User login
Infectious Diseases Society of America (IDSA)/ Society for Healthcare Epidemiology of America (SHEA)/ HIV Medicine Association (HIVMA)/ Pediatric Infectious Diseases Society (PIDS): IDWeek 2014
Fidaxomicin appears safe, effective for CDAD in children
PHILADELPHIA – Fidaxomicin, an approved treatment for Clostridium difficile-associated diarrhea in adults, appears safe and effective in children, according to findings from an open-label study.
The overall clinical response rate was 92% in 38 children aged 11 months through 17 years who were treated with 32 mg/kg/day for 10 days. Although 74% of patients had at least one adverse event, most of the events were mild (45%) or moderate (21%) in severity and were the type of events that would be expected in children with moderate to severe underlying illness, Pam Sears, Ph.D. of Cubist Pharmaceuticals, San Diego, reported at an annual scientific meeting on infectious diseases.
The children included in this first pediatric study of fidaxomicin had diarrhea and tested positive for C. difficile toxin. Most had relatively complex medical histories; 24% had neoplasms and 79% had gastrointestinal disorders. They received either the commercial tablet formulation of fidaxomicin or an oral suspension.
Plasma concentrations were generally low, with a mean across the strata ranging from 8.87-16.6 ng/mL and metabolite OP-1118 levels that ranged from 27.5-130 ng/mL at 1-2 hours following the first dose. No age-related trends in concentrations were seen.
Fecal concentrations of fidaxomicin averaged 3,230 mcg/g with a trend toward higher concentrations in the youngest age group. This could be because samples from the youngest group were collected from diapers and could have become dehydrated, Dr. Sears explained the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Of the children in the study with a clinical response, 29% experienced a relapse, but all but one of these children had a history of recurrent C. difficile-related diarrhea.
Fidaxomicin is a first-in class narrow spectrum macrocyclic antibiotic drug approved in the United States and several other countries for the treatment of C. difficile-associated diarrhea in adults.
These findings demonstrate that the pharmacokinetic profile in children is similar to that in adults – with low plasma levels and high fecal concentrations, and suggest that clinical response in children is also excellent, Dr. Sears said.
This study was funded by Cubist Pharmaceuticals. Dr. Sears is an employee of Cubist Pharmaceuticals.
PHILADELPHIA – Fidaxomicin, an approved treatment for Clostridium difficile-associated diarrhea in adults, appears safe and effective in children, according to findings from an open-label study.
The overall clinical response rate was 92% in 38 children aged 11 months through 17 years who were treated with 32 mg/kg/day for 10 days. Although 74% of patients had at least one adverse event, most of the events were mild (45%) or moderate (21%) in severity and were the type of events that would be expected in children with moderate to severe underlying illness, Pam Sears, Ph.D. of Cubist Pharmaceuticals, San Diego, reported at an annual scientific meeting on infectious diseases.
The children included in this first pediatric study of fidaxomicin had diarrhea and tested positive for C. difficile toxin. Most had relatively complex medical histories; 24% had neoplasms and 79% had gastrointestinal disorders. They received either the commercial tablet formulation of fidaxomicin or an oral suspension.
Plasma concentrations were generally low, with a mean across the strata ranging from 8.87-16.6 ng/mL and metabolite OP-1118 levels that ranged from 27.5-130 ng/mL at 1-2 hours following the first dose. No age-related trends in concentrations were seen.
Fecal concentrations of fidaxomicin averaged 3,230 mcg/g with a trend toward higher concentrations in the youngest age group. This could be because samples from the youngest group were collected from diapers and could have become dehydrated, Dr. Sears explained the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Of the children in the study with a clinical response, 29% experienced a relapse, but all but one of these children had a history of recurrent C. difficile-related diarrhea.
Fidaxomicin is a first-in class narrow spectrum macrocyclic antibiotic drug approved in the United States and several other countries for the treatment of C. difficile-associated diarrhea in adults.
These findings demonstrate that the pharmacokinetic profile in children is similar to that in adults – with low plasma levels and high fecal concentrations, and suggest that clinical response in children is also excellent, Dr. Sears said.
This study was funded by Cubist Pharmaceuticals. Dr. Sears is an employee of Cubist Pharmaceuticals.
PHILADELPHIA – Fidaxomicin, an approved treatment for Clostridium difficile-associated diarrhea in adults, appears safe and effective in children, according to findings from an open-label study.
The overall clinical response rate was 92% in 38 children aged 11 months through 17 years who were treated with 32 mg/kg/day for 10 days. Although 74% of patients had at least one adverse event, most of the events were mild (45%) or moderate (21%) in severity and were the type of events that would be expected in children with moderate to severe underlying illness, Pam Sears, Ph.D. of Cubist Pharmaceuticals, San Diego, reported at an annual scientific meeting on infectious diseases.
The children included in this first pediatric study of fidaxomicin had diarrhea and tested positive for C. difficile toxin. Most had relatively complex medical histories; 24% had neoplasms and 79% had gastrointestinal disorders. They received either the commercial tablet formulation of fidaxomicin or an oral suspension.
Plasma concentrations were generally low, with a mean across the strata ranging from 8.87-16.6 ng/mL and metabolite OP-1118 levels that ranged from 27.5-130 ng/mL at 1-2 hours following the first dose. No age-related trends in concentrations were seen.
Fecal concentrations of fidaxomicin averaged 3,230 mcg/g with a trend toward higher concentrations in the youngest age group. This could be because samples from the youngest group were collected from diapers and could have become dehydrated, Dr. Sears explained the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Of the children in the study with a clinical response, 29% experienced a relapse, but all but one of these children had a history of recurrent C. difficile-related diarrhea.
Fidaxomicin is a first-in class narrow spectrum macrocyclic antibiotic drug approved in the United States and several other countries for the treatment of C. difficile-associated diarrhea in adults.
These findings demonstrate that the pharmacokinetic profile in children is similar to that in adults – with low plasma levels and high fecal concentrations, and suggest that clinical response in children is also excellent, Dr. Sears said.
This study was funded by Cubist Pharmaceuticals. Dr. Sears is an employee of Cubist Pharmaceuticals.
Key clinical point: Fidaxomicin appear to have excellent clinical efficacy in children with C. difficile-associated diarrhea and a pharmacokinetic profile similar to that seen in adults.
Major finding: The overall clinical response rate was 92%.
Data source: An open-label study in 38 children.
Disclosures: This study was funded by Cubist Pharmaceuticals. Dr. Sears is an employee of Cubist Pharmaceuticals.
Early Data Find Frozen Fecal Capsules Effective for C. Difficile
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
FROM IDWEEK 2014
Early data find frozen fecal capsules effective for C. difficile
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
Treatment of relapsing or recurrent Clostridium difficile infection with frozen, orally administered capsules containing a solution of fecal matter from healthy unrelated donors had promising results, with diarrhea resolving in 90% of patients after one or two rounds of treatment.
“We demonstrated the feasibility of oral administration of frozen encapsulated fecal material from unrelated donors to treat patients with recurrent [Clostridium difficile infection (CDI)],” concluded Dr. Ilan Youngster, of the division of infectious diseases at Massachusetts General Hospital, Boston, and his associates. While the study was limited by the small number patients (20) and the lack of a placebo or comparator group, “if reproduced in future studies with active controls, these results may help make FMT accessible to a wider population of patients, in addition to potentially making the procedure safer.”
The study was published Oct. 11 in JAMA, in conjunction with its presenation at ID Week 2014 (doi:10.1001/jama.2014.13875)
Instead of the most common type of fecal microbiota transplantation (FMT) procedures, which use a suspension of fresh stool from donors related to the patient to reconstitute the normal flora, this feasibility study evaluated the safety and effectiveness of FMT with fecal matter from unrelated, carefully screened healthy donors, which was processed into a solution that was placed into small capsules and then frozen.
The study enrolled 20 patients whose mean age was 64.5 years (one patient was aged 11, the rest were aged 17-89) between August 2013 and June 2014 at Massachusetts General. Patient had had at least three episodes of mild to moderate CDI and failed treatment with vancomycin, with or without an alternative antibiotic; or had been hospitalized with at least 2 episodes of severe CDI.
After one round of treatment with 15 capsules over 2 days, diarrhea resolved (defined as fewer than three bowel movements over 24 hours) in 14 of the 20 patients (70%); at 8 weeks, they remained symptom free. The remaining 6 patients were treated again, a mean of 7 days after the first treatment, and diarrhea resolved in 5. One of the 5 patients relapsed within the 8 week follow-up period, so the overall rate of diarrhea resolution at 8 weeks was 90%.
Overall health score before treatment was the only factor significantly associated with treatment response. Those who required a second treatment had more symptoms and had lower health scores before treatment than those who responded to the first treatment.
The number of daily bowel movements dropped from a median of five per day before treatment to a median of 2 at day 3, and one at 8 weeks, both statistically significant reductions from baseline. Patients also felt better, reflected in improvements in scores on health questionnaires evaluating overall and gastrointestinal health.
There were no cases of vomiting or aspiration and no serious adverse events were observed, Dr. Youngster said. Six patients experienced abdominal cramping and bloating after treatment, which were considered to be treatment related, but resolved.
The 90% clinical resolution rate with this treatment are comparable those in case studies and a randomized study using fresh stool preparations to treat CDI, Dr. Youngster said. “Larger studied are needed to confirm these results and to evaluate long-term safety and effectiveness.
The study was funded with internal hospital division funds. One author is a recipient of a research award sponsored by Seres Health, Cambridge, Mass., for an unrelated clinical trial of a C. difficile colitis treatment. No other author disclosures were reported.
FROM IDWEEK 2014
Key clinical point: Fecal microbiota transplantation (FMT) with a frozen capsule formulation could be a practical and cost-effective treatment for C. difficile infections.
Major finding: Overall, diarrhea resolved in 90% of the patients after one or two rounds of treatment, with no relapses at 8 weeks and no serious adverse events.
Data source: An open-label, preliminary feasibility study of the safety and effectiveness of a fecal suspension derived from healthy donors, provided in oral capsules that were frozen, in 20 patients with relapsing or recurrent C. difficile infections.
Disclosures: The study, conducted at Massachusetts General Hospital, Boston, was funded with internal hospital division funds. The authors reported no relevant conflicts of interest.
Pleconaril shows promise for neonatal enteroviral sepsis
PHILADELPHIA – Pleconaril, an oral capsid binder with activity against enterovirus infections, shows promise for the treatment of neonates with enterovirus sepsis, according to findings from a randomized, double-blind, placebo-controlled trial.
Time to culture-negativity for all types of collected specimens combined – including those from the oropharynx, rectum, urine, and serum – was faster in 43 patients treated with 5 mg/kg of pleconaril every 8 hours for 7 days than in18 patients who received placebo (median of 4.0 vs. 7.0 days). The difference approached statistical significance.
Fewer subjects in the treatment group remained polymerase chain reaction-positive at last oropharynx sample (83% and 23% were positive on day 1 and at a median of day 14 in the treatment group, vs. 100% and 58%, respectively, in the placebo group), Dr. Mark Abzug of the University of Colorado, Aurora, reported at an annual scientific meeting on infectious diseases.
Mortality in an intention-to-treat analysis was 23% in the treatment group, compared with 44% in the placebo group, and mortality in those with confirmed enterovirus infection was 23% and 42% in the treatment and placebo groups, respectively, Dr. Abzug said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Patients were neonates with suspected enterovirus sepsis with illness onset in the first 15 days of life. They were randomized 2:1 to receive active treatment or placebo for 7 days. Specimens were obtained serially for 14 days for viral culture and PCR, pharmacokinetic analysis, and safety evaluations, and clinical assessments were performed over 24 months.
Enterovirus was confirmed by culture or PCR in 43 of the 61 patients, including 31 in the treatment group and 12 in the placebo group. The two groups were similar with respect to baseline characteristics, including median age at illness onset (4.5 and 5.0 days, respectively) and time until enrollment (6 to 7 days into the course of their illness).
Of note, pleconaril concentrations exceeded the 90% inhibitory concentration (IC90) level after the first day of treatment in the treatment group, but 41% of subjects did not achieve this target until after day 4, suggesting the need for a loading dose.
Neonatal enterovirus infections are associated with high morbidity and mortality, and therapy is mainly supportive. While intravenous immunoglobulin is thought to confer potential benefit, it remains unproven, and no specific antiviral therapies are currently available, Dr. Abzug said.
Pleconaril has been shown previously to have activity against most enteroviruses and many rhinoviruses. It is well tolerated: In the current study, treatment-related adverse effects occurred in 1 subject in the treatment group, and in 3 in the placebo group.
While the unexpectedly low yield of viral cultures in this study precluded the demonstration of a difference between the groups with regard to the primary endpoint of day 5 oropharyngeal culture positivity, which was 25% on day 1 and 0% on day 5 in the treatment group, vs. 30% on day 1 and 0% on day 5 in the placebo group, the shorter times to culture and PCR negativity and the suggestion of greater survival in the treatment group are encouraging, Dr. Abzug said.
These indicators of biological and clinical efficacy warrant further investigation of pleconaril for neonatal enteroviral disease, he concluded.The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Abzug reported having no disclosures.
PHILADELPHIA – Pleconaril, an oral capsid binder with activity against enterovirus infections, shows promise for the treatment of neonates with enterovirus sepsis, according to findings from a randomized, double-blind, placebo-controlled trial.
Time to culture-negativity for all types of collected specimens combined – including those from the oropharynx, rectum, urine, and serum – was faster in 43 patients treated with 5 mg/kg of pleconaril every 8 hours for 7 days than in18 patients who received placebo (median of 4.0 vs. 7.0 days). The difference approached statistical significance.
Fewer subjects in the treatment group remained polymerase chain reaction-positive at last oropharynx sample (83% and 23% were positive on day 1 and at a median of day 14 in the treatment group, vs. 100% and 58%, respectively, in the placebo group), Dr. Mark Abzug of the University of Colorado, Aurora, reported at an annual scientific meeting on infectious diseases.
Mortality in an intention-to-treat analysis was 23% in the treatment group, compared with 44% in the placebo group, and mortality in those with confirmed enterovirus infection was 23% and 42% in the treatment and placebo groups, respectively, Dr. Abzug said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Patients were neonates with suspected enterovirus sepsis with illness onset in the first 15 days of life. They were randomized 2:1 to receive active treatment or placebo for 7 days. Specimens were obtained serially for 14 days for viral culture and PCR, pharmacokinetic analysis, and safety evaluations, and clinical assessments were performed over 24 months.
Enterovirus was confirmed by culture or PCR in 43 of the 61 patients, including 31 in the treatment group and 12 in the placebo group. The two groups were similar with respect to baseline characteristics, including median age at illness onset (4.5 and 5.0 days, respectively) and time until enrollment (6 to 7 days into the course of their illness).
Of note, pleconaril concentrations exceeded the 90% inhibitory concentration (IC90) level after the first day of treatment in the treatment group, but 41% of subjects did not achieve this target until after day 4, suggesting the need for a loading dose.
Neonatal enterovirus infections are associated with high morbidity and mortality, and therapy is mainly supportive. While intravenous immunoglobulin is thought to confer potential benefit, it remains unproven, and no specific antiviral therapies are currently available, Dr. Abzug said.
Pleconaril has been shown previously to have activity against most enteroviruses and many rhinoviruses. It is well tolerated: In the current study, treatment-related adverse effects occurred in 1 subject in the treatment group, and in 3 in the placebo group.
While the unexpectedly low yield of viral cultures in this study precluded the demonstration of a difference between the groups with regard to the primary endpoint of day 5 oropharyngeal culture positivity, which was 25% on day 1 and 0% on day 5 in the treatment group, vs. 30% on day 1 and 0% on day 5 in the placebo group, the shorter times to culture and PCR negativity and the suggestion of greater survival in the treatment group are encouraging, Dr. Abzug said.
These indicators of biological and clinical efficacy warrant further investigation of pleconaril for neonatal enteroviral disease, he concluded.The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Abzug reported having no disclosures.
PHILADELPHIA – Pleconaril, an oral capsid binder with activity against enterovirus infections, shows promise for the treatment of neonates with enterovirus sepsis, according to findings from a randomized, double-blind, placebo-controlled trial.
Time to culture-negativity for all types of collected specimens combined – including those from the oropharynx, rectum, urine, and serum – was faster in 43 patients treated with 5 mg/kg of pleconaril every 8 hours for 7 days than in18 patients who received placebo (median of 4.0 vs. 7.0 days). The difference approached statistical significance.
Fewer subjects in the treatment group remained polymerase chain reaction-positive at last oropharynx sample (83% and 23% were positive on day 1 and at a median of day 14 in the treatment group, vs. 100% and 58%, respectively, in the placebo group), Dr. Mark Abzug of the University of Colorado, Aurora, reported at an annual scientific meeting on infectious diseases.
Mortality in an intention-to-treat analysis was 23% in the treatment group, compared with 44% in the placebo group, and mortality in those with confirmed enterovirus infection was 23% and 42% in the treatment and placebo groups, respectively, Dr. Abzug said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Patients were neonates with suspected enterovirus sepsis with illness onset in the first 15 days of life. They were randomized 2:1 to receive active treatment or placebo for 7 days. Specimens were obtained serially for 14 days for viral culture and PCR, pharmacokinetic analysis, and safety evaluations, and clinical assessments were performed over 24 months.
Enterovirus was confirmed by culture or PCR in 43 of the 61 patients, including 31 in the treatment group and 12 in the placebo group. The two groups were similar with respect to baseline characteristics, including median age at illness onset (4.5 and 5.0 days, respectively) and time until enrollment (6 to 7 days into the course of their illness).
Of note, pleconaril concentrations exceeded the 90% inhibitory concentration (IC90) level after the first day of treatment in the treatment group, but 41% of subjects did not achieve this target until after day 4, suggesting the need for a loading dose.
Neonatal enterovirus infections are associated with high morbidity and mortality, and therapy is mainly supportive. While intravenous immunoglobulin is thought to confer potential benefit, it remains unproven, and no specific antiviral therapies are currently available, Dr. Abzug said.
Pleconaril has been shown previously to have activity against most enteroviruses and many rhinoviruses. It is well tolerated: In the current study, treatment-related adverse effects occurred in 1 subject in the treatment group, and in 3 in the placebo group.
While the unexpectedly low yield of viral cultures in this study precluded the demonstration of a difference between the groups with regard to the primary endpoint of day 5 oropharyngeal culture positivity, which was 25% on day 1 and 0% on day 5 in the treatment group, vs. 30% on day 1 and 0% on day 5 in the placebo group, the shorter times to culture and PCR negativity and the suggestion of greater survival in the treatment group are encouraging, Dr. Abzug said.
These indicators of biological and clinical efficacy warrant further investigation of pleconaril for neonatal enteroviral disease, he concluded.The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Abzug reported having no disclosures.
AT ID Week 2014
Key clinical point: Pleconaril showed some signs of efficacy for enteroviral sepsis in neonates in a randomized controlled trial.
Major finding: Mortality was 23% in the treatment group, compared with 44% in the placebo group.
Data source: A randomized placebo-controlled trial of 61 neonates.
Disclosures: The study was funded by the National Institute for Allergy and Infectious Diseases. Dr. Abzug reported having no disclosures.
Antibiotic stewardship program reduced pediatric LOS, readmission rate
PHILADELPHIA – Adherence to the recommendations of an antibiotic stewardship program committee decreased 30-day readmissions without increasing length of stay at a freestanding children’s hospital.
Between March 3, 2008, and March 3, 2013, the antibiotic stewardship program (ASP) committee at Children’s Mercy Hospital–Kansas City, Mo., recommended discontinuing a prescribed antibiotic, changing the antibiotic, or reducing the antibiotic dose in 1,240 patients. When the recommendations were followed, no 30-day readmissions occurred, and median length of stay was 79 hours. When they were not followed, readmissions within 30 days occurred in 3% and 4% of otherwise healthy surgical and medical patients and in patients with chronic complex medical conditions, respectively, and median length of stay was 82 hours, Dr. Jason G. Newland reported at an annual scientific meeting on infectious diseases.
The study is the first to demonstrate that a stewardship program designed to control antibiotic prescription and treatment in the hospital setting has beneficial effects on children’s health, Dr. Newland, medical director of patient safety and systems reliability at Children’s Mercy Hospitals and Clinics and the University of Missouri–-Kansas City said during a press briefing at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“We obviously were excited to see that we didn’t impact length of stay on a negative basis,” he said, adding that the 0% readmission rates in cases in which the physician agreed with the antibiotic stewardship program (ASP) recommendation was a particularly encouraging finding.
The ASP committee at Children’s Mercy Hospital, like most such programs, is led by epidemiologists and infectious disease physicians who are tasked with promoting the appropriate use of antibiotics in an effort to prevent the development of antibiotic resistance.
In the vast majority of cases included in the current study, the ASP committee’s recommendation was to discontinue the antibiotic, as it was deemed unnecessary, Dr. Newland noted.
ASP interventions occurred most often in patients receiving ceftriaxone/cefotaxime (62%), vancomycin (11%), and meropenem (5%). The most common diagnoses were pneumonia (22%), urinary tract infections (19%), and rule out sepsis (9%).
The findings reinforce the importance of viewing ASP committees as extensions of patient-safety initiatives, “as their presence really exemplifies the idea of do no harm,” said Dr. Pranita D. Tamma of Johns Hopkins Children’s Center, Baltimore, who moderated the press briefing.
Dr. Newland and his colleagues demonstrated the value of ASP committees for reducing the likelihood of further negative sequelae to which a child could be exposed as a result of inappropriate antibiotic use, such as the increased risk of health care associated infections that might come with readmission, having to take further medications, and undergo other interventions, and the cost and other burdens to families and the health care system as a whole, she said.
Dr. Newland reported receiving grant funding from Pfizer.
PHILADELPHIA – Adherence to the recommendations of an antibiotic stewardship program committee decreased 30-day readmissions without increasing length of stay at a freestanding children’s hospital.
Between March 3, 2008, and March 3, 2013, the antibiotic stewardship program (ASP) committee at Children’s Mercy Hospital–Kansas City, Mo., recommended discontinuing a prescribed antibiotic, changing the antibiotic, or reducing the antibiotic dose in 1,240 patients. When the recommendations were followed, no 30-day readmissions occurred, and median length of stay was 79 hours. When they were not followed, readmissions within 30 days occurred in 3% and 4% of otherwise healthy surgical and medical patients and in patients with chronic complex medical conditions, respectively, and median length of stay was 82 hours, Dr. Jason G. Newland reported at an annual scientific meeting on infectious diseases.
The study is the first to demonstrate that a stewardship program designed to control antibiotic prescription and treatment in the hospital setting has beneficial effects on children’s health, Dr. Newland, medical director of patient safety and systems reliability at Children’s Mercy Hospitals and Clinics and the University of Missouri–-Kansas City said during a press briefing at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“We obviously were excited to see that we didn’t impact length of stay on a negative basis,” he said, adding that the 0% readmission rates in cases in which the physician agreed with the antibiotic stewardship program (ASP) recommendation was a particularly encouraging finding.
The ASP committee at Children’s Mercy Hospital, like most such programs, is led by epidemiologists and infectious disease physicians who are tasked with promoting the appropriate use of antibiotics in an effort to prevent the development of antibiotic resistance.
In the vast majority of cases included in the current study, the ASP committee’s recommendation was to discontinue the antibiotic, as it was deemed unnecessary, Dr. Newland noted.
ASP interventions occurred most often in patients receiving ceftriaxone/cefotaxime (62%), vancomycin (11%), and meropenem (5%). The most common diagnoses were pneumonia (22%), urinary tract infections (19%), and rule out sepsis (9%).
The findings reinforce the importance of viewing ASP committees as extensions of patient-safety initiatives, “as their presence really exemplifies the idea of do no harm,” said Dr. Pranita D. Tamma of Johns Hopkins Children’s Center, Baltimore, who moderated the press briefing.
Dr. Newland and his colleagues demonstrated the value of ASP committees for reducing the likelihood of further negative sequelae to which a child could be exposed as a result of inappropriate antibiotic use, such as the increased risk of health care associated infections that might come with readmission, having to take further medications, and undergo other interventions, and the cost and other burdens to families and the health care system as a whole, she said.
Dr. Newland reported receiving grant funding from Pfizer.
PHILADELPHIA – Adherence to the recommendations of an antibiotic stewardship program committee decreased 30-day readmissions without increasing length of stay at a freestanding children’s hospital.
Between March 3, 2008, and March 3, 2013, the antibiotic stewardship program (ASP) committee at Children’s Mercy Hospital–Kansas City, Mo., recommended discontinuing a prescribed antibiotic, changing the antibiotic, or reducing the antibiotic dose in 1,240 patients. When the recommendations were followed, no 30-day readmissions occurred, and median length of stay was 79 hours. When they were not followed, readmissions within 30 days occurred in 3% and 4% of otherwise healthy surgical and medical patients and in patients with chronic complex medical conditions, respectively, and median length of stay was 82 hours, Dr. Jason G. Newland reported at an annual scientific meeting on infectious diseases.
The study is the first to demonstrate that a stewardship program designed to control antibiotic prescription and treatment in the hospital setting has beneficial effects on children’s health, Dr. Newland, medical director of patient safety and systems reliability at Children’s Mercy Hospitals and Clinics and the University of Missouri–-Kansas City said during a press briefing at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“We obviously were excited to see that we didn’t impact length of stay on a negative basis,” he said, adding that the 0% readmission rates in cases in which the physician agreed with the antibiotic stewardship program (ASP) recommendation was a particularly encouraging finding.
The ASP committee at Children’s Mercy Hospital, like most such programs, is led by epidemiologists and infectious disease physicians who are tasked with promoting the appropriate use of antibiotics in an effort to prevent the development of antibiotic resistance.
In the vast majority of cases included in the current study, the ASP committee’s recommendation was to discontinue the antibiotic, as it was deemed unnecessary, Dr. Newland noted.
ASP interventions occurred most often in patients receiving ceftriaxone/cefotaxime (62%), vancomycin (11%), and meropenem (5%). The most common diagnoses were pneumonia (22%), urinary tract infections (19%), and rule out sepsis (9%).
The findings reinforce the importance of viewing ASP committees as extensions of patient-safety initiatives, “as their presence really exemplifies the idea of do no harm,” said Dr. Pranita D. Tamma of Johns Hopkins Children’s Center, Baltimore, who moderated the press briefing.
Dr. Newland and his colleagues demonstrated the value of ASP committees for reducing the likelihood of further negative sequelae to which a child could be exposed as a result of inappropriate antibiotic use, such as the increased risk of health care associated infections that might come with readmission, having to take further medications, and undergo other interventions, and the cost and other burdens to families and the health care system as a whole, she said.
Dr. Newland reported receiving grant funding from Pfizer.
Key clinical point: An antibiotic stewardship program benefited hospitalized children’s health outcomes.
Major finding: At 30 days, readmissions were 0% and 3%-4%, and median length of stay was 79 vs. 82 hours; when recommendations were vs. were not followed.
Data source: Observational study of outcomes following intervention in 1,240 of more than 7,000 patients.
Disclosures: Dr. Newland reported receiving grant funding from Pfizer.
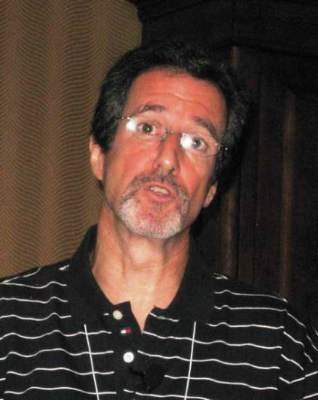
VIDEO: Ebola's U.S. threat low, but delivers infectious disease ‘wake-up call’
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT IDWEEK 2014