User login
Second dose rates of meningococcal vaccines low among HIV-positive men who have sex with men
ATLANTA – HIV-positive men who have sex with men should be getting vaccinated against invasive meningococcal disease twice, but an alarming majority are only getting vaccinated once, according to a new study presented at a conference on STD prevention sponsored the Centers for Disease Control and Prevention.
“This analysis underscores the need for active patient recall in order to maximize return for second dose among HIV-infected [men who have sex with men], although [that] may be resource-intensive,” said Kelly Jamison, MPH, of New York City’s department of health and mental hygiene.
Ms. Jamison and her coinvestigators examined medical record data of HIV-infected men who have sex with men who visited New York City STD clinics between Oct. 5, 2012 and Dec. 31, 2014, looking for individuals who received their first meningococcal vaccinations during that time period. The primary endpoint was to find the rate at which individuals who received the first vaccination came back within 1 year (Dec. 31, 2015) to receive a second vaccination.
The study was prompted by the invasive meningococcal disease (IMD) outbreak that New York City experienced from 2010-2013, in which 22 cases were identified in men who have sex with men, of which 55% involved men who were HIV-infected. All IMD cases involved serotype C, with a case fatality rate that was three times what public health officials anticipated at the time.
Because of this, the city launched a meningitis vaccination campaign. Vaccination was recommended for all men who have sex with men who were residents of New York City and had high-risk sexual exposure after Sept. 1, 2012. In early October, STD clinics around the city began offering free MCV4 vaccines. By late November, the recommendations were updated to include men who have sex with men who lived in specific parts of Brooklyn and had experienced high-risk sexual exposure after Sept. 1. In March 2013, the recommendations were further updated to state that all HIV-infected men who have sex with men and all such men with high-risk sexual exposure should be vaccinated. In August 2013, after the outbreak was over, the recommendations were updated one last time to state that they were recommendations for “ongoing vaccination.”
“A single dose of MCV4 is not sufficient for HIV-infected persons, so a second dose is recommended to occur 8 weeks after the first dose, and in order to increase two-dose coverage among HIV-infected MSM, STD clinicians provided the date for person to return for their second dose on a vaccine card given to patients at time of their first dose,” Ms. Jamison explained.
In total, 1,212 individuals were included in study. Over the course of the study period, only 322 (26.6%) returned within 1 year for a second vaccination. In terms of individual years, 2012 experienced the highest rate of second vaccination returns, at 38.6% (P less than .001). Of the 322 who received the second vaccination, 144 (44.7%) came to the STD clinic specifically for the second dose, 69 (21.4%) asked for the second vaccination along with other STD services, and 109 (33.9%) were “opportunistically vaccinated while presenting for other services.”
Older men who have sex with men were more likely to return for their second vaccination, as only 63 (18%) of those who did were under the age of 30. Those aged between 30 and 39 years numbered 80 (23%), those between 40 and 49 years numbered 102 (33%), and those aged 50 years or older numbered 77 (40%), meaning that older men were two to three times more likely to get that second dose (P less than .001).
“We did see suboptimal return for second doses, but this may be an underestimate, [because] we were unable to capture second doses received at non-STD clinic providers,” Ms. Jamison noted.
Ms. Jamison did not report any financial disclosures for this study.
ATLANTA – HIV-positive men who have sex with men should be getting vaccinated against invasive meningococcal disease twice, but an alarming majority are only getting vaccinated once, according to a new study presented at a conference on STD prevention sponsored the Centers for Disease Control and Prevention.
“This analysis underscores the need for active patient recall in order to maximize return for second dose among HIV-infected [men who have sex with men], although [that] may be resource-intensive,” said Kelly Jamison, MPH, of New York City’s department of health and mental hygiene.
Ms. Jamison and her coinvestigators examined medical record data of HIV-infected men who have sex with men who visited New York City STD clinics between Oct. 5, 2012 and Dec. 31, 2014, looking for individuals who received their first meningococcal vaccinations during that time period. The primary endpoint was to find the rate at which individuals who received the first vaccination came back within 1 year (Dec. 31, 2015) to receive a second vaccination.
The study was prompted by the invasive meningococcal disease (IMD) outbreak that New York City experienced from 2010-2013, in which 22 cases were identified in men who have sex with men, of which 55% involved men who were HIV-infected. All IMD cases involved serotype C, with a case fatality rate that was three times what public health officials anticipated at the time.
Because of this, the city launched a meningitis vaccination campaign. Vaccination was recommended for all men who have sex with men who were residents of New York City and had high-risk sexual exposure after Sept. 1, 2012. In early October, STD clinics around the city began offering free MCV4 vaccines. By late November, the recommendations were updated to include men who have sex with men who lived in specific parts of Brooklyn and had experienced high-risk sexual exposure after Sept. 1. In March 2013, the recommendations were further updated to state that all HIV-infected men who have sex with men and all such men with high-risk sexual exposure should be vaccinated. In August 2013, after the outbreak was over, the recommendations were updated one last time to state that they were recommendations for “ongoing vaccination.”
“A single dose of MCV4 is not sufficient for HIV-infected persons, so a second dose is recommended to occur 8 weeks after the first dose, and in order to increase two-dose coverage among HIV-infected MSM, STD clinicians provided the date for person to return for their second dose on a vaccine card given to patients at time of their first dose,” Ms. Jamison explained.
In total, 1,212 individuals were included in study. Over the course of the study period, only 322 (26.6%) returned within 1 year for a second vaccination. In terms of individual years, 2012 experienced the highest rate of second vaccination returns, at 38.6% (P less than .001). Of the 322 who received the second vaccination, 144 (44.7%) came to the STD clinic specifically for the second dose, 69 (21.4%) asked for the second vaccination along with other STD services, and 109 (33.9%) were “opportunistically vaccinated while presenting for other services.”
Older men who have sex with men were more likely to return for their second vaccination, as only 63 (18%) of those who did were under the age of 30. Those aged between 30 and 39 years numbered 80 (23%), those between 40 and 49 years numbered 102 (33%), and those aged 50 years or older numbered 77 (40%), meaning that older men were two to three times more likely to get that second dose (P less than .001).
“We did see suboptimal return for second doses, but this may be an underestimate, [because] we were unable to capture second doses received at non-STD clinic providers,” Ms. Jamison noted.
Ms. Jamison did not report any financial disclosures for this study.
ATLANTA – HIV-positive men who have sex with men should be getting vaccinated against invasive meningococcal disease twice, but an alarming majority are only getting vaccinated once, according to a new study presented at a conference on STD prevention sponsored the Centers for Disease Control and Prevention.
“This analysis underscores the need for active patient recall in order to maximize return for second dose among HIV-infected [men who have sex with men], although [that] may be resource-intensive,” said Kelly Jamison, MPH, of New York City’s department of health and mental hygiene.
Ms. Jamison and her coinvestigators examined medical record data of HIV-infected men who have sex with men who visited New York City STD clinics between Oct. 5, 2012 and Dec. 31, 2014, looking for individuals who received their first meningococcal vaccinations during that time period. The primary endpoint was to find the rate at which individuals who received the first vaccination came back within 1 year (Dec. 31, 2015) to receive a second vaccination.
The study was prompted by the invasive meningococcal disease (IMD) outbreak that New York City experienced from 2010-2013, in which 22 cases were identified in men who have sex with men, of which 55% involved men who were HIV-infected. All IMD cases involved serotype C, with a case fatality rate that was three times what public health officials anticipated at the time.
Because of this, the city launched a meningitis vaccination campaign. Vaccination was recommended for all men who have sex with men who were residents of New York City and had high-risk sexual exposure after Sept. 1, 2012. In early October, STD clinics around the city began offering free MCV4 vaccines. By late November, the recommendations were updated to include men who have sex with men who lived in specific parts of Brooklyn and had experienced high-risk sexual exposure after Sept. 1. In March 2013, the recommendations were further updated to state that all HIV-infected men who have sex with men and all such men with high-risk sexual exposure should be vaccinated. In August 2013, after the outbreak was over, the recommendations were updated one last time to state that they were recommendations for “ongoing vaccination.”
“A single dose of MCV4 is not sufficient for HIV-infected persons, so a second dose is recommended to occur 8 weeks after the first dose, and in order to increase two-dose coverage among HIV-infected MSM, STD clinicians provided the date for person to return for their second dose on a vaccine card given to patients at time of their first dose,” Ms. Jamison explained.
In total, 1,212 individuals were included in study. Over the course of the study period, only 322 (26.6%) returned within 1 year for a second vaccination. In terms of individual years, 2012 experienced the highest rate of second vaccination returns, at 38.6% (P less than .001). Of the 322 who received the second vaccination, 144 (44.7%) came to the STD clinic specifically for the second dose, 69 (21.4%) asked for the second vaccination along with other STD services, and 109 (33.9%) were “opportunistically vaccinated while presenting for other services.”
Older men who have sex with men were more likely to return for their second vaccination, as only 63 (18%) of those who did were under the age of 30. Those aged between 30 and 39 years numbered 80 (23%), those between 40 and 49 years numbered 102 (33%), and those aged 50 years or older numbered 77 (40%), meaning that older men were two to three times more likely to get that second dose (P less than .001).
“We did see suboptimal return for second doses, but this may be an underestimate, [because] we were unable to capture second doses received at non-STD clinic providers,” Ms. Jamison noted.
Ms. Jamison did not report any financial disclosures for this study.
AT THE 2016 STD PREVENTION CONFERENCE
Key clinical point:
Major finding: Only 26.6% (322 of 1,212) of men who have sex with men received a second dose within a year of receiving their first, with older men who have sex with men 2-3 times more likely to get the second dose than younger men who have sex with men.
Data source: Retrospective analysis of 1,212 men who have sex with men who visited New York City STD clinics from 2012-2015.
Disclosures: Ms. Jamison did not report any financial disclosures.
Multidose metronidazole may be better option for trichomoniasis treatment
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
AT THE 2016 STD PREVENTION CONFERENCE
Key clinical point:
Major finding: A single-dose regimen of metronidazole was more likely to fail, compared with a multidose regimen, with a pooled risk ratio of 1.87 (95% CI, 1.23-2.82; P less than .01).
Data source: Meta-analysis of six studies that evaluated single- and multidose metronidazole in treating T. vaginalis infections.
Disclosures: Dr. Kissinger did not report information on financial disclosures.
Syphilis testing before and after stillbirth is suboptimal
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
ATLANTA – Physicians are falling short on syphilis testing in both the prenatal period and at the time of delivery, suggest the findings of a study examining insurance claims from nearly 10,000 women who experienced stillbirths.
Overall, less than 10% of women in the study were tested for syphilis following a stillbirth delivery, while less than two-thirds of women who experienced a stillbirth had received prenatal syphilis testing.
Dr. Patel and his coinvestigators examined data from the Truven Health MarketScan Medicaid and commercial claims database to evaluate the proportion of women who had syphilis testing within at least 1 week before and 1 week after a stillbirth delivery.
The investigators identified women aged 15-44 years who had a stillbirth delivery in 2013. Stillbirths were identified via ICD-9 codes and these codes were also used to track prenatal syphilis testing, as well as syphilis testing, placental examination and complete blood count (CBC) performed at the time of delivery.
In total, there were 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who experienced stillbirths and were included in the study. Of these women, 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-insured women and 9.3% of commercially-insured women received syphilis testing.
Most women in the study were receiving prenatal care. In all, 73.2% of Medicaid-covered women and 76.5% of commercially-insured women received it. Placental examination at the time of delivery occurred for 61.5% of Medicaid-covered women and 58.0% of commercially-insured women, while CBC was performed in 31.2% and 35.8% of women, respectively.
“Overall, prenatal syphilis testing was significantly higher than syphilis testing at the time of delivery,” Dr. Patel said. “Women with prenatal syphilis testing were more likely to be tested for syphilis at delivery than those not tested, regardless of [their] insurance.”
Dr. Patel did not report information on financial disclosures.
AT THE 2016 STD PREVENTION CONFERENCE
Key clinical point:
Major finding: A total of 65.5% of Medicaid-covered women and 56.6% of commercially-insured women received prenatal syphilis testing. At delivery, 6.5% of Medicaid-covered women and 9.3% of commercially-insured women received syphilis testing.
Data source: Review of claims data from 3,731 women enrolled in Medicaid and 6,096 commercially-insured women who had stillbirth deliveries in 2013.
Disclosures: Dr. Patel did not report information on financial disclosures.
HIV PrEP facing challenges, but implementation outlook positive
ATLANTA – Implementation of HIV preexposure prophylaxis (PrEP) by local health departments in the United States faces several challenges, but the majority of those already engaged plan to increase their participation soon, a study showed.
“For the purposes of this study, we very broadly defined engagement in PrEP implementation as anything from participating in a local or statewide working group, to planning and supporting implementation of PrEP, to doing community education and outreach, or working with providers to deliver PrEP via health department clinics,” explained Gretchen Weiss, director of HIV, STI, and viral hepatitis at the National Association of County and City Health Officials in Washington, D.C.
A total of 53% of LHDs now engaged in PrEP implementation anticipate expanding their engagement soon, 39% responded that they were unsure about expanding, and 8% said that they did not plan to expand PrEP engagement. Of the LHDs not currently implementing PrEP, 18% reported that they plan to implement PrEP within the next 4 years, while 46% were undecided, and 36% said they had no plans to implement PrEP, Ms. Weiss reported at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Of the 109 LHDs using HIV PrEP, 75% reported that they are referring individuals at high risk for sexually transmitted diseases to PrEP, while 50% said that they conduct community outreach and education regarding the benefits of using PrEP. When asked what they viewed as their “optimal role” with regard to PrEP, 77% said that it was referring high-risk individuals for treatment. Sixty-five percent reported that their optimal role was to identify PrEP providers and develop referral lists, while 33% thought that delivering PrEP via health department clinics was the optimal role for their engagement in PrEP.
“In terms of the challenges faced by LHDs, 64% reported limited staff capacity, 57% reported concerns about financial access to PrEP, and 47% responded not having enough providers that are willing to provide PrEP,” Ms. Weiss said. “Thirteen percent reported that they didn’t face any significant challenges.”
No funding source for this study was disclosed. Ms. Weiss did not report any relevant financial disclosures.
ATLANTA – Implementation of HIV preexposure prophylaxis (PrEP) by local health departments in the United States faces several challenges, but the majority of those already engaged plan to increase their participation soon, a study showed.
“For the purposes of this study, we very broadly defined engagement in PrEP implementation as anything from participating in a local or statewide working group, to planning and supporting implementation of PrEP, to doing community education and outreach, or working with providers to deliver PrEP via health department clinics,” explained Gretchen Weiss, director of HIV, STI, and viral hepatitis at the National Association of County and City Health Officials in Washington, D.C.
A total of 53% of LHDs now engaged in PrEP implementation anticipate expanding their engagement soon, 39% responded that they were unsure about expanding, and 8% said that they did not plan to expand PrEP engagement. Of the LHDs not currently implementing PrEP, 18% reported that they plan to implement PrEP within the next 4 years, while 46% were undecided, and 36% said they had no plans to implement PrEP, Ms. Weiss reported at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Of the 109 LHDs using HIV PrEP, 75% reported that they are referring individuals at high risk for sexually transmitted diseases to PrEP, while 50% said that they conduct community outreach and education regarding the benefits of using PrEP. When asked what they viewed as their “optimal role” with regard to PrEP, 77% said that it was referring high-risk individuals for treatment. Sixty-five percent reported that their optimal role was to identify PrEP providers and develop referral lists, while 33% thought that delivering PrEP via health department clinics was the optimal role for their engagement in PrEP.
“In terms of the challenges faced by LHDs, 64% reported limited staff capacity, 57% reported concerns about financial access to PrEP, and 47% responded not having enough providers that are willing to provide PrEP,” Ms. Weiss said. “Thirteen percent reported that they didn’t face any significant challenges.”
No funding source for this study was disclosed. Ms. Weiss did not report any relevant financial disclosures.
ATLANTA – Implementation of HIV preexposure prophylaxis (PrEP) by local health departments in the United States faces several challenges, but the majority of those already engaged plan to increase their participation soon, a study showed.
“For the purposes of this study, we very broadly defined engagement in PrEP implementation as anything from participating in a local or statewide working group, to planning and supporting implementation of PrEP, to doing community education and outreach, or working with providers to deliver PrEP via health department clinics,” explained Gretchen Weiss, director of HIV, STI, and viral hepatitis at the National Association of County and City Health Officials in Washington, D.C.
A total of 53% of LHDs now engaged in PrEP implementation anticipate expanding their engagement soon, 39% responded that they were unsure about expanding, and 8% said that they did not plan to expand PrEP engagement. Of the LHDs not currently implementing PrEP, 18% reported that they plan to implement PrEP within the next 4 years, while 46% were undecided, and 36% said they had no plans to implement PrEP, Ms. Weiss reported at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Of the 109 LHDs using HIV PrEP, 75% reported that they are referring individuals at high risk for sexually transmitted diseases to PrEP, while 50% said that they conduct community outreach and education regarding the benefits of using PrEP. When asked what they viewed as their “optimal role” with regard to PrEP, 77% said that it was referring high-risk individuals for treatment. Sixty-five percent reported that their optimal role was to identify PrEP providers and develop referral lists, while 33% thought that delivering PrEP via health department clinics was the optimal role for their engagement in PrEP.
“In terms of the challenges faced by LHDs, 64% reported limited staff capacity, 57% reported concerns about financial access to PrEP, and 47% responded not having enough providers that are willing to provide PrEP,” Ms. Weiss said. “Thirteen percent reported that they didn’t face any significant challenges.”
No funding source for this study was disclosed. Ms. Weiss did not report any relevant financial disclosures.
Key clinical point:
Major finding: 53% of LHDs engaged in PrEP plan to increase participation; 18% of LHDs not currently engaged in PrEP plan to implement within the next 4 years.
Data source: A survey of 284 local health departments from across the United States.
Disclosures: Ms. Weiss did not report any relevant financial conflicts.
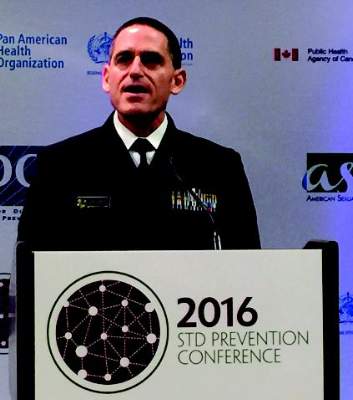
Gonorrhea cluster shows increased antibiotic resistance
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
AT THE 2016 STD PREVENTION CONFERENCE