User login
New data bolster latitude’s association with MS prevalence
DALLAS – Latitude continues to be associated with the prevalence of multiple sclerosis (MS), according to an updated meta-analysis presented at ACTRIMS Forum 2019, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
After integrating data from 94 new studies, “the latitudinal gradient in MS prevalence ... significantly enhanced in magnitude,” said presenting author Steve Simpson Jr., PhD, and his colleagues. Dr. Simpson is a researcher at the Melbourne School of Population & Global Health at the University of Melbourne and the Menzies Institute for Medical Research at the University of Tasmania.
The researchers’ original study, published in 2011, found a slope of 2.68.
Latitudinal variations in MS prevalence have given credence to the theory that sun exposure and vitamin D may play a role in MS onset. The researchers’ original meta-analysis – based on 650 prevalence estimates from 321 studies – “confirmed the existence of a robust latitudinal gradient,” they said. To examine whether the gradient has changed, the researchers identified relevant studies published between 2010 and 2018.
They included complete, peer-reviewed articles in their analysis and extracted data about the study area, prevalence year, MS diagnostic criteria used, sample size, source population, crude prevalence, and age-specific prevalence. They combined the new prevalence estimates with those from their original study. The estimates were log-transformed and weighted with the inverse of the variance. In addition, the researchers used random-effects meta-regression models that adjusted for prevalence year and method of case ascertainment.
Their literature review identified 126 new studies, 94 of which met inclusion criteria. The new studies yielded 230 additional prevalence points, predominantly in Scandinavia, France, and the Middle East.
“Latitude was consistently and significantly associated with MS prevalence in all analyses, increasing in magnitude on adjustment and persisting on age-standardization,” Dr. Simpson and his colleagues reported.
By region, strong and significant positive gradients continue to exist in Australasia, the United Kingdom/Ireland, and North America. Meanwhile, a significant inverse gradient continues to exist in the Italian region, which the researchers have said relates to the frequency of an MS-related HLA-DRB1 allele there. A negative gradient in the Scandinavian/North Atlantic region in the original meta-analysis, considered potentially related to dietary differences, was “markedly reduced” and no longer statistically significant in the updated meta-analysis.
“While there are potential intra-regional effects contributing to the latitudinal variation in MS prevalence, these results and the relative consistency across the whole of the globe continue to provide indirect evidence in support of the role of sun and vitamin D in MS etiology,” Dr. Simpson and his colleagues concluded.
The researchers had no disclosures.
SOURCE: Simpson S Jr et al. ACTRIMS Forum 2019, Abstract 126.
DALLAS – Latitude continues to be associated with the prevalence of multiple sclerosis (MS), according to an updated meta-analysis presented at ACTRIMS Forum 2019, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
After integrating data from 94 new studies, “the latitudinal gradient in MS prevalence ... significantly enhanced in magnitude,” said presenting author Steve Simpson Jr., PhD, and his colleagues. Dr. Simpson is a researcher at the Melbourne School of Population & Global Health at the University of Melbourne and the Menzies Institute for Medical Research at the University of Tasmania.
The researchers’ original study, published in 2011, found a slope of 2.68.
Latitudinal variations in MS prevalence have given credence to the theory that sun exposure and vitamin D may play a role in MS onset. The researchers’ original meta-analysis – based on 650 prevalence estimates from 321 studies – “confirmed the existence of a robust latitudinal gradient,” they said. To examine whether the gradient has changed, the researchers identified relevant studies published between 2010 and 2018.
They included complete, peer-reviewed articles in their analysis and extracted data about the study area, prevalence year, MS diagnostic criteria used, sample size, source population, crude prevalence, and age-specific prevalence. They combined the new prevalence estimates with those from their original study. The estimates were log-transformed and weighted with the inverse of the variance. In addition, the researchers used random-effects meta-regression models that adjusted for prevalence year and method of case ascertainment.
Their literature review identified 126 new studies, 94 of which met inclusion criteria. The new studies yielded 230 additional prevalence points, predominantly in Scandinavia, France, and the Middle East.
“Latitude was consistently and significantly associated with MS prevalence in all analyses, increasing in magnitude on adjustment and persisting on age-standardization,” Dr. Simpson and his colleagues reported.
