User login
Liver disease likely to become increasing indication for bariatric surgery
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
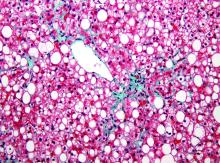
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
AGA Resource
The AGA Obesity Practice Guide provides tools for gastroenterologists to lead a multidisciplinary team of health-care professionals for the management of patients with obesity. Learn more at www.gastro.org/obesity.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
AGA Resource
The AGA Obesity Practice Guide provides tools for gastroenterologists to lead a multidisciplinary team of health-care professionals for the management of patients with obesity. Learn more at www.gastro.org/obesity.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
AGA Resource
The AGA Obesity Practice Guide provides tools for gastroenterologists to lead a multidisciplinary team of health-care professionals for the management of patients with obesity. Learn more at www.gastro.org/obesity.
AT DIGESTIVE DISEASES: NEW ADVANCES
Doubt expressed about potential of any single regimen to treat all hep C
PHILADELPHIA – Despite combination therapies for hepatitis C virus (HCV) that are now showing high rates of sustained viral remission (SVR) across all genotypes, a one-size-fits-all treatment will not be practical in the near future, according to a review of current and coming HCV therapies at Digestive Diseases: New Advances meeting held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The focus for improving HCV care is “now shifting, I think, from this one-size-fits-all treatment to identifying, really, the one-size-fits all provider,” reported Kimberly A. Brown, MD, division head of gastroenterology/hepatology at Henry Ford Health System, Detroit.
The presence of cirrhosis in some patients demonstrates the need for this care, for example. Many of the most effective single-pill DAA combinations are demonstrating high SVR rates for HCV patients with cirrhosis, but Dr. Brown said that identification of cirrhosis prior to HCV treatment “remains imperative.” Some pangenotypic therapies require a longer duration of treatment when cirrhosis is present, and patients with cirrhosis require posttreatment monitoring for decompensation and hepatocellular carcinoma (HCC). Patients who have failed a prior anti-HCV regimen or who are in renal failure also require more individualized care.
“There is no current therapy in my opinion that allows for one combination, for one length of treatment, without consideration of any patient characteristics,” Dr. Brown said at the meeting. Although several newer combination drugs with pangenotypic properties are likely to be approved for HCV in 2017, Dr. Brown believes that the one-size-fits-all ideal is not going to be fulfilled “anytime soon.”
However, Dr. Brown does believe that HCV care can and should be shifted to trained primary care providers in order to increase the proportion of infected patients who are treated. She indicated that the pangenotypic drugs are making this easier to accomplish and cited a study from the most recent annual meeting of the American Society for the Study of Liver Diseases that showed comparable SVR rates for primary care physicians, nurse practitioners, and specialists when the primary care clinicians underwent a uniform 3-hour training program (Emmanuel B. et al. AASLD 2016;Abstract 22).
“There is an evidence basis for shifting care to primary care providers in order to expand treatment, but, certainly, these providers must have an interest,” Dr. Brown said. She also said that treatment from a primary care provider must be accompanied by follow-up care, which, for example, might include clinics specializing in alcohol or drug dependency.
In treatment-naive patients with uncomplicated HCV, nearly 100% of patients will achieve an SVR on 8-12 weeks of therapy, regardless of genotype, with the newest and most potent DAA regimens, according to data cited by Dr. Brown. However, she cautioned that, even in these patients, it would be inaccurate to conclude that one-size-fits-all therapy is sufficient.
One relatively recent concern is HBV activation. “The reactivation of HBV appears to be temporally related to use of DAAs, and this seems to be independent of HCV genotype, type of DAA received, or [the patient’s] HCV parameters,” Dr. Brown reported, citing data from the Food and Drug Administration. “The clinical implications for this are that HBV DNA must now be monitored, so this is another level of complexity for our care providers.”
Other considerations for care of HCV despite achieving SVR with current treatments include monitoring for HCC and preventing reinfection. Dr. Brown cautioned that the risk of HCC, although greatly reduced after SVR, is not eliminated, and specific monitoring strategies are particularly important for those with fibrosis or cirrhosis prior to SVR.
In addition, the same risks for primary HCV are relevant for reinfection, according to Dr. Brown. She pointed out that these reinfection rates can be substantial in populations that persist in behaviors that result in HCV exposure.
“We are getting very close to the ideal of a one-size-fits-all treatment regimen for HCV, which would include no need to check genotype, no contraindications, no need for close monitoring, and no need to document cirrhosis, but we are not there yet,” Dr. Brown said. Even if such a regimen does emerge, she indicated that clinicians are not likely to ever be absolved from important management decisions that ensure an optimal long-term outcome.
PHILADELPHIA – Despite combination therapies for hepatitis C virus (HCV) that are now showing high rates of sustained viral remission (SVR) across all genotypes, a one-size-fits-all treatment will not be practical in the near future, according to a review of current and coming HCV therapies at Digestive Diseases: New Advances meeting held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The focus for improving HCV care is “now shifting, I think, from this one-size-fits-all treatment to identifying, really, the one-size-fits all provider,” reported Kimberly A. Brown, MD, division head of gastroenterology/hepatology at Henry Ford Health System, Detroit.
The presence of cirrhosis in some patients demonstrates the need for this care, for example. Many of the most effective single-pill DAA combinations are demonstrating high SVR rates for HCV patients with cirrhosis, but Dr. Brown said that identification of cirrhosis prior to HCV treatment “remains imperative.” Some pangenotypic therapies require a longer duration of treatment when cirrhosis is present, and patients with cirrhosis require posttreatment monitoring for decompensation and hepatocellular carcinoma (HCC). Patients who have failed a prior anti-HCV regimen or who are in renal failure also require more individualized care.
“There is no current therapy in my opinion that allows for one combination, for one length of treatment, without consideration of any patient characteristics,” Dr. Brown said at the meeting. Although several newer combination drugs with pangenotypic properties are likely to be approved for HCV in 2017, Dr. Brown believes that the one-size-fits-all ideal is not going to be fulfilled “anytime soon.”
However, Dr. Brown does believe that HCV care can and should be shifted to trained primary care providers in order to increase the proportion of infected patients who are treated. She indicated that the pangenotypic drugs are making this easier to accomplish and cited a study from the most recent annual meeting of the American Society for the Study of Liver Diseases that showed comparable SVR rates for primary care physicians, nurse practitioners, and specialists when the primary care clinicians underwent a uniform 3-hour training program (Emmanuel B. et al. AASLD 2016;Abstract 22).
“There is an evidence basis for shifting care to primary care providers in order to expand treatment, but, certainly, these providers must have an interest,” Dr. Brown said. She also said that treatment from a primary care provider must be accompanied by follow-up care, which, for example, might include clinics specializing in alcohol or drug dependency.
In treatment-naive patients with uncomplicated HCV, nearly 100% of patients will achieve an SVR on 8-12 weeks of therapy, regardless of genotype, with the newest and most potent DAA regimens, according to data cited by Dr. Brown. However, she cautioned that, even in these patients, it would be inaccurate to conclude that one-size-fits-all therapy is sufficient.
One relatively recent concern is HBV activation. “The reactivation of HBV appears to be temporally related to use of DAAs, and this seems to be independent of HCV genotype, type of DAA received, or [the patient’s] HCV parameters,” Dr. Brown reported, citing data from the Food and Drug Administration. “The clinical implications for this are that HBV DNA must now be monitored, so this is another level of complexity for our care providers.”
Other considerations for care of HCV despite achieving SVR with current treatments include monitoring for HCC and preventing reinfection. Dr. Brown cautioned that the risk of HCC, although greatly reduced after SVR, is not eliminated, and specific monitoring strategies are particularly important for those with fibrosis or cirrhosis prior to SVR.
In addition, the same risks for primary HCV are relevant for reinfection, according to Dr. Brown. She pointed out that these reinfection rates can be substantial in populations that persist in behaviors that result in HCV exposure.
“We are getting very close to the ideal of a one-size-fits-all treatment regimen for HCV, which would include no need to check genotype, no contraindications, no need for close monitoring, and no need to document cirrhosis, but we are not there yet,” Dr. Brown said. Even if such a regimen does emerge, she indicated that clinicians are not likely to ever be absolved from important management decisions that ensure an optimal long-term outcome.
PHILADELPHIA – Despite combination therapies for hepatitis C virus (HCV) that are now showing high rates of sustained viral remission (SVR) across all genotypes, a one-size-fits-all treatment will not be practical in the near future, according to a review of current and coming HCV therapies at Digestive Diseases: New Advances meeting held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The focus for improving HCV care is “now shifting, I think, from this one-size-fits-all treatment to identifying, really, the one-size-fits all provider,” reported Kimberly A. Brown, MD, division head of gastroenterology/hepatology at Henry Ford Health System, Detroit.
The presence of cirrhosis in some patients demonstrates the need for this care, for example. Many of the most effective single-pill DAA combinations are demonstrating high SVR rates for HCV patients with cirrhosis, but Dr. Brown said that identification of cirrhosis prior to HCV treatment “remains imperative.” Some pangenotypic therapies require a longer duration of treatment when cirrhosis is present, and patients with cirrhosis require posttreatment monitoring for decompensation and hepatocellular carcinoma (HCC). Patients who have failed a prior anti-HCV regimen or who are in renal failure also require more individualized care.
“There is no current therapy in my opinion that allows for one combination, for one length of treatment, without consideration of any patient characteristics,” Dr. Brown said at the meeting. Although several newer combination drugs with pangenotypic properties are likely to be approved for HCV in 2017, Dr. Brown believes that the one-size-fits-all ideal is not going to be fulfilled “anytime soon.”
However, Dr. Brown does believe that HCV care can and should be shifted to trained primary care providers in order to increase the proportion of infected patients who are treated. She indicated that the pangenotypic drugs are making this easier to accomplish and cited a study from the most recent annual meeting of the American Society for the Study of Liver Diseases that showed comparable SVR rates for primary care physicians, nurse practitioners, and specialists when the primary care clinicians underwent a uniform 3-hour training program (Emmanuel B. et al. AASLD 2016;Abstract 22).
“There is an evidence basis for shifting care to primary care providers in order to expand treatment, but, certainly, these providers must have an interest,” Dr. Brown said. She also said that treatment from a primary care provider must be accompanied by follow-up care, which, for example, might include clinics specializing in alcohol or drug dependency.
In treatment-naive patients with uncomplicated HCV, nearly 100% of patients will achieve an SVR on 8-12 weeks of therapy, regardless of genotype, with the newest and most potent DAA regimens, according to data cited by Dr. Brown. However, she cautioned that, even in these patients, it would be inaccurate to conclude that one-size-fits-all therapy is sufficient.
One relatively recent concern is HBV activation. “The reactivation of HBV appears to be temporally related to use of DAAs, and this seems to be independent of HCV genotype, type of DAA received, or [the patient’s] HCV parameters,” Dr. Brown reported, citing data from the Food and Drug Administration. “The clinical implications for this are that HBV DNA must now be monitored, so this is another level of complexity for our care providers.”
Other considerations for care of HCV despite achieving SVR with current treatments include monitoring for HCC and preventing reinfection. Dr. Brown cautioned that the risk of HCC, although greatly reduced after SVR, is not eliminated, and specific monitoring strategies are particularly important for those with fibrosis or cirrhosis prior to SVR.
In addition, the same risks for primary HCV are relevant for reinfection, according to Dr. Brown. She pointed out that these reinfection rates can be substantial in populations that persist in behaviors that result in HCV exposure.
“We are getting very close to the ideal of a one-size-fits-all treatment regimen for HCV, which would include no need to check genotype, no contraindications, no need for close monitoring, and no need to document cirrhosis, but we are not there yet,” Dr. Brown said. Even if such a regimen does emerge, she indicated that clinicians are not likely to ever be absolved from important management decisions that ensure an optimal long-term outcome.
AT DIGESTIVE DISEASES: NEW ADVANCES MEETING
Key clinical point: Pangenotypic efficacy is not sufficient to create a one-size-fits-all regimen for HCV treatment, according to an assessment of evolving options.
Major finding: More-effective pills have moved the focus for progress in hepatitis C to more effective delivery of care.
Data source: A research review of current and coming HCV therapies.
Disclosures: Dr. Brown reported financial relationships with AbbVie, Bayer, Bristol-Myers Squibb, Gilead, Merck, and Novartis.
Of six milestones, only two left on route to hep B cure
PHILADELPHIA – The road to absolute cure of hepatitis B virus (HBV) is so well understood that the strategies now being actively pursued may conceivably eliminate this infection from the human population, according to a summary of progress presented at Digestive Diseases: New Advances.
“As in HIV and hepatitis C infections, combination therapies of drugs with different mechanisms of action will be the solution. Which combination will deliver the ultimate cure is yet to be determined, but within 5 years we should have a cure,” reported Vinod K. Rustgi, MD, chief of hepatology at Robert Wood Johnson Medical School, New Brunswick, N.J.
The biggest hurdle to cure may be clearing covalently closed circular DNA (cccDNA) from the hepatocytes of HBV-infected individuals. This structure is derived from cytoplasmic capsid–relaxed circular DNA (rcDNA) and creates a transcriptional template in the nucleus of hepatocytes. This HBV reservoir has been thus far resistant to therapy. According to Dr. Rustgi, eliminating cccDNA along with integrated HBV RNA sequences represents the final two milestones in the road to cure. There are at least theoretical approaches to eliminating both obstacles.
For many patients, available therapies already provide a functional cure of HBV, defined as viral loads below detection. Long-term data show that such patients can anticipate a lifespan equivalent to those without HBV infection, according to Dr. Rustgi, who listed this as one of the three milestones on the road to cure that have already been achieved. The first milestone was identified as a simple reduction in viral load. The second was anti-HBe seroconversion, which can be achieved in most with available treatments. Following functional cure, the fourth milestone, clearance of HBsAg antigen, is not yet reliably achieved, although this has been documented in a proportion of patients on the most effective long-term regimens.
Understanding these milestones is important, because each has prognostic relevance, according to Dr. Rustgi. Noting the direct correlation between increasing levels of serum HBV DNA and risk of hepatocellular carcinoma (HCC) over time, he indicated that reducing HBV DNA replication already reduces risk of complications. It is possible that virologic cure, which he defined as a stable off-drug suppression of HBV viremia and normalization of liver function tests, may be achieved in a larger proportion of patients with more potent versions of existing therapies. However, absolute cure, which includes complete clearance of cccDNA and other integrated HBV DNA, is the ultimate goal. It is expected that complete clearance will eliminate the threat of HCC or other liver complications.
Based on what is understood about HBV infection, increasing the potency of nucleoside analogues, which are the mainstay of current HBV therapy, will only go so far toward absolute cure. These drugs reduce viral replication to prevent liver damage. Although new drugs to prevent cccDNA formation and HBV life cycle events such as capsid assembly and HBeAg expression may further improve outcomes, they still may not be curative without better host defenses.
“One of the ways for trying to get rid of the virus is restoration of antiviral immunity, and there are several strategies to accomplish this,” reported Dr. Rustgi, citing active efforts to mobilize T cells that attack the virus and create toll-like receptor agonists, which play a key role in the innate immune response. He suggested that several strategies now demonstrating benefit in cancer, such as blocking proteins involved in the inhibition of the immune response, are being explored in the treatment of HBV. All of these strategies may be needed.
“No single approach will be sufficient to deliver a cure,” maintained Dr. Rustgi, outlining the many mechanisms HBV employs to defend against eradication. However, he provided a long list of HBV-targeted drugs and immunotherapies, including vaccines, which are now in clinical trials, enabling combinations to attack this infection from multiple fronts.
“A curative regimen might consist of an HBV antigen inhibitor, an immune activator, a cccDNA inhibitor, and a potent nucleoside analogue,” Dr. Rustgi said. Despite the multiple mechanisms that HBV now employs to evade eradication, there are now strategies being pursued to address most of the known vulnerabilities, he said. “I hope I have given you an idea where we are going.”
Digestive Diseases: New Advances was held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company. Dr. Rustgi reported financial relationships with AbbVie, Gilead, Innovimmune, Intercept, and Merck.
PHILADELPHIA – The road to absolute cure of hepatitis B virus (HBV) is so well understood that the strategies now being actively pursued may conceivably eliminate this infection from the human population, according to a summary of progress presented at Digestive Diseases: New Advances.
“As in HIV and hepatitis C infections, combination therapies of drugs with different mechanisms of action will be the solution. Which combination will deliver the ultimate cure is yet to be determined, but within 5 years we should have a cure,” reported Vinod K. Rustgi, MD, chief of hepatology at Robert Wood Johnson Medical School, New Brunswick, N.J.
The biggest hurdle to cure may be clearing covalently closed circular DNA (cccDNA) from the hepatocytes of HBV-infected individuals. This structure is derived from cytoplasmic capsid–relaxed circular DNA (rcDNA) and creates a transcriptional template in the nucleus of hepatocytes. This HBV reservoir has been thus far resistant to therapy. According to Dr. Rustgi, eliminating cccDNA along with integrated HBV RNA sequences represents the final two milestones in the road to cure. There are at least theoretical approaches to eliminating both obstacles.
For many patients, available therapies already provide a functional cure of HBV, defined as viral loads below detection. Long-term data show that such patients can anticipate a lifespan equivalent to those without HBV infection, according to Dr. Rustgi, who listed this as one of the three milestones on the road to cure that have already been achieved. The first milestone was identified as a simple reduction in viral load. The second was anti-HBe seroconversion, which can be achieved in most with available treatments. Following functional cure, the fourth milestone, clearance of HBsAg antigen, is not yet reliably achieved, although this has been documented in a proportion of patients on the most effective long-term regimens.
Understanding these milestones is important, because each has prognostic relevance, according to Dr. Rustgi. Noting the direct correlation between increasing levels of serum HBV DNA and risk of hepatocellular carcinoma (HCC) over time, he indicated that reducing HBV DNA replication already reduces risk of complications. It is possible that virologic cure, which he defined as a stable off-drug suppression of HBV viremia and normalization of liver function tests, may be achieved in a larger proportion of patients with more potent versions of existing therapies. However, absolute cure, which includes complete clearance of cccDNA and other integrated HBV DNA, is the ultimate goal. It is expected that complete clearance will eliminate the threat of HCC or other liver complications.
Based on what is understood about HBV infection, increasing the potency of nucleoside analogues, which are the mainstay of current HBV therapy, will only go so far toward absolute cure. These drugs reduce viral replication to prevent liver damage. Although new drugs to prevent cccDNA formation and HBV life cycle events such as capsid assembly and HBeAg expression may further improve outcomes, they still may not be curative without better host defenses.
“One of the ways for trying to get rid of the virus is restoration of antiviral immunity, and there are several strategies to accomplish this,” reported Dr. Rustgi, citing active efforts to mobilize T cells that attack the virus and create toll-like receptor agonists, which play a key role in the innate immune response. He suggested that several strategies now demonstrating benefit in cancer, such as blocking proteins involved in the inhibition of the immune response, are being explored in the treatment of HBV. All of these strategies may be needed.
“No single approach will be sufficient to deliver a cure,” maintained Dr. Rustgi, outlining the many mechanisms HBV employs to defend against eradication. However, he provided a long list of HBV-targeted drugs and immunotherapies, including vaccines, which are now in clinical trials, enabling combinations to attack this infection from multiple fronts.
“A curative regimen might consist of an HBV antigen inhibitor, an immune activator, a cccDNA inhibitor, and a potent nucleoside analogue,” Dr. Rustgi said. Despite the multiple mechanisms that HBV now employs to evade eradication, there are now strategies being pursued to address most of the known vulnerabilities, he said. “I hope I have given you an idea where we are going.”
Digestive Diseases: New Advances was held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company. Dr. Rustgi reported financial relationships with AbbVie, Gilead, Innovimmune, Intercept, and Merck.
PHILADELPHIA – The road to absolute cure of hepatitis B virus (HBV) is so well understood that the strategies now being actively pursued may conceivably eliminate this infection from the human population, according to a summary of progress presented at Digestive Diseases: New Advances.
“As in HIV and hepatitis C infections, combination therapies of drugs with different mechanisms of action will be the solution. Which combination will deliver the ultimate cure is yet to be determined, but within 5 years we should have a cure,” reported Vinod K. Rustgi, MD, chief of hepatology at Robert Wood Johnson Medical School, New Brunswick, N.J.
The biggest hurdle to cure may be clearing covalently closed circular DNA (cccDNA) from the hepatocytes of HBV-infected individuals. This structure is derived from cytoplasmic capsid–relaxed circular DNA (rcDNA) and creates a transcriptional template in the nucleus of hepatocytes. This HBV reservoir has been thus far resistant to therapy. According to Dr. Rustgi, eliminating cccDNA along with integrated HBV RNA sequences represents the final two milestones in the road to cure. There are at least theoretical approaches to eliminating both obstacles.
For many patients, available therapies already provide a functional cure of HBV, defined as viral loads below detection. Long-term data show that such patients can anticipate a lifespan equivalent to those without HBV infection, according to Dr. Rustgi, who listed this as one of the three milestones on the road to cure that have already been achieved. The first milestone was identified as a simple reduction in viral load. The second was anti-HBe seroconversion, which can be achieved in most with available treatments. Following functional cure, the fourth milestone, clearance of HBsAg antigen, is not yet reliably achieved, although this has been documented in a proportion of patients on the most effective long-term regimens.
Understanding these milestones is important, because each has prognostic relevance, according to Dr. Rustgi. Noting the direct correlation between increasing levels of serum HBV DNA and risk of hepatocellular carcinoma (HCC) over time, he indicated that reducing HBV DNA replication already reduces risk of complications. It is possible that virologic cure, which he defined as a stable off-drug suppression of HBV viremia and normalization of liver function tests, may be achieved in a larger proportion of patients with more potent versions of existing therapies. However, absolute cure, which includes complete clearance of cccDNA and other integrated HBV DNA, is the ultimate goal. It is expected that complete clearance will eliminate the threat of HCC or other liver complications.
Based on what is understood about HBV infection, increasing the potency of nucleoside analogues, which are the mainstay of current HBV therapy, will only go so far toward absolute cure. These drugs reduce viral replication to prevent liver damage. Although new drugs to prevent cccDNA formation and HBV life cycle events such as capsid assembly and HBeAg expression may further improve outcomes, they still may not be curative without better host defenses.
“One of the ways for trying to get rid of the virus is restoration of antiviral immunity, and there are several strategies to accomplish this,” reported Dr. Rustgi, citing active efforts to mobilize T cells that attack the virus and create toll-like receptor agonists, which play a key role in the innate immune response. He suggested that several strategies now demonstrating benefit in cancer, such as blocking proteins involved in the inhibition of the immune response, are being explored in the treatment of HBV. All of these strategies may be needed.
“No single approach will be sufficient to deliver a cure,” maintained Dr. Rustgi, outlining the many mechanisms HBV employs to defend against eradication. However, he provided a long list of HBV-targeted drugs and immunotherapies, including vaccines, which are now in clinical trials, enabling combinations to attack this infection from multiple fronts.
“A curative regimen might consist of an HBV antigen inhibitor, an immune activator, a cccDNA inhibitor, and a potent nucleoside analogue,” Dr. Rustgi said. Despite the multiple mechanisms that HBV now employs to evade eradication, there are now strategies being pursued to address most of the known vulnerabilities, he said. “I hope I have given you an idea where we are going.”
Digestive Diseases: New Advances was held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company. Dr. Rustgi reported financial relationships with AbbVie, Gilead, Innovimmune, Intercept, and Merck.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Three clinical disorders confound diagnosis of gastroparesis
PHILADELPHIA – Particularly in adults, there are three conditions that produce symptoms consistent with idiopathic gastroparesis and should be specifically considered in a detailed history conducted before advanced diagnostic tests, according to a clinical update at the Fourth Annual Digestive Diseases: New Advances meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The three disorders “are very important, because we see them missed all the time,” reported Anthony J. Lembo, MD, director of the GI Motility Laboratory, Beth Israel Deaconess Medical Center, Boston.
“If you do not take a detailed enough history or if the patient is not willing to tell you about their past history, there is a good chance that these will go undetected,” Dr. Lembo explained. In his update on gastroparesis, he identified the recognition of these disorders as the most important clinical pearl of his overview of the challenges faced when evaluating the highly nonspecific symptoms of delayed–bowel transit time.
“Rumination syndrome has a very classic set of symptoms. When the patient swallows food, it will almost immediately or very quickly come back up. Sometimes the food is vomited. Often, it gets swallowed back down. That is not gastroparesis,” Dr. Lembo explained. Although vomiting after eating is a common symptom of gastroparesis, it is typically delayed by hours.
Cyclical vomiting syndrome, perhaps more readily recognized in children, does occur in adults more than many clinicians appreciate, according to Dr. Lembo. He said that there is one key giveaway for this condition: patients are asymptomatic between episodes. He also said that episodes are separated by substantial intervals of weeks to months.
Symptoms associated with cannabinoids are most commonly observed in young men frequently using marijuana over an extended period, according to Dr. Lembo. He said reports that symptoms are improved with hot showers may be a clue that marijuana is involved in the etiology. Urine tests are useful when patients suspected of marijuana use deny this history.
The problem is that, even when cannabinoid use is isolated as the cause of bowel symptoms, many patients are convinced that their symptoms improve, rather than get worse, with marijuana use. This is a common obstacle to the abstention needed to evaluate benefit, according to Dr. Lembo.
As for other possible etiologies, Dr. Lembo advised upper endoscopy to rule out mechanical causes of gastroparesis, such as peptic ulcer disease, proximal bowel obstruction, or gastrointestinal cancer. He specifically recommended scoping to the “third portion of the duodenum” when obstruction is being considered in the differential diagnosis.
When gastroparesis is considered the most likely cause of symptoms, Dr. Lembo recommended a gastric-emptying study to increase confidence in the diagnosis. He identified 4-hour scintigraphy as the standard of care, as defined by current guidelines. However, he warned that even well-regarded centers do not always follow this standard. Based on the lower sensitivity and specificity of shorter duration tests and of other options such as breath tests or wireless motility capsules, clinicians “should really insist” on the 4-hour gastric-emptying test when they are concerned about documentation, he said.
Once the diagnosis has been made, there are numerous therapeutic options, but the top three are “diet, diet, and diet,” according to Dr. Lembo. In his review of prokinetic drugs, such as metoclopramide and motilin agonists, he cautioned that there is often a delicate balance between risk and benefit. New options on the horizon include a ghrelin agonist that showed promise in a phase III trial, but he noted that many patients with severe unremitting symptoms are prepared to try almost anything.
“These can be desperate people when they have failed everything that is out there,” Dr. Lembo noted. He acknowledged that such patients express interest even in strategies that have failed to show convincing benefit in controlled trials, such as botulism toxin injection and neuroenteric gastric stimulators. When all other options have been exhausted, a referral to a specialist for experimental therapies may be appropriate because of the major adverse impact of unremitting symptoms on quality of life.
Dr. Lembo reported financial relationships with Alkermes, Allergan, Forest, Ironwood, Prometheus, and Salix.
PHILADELPHIA – Particularly in adults, there are three conditions that produce symptoms consistent with idiopathic gastroparesis and should be specifically considered in a detailed history conducted before advanced diagnostic tests, according to a clinical update at the Fourth Annual Digestive Diseases: New Advances meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The three disorders “are very important, because we see them missed all the time,” reported Anthony J. Lembo, MD, director of the GI Motility Laboratory, Beth Israel Deaconess Medical Center, Boston.
“If you do not take a detailed enough history or if the patient is not willing to tell you about their past history, there is a good chance that these will go undetected,” Dr. Lembo explained. In his update on gastroparesis, he identified the recognition of these disorders as the most important clinical pearl of his overview of the challenges faced when evaluating the highly nonspecific symptoms of delayed–bowel transit time.
“Rumination syndrome has a very classic set of symptoms. When the patient swallows food, it will almost immediately or very quickly come back up. Sometimes the food is vomited. Often, it gets swallowed back down. That is not gastroparesis,” Dr. Lembo explained. Although vomiting after eating is a common symptom of gastroparesis, it is typically delayed by hours.
Cyclical vomiting syndrome, perhaps more readily recognized in children, does occur in adults more than many clinicians appreciate, according to Dr. Lembo. He said that there is one key giveaway for this condition: patients are asymptomatic between episodes. He also said that episodes are separated by substantial intervals of weeks to months.
Symptoms associated with cannabinoids are most commonly observed in young men frequently using marijuana over an extended period, according to Dr. Lembo. He said reports that symptoms are improved with hot showers may be a clue that marijuana is involved in the etiology. Urine tests are useful when patients suspected of marijuana use deny this history.
The problem is that, even when cannabinoid use is isolated as the cause of bowel symptoms, many patients are convinced that their symptoms improve, rather than get worse, with marijuana use. This is a common obstacle to the abstention needed to evaluate benefit, according to Dr. Lembo.
As for other possible etiologies, Dr. Lembo advised upper endoscopy to rule out mechanical causes of gastroparesis, such as peptic ulcer disease, proximal bowel obstruction, or gastrointestinal cancer. He specifically recommended scoping to the “third portion of the duodenum” when obstruction is being considered in the differential diagnosis.
When gastroparesis is considered the most likely cause of symptoms, Dr. Lembo recommended a gastric-emptying study to increase confidence in the diagnosis. He identified 4-hour scintigraphy as the standard of care, as defined by current guidelines. However, he warned that even well-regarded centers do not always follow this standard. Based on the lower sensitivity and specificity of shorter duration tests and of other options such as breath tests or wireless motility capsules, clinicians “should really insist” on the 4-hour gastric-emptying test when they are concerned about documentation, he said.
Once the diagnosis has been made, there are numerous therapeutic options, but the top three are “diet, diet, and diet,” according to Dr. Lembo. In his review of prokinetic drugs, such as metoclopramide and motilin agonists, he cautioned that there is often a delicate balance between risk and benefit. New options on the horizon include a ghrelin agonist that showed promise in a phase III trial, but he noted that many patients with severe unremitting symptoms are prepared to try almost anything.
“These can be desperate people when they have failed everything that is out there,” Dr. Lembo noted. He acknowledged that such patients express interest even in strategies that have failed to show convincing benefit in controlled trials, such as botulism toxin injection and neuroenteric gastric stimulators. When all other options have been exhausted, a referral to a specialist for experimental therapies may be appropriate because of the major adverse impact of unremitting symptoms on quality of life.
Dr. Lembo reported financial relationships with Alkermes, Allergan, Forest, Ironwood, Prometheus, and Salix.
PHILADELPHIA – Particularly in adults, there are three conditions that produce symptoms consistent with idiopathic gastroparesis and should be specifically considered in a detailed history conducted before advanced diagnostic tests, according to a clinical update at the Fourth Annual Digestive Diseases: New Advances meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The three disorders “are very important, because we see them missed all the time,” reported Anthony J. Lembo, MD, director of the GI Motility Laboratory, Beth Israel Deaconess Medical Center, Boston.
“If you do not take a detailed enough history or if the patient is not willing to tell you about their past history, there is a good chance that these will go undetected,” Dr. Lembo explained. In his update on gastroparesis, he identified the recognition of these disorders as the most important clinical pearl of his overview of the challenges faced when evaluating the highly nonspecific symptoms of delayed–bowel transit time.
“Rumination syndrome has a very classic set of symptoms. When the patient swallows food, it will almost immediately or very quickly come back up. Sometimes the food is vomited. Often, it gets swallowed back down. That is not gastroparesis,” Dr. Lembo explained. Although vomiting after eating is a common symptom of gastroparesis, it is typically delayed by hours.
Cyclical vomiting syndrome, perhaps more readily recognized in children, does occur in adults more than many clinicians appreciate, according to Dr. Lembo. He said that there is one key giveaway for this condition: patients are asymptomatic between episodes. He also said that episodes are separated by substantial intervals of weeks to months.
Symptoms associated with cannabinoids are most commonly observed in young men frequently using marijuana over an extended period, according to Dr. Lembo. He said reports that symptoms are improved with hot showers may be a clue that marijuana is involved in the etiology. Urine tests are useful when patients suspected of marijuana use deny this history.
The problem is that, even when cannabinoid use is isolated as the cause of bowel symptoms, many patients are convinced that their symptoms improve, rather than get worse, with marijuana use. This is a common obstacle to the abstention needed to evaluate benefit, according to Dr. Lembo.
As for other possible etiologies, Dr. Lembo advised upper endoscopy to rule out mechanical causes of gastroparesis, such as peptic ulcer disease, proximal bowel obstruction, or gastrointestinal cancer. He specifically recommended scoping to the “third portion of the duodenum” when obstruction is being considered in the differential diagnosis.
When gastroparesis is considered the most likely cause of symptoms, Dr. Lembo recommended a gastric-emptying study to increase confidence in the diagnosis. He identified 4-hour scintigraphy as the standard of care, as defined by current guidelines. However, he warned that even well-regarded centers do not always follow this standard. Based on the lower sensitivity and specificity of shorter duration tests and of other options such as breath tests or wireless motility capsules, clinicians “should really insist” on the 4-hour gastric-emptying test when they are concerned about documentation, he said.
Once the diagnosis has been made, there are numerous therapeutic options, but the top three are “diet, diet, and diet,” according to Dr. Lembo. In his review of prokinetic drugs, such as metoclopramide and motilin agonists, he cautioned that there is often a delicate balance between risk and benefit. New options on the horizon include a ghrelin agonist that showed promise in a phase III trial, but he noted that many patients with severe unremitting symptoms are prepared to try almost anything.
“These can be desperate people when they have failed everything that is out there,” Dr. Lembo noted. He acknowledged that such patients express interest even in strategies that have failed to show convincing benefit in controlled trials, such as botulism toxin injection and neuroenteric gastric stimulators. When all other options have been exhausted, a referral to a specialist for experimental therapies may be appropriate because of the major adverse impact of unremitting symptoms on quality of life.
Dr. Lembo reported financial relationships with Alkermes, Allergan, Forest, Ironwood, Prometheus, and Salix.
Therapeutic window is narrow for steroids in alcoholic hepatitis
PHILADELPHIA – The main lesson for discordant data regarding the benefit of corticosteroids for alcoholic hepatitis is that mortality reductions accrue only to those patients who have advanced hepatitis but have not yet developed end-stage disease, according to a detailed look at published studies presented at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The relative benefit even in appropriate candidates is modest, according to Kevin Mullen, MD, chief of digestive diseases, West Virginia University, Morgantown. By his calculations, there is a survival benefit for one of every five to seven patients treated, and that survival benefit endures only 6-12 months.
These calculations were extrapolated from a long list of studies published over the last 45 years, some of the largest of which concluded that steroids are ineffective, according to Dr. Mullen. The likely source of the conflicting data is the timing of steroids over the course of the disease and the disparity in the scales used to define severity.
Of the scales employed to select candidates for steroid therapy, the Maddrey Discriminant Function (MDF) may be the best supported, according to Dr. Mullen. He suggested that other options, such as the MELD (Model for End-Stage Liver Disease) score and the presence or absence of hepatic encephalopathy are also likely to have discriminatory value in selecting patients for steroid therapy, but these have been largely evaluated in retrospective studies using disparate methodologies.
“The problem arises from so many trials using different criteria for patient selection,” Dr. Mullen explained.
Nevertheless, drawing on the preponderance of data, Dr. Mullen concluded that there is likely to be a therapeutic window within which steroids are beneficial. Using one prednisolone study that stratified patients by MDF score to illustrate this point, he noted that 6-month survival on active therapy was no better than placebo in patients with an MDF less than 25 and numerically but not necessarily clinically significantly better in those scoring 25-34. In the groups with an MDF score of 35-44 or 44-54, the survival at 6 months was several times higher (greater than 60% vs. less than 20%), but there was no advantage with scores greater than 54. In this latter group, the mortality rate at 6 months was 100% in those receiving steroids but only 80% among those given placebo.
“In my mind, there is no question that steroids can be of benefit, but it is a question of picking the right patient. If steroids are given too late in the disease process, it can exacerbate end-stage problems, leading to death,” Dr. Mullen said.
The potential mechanisms of benefit from steroids in alcoholic hepatitis include a reduction in collagen formation and an increase in albumin production, according to Dr. Mullen. In addition, steroids have the potential to suppress the cytokine-mediated inflammation that drives progressive liver dysfunction. However, steroids also have the potential of exacerbating existing infections by suppressing immune function. Moreover, he cautioned that steroids are contraindicated in patients with gastrointestinal bleeding or pancreatitis.
Importantly, patients with alcoholic hepatitis who are going to respond to steroids typically demonstrate a reduction in bilirubin within the first week, according to Dr. Mullen. He cautioned that continuing steroids in the absence of a change in bilirubin should be weighed again potential harms, including the exacerbation of liver disease or comorbidities. Even in responders, he recommended no more than 3 weeks to preserve a favorable benefit-to-risk ratio.
“Four weeks may be too long,” Dr. Mullen advised, but he also suggested that the management of advanced alcoholic hepatitis may be best left to specialists.
“Patients with severe alcoholic hepatitis should be referred and the referral should be to a hepatologist accustomed to managing these patients,” said Dr. Mullen, who cautioned that this is a challenging disease. “We have not been making a huge amount of progress” in the treatment of alcoholic hepatitis, which can be a frustrating disease because of alcoholic recidivism and poor prognosis in advanced stages, he said.
“I would argue that severe alcoholic liver disease has been one of the barriers for recruiting physicians into hepatology, because it is a very arduous group of people to look after, they get very sick, and the treatments are often not very successful,” he noted.
Global Academy and this news organization are owned by the same company. Dr. Mullen had no disclosures to report.
PHILADELPHIA – The main lesson for discordant data regarding the benefit of corticosteroids for alcoholic hepatitis is that mortality reductions accrue only to those patients who have advanced hepatitis but have not yet developed end-stage disease, according to a detailed look at published studies presented at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The relative benefit even in appropriate candidates is modest, according to Kevin Mullen, MD, chief of digestive diseases, West Virginia University, Morgantown. By his calculations, there is a survival benefit for one of every five to seven patients treated, and that survival benefit endures only 6-12 months.
These calculations were extrapolated from a long list of studies published over the last 45 years, some of the largest of which concluded that steroids are ineffective, according to Dr. Mullen. The likely source of the conflicting data is the timing of steroids over the course of the disease and the disparity in the scales used to define severity.
Of the scales employed to select candidates for steroid therapy, the Maddrey Discriminant Function (MDF) may be the best supported, according to Dr. Mullen. He suggested that other options, such as the MELD (Model for End-Stage Liver Disease) score and the presence or absence of hepatic encephalopathy are also likely to have discriminatory value in selecting patients for steroid therapy, but these have been largely evaluated in retrospective studies using disparate methodologies.
“The problem arises from so many trials using different criteria for patient selection,” Dr. Mullen explained.
Nevertheless, drawing on the preponderance of data, Dr. Mullen concluded that there is likely to be a therapeutic window within which steroids are beneficial. Using one prednisolone study that stratified patients by MDF score to illustrate this point, he noted that 6-month survival on active therapy was no better than placebo in patients with an MDF less than 25 and numerically but not necessarily clinically significantly better in those scoring 25-34. In the groups with an MDF score of 35-44 or 44-54, the survival at 6 months was several times higher (greater than 60% vs. less than 20%), but there was no advantage with scores greater than 54. In this latter group, the mortality rate at 6 months was 100% in those receiving steroids but only 80% among those given placebo.
“In my mind, there is no question that steroids can be of benefit, but it is a question of picking the right patient. If steroids are given too late in the disease process, it can exacerbate end-stage problems, leading to death,” Dr. Mullen said.
The potential mechanisms of benefit from steroids in alcoholic hepatitis include a reduction in collagen formation and an increase in albumin production, according to Dr. Mullen. In addition, steroids have the potential to suppress the cytokine-mediated inflammation that drives progressive liver dysfunction. However, steroids also have the potential of exacerbating existing infections by suppressing immune function. Moreover, he cautioned that steroids are contraindicated in patients with gastrointestinal bleeding or pancreatitis.
Importantly, patients with alcoholic hepatitis who are going to respond to steroids typically demonstrate a reduction in bilirubin within the first week, according to Dr. Mullen. He cautioned that continuing steroids in the absence of a change in bilirubin should be weighed again potential harms, including the exacerbation of liver disease or comorbidities. Even in responders, he recommended no more than 3 weeks to preserve a favorable benefit-to-risk ratio.
“Four weeks may be too long,” Dr. Mullen advised, but he also suggested that the management of advanced alcoholic hepatitis may be best left to specialists.
“Patients with severe alcoholic hepatitis should be referred and the referral should be to a hepatologist accustomed to managing these patients,” said Dr. Mullen, who cautioned that this is a challenging disease. “We have not been making a huge amount of progress” in the treatment of alcoholic hepatitis, which can be a frustrating disease because of alcoholic recidivism and poor prognosis in advanced stages, he said.
“I would argue that severe alcoholic liver disease has been one of the barriers for recruiting physicians into hepatology, because it is a very arduous group of people to look after, they get very sick, and the treatments are often not very successful,” he noted.
Global Academy and this news organization are owned by the same company. Dr. Mullen had no disclosures to report.
PHILADELPHIA – The main lesson for discordant data regarding the benefit of corticosteroids for alcoholic hepatitis is that mortality reductions accrue only to those patients who have advanced hepatitis but have not yet developed end-stage disease, according to a detailed look at published studies presented at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
The relative benefit even in appropriate candidates is modest, according to Kevin Mullen, MD, chief of digestive diseases, West Virginia University, Morgantown. By his calculations, there is a survival benefit for one of every five to seven patients treated, and that survival benefit endures only 6-12 months.
These calculations were extrapolated from a long list of studies published over the last 45 years, some of the largest of which concluded that steroids are ineffective, according to Dr. Mullen. The likely source of the conflicting data is the timing of steroids over the course of the disease and the disparity in the scales used to define severity.
Of the scales employed to select candidates for steroid therapy, the Maddrey Discriminant Function (MDF) may be the best supported, according to Dr. Mullen. He suggested that other options, such as the MELD (Model for End-Stage Liver Disease) score and the presence or absence of hepatic encephalopathy are also likely to have discriminatory value in selecting patients for steroid therapy, but these have been largely evaluated in retrospective studies using disparate methodologies.
“The problem arises from so many trials using different criteria for patient selection,” Dr. Mullen explained.
Nevertheless, drawing on the preponderance of data, Dr. Mullen concluded that there is likely to be a therapeutic window within which steroids are beneficial. Using one prednisolone study that stratified patients by MDF score to illustrate this point, he noted that 6-month survival on active therapy was no better than placebo in patients with an MDF less than 25 and numerically but not necessarily clinically significantly better in those scoring 25-34. In the groups with an MDF score of 35-44 or 44-54, the survival at 6 months was several times higher (greater than 60% vs. less than 20%), but there was no advantage with scores greater than 54. In this latter group, the mortality rate at 6 months was 100% in those receiving steroids but only 80% among those given placebo.
“In my mind, there is no question that steroids can be of benefit, but it is a question of picking the right patient. If steroids are given too late in the disease process, it can exacerbate end-stage problems, leading to death,” Dr. Mullen said.
The potential mechanisms of benefit from steroids in alcoholic hepatitis include a reduction in collagen formation and an increase in albumin production, according to Dr. Mullen. In addition, steroids have the potential to suppress the cytokine-mediated inflammation that drives progressive liver dysfunction. However, steroids also have the potential of exacerbating existing infections by suppressing immune function. Moreover, he cautioned that steroids are contraindicated in patients with gastrointestinal bleeding or pancreatitis.
Importantly, patients with alcoholic hepatitis who are going to respond to steroids typically demonstrate a reduction in bilirubin within the first week, according to Dr. Mullen. He cautioned that continuing steroids in the absence of a change in bilirubin should be weighed again potential harms, including the exacerbation of liver disease or comorbidities. Even in responders, he recommended no more than 3 weeks to preserve a favorable benefit-to-risk ratio.
“Four weeks may be too long,” Dr. Mullen advised, but he also suggested that the management of advanced alcoholic hepatitis may be best left to specialists.
“Patients with severe alcoholic hepatitis should be referred and the referral should be to a hepatologist accustomed to managing these patients,” said Dr. Mullen, who cautioned that this is a challenging disease. “We have not been making a huge amount of progress” in the treatment of alcoholic hepatitis, which can be a frustrating disease because of alcoholic recidivism and poor prognosis in advanced stages, he said.
“I would argue that severe alcoholic liver disease has been one of the barriers for recruiting physicians into hepatology, because it is a very arduous group of people to look after, they get very sick, and the treatments are often not very successful,” he noted.
Global Academy and this news organization are owned by the same company. Dr. Mullen had no disclosures to report.
Liver disease likely to become increasing indication for bariatric surgery
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
PHILADELPHIA – There is a long list of benefits from bariatric surgery in the morbidly obese, but prevention of end-stage liver disease and the need for a first or second liver transplant is likely to grow as an indication, according to an overview of weight loss surgery at Digestive Diseases: New Advances, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education.
“Bariatric surgery is associated with significant improvement not just in diabetes, dyslipidemia, hypertension, and other complications of metabolic disorders but for me more interestingly, it is effective for treating fatty liver disease where you can see a 90% improvement in steatosis,” reported Subhashini Ayloo, MD, chief of minimally invasive robotic hepato-pancreato-biliary surgery and liver transplantation at New Jersey Medical School, Newark.
Trained in both bariatric surgery and liver transplant, Dr. Ayloo predicts that these fields will become increasingly connected because of the obesity epidemic and the related rise in nonalcoholic fatty liver disease (NAFLD). Dr. Ayloo reported that bariatric surgery is already being used in her center to avoid a second liver transplant in obese patients who are unable to lose sufficient weight to prevent progressive NAFLD after a first transplant.
The emphasis Dr. Ayloo placed on the role of bariatric surgery in preventing progression of NAFLD to nonalcoholic steatohepatitis and the inflammatory process that leads to fibrosis, cirrhosis, and liver decompensation, was drawn from her interest in these two fields. However, she did not ignore the potential of protection from obesity control for other diseases.
“Obesity adversely affects every organ in the body,” Dr. Ayloo pointed out. As a result of weight loss achieved with bariatric surgery, there is now a large body of evidence supporting broad benefits, not just those related to fat deposited in hepatocytes.
“We have a couple of decades of experience that has been published [with bariatric surgery], and this has shown that it maintains weight loss long term, it improves all the obesity-associated comorbidities, and it is cost effective,” Dr. Ayloo said. Now with long-term follow-up, “all of the studies are showing that bariatric surgery improves survival.”
Although most of the survival data have been generated by retrospective cohort studies, Dr. Ayloo cited nine sets of data showing odds ratios associating bariatric surgery with up to a 90% reduction in death over periods of up to 10 years of follow-up. In a summary slide presented by Dr. Ayloo, the estimated mortality benefit over 5 years was listed as 85%. The same summary slide listed large improvements in relevant measures of morbidity for more than 10 organ systems, such as improvement or resolution of dyslipidemia and hypertension in the circulatory system, improvement or resolution of asthma and other diseases affecting the respiratory system, and resolution or improvement of gastroesophageal reflux disease and other diseases affecting the gastrointestinal system.
Specific to the liver, these benefits included a nearly 40% reduction in liver inflammation and 20% reduction in fibrosis. According to Dr. Ayloo, who noted that NAFLD is expected to overtake hepatitis C virus as the No. 1 cause of liver transplant within the next 5 years, these data are important for drawing attention to bariatric surgery as a strategy to control liver disease. She suggested that there is a need to create a tighter link between efforts to treat morbid obesity and advanced liver disease.
“There is an established literature showing that if somebody is morbidly obese, the rate of liver transplant is lower than when compared to patients with normal weight,” Dr. Ayloo said. “There is a call out in the transplant community that we need to address this and we cannot just be throwing this under the table.”
Because of the strong relationship between obesity and NAFLD, a systematic approach is needed to consider liver disease in obese patients and obesity in patients with liver disease, she said. The close relationship is relevant when planning interventions for either. Liver disease should be assessed prior to bariatric surgery regardless of the indication and then monitored closely as part of postoperative care, she said.
Dr. Ayloo identified weight control as an essential part of posttransplant care to prevent hepatic fat deposition that threatens transplant-free survival.
Global Academy and this news organization are owned by the same company. Dr. Ayloo reports no relevant financial relationships.
PPI-responsive eosinophilic esophagitis may be misnomer
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
PHILADELPHIA – Eosinophilic esophagitis (EoE) responsive to a proton pump inhibitor (PPI) has been characterized as PPI-responsive esophageal eosinophilia (PPI-REE), but there is no compelling evidence that it is a distinct EoE subgroup, according to an expert who updated current thinking about this disease at Digestive Diseases: New Advances.
“Multivariate analyses have not identified any feature that distinguishes PPI-REE from EoE. Why? Because they are probably the same disorder,” reported Stuart J. Spechler, MD, AGAF, codirector of the center for esophageal diseases at Baylor University Medical Center at Dallas.
Although it is true that only a subset of EoE patients respond to PPIs, few therapies are effective for all patients in any disease Dr. Spechler observed. As an example, he noted that ulcerative colitis patients who respond to sulfasalazine are not subclassified as sulfasalazine-responsive ulcerative colitis.
“I do think the term PPI-REE should be retired, although I acknowledge that not everyone in this field is ready to agree,” Dr. Spechler said at the meeting, held by Rutgers, the State University of New Jersey, and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
The confusion regarding PPI responsiveness in EoE has been driven by the fact that acid control has been widely regarded as the only pertinent mechanism of action from PPIs. Although coexisting gastroesophageal reflux disease could explain symptom relief in some patients with EoE, no evidence of excess acid is found in many responders. Detailed evaluations of the PPI-REE subgroup relative to EOE overall emphasize this point, according to Dr. Spechler.
“Studies have shown that the clinical, endoscopic, histologic, and gene expression features of these two disorders are identical,” he reported.
The lack of distinction is now easier to understand with a growing body of evidence that PPIs have acid-independent effects relevant to benefit in EoE, according to Dr. Spechler. Tracing the advances in understanding the pathogenesis in EoE since it was first described in 1978, Dr. Spechler explained that EoE is now understood to be an antigen-driven expression of food allergy related to up-regulation of the Th2 helper adaptive response. After briefly reviewing several potential anti-inflammatory effects of PPIs, Dr. Spechler focused on evidence that PPIs inhibit the adhesion molecule eotaxin-3.
Specifically, when squamous cells from EoE patients are exposed to the cytokine interleukin-4 (IL-4), “production of eotaxin-3 is increased dramatically but you can block that cytokine Th2 stimulation with [the PPI] omeprazole,” said Dr. Spechler, citing published work by Edaire Cheng, MD, a researcher with whom he has collaborated at the University of Texas Southwestern Medical School, Dallas. This is a potentially important observation, because up-regulation of eotaxin-3 is considered a critical molecular event for the activation of eosinophils and their migration.
The relative importance of this specific mechanism for explaining the benefits of PPIs in EoE requires additional confirmation, but Dr. Spechler indicated that there is strong evidence of acid-independent effects from PPIs. In fact, in outlining an algorithm for treatment of EoE, he listed a trial of PPIs as a reasonable first choice.
“In my opinion, the major reason that we created an arbitrary distinction is this persistent notion that acid inhibition is the only possible therapeutic effect of PPIs,” Dr. Spechler reported. “I hope I have convinced you otherwise.”
In his brief update of EoE treatment in 2017, Dr. Spechler identified a trial of PPIs as first line “simply because they work.” However PPIs have been rendered even more attractive by the evidence of a plausible mechanism of action in EoE. Conversely, he cautioned that steroids are “just a band-aid” because “they cover up the allergy but the allergy remains.” Ultimately, while PPIs are a reasonable first-line therapy to control symptoms, Dr. Spechler suggested that elimination diets are ultimately the best strategy for treating the underlying cause of EoE.
Dr. Spechler reported a financial relationship with Ironwood Pharmaceuticals.
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES