User login
Anxiety and Depression Association of America (ADAA): Annual Conference
VIDEO: No longer ‘haunted’: a novel treatment for PTSD
CHICAGO – The driving force behind anxiety is avoidance, according to Barbara Rothbaum, Ph.D., an expert in exposure therapy and a presenter at this year’s annual conference of the Anxiety and Depression Association of America.
"What we think maintains [a person’s] anxiety is avoidance of what they’re scared of," says Dr. Rothbaum in this video. "We help people confront what they’re scared of, in a therapeutic manner."
Particularly in posttraumatic stress disorder, there are two drivers holding anxiety in place, which when addressed by repeatedly immersing a patient in a virtual re-creation of the traumatic event, are relieved so the person can find peace. Many patients say, "It doesn’t haunt me anymore," according to Dr. Rothbaum, professor in the department of psychiatry and behavioral sciences and director of the trauma and anxiety recovery program at Emory University, Atlanta.
In this video, Dr. Rothbaum explores what drives anxiety and how the therapeutic, virtual re-creations of painful memories is helping patients with PTSD accept that although certain things will always be "sad," they need not negate joy and pleasure in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
CHICAGO – The driving force behind anxiety is avoidance, according to Barbara Rothbaum, Ph.D., an expert in exposure therapy and a presenter at this year’s annual conference of the Anxiety and Depression Association of America.
"What we think maintains [a person’s] anxiety is avoidance of what they’re scared of," says Dr. Rothbaum in this video. "We help people confront what they’re scared of, in a therapeutic manner."
Particularly in posttraumatic stress disorder, there are two drivers holding anxiety in place, which when addressed by repeatedly immersing a patient in a virtual re-creation of the traumatic event, are relieved so the person can find peace. Many patients say, "It doesn’t haunt me anymore," according to Dr. Rothbaum, professor in the department of psychiatry and behavioral sciences and director of the trauma and anxiety recovery program at Emory University, Atlanta.
In this video, Dr. Rothbaum explores what drives anxiety and how the therapeutic, virtual re-creations of painful memories is helping patients with PTSD accept that although certain things will always be "sad," they need not negate joy and pleasure in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
CHICAGO – The driving force behind anxiety is avoidance, according to Barbara Rothbaum, Ph.D., an expert in exposure therapy and a presenter at this year’s annual conference of the Anxiety and Depression Association of America.
"What we think maintains [a person’s] anxiety is avoidance of what they’re scared of," says Dr. Rothbaum in this video. "We help people confront what they’re scared of, in a therapeutic manner."
Particularly in posttraumatic stress disorder, there are two drivers holding anxiety in place, which when addressed by repeatedly immersing a patient in a virtual re-creation of the traumatic event, are relieved so the person can find peace. Many patients say, "It doesn’t haunt me anymore," according to Dr. Rothbaum, professor in the department of psychiatry and behavioral sciences and director of the trauma and anxiety recovery program at Emory University, Atlanta.
In this video, Dr. Rothbaum explores what drives anxiety and how the therapeutic, virtual re-creations of painful memories is helping patients with PTSD accept that although certain things will always be "sad," they need not negate joy and pleasure in life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE AADA ANNUAL CONFERENCE
VIDEO: Virtual adjunct psychotherapies used to de-escalate suicide risk
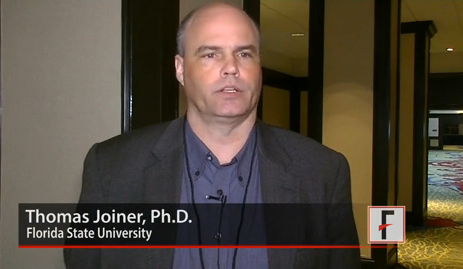
CHICAGO – Because not everyone has immediate access to treatment for suicidal depression, Thomas Joiner, Ph.D., codirector of the Military Suicide Research Consortium in Tallahassee, Fla., is helping develop virtual adjunct psychotherapies to help de-escalate acute suicide until first-line therapy can be administered.
"We are trying to locate really simple but effective interventions for suicide in service members – but we think it’s going to be generalizable beyond the military – take those risk factors from a level that is worrisome and in some cases catastrophic and make them more manageable so that other treatments have a chance to take hold and to do their work," Dr. Joiner said in an interview after his presentation given at the scientific session of the annual conference of the Anxiety and Depression Association of America.
The technology for these interventions is basic and "available to most people," according to Dr. Joiner, and includes at least one smartphone app that reminds people experiencing suicidal ideation that they matter to others and that their death would adversely affect people they love.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
CHICAGO – Because not everyone has immediate access to treatment for suicidal depression, Thomas Joiner, Ph.D., codirector of the Military Suicide Research Consortium in Tallahassee, Fla., is helping develop virtual adjunct psychotherapies to help de-escalate acute suicide until first-line therapy can be administered.
"We are trying to locate really simple but effective interventions for suicide in service members – but we think it’s going to be generalizable beyond the military – take those risk factors from a level that is worrisome and in some cases catastrophic and make them more manageable so that other treatments have a chance to take hold and to do their work," Dr. Joiner said in an interview after his presentation given at the scientific session of the annual conference of the Anxiety and Depression Association of America.