By region, strong and significant positive gradients continue to exist in Australasia, the United Kingdom/Ireland, and North America. Meanwhile, a significant inverse gradient continues to exist in the Italian region, which the researchers have said relates to the frequency of an MS-related HLA-DRB1 allele there. A negative gradient in the Scandinavian/North Atlantic region in the original meta-analysis, considered potentially related to dietary differences, was “markedly reduced” and no longer statistically significant in the updated meta-analysis.
“While there are potential intra-regional effects contributing to the latitudinal variation in MS prevalence, these results and the relative consistency across the whole of the globe continue to provide indirect evidence in support of the role of sun and vitamin D in MS etiology,” Dr. Simpson and his colleagues concluded.
The researchers had no disclosures.
SOURCE: Simpson S Jr et al. ACTRIMS Forum 2019, Abstract 126.
DALLAS – Latitude continues to be associated with the prevalence of multiple sclerosis (MS), according to an updated meta-analysis presented at ACTRIMS Forum 2019, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
After integrating data from 94 new studies, “the latitudinal gradient in MS prevalence ... significantly enhanced in magnitude,” said presenting author Steve Simpson Jr., PhD, and his colleagues. Dr. Simpson is a researcher at the Melbourne School of Population & Global Health at the University of Melbourne and the Menzies Institute for Medical Research at the University of Tasmania.
The researchers’ original study, published in 2011, found a slope of 2.68.
Latitudinal variations in MS prevalence have given credence to the theory that sun exposure and vitamin D may play a role in MS onset. The researchers’ original meta-analysis – based on 650 prevalence estimates from 321 studies – “confirmed the existence of a robust latitudinal gradient,” they said. To examine whether the gradient has changed, the researchers identified relevant studies published between 2010 and 2018.
They included complete, peer-reviewed articles in their analysis and extracted data about the study area, prevalence year, MS diagnostic criteria used, sample size, source population, crude prevalence, and age-specific prevalence. They combined the new prevalence estimates with those from their original study. The estimates were log-transformed and weighted with the inverse of the variance. In addition, the researchers used random-effects meta-regression models that adjusted for prevalence year and method of case ascertainment.
Their literature review identified 126 new studies, 94 of which met inclusion criteria. The new studies yielded 230 additional prevalence points, predominantly in Scandinavia, France, and the Middle East.
“Latitude was consistently and significantly associated with MS prevalence in all analyses, increasing in magnitude on adjustment and persisting on age-standardization,” Dr. Simpson and his colleagues reported.
By region, strong and significant positive gradients continue to exist in Australasia, the United Kingdom/Ireland, and North America. Meanwhile, a significant inverse gradient continues to exist in the Italian region, which the researchers have said relates to the frequency of an MS-related HLA-DRB1 allele there. A negative gradient in the Scandinavian/North Atlantic region in the original meta-analysis, considered potentially related to dietary differences, was “markedly reduced” and no longer statistically significant in the updated meta-analysis.
“While there are potential intra-regional effects contributing to the latitudinal variation in MS prevalence, these results and the relative consistency across the whole of the globe continue to provide indirect evidence in support of the role of sun and vitamin D in MS etiology,” Dr. Simpson and his colleagues concluded.
The researchers had no disclosures.
SOURCE: Simpson S Jr et al. ACTRIMS Forum 2019, Abstract 126.
REPORTING FROM ACTRIMS FORUM 2019
Key clinical point: Latitude continues to be associated with the prevalence of multiple sclerosis (MS).
Major finding: For every degree of latitude increase, prevalence of MS per 100,000 people increased by 3.64 in a fully adjusted, age-standardized model.
Study details: A meta-analysis of data from more than 400 studies.
Disclosures: The investigators had no disclosures.
Source: Simpson S Jr et al. ACTRIMS Forum 2019, Abstract 126.
Sex differences in MS: It’s the chromosomes, not just the hormones
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
REPORTING FROM ACTRIMS FORUM 2019
Genetic signature helps identify those at risk of MS
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
DALLAS – in a precision medicine–focused session at the meeting of the Americas Committee on Treatment and Research in Multiple Sclerosis.
“MS remains a diagnosis of exclusion ... But we’re now beginning to understand a lot more about the earliest stages of the disease, and we’re constantly redefining the disease in terms of when it starts, and what it consists of,” said Dr. De Jager, professor of neurology and chief of neuroimmunology at Columbia University, New York, in an interview.
For example, physicians are now starting to treat asymptomatic individuals with radiologically isolated syndrome, he said. “Is that part of the disease? Well, a lot of us think so, and we’re currently doing the studies to see whether treating them has an impact on long-term disability.”
“In this effort to redefine this disease and when it starts, these molecular and cellular studies are becoming very important,” Dr. De Jager said. Both individuals in the general population and high-risk individuals, such as family members of people with MS, will benefit from these research approaches, he said.
Right now, it’s hard to know who could benefit most from future preventive therapies, or who should have the most rigorous surveillance.
Dr. De Jager pointed to a presentation by his collaborator, Nikolaos Patsopoulos, MD, PhD, of Brigham and Women’s Hospital, Boston, who reported on the activities of the International MS Genetics Consortium. The consortium has collected and is nearing publication of data from more than 45,000 people with MS and 65,000 control participants to identify the genetic architecture of MS onset.
“We’re going to be reporting that there are over 234 genetic variations” that contribute to the onset of MS, Dr. De Jager said. “There are more to be found, but that’s a large number,” he said. The data point toward a genetic fingerprint that’s close to lupus, type 1 diabetes, and other inflammatory diseases. This shared genetic architecture means that there’s overlapping susceptibility for many diseases in this spectrum.
REPORTING FROM ACTRIMS FORUM 2019
Which comorbidities most diminish quality of life in patients with MS?
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
REPORTING FROM ACTRIMS FORUM 2019
MRI is a critical part of the MS precision medicine toolkit
DALLAS – MRI has long been important in both diagnosis and management of multiple sclerosis (MS). It’s more important than ever though, as perivenular demyelinating lesions emerge as a potential biomarker of the disease, and a key tool in precision medicine initiatives that target MS.
“The central vein sign is at the current time still a research tool that is being touted as an imaging finding that may be a very useful biomarker for diagnosis in MS,” said Jiwon Oh, MD, PhD, in an interview at the meeting presented by the Americas Committee for Treatment and Research in Multiple Sclerosis.
It’s almost ready for “prime time,” she said, “because it can easily be acquired on most conventional 3 Tesla MRI scanners, the sequences that you use don’t require an inordinate amount of time [and] it doesn’t take too much training to be able to easily identify the sign.”
A number of groups have evaluated the central vein sign and are finding it “a very specific biomarker” for MS, Dr. Oh said.
“It would be very useful in very early stages of diagnosis because it would prevent people from being misdiagnosed” and being treated unnecessarily, she said.
In her own work, Dr. Oh and her collaborators are following a cohort of people with radiologically isolated syndrome (RIS) discovered incidentally on brain imaging. “It’s a very valuable patient population to study because it may give us insight into the very earliest stages of MS,” as the lesions were not accompanied by any symptoms when they were first noticed.
Dr. Oh and her colleagues are finding that, among RIS patients, “the vast, vast majority of people have lesions with central veins; in our cohort, over 90% of patients met the 40% threshold that has been proposed to distinguish MS from other white matter changes.”
Dr. Oh said that the central vein sign may prove to be prognostic among RIS patients; they continue to follow the cohort being studied at the University of Toronto, where Dr. Oh is a neurologist.
DALLAS – MRI has long been important in both diagnosis and management of multiple sclerosis (MS). It’s more important than ever though, as perivenular demyelinating lesions emerge as a potential biomarker of the disease, and a key tool in precision medicine initiatives that target MS.
“The central vein sign is at the current time still a research tool that is being touted as an imaging finding that may be a very useful biomarker for diagnosis in MS,” said Jiwon Oh, MD, PhD, in an interview at the meeting presented by the Americas Committee for Treatment and Research in Multiple Sclerosis.
It’s almost ready for “prime time,” she said, “because it can easily be acquired on most conventional 3 Tesla MRI scanners, the sequences that you use don’t require an inordinate amount of time [and] it doesn’t take too much training to be able to easily identify the sign.”
A number of groups have evaluated the central vein sign and are finding it “a very specific biomarker” for MS, Dr. Oh said.
“It would be very useful in very early stages of diagnosis because it would prevent people from being misdiagnosed” and being treated unnecessarily, she said.
In her own work, Dr. Oh and her collaborators are following a cohort of people with radiologically isolated syndrome (RIS) discovered incidentally on brain imaging. “It’s a very valuable patient population to study because it may give us insight into the very earliest stages of MS,” as the lesions were not accompanied by any symptoms when they were first noticed.
Dr. Oh and her colleagues are finding that, among RIS patients, “the vast, vast majority of people have lesions with central veins; in our cohort, over 90% of patients met the 40% threshold that has been proposed to distinguish MS from other white matter changes.”
Dr. Oh said that the central vein sign may prove to be prognostic among RIS patients; they continue to follow the cohort being studied at the University of Toronto, where Dr. Oh is a neurologist.
DALLAS – MRI has long been important in both diagnosis and management of multiple sclerosis (MS). It’s more important than ever though, as perivenular demyelinating lesions emerge as a potential biomarker of the disease, and a key tool in precision medicine initiatives that target MS.
“The central vein sign is at the current time still a research tool that is being touted as an imaging finding that may be a very useful biomarker for diagnosis in MS,” said Jiwon Oh, MD, PhD, in an interview at the meeting presented by the Americas Committee for Treatment and Research in Multiple Sclerosis.
It’s almost ready for “prime time,” she said, “because it can easily be acquired on most conventional 3 Tesla MRI scanners, the sequences that you use don’t require an inordinate amount of time [and] it doesn’t take too much training to be able to easily identify the sign.”
A number of groups have evaluated the central vein sign and are finding it “a very specific biomarker” for MS, Dr. Oh said.
“It would be very useful in very early stages of diagnosis because it would prevent people from being misdiagnosed” and being treated unnecessarily, she said.
In her own work, Dr. Oh and her collaborators are following a cohort of people with radiologically isolated syndrome (RIS) discovered incidentally on brain imaging. “It’s a very valuable patient population to study because it may give us insight into the very earliest stages of MS,” as the lesions were not accompanied by any symptoms when they were first noticed.
Dr. Oh and her colleagues are finding that, among RIS patients, “the vast, vast majority of people have lesions with central veins; in our cohort, over 90% of patients met the 40% threshold that has been proposed to distinguish MS from other white matter changes.”
Dr. Oh said that the central vein sign may prove to be prognostic among RIS patients; they continue to follow the cohort being studied at the University of Toronto, where Dr. Oh is a neurologist.
REPORTING FROM ACTRIMS FORUM 2019
Survey of MS patients reveals numerous pregnancy-related concerns
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
DALLAS – When it comes to family planning and pregnancy-related decisions such as breastfeeding and medication management, patients with multiple sclerosis (MS) receive a wide variety of advice, guidance, and engagement from their health care providers, results from a single-center survey demonstrated.
“We want our patients to feel comfortable when they come to us in their 20s or 30s and they get diagnosed, they’re scared, and it’s all new to them,” one of the study authors, Casey E. Engel said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “We want them to know that family planning is something to consider and that they can proceed with having a family with our help and guidance.”
In an effort to collect patient-experience data around family planning, pregnancy, and breastfeeding post-MS diagnosis, Ms. Engel and senior author Myla D. Goldman, MD, mailed a survey to 1,000 women with confirmed MS diagnosis who had received care at the University of Virginia Medical Center in Charlottesville. The researchers reported findings from 173 respondents, of whom 70% were receiving specialty care for MS. Most of the survey participants (137) did not become pregnant following their diagnosis, while 36 did.
Of the 137 respondents who did not become pregnant following diagnosis, 22 (16%) indicated that their decision was driven by MS-related concerns, including MS worsening with pregnancy (64%), ability to care for child secondary to MS (46%), lack of knowledge about options for pregnancy and MS (18%), passing MS onto child (18%), and stopping disease-modifying therapy (DMT) to attempt pregnancy (9%).
Of the 36 women who had a pregnancy following diagnosis, 20% reported postpartum depression or anxiety, higher than the national average of 10%-15%. In addition, 79% reported not being on DMT at the time of conception, 9% were on either glatiramer acetate injection or interferon beta-1a at time of conception, and 3% were on fingolimod (Gilenya) at time of conception. The majority reported receiving inconsistent advice about when to discontinue DMT before attempting pregnancy (a range from 0 to 6 months).
“It’s also noteworthy that 20% took a year to achieve pregnancy,” said Dr. Goldman, a neurologist who directs the university’s MS clinic. “If these women stop [their DMT] 6 months in advance and they take a year to achieve pregnancy, that’s 18 months without therapeutic coverage. That’s a concern to bring to light.”
Breastfeeding was reported in 71% of mothers in postdiagnosis pregnancy with a range between 1 week and 10 months, driven in part by variable guidelines regarding DMT reinitiation. In the meantime, respondents who did not breastfeed made this decision due to fear of relapse, glucocorticoids, or desire to reinitiate medication.
“Though our study was limited by low survey response, we hope that our work may highlight the difficulty our patients face and foster discussions within the MS community around these issues to improve the individual patient experience,” the researchers wrote in their poster.
Ms. Engel worked on the study while an undergraduate at the University of Virginia. The study was supported by the ziMS Foundation.
SOURCE: Engel CE et al. ACTRIMS Forum 2019, Poster 307.
REPORTING FROM ACTRIMS FORUM 2019
Teriflunomide transmission can occur in female partners of men taking the drug
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
DALLAS – Low or undetectable levels of teriflunomide (Aubagio) occur in women who are sexually active with men taking the drug for relapsing multiple sclerosis, results from a small study demonstrated.
“One of the issues with this particular drug is that it carries a strong pregnancy warning because in animal studies the drug has been teratogenic,” Joseph B. Guarnaccia, MD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “The other issue is that it remains detectable in the body for some time. The issue of females taking this drug and conception are well known. There are strong warnings that, if a woman wants to become pregnant, the drug should be removed quickly from the system. But if their male partner is on the drug, does that pose a risk to their female partner? That question has never been addressed in a human study.”
The Food and Drug Administration prescribing information recommends that men wishing to father a child should discontinue use of teriflunomide and undergo the accelerated elimination procedure. It also recommends that female partners wishing to become pregnant should discontinue the drug and undergo an accelerated elimination procedure to verify that the plasma teriflunomide concentration is less than 0.020 mcg/mL.
In an effort to test the risk of female exposure to potentially teratogenic levels of teriflunomide through sexual intercourse, Dr. Guarnaccia, a neurologist with the Multiple Sclerosis Treatment Center at Griffin Hospital in Derby, Conn., and his colleagues recruited 10 couples and compared serum levels of teriflunomide in men with relapsing multiple sclerosis with those of their female partners. Enrollment criteria for men included a diagnosis of relapsing multiple sclerosis, age between 18 and 55 years, treatment with teriflunomide for at least 2 months prior to study entry, and frequency of sexual intercourse with their female partners at least twice a month. Pregnancy was excluded in females, and couples could not use barrier or withdrawal methods of contraception. The couples completed a brief questionnaire and underwent a one-time blood draw for teriflunomide levels either at the investigator’s office or at a LabCorp facility.
The mean age of study participants was 47 years and the mean frequency of intercourse was seven episodes per month. The mean teriflunomide concentration in men was 42.30 mcg/mL (ranged from 10.07 to 142.84 mcg/mL). Six women had teriflunomide below detection levels (0.020 mcg/mL). However, four women had detectable levels that averaged 0.045 mcg/mL (ranging from 0.022 to 0.077 mcg/mL).
“This small study demonstrates that low or undetectable levels of teriflunomide occur in females who are sexually active with males taking teriflunomide for relapsing multiple sclerosis,” the researchers wrote in their poster. They found that women who had low detectable levels of teriflunomide, compared with women with undetectable levels, did not engage in more frequent sexual intercourse nor were their levels associated with higher levels of teriflunomide in their male partners.
“Indeed, one might have expected a positive correlation between serum levels of teriflunomide in females and the frequency or concentration of inoculation in semen from their partners,” the researchers wrote. “While semen levels of teriflunomide were not measured in this study, it might be assumed that serum and semen concentrations of small molecules like teriflunomide are similar.”
The study was supported by a investigator-sponsored research grant from Sanofi-Genzyme. Dr. Guarnaccia reported that he has received speaking honoraria and educational grants from Sanofi-Genzyme, Biogen, Teva, Acorda Therapeutics, Bayer, EMD Serono, and Genentech.
SOURCE: Guarnaccia JB et al. ACTRIMS Forum 2019, Poster 115.
REPORTING FROM ACTRIMS FORUM 2019
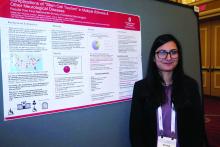
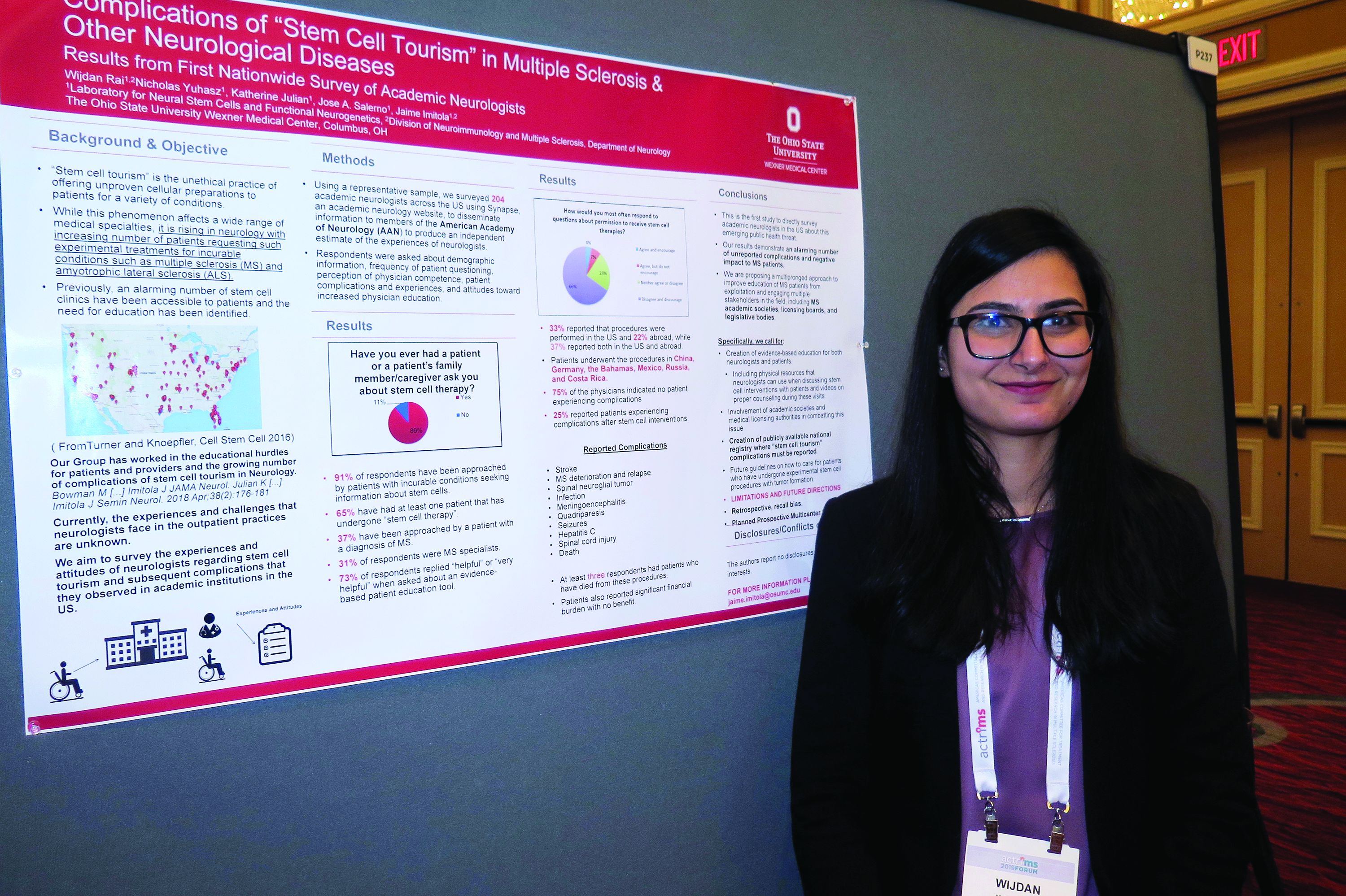
Neurologists grappling with patients who embrace ‘stem cell tourism’
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
DALLAS – Stem cell tourism – the unethical practice of offering unproven cellular preparations to patients for a variety of conditions – is increasingly sought by patients with incurable conditions such as multiple sclerosis and amyotrophic lateral sclerosis, results from a novel survey suggest.
In fact, most academic neurologists have been approached by patients with incurable conditions who ask them about stem cell therapy, while about two-thirds have had at least one patient who has undergone stem cell therapy.
“It’s really scary,” Wijdan Rai, MBBS, the study’s first author, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “This is a more prevalent issue than we think, and the complication rates are higher than we think.”
According to the study’s senior author, Jaime Imitola, MD, who directs the Progressive Multiple Sclerosis Multidisciplinary Clinic and Translational Research Program at the Ohio State University Wexner Medical Center, Columbus, the results “call for the creation of a nationwide registry where neurologists can document adverse reactions to stem cell procedures and further support dedicated patient and neurologist education as we have proposed before” (See Semin Neurol. 2018; 38[2]:176-81 and JAMA Neurol. 2015;72[11]:1342-5).
In an effort to understand the experiences and attitudes of academic neurologists regarding stem cell tourism and patient-reported complications, the researchers developed a 25-question survey disseminated via Synapse, a web tool from the American Academy of Neurology. Respondents were asked about demographic information, frequency of patient questioning, perception of physician competence, patient complications and experiences, and attitudes toward increased physician education.
Dr. Rai, who is a senior neurology resident at the medical center, presented findings from 204 neurologist respondents, of whom 31% identified themselves as MS specialists. Nearly all respondents (91%) said they have been approached by patients with incurable conditions seeking information about stem cells (37% of whom had diagnosis of MS). In addition, 65% have had at least one patient that has undergone “stem cell therapy,” and 73% said it would be “helpful” or “very helpful” to have an evidence-based patient education tool on the topic. “Patients most often wanted general information,” Dr. Rai said. “However, 50% requested permission to undergo a stem cell procedure, and 31% approached their neurologist after the procedure.”
Survey respondents reported that 33% of the stem cell interventions were performed in the United States and 22% abroad, while 37% reported both in the U.S. and abroad. Patients underwent the procedures in China, Germany, the Bahamas, Mexico, Russia, and Costa Rica. Three-quarters of respondents (75%) indicated no patient experiencing complications from the stem cell interventions. However, 25% reported patients experiencing a variety of complications from the procedures, including strokes, meningoencephalitis, quadriparesis, MS deterioration, sepsis, hepatitis C, seizures, meningitis from intrathecal cell injections, infections, and spinal cord tumors. “At least three respondents had a patient who died as a direct complication from stem cell therapy,” Dr. Rai said.
In their poster, the researchers recommended a “multipronged approach to improve education of MS patients from exploitation and engaging multiple stakeholders in the field, including MS academic societies, licensing boards, and legislative bodies. Specifically, we call for creation of evidence-based education for both neurologists and patients, including physical resources that neurologists can use when discussing stem cell interventions with patients and videos on proper counseling during these visits.”
Colleagues from OSU’s Laboratory for Neural Stem Cells and Functional Neurogenetics contributed to this work. The researchers reported having no financial disclosures.
SOURCE: Rai W et al. ACTRIMS Forum 2019, Poster 237.
REPORTING FROM ACTRIMS FORUM 2019
Evaluations for possible MS often turn up one of its many mimics
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
REPORTING FROM ACTRIMS FORUM 2019
Barancik award winner probes role of fibrinogen in MS
DALLAS – The National Multiple Sclerosis society has awarded the 2018 Barancik Prize for Innovation in Multiple Sclerosis Research to Katerina Akassoglou, PhD.
Dr. Akassoglou laid out the course of research into the role of fibrinogen in multiple sclerosis and other neurodegenerative disorders during her talk at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Akassoglou and her collaborators questioned the received wisdom about what happens when the brain’s vasculature is disrupted, she said in a video interview. “Fibrinogen was studied for several decades as only a marker of blood-brain barrier disruption. We asked the question, ‘Is it possible that it’s not only a marker, but it also plays a role in disease pathogenesis?’ ”
Over the years, said Dr. Akassoglou, she and her collaborators have developed tools “to dissect this chicken-and-egg question.” A key answer came when the researchers found that when fibrinogen leaks through the vasculature into brain tissue, it can promote inflammatory processes. “At the same time, it induced pathogenic responses in brain immune cells, causing them to be toxic to neuronal cells.”
“Using genetic models of depleting fibrinogen, or blocking its interactions with immune receptors, provided compelling data that this could be an important target for neurodegeneration and neuroinflammation,” said Dr. Akassoglou, professor of neurology at the University of California, San Francisco.
The problem came in trying to find a way to block or deplete fibrinogen inside central nervous system tissue without inactivating it throughout the circulation, since it’s essential for hemostasis.
A promising answer to this problem lies in an investigational monoclonal antibody that binds selectively to sites on fibrinogen that are activated in the brain but are not involved with fibrinogen’s usual role in the clotting cascade in the peripheral circulation, she said.
DALLAS – The National Multiple Sclerosis society has awarded the 2018 Barancik Prize for Innovation in Multiple Sclerosis Research to Katerina Akassoglou, PhD.
Dr. Akassoglou laid out the course of research into the role of fibrinogen in multiple sclerosis and other neurodegenerative disorders during her talk at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Akassoglou and her collaborators questioned the received wisdom about what happens when the brain’s vasculature is disrupted, she said in a video interview. “Fibrinogen was studied for several decades as only a marker of blood-brain barrier disruption. We asked the question, ‘Is it possible that it’s not only a marker, but it also plays a role in disease pathogenesis?’ ”
Over the years, said Dr. Akassoglou, she and her collaborators have developed tools “to dissect this chicken-and-egg question.” A key answer came when the researchers found that when fibrinogen leaks through the vasculature into brain tissue, it can promote inflammatory processes. “At the same time, it induced pathogenic responses in brain immune cells, causing them to be toxic to neuronal cells.”
“Using genetic models of depleting fibrinogen, or blocking its interactions with immune receptors, provided compelling data that this could be an important target for neurodegeneration and neuroinflammation,” said Dr. Akassoglou, professor of neurology at the University of California, San Francisco.
The problem came in trying to find a way to block or deplete fibrinogen inside central nervous system tissue without inactivating it throughout the circulation, since it’s essential for hemostasis.
A promising answer to this problem lies in an investigational monoclonal antibody that binds selectively to sites on fibrinogen that are activated in the brain but are not involved with fibrinogen’s usual role in the clotting cascade in the peripheral circulation, she said.
DALLAS – The National Multiple Sclerosis society has awarded the 2018 Barancik Prize for Innovation in Multiple Sclerosis Research to Katerina Akassoglou, PhD.
Dr. Akassoglou laid out the course of research into the role of fibrinogen in multiple sclerosis and other neurodegenerative disorders during her talk at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Akassoglou and her collaborators questioned the received wisdom about what happens when the brain’s vasculature is disrupted, she said in a video interview. “Fibrinogen was studied for several decades as only a marker of blood-brain barrier disruption. We asked the question, ‘Is it possible that it’s not only a marker, but it also plays a role in disease pathogenesis?’ ”
Over the years, said Dr. Akassoglou, she and her collaborators have developed tools “to dissect this chicken-and-egg question.” A key answer came when the researchers found that when fibrinogen leaks through the vasculature into brain tissue, it can promote inflammatory processes. “At the same time, it induced pathogenic responses in brain immune cells, causing them to be toxic to neuronal cells.”
“Using genetic models of depleting fibrinogen, or blocking its interactions with immune receptors, provided compelling data that this could be an important target for neurodegeneration and neuroinflammation,” said Dr. Akassoglou, professor of neurology at the University of California, San Francisco.
The problem came in trying to find a way to block or deplete fibrinogen inside central nervous system tissue without inactivating it throughout the circulation, since it’s essential for hemostasis.
A promising answer to this problem lies in an investigational monoclonal antibody that binds selectively to sites on fibrinogen that are activated in the brain but are not involved with fibrinogen’s usual role in the clotting cascade in the peripheral circulation, she said.
REPORTING FROM ACTRIMS FORUM 2019