User login
International Conference on Emerging Infectious Diseases (ICEID 2015)
ICEID: Surveillance program identifies enterovirus strain early
ATLANTA – Implementing surveillance programs at area hospitals is an effective tool for health care providers and public health officials to identify severe acute respiratory illness (SARI) and enterovirus specifically early.
“We do surveillance for respiratory illness [at] three sentinel sites that participate in the Minneapolis-St. Paul metro area,” explained Hannah Friedlander, an epidemiologist with the Minnesota Department of Health in St. Paul, who presented the study. “[But] our surveillance didn’t actually actively look for enterovirus, it looked for rhinovirus, which is known to cross-react with enterovirus on PCRs [polymerase chain reactions],” she said at the International Conference on Emerging Infectious Diseases
To remedy that, the surveillance program – which involves the participation of one pediatric hospital, one hospital serving both children and adults, and one primarily serving adults – added testing for enterovirus to PCRs of all SARI specimens collected from Sept. 1 through Oct. 31, 2014. In total, 363 SARI specimens were collected over that time frame, of which 100 (28%) were found to be pan-EV positive and underwent further evaluation for EV-D68. Ultimately, 64 of the EV-positive specimens were found to be EV-D68 strains.
The vast majority of cases identified as being caused by the EV-D68 strain (73%) were collected between Sept. 6 and Sept. 20.
This indicates that starting surveillance of SARI cases when enteroviruses traditionally become more frequent could allow for faster determination of which strain is most prevalent and what the optimal treatment should be.
“It’s hard to say if this was surprising because we hadn’t previously been looking for enterovirus, so we don’t have another year to compare [these] data to,” Ms. Friedlander explained. “But I think it’s surprising that we saw as much of [enterovirus] as we did.”
Most cases of EV-D68 (64, or 36%) were in patients between the ages of 5 and 11 years, with a median age of 6 years. A total of 52 (81%) EV-D68 cases presented with shortness of breath, and 31 cases (48%) presented with wheezing or cough. Hospital stays of 4 days or fewer occurred in 73% of cases, with a median stay length of 3 days; 33% of EV-D68 patients required admittance to the ICU, and 13% of EV-D68 patients were placed on a mechanical ventilator at some point during treatment.
“This fall is our third year doing this type of surveillance, so at the time the data for this [were] collected, we only had 1 year of surveillance under our belt,” explained Ms. Friedlander. “We now look prospectively for enterovirus, not EV-D68 specifically, so it’ll be interesting to see as the years go on if this was an outlier year.”
Ms. Friedlander and her coinvestigators say they hope that further SARI surveillance will shed more light on the trends of viral pathogens and the impact that these have on hospitalization rates. They implore hospital systems to not only have surveillance programs in place, but also for them to have the flexibility to include additional testing should the need for it arise. That flexibility, Ms. Friedlander said, is what proved crucial in the early identification of EV-D68 in her own study population.
This study was funded by the Council of State and Territorial Epidemiologists, and the Centers for the Disease Control and Prevention. Ms. Friedlander did not report any relevant financial disclosures.
ATLANTA – Implementing surveillance programs at area hospitals is an effective tool for health care providers and public health officials to identify severe acute respiratory illness (SARI) and enterovirus specifically early.
“We do surveillance for respiratory illness [at] three sentinel sites that participate in the Minneapolis-St. Paul metro area,” explained Hannah Friedlander, an epidemiologist with the Minnesota Department of Health in St. Paul, who presented the study. “[But] our surveillance didn’t actually actively look for enterovirus, it looked for rhinovirus, which is known to cross-react with enterovirus on PCRs [polymerase chain reactions],” she said at the International Conference on Emerging Infectious Diseases
To remedy that, the surveillance program – which involves the participation of one pediatric hospital, one hospital serving both children and adults, and one primarily serving adults – added testing for enterovirus to PCRs of all SARI specimens collected from Sept. 1 through Oct. 31, 2014. In total, 363 SARI specimens were collected over that time frame, of which 100 (28%) were found to be pan-EV positive and underwent further evaluation for EV-D68. Ultimately, 64 of the EV-positive specimens were found to be EV-D68 strains.
The vast majority of cases identified as being caused by the EV-D68 strain (73%) were collected between Sept. 6 and Sept. 20.
This indicates that starting surveillance of SARI cases when enteroviruses traditionally become more frequent could allow for faster determination of which strain is most prevalent and what the optimal treatment should be.
“It’s hard to say if this was surprising because we hadn’t previously been looking for enterovirus, so we don’t have another year to compare [these] data to,” Ms. Friedlander explained. “But I think it’s surprising that we saw as much of [enterovirus] as we did.”
Most cases of EV-D68 (64, or 36%) were in patients between the ages of 5 and 11 years, with a median age of 6 years. A total of 52 (81%) EV-D68 cases presented with shortness of breath, and 31 cases (48%) presented with wheezing or cough. Hospital stays of 4 days or fewer occurred in 73% of cases, with a median stay length of 3 days; 33% of EV-D68 patients required admittance to the ICU, and 13% of EV-D68 patients were placed on a mechanical ventilator at some point during treatment.
“This fall is our third year doing this type of surveillance, so at the time the data for this [were] collected, we only had 1 year of surveillance under our belt,” explained Ms. Friedlander. “We now look prospectively for enterovirus, not EV-D68 specifically, so it’ll be interesting to see as the years go on if this was an outlier year.”
Ms. Friedlander and her coinvestigators say they hope that further SARI surveillance will shed more light on the trends of viral pathogens and the impact that these have on hospitalization rates. They implore hospital systems to not only have surveillance programs in place, but also for them to have the flexibility to include additional testing should the need for it arise. That flexibility, Ms. Friedlander said, is what proved crucial in the early identification of EV-D68 in her own study population.
This study was funded by the Council of State and Territorial Epidemiologists, and the Centers for the Disease Control and Prevention. Ms. Friedlander did not report any relevant financial disclosures.
ATLANTA – Implementing surveillance programs at area hospitals is an effective tool for health care providers and public health officials to identify severe acute respiratory illness (SARI) and enterovirus specifically early.
“We do surveillance for respiratory illness [at] three sentinel sites that participate in the Minneapolis-St. Paul metro area,” explained Hannah Friedlander, an epidemiologist with the Minnesota Department of Health in St. Paul, who presented the study. “[But] our surveillance didn’t actually actively look for enterovirus, it looked for rhinovirus, which is known to cross-react with enterovirus on PCRs [polymerase chain reactions],” she said at the International Conference on Emerging Infectious Diseases
To remedy that, the surveillance program – which involves the participation of one pediatric hospital, one hospital serving both children and adults, and one primarily serving adults – added testing for enterovirus to PCRs of all SARI specimens collected from Sept. 1 through Oct. 31, 2014. In total, 363 SARI specimens were collected over that time frame, of which 100 (28%) were found to be pan-EV positive and underwent further evaluation for EV-D68. Ultimately, 64 of the EV-positive specimens were found to be EV-D68 strains.
The vast majority of cases identified as being caused by the EV-D68 strain (73%) were collected between Sept. 6 and Sept. 20.
This indicates that starting surveillance of SARI cases when enteroviruses traditionally become more frequent could allow for faster determination of which strain is most prevalent and what the optimal treatment should be.
“It’s hard to say if this was surprising because we hadn’t previously been looking for enterovirus, so we don’t have another year to compare [these] data to,” Ms. Friedlander explained. “But I think it’s surprising that we saw as much of [enterovirus] as we did.”
Most cases of EV-D68 (64, or 36%) were in patients between the ages of 5 and 11 years, with a median age of 6 years. A total of 52 (81%) EV-D68 cases presented with shortness of breath, and 31 cases (48%) presented with wheezing or cough. Hospital stays of 4 days or fewer occurred in 73% of cases, with a median stay length of 3 days; 33% of EV-D68 patients required admittance to the ICU, and 13% of EV-D68 patients were placed on a mechanical ventilator at some point during treatment.
“This fall is our third year doing this type of surveillance, so at the time the data for this [were] collected, we only had 1 year of surveillance under our belt,” explained Ms. Friedlander. “We now look prospectively for enterovirus, not EV-D68 specifically, so it’ll be interesting to see as the years go on if this was an outlier year.”
Ms. Friedlander and her coinvestigators say they hope that further SARI surveillance will shed more light on the trends of viral pathogens and the impact that these have on hospitalization rates. They implore hospital systems to not only have surveillance programs in place, but also for them to have the flexibility to include additional testing should the need for it arise. That flexibility, Ms. Friedlander said, is what proved crucial in the early identification of EV-D68 in her own study population.
This study was funded by the Council of State and Territorial Epidemiologists, and the Centers for the Disease Control and Prevention. Ms. Friedlander did not report any relevant financial disclosures.
AT ICEID 2015
Key clinical point: Early detection of a potential enterovirus outbreak – specifically, the EV-D68 strain – can be facilitated by adopting a severe acute respiratory infection (SARI) surveillance program.
Major finding: Of 363 SARI samples collected from surveillance programs hospitals, 100 (28%) were pan-EV positive, and 64% of those were identified as EV-D68.
Data source: Retrospective analysis of data collected from 363 SARI cases between Sept. 1, 2014, and Oct. 31, 2014, in the Minneapolis-St. Paul metropolitan area.
Disclosures: Study funded by the Council of State and Territorial Epidemiologists and the Centers for Disease Control and Prevention.
ICEID: Clothing may transmit respiratory syncytial virus in NICU
ATLANTA – Clothing worn by caregivers and visitors may be an important vehicle for the transmission of respiratory syncytial virus in the neonatal intensive care unit setting, according to findings from a prospective study conducted in an Australian hospital.
In an effort to identify potential sources of RSV transmission and to facilitate development of infection control strategies, the investigators swabbed all health personnel, every third neonate and their visitors, and any child clinically suspected of having an RSV infection. They detected RSV in one of 81 nasal specimens collected from 55 neonates and in 4% of 80 visitors’ clothing swabs, Nusrat Homaira, Ph.D., of the University of New South Wales, Sydney, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
RSV also was detected in 1% of nose swabs from the visitors and in 1% of nose swabs from 84 health care workers.
No RSV was detected on the clothing of health care workers or on the hands of visitors or health care workers, which may be explained by the presence of alcohol-based hand rub at the point of care and by prevalent hand hygiene practices within the neonatal intensive care unit (NICU), the investigators noted.
The investigators also collected environmental swabs and detected RSV on 9% of high-touch areas, including bed rails; chairs; bed surfaces; countertops; and nurse’s and doctor’s station tables, computers, and chairs.
Samples were collected once each week for 8 weeks during May and June of 2014.
RSV is a major cause of morbidity in very young children, and premature infants have a 10-fold increase in the risk of acquiring RSV infection. Hospital-acquired cases are an important cause of prolonged hospitalization, Dr. Homaira and her associates noted.
The findings suggest that personal clothing may be one of the modes of virus transmission, they said.
“Though the detection rate is low, personal clothing of caregivers/visitors do get contaminated with RSV,” Dr. Homaira said in a written statement, noting that caregivers and visitors are not required to change clothing when they walk into the NICU.
“There is a need for further research to evaluate how long the virus remains infectious on personal clothing, which will have policy implications in terms of need for use of separate gowns by the visitors while they are in the NICU,” Dr. Homaira added, concluding that frequent cleaning of high-touch areas and periodic screening of visitors for RSV as they enter the NICU during seasonal epidemics also may help limit disease transmission.
The investigators reported having no disclosures.
ATLANTA – Clothing worn by caregivers and visitors may be an important vehicle for the transmission of respiratory syncytial virus in the neonatal intensive care unit setting, according to findings from a prospective study conducted in an Australian hospital.
In an effort to identify potential sources of RSV transmission and to facilitate development of infection control strategies, the investigators swabbed all health personnel, every third neonate and their visitors, and any child clinically suspected of having an RSV infection. They detected RSV in one of 81 nasal specimens collected from 55 neonates and in 4% of 80 visitors’ clothing swabs, Nusrat Homaira, Ph.D., of the University of New South Wales, Sydney, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
RSV also was detected in 1% of nose swabs from the visitors and in 1% of nose swabs from 84 health care workers.
No RSV was detected on the clothing of health care workers or on the hands of visitors or health care workers, which may be explained by the presence of alcohol-based hand rub at the point of care and by prevalent hand hygiene practices within the neonatal intensive care unit (NICU), the investigators noted.
The investigators also collected environmental swabs and detected RSV on 9% of high-touch areas, including bed rails; chairs; bed surfaces; countertops; and nurse’s and doctor’s station tables, computers, and chairs.
Samples were collected once each week for 8 weeks during May and June of 2014.
RSV is a major cause of morbidity in very young children, and premature infants have a 10-fold increase in the risk of acquiring RSV infection. Hospital-acquired cases are an important cause of prolonged hospitalization, Dr. Homaira and her associates noted.
The findings suggest that personal clothing may be one of the modes of virus transmission, they said.
“Though the detection rate is low, personal clothing of caregivers/visitors do get contaminated with RSV,” Dr. Homaira said in a written statement, noting that caregivers and visitors are not required to change clothing when they walk into the NICU.
“There is a need for further research to evaluate how long the virus remains infectious on personal clothing, which will have policy implications in terms of need for use of separate gowns by the visitors while they are in the NICU,” Dr. Homaira added, concluding that frequent cleaning of high-touch areas and periodic screening of visitors for RSV as they enter the NICU during seasonal epidemics also may help limit disease transmission.
The investigators reported having no disclosures.
ATLANTA – Clothing worn by caregivers and visitors may be an important vehicle for the transmission of respiratory syncytial virus in the neonatal intensive care unit setting, according to findings from a prospective study conducted in an Australian hospital.
In an effort to identify potential sources of RSV transmission and to facilitate development of infection control strategies, the investigators swabbed all health personnel, every third neonate and their visitors, and any child clinically suspected of having an RSV infection. They detected RSV in one of 81 nasal specimens collected from 55 neonates and in 4% of 80 visitors’ clothing swabs, Nusrat Homaira, Ph.D., of the University of New South Wales, Sydney, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
RSV also was detected in 1% of nose swabs from the visitors and in 1% of nose swabs from 84 health care workers.
No RSV was detected on the clothing of health care workers or on the hands of visitors or health care workers, which may be explained by the presence of alcohol-based hand rub at the point of care and by prevalent hand hygiene practices within the neonatal intensive care unit (NICU), the investigators noted.
The investigators also collected environmental swabs and detected RSV on 9% of high-touch areas, including bed rails; chairs; bed surfaces; countertops; and nurse’s and doctor’s station tables, computers, and chairs.
Samples were collected once each week for 8 weeks during May and June of 2014.
RSV is a major cause of morbidity in very young children, and premature infants have a 10-fold increase in the risk of acquiring RSV infection. Hospital-acquired cases are an important cause of prolonged hospitalization, Dr. Homaira and her associates noted.
The findings suggest that personal clothing may be one of the modes of virus transmission, they said.
“Though the detection rate is low, personal clothing of caregivers/visitors do get contaminated with RSV,” Dr. Homaira said in a written statement, noting that caregivers and visitors are not required to change clothing when they walk into the NICU.
“There is a need for further research to evaluate how long the virus remains infectious on personal clothing, which will have policy implications in terms of need for use of separate gowns by the visitors while they are in the NICU,” Dr. Homaira added, concluding that frequent cleaning of high-touch areas and periodic screening of visitors for RSV as they enter the NICU during seasonal epidemics also may help limit disease transmission.
The investigators reported having no disclosures.
AT ICEID 2015
Key clinical point: Clothing worn by caregivers and visitors may be an important vehicle for the transmission of respiratory syncytial virus in the neonatal intensive care unit setting.
Major finding: RSV was detected in 4% of 80 visitors’ clothing swabs.
Data source: A prospective study of 55 neonates, 80 visitors, and 85 health care workers.
Disclosures: The investigators reported having no disclosures.
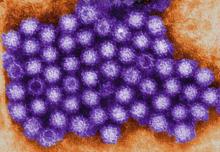
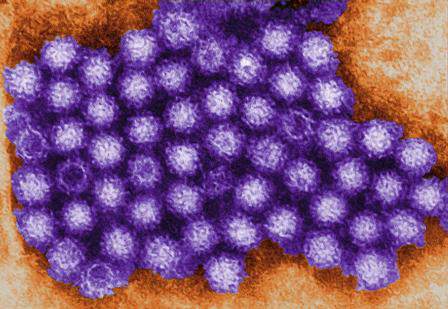
Most pediatric norovirus cases occur from 6 to 23 months
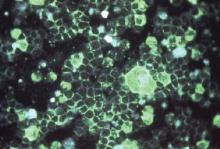
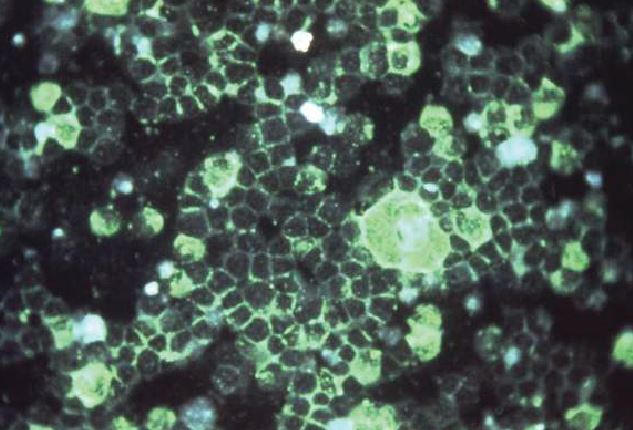
ATLANTA – Norovirus vaccines currently in development should be administered before age 6 months to provide the most benefit, according to the findings of a global age distribution study.
The meta-analysis of data from 35 papers representing children from 23 countries showed that completion of the vaccination schedule by age 6 months could prevent about 85% of pediatric cases, compared with only about 50% of cases with delivery by age 12 months, Kayoko Shioda, D.V.M., of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, Atlanta, reported in a poster at the International Conference on Emerging Infectious Diseases.
For the study, Dr. Shioda and her colleagues at the CDC looked at studies involving norovirus cases among children under age 5 years. After weighting by the number of pediatric cases in each study, they found that 13% of cases occurred in those aged 0-5 months, 33% occurred among those aged 6-11 months, 36% occurred in those aged 12-23 months, and 18% were in those aged 24-59 months.
The age distribution was younger in developing countries vs. developed countries, in low income vs. high income countries, and in inpatient vs. outpatient and community settings, she said in an interview.
Also, the age distribution of severe cases was younger than for mild cases, she noted.
The findings suggest that early vaccination is particularly important in low-income settings, which had a younger age distribution that might be attributable to poorer hygiene and sanitation and/or higher levels of contact between individuals, she said, noting that the cumulative proportion of cases by 12 months was reduced by 4.1% for every $10,000 increase in per capita gross domestic product after controlling for study settings.
"Early vaccination is even more critical in low income countries, given the fact that more children get infected earlier," she added.
The findings were published earlier this summer (Vaccine. 2015, June doi: 10.1016/j.vaccine.2015.05.051).
Norovirus is increasingly recognized as a main cause of acute gastroenteritis, which occurs most often in young children. No vaccine is currently available, but one developed by Takeda is currently entering phase III trials, Dr. Shioda said.
This study was supported by the Oak Ridge (Tenn.) Institute for Science and Technology. Dr. Shioda reported having no other relevant disclosures.
ATLANTA – Norovirus vaccines currently in development should be administered before age 6 months to provide the most benefit, according to the findings of a global age distribution study.
The meta-analysis of data from 35 papers representing children from 23 countries showed that completion of the vaccination schedule by age 6 months could prevent about 85% of pediatric cases, compared with only about 50% of cases with delivery by age 12 months, Kayoko Shioda, D.V.M., of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, Atlanta, reported in a poster at the International Conference on Emerging Infectious Diseases.
For the study, Dr. Shioda and her colleagues at the CDC looked at studies involving norovirus cases among children under age 5 years. After weighting by the number of pediatric cases in each study, they found that 13% of cases occurred in those aged 0-5 months, 33% occurred among those aged 6-11 months, 36% occurred in those aged 12-23 months, and 18% were in those aged 24-59 months.
The age distribution was younger in developing countries vs. developed countries, in low income vs. high income countries, and in inpatient vs. outpatient and community settings, she said in an interview.
Also, the age distribution of severe cases was younger than for mild cases, she noted.
The findings suggest that early vaccination is particularly important in low-income settings, which had a younger age distribution that might be attributable to poorer hygiene and sanitation and/or higher levels of contact between individuals, she said, noting that the cumulative proportion of cases by 12 months was reduced by 4.1% for every $10,000 increase in per capita gross domestic product after controlling for study settings.
"Early vaccination is even more critical in low income countries, given the fact that more children get infected earlier," she added.
The findings were published earlier this summer (Vaccine. 2015, June doi: 10.1016/j.vaccine.2015.05.051).
Norovirus is increasingly recognized as a main cause of acute gastroenteritis, which occurs most often in young children. No vaccine is currently available, but one developed by Takeda is currently entering phase III trials, Dr. Shioda said.
This study was supported by the Oak Ridge (Tenn.) Institute for Science and Technology. Dr. Shioda reported having no other relevant disclosures.
ATLANTA – Norovirus vaccines currently in development should be administered before age 6 months to provide the most benefit, according to the findings of a global age distribution study.
The meta-analysis of data from 35 papers representing children from 23 countries showed that completion of the vaccination schedule by age 6 months could prevent about 85% of pediatric cases, compared with only about 50% of cases with delivery by age 12 months, Kayoko Shioda, D.V.M., of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, Atlanta, reported in a poster at the International Conference on Emerging Infectious Diseases.
For the study, Dr. Shioda and her colleagues at the CDC looked at studies involving norovirus cases among children under age 5 years. After weighting by the number of pediatric cases in each study, they found that 13% of cases occurred in those aged 0-5 months, 33% occurred among those aged 6-11 months, 36% occurred in those aged 12-23 months, and 18% were in those aged 24-59 months.
The age distribution was younger in developing countries vs. developed countries, in low income vs. high income countries, and in inpatient vs. outpatient and community settings, she said in an interview.
Also, the age distribution of severe cases was younger than for mild cases, she noted.
The findings suggest that early vaccination is particularly important in low-income settings, which had a younger age distribution that might be attributable to poorer hygiene and sanitation and/or higher levels of contact between individuals, she said, noting that the cumulative proportion of cases by 12 months was reduced by 4.1% for every $10,000 increase in per capita gross domestic product after controlling for study settings.
"Early vaccination is even more critical in low income countries, given the fact that more children get infected earlier," she added.
The findings were published earlier this summer (Vaccine. 2015, June doi: 10.1016/j.vaccine.2015.05.051).
Norovirus is increasingly recognized as a main cause of acute gastroenteritis, which occurs most often in young children. No vaccine is currently available, but one developed by Takeda is currently entering phase III trials, Dr. Shioda said.
This study was supported by the Oak Ridge (Tenn.) Institute for Science and Technology. Dr. Shioda reported having no other relevant disclosures.
AT ICEID 2015
Key clinical point: Should norovirus vaccines currently in development gain approval, immunization should be completed before age 6 months to provide the most benefit, according to the findings of a global age distribution study.
Major finding: Completion of a norovirus vaccination schedule by age 6 months could prevent about 85% of pediatric cases.
Data source: A meta-analysis of 35 studies.
Disclosures: This study was supported by the Oak Ridge (Tenn.) Institute for Science and Technology. Dr. Shioda reported having no other relevant disclosures.
ICEID: Fish-based outbreaks may be on the rise despite drop-off in recent years
ATLANTA – Despite the fact that foodborne outbreaks caused by consumption of fish have decreased over the last 15-20 years, prevalence of such outbreaks still remains relatively high, and the risk of future outbreaks therefore is not one to take lightly.
Kelly A. Walsh of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, said her study findings show, “while there was an overall decline in the number of fish outbreaks, they appear to be increasing in recent years,” meaning that public health officials and health care providers should be vigilant, as several popularly consumed fish are the most likely to cause disease.
The two most common etiologic agents behind outbreaks over this time span were scombroid toxin (380 outbreaks, 55%) and ciguatoxin (224 outbreaks, 33%). Onset of symptoms caused by scombroid toxin – including facial and lingual swelling, pruritic rash, diarrhea, and vomiting – can begin in a matter of minutes, and it is typically caused by consumption of tuna and mahi mahi, which were the first (36%) and second most-common (11%) cause of outbreaks between 1998 and 2013, respectively. Ciguatoxin is found in fish such as barracuda and grouper, which caused 6% and 9% of all outbreaks during 1998-2013, respectively. Onset of symptoms can occur in 3-30 hours after consumption of fish, and can cause gastrointestinal, cardiac, and neurologic symptoms, such as fatigue or “aberrant temperature perception,” Ms. Walsh said at the International Conference on Emerging Infectious Diseases.
“Seeing tuna come up most commonly with scombroid toxin is no surprise, but what was surprising is that raw or undercooked fish only accounted for 11% of outbreaks,” Ms. Walsh explained. In instances of undercooked fish causing outbreaks, tuna and salmon were the most commonly reported.
Ms. Walsh and her coinvestigators examined data from the CDC’s Foodborne Disease Outbreak Surveillance System collected between 1998 and 2013, looking specifically at the number of outbreaks, illnesses, hospitalizations, and deaths attributed to fish, as well as which etiologic agents were responsible, the associated fish types these agents were identified in, how the fish were prepared and served for consumption, and the states in which these outbreaks occurred.
In total, 764 outbreaks occurred and led to 4,401 illnesses, with a median of 3 illnesses per outbreak and a range between 2 and 425 illnesses. These outbreaks resulted in 322 hospitalizations and three deaths. However, despite finding that fish-based outbreaks dropped from an average of 62 per year during 1998-2004 to 32 per year during 2005-2012, the number of outbreaks in 2013 alone spiked to 50. The largest outbreak that occurred during 1998-2013 happened in 2012, when 425 illnesses were reported in a multistate outbreak caused by consumption of tuna that was found to have traces of Salmonella Nchanga, and Salmonella Bareilly.
Ms. Walsh and her coinvestigators hope their findings will bring to light the need for better control measures on the fish implicated in recent outbreaks, such as proper fish storage and appropriate preparation of fish. “We’re working with our partners at [the Food and Drug Administration] to inform them of the data that we’ve seen [so] we can inform regulations such as HACCP [Hazard Analysis & Critical Control Points].”
Ms. Walsh did not report any relevant financial disclosures.
ATLANTA – Despite the fact that foodborne outbreaks caused by consumption of fish have decreased over the last 15-20 years, prevalence of such outbreaks still remains relatively high, and the risk of future outbreaks therefore is not one to take lightly.
Kelly A. Walsh of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, said her study findings show, “while there was an overall decline in the number of fish outbreaks, they appear to be increasing in recent years,” meaning that public health officials and health care providers should be vigilant, as several popularly consumed fish are the most likely to cause disease.
The two most common etiologic agents behind outbreaks over this time span were scombroid toxin (380 outbreaks, 55%) and ciguatoxin (224 outbreaks, 33%). Onset of symptoms caused by scombroid toxin – including facial and lingual swelling, pruritic rash, diarrhea, and vomiting – can begin in a matter of minutes, and it is typically caused by consumption of tuna and mahi mahi, which were the first (36%) and second most-common (11%) cause of outbreaks between 1998 and 2013, respectively. Ciguatoxin is found in fish such as barracuda and grouper, which caused 6% and 9% of all outbreaks during 1998-2013, respectively. Onset of symptoms can occur in 3-30 hours after consumption of fish, and can cause gastrointestinal, cardiac, and neurologic symptoms, such as fatigue or “aberrant temperature perception,” Ms. Walsh said at the International Conference on Emerging Infectious Diseases.
“Seeing tuna come up most commonly with scombroid toxin is no surprise, but what was surprising is that raw or undercooked fish only accounted for 11% of outbreaks,” Ms. Walsh explained. In instances of undercooked fish causing outbreaks, tuna and salmon were the most commonly reported.
Ms. Walsh and her coinvestigators examined data from the CDC’s Foodborne Disease Outbreak Surveillance System collected between 1998 and 2013, looking specifically at the number of outbreaks, illnesses, hospitalizations, and deaths attributed to fish, as well as which etiologic agents were responsible, the associated fish types these agents were identified in, how the fish were prepared and served for consumption, and the states in which these outbreaks occurred.
In total, 764 outbreaks occurred and led to 4,401 illnesses, with a median of 3 illnesses per outbreak and a range between 2 and 425 illnesses. These outbreaks resulted in 322 hospitalizations and three deaths. However, despite finding that fish-based outbreaks dropped from an average of 62 per year during 1998-2004 to 32 per year during 2005-2012, the number of outbreaks in 2013 alone spiked to 50. The largest outbreak that occurred during 1998-2013 happened in 2012, when 425 illnesses were reported in a multistate outbreak caused by consumption of tuna that was found to have traces of Salmonella Nchanga, and Salmonella Bareilly.
Ms. Walsh and her coinvestigators hope their findings will bring to light the need for better control measures on the fish implicated in recent outbreaks, such as proper fish storage and appropriate preparation of fish. “We’re working with our partners at [the Food and Drug Administration] to inform them of the data that we’ve seen [so] we can inform regulations such as HACCP [Hazard Analysis & Critical Control Points].”
Ms. Walsh did not report any relevant financial disclosures.
ATLANTA – Despite the fact that foodborne outbreaks caused by consumption of fish have decreased over the last 15-20 years, prevalence of such outbreaks still remains relatively high, and the risk of future outbreaks therefore is not one to take lightly.
Kelly A. Walsh of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, said her study findings show, “while there was an overall decline in the number of fish outbreaks, they appear to be increasing in recent years,” meaning that public health officials and health care providers should be vigilant, as several popularly consumed fish are the most likely to cause disease.
The two most common etiologic agents behind outbreaks over this time span were scombroid toxin (380 outbreaks, 55%) and ciguatoxin (224 outbreaks, 33%). Onset of symptoms caused by scombroid toxin – including facial and lingual swelling, pruritic rash, diarrhea, and vomiting – can begin in a matter of minutes, and it is typically caused by consumption of tuna and mahi mahi, which were the first (36%) and second most-common (11%) cause of outbreaks between 1998 and 2013, respectively. Ciguatoxin is found in fish such as barracuda and grouper, which caused 6% and 9% of all outbreaks during 1998-2013, respectively. Onset of symptoms can occur in 3-30 hours after consumption of fish, and can cause gastrointestinal, cardiac, and neurologic symptoms, such as fatigue or “aberrant temperature perception,” Ms. Walsh said at the International Conference on Emerging Infectious Diseases.
“Seeing tuna come up most commonly with scombroid toxin is no surprise, but what was surprising is that raw or undercooked fish only accounted for 11% of outbreaks,” Ms. Walsh explained. In instances of undercooked fish causing outbreaks, tuna and salmon were the most commonly reported.
Ms. Walsh and her coinvestigators examined data from the CDC’s Foodborne Disease Outbreak Surveillance System collected between 1998 and 2013, looking specifically at the number of outbreaks, illnesses, hospitalizations, and deaths attributed to fish, as well as which etiologic agents were responsible, the associated fish types these agents were identified in, how the fish were prepared and served for consumption, and the states in which these outbreaks occurred.
In total, 764 outbreaks occurred and led to 4,401 illnesses, with a median of 3 illnesses per outbreak and a range between 2 and 425 illnesses. These outbreaks resulted in 322 hospitalizations and three deaths. However, despite finding that fish-based outbreaks dropped from an average of 62 per year during 1998-2004 to 32 per year during 2005-2012, the number of outbreaks in 2013 alone spiked to 50. The largest outbreak that occurred during 1998-2013 happened in 2012, when 425 illnesses were reported in a multistate outbreak caused by consumption of tuna that was found to have traces of Salmonella Nchanga, and Salmonella Bareilly.
Ms. Walsh and her coinvestigators hope their findings will bring to light the need for better control measures on the fish implicated in recent outbreaks, such as proper fish storage and appropriate preparation of fish. “We’re working with our partners at [the Food and Drug Administration] to inform them of the data that we’ve seen [so] we can inform regulations such as HACCP [Hazard Analysis & Critical Control Points].”
Ms. Walsh did not report any relevant financial disclosures.
AT ICEID 2015
Key clinical point: Although there has been a decline in the number of foodborne outbreaks caused by consumption of fish, recent data point to a slight increase in the last year reported, with specific types of fish still posing a serious threat of widespread illness.
Major finding: A total of 55% of outbreaks between 1998 and 2013 were attributed to scombroid toxin – commonly found in tuna and mahi mahi – and 33% to ciguatoxin – which is prevalent in grouper, among other types of popular fish.
Data source: Retrospective review of data from the CDC’s Foodborne Disease Outbreak Surveillance System for outbreaks attributed to fish from 1998 to 2013.
Disclosures: Ms. Walsh did not report any relevant financial disclosures.