User login
American Association for the Study of Liver Disease (AASLD): The Liver Meeting
AASLD: Pilot study shows value of response-guided therapy for HCV GT1b
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
AT THE LIVER MEETING 2015
Key clinical point: Response-guided therapy using all-oral, triple direct-acting antiviral therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection according to a proof-of-concept study.
Major finding: Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients; all 18 subjects with rapid virologic response achieved SVR12.
Data source: A randomized, open-label pilot study of 26 patients.
Disclosures: Dr. Lau is a consultant for Roche and Novartis.
Best HCV value? Screen all baby boomers, treat all infections
BOSTON – Screening all adults born between 1945 and 1965 for hepatitis C and then treating all infected patients with oral drug regimens is the most cost effective strategy for society, because better outcomes more than offset the higher costs of wider screening and newer drugs, Dr. Zobair Younossi said.
A computer simulation analysis that compared four strategies for screening and treatment (plus the option of no screening or treatment) found that birth cohort screening and treatment of all hepatitis C virus–positive patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY), he reported at the annual meeting of the American Association for the Study of Liver Diseases.
That strategy produced an incremental cost-effectiveness ratio well below the widely accepted threshold of $50,000 per QALY used to define cost effectiveness in health care, said Dr. Younossi, professor of medicine at Virginia Commonwealth University’s Inova Campus and chair of Liver Disease Services for Inova, Falls Church, Va.
In first-generation treatment with direct-acting antivirals – namely, triple therapy with protease inhibitors – the mean cost to achieve a sustained virologic response was $172,889, he said, “and we did not get a lot of pushback from the payers at that point.”
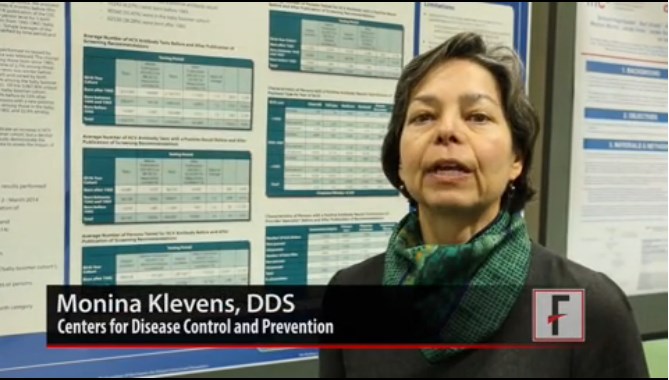
Risk-based screening for HCV has been recommended, and the Centers for Disease Control and Prevention recently recommended birth cohort screening of people born between 1945 and 1965, the so-called baby boomers, Dr. Younossi said.
Still, studies suggest that less than 10% of patients with chronic HCV have been treated successfully, because of the failure of risk-based screening to identify all infected patients and the low efficacy and high rate of side effects from regimens based on interferon and ribavirin, he said.
Higher costs, lower risks
Dr. Younossi’s study used computer simulations to analyze the economic impact of various screening strategies followed by treatment with oral anti-HCV regimens.
The four strategies involved either risk-based screening or birth cohort screening, followed by treatment that either gave all HCV-infected patients oral regimens or that based treatment on staging, giving oral medications only to patients with significant fibrosis. The investigators also considered a fifth strategy: no screening and no treatment.
Birth cohort screening would lead to 1,162,323 patients being diagnosed with previously unknown chronic HCV, they estimated.
To estimate treatment costs, the investigators began with risk-based screening probabilities from a previous study: They assumed that 98% of patients would be medically eligible for treatment and have no contraindications to all-oral treatment regimens, and 98% of those treated would achieve a sustained virologic response for 12 weeks (SVR12), based on results of published trials.
The cost of oral direct-acting antiviral therapy was based on the cost of sofosbuvir – around $1,000 per day for 12 weeks, Dr. Younossi said. Costs for testing, staging, monitoring, and other data were taken from previous treatment models. The investigators calculated QALY from patients’ health utility reports in clinical trials.
Costs averaged approximately $88,000 per patient with birth cohort screening and treating all positive patients, $72,000 per patient with birth cohort screening and treatment based on staging, $60,000-$61,000 per patient for the risk-based screening strategies, and $53,000 per patient with no screening and no treatment.
The probabilities of cirrhosis, hepatocellular carcinoma, or liver transplant were much lower with either birth cohort screening strategy, however, compared with the risk-based strategies or no screening. The probability of cirrhosis was approximately 1% with birth cohort screening and treating all positive patients, 7% with birth cohort screening and treatment based on staging, 55%-60% with the risk-based strategies, and 67% with no screening.
The risk of hepatocellular carcinoma was 4% with birth cohort screening and treating all positive patients, 5% with birth cohort screening and treatment based on staging, 15% with either risk-based screening strategy, and 20% with no screening. The risk of liver transplant was 0.6% with either birth cohort screening strategy, 3% with either risk-based screening strategy, and nearly 4% with no screening.
A total of 4% of patients would be expected to die of liver-related causes after birth cohort screening and treating all positive patients, compared with 7% liver-related mortality after birth cohort screening and staging-based treatment, 25% liver-related mortality in either of the risk-based screening groups, and 34% liver-related mortality with no screening.
HCV costlier than other conditions?
When considering governmental health policy and budgetary issues, Dr. Younossi explained, the cost of curing HCV is not very different from lifetime treatment costs for type 2 diabetes, rheumatoid arthritis, or breast cancer with metastases – and it’s significantly lower than lifetime treatment costs for HIV or relapsing-remitting multiple sclerosis.
As advocates for patients, physicians need to lobby officials so that “as they are dividing the pie, hepatology and HCV are represented,” he said. “These regimens are cost effective.”
The study was an underestimation of savings from birth cohort screening and treating all HCV positives, Dr. Younossi noted, because it did not incorporate an estimated $3 billion per year in savings from work productivity in the United States by curing HCV.
A physician in the audience countered Dr. Younossi’s call for more enlightened health policy supporting funding for HCV treatment, noting that drug companies also need to be pressured to lower the price of the newer drugs.
“The biggest bridge we have to cross is the cost of the drugs,” he said. “This is like denying somebody treatment for tuberculosis by making the cost of the drug too high.”
“I agree,” Dr. Younossi said. “We have to focus on our colleagues in the industry. But we also have to focus on our colleagues in Congress and the policymakers to make sure that, even if we get help from the industry side, we also get help from the policymakers to provide us” with the funding for access to HCV screening and treatment.
Dr. Younossi reported having no financial disclosures. One of his coinvestigators reported financial associations with Gilead and Bristol-Myers Squibb.
On Twitter @sherryboschert
AGA RESOURCE
View the technical review, guideline and clinical decision support tool at www.gastro.org/guideline. Join the guideline authors for a webinar about the guidelines on Jan. 29, 2015, at noon ET. Register at http://ow.ly/FWcsx.
Chronic HCV infection is a common worldwide problem afflicting approximately 170 million people. HCV has significant morbidity and mortality, and it is currently the leading indication for liver transplantation in the Western world. Yet, the natural history is long, and most patients are asymptomatic and will not develop advanced liver disease.
The recent year has been marked by the stunning approval in the U.S. of all-oral, interferon-free treatments for chronic HCV, including genotypes 1, 2, and 3. Approved regimens are characterized by excellent tolerability and cure (sustained virologic response, SVR) rates for most patient subgroups above 90%. For genotype 1, the most common in the U.S., SVR rates in excess of 95% were observed in clinical trials.
Since the regimens are so well tolerated and effective, the number of patients seeking therapy has increased dramatically. Because the medical regimens are expensive, there have been draconian restrictions by many third-party payers for provision of antiviral therapy for HCV patients. This has led to analyses on cost-effectiveness of contemporary therapy.
The article describing a study presented at AASLD 2014 by Younossi et al. is an important contribution to this discussion. Younossi assessed a computer simulation analysis comparing four strategies for screening and treatment of HCV plus an option of no screening or treatment. He found that birth cohort screening and treatment of all HCV patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY); well below the accepted threshold used to define cost-effectiveness in health care. The assumptions regarding cost of the regimens, the rates of cirrhosis, hepatocellular carcinoma, liver transplantation and liver-related death were appropriate. The conclusion that all baby boomers should be screened and treated is not surprising.
The savings did not include an estimated $3 billion dollars annually in savings from work productivity. The analysis also did not account for the costs associated with many extrahepatic manifestations of HCV including diabetes mellitus, lymphoma, cryoglublinemia, chronic renal disease, and others that are not associated with the stage of liver disease and have significant morbidity and mortality. All-cause mortality, not only liver-related mortality, has been shown to decline in patients treated successfully compared with unsuccessful therapeutic attempts.
Never before has there been a serious medical illness for which a well-tolerated and highly effective therapy is available that has been subject to denial of therapy based upon cost by third-party payers. This is an unfortunate precedent.
All patients do not require therapy on an urgent basis. However, the decision to initiate therapy should be between a patient and his or her health care provider. Although it would be best if the cost of the medications could be reduced, even at the current costs, Younossi’s study provides clear data to support identification and treatment of HCV patients sooner rather than later.
Dr. Steven L. Flamm is chief of transplantation hepatology and professor of medicine and surgery at Northwestern University Feinberg School of Medicine, Chicago. He is a speaker for AbbVie, Janssen, and Gilead; and consults for AbbVie, Gilead, Janssen, BMS, and Merck.
Chronic HCV infection is a common worldwide problem afflicting approximately 170 million people. HCV has significant morbidity and mortality, and it is currently the leading indication for liver transplantation in the Western world. Yet, the natural history is long, and most patients are asymptomatic and will not develop advanced liver disease.
The recent year has been marked by the stunning approval in the U.S. of all-oral, interferon-free treatments for chronic HCV, including genotypes 1, 2, and 3. Approved regimens are characterized by excellent tolerability and cure (sustained virologic response, SVR) rates for most patient subgroups above 90%. For genotype 1, the most common in the U.S., SVR rates in excess of 95% were observed in clinical trials.
Since the regimens are so well tolerated and effective, the number of patients seeking therapy has increased dramatically. Because the medical regimens are expensive, there have been draconian restrictions by many third-party payers for provision of antiviral therapy for HCV patients. This has led to analyses on cost-effectiveness of contemporary therapy.
The article describing a study presented at AASLD 2014 by Younossi et al. is an important contribution to this discussion. Younossi assessed a computer simulation analysis comparing four strategies for screening and treatment of HCV plus an option of no screening or treatment. He found that birth cohort screening and treatment of all HCV patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY); well below the accepted threshold used to define cost-effectiveness in health care. The assumptions regarding cost of the regimens, the rates of cirrhosis, hepatocellular carcinoma, liver transplantation and liver-related death were appropriate. The conclusion that all baby boomers should be screened and treated is not surprising.
The savings did not include an estimated $3 billion dollars annually in savings from work productivity. The analysis also did not account for the costs associated with many extrahepatic manifestations of HCV including diabetes mellitus, lymphoma, cryoglublinemia, chronic renal disease, and others that are not associated with the stage of liver disease and have significant morbidity and mortality. All-cause mortality, not only liver-related mortality, has been shown to decline in patients treated successfully compared with unsuccessful therapeutic attempts.
Never before has there been a serious medical illness for which a well-tolerated and highly effective therapy is available that has been subject to denial of therapy based upon cost by third-party payers. This is an unfortunate precedent.
All patients do not require therapy on an urgent basis. However, the decision to initiate therapy should be between a patient and his or her health care provider. Although it would be best if the cost of the medications could be reduced, even at the current costs, Younossi’s study provides clear data to support identification and treatment of HCV patients sooner rather than later.
Dr. Steven L. Flamm is chief of transplantation hepatology and professor of medicine and surgery at Northwestern University Feinberg School of Medicine, Chicago. He is a speaker for AbbVie, Janssen, and Gilead; and consults for AbbVie, Gilead, Janssen, BMS, and Merck.
Chronic HCV infection is a common worldwide problem afflicting approximately 170 million people. HCV has significant morbidity and mortality, and it is currently the leading indication for liver transplantation in the Western world. Yet, the natural history is long, and most patients are asymptomatic and will not develop advanced liver disease.
The recent year has been marked by the stunning approval in the U.S. of all-oral, interferon-free treatments for chronic HCV, including genotypes 1, 2, and 3. Approved regimens are characterized by excellent tolerability and cure (sustained virologic response, SVR) rates for most patient subgroups above 90%. For genotype 1, the most common in the U.S., SVR rates in excess of 95% were observed in clinical trials.
Since the regimens are so well tolerated and effective, the number of patients seeking therapy has increased dramatically. Because the medical regimens are expensive, there have been draconian restrictions by many third-party payers for provision of antiviral therapy for HCV patients. This has led to analyses on cost-effectiveness of contemporary therapy.
The article describing a study presented at AASLD 2014 by Younossi et al. is an important contribution to this discussion. Younossi assessed a computer simulation analysis comparing four strategies for screening and treatment of HCV plus an option of no screening or treatment. He found that birth cohort screening and treatment of all HCV patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY); well below the accepted threshold used to define cost-effectiveness in health care. The assumptions regarding cost of the regimens, the rates of cirrhosis, hepatocellular carcinoma, liver transplantation and liver-related death were appropriate. The conclusion that all baby boomers should be screened and treated is not surprising.
The savings did not include an estimated $3 billion dollars annually in savings from work productivity. The analysis also did not account for the costs associated with many extrahepatic manifestations of HCV including diabetes mellitus, lymphoma, cryoglublinemia, chronic renal disease, and others that are not associated with the stage of liver disease and have significant morbidity and mortality. All-cause mortality, not only liver-related mortality, has been shown to decline in patients treated successfully compared with unsuccessful therapeutic attempts.
Never before has there been a serious medical illness for which a well-tolerated and highly effective therapy is available that has been subject to denial of therapy based upon cost by third-party payers. This is an unfortunate precedent.
All patients do not require therapy on an urgent basis. However, the decision to initiate therapy should be between a patient and his or her health care provider. Although it would be best if the cost of the medications could be reduced, even at the current costs, Younossi’s study provides clear data to support identification and treatment of HCV patients sooner rather than later.
Dr. Steven L. Flamm is chief of transplantation hepatology and professor of medicine and surgery at Northwestern University Feinberg School of Medicine, Chicago. He is a speaker for AbbVie, Janssen, and Gilead; and consults for AbbVie, Gilead, Janssen, BMS, and Merck.
BOSTON – Screening all adults born between 1945 and 1965 for hepatitis C and then treating all infected patients with oral drug regimens is the most cost effective strategy for society, because better outcomes more than offset the higher costs of wider screening and newer drugs, Dr. Zobair Younossi said.
A computer simulation analysis that compared four strategies for screening and treatment (plus the option of no screening or treatment) found that birth cohort screening and treatment of all hepatitis C virus–positive patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY), he reported at the annual meeting of the American Association for the Study of Liver Diseases.
That strategy produced an incremental cost-effectiveness ratio well below the widely accepted threshold of $50,000 per QALY used to define cost effectiveness in health care, said Dr. Younossi, professor of medicine at Virginia Commonwealth University’s Inova Campus and chair of Liver Disease Services for Inova, Falls Church, Va.
In first-generation treatment with direct-acting antivirals – namely, triple therapy with protease inhibitors – the mean cost to achieve a sustained virologic response was $172,889, he said, “and we did not get a lot of pushback from the payers at that point.”
Risk-based screening for HCV has been recommended, and the Centers for Disease Control and Prevention recently recommended birth cohort screening of people born between 1945 and 1965, the so-called baby boomers, Dr. Younossi said.
Still, studies suggest that less than 10% of patients with chronic HCV have been treated successfully, because of the failure of risk-based screening to identify all infected patients and the low efficacy and high rate of side effects from regimens based on interferon and ribavirin, he said.
Higher costs, lower risks
Dr. Younossi’s study used computer simulations to analyze the economic impact of various screening strategies followed by treatment with oral anti-HCV regimens.
The four strategies involved either risk-based screening or birth cohort screening, followed by treatment that either gave all HCV-infected patients oral regimens or that based treatment on staging, giving oral medications only to patients with significant fibrosis. The investigators also considered a fifth strategy: no screening and no treatment.
Birth cohort screening would lead to 1,162,323 patients being diagnosed with previously unknown chronic HCV, they estimated.
To estimate treatment costs, the investigators began with risk-based screening probabilities from a previous study: They assumed that 98% of patients would be medically eligible for treatment and have no contraindications to all-oral treatment regimens, and 98% of those treated would achieve a sustained virologic response for 12 weeks (SVR12), based on results of published trials.
The cost of oral direct-acting antiviral therapy was based on the cost of sofosbuvir – around $1,000 per day for 12 weeks, Dr. Younossi said. Costs for testing, staging, monitoring, and other data were taken from previous treatment models. The investigators calculated QALY from patients’ health utility reports in clinical trials.
Costs averaged approximately $88,000 per patient with birth cohort screening and treating all positive patients, $72,000 per patient with birth cohort screening and treatment based on staging, $60,000-$61,000 per patient for the risk-based screening strategies, and $53,000 per patient with no screening and no treatment.
The probabilities of cirrhosis, hepatocellular carcinoma, or liver transplant were much lower with either birth cohort screening strategy, however, compared with the risk-based strategies or no screening. The probability of cirrhosis was approximately 1% with birth cohort screening and treating all positive patients, 7% with birth cohort screening and treatment based on staging, 55%-60% with the risk-based strategies, and 67% with no screening.
The risk of hepatocellular carcinoma was 4% with birth cohort screening and treating all positive patients, 5% with birth cohort screening and treatment based on staging, 15% with either risk-based screening strategy, and 20% with no screening. The risk of liver transplant was 0.6% with either birth cohort screening strategy, 3% with either risk-based screening strategy, and nearly 4% with no screening.
A total of 4% of patients would be expected to die of liver-related causes after birth cohort screening and treating all positive patients, compared with 7% liver-related mortality after birth cohort screening and staging-based treatment, 25% liver-related mortality in either of the risk-based screening groups, and 34% liver-related mortality with no screening.
HCV costlier than other conditions?
When considering governmental health policy and budgetary issues, Dr. Younossi explained, the cost of curing HCV is not very different from lifetime treatment costs for type 2 diabetes, rheumatoid arthritis, or breast cancer with metastases – and it’s significantly lower than lifetime treatment costs for HIV or relapsing-remitting multiple sclerosis.
As advocates for patients, physicians need to lobby officials so that “as they are dividing the pie, hepatology and HCV are represented,” he said. “These regimens are cost effective.”
The study was an underestimation of savings from birth cohort screening and treating all HCV positives, Dr. Younossi noted, because it did not incorporate an estimated $3 billion per year in savings from work productivity in the United States by curing HCV.
A physician in the audience countered Dr. Younossi’s call for more enlightened health policy supporting funding for HCV treatment, noting that drug companies also need to be pressured to lower the price of the newer drugs.
“The biggest bridge we have to cross is the cost of the drugs,” he said. “This is like denying somebody treatment for tuberculosis by making the cost of the drug too high.”
“I agree,” Dr. Younossi said. “We have to focus on our colleagues in the industry. But we also have to focus on our colleagues in Congress and the policymakers to make sure that, even if we get help from the industry side, we also get help from the policymakers to provide us” with the funding for access to HCV screening and treatment.
Dr. Younossi reported having no financial disclosures. One of his coinvestigators reported financial associations with Gilead and Bristol-Myers Squibb.
On Twitter @sherryboschert
AGA RESOURCE
View the technical review, guideline and clinical decision support tool at www.gastro.org/guideline. Join the guideline authors for a webinar about the guidelines on Jan. 29, 2015, at noon ET. Register at http://ow.ly/FWcsx.
BOSTON – Screening all adults born between 1945 and 1965 for hepatitis C and then treating all infected patients with oral drug regimens is the most cost effective strategy for society, because better outcomes more than offset the higher costs of wider screening and newer drugs, Dr. Zobair Younossi said.
A computer simulation analysis that compared four strategies for screening and treatment (plus the option of no screening or treatment) found that birth cohort screening and treatment of all hepatitis C virus–positive patients would save more than 4 million life-years at an incremental cost of $36,585 per quality-adjusted life-year (QALY), he reported at the annual meeting of the American Association for the Study of Liver Diseases.
That strategy produced an incremental cost-effectiveness ratio well below the widely accepted threshold of $50,000 per QALY used to define cost effectiveness in health care, said Dr. Younossi, professor of medicine at Virginia Commonwealth University’s Inova Campus and chair of Liver Disease Services for Inova, Falls Church, Va.
In first-generation treatment with direct-acting antivirals – namely, triple therapy with protease inhibitors – the mean cost to achieve a sustained virologic response was $172,889, he said, “and we did not get a lot of pushback from the payers at that point.”
Risk-based screening for HCV has been recommended, and the Centers for Disease Control and Prevention recently recommended birth cohort screening of people born between 1945 and 1965, the so-called baby boomers, Dr. Younossi said.
Still, studies suggest that less than 10% of patients with chronic HCV have been treated successfully, because of the failure of risk-based screening to identify all infected patients and the low efficacy and high rate of side effects from regimens based on interferon and ribavirin, he said.
Higher costs, lower risks
Dr. Younossi’s study used computer simulations to analyze the economic impact of various screening strategies followed by treatment with oral anti-HCV regimens.
The four strategies involved either risk-based screening or birth cohort screening, followed by treatment that either gave all HCV-infected patients oral regimens or that based treatment on staging, giving oral medications only to patients with significant fibrosis. The investigators also considered a fifth strategy: no screening and no treatment.
Birth cohort screening would lead to 1,162,323 patients being diagnosed with previously unknown chronic HCV, they estimated.
To estimate treatment costs, the investigators began with risk-based screening probabilities from a previous study: They assumed that 98% of patients would be medically eligible for treatment and have no contraindications to all-oral treatment regimens, and 98% of those treated would achieve a sustained virologic response for 12 weeks (SVR12), based on results of published trials.
The cost of oral direct-acting antiviral therapy was based on the cost of sofosbuvir – around $1,000 per day for 12 weeks, Dr. Younossi said. Costs for testing, staging, monitoring, and other data were taken from previous treatment models. The investigators calculated QALY from patients’ health utility reports in clinical trials.
Costs averaged approximately $88,000 per patient with birth cohort screening and treating all positive patients, $72,000 per patient with birth cohort screening and treatment based on staging, $60,000-$61,000 per patient for the risk-based screening strategies, and $53,000 per patient with no screening and no treatment.
The probabilities of cirrhosis, hepatocellular carcinoma, or liver transplant were much lower with either birth cohort screening strategy, however, compared with the risk-based strategies or no screening. The probability of cirrhosis was approximately 1% with birth cohort screening and treating all positive patients, 7% with birth cohort screening and treatment based on staging, 55%-60% with the risk-based strategies, and 67% with no screening.
The risk of hepatocellular carcinoma was 4% with birth cohort screening and treating all positive patients, 5% with birth cohort screening and treatment based on staging, 15% with either risk-based screening strategy, and 20% with no screening. The risk of liver transplant was 0.6% with either birth cohort screening strategy, 3% with either risk-based screening strategy, and nearly 4% with no screening.
A total of 4% of patients would be expected to die of liver-related causes after birth cohort screening and treating all positive patients, compared with 7% liver-related mortality after birth cohort screening and staging-based treatment, 25% liver-related mortality in either of the risk-based screening groups, and 34% liver-related mortality with no screening.
HCV costlier than other conditions?
When considering governmental health policy and budgetary issues, Dr. Younossi explained, the cost of curing HCV is not very different from lifetime treatment costs for type 2 diabetes, rheumatoid arthritis, or breast cancer with metastases – and it’s significantly lower than lifetime treatment costs for HIV or relapsing-remitting multiple sclerosis.
As advocates for patients, physicians need to lobby officials so that “as they are dividing the pie, hepatology and HCV are represented,” he said. “These regimens are cost effective.”
The study was an underestimation of savings from birth cohort screening and treating all HCV positives, Dr. Younossi noted, because it did not incorporate an estimated $3 billion per year in savings from work productivity in the United States by curing HCV.
A physician in the audience countered Dr. Younossi’s call for more enlightened health policy supporting funding for HCV treatment, noting that drug companies also need to be pressured to lower the price of the newer drugs.
“The biggest bridge we have to cross is the cost of the drugs,” he said. “This is like denying somebody treatment for tuberculosis by making the cost of the drug too high.”
“I agree,” Dr. Younossi said. “We have to focus on our colleagues in the industry. But we also have to focus on our colleagues in Congress and the policymakers to make sure that, even if we get help from the industry side, we also get help from the policymakers to provide us” with the funding for access to HCV screening and treatment.
Dr. Younossi reported having no financial disclosures. One of his coinvestigators reported financial associations with Gilead and Bristol-Myers Squibb.
On Twitter @sherryboschert
AGA RESOURCE
View the technical review, guideline and clinical decision support tool at www.gastro.org/guideline. Join the guideline authors for a webinar about the guidelines on Jan. 29, 2015, at noon ET. Register at http://ow.ly/FWcsx.
AT THE LIVER MEETING 2014
Key clinical point: Screening adults born in 1945-1965 and treating all who have HCV with oral anti-HCV regimens is most cost effective.
Major finding: The strategy’s incremental cost of $36,585 is below the $50,000 per QALY threshold for cost effectiveness.
Data source: A computer simulation analysis that compared four strategies for screening and treatment, with treatment costs based on an estimated $1,000/day for sofosbuvir.
Disclosures: Dr. Younossi reported having no financial disclosures. One of his coinvestigators reported financial associations with Gilead, which markets sofosbuvir, and Bristol-Myers Squibb.
Adding terlipressin didn’t help hepatorenal syndrome
BOSTON – Treating patients with hepatorenal syndrome type 1 for up to 14 days using terlipressin plus albumin rather than albumin alone did not improve the chances of confirmed reversal of hepatorenal syndrome in a multicenter, randomized, double-blind, placebo-controlled trial in 196 patients.
Investigators confirmed reversal of hepatorenal syndrome type 1 (HRS-1) in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%), a difference between groups that was not statistically significant, Dr. Thomas D. Boyer reported at the annual meeting of the American Association for the Study of Liver Diseases.
He and his associates defined confirmed reversal of HRS-1 as two serum creatinine values no higher than 1.5 mg/dL at least 48 hours apart while on treatment, without renal replacement therapy or liver transplant.
Secondary outcomes included reversal of HRS-1, defined as a decrease in serum creatinine to no higher than 1.5 mg/dL. This goal was reached by 23 patients on terlipressin plus albumin, and 15 patients on albumin alone achieved reversal of HRS-1 (24% vs. 15%, respectively), a difference that also was not statistically significant.
Among other secondary outcomes, though, terlipressin showed some potential advantages in subgroup analyses, said Dr. Boyer, professor of medicine and director of the Liver Research Institute at the University of Arizona, Tucson.
Significantly greater improvements in serum creatinine during treatment with terlipressin correlated with survival. Compared with baseline levels, serum creatinine decreased by 1.2 mg/dL in the terlipressin group and 0.6 mg/dL in the placebo group, a statistically significant difference between groups.
All 19 patients who achieve confirmed reversal of HRS-1 on terlipressin were alive without renal replacement therapy at 90-day follow-up, significantly more than the 6 of 13 patients with confirmed reversal of HRS-1 in the placebo group who remained alive at 90 days (46%).
Overall survival and transplant-free survival rates did not differ significantly between groups.
Serious adverse events occurred in 59 patients in the terlipressin group (61%) and 53 patients in the placebo group (54%), rates that did not differ significantly between groups. No new or unexpected adverse events were seen.
The REVERSE trial (Phase III, Multi-Center Randomized, Placebo-Controlled, Double-Blind Study to Confirm the Reversal of Hepatorenal Syndrome Type 1 with Lucassin [Terlipressin]) enrolled adults with cirrhosis, ascites, and HRS-1. The study defined HRS-1 as rapidly deteriorating renal function that didn’t improve within 48 hours of diuretic withdrawal and albumin-fluid challenge. Rapidly deteriorating renal function was defined as a serum creatinine level of at least 2.5 mg/dL and actual or projected doubling of serum creatinine within 2 weeks. Improvement in renal function was defined as less than a 20% decrease in serum creatinine and a serum creatinine level of at least 2.5 mg/dL.
Patients received IV infusions of 6 mg terlipressin or placebo every 6 hours, plus albumin.
Ikaria, which markets terlipressin (Lucassin), funded the study. Dr. Boyer is a consultant for Ikaria and he reported financial associations with AbbVie, Gilead, and Merck. His associates reported financial associations with Ikaria and multiple companies.
On Twitter @sherryboschert
BOSTON – Treating patients with hepatorenal syndrome type 1 for up to 14 days using terlipressin plus albumin rather than albumin alone did not improve the chances of confirmed reversal of hepatorenal syndrome in a multicenter, randomized, double-blind, placebo-controlled trial in 196 patients.
Investigators confirmed reversal of hepatorenal syndrome type 1 (HRS-1) in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%), a difference between groups that was not statistically significant, Dr. Thomas D. Boyer reported at the annual meeting of the American Association for the Study of Liver Diseases.
He and his associates defined confirmed reversal of HRS-1 as two serum creatinine values no higher than 1.5 mg/dL at least 48 hours apart while on treatment, without renal replacement therapy or liver transplant.
Secondary outcomes included reversal of HRS-1, defined as a decrease in serum creatinine to no higher than 1.5 mg/dL. This goal was reached by 23 patients on terlipressin plus albumin, and 15 patients on albumin alone achieved reversal of HRS-1 (24% vs. 15%, respectively), a difference that also was not statistically significant.
Among other secondary outcomes, though, terlipressin showed some potential advantages in subgroup analyses, said Dr. Boyer, professor of medicine and director of the Liver Research Institute at the University of Arizona, Tucson.
Significantly greater improvements in serum creatinine during treatment with terlipressin correlated with survival. Compared with baseline levels, serum creatinine decreased by 1.2 mg/dL in the terlipressin group and 0.6 mg/dL in the placebo group, a statistically significant difference between groups.
All 19 patients who achieve confirmed reversal of HRS-1 on terlipressin were alive without renal replacement therapy at 90-day follow-up, significantly more than the 6 of 13 patients with confirmed reversal of HRS-1 in the placebo group who remained alive at 90 days (46%).
Overall survival and transplant-free survival rates did not differ significantly between groups.
Serious adverse events occurred in 59 patients in the terlipressin group (61%) and 53 patients in the placebo group (54%), rates that did not differ significantly between groups. No new or unexpected adverse events were seen.
The REVERSE trial (Phase III, Multi-Center Randomized, Placebo-Controlled, Double-Blind Study to Confirm the Reversal of Hepatorenal Syndrome Type 1 with Lucassin [Terlipressin]) enrolled adults with cirrhosis, ascites, and HRS-1. The study defined HRS-1 as rapidly deteriorating renal function that didn’t improve within 48 hours of diuretic withdrawal and albumin-fluid challenge. Rapidly deteriorating renal function was defined as a serum creatinine level of at least 2.5 mg/dL and actual or projected doubling of serum creatinine within 2 weeks. Improvement in renal function was defined as less than a 20% decrease in serum creatinine and a serum creatinine level of at least 2.5 mg/dL.
Patients received IV infusions of 6 mg terlipressin or placebo every 6 hours, plus albumin.
Ikaria, which markets terlipressin (Lucassin), funded the study. Dr. Boyer is a consultant for Ikaria and he reported financial associations with AbbVie, Gilead, and Merck. His associates reported financial associations with Ikaria and multiple companies.
On Twitter @sherryboschert
BOSTON – Treating patients with hepatorenal syndrome type 1 for up to 14 days using terlipressin plus albumin rather than albumin alone did not improve the chances of confirmed reversal of hepatorenal syndrome in a multicenter, randomized, double-blind, placebo-controlled trial in 196 patients.
Investigators confirmed reversal of hepatorenal syndrome type 1 (HRS-1) in 19 of 97 patients on terlipressin plus albumin (20%) and 13 of 99 patients on albumin plus placebo (13%), a difference between groups that was not statistically significant, Dr. Thomas D. Boyer reported at the annual meeting of the American Association for the Study of Liver Diseases.
He and his associates defined confirmed reversal of HRS-1 as two serum creatinine values no higher than 1.5 mg/dL at least 48 hours apart while on treatment, without renal replacement therapy or liver transplant.
Secondary outcomes included reversal of HRS-1, defined as a decrease in serum creatinine to no higher than 1.5 mg/dL. This goal was reached by 23 patients on terlipressin plus albumin, and 15 patients on albumin alone achieved reversal of HRS-1 (24% vs. 15%, respectively), a difference that also was not statistically significant.
Among other secondary outcomes, though, terlipressin showed some potential advantages in subgroup analyses, said Dr. Boyer, professor of medicine and director of the Liver Research Institute at the University of Arizona, Tucson.
Significantly greater improvements in serum creatinine during treatment with terlipressin correlated with survival. Compared with baseline levels, serum creatinine decreased by 1.2 mg/dL in the terlipressin group and 0.6 mg/dL in the placebo group, a statistically significant difference between groups.
All 19 patients who achieve confirmed reversal of HRS-1 on terlipressin were alive without renal replacement therapy at 90-day follow-up, significantly more than the 6 of 13 patients with confirmed reversal of HRS-1 in the placebo group who remained alive at 90 days (46%).
Overall survival and transplant-free survival rates did not differ significantly between groups.
Serious adverse events occurred in 59 patients in the terlipressin group (61%) and 53 patients in the placebo group (54%), rates that did not differ significantly between groups. No new or unexpected adverse events were seen.
The REVERSE trial (Phase III, Multi-Center Randomized, Placebo-Controlled, Double-Blind Study to Confirm the Reversal of Hepatorenal Syndrome Type 1 with Lucassin [Terlipressin]) enrolled adults with cirrhosis, ascites, and HRS-1. The study defined HRS-1 as rapidly deteriorating renal function that didn’t improve within 48 hours of diuretic withdrawal and albumin-fluid challenge. Rapidly deteriorating renal function was defined as a serum creatinine level of at least 2.5 mg/dL and actual or projected doubling of serum creatinine within 2 weeks. Improvement in renal function was defined as less than a 20% decrease in serum creatinine and a serum creatinine level of at least 2.5 mg/dL.
Patients received IV infusions of 6 mg terlipressin or placebo every 6 hours, plus albumin.
Ikaria, which markets terlipressin (Lucassin), funded the study. Dr. Boyer is a consultant for Ikaria and he reported financial associations with AbbVie, Gilead, and Merck. His associates reported financial associations with Ikaria and multiple companies.
On Twitter @sherryboschert
AT THE LIVER MEETING 2014
Key clinical point: Adding terlipressin to albumin didn’t help reverse hepatorenal syndrome type 1, but there were hints of improved survival.
Major finding: Confirmed reversal of HRS-1 occurred in 20% on terlipressin and albumin and 13% on placebo and albumin.
Data source: A multicenter, randomized, controlled, double-blind trial in 196 adults with cirrhosis, ascites, and HRS-1.
Disclosures: Ikaria, which markets terlipressin (Lucassin), funded the study. Dr. Boyer is a consultant for Ikaria and he reported financial associations with AbbVie, Gilead, and Merck. His associates reported financial associations with Ikaria and multiple companies.
Diet, exercise reduced portal hypertension in obese cirrhotic patients
BOSTON – A 16-week diet and exercise program reduced body weight and portal pressure in a prospective pilot study of 50 obese patients with cirrhosis and portal hypertension.
Twenty-six patients achieved a clinically relevant weight loss of at least 5%, compared with baseline weight (52% of the cohort). The hepatic venous pressure gradient (HVPG) decreased by at least 10% in 21 patients (42%), compared with baseline, Dr. Annalisa Berzigotti and her associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
Obesity has been shown to increase the risk of clinical decompensation in patients with compensated cirrhosis and portal hypertension, possibly by increasing portal hypertension, said Dr. Berzigotti of the Networked Research Center for Hepatic and Digestive Diseases (CIBERehd), Barcelona.
“An intensive 16-week program of tailored diet and moderate exercise can be safely recommended to obtain weight loss,” she said.
Dr. Berzigotti and her associates at two Spanish centers put patients through a 16-week program of a normoproteic, hypocaloric diet supervised by nutritionists. It followed a personalized decrease of 500-1,000 kcal/day, with 20%-25% of the diet consisting of proteins. The exercise intervention consisted of 60 minutes per week of supervised, moderately-intense physical activity in small groups plus personalized advice and use of a daily physical activity log.
Patients had a baseline HVPG of at least 6 mm Hg with or without esophageal varices and regardless of whether they were receiving nonselective beta-blocker medications.
The investigators recruited 60 patients, 50 of whom completed the study and were included in the analysis.
The lifestyle intervention decreased the mean body weight by 5 kg and the median body weight by 5%, which was associated with significant decreases in waist circumference and percentage body fat. Eight patients achieved at least a 10% reduction in body weight (16%), she reported.
The mean HVPG decreased significantly from 13.9 mm Hg at baseline to 12.3 mm Hg after treatment, with an average 11% reduction. The HVPG decreased by at least 20% in 12 patients (24%).
Four patients who lost at least 5% of their body weight reduced their HVPG to below 10 mm Hg. Patients who lost at least 10% of body weight reduced their HVPG to a greater degree than did patients who lost less than 10% of body weight, with 24% and 8% reductions in HVPG, respectively.
Changes in body weight and HVPG were more subtle in patients with diabetes than in those without diabetes. Results did not differ significantly across other subgroups based on cirrhosis etiology, clinically significant portal hypertension and esophageal varices, treatment with nonselective beta-blockers, history of variceal bleeding, or medical center.
No patients clinically decompensated during the study. Patients’ Child-Pugh scores and Model for End-Stage Liver Disease scores did not change.
Patients who lost weight kept it off for 6 months, with average weights of 86 kg at 16 weeks and 85 kg at a 6-month follow-up.
Patients had a mean age of 56 years and 62% were male. The etiologies of cirrhosis were viral in 36% of patients, alcoholic in 38%, and nonalcoholic steatohepatitis in 26%. Patients had an average body mass index of 33 kg/m2, and 72% had an HVPG of at least 10 mm Hg at baseline. Thirty percent of patients had a previous variceal hemorrhage but currently were compensated. Sixty-two percent of patients had a history of esophageal varices and 60% were on nonselective beta-blockers.
Dr. Berzigotti reported having no financial disclosures. One of her associates reported financial associations with Falk, Gilead, Norgine, Ono Pharma USA, Intercept Pharmaceuticals, Exalenz Bioscience, Almirall, and Conatus Pharmaceuticals.
On Twitter @sherryboschert
BOSTON – A 16-week diet and exercise program reduced body weight and portal pressure in a prospective pilot study of 50 obese patients with cirrhosis and portal hypertension.
Twenty-six patients achieved a clinically relevant weight loss of at least 5%, compared with baseline weight (52% of the cohort). The hepatic venous pressure gradient (HVPG) decreased by at least 10% in 21 patients (42%), compared with baseline, Dr. Annalisa Berzigotti and her associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
Obesity has been shown to increase the risk of clinical decompensation in patients with compensated cirrhosis and portal hypertension, possibly by increasing portal hypertension, said Dr. Berzigotti of the Networked Research Center for Hepatic and Digestive Diseases (CIBERehd), Barcelona.
“An intensive 16-week program of tailored diet and moderate exercise can be safely recommended to obtain weight loss,” she said.
Dr. Berzigotti and her associates at two Spanish centers put patients through a 16-week program of a normoproteic, hypocaloric diet supervised by nutritionists. It followed a personalized decrease of 500-1,000 kcal/day, with 20%-25% of the diet consisting of proteins. The exercise intervention consisted of 60 minutes per week of supervised, moderately-intense physical activity in small groups plus personalized advice and use of a daily physical activity log.
Patients had a baseline HVPG of at least 6 mm Hg with or without esophageal varices and regardless of whether they were receiving nonselective beta-blocker medications.
The investigators recruited 60 patients, 50 of whom completed the study and were included in the analysis.
The lifestyle intervention decreased the mean body weight by 5 kg and the median body weight by 5%, which was associated with significant decreases in waist circumference and percentage body fat. Eight patients achieved at least a 10% reduction in body weight (16%), she reported.
The mean HVPG decreased significantly from 13.9 mm Hg at baseline to 12.3 mm Hg after treatment, with an average 11% reduction. The HVPG decreased by at least 20% in 12 patients (24%).
Four patients who lost at least 5% of their body weight reduced their HVPG to below 10 mm Hg. Patients who lost at least 10% of body weight reduced their HVPG to a greater degree than did patients who lost less than 10% of body weight, with 24% and 8% reductions in HVPG, respectively.
Changes in body weight and HVPG were more subtle in patients with diabetes than in those without diabetes. Results did not differ significantly across other subgroups based on cirrhosis etiology, clinically significant portal hypertension and esophageal varices, treatment with nonselective beta-blockers, history of variceal bleeding, or medical center.
No patients clinically decompensated during the study. Patients’ Child-Pugh scores and Model for End-Stage Liver Disease scores did not change.
Patients who lost weight kept it off for 6 months, with average weights of 86 kg at 16 weeks and 85 kg at a 6-month follow-up.
Patients had a mean age of 56 years and 62% were male. The etiologies of cirrhosis were viral in 36% of patients, alcoholic in 38%, and nonalcoholic steatohepatitis in 26%. Patients had an average body mass index of 33 kg/m2, and 72% had an HVPG of at least 10 mm Hg at baseline. Thirty percent of patients had a previous variceal hemorrhage but currently were compensated. Sixty-two percent of patients had a history of esophageal varices and 60% were on nonselective beta-blockers.
Dr. Berzigotti reported having no financial disclosures. One of her associates reported financial associations with Falk, Gilead, Norgine, Ono Pharma USA, Intercept Pharmaceuticals, Exalenz Bioscience, Almirall, and Conatus Pharmaceuticals.
On Twitter @sherryboschert
BOSTON – A 16-week diet and exercise program reduced body weight and portal pressure in a prospective pilot study of 50 obese patients with cirrhosis and portal hypertension.
Twenty-six patients achieved a clinically relevant weight loss of at least 5%, compared with baseline weight (52% of the cohort). The hepatic venous pressure gradient (HVPG) decreased by at least 10% in 21 patients (42%), compared with baseline, Dr. Annalisa Berzigotti and her associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
Obesity has been shown to increase the risk of clinical decompensation in patients with compensated cirrhosis and portal hypertension, possibly by increasing portal hypertension, said Dr. Berzigotti of the Networked Research Center for Hepatic and Digestive Diseases (CIBERehd), Barcelona.
“An intensive 16-week program of tailored diet and moderate exercise can be safely recommended to obtain weight loss,” she said.
Dr. Berzigotti and her associates at two Spanish centers put patients through a 16-week program of a normoproteic, hypocaloric diet supervised by nutritionists. It followed a personalized decrease of 500-1,000 kcal/day, with 20%-25% of the diet consisting of proteins. The exercise intervention consisted of 60 minutes per week of supervised, moderately-intense physical activity in small groups plus personalized advice and use of a daily physical activity log.
Patients had a baseline HVPG of at least 6 mm Hg with or without esophageal varices and regardless of whether they were receiving nonselective beta-blocker medications.
The investigators recruited 60 patients, 50 of whom completed the study and were included in the analysis.
The lifestyle intervention decreased the mean body weight by 5 kg and the median body weight by 5%, which was associated with significant decreases in waist circumference and percentage body fat. Eight patients achieved at least a 10% reduction in body weight (16%), she reported.
The mean HVPG decreased significantly from 13.9 mm Hg at baseline to 12.3 mm Hg after treatment, with an average 11% reduction. The HVPG decreased by at least 20% in 12 patients (24%).
Four patients who lost at least 5% of their body weight reduced their HVPG to below 10 mm Hg. Patients who lost at least 10% of body weight reduced their HVPG to a greater degree than did patients who lost less than 10% of body weight, with 24% and 8% reductions in HVPG, respectively.
Changes in body weight and HVPG were more subtle in patients with diabetes than in those without diabetes. Results did not differ significantly across other subgroups based on cirrhosis etiology, clinically significant portal hypertension and esophageal varices, treatment with nonselective beta-blockers, history of variceal bleeding, or medical center.
No patients clinically decompensated during the study. Patients’ Child-Pugh scores and Model for End-Stage Liver Disease scores did not change.
Patients who lost weight kept it off for 6 months, with average weights of 86 kg at 16 weeks and 85 kg at a 6-month follow-up.
Patients had a mean age of 56 years and 62% were male. The etiologies of cirrhosis were viral in 36% of patients, alcoholic in 38%, and nonalcoholic steatohepatitis in 26%. Patients had an average body mass index of 33 kg/m2, and 72% had an HVPG of at least 10 mm Hg at baseline. Thirty percent of patients had a previous variceal hemorrhage but currently were compensated. Sixty-two percent of patients had a history of esophageal varices and 60% were on nonselective beta-blockers.
Dr. Berzigotti reported having no financial disclosures. One of her associates reported financial associations with Falk, Gilead, Norgine, Ono Pharma USA, Intercept Pharmaceuticals, Exalenz Bioscience, Almirall, and Conatus Pharmaceuticals.
On Twitter @sherryboschert
AT THE LIVER MEETING 2014
Key clinical point: A 16-week lifestyle intervention safely reduced body weight and portal pressure in obese patients with cirrhosis.
Major finding: Clinically relevant weight loss occurred in 26 patients (52%) and the HVPG decreased by at least 10% in 21 patients (42%), compared with baseline.
Data source: A prospective, multicenter pilot study of 50 obese patients with cirrhosis and portal hypertension.
Disclosures:Dr. Berzigotti reported having no financial disclosures. One of her associates reported ties with Falk, Gilead, Norgine, Ono Pharma USA, Intercept Pharmaceuticals, Exalenz Bioscience, Almirall, and Conatus Pharmaceuticals.
Vasopressor terlipressin helped patients with cirrhosis, shock
BOSTON – Terlipressin proved noninferior to noradrenaline as a vasopressor for patients with cirrhosis and septic shock in an open-label study that randomized 84 patients.
Terlipressin also seemed to provide advantages over noradrenaline by contributing to greater hemodynamic stability, improved urine output, reduced variceal bleeding, a lower risk of spontaneous bacterial peritonitis, and reduced mortality in the first 48 hours but not at 28 days, Dr. Ashok K. Choudhury and his associates reported.
“Terlipressin is noninferior to noradrenaline as a vasopressor,” he said at the annual meeting of the American Association for the Study of Liver Diseases.
The investigators randomized consecutive, matched adults with cirrhosis and septic shock not responding to fluid resuscitation for 2 hours. They aimed to achieve a mean arterial pressure (MAP) > 65 mm Hg at 6 hours by treating 42 patients with a continuous infusion of terlipressin 1.3-5.2 mcg/min, stepped up every 15 minutes, and 42 patients with noradrenaline 7.5-6 mcg/min, stepped up every 15 minutes. Both groups received standard medical care of intravenous fluids, antibiotics, and ICU care.
The target MAP was reached within 6 hours in 28 patients on terlipressin (67%) and 23 patients on noradrenaline (55%), a difference that was not statistically significant, said Dr. Choudhury of the Institute of Liver and Biliary Sciences, New Delhi. He won a research award from the Association.
Patients in the two groups were matched by age, sex, etiology and severity of cirrhosis, and scores on the Model for End-Stage Liver Disease and the Sequential Organ Failure Assessment.
Spontaneous bacterial peritonitis was the main cause of sepsis at admission, followed by pneumonia, but pneumonia was the main cause of “second hit” pneumonia, he said.
Terlipressin therapy was associated with a lower failure rate at 6 hours, a greater likelihood of MAP maintenance with cessation of vasopressor requirements at 48 hours, and improved urine output at 24 hours, compared with noradrenaline treatment. At 48 hours, 19 of 40 patients on terlipressin (48%) and 11 of 30 patients on noradrenaline (36%) had an MAP > 65 mm Hg.
No patients on terlipressin developed a variceal bleed, compared with seven patients in the noradrenaline group (10%). Overall rates of adverse events did not differ significantly between groups, but were higher in the terlipressin group than in the noradrenaline group.
Better rates of lactate clearance, central venous oxygen saturation, and carbon dioxide gradient in venous-arterial blood gases in the terlipressin group were not statistically different from rates in the noradrenaline group.
Significantly more patients on terlipressin survived the first 48 hours than patients on noradrenaline, but by day 28 of follow-up survival rates did not differ significantly between groups.
On the whole, septic shock in these patients with cirrhosis was associated with a high mortality rate (80%). Twelve percent of patients were responsive to fluids in 2 hours.
Dr. Choudhury reported having no financial disclosures.
On Twitter @sherryboschert
BOSTON – Terlipressin proved noninferior to noradrenaline as a vasopressor for patients with cirrhosis and septic shock in an open-label study that randomized 84 patients.
Terlipressin also seemed to provide advantages over noradrenaline by contributing to greater hemodynamic stability, improved urine output, reduced variceal bleeding, a lower risk of spontaneous bacterial peritonitis, and reduced mortality in the first 48 hours but not at 28 days, Dr. Ashok K. Choudhury and his associates reported.
“Terlipressin is noninferior to noradrenaline as a vasopressor,” he said at the annual meeting of the American Association for the Study of Liver Diseases.
The investigators randomized consecutive, matched adults with cirrhosis and septic shock not responding to fluid resuscitation for 2 hours. They aimed to achieve a mean arterial pressure (MAP) > 65 mm Hg at 6 hours by treating 42 patients with a continuous infusion of terlipressin 1.3-5.2 mcg/min, stepped up every 15 minutes, and 42 patients with noradrenaline 7.5-6 mcg/min, stepped up every 15 minutes. Both groups received standard medical care of intravenous fluids, antibiotics, and ICU care.
The target MAP was reached within 6 hours in 28 patients on terlipressin (67%) and 23 patients on noradrenaline (55%), a difference that was not statistically significant, said Dr. Choudhury of the Institute of Liver and Biliary Sciences, New Delhi. He won a research award from the Association.
Patients in the two groups were matched by age, sex, etiology and severity of cirrhosis, and scores on the Model for End-Stage Liver Disease and the Sequential Organ Failure Assessment.
Spontaneous bacterial peritonitis was the main cause of sepsis at admission, followed by pneumonia, but pneumonia was the main cause of “second hit” pneumonia, he said.
Terlipressin therapy was associated with a lower failure rate at 6 hours, a greater likelihood of MAP maintenance with cessation of vasopressor requirements at 48 hours, and improved urine output at 24 hours, compared with noradrenaline treatment. At 48 hours, 19 of 40 patients on terlipressin (48%) and 11 of 30 patients on noradrenaline (36%) had an MAP > 65 mm Hg.
No patients on terlipressin developed a variceal bleed, compared with seven patients in the noradrenaline group (10%). Overall rates of adverse events did not differ significantly between groups, but were higher in the terlipressin group than in the noradrenaline group.
Better rates of lactate clearance, central venous oxygen saturation, and carbon dioxide gradient in venous-arterial blood gases in the terlipressin group were not statistically different from rates in the noradrenaline group.
Significantly more patients on terlipressin survived the first 48 hours than patients on noradrenaline, but by day 28 of follow-up survival rates did not differ significantly between groups.
On the whole, septic shock in these patients with cirrhosis was associated with a high mortality rate (80%). Twelve percent of patients were responsive to fluids in 2 hours.
Dr. Choudhury reported having no financial disclosures.
On Twitter @sherryboschert
BOSTON – Terlipressin proved noninferior to noradrenaline as a vasopressor for patients with cirrhosis and septic shock in an open-label study that randomized 84 patients.
Terlipressin also seemed to provide advantages over noradrenaline by contributing to greater hemodynamic stability, improved urine output, reduced variceal bleeding, a lower risk of spontaneous bacterial peritonitis, and reduced mortality in the first 48 hours but not at 28 days, Dr. Ashok K. Choudhury and his associates reported.
“Terlipressin is noninferior to noradrenaline as a vasopressor,” he said at the annual meeting of the American Association for the Study of Liver Diseases.
The investigators randomized consecutive, matched adults with cirrhosis and septic shock not responding to fluid resuscitation for 2 hours. They aimed to achieve a mean arterial pressure (MAP) > 65 mm Hg at 6 hours by treating 42 patients with a continuous infusion of terlipressin 1.3-5.2 mcg/min, stepped up every 15 minutes, and 42 patients with noradrenaline 7.5-6 mcg/min, stepped up every 15 minutes. Both groups received standard medical care of intravenous fluids, antibiotics, and ICU care.
The target MAP was reached within 6 hours in 28 patients on terlipressin (67%) and 23 patients on noradrenaline (55%), a difference that was not statistically significant, said Dr. Choudhury of the Institute of Liver and Biliary Sciences, New Delhi. He won a research award from the Association.
Patients in the two groups were matched by age, sex, etiology and severity of cirrhosis, and scores on the Model for End-Stage Liver Disease and the Sequential Organ Failure Assessment.
Spontaneous bacterial peritonitis was the main cause of sepsis at admission, followed by pneumonia, but pneumonia was the main cause of “second hit” pneumonia, he said.
Terlipressin therapy was associated with a lower failure rate at 6 hours, a greater likelihood of MAP maintenance with cessation of vasopressor requirements at 48 hours, and improved urine output at 24 hours, compared with noradrenaline treatment. At 48 hours, 19 of 40 patients on terlipressin (48%) and 11 of 30 patients on noradrenaline (36%) had an MAP > 65 mm Hg.
No patients on terlipressin developed a variceal bleed, compared with seven patients in the noradrenaline group (10%). Overall rates of adverse events did not differ significantly between groups, but were higher in the terlipressin group than in the noradrenaline group.
Better rates of lactate clearance, central venous oxygen saturation, and carbon dioxide gradient in venous-arterial blood gases in the terlipressin group were not statistically different from rates in the noradrenaline group.
Significantly more patients on terlipressin survived the first 48 hours than patients on noradrenaline, but by day 28 of follow-up survival rates did not differ significantly between groups.
On the whole, septic shock in these patients with cirrhosis was associated with a high mortality rate (80%). Twelve percent of patients were responsive to fluids in 2 hours.
Dr. Choudhury reported having no financial disclosures.
On Twitter @sherryboschert
AT THE LIVER MEETING 2014
Key clinical point: Terlipressin worked as well as noradrenaline as a vasopressor.
Major finding: Treatment achieved a MAP of >65 mm Hg by 6 hours in 28 patients on terlipressin (67%) and in 23 patients on noradrenaline (55%).
Data source: A prospective, randomized, open-label study of 84 patients with cirrhosis and septic shock.
Disclosures: Dr. Choudhury reported having no financial disclosures.
Axial spondyloarthropathy guidelines: NSAIDs and PT first
BOSTON – A nonsteroidal anti-inflammatory drug and exercise may be enough to control active axial spondyloarthritis in some patients, suggest authors of draft guidelines on the management of patients with the condition.
The guidelines, not ready for prime time, have yet to be reviewed or endorsed by the American College of Rheumatology (ACR) and the Spondylitis Association of America, or the SpondyloArthritis Research and Treatment Network (SPARTAN), and are subject to change, emphasized Dr. Michael M. Ward, senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
With that caveat in mind, Dr. Ward presented a sneak peek at the guidelines to a standing-room only crowd at the ACR annual meeting in Boston.
Some definitions
The guidelines offer recommendations on the management of patients with active and stable ankylosing spondylitis (AS) and axial spondyloarthropathies (axSpA) that are symptomatic but without radiographic evidence (nonradiographic, or nr-axSpA).
Active AS is defined as disease that causes symptoms at an unacceptably burdensome level as reported by the patient that are judged by the examining clinician to be caused by AS. The same definition also applies to nr-axSpA.
Stable disease is defined as either an asymptomatic state or symptoms that were previously bothersome but are currently at an acceptable level as reported by the patient. The patient had to have had bothersome symptoms for at least 6 months before entering the stable disease state. This definition is also applicable to stable nr-axSpA.
The investigators considered the best available evidence on the use of NSAIDs (running the gamut from aspirin to tolmetin), slow-acting antirheumatic agents such as methotrexate, glucocorticoids (prednisone and others), tumor necrosis factor (TNF) inhibitors, such as adalimumab, etanercept, and others), and non-TNF biologic agents (abatacept, rituximab, tocilizumab, and others).
Active AS
Dr. Ward presented a management flow tree for patients with active AS, starting with a strong recommendation for an NSAID, conditionally recommended to be used continuously. The authors felt, however, that there was not enough evidence to support the use of one NSAID over another. They also strongly recommended physical therapy, with less robust recommendations for active than for passive exercise and for exercises performed in water rather than on land. The latter recommendation is based on the fact that, although water-based exercises have been shown to be as good as or better than dry land exercises for relieving symptoms, water-based exercise may be impractical for many patients, Dr. Ward noted.
For patients whose disease remains active despite NSAIDs and exercise, the committee strongly recommends use of a tumor necrosis factor inhibitor (TNFi) (no specific agent preferred). If a patient on a TNFi has recurrent iritis, the guidelines have a conditional recommendation for the use of infliximab or adalimumab. For patients with inflammatory bowel disease (IBD), the authors conditionally recommend a TNFi monoclonal antibody as opposed to etanercept.
If the disease remains active on a TNFi, an alternative TNFi can be considered.
“For patients who have contraindications to TNF inhibitors, we considered the choice between adding a slow-acting drug such as sulfasalazine or pamidronate or treating with a non-TNF biologic. Of course, there are no head-to-head trials between those two options, so based on the indirect evidence that’s available, the committee voted for a conditional recommendation against the use of a non-TNF biologic in favor of a slow-acting drug in that setting,” Dr. Ward said.
If there are no contraindications to a TNF inhibitor, however, the committee strongly favored the use of a TNF inhibitor over a slow-acting agent, he emphasized.
For patients who have isolated sacroiliitis, peripheral arthritis, or enthesis, the committee provisionally recommends local injection of a glucocorticoid, with cautions to use infrequently and only if two or fewer joints are involved in peripheral arthritis, and avoidance of injection of the Achilles, patellar, or quadriceps tendons in patients with enthesitis.
For all patients, the guidelines half-heartedly recommend monitoring validated axSpA disease activity measures and C-reactive protein and erythrocyte sedimentation rate (ESR). The group also conditionally supported unsupervised back exercises, formal group or individual self-management education, and fall evaluation and counseling.
Committee members strongly felt that systemic glucocorticoids should not be used in patients with active axSpA, except in cases where a short-term course with quick taper may be helpful, such as in patients with peripheral flare, or during pregnancy or a concomitant IBD flare.
Stable AS
“For patients with stable ankylosing spondylitis who are on combination therapy, either combination therapy with NSAIDs and a TNF inhibitor, or a slow-acting drug and a TNF inhibitor, the committee voted against continuation of a combination in favor of TNF monotherapy. It’s a conditional recommendation, so there certainly would be situations where one would not want to do that, but in general the committee thought that was the preferable approach, balancing the benefits and potential risks of combination therapy against monotherapy in patients with stable AS,” Dr. Ward said.
The committee members strongly supported physical therapy in patients with stable AS and gave a conditional nod to monitoring, back exercises, group support, and fall counseling.
For patients with stable AS and advanced hip arthritis, hip replacement is strongly recommended. Recommendations for and against other special conditions include severe kyphosis (strongly against elective spine osteotomy except in specialized centers), acute iritis (strong support for an ophthalmology consultant), recurrent iritis (conditional support for at home use of a topical glucocorticoid under the supervision of an eye care provider, and use of infliximab or adalimumab over etanercept), and IBD (strong recommendation for TNFi monoclonals over etanercept and conditional endorsement of no preferred NSAID).
Active nr-axSpA
Recommendations for the treatment of nr-axSpA are essentially identical to those for treating active AS, Dr. Ward noted, except that in contrast to active AS, where the recommendation is strongly in favor of TNF inhibitors, the committee gave only a conditional recommendation for the use of a TNF inhibitor in this clinical situation.
Stable nr-axSpA
For patients with stable nr-axSpA, the recommendations are strongly in favor of NSAID use, with a conditional suggestion to use on demand. The recommendations also are conditionally against combination therapy with either an NSAID or slow-acting agent plus a TNF inhibitor, with a conditional approval for TNF inhibitor monotherapy instead. The committee strongly supported physical therapy for these patients and gave a lukewarm embrace of monitoring for disease activity, CRP, or ESR.
Dr. Ward noted that the guidelines are designed to help clinicians with treatment decisions for the typical patient with AS or nr-axSpA, and do not address the needs of all populations or all clinical circumstances or contingencies.
He also noted that for many of the questions the committee members tried to address, high-quality evidence was limited.
Dr. Ward did not mention a projected publication date for the guidelines. He had no relevant financial conflicts to disclose.
BOSTON – A nonsteroidal anti-inflammatory drug and exercise may be enough to control active axial spondyloarthritis in some patients, suggest authors of draft guidelines on the management of patients with the condition.
The guidelines, not ready for prime time, have yet to be reviewed or endorsed by the American College of Rheumatology (ACR) and the Spondylitis Association of America, or the SpondyloArthritis Research and Treatment Network (SPARTAN), and are subject to change, emphasized Dr. Michael M. Ward, senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
With that caveat in mind, Dr. Ward presented a sneak peek at the guidelines to a standing-room only crowd at the ACR annual meeting in Boston.
Some definitions
The guidelines offer recommendations on the management of patients with active and stable ankylosing spondylitis (AS) and axial spondyloarthropathies (axSpA) that are symptomatic but without radiographic evidence (nonradiographic, or nr-axSpA).
Active AS is defined as disease that causes symptoms at an unacceptably burdensome level as reported by the patient that are judged by the examining clinician to be caused by AS. The same definition also applies to nr-axSpA.
Stable disease is defined as either an asymptomatic state or symptoms that were previously bothersome but are currently at an acceptable level as reported by the patient. The patient had to have had bothersome symptoms for at least 6 months before entering the stable disease state. This definition is also applicable to stable nr-axSpA.
The investigators considered the best available evidence on the use of NSAIDs (running the gamut from aspirin to tolmetin), slow-acting antirheumatic agents such as methotrexate, glucocorticoids (prednisone and others), tumor necrosis factor (TNF) inhibitors, such as adalimumab, etanercept, and others), and non-TNF biologic agents (abatacept, rituximab, tocilizumab, and others).
Active AS
Dr. Ward presented a management flow tree for patients with active AS, starting with a strong recommendation for an NSAID, conditionally recommended to be used continuously. The authors felt, however, that there was not enough evidence to support the use of one NSAID over another. They also strongly recommended physical therapy, with less robust recommendations for active than for passive exercise and for exercises performed in water rather than on land. The latter recommendation is based on the fact that, although water-based exercises have been shown to be as good as or better than dry land exercises for relieving symptoms, water-based exercise may be impractical for many patients, Dr. Ward noted.
For patients whose disease remains active despite NSAIDs and exercise, the committee strongly recommends use of a tumor necrosis factor inhibitor (TNFi) (no specific agent preferred). If a patient on a TNFi has recurrent iritis, the guidelines have a conditional recommendation for the use of infliximab or adalimumab. For patients with inflammatory bowel disease (IBD), the authors conditionally recommend a TNFi monoclonal antibody as opposed to etanercept.
If the disease remains active on a TNFi, an alternative TNFi can be considered.
“For patients who have contraindications to TNF inhibitors, we considered the choice between adding a slow-acting drug such as sulfasalazine or pamidronate or treating with a non-TNF biologic. Of course, there are no head-to-head trials between those two options, so based on the indirect evidence that’s available, the committee voted for a conditional recommendation against the use of a non-TNF biologic in favor of a slow-acting drug in that setting,” Dr. Ward said.
If there are no contraindications to a TNF inhibitor, however, the committee strongly favored the use of a TNF inhibitor over a slow-acting agent, he emphasized.
For patients who have isolated sacroiliitis, peripheral arthritis, or enthesis, the committee provisionally recommends local injection of a glucocorticoid, with cautions to use infrequently and only if two or fewer joints are involved in peripheral arthritis, and avoidance of injection of the Achilles, patellar, or quadriceps tendons in patients with enthesitis.
For all patients, the guidelines half-heartedly recommend monitoring validated axSpA disease activity measures and C-reactive protein and erythrocyte sedimentation rate (ESR). The group also conditionally supported unsupervised back exercises, formal group or individual self-management education, and fall evaluation and counseling.
Committee members strongly felt that systemic glucocorticoids should not be used in patients with active axSpA, except in cases where a short-term course with quick taper may be helpful, such as in patients with peripheral flare, or during pregnancy or a concomitant IBD flare.
Stable AS
“For patients with stable ankylosing spondylitis who are on combination therapy, either combination therapy with NSAIDs and a TNF inhibitor, or a slow-acting drug and a TNF inhibitor, the committee voted against continuation of a combination in favor of TNF monotherapy. It’s a conditional recommendation, so there certainly would be situations where one would not want to do that, but in general the committee thought that was the preferable approach, balancing the benefits and potential risks of combination therapy against monotherapy in patients with stable AS,” Dr. Ward said.
The committee members strongly supported physical therapy in patients with stable AS and gave a conditional nod to monitoring, back exercises, group support, and fall counseling.
For patients with stable AS and advanced hip arthritis, hip replacement is strongly recommended. Recommendations for and against other special conditions include severe kyphosis (strongly against elective spine osteotomy except in specialized centers), acute iritis (strong support for an ophthalmology consultant), recurrent iritis (conditional support for at home use of a topical glucocorticoid under the supervision of an eye care provider, and use of infliximab or adalimumab over etanercept), and IBD (strong recommendation for TNFi monoclonals over etanercept and conditional endorsement of no preferred NSAID).
Active nr-axSpA
Recommendations for the treatment of nr-axSpA are essentially identical to those for treating active AS, Dr. Ward noted, except that in contrast to active AS, where the recommendation is strongly in favor of TNF inhibitors, the committee gave only a conditional recommendation for the use of a TNF inhibitor in this clinical situation.
Stable nr-axSpA
For patients with stable nr-axSpA, the recommendations are strongly in favor of NSAID use, with a conditional suggestion to use on demand. The recommendations also are conditionally against combination therapy with either an NSAID or slow-acting agent plus a TNF inhibitor, with a conditional approval for TNF inhibitor monotherapy instead. The committee strongly supported physical therapy for these patients and gave a lukewarm embrace of monitoring for disease activity, CRP, or ESR.
Dr. Ward noted that the guidelines are designed to help clinicians with treatment decisions for the typical patient with AS or nr-axSpA, and do not address the needs of all populations or all clinical circumstances or contingencies.
He also noted that for many of the questions the committee members tried to address, high-quality evidence was limited.
Dr. Ward did not mention a projected publication date for the guidelines. He had no relevant financial conflicts to disclose.
BOSTON – A nonsteroidal anti-inflammatory drug and exercise may be enough to control active axial spondyloarthritis in some patients, suggest authors of draft guidelines on the management of patients with the condition.
The guidelines, not ready for prime time, have yet to be reviewed or endorsed by the American College of Rheumatology (ACR) and the Spondylitis Association of America, or the SpondyloArthritis Research and Treatment Network (SPARTAN), and are subject to change, emphasized Dr. Michael M. Ward, senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
With that caveat in mind, Dr. Ward presented a sneak peek at the guidelines to a standing-room only crowd at the ACR annual meeting in Boston.
Some definitions
The guidelines offer recommendations on the management of patients with active and stable ankylosing spondylitis (AS) and axial spondyloarthropathies (axSpA) that are symptomatic but without radiographic evidence (nonradiographic, or nr-axSpA).
Active AS is defined as disease that causes symptoms at an unacceptably burdensome level as reported by the patient that are judged by the examining clinician to be caused by AS. The same definition also applies to nr-axSpA.
Stable disease is defined as either an asymptomatic state or symptoms that were previously bothersome but are currently at an acceptable level as reported by the patient. The patient had to have had bothersome symptoms for at least 6 months before entering the stable disease state. This definition is also applicable to stable nr-axSpA.
The investigators considered the best available evidence on the use of NSAIDs (running the gamut from aspirin to tolmetin), slow-acting antirheumatic agents such as methotrexate, glucocorticoids (prednisone and others), tumor necrosis factor (TNF) inhibitors, such as adalimumab, etanercept, and others), and non-TNF biologic agents (abatacept, rituximab, tocilizumab, and others).
Active AS
Dr. Ward presented a management flow tree for patients with active AS, starting with a strong recommendation for an NSAID, conditionally recommended to be used continuously. The authors felt, however, that there was not enough evidence to support the use of one NSAID over another. They also strongly recommended physical therapy, with less robust recommendations for active than for passive exercise and for exercises performed in water rather than on land. The latter recommendation is based on the fact that, although water-based exercises have been shown to be as good as or better than dry land exercises for relieving symptoms, water-based exercise may be impractical for many patients, Dr. Ward noted.
For patients whose disease remains active despite NSAIDs and exercise, the committee strongly recommends use of a tumor necrosis factor inhibitor (TNFi) (no specific agent preferred). If a patient on a TNFi has recurrent iritis, the guidelines have a conditional recommendation for the use of infliximab or adalimumab. For patients with inflammatory bowel disease (IBD), the authors conditionally recommend a TNFi monoclonal antibody as opposed to etanercept.
If the disease remains active on a TNFi, an alternative TNFi can be considered.
“For patients who have contraindications to TNF inhibitors, we considered the choice between adding a slow-acting drug such as sulfasalazine or pamidronate or treating with a non-TNF biologic. Of course, there are no head-to-head trials between those two options, so based on the indirect evidence that’s available, the committee voted for a conditional recommendation against the use of a non-TNF biologic in favor of a slow-acting drug in that setting,” Dr. Ward said.
If there are no contraindications to a TNF inhibitor, however, the committee strongly favored the use of a TNF inhibitor over a slow-acting agent, he emphasized.
For patients who have isolated sacroiliitis, peripheral arthritis, or enthesis, the committee provisionally recommends local injection of a glucocorticoid, with cautions to use infrequently and only if two or fewer joints are involved in peripheral arthritis, and avoidance of injection of the Achilles, patellar, or quadriceps tendons in patients with enthesitis.
For all patients, the guidelines half-heartedly recommend monitoring validated axSpA disease activity measures and C-reactive protein and erythrocyte sedimentation rate (ESR). The group also conditionally supported unsupervised back exercises, formal group or individual self-management education, and fall evaluation and counseling.
Committee members strongly felt that systemic glucocorticoids should not be used in patients with active axSpA, except in cases where a short-term course with quick taper may be helpful, such as in patients with peripheral flare, or during pregnancy or a concomitant IBD flare.
Stable AS
“For patients with stable ankylosing spondylitis who are on combination therapy, either combination therapy with NSAIDs and a TNF inhibitor, or a slow-acting drug and a TNF inhibitor, the committee voted against continuation of a combination in favor of TNF monotherapy. It’s a conditional recommendation, so there certainly would be situations where one would not want to do that, but in general the committee thought that was the preferable approach, balancing the benefits and potential risks of combination therapy against monotherapy in patients with stable AS,” Dr. Ward said.
The committee members strongly supported physical therapy in patients with stable AS and gave a conditional nod to monitoring, back exercises, group support, and fall counseling.
For patients with stable AS and advanced hip arthritis, hip replacement is strongly recommended. Recommendations for and against other special conditions include severe kyphosis (strongly against elective spine osteotomy except in specialized centers), acute iritis (strong support for an ophthalmology consultant), recurrent iritis (conditional support for at home use of a topical glucocorticoid under the supervision of an eye care provider, and use of infliximab or adalimumab over etanercept), and IBD (strong recommendation for TNFi monoclonals over etanercept and conditional endorsement of no preferred NSAID).
Active nr-axSpA
Recommendations for the treatment of nr-axSpA are essentially identical to those for treating active AS, Dr. Ward noted, except that in contrast to active AS, where the recommendation is strongly in favor of TNF inhibitors, the committee gave only a conditional recommendation for the use of a TNF inhibitor in this clinical situation.
Stable nr-axSpA
For patients with stable nr-axSpA, the recommendations are strongly in favor of NSAID use, with a conditional suggestion to use on demand. The recommendations also are conditionally against combination therapy with either an NSAID or slow-acting agent plus a TNF inhibitor, with a conditional approval for TNF inhibitor monotherapy instead. The committee strongly supported physical therapy for these patients and gave a lukewarm embrace of monitoring for disease activity, CRP, or ESR.
Dr. Ward noted that the guidelines are designed to help clinicians with treatment decisions for the typical patient with AS or nr-axSpA, and do not address the needs of all populations or all clinical circumstances or contingencies.
He also noted that for many of the questions the committee members tried to address, high-quality evidence was limited.
Dr. Ward did not mention a projected publication date for the guidelines. He had no relevant financial conflicts to disclose.
VIDEO: Hepatitis C Screening Rises, But Where Are the Positive Cases?
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM THE LIVER MEETING 2014
VIDEO: Hepatitis C screening rises, but where are the positive cases?
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The number of hepatitis C virus antibody tests increased by 15.4% after the 2012 Centers for Disease Control and Prevention task force recommendation calling for one-time HCV testing in baby boomers, according to preliminary results from an analysis of 4.5 million tests.
Surprisingly, that increase in testing did not lead to an increase in the number of positive tests, which actually declined by 4.1%, R. Monina Klevens, D.D.S., MPH, reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is a huge question that we need to look at for implementation,” said Dr. Klevens, a medical epidemiologist with the CDC.
For a deep dive into the data and to hear what’s next, click here to see an interview with Dr Klevens.
Dr. Klevens reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM THE LIVER MEETING 2014
Direct-acting Antivirals Treat Recurrent HCV After Transplant
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Next page: Adverse events >>
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Next page: Adverse events >>
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Next page: Adverse events >>
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
AT THE LIVER MEETING 2014
Direct-acting antivirals treat recurrent HCV after transplant
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
On Twitter @sherryboschert
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
On Twitter @sherryboschert
BOSTON – Treating recurrent hepatitis C infection after liver transplantation using sofosbuvir-containing regimens produced a sustained virologic response 4 weeks later in 60%-90% of 237 patients, depending on genotype and the presence of cirrhosis.
Investigators analyzed data on 245 posttransplant patients with hepatitis C (HCV) collected from 38 academic medical centers and 15 community medical centers in North America and Europe participating in the prospective, longitudinal, observational HCV-Target study. Of the 227 patients who started treatment, 69% completed treatment, 3% discontinued treatment prematurely, and 28% are undergoing treatment.
Among the 68 patients with HCV genotype 1 and a known virologic outcome who were treated with sofosbuvir and simeprevir with or without ribavirin, 61 (90%) achieved a sustained virologic response for 4 weeks (SVR4).
Response rates in that group varied, however, depending on whether patients had cirrhosis (SVR4 in 32 of 37, 86%) or no cirrhosis (SVR4 in 29 of 31, 94%). Results also varied in that group by genotype, with SVR4 in 30 of 36 patients with genotype 1a infection (83%) and SVR4 in 18 of 19 patients with genotype 1b (95%), Dr. Robert S. Brown Jr. and his associates reported at the annual meeting of the American Association for the Study of Liver Diseases.
“This is the regimen that probably holds the highest interest,” Dr. Brown said, because most of the patients in the study were genotype 1, and most genotype 1 patients received sofosbuvir and simeprevir with or without ribavirin.
A total of 10 of 12 patients with HCV genotype 1 infection who were treated with sofosbuvir plus pegylated interferon and ribavirin achieved SVR4 (83%).
A total of 9 of 10 patients with HCV genotype 2 infection who had complete data and who received sofosbuvir plus ribavirin achieved SVR4 (90%), reported Dr. Brown, the Frank Cardile Professor of Medicine and Pediatrics (in Surgery) at Columbia University, New York, and director of the Center for Liver Disease and Transplantation at New York-Presbyterian Hospital/Columbia University Medical Center.
Three of five patients with genotype 3 infection and complete data who received sofosbuvir plus ribavirin achieved SVR4 (60%), and one patient with genotype 3 achieved SVR4 after treatment with sofosbuvir, pegylated interferon, and ribavirin.
Adverse events were reported by 82% of patients, with rates ranging from 77% to 92% in different treatment groups. “The majority of these were mild and manageable,” Dr. Brown noted. The overall rate of serious adverse events was 8%, ranging from 0% to 21% in different treatment groups, though some of those cases were unlikely to be related to treatment, he added.
In general, interferon-free regimens had low rates of serious adverse events, Dr. Brown said. No patients developed acute liver graft rejection.
“Hepatitis C following liver transplant does remain a problem in 2014, because reinfection is universal and therapeutic options, at least to date, have been limited,” he said. The study’s real-world data supplement encouraging results from small, controlled trials of newer anti-HCV agents in posttransplant patients.
Most of the patients in the study were treated for recurrent HCV “well after” transplantation, Dr. Brown said. “The optimal treatment regimen and the duration of therapy still remain to be determined.”
Treatment regimens in the HCV-Target study are selected by physicians according to the local standard of care.
The study was too small to do a multivariate analysis of predictive factors for SVR4, Dr. Brown commented.
The HCV-Target study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.
On Twitter @sherryboschert
AT THE LIVER MEETING 2014
Key clinical point: Direct-acting antivirals can help most patients with recurrent HCV after liver transplantation.
Major finding: A sustained virologic response after 4 weeks was seen in 60%-90% of patients, depending on genotype and cirrhosis.
Data source: An analysis of a multicenter database on 227 patients treated with sofosbuvir-containing regimens since December 2013 for recurrent HCV after liver transplantation.
Disclosures: The study was funded by AbbVie, Bristol Myers Squibb, Genentech, Gilead, GlaxoSmithKline, Kadmon, Janssen, Merck, and Vertex. Dr. Brown reported financial associations with AbbVie, Genentech, Gilead, Janssen, Merck, Salix, Vertex, and Vital Therapies.