User login
American College of Surgeons (ACS)/ National Surgical Quality Improvement Program (NSQIP): National Conference
Scoring tool points to postop ventilator dependence
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A preoperative risk score can help identify patients at highest risk for postoperative ventilator dependence.
Major finding: A risk score greater than 3 identified the top 20%-30% of patients experiencing 60%-70% of postop ventilator dependence events.
Data source: Retrospective analysis of 7,473 elective general and vascular surgical patients.
Disclosures: The authors reported having no financial disclosures.
More octogenarians muscling through emergent surgeries
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
OR-focused effort cuts catheter use, surgical UTIs
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: An OR-focused multidisciplinary effort decreased catheter use in the operating room and catheter-associated UTIs.
Major finding: Catheter utilization in short cases declined 9% and surgical CAUTI by 89%.
Data source: Observational analysis of 2,809 surgical catheters placed.
Disclosures: The authors reported having no financial disclosures.
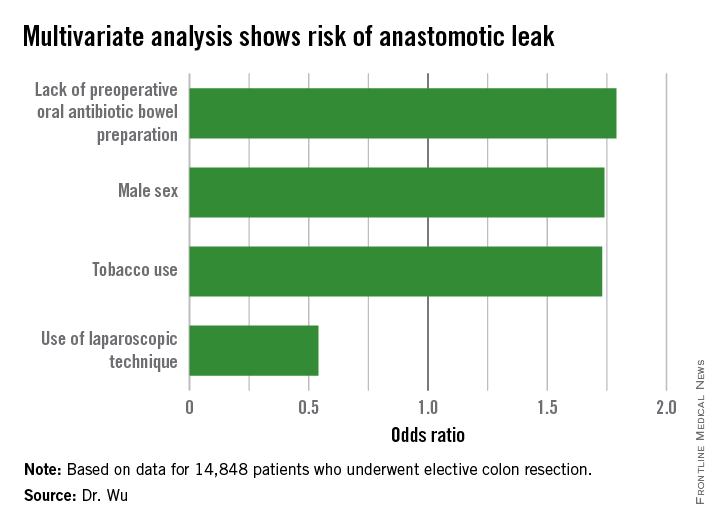
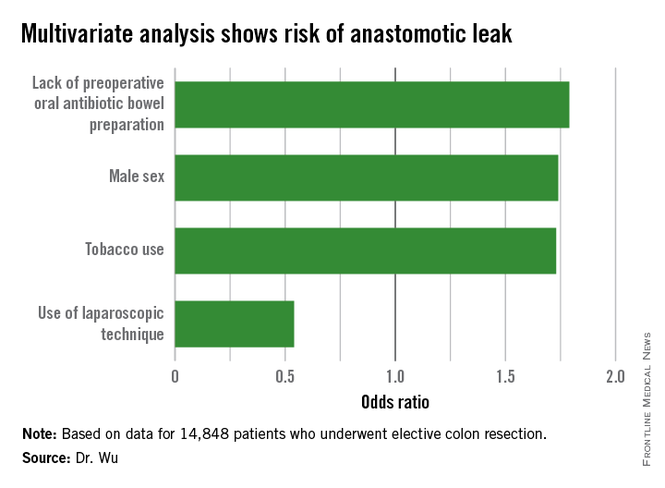
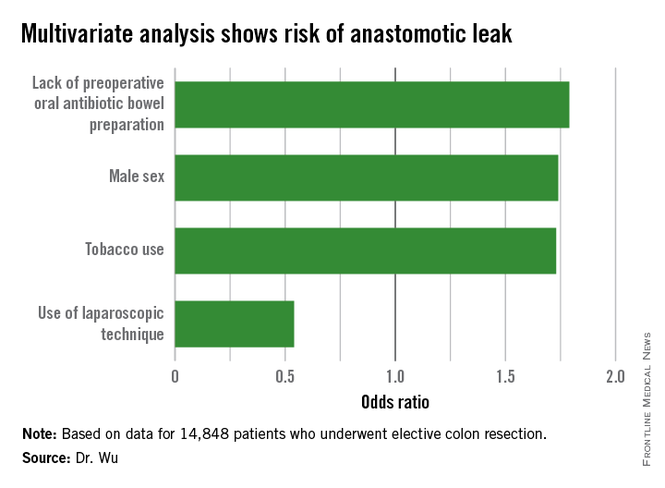
Modifiable risk factors foretell colonic anastomotic leak
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
CHICAGO – Several modifiable risk factors predicted the development of anastomotic leak following elective colon resection, a large national analysis found.
“Preoperative smoking cessation, preoperative administration of oral antibiotic bowel preparation, and laparoscopic approach are modifiable factors that could reduce the risk of anastomotic leak,” Dr. Cindy Wu said at the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) National Conference.
Anastomotic leakage results in increased morbidity and mortality, yet the current literature analyzing risk factors for this complication is generally limited to retrospective studies of single institutions, she said.
To examine data from a larger sample of colectomy patients from multiple centers, the investigators used the NSQIP Participant Use Data File specifically targeted to colectomy to identify 14,848 patients who underwent elective colon resection from 2012 to 2013. Chi-square, Wald chi-square, and logistic regression analyses were performed examining patient factors (sex, race, comorbidities, smoking status, American Society of Anesthesiologists class, functional status, steroid use, and preoperative albumin), oncologic factors (chemotherapy, tumor stage, and presence or absence of disseminated cancer), and operative factors (wound class, mechanical bowel preparation, oral antibiotic preparation, surgical approach, colectomy site, surgical indication, and operative time).
In all, 3.4%, or 498 patients, experienced an anastomotic leak, which is consistent with the literature, Dr. Wu of Temple University in Philadelphia said. Of these patients, 101 required no intervention, while 272 required surgery and 125 needed percutaneous drainage. The mean age of the patients was 60.7 years and 57% were male.
In a univariate analysis, male sex (chi-square = 17.4; P less than .01), diabetes controlled with either oral medication or insulin (X2 = 9.5; P less than .01), and smoking within the last year (X2 = 20.4; P less than .01) were associated with a greater incidence of anastomotic leak.
Other risk factors that were significant in additional univariate analysis were ASA class (X2 = 23.3; P = .0001), functional status (X2 = 9.15; P = .01), 10% weight loss over the last 6 months (X2 = 5.83; P = .02), wound class (X2 = 10.8; P = .01), mechanical bowel preparation (X2 = 5.89; P = .01), lack of oral antibiotic preparation (X2 = 17.5; P less than .0001), open vs. laparoscopic/minimally invasive surgery (X2 = 60.0; P less than .0001), chemotherapy in the last 90 days (X2 = 23.1; P less than .0001), and presence of disseminated cancer (X2 = 7.41; P = .01), Dr. Wu said.
With all of these factors taken into account in multivariate analysis, independent predictors of an increased risk of anastomotic leak were male sex (odds ratio, 1.74; P = .01), tobacco use (OR, 1.73; P = .03), and lack of a preoperative oral antibiotic bowel preparation (OR, 1.79; P less than .01).
Interestingly, use of a laparoscopic technique was protective against the development of anastomotic leakage (OR, 0.54; P less than .01), she said.
The authors reported having no relevant financial disclosures.
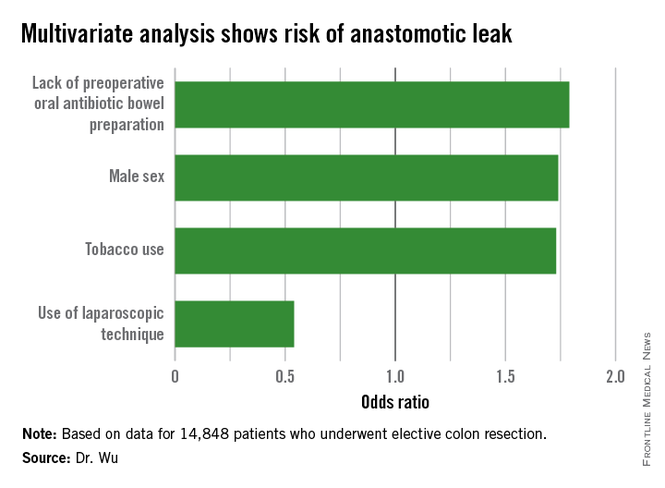
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Altering specific patient and operative factors can modify the risk of anastomotic leakage after colectomy.
Major finding: Male sex (OR, 1.74), tobacco use (OR, 1.73), and lack of an oral antibiotic bowel preparation (OR, 1.79) predicted anastomotic leak.
Data source: A retrospective study of 14,848 elective colectomies.
Disclosures: The authors reported having no relevant financial disclosures.
For Diabetic Patients, LRYGB Safety Comparable to Other Common Procedures
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
AT THE ACS NSQIP NATIONAL CONFERENCE
For diabetic patients, LRYGB safety comparable to other common procedures
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Laparoscopic Roux-en-Y gastric bypass in patients with diabetes is as safe as other common procedures.
Major finding: At 30 days, LRYGB mortality was 0.3% and the composite complication rate was 3.4%.
Data source: Retrospective study in 16,509 diabetic patients who underwent Roux-en-Y gastric bypass and 50,169 patients who had other surgical procedures.
Disclosures: The investigators and Dr. Umanskiy reported having no conflicts of interest.
Are oral antibiotics enough to reduce colorectal surgery infections?
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
CHICAGO – Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection in a large national patient sample.
Oral antibiotics (OA) alone significantly reduced the rate of any surgical site infection (SSI) by 44% (odds ratio, 0.56; 95% confidence interval, 0.36-0.87) and wound SSI by 59% (OR, 0.41; 95% CI, 0.23-0.72), compared with no bowel preparation in propensity-adjusted multivariate analysis.
OA combined with mechanical bowel preparation (MBP) was independently associated with significant reductions of 54%, 58%, and 41%, respectively, for any SSI (OR, 0.46; 95% CI, 0.38-0.55), wound SSI (OR, 0.42; 95% CI, 0.33-0.53), and organ space SSI (OR, 0.59; 95% CI, 0.44-0.78).
In contrast, MBP, which was used in 40.8% of cases, was not independently associated with reduced rates of any SSI (OR, 0.95; 95% CI, 0.82-1.10), wound SSI (OR, 0.91; 95% CI, 0.76-1.09), or organ space SSI (OR, 1.0; 95% CI, 0.79-1.27), according to Dr. Sarah Koller of Temple University Hospital in Philadelphia and her associates.
A limitation of the study was the lack of information on type of OA or MBP used, patient compliance, and use of parenteral antibiotic prophylaxis.
“Randomized clinical trials are needed to determine the true benefits of oral antibiotics alone versus combined oral antibiotics and mechanical bowel prep prior to elective colorectal resection,” Dr. Koller said at the American College of Surgeons/National Surgery Quality Improvement Program National Conference.
Session comoderator Dr. E. Patchen Dellinger, of the University of Washington in Seattle, commented, “Logically, it’s hard for me to believe that oral antibiotics would affect a couple of kilograms of stool in the colon and yet here are these tantalizing data. So we do need the prospective trial you mention.
“But, the other thing that blows my mind every time I see these data is 49% of people getting a mechanical bowel prep without oral antibiotics, which has conclusively been shown to be useless for anything but torture of the patient.”
Significant variability in the use of bowel preparation exists within the surgical community, with a recent survey of colorectal surgeons revealing that 76% routinely used MBP and only 36% routinely used oral antibiotics, Dr. Koller observed.
In the current analysis, just 3.3% of patients received OA, 30.4% OA plus MBP, 40.8% MBP, and 25.5% no bowel preparation.
Physicians have been slow to abandon MBP, despite multiple studies showing that MBP alone does not reduce SSIs in elective colon and rectal surgery. There also have been reports of higher rates of anastomotic leak, increased cardiac or metabolic complications, and a slower return of bowel function with MBP.
Several studies, including a recent Cochrane Database Review, have shown that oral or intravenous antibiotic prophylaxis reduces surgical wound infection after colorectal surgery. The comparison groups are not uniform across the studies, however, and the controversy persists as to which type of bowel prep best reduces SSI after colorectal surgery, she said.
To explore this issue, the investigators identified all patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013. The cohort included 19,372 patients with complete preoperative bowel preparation data. Patients who were ventilator dependent or had infections or open wounds at the time of surgery were excluded.
The overall rates of any SSI, wound SSI (superficial and/or deep), and organ space SSI were 9.5%, 6.4%, and 3.5%, respectively.
With regard to adverse outcomes cited in previous studies, only OA plus MBP was shown to independently reduce anastomotic leak (OR, 0.57; 95% CI, 0.42-0.78) and postoperative ileus (OR, 0.79; 95% CI, 0.68-0.92), compared with no bowel prep, Dr. Koller reported.
Both OA and OA plus MBP, however, decreased length of stay by 0.83 days.
None of the bowel preparations were independently associated with increased rates of cardiac or renal complications, she said.
The investigators were not able to track rates of Clostridium difficile colitis after administration of the oral antibiotics. Dr. Koller acknowledged this is a concern when using oral antibiotics and may contribute to why they aren’t used frequently.
Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Oral antibiotics alone or in combination with mechanical bowel preparation were independently associated with reduced surgical site infections after elective colorectal resection.
Major finding: Oral antibiotics alone significantly reduced the rate of any surgical site infection by 44% and wound SSI by 59%.
Data source: Data from 19,372 patients who underwent elective, nonemergent colorectal resections in both the ACS NSQIP Participant Use Data File (PUF) and the Procedure Targeted PUF for colectomy from 2012 to 2013.
Disclosures: Dr. Koller reported having no conflicts of interest. A coauthor disclosed consulting for Intuitive Surgical.
ERAS protocol cuts colorectal surgery morbidity, SSIs
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Through an ERAS protocol, attention to details and small multiple changes can result in dramatic improvements in patient outcomes.
Major finding: After full ERAS implementation, rates of postoperative morbidity and total surgical site infection were reduced 48.7% and 45%, respectively.
Data source: A retrospective analysis of 278 patients undergoing elective colorectal surgery.
Disclosures: The study authors reported having no relevant financial conflicts.