The technology for these interventions is basic and "available to most people," according to Dr. Joiner, and includes at least one smartphone app that reminds people experiencing suicidal ideation that they matter to others and that their death would adversely affect people they love.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
CHICAGO – Because not everyone has immediate access to treatment for suicidal depression, Thomas Joiner, Ph.D., codirector of the Military Suicide Research Consortium in Tallahassee, Fla., is helping develop virtual adjunct psychotherapies to help de-escalate acute suicide until first-line therapy can be administered.
"We are trying to locate really simple but effective interventions for suicide in service members – but we think it’s going to be generalizable beyond the military – take those risk factors from a level that is worrisome and in some cases catastrophic and make them more manageable so that other treatments have a chance to take hold and to do their work," Dr. Joiner said in an interview after his presentation given at the scientific session of the annual conference of the Anxiety and Depression Association of America.
The technology for these interventions is basic and "available to most people," according to Dr. Joiner, and includes at least one smartphone app that reminds people experiencing suicidal ideation that they matter to others and that their death would adversely affect people they love.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE ADAA ANNUAL CONFERENCE
AUDIO: Despite low efficacy in OCD, adjunct antipsychotics still prescribed
CHICAGO – At best, only a third of adults treated with selective serotonin reuptake inhibitors for obsessive-compulsive disorder respond to adjunctive therapy with the second-generation antipsychotic risperidone.
That’s according to Dr. H. Blair Simpson, professor of psychiatry at Columbia University and the director of the Center for Obsessive-Compulsive and Related Disorders and the Anxiety and Related Disorders Clinic at the New York State Psychiatric Institute/Columbia University.
"And if they do, typically you will know within about 4 weeks," said Dr. Simpson at the annual conference of the Anxiety and Depression Association of America.
So, why do so many patients with OCD – even pediatric ones for whom there are even fewer efficacy data – receive the second-generation antipsychotic (SGA) instead of cognitive-behavioral therapy, which does have more efficacy data? And for patients who do respond, what is the best way to titrate them off the SGA?
In an interview, Dr. Simpson and her colleague Dr. Moira Rynn, director of the Child and Adolescent Psychiatric Evaluation Service at the New York State Psychiatric Institute/Columbia University, explore the answers to these questions, as well as discuss whether two standards of mental health care are developing by default – and if so, why, as academic centers offer a wider range of treatments for refractory cases of OCD than do community-based clinicians.
CHICAGO – At best, only a third of adults treated with selective serotonin reuptake inhibitors for obsessive-compulsive disorder respond to adjunctive therapy with the second-generation antipsychotic risperidone.
That’s according to Dr. H. Blair Simpson, professor of psychiatry at Columbia University and the director of the Center for Obsessive-Compulsive and Related Disorders and the Anxiety and Related Disorders Clinic at the New York State Psychiatric Institute/Columbia University.
"And if they do, typically you will know within about 4 weeks," said Dr. Simpson at the annual conference of the Anxiety and Depression Association of America.
So, why do so many patients with OCD – even pediatric ones for whom there are even fewer efficacy data – receive the second-generation antipsychotic (SGA) instead of cognitive-behavioral therapy, which does have more efficacy data? And for patients who do respond, what is the best way to titrate them off the SGA?
In an interview, Dr. Simpson and her colleague Dr. Moira Rynn, director of the Child and Adolescent Psychiatric Evaluation Service at the New York State Psychiatric Institute/Columbia University, explore the answers to these questions, as well as discuss whether two standards of mental health care are developing by default – and if so, why, as academic centers offer a wider range of treatments for refractory cases of OCD than do community-based clinicians.
CHICAGO – At best, only a third of adults treated with selective serotonin reuptake inhibitors for obsessive-compulsive disorder respond to adjunctive therapy with the second-generation antipsychotic risperidone.
That’s according to Dr. H. Blair Simpson, professor of psychiatry at Columbia University and the director of the Center for Obsessive-Compulsive and Related Disorders and the Anxiety and Related Disorders Clinic at the New York State Psychiatric Institute/Columbia University.
"And if they do, typically you will know within about 4 weeks," said Dr. Simpson at the annual conference of the Anxiety and Depression Association of America.
So, why do so many patients with OCD – even pediatric ones for whom there are even fewer efficacy data – receive the second-generation antipsychotic (SGA) instead of cognitive-behavioral therapy, which does have more efficacy data? And for patients who do respond, what is the best way to titrate them off the SGA?
In an interview, Dr. Simpson and her colleague Dr. Moira Rynn, director of the Child and Adolescent Psychiatric Evaluation Service at the New York State Psychiatric Institute/Columbia University, explore the answers to these questions, as well as discuss whether two standards of mental health care are developing by default – and if so, why, as academic centers offer a wider range of treatments for refractory cases of OCD than do community-based clinicians.
EXPERT ANALYSIS FROM THE AADA ANNUAL CONFERENCE