User login
Society of Hospital Medicine (SHM): Pediatric Hospital Medicine 2014
Clinics, EDs miss many flu vaccination opportunities
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to a chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote. Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.

|
|
Dr. Burt Lesnick, FCCP, comments: The federally funded Vaccine for Children program provides free influenza vaccine in most states. However, many states require that a specialist take shipment and administer all the childhood vaccines offered in order to get the influenza vaccine. Such roadblocks are common and need to be removed if we are to achieve our goal of universal pediatric influenza vaccination. Among elderly individuals most at risk, the evolving concept of a medical home should support vaccination. However, if primary care physicians believe that specialists giving influenza vaccine undercuts the medical home concept, then the patient loses. A medical home with a good medical neighbor may be the best combination."
Burt Lesnick, M.D., FCCP, is currently a practicing pediatric pulmonologist in Atlanta, Georgia, where he is the assistant managing partner of Georgia Pediatric Pulmonology Associates, a group of 14 pediatric pulmonologists. He also serves as President of the Medical Staff for Children's Healthcare of Atlanta.

|
|
Dr. Burt Lesnick, FCCP, comments: The federally funded Vaccine for Children program provides free influenza vaccine in most states. However, many states require that a specialist take shipment and administer all the childhood vaccines offered in order to get the influenza vaccine. Such roadblocks are common and need to be removed if we are to achieve our goal of universal pediatric influenza vaccination. Among elderly individuals most at risk, the evolving concept of a medical home should support vaccination. However, if primary care physicians believe that specialists giving influenza vaccine undercuts the medical home concept, then the patient loses. A medical home with a good medical neighbor may be the best combination."
Burt Lesnick, M.D., FCCP, is currently a practicing pediatric pulmonologist in Atlanta, Georgia, where he is the assistant managing partner of Georgia Pediatric Pulmonology Associates, a group of 14 pediatric pulmonologists. He also serves as President of the Medical Staff for Children's Healthcare of Atlanta.

|
|
Dr. Burt Lesnick, FCCP, comments: The federally funded Vaccine for Children program provides free influenza vaccine in most states. However, many states require that a specialist take shipment and administer all the childhood vaccines offered in order to get the influenza vaccine. Such roadblocks are common and need to be removed if we are to achieve our goal of universal pediatric influenza vaccination. Among elderly individuals most at risk, the evolving concept of a medical home should support vaccination. However, if primary care physicians believe that specialists giving influenza vaccine undercuts the medical home concept, then the patient loses. A medical home with a good medical neighbor may be the best combination."
Burt Lesnick, M.D., FCCP, is currently a practicing pediatric pulmonologist in Atlanta, Georgia, where he is the assistant managing partner of Georgia Pediatric Pulmonology Associates, a group of 14 pediatric pulmonologists. He also serves as President of the Medical Staff for Children's Healthcare of Atlanta.
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to a chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote. Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to a chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote. Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.
Key clinical point: Specialty outpatient visits offer an important opportunity for influenza vaccinations.
Major finding: A total of 44% of 197 patients had a total of 507 missed opportunities for vaccination.
Data source: A review of the charts of 197 incompletely vaccinated children with the flu.
Disclosures: The investigators reported having no relevant financial disclosures.
Palliative care consultations linked to reduced hospitalization, ED care
LAKE BUENA VISTA, FLA. – Palliative care consultations were linked to decreases in hospitalizations and hospital days, as well as emergency department visits, among pediatric patients with life-threatening or terminal conditions, according to a retrospective chart review at a large children’s hospital.
The 36 patients in the study – patients at Rady Children’s Hospital–San Diego, ranged in age from 1 to 24 years; most had a neurological diagnosis and none had cancer. The Pediatric Advanced Care Team (PACT) services at the hospital include consultations with patients and their families to clarify goals of care, which are then used to determine treatment options and to define limits of therapy.
In 2009, the year prior to implementation of PACT, the 36 patients had 121 hospitalizations; in the year after their PACT consultations, the patients had 61 hospitalizations, Dr. Ami Doshi reported at the Pediatric Hospital Medicine 2014 annual meeting.
Emergency department visits decreased from 100 before PACT consultation to 84 after consultation. Total hospital days exceeded 1,100 days in the year before PACT consultation compared with 684 days after consultation. Length of stay decreased significantly from 31 days to 19 days, said Dr. Doshi, a pediatrician at Rady and a PACT member.
Because of the small sample size, the findings require replication in a larger study, she said. It would be worthwhile to redo the study with cost information included.
"We cannot directly attribute the decrease in utilization to PACT intervention as a direct cause-effect relationship. Doing the study again and comparing patients with the same diagnosis who did and did not receive palliative care would eliminate some potentially confounding variables," she added, noting that it would be useful to look at ambulatory and outpatient data to see if these offset any of the inpatient findings.
As hospitals will now be negotiating for a set payment to manage each patient regardless of the setting, hospitals will be motivated to move care, resources, and the associated dollars from the inpatient to the less costly outpatient setting, Dr. Doshi said. "These data suggest that palliative care can be a prime change agent in that shift. Most importantly, it’s great that palliative care can decrease utilization, but palliative care is really, truly unique in that it can do so while simultaneously improving quality of life and improving patient and family satisfaction."
Dr. Doshi reported having no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
LAKE BUENA VISTA, FLA. – Palliative care consultations were linked to decreases in hospitalizations and hospital days, as well as emergency department visits, among pediatric patients with life-threatening or terminal conditions, according to a retrospective chart review at a large children’s hospital.
The 36 patients in the study – patients at Rady Children’s Hospital–San Diego, ranged in age from 1 to 24 years; most had a neurological diagnosis and none had cancer. The Pediatric Advanced Care Team (PACT) services at the hospital include consultations with patients and their families to clarify goals of care, which are then used to determine treatment options and to define limits of therapy.
In 2009, the year prior to implementation of PACT, the 36 patients had 121 hospitalizations; in the year after their PACT consultations, the patients had 61 hospitalizations, Dr. Ami Doshi reported at the Pediatric Hospital Medicine 2014 annual meeting.
Emergency department visits decreased from 100 before PACT consultation to 84 after consultation. Total hospital days exceeded 1,100 days in the year before PACT consultation compared with 684 days after consultation. Length of stay decreased significantly from 31 days to 19 days, said Dr. Doshi, a pediatrician at Rady and a PACT member.
Because of the small sample size, the findings require replication in a larger study, she said. It would be worthwhile to redo the study with cost information included.
"We cannot directly attribute the decrease in utilization to PACT intervention as a direct cause-effect relationship. Doing the study again and comparing patients with the same diagnosis who did and did not receive palliative care would eliminate some potentially confounding variables," she added, noting that it would be useful to look at ambulatory and outpatient data to see if these offset any of the inpatient findings.
As hospitals will now be negotiating for a set payment to manage each patient regardless of the setting, hospitals will be motivated to move care, resources, and the associated dollars from the inpatient to the less costly outpatient setting, Dr. Doshi said. "These data suggest that palliative care can be a prime change agent in that shift. Most importantly, it’s great that palliative care can decrease utilization, but palliative care is really, truly unique in that it can do so while simultaneously improving quality of life and improving patient and family satisfaction."
Dr. Doshi reported having no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
LAKE BUENA VISTA, FLA. – Palliative care consultations were linked to decreases in hospitalizations and hospital days, as well as emergency department visits, among pediatric patients with life-threatening or terminal conditions, according to a retrospective chart review at a large children’s hospital.
The 36 patients in the study – patients at Rady Children’s Hospital–San Diego, ranged in age from 1 to 24 years; most had a neurological diagnosis and none had cancer. The Pediatric Advanced Care Team (PACT) services at the hospital include consultations with patients and their families to clarify goals of care, which are then used to determine treatment options and to define limits of therapy.
In 2009, the year prior to implementation of PACT, the 36 patients had 121 hospitalizations; in the year after their PACT consultations, the patients had 61 hospitalizations, Dr. Ami Doshi reported at the Pediatric Hospital Medicine 2014 annual meeting.
Emergency department visits decreased from 100 before PACT consultation to 84 after consultation. Total hospital days exceeded 1,100 days in the year before PACT consultation compared with 684 days after consultation. Length of stay decreased significantly from 31 days to 19 days, said Dr. Doshi, a pediatrician at Rady and a PACT member.
Because of the small sample size, the findings require replication in a larger study, she said. It would be worthwhile to redo the study with cost information included.
"We cannot directly attribute the decrease in utilization to PACT intervention as a direct cause-effect relationship. Doing the study again and comparing patients with the same diagnosis who did and did not receive palliative care would eliminate some potentially confounding variables," she added, noting that it would be useful to look at ambulatory and outpatient data to see if these offset any of the inpatient findings.
As hospitals will now be negotiating for a set payment to manage each patient regardless of the setting, hospitals will be motivated to move care, resources, and the associated dollars from the inpatient to the less costly outpatient setting, Dr. Doshi said. "These data suggest that palliative care can be a prime change agent in that shift. Most importantly, it’s great that palliative care can decrease utilization, but palliative care is really, truly unique in that it can do so while simultaneously improving quality of life and improving patient and family satisfaction."
Dr. Doshi reported having no disclosures. The meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical point: Palliative care consultations can reduce inpatient and emergency department care.
Major finding: Palliative care consultation was associated with a 50% decrease in hospitalizations.
Data source: A retrospective review of 36 patient charts.
Disclosures: Dr. Doshi reported having no disclosures.
Attention to risk factors could reduce CAP-related emergency revisits
LAKE BUENA VISTA, FLA. – Fever or lack of an antibiotic prescription are two factors that increase the risk of a return visit to the emergency department and subsequent hospital admission in children with community-acquired pneumonia, according to a review of ED medical records.
Of 1,857 children aged 3 months to 18 years with a diagnosis of pneumonia who were discharged to home after the index ED visit between November 2009 and April 2013, 131 (7.1%) returned to the ED within 7 days, 90 of those (4.8%) were discharged to home, and 41 (2.2%) were admitted, Dr. Emily Fain of Cincinnati Children’s Hospital reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
Factors shown on multivariable analyses to be significantly associated with a return visit were tachycardia at discharge (odds ratio, 1.48), fever at discharge (OR, 1.89 for a temperature of 99.5-101.2° F, and 2.35 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), and lack of an antibiotic prescription (OR, 0.44 among those who received a prescription).
Factors associated with admission at the time of the ED revisit were tachypnea in the ED (OR, 2.01), fever at discharge (OR, 3.48 for a temperature of 99.5-101.2° F, and 4.51 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), history of community-acquired pneumonia (CAP) (OR, 3.98), lack of an antibiotic prescription (OR, 0.32 for those who received a prescription), time of visit (OR, 0.43 for those who arrived between 4 p.m. and 12 a.m., compared with arrival between 8 a.m. and 4 p.m.), and race (OR, 0.44 for African Americans vs. whites).
Revisits to the ED are an indicator of quality of care and disease progression, and CAP is among the most common reasons for ED visits, the investigators noted at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
"Attention to these risk factors, particularly potentially modifiable factors such as vital signs, could influence decision making when treating patients for CAP. Further investigation is warranted to better understand the association between lack of antibiotic prescription and revisit to the ED with and without subsequent hospitalization," they concluded.
This study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. Dr. Fain and her colleagues reported having no disclosures.
LAKE BUENA VISTA, FLA. – Fever or lack of an antibiotic prescription are two factors that increase the risk of a return visit to the emergency department and subsequent hospital admission in children with community-acquired pneumonia, according to a review of ED medical records.
Of 1,857 children aged 3 months to 18 years with a diagnosis of pneumonia who were discharged to home after the index ED visit between November 2009 and April 2013, 131 (7.1%) returned to the ED within 7 days, 90 of those (4.8%) were discharged to home, and 41 (2.2%) were admitted, Dr. Emily Fain of Cincinnati Children’s Hospital reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
Factors shown on multivariable analyses to be significantly associated with a return visit were tachycardia at discharge (odds ratio, 1.48), fever at discharge (OR, 1.89 for a temperature of 99.5-101.2° F, and 2.35 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), and lack of an antibiotic prescription (OR, 0.44 among those who received a prescription).
Factors associated with admission at the time of the ED revisit were tachypnea in the ED (OR, 2.01), fever at discharge (OR, 3.48 for a temperature of 99.5-101.2° F, and 4.51 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), history of community-acquired pneumonia (CAP) (OR, 3.98), lack of an antibiotic prescription (OR, 0.32 for those who received a prescription), time of visit (OR, 0.43 for those who arrived between 4 p.m. and 12 a.m., compared with arrival between 8 a.m. and 4 p.m.), and race (OR, 0.44 for African Americans vs. whites).
Revisits to the ED are an indicator of quality of care and disease progression, and CAP is among the most common reasons for ED visits, the investigators noted at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
"Attention to these risk factors, particularly potentially modifiable factors such as vital signs, could influence decision making when treating patients for CAP. Further investigation is warranted to better understand the association between lack of antibiotic prescription and revisit to the ED with and without subsequent hospitalization," they concluded.
This study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. Dr. Fain and her colleagues reported having no disclosures.
LAKE BUENA VISTA, FLA. – Fever or lack of an antibiotic prescription are two factors that increase the risk of a return visit to the emergency department and subsequent hospital admission in children with community-acquired pneumonia, according to a review of ED medical records.
Of 1,857 children aged 3 months to 18 years with a diagnosis of pneumonia who were discharged to home after the index ED visit between November 2009 and April 2013, 131 (7.1%) returned to the ED within 7 days, 90 of those (4.8%) were discharged to home, and 41 (2.2%) were admitted, Dr. Emily Fain of Cincinnati Children’s Hospital reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
Factors shown on multivariable analyses to be significantly associated with a return visit were tachycardia at discharge (odds ratio, 1.48), fever at discharge (OR, 1.89 for a temperature of 99.5-101.2° F, and 2.35 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), and lack of an antibiotic prescription (OR, 0.44 among those who received a prescription).
Factors associated with admission at the time of the ED revisit were tachypnea in the ED (OR, 2.01), fever at discharge (OR, 3.48 for a temperature of 99.5-101.2° F, and 4.51 for a temperature greater than 101.3° F, compared with a temperature less than 99.5° F), history of community-acquired pneumonia (CAP) (OR, 3.98), lack of an antibiotic prescription (OR, 0.32 for those who received a prescription), time of visit (OR, 0.43 for those who arrived between 4 p.m. and 12 a.m., compared with arrival between 8 a.m. and 4 p.m.), and race (OR, 0.44 for African Americans vs. whites).
Revisits to the ED are an indicator of quality of care and disease progression, and CAP is among the most common reasons for ED visits, the investigators noted at the meeting sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
"Attention to these risk factors, particularly potentially modifiable factors such as vital signs, could influence decision making when treating patients for CAP. Further investigation is warranted to better understand the association between lack of antibiotic prescription and revisit to the ED with and without subsequent hospitalization," they concluded.
This study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. Dr. Fain and her colleagues reported having no disclosures.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical point: In children with community-acquired pneumonia, fever or lack of an antibiotic prescription are two factors that increase the risk of a return visit to the ED.
Major finding: A total of 7.1% of children seen in the ED for CAP had a return visit within 7 days.
Data source: A retrospective cohort study involving 1,857 children.
Disclosures: This study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. Dr. Fain and her colleagues reported having no disclosures.
Renal ultrasound in neonates with febrile UTI can rule out high-grade vesicoureteral reflux
LAKE BUENA VISTA, FLA. – Renal ultrasound in infants under 2 months of age with febrile urinary tract infection can be used to rule out high-grade vesicoureteral reflux, according to findings from a retrospective cross-sectional study.
This is because renal ultrasound has a high negative predictive value for detecting high-grade vesicoureteral reflux (VUR) in neonates, and although it has poor sensitivity for detecting low-grade VUR, its sensitivity for detecting high-grade VUR is quite good in this population.
The findings could have important implications for the management of neonates with febrile urinary tract infection (UTI), who are not included in American Academy of Pediatrics guidelines for febrile UTI. A 2011 update to those guidelines calls for the use of screening renal and bladder ultrasound, but recommends against routine voiding cystourethrogram (VCUG) after an initial febrile UTI in young children unless indicated by sonographic findings; however, these guidelines apply to children aged 2 months to 2 years only.
Younger infants who present with febrile UTI differ from those over 2 months of age in that they are more likely to be male – a high percentage of whom are uncircumcised and prone to UTI because of colonization, they have a more immature immune system that can also contribute to greater likelihood of UTI, and they can have higher rates of reflux and anatomical anomalies, Dr. Sowdhamini S. Wallace, director of pediatric hospital medicine research at Texas Children’s Hospital, Houston, reported at the Pediatric Hospital Medicine 2014 meeting.
Although many studies have included older children, they have limited applicability to younger infants because of these differences, and those studies that have included infants less than 2 months of age have been of small size or questionable quality, Dr. Wallace noted.
"So the objective of our study was to determine the test properties of renal ultrasound for detecting VUR and high-grade VUR and obstructive uropathies in this [younger] age group," she said at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of 200 eligible neonates with a mean age of 33 days, 30% had an abnormal renal ultrasound after presenting with febrile UTI. The most common reason for an abnormal finding was hydronephrosis.
Twenty-six percent of the neonates had reflux and 8% had high-grade reflux; 8% had obstructive uropathies or nonobstructive lower tract anomalies, Dr. Wallace said.
The sensitivity of renal ultrasound for all grades of VUR was 31% overall, but was 87% for high-grade VUR.
"For high-grade VUR, the negative predictive value was 99%, with a 95%-100% confidence interval. There were no obstructive uropathies that were diagnosed by VCUG in patients with a normal renal ultrasound," she said.
The number of patients with a normal ultrasound who would need to undergo VCUG to detect one case of high-grade VUR was 70; the number needed to test to detect one case of low-grade VUR was 4, she said.
The number needed to test "should be very helpful for physicians when they are deciding whether to get a VCUG on a neonate under 2 months if they have a normal renal ultrasound, Dr. Wallace said.
"Overall, I think you can see, with the number needed to test of 70, that you would have to test many babies with normal renal ultrasound to detect one case of high-grade VUR, so you may be able to spare many infants from VCUG," she concluded.
The infants presented to the emergency department during 2008-2011 with culture-proven UTI and fever of at least 100.4° F. They were identified through a microbiology database; those included in the study had urine collected through a catheterization or suprapubic aspiration, and those with a history of abnormal prenatal ultrasound, a previous diagnosis of genitourinary tract anomalies, or greater than 30 days between ultrasound and VCUG were excluded.
Imaging studies were reviewed independently by two radiologists who were blinded to the VCUG findings. Any discrepancies were resolved by a third radiologist.
Renal ultrasound was categorized as abnormal if it showed hydronephrosis and/or caliectasis, or if there was renal size discrepancy greater than 10%, findings of a duplicated collecting system, or urethral thickening, urethral dilatation, or bladder abnormalities.
VUR severity was determined by the standard classification system.
The study is limited by the fact that most renal ultrasounds were performed at the time of UTI diagnosis when inflammation is likely present. Inflammation may also be present in patients with VUR, thus the sensitivity of renal ultrasound in this study may have been higher than with renal ultrasound performed after a UTI has resolved. Also, in the absence of a standard definition for hydronephrosis in infants less than 2 months of age the prenatal parameter of 4 mL was used.
Dr. Wallace reported having no disclosures.
LAKE BUENA VISTA, FLA. – Renal ultrasound in infants under 2 months of age with febrile urinary tract infection can be used to rule out high-grade vesicoureteral reflux, according to findings from a retrospective cross-sectional study.
This is because renal ultrasound has a high negative predictive value for detecting high-grade vesicoureteral reflux (VUR) in neonates, and although it has poor sensitivity for detecting low-grade VUR, its sensitivity for detecting high-grade VUR is quite good in this population.
The findings could have important implications for the management of neonates with febrile urinary tract infection (UTI), who are not included in American Academy of Pediatrics guidelines for febrile UTI. A 2011 update to those guidelines calls for the use of screening renal and bladder ultrasound, but recommends against routine voiding cystourethrogram (VCUG) after an initial febrile UTI in young children unless indicated by sonographic findings; however, these guidelines apply to children aged 2 months to 2 years only.
Younger infants who present with febrile UTI differ from those over 2 months of age in that they are more likely to be male – a high percentage of whom are uncircumcised and prone to UTI because of colonization, they have a more immature immune system that can also contribute to greater likelihood of UTI, and they can have higher rates of reflux and anatomical anomalies, Dr. Sowdhamini S. Wallace, director of pediatric hospital medicine research at Texas Children’s Hospital, Houston, reported at the Pediatric Hospital Medicine 2014 meeting.
Although many studies have included older children, they have limited applicability to younger infants because of these differences, and those studies that have included infants less than 2 months of age have been of small size or questionable quality, Dr. Wallace noted.
"So the objective of our study was to determine the test properties of renal ultrasound for detecting VUR and high-grade VUR and obstructive uropathies in this [younger] age group," she said at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of 200 eligible neonates with a mean age of 33 days, 30% had an abnormal renal ultrasound after presenting with febrile UTI. The most common reason for an abnormal finding was hydronephrosis.
Twenty-six percent of the neonates had reflux and 8% had high-grade reflux; 8% had obstructive uropathies or nonobstructive lower tract anomalies, Dr. Wallace said.
The sensitivity of renal ultrasound for all grades of VUR was 31% overall, but was 87% for high-grade VUR.
"For high-grade VUR, the negative predictive value was 99%, with a 95%-100% confidence interval. There were no obstructive uropathies that were diagnosed by VCUG in patients with a normal renal ultrasound," she said.
The number of patients with a normal ultrasound who would need to undergo VCUG to detect one case of high-grade VUR was 70; the number needed to test to detect one case of low-grade VUR was 4, she said.
The number needed to test "should be very helpful for physicians when they are deciding whether to get a VCUG on a neonate under 2 months if they have a normal renal ultrasound, Dr. Wallace said.
"Overall, I think you can see, with the number needed to test of 70, that you would have to test many babies with normal renal ultrasound to detect one case of high-grade VUR, so you may be able to spare many infants from VCUG," she concluded.
The infants presented to the emergency department during 2008-2011 with culture-proven UTI and fever of at least 100.4° F. They were identified through a microbiology database; those included in the study had urine collected through a catheterization or suprapubic aspiration, and those with a history of abnormal prenatal ultrasound, a previous diagnosis of genitourinary tract anomalies, or greater than 30 days between ultrasound and VCUG were excluded.
Imaging studies were reviewed independently by two radiologists who were blinded to the VCUG findings. Any discrepancies were resolved by a third radiologist.
Renal ultrasound was categorized as abnormal if it showed hydronephrosis and/or caliectasis, or if there was renal size discrepancy greater than 10%, findings of a duplicated collecting system, or urethral thickening, urethral dilatation, or bladder abnormalities.
VUR severity was determined by the standard classification system.
The study is limited by the fact that most renal ultrasounds were performed at the time of UTI diagnosis when inflammation is likely present. Inflammation may also be present in patients with VUR, thus the sensitivity of renal ultrasound in this study may have been higher than with renal ultrasound performed after a UTI has resolved. Also, in the absence of a standard definition for hydronephrosis in infants less than 2 months of age the prenatal parameter of 4 mL was used.
Dr. Wallace reported having no disclosures.
LAKE BUENA VISTA, FLA. – Renal ultrasound in infants under 2 months of age with febrile urinary tract infection can be used to rule out high-grade vesicoureteral reflux, according to findings from a retrospective cross-sectional study.
This is because renal ultrasound has a high negative predictive value for detecting high-grade vesicoureteral reflux (VUR) in neonates, and although it has poor sensitivity for detecting low-grade VUR, its sensitivity for detecting high-grade VUR is quite good in this population.
The findings could have important implications for the management of neonates with febrile urinary tract infection (UTI), who are not included in American Academy of Pediatrics guidelines for febrile UTI. A 2011 update to those guidelines calls for the use of screening renal and bladder ultrasound, but recommends against routine voiding cystourethrogram (VCUG) after an initial febrile UTI in young children unless indicated by sonographic findings; however, these guidelines apply to children aged 2 months to 2 years only.
Younger infants who present with febrile UTI differ from those over 2 months of age in that they are more likely to be male – a high percentage of whom are uncircumcised and prone to UTI because of colonization, they have a more immature immune system that can also contribute to greater likelihood of UTI, and they can have higher rates of reflux and anatomical anomalies, Dr. Sowdhamini S. Wallace, director of pediatric hospital medicine research at Texas Children’s Hospital, Houston, reported at the Pediatric Hospital Medicine 2014 meeting.
Although many studies have included older children, they have limited applicability to younger infants because of these differences, and those studies that have included infants less than 2 months of age have been of small size or questionable quality, Dr. Wallace noted.
"So the objective of our study was to determine the test properties of renal ultrasound for detecting VUR and high-grade VUR and obstructive uropathies in this [younger] age group," she said at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of 200 eligible neonates with a mean age of 33 days, 30% had an abnormal renal ultrasound after presenting with febrile UTI. The most common reason for an abnormal finding was hydronephrosis.
Twenty-six percent of the neonates had reflux and 8% had high-grade reflux; 8% had obstructive uropathies or nonobstructive lower tract anomalies, Dr. Wallace said.
The sensitivity of renal ultrasound for all grades of VUR was 31% overall, but was 87% for high-grade VUR.
"For high-grade VUR, the negative predictive value was 99%, with a 95%-100% confidence interval. There were no obstructive uropathies that were diagnosed by VCUG in patients with a normal renal ultrasound," she said.
The number of patients with a normal ultrasound who would need to undergo VCUG to detect one case of high-grade VUR was 70; the number needed to test to detect one case of low-grade VUR was 4, she said.
The number needed to test "should be very helpful for physicians when they are deciding whether to get a VCUG on a neonate under 2 months if they have a normal renal ultrasound, Dr. Wallace said.
"Overall, I think you can see, with the number needed to test of 70, that you would have to test many babies with normal renal ultrasound to detect one case of high-grade VUR, so you may be able to spare many infants from VCUG," she concluded.
The infants presented to the emergency department during 2008-2011 with culture-proven UTI and fever of at least 100.4° F. They were identified through a microbiology database; those included in the study had urine collected through a catheterization or suprapubic aspiration, and those with a history of abnormal prenatal ultrasound, a previous diagnosis of genitourinary tract anomalies, or greater than 30 days between ultrasound and VCUG were excluded.
Imaging studies were reviewed independently by two radiologists who were blinded to the VCUG findings. Any discrepancies were resolved by a third radiologist.
Renal ultrasound was categorized as abnormal if it showed hydronephrosis and/or caliectasis, or if there was renal size discrepancy greater than 10%, findings of a duplicated collecting system, or urethral thickening, urethral dilatation, or bladder abnormalities.
VUR severity was determined by the standard classification system.
The study is limited by the fact that most renal ultrasounds were performed at the time of UTI diagnosis when inflammation is likely present. Inflammation may also be present in patients with VUR, thus the sensitivity of renal ultrasound in this study may have been higher than with renal ultrasound performed after a UTI has resolved. Also, in the absence of a standard definition for hydronephrosis in infants less than 2 months of age the prenatal parameter of 4 mL was used.
Dr. Wallace reported having no disclosures.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical finding: With the number needed to test of 70, you would have to test many babies with normal renal ultrasound to detect one case of high-grade VUR, so you may be able to spare many infants from VCUG.
Major finding: Number needed to test to detect one case of high-grade VUR: 70.
Data source: A retrospective cross-sectional study of 200 neonates.
Disclosures: Dr. Wallace reported having no disclosures.
Subspecialty outpatient clinics, EDs miss many flu vaccination opportunities
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to retrospective chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, although this finding was not statistically significant, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote.
Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to retrospective chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, although this finding was not statistically significant, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote.
Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.
LAKE BUENA VISTA, FLA. – Nearly 44% of incompletely vaccinated inpatients with influenza had a missed opportunity for vaccination, according to retrospective chart review at Children’s Hospital Colorado.
Among 197 such children admitted with confirmed influenza in 2010-2014, 86 (44%) had a total of 507 medical visits during which influenza vaccine was available, Dr. Suchitra Rao of the University of Colorado, Denver, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
The majority of patients with missed opportunity visits were considered high risk for severe complications from influenza from factors such as age younger than 2 years, immunosuppression, pregnancy, or an underlying chronic pulmonary, cardiovascular, renal, hepatic, neurological, hematologic, or metabolic disorder, although this finding was not statistically significant, Dr. Rao reported.
The bulk of missed opportunity visits occurred during September, October, and November (20%-23% each month) prior to onset of the influenza season, with declining percentages taking place between December and April. Most of the visits (45%) occurred at specialty clinics, followed by the emergency department or urgent care setting (22%).
"Subspecialty outpatient visits provide an excellent opportunity for influenza vaccination because they target high-risk patients and they represent the highest proportion of missed opportunities for vaccination," Dr. Rao and her colleagues wrote.
Future analyses will explore independent risk factors for missed opportunities, and identify differences in visit characteristic for high vs. low risk groups, they noted.
The Pediatric Hospital Medicine 2014 meeting was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The authors reported having no relevant financial disclosures.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical point: Specialty outpatient visits offer an important opportunity for influenza vaccinations.
Major finding: A total of 44% of 197 patients had a total of 507 missed opportunities for vaccination.
Data source: A retrospective review of the charts of 197 incompletely vaccinated children with the flu.
Disclosures: The authors reported having no relevant financial disclosures.
High-flow nasal cannulas support children outside the ICU
LAKE BUENA VISTA, FLA. – The use of high-flow nasal cannulas for respiratory support in young children with acute bronchiolitis is safe outside the intensive care unit setting, according to a retrospective cohort study.
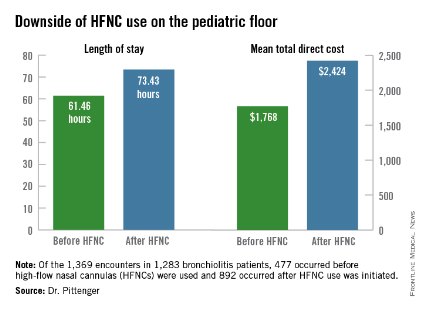
However, initiating the use of high-flow nasal cannulas (HFNCs) on the pediatric floor increases length of stay and direct cost, Dr. Jaime Pittenger of the University of Kentucky, Lexington, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
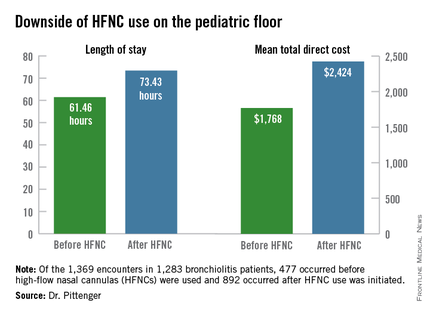
Of 1,369 encounters in 1,283 non-ICU bronchiolitis patients under age 2 who were seen between October 2008 and May 2013, 477 occurred before HFNC use on the floor was initiated in 2010, and 892 occurred after such use was initiated. Of these, 139 involved receipt of HFNCs outside the ICU, Dr. Pittenger reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of those who received HFNCs outside the ICU, 66% who would have previously gone to the ICU remained on the floor, she noted.
Furthermore, a reduction was seen in noninvasive and invasive ventilation in the ICU after HFNC use outside the ICU was initiated, although this did not reach significance (P = .19).
Use of HFNCs on the floor was associated with a relatively low frequency of complications, but mean length of stay was 61.46 hours before HFNC was used outside the ICU, compared with 73.43 hours. Mean total direct cost was $1,768 before HFNC was used outside the ICU, vs. $2,424 after it began to be used outside the ICU after non-ICU HFNC initiation.
HFNC use outside the ICU for respiratory support in pediatric patients with bronchiolitis has increased in recent years, but there has been little evidence to support the safety and effectiveness of this paradigm shift. Though limited by lack of standardization, patient and treatment selection biases, and a small cohort size for ascertaining the frequency of complications, these findings suggest that the practice is feasible.
However, future studies should evaluate the cost-effectiveness of using HFNC on the floor, Dr. Pittenger concluded, noting that standardization of initiation, escalation, and de-escalation of HFNC are also needed.
Dr. Pittenger reported having no disclosures.
LAKE BUENA VISTA, FLA. – The use of high-flow nasal cannulas for respiratory support in young children with acute bronchiolitis is safe outside the intensive care unit setting, according to a retrospective cohort study.
However, initiating the use of high-flow nasal cannulas (HFNCs) on the pediatric floor increases length of stay and direct cost, Dr. Jaime Pittenger of the University of Kentucky, Lexington, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
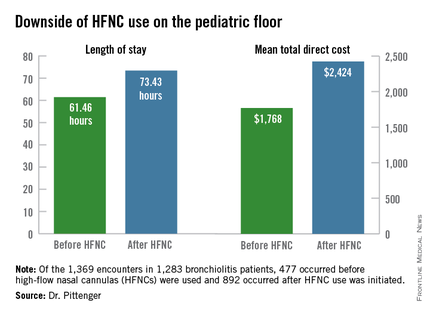
Of 1,369 encounters in 1,283 non-ICU bronchiolitis patients under age 2 who were seen between October 2008 and May 2013, 477 occurred before HFNC use on the floor was initiated in 2010, and 892 occurred after such use was initiated. Of these, 139 involved receipt of HFNCs outside the ICU, Dr. Pittenger reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of those who received HFNCs outside the ICU, 66% who would have previously gone to the ICU remained on the floor, she noted.
Furthermore, a reduction was seen in noninvasive and invasive ventilation in the ICU after HFNC use outside the ICU was initiated, although this did not reach significance (P = .19).
Use of HFNCs on the floor was associated with a relatively low frequency of complications, but mean length of stay was 61.46 hours before HFNC was used outside the ICU, compared with 73.43 hours. Mean total direct cost was $1,768 before HFNC was used outside the ICU, vs. $2,424 after it began to be used outside the ICU after non-ICU HFNC initiation.
HFNC use outside the ICU for respiratory support in pediatric patients with bronchiolitis has increased in recent years, but there has been little evidence to support the safety and effectiveness of this paradigm shift. Though limited by lack of standardization, patient and treatment selection biases, and a small cohort size for ascertaining the frequency of complications, these findings suggest that the practice is feasible.
However, future studies should evaluate the cost-effectiveness of using HFNC on the floor, Dr. Pittenger concluded, noting that standardization of initiation, escalation, and de-escalation of HFNC are also needed.
Dr. Pittenger reported having no disclosures.
LAKE BUENA VISTA, FLA. – The use of high-flow nasal cannulas for respiratory support in young children with acute bronchiolitis is safe outside the intensive care unit setting, according to a retrospective cohort study.
However, initiating the use of high-flow nasal cannulas (HFNCs) on the pediatric floor increases length of stay and direct cost, Dr. Jaime Pittenger of the University of Kentucky, Lexington, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
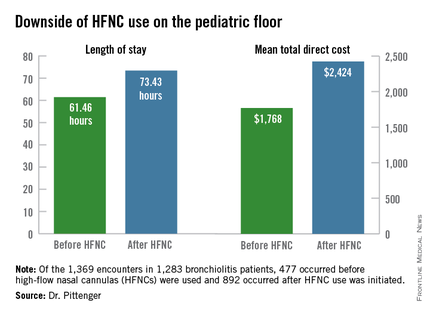
Of 1,369 encounters in 1,283 non-ICU bronchiolitis patients under age 2 who were seen between October 2008 and May 2013, 477 occurred before HFNC use on the floor was initiated in 2010, and 892 occurred after such use was initiated. Of these, 139 involved receipt of HFNCs outside the ICU, Dr. Pittenger reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of those who received HFNCs outside the ICU, 66% who would have previously gone to the ICU remained on the floor, she noted.
Furthermore, a reduction was seen in noninvasive and invasive ventilation in the ICU after HFNC use outside the ICU was initiated, although this did not reach significance (P = .19).
Use of HFNCs on the floor was associated with a relatively low frequency of complications, but mean length of stay was 61.46 hours before HFNC was used outside the ICU, compared with 73.43 hours. Mean total direct cost was $1,768 before HFNC was used outside the ICU, vs. $2,424 after it began to be used outside the ICU after non-ICU HFNC initiation.
HFNC use outside the ICU for respiratory support in pediatric patients with bronchiolitis has increased in recent years, but there has been little evidence to support the safety and effectiveness of this paradigm shift. Though limited by lack of standardization, patient and treatment selection biases, and a small cohort size for ascertaining the frequency of complications, these findings suggest that the practice is feasible.
However, future studies should evaluate the cost-effectiveness of using HFNC on the floor, Dr. Pittenger concluded, noting that standardization of initiation, escalation, and de-escalation of HFNC are also needed.
Dr. Pittenger reported having no disclosures.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical point: HFNC use outside the ICU is feasible for respiratory support in young children with bronchiolitis.
Major finding: A total of 66% of HFNC patients who would have been sent to the ICU remained on the pediatric floor.
Data source: A retrospective cohort study of 1,369 encounters in 1,283 non-ICU bronchiolitis patients under age 2.
Disclosures: Dr. Pittenger reported having no disclosures.
RCT: 3% hypertonic saline fails to improve bronchiolitis outcomes
LAKE BUENA VISTA, FLA. – The median length of stay and rate of readmission did not differ between infants with bronchiolitis who were treated with nebulized 3% hypertonic saline and those treated with normal saline in the first U.S. prospective, double-blind, randomized controlled trial comparing the two treatments.*
The median length of stay was 2.0 days in 93 infants younger than age 12 months who were admitted to an urban tertiary care children’s hospital with a diagnosis of bronchiolitis and who were randomized to receive the hypertonic saline treatments without concomitant bronchodilators, and 2.0 days in 97 such infants who received normal saline without bronchodilators, Dr. Alyssa Silver reported at the Pediatric Hospital Medicine 2014 meeting.
The mean length of stay also did not differ significantly between the groups, nor did the rate of readmission and rate of adverse event, Dr. Silver, a pediatric hospitalist and director of pediatric inpatient physician assistant services at the Children’s Hospital at Montefiore, Bronx, N.Y., reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Infants offered enrollment were those admitted with bronchiolitis to an urban tertiary care children’s hospital in a population with a high endemic prevalence of asthma. Those with status asthmaticus, certain chronic diseases, and prior exposure to hypertonic saline were among those excluded.
The infants included in the study were enrolled within 12 hours of admission between 2011 and 2014, received 4 mL of hypertonic or normal saline every 4 hours via standard hospital wall nebulizer until discharge and were assessed daily by study personnel who made follow-up calls at 1 week and 1 month after discharge to document readmissions.
To address the theoretical concern of bronchospasm with hypertonic saline, patients were evaluated using the Respiratory Distress Assessment Instrument prior to first study treatment and at 30 minutes after the treatment as a safety measure and were withdrawn if the measure increased by four or more points, Dr. Silver said.
The treatment and control groups were similar with respect to demographic factors.
Subgroup analyses showed no differences in length of stay between infants in the treatment and control groups who were respiratory syncytial virus positive, had a history of wheezing, or had a history of prematurity, Dr. Silver noted.
Enrollment in the study was halted at the time of an interim analysis because of the demonstrated lack of difference in length of stay between the groups.
Bronchiolitis is the leading cause of hospitalization for children under 12 months of age – at a cost of about $500 million each year. The national average length of stay for infants with bronchiolitis is 3.3 days.
"Despite the high incidence of bronchiolitis, there is a lack of a unified inpatient treatment plan beyond supportive care of oxygen and intravenous hydration. Many different approaches have been used, but none have proven useful," Dr. Silver said, adding that interest in the use of nebulized hypertonic saline has been on the rise.
Based on literature from its use in patients with cystic fibrosis, the proposed mechanism of action is hydration of the airway surface liquid, which decreases airway wall edema and improves ciliary function, thereby assisting with the clearance of secretions, she explained.
A Cochrane review suggested benefit, but there are a number of concerns about generalizing the findings. For example, all of the included studies were performed outside of the United States, included varying dosing regimens, and excluded patients with a history of wheeze, and most allowed the use of adjunctive bronchodilators and were performed in areas with a much longer length of stay than occurs in the United States.
More recent studies in the United States questioned the utility of hypertonic saline, but also allowed the use of bronchodilators and excluded patients with a history of wheezing.
The findings of the current study suggest that although 3% hypertonic saline is safe in infants with bronchiolitis – including those with a history of wheeze, and even in a population with high endemic prevalence of asthma – there is no utility for the routine use of 3% hypertonic saline vs. normal saline without adjunctive bronchodilators in this population, she said.
However, the study is limited by the single-center design, and lack of complete coverage for recruiting of admitted patients (the study was unfunded and relied on voluntary study personnel), although more than 75% of patients admitted for bronchiolitis were offered enrollment.
Future studies might benefit by enrolling patients earlier than within 12 hours of admission with a minimum severity score to enter, assessing similar outcomes using higher concentrations of nebulized sodium chloride, studying on demand vs. scheduled saline treatments for bronchiolitis, and/or by comparing either intervention to supportive care alone, Dr. Silver said.
Dr. Silver reported having no disclosures.
*An earlier version of this article misstated the city name in the dateline.
LAKE BUENA VISTA, FLA. – The median length of stay and rate of readmission did not differ between infants with bronchiolitis who were treated with nebulized 3% hypertonic saline and those treated with normal saline in the first U.S. prospective, double-blind, randomized controlled trial comparing the two treatments.*
The median length of stay was 2.0 days in 93 infants younger than age 12 months who were admitted to an urban tertiary care children’s hospital with a diagnosis of bronchiolitis and who were randomized to receive the hypertonic saline treatments without concomitant bronchodilators, and 2.0 days in 97 such infants who received normal saline without bronchodilators, Dr. Alyssa Silver reported at the Pediatric Hospital Medicine 2014 meeting.
The mean length of stay also did not differ significantly between the groups, nor did the rate of readmission and rate of adverse event, Dr. Silver, a pediatric hospitalist and director of pediatric inpatient physician assistant services at the Children’s Hospital at Montefiore, Bronx, N.Y., reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Infants offered enrollment were those admitted with bronchiolitis to an urban tertiary care children’s hospital in a population with a high endemic prevalence of asthma. Those with status asthmaticus, certain chronic diseases, and prior exposure to hypertonic saline were among those excluded.
The infants included in the study were enrolled within 12 hours of admission between 2011 and 2014, received 4 mL of hypertonic or normal saline every 4 hours via standard hospital wall nebulizer until discharge and were assessed daily by study personnel who made follow-up calls at 1 week and 1 month after discharge to document readmissions.
To address the theoretical concern of bronchospasm with hypertonic saline, patients were evaluated using the Respiratory Distress Assessment Instrument prior to first study treatment and at 30 minutes after the treatment as a safety measure and were withdrawn if the measure increased by four or more points, Dr. Silver said.
The treatment and control groups were similar with respect to demographic factors.
Subgroup analyses showed no differences in length of stay between infants in the treatment and control groups who were respiratory syncytial virus positive, had a history of wheezing, or had a history of prematurity, Dr. Silver noted.
Enrollment in the study was halted at the time of an interim analysis because of the demonstrated lack of difference in length of stay between the groups.
Bronchiolitis is the leading cause of hospitalization for children under 12 months of age – at a cost of about $500 million each year. The national average length of stay for infants with bronchiolitis is 3.3 days.
"Despite the high incidence of bronchiolitis, there is a lack of a unified inpatient treatment plan beyond supportive care of oxygen and intravenous hydration. Many different approaches have been used, but none have proven useful," Dr. Silver said, adding that interest in the use of nebulized hypertonic saline has been on the rise.
Based on literature from its use in patients with cystic fibrosis, the proposed mechanism of action is hydration of the airway surface liquid, which decreases airway wall edema and improves ciliary function, thereby assisting with the clearance of secretions, she explained.
A Cochrane review suggested benefit, but there are a number of concerns about generalizing the findings. For example, all of the included studies were performed outside of the United States, included varying dosing regimens, and excluded patients with a history of wheeze, and most allowed the use of adjunctive bronchodilators and were performed in areas with a much longer length of stay than occurs in the United States.
More recent studies in the United States questioned the utility of hypertonic saline, but also allowed the use of bronchodilators and excluded patients with a history of wheezing.
The findings of the current study suggest that although 3% hypertonic saline is safe in infants with bronchiolitis – including those with a history of wheeze, and even in a population with high endemic prevalence of asthma – there is no utility for the routine use of 3% hypertonic saline vs. normal saline without adjunctive bronchodilators in this population, she said.
However, the study is limited by the single-center design, and lack of complete coverage for recruiting of admitted patients (the study was unfunded and relied on voluntary study personnel), although more than 75% of patients admitted for bronchiolitis were offered enrollment.
Future studies might benefit by enrolling patients earlier than within 12 hours of admission with a minimum severity score to enter, assessing similar outcomes using higher concentrations of nebulized sodium chloride, studying on demand vs. scheduled saline treatments for bronchiolitis, and/or by comparing either intervention to supportive care alone, Dr. Silver said.
Dr. Silver reported having no disclosures.
*An earlier version of this article misstated the city name in the dateline.
LAKE BUENA VISTA, FLA. – The median length of stay and rate of readmission did not differ between infants with bronchiolitis who were treated with nebulized 3% hypertonic saline and those treated with normal saline in the first U.S. prospective, double-blind, randomized controlled trial comparing the two treatments.*
The median length of stay was 2.0 days in 93 infants younger than age 12 months who were admitted to an urban tertiary care children’s hospital with a diagnosis of bronchiolitis and who were randomized to receive the hypertonic saline treatments without concomitant bronchodilators, and 2.0 days in 97 such infants who received normal saline without bronchodilators, Dr. Alyssa Silver reported at the Pediatric Hospital Medicine 2014 meeting.
The mean length of stay also did not differ significantly between the groups, nor did the rate of readmission and rate of adverse event, Dr. Silver, a pediatric hospitalist and director of pediatric inpatient physician assistant services at the Children’s Hospital at Montefiore, Bronx, N.Y., reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Infants offered enrollment were those admitted with bronchiolitis to an urban tertiary care children’s hospital in a population with a high endemic prevalence of asthma. Those with status asthmaticus, certain chronic diseases, and prior exposure to hypertonic saline were among those excluded.
The infants included in the study were enrolled within 12 hours of admission between 2011 and 2014, received 4 mL of hypertonic or normal saline every 4 hours via standard hospital wall nebulizer until discharge and were assessed daily by study personnel who made follow-up calls at 1 week and 1 month after discharge to document readmissions.
To address the theoretical concern of bronchospasm with hypertonic saline, patients were evaluated using the Respiratory Distress Assessment Instrument prior to first study treatment and at 30 minutes after the treatment as a safety measure and were withdrawn if the measure increased by four or more points, Dr. Silver said.
The treatment and control groups were similar with respect to demographic factors.
Subgroup analyses showed no differences in length of stay between infants in the treatment and control groups who were respiratory syncytial virus positive, had a history of wheezing, or had a history of prematurity, Dr. Silver noted.
Enrollment in the study was halted at the time of an interim analysis because of the demonstrated lack of difference in length of stay between the groups.
Bronchiolitis is the leading cause of hospitalization for children under 12 months of age – at a cost of about $500 million each year. The national average length of stay for infants with bronchiolitis is 3.3 days.
"Despite the high incidence of bronchiolitis, there is a lack of a unified inpatient treatment plan beyond supportive care of oxygen and intravenous hydration. Many different approaches have been used, but none have proven useful," Dr. Silver said, adding that interest in the use of nebulized hypertonic saline has been on the rise.
Based on literature from its use in patients with cystic fibrosis, the proposed mechanism of action is hydration of the airway surface liquid, which decreases airway wall edema and improves ciliary function, thereby assisting with the clearance of secretions, she explained.
A Cochrane review suggested benefit, but there are a number of concerns about generalizing the findings. For example, all of the included studies were performed outside of the United States, included varying dosing regimens, and excluded patients with a history of wheeze, and most allowed the use of adjunctive bronchodilators and were performed in areas with a much longer length of stay than occurs in the United States.
More recent studies in the United States questioned the utility of hypertonic saline, but also allowed the use of bronchodilators and excluded patients with a history of wheezing.
The findings of the current study suggest that although 3% hypertonic saline is safe in infants with bronchiolitis – including those with a history of wheeze, and even in a population with high endemic prevalence of asthma – there is no utility for the routine use of 3% hypertonic saline vs. normal saline without adjunctive bronchodilators in this population, she said.
However, the study is limited by the single-center design, and lack of complete coverage for recruiting of admitted patients (the study was unfunded and relied on voluntary study personnel), although more than 75% of patients admitted for bronchiolitis were offered enrollment.
Future studies might benefit by enrolling patients earlier than within 12 hours of admission with a minimum severity score to enter, assessing similar outcomes using higher concentrations of nebulized sodium chloride, studying on demand vs. scheduled saline treatments for bronchiolitis, and/or by comparing either intervention to supportive care alone, Dr. Silver said.
Dr. Silver reported having no disclosures.
*An earlier version of this article misstated the city name in the dateline.
AT PEDIATRIC HOSPITAL MEDICINE 2014
Key clinical point: There is no reason for routine use of 3% hypertonic saline vs. normal saline without adjunctive bronchodilators in infants.
Major finding: Length of stay was approximately 2.0 days in both the treatment and control groups.
Data source: A prospective, double-blind, randomized, controlled study of 190 bronchiolitic infants younger than 12 months.
Disclosures: Dr. Silver reported no disclosures.