User login
Cutaneous laser surgery: Basic caution isn’t enough to prevent lawsuits
SAN DIEGO – Injuries and lawsuits related to laser cosmetic surgery are increasing and potential legal threats are not always easy to predict, according to two dermatologists who spoke at the annual meeting of the American Society for Laser Medicine and Surgery (ASLMS).
A laser procedure could go smoothly, for example, but the patient might be able to successfully sue if he or she is allowed to drive home after receiving a sedative. Or a physician might get sued because his or her nurse set a laser at the wrong setting and singed a patient.
The risk of a lawsuit is high, H. Ray Jalian, MD, a dermatologist in Los Angeles, said at the meeting. “The reality is that we’re all at some point going to face this.”
The most common procedure litigated was laser hair removal, making up almost 40% of the cases, which is not an indication that this particular procedure is dangerous, Dr. Jalian said. “It’s quite safe, and the complication rate is quite low,” but more of these procedures are being done, he noted. Rejuvenation procedures followed, accounting for 25% of cases.
The alleged injuries sustained from laser surgery included burns (47%), scars (39%), and pigmentation problems (24%). Deaths occurred in just over 2% of the cases. In the study, almost a third of plaintiffs alleged that they were not provided informed consent. Plaintiffs also alleged fraud (9%) and assault/battery (5%), and a family member occasionally sued for loss of consortium (8% of cases). The specialty with the largest percentage of the cases was plastic surgery (26%), followed by dermatology (21%).
Dr. Jalian and his copresenter, Mathew Avram, MD, JD, director of the Dermatology Laser & Cosmetic Center, and director of dermatologic surgery at Massachusetts General Hospital, Boston, offered these lessons about the legal risks associated with laser procedures:
• You may have a duty to protect your patient from bad choices.
Physicians aren’t expected to keep patients from making certain bad decisions such as sunbathing after a traditional resurfacing procedure, said Dr. Avram, of the department of dermatology, Harvard Medical School, Boston, and the ASLMS president. But in some cases, he said, the law may expect the physician to step in to prevent harm. For example, he said, a patient who has undergone a fractional ablative laser procedure and has received a sedative should not be allowed to drive home.
• You may get sued even if your employee is at fault.
The 2013 study found physicians were often sued even when they did not perform the laser procedure in question. Nonphysicians such as physician assistants and nurses often perform laser operations, and many states allow them to do so. “Nonphysicians were less likely to be sued even if they were the operators,” Dr. Jalian said. In the study, almost 38% of the 174 analyzed cases involved nonphysician operators, but they were sued in just 26% of the cases. In 33 of the 174 cases in the study, plaintiffs alleged failure to properly hire, train, or supervise staff.
He recommended looking at state laws, which differ greatly in their regulations – or lack of them – regarding the operation of medical lasers. In some cases, physicians must supervise laser use, he said. “But what are the requirements? Can you be available by phone down the street or in the Caribbean?”
Dr. Jalian, Dr. Avram, and a colleague followed up the 2013 study with another study that tracked 175 legal cases from 1999 to 2012 involving alleged injuries from cutaneous laser surgery. During this time period, 75 (43%) involved a nonphysician operating a laser, increasing from 36% in 2008 to 78% in 2012.
In almost two-thirds of cases, the procedures in question were done by nonphysicians outside a “traditional medical setting” such as a salon or spa (JAMA Dermatol. 2014 Apr;150[4]:407-11).
• Delayed side effects could mean delayed lawsuits.
According to Dr. Avram, statutes of limitations – the length of time in which a patient can file a lawsuit – typically last for 2-3 years in malpractice cases. But he said that the period begins when the physician is alleged to have made a mistake or when the patient becomes aware of – or should reasonably be aware of – an injury. Therefore, physicians could face legal trouble over delayed hypopigmentation that appears 6 months after a laser resurfacing treatment, or granulomas that appear years after a filler treatment, he said.
• A signed form is not a cure-all.
It is wise to make patients sign an extensive informed consent form, but this will not protect a physician against a claim of negligence, Dr. Avram said. And the reverse is also true: If a patient did not sign a proper consent form, he or she could still sue even if the procedure went perfectly, he noted.
• Your instincts are worth trusting.
When it comes to lawsuit prevention, Dr. Avram said, “by far the most important thing you can do happens within a minute of when you see the patient. Assess and trust your own intuition and your staff’s intuition. For elective, cosmetic treatments, don’t be afraid to say no. There’s no legal obligation to perform a cosmetic treatment on a patient.”
If you do choose to treat a patient, he advised, be open about the procedure and “maybe even tell them some of the tougher, worse-case scenarios.” If a procedure goes poorly, he said, consider how to fix it. “Many complications can be significantly improved or cleared with timely and appropriate intervention,” he said.
In some cases, refunding the patient’s money can be considered, with the patient signing a release, he said. “Document that you are refunding the money in order to preserve the doctor-patient relationship, not to avoid negligence.”
Dr. Jalian and Dr. Avram reported no relevant disclosures.
SAN DIEGO – Injuries and lawsuits related to laser cosmetic surgery are increasing and potential legal threats are not always easy to predict, according to two dermatologists who spoke at the annual meeting of the American Society for Laser Medicine and Surgery (ASLMS).
A laser procedure could go smoothly, for example, but the patient might be able to successfully sue if he or she is allowed to drive home after receiving a sedative. Or a physician might get sued because his or her nurse set a laser at the wrong setting and singed a patient.
The risk of a lawsuit is high, H. Ray Jalian, MD, a dermatologist in Los Angeles, said at the meeting. “The reality is that we’re all at some point going to face this.”
The most common procedure litigated was laser hair removal, making up almost 40% of the cases, which is not an indication that this particular procedure is dangerous, Dr. Jalian said. “It’s quite safe, and the complication rate is quite low,” but more of these procedures are being done, he noted. Rejuvenation procedures followed, accounting for 25% of cases.
The alleged injuries sustained from laser surgery included burns (47%), scars (39%), and pigmentation problems (24%). Deaths occurred in just over 2% of the cases. In the study, almost a third of plaintiffs alleged that they were not provided informed consent. Plaintiffs also alleged fraud (9%) and assault/battery (5%), and a family member occasionally sued for loss of consortium (8% of cases). The specialty with the largest percentage of the cases was plastic surgery (26%), followed by dermatology (21%).
Dr. Jalian and his copresenter, Mathew Avram, MD, JD, director of the Dermatology Laser & Cosmetic Center, and director of dermatologic surgery at Massachusetts General Hospital, Boston, offered these lessons about the legal risks associated with laser procedures:
• You may have a duty to protect your patient from bad choices.
Physicians aren’t expected to keep patients from making certain bad decisions such as sunbathing after a traditional resurfacing procedure, said Dr. Avram, of the department of dermatology, Harvard Medical School, Boston, and the ASLMS president. But in some cases, he said, the law may expect the physician to step in to prevent harm. For example, he said, a patient who has undergone a fractional ablative laser procedure and has received a sedative should not be allowed to drive home.
• You may get sued even if your employee is at fault.
The 2013 study found physicians were often sued even when they did not perform the laser procedure in question. Nonphysicians such as physician assistants and nurses often perform laser operations, and many states allow them to do so. “Nonphysicians were less likely to be sued even if they were the operators,” Dr. Jalian said. In the study, almost 38% of the 174 analyzed cases involved nonphysician operators, but they were sued in just 26% of the cases. In 33 of the 174 cases in the study, plaintiffs alleged failure to properly hire, train, or supervise staff.
He recommended looking at state laws, which differ greatly in their regulations – or lack of them – regarding the operation of medical lasers. In some cases, physicians must supervise laser use, he said. “But what are the requirements? Can you be available by phone down the street or in the Caribbean?”
Dr. Jalian, Dr. Avram, and a colleague followed up the 2013 study with another study that tracked 175 legal cases from 1999 to 2012 involving alleged injuries from cutaneous laser surgery. During this time period, 75 (43%) involved a nonphysician operating a laser, increasing from 36% in 2008 to 78% in 2012.
In almost two-thirds of cases, the procedures in question were done by nonphysicians outside a “traditional medical setting” such as a salon or spa (JAMA Dermatol. 2014 Apr;150[4]:407-11).
• Delayed side effects could mean delayed lawsuits.
According to Dr. Avram, statutes of limitations – the length of time in which a patient can file a lawsuit – typically last for 2-3 years in malpractice cases. But he said that the period begins when the physician is alleged to have made a mistake or when the patient becomes aware of – or should reasonably be aware of – an injury. Therefore, physicians could face legal trouble over delayed hypopigmentation that appears 6 months after a laser resurfacing treatment, or granulomas that appear years after a filler treatment, he said.
• A signed form is not a cure-all.
It is wise to make patients sign an extensive informed consent form, but this will not protect a physician against a claim of negligence, Dr. Avram said. And the reverse is also true: If a patient did not sign a proper consent form, he or she could still sue even if the procedure went perfectly, he noted.
• Your instincts are worth trusting.
When it comes to lawsuit prevention, Dr. Avram said, “by far the most important thing you can do happens within a minute of when you see the patient. Assess and trust your own intuition and your staff’s intuition. For elective, cosmetic treatments, don’t be afraid to say no. There’s no legal obligation to perform a cosmetic treatment on a patient.”
If you do choose to treat a patient, he advised, be open about the procedure and “maybe even tell them some of the tougher, worse-case scenarios.” If a procedure goes poorly, he said, consider how to fix it. “Many complications can be significantly improved or cleared with timely and appropriate intervention,” he said.
In some cases, refunding the patient’s money can be considered, with the patient signing a release, he said. “Document that you are refunding the money in order to preserve the doctor-patient relationship, not to avoid negligence.”
Dr. Jalian and Dr. Avram reported no relevant disclosures.
SAN DIEGO – Injuries and lawsuits related to laser cosmetic surgery are increasing and potential legal threats are not always easy to predict, according to two dermatologists who spoke at the annual meeting of the American Society for Laser Medicine and Surgery (ASLMS).
A laser procedure could go smoothly, for example, but the patient might be able to successfully sue if he or she is allowed to drive home after receiving a sedative. Or a physician might get sued because his or her nurse set a laser at the wrong setting and singed a patient.
The risk of a lawsuit is high, H. Ray Jalian, MD, a dermatologist in Los Angeles, said at the meeting. “The reality is that we’re all at some point going to face this.”
The most common procedure litigated was laser hair removal, making up almost 40% of the cases, which is not an indication that this particular procedure is dangerous, Dr. Jalian said. “It’s quite safe, and the complication rate is quite low,” but more of these procedures are being done, he noted. Rejuvenation procedures followed, accounting for 25% of cases.
The alleged injuries sustained from laser surgery included burns (47%), scars (39%), and pigmentation problems (24%). Deaths occurred in just over 2% of the cases. In the study, almost a third of plaintiffs alleged that they were not provided informed consent. Plaintiffs also alleged fraud (9%) and assault/battery (5%), and a family member occasionally sued for loss of consortium (8% of cases). The specialty with the largest percentage of the cases was plastic surgery (26%), followed by dermatology (21%).
Dr. Jalian and his copresenter, Mathew Avram, MD, JD, director of the Dermatology Laser & Cosmetic Center, and director of dermatologic surgery at Massachusetts General Hospital, Boston, offered these lessons about the legal risks associated with laser procedures:
• You may have a duty to protect your patient from bad choices.
Physicians aren’t expected to keep patients from making certain bad decisions such as sunbathing after a traditional resurfacing procedure, said Dr. Avram, of the department of dermatology, Harvard Medical School, Boston, and the ASLMS president. But in some cases, he said, the law may expect the physician to step in to prevent harm. For example, he said, a patient who has undergone a fractional ablative laser procedure and has received a sedative should not be allowed to drive home.
• You may get sued even if your employee is at fault.
The 2013 study found physicians were often sued even when they did not perform the laser procedure in question. Nonphysicians such as physician assistants and nurses often perform laser operations, and many states allow them to do so. “Nonphysicians were less likely to be sued even if they were the operators,” Dr. Jalian said. In the study, almost 38% of the 174 analyzed cases involved nonphysician operators, but they were sued in just 26% of the cases. In 33 of the 174 cases in the study, plaintiffs alleged failure to properly hire, train, or supervise staff.
He recommended looking at state laws, which differ greatly in their regulations – or lack of them – regarding the operation of medical lasers. In some cases, physicians must supervise laser use, he said. “But what are the requirements? Can you be available by phone down the street or in the Caribbean?”
Dr. Jalian, Dr. Avram, and a colleague followed up the 2013 study with another study that tracked 175 legal cases from 1999 to 2012 involving alleged injuries from cutaneous laser surgery. During this time period, 75 (43%) involved a nonphysician operating a laser, increasing from 36% in 2008 to 78% in 2012.
In almost two-thirds of cases, the procedures in question were done by nonphysicians outside a “traditional medical setting” such as a salon or spa (JAMA Dermatol. 2014 Apr;150[4]:407-11).
• Delayed side effects could mean delayed lawsuits.
According to Dr. Avram, statutes of limitations – the length of time in which a patient can file a lawsuit – typically last for 2-3 years in malpractice cases. But he said that the period begins when the physician is alleged to have made a mistake or when the patient becomes aware of – or should reasonably be aware of – an injury. Therefore, physicians could face legal trouble over delayed hypopigmentation that appears 6 months after a laser resurfacing treatment, or granulomas that appear years after a filler treatment, he said.
• A signed form is not a cure-all.
It is wise to make patients sign an extensive informed consent form, but this will not protect a physician against a claim of negligence, Dr. Avram said. And the reverse is also true: If a patient did not sign a proper consent form, he or she could still sue even if the procedure went perfectly, he noted.
• Your instincts are worth trusting.
When it comes to lawsuit prevention, Dr. Avram said, “by far the most important thing you can do happens within a minute of when you see the patient. Assess and trust your own intuition and your staff’s intuition. For elective, cosmetic treatments, don’t be afraid to say no. There’s no legal obligation to perform a cosmetic treatment on a patient.”
If you do choose to treat a patient, he advised, be open about the procedure and “maybe even tell them some of the tougher, worse-case scenarios.” If a procedure goes poorly, he said, consider how to fix it. “Many complications can be significantly improved or cleared with timely and appropriate intervention,” he said.
In some cases, refunding the patient’s money can be considered, with the patient signing a release, he said. “Document that you are refunding the money in order to preserve the doctor-patient relationship, not to avoid negligence.”
Dr. Jalian and Dr. Avram reported no relevant disclosures.
AT LASER 2017
RF, IPL score highest for facial rejuvenation in review
SAN DIEGO – A review of existing research found that newer technologies are safer and more effective at skin rejuvenation than older ones, with two types – intense pulsed laser (IPL) and radiofrequency (RF) – at or near the head of the pack on both fronts.
In addition, 10 types of treatments, including multiple laser technologies, scored higher than facial peels on safety, although the peels beat almost all comers in terms of efficacy, the study’s lead author, Caerwyn Ash, PhD, said in an interview after presenting the results at the annual meeting of the American Society for Laser Medicine and Surgery.
The review is unique because it maps the various treatments on two axes – safety and efficacy – in a chart. Viewers gain an instant perspective on how the individual treatments fare when stacked up against each other. “The study gives credence to the new technologies,” said Dr. Ash, associate professor of medical devices at the University of Wales Trinity Saint David, Swansea. “We’re moving toward safer and more efficacious results.”
He and his colleagues analyzed more than 500 studies published since 1985, which evaluated 15 different types of technology used for facial rejuvenation. They reviewed at least 35 clinical studies per platform. They also reported on the safety and efficacy of facial peels.
The technologies examined included RF, light emitting diode (LED), pulsed dyed laser (PDL), frequency doubled 532-nm potassium-titanyl-phosphate neodymium:YAG laser (which had a low number of clinical studies), 980-nm diode laser, Q-switched Nd:YAG laser, 1320-nm Nd:YAG laser, 1540-nm Erbium:glass laser, 1450-nm diode laser, IPL, long pulsed Nd:YAG laser, plasma, and copper bromide laser.
Another technology reviewed was fractional selective photothermolysis, but studies of this modality were difficult to compare, according to the authors. Also included was the carbon dioxide laser, which the authors described as being hampered by long healing times and discomfort that requires anesthesia.
The review notes that comparisons between studies of the different treatments in the review were limited by such factors as varied beam and tip sizes (even within individual studies), various pulse durations, and different treatment times and intervals.
The researchers mapped the treatments in a single chart on two axes, safety and efficacy.
Three treatments scored the best in terms of efficacy: RF, IPL and chemical peels. However, while RF and IPL scored near the top of all treatments on the safety scale, chemical peels pulled up the rear.
The treatment strategies on the safety scale, ranked from most safe to least safe, were LED, IPL, diode laser, RF, argon laser, PDL and carbon dioxide laser, Nd:YAG, ablative Erbium, plasma, and chemical peel.
Radiofrequency topped the efficacy scale, followed closely by chemical peel and IPL. Following them, from most efficacious to least efficacious, were carbon dioxide laser, ablative Erbium, plasma treatments, and PDL, Nd:YAG and argon laser, diode laser, and LED.
The study was funded by the University of Wales Trinity Saint David. The authors had no disclosures.
SAN DIEGO – A review of existing research found that newer technologies are safer and more effective at skin rejuvenation than older ones, with two types – intense pulsed laser (IPL) and radiofrequency (RF) – at or near the head of the pack on both fronts.
In addition, 10 types of treatments, including multiple laser technologies, scored higher than facial peels on safety, although the peels beat almost all comers in terms of efficacy, the study’s lead author, Caerwyn Ash, PhD, said in an interview after presenting the results at the annual meeting of the American Society for Laser Medicine and Surgery.
The review is unique because it maps the various treatments on two axes – safety and efficacy – in a chart. Viewers gain an instant perspective on how the individual treatments fare when stacked up against each other. “The study gives credence to the new technologies,” said Dr. Ash, associate professor of medical devices at the University of Wales Trinity Saint David, Swansea. “We’re moving toward safer and more efficacious results.”
He and his colleagues analyzed more than 500 studies published since 1985, which evaluated 15 different types of technology used for facial rejuvenation. They reviewed at least 35 clinical studies per platform. They also reported on the safety and efficacy of facial peels.
The technologies examined included RF, light emitting diode (LED), pulsed dyed laser (PDL), frequency doubled 532-nm potassium-titanyl-phosphate neodymium:YAG laser (which had a low number of clinical studies), 980-nm diode laser, Q-switched Nd:YAG laser, 1320-nm Nd:YAG laser, 1540-nm Erbium:glass laser, 1450-nm diode laser, IPL, long pulsed Nd:YAG laser, plasma, and copper bromide laser.
Another technology reviewed was fractional selective photothermolysis, but studies of this modality were difficult to compare, according to the authors. Also included was the carbon dioxide laser, which the authors described as being hampered by long healing times and discomfort that requires anesthesia.
The review notes that comparisons between studies of the different treatments in the review were limited by such factors as varied beam and tip sizes (even within individual studies), various pulse durations, and different treatment times and intervals.
The researchers mapped the treatments in a single chart on two axes, safety and efficacy.
Three treatments scored the best in terms of efficacy: RF, IPL and chemical peels. However, while RF and IPL scored near the top of all treatments on the safety scale, chemical peels pulled up the rear.
The treatment strategies on the safety scale, ranked from most safe to least safe, were LED, IPL, diode laser, RF, argon laser, PDL and carbon dioxide laser, Nd:YAG, ablative Erbium, plasma, and chemical peel.
Radiofrequency topped the efficacy scale, followed closely by chemical peel and IPL. Following them, from most efficacious to least efficacious, were carbon dioxide laser, ablative Erbium, plasma treatments, and PDL, Nd:YAG and argon laser, diode laser, and LED.
The study was funded by the University of Wales Trinity Saint David. The authors had no disclosures.
SAN DIEGO – A review of existing research found that newer technologies are safer and more effective at skin rejuvenation than older ones, with two types – intense pulsed laser (IPL) and radiofrequency (RF) – at or near the head of the pack on both fronts.
In addition, 10 types of treatments, including multiple laser technologies, scored higher than facial peels on safety, although the peels beat almost all comers in terms of efficacy, the study’s lead author, Caerwyn Ash, PhD, said in an interview after presenting the results at the annual meeting of the American Society for Laser Medicine and Surgery.
The review is unique because it maps the various treatments on two axes – safety and efficacy – in a chart. Viewers gain an instant perspective on how the individual treatments fare when stacked up against each other. “The study gives credence to the new technologies,” said Dr. Ash, associate professor of medical devices at the University of Wales Trinity Saint David, Swansea. “We’re moving toward safer and more efficacious results.”
He and his colleagues analyzed more than 500 studies published since 1985, which evaluated 15 different types of technology used for facial rejuvenation. They reviewed at least 35 clinical studies per platform. They also reported on the safety and efficacy of facial peels.
The technologies examined included RF, light emitting diode (LED), pulsed dyed laser (PDL), frequency doubled 532-nm potassium-titanyl-phosphate neodymium:YAG laser (which had a low number of clinical studies), 980-nm diode laser, Q-switched Nd:YAG laser, 1320-nm Nd:YAG laser, 1540-nm Erbium:glass laser, 1450-nm diode laser, IPL, long pulsed Nd:YAG laser, plasma, and copper bromide laser.
Another technology reviewed was fractional selective photothermolysis, but studies of this modality were difficult to compare, according to the authors. Also included was the carbon dioxide laser, which the authors described as being hampered by long healing times and discomfort that requires anesthesia.
The review notes that comparisons between studies of the different treatments in the review were limited by such factors as varied beam and tip sizes (even within individual studies), various pulse durations, and different treatment times and intervals.
The researchers mapped the treatments in a single chart on two axes, safety and efficacy.
Three treatments scored the best in terms of efficacy: RF, IPL and chemical peels. However, while RF and IPL scored near the top of all treatments on the safety scale, chemical peels pulled up the rear.
The treatment strategies on the safety scale, ranked from most safe to least safe, were LED, IPL, diode laser, RF, argon laser, PDL and carbon dioxide laser, Nd:YAG, ablative Erbium, plasma, and chemical peel.
Radiofrequency topped the efficacy scale, followed closely by chemical peel and IPL. Following them, from most efficacious to least efficacious, were carbon dioxide laser, ablative Erbium, plasma treatments, and PDL, Nd:YAG and argon laser, diode laser, and LED.
The study was funded by the University of Wales Trinity Saint David. The authors had no disclosures.
AT LASER 2017
Key clinical point:
Major finding: IPL and RF were among the modalities that were safer and more effective at skin rejuvenation than were older ones.
Data source: An analysis of more than 500 studies published since 1985 evaluating of 15 different types of technology used for facial rejuvenation, reviewing at least 35 clinical studies per platform.
Disclosures: The study was funded by the University of Wales Trinity Saint David. The authors had no disclosures.
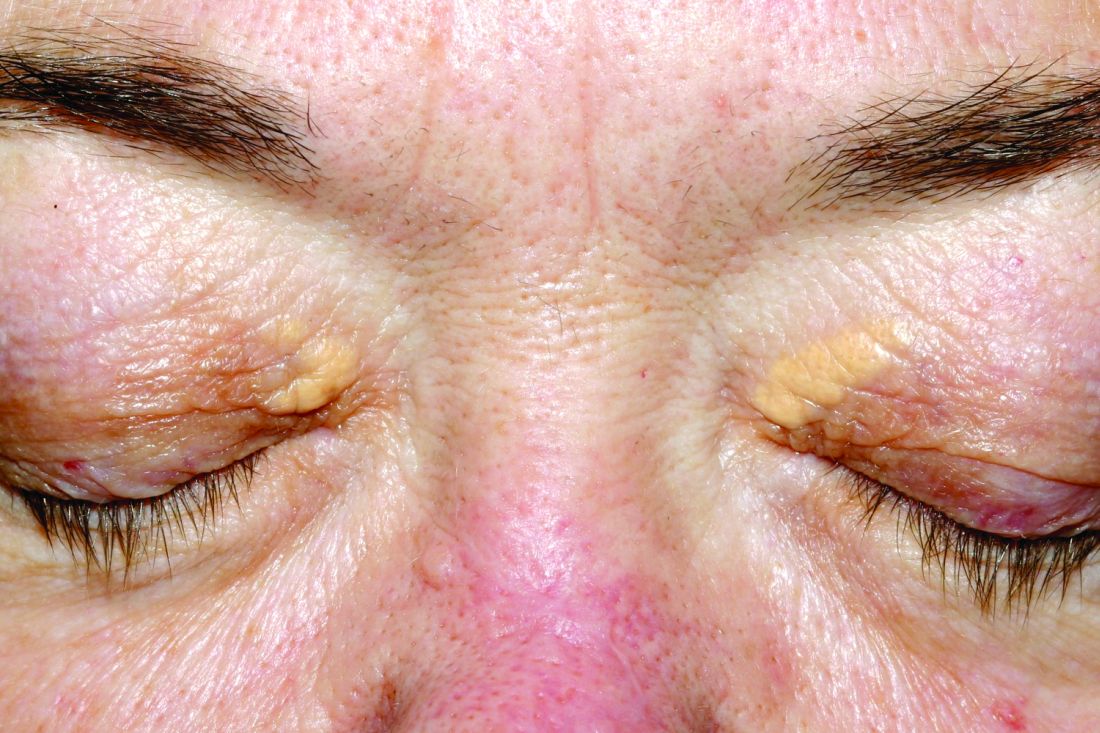
Lasers may be effective for treating xanthelasma
SAN DIEGO – Laser treatments may be effective for xanthelasma palpebrarum lesions, based on a systematic review of existing studies, although the research is limited.
“The number of cases we looked at was relatively small, so you can’t come up with any definite conclusions,” said review coauthor Christopher J. Huerter, MD, head of the division of dermatology at Creighton University, Omaha. “But it’s promising since the lasers we examined all work with some efficacy, with the CO2 and Er:YAG [erbium:YAG] lasers probably having the best results.”
Xanthelasma lesions appear as small yellowish plaques on the eyelids. “About half the people who have it have some blood lipid abnormality,” Dr. Huerter said in an interview. “If a person has it, it’s worthwhile to do a cholesterol screen or a lipid profile.”
Treatment with trichloroacetic acid is one option, although it was more common before lasers began to be used. In addition, “surgical incision can be very effective,” he said, although the review notes that it can create undesirable scarring.
Researchers have studied laser treatment for xanthelasma for at least 30 years. Dr. Huerter and his colleagues examined 21 studies published since 1987, with the following lasers: CO2 laser (three studies), argon laser (one study), Er:YAG laser (four studies), ultrapulse CO2 laser (five studies), 1,450-nm diode laser (one study), pulsed dye laser (PDL, two studies), superpulsed or fractional CO2 laser (one study), and Q-switched neodymium:YAG laser (three studies). An additional study examined both argon and Er:YAG lasers.
The number of treated patients in the studies ranged from 1 to 50, and the number of treated lesions ranged from 1 to 76. (Patients often had more than one lesion.) “It would be nice to have bigger studies and bigger numbers,” Dr. Huerter said at the annual meeting of the American Society for Laser Medicine and Surgery.
Although the studies were limited by small cohorts, short follow-up, and lack of comparison groups, the findings did reveal signs of effectiveness: Clearance rates were 100% in CO2, argon, and PDL cases and about 85% with Er:YAG lasers. Clearance rates were lower with Nd:YAG (about 55%) and 1,450-nm diode (about 48%) lasers.
Edema was reported in all PDL cases and erythema in almost 20% of CO2 cases. Dyspigmentation was most common – at about 30% – in Er:YAG and 1,450-nm diode cases. Visible scars were reported in more than 5% of Er:YAG cases.
The review concluded that “sufficient evidence is available to suggest laser therapies to be a cosmetically excellent treatment option for xanthelasma , particularly applicable in patients who are not good candidates for surgical excision,” he said.
As for advice to dermatologists, Dr. Huerter pointed to the positive results for CO2 and Er:YAG lasers. He said PDL lasers could also be used. As for argon lasers, he noted that it’s not as likely for dermatologists to have them on hand, he said.
In regard to choosing which xanthelasma lesions to treat with laser, he said thicker ones may not be as amenable. “But if you do laser treatment and don’t get the results you want, you can always excise.”
No funding for the study was reported. Dr. Huerter reported no disclosures.
SAN DIEGO – Laser treatments may be effective for xanthelasma palpebrarum lesions, based on a systematic review of existing studies, although the research is limited.
“The number of cases we looked at was relatively small, so you can’t come up with any definite conclusions,” said review coauthor Christopher J. Huerter, MD, head of the division of dermatology at Creighton University, Omaha. “But it’s promising since the lasers we examined all work with some efficacy, with the CO2 and Er:YAG [erbium:YAG] lasers probably having the best results.”
Xanthelasma lesions appear as small yellowish plaques on the eyelids. “About half the people who have it have some blood lipid abnormality,” Dr. Huerter said in an interview. “If a person has it, it’s worthwhile to do a cholesterol screen or a lipid profile.”
Treatment with trichloroacetic acid is one option, although it was more common before lasers began to be used. In addition, “surgical incision can be very effective,” he said, although the review notes that it can create undesirable scarring.
Researchers have studied laser treatment for xanthelasma for at least 30 years. Dr. Huerter and his colleagues examined 21 studies published since 1987, with the following lasers: CO2 laser (three studies), argon laser (one study), Er:YAG laser (four studies), ultrapulse CO2 laser (five studies), 1,450-nm diode laser (one study), pulsed dye laser (PDL, two studies), superpulsed or fractional CO2 laser (one study), and Q-switched neodymium:YAG laser (three studies). An additional study examined both argon and Er:YAG lasers.
The number of treated patients in the studies ranged from 1 to 50, and the number of treated lesions ranged from 1 to 76. (Patients often had more than one lesion.) “It would be nice to have bigger studies and bigger numbers,” Dr. Huerter said at the annual meeting of the American Society for Laser Medicine and Surgery.
Although the studies were limited by small cohorts, short follow-up, and lack of comparison groups, the findings did reveal signs of effectiveness: Clearance rates were 100% in CO2, argon, and PDL cases and about 85% with Er:YAG lasers. Clearance rates were lower with Nd:YAG (about 55%) and 1,450-nm diode (about 48%) lasers.
Edema was reported in all PDL cases and erythema in almost 20% of CO2 cases. Dyspigmentation was most common – at about 30% – in Er:YAG and 1,450-nm diode cases. Visible scars were reported in more than 5% of Er:YAG cases.
The review concluded that “sufficient evidence is available to suggest laser therapies to be a cosmetically excellent treatment option for xanthelasma , particularly applicable in patients who are not good candidates for surgical excision,” he said.
As for advice to dermatologists, Dr. Huerter pointed to the positive results for CO2 and Er:YAG lasers. He said PDL lasers could also be used. As for argon lasers, he noted that it’s not as likely for dermatologists to have them on hand, he said.
In regard to choosing which xanthelasma lesions to treat with laser, he said thicker ones may not be as amenable. “But if you do laser treatment and don’t get the results you want, you can always excise.”
No funding for the study was reported. Dr. Huerter reported no disclosures.
SAN DIEGO – Laser treatments may be effective for xanthelasma palpebrarum lesions, based on a systematic review of existing studies, although the research is limited.
“The number of cases we looked at was relatively small, so you can’t come up with any definite conclusions,” said review coauthor Christopher J. Huerter, MD, head of the division of dermatology at Creighton University, Omaha. “But it’s promising since the lasers we examined all work with some efficacy, with the CO2 and Er:YAG [erbium:YAG] lasers probably having the best results.”
Xanthelasma lesions appear as small yellowish plaques on the eyelids. “About half the people who have it have some blood lipid abnormality,” Dr. Huerter said in an interview. “If a person has it, it’s worthwhile to do a cholesterol screen or a lipid profile.”
Treatment with trichloroacetic acid is one option, although it was more common before lasers began to be used. In addition, “surgical incision can be very effective,” he said, although the review notes that it can create undesirable scarring.
Researchers have studied laser treatment for xanthelasma for at least 30 years. Dr. Huerter and his colleagues examined 21 studies published since 1987, with the following lasers: CO2 laser (three studies), argon laser (one study), Er:YAG laser (four studies), ultrapulse CO2 laser (five studies), 1,450-nm diode laser (one study), pulsed dye laser (PDL, two studies), superpulsed or fractional CO2 laser (one study), and Q-switched neodymium:YAG laser (three studies). An additional study examined both argon and Er:YAG lasers.
The number of treated patients in the studies ranged from 1 to 50, and the number of treated lesions ranged from 1 to 76. (Patients often had more than one lesion.) “It would be nice to have bigger studies and bigger numbers,” Dr. Huerter said at the annual meeting of the American Society for Laser Medicine and Surgery.
Although the studies were limited by small cohorts, short follow-up, and lack of comparison groups, the findings did reveal signs of effectiveness: Clearance rates were 100% in CO2, argon, and PDL cases and about 85% with Er:YAG lasers. Clearance rates were lower with Nd:YAG (about 55%) and 1,450-nm diode (about 48%) lasers.
Edema was reported in all PDL cases and erythema in almost 20% of CO2 cases. Dyspigmentation was most common – at about 30% – in Er:YAG and 1,450-nm diode cases. Visible scars were reported in more than 5% of Er:YAG cases.
The review concluded that “sufficient evidence is available to suggest laser therapies to be a cosmetically excellent treatment option for xanthelasma , particularly applicable in patients who are not good candidates for surgical excision,” he said.
As for advice to dermatologists, Dr. Huerter pointed to the positive results for CO2 and Er:YAG lasers. He said PDL lasers could also be used. As for argon lasers, he noted that it’s not as likely for dermatologists to have them on hand, he said.
In regard to choosing which xanthelasma lesions to treat with laser, he said thicker ones may not be as amenable. “But if you do laser treatment and don’t get the results you want, you can always excise.”
No funding for the study was reported. Dr. Huerter reported no disclosures.
Key clinical point:
Major finding: Clearance rates of about 85%-100% were reported for xanthelasma treatment with CO2, argon, pulsed dye, and Er:YAG laser treatments.
Data source: A systematic review of 21 studies evaluating different laser treatments for xanthelasma.
Disclosures: No funding was reported. Dr. Huerter reported no disclosures.
Study reveals crazy quilt of laser laws across the United States
SAN DIEGO – Laser hair removal isn’t typically in an office cleaner’s job description. So it’s no wonder that Virginia legislators were spooked when they heard from a constituent who was treated by a spa worker who turned out to be a janitor.
Earlier this year, legislators in the Old Dominion passed a bill limiting laser hair removal procedures to a “properly trained” medical doctor, physician assistant, or nurse practitioner – or a “properly trained” person who is supervised by one of these professionals. Therefore, it’s still possible for a “properly trained” person without a degree of any kind to operate a laser in Virginia.
To the north in New Jersey, the rules are much stricter: Only physicians can perform laser procedures. But in New York, it appears that anyone can fire up a laser and go to work on unwanted hair. And in Florida, nonphysicians can perform laser procedures only if they’re physician assistants or nurse practitioners. But they’re only allowed to remove hair with lasers at a clinic that just performs laser hair removal.
Such is the chaotic state of laser law in the United States, a new study finds. The rules, which vary widely from state to state, are often vague and confusing. And, as Virginia’s new law shows, they’re still evolving. (The study is current as of March 2016.)
She and study coauthor Mathew M. Avram, MD, JD, director of the Laser and Cosmetic Center at Massachusetts General, analyzed regulations in the 50 states regarding the operation of lasers. They reported their findings at the annual meeting of the American Society for Laser Medicine and Surgery.
Dr. DiGiorgio said that laser operator laws address three issues:
1. Who can operate a laser?
At other clinics across the country, nonphysician employees — such as nurse practitioners and registered nurses – often operate lasers. Whether they can legally actually do so isn’t always obvious.
New Jersey is the only state that requires laser operators to be physicians. At the other extreme, 11 states, including Massachusetts, Colorado, Florida, Missouri, New York, and Pennsylvania, have “no” limits on who can perform laser procedures. (At Massachusetts General Hospital, physicians perform all laser procedures.)
So does that mean anyone can perform a laser procedure? It’s not clear. “The laws are a lot more vague than they should be,” Dr. DiGiorgio said in an interview.
Eighteen states allow people to perform laser procedures as part of the “practice of medicine,” although legislation can be vague on what that means. Those states include Illinois, Michigan, Minnesota, North Carolina, and Texas.
Another 19 states, including California, Ohio, Washington, Wisconsin, and now Virginia, have specific limits on who can perform laser procedures. In California, for example, physician assistants and registered nurses – but not licensed vocational nurses – are allowed to use lasers to remove hair, spider veins, and tattoos. Unlicensed medical assistants, cosmetologists, electrologists, and estheticians are not allowed to perform the procedures
2. Can someone delegate laser procedures to someone else?
In nine states, including Iowa and New Hampshire, there’s no oversight of delegation or nonphysicians can delegate procedures to someone else.
In another nine states, certain procedures can be delegated with no physician oversight, such as laser hair removal in Alaska and ablative procedures (to advanced practice registered nurses only) in Utah.
3. Is supervision required of nonphysicians?
Physicians don’t need to supervise certain laser procedures in 11 states, including Hawaii, Oregon, and Vermont, where they can be performed by a nonphysician with no supervision or under supervision by a non-physician.
In 17 states, supervision isn’t always required or it’s under the discretion of the supervising physician. These states include California, Michigan, Pennsylvania, and Wisconsin.
In 11 states, including Illinois and Massachusetts, only certain procedures require on-site supervision. Six states, including Connecticut and Maryland, require on-site physician supervision for all laser procedures, but Dr. DiGiorgio said the requirements can be vague about what “on site” actually means.
Idaho requires the physician to be on site or immediately available, and South Carolina allows registered nurses to perform laser hair and leg vein removal if a physician is on site and can respond within 5 minutes.
“We don’t know what the ideal regulation is,” Dr. DiGiorgio said. But she believes laser regulations are crucial to safety, especially as fields such as plastic surgery, ophthalmology, and gynecology embrace cosmetic laser procedures.
Information about state-by-state laser operator laws is available on the American Med Spa Association website.
Dr. DiGiorgio reported no relevant disclosures.
SAN DIEGO – Laser hair removal isn’t typically in an office cleaner’s job description. So it’s no wonder that Virginia legislators were spooked when they heard from a constituent who was treated by a spa worker who turned out to be a janitor.
Earlier this year, legislators in the Old Dominion passed a bill limiting laser hair removal procedures to a “properly trained” medical doctor, physician assistant, or nurse practitioner – or a “properly trained” person who is supervised by one of these professionals. Therefore, it’s still possible for a “properly trained” person without a degree of any kind to operate a laser in Virginia.
To the north in New Jersey, the rules are much stricter: Only physicians can perform laser procedures. But in New York, it appears that anyone can fire up a laser and go to work on unwanted hair. And in Florida, nonphysicians can perform laser procedures only if they’re physician assistants or nurse practitioners. But they’re only allowed to remove hair with lasers at a clinic that just performs laser hair removal.
Such is the chaotic state of laser law in the United States, a new study finds. The rules, which vary widely from state to state, are often vague and confusing. And, as Virginia’s new law shows, they’re still evolving. (The study is current as of March 2016.)
She and study coauthor Mathew M. Avram, MD, JD, director of the Laser and Cosmetic Center at Massachusetts General, analyzed regulations in the 50 states regarding the operation of lasers. They reported their findings at the annual meeting of the American Society for Laser Medicine and Surgery.
Dr. DiGiorgio said that laser operator laws address three issues:
1. Who can operate a laser?
At other clinics across the country, nonphysician employees — such as nurse practitioners and registered nurses – often operate lasers. Whether they can legally actually do so isn’t always obvious.
New Jersey is the only state that requires laser operators to be physicians. At the other extreme, 11 states, including Massachusetts, Colorado, Florida, Missouri, New York, and Pennsylvania, have “no” limits on who can perform laser procedures. (At Massachusetts General Hospital, physicians perform all laser procedures.)
So does that mean anyone can perform a laser procedure? It’s not clear. “The laws are a lot more vague than they should be,” Dr. DiGiorgio said in an interview.
Eighteen states allow people to perform laser procedures as part of the “practice of medicine,” although legislation can be vague on what that means. Those states include Illinois, Michigan, Minnesota, North Carolina, and Texas.
Another 19 states, including California, Ohio, Washington, Wisconsin, and now Virginia, have specific limits on who can perform laser procedures. In California, for example, physician assistants and registered nurses – but not licensed vocational nurses – are allowed to use lasers to remove hair, spider veins, and tattoos. Unlicensed medical assistants, cosmetologists, electrologists, and estheticians are not allowed to perform the procedures
2. Can someone delegate laser procedures to someone else?
In nine states, including Iowa and New Hampshire, there’s no oversight of delegation or nonphysicians can delegate procedures to someone else.
In another nine states, certain procedures can be delegated with no physician oversight, such as laser hair removal in Alaska and ablative procedures (to advanced practice registered nurses only) in Utah.
3. Is supervision required of nonphysicians?
Physicians don’t need to supervise certain laser procedures in 11 states, including Hawaii, Oregon, and Vermont, where they can be performed by a nonphysician with no supervision or under supervision by a non-physician.
In 17 states, supervision isn’t always required or it’s under the discretion of the supervising physician. These states include California, Michigan, Pennsylvania, and Wisconsin.
In 11 states, including Illinois and Massachusetts, only certain procedures require on-site supervision. Six states, including Connecticut and Maryland, require on-site physician supervision for all laser procedures, but Dr. DiGiorgio said the requirements can be vague about what “on site” actually means.
Idaho requires the physician to be on site or immediately available, and South Carolina allows registered nurses to perform laser hair and leg vein removal if a physician is on site and can respond within 5 minutes.
“We don’t know what the ideal regulation is,” Dr. DiGiorgio said. But she believes laser regulations are crucial to safety, especially as fields such as plastic surgery, ophthalmology, and gynecology embrace cosmetic laser procedures.
Information about state-by-state laser operator laws is available on the American Med Spa Association website.
Dr. DiGiorgio reported no relevant disclosures.
SAN DIEGO – Laser hair removal isn’t typically in an office cleaner’s job description. So it’s no wonder that Virginia legislators were spooked when they heard from a constituent who was treated by a spa worker who turned out to be a janitor.
Earlier this year, legislators in the Old Dominion passed a bill limiting laser hair removal procedures to a “properly trained” medical doctor, physician assistant, or nurse practitioner – or a “properly trained” person who is supervised by one of these professionals. Therefore, it’s still possible for a “properly trained” person without a degree of any kind to operate a laser in Virginia.
To the north in New Jersey, the rules are much stricter: Only physicians can perform laser procedures. But in New York, it appears that anyone can fire up a laser and go to work on unwanted hair. And in Florida, nonphysicians can perform laser procedures only if they’re physician assistants or nurse practitioners. But they’re only allowed to remove hair with lasers at a clinic that just performs laser hair removal.
Such is the chaotic state of laser law in the United States, a new study finds. The rules, which vary widely from state to state, are often vague and confusing. And, as Virginia’s new law shows, they’re still evolving. (The study is current as of March 2016.)
She and study coauthor Mathew M. Avram, MD, JD, director of the Laser and Cosmetic Center at Massachusetts General, analyzed regulations in the 50 states regarding the operation of lasers. They reported their findings at the annual meeting of the American Society for Laser Medicine and Surgery.
Dr. DiGiorgio said that laser operator laws address three issues:
1. Who can operate a laser?
At other clinics across the country, nonphysician employees — such as nurse practitioners and registered nurses – often operate lasers. Whether they can legally actually do so isn’t always obvious.
New Jersey is the only state that requires laser operators to be physicians. At the other extreme, 11 states, including Massachusetts, Colorado, Florida, Missouri, New York, and Pennsylvania, have “no” limits on who can perform laser procedures. (At Massachusetts General Hospital, physicians perform all laser procedures.)
So does that mean anyone can perform a laser procedure? It’s not clear. “The laws are a lot more vague than they should be,” Dr. DiGiorgio said in an interview.
Eighteen states allow people to perform laser procedures as part of the “practice of medicine,” although legislation can be vague on what that means. Those states include Illinois, Michigan, Minnesota, North Carolina, and Texas.
Another 19 states, including California, Ohio, Washington, Wisconsin, and now Virginia, have specific limits on who can perform laser procedures. In California, for example, physician assistants and registered nurses – but not licensed vocational nurses – are allowed to use lasers to remove hair, spider veins, and tattoos. Unlicensed medical assistants, cosmetologists, electrologists, and estheticians are not allowed to perform the procedures
2. Can someone delegate laser procedures to someone else?
In nine states, including Iowa and New Hampshire, there’s no oversight of delegation or nonphysicians can delegate procedures to someone else.
In another nine states, certain procedures can be delegated with no physician oversight, such as laser hair removal in Alaska and ablative procedures (to advanced practice registered nurses only) in Utah.
3. Is supervision required of nonphysicians?
Physicians don’t need to supervise certain laser procedures in 11 states, including Hawaii, Oregon, and Vermont, where they can be performed by a nonphysician with no supervision or under supervision by a non-physician.
In 17 states, supervision isn’t always required or it’s under the discretion of the supervising physician. These states include California, Michigan, Pennsylvania, and Wisconsin.
In 11 states, including Illinois and Massachusetts, only certain procedures require on-site supervision. Six states, including Connecticut and Maryland, require on-site physician supervision for all laser procedures, but Dr. DiGiorgio said the requirements can be vague about what “on site” actually means.
Idaho requires the physician to be on site or immediately available, and South Carolina allows registered nurses to perform laser hair and leg vein removal if a physician is on site and can respond within 5 minutes.
“We don’t know what the ideal regulation is,” Dr. DiGiorgio said. But she believes laser regulations are crucial to safety, especially as fields such as plastic surgery, ophthalmology, and gynecology embrace cosmetic laser procedures.
Information about state-by-state laser operator laws is available on the American Med Spa Association website.
Dr. DiGiorgio reported no relevant disclosures.
AT LASER 2017
Key clinical point:
Major finding: The study found wide variations in who can operate lasers, and in regulations regarding the delegation and supervision of laser treatments in the different states.
Data source: Analysis of regulations in the 50 states regarding the operation of lasers.
Disclosures: Dr. DiGiorgio reported no relevant disclosures
Nitrous oxide linked to less pain in tattoo removal
SAN DIEGO – The results of a small, single-site study suggest that nitrous oxide (NO) can play a significant role in reducing pain during laser tattoo removal.
“Nitrous oxide is a safe and effective option for patients, particularly those who have large tattoos that can’t be adequately numbed with injections or topical numbing,” the study’s lead author, Jared Mallalieu, DO, said in an interview. “NO has allowed us to treat larger tattoos – full sleeve or large back tattoos – in a single setting, which has made treatment more convenient for patients.”
Patients fared better on pain measures when they received NO, compared with topical and injectable anesthetics, according to Dr. Mallalieu, a cosmetic surgeon at the Laser Center of Maryland, Severna Park. The results were so dramatic that EMLA cream is now rarely used for patients in his clinic, although injectable lidocaine is used on smaller tattoos (smaller than 5 inches by 5 inches), he said.
The use of NO comes with challenges, however, in terms of the extra time and patient monitoring required, he said.
Dr. Mallalieu and his associates reported the results in an e-poster at the annual meeting of the American Society for Laser Medicine and Surgery.
Laser tattoo removal can be an agonizing process. “Patients describe it as being significantly more painful than getting a tattoo,” Dr. Mallalieu said. “The intense pain only lasts during the treatment,” he said, “though many patients will note some discomfort for a few hours after a treatment session.”
Most clinics use a topical cream, such as lidocaine/prilocaine (EMLA) or topical benzocaine/lidocaine/tetracaine (BLT), as an anesthetic for these procedures. “Our center has also used 1% lidocaine with epinephrine in small doses of up to 7 mg/kg,” he said. “The injections are much better than the cream.”
Sometimes the clinic uses a device that blows cold air on the skin, which “helps a little,” he added.
For the study, conducted in 2014, 23 laser tattoo removal patients were surveyed about their pain levels using a 1-10 scale, after undergoing a total of 41 single-location procedures.
The average pain rating during the procedure was 9.1 for those treated only with lidocaine/prilocaine, 5.4 for injections of lidocaine with epinephrine alone, and 6.8 for both lidocaine/prilocaine and lidocaine with epinephrine injections.
The average pain rating for NO alone was 2.6, and was 3.6 for those who received both the injection treatment and lidocaine/prilocaine. Three of 12 NO patients reported anxiety.
Another benefit is that patients can drive after receiving NO, unlike other anesthetics, which leave patients sedated, he said. “Levels of NO are titrated to keep the patient sedated, but breathing on their own,” and patients can be easily woken up within moments of stopping the NO.
However, the use of NO requires more time to set up and more monitoring, he added. The average treatment time for procedures with NO was 27 minutes compared with 4 minutes for the other procedure, and “the patient is put on a monitor that measures pulse rate and oxygenation levels,” which not only takes more time, but requires additional staff to watch the patient. “Also, it takes about 3-5 minutes to slowly the titrate the NO to a perfect level.”
The study points out that physicians at the clinic are the only ones who perform the procedures that use NO, but at many clinics, nonphysicians perform tattoo removals.
As for cost, “NO and oxygen tanks are rather inexpensive to purchase and maintain, and there are various small units which serve to titrate the gas,” Dr. Mallalieu said. “We do charge our patients a small fee because of the added personnel and time cost associated with the procedure. As tattoo removal is considered a cosmetic procedure, insurance doesn’t come into play.”
Training to administer NO brings up the issue of what is allowed in the state, he said. Physicians can give sedation to patients, “but some states may limit the degree to which a patient can be sedated in an office. If the physician has a certified operating room, this is not a problem,” he added. “Because dentists commonly use NO, we followed the American Dental Association guidelines ... As we employ an anesthesiologist, we were quite familiar with it. That said, the administration of NO is not complex and [is] easily mastered.”
Dr. Mallalieu reported no relevant disclosures.
SAN DIEGO – The results of a small, single-site study suggest that nitrous oxide (NO) can play a significant role in reducing pain during laser tattoo removal.
“Nitrous oxide is a safe and effective option for patients, particularly those who have large tattoos that can’t be adequately numbed with injections or topical numbing,” the study’s lead author, Jared Mallalieu, DO, said in an interview. “NO has allowed us to treat larger tattoos – full sleeve or large back tattoos – in a single setting, which has made treatment more convenient for patients.”
Patients fared better on pain measures when they received NO, compared with topical and injectable anesthetics, according to Dr. Mallalieu, a cosmetic surgeon at the Laser Center of Maryland, Severna Park. The results were so dramatic that EMLA cream is now rarely used for patients in his clinic, although injectable lidocaine is used on smaller tattoos (smaller than 5 inches by 5 inches), he said.
The use of NO comes with challenges, however, in terms of the extra time and patient monitoring required, he said.
Dr. Mallalieu and his associates reported the results in an e-poster at the annual meeting of the American Society for Laser Medicine and Surgery.
Laser tattoo removal can be an agonizing process. “Patients describe it as being significantly more painful than getting a tattoo,” Dr. Mallalieu said. “The intense pain only lasts during the treatment,” he said, “though many patients will note some discomfort for a few hours after a treatment session.”
Most clinics use a topical cream, such as lidocaine/prilocaine (EMLA) or topical benzocaine/lidocaine/tetracaine (BLT), as an anesthetic for these procedures. “Our center has also used 1% lidocaine with epinephrine in small doses of up to 7 mg/kg,” he said. “The injections are much better than the cream.”
Sometimes the clinic uses a device that blows cold air on the skin, which “helps a little,” he added.
For the study, conducted in 2014, 23 laser tattoo removal patients were surveyed about their pain levels using a 1-10 scale, after undergoing a total of 41 single-location procedures.
The average pain rating during the procedure was 9.1 for those treated only with lidocaine/prilocaine, 5.4 for injections of lidocaine with epinephrine alone, and 6.8 for both lidocaine/prilocaine and lidocaine with epinephrine injections.
The average pain rating for NO alone was 2.6, and was 3.6 for those who received both the injection treatment and lidocaine/prilocaine. Three of 12 NO patients reported anxiety.
Another benefit is that patients can drive after receiving NO, unlike other anesthetics, which leave patients sedated, he said. “Levels of NO are titrated to keep the patient sedated, but breathing on their own,” and patients can be easily woken up within moments of stopping the NO.
However, the use of NO requires more time to set up and more monitoring, he added. The average treatment time for procedures with NO was 27 minutes compared with 4 minutes for the other procedure, and “the patient is put on a monitor that measures pulse rate and oxygenation levels,” which not only takes more time, but requires additional staff to watch the patient. “Also, it takes about 3-5 minutes to slowly the titrate the NO to a perfect level.”
The study points out that physicians at the clinic are the only ones who perform the procedures that use NO, but at many clinics, nonphysicians perform tattoo removals.
As for cost, “NO and oxygen tanks are rather inexpensive to purchase and maintain, and there are various small units which serve to titrate the gas,” Dr. Mallalieu said. “We do charge our patients a small fee because of the added personnel and time cost associated with the procedure. As tattoo removal is considered a cosmetic procedure, insurance doesn’t come into play.”
Training to administer NO brings up the issue of what is allowed in the state, he said. Physicians can give sedation to patients, “but some states may limit the degree to which a patient can be sedated in an office. If the physician has a certified operating room, this is not a problem,” he added. “Because dentists commonly use NO, we followed the American Dental Association guidelines ... As we employ an anesthesiologist, we were quite familiar with it. That said, the administration of NO is not complex and [is] easily mastered.”
Dr. Mallalieu reported no relevant disclosures.
SAN DIEGO – The results of a small, single-site study suggest that nitrous oxide (NO) can play a significant role in reducing pain during laser tattoo removal.
“Nitrous oxide is a safe and effective option for patients, particularly those who have large tattoos that can’t be adequately numbed with injections or topical numbing,” the study’s lead author, Jared Mallalieu, DO, said in an interview. “NO has allowed us to treat larger tattoos – full sleeve or large back tattoos – in a single setting, which has made treatment more convenient for patients.”
Patients fared better on pain measures when they received NO, compared with topical and injectable anesthetics, according to Dr. Mallalieu, a cosmetic surgeon at the Laser Center of Maryland, Severna Park. The results were so dramatic that EMLA cream is now rarely used for patients in his clinic, although injectable lidocaine is used on smaller tattoos (smaller than 5 inches by 5 inches), he said.
The use of NO comes with challenges, however, in terms of the extra time and patient monitoring required, he said.
Dr. Mallalieu and his associates reported the results in an e-poster at the annual meeting of the American Society for Laser Medicine and Surgery.
Laser tattoo removal can be an agonizing process. “Patients describe it as being significantly more painful than getting a tattoo,” Dr. Mallalieu said. “The intense pain only lasts during the treatment,” he said, “though many patients will note some discomfort for a few hours after a treatment session.”
Most clinics use a topical cream, such as lidocaine/prilocaine (EMLA) or topical benzocaine/lidocaine/tetracaine (BLT), as an anesthetic for these procedures. “Our center has also used 1% lidocaine with epinephrine in small doses of up to 7 mg/kg,” he said. “The injections are much better than the cream.”
Sometimes the clinic uses a device that blows cold air on the skin, which “helps a little,” he added.
For the study, conducted in 2014, 23 laser tattoo removal patients were surveyed about their pain levels using a 1-10 scale, after undergoing a total of 41 single-location procedures.
The average pain rating during the procedure was 9.1 for those treated only with lidocaine/prilocaine, 5.4 for injections of lidocaine with epinephrine alone, and 6.8 for both lidocaine/prilocaine and lidocaine with epinephrine injections.
The average pain rating for NO alone was 2.6, and was 3.6 for those who received both the injection treatment and lidocaine/prilocaine. Three of 12 NO patients reported anxiety.
Another benefit is that patients can drive after receiving NO, unlike other anesthetics, which leave patients sedated, he said. “Levels of NO are titrated to keep the patient sedated, but breathing on their own,” and patients can be easily woken up within moments of stopping the NO.
However, the use of NO requires more time to set up and more monitoring, he added. The average treatment time for procedures with NO was 27 minutes compared with 4 minutes for the other procedure, and “the patient is put on a monitor that measures pulse rate and oxygenation levels,” which not only takes more time, but requires additional staff to watch the patient. “Also, it takes about 3-5 minutes to slowly the titrate the NO to a perfect level.”
The study points out that physicians at the clinic are the only ones who perform the procedures that use NO, but at many clinics, nonphysicians perform tattoo removals.
As for cost, “NO and oxygen tanks are rather inexpensive to purchase and maintain, and there are various small units which serve to titrate the gas,” Dr. Mallalieu said. “We do charge our patients a small fee because of the added personnel and time cost associated with the procedure. As tattoo removal is considered a cosmetic procedure, insurance doesn’t come into play.”
Training to administer NO brings up the issue of what is allowed in the state, he said. Physicians can give sedation to patients, “but some states may limit the degree to which a patient can be sedated in an office. If the physician has a certified operating room, this is not a problem,” he added. “Because dentists commonly use NO, we followed the American Dental Association guidelines ... As we employ an anesthesiologist, we were quite familiar with it. That said, the administration of NO is not complex and [is] easily mastered.”
Dr. Mallalieu reported no relevant disclosures.