution. I think this is part of the new environment of practice that we’re in.”
Physicians can learn more about genetic testing from ACOG and from the Perinatal Quality Foundation, Dr. Lutgendorf said. The study won first prize among oral abstracts presented at the ACOG meeting. The researchers reported having no financial disclosures.
SAN DIEGO – A review of genetic tests ordered during a 3-month period found that more than one-third were misordered, leading to more than $20,000 in unnecessary health care costs, results from a single-center quality improvement project showed.
“We know there is an ever-expanding number of genetic tests available for clinicians to order, and there is more direct marketing to the patient,” Kathleen Ruzzo, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “It can be difficult to stay on top of that as we have so many different clinical responsibilities.”
Of genetic tests ordered for the 114 patients, 44 (39%) were deemed to be misordered based on published clinical practice guidelines. Of the rest, 24 tests were misordered/not indicated, 8 tests were misordered/false reassurance, and 12 tests were misordered/inadequate.
The costs of ordered genetic testing totaled approximately $75,000, while the cost of recommended testing following the chart review was approximately $54,000, a difference of more than $20,000.
When Dr. Ruzzo shared results of the study with her colleagues at Naval Medical Center San Diego, “I think it opened a lot of people’s eyes … to be more meticulous about [genetic] testing and to ask for help when you need help,” she said. “Having trained individuals, reviewing genetic tests could save money in the health care system more broadly. We could also approve the appropriate testing for the patient.”
She acknowledged certain limitations of the study, including the fact that it “reviewed a very narrow scope of [genetic] tests for a short amount of time, so we think we underestimated the appropriate health care expenditures. Additionally, we didn’t focus on the clinical ramifications of the misordering for patients.”
Study coauthor Monica A. Lutgendorf, MD, a maternal-fetal medicine physician at the medical center, characterized the study findings as “a call to action in general for ob.gyns. to get additional training and resources to handle the ever-expanding number of [genetic] tests,” she said. “I don’t think that this is unique to any specific institution. I think this is part of the new environment of practice that we’re in.”
Physicians can learn more about genetic testing from ACOG and from the Perinatal Quality Foundation, Dr. Lutgendorf said. The study won first prize among oral abstracts presented at the ACOG meeting. The researchers reported having no financial disclosures.
AT ACOG 2017
Key clinical point:
Major finding: Of genetic tests ordered by clinicians, 39% were deemed to be misordered.
Data source: A review of 114 genetic tests ordered over a 3-month period at a single center.
Disclosures: The researchers reported having no financial disclosures.
Changing gloves before closure cut wound-related cesarean complications
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
SAN DIEGO – Changing gloves before closure during cesarean deliveries can reduce overall wound morbidity, a study showed.
Glove changing during the study had a number needed to treat (NNT) of 14 to see benefit, no demonstrated risk, and a total cost per procedure of about $5.
Researchers led by Buvana Reddy, MD, an ob.gyn. in group practice in Woodbury, Minn., used a randomized trial design to determine whether donning a fresh pair of gloves makes a difference in the rate of surgical complications during cesarean delivery. .
Just one previous study had shown a reduced wound infection rate when gloves were changed after placental delivery (J Reprod Med. 2004 Jan;49[1]:13-6). The study showed a statistically significant drop in wound infections, but Dr. Scrafford said that the sample size was small, and the point at which glove changing was performed is not very practical in terms of the flow of surgery.
Building on this study, Dr. Scrafford and his colleagues designed a trial that was meant to be larger, incorporated a composite wound outcome score rather than just focusing strictly on infection, and switched the timing of glove change to just before abdominal closure.
The randomized controlled trial included all women who underwent nonemergent cesarean delivery at the investigators’ home facility during a 15-month period. The patient allocation was not known until the presurgical “time-out.” Patients allocated to the control condition did not have any change in operative procedures; the surgical team of patients allocated to the intervention arm changed their outer gloves immediately before peritoneal or fascial closure.
The composite primary outcome measure assessed wound seroma, hematoma, or dehiscence (defined as a separation of at least 1 cm), as well as wound infection and any other wound abnormality. Secondary outcome measures included whether patients had a fever or peri-incisional cellulitis.
A total of 553 patients were randomized. Follow-up was high, so Dr. Scrafford and his colleagues were able to analyze data from a total of 250 patients in the control arm and 236 patients who received the glove-changing intervention.
Patient demographics and comorbidities were similar between groups, as was the surgical time and estimated blood loss. Dr. Scrafford noted that significantly more patients in the glove-changing group than in the control group received presurgical vaginal preparation with antiseptic solution (20.3% vs. 10.5%; P = .001). However, he reported, statistical analysis showed that this difference had no effect on the results.
Overall, 15 (6.4%) of the patients in the glove-changing group met the criteria for wound complication, compared with 34 (13.6%) in the control group (P = .008). Of the individual components of the primary outcome measure, the difference in incidence of skin separation was also significant; separation was experienced by five patients (2.1%) in the glove-changing group, compared with 14 (5.6%) in the control group (P = .01).
The rate of wound infections was numerically lower in the intervention group, compared with the control group (8 vs. 14), but the difference was not statistically significant.
There were no significant differences between the groups when secondary outcomes were analyzed, Dr. Scrafford said.
The lack of block randomization in the study left open the potential for historical bias, Dr. Scrafford said. Since surgeons couldn’t be blinded as to study arm, the potential for observer bias also existed. Still, he said, the study’s strengths included its large size, and the real-world applicability of the broad inclusion criteria and diverse patient population.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: The number needed to treat to see benefit from glove changing was 14; the cost per procedure was about $5.
Data source: A randomized controlled trial of 553 patients undergoing nonemergent cesarean delivery.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Endometrial cancer rates increased following WHI
SAN DIEGO – Endometrial cancer (EC) rates increased after 2002, coinciding with the release of results from the Women’s Health Initiative and including a 10% spike between 2006 and 2014, according to a large analysis of national data.
“Be aware of an increase of endometrial cancer and, whenever possible, look to minimize possible inciting causes,” Ginger Constantine, MD, lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Be certain that the hormonal products that patients are taking are delivering adequate progesterone to the endometrium in those patients at an increased risk of endometrial cancer, such as those with unopposed estrogen.”
“We sought to look at possible causes for the increase of the known risk factors for EC,” she said. “What has changed in the years leading up to 2006?” To find out, she and her associates obtained EC incidence from the Surveillance, Epidemiology, and End Result Program database from 1975 through 2014. They evaluated the incidence of risk factors thought to be associated with EC, including age, obesity, race, number of menstrual cycles, gravidity and parity, metabolic syndromes, diet and exercise, and medications, including various types of hormone therapy, tamoxifen, and hormonal contraceptives.
Shelli Graham, PhD, vice president of medical affairs for Boca Raton, Florida–based TherapeuticsMD, presented the study findings on behalf of Dr. Constantine, who was unable to attend the meeting. The rates of EC were relatively constant from 1992 to 2002 (at about 76/100,000 cases per year) but have increased 2.5% annually, with a 10% increase from 2006 to 2014, especially in women aged 55-64 years.
Use of estrogen and progestin combinations have decreased while risk factors remained constant or decreased during the same time period. However, the researchers observed a “huge increase (of 1-2.5 million U.S. women) using non-FDA approved compounded estrogen and estrogen and progesterone, which may not provide adequate endometrial protection from estrogen, a known cause of EC,” Dr. Constantine said. “Additionally, there is less progestin use subsequent to the [Women’s Health Initiative] and it is known that progestin is protective on the endometrium.”
The researchers also examined the incidence of obesity – another known risk factor for EC – and found that, although obesity has continued to increase in incidence, “it does not appear to be increasing at the same rate as EC, so [it] does not appear to be enough to explain the increase in EC from 2006,” Dr. Constantine said. “I was surprised at the rate of increase of EC from 2006 to 2014 and have also been surprised by the amount of non-FDA compounded hormone use.”
Dr. Graham characterized the increase in EC incidence as “a public health concern that is most likely multifactorial in etiology.” Contributors, she said, include the combination of an increase in obesity with an inherent increase in endogenous estrogen, decreasing progesterone use from a decrease in the use of FDA-approved hormone therapy products, and an increase in compounded hormone therapy that may not deliver adequate endometrial protection.
Dr. Constantine acknowledged certain limitations of the study, including the fact that it is “an ecological analysis, not a randomized clinical trial. It is hypothesis-generating.”
Dr. Constantine reported that she is a consultant/advisory member for TherapeuticsMD and other pharmaceutical companies. She owns stock in TherapeuticsMD. Coauthor Steven R. Goldstein, MD, reported having numerous financial relationships with pharmaceutical companies including TherapeuticsMD. Dr. Graham is an employee of TherapeuticsMD.
SAN DIEGO – Endometrial cancer (EC) rates increased after 2002, coinciding with the release of results from the Women’s Health Initiative and including a 10% spike between 2006 and 2014, according to a large analysis of national data.
“Be aware of an increase of endometrial cancer and, whenever possible, look to minimize possible inciting causes,” Ginger Constantine, MD, lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Be certain that the hormonal products that patients are taking are delivering adequate progesterone to the endometrium in those patients at an increased risk of endometrial cancer, such as those with unopposed estrogen.”
“We sought to look at possible causes for the increase of the known risk factors for EC,” she said. “What has changed in the years leading up to 2006?” To find out, she and her associates obtained EC incidence from the Surveillance, Epidemiology, and End Result Program database from 1975 through 2014. They evaluated the incidence of risk factors thought to be associated with EC, including age, obesity, race, number of menstrual cycles, gravidity and parity, metabolic syndromes, diet and exercise, and medications, including various types of hormone therapy, tamoxifen, and hormonal contraceptives.
Shelli Graham, PhD, vice president of medical affairs for Boca Raton, Florida–based TherapeuticsMD, presented the study findings on behalf of Dr. Constantine, who was unable to attend the meeting. The rates of EC were relatively constant from 1992 to 2002 (at about 76/100,000 cases per year) but have increased 2.5% annually, with a 10% increase from 2006 to 2014, especially in women aged 55-64 years.
Use of estrogen and progestin combinations have decreased while risk factors remained constant or decreased during the same time period. However, the researchers observed a “huge increase (of 1-2.5 million U.S. women) using non-FDA approved compounded estrogen and estrogen and progesterone, which may not provide adequate endometrial protection from estrogen, a known cause of EC,” Dr. Constantine said. “Additionally, there is less progestin use subsequent to the [Women’s Health Initiative] and it is known that progestin is protective on the endometrium.”
The researchers also examined the incidence of obesity – another known risk factor for EC – and found that, although obesity has continued to increase in incidence, “it does not appear to be increasing at the same rate as EC, so [it] does not appear to be enough to explain the increase in EC from 2006,” Dr. Constantine said. “I was surprised at the rate of increase of EC from 2006 to 2014 and have also been surprised by the amount of non-FDA compounded hormone use.”
Dr. Graham characterized the increase in EC incidence as “a public health concern that is most likely multifactorial in etiology.” Contributors, she said, include the combination of an increase in obesity with an inherent increase in endogenous estrogen, decreasing progesterone use from a decrease in the use of FDA-approved hormone therapy products, and an increase in compounded hormone therapy that may not deliver adequate endometrial protection.
Dr. Constantine acknowledged certain limitations of the study, including the fact that it is “an ecological analysis, not a randomized clinical trial. It is hypothesis-generating.”
Dr. Constantine reported that she is a consultant/advisory member for TherapeuticsMD and other pharmaceutical companies. She owns stock in TherapeuticsMD. Coauthor Steven R. Goldstein, MD, reported having numerous financial relationships with pharmaceutical companies including TherapeuticsMD. Dr. Graham is an employee of TherapeuticsMD.
SAN DIEGO – Endometrial cancer (EC) rates increased after 2002, coinciding with the release of results from the Women’s Health Initiative and including a 10% spike between 2006 and 2014, according to a large analysis of national data.
“Be aware of an increase of endometrial cancer and, whenever possible, look to minimize possible inciting causes,” Ginger Constantine, MD, lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Be certain that the hormonal products that patients are taking are delivering adequate progesterone to the endometrium in those patients at an increased risk of endometrial cancer, such as those with unopposed estrogen.”
“We sought to look at possible causes for the increase of the known risk factors for EC,” she said. “What has changed in the years leading up to 2006?” To find out, she and her associates obtained EC incidence from the Surveillance, Epidemiology, and End Result Program database from 1975 through 2014. They evaluated the incidence of risk factors thought to be associated with EC, including age, obesity, race, number of menstrual cycles, gravidity and parity, metabolic syndromes, diet and exercise, and medications, including various types of hormone therapy, tamoxifen, and hormonal contraceptives.
Shelli Graham, PhD, vice president of medical affairs for Boca Raton, Florida–based TherapeuticsMD, presented the study findings on behalf of Dr. Constantine, who was unable to attend the meeting. The rates of EC were relatively constant from 1992 to 2002 (at about 76/100,000 cases per year) but have increased 2.5% annually, with a 10% increase from 2006 to 2014, especially in women aged 55-64 years.
Use of estrogen and progestin combinations have decreased while risk factors remained constant or decreased during the same time period. However, the researchers observed a “huge increase (of 1-2.5 million U.S. women) using non-FDA approved compounded estrogen and estrogen and progesterone, which may not provide adequate endometrial protection from estrogen, a known cause of EC,” Dr. Constantine said. “Additionally, there is less progestin use subsequent to the [Women’s Health Initiative] and it is known that progestin is protective on the endometrium.”
The researchers also examined the incidence of obesity – another known risk factor for EC – and found that, although obesity has continued to increase in incidence, “it does not appear to be increasing at the same rate as EC, so [it] does not appear to be enough to explain the increase in EC from 2006,” Dr. Constantine said. “I was surprised at the rate of increase of EC from 2006 to 2014 and have also been surprised by the amount of non-FDA compounded hormone use.”
Dr. Graham characterized the increase in EC incidence as “a public health concern that is most likely multifactorial in etiology.” Contributors, she said, include the combination of an increase in obesity with an inherent increase in endogenous estrogen, decreasing progesterone use from a decrease in the use of FDA-approved hormone therapy products, and an increase in compounded hormone therapy that may not deliver adequate endometrial protection.
Dr. Constantine acknowledged certain limitations of the study, including the fact that it is “an ecological analysis, not a randomized clinical trial. It is hypothesis-generating.”
Dr. Constantine reported that she is a consultant/advisory member for TherapeuticsMD and other pharmaceutical companies. She owns stock in TherapeuticsMD. Coauthor Steven R. Goldstein, MD, reported having numerous financial relationships with pharmaceutical companies including TherapeuticsMD. Dr. Graham is an employee of TherapeuticsMD.
Key clinical point:
Major finding: Rates of endometrial cancer increased 10% between 2006 and 2014.
Data source: An analysis of the Surveillance, Epidemiology, and End Result Program database.
Disclosures: Dr. Constantine reported that she is a consultant/advisory board member for TherapeuticsMD as well as other pharmaceutical companies. She also owns stock in TherapeuticsMD. Coauthor Steven R. Goldstein, MD, reported having numerous financial relationships with pharmaceutical companies including TherapeuticsMD. Dr. Graham is an employee of TherapeuticsMD.
Beware hormonal IUD expulsion in obese women
SAN DIEGO – Obese women with a body mass index of 40 or greater are more likely to experience expulsion of levonorgestrel IUDs than women with lower BMI, according to findings from a retrospective cohort study.
Women with class III obesity (a BMI of 40 or greater) had a 3.06-times higher odds of expulsion (95% confidence interval, 1.69-5.57) with a levonorgestrel IUD, compared with a control group of women with a BMI of less than 35, Lynne Saito-Tom, MD, of the University of Hawaii at Manoa, Honolulu, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Saito-Tom and her colleagues looked at other potential IUD complications, including infection, perforation, and pregnancy. Women with class III obesity also had a higher rate of all complications combined at 24%, compared with 10% among women with class I obesity.
Although complications were higher for more severely obese women, there were no differences between BMI groups in difficulty with insertion (P = .59) or 12-month continuation (P = .69).
The study was unique because it included a diverse ethnic population, with 36% Native Hawaiian/Pacific Islander women and 31% Asian women.
The study wasn’t powered to identify the reasons for greater expulsion in obese women, but some theories include that the IUD could be more difficult to place in larger women without adequate instrumentation or exam tables. Women with class III obesity also tend to have higher rates of heavy menstrual bleeding, which could be driving expulsion, Dr. Saito-Tom said.
However, the results should not deter physicians from placing hormonal IUD in these women, she said. While the expulsion rate was higher than seen generally, it is still an effective method for most obese women. “That’s much more beneficial than discouraging patients,” Dr. Saito-Tom said.
Physicians should continue to educate patients about the benefits of long-acting reversible contraceptives and encourage all patients to utilize them, regardless of their weight, she said.
Dr. Saito-Tom reported having no relevant financial disclosures. One of her colleagues reported grant support from Merck and being a consultant for UpToDate.
[email protected]
On Twitter @maryellenny
SAN DIEGO – Obese women with a body mass index of 40 or greater are more likely to experience expulsion of levonorgestrel IUDs than women with lower BMI, according to findings from a retrospective cohort study.
Women with class III obesity (a BMI of 40 or greater) had a 3.06-times higher odds of expulsion (95% confidence interval, 1.69-5.57) with a levonorgestrel IUD, compared with a control group of women with a BMI of less than 35, Lynne Saito-Tom, MD, of the University of Hawaii at Manoa, Honolulu, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Saito-Tom and her colleagues looked at other potential IUD complications, including infection, perforation, and pregnancy. Women with class III obesity also had a higher rate of all complications combined at 24%, compared with 10% among women with class I obesity.
Although complications were higher for more severely obese women, there were no differences between BMI groups in difficulty with insertion (P = .59) or 12-month continuation (P = .69).
The study was unique because it included a diverse ethnic population, with 36% Native Hawaiian/Pacific Islander women and 31% Asian women.
The study wasn’t powered to identify the reasons for greater expulsion in obese women, but some theories include that the IUD could be more difficult to place in larger women without adequate instrumentation or exam tables. Women with class III obesity also tend to have higher rates of heavy menstrual bleeding, which could be driving expulsion, Dr. Saito-Tom said.
However, the results should not deter physicians from placing hormonal IUD in these women, she said. While the expulsion rate was higher than seen generally, it is still an effective method for most obese women. “That’s much more beneficial than discouraging patients,” Dr. Saito-Tom said.
Physicians should continue to educate patients about the benefits of long-acting reversible contraceptives and encourage all patients to utilize them, regardless of their weight, she said.
Dr. Saito-Tom reported having no relevant financial disclosures. One of her colleagues reported grant support from Merck and being a consultant for UpToDate.
[email protected]
On Twitter @maryellenny
SAN DIEGO – Obese women with a body mass index of 40 or greater are more likely to experience expulsion of levonorgestrel IUDs than women with lower BMI, according to findings from a retrospective cohort study.
Women with class III obesity (a BMI of 40 or greater) had a 3.06-times higher odds of expulsion (95% confidence interval, 1.69-5.57) with a levonorgestrel IUD, compared with a control group of women with a BMI of less than 35, Lynne Saito-Tom, MD, of the University of Hawaii at Manoa, Honolulu, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Saito-Tom and her colleagues looked at other potential IUD complications, including infection, perforation, and pregnancy. Women with class III obesity also had a higher rate of all complications combined at 24%, compared with 10% among women with class I obesity.
Although complications were higher for more severely obese women, there were no differences between BMI groups in difficulty with insertion (P = .59) or 12-month continuation (P = .69).
The study was unique because it included a diverse ethnic population, with 36% Native Hawaiian/Pacific Islander women and 31% Asian women.
The study wasn’t powered to identify the reasons for greater expulsion in obese women, but some theories include that the IUD could be more difficult to place in larger women without adequate instrumentation or exam tables. Women with class III obesity also tend to have higher rates of heavy menstrual bleeding, which could be driving expulsion, Dr. Saito-Tom said.
However, the results should not deter physicians from placing hormonal IUD in these women, she said. While the expulsion rate was higher than seen generally, it is still an effective method for most obese women. “That’s much more beneficial than discouraging patients,” Dr. Saito-Tom said.
Physicians should continue to educate patients about the benefits of long-acting reversible contraceptives and encourage all patients to utilize them, regardless of their weight, she said.
Dr. Saito-Tom reported having no relevant financial disclosures. One of her colleagues reported grant support from Merck and being a consultant for UpToDate.
[email protected]
On Twitter @maryellenny
Key clinical point:
Major finding: Women with class III obesity had 3.06 higher odds of levonorgestrel IUD expulsion, compared with a control group of women with a BMI of less than 35.
Data source: A retrospective cohort study of 1,071 women who had a levonorgestrel IUD inserted between January 2009 and December 2010.
Disclosures: Dr. Saito-Tom reported having no relevant financial disclosures. One of her colleagues reported grant support from Merck and being a consultant for UpToDate.
Medicaid paperwork adds barrier to postpartum sterilization
SAN DIEGO – Just over half of women who requested immediate postpartum sterilization received it in a prospective study of 334 women, with Medicaid paperwork serving as a barrier for many of the unfulfilled requests.
All of the women in the study delivered a baby and had requested immediate postpartum sterilization at some point before delivery, but just 173 women (52%) received the procedure, Taylor Hahn, MD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. A total of 161 women (48%) did not receive the procedure.
Dr. Hahn, a fourth-year resident at Indiana University, Indianapolis, and her colleagues followed these women for up to 3 months post partum and found that, within the group that didn’t receive immediate postpartum sterilization, just six women – less than 10% – had received sterilization by the end of the follow-up period. The remaining women had chosen an alternative contraceptive method, were still awaiting interval sterilization, or did not receive postpartum care.
This is concerning, Dr. Hahn said, because Medicaid coverage for sterilization typically expires after 60 days post partum.
The consent form was developed in the 1970s to protect women in vulnerable populations from being coerced into sterilization, but Dr. Hahn said that, today, “it really has created such a barrier to these women getting the care that they want and desire.” She contrasted the Medicaid procedure with what is typical in private insurance, which generally covers immediate postpartum sterilization, and the decision can be made the same day.
The researchers reported having no relevant financial disclosures.
[email protected]
On Twitter @maryellenny
SAN DIEGO – Just over half of women who requested immediate postpartum sterilization received it in a prospective study of 334 women, with Medicaid paperwork serving as a barrier for many of the unfulfilled requests.
All of the women in the study delivered a baby and had requested immediate postpartum sterilization at some point before delivery, but just 173 women (52%) received the procedure, Taylor Hahn, MD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. A total of 161 women (48%) did not receive the procedure.
Dr. Hahn, a fourth-year resident at Indiana University, Indianapolis, and her colleagues followed these women for up to 3 months post partum and found that, within the group that didn’t receive immediate postpartum sterilization, just six women – less than 10% – had received sterilization by the end of the follow-up period. The remaining women had chosen an alternative contraceptive method, were still awaiting interval sterilization, or did not receive postpartum care.
This is concerning, Dr. Hahn said, because Medicaid coverage for sterilization typically expires after 60 days post partum.
The consent form was developed in the 1970s to protect women in vulnerable populations from being coerced into sterilization, but Dr. Hahn said that, today, “it really has created such a barrier to these women getting the care that they want and desire.” She contrasted the Medicaid procedure with what is typical in private insurance, which generally covers immediate postpartum sterilization, and the decision can be made the same day.
The researchers reported having no relevant financial disclosures.
[email protected]
On Twitter @maryellenny
SAN DIEGO – Just over half of women who requested immediate postpartum sterilization received it in a prospective study of 334 women, with Medicaid paperwork serving as a barrier for many of the unfulfilled requests.
All of the women in the study delivered a baby and had requested immediate postpartum sterilization at some point before delivery, but just 173 women (52%) received the procedure, Taylor Hahn, MD, reported at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. A total of 161 women (48%) did not receive the procedure.
Dr. Hahn, a fourth-year resident at Indiana University, Indianapolis, and her colleagues followed these women for up to 3 months post partum and found that, within the group that didn’t receive immediate postpartum sterilization, just six women – less than 10% – had received sterilization by the end of the follow-up period. The remaining women had chosen an alternative contraceptive method, were still awaiting interval sterilization, or did not receive postpartum care.
This is concerning, Dr. Hahn said, because Medicaid coverage for sterilization typically expires after 60 days post partum.
The consent form was developed in the 1970s to protect women in vulnerable populations from being coerced into sterilization, but Dr. Hahn said that, today, “it really has created such a barrier to these women getting the care that they want and desire.” She contrasted the Medicaid procedure with what is typical in private insurance, which generally covers immediate postpartum sterilization, and the decision can be made the same day.
The researchers reported having no relevant financial disclosures.
[email protected]
On Twitter @maryellenny
Key clinical point:
Major finding: A total of 48% of women who requested immediate postpartum sterilization did not receive it.
Data source: A prospective study of 334 women who delivered and requested immediate postpartum sterilization.
Disclosures: The researchers reported having no relevant financial disclosures.
Weight loss by obese women linked to perinatal improvements
SAN DIEGO – Among obese women, weight loss, stable weight, or weight gain below Institute of Medicine guidelines may result in more favorable or similar perinatal outcomes, compared with weight gain within IOM guidelines, but not for small for gestational age, results from a retrospective cohort study showed.
“This study adds to the limited body of evidence regarding associations of low weight gain and perinatal outcomes among obese women,” Emilia G. Wilkins, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “This is the first study that uses data collected after the 2009 IOM guidelines were published. Although there have been some studies published after that time, they used older cohorts. We have a large, diverse cohort and had access to robust electronic health records, which allowed for inclusion of multiple relevant covariates.”
Dr. Wilkins, a fourth-year ob.gyn. resident at Kaiser Permanente in Oakland, Calif., reported that 59% of obese women gained weight above the IOM guidelines and that gestational weight gain above the IOM guidelines was consistently associated with worse perinatal outcomes.
Among class III obese women (BMI of 40 or greater), gestational weight gain below –2 kg, compared with gestational weight gain within IOM guidelines, was associated with lower odds of large-for-gestational-age infants (OR, 0.4; 95% CI, 0.3–0.7), preeclampsia/eclampsia (OR, 0.5; 95% CI, 0.3–0.9), cesarean section (OR, 0.5; 95% CI, 0.4–0.7), NICU admission (OR, 0.7; 95% CI, 0.5–1.1), and length of stay greater than 3 days (OR, 0.5; 95% CI, 0.4–0.8), but higher odds of small for gestational age (OR, 2.61; 95% CI, 1.11–6.20). Findings were similar for other obesity classes.
“It is surprising that the protective associations for weight loss were so strong,” Dr. Wilkins said. “At least 50% lower odds of adverse outcomes [were seen], including large for gestational age, cesarean delivery, preeclampsia/eclampsia, and extended neonatal hospital stay – all of which are clinically significant and could have a major implications for maternal and child health. The degree of increased odds (2- to 2.7-fold higher) of small for gestational age was also a surprising finding and indicates the need to further assess whether the health of the small-for-gestational-age babies differed across the gestational weight gain categories.”
One surprise was that, although the weight loss group had higher odds of delivering a small for gestational age infant, there was no association with increased NICU admission or increased neonatal hospital stay,” Dr. Wilkins added.
She acknowledged certain limitations of the study, including the fact that approximately 10% of the prepregnancy weights were self-measured. Additionally, there was low statistical power to evaluate NICU and length of stay data, and maternal conditions associated with prior weight loss such as bariatric surgery were not evaluated.
Dr. Wilkins reported having no financial disclosures.
SAN DIEGO – Among obese women, weight loss, stable weight, or weight gain below Institute of Medicine guidelines may result in more favorable or similar perinatal outcomes, compared with weight gain within IOM guidelines, but not for small for gestational age, results from a retrospective cohort study showed.
“This study adds to the limited body of evidence regarding associations of low weight gain and perinatal outcomes among obese women,” Emilia G. Wilkins, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “This is the first study that uses data collected after the 2009 IOM guidelines were published. Although there have been some studies published after that time, they used older cohorts. We have a large, diverse cohort and had access to robust electronic health records, which allowed for inclusion of multiple relevant covariates.”
Dr. Wilkins, a fourth-year ob.gyn. resident at Kaiser Permanente in Oakland, Calif., reported that 59% of obese women gained weight above the IOM guidelines and that gestational weight gain above the IOM guidelines was consistently associated with worse perinatal outcomes.
Among class III obese women (BMI of 40 or greater), gestational weight gain below –2 kg, compared with gestational weight gain within IOM guidelines, was associated with lower odds of large-for-gestational-age infants (OR, 0.4; 95% CI, 0.3–0.7), preeclampsia/eclampsia (OR, 0.5; 95% CI, 0.3–0.9), cesarean section (OR, 0.5; 95% CI, 0.4–0.7), NICU admission (OR, 0.7; 95% CI, 0.5–1.1), and length of stay greater than 3 days (OR, 0.5; 95% CI, 0.4–0.8), but higher odds of small for gestational age (OR, 2.61; 95% CI, 1.11–6.20). Findings were similar for other obesity classes.
“It is surprising that the protective associations for weight loss were so strong,” Dr. Wilkins said. “At least 50% lower odds of adverse outcomes [were seen], including large for gestational age, cesarean delivery, preeclampsia/eclampsia, and extended neonatal hospital stay – all of which are clinically significant and could have a major implications for maternal and child health. The degree of increased odds (2- to 2.7-fold higher) of small for gestational age was also a surprising finding and indicates the need to further assess whether the health of the small-for-gestational-age babies differed across the gestational weight gain categories.”
One surprise was that, although the weight loss group had higher odds of delivering a small for gestational age infant, there was no association with increased NICU admission or increased neonatal hospital stay,” Dr. Wilkins added.
She acknowledged certain limitations of the study, including the fact that approximately 10% of the prepregnancy weights were self-measured. Additionally, there was low statistical power to evaluate NICU and length of stay data, and maternal conditions associated with prior weight loss such as bariatric surgery were not evaluated.
Dr. Wilkins reported having no financial disclosures.
SAN DIEGO – Among obese women, weight loss, stable weight, or weight gain below Institute of Medicine guidelines may result in more favorable or similar perinatal outcomes, compared with weight gain within IOM guidelines, but not for small for gestational age, results from a retrospective cohort study showed.
“This study adds to the limited body of evidence regarding associations of low weight gain and perinatal outcomes among obese women,” Emilia G. Wilkins, MD, the lead study author, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “This is the first study that uses data collected after the 2009 IOM guidelines were published. Although there have been some studies published after that time, they used older cohorts. We have a large, diverse cohort and had access to robust electronic health records, which allowed for inclusion of multiple relevant covariates.”
Dr. Wilkins, a fourth-year ob.gyn. resident at Kaiser Permanente in Oakland, Calif., reported that 59% of obese women gained weight above the IOM guidelines and that gestational weight gain above the IOM guidelines was consistently associated with worse perinatal outcomes.
Among class III obese women (BMI of 40 or greater), gestational weight gain below –2 kg, compared with gestational weight gain within IOM guidelines, was associated with lower odds of large-for-gestational-age infants (OR, 0.4; 95% CI, 0.3–0.7), preeclampsia/eclampsia (OR, 0.5; 95% CI, 0.3–0.9), cesarean section (OR, 0.5; 95% CI, 0.4–0.7), NICU admission (OR, 0.7; 95% CI, 0.5–1.1), and length of stay greater than 3 days (OR, 0.5; 95% CI, 0.4–0.8), but higher odds of small for gestational age (OR, 2.61; 95% CI, 1.11–6.20). Findings were similar for other obesity classes.
“It is surprising that the protective associations for weight loss were so strong,” Dr. Wilkins said. “At least 50% lower odds of adverse outcomes [were seen], including large for gestational age, cesarean delivery, preeclampsia/eclampsia, and extended neonatal hospital stay – all of which are clinically significant and could have a major implications for maternal and child health. The degree of increased odds (2- to 2.7-fold higher) of small for gestational age was also a surprising finding and indicates the need to further assess whether the health of the small-for-gestational-age babies differed across the gestational weight gain categories.”
One surprise was that, although the weight loss group had higher odds of delivering a small for gestational age infant, there was no association with increased NICU admission or increased neonatal hospital stay,” Dr. Wilkins added.
She acknowledged certain limitations of the study, including the fact that approximately 10% of the prepregnancy weights were self-measured. Additionally, there was low statistical power to evaluate NICU and length of stay data, and maternal conditions associated with prior weight loss such as bariatric surgery were not evaluated.
Dr. Wilkins reported having no financial disclosures.
AT ACOG 2017
Key clinical point:
Major finding: Among class III obese women, gestational weight gain below –2 kg, compared with gestational weight gain within IOM guidelines, was associated with lower odds of large-for-gestational-age infants (OR, 0.4), preeclampsia/eclampsia (OR, 0.5), cesarean section (OR, 0.5), NICU admission (OR, 0.7), and length of stay greater than 3 days (OR, 0.5), but higher odds of small for gestational age (OR, 2.61).
Data source: A retrospective cohort analysis of 19,810 obese women who delivered singleton, live births greater than 35 weeks between 2009 and 2012.
Disclosures: Dr. Wilkins reported having no financial disclosures.
Vulnerable patients face higher risk of 30-day postpartum readmission
SAN DIEGO – Vulnerable patients experienced higher 30-day postpartum readmission rates, regardless of site of care, results from a large national analysis demonstrated.
“Although childbirth is the most common indication for inpatient admission in the United States – accounting for up to 4 million inpatient stays per year – national 30-day postpartum readmission rates, reasons for readmissions, and variation in readmission rates according to patient clinical and demographic characteristics on a national scale remain unknown,” Anju Ranjit, MD, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Ranjit, a postdoctoral research fellow at Brigham and Women’s Hospital, Boston, and her associates used multivariable logistic regression to compare differences in 30-day readmissions among 499,578 patients treated at hospitals serving a higher proportion of vulnerable patients (safety net hospitals) with the 30-day readmissions among 877,325 patients treated at hospitals serving a higher proportion of nonvulnerable patients (non–safety net hospitals). Models were adjusted for differences in patient demographics, comorbidities, pregnancy risk-status, type of deliveries, and hospital characteristics.
The researchers included 1,374,903 deliveries in the analysis, which were weighted to represent 3,113,047 deliveries nationwide. The national 30-day postpartum readmission rate was 1.4/100 deliveries. The top three reasons for readmission were wound infection (20.8%), infection (7.7%), and hypertension-related complications (6.2%).
Dr. Ranjit reported that in 2013, a total of 724,833 (53.3%) deliveries were to vulnerable patients and the remaining 652,070 (47.4%) to nonvulnerable patients. The rate of 30-day postpartum readmissions were higher among vulnerable patients, compared with their nonvulnerable counterparts (1.52% vs. 1.18%, respectively; adjusted odds ratio, 1.31; confidence interval, 1.26-1.37) and among patients who were treated at hospitals managing a higher proportion of vulnerable patients (1.51% vs. 1.27%; adjusted OR 1.19; CI, 1.12-1.27).*
“Higher readmission rates seen among vulnerable patients across institutions speak to the need to address disparities in perinatal care,” Dr. Ranjit said. “Quality improvement interventions targeted at safety net hospitals, where the majority of vulnerable patients seek care, could be helpful in reducing readmission rates among vulnerable populations.”
She acknowledged certain limitations of study, including the use of administrative data that is subject to coding error and that lacks clinical granularity.
“We were unable to control for patient’s race and region of residence due of lack of information,” she added. “Classification of hospitals into ‘safety net’ and ‘non–safety net’ hospitals was done – based on the proportion of vulnerable patients served, as identified in the national readmissions database – for the purpose of this study only.”
Dr. Ranjit reported having no financial disclosures.
* Correction, 05/08/17: An earlier version of this article incorrectly described the patient populations.
[email protected]
SAN DIEGO – Vulnerable patients experienced higher 30-day postpartum readmission rates, regardless of site of care, results from a large national analysis demonstrated.
“Although childbirth is the most common indication for inpatient admission in the United States – accounting for up to 4 million inpatient stays per year – national 30-day postpartum readmission rates, reasons for readmissions, and variation in readmission rates according to patient clinical and demographic characteristics on a national scale remain unknown,” Anju Ranjit, MD, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Ranjit, a postdoctoral research fellow at Brigham and Women’s Hospital, Boston, and her associates used multivariable logistic regression to compare differences in 30-day readmissions among 499,578 patients treated at hospitals serving a higher proportion of vulnerable patients (safety net hospitals) with the 30-day readmissions among 877,325 patients treated at hospitals serving a higher proportion of nonvulnerable patients (non–safety net hospitals). Models were adjusted for differences in patient demographics, comorbidities, pregnancy risk-status, type of deliveries, and hospital characteristics.
The researchers included 1,374,903 deliveries in the analysis, which were weighted to represent 3,113,047 deliveries nationwide. The national 30-day postpartum readmission rate was 1.4/100 deliveries. The top three reasons for readmission were wound infection (20.8%), infection (7.7%), and hypertension-related complications (6.2%).
Dr. Ranjit reported that in 2013, a total of 724,833 (53.3%) deliveries were to vulnerable patients and the remaining 652,070 (47.4%) to nonvulnerable patients. The rate of 30-day postpartum readmissions were higher among vulnerable patients, compared with their nonvulnerable counterparts (1.52% vs. 1.18%, respectively; adjusted odds ratio, 1.31; confidence interval, 1.26-1.37) and among patients who were treated at hospitals managing a higher proportion of vulnerable patients (1.51% vs. 1.27%; adjusted OR 1.19; CI, 1.12-1.27).*
“Higher readmission rates seen among vulnerable patients across institutions speak to the need to address disparities in perinatal care,” Dr. Ranjit said. “Quality improvement interventions targeted at safety net hospitals, where the majority of vulnerable patients seek care, could be helpful in reducing readmission rates among vulnerable populations.”
She acknowledged certain limitations of study, including the use of administrative data that is subject to coding error and that lacks clinical granularity.
“We were unable to control for patient’s race and region of residence due of lack of information,” she added. “Classification of hospitals into ‘safety net’ and ‘non–safety net’ hospitals was done – based on the proportion of vulnerable patients served, as identified in the national readmissions database – for the purpose of this study only.”
Dr. Ranjit reported having no financial disclosures.
* Correction, 05/08/17: An earlier version of this article incorrectly described the patient populations.
[email protected]
SAN DIEGO – Vulnerable patients experienced higher 30-day postpartum readmission rates, regardless of site of care, results from a large national analysis demonstrated.
“Although childbirth is the most common indication for inpatient admission in the United States – accounting for up to 4 million inpatient stays per year – national 30-day postpartum readmission rates, reasons for readmissions, and variation in readmission rates according to patient clinical and demographic characteristics on a national scale remain unknown,” Anju Ranjit, MD, said in an interview prior to the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Dr. Ranjit, a postdoctoral research fellow at Brigham and Women’s Hospital, Boston, and her associates used multivariable logistic regression to compare differences in 30-day readmissions among 499,578 patients treated at hospitals serving a higher proportion of vulnerable patients (safety net hospitals) with the 30-day readmissions among 877,325 patients treated at hospitals serving a higher proportion of nonvulnerable patients (non–safety net hospitals). Models were adjusted for differences in patient demographics, comorbidities, pregnancy risk-status, type of deliveries, and hospital characteristics.
The researchers included 1,374,903 deliveries in the analysis, which were weighted to represent 3,113,047 deliveries nationwide. The national 30-day postpartum readmission rate was 1.4/100 deliveries. The top three reasons for readmission were wound infection (20.8%), infection (7.7%), and hypertension-related complications (6.2%).
Dr. Ranjit reported that in 2013, a total of 724,833 (53.3%) deliveries were to vulnerable patients and the remaining 652,070 (47.4%) to nonvulnerable patients. The rate of 30-day postpartum readmissions were higher among vulnerable patients, compared with their nonvulnerable counterparts (1.52% vs. 1.18%, respectively; adjusted odds ratio, 1.31; confidence interval, 1.26-1.37) and among patients who were treated at hospitals managing a higher proportion of vulnerable patients (1.51% vs. 1.27%; adjusted OR 1.19; CI, 1.12-1.27).*
“Higher readmission rates seen among vulnerable patients across institutions speak to the need to address disparities in perinatal care,” Dr. Ranjit said. “Quality improvement interventions targeted at safety net hospitals, where the majority of vulnerable patients seek care, could be helpful in reducing readmission rates among vulnerable populations.”
She acknowledged certain limitations of study, including the use of administrative data that is subject to coding error and that lacks clinical granularity.
“We were unable to control for patient’s race and region of residence due of lack of information,” she added. “Classification of hospitals into ‘safety net’ and ‘non–safety net’ hospitals was done – based on the proportion of vulnerable patients served, as identified in the national readmissions database – for the purpose of this study only.”
Dr. Ranjit reported having no financial disclosures.
* Correction, 05/08/17: An earlier version of this article incorrectly described the patient populations.
[email protected]
AT ACOG 2017
Key clinical point:
Major finding: Vulnerable patients and safety net hospitals had higher rates and adjusted odds of readmission within 30 postdischarge days after delivery.
Data source: An analysis of the Nationwide Readmissions Database to identify deliveries during January 2013-October 2013.
Disclosures: Dr. Ranjit reported having no financial disclosures.
ACOG vows continued fight against rollback of women’s health protections
SAN DIEGO – Just days after the House passage of the GOP-backed American Health Care Act and signals that the Trump administration will revisit mandated coverage of contraception, leaders of the American Congress of Obstetricians and Gynecologists promised to continue fighting for coverage of women’s health services.
ACOG leaders said they have been working on advocacy in the Senate for months already, recognizing that a bill to repeal the Affordable Care Act could pass the House this year. The House-passed legislation, which still must pass the Senate, could be particularly detrimental to women’s health care, they said, because it includes a provision that would allow states to seek waivers for coverage of the essential health benefits package, which includes coverage of maternity care and contraceptives.
Before the ACA was enacted, only about 12% of insurance companies offered maternity care coverage and only three of four states required it, according to Thomas M. Gellhaus, MD, the outgoing ACOG president and an ob.gyn. in Iowa City. Because of the ACA requirements, all women now have that coverage. Additionally, the contraception coverage is what reduces maternal mortality, he said. “The fight will go on,” Dr. Gellhaus said. “We will not give up on this.”
ACOG has already been coordinating meetings between ob.gyns. and members of Congress and telephone calls before votes to reinforce the concerns with pending legislation and the impact it would have on women’s health care, Dr. Gellhaus said.
But this advocacy effort is not a partisan endeavor, said Mark DeFrancesco, MD, an ACOG past president and an ob.gyn. in Cheshire, Conn. “We’re going to stay out of politics,” he said. “You do that by making the only litmus test, ‘Is this good for women or not?’ ”
He added, “If you get out there with the ‘real facts’ ... it shouldn’t matter what your politics are or what your party is. It’s on us to explain things in such a way that we avoid rhetoric and we avoid the ideology.”
Dr. Brown, who encouraged ob.gyns. and their patients to reach out to their members of Congress in person in their home districts, said the message is simple: “This is what it means for your mother, this what it means for your sister, this is what it means for your wife, this is what it means for your daughters.”
[email protected]
On Twitter @maryellenny
SAN DIEGO – Just days after the House passage of the GOP-backed American Health Care Act and signals that the Trump administration will revisit mandated coverage of contraception, leaders of the American Congress of Obstetricians and Gynecologists promised to continue fighting for coverage of women’s health services.
ACOG leaders said they have been working on advocacy in the Senate for months already, recognizing that a bill to repeal the Affordable Care Act could pass the House this year. The House-passed legislation, which still must pass the Senate, could be particularly detrimental to women’s health care, they said, because it includes a provision that would allow states to seek waivers for coverage of the essential health benefits package, which includes coverage of maternity care and contraceptives.
Before the ACA was enacted, only about 12% of insurance companies offered maternity care coverage and only three of four states required it, according to Thomas M. Gellhaus, MD, the outgoing ACOG president and an ob.gyn. in Iowa City. Because of the ACA requirements, all women now have that coverage. Additionally, the contraception coverage is what reduces maternal mortality, he said. “The fight will go on,” Dr. Gellhaus said. “We will not give up on this.”
ACOG has already been coordinating meetings between ob.gyns. and members of Congress and telephone calls before votes to reinforce the concerns with pending legislation and the impact it would have on women’s health care, Dr. Gellhaus said.
But this advocacy effort is not a partisan endeavor, said Mark DeFrancesco, MD, an ACOG past president and an ob.gyn. in Cheshire, Conn. “We’re going to stay out of politics,” he said. “You do that by making the only litmus test, ‘Is this good for women or not?’ ”
He added, “If you get out there with the ‘real facts’ ... it shouldn’t matter what your politics are or what your party is. It’s on us to explain things in such a way that we avoid rhetoric and we avoid the ideology.”
Dr. Brown, who encouraged ob.gyns. and their patients to reach out to their members of Congress in person in their home districts, said the message is simple: “This is what it means for your mother, this what it means for your sister, this is what it means for your wife, this is what it means for your daughters.”
[email protected]
On Twitter @maryellenny
SAN DIEGO – Just days after the House passage of the GOP-backed American Health Care Act and signals that the Trump administration will revisit mandated coverage of contraception, leaders of the American Congress of Obstetricians and Gynecologists promised to continue fighting for coverage of women’s health services.
ACOG leaders said they have been working on advocacy in the Senate for months already, recognizing that a bill to repeal the Affordable Care Act could pass the House this year. The House-passed legislation, which still must pass the Senate, could be particularly detrimental to women’s health care, they said, because it includes a provision that would allow states to seek waivers for coverage of the essential health benefits package, which includes coverage of maternity care and contraceptives.
Before the ACA was enacted, only about 12% of insurance companies offered maternity care coverage and only three of four states required it, according to Thomas M. Gellhaus, MD, the outgoing ACOG president and an ob.gyn. in Iowa City. Because of the ACA requirements, all women now have that coverage. Additionally, the contraception coverage is what reduces maternal mortality, he said. “The fight will go on,” Dr. Gellhaus said. “We will not give up on this.”
ACOG has already been coordinating meetings between ob.gyns. and members of Congress and telephone calls before votes to reinforce the concerns with pending legislation and the impact it would have on women’s health care, Dr. Gellhaus said.
But this advocacy effort is not a partisan endeavor, said Mark DeFrancesco, MD, an ACOG past president and an ob.gyn. in Cheshire, Conn. “We’re going to stay out of politics,” he said. “You do that by making the only litmus test, ‘Is this good for women or not?’ ”
He added, “If you get out there with the ‘real facts’ ... it shouldn’t matter what your politics are or what your party is. It’s on us to explain things in such a way that we avoid rhetoric and we avoid the ideology.”
Dr. Brown, who encouraged ob.gyns. and their patients to reach out to their members of Congress in person in their home districts, said the message is simple: “This is what it means for your mother, this what it means for your sister, this is what it means for your wife, this is what it means for your daughters.”
[email protected]
On Twitter @maryellenny
AT ACOG 2017