User login
SGLT2 inhibitors linked with fewer gout flares in diabetes
TOPLINE:
compared with matched patients treated with a dipeptidyl peptidase–4 (DPP-4) inhibitor.
METHODOLOGY:
- The study used observational data collected from the entire population of British Columbia that included 15,067 adults with both gout and type 2 diabetes in 2014-2020.
- The group included 8,318 patients who initiated an SGLT2 inhibitor and 6,749 patients who initiated a DPP-4 inhibitor during the study period after at least 1 year of continuous enrollment.
- Using propensity-score matching, 4,075 matched pairs were identified, where one person initiated an SGLT2 inhibitor and the other started a DPP-4 inhibitor.
- Primary outcome was recurrent gout flare counts during follow-up that required an ED visit, hospital admission, or an outpatient visit for a gout flare coupled with appropriate treatment, tallied from the first day of drug receipt until June 30, 2022, with an average follow-up of 1.6 years.
- Secondary endpoints included the incidence of myocardial infarction and stroke.
TAKEAWAY:
- Total gout-flare rates after SGLT2 inhibitor initiation were 52.4/1000 person-years and after DPP-4 inhibitor initiation were 79.7/1,000 person-years, an adjusted rate ratio of 0.66, a reduction significantly linked with SGLT2 inhibitor use.
- For flares that required an ED visit or hospitalization, initiation of an SGLT2 inhibitor was linked with a significant, reduced aRR of 0.52, compared with DPP-4 inhibitor initiation.
- The flare-rate reduction linked with SGLT2 inhibitor use was consistent regardless of sex, age, baseline diuretic use, prior treatment with a urate-lowering agent, and baseline gout intensity.
- SGLT2 inhibitor initiation was also significantly linked with an adjusted reduced hazard ratio of 0.69 in the incidence of myocardial infarction, compared with DPP-4 inhibitor initiation, but stroke incidence was not significantly different between the groups.
IN PRACTICE:
These findings suggest that SGLT2 inhibitors could have a much-needed ability to simultaneously reduce the burden of recurrent gout flares and coronary sequelae in patients with gout and type 2 diabetes, indicating that “SGLT2 inhibitors may offer distinct benefits,” making the drug class “a particularly attractive addition to current urate-lowering therapies,” the researchers write.
SOURCE:
The study was primarily conducted by researchers at Massachusetts General Hospital in Boston. The study was published online July 24 in Annals of Internal Medicine.
LIMITATIONS:
The data used in the study did not include gout flares that did not require medical attention and did not include laboratory findings for study participants. Because the data were observational the findings may be susceptible to unmeasured confounding.
DISCLOSURES:
The study received no commercial funding. One author has reported receiving consulting fees from ANI and LG Chem.
A version of this article first appeared on Medscape.com.
TOPLINE:
compared with matched patients treated with a dipeptidyl peptidase–4 (DPP-4) inhibitor.
METHODOLOGY:
- The study used observational data collected from the entire population of British Columbia that included 15,067 adults with both gout and type 2 diabetes in 2014-2020.
- The group included 8,318 patients who initiated an SGLT2 inhibitor and 6,749 patients who initiated a DPP-4 inhibitor during the study period after at least 1 year of continuous enrollment.
- Using propensity-score matching, 4,075 matched pairs were identified, where one person initiated an SGLT2 inhibitor and the other started a DPP-4 inhibitor.
- Primary outcome was recurrent gout flare counts during follow-up that required an ED visit, hospital admission, or an outpatient visit for a gout flare coupled with appropriate treatment, tallied from the first day of drug receipt until June 30, 2022, with an average follow-up of 1.6 years.
- Secondary endpoints included the incidence of myocardial infarction and stroke.
TAKEAWAY:
- Total gout-flare rates after SGLT2 inhibitor initiation were 52.4/1000 person-years and after DPP-4 inhibitor initiation were 79.7/1,000 person-years, an adjusted rate ratio of 0.66, a reduction significantly linked with SGLT2 inhibitor use.
- For flares that required an ED visit or hospitalization, initiation of an SGLT2 inhibitor was linked with a significant, reduced aRR of 0.52, compared with DPP-4 inhibitor initiation.
- The flare-rate reduction linked with SGLT2 inhibitor use was consistent regardless of sex, age, baseline diuretic use, prior treatment with a urate-lowering agent, and baseline gout intensity.
- SGLT2 inhibitor initiation was also significantly linked with an adjusted reduced hazard ratio of 0.69 in the incidence of myocardial infarction, compared with DPP-4 inhibitor initiation, but stroke incidence was not significantly different between the groups.
IN PRACTICE:
These findings suggest that SGLT2 inhibitors could have a much-needed ability to simultaneously reduce the burden of recurrent gout flares and coronary sequelae in patients with gout and type 2 diabetes, indicating that “SGLT2 inhibitors may offer distinct benefits,” making the drug class “a particularly attractive addition to current urate-lowering therapies,” the researchers write.
SOURCE:
The study was primarily conducted by researchers at Massachusetts General Hospital in Boston. The study was published online July 24 in Annals of Internal Medicine.
LIMITATIONS:
The data used in the study did not include gout flares that did not require medical attention and did not include laboratory findings for study participants. Because the data were observational the findings may be susceptible to unmeasured confounding.
DISCLOSURES:
The study received no commercial funding. One author has reported receiving consulting fees from ANI and LG Chem.
A version of this article first appeared on Medscape.com.
TOPLINE:
compared with matched patients treated with a dipeptidyl peptidase–4 (DPP-4) inhibitor.
METHODOLOGY:
- The study used observational data collected from the entire population of British Columbia that included 15,067 adults with both gout and type 2 diabetes in 2014-2020.
- The group included 8,318 patients who initiated an SGLT2 inhibitor and 6,749 patients who initiated a DPP-4 inhibitor during the study period after at least 1 year of continuous enrollment.
- Using propensity-score matching, 4,075 matched pairs were identified, where one person initiated an SGLT2 inhibitor and the other started a DPP-4 inhibitor.
- Primary outcome was recurrent gout flare counts during follow-up that required an ED visit, hospital admission, or an outpatient visit for a gout flare coupled with appropriate treatment, tallied from the first day of drug receipt until June 30, 2022, with an average follow-up of 1.6 years.
- Secondary endpoints included the incidence of myocardial infarction and stroke.
TAKEAWAY:
- Total gout-flare rates after SGLT2 inhibitor initiation were 52.4/1000 person-years and after DPP-4 inhibitor initiation were 79.7/1,000 person-years, an adjusted rate ratio of 0.66, a reduction significantly linked with SGLT2 inhibitor use.
- For flares that required an ED visit or hospitalization, initiation of an SGLT2 inhibitor was linked with a significant, reduced aRR of 0.52, compared with DPP-4 inhibitor initiation.
- The flare-rate reduction linked with SGLT2 inhibitor use was consistent regardless of sex, age, baseline diuretic use, prior treatment with a urate-lowering agent, and baseline gout intensity.
- SGLT2 inhibitor initiation was also significantly linked with an adjusted reduced hazard ratio of 0.69 in the incidence of myocardial infarction, compared with DPP-4 inhibitor initiation, but stroke incidence was not significantly different between the groups.
IN PRACTICE:
These findings suggest that SGLT2 inhibitors could have a much-needed ability to simultaneously reduce the burden of recurrent gout flares and coronary sequelae in patients with gout and type 2 diabetes, indicating that “SGLT2 inhibitors may offer distinct benefits,” making the drug class “a particularly attractive addition to current urate-lowering therapies,” the researchers write.
SOURCE:
The study was primarily conducted by researchers at Massachusetts General Hospital in Boston. The study was published online July 24 in Annals of Internal Medicine.
LIMITATIONS:
The data used in the study did not include gout flares that did not require medical attention and did not include laboratory findings for study participants. Because the data were observational the findings may be susceptible to unmeasured confounding.
DISCLOSURES:
The study received no commercial funding. One author has reported receiving consulting fees from ANI and LG Chem.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Squamous cell carcinoma
THE COMPARISON
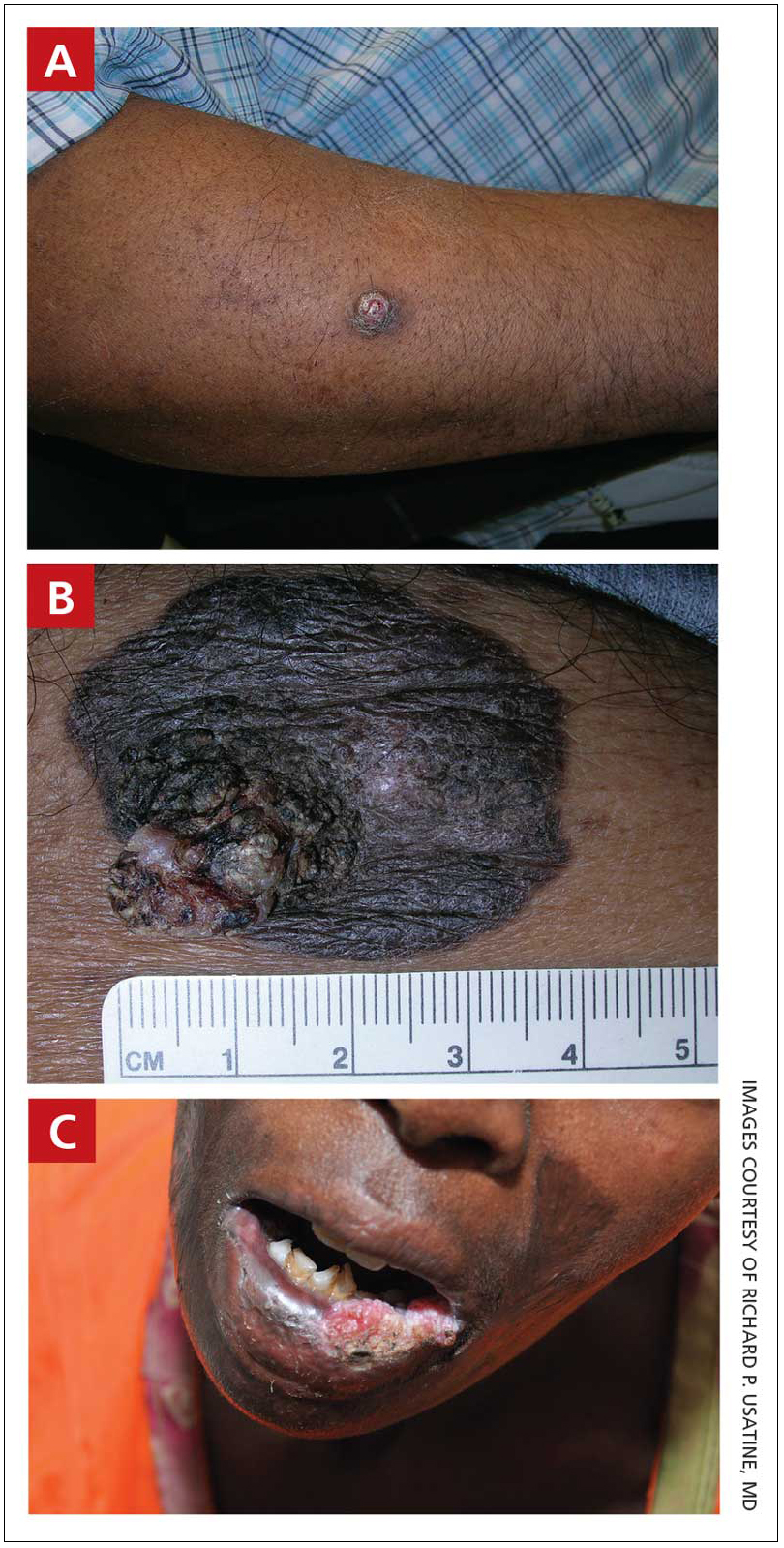
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
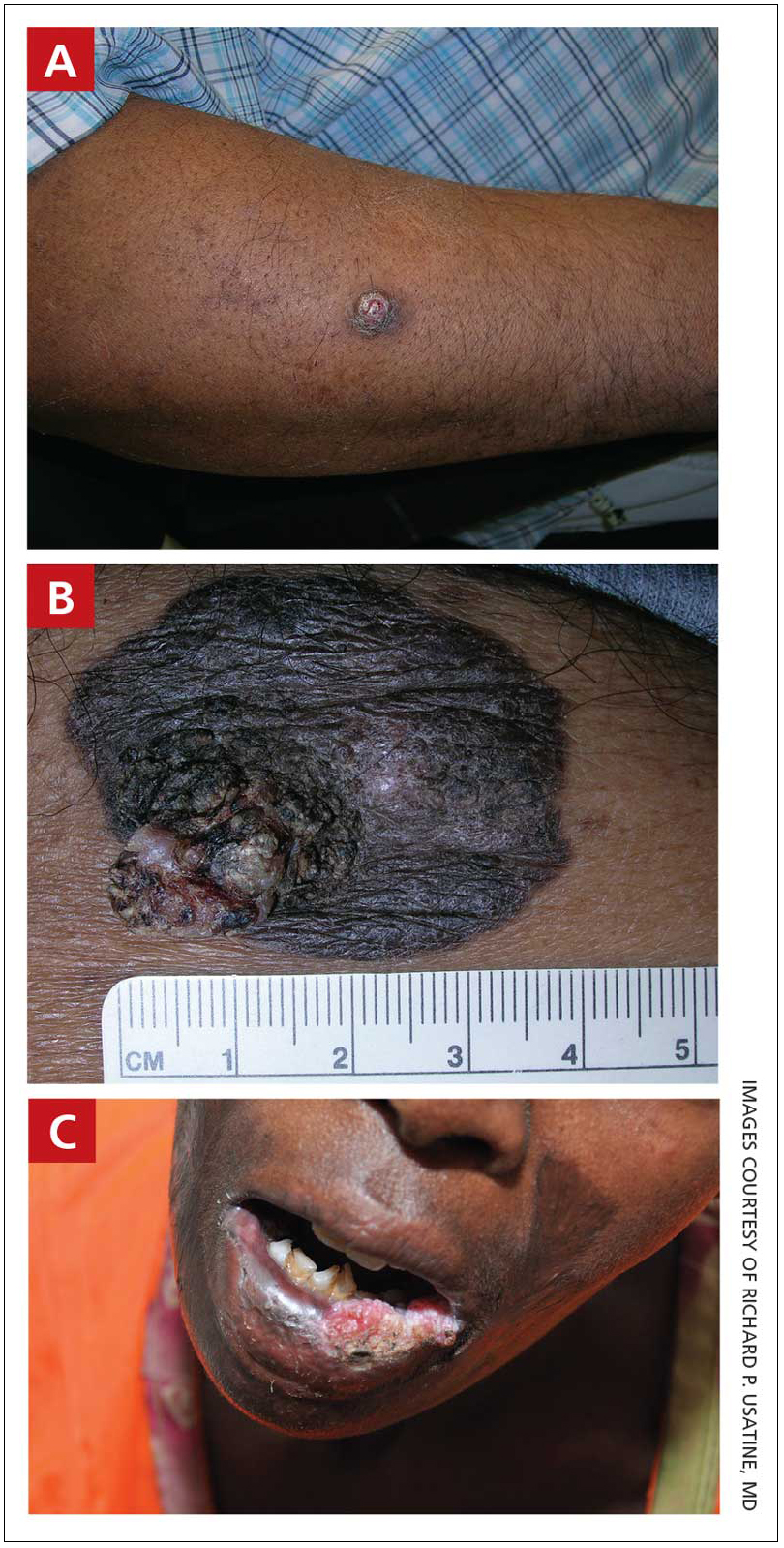
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
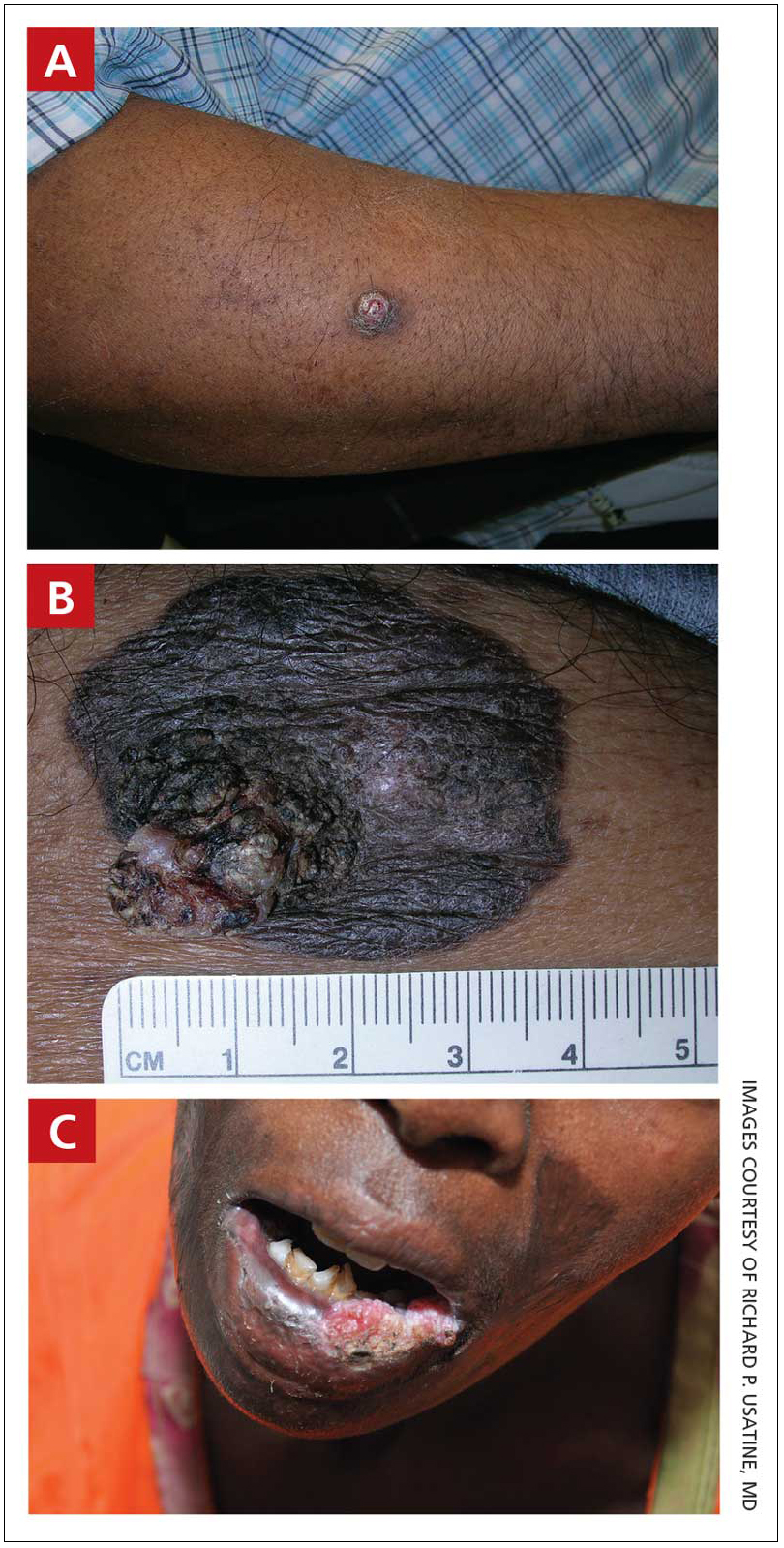
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
THE COMPARISON
A A 51-year-old Hispanic man with a squamous cell carcinoma (SCC) of the keratoacanthoma type on the arm.
B A 75-year-old Black man with an SCC of the keratoacanthoma type on the abdomen.
C An African woman with an SCC on the lower lip decades after a large facial burn, which is known as a Marjolin ulcer.
Cutaneous squamous cell carcinoma (SCC) develops from a malignant tumor of the keratinocytes, eccrine glands, or pilosebaceous units that invades the dermis. Risk factors include lighter skin tone, higher cumulative sun exposure, human papillomavirus (HPV) infection, hidradenitis suppurativa (HS), lichen sclerosus, family history of skin cancer,1 and immunosuppression.2 It typically affects sun-exposed areas of the body such as the face, scalp, neck, and extensor surfaces of the arms (FIGURE A).3,4 However, in those with darker skin tones, the most common anatomic sites are those that are not exposed to the sun (FIGURE B). SCC is diagnosed via skin biopsy. Treatment options include surgical excision, destructive methods such as electrodesiccation and curettage, and Mohs micrographic surgery. Cutaneous SCC has a cure rate of more than 95% and a mortality rate of 1.5% to 2% in the United States.3
Epidemiology
SCC is the most common skin cancer occurring in Black individuals, manifesting primarily in the fifth decade of life.5-7 It is the second most common skin cancer in White, Hispanic, and Asian individuals and is more common in males.8 In a study of organ transplant recipients (N = 413), Pritchett et al9 reported that HPV infection was a major risk factor in Hispanic patients because 66.7% of those with SCC had a history of HPV. However, HPV is a risk factor for SCC in all ethnic groups.10
Key clinical features in people with darker skin tones
Anatomic location
- The lower legs and anogenital areas are the most common sites for SCC in patients with skin of color.4,11
- In Black women, SCC occurs more often on sun-exposed areas such as the arms and legs compared to Black men.7,12-14
- The genitalia, perianal area, ocular mucosa, and oral mucosa are the least likely areas to be routinely examined, even in skin cancer clinics that see highrisk patients, despite the SCC risk in the anogenital area.15,16
- Squamous cell carcinoma of the lips and scalp is more likely to occur in Black women vs Black men.4,7,17
Clinical appearance
- In those with darker skin tones, SCCs may appear hyperpigmented4 or hyperkeratotic with a lack of erythema and an inconsistent appearance.6,7,18
- A nonhealing ulceration of the skin should prompt a biopsy to rule out SCC.3,19
Worth noting
In patients with darker skin tones, the risk for SCC increases in areas with chronic inflammation and scarring of the skin.4,6,7,11,18,20-22 In Black patients, 20% to 40% of cases of SCC occur in the setting of chronic inflammation and scarring.6,7,18 Chronic inflammatory conditions include ulcers, lupus vulgaris, discoid lupus erythematosus, and HPV. In patients with discoid lupus erythematosus, there is an additive effect of sun exposure on the scars, which may play a role in the pathogenesis and metastasis risk for skin cancer in Black patients.4 Other scarring conditions include thermal or chemical burn scars, areas of physical trauma, and prior sites of radiation treatment.14,23 SCC arising in a burn scar is called a Marjolin ulcer or malignant degeneration of a scar (FIGURE C). It is reported more often in lower-income, underresourced countries, which may suggest the need for early detection in populations with skin of color.24
SCC is more aggressive in sites that are not exposed to sun compared to sun-exposed areas.17,25
Continue to: The risk for SCC...
The risk for SCC is increased in immunocompromised patients,2 especially those with HPV.10
The prevalence of SCC in those with HS is approximately 4.6%. The chronic inflammation and irritation from HS in association with other risk factors such as tobacco use may contribute to the malignant transformation to SCC.26
Health disparity highlight
- The risk for metastasis from SCC is 20% to 40% in Black patients vs 1% to 4% in White patients.4,6,27
- Penile SCC was associated with a lower overall survival rate in patients of African descent.20,21
- The increased morbidity and mortality from SCC in patients with skin of color may be attributed to delays in diagnosis and treatment as well as an incomplete understanding of tumor genetics.4,6,18
ACKNOWLEDGMENT
The authors thank Elyse Gadra (Philadelphia, Pennsylvania) for assistance in the preparation of this manuscript.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
1. Asgari MM, Warton EM, Whittemore AS. Family history of skin cancer is associated with increased risk of cutaneous squamous cell carcinoma. Dermatol Surg. 2015;41:481-486. doi: 10.1097/ DSS.0000000000000292
2. Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol. 2000;61:289-297. doi: 10.1002/1096-9071(200007)61:3<289::aidjmv2> 3.0.co;2-z
3. Kallini JR, Nouran H, Khachemoune A. Squamous cell carcinoma of the skin: epidemiology, classification, management, and novel trends. Int J Dermatol. 2015;54:130-140. doi: 10.1111/ijd.12553.
4. Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public J Am Acad Dermatol. 2014;70:748-762. doi: 10.1016/j.jaad.2013.11.038
5. Bradford PT. Skin cancer in skin of color. Dermatol Nurse. 2009;21:170-177.
6. Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol. 2006;55:741-760.
7. Davis DS, Robinson C, Callender VD. Skin cancer in women of color: epidemiology, pathogenesis and clinical manifestations. Int J Womens Dermatol. 2021;7:127-134. doi: 10.1016/ j.ijwd.2021.01.017
8. Baum B, Duarte AM. Skin cancer epidemic in American Hispanic and Latino patients. In: Silverberg N, Duran-McKinster C, Tay Y-K, eds. Pediatric Skin of Color. Springer; 2015:453-460.
9. Pritchett EN, Doyle A, Shaver CM, et al. Nonmelanoma skin cancer in nonwhite organ transplant recipients. JAMA Dermatol. 2016;152: 1348-1353. doi: 10.1001/jamadermatol.2016.3328
10. Karagas MR, Nelson HH, Sehr P, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389-395. doi: 10.1093/jnci/ djj092
11. Gohara M. Skin cancer: an African perspective. Br J Dermatol. 2015;173:17-21. doi: 10.1111/bjd.13380
12. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8-18. doi: 10.1016/ s1011-1344(01)00198-1
13. Halder RM, Bang KM. Skin cancer in African Americans in the United States. Dermatol Clin. 1988;6:397-407.
14. Mora RG, Perniciaro C. Cancer of the skin in blacks. I. a review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535-543. doi: 10.1016/s0190-9622 (81)70113-0
15. Bajaj S, Wolner ZJ, Dusza SW, et al. Total body skin examination practices: a survey study amongst dermatologists at high-risk skin cancer clinics. Dermatol Pract Concept. 2019;9:132-138. doi: 10.5826/dpc.0902a09
16. Rieder EA, Mu EW, Wang J, et al. Dermatologist practices during total body skin examinations: a survey study. J Drugs Dermatol. 2018;17:516-520.
17. Halder RM, Ara CJ. Skin cancer and photoaging in ethnic skin. Dermatol Clin. 2003;21:725-732, x. doi: 10.1016/s0733-8635 (03)00085-8
18. Higgins S, Nazemi A, Chow M, et al. Review of nonmelanoma skin cancer in African Americans, Hispanics, and Asians. Dermatol Surg. 2018;44:903-910.
19. Sng J, Koh D, Siong WC, et al. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61:426-432.
20. Shao K, Feng H. Racial and ethnic healthcare disparities in skin cancer in the United States: a review of existing inequities, contributing factors, and potential solutions. J Clin Aesthet Dermatol. 2022;15:16-22.
21. Shao K, Hooper J, Feng H. Racial and ethnic health disparities in dermatology in the United States. Part 2: disease-specific epidemiology, characteristics, management, and outcomes. J Am Acad Dermatol. 2022;87:733-744. doi: 10.1016/j.jaad.2021. 12.062
22. Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137- 151. doi: 10.1007/s40257-021-00662-z
23. Copcu E, Aktas A, Sis¸man N, et al. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol. 2003;28:138-141. doi: 10.1046/j.1365- 2230.2003.01210.x
24. Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the skin. JCO Glob Oncol. 2020;6:809-818. doi: 10.1200/ GO.20.00094
25. Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi: 10.1016/j.det.2019.05.009
26. Chapman S, Delgadillo D, Barber C, et al. Cutanteous squamous cell complicating hidradenitis suppurativa: a review of the prevalence, pathogenesis, and treatment of this dreaded complication. Acta Dermatovenerol Al Pannocica Adriat. 2018;27:25-28.
27. Kailas A, Botwin AL, Pritchett EN, et al. Assessing the effectiveness of knowledge-based interventions in increasing skin cancer awareness, knowledge, and protective behaviors in skin of color populations. Cutis. 2017;100:235-240.
Reducing Risk for Clostridioides difficile Recurrence
Incidence of C difficile infection has been increasing over the past two decades, accounting for nearly 460,000 cases of illness and 20,000 deaths annually in the United States.
Antibiotic treatment is the standard of care for C difficile infection, but the treatment can disrupt a patient's gastrointestinal microbiome, thereby contributing to the risk for disease recurrence.
Recurrence rates are proven to increase with each episode of C difficile, making prevention essential.
In this ReCAP, Dr David Johnson, of Eastern Virginia Medical School, discusses treatment options to avoid recurrence. He considers multiple means of prevention, including disinfection, infusions of monoclonal antibodies, and the latest advances in fecal microbiota-based biotherapies. Dr Johnson provides data regarding the success rates of pharmaceutical-grade options for prevention of relapse of C difficile.
--
David A. Johnson, MD, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School; Chief of Gastroenterology, Digestive and Liver Disease Specialists, Division of Capital Digestive Care, Norfolk, Virginia
David A. Johnson, MD, has disclosed the following relevant financial relationships:
Serve(d) on a board for: ACG Institute for Clinical Research and Education; Adjudication Board Parexel
Serve(d) as a consultant for: Johnson & Johnson; Isothrive
Received research grant from: ISOThrive
Have a 5% or greater equity interest in: American College of Gastroenterology
Received income in an amount equal to or greater than $250 from: Parexel; Johnson & Johnson
Incidence of C difficile infection has been increasing over the past two decades, accounting for nearly 460,000 cases of illness and 20,000 deaths annually in the United States.
Antibiotic treatment is the standard of care for C difficile infection, but the treatment can disrupt a patient's gastrointestinal microbiome, thereby contributing to the risk for disease recurrence.
Recurrence rates are proven to increase with each episode of C difficile, making prevention essential.
In this ReCAP, Dr David Johnson, of Eastern Virginia Medical School, discusses treatment options to avoid recurrence. He considers multiple means of prevention, including disinfection, infusions of monoclonal antibodies, and the latest advances in fecal microbiota-based biotherapies. Dr Johnson provides data regarding the success rates of pharmaceutical-grade options for prevention of relapse of C difficile.
--
David A. Johnson, MD, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School; Chief of Gastroenterology, Digestive and Liver Disease Specialists, Division of Capital Digestive Care, Norfolk, Virginia
David A. Johnson, MD, has disclosed the following relevant financial relationships:
Serve(d) on a board for: ACG Institute for Clinical Research and Education; Adjudication Board Parexel
Serve(d) as a consultant for: Johnson & Johnson; Isothrive
Received research grant from: ISOThrive
Have a 5% or greater equity interest in: American College of Gastroenterology
Received income in an amount equal to or greater than $250 from: Parexel; Johnson & Johnson
Incidence of C difficile infection has been increasing over the past two decades, accounting for nearly 460,000 cases of illness and 20,000 deaths annually in the United States.
Antibiotic treatment is the standard of care for C difficile infection, but the treatment can disrupt a patient's gastrointestinal microbiome, thereby contributing to the risk for disease recurrence.
Recurrence rates are proven to increase with each episode of C difficile, making prevention essential.
In this ReCAP, Dr David Johnson, of Eastern Virginia Medical School, discusses treatment options to avoid recurrence. He considers multiple means of prevention, including disinfection, infusions of monoclonal antibodies, and the latest advances in fecal microbiota-based biotherapies. Dr Johnson provides data regarding the success rates of pharmaceutical-grade options for prevention of relapse of C difficile.
--
David A. Johnson, MD, Professor of Medicine, Chief of Gastroenterology, Eastern Virginia Medical School; Chief of Gastroenterology, Digestive and Liver Disease Specialists, Division of Capital Digestive Care, Norfolk, Virginia
David A. Johnson, MD, has disclosed the following relevant financial relationships:
Serve(d) on a board for: ACG Institute for Clinical Research and Education; Adjudication Board Parexel
Serve(d) as a consultant for: Johnson & Johnson; Isothrive
Received research grant from: ISOThrive
Have a 5% or greater equity interest in: American College of Gastroenterology
Received income in an amount equal to or greater than $250 from: Parexel; Johnson & Johnson

Study examines burden of vitiligo in the U.S.
To investigate the incidence and prevalence of diagnosed vitiligo in the United States, researchers used a 15% random sample of electronic medical records from the IBM Explorys database. Two cohorts were included: 2,980,778 patients diagnosed with vitiligo between Jan. 1, 2015, and Dec. 31, 2019 (incidence analysis), and 1,057,534 patients diagnosed with vitiligo between Jan. 1 and Dec. 31, 2019 (prevalence analysis).The main outcomes were incidence (per 100,000 person-years) and prevalence of diagnosed vitiligo overall and by age, race/ethnicity, and sex. Amit Garg, MD, a dermatologist with Northwell Health, New Hyde Park, N.Y., led the study, which was published in JAMA Dermatology.
The age- and sex-adjusted overall incidence rate of diagnosed vitiligo was 22.6 per 100,000 person-years, and the prevalence was 0.16%, the authors reported. The sex-adjusted IR was highest among patients aged 60-69 years (25.3 per 100,000 person-years); prevalence was highest among patients aged 70 years or older (0.21%).
The highest age-adjusted IR was among Asian American patients (41.2 per 100,000 person-years), followed by Hispanic/Latino patients (37.3 per 100,000 PY), those reporting other or multiple races (31.1 per 100,000), Black patients (29.6 per 100,000 person-years), and White patients (18.7 per 100,000 person-years). The highest age-adjusted prevalence was among Hispanic/Latino patients (0.29%), followed by Asian American patients (0.27%), those reporting other or multiple races (0.24%), Black patients (0.22%), and White patients (0.13%).
The burden of vitiligo in the United States is poorly understood, and the findings “may support improving awareness of vitiligo disease burden in medical and public sectors, informing research agendas, improving enrollment of racial and ethnic minority populations in trials, and developing health policies,” the authors wrote.
Limitations of the study included that the analysis only captured patients who sought care in health systems included in the database, and there was the potential for underreporting, “since not all patients with vitiligo seek care,” the authors noted.
Dr. Garg reported being an adviser for and receiving honoraria from many pharmaceutical companies. He has also received research grants from AbbVie, UCB, the National Psoriasis Foundation, and the CHORD COUSIN Collaboration. No other disclosures were reported.
A version of this article first appeared on Medscape.com .
To investigate the incidence and prevalence of diagnosed vitiligo in the United States, researchers used a 15% random sample of electronic medical records from the IBM Explorys database. Two cohorts were included: 2,980,778 patients diagnosed with vitiligo between Jan. 1, 2015, and Dec. 31, 2019 (incidence analysis), and 1,057,534 patients diagnosed with vitiligo between Jan. 1 and Dec. 31, 2019 (prevalence analysis).The main outcomes were incidence (per 100,000 person-years) and prevalence of diagnosed vitiligo overall and by age, race/ethnicity, and sex. Amit Garg, MD, a dermatologist with Northwell Health, New Hyde Park, N.Y., led the study, which was published in JAMA Dermatology.
The age- and sex-adjusted overall incidence rate of diagnosed vitiligo was 22.6 per 100,000 person-years, and the prevalence was 0.16%, the authors reported. The sex-adjusted IR was highest among patients aged 60-69 years (25.3 per 100,000 person-years); prevalence was highest among patients aged 70 years or older (0.21%).
The highest age-adjusted IR was among Asian American patients (41.2 per 100,000 person-years), followed by Hispanic/Latino patients (37.3 per 100,000 PY), those reporting other or multiple races (31.1 per 100,000), Black patients (29.6 per 100,000 person-years), and White patients (18.7 per 100,000 person-years). The highest age-adjusted prevalence was among Hispanic/Latino patients (0.29%), followed by Asian American patients (0.27%), those reporting other or multiple races (0.24%), Black patients (0.22%), and White patients (0.13%).
The burden of vitiligo in the United States is poorly understood, and the findings “may support improving awareness of vitiligo disease burden in medical and public sectors, informing research agendas, improving enrollment of racial and ethnic minority populations in trials, and developing health policies,” the authors wrote.
Limitations of the study included that the analysis only captured patients who sought care in health systems included in the database, and there was the potential for underreporting, “since not all patients with vitiligo seek care,” the authors noted.
Dr. Garg reported being an adