User login
University of California, San Francisco (UCSF): Antepartum and Intrapartum Management Meeting
Get umbilical artery systolic-to-diastolic ratio in intrauterine growth restriction
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
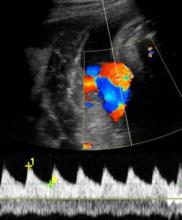
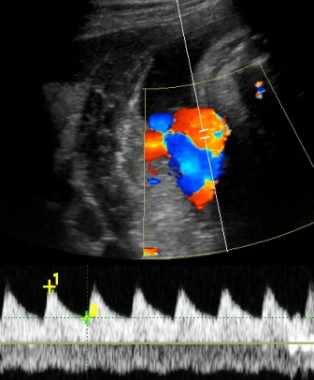
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Identify monochorionic twins to guide pregnancy management
SAN FRANCISCO – The physician is responsible for knowing the chorionicity of a pregnant patient’s twins, so if you don’t offer diagnostic ultrasound or can’t make the diagnosis yourself, refer the patient to someone who can.
Knowing the chorionicity is essential because "it literally will define how you manage the pregnancy," Dr. Larry Rand said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"This is a critical, critical concept," said Dr. Rand, director of perinatal services for the Fetal Treatment Program at the university. The chorionicity "should be the very first question that you ask yourself when you have a patient with twins."
You don’t need to be an expert on monochorionic twins; you just need to know if the patient is at high risk because of monochorionicity. Determining the chorionicity of twins before 14 weeks’ gestation is considered the standard of care, he stressed, and a physician who doesn’t know that twins are monochorionic could be liable if something goes wrong.
If the chorionicity is undetermined on your office ultrasound, refer the patient and request a chorionicity determination, he advised.
"This is one of the times that I have to say that ultrasound makes all the difference," Dr. Rand said. "The single most important ultrasound finding in the entire pregnancy is going to be the chorionicity."
A patient deserves to know whether her twins are monochorionic because she needs to be counseled appropriately about the risks. "It’s not the radiologist’s responsibility," he said. "The obstetrician is responsible for knowing the effect of chorionicity." Make sure to document that you have either determined the chorionicity yourself or have asked for an exam to assess chorionicity.
The rate of congenital anomalies in monochorionic twins, for example, is similar to the rate seen in diabetic mothers. This "changes the kind of tests you order and the things you see" compared with dichorionic twins, he said. Level II ultrasound examinations of anatomy that would be done in high-risk cases such as diabetic pregnancies, for example, should be done for monochorionic twins, whose elevated risk for anomalies may be due to an imperfect splitting of the single egg from which they came.
Compared with dichorionic twins, monochorionic twins also have increased risk for neurologic injury, including an eightfold increased incidence of cerebral palsy, and for preterm birth, spontaneous abortion, intrauterine growth restriction and growth discordance, intrauterine fetal demise, and twin-to-twin transfusion syndrome. Specialized centers can treat twin-to-twin transfusion syndrome with laser therapy if patients are diagnosed and referred in a timely manner – which is the reason for more-frequent screening of monochorionic twins. (See management recommendations below.)
Aterio-arterial (AA) anastomosis, a type of vascular connection within the placenta, can be detected on antenatal ultrasound. If present, the risk of twin-to-twin transfusion syndrome decreases 10-fold and the risk of intrauterine fetal demise decreases sevenfold. "It’s very helpful prognostically," he said.
Although AA anastomosis is not a new concept, it’s only recently that obstetrical imaging has evolved to identify it on antenatal ultrasound, which is "so helpful for counseling and management," said Dr. Rand, also the Lynne and Marc Benioff Endowed Chair in Maternal and Fetal Medicine at the university.
The major fear in monochorionic twins is intrauterine fetal demise of one twin, which leaves the surviving twin with a 10%-20% risk of death and a 20%-40% risk of long-term neurologic injury if the second twin survives. The difference even comes into play with genetic counseling. Aneuploidy risk in monochorionic twins is similar to risk in singletons (because they originated from a single egg). For invasive testing, one chorionic villus sampling covers both monochorionic twins (because there’s only one placenta to sample), but amniocentesis typically is performed on each amniotic sac. Some physicians sample just one amniotic sac for amniocentesis, thinking that it should cover both twins because they’re identical, but there are extremely rare cases of subtle differences that would not be detected by single-sac sampling, he said.
The other outcomes differ between monochorionic and dichorionic twins because the splitting of an egg can be imperfect; monochorionic twins share "plumbing" and vascular connections, and they have to share the resources of one placenta, Dr. Rand explained.
Before 14 weeks’ gestation, ultrasound is 99% sensitive and 100% specific for chorionicity, and it’s an easy assessment to do. In the second trimester, it gets trickier, which is why determining chorionicity early is so important, he said.
Dr. Rand gave several recommendations for management of monochorionic twins. In the first trimester, he said, determine the chorionicity, check the nuchal translucency, and assess fetal growth.
In the second trimester, conduct level II (high risk) anatomical surveys and echocardiograms to screen for fetal cardiac disease (as you would in a diabetic mother). Establish a minimum surveillance schedule of at least every 2 weeks for amniotic fluid between 16 and 28 weeks’ gestation, and every 4 weeks for fetal growth between 16 and 32 weeks’ gestation.
In the third trimester, continue the surveillance of amniotic fluid and fetal growth. Consider performing non–stress tests and Doppler ultrasounds. There’s debate about the optimal gestational age for delivery of monochorionic twins, between 36 and 38 weeks. "We’re not sure when to deliver," Dr. Rand said, but he recommends delivering monochorionic twins who’ve had issues with growth, fluid, or other aspects during pregnancy closer to 36 weeks and delivering twins with no issues closer to 38 weeks. "Monochorionicity is not, in and of itself, an indication for cesarean delivery," he added.
Approximately 75% of twins are dizygotic (from two separate eggs, each fertilized by sperm) and thus dichorionic. Among the 25% of twin pregnancies that are monozygotic (from one egg), the egg splits more slowly in 75% of cases, creating monochorionic twins that share a placenta and circulation. In the other 25% of monozygotic twins, the egg splits quickly, within 3 days, yielding two separate units and creating dichorionic twins, each with their own placenta.
Dr. Rand reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The physician is responsible for knowing the chorionicity of a pregnant patient’s twins, so if you don’t offer diagnostic ultrasound or can’t make the diagnosis yourself, refer the patient to someone who can.
Knowing the chorionicity is essential because "it literally will define how you manage the pregnancy," Dr. Larry Rand said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"This is a critical, critical concept," said Dr. Rand, director of perinatal services for the Fetal Treatment Program at the university. The chorionicity "should be the very first question that you ask yourself when you have a patient with twins."
You don’t need to be an expert on monochorionic twins; you just need to know if the patient is at high risk because of monochorionicity. Determining the chorionicity of twins before 14 weeks’ gestation is considered the standard of care, he stressed, and a physician who doesn’t know that twins are monochorionic could be liable if something goes wrong.
If the chorionicity is undetermined on your office ultrasound, refer the patient and request a chorionicity determination, he advised.
"This is one of the times that I have to say that ultrasound makes all the difference," Dr. Rand said. "The single most important ultrasound finding in the entire pregnancy is going to be the chorionicity."
A patient deserves to know whether her twins are monochorionic because she needs to be counseled appropriately about the risks. "It’s not the radiologist’s responsibility," he said. "The obstetrician is responsible for knowing the effect of chorionicity." Make sure to document that you have either determined the chorionicity yourself or have asked for an exam to assess chorionicity.
The rate of congenital anomalies in monochorionic twins, for example, is similar to the rate seen in diabetic mothers. This "changes the kind of tests you order and the things you see" compared with dichorionic twins, he said. Level II ultrasound examinations of anatomy that would be done in high-risk cases such as diabetic pregnancies, for example, should be done for monochorionic twins, whose elevated risk for anomalies may be due to an imperfect splitting of the single egg from which they came.
Compared with dichorionic twins, monochorionic twins also have increased risk for neurologic injury, including an eightfold increased incidence of cerebral palsy, and for preterm birth, spontaneous abortion, intrauterine growth restriction and growth discordance, intrauterine fetal demise, and twin-to-twin transfusion syndrome. Specialized centers can treat twin-to-twin transfusion syndrome with laser therapy if patients are diagnosed and referred in a timely manner – which is the reason for more-frequent screening of monochorionic twins. (See management recommendations below.)
Aterio-arterial (AA) anastomosis, a type of vascular connection within the placenta, can be detected on antenatal ultrasound. If present, the risk of twin-to-twin transfusion syndrome decreases 10-fold and the risk of intrauterine fetal demise decreases sevenfold. "It’s very helpful prognostically," he said.
Although AA anastomosis is not a new concept, it’s only recently that obstetrical imaging has evolved to identify it on antenatal ultrasound, which is "so helpful for counseling and management," said Dr. Rand, also the Lynne and Marc Benioff Endowed Chair in Maternal and Fetal Medicine at the university.
The major fear in monochorionic twins is intrauterine fetal demise of one twin, which leaves the surviving twin with a 10%-20% risk of death and a 20%-40% risk of long-term neurologic injury if the second twin survives. The difference even comes into play with genetic counseling. Aneuploidy risk in monochorionic twins is similar to risk in singletons (because they originated from a single egg). For invasive testing, one chorionic villus sampling covers both monochorionic twins (because there’s only one placenta to sample), but amniocentesis typically is performed on each amniotic sac. Some physicians sample just one amniotic sac for amniocentesis, thinking that it should cover both twins because they’re identical, but there are extremely rare cases of subtle differences that would not be detected by single-sac sampling, he said.
The other outcomes differ between monochorionic and dichorionic twins because the splitting of an egg can be imperfect; monochorionic twins share "plumbing" and vascular connections, and they have to share the resources of one placenta, Dr. Rand explained.
Before 14 weeks’ gestation, ultrasound is 99% sensitive and 100% specific for chorionicity, and it’s an easy assessment to do. In the second trimester, it gets trickier, which is why determining chorionicity early is so important, he said.
Dr. Rand gave several recommendations for management of monochorionic twins. In the first trimester, he said, determine the chorionicity, check the nuchal translucency, and assess fetal growth.
In the second trimester, conduct level II (high risk) anatomical surveys and echocardiograms to screen for fetal cardiac disease (as you would in a diabetic mother). Establish a minimum surveillance schedule of at least every 2 weeks for amniotic fluid between 16 and 28 weeks’ gestation, and every 4 weeks for fetal growth between 16 and 32 weeks’ gestation.
In the third trimester, continue the surveillance of amniotic fluid and fetal growth. Consider performing non–stress tests and Doppler ultrasounds. There’s debate about the optimal gestational age for delivery of monochorionic twins, between 36 and 38 weeks. "We’re not sure when to deliver," Dr. Rand said, but he recommends delivering monochorionic twins who’ve had issues with growth, fluid, or other aspects during pregnancy closer to 36 weeks and delivering twins with no issues closer to 38 weeks. "Monochorionicity is not, in and of itself, an indication for cesarean delivery," he added.
Approximately 75% of twins are dizygotic (from two separate eggs, each fertilized by sperm) and thus dichorionic. Among the 25% of twin pregnancies that are monozygotic (from one egg), the egg splits more slowly in 75% of cases, creating monochorionic twins that share a placenta and circulation. In the other 25% of monozygotic twins, the egg splits quickly, within 3 days, yielding two separate units and creating dichorionic twins, each with their own placenta.
Dr. Rand reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The physician is responsible for knowing the chorionicity of a pregnant patient’s twins, so if you don’t offer diagnostic ultrasound or can’t make the diagnosis yourself, refer the patient to someone who can.
Knowing the chorionicity is essential because "it literally will define how you manage the pregnancy," Dr. Larry Rand said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"This is a critical, critical concept," said Dr. Rand, director of perinatal services for the Fetal Treatment Program at the university. The chorionicity "should be the very first question that you ask yourself when you have a patient with twins."
You don’t need to be an expert on monochorionic twins; you just need to know if the patient is at high risk because of monochorionicity. Determining the chorionicity of twins before 14 weeks’ gestation is considered the standard of care, he stressed, and a physician who doesn’t know that twins are monochorionic could be liable if something goes wrong.
If the chorionicity is undetermined on your office ultrasound, refer the patient and request a chorionicity determination, he advised.
"This is one of the times that I have to say that ultrasound makes all the difference," Dr. Rand said. "The single most important ultrasound finding in the entire pregnancy is going to be the chorionicity."
A patient deserves to know whether her twins are monochorionic because she needs to be counseled appropriately about the risks. "It’s not the radiologist’s responsibility," he said. "The obstetrician is responsible for knowing the effect of chorionicity." Make sure to document that you have either determined the chorionicity yourself or have asked for an exam to assess chorionicity.
The rate of congenital anomalies in monochorionic twins, for example, is similar to the rate seen in diabetic mothers. This "changes the kind of tests you order and the things you see" compared with dichorionic twins, he said. Level II ultrasound examinations of anatomy that would be done in high-risk cases such as diabetic pregnancies, for example, should be done for monochorionic twins, whose elevated risk for anomalies may be due to an imperfect splitting of the single egg from which they came.
Compared with dichorionic twins, monochorionic twins also have increased risk for neurologic injury, including an eightfold increased incidence of cerebral palsy, and for preterm birth, spontaneous abortion, intrauterine growth restriction and growth discordance, intrauterine fetal demise, and twin-to-twin transfusion syndrome. Specialized centers can treat twin-to-twin transfusion syndrome with laser therapy if patients are diagnosed and referred in a timely manner – which is the reason for more-frequent screening of monochorionic twins. (See management recommendations below.)
Aterio-arterial (AA) anastomosis, a type of vascular connection within the placenta, can be detected on antenatal ultrasound. If present, the risk of twin-to-twin transfusion syndrome decreases 10-fold and the risk of intrauterine fetal demise decreases sevenfold. "It’s very helpful prognostically," he said.
Although AA anastomosis is not a new concept, it’s only recently that obstetrical imaging has evolved to identify it on antenatal ultrasound, which is "so helpful for counseling and management," said Dr. Rand, also the Lynne and Marc Benioff Endowed Chair in Maternal and Fetal Medicine at the university.
The major fear in monochorionic twins is intrauterine fetal demise of one twin, which leaves the surviving twin with a 10%-20% risk of death and a 20%-40% risk of long-term neurologic injury if the second twin survives. The difference even comes into play with genetic counseling. Aneuploidy risk in monochorionic twins is similar to risk in singletons (because they originated from a single egg). For invasive testing, one chorionic villus sampling covers both monochorionic twins (because there’s only one placenta to sample), but amniocentesis typically is performed on each amniotic sac. Some physicians sample just one amniotic sac for amniocentesis, thinking that it should cover both twins because they’re identical, but there are extremely rare cases of subtle differences that would not be detected by single-sac sampling, he said.
The other outcomes differ between monochorionic and dichorionic twins because the splitting of an egg can be imperfect; monochorionic twins share "plumbing" and vascular connections, and they have to share the resources of one placenta, Dr. Rand explained.
Before 14 weeks’ gestation, ultrasound is 99% sensitive and 100% specific for chorionicity, and it’s an easy assessment to do. In the second trimester, it gets trickier, which is why determining chorionicity early is so important, he said.
Dr. Rand gave several recommendations for management of monochorionic twins. In the first trimester, he said, determine the chorionicity, check the nuchal translucency, and assess fetal growth.
In the second trimester, conduct level II (high risk) anatomical surveys and echocardiograms to screen for fetal cardiac disease (as you would in a diabetic mother). Establish a minimum surveillance schedule of at least every 2 weeks for amniotic fluid between 16 and 28 weeks’ gestation, and every 4 weeks for fetal growth between 16 and 32 weeks’ gestation.
In the third trimester, continue the surveillance of amniotic fluid and fetal growth. Consider performing non–stress tests and Doppler ultrasounds. There’s debate about the optimal gestational age for delivery of monochorionic twins, between 36 and 38 weeks. "We’re not sure when to deliver," Dr. Rand said, but he recommends delivering monochorionic twins who’ve had issues with growth, fluid, or other aspects during pregnancy closer to 36 weeks and delivering twins with no issues closer to 38 weeks. "Monochorionicity is not, in and of itself, an indication for cesarean delivery," he added.
Approximately 75% of twins are dizygotic (from two separate eggs, each fertilized by sperm) and thus dichorionic. Among the 25% of twin pregnancies that are monozygotic (from one egg), the egg splits more slowly in 75% of cases, creating monochorionic twins that share a placenta and circulation. In the other 25% of monozygotic twins, the egg splits quickly, within 3 days, yielding two separate units and creating dichorionic twins, each with their own placenta.
Dr. Rand reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Noninvasive prenatal testing could be secondary screen
SAN FRANCISCO – Using noninvasive prenatal DNA testing as a secondary screen after conventional prenatal testing could decrease the number of amniocenteses by more than 90%, reduce fetal losses, and improve the ratio of Down syndrome cases detected per amniocentesis, according to Dr. Mary E. Norton.
On the other hand, using noninvasive prenatal testing as the primary screen would increase the rate of detecting trisomy 13, 18, or 21 by a bit, but many women will have unsuccessful test results and will go on to have amniocentesis, negatively affecting the fetal loss rate and the ratio of Down syndrome detected per amniocentesis, she said.
For these and other reasons, it’s premature to abandon current prenatal screening for noninvasive prenatal testing, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
She used available data to compare three hypothetical scenarios in which 2.9 million pregnant women would be screened and 5,110 pregnancies would be affected by trisomy 13, 18, or 21. The women would be screened by conventional prenatal testing alone, by current screening methods followed by noninvasive prenatal testing, or solely by the noninvasive Digital Analysis of Selected Regions (DANSR) assay that can identify chromosome abnormalities by evaluating specific fragments of maternal cell-free DNA.
Approximately 145,000 of the women would have a positive screen under current testing or with current testing plus noninvasive testing as a secondary screen, but only 45,710 would have a positive screen with noninvasive testing as the primary screen, she estimated. The number of trisomy 13, 18, or 21 cases identified would be 4,667 under scenario one or two and slightly higher – 5,100 – using the noninvasive screening test primarily, said Dr. Norton, professor of obstetrics and gynecology at the university. Current screening can detect many more problems than can noninvasive screening, so 2,004 other abnormalities would be detected using current methods, compared with none using noninvasive testing.
A proportion of patients undergoing noninvasive prenatal screening would have no test result because the sequencing failed to work or not enough DNA was present to get a result – 4,350 women undergoing noninvasive testing as a secondary screen and 87,000 women with noninvasive testing as the primary screen, she estimated.
The total number of amniocenteses would be 145,000 under current testing (one for every positive screen), but would be reduced to 11,047 if noninvasive testing was used as a secondary screen to detect aneuploidies. With noninvasive testing as the primary screen, 67,460 women would undergo amniocentesis. That would result in 435 fetal losses with current testing alone, 33 with current testing and secondary noninvasive prenatal testing, or 202 fetal losses with noninvasive testing as the primary screen.
Eighteen amniocenteses would have to be performed to detect one case of Down syndrome with current prenatal testing alone. With noninvasive testing as a secondary screen, every two amniocenteses would detect a case of Down syndrome. With noninvasive testing as the primary screen, 13 amniocenteses would be needed to detect one case of Down syndrome, Dr. Norton said.
The relative benefits of each scenario remain controversial and may vary by each patient’s level of risk. Further study is needed before the standard of care in prenatal screening is changed.
"Prenatal screening is changing at a rapid pace," Dr. Norton said. Even experts are struggling with how best to incorporate all the new information and new tools. "It’s very exciting times, but confusing even for those of us who practice in the field," she commented.
Dr. Norton has received research funding from Ariosa Diagnostics and CellScape, which are involved in prenatal diagnosis products.
On Twitter @sherryboschert
SAN FRANCISCO – Using noninvasive prenatal DNA testing as a secondary screen after conventional prenatal testing could decrease the number of amniocenteses by more than 90%, reduce fetal losses, and improve the ratio of Down syndrome cases detected per amniocentesis, according to Dr. Mary E. Norton.
On the other hand, using noninvasive prenatal testing as the primary screen would increase the rate of detecting trisomy 13, 18, or 21 by a bit, but many women will have unsuccessful test results and will go on to have amniocentesis, negatively affecting the fetal loss rate and the ratio of Down syndrome detected per amniocentesis, she said.
For these and other reasons, it’s premature to abandon current prenatal screening for noninvasive prenatal testing, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
She used available data to compare three hypothetical scenarios in which 2.9 million pregnant women would be screened and 5,110 pregnancies would be affected by trisomy 13, 18, or 21. The women would be screened by conventional prenatal testing alone, by current screening methods followed by noninvasive prenatal testing, or solely by the noninvasive Digital Analysis of Selected Regions (DANSR) assay that can identify chromosome abnormalities by evaluating specific fragments of maternal cell-free DNA.
Approximately 145,000 of the women would have a positive screen under current testing or with current testing plus noninvasive testing as a secondary screen, but only 45,710 would have a positive screen with noninvasive testing as the primary screen, she estimated. The number of trisomy 13, 18, or 21 cases identified would be 4,667 under scenario one or two and slightly higher – 5,100 – using the noninvasive screening test primarily, said Dr. Norton, professor of obstetrics and gynecology at the university. Current screening can detect many more problems than can noninvasive screening, so 2,004 other abnormalities would be detected using current methods, compared with none using noninvasive testing.
A proportion of patients undergoing noninvasive prenatal screening would have no test result because the sequencing failed to work or not enough DNA was present to get a result – 4,350 women undergoing noninvasive testing as a secondary screen and 87,000 women with noninvasive testing as the primary screen, she estimated.
The total number of amniocenteses would be 145,000 under current testing (one for every positive screen), but would be reduced to 11,047 if noninvasive testing was used as a secondary screen to detect aneuploidies. With noninvasive testing as the primary screen, 67,460 women would undergo amniocentesis. That would result in 435 fetal losses with current testing alone, 33 with current testing and secondary noninvasive prenatal testing, or 202 fetal losses with noninvasive testing as the primary screen.
Eighteen amniocenteses would have to be performed to detect one case of Down syndrome with current prenatal testing alone. With noninvasive testing as a secondary screen, every two amniocenteses would detect a case of Down syndrome. With noninvasive testing as the primary screen, 13 amniocenteses would be needed to detect one case of Down syndrome, Dr. Norton said.
The relative benefits of each scenario remain controversial and may vary by each patient’s level of risk. Further study is needed before the standard of care in prenatal screening is changed.
"Prenatal screening is changing at a rapid pace," Dr. Norton said. Even experts are struggling with how best to incorporate all the new information and new tools. "It’s very exciting times, but confusing even for those of us who practice in the field," she commented.
Dr. Norton has received research funding from Ariosa Diagnostics and CellScape, which are involved in prenatal diagnosis products.
On Twitter @sherryboschert
SAN FRANCISCO – Using noninvasive prenatal DNA testing as a secondary screen after conventional prenatal testing could decrease the number of amniocenteses by more than 90%, reduce fetal losses, and improve the ratio of Down syndrome cases detected per amniocentesis, according to Dr. Mary E. Norton.
On the other hand, using noninvasive prenatal testing as the primary screen would increase the rate of detecting trisomy 13, 18, or 21 by a bit, but many women will have unsuccessful test results and will go on to have amniocentesis, negatively affecting the fetal loss rate and the ratio of Down syndrome detected per amniocentesis, she said.
For these and other reasons, it’s premature to abandon current prenatal screening for noninvasive prenatal testing, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
She used available data to compare three hypothetical scenarios in which 2.9 million pregnant women would be screened and 5,110 pregnancies would be affected by trisomy 13, 18, or 21. The women would be screened by conventional prenatal testing alone, by current screening methods followed by noninvasive prenatal testing, or solely by the noninvasive Digital Analysis of Selected Regions (DANSR) assay that can identify chromosome abnormalities by evaluating specific fragments of maternal cell-free DNA.
Approximately 145,000 of the women would have a positive screen under current testing or with current testing plus noninvasive testing as a secondary screen, but only 45,710 would have a positive screen with noninvasive testing as the primary screen, she estimated. The number of trisomy 13, 18, or 21 cases identified would be 4,667 under scenario one or two and slightly higher – 5,100 – using the noninvasive screening test primarily, said Dr. Norton, professor of obstetrics and gynecology at the university. Current screening can detect many more problems than can noninvasive screening, so 2,004 other abnormalities would be detected using current methods, compared with none using noninvasive testing.
A proportion of patients undergoing noninvasive prenatal screening would have no test result because the sequencing failed to work or not enough DNA was present to get a result – 4,350 women undergoing noninvasive testing as a secondary screen and 87,000 women with noninvasive testing as the primary screen, she estimated.
The total number of amniocenteses would be 145,000 under current testing (one for every positive screen), but would be reduced to 11,047 if noninvasive testing was used as a secondary screen to detect aneuploidies. With noninvasive testing as the primary screen, 67,460 women would undergo amniocentesis. That would result in 435 fetal losses with current testing alone, 33 with current testing and secondary noninvasive prenatal testing, or 202 fetal losses with noninvasive testing as the primary screen.
Eighteen amniocenteses would have to be performed to detect one case of Down syndrome with current prenatal testing alone. With noninvasive testing as a secondary screen, every two amniocenteses would detect a case of Down syndrome. With noninvasive testing as the primary screen, 13 amniocenteses would be needed to detect one case of Down syndrome, Dr. Norton said.
The relative benefits of each scenario remain controversial and may vary by each patient’s level of risk. Further study is needed before the standard of care in prenatal screening is changed.
"Prenatal screening is changing at a rapid pace," Dr. Norton said. Even experts are struggling with how best to incorporate all the new information and new tools. "It’s very exciting times, but confusing even for those of us who practice in the field," she commented.
Dr. Norton has received research funding from Ariosa Diagnostics and CellScape, which are involved in prenatal diagnosis products.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Tracking quality measures improved perinatal care
SAN FRANCISCO – One California community-based hospital got a head start on tracking core measures of quality in perinatal care that all U.S. hospitals will have to report to The Joint Commission beginning January 2014.
Over the past 2 years, the ob.gyns. found it wasn’t easy, but that tracking core measures of quality significantly improved perinatal care.
Sutter Medical Center in Sacramento, Calif., formed a perinatal data committee in 2010 to identify barriers and develop processes for tracking six quality measures, including the five for The Joint Commission. They worked to overcome doubters on their staff, internally published individual doctors’ rates of cesarean section deliveries and episiotomies, and shared the results for each prenatal obstetrics group.
Their overall rate of elective deliveries at less than 39 weeks’ gestation decreased from 25% of the 4,958 deliveries in October 2010 to 2% of the 5,577 deliveries in December 2012. The cesarean section rate for nulliparous women with a term, singleton fetus in a vertex position dropped from 31% in 2010 to 25% in 2012, Dr. William M. Gilbert reported at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
They also improved significantly in two other core measures of quality mandated by The Joint Commission: The proportion of preterm infants who received antenatal steroids before delivery jumped from 80% to 100%, and the proportion of newborns who were fed exclusively breast milk during their entire hospitalization improved from 58% to 70%. The hospital has begun collecting data on a fifth core measure for The Joint Commission: the rate of health care-associated bloodstream infections in newborns.
Dr. Gilbert and his group also tracked two measures that are endorsed by the National Quality Forum but are not yet required by The Joint Commission. Their episiotomy rate decreased significantly from 5% to 2%, and the proportion of women undergoing cesarean section who received appropriate prophylaxis against deep vein thrombosis increased from 95% to 98% (Jt. Comm. J. Qual. Patient Saf. 2013;39:258-66).
"It took us 1-2 years to get the bugs worked out" in tracking core quality measures, said Dr. Gilbert, regional medical director of women’s services for Sutter Health’s Sacramento-Sierra Region, Sacramento, Calif. The effort required leadership from doctors and nurses, administrative and medical records support, and education for coders.
"If your hospital has done nothing to look at what you’re going to be submitting" to The Joint Commission, he added, "I can guarantee you that even if you think you’re doing great, the data are going to be awful, and you’re going to be scrambling to fix a problem that has occurred."
This kind of attention to quality measures in perinatal care is long overdue, he said. Despite the fact that the 4.2 million normal vaginal deliveries per year represent the No. 1 hospital discharge diagnosis in the United States, and studies show immense variation in perinatal practices between hospitals and geographical regions, efforts to measure the quality of hospital care largely have ignored obstetrics because those efforts have focused on Medicare, and few obstetrical patients are covered by Medicare.
Previous studies show a 10-fold variation in cesarean section rates around the country, and cesarean section rates in low-risk patients vary from 2% to 36%. "I would put to you, if you were making widgets or tanks, and you had such variation in the quality of your tanks that the government was paying for, you’d be out of work and probably in jail, but that’s what we tolerate" in health care, he said. Huge variations also have been reported in rates of induction, episiotomy, breastfeeding, and use of antenatal steroids.
The 40 ob.gyns. affiliated with Dr. Gilbert’s hospital had cesarean rates for nulliparous, term, singleton, vertex pregnancies ranging from approximately 8% to 60% when the tracking efforts began, he said. The committee assigned two-digit alphanumeric codes for each provider and posted individual rates of cesarean sections and episiotomies by provider code for 6 months, to start. It took a year of convincing before getting agreement, but then individual rates were posted in the doctors’ and labor and delivery lounges and were e-mailed to all medical staff.
"It’s amazing – amazing what that did," he said. Doctors with the highest cesarean section rates reduced their use of cesarean sections.
The category of elective deliveries at less than 39 weeks’ gestation excluded cases with medical indications for early delivery, but tracking ran into problems initially because ICD-9 codes did not exist for some exemptions, including prior classical cesarean section or prior myomectomy. "You got dinged for that" in the tracking despite the medical indication, he said. So the committee created tracking categories of "avoidable" and "unavoidable" early deliveries, and doctors didn’t get dinged for unavoidable cases.
Some doctors wrote the reason for early delivery as "intrahepatic cholestasis of pregnancy," which is an appropriate indication, but the medical coders told Dr. Gilbert that having the word "intrahepatic" flagged it as gall bladder disease, which is no reason to deliver early. "We had to work with our coders to help us understand," he said.
Every patient at risk of preterm delivery received antenatal steroids at his hospital, Dr. Gilbert said, "but we weren’t documenting it properly." There had been no uniform spot in the medical record to document administration of antenatal steroids, or to show that they had been given before the current hospitalization. Dr. Gilbert’s team worked with the medical records department to change the electronic health records. Nurses now check off if the patient received a full course of antenatal steroids. If this is missing, the doctor gets a pop-up window where a reason must be given.
"That really was effective," he said.
Tracking of episiotomy excluded cases of shoulder dystocia, but not episiotomy for fetal distress. Despite individual rates being internally publicized, the episiotomy rate seems to be stuck at around 2% because "I do have a couple of old-timers," he said. "Even public embarrassment will not get them to change."
"As an individual and as a hospital, we need to make sure we’re doing the best we can."
Capturing data on whether or not newborns are fed exclusively with breast milk can be difficult, in part because it’s often not clear whether the ob.gyn., the nursing staff, or the pediatrician is responsible for this. Dr. Gilbert’s team analyzed 18 cases at his hospital in which women came in saying they wanted to breastfeed the newborn exclusively, but that didn’t happen. In most cases, the babies received formula after a night nurse moved the baby to the nursery so the mother could sleep, a problem that was addressed. Publicizing exclusive breastfeeding rates for 20 different perinatal obstetrics groups – which ranged from 33% to 93% also helped improve breastfeeding rates.
The perinatal data committee also posted a color-coded "dashboard" showing trends in the hospital’s rates for all these measures over time.
Starting in 2014, The Joint Commission will publish hospital rates for cesarean sections and episiotomies, but not rates for individual doctors. Patient access to individual doctors’ rates of cesarean section, early elective delivery, and episiotomy is likely to come in the future, Dr. Gilbert said, and insurers eventually may select physicians and reimbursement rates based on these outcomes.
"As an individual and as a hospital, we need to make sure we’re doing the best we can," he said.
Dr. Gilbert reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – One California community-based hospital got a head start on tracking core measures of quality in perinatal care that all U.S. hospitals will have to report to The Joint Commission beginning January 2014.
Over the past 2 years, the ob.gyns. found it wasn’t easy, but that tracking core measures of quality significantly improved perinatal care.
Sutter Medical Center in Sacramento, Calif., formed a perinatal data committee in 2010 to identify barriers and develop processes for tracking six quality measures, including the five for The Joint Commission. They worked to overcome doubters on their staff, internally published individual doctors’ rates of cesarean section deliveries and episiotomies, and shared the results for each prenatal obstetrics group.
Their overall rate of elective deliveries at less than 39 weeks’ gestation decreased from 25% of the 4,958 deliveries in October 2010 to 2% of the 5,577 deliveries in December 2012. The cesarean section rate for nulliparous women with a term, singleton fetus in a vertex position dropped from 31% in 2010 to 25% in 2012, Dr. William M. Gilbert reported at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
They also improved significantly in two other core measures of quality mandated by The Joint Commission: The proportion of preterm infants who received antenatal steroids before delivery jumped from 80% to 100%, and the proportion of newborns who were fed exclusively breast milk during their entire hospitalization improved from 58% to 70%. The hospital has begun collecting data on a fifth core measure for The Joint Commission: the rate of health care-associated bloodstream infections in newborns.
Dr. Gilbert and his group also tracked two measures that are endorsed by the National Quality Forum but are not yet required by The Joint Commission. Their episiotomy rate decreased significantly from 5% to 2%, and the proportion of women undergoing cesarean section who received appropriate prophylaxis against deep vein thrombosis increased from 95% to 98% (Jt. Comm. J. Qual. Patient Saf. 2013;39:258-66).
"It took us 1-2 years to get the bugs worked out" in tracking core quality measures, said Dr. Gilbert, regional medical director of women’s services for Sutter Health’s Sacramento-Sierra Region, Sacramento, Calif. The effort required leadership from doctors and nurses, administrative and medical records support, and education for coders.
"If your hospital has done nothing to look at what you’re going to be submitting" to The Joint Commission, he added, "I can guarantee you that even if you think you’re doing great, the data are going to be awful, and you’re going to be scrambling to fix a problem that has occurred."
This kind of attention to quality measures in perinatal care is long overdue, he said. Despite the fact that the 4.2 million normal vaginal deliveries per year represent the No. 1 hospital discharge diagnosis in the United States, and studies show immense variation in perinatal practices between hospitals and geographical regions, efforts to measure the quality of hospital care largely have ignored obstetrics because those efforts have focused on Medicare, and few obstetrical patients are covered by Medicare.
Previous studies show a 10-fold variation in cesarean section rates around the country, and cesarean section rates in low-risk patients vary from 2% to 36%. "I would put to you, if you were making widgets or tanks, and you had such variation in the quality of your tanks that the government was paying for, you’d be out of work and probably in jail, but that’s what we tolerate" in health care, he said. Huge variations also have been reported in rates of induction, episiotomy, breastfeeding, and use of antenatal steroids.
The 40 ob.gyns. affiliated with Dr. Gilbert’s hospital had cesarean rates for nulliparous, term, singleton, vertex pregnancies ranging from approximately 8% to 60% when the tracking efforts began, he said. The committee assigned two-digit alphanumeric codes for each provider and posted individual rates of cesarean sections and episiotomies by provider code for 6 months, to start. It took a year of convincing before getting agreement, but then individual rates were posted in the doctors’ and labor and delivery lounges and were e-mailed to all medical staff.
"It’s amazing – amazing what that did," he said. Doctors with the highest cesarean section rates reduced their use of cesarean sections.
The category of elective deliveries at less than 39 weeks’ gestation excluded cases with medical indications for early delivery, but tracking ran into problems initially because ICD-9 codes did not exist for some exemptions, including prior classical cesarean section or prior myomectomy. "You got dinged for that" in the tracking despite the medical indication, he said. So the committee created tracking categories of "avoidable" and "unavoidable" early deliveries, and doctors didn’t get dinged for unavoidable cases.
Some doctors wrote the reason for early delivery as "intrahepatic cholestasis of pregnancy," which is an appropriate indication, but the medical coders told Dr. Gilbert that having the word "intrahepatic" flagged it as gall bladder disease, which is no reason to deliver early. "We had to work with our coders to help us understand," he said.
Every patient at risk of preterm delivery received antenatal steroids at his hospital, Dr. Gilbert said, "but we weren’t documenting it properly." There had been no uniform spot in the medical record to document administration of antenatal steroids, or to show that they had been given before the current hospitalization. Dr. Gilbert’s team worked with the medical records department to change the electronic health records. Nurses now check off if the patient received a full course of antenatal steroids. If this is missing, the doctor gets a pop-up window where a reason must be given.
"That really was effective," he said.
Tracking of episiotomy excluded cases of shoulder dystocia, but not episiotomy for fetal distress. Despite individual rates being internally publicized, the episiotomy rate seems to be stuck at around 2% because "I do have a couple of old-timers," he said. "Even public embarrassment will not get them to change."
"As an individual and as a hospital, we need to make sure we’re doing the best we can."
Capturing data on whether or not newborns are fed exclusively with breast milk can be difficult, in part because it’s often not clear whether the ob.gyn., the nursing staff, or the pediatrician is responsible for this. Dr. Gilbert’s team analyzed 18 cases at his hospital in which women came in saying they wanted to breastfeed the newborn exclusively, but that didn’t happen. In most cases, the babies received formula after a night nurse moved the baby to the nursery so the mother could sleep, a problem that was addressed. Publicizing exclusive breastfeeding rates for 20 different perinatal obstetrics groups – which ranged from 33% to 93% also helped improve breastfeeding rates.
The perinatal data committee also posted a color-coded "dashboard" showing trends in the hospital’s rates for all these measures over time.
Starting in 2014, The Joint Commission will publish hospital rates for cesarean sections and episiotomies, but not rates for individual doctors. Patient access to individual doctors’ rates of cesarean section, early elective delivery, and episiotomy is likely to come in the future, Dr. Gilbert said, and insurers eventually may select physicians and reimbursement rates based on these outcomes.
"As an individual and as a hospital, we need to make sure we’re doing the best we can," he said.
Dr. Gilbert reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – One California community-based hospital got a head start on tracking core measures of quality in perinatal care that all U.S. hospitals will have to report to The Joint Commission beginning January 2014.
Over the past 2 years, the ob.gyns. found it wasn’t easy, but that tracking core measures of quality significantly improved perinatal care.
Sutter Medical Center in Sacramento, Calif., formed a perinatal data committee in 2010 to identify barriers and develop processes for tracking six quality measures, including the five for The Joint Commission. They worked to overcome doubters on their staff, internally published individual doctors’ rates of cesarean section deliveries and episiotomies, and shared the results for each prenatal obstetrics group.
Their overall rate of elective deliveries at less than 39 weeks’ gestation decreased from 25% of the 4,958 deliveries in October 2010 to 2% of the 5,577 deliveries in December 2012. The cesarean section rate for nulliparous women with a term, singleton fetus in a vertex position dropped from 31% in 2010 to 25% in 2012, Dr. William M. Gilbert reported at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
They also improved significantly in two other core measures of quality mandated by The Joint Commission: The proportion of preterm infants who received antenatal steroids before delivery jumped from 80% to 100%, and the proportion of newborns who were fed exclusively breast milk during their entire hospitalization improved from 58% to 70%. The hospital has begun collecting data on a fifth core measure for The Joint Commission: the rate of health care-associated bloodstream infections in newborns.
Dr. Gilbert and his group also tracked two measures that are endorsed by the National Quality Forum but are not yet required by The Joint Commission. Their episiotomy rate decreased significantly from 5% to 2%, and the proportion of women undergoing cesarean section who received appropriate prophylaxis against deep vein thrombosis increased from 95% to 98% (Jt. Comm. J. Qual. Patient Saf. 2013;39:258-66).
"It took us 1-2 years to get the bugs worked out" in tracking core quality measures, said Dr. Gilbert, regional medical director of women’s services for Sutter Health’s Sacramento-Sierra Region, Sacramento, Calif. The effort required leadership from doctors and nurses, administrative and medical records support, and education for coders.
"If your hospital has done nothing to look at what you’re going to be submitting" to The Joint Commission, he added, "I can guarantee you that even if you think you’re doing great, the data are going to be awful, and you’re going to be scrambling to fix a problem that has occurred."
This kind of attention to quality measures in perinatal care is long overdue, he said. Despite the fact that the 4.2 million normal vaginal deliveries per year represent the No. 1 hospital discharge diagnosis in the United States, and studies show immense variation in perinatal practices between hospitals and geographical regions, efforts to measure the quality of hospital care largely have ignored obstetrics because those efforts have focused on Medicare, and few obstetrical patients are covered by Medicare.
Previous studies show a 10-fold variation in cesarean section rates around the country, and cesarean section rates in low-risk patients vary from 2% to 36%. "I would put to you, if you were making widgets or tanks, and you had such variation in the quality of your tanks that the government was paying for, you’d be out of work and probably in jail, but that’s what we tolerate" in health care, he said. Huge variations also have been reported in rates of induction, episiotomy, breastfeeding, and use of antenatal steroids.
The 40 ob.gyns. affiliated with Dr. Gilbert’s hospital had cesarean rates for nulliparous, term, singleton, vertex pregnancies ranging from approximately 8% to 60% when the tracking efforts began, he said. The committee assigned two-digit alphanumeric codes for each provider and posted individual rates of cesarean sections and episiotomies by provider code for 6 months, to start. It took a year of convincing before getting agreement, but then individual rates were posted in the doctors’ and labor and delivery lounges and were e-mailed to all medical staff.
"It’s amazing – amazing what that did," he said. Doctors with the highest cesarean section rates reduced their use of cesarean sections.
The category of elective deliveries at less than 39 weeks’ gestation excluded cases with medical indications for early delivery, but tracking ran into problems initially because ICD-9 codes did not exist for some exemptions, including prior classical cesarean section or prior myomectomy. "You got dinged for that" in the tracking despite the medical indication, he said. So the committee created tracking categories of "avoidable" and "unavoidable" early deliveries, and doctors didn’t get dinged for unavoidable cases.
Some doctors wrote the reason for early delivery as "intrahepatic cholestasis of pregnancy," which is an appropriate indication, but the medical coders told Dr. Gilbert that having the word "intrahepatic" flagged it as gall bladder disease, which is no reason to deliver early. "We had to work with our coders to help us understand," he said.
Every patient at risk of preterm delivery received antenatal steroids at his hospital, Dr. Gilbert said, "but we weren’t documenting it properly." There had been no uniform spot in the medical record to document administration of antenatal steroids, or to show that they had been given before the current hospitalization. Dr. Gilbert’s team worked with the medical records department to change the electronic health records. Nurses now check off if the patient received a full course of antenatal steroids. If this is missing, the doctor gets a pop-up window where a reason must be given.
"That really was effective," he said.
Tracking of episiotomy excluded cases of shoulder dystocia, but not episiotomy for fetal distress. Despite individual rates being internally publicized, the episiotomy rate seems to be stuck at around 2% because "I do have a couple of old-timers," he said. "Even public embarrassment will not get them to change."
"As an individual and as a hospital, we need to make sure we’re doing the best we can."
Capturing data on whether or not newborns are fed exclusively with breast milk can be difficult, in part because it’s often not clear whether the ob.gyn., the nursing staff, or the pediatrician is responsible for this. Dr. Gilbert’s team analyzed 18 cases at his hospital in which women came in saying they wanted to breastfeed the newborn exclusively, but that didn’t happen. In most cases, the babies received formula after a night nurse moved the baby to the nursery so the mother could sleep, a problem that was addressed. Publicizing exclusive breastfeeding rates for 20 different perinatal obstetrics groups – which ranged from 33% to 93% also helped improve breastfeeding rates.
The perinatal data committee also posted a color-coded "dashboard" showing trends in the hospital’s rates for all these measures over time.
Starting in 2014, The Joint Commission will publish hospital rates for cesarean sections and episiotomies, but not rates for individual doctors. Patient access to individual doctors’ rates of cesarean section, early elective delivery, and episiotomy is likely to come in the future, Dr. Gilbert said, and insurers eventually may select physicians and reimbursement rates based on these outcomes.
"As an individual and as a hospital, we need to make sure we’re doing the best we can," he said.
Dr. Gilbert reported having no financial disclosures.
On Twitter @sherryboschert
AT A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Major finding: Tracking quality measures decreased the rate of elective deliveries before 39 weeks’ gestation from 25% to 2% and the cesarean section rate for nulliparous, term, singleton, vertex deliveries from 31% to 25%.
Data source: Two-year data from one community-based medical center with multiple private practitioners.
Disclosures: Dr. Gilbert reported having no financial disclosures.
Three steps identify causes of most stillbirths
SAN FRANCISCO – The cause of stillbirth can be identified in two-thirds of cases by checking the placental histology, conducting an autopsy, and karyotype testing.
That’s a "major, major take-home point" that’s "very different than what I was taught" in medical training, Dr. Yair J. Blumenfeld said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
That finding from an important 2011 study and other new data in the past 5 years suggests that perhaps clinicians should take a staggered approach when ordering tests to search for the etiology of a stillbirth. "Maybe I shouldn’t do a $2,000 workup for thrombophilia and anticardiolipin antibodies if the autopsy showed me that there’s an underlying structural abnormality, or if there’s an abnormal karyotype," he suggested.
In general, a growing proportion of stillbirths is being attributed to maternal, fetal, or placental causes, shrinking the proportion relegated to "idiopathic" or unexplained stillbirth. The idea that most stillbirths are idiopathic is "somewhat old thinking" at this point, said Dr. Blumenfeld of Stanford (Calif.) University.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development created the Stillbirth Collaborative Research Network, which developed a new system of determining the causes of stillbirth and tested it in a multicenter, population-based case-control study in five U.S. states during 2006-2008. Potential etiologies for each stillbirth were graded as a possible or probable cause of death based on a complete evaluation including autopsy, placental pathology, medical records, maternal interview, karyotype, and other laboratory tests.
Investigators found a probable cause in 61% of the 512 stillbirths from 500 women and a possible or probable cause in 76%. More than one possible or probable cause was found in 31% of stillbirths, showing some overlap in the causes of stillbirth. The leading causes of antepartum stillbirths were obstetric complications in 29% and placental pathology in 23%, although some of the causes of stillbirth varied significantly by race (JAMA 2011;306:2459-68).
Obstetric complications were less likely to be the cause of stillbirths in white women (in 22%) or Hispanic women (25%), compared with black women (44%) or women of other races (41%). Infection as a cause of stillbirth also was less likely in whites (7%) or Hispanics (8%), compared with blacks (25%) or other races (22%). Hispanics and whites, however, had higher rates of umbilical cord complications as a cause of stillbirth (13% for each), compared with blacks (4%) or other races (5%).
Among the clinically indicated tests for stillbirths, the placental histology identified a cause of stillbirth 52% of the time. An autopsy found a cause in 31% of cases, and karyotype testing identified a cause 9% of the time. Eight other screening tests found a cause for stillbirth in 0.4%-4.8% of cases, depending on the test. These included screens for antibodies, toxicology, or blood glucose; tests for syphilis, parvovirus, lupus anticoagulant, or anticardiolipin antibody; or detection of fetal blood in fetal-maternal hemorrhage.
"I’m not saying we shouldn’t do these things, but I think in today’s health care climate, especially with health care economics, you should start to think about maybe a staggered approach" in order to control costs, Dr. Blumenfeld said.
Controversy surrounds several topics in the search for stillbirth etiologies: whether chromosomal microarrays are better than karyotype testing; whether or not to order screening for thrombophilias and antiphospholipid antibodies; and what to do if the parents reject an autopsy.
In a study of 532 stillbirths, chromosomal microarray testing yielded results more often than did karyotyping – in 87% of cases vs. 71% – and detected aneuploidy or copy number variants more often, in 8.8% of cases vs. 6.5% (New Engl. J. Med. 2012;367:2185-93). Whether that difference is worth a price tag of approximately $2,000 for microarray testing remains to be seen, but "we’re going to see a lot more studies" of stillbirths using this and other new technologies, Dr. Blumenfeld said.
Practice bulletins from the American College of Obstetricians and Gynecologists are "all over the map" when it comes to deciding whether or not to test for thrombophilias and antiphospholipid antibodies when there’s a stillbirth," he said. "It’s still very, very controversial." It’s probably wise to use the results of autopsy, karyotyping, and placental histology to help decide whether to pursue these other tests, and to talk with patients about their family history of thrombophilia, what the placenta looked like, and other factors that could guide decision-making, he added.
How health care providers counseled parents affected parents’ decision to accept or decline an autopsy of their stillborn infant in 22% of cases, according to one study of 460 parents, 354 obstetricians, 21 perinatal pathologists, and 2,256 midwives (BJOG 2012;119:987-97). Altogether, 62% of parents agreed to an autopsy.
Parents who decline an autopsy still are likely to consent to a "fetal virtuopsy" – a physical exam and MRI or CT imaging of the stillborn infant, a separate study of 96 mothers suggests. Although 62% consented to autopsy, 99% consented to a virtuopsy. In a few cases, the MRI detected abnormalities that were missed on autopsy (Ultrasound Obstet. Gynecol. 2012;39:659-65).
"Clearly, this is not standard, but I think we’re going to see a lot more studies taking this kind of approach to women who are not accepting of an autopsy," Dr. Blumenfeld said. "Go back to your home institutions, find your favorite pediatrician, geneticist, or dysmorphologist, and ask them, ‘Are you willing to come and look at this stillbirth once it is born, and try to get some information just by looking at the infant?’ I guarantee that you will be able to find somebody like that in your institution. It’s something that we do at Stanford."
National statistics from 2006 suggest that 6 of every 1,000 live births will be stillbirths, a rate similar to the prevalence of congenital heart disease, he said. In 2006, there were 25,972 fetal deaths after 20 weeks’ gestation in the United States (Natl. Vital Stat. Rep. 2012:60;1-23). Long-term trends show that the rate of stillbirths has declined after 28 weeks’ gestation but not between 20 and 27 weeks’ gestation.
Dr. Blumenfeld reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The cause of stillbirth can be identified in two-thirds of cases by checking the placental histology, conducting an autopsy, and karyotype testing.
That’s a "major, major take-home point" that’s "very different than what I was taught" in medical training, Dr. Yair J. Blumenfeld said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
That finding from an important 2011 study and other new data in the past 5 years suggests that perhaps clinicians should take a staggered approach when ordering tests to search for the etiology of a stillbirth. "Maybe I shouldn’t do a $2,000 workup for thrombophilia and anticardiolipin antibodies if the autopsy showed me that there’s an underlying structural abnormality, or if there’s an abnormal karyotype," he suggested.
In general, a growing proportion of stillbirths is being attributed to maternal, fetal, or placental causes, shrinking the proportion relegated to "idiopathic" or unexplained stillbirth. The idea that most stillbirths are idiopathic is "somewhat old thinking" at this point, said Dr. Blumenfeld of Stanford (Calif.) University.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development created the Stillbirth Collaborative Research Network, which developed a new system of determining the causes of stillbirth and tested it in a multicenter, population-based case-control study in five U.S. states during 2006-2008. Potential etiologies for each stillbirth were graded as a possible or probable cause of death based on a complete evaluation including autopsy, placental pathology, medical records, maternal interview, karyotype, and other laboratory tests.
Investigators found a probable cause in 61% of the 512 stillbirths from 500 women and a possible or probable cause in 76%. More than one possible or probable cause was found in 31% of stillbirths, showing some overlap in the causes of stillbirth. The leading causes of antepartum stillbirths were obstetric complications in 29% and placental pathology in 23%, although some of the causes of stillbirth varied significantly by race (JAMA 2011;306:2459-68).
Obstetric complications were less likely to be the cause of stillbirths in white women (in 22%) or Hispanic women (25%), compared with black women (44%) or women of other races (41%). Infection as a cause of stillbirth also was less likely in whites (7%) or Hispanics (8%), compared with blacks (25%) or other races (22%). Hispanics and whites, however, had higher rates of umbilical cord complications as a cause of stillbirth (13% for each), compared with blacks (4%) or other races (5%).
Among the clinically indicated tests for stillbirths, the placental histology identified a cause of stillbirth 52% of the time. An autopsy found a cause in 31% of cases, and karyotype testing identified a cause 9% of the time. Eight other screening tests found a cause for stillbirth in 0.4%-4.8% of cases, depending on the test. These included screens for antibodies, toxicology, or blood glucose; tests for syphilis, parvovirus, lupus anticoagulant, or anticardiolipin antibody; or detection of fetal blood in fetal-maternal hemorrhage.
"I’m not saying we shouldn’t do these things, but I think in today’s health care climate, especially with health care economics, you should start to think about maybe a staggered approach" in order to control costs, Dr. Blumenfeld said.
Controversy surrounds several topics in the search for stillbirth etiologies: whether chromosomal microarrays are better than karyotype testing; whether or not to order screening for thrombophilias and antiphospholipid antibodies; and what to do if the parents reject an autopsy.
In a study of 532 stillbirths, chromosomal microarray testing yielded results more often than did karyotyping – in 87% of cases vs. 71% – and detected aneuploidy or copy number variants more often, in 8.8% of cases vs. 6.5% (New Engl. J. Med. 2012;367:2185-93). Whether that difference is worth a price tag of approximately $2,000 for microarray testing remains to be seen, but "we’re going to see a lot more studies" of stillbirths using this and other new technologies, Dr. Blumenfeld said.
Practice bulletins from the American College of Obstetricians and Gynecologists are "all over the map" when it comes to deciding whether or not to test for thrombophilias and antiphospholipid antibodies when there’s a stillbirth," he said. "It’s still very, very controversial." It’s probably wise to use the results of autopsy, karyotyping, and placental histology to help decide whether to pursue these other tests, and to talk with patients about their family history of thrombophilia, what the placenta looked like, and other factors that could guide decision-making, he added.
How health care providers counseled parents affected parents’ decision to accept or decline an autopsy of their stillborn infant in 22% of cases, according to one study of 460 parents, 354 obstetricians, 21 perinatal pathologists, and 2,256 midwives (BJOG 2012;119:987-97). Altogether, 62% of parents agreed to an autopsy.
Parents who decline an autopsy still are likely to consent to a "fetal virtuopsy" – a physical exam and MRI or CT imaging of the stillborn infant, a separate study of 96 mothers suggests. Although 62% consented to autopsy, 99% consented to a virtuopsy. In a few cases, the MRI detected abnormalities that were missed on autopsy (Ultrasound Obstet. Gynecol. 2012;39:659-65).
"Clearly, this is not standard, but I think we’re going to see a lot more studies taking this kind of approach to women who are not accepting of an autopsy," Dr. Blumenfeld said. "Go back to your home institutions, find your favorite pediatrician, geneticist, or dysmorphologist, and ask them, ‘Are you willing to come and look at this stillbirth once it is born, and try to get some information just by looking at the infant?’ I guarantee that you will be able to find somebody like that in your institution. It’s something that we do at Stanford."
National statistics from 2006 suggest that 6 of every 1,000 live births will be stillbirths, a rate similar to the prevalence of congenital heart disease, he said. In 2006, there were 25,972 fetal deaths after 20 weeks’ gestation in the United States (Natl. Vital Stat. Rep. 2012:60;1-23). Long-term trends show that the rate of stillbirths has declined after 28 weeks’ gestation but not between 20 and 27 weeks’ gestation.
Dr. Blumenfeld reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The cause of stillbirth can be identified in two-thirds of cases by checking the placental histology, conducting an autopsy, and karyotype testing.
That’s a "major, major take-home point" that’s "very different than what I was taught" in medical training, Dr. Yair J. Blumenfeld said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
That finding from an important 2011 study and other new data in the past 5 years suggests that perhaps clinicians should take a staggered approach when ordering tests to search for the etiology of a stillbirth. "Maybe I shouldn’t do a $2,000 workup for thrombophilia and anticardiolipin antibodies if the autopsy showed me that there’s an underlying structural abnormality, or if there’s an abnormal karyotype," he suggested.
In general, a growing proportion of stillbirths is being attributed to maternal, fetal, or placental causes, shrinking the proportion relegated to "idiopathic" or unexplained stillbirth. The idea that most stillbirths are idiopathic is "somewhat old thinking" at this point, said Dr. Blumenfeld of Stanford (Calif.) University.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development created the Stillbirth Collaborative Research Network, which developed a new system of determining the causes of stillbirth and tested it in a multicenter, population-based case-control study in five U.S. states during 2006-2008. Potential etiologies for each stillbirth were graded as a possible or probable cause of death based on a complete evaluation including autopsy, placental pathology, medical records, maternal interview, karyotype, and other laboratory tests.
Investigators found a probable cause in 61% of the 512 stillbirths from 500 women and a possible or probable cause in 76%. More than one possible or probable cause was found in 31% of stillbirths, showing some overlap in the causes of stillbirth. The leading causes of antepartum stillbirths were obstetric complications in 29% and placental pathology in 23%, although some of the causes of stillbirth varied significantly by race (JAMA 2011;306:2459-68).
Obstetric complications were less likely to be the cause of stillbirths in white women (in 22%) or Hispanic women (25%), compared with black women (44%) or women of other races (41%). Infection as a cause of stillbirth also was less likely in whites (7%) or Hispanics (8%), compared with blacks (25%) or other races (22%). Hispanics and whites, however, had higher rates of umbilical cord complications as a cause of stillbirth (13% for each), compared with blacks (4%) or other races (5%).
Among the clinically indicated tests for stillbirths, the placental histology identified a cause of stillbirth 52% of the time. An autopsy found a cause in 31% of cases, and karyotype testing identified a cause 9% of the time. Eight other screening tests found a cause for stillbirth in 0.4%-4.8% of cases, depending on the test. These included screens for antibodies, toxicology, or blood glucose; tests for syphilis, parvovirus, lupus anticoagulant, or anticardiolipin antibody; or detection of fetal blood in fetal-maternal hemorrhage.
"I’m not saying we shouldn’t do these things, but I think in today’s health care climate, especially with health care economics, you should start to think about maybe a staggered approach" in order to control costs, Dr. Blumenfeld said.
Controversy surrounds several topics in the search for stillbirth etiologies: whether chromosomal microarrays are better than karyotype testing; whether or not to order screening for thrombophilias and antiphospholipid antibodies; and what to do if the parents reject an autopsy.
In a study of 532 stillbirths, chromosomal microarray testing yielded results more often than did karyotyping – in 87% of cases vs. 71% – and detected aneuploidy or copy number variants more often, in 8.8% of cases vs. 6.5% (New Engl. J. Med. 2012;367:2185-93). Whether that difference is worth a price tag of approximately $2,000 for microarray testing remains to be seen, but "we’re going to see a lot more studies" of stillbirths using this and other new technologies, Dr. Blumenfeld said.
Practice bulletins from the American College of Obstetricians and Gynecologists are "all over the map" when it comes to deciding whether or not to test for thrombophilias and antiphospholipid antibodies when there’s a stillbirth," he said. "It’s still very, very controversial." It’s probably wise to use the results of autopsy, karyotyping, and placental histology to help decide whether to pursue these other tests, and to talk with patients about their family history of thrombophilia, what the placenta looked like, and other factors that could guide decision-making, he added.
How health care providers counseled parents affected parents’ decision to accept or decline an autopsy of their stillborn infant in 22% of cases, according to one study of 460 parents, 354 obstetricians, 21 perinatal pathologists, and 2,256 midwives (BJOG 2012;119:987-97). Altogether, 62% of parents agreed to an autopsy.
Parents who decline an autopsy still are likely to consent to a "fetal virtuopsy" – a physical exam and MRI or CT imaging of the stillborn infant, a separate study of 96 mothers suggests. Although 62% consented to autopsy, 99% consented to a virtuopsy. In a few cases, the MRI detected abnormalities that were missed on autopsy (Ultrasound Obstet. Gynecol. 2012;39:659-65).
"Clearly, this is not standard, but I think we’re going to see a lot more studies taking this kind of approach to women who are not accepting of an autopsy," Dr. Blumenfeld said. "Go back to your home institutions, find your favorite pediatrician, geneticist, or dysmorphologist, and ask them, ‘Are you willing to come and look at this stillbirth once it is born, and try to get some information just by looking at the infant?’ I guarantee that you will be able to find somebody like that in your institution. It’s something that we do at Stanford."
National statistics from 2006 suggest that 6 of every 1,000 live births will be stillbirths, a rate similar to the prevalence of congenital heart disease, he said. In 2006, there were 25,972 fetal deaths after 20 weeks’ gestation in the United States (Natl. Vital Stat. Rep. 2012:60;1-23). Long-term trends show that the rate of stillbirths has declined after 28 weeks’ gestation but not between 20 and 27 weeks’ gestation.
Dr. Blumenfeld reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Initial prenatal care visit is myth-busting time
SAN FRANCISCO – Dr. Meg Autry typically spends a first prenatal care visit talking about what her pregnant patient may have heard – the myths and the facts – regarding the dos and don’ts during pregnancy.
She’s not alone. Patients hear plenty of prenatal myths perpetuated not only by their peers but by some health care providers, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
An informal electronic poll of the physicians, nurses, and nurse-midwives at the meeting showed that 63% discuss diet at a new patient visit, 17% talk about environmental exposures, 12% discuss exercise, and 8% discuss dietary supplements. These topics were generated more by the health care providers than by the patients, they said.
Deli meats were the leading dietary topic, discussed by 34%, followed by cooked fish, sushi, vegetarian diets, and cheese, in that order. Most of the questions about exercise come from women who exercise a lot, 73% of respondents said, than from women who don’t exercise enough (27%). Iron led the list of supplements discussed (by 36%), followed by omega-3 fatty acids, and (in a third-place tie) calcium and vitamin D.
Dr. Autry, professor of ob.gyn. and reproductive sciences at the university, offered the following myth busters and evidence-based advice for prenatal care. "My goal is to give you a basis for what you talk about with patients," she said.
• Fish: A food that’s high in quality protein, low in saturated fat, and full of beneficial omega-3 fatty acids comes with a downside: Methylmercury that can impair fetal and newborn motor and cognitive skills. Two prospective studies of dietary fish’s effects in pregnancy produced conflicting results. One study that found adverse effects from daily eating of fish was conducted in the Danish Faeroe Islands, where much of what they ate was whale. The other study, in the Pacific Ocean’s Seychelles Islands, found infant neurodevelopmental benefits when mothers ate fish in 12 meals/week, including types of fish that were more similar to those eaten in the United States, Dr. Autry said.
The Food and Drug Administration and Environmental Protection Agency in 2004 advised consumers to eat up to 12 ounces (two average meals) per week of a variety of fish that are low in mercury and to check local advisories about the safety of locally caught fish.
Encourage women to eat fish, she said, "but don’t eat fish that live for a long time and that eat lots of other fish," such as shark, swordfish, king mackerel, tilefish, whale, or albacore tuna.
• Sushi: Very rare infectious diseases from raw fish are virtually a nonproblem in the United States, because most sushi is flash frozen, which kills most pathogens. "I don’t think you need to tell patients they need to stop eating sushi," she said. "Talk to them more about mercury" and talk about the benefits of eating moderate amounts of fish.
• Supplements: There’s no evidence that taking a supplement to get omega-3 fatty acids is beneficial, especially compared with eating fish. "We’re just supposed to eat it, we’re not supposed to have a pill to fix everything," she said.
A standard prenatal vitamin supplies the iron and other vitamins and minerals needed, and it’s good to advise patients to eat foods that promote iron absorption and are high in vitamin C, such as strawberries or broccoli. Warn women that their prenatal vitamin should be their maximum dose of vitamin A, a known teratogen. There’s no good evidence that taking extra calcium or vitamin D supplements generally is helpful in pregnancy, but the American College of Obstetricians and Gynecologists recommends considering vitamin D supplementation in women at risk of deficiency.
• Cheese: A third of U.S. cases of listeriosis occurs in pregnant women and is associated with miscarriage and stillbirth. Nationally, the bacteria Listeria reaches people most commonly through hot dogs. In California, it’s the queso fresco. The FDA and/or the U.S. Department of Agriculture advise pregnant women not to eat hot dogs or luncheon meats unless they’re reheating to steaming, and to avoid soft cheeses; refrigerated pâtés or meat spreads; smoked seafood; raw or unpasteurized milk; and raw or undercooked meats.
• Caffeine: Approximately 85% of U.S. women report eating or drinking caffeine-containing food or drinks, Dr. Autry said. Concerns that caffeine consumption might be associated with low birth weight, congenital anomalies, delay in conception, or miscarriage were poorly designed and confounded by an association between caffeine intake and cigarette smoking. More recent studies predominantly have been negative, and a randomized, controlled trial found no association between moderate caffeine intake and gestational age or birth weight (BMJ 2007;334:409).
• Alcohol: Bad news for the 10% of pregnant women who report ingesting alcohol and especially for the 2% who binge drink during pregnancy: There’s no safe level of alcohol intake during pregnancy. Federal data suggest that 1 in 6,000 U.S. newborns have fetal alcohol syndrome or fetal alcohol spectrum disorder.
• Nicotine: The tricky problem with nicotine is not just that it’s "associated with everything bad," Dr. Autry said, but that people know it’s bad, so an estimated 25%-50% of pregnant women don’t disclose that they smoke. Smoking in pregnancy is associated with miscarriage, abruption, ectopic pregnancy, preterm delivery, and more. Among mothers who quit smoking during pregnancy, 90% relapse after delivery. "It’s really important to continue the smoking cessation discussion during pregnancy," she said. "It’s important to say, ‘If you go back to smoking, don’t do it in the house, because it’s bad for the kid.’"
• Hot tubs: Soaking during the first trimester, or any time in pregnancy in water heated to 100 F or higher, is potentially teratogenic, two studies suggest. Maternal hyperthermia from hot tubs has been associated with first trimester fetal loss and with a nearly doubling in risk for neural tube defects.
• Exercise: The general recommendation to get 30 minutes or more of moderate exercise on most days applies to pregnant women unless they have some medical or obstetric complication. Exercise is believed to help prevent gestational diabetes, reduce the risk for preeclampsia and premature labor, and decrease the risk for postpartum depression. ACOG recommends avoiding scuba diving, contact sports, and supine activities or motionless standings. Yoga is fine, but avoid so-called "hot yoga," Dr. Autry said.
For high-performance athletes, exertion at high altitudes appears to be safe. There is no pregnancy-specific maximum heart rate.
"Just don’t do anything in pregnancy that you wouldn’t do before," Dr. Autry said. If you’ve never run a marathon, pregnancy is not the time to start.
• Hair dye: There are no data to support the idea of teratogenic effects from the chemicals in hair dyes. But it’s probably still a good idea to look at the labels and choose products with ingredients that are less long acting and organic, if possible, she said.
For resources on environmental exposures during pregnancy, see the university’s Program on Reproductive Health and the Environment.
Dr. Autry reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Meg Autry typically spends a first prenatal care visit talking about what her pregnant patient may have heard – the myths and the facts – regarding the dos and don’ts during pregnancy.
She’s not alone. Patients hear plenty of prenatal myths perpetuated not only by their peers but by some health care providers, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
An informal electronic poll of the physicians, nurses, and nurse-midwives at the meeting showed that 63% discuss diet at a new patient visit, 17% talk about environmental exposures, 12% discuss exercise, and 8% discuss dietary supplements. These topics were generated more by the health care providers than by the patients, they said.
Deli meats were the leading dietary topic, discussed by 34%, followed by cooked fish, sushi, vegetarian diets, and cheese, in that order. Most of the questions about exercise come from women who exercise a lot, 73% of respondents said, than from women who don’t exercise enough (27%). Iron led the list of supplements discussed (by 36%), followed by omega-3 fatty acids, and (in a third-place tie) calcium and vitamin D.
Dr. Autry, professor of ob.gyn. and reproductive sciences at the university, offered the following myth busters and evidence-based advice for prenatal care. "My goal is to give you a basis for what you talk about with patients," she said.
• Fish: A food that’s high in quality protein, low in saturated fat, and full of beneficial omega-3 fatty acids comes with a downside: Methylmercury that can impair fetal and newborn motor and cognitive skills. Two prospective studies of dietary fish’s effects in pregnancy produced conflicting results. One study that found adverse effects from daily eating of fish was conducted in the Danish Faeroe Islands, where much of what they ate was whale. The other study, in the Pacific Ocean’s Seychelles Islands, found infant neurodevelopmental benefits when mothers ate fish in 12 meals/week, including types of fish that were more similar to those eaten in the United States, Dr. Autry said.
The Food and Drug Administration and Environmental Protection Agency in 2004 advised consumers to eat up to 12 ounces (two average meals) per week of a variety of fish that are low in mercury and to check local advisories about the safety of locally caught fish.
Encourage women to eat fish, she said, "but don’t eat fish that live for a long time and that eat lots of other fish," such as shark, swordfish, king mackerel, tilefish, whale, or albacore tuna.
• Sushi: Very rare infectious diseases from raw fish are virtually a nonproblem in the United States, because most sushi is flash frozen, which kills most pathogens. "I don’t think you need to tell patients they need to stop eating sushi," she said. "Talk to them more about mercury" and talk about the benefits of eating moderate amounts of fish.
• Supplements: There’s no evidence that taking a supplement to get omega-3 fatty acids is beneficial, especially compared with eating fish. "We’re just supposed to eat it, we’re not supposed to have a pill to fix everything," she said.
A standard prenatal vitamin supplies the iron and other vitamins and minerals needed, and it’s good to advise patients to eat foods that promote iron absorption and are high in vitamin C, such as strawberries or broccoli. Warn women that their prenatal vitamin should be their maximum dose of vitamin A, a known teratogen. There’s no good evidence that taking extra calcium or vitamin D supplements generally is helpful in pregnancy, but the American College of Obstetricians and Gynecologists recommends considering vitamin D supplementation in women at risk of deficiency.
• Cheese: A third of U.S. cases of listeriosis occurs in pregnant women and is associated with miscarriage and stillbirth. Nationally, the bacteria Listeria reaches people most commonly through hot dogs. In California, it’s the queso fresco. The FDA and/or the U.S. Department of Agriculture advise pregnant women not to eat hot dogs or luncheon meats unless they’re reheating to steaming, and to avoid soft cheeses; refrigerated pâtés or meat spreads; smoked seafood; raw or unpasteurized milk; and raw or undercooked meats.
• Caffeine: Approximately 85% of U.S. women report eating or drinking caffeine-containing food or drinks, Dr. Autry said. Concerns that caffeine consumption might be associated with low birth weight, congenital anomalies, delay in conception, or miscarriage were poorly designed and confounded by an association between caffeine intake and cigarette smoking. More recent studies predominantly have been negative, and a randomized, controlled trial found no association between moderate caffeine intake and gestational age or birth weight (BMJ 2007;334:409).
• Alcohol: Bad news for the 10% of pregnant women who report ingesting alcohol and especially for the 2% who binge drink during pregnancy: There’s no safe level of alcohol intake during pregnancy. Federal data suggest that 1 in 6,000 U.S. newborns have fetal alcohol syndrome or fetal alcohol spectrum disorder.
• Nicotine: The tricky problem with nicotine is not just that it’s "associated with everything bad," Dr. Autry said, but that people know it’s bad, so an estimated 25%-50% of pregnant women don’t disclose that they smoke. Smoking in pregnancy is associated with miscarriage, abruption, ectopic pregnancy, preterm delivery, and more. Among mothers who quit smoking during pregnancy, 90% relapse after delivery. "It’s really important to continue the smoking cessation discussion during pregnancy," she said. "It’s important to say, ‘If you go back to smoking, don’t do it in the house, because it’s bad for the kid.’"
• Hot tubs: Soaking during the first trimester, or any time in pregnancy in water heated to 100 F or higher, is potentially teratogenic, two studies suggest. Maternal hyperthermia from hot tubs has been associated with first trimester fetal loss and with a nearly doubling in risk for neural tube defects.
• Exercise: The general recommendation to get 30 minutes or more of moderate exercise on most days applies to pregnant women unless they have some medical or obstetric complication. Exercise is believed to help prevent gestational diabetes, reduce the risk for preeclampsia and premature labor, and decrease the risk for postpartum depression. ACOG recommends avoiding scuba diving, contact sports, and supine activities or motionless standings. Yoga is fine, but avoid so-called "hot yoga," Dr. Autry said.
For high-performance athletes, exertion at high altitudes appears to be safe. There is no pregnancy-specific maximum heart rate.
"Just don’t do anything in pregnancy that you wouldn’t do before," Dr. Autry said. If you’ve never run a marathon, pregnancy is not the time to start.
• Hair dye: There are no data to support the idea of teratogenic effects from the chemicals in hair dyes. But it’s probably still a good idea to look at the labels and choose products with ingredients that are less long acting and organic, if possible, she said.
For resources on environmental exposures during pregnancy, see the university’s Program on Reproductive Health and the Environment.
Dr. Autry reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Meg Autry typically spends a first prenatal care visit talking about what her pregnant patient may have heard – the myths and the facts – regarding the dos and don’ts during pregnancy.
She’s not alone. Patients hear plenty of prenatal myths perpetuated not only by their peers but by some health care providers, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
An informal electronic poll of the physicians, nurses, and nurse-midwives at the meeting showed that 63% discuss diet at a new patient visit, 17% talk about environmental exposures, 12% discuss exercise, and 8% discuss dietary supplements. These topics were generated more by the health care providers than by the patients, they said.
Deli meats were the leading dietary topic, discussed by 34%, followed by cooked fish, sushi, vegetarian diets, and cheese, in that order. Most of the questions about exercise come from women who exercise a lot, 73% of respondents said, than from women who don’t exercise enough (27%). Iron led the list of supplements discussed (by 36%), followed by omega-3 fatty acids, and (in a third-place tie) calcium and vitamin D.
Dr. Autry, professor of ob.gyn. and reproductive sciences at the university, offered the following myth busters and evidence-based advice for prenatal care. "My goal is to give you a basis for what you talk about with patients," she said.
• Fish: A food that’s high in quality protein, low in saturated fat, and full of beneficial omega-3 fatty acids comes with a downside: Methylmercury that can impair fetal and newborn motor and cognitive skills. Two prospective studies of dietary fish’s effects in pregnancy produced conflicting results. One study that found adverse effects from daily eating of fish was conducted in the Danish Faeroe Islands, where much of what they ate was whale. The other study, in the Pacific Ocean’s Seychelles Islands, found infant neurodevelopmental benefits when mothers ate fish in 12 meals/week, including types of fish that were more similar to those eaten in the United States, Dr. Autry said.
The Food and Drug Administration and Environmental Protection Agency in 2004 advised consumers to eat up to 12 ounces (two average meals) per week of a variety of fish that are low in mercury and to check local advisories about the safety of locally caught fish.
Encourage women to eat fish, she said, "but don’t eat fish that live for a long time and that eat lots of other fish," such as shark, swordfish, king mackerel, tilefish, whale, or albacore tuna.
• Sushi: Very rare infectious diseases from raw fish are virtually a nonproblem in the United States, because most sushi is flash frozen, which kills most pathogens. "I don’t think you need to tell patients they need to stop eating sushi," she said. "Talk to them more about mercury" and talk about the benefits of eating moderate amounts of fish.
• Supplements: There’s no evidence that taking a supplement to get omega-3 fatty acids is beneficial, especially compared with eating fish. "We’re just supposed to eat it, we’re not supposed to have a pill to fix everything," she said.
A standard prenatal vitamin supplies the iron and other vitamins and minerals needed, and it’s good to advise patients to eat foods that promote iron absorption and are high in vitamin C, such as strawberries or broccoli. Warn women that their prenatal vitamin should be their maximum dose of vitamin A, a known teratogen. There’s no good evidence that taking extra calcium or vitamin D supplements generally is helpful in pregnancy, but the American College of Obstetricians and Gynecologists recommends considering vitamin D supplementation in women at risk of deficiency.
• Cheese: A third of U.S. cases of listeriosis occurs in pregnant women and is associated with miscarriage and stillbirth. Nationally, the bacteria Listeria reaches people most commonly through hot dogs. In California, it’s the queso fresco. The FDA and/or the U.S. Department of Agriculture advise pregnant women not to eat hot dogs or luncheon meats unless they’re reheating to steaming, and to avoid soft cheeses; refrigerated pâtés or meat spreads; smoked seafood; raw or unpasteurized milk; and raw or undercooked meats.
• Caffeine: Approximately 85% of U.S. women report eating or drinking caffeine-containing food or drinks, Dr. Autry said. Concerns that caffeine consumption might be associated with low birth weight, congenital anomalies, delay in conception, or miscarriage were poorly designed and confounded by an association between caffeine intake and cigarette smoking. More recent studies predominantly have been negative, and a randomized, controlled trial found no association between moderate caffeine intake and gestational age or birth weight (BMJ 2007;334:409).
• Alcohol: Bad news for the 10% of pregnant women who report ingesting alcohol and especially for the 2% who binge drink during pregnancy: There’s no safe level of alcohol intake during pregnancy. Federal data suggest that 1 in 6,000 U.S. newborns have fetal alcohol syndrome or fetal alcohol spectrum disorder.
• Nicotine: The tricky problem with nicotine is not just that it’s "associated with everything bad," Dr. Autry said, but that people know it’s bad, so an estimated 25%-50% of pregnant women don’t disclose that they smoke. Smoking in pregnancy is associated with miscarriage, abruption, ectopic pregnancy, preterm delivery, and more. Among mothers who quit smoking during pregnancy, 90% relapse after delivery. "It’s really important to continue the smoking cessation discussion during pregnancy," she said. "It’s important to say, ‘If you go back to smoking, don’t do it in the house, because it’s bad for the kid.’"
• Hot tubs: Soaking during the first trimester, or any time in pregnancy in water heated to 100 F or higher, is potentially teratogenic, two studies suggest. Maternal hyperthermia from hot tubs has been associated with first trimester fetal loss and with a nearly doubling in risk for neural tube defects.
• Exercise: The general recommendation to get 30 minutes or more of moderate exercise on most days applies to pregnant women unless they have some medical or obstetric complication. Exercise is believed to help prevent gestational diabetes, reduce the risk for preeclampsia and premature labor, and decrease the risk for postpartum depression. ACOG recommends avoiding scuba diving, contact sports, and supine activities or motionless standings. Yoga is fine, but avoid so-called "hot yoga," Dr. Autry said.
For high-performance athletes, exertion at high altitudes appears to be safe. There is no pregnancy-specific maximum heart rate.
"Just don’t do anything in pregnancy that you wouldn’t do before," Dr. Autry said. If you’ve never run a marathon, pregnancy is not the time to start.
• Hair dye: There are no data to support the idea of teratogenic effects from the chemicals in hair dyes. But it’s probably still a good idea to look at the labels and choose products with ingredients that are less long acting and organic, if possible, she said.
For resources on environmental exposures during pregnancy, see the university’s Program on Reproductive Health and the Environment.
Dr. Autry reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS AT A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
No benefit seen with nifedipine maintenance tocolysis
SAN FRANCISCO – A large randomized, double-blind placebo-controlled study in the Netherlands supports earlier studies that found no benefit from routine maintenance tocolysis using nifedipine in women with arrested preterm labor.
What to do when preterm labor stops is "a million dollar question that many of us have faced," Dr. Deirdre J. Lyell said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco. Surveys suggest that more than a quarter of maternal-fetal medicine specialists routinely use maintenance tocolysis, most often with nifedipine, despite its questionable utility.
The Dutch study of 406 women "puts the question to bed," said Dr. Lyell, a maternal-fetal medicine ob.gyn. at Stanford (Calif.) University. She was not involved in the study.
The multicenter trial in these women was underpowered to show a statistically significant difference in its primary outcome – a composite of perinatal adverse outcomes – because of a lower-than-expected rate of adverse events in the control group, so it couldn’t exclude a possible benefit from nifedipine. However, "its use for maintenance tocolysis does not appear beneficial at this time," the investigators wrote (JAMA 2013;309:41-7).
Women in the study had arrested preterm labor at 24-34 weeks’ gestation. They were randomized to maintenance tocolysis with 20 mg nifedipine or placebo every 4-6 hours. Delivery occurred at 35 weeks in the nifedipine group and at 35 weeks and 2 days in the control group. The number of days of pregnancy after starting treatment was 34 and 33, respectively, and the two groups had similar rates of recurrent preterm labor. Twelve percent in the nifedipine group and 14% in the control group developed one of the problems in the primary composite outcome: perinatal death, chronic lung disease, neonatal sepsis, intraventricular hemorrhage greater than grade 2, periventricular leukomalacia greater than grade 1, or necrotizing enterocolitis.
"There’s no evidence these medications were able to delay delivery," Dr. Lyell said.
Three previous randomized trials also found no benefit from maintenance tocolysis with nifedipine. One nonblinded study of 74 U.S. women found no difference in outcomes (Am. J. Obstet. Gynecol. 1999;181:822-7). Neither did a nonblinded Iranian study that randomized 73 women but did not report how the randomization was conducted (J. Perinat. Med. 2004;32:220-4). Dr. Lyell and her associates then conducted a double-blind placebo-controlled trial in 68 women, which again was negative (Obstet. Gynecol. 2008;112:1221-6).
These studies were small, "but we still haven’t seen anything robust to say this is something we should do," Dr. Lyell said.
Nifedipine can produce maternal side effects. In a trial comparing intravenous magnesium sulfate with oral nifedipine for acute tocolysis, nifedipine caused headache in 24% of women who received the drug, vomiting in 5%, hypotension in 5%, shortness of breath in 5%, and lethargy in 5% (Obstet. Gynecol. 2007;110:61-7).
Beta-mimetics such as terbutaline have a much longer list of maternal, fetal, and neonatal side effects, and two randomized controlled trials have shown that maintenance tocolysis using a terbutaline pump was not more effective than giving saline to prevent recurrent preterm labor, Dr. Lyell said.
A 2008 survey of 827 members of the Society of Maternal-Fetal Medicine found that 29% routinely use maintenance tocolysis and 31% will use it if the patient desires. Among members who employ maintenance tocolysis, nifedipine was the first choice of 79% (Obstet. Gynecol. 2008;112:42-7).
In an informal electronic survey of the physicians, nurses, and midwives at the meeting, 6% said they routinely use maintenance tocolysis, 67% occasionally use it, and 26% never use it. In a repeat survey after Dr. Lyell’s talk, none favored routine maintenance tocolysis, 53% said they would use it occasionally, and 47% said they would no longer use it.
The Netherlands Organization for Health Research and Development funded the study. Dr. Lyell reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A large randomized, double-blind placebo-controlled study in the Netherlands supports earlier studies that found no benefit from routine maintenance tocolysis using nifedipine in women with arrested preterm labor.
What to do when preterm labor stops is "a million dollar question that many of us have faced," Dr. Deirdre J. Lyell said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco. Surveys suggest that more than a quarter of maternal-fetal medicine specialists routinely use maintenance tocolysis, most often with nifedipine, despite its questionable utility.
The Dutch study of 406 women "puts the question to bed," said Dr. Lyell, a maternal-fetal medicine ob.gyn. at Stanford (Calif.) University. She was not involved in the study.
The multicenter trial in these women was underpowered to show a statistically significant difference in its primary outcome – a composite of perinatal adverse outcomes – because of a lower-than-expected rate of adverse events in the control group, so it couldn’t exclude a possible benefit from nifedipine. However, "its use for maintenance tocolysis does not appear beneficial at this time," the investigators wrote (JAMA 2013;309:41-7).
Women in the study had arrested preterm labor at 24-34 weeks’ gestation. They were randomized to maintenance tocolysis with 20 mg nifedipine or placebo every 4-6 hours. Delivery occurred at 35 weeks in the nifedipine group and at 35 weeks and 2 days in the control group. The number of days of pregnancy after starting treatment was 34 and 33, respectively, and the two groups had similar rates of recurrent preterm labor. Twelve percent in the nifedipine group and 14% in the control group developed one of the problems in the primary composite outcome: perinatal death, chronic lung disease, neonatal sepsis, intraventricular hemorrhage greater than grade 2, periventricular leukomalacia greater than grade 1, or necrotizing enterocolitis.
"There’s no evidence these medications were able to delay delivery," Dr. Lyell said.
Three previous randomized trials also found no benefit from maintenance tocolysis with nifedipine. One nonblinded study of 74 U.S. women found no difference in outcomes (Am. J. Obstet. Gynecol. 1999;181:822-7). Neither did a nonblinded Iranian study that randomized 73 women but did not report how the randomization was conducted (J. Perinat. Med. 2004;32:220-4). Dr. Lyell and her associates then conducted a double-blind placebo-controlled trial in 68 women, which again was negative (Obstet. Gynecol. 2008;112:1221-6).
These studies were small, "but we still haven’t seen anything robust to say this is something we should do," Dr. Lyell said.
Nifedipine can produce maternal side effects. In a trial comparing intravenous magnesium sulfate with oral nifedipine for acute tocolysis, nifedipine caused headache in 24% of women who received the drug, vomiting in 5%, hypotension in 5%, shortness of breath in 5%, and lethargy in 5% (Obstet. Gynecol. 2007;110:61-7).
Beta-mimetics such as terbutaline have a much longer list of maternal, fetal, and neonatal side effects, and two randomized controlled trials have shown that maintenance tocolysis using a terbutaline pump was not more effective than giving saline to prevent recurrent preterm labor, Dr. Lyell said.
A 2008 survey of 827 members of the Society of Maternal-Fetal Medicine found that 29% routinely use maintenance tocolysis and 31% will use it if the patient desires. Among members who employ maintenance tocolysis, nifedipine was the first choice of 79% (Obstet. Gynecol. 2008;112:42-7).
In an informal electronic survey of the physicians, nurses, and midwives at the meeting, 6% said they routinely use maintenance tocolysis, 67% occasionally use it, and 26% never use it. In a repeat survey after Dr. Lyell’s talk, none favored routine maintenance tocolysis, 53% said they would use it occasionally, and 47% said they would no longer use it.
The Netherlands Organization for Health Research and Development funded the study. Dr. Lyell reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A large randomized, double-blind placebo-controlled study in the Netherlands supports earlier studies that found no benefit from routine maintenance tocolysis using nifedipine in women with arrested preterm labor.
What to do when preterm labor stops is "a million dollar question that many of us have faced," Dr. Deirdre J. Lyell said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco. Surveys suggest that more than a quarter of maternal-fetal medicine specialists routinely use maintenance tocolysis, most often with nifedipine, despite its questionable utility.
The Dutch study of 406 women "puts the question to bed," said Dr. Lyell, a maternal-fetal medicine ob.gyn. at Stanford (Calif.) University. She was not involved in the study.
The multicenter trial in these women was underpowered to show a statistically significant difference in its primary outcome – a composite of perinatal adverse outcomes – because of a lower-than-expected rate of adverse events in the control group, so it couldn’t exclude a possible benefit from nifedipine. However, "its use for maintenance tocolysis does not appear beneficial at this time," the investigators wrote (JAMA 2013;309:41-7).
Women in the study had arrested preterm labor at 24-34 weeks’ gestation. They were randomized to maintenance tocolysis with 20 mg nifedipine or placebo every 4-6 hours. Delivery occurred at 35 weeks in the nifedipine group and at 35 weeks and 2 days in the control group. The number of days of pregnancy after starting treatment was 34 and 33, respectively, and the two groups had similar rates of recurrent preterm labor. Twelve percent in the nifedipine group and 14% in the control group developed one of the problems in the primary composite outcome: perinatal death, chronic lung disease, neonatal sepsis, intraventricular hemorrhage greater than grade 2, periventricular leukomalacia greater than grade 1, or necrotizing enterocolitis.
"There’s no evidence these medications were able to delay delivery," Dr. Lyell said.
Three previous randomized trials also found no benefit from maintenance tocolysis with nifedipine. One nonblinded study of 74 U.S. women found no difference in outcomes (Am. J. Obstet. Gynecol. 1999;181:822-7). Neither did a nonblinded Iranian study that randomized 73 women but did not report how the randomization was conducted (J. Perinat. Med. 2004;32:220-4). Dr. Lyell and her associates then conducted a double-blind placebo-controlled trial in 68 women, which again was negative (Obstet. Gynecol. 2008;112:1221-6).
These studies were small, "but we still haven’t seen anything robust to say this is something we should do," Dr. Lyell said.
Nifedipine can produce maternal side effects. In a trial comparing intravenous magnesium sulfate with oral nifedipine for acute tocolysis, nifedipine caused headache in 24% of women who received the drug, vomiting in 5%, hypotension in 5%, shortness of breath in 5%, and lethargy in 5% (Obstet. Gynecol. 2007;110:61-7).
Beta-mimetics such as terbutaline have a much longer list of maternal, fetal, and neonatal side effects, and two randomized controlled trials have shown that maintenance tocolysis using a terbutaline pump was not more effective than giving saline to prevent recurrent preterm labor, Dr. Lyell said.
A 2008 survey of 827 members of the Society of Maternal-Fetal Medicine found that 29% routinely use maintenance tocolysis and 31% will use it if the patient desires. Among members who employ maintenance tocolysis, nifedipine was the first choice of 79% (Obstet. Gynecol. 2008;112:42-7).
In an informal electronic survey of the physicians, nurses, and midwives at the meeting, 6% said they routinely use maintenance tocolysis, 67% occasionally use it, and 26% never use it. In a repeat survey after Dr. Lyell’s talk, none favored routine maintenance tocolysis, 53% said they would use it occasionally, and 47% said they would no longer use it.
The Netherlands Organization for Health Research and Development funded the study. Dr. Lyell reported having no relevant financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS AT A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Ten steps reduce dangerous chemicals in pregnancy
SAN FRANCISCO – Pregnant women, more than anyone, face a challenge that Rachel Carson described in her 1962 book "Silent Spring": "What we have to face is not an occasional dose of poison which has accidentally got into some article of food, but a persistent and continuous poisoning of the whole human environment."
Modern science suggests that this is truer than ever, and that the danger especially applies to fetuses, Dr. Marya G. Zlatnik said.
One study reported that 43 of 163 (26%) unwanted chemicals could be detected in 99% of pregnant women in the United States, even though some chemicals had been banned for years (Environ. Health Perspect. 2011;119:878-85).
What’s a woman – and her physician – to do? Physicians can recommend 10 relatively simple steps that their pregnant patients can take today to protect themselves and their babies, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
• Buy organic. It’s not cheap, but buying organic foods such as fruit and produce make a big difference in reducing exposure to pesticides, said Dr. Zlatnik, a high-risk ob.gyn. and perinatologist at the university. One study of 23 schoolchildren substituted organic food for their conventional diets and found a dramatic drop in organophosphorus pesticide levels in their urine while eating organically, but not before or after (Environ. Health Perspect. 2006;114:260-3).
• Don’t microwave plastic. Taking that plastic tub of leftovers directly from the refrigerator to the microwave oven may be convenient, but it can contaminate your food with bisphenol A (BPA) or other endocrine disrupting chemicals that may be in the plastic container. Why does that matter? A growing number of studies suggest that fetal exposure to BPA increases the risks for multiple health problems.
One study of 244 mothers and their children showed that each 10-fold increase in maternal serum BPA levels was associated with more anxious and depressed behavior in the children by age 3 years (Pediatrics 2011;128:873-882). Another study in mice found that BPA may increase the risk for metabolic disorders and diabetes and that the fetal development stage was the critical window of susceptibility to BPA exposure (PLoS One 2013;8:e64143). Swedish investigators showed in a separate study that BPA increases angiogenesis in human endometrial cells in vitro, suggesting that the chemical could disturb normal endometrial functioning related to pregnancy and fertility.
• Avoid plastic contact with food/drinks. Plastic storage containers for food aren’t the only problem. Even without heating in a microwave, plastic can leach BPA or other endocrine-disrupting chemicals into your food or drinks. And plastic is ubiquitous – it’s in the linings of most canned foods, in polycarbonate water bottles, and in the plastic pouches or soft-box linings of wet foods. Try to avoid any food item with substantial plastic content.
• Don’t accept the receipt. Carbonless receipts – the kind you get at the ATM or in any store where you pay by credit card – commonly contain BPA, phthalates, or other endocrine disruptors. In response to concerns about BPA, some stores have started to use BPA-free receipts, "but many times when the BPA is removed, another phthalate gets added, so don’t even take the receipts," Dr. Zlatnik advised. Workers who have to handle carbonless receipts should wear gloves and/or wash their hands frequently, she added.
• Limit pesticide use around the home. A good principle in general, this is especially important during pregnancy.
• Be thoughtful about personal care products. Cosmetics and other personal care products can contain BPA or other endocrine disruptors. Skip the lipstick during pregnancy if you can’t verify that it’s free of harmful chemicals, for example.
• Mop daily. Dust mopping or damp mopping to remove dust that may contain lead or potentially harmful chemicals. "Along those lines, don’t wear shoes in the house," because they track these substances into the home, Dr. Zlatnik said.
• Replace foam furniture. Ubiquitous laws require furniture or mattresses containing foam to be treated with flame-retardant chemicals to reduce fire risk, but now it’s becoming clear that polybrominated diphenyl ethers (PBDEs) in the those chemicals can pose health risks.
Maternal prenatal PBDE concentrations were associated with impaired attention in children at age 5 years, poorer fine-motor coordination at ages 5 and 7 years, and lower scores on some sections of IQ tests at age 7 years in a study of 323 mothers and children (Environ. Health Perspect. 2013;121:257-62). A separate study of 210 cord blood samples found lower scores on tests of mental and physical development (including IQ) at 12-72 months of age in children who had higher concentrations of PBDEs at birth (Environ. Health Perspect. 2010;118:712-9). Serum levels of PBDE in the second trimester of pregnancy were associated with thyroid-stimulating hormone levels in a study of 25 pregnant Californians (Environ. Sci. Technol. 2011;45:7896-905).
• Quit smoking. Avoid second-hand smoke. Remind patients that toxins in cigarette smoke increase the risk for miscarriage, infertility, and preterm birth, among other problems.
• Avoid lead. This can be simple and inexpensive, such as dust mopping daily and avoiding lead-containing lipsticks, or complicated and expensive, such as staying away from jobs or hobbies with exposure to lead, or lead paint–abatement remedies. Women with a history of lead exposure can take calcium supplements to minimize the release of lead stored in bone.
"This is not a comprehensive list, but these are some relatively simple things to do" to avoid troublesome environmental chemicals during pregnancy, Dr. Zlatnik said.
She reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Pregnant women, more than anyone, face a challenge that Rachel Carson described in her 1962 book "Silent Spring": "What we have to face is not an occasional dose of poison which has accidentally got into some article of food, but a persistent and continuous poisoning of the whole human environment."
Modern science suggests that this is truer than ever, and that the danger especially applies to fetuses, Dr. Marya G. Zlatnik said.
One study reported that 43 of 163 (26%) unwanted chemicals could be detected in 99% of pregnant women in the United States, even though some chemicals had been banned for years (Environ. Health Perspect. 2011;119:878-85).
What’s a woman – and her physician – to do? Physicians can recommend 10 relatively simple steps that their pregnant patients can take today to protect themselves and their babies, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
• Buy organic. It’s not cheap, but buying organic foods such as fruit and produce make a big difference in reducing exposure to pesticides, said Dr. Zlatnik, a high-risk ob.gyn. and perinatologist at the university. One study of 23 schoolchildren substituted organic food for their conventional diets and found a dramatic drop in organophosphorus pesticide levels in their urine while eating organically, but not before or after (Environ. Health Perspect. 2006;114:260-3).
• Don’t microwave plastic. Taking that plastic tub of leftovers directly from the refrigerator to the microwave oven may be convenient, but it can contaminate your food with bisphenol A (BPA) or other endocrine disrupting chemicals that may be in the plastic container. Why does that matter? A growing number of studies suggest that fetal exposure to BPA increases the risks for multiple health problems.
One study of 244 mothers and their children showed that each 10-fold increase in maternal serum BPA levels was associated with more anxious and depressed behavior in the children by age 3 years (Pediatrics 2011;128:873-882). Another study in mice found that BPA may increase the risk for metabolic disorders and diabetes and that the fetal development stage was the critical window of susceptibility to BPA exposure (PLoS One 2013;8:e64143). Swedish investigators showed in a separate study that BPA increases angiogenesis in human endometrial cells in vitro, suggesting that the chemical could disturb normal endometrial functioning related to pregnancy and fertility.
• Avoid plastic contact with food/drinks. Plastic storage containers for food aren’t the only problem. Even without heating in a microwave, plastic can leach BPA or other endocrine-disrupting chemicals into your food or drinks. And plastic is ubiquitous – it’s in the linings of most canned foods, in polycarbonate water bottles, and in the plastic pouches or soft-box linings of wet foods. Try to avoid any food item with substantial plastic content.
• Don’t accept the receipt. Carbonless receipts – the kind you get at the ATM or in any store where you pay by credit card – commonly contain BPA, phthalates, or other endocrine disruptors. In response to concerns about BPA, some stores have started to use BPA-free receipts, "but many times when the BPA is removed, another phthalate gets added, so don’t even take the receipts," Dr. Zlatnik advised. Workers who have to handle carbonless receipts should wear gloves and/or wash their hands frequently, she added.
• Limit pesticide use around the home. A good principle in general, this is especially important during pregnancy.
• Be thoughtful about personal care products. Cosmetics and other personal care products can contain BPA or other endocrine disruptors. Skip the lipstick during pregnancy if you can’t verify that it’s free of harmful chemicals, for example.
• Mop daily. Dust mopping or damp mopping to remove dust that may contain lead or potentially harmful chemicals. "Along those lines, don’t wear shoes in the house," because they track these substances into the home, Dr. Zlatnik said.
• Replace foam furniture. Ubiquitous laws require furniture or mattresses containing foam to be treated with flame-retardant chemicals to reduce fire risk, but now it’s becoming clear that polybrominated diphenyl ethers (PBDEs) in the those chemicals can pose health risks.
Maternal prenatal PBDE concentrations were associated with impaired attention in children at age 5 years, poorer fine-motor coordination at ages 5 and 7 years, and lower scores on some sections of IQ tests at age 7 years in a study of 323 mothers and children (Environ. Health Perspect. 2013;121:257-62). A separate study of 210 cord blood samples found lower scores on tests of mental and physical development (including IQ) at 12-72 months of age in children who had higher concentrations of PBDEs at birth (Environ. Health Perspect. 2010;118:712-9). Serum levels of PBDE in the second trimester of pregnancy were associated with thyroid-stimulating hormone levels in a study of 25 pregnant Californians (Environ. Sci. Technol. 2011;45:7896-905).
• Quit smoking. Avoid second-hand smoke. Remind patients that toxins in cigarette smoke increase the risk for miscarriage, infertility, and preterm birth, among other problems.
• Avoid lead. This can be simple and inexpensive, such as dust mopping daily and avoiding lead-containing lipsticks, or complicated and expensive, such as staying away from jobs or hobbies with exposure to lead, or lead paint–abatement remedies. Women with a history of lead exposure can take calcium supplements to minimize the release of lead stored in bone.
"This is not a comprehensive list, but these are some relatively simple things to do" to avoid troublesome environmental chemicals during pregnancy, Dr. Zlatnik said.
She reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Pregnant women, more than anyone, face a challenge that Rachel Carson described in her 1962 book "Silent Spring": "What we have to face is not an occasional dose of poison which has accidentally got into some article of food, but a persistent and continuous poisoning of the whole human environment."
Modern science suggests that this is truer than ever, and that the danger especially applies to fetuses, Dr. Marya G. Zlatnik said.
One study reported that 43 of 163 (26%) unwanted chemicals could be detected in 99% of pregnant women in the United States, even though some chemicals had been banned for years (Environ. Health Perspect. 2011;119:878-85).
What’s a woman – and her physician – to do? Physicians can recommend 10 relatively simple steps that their pregnant patients can take today to protect themselves and their babies, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
• Buy organic. It’s not cheap, but buying organic foods such as fruit and produce make a big difference in reducing exposure to pesticides, said Dr. Zlatnik, a high-risk ob.gyn. and perinatologist at the university. One study of 23 schoolchildren substituted organic food for their conventional diets and found a dramatic drop in organophosphorus pesticide levels in their urine while eating organically, but not before or after (Environ. Health Perspect. 2006;114:260-3).
• Don’t microwave plastic. Taking that plastic tub of leftovers directly from the refrigerator to the microwave oven may be convenient, but it can contaminate your food with bisphenol A (BPA) or other endocrine disrupting chemicals that may be in the plastic container. Why does that matter? A growing number of studies suggest that fetal exposure to BPA increases the risks for multiple health problems.
One study of 244 mothers and their children showed that each 10-fold increase in maternal serum BPA levels was associated with more anxious and depressed behavior in the children by age 3 years (Pediatrics 2011;128:873-882). Another study in mice found that BPA may increase the risk for metabolic disorders and diabetes and that the fetal development stage was the critical window of susceptibility to BPA exposure (PLoS One 2013;8:e64143). Swedish investigators showed in a separate study that BPA increases angiogenesis in human endometrial cells in vitro, suggesting that the chemical could disturb normal endometrial functioning related to pregnancy and fertility.
• Avoid plastic contact with food/drinks. Plastic storage containers for food aren’t the only problem. Even without heating in a microwave, plastic can leach BPA or other endocrine-disrupting chemicals into your food or drinks. And plastic is ubiquitous – it’s in the linings of most canned foods, in polycarbonate water bottles, and in the plastic pouches or soft-box linings of wet foods. Try to avoid any food item with substantial plastic content.
• Don’t accept the receipt. Carbonless receipts – the kind you get at the ATM or in any store where you pay by credit card – commonly contain BPA, phthalates, or other endocrine disruptors. In response to concerns about BPA, some stores have started to use BPA-free receipts, "but many times when the BPA is removed, another phthalate gets added, so don’t even take the receipts," Dr. Zlatnik advised. Workers who have to handle carbonless receipts should wear gloves and/or wash their hands frequently, she added.
• Limit pesticide use around the home. A good principle in general, this is especially important during pregnancy.
• Be thoughtful about personal care products. Cosmetics and other personal care products can contain BPA or other endocrine disruptors. Skip the lipstick during pregnancy if you can’t verify that it’s free of harmful chemicals, for example.
• Mop daily. Dust mopping or damp mopping to remove dust that may contain lead or potentially harmful chemicals. "Along those lines, don’t wear shoes in the house," because they track these substances into the home, Dr. Zlatnik said.
• Replace foam furniture. Ubiquitous laws require furniture or mattresses containing foam to be treated with flame-retardant chemicals to reduce fire risk, but now it’s becoming clear that polybrominated diphenyl ethers (PBDEs) in the those chemicals can pose health risks.
Maternal prenatal PBDE concentrations were associated with impaired attention in children at age 5 years, poorer fine-motor coordination at ages 5 and 7 years, and lower scores on some sections of IQ tests at age 7 years in a study of 323 mothers and children (Environ. Health Perspect. 2013;121:257-62). A separate study of 210 cord blood samples found lower scores on tests of mental and physical development (including IQ) at 12-72 months of age in children who had higher concentrations of PBDEs at birth (Environ. Health Perspect. 2010;118:712-9). Serum levels of PBDE in the second trimester of pregnancy were associated with thyroid-stimulating hormone levels in a study of 25 pregnant Californians (Environ. Sci. Technol. 2011;45:7896-905).
• Quit smoking. Avoid second-hand smoke. Remind patients that toxins in cigarette smoke increase the risk for miscarriage, infertility, and preterm birth, among other problems.
• Avoid lead. This can be simple and inexpensive, such as dust mopping daily and avoiding lead-containing lipsticks, or complicated and expensive, such as staying away from jobs or hobbies with exposure to lead, or lead paint–abatement remedies. Women with a history of lead exposure can take calcium supplements to minimize the release of lead stored in bone.
"This is not a comprehensive list, but these are some relatively simple things to do" to avoid troublesome environmental chemicals during pregnancy, Dr. Zlatnik said.
She reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Ask pregnant patients about alternative products, practices
SAN FRANCISCO – Only 29% of pregnant women who were taking complementary and alternative medication products, such as dietary supplements, had discussed them with their doctor, judging from the findings of one recent study of 500 patients.
"This is really important. We should talk to our patients about their use of integrative medicine," Margaret A. Chesney, Ph.D. said.
The safety of most complementary and alternative medication (CAM) products on the market is assumed, not proved. The products are not standardized, their labeling may not be accurate, and some products are contaminated, particularly dietary supplement products from China, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The study found that 28% of 250 obstetric patients in a faculty-led practice and 9% of 250 obstetric patients in a resident-led practice were using CAM products. Of the women using the products, 29% said they had spoken with their health care provider about their use (J. Reprod. Med. 2012;57:390-6). Older women and whites were more likely to use CAM products, which may be related to socioeconomic status, said Dr. Chesney, director of the university’s Osher Center for Integrative Medicine.
Published studies of the utility of CAM during pregnancy are few and preliminary, but their findings suggest that ginger may help nausea in pregnancy, yoga might help reduce pain and discomfort, and mindfulness-based stress reduction techniques could reduce pregnancy-related anxiety and depression. Acupuncture, on the other hand, did not seem to help with infertility, and there’s no evidence to support claims of it helping labor pain, she said.
Ginger was effective as vitamin B6 in reducing first-trimester nausea, retching, and vomiting in a randomized, controlled trial involving 291 patients who were less than 16-weeks pregnant. The women took either 350 mg ginger or 25 mg vitamin B6 three times per day for 3 weeks. Nausea and vomiting were assessed at 7, 14, and 21 days (Obstet. Gynecol. 103:639-45). The investigators made their own ginger pills by loading capsules with crystallized ginger, Dr. Chesney noted.
The findings need to be replicated, "but there are not a lot of bad side effects from ginger, so it’s something to consider" for patients experiencing nausea in pregnancy, she said.
A review of three poorly designed randomized, controlled trials of yoga in 298 pregnancy women suggests that yoga might significantly reduce pain, discomfort, and perceived stress and improve scores for physical domain in quality of life measures during pregnancy, but the studies’ designs did not meet guidelines from the Consolidated Standard of Reporting Trials.
Despite claims that acupuncture can help improve fertility, there was no difference in pregnancy rates in 160 women who were undergoing in vitro fertilization who were randomized to treatment with acupuncture or a sham procedure, a randomized, double-blind study found (Fertil. Steril. 2011;95:583-7). No good evidence is available to support separate claims that acupuncture can reduce labor pain, Dr. Chesney added.
A pilot study of 27 pregnant women who participated in nine weekly classes and a retreat to learn mindfulness-based stress reduction techniques found that their scores for mindfulness and positive affect significantly increased, with decreases in scores for pregnancy anxiety, depression, and negative affect at the end of the trial compared with the start (J. Child Fam. Stud. 2010;19:190-202).
That preliminary evidence was good enough that the National Institutes of Health are funding a larger study of mindfulness-based stress reduction in pregnancy, she said.
Dr. Chesney reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Only 29% of pregnant women who were taking complementary and alternative medication products, such as dietary supplements, had discussed them with their doctor, judging from the findings of one recent study of 500 patients.
"This is really important. We should talk to our patients about their use of integrative medicine," Margaret A. Chesney, Ph.D. said.
The safety of most complementary and alternative medication (CAM) products on the market is assumed, not proved. The products are not standardized, their labeling may not be accurate, and some products are contaminated, particularly dietary supplement products from China, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The study found that 28% of 250 obstetric patients in a faculty-led practice and 9% of 250 obstetric patients in a resident-led practice were using CAM products. Of the women using the products, 29% said they had spoken with their health care provider about their use (J. Reprod. Med. 2012;57:390-6). Older women and whites were more likely to use CAM products, which may be related to socioeconomic status, said Dr. Chesney, director of the university’s Osher Center for Integrative Medicine.
Published studies of the utility of CAM during pregnancy are few and preliminary, but their findings suggest that ginger may help nausea in pregnancy, yoga might help reduce pain and discomfort, and mindfulness-based stress reduction techniques could reduce pregnancy-related anxiety and depression. Acupuncture, on the other hand, did not seem to help with infertility, and there’s no evidence to support claims of it helping labor pain, she said.
Ginger was effective as vitamin B6 in reducing first-trimester nausea, retching, and vomiting in a randomized, controlled trial involving 291 patients who were less than 16-weeks pregnant. The women took either 350 mg ginger or 25 mg vitamin B6 three times per day for 3 weeks. Nausea and vomiting were assessed at 7, 14, and 21 days (Obstet. Gynecol. 103:639-45). The investigators made their own ginger pills by loading capsules with crystallized ginger, Dr. Chesney noted.
The findings need to be replicated, "but there are not a lot of bad side effects from ginger, so it’s something to consider" for patients experiencing nausea in pregnancy, she said.
A review of three poorly designed randomized, controlled trials of yoga in 298 pregnancy women suggests that yoga might significantly reduce pain, discomfort, and perceived stress and improve scores for physical domain in quality of life measures during pregnancy, but the studies’ designs did not meet guidelines from the Consolidated Standard of Reporting Trials.
Despite claims that acupuncture can help improve fertility, there was no difference in pregnancy rates in 160 women who were undergoing in vitro fertilization who were randomized to treatment with acupuncture or a sham procedure, a randomized, double-blind study found (Fertil. Steril. 2011;95:583-7). No good evidence is available to support separate claims that acupuncture can reduce labor pain, Dr. Chesney added.
A pilot study of 27 pregnant women who participated in nine weekly classes and a retreat to learn mindfulness-based stress reduction techniques found that their scores for mindfulness and positive affect significantly increased, with decreases in scores for pregnancy anxiety, depression, and negative affect at the end of the trial compared with the start (J. Child Fam. Stud. 2010;19:190-202).
That preliminary evidence was good enough that the National Institutes of Health are funding a larger study of mindfulness-based stress reduction in pregnancy, she said.
Dr. Chesney reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Only 29% of pregnant women who were taking complementary and alternative medication products, such as dietary supplements, had discussed them with their doctor, judging from the findings of one recent study of 500 patients.
"This is really important. We should talk to our patients about their use of integrative medicine," Margaret A. Chesney, Ph.D. said.
The safety of most complementary and alternative medication (CAM) products on the market is assumed, not proved. The products are not standardized, their labeling may not be accurate, and some products are contaminated, particularly dietary supplement products from China, she said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The study found that 28% of 250 obstetric patients in a faculty-led practice and 9% of 250 obstetric patients in a resident-led practice were using CAM products. Of the women using the products, 29% said they had spoken with their health care provider about their use (J. Reprod. Med. 2012;57:390-6). Older women and whites were more likely to use CAM products, which may be related to socioeconomic status, said Dr. Chesney, director of the university’s Osher Center for Integrative Medicine.
Published studies of the utility of CAM during pregnancy are few and preliminary, but their findings suggest that ginger may help nausea in pregnancy, yoga might help reduce pain and discomfort, and mindfulness-based stress reduction techniques could reduce pregnancy-related anxiety and depression. Acupuncture, on the other hand, did not seem to help with infertility, and there’s no evidence to support claims of it helping labor pain, she said.
Ginger was effective as vitamin B6 in reducing first-trimester nausea, retching, and vomiting in a randomized, controlled trial involving 291 patients who were less than 16-weeks pregnant. The women took either 350 mg ginger or 25 mg vitamin B6 three times per day for 3 weeks. Nausea and vomiting were assessed at 7, 14, and 21 days (Obstet. Gynecol. 103:639-45). The investigators made their own ginger pills by loading capsules with crystallized ginger, Dr. Chesney noted.
The findings need to be replicated, "but there are not a lot of bad side effects from ginger, so it’s something to consider" for patients experiencing nausea in pregnancy, she said.
A review of three poorly designed randomized, controlled trials of yoga in 298 pregnancy women suggests that yoga might significantly reduce pain, discomfort, and perceived stress and improve scores for physical domain in quality of life measures during pregnancy, but the studies’ designs did not meet guidelines from the Consolidated Standard of Reporting Trials.
Despite claims that acupuncture can help improve fertility, there was no difference in pregnancy rates in 160 women who were undergoing in vitro fertilization who were randomized to treatment with acupuncture or a sham procedure, a randomized, double-blind study found (Fertil. Steril. 2011;95:583-7). No good evidence is available to support separate claims that acupuncture can reduce labor pain, Dr. Chesney added.
A pilot study of 27 pregnant women who participated in nine weekly classes and a retreat to learn mindfulness-based stress reduction techniques found that their scores for mindfulness and positive affect significantly increased, with decreases in scores for pregnancy anxiety, depression, and negative affect at the end of the trial compared with the start (J. Child Fam. Stud. 2010;19:190-202).
That preliminary evidence was good enough that the National Institutes of Health are funding a larger study of mindfulness-based stress reduction in pregnancy, she said.
Dr. Chesney reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT
Maternal safety blueprint outlined
SAN FRANCISCO – Every birthing facility in the United States should have specific practices and equipment to optimize maternal safety in pregnancy, according to a recent consensus meeting of national medical organizations.
These include so-called "safety bundles," or safety initiatives, of protocols and equipment for preventing and managing obstetric hemorrhage, venous thromboembolism, and severe hypertension, as well as for supporting patients, families, and staff. Specific early-warning criteria should trigger a maternal evaluation, and facilities should regularly review severe maternal morbidity from a systems perspective.
Motivated by climbing maternal mortality rates in the United States in recent decades, the recommendations build on preliminary success from California efforts to improve maternal safety, said Dr. Elliott K. Main, who cochaired the "National Maternal Health Initiative: Strategies to Improve Maternal Health and Safety" consensus meeting in New Orleans in May 2013.
Maternal mortality rates declined in California since 1970, but started increasing again around 2000, so that by 2005, the rate of 17 maternal deaths/100,000 live births was similar to rates in the early 1970s. Nationally, U.S. maternal mortality rates increased from 1980 to 2008, in contrast with decreases in many other developed countries, he said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The U.S. rates of pregnancy-related deaths from hemorrhage or hypertensive disorders of pregnancy decreased from the periods of 1987-1990 to 1998-2005, but increased for deaths associated with cardiomyopathy or other cardiovascular conditions, one study showed (Obstet. Gynecol. 2010;116:1302-9). Other data suggest that hemorrhage and preeclampsia cause the lion’s share of morbidity.
The Joint Commission in 2010 issued Sentinel Alert #44 to suggest ways that birthing centers might better improve maternal morbidity and mortality, and Dr. Main directed ongoing work by the California Maternal Quality Care Collaborative (CMQCC) to identify and address common causes of pregnancy-related deaths that have a good chance of being altered to improve outcomes.Free "toolkits" of best practices with guidelines, protocols, sample policies, and more are available on the CMQCC website .
Representatives of more than 30 organizations participated in the May consensus meeting, including the American College of Obstetricians and Gynecologists (ACOG), the American Academy of Family Physicians, the Society for Maternal-Fetal Medicine, the American Hospital Association, the Centers for Disease Control and Prevention, and the Joint Commission.
Dr. Main, director of maternal-fetal medicine at California Pacific Medical Center, San Francisco, described some of the "safety bundles" that emerged from the consensus meeting and will be recommended nationally. "We’re not expecting you to implement all of these at once, but these are what you want to be working toward," he said.
• Hemorrhage: Be ready for obstetric hemorrhage by having a hemorrhage cart of equipment with instructions for newer procedures such as intrauterine balloons and compression sutures. Partner with your local blood bank to make sure that blood products at the right ratios are available rapidly and reliably, he said. Hold hemorrhage-response drills regularly with post-drill debriefs or "huddles." Ensure rapid availability of medications, establish easy availability of special care resources, and educate the unit staff about hemorrhage protocols.
To better recognize obstetric hemorrhage, assess a patient’s risk on admission and late in labor. Use the Early Warning Tool (see below) for vital signs and symptoms, and get semiquantitative assessments of cumulative blood loss, with the emphasis on cumulative, Dr. Main said.
Response to obstetric hemorrhage should rely on a protocol standardized for your unit with checklists. Universal use of active management in the third stage of labor is important for hemorrhage prevention. To promote learning, establish a culture of post-hemorrhage debrief/huddles, and review all serious cases for systems issues.
In an informal poll of the physicians and nurses in the audience, 58% said they have a comprehensive, standardized protocol for obstetric hemorrhage in their hospital, 23% have one that could be improved, 11% don’t have one, and 8% had no clue.
• Hypertension: Debate continues about the definition of severe preeclampsia, and ACOG should be issuing a presidential task force statement later this year on the topic, Dr. Main said.
Meanwhile, key elements of a "safety bundle" for hypertension in pregnancy include having unit-standard protocols and policies for the treatment of severe hypertension and eclampsia, safe use of magnesium therapy, and managing magnesium overdose, he said. The birthing unit also should have an agreed-upon definition of severe preeclampsia, early warning tools employing vital signs and symptoms, and regular review of all hypertension cases with severe morbidity to look for systems issues.
The CMQCC is expected soon to publish a California Preeclampsia QI Toolkit for quality improvement, which will be tested in 26 hospitals, he added.
A poll of the audience found that 31% have a comprehensive, standardized protocol for severe pregnancy hypertension in their hospital, 22% have one that could be improved, 35% don’t have one, and 11% had not a clue.(The percentages added up to 99% rather than 100% when the survey results were displayed at the meeting.)
• Thromboembolism: The keys to preventing venous thromboembolism are to have protocols for use of a sequential compression device, pharmacologic prophylaxis for higher-risk mothers, and antenatal prophylaxis, Dr. Main said.
A draft safety bundle for prevention of venous thromboembolism during cesarean section calls for applying a sequential compression device prior to delivery. Add chemoprophylaxis to all who already are receiving prophylaxis or full anticoagulation, patients with a history of thromboembolism who are not already on chemoprophylaxis, mothers with a family history of venous thromboembolism and any thrombophilia, mothers who are morbidly obese, or any patients with a score of two or more for other, more minor risk factors.
Obesity is "the big risk factor in California," he said. Two-thirds of pregnant Californians who die from thomboembolism have a body mass index greater then 40 kg/m2.
An unexpectedly high proportion of the audience – 29% said that their hospital has a standardized protocol for using Lovenox (enoxaparin) for obstetric patients at higher risk for venous thromboembolism. Few local hospitals will have such protocols, Dr. Main noted, and if they have them, they’re usually very complicated. Another 18% at the meeting said they have such a protocol but it could be improved; 38% said they don’t have a protocol, and 15% had no clue.
• Warnings: Draft criteria for an Early Warning Tool that should trigger an evaluation of maternal safety include specific vital signs and important symptoms. Troubling vital signs include a systolic blood pressure below 90 mm Hg or above 160 mm Hg; diastolic blood pressure higher than 100 mm Hg; sustained heart rate below 50 or above 120 beats per minute; respiratory rate slower than 10 or faster than 30 breaths/minute; oxygen saturation less than 95% room air (at sea level); or oliguria less than 30 mL/hour for 2 hours.
Among symptoms, maternal agitation, confusion or unresponsiveness often is a sign of low oxygen saturation, Dr. Main said. A patient with hypertension who reports an unremitting headache is a red flag. Shortness of breath in a patient with preeclampsia or hypertension should raise big concerns about the development of pulmonary edema and cardiovascular problems.
As a core safety principal, however, the bedside clinician should always feel comfortable escalating concern at any point, because these criteria can’t address all scenarios, he added. These warning criteria are being rolled out in New York State hospitals for a trial, he said.
• Cardiovascular: There are not enough data yet to identify opportunities for safety improvements related to cardiovascular or cardiomyopathy risks in pregnancy, so instead of a safety bundle Dr. Main presented three clinical pearls from California’s work on maternal safety.
Morbid obesity plus hypertension equals high risk for cardiomyopathy, especially if the patient is African American and older than 35 years, he said. There are not many pregnant women with known underlying cardiovascular disease, but this group should be followed closely by a multidisciplinary team, perhaps in a tertiary care center. The third pearl was new to Dr. Main: the onset of wheezing in the third trimester, which is not likely to be asthma but cardiac in origin and deserves a patient referral for evaluation.
Dr. Main reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Every birthing facility in the United States should have specific practices and equipment to optimize maternal safety in pregnancy, according to a recent consensus meeting of national medical organizations.
These include so-called "safety bundles," or safety initiatives, of protocols and equipment for preventing and managing obstetric hemorrhage, venous thromboembolism, and severe hypertension, as well as for supporting patients, families, and staff. Specific early-warning criteria should trigger a maternal evaluation, and facilities should regularly review severe maternal morbidity from a systems perspective.
Motivated by climbing maternal mortality rates in the United States in recent decades, the recommendations build on preliminary success from California efforts to improve maternal safety, said Dr. Elliott K. Main, who cochaired the "National Maternal Health Initiative: Strategies to Improve Maternal Health and Safety" consensus meeting in New Orleans in May 2013.
Maternal mortality rates declined in California since 1970, but started increasing again around 2000, so that by 2005, the rate of 17 maternal deaths/100,000 live births was similar to rates in the early 1970s. Nationally, U.S. maternal mortality rates increased from 1980 to 2008, in contrast with decreases in many other developed countries, he said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The U.S. rates of pregnancy-related deaths from hemorrhage or hypertensive disorders of pregnancy decreased from the periods of 1987-1990 to 1998-2005, but increased for deaths associated with cardiomyopathy or other cardiovascular conditions, one study showed (Obstet. Gynecol. 2010;116:1302-9). Other data suggest that hemorrhage and preeclampsia cause the lion’s share of morbidity.
The Joint Commission in 2010 issued Sentinel Alert #44 to suggest ways that birthing centers might better improve maternal morbidity and mortality, and Dr. Main directed ongoing work by the California Maternal Quality Care Collaborative (CMQCC) to identify and address common causes of pregnancy-related deaths that have a good chance of being altered to improve outcomes.Free "toolkits" of best practices with guidelines, protocols, sample policies, and more are available on the CMQCC website .
Representatives of more than 30 organizations participated in the May consensus meeting, including the American College of Obstetricians and Gynecologists (ACOG), the American Academy of Family Physicians, the Society for Maternal-Fetal Medicine, the American Hospital Association, the Centers for Disease Control and Prevention, and the Joint Commission.
Dr. Main, director of maternal-fetal medicine at California Pacific Medical Center, San Francisco, described some of the "safety bundles" that emerged from the consensus meeting and will be recommended nationally. "We’re not expecting you to implement all of these at once, but these are what you want to be working toward," he said.
• Hemorrhage: Be ready for obstetric hemorrhage by having a hemorrhage cart of equipment with instructions for newer procedures such as intrauterine balloons and compression sutures. Partner with your local blood bank to make sure that blood products at the right ratios are available rapidly and reliably, he said. Hold hemorrhage-response drills regularly with post-drill debriefs or "huddles." Ensure rapid availability of medications, establish easy availability of special care resources, and educate the unit staff about hemorrhage protocols.
To better recognize obstetric hemorrhage, assess a patient’s risk on admission and late in labor. Use the Early Warning Tool (see below) for vital signs and symptoms, and get semiquantitative assessments of cumulative blood loss, with the emphasis on cumulative, Dr. Main said.
Response to obstetric hemorrhage should rely on a protocol standardized for your unit with checklists. Universal use of active management in the third stage of labor is important for hemorrhage prevention. To promote learning, establish a culture of post-hemorrhage debrief/huddles, and review all serious cases for systems issues.
In an informal poll of the physicians and nurses in the audience, 58% said they have a comprehensive, standardized protocol for obstetric hemorrhage in their hospital, 23% have one that could be improved, 11% don’t have one, and 8% had no clue.
• Hypertension: Debate continues about the definition of severe preeclampsia, and ACOG should be issuing a presidential task force statement later this year on the topic, Dr. Main said.
Meanwhile, key elements of a "safety bundle" for hypertension in pregnancy include having unit-standard protocols and policies for the treatment of severe hypertension and eclampsia, safe use of magnesium therapy, and managing magnesium overdose, he said. The birthing unit also should have an agreed-upon definition of severe preeclampsia, early warning tools employing vital signs and symptoms, and regular review of all hypertension cases with severe morbidity to look for systems issues.
The CMQCC is expected soon to publish a California Preeclampsia QI Toolkit for quality improvement, which will be tested in 26 hospitals, he added.
A poll of the audience found that 31% have a comprehensive, standardized protocol for severe pregnancy hypertension in their hospital, 22% have one that could be improved, 35% don’t have one, and 11% had not a clue.(The percentages added up to 99% rather than 100% when the survey results were displayed at the meeting.)
• Thromboembolism: The keys to preventing venous thromboembolism are to have protocols for use of a sequential compression device, pharmacologic prophylaxis for higher-risk mothers, and antenatal prophylaxis, Dr. Main said.
A draft safety bundle for prevention of venous thromboembolism during cesarean section calls for applying a sequential compression device prior to delivery. Add chemoprophylaxis to all who already are receiving prophylaxis or full anticoagulation, patients with a history of thromboembolism who are not already on chemoprophylaxis, mothers with a family history of venous thromboembolism and any thrombophilia, mothers who are morbidly obese, or any patients with a score of two or more for other, more minor risk factors.
Obesity is "the big risk factor in California," he said. Two-thirds of pregnant Californians who die from thomboembolism have a body mass index greater then 40 kg/m2.
An unexpectedly high proportion of the audience – 29% said that their hospital has a standardized protocol for using Lovenox (enoxaparin) for obstetric patients at higher risk for venous thromboembolism. Few local hospitals will have such protocols, Dr. Main noted, and if they have them, they’re usually very complicated. Another 18% at the meeting said they have such a protocol but it could be improved; 38% said they don’t have a protocol, and 15% had no clue.
• Warnings: Draft criteria for an Early Warning Tool that should trigger an evaluation of maternal safety include specific vital signs and important symptoms. Troubling vital signs include a systolic blood pressure below 90 mm Hg or above 160 mm Hg; diastolic blood pressure higher than 100 mm Hg; sustained heart rate below 50 or above 120 beats per minute; respiratory rate slower than 10 or faster than 30 breaths/minute; oxygen saturation less than 95% room air (at sea level); or oliguria less than 30 mL/hour for 2 hours.
Among symptoms, maternal agitation, confusion or unresponsiveness often is a sign of low oxygen saturation, Dr. Main said. A patient with hypertension who reports an unremitting headache is a red flag. Shortness of breath in a patient with preeclampsia or hypertension should raise big concerns about the development of pulmonary edema and cardiovascular problems.
As a core safety principal, however, the bedside clinician should always feel comfortable escalating concern at any point, because these criteria can’t address all scenarios, he added. These warning criteria are being rolled out in New York State hospitals for a trial, he said.
• Cardiovascular: There are not enough data yet to identify opportunities for safety improvements related to cardiovascular or cardiomyopathy risks in pregnancy, so instead of a safety bundle Dr. Main presented three clinical pearls from California’s work on maternal safety.
Morbid obesity plus hypertension equals high risk for cardiomyopathy, especially if the patient is African American and older than 35 years, he said. There are not many pregnant women with known underlying cardiovascular disease, but this group should be followed closely by a multidisciplinary team, perhaps in a tertiary care center. The third pearl was new to Dr. Main: the onset of wheezing in the third trimester, which is not likely to be asthma but cardiac in origin and deserves a patient referral for evaluation.
Dr. Main reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Every birthing facility in the United States should have specific practices and equipment to optimize maternal safety in pregnancy, according to a recent consensus meeting of national medical organizations.
These include so-called "safety bundles," or safety initiatives, of protocols and equipment for preventing and managing obstetric hemorrhage, venous thromboembolism, and severe hypertension, as well as for supporting patients, families, and staff. Specific early-warning criteria should trigger a maternal evaluation, and facilities should regularly review severe maternal morbidity from a systems perspective.
Motivated by climbing maternal mortality rates in the United States in recent decades, the recommendations build on preliminary success from California efforts to improve maternal safety, said Dr. Elliott K. Main, who cochaired the "National Maternal Health Initiative: Strategies to Improve Maternal Health and Safety" consensus meeting in New Orleans in May 2013.
Maternal mortality rates declined in California since 1970, but started increasing again around 2000, so that by 2005, the rate of 17 maternal deaths/100,000 live births was similar to rates in the early 1970s. Nationally, U.S. maternal mortality rates increased from 1980 to 2008, in contrast with decreases in many other developed countries, he said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
The U.S. rates of pregnancy-related deaths from hemorrhage or hypertensive disorders of pregnancy decreased from the periods of 1987-1990 to 1998-2005, but increased for deaths associated with cardiomyopathy or other cardiovascular conditions, one study showed (Obstet. Gynecol. 2010;116:1302-9). Other data suggest that hemorrhage and preeclampsia cause the lion’s share of morbidity.
The Joint Commission in 2010 issued Sentinel Alert #44 to suggest ways that birthing centers might better improve maternal morbidity and mortality, and Dr. Main directed ongoing work by the California Maternal Quality Care Collaborative (CMQCC) to identify and address common causes of pregnancy-related deaths that have a good chance of being altered to improve outcomes.Free "toolkits" of best practices with guidelines, protocols, sample policies, and more are available on the CMQCC website .
Representatives of more than 30 organizations participated in the May consensus meeting, including the American College of Obstetricians and Gynecologists (ACOG), the American Academy of Family Physicians, the Society for Maternal-Fetal Medicine, the American Hospital Association, the Centers for Disease Control and Prevention, and the Joint Commission.
Dr. Main, director of maternal-fetal medicine at California Pacific Medical Center, San Francisco, described some of the "safety bundles" that emerged from the consensus meeting and will be recommended nationally. "We’re not expecting you to implement all of these at once, but these are what you want to be working toward," he said.
• Hemorrhage: Be ready for obstetric hemorrhage by having a hemorrhage cart of equipment with instructions for newer procedures such as intrauterine balloons and compression sutures. Partner with your local blood bank to make sure that blood products at the right ratios are available rapidly and reliably, he said. Hold hemorrhage-response drills regularly with post-drill debriefs or "huddles." Ensure rapid availability of medications, establish easy availability of special care resources, and educate the unit staff about hemorrhage protocols.
To better recognize obstetric hemorrhage, assess a patient’s risk on admission and late in labor. Use the Early Warning Tool (see below) for vital signs and symptoms, and get semiquantitative assessments of cumulative blood loss, with the emphasis on cumulative, Dr. Main said.
Response to obstetric hemorrhage should rely on a protocol standardized for your unit with checklists. Universal use of active management in the third stage of labor is important for hemorrhage prevention. To promote learning, establish a culture of post-hemorrhage debrief/huddles, and review all serious cases for systems issues.
In an informal poll of the physicians and nurses in the audience, 58% said they have a comprehensive, standardized protocol for obstetric hemorrhage in their hospital, 23% have one that could be improved, 11% don’t have one, and 8% had no clue.
• Hypertension: Debate continues about the definition of severe preeclampsia, and ACOG should be issuing a presidential task force statement later this year on the topic, Dr. Main said.
Meanwhile, key elements of a "safety bundle" for hypertension in pregnancy include having unit-standard protocols and policies for the treatment of severe hypertension and eclampsia, safe use of magnesium therapy, and managing magnesium overdose, he said. The birthing unit also should have an agreed-upon definition of severe preeclampsia, early warning tools employing vital signs and symptoms, and regular review of all hypertension cases with severe morbidity to look for systems issues.
The CMQCC is expected soon to publish a California Preeclampsia QI Toolkit for quality improvement, which will be tested in 26 hospitals, he added.
A poll of the audience found that 31% have a comprehensive, standardized protocol for severe pregnancy hypertension in their hospital, 22% have one that could be improved, 35% don’t have one, and 11% had not a clue.(The percentages added up to 99% rather than 100% when the survey results were displayed at the meeting.)
• Thromboembolism: The keys to preventing venous thromboembolism are to have protocols for use of a sequential compression device, pharmacologic prophylaxis for higher-risk mothers, and antenatal prophylaxis, Dr. Main said.
A draft safety bundle for prevention of venous thromboembolism during cesarean section calls for applying a sequential compression device prior to delivery. Add chemoprophylaxis to all who already are receiving prophylaxis or full anticoagulation, patients with a history of thromboembolism who are not already on chemoprophylaxis, mothers with a family history of venous thromboembolism and any thrombophilia, mothers who are morbidly obese, or any patients with a score of two or more for other, more minor risk factors.
Obesity is "the big risk factor in California," he said. Two-thirds of pregnant Californians who die from thomboembolism have a body mass index greater then 40 kg/m2.
An unexpectedly high proportion of the audience – 29% said that their hospital has a standardized protocol for using Lovenox (enoxaparin) for obstetric patients at higher risk for venous thromboembolism. Few local hospitals will have such protocols, Dr. Main noted, and if they have them, they’re usually very complicated. Another 18% at the meeting said they have such a protocol but it could be improved; 38% said they don’t have a protocol, and 15% had no clue.
• Warnings: Draft criteria for an Early Warning Tool that should trigger an evaluation of maternal safety include specific vital signs and important symptoms. Troubling vital signs include a systolic blood pressure below 90 mm Hg or above 160 mm Hg; diastolic blood pressure higher than 100 mm Hg; sustained heart rate below 50 or above 120 beats per minute; respiratory rate slower than 10 or faster than 30 breaths/minute; oxygen saturation less than 95% room air (at sea level); or oliguria less than 30 mL/hour for 2 hours.
Among symptoms, maternal agitation, confusion or unresponsiveness often is a sign of low oxygen saturation, Dr. Main said. A patient with hypertension who reports an unremitting headache is a red flag. Shortness of breath in a patient with preeclampsia or hypertension should raise big concerns about the development of pulmonary edema and cardiovascular problems.
As a core safety principal, however, the bedside clinician should always feel comfortable escalating concern at any point, because these criteria can’t address all scenarios, he added. These warning criteria are being rolled out in New York State hospitals for a trial, he said.
• Cardiovascular: There are not enough data yet to identify opportunities for safety improvements related to cardiovascular or cardiomyopathy risks in pregnancy, so instead of a safety bundle Dr. Main presented three clinical pearls from California’s work on maternal safety.
Morbid obesity plus hypertension equals high risk for cardiomyopathy, especially if the patient is African American and older than 35 years, he said. There are not many pregnant women with known underlying cardiovascular disease, but this group should be followed closely by a multidisciplinary team, perhaps in a tertiary care center. The third pearl was new to Dr. Main: the onset of wheezing in the third trimester, which is not likely to be asthma but cardiac in origin and deserves a patient referral for evaluation.
Dr. Main reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS AT A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT