User login
New oral anti-angiogenic agent slows metastatic CRC progression
SAN FRANCISCO – Famitinib, a novel oral anti-angiogenic agent, prolongs progression-free survival by 1.3 months in patients with metastatic colorectal cancer when given alone as third- or later-line therapy, in a randomized phase II trial.
“This trial reached its primary endpoint,” co–principal investigator Dr. Rui-hua Xu of Sun Yat-Sen University Cancer Center, Guangzhou, China, said at the annual Gastrointestinal Cancers Symposium, sponsored by the American Society of Clinical Oncology.
“Famitinib demonstrated a similar safety profile with other small-molecule anti-VEGFR [vascular endothelial growth factor receptor] agents,” he said.
There was no significant improvement in overall survival, however, although analyses suggested a possible trend toward benefit in the subset of patients with more heavily pretreated disease.
Invited discussant Dr. Wafik S. El-Deiry, professor and the Deputy Cancer Center Director for Translational Research at Fox Chase Cancer Center, Philadelphia, noted that the patients’ previous targeted therapies were not well described. “It is clear that a significant number of patients did get cetuximab [Erbitux] and bevacizumab [Avastin], but the breakdown was not mentioned,” he elaborated.
He compared the trial with the similar CORRECT trial, which led to approval by the Food and Drug Administration of regorafenib (Stivarga) for metastatic colorectal cancer. In that trial, regorafenib monotherapy yielded a progression-free survival benefit of 1.9 months, as well as an overall survival benefit.
“Subgroup analyses supported an impact of regorafenib on overall survival including KRAS-mutant colorectal cancer,” Dr. El-Deiry noted. “The lack of demonstrated efficacy on overall survival by famitinib may be aided if biomarkers are developed or if it is combined with other agents ... I can’t overemphasize the need to develop and incorporate biomarkers so we can learn.
“Famitinib is not better in third line than approved regimens,” he concluded. “However, randomized comparisons or combination regimens may or may not in the future show improved or better outcomes. There is potential for pushing the doses.”
Patients were eligible for the trial if they had experienced failure of at least two prior lines of standard chemotherapy. They were ineligible if they had previously received a tyrosine kinase inhibitor targeting VEGF, had proteinuria or uncontrolled hypertension, or had a tendency for gastrointestinal bleeding.
A total of 154 patients were randomized in 2:1 ratio to double-blind treatment with either single-agent famitinib – a multitargeted tyrosine kinase inhibitor that mainly targets the vascular endothelial growth factor receptor 2 (VEGFR2), c-Kit, and the platelet-derived growth factor receptor (PDGFR) – or placebo, each taken once daily.
Results showed that median progression-free survival was 2.8 months with famitinib versus 1.5 months with placebo (hazard ratio, 0.59; P = .0053), Dr. Xu reported. Findings were similar across subgroups. There was no significant difference in overall survival, which stood at about 7.5 months in each group. The overall response rate was statistically indistinguishable between groups, but the famitinib group had a higher disease control rate (59% vs. 31%, P = .0016).
There was no significant difference in quality of life, according to Dr. Xu, who disclosed that he had no relevant conflicts of interest.
Patients treated with famitinib had a higher rate of grade 3 or worse drug-related adverse events (46% vs. 20%) and drug-related adverse events leading to treatment discontinuation (13% vs. 5%).
The main grade 3 or 4 adverse events in the famitinib group were hypertension (11%), thrombocytopenia (10%), hand-foot syndrome (10%), and neutropenia (9%).
SAN FRANCISCO – Famitinib, a novel oral anti-angiogenic agent, prolongs progression-free survival by 1.3 months in patients with metastatic colorectal cancer when given alone as third- or later-line therapy, in a randomized phase II trial.
“This trial reached its primary endpoint,” co–principal investigator Dr. Rui-hua Xu of Sun Yat-Sen University Cancer Center, Guangzhou, China, said at the annual Gastrointestinal Cancers Symposium, sponsored by the American Society of Clinical Oncology.
“Famitinib demonstrated a similar safety profile with other small-molecule anti-VEGFR [vascular endothelial growth factor receptor] agents,” he said.
There was no significant improvement in overall survival, however, although analyses suggested a possible trend toward benefit in the subset of patients with more heavily pretreated disease.
Invited discussant Dr. Wafik S. El-Deiry, professor and the Deputy Cancer Center Director for Translational Research at Fox Chase Cancer Center, Philadelphia, noted that the patients’ previous targeted therapies were not well described. “It is clear that a significant number of patients did get cetuximab [Erbitux] and bevacizumab [Avastin], but the breakdown was not mentioned,” he elaborated.
He compared the trial with the similar CORRECT trial, which led to approval by the Food and Drug Administration of regorafenib (Stivarga) for metastatic colorectal cancer. In that trial, regorafenib monotherapy yielded a progression-free survival benefit of 1.9 months, as well as an overall survival benefit.
“Subgroup analyses supported an impact of regorafenib on overall survival including KRAS-mutant colorectal cancer,” Dr. El-Deiry noted. “The lack of demonstrated efficacy on overall survival by famitinib may be aided if biomarkers are developed or if it is combined with other agents ... I can’t overemphasize the need to develop and incorporate biomarkers so we can learn.
“Famitinib is not better in third line than approved regimens,” he concluded. “However, randomized comparisons or combination regimens may or may not in the future show improved or better outcomes. There is potential for pushing the doses.”
Patients were eligible for the trial if they had experienced failure of at least two prior lines of standard chemotherapy. They were ineligible if they had previously received a tyrosine kinase inhibitor targeting VEGF, had proteinuria or uncontrolled hypertension, or had a tendency for gastrointestinal bleeding.
A total of 154 patients were randomized in 2:1 ratio to double-blind treatment with either single-agent famitinib – a multitargeted tyrosine kinase inhibitor that mainly targets the vascular endothelial growth factor receptor 2 (VEGFR2), c-Kit, and the platelet-derived growth factor receptor (PDGFR) – or placebo, each taken once daily.
Results showed that median progression-free survival was 2.8 months with famitinib versus 1.5 months with placebo (hazard ratio, 0.59; P = .0053), Dr. Xu reported. Findings were similar across subgroups. There was no significant difference in overall survival, which stood at about 7.5 months in each group. The overall response rate was statistically indistinguishable between groups, but the famitinib group had a higher disease control rate (59% vs. 31%, P = .0016).
There was no significant difference in quality of life, according to Dr. Xu, who disclosed that he had no relevant conflicts of interest.
Patients treated with famitinib had a higher rate of grade 3 or worse drug-related adverse events (46% vs. 20%) and drug-related adverse events leading to treatment discontinuation (13% vs. 5%).
The main grade 3 or 4 adverse events in the famitinib group were hypertension (11%), thrombocytopenia (10%), hand-foot syndrome (10%), and neutropenia (9%).
SAN FRANCISCO – Famitinib, a novel oral anti-angiogenic agent, prolongs progression-free survival by 1.3 months in patients with metastatic colorectal cancer when given alone as third- or later-line therapy, in a randomized phase II trial.
“This trial reached its primary endpoint,” co–principal investigator Dr. Rui-hua Xu of Sun Yat-Sen University Cancer Center, Guangzhou, China, said at the annual Gastrointestinal Cancers Symposium, sponsored by the American Society of Clinical Oncology.
“Famitinib demonstrated a similar safety profile with other small-molecule anti-VEGFR [vascular endothelial growth factor receptor] agents,” he said.
There was no significant improvement in overall survival, however, although analyses suggested a possible trend toward benefit in the subset of patients with more heavily pretreated disease.
Invited discussant Dr. Wafik S. El-Deiry, professor and the Deputy Cancer Center Director for Translational Research at Fox Chase Cancer Center, Philadelphia, noted that the patients’ previous targeted therapies were not well described. “It is clear that a significant number of patients did get cetuximab [Erbitux] and bevacizumab [Avastin], but the breakdown was not mentioned,” he elaborated.
He compared the trial with the similar CORRECT trial, which led to approval by the Food and Drug Administration of regorafenib (Stivarga) for metastatic colorectal cancer. In that trial, regorafenib monotherapy yielded a progression-free survival benefit of 1.9 months, as well as an overall survival benefit.
“Subgroup analyses supported an impact of regorafenib on overall survival including KRAS-mutant colorectal cancer,” Dr. El-Deiry noted. “The lack of demonstrated efficacy on overall survival by famitinib may be aided if biomarkers are developed or if it is combined with other agents ... I can’t overemphasize the need to develop and incorporate biomarkers so we can learn.
“Famitinib is not better in third line than approved regimens,” he concluded. “However, randomized comparisons or combination regimens may or may not in the future show improved or better outcomes. There is potential for pushing the doses.”
Patients were eligible for the trial if they had experienced failure of at least two prior lines of standard chemotherapy. They were ineligible if they had previously received a tyrosine kinase inhibitor targeting VEGF, had proteinuria or uncontrolled hypertension, or had a tendency for gastrointestinal bleeding.
A total of 154 patients were randomized in 2:1 ratio to double-blind treatment with either single-agent famitinib – a multitargeted tyrosine kinase inhibitor that mainly targets the vascular endothelial growth factor receptor 2 (VEGFR2), c-Kit, and the platelet-derived growth factor receptor (PDGFR) – or placebo, each taken once daily.
Results showed that median progression-free survival was 2.8 months with famitinib versus 1.5 months with placebo (hazard ratio, 0.59; P = .0053), Dr. Xu reported. Findings were similar across subgroups. There was no significant difference in overall survival, which stood at about 7.5 months in each group. The overall response rate was statistically indistinguishable between groups, but the famitinib group had a higher disease control rate (59% vs. 31%, P = .0016).
There was no significant difference in quality of life, according to Dr. Xu, who disclosed that he had no relevant conflicts of interest.
Patients treated with famitinib had a higher rate of grade 3 or worse drug-related adverse events (46% vs. 20%) and drug-related adverse events leading to treatment discontinuation (13% vs. 5%).
The main grade 3 or 4 adverse events in the famitinib group were hypertension (11%), thrombocytopenia (10%), hand-foot syndrome (10%), and neutropenia (9%).
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Famitinib is active and has manageable toxicity in patients with metastatic colorectal cancer.
Major finding: Median progression-free survival was 2.8 months with famitinib monotherapy versus 1.5 months with placebo.
Data source: A randomized phase II trial of 154 patients with previously treated metastatic colorectal cancer.
Disclosures: Dr. Xu disclosed that he had no conflicts of interest. The trial was sponsored by Jiangsu HengRui Medicine Co. Ltd.
Preoperative hepatic, regional arterial chemo nets better outcomes in early CRC
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
AT THE 2015 GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Preoperative arterial chemotherapy improves outcomes, but mainly for stage III patients.
Major finding: Five-year disease-free survival was 75% with preoperative arterial chemotherapy vs. 61% without it.
Data source: A randomized phase III trial among 688 patients undergoing curative resection of stage II or III colorectal cancer.
Disclosures: Dr. Xu disclosed that he had no relevant conflicts of interest.
New kinase inhibitor is highly active in MET-amplified gastric cancer
SAN FRANCISCO – An investigational kinase inhibitor that blocks the MET signaling pathway is highly active and well tolerated in patients with gastric and related cancers that have amplification of the MET gene, according to a trial a reported at the annual Gastrointestinal Cancers Symposium.
Nearly two-thirds of such patients in the open-label phase 1 trial had a response to AMG 337, an oral, potent, and highly selective inhibitor of c-Met, reported lead investigator Dr. Eunice L. Kwak, a medical oncologist at the Massachusetts General Hospital, Boston.
“Dramatic responses to AMG 337 were observed in a subset of patients with MET-amplified esophagogastric cancers. This demonstrates that MET amplification is an oncogenic driver in some of these cancers,” she contended at the meeting, cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology .
The dose-limiting toxicity was headache, seen at any grade in half of the entire trial population and at grade 3 or 4 in about one-tenth. “This is an interesting toxicity thought to occur because of AMG’s binding of the adenosine transporter,” Dr. Kwak noted. “Interestingly, caffeine seems to ameliorate the headaches that people experience on this trial. A cup of coffee is part of the management strategy that we use for patients who get headaches while being treated.”
In an interview, session chair Dr. Peter C. Enzinger, who is director of the Center for Esophageal and Gastric Cancer at the associated Dana-Farber Cancer Institute but did not participate in the trial, said, “Certainly, these data suggest that there are a subgroup of patients that can respond to MET inhibition. [The investigators] have used amplification, and perhaps it is that group of patients that should be considered further for this type of therapy.”
“The problem is that unfortunately, not the majority of [unselected] patients respond to this type of therapy, and until we can better select patients or find better MET inhibitors, this drug is probably going to have difficulty having a positive result in a randomized, phase III study,” he added. “It will also be pretty difficult if we are only treating patients who have amplifications to find enough patients to do a large-scale study.”
Dr. Kwak and her coinvestigators enrolled 90 adults with a variety of advanced solid cancers in the Amgen-sponsored trial. The median number of prior therapies was two.
The patients were treated according to a dose-escalation scheme with AMG 337 until progression or unacceptable toxicity, or were enrolled as part of an expansion cohort that required MET-amplified cancers (established by fluorescence in situ hybridization or next-generation sequencing) and entailed treatment with the maximum tolerated dose of 300 mg daily.
Results showed that among all 90 patients, the rate of grade 3 or 4 adverse events was 21%. The most common was headache, seen in 8%.
Just 11% of patients overall had a response according to RECIST (Response Evaluation Criteria in Solid Tumors) criteria; of note, all had tumors showing either MET amplification or MET overexpression.
Among the 13 patients who had gastric, esophageal, or gastroesophageal junction cancers with MET amplification, the response rate was 62%.
“Patients responses have been rapid. The time to response has been 4 weeks in those patients experiencing tumor shrinkage and symptomatic improvement quickly,” Dr. Kwak noted. “Patients have been on treatment sometimes for extended periods of time. … In particular, there are several patients who have been on study for approximately 2 years or more. Of note, of the nine patients who did not have MET amplification in the esophagogastric cancers, none achieved a partial response.”
On the basis of these positive findings, the investigators plan a follow-on single-arm phase II trial among patients with MET-amplified esophagogastric and other cancers, according to Dr. Kwak.
Contrasting with this trial, another presented in the same session by Dr. Manish A. Shah, an associate professor at the Cornell University in New York, had negative findings with onartuzumab, an investigational anti-MET antibody.
A total of 123 patients with HER2-negative metastatic gastroesophageal adenocarcinoma were enrolled in the randomized phase II trial, which was sponsored by Hoffmann-La Roche with collaboration of Genentech, manufacturer of the antibody. The patients were treated with the modified FOLFOX6 chemotherapy regimen plus either placebo or onartuzumab.
Results showed no significant progression-free survival benefit of onartuzumab in the trial population overall or in the patients whose tumors overexpressed MET as determined by immunohistochemistry (IHC), Dr. Shah reported. There was also no signal of benefit in any of a variety patient subgroups.
“One of the main questions of this study is how do we identify tumors that are truly MET driven. Is it IHC? Perhaps it’s amplification, or perhaps it’s something else. I think that’s the main question for MET inhibition moving forward,” commented Dr. Shah.
Dr. Enzinger, the session chair, commented, “This study I think just shows that using immunohistochemistry as a selector probably is not the ideal way of moving forward with this particular pathway, and that this drug, onartuzumab, probably shouldn’t be pursued further in this particular arena.”
Invited discussant Dr. Jaffer A. Ajani, a professor at the University of Texas MD Anderson Cancer Center, Houston, commented, “AMG 337 showed impressive cytotoxic or cytoreductive activity. Granted, it’s only 13 patients, but in 13 patients, 8 is a big number. So here we can say that the biomarker is good and the drug is good, and this should really be pursued further.”
The literature and clinical experience suggest that resistance to this agent will emerge, he added; therefore, combinations of inhibitors of MET and other pathways should be explored.
On the other hand, “antibodies that inhibit the MET receptor have not produced reliable results,” Dr. Ajani maintained, although it is unclear whether the biomarker, the antibody, or both are problematic in this case.
“The solution to the problem is to develop a conjugate—I just call it MET-BOMB – where you can take the antibody and hook it up to a [toxin-]conjugate. In this way, you can make the drug better and you can make the biomarker more relevant,” he concluded.
SAN FRANCISCO – An investigational kinase inhibitor that blocks the MET signaling pathway is highly active and well tolerated in patients with gastric and related cancers that have amplification of the MET gene, according to a trial a reported at the annual Gastrointestinal Cancers Symposium.
Nearly two-thirds of such patients in the open-label phase 1 trial had a response to AMG 337, an oral, potent, and highly selective inhibitor of c-Met, reported lead investigator Dr. Eunice L. Kwak, a medical oncologist at the Massachusetts General Hospital, Boston.
“Dramatic responses to AMG 337 were observed in a subset of patients with MET-amplified esophagogastric cancers. This demonstrates that MET amplification is an oncogenic driver in some of these cancers,” she contended at the meeting, cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology .
The dose-limiting toxicity was headache, seen at any grade in half of the entire trial population and at grade 3 or 4 in about one-tenth. “This is an interesting toxicity thought to occur because of AMG’s binding of the adenosine transporter,” Dr. Kwak noted. “Interestingly, caffeine seems to ameliorate the headaches that people experience on this trial. A cup of coffee is part of the management strategy that we use for patients who get headaches while being treated.”
In an interview, session chair Dr. Peter C. Enzinger, who is director of the Center for Esophageal and Gastric Cancer at the associated Dana-Farber Cancer Institute but did not participate in the trial, said, “Certainly, these data suggest that there are a subgroup of patients that can respond to MET inhibition. [The investigators] have used amplification, and perhaps it is that group of patients that should be considered further for this type of therapy.”
“The problem is that unfortunately, not the majority of [unselected] patients respond to this type of therapy, and until we can better select patients or find better MET inhibitors, this drug is probably going to have difficulty having a positive result in a randomized, phase III study,” he added. “It will also be pretty difficult if we are only treating patients who have amplifications to find enough patients to do a large-scale study.”
Dr. Kwak and her coinvestigators enrolled 90 adults with a variety of advanced solid cancers in the Amgen-sponsored trial. The median number of prior therapies was two.
The patients were treated according to a dose-escalation scheme with AMG 337 until progression or unacceptable toxicity, or were enrolled as part of an expansion cohort that required MET-amplified cancers (established by fluorescence in situ hybridization or next-generation sequencing) and entailed treatment with the maximum tolerated dose of 300 mg daily.
Results showed that among all 90 patients, the rate of grade 3 or 4 adverse events was 21%. The most common was headache, seen in 8%.
Just 11% of patients overall had a response according to RECIST (Response Evaluation Criteria in Solid Tumors) criteria; of note, all had tumors showing either MET amplification or MET overexpression.
Among the 13 patients who had gastric, esophageal, or gastroesophageal junction cancers with MET amplification, the response rate was 62%.
“Patients responses have been rapid. The time to response has been 4 weeks in those patients experiencing tumor shrinkage and symptomatic improvement quickly,” Dr. Kwak noted. “Patients have been on treatment sometimes for extended periods of time. … In particular, there are several patients who have been on study for approximately 2 years or more. Of note, of the nine patients who did not have MET amplification in the esophagogastric cancers, none achieved a partial response.”
On the basis of these positive findings, the investigators plan a follow-on single-arm phase II trial among patients with MET-amplified esophagogastric and other cancers, according to Dr. Kwak.
Contrasting with this trial, another presented in the same session by Dr. Manish A. Shah, an associate professor at the Cornell University in New York, had negative findings with onartuzumab, an investigational anti-MET antibody.
A total of 123 patients with HER2-negative metastatic gastroesophageal adenocarcinoma were enrolled in the randomized phase II trial, which was sponsored by Hoffmann-La Roche with collaboration of Genentech, manufacturer of the antibody. The patients were treated with the modified FOLFOX6 chemotherapy regimen plus either placebo or onartuzumab.
Results showed no significant progression-free survival benefit of onartuzumab in the trial population overall or in the patients whose tumors overexpressed MET as determined by immunohistochemistry (IHC), Dr. Shah reported. There was also no signal of benefit in any of a variety patient subgroups.
“One of the main questions of this study is how do we identify tumors that are truly MET driven. Is it IHC? Perhaps it’s amplification, or perhaps it’s something else. I think that’s the main question for MET inhibition moving forward,” commented Dr. Shah.
Dr. Enzinger, the session chair, commented, “This study I think just shows that using immunohistochemistry as a selector probably is not the ideal way of moving forward with this particular pathway, and that this drug, onartuzumab, probably shouldn’t be pursued further in this particular arena.”
Invited discussant Dr. Jaffer A. Ajani, a professor at the University of Texas MD Anderson Cancer Center, Houston, commented, “AMG 337 showed impressive cytotoxic or cytoreductive activity. Granted, it’s only 13 patients, but in 13 patients, 8 is a big number. So here we can say that the biomarker is good and the drug is good, and this should really be pursued further.”
The literature and clinical experience suggest that resistance to this agent will emerge, he added; therefore, combinations of inhibitors of MET and other pathways should be explored.
On the other hand, “antibodies that inhibit the MET receptor have not produced reliable results,” Dr. Ajani maintained, although it is unclear whether the biomarker, the antibody, or both are problematic in this case.
“The solution to the problem is to develop a conjugate—I just call it MET-BOMB – where you can take the antibody and hook it up to a [toxin-]conjugate. In this way, you can make the drug better and you can make the biomarker more relevant,” he concluded.
SAN FRANCISCO – An investigational kinase inhibitor that blocks the MET signaling pathway is highly active and well tolerated in patients with gastric and related cancers that have amplification of the MET gene, according to a trial a reported at the annual Gastrointestinal Cancers Symposium.
Nearly two-thirds of such patients in the open-label phase 1 trial had a response to AMG 337, an oral, potent, and highly selective inhibitor of c-Met, reported lead investigator Dr. Eunice L. Kwak, a medical oncologist at the Massachusetts General Hospital, Boston.
“Dramatic responses to AMG 337 were observed in a subset of patients with MET-amplified esophagogastric cancers. This demonstrates that MET amplification is an oncogenic driver in some of these cancers,” she contended at the meeting, cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology .
The dose-limiting toxicity was headache, seen at any grade in half of the entire trial population and at grade 3 or 4 in about one-tenth. “This is an interesting toxicity thought to occur because of AMG’s binding of the adenosine transporter,” Dr. Kwak noted. “Interestingly, caffeine seems to ameliorate the headaches that people experience on this trial. A cup of coffee is part of the management strategy that we use for patients who get headaches while being treated.”
In an interview, session chair Dr. Peter C. Enzinger, who is director of the Center for Esophageal and Gastric Cancer at the associated Dana-Farber Cancer Institute but did not participate in the trial, said, “Certainly, these data suggest that there are a subgroup of patients that can respond to MET inhibition. [The investigators] have used amplification, and perhaps it is that group of patients that should be considered further for this type of therapy.”
“The problem is that unfortunately, not the majority of [unselected] patients respond to this type of therapy, and until we can better select patients or find better MET inhibitors, this drug is probably going to have difficulty having a positive result in a randomized, phase III study,” he added. “It will also be pretty difficult if we are only treating patients who have amplifications to find enough patients to do a large-scale study.”
Dr. Kwak and her coinvestigators enrolled 90 adults with a variety of advanced solid cancers in the Amgen-sponsored trial. The median number of prior therapies was two.
The patients were treated according to a dose-escalation scheme with AMG 337 until progression or unacceptable toxicity, or were enrolled as part of an expansion cohort that required MET-amplified cancers (established by fluorescence in situ hybridization or next-generation sequencing) and entailed treatment with the maximum tolerated dose of 300 mg daily.
Results showed that among all 90 patients, the rate of grade 3 or 4 adverse events was 21%. The most common was headache, seen in 8%.
Just 11% of patients overall had a response according to RECIST (Response Evaluation Criteria in Solid Tumors) criteria; of note, all had tumors showing either MET amplification or MET overexpression.
Among the 13 patients who had gastric, esophageal, or gastroesophageal junction cancers with MET amplification, the response rate was 62%.
“Patients responses have been rapid. The time to response has been 4 weeks in those patients experiencing tumor shrinkage and symptomatic improvement quickly,” Dr. Kwak noted. “Patients have been on treatment sometimes for extended periods of time. … In particular, there are several patients who have been on study for approximately 2 years or more. Of note, of the nine patients who did not have MET amplification in the esophagogastric cancers, none achieved a partial response.”
On the basis of these positive findings, the investigators plan a follow-on single-arm phase II trial among patients with MET-amplified esophagogastric and other cancers, according to Dr. Kwak.
Contrasting with this trial, another presented in the same session by Dr. Manish A. Shah, an associate professor at the Cornell University in New York, had negative findings with onartuzumab, an investigational anti-MET antibody.
A total of 123 patients with HER2-negative metastatic gastroesophageal adenocarcinoma were enrolled in the randomized phase II trial, which was sponsored by Hoffmann-La Roche with collaboration of Genentech, manufacturer of the antibody. The patients were treated with the modified FOLFOX6 chemotherapy regimen plus either placebo or onartuzumab.
Results showed no significant progression-free survival benefit of onartuzumab in the trial population overall or in the patients whose tumors overexpressed MET as determined by immunohistochemistry (IHC), Dr. Shah reported. There was also no signal of benefit in any of a variety patient subgroups.
“One of the main questions of this study is how do we identify tumors that are truly MET driven. Is it IHC? Perhaps it’s amplification, or perhaps it’s something else. I think that’s the main question for MET inhibition moving forward,” commented Dr. Shah.
Dr. Enzinger, the session chair, commented, “This study I think just shows that using immunohistochemistry as a selector probably is not the ideal way of moving forward with this particular pathway, and that this drug, onartuzumab, probably shouldn’t be pursued further in this particular arena.”
Invited discussant Dr. Jaffer A. Ajani, a professor at the University of Texas MD Anderson Cancer Center, Houston, commented, “AMG 337 showed impressive cytotoxic or cytoreductive activity. Granted, it’s only 13 patients, but in 13 patients, 8 is a big number. So here we can say that the biomarker is good and the drug is good, and this should really be pursued further.”
The literature and clinical experience suggest that resistance to this agent will emerge, he added; therefore, combinations of inhibitors of MET and other pathways should be explored.
On the other hand, “antibodies that inhibit the MET receptor have not produced reliable results,” Dr. Ajani maintained, although it is unclear whether the biomarker, the antibody, or both are problematic in this case.
“The solution to the problem is to develop a conjugate—I just call it MET-BOMB – where you can take the antibody and hook it up to a [toxin-]conjugate. In this way, you can make the drug better and you can make the biomarker more relevant,” he concluded.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: AMG 337 promoted tumor regression in patients with MET-amplified esophagogastric cancers.
Major finding: The response rate was 62% among patients with MET-amplified gastric, esophageal, or gastroesophageal junction cancer.
Data source: A phase 1 trial among 90 patients with various types of advanced solid cancers.
Disclosures: Dr. Kwak disclosed that she receives research funding from Amgen. The trial was sponsored by Amgen.
Vitamin D appears protective in patients with metastatic colorectal cancer
SAN FRANCISCO – Patients with metastatic colorectal cancer fared better if they had higher pretreatment levels of vitamin D, according to a prospective analysis from a phase III trial.
On average, the 1,043 patients studied were deficient in vitamin D (25-hydroxyvitamin D), reported lead investigator Dr. Kimmie Ng of the Dana-Farber Cancer Institute, Harvard Medical School, in Boston.
The risks of adverse outcomes fell as vitamin D plasma levels rose. Relative to peers who had levels in the bottom quintile, patients who had levels in the top quintile were 21% less likely to experience progression or death and 35% less likely to die. The findings were consistent across patient subgroups.
“Our previous work has also demonstrated that metastatic colorectal cancer patients are commonly deficient in vitamin D, and this is concerning if we believe that higher levels may be beneficial,” Dr. Ng commented in a press briefing at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
However, “it’s too early to recommend vitamin D supplementation as a treatment for colon cancer,” she cautioned. “Randomized clinical trials are needed to establish causality and are currently ongoing.”
Press briefing moderator Dr. Smitha S. Krishnamurthi, medical oncologist at University Hospitals Case Medical Center, Cleveland, commented, “This study will be of great interest to patients with colorectal cancer, who frequently want to know if there is anything they can do besides chemotherapy to improve their outcomes. This study adds to the literature that suggests that vitamin D may have protective effects in preventing colorectal polyps and could help patients with colorectal cancer live longer.”
The observed benefits suggest that this vitamin may slow tumor growth or enhance the effects of chemotherapy, she proposed. “But we really need a randomized, controlled trial of vitamin D supplementation versus placebo to know if vitamin D has anticancer effects,” she agreed. “Until then, patients should have their vitamin D levels checked and undergo supplementation if needed because we know vitamin D is necessary for bone health. But it’s too soon to recommend vitamin D supplementation for anticancer effects.”
Introducing the study, Dr. Ng noted that vitamin D inhibits cell proliferation and angiogenesis, induces cell differentiation and apoptosis, and has anti-inflammatory effects. “Obviously, many of these processes are quite dysregulated in cancer, which led to the hypothesis that perhaps vitamin D has anticancer activity,” she said. Both preclinical research and epidemiologic data have indeed suggested a benefit of higher vitamin D levels in terms of preventing colorectal cancer and improving its outcome.
The investigators studied patients enrolled in CALGB 80405, a randomized, phase III trial of first-line chemotherapy plus biologics. The patients had blood drawn for 25-hydroxyvitamin D measurement and completed questionnaires about diet and lifestyle factors before starting treatment.
Results showed that the median 25-hydroxyvitamin D level in plasma was 17.2 ng/mL in the patients overall, reported Dr. Ng, who disclosed that she has a consulting or advisory role with Genentech/Roche. “This falls within the deficient range, which is typically defined as a 25-hydroxyvitamin D level less than 20 ng/mL,” she noted. When patients were split into quintiles, the median ranged from 8.0 ng/mL in the lowest to 27.5 ng/mL in the highest.
Median overall survival rose across quintiles of 25-hydroxyvitamin D levels (P = .01), from 24.5 months in the lowest to 32.6 months in the highest. After adjustment for age, sex, season, obesity, physical activity, and other potential confounders, the hazard ratio for death also fell significantly with increasing quintile of levels (P = .001). Relative to lowest-quintile peers, patients in the highest quintile had a more than one-third reduction in the risk of death (hazard ratio, 0.65).
Findings were similar for progression-free survival, with the median rising across quintiles (P = .02) from 10.1 months in the lowest to 12.2 months in the highest. The hazard ratio for progression or death fell with rising quintile (P = .01); highest-quintile patients had a more than one-fifth reduction in risk relative to lowest-quintile peers (hazard ratio, 0.79).
“We took great pains to try and control for various lifestyle factors or other indicators of poor health that may potentially explain what we found” to minimize confounding, Dr. Ng commented. “We also tried to address the issue by excluding patients who died very quickly after their blood levels of vitamin D were measured. Those tend to be the patients with the most aggressive disease and who tend to do more poorly. And even after excluding that group of patients, the persistence of the significant relationship between higher levels and survival was seen.”
The research was supported by the National Cancer Institute. Dr. Krishnamurthi had no relevant disclosures. Many of Dr. Ng’s coauthors reported financial ties to multiple companies, including Bristol-Myers Squibb, which funded the CALGB 80405 trial.
SAN FRANCISCO – Patients with metastatic colorectal cancer fared better if they had higher pretreatment levels of vitamin D, according to a prospective analysis from a phase III trial.
On average, the 1,043 patients studied were deficient in vitamin D (25-hydroxyvitamin D), reported lead investigator Dr. Kimmie Ng of the Dana-Farber Cancer Institute, Harvard Medical School, in Boston.
The risks of adverse outcomes fell as vitamin D plasma levels rose. Relative to peers who had levels in the bottom quintile, patients who had levels in the top quintile were 21% less likely to experience progression or death and 35% less likely to die. The findings were consistent across patient subgroups.
“Our previous work has also demonstrated that metastatic colorectal cancer patients are commonly deficient in vitamin D, and this is concerning if we believe that higher levels may be beneficial,” Dr. Ng commented in a press briefing at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
However, “it’s too early to recommend vitamin D supplementation as a treatment for colon cancer,” she cautioned. “Randomized clinical trials are needed to establish causality and are currently ongoing.”
Press briefing moderator Dr. Smitha S. Krishnamurthi, medical oncologist at University Hospitals Case Medical Center, Cleveland, commented, “This study will be of great interest to patients with colorectal cancer, who frequently want to know if there is anything they can do besides chemotherapy to improve their outcomes. This study adds to the literature that suggests that vitamin D may have protective effects in preventing colorectal polyps and could help patients with colorectal cancer live longer.”
The observed benefits suggest that this vitamin may slow tumor growth or enhance the effects of chemotherapy, she proposed. “But we really need a randomized, controlled trial of vitamin D supplementation versus placebo to know if vitamin D has anticancer effects,” she agreed. “Until then, patients should have their vitamin D levels checked and undergo supplementation if needed because we know vitamin D is necessary for bone health. But it’s too soon to recommend vitamin D supplementation for anticancer effects.”
Introducing the study, Dr. Ng noted that vitamin D inhibits cell proliferation and angiogenesis, induces cell differentiation and apoptosis, and has anti-inflammatory effects. “Obviously, many of these processes are quite dysregulated in cancer, which led to the hypothesis that perhaps vitamin D has anticancer activity,” she said. Both preclinical research and epidemiologic data have indeed suggested a benefit of higher vitamin D levels in terms of preventing colorectal cancer and improving its outcome.
The investigators studied patients enrolled in CALGB 80405, a randomized, phase III trial of first-line chemotherapy plus biologics. The patients had blood drawn for 25-hydroxyvitamin D measurement and completed questionnaires about diet and lifestyle factors before starting treatment.
Results showed that the median 25-hydroxyvitamin D level in plasma was 17.2 ng/mL in the patients overall, reported Dr. Ng, who disclosed that she has a consulting or advisory role with Genentech/Roche. “This falls within the deficient range, which is typically defined as a 25-hydroxyvitamin D level less than 20 ng/mL,” she noted. When patients were split into quintiles, the median ranged from 8.0 ng/mL in the lowest to 27.5 ng/mL in the highest.
Median overall survival rose across quintiles of 25-hydroxyvitamin D levels (P = .01), from 24.5 months in the lowest to 32.6 months in the highest. After adjustment for age, sex, season, obesity, physical activity, and other potential confounders, the hazard ratio for death also fell significantly with increasing quintile of levels (P = .001). Relative to lowest-quintile peers, patients in the highest quintile had a more than one-third reduction in the risk of death (hazard ratio, 0.65).
Findings were similar for progression-free survival, with the median rising across quintiles (P = .02) from 10.1 months in the lowest to 12.2 months in the highest. The hazard ratio for progression or death fell with rising quintile (P = .01); highest-quintile patients had a more than one-fifth reduction in risk relative to lowest-quintile peers (hazard ratio, 0.79).
“We took great pains to try and control for various lifestyle factors or other indicators of poor health that may potentially explain what we found” to minimize confounding, Dr. Ng commented. “We also tried to address the issue by excluding patients who died very quickly after their blood levels of vitamin D were measured. Those tend to be the patients with the most aggressive disease and who tend to do more poorly. And even after excluding that group of patients, the persistence of the significant relationship between higher levels and survival was seen.”
The research was supported by the National Cancer Institute. Dr. Krishnamurthi had no relevant disclosures. Many of Dr. Ng’s coauthors reported financial ties to multiple companies, including Bristol-Myers Squibb, which funded the CALGB 80405 trial.
SAN FRANCISCO – Patients with metastatic colorectal cancer fared better if they had higher pretreatment levels of vitamin D, according to a prospective analysis from a phase III trial.
On average, the 1,043 patients studied were deficient in vitamin D (25-hydroxyvitamin D), reported lead investigator Dr. Kimmie Ng of the Dana-Farber Cancer Institute, Harvard Medical School, in Boston.
The risks of adverse outcomes fell as vitamin D plasma levels rose. Relative to peers who had levels in the bottom quintile, patients who had levels in the top quintile were 21% less likely to experience progression or death and 35% less likely to die. The findings were consistent across patient subgroups.
“Our previous work has also demonstrated that metastatic colorectal cancer patients are commonly deficient in vitamin D, and this is concerning if we believe that higher levels may be beneficial,” Dr. Ng commented in a press briefing at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
However, “it’s too early to recommend vitamin D supplementation as a treatment for colon cancer,” she cautioned. “Randomized clinical trials are needed to establish causality and are currently ongoing.”
Press briefing moderator Dr. Smitha S. Krishnamurthi, medical oncologist at University Hospitals Case Medical Center, Cleveland, commented, “This study will be of great interest to patients with colorectal cancer, who frequently want to know if there is anything they can do besides chemotherapy to improve their outcomes. This study adds to the literature that suggests that vitamin D may have protective effects in preventing colorectal polyps and could help patients with colorectal cancer live longer.”
The observed benefits suggest that this vitamin may slow tumor growth or enhance the effects of chemotherapy, she proposed. “But we really need a randomized, controlled trial of vitamin D supplementation versus placebo to know if vitamin D has anticancer effects,” she agreed. “Until then, patients should have their vitamin D levels checked and undergo supplementation if needed because we know vitamin D is necessary for bone health. But it’s too soon to recommend vitamin D supplementation for anticancer effects.”
Introducing the study, Dr. Ng noted that vitamin D inhibits cell proliferation and angiogenesis, induces cell differentiation and apoptosis, and has anti-inflammatory effects. “Obviously, many of these processes are quite dysregulated in cancer, which led to the hypothesis that perhaps vitamin D has anticancer activity,” she said. Both preclinical research and epidemiologic data have indeed suggested a benefit of higher vitamin D levels in terms of preventing colorectal cancer and improving its outcome.
The investigators studied patients enrolled in CALGB 80405, a randomized, phase III trial of first-line chemotherapy plus biologics. The patients had blood drawn for 25-hydroxyvitamin D measurement and completed questionnaires about diet and lifestyle factors before starting treatment.
Results showed that the median 25-hydroxyvitamin D level in plasma was 17.2 ng/mL in the patients overall, reported Dr. Ng, who disclosed that she has a consulting or advisory role with Genentech/Roche. “This falls within the deficient range, which is typically defined as a 25-hydroxyvitamin D level less than 20 ng/mL,” she noted. When patients were split into quintiles, the median ranged from 8.0 ng/mL in the lowest to 27.5 ng/mL in the highest.
Median overall survival rose across quintiles of 25-hydroxyvitamin D levels (P = .01), from 24.5 months in the lowest to 32.6 months in the highest. After adjustment for age, sex, season, obesity, physical activity, and other potential confounders, the hazard ratio for death also fell significantly with increasing quintile of levels (P = .001). Relative to lowest-quintile peers, patients in the highest quintile had a more than one-third reduction in the risk of death (hazard ratio, 0.65).
Findings were similar for progression-free survival, with the median rising across quintiles (P = .02) from 10.1 months in the lowest to 12.2 months in the highest. The hazard ratio for progression or death fell with rising quintile (P = .01); highest-quintile patients had a more than one-fifth reduction in risk relative to lowest-quintile peers (hazard ratio, 0.79).
“We took great pains to try and control for various lifestyle factors or other indicators of poor health that may potentially explain what we found” to minimize confounding, Dr. Ng commented. “We also tried to address the issue by excluding patients who died very quickly after their blood levels of vitamin D were measured. Those tend to be the patients with the most aggressive disease and who tend to do more poorly. And even after excluding that group of patients, the persistence of the significant relationship between higher levels and survival was seen.”
The research was supported by the National Cancer Institute. Dr. Krishnamurthi had no relevant disclosures. Many of Dr. Ng’s coauthors reported financial ties to multiple companies, including Bristol-Myers Squibb, which funded the CALGB 80405 trial.
AT THE 2015 GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Patients with higher 25-hydroxyvitamin D levels had better progression-free and overall survival.
Major finding: Median survival was 8 months longer for patients with top- versus bottom-quintile 25-hydroxyvitamin D levels.
Data source: A prospective analysis from a phase III trial among 1,043 patients with untreated metastatic colorectal cancer.
Disclosures: The research was supported by the National Cancer Institute. Dr. Ng disclosed that she has a consulting or advisory role with Genentech/Roche, and many of her coauthors reported financial ties to multiple companies, including Bristol-Myers Squibb, which funded the CALGB 80405 trial. Dr. Krishnamurthi had no relevant disclosures.
Ramucirumab may expand treatment options for metastatic colorectal cancer
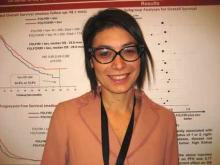
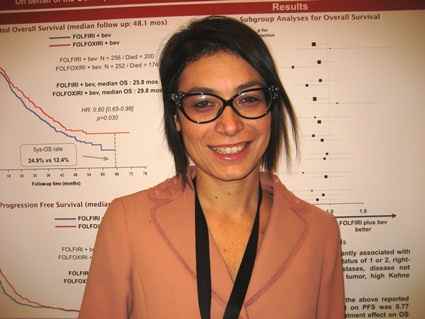
Adding the antiangiogenic antibody ramucirumab to second-line therapy for metastatic colorectal cancer improves outcomes with acceptable toxicity, according to results of a randomized, phase III trial that will be reported this week at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
Researchers led by Dr. Josep Tabernero, director of the Vall d’Hebron Institute of Oncology in Barcelona, enrolled 1,072 patients with metastatic colorectal cancer that had progressed after receipt of first-line therapy containing bevacizumab (Avastin).
They randomized the patients evenly to receive FOLFIRI (folinic acid, 5-fluorouracil, and irinotecan) chemotherapy plus either placebo or ramucirumab (Cyramza), an antibody to vascular endothelial growth factor receptor 2 (VEGFR-2) that is approved by the Food and Drug Administration for treatment of advanced stomach, gastroesophageal junction, and non–small cell lung cancers.
Main results showed that relative to the placebo group, the ramucirumab group had superior overall survival (median 13.3 vs. 11.7 months; hazard ratio, 0.84; P = .022), the primary endpoint, and progression-free survival (median 5.7 vs. 4.5 months; HR, 0.79; P = .0005).
The survival benefit was similar across patients stratified by various clinical and disease factors, including tumor KRAS mutational status and time to progression after first-line therapy, Dr. Tabernero reported.
Patients in the ramucirumab group had higher rates of certain grade 3 and 4 adverse events, most commonly neutropenia, fatigue, diarrhea, and hypertension. But the rate of febrile neutropenia was similar for the ramucirumab and placebo groups (3.6% vs. 2.7%).
The trial, known as RAISE (A Randomized, Double-blind, Multicenter Phase III Study of Irinotecan, Folinic Acid, and 5-Fluorouracil [FOLFIRI] Plus Ramucirumab or Placebo in Patients With Metastatic Colorectal Carcinoma Progressive During or Following First-Line Combination Therapy With Bevacizumab, Oxaliplatin, and a Fluoropyrimidine), was sponsored by Eli Lilly and Company.
“The RAISE study met its primary endpoint,” Dr. Tabernero said in a press briefing held before the symposium. “The combination of ramucirumab and FOLFIRI was well tolerated, and overall, the adverse events that patients presented with were manageable.”
“The RAISE study clearly demonstrates that sustained inhibition of the angiogenesis pathway from first-line to second-line metastatic colorectal cancer improves survival in a clinically representative metastatic colorectal cancer population,” he added. “Therefore, ramucirumab is an effective new treatment option for second-line treatment, including patients with poor prognosis.”
“This is the first randomized study indicating activity for ramucirumab in colorectal cancer,” noted press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland. “It’s always exciting to have a new active drug for our patients.”
Ramucirumab now adds to the options of continuing bevacizumab and switching to ziv-aflibercept (Zaltrap) as a component of second-line therapy when patients have a failure of bevacizumab-containing first-line therapy, she said. Oncologists in the United States typically continue bevacizumab, likely because patients are familiar with this agent and presumably tolerating it, but emerging data may establish differing safety and/or efficacy profiles that could shift practice patterns.
“All of these approaches have had a similar increase in survival. It will be interesting to see the effect of ramucirumab in other randomized studies and settings for colorectal cancer,” she added.
Dr. Krishnamurthi acknowledged that the absolute gain in survival with ramucirumab in RAISE was modest. “We’d like the results to be even stronger, but what we find with our patients with colorectal cancer is that as they get exposed to all of our active drugs; it does translate into them living longer,” she said. “So I understand 1.5 months is not a long time, but we want to offer everything that we can to our patients, especially because these agents tend to be well tolerated and can be easily combined with chemotherapy.”
Adding the antiangiogenic antibody ramucirumab to second-line therapy for metastatic colorectal cancer improves outcomes with acceptable toxicity, according to results of a randomized, phase III trial that will be reported this week at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
Researchers led by Dr. Josep Tabernero, director of the Vall d’Hebron Institute of Oncology in Barcelona, enrolled 1,072 patients with metastatic colorectal cancer that had progressed after receipt of first-line therapy containing bevacizumab (Avastin).
They randomized the patients evenly to receive FOLFIRI (folinic acid, 5-fluorouracil, and irinotecan) chemotherapy plus either placebo or ramucirumab (Cyramza), an antibody to vascular endothelial growth factor receptor 2 (VEGFR-2) that is approved by the Food and Drug Administration for treatment of advanced stomach, gastroesophageal junction, and non–small cell lung cancers.
Main results showed that relative to the placebo group, the ramucirumab group had superior overall survival (median 13.3 vs. 11.7 months; hazard ratio, 0.84; P = .022), the primary endpoint, and progression-free survival (median 5.7 vs. 4.5 months; HR, 0.79; P = .0005).
The survival benefit was similar across patients stratified by various clinical and disease factors, including tumor KRAS mutational status and time to progression after first-line therapy, Dr. Tabernero reported.
Patients in the ramucirumab group had higher rates of certain grade 3 and 4 adverse events, most commonly neutropenia, fatigue, diarrhea, and hypertension. But the rate of febrile neutropenia was similar for the ramucirumab and placebo groups (3.6% vs. 2.7%).
The trial, known as RAISE (A Randomized, Double-blind, Multicenter Phase III Study of Irinotecan, Folinic Acid, and 5-Fluorouracil [FOLFIRI] Plus Ramucirumab or Placebo in Patients With Metastatic Colorectal Carcinoma Progressive During or Following First-Line Combination Therapy With Bevacizumab, Oxaliplatin, and a Fluoropyrimidine), was sponsored by Eli Lilly and Company.
“The RAISE study met its primary endpoint,” Dr. Tabernero said in a press briefing held before the symposium. “The combination of ramucirumab and FOLFIRI was well tolerated, and overall, the adverse events that patients presented with were manageable.”
“The RAISE study clearly demonstrates that sustained inhibition of the angiogenesis pathway from first-line to second-line metastatic colorectal cancer improves survival in a clinically representative metastatic colorectal cancer population,” he added. “Therefore, ramucirumab is an effective new treatment option for second-line treatment, including patients with poor prognosis.”
“This is the first randomized study indicating activity for ramucirumab in colorectal cancer,” noted press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland. “It’s always exciting to have a new active drug for our patients.”
Ramucirumab now adds to the options of continuing bevacizumab and switching to ziv-aflibercept (Zaltrap) as a component of second-line therapy when patients have a failure of bevacizumab-containing first-line therapy, she said. Oncologists in the United States typically continue bevacizumab, likely because patients are familiar with this agent and presumably tolerating it, but emerging data may establish differing safety and/or efficacy profiles that could shift practice patterns.
“All of these approaches have had a similar increase in survival. It will be interesting to see the effect of ramucirumab in other randomized studies and settings for colorectal cancer,” she added.
Dr. Krishnamurthi acknowledged that the absolute gain in survival with ramucirumab in RAISE was modest. “We’d like the results to be even stronger, but what we find with our patients with colorectal cancer is that as they get exposed to all of our active drugs; it does translate into them living longer,” she said. “So I understand 1.5 months is not a long time, but we want to offer everything that we can to our patients, especially because these agents tend to be well tolerated and can be easily combined with chemotherapy.”
Adding the antiangiogenic antibody ramucirumab to second-line therapy for metastatic colorectal cancer improves outcomes with acceptable toxicity, according to results of a randomized, phase III trial that will be reported this week at the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
Researchers led by Dr. Josep Tabernero, director of the Vall d’Hebron Institute of Oncology in Barcelona, enrolled 1,072 patients with metastatic colorectal cancer that had progressed after receipt of first-line therapy containing bevacizumab (Avastin).
They randomized the patients evenly to receive FOLFIRI (folinic acid, 5-fluorouracil, and irinotecan) chemotherapy plus either placebo or ramucirumab (Cyramza), an antibody to vascular endothelial growth factor receptor 2 (VEGFR-2) that is approved by the Food and Drug Administration for treatment of advanced stomach, gastroesophageal junction, and non–small cell lung cancers.
Main results showed that relative to the placebo group, the ramucirumab group had superior overall survival (median 13.3 vs. 11.7 months; hazard ratio, 0.84; P = .022), the primary endpoint, and progression-free survival (median 5.7 vs. 4.5 months; HR, 0.79; P = .0005).
The survival benefit was similar across patients stratified by various clinical and disease factors, including tumor KRAS mutational status and time to progression after first-line therapy, Dr. Tabernero reported.
Patients in the ramucirumab group had higher rates of certain grade 3 and 4 adverse events, most commonly neutropenia, fatigue, diarrhea, and hypertension. But the rate of febrile neutropenia was similar for the ramucirumab and placebo groups (3.6% vs. 2.7%).
The trial, known as RAISE (A Randomized, Double-blind, Multicenter Phase III Study of Irinotecan, Folinic Acid, and 5-Fluorouracil [FOLFIRI] Plus Ramucirumab or Placebo in Patients With Metastatic Colorectal Carcinoma Progressive During or Following First-Line Combination Therapy With Bevacizumab, Oxaliplatin, and a Fluoropyrimidine), was sponsored by Eli Lilly and Company.
“The RAISE study met its primary endpoint,” Dr. Tabernero said in a press briefing held before the symposium. “The combination of ramucirumab and FOLFIRI was well tolerated, and overall, the adverse events that patients presented with were manageable.”
“The RAISE study clearly demonstrates that sustained inhibition of the angiogenesis pathway from first-line to second-line metastatic colorectal cancer improves survival in a clinically representative metastatic colorectal cancer population,” he added. “Therefore, ramucirumab is an effective new treatment option for second-line treatment, including patients with poor prognosis.”
“This is the first randomized study indicating activity for ramucirumab in colorectal cancer,” noted press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland. “It’s always exciting to have a new active drug for our patients.”
Ramucirumab now adds to the options of continuing bevacizumab and switching to ziv-aflibercept (Zaltrap) as a component of second-line therapy when patients have a failure of bevacizumab-containing first-line therapy, she said. Oncologists in the United States typically continue bevacizumab, likely because patients are familiar with this agent and presumably tolerating it, but emerging data may establish differing safety and/or efficacy profiles that could shift practice patterns.
“All of these approaches have had a similar increase in survival. It will be interesting to see the effect of ramucirumab in other randomized studies and settings for colorectal cancer,” she added.
Dr. Krishnamurthi acknowledged that the absolute gain in survival with ramucirumab in RAISE was modest. “We’d like the results to be even stronger, but what we find with our patients with colorectal cancer is that as they get exposed to all of our active drugs; it does translate into them living longer,” she said. “So I understand 1.5 months is not a long time, but we want to offer everything that we can to our patients, especially because these agents tend to be well tolerated and can be easily combined with chemotherapy.”
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Adding ramucirumab to second-line chemotherapy delayed progression and prolonged survival, with manageable toxicity.
Major finding: Median overall survival was 13.3 months with ramucirumab versus 11.7 months with placebo.
Data source: A randomized, phase III trial of 1,072 patients with metastatic colorectal cancer progressing after first-line therapy.
Disclosures: Dr. Tabernero disclosed that he has a consulting or advisory role with Eli Lilly, ImClone Systems, and other companies. The trial was sponsored by Eli Lilly, with collaboration of ImClone Systems.
Skipping surgery is an option for some patients with rectal cancer
Patients with locally advanced rectal cancer who have a complete response to neoadjuvant therapy can skip surgery with little compromise in outcomes, according to a retrospective review that will be reported this week at the annual Gastrointestinal Cancers Symposium.
Investigators at the Memorial Sloan-Kettering Cancer Center in New York studied 145 patients with stage I to III rectal cancer who received neoadjuvant therapy there between 2006 and 2013. The meeting was cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology
After a median follow-up of 3.5 years, there were no significant differences in disease-specific or overall survival between patients who had a clinical complete response to neoadjuvant therapy of radiation and chemotherapy and skipped surgery, and patients who underwent rectal resection (the current standard strategy in the United States) with a pathologic complete response. Additionally, more than three-fourths of the group skipping surgery had preservation of rectal function.
“Nonoperative management appears to be a safe and effective treatment strategy and achieves a high rate of rectal preservation,” senior investigator Dr. Philip B. Paty, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York, commented in a press briefing held before the symposium.
Ideally, the findings would be tested in a randomized trial, he said; however, “there’s too many factors and too much patient autonomy involved here, so that no one really believes asking people to sign up for a randomized trial where rectal resection is decided by a flip of the coin would ever accrue patients.” Short of that, rigorous prospective studies, such as a phase II trial now open at the center, will provide critical information.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “These are important findings for patients with rectal cancer because removal of the rectum can result in altered bowel habits or the need for permanent colostomy. This study set the bar very high, comparing the results of nonoperative management to the results seen in patients who had no cancer left under the microscope at the time of surgery, and in this study, the nonoperative management appears to compare favorably.”
“We do need longer follow-up though, to be sure that these patients will have disease-specific survival that equals what is achieved with surgery in the long term,” she cautioned, such as the conventional 5 years of observation patients typically receive. “And then of course a prospective study also would be helpful to see the effects of this approach.”
In the study, Dr. Paty and colleagues identified 73 patients who had a clinical complete response (no cancer detected on physical exam, endoscopy, or imaging) to neoadjuvant therapy of radiation and chemotherapy and—by mutual agreement of physician and patient—had nonoperative management (watchful waiting), consisting initially of follow-up at 3- to 4-month intervals by digital rectal and endoscopic exams and at 6-month intervals by imaging. They used as a comparison group 72 patients who underwent standard total mesorectal excision and had a pathologic complete response (no viable cancer cells found microscopically in the resected tissue).
Results showed that 74% of the patients who did not have surgery had a sustained clinical complete response, with no regrowth of tumor during follow-up, reported Dr. Paty. Among the other 26% whose tumors regrew, most of the recurrences were clinically detectable and all patients had successful resections with clean margins. Overall, 77% of the nonsurgical patients had rectal preservation and 98% had local control.
The nonsurgical group did not differ significantly from the surgical group with respect to 4-year rates of disease-specific survival (91% vs. 96%) and overall survival (91% vs. 95%).
The investigators plan to report quality of life data in the future, Dr. Paty said. “But I think it’s pretty obvious to everyone who’s managed these patients that if you can avoid rectal surgery, the quality of life and particularly bowel function is far superior to those who have had rectal resection.”
Successful nonoperative management hinges critically on careful patient selection, close follow-up, and use of salvage surgery, he stressed. Additionally, “the informed consent process in nonoperative management is extremely important, and I always tell patients that they are taking a slight risk. It’s hard to imagine that not operating is going to have 100% equivalent cancer outcomes as operating. That is hard to believe. So we never sell it as being absolutely as good, but …with good follow-up, the results seem to be very close if not equivalent.”
In his experience, most patients are willing to accept this option. “In fact, I have only had two patients [out of more than 100] decline nonoperative management when I thought they were candidates—both young, both with young children, both not wanting to take even the slightest risk of leaving cancer in the rectal wall or their body,” he commented.
Adoption of nonoperative management has been slow in the United States for a variety of reasons, according to Dr. Paty. “I think the bottom line is that practicing watch and wait, nonoperative management is more difficult for the surgeon. It requires first the judgment that the cancer’s gone. You have to follow the patient longer after radiation; sometimes the complete response will take up to 3 months. And there is also the medical-legal issue of deviating from the standard of care. … So I think it was operationally a difficult thing to do, it didn’t fit with the existing paradigm very well.”
But that is changing as more data roll in. “What’s happened in the last I will say 2-3 years is that there are centers publishing their experience, ours being the largest outside Brazil and the first in North America. Another group in the Netherlands has published a group of about 25 patients,” he explained. “Talking with people at meetings around the world, centers are adopting it, and I think that many leaders in clinical trials in rectal cancer recognize that this option is not only reasonable, but perhaps it’s necessary to inform patients that it is an option.”
Patients with locally advanced rectal cancer who have a complete response to neoadjuvant therapy can skip surgery with little compromise in outcomes, according to a retrospective review that will be reported this week at the annual Gastrointestinal Cancers Symposium.
Investigators at the Memorial Sloan-Kettering Cancer Center in New York studied 145 patients with stage I to III rectal cancer who received neoadjuvant therapy there between 2006 and 2013. The meeting was cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology
After a median follow-up of 3.5 years, there were no significant differences in disease-specific or overall survival between patients who had a clinical complete response to neoadjuvant therapy of radiation and chemotherapy and skipped surgery, and patients who underwent rectal resection (the current standard strategy in the United States) with a pathologic complete response. Additionally, more than three-fourths of the group skipping surgery had preservation of rectal function.
“Nonoperative management appears to be a safe and effective treatment strategy and achieves a high rate of rectal preservation,” senior investigator Dr. Philip B. Paty, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York, commented in a press briefing held before the symposium.
Ideally, the findings would be tested in a randomized trial, he said; however, “there’s too many factors and too much patient autonomy involved here, so that no one really believes asking people to sign up for a randomized trial where rectal resection is decided by a flip of the coin would ever accrue patients.” Short of that, rigorous prospective studies, such as a phase II trial now open at the center, will provide critical information.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “These are important findings for patients with rectal cancer because removal of the rectum can result in altered bowel habits or the need for permanent colostomy. This study set the bar very high, comparing the results of nonoperative management to the results seen in patients who had no cancer left under the microscope at the time of surgery, and in this study, the nonoperative management appears to compare favorably.”
“We do need longer follow-up though, to be sure that these patients will have disease-specific survival that equals what is achieved with surgery in the long term,” she cautioned, such as the conventional 5 years of observation patients typically receive. “And then of course a prospective study also would be helpful to see the effects of this approach.”
In the study, Dr. Paty and colleagues identified 73 patients who had a clinical complete response (no cancer detected on physical exam, endoscopy, or imaging) to neoadjuvant therapy of radiation and chemotherapy and—by mutual agreement of physician and patient—had nonoperative management (watchful waiting), consisting initially of follow-up at 3- to 4-month intervals by digital rectal and endoscopic exams and at 6-month intervals by imaging. They used as a comparison group 72 patients who underwent standard total mesorectal excision and had a pathologic complete response (no viable cancer cells found microscopically in the resected tissue).
Results showed that 74% of the patients who did not have surgery had a sustained clinical complete response, with no regrowth of tumor during follow-up, reported Dr. Paty. Among the other 26% whose tumors regrew, most of the recurrences were clinically detectable and all patients had successful resections with clean margins. Overall, 77% of the nonsurgical patients had rectal preservation and 98% had local control.
The nonsurgical group did not differ significantly from the surgical group with respect to 4-year rates of disease-specific survival (91% vs. 96%) and overall survival (91% vs. 95%).
The investigators plan to report quality of life data in the future, Dr. Paty said. “But I think it’s pretty obvious to everyone who’s managed these patients that if you can avoid rectal surgery, the quality of life and particularly bowel function is far superior to those who have had rectal resection.”
Successful nonoperative management hinges critically on careful patient selection, close follow-up, and use of salvage surgery, he stressed. Additionally, “the informed consent process in nonoperative management is extremely important, and I always tell patients that they are taking a slight risk. It’s hard to imagine that not operating is going to have 100% equivalent cancer outcomes as operating. That is hard to believe. So we never sell it as being absolutely as good, but …with good follow-up, the results seem to be very close if not equivalent.”
In his experience, most patients are willing to accept this option. “In fact, I have only had two patients [out of more than 100] decline nonoperative management when I thought they were candidates—both young, both with young children, both not wanting to take even the slightest risk of leaving cancer in the rectal wall or their body,” he commented.
Adoption of nonoperative management has been slow in the United States for a variety of reasons, according to Dr. Paty. “I think the bottom line is that practicing watch and wait, nonoperative management is more difficult for the surgeon. It requires first the judgment that the cancer’s gone. You have to follow the patient longer after radiation; sometimes the complete response will take up to 3 months. And there is also the medical-legal issue of deviating from the standard of care. … So I think it was operationally a difficult thing to do, it didn’t fit with the existing paradigm very well.”
But that is changing as more data roll in. “What’s happened in the last I will say 2-3 years is that there are centers publishing their experience, ours being the largest outside Brazil and the first in North America. Another group in the Netherlands has published a group of about 25 patients,” he explained. “Talking with people at meetings around the world, centers are adopting it, and I think that many leaders in clinical trials in rectal cancer recognize that this option is not only reasonable, but perhaps it’s necessary to inform patients that it is an option.”
Patients with locally advanced rectal cancer who have a complete response to neoadjuvant therapy can skip surgery with little compromise in outcomes, according to a retrospective review that will be reported this week at the annual Gastrointestinal Cancers Symposium.
Investigators at the Memorial Sloan-Kettering Cancer Center in New York studied 145 patients with stage I to III rectal cancer who received neoadjuvant therapy there between 2006 and 2013. The meeting was cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology
After a median follow-up of 3.5 years, there were no significant differences in disease-specific or overall survival between patients who had a clinical complete response to neoadjuvant therapy of radiation and chemotherapy and skipped surgery, and patients who underwent rectal resection (the current standard strategy in the United States) with a pathologic complete response. Additionally, more than three-fourths of the group skipping surgery had preservation of rectal function.
“Nonoperative management appears to be a safe and effective treatment strategy and achieves a high rate of rectal preservation,” senior investigator Dr. Philip B. Paty, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York, commented in a press briefing held before the symposium.
Ideally, the findings would be tested in a randomized trial, he said; however, “there’s too many factors and too much patient autonomy involved here, so that no one really believes asking people to sign up for a randomized trial where rectal resection is decided by a flip of the coin would ever accrue patients.” Short of that, rigorous prospective studies, such as a phase II trial now open at the center, will provide critical information.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “These are important findings for patients with rectal cancer because removal of the rectum can result in altered bowel habits or the need for permanent colostomy. This study set the bar very high, comparing the results of nonoperative management to the results seen in patients who had no cancer left under the microscope at the time of surgery, and in this study, the nonoperative management appears to compare favorably.”
“We do need longer follow-up though, to be sure that these patients will have disease-specific survival that equals what is achieved with surgery in the long term,” she cautioned, such as the conventional 5 years of observation patients typically receive. “And then of course a prospective study also would be helpful to see the effects of this approach.”
In the study, Dr. Paty and colleagues identified 73 patients who had a clinical complete response (no cancer detected on physical exam, endoscopy, or imaging) to neoadjuvant therapy of radiation and chemotherapy and—by mutual agreement of physician and patient—had nonoperative management (watchful waiting), consisting initially of follow-up at 3- to 4-month intervals by digital rectal and endoscopic exams and at 6-month intervals by imaging. They used as a comparison group 72 patients who underwent standard total mesorectal excision and had a pathologic complete response (no viable cancer cells found microscopically in the resected tissue).
Results showed that 74% of the patients who did not have surgery had a sustained clinical complete response, with no regrowth of tumor during follow-up, reported Dr. Paty. Among the other 26% whose tumors regrew, most of the recurrences were clinically detectable and all patients had successful resections with clean margins. Overall, 77% of the nonsurgical patients had rectal preservation and 98% had local control.
The nonsurgical group did not differ significantly from the surgical group with respect to 4-year rates of disease-specific survival (91% vs. 96%) and overall survival (91% vs. 95%).
The investigators plan to report quality of life data in the future, Dr. Paty said. “But I think it’s pretty obvious to everyone who’s managed these patients that if you can avoid rectal surgery, the quality of life and particularly bowel function is far superior to those who have had rectal resection.”
Successful nonoperative management hinges critically on careful patient selection, close follow-up, and use of salvage surgery, he stressed. Additionally, “the informed consent process in nonoperative management is extremely important, and I always tell patients that they are taking a slight risk. It’s hard to imagine that not operating is going to have 100% equivalent cancer outcomes as operating. That is hard to believe. So we never sell it as being absolutely as good, but …with good follow-up, the results seem to be very close if not equivalent.”
In his experience, most patients are willing to accept this option. “In fact, I have only had two patients [out of more than 100] decline nonoperative management when I thought they were candidates—both young, both with young children, both not wanting to take even the slightest risk of leaving cancer in the rectal wall or their body,” he commented.
Adoption of nonoperative management has been slow in the United States for a variety of reasons, according to Dr. Paty. “I think the bottom line is that practicing watch and wait, nonoperative management is more difficult for the surgeon. It requires first the judgment that the cancer’s gone. You have to follow the patient longer after radiation; sometimes the complete response will take up to 3 months. And there is also the medical-legal issue of deviating from the standard of care. … So I think it was operationally a difficult thing to do, it didn’t fit with the existing paradigm very well.”
But that is changing as more data roll in. “What’s happened in the last I will say 2-3 years is that there are centers publishing their experience, ours being the largest outside Brazil and the first in North America. Another group in the Netherlands has published a group of about 25 patients,” he explained. “Talking with people at meetings around the world, centers are adopting it, and I think that many leaders in clinical trials in rectal cancer recognize that this option is not only reasonable, but perhaps it’s necessary to inform patients that it is an option.”
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Patients with rectal cancer who have a clinical complete response to neoadjuvant therapy can safely skip surgery.
Major finding: Nonsurgical patients with clinical complete response did not differ significantly from surgical patients with pathologic complete response in terms of 4-year overall survival (91% vs. 95%) and disease-specific survival (91% vs. 96%).
Data source: A retrospective review of 145 patients given neoadjuvant therapy for stage I to III rectal cancer.
Disclosures: Dr. Paty disclosed that he had no relevant conflicts of interest.
TRIBE update: FOLFOXIRI-bevacizumab boosts survival in metastatic CRC
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Long-term survival was better with FOLFOXIRI-bevacizumab than with FOLFIRI-bevacizumab.
Major finding: Median overall survival was 29.8 months with FOLFOXIRI-bevacizumab versus 25.8 months with FOLFIRI-bevacizumab.
Data source: A randomized, phase III trial of 508 patients with newly diagnosed metastatic colorectal cancer.
Disclosures: Dr. Cremolini disclosed that she has a consulting or advisory role with Bayer and Roche, and is on the speakers’ bureau with Bayer. The trial was supported in part by a research grant from F. Hoffmann-La Roche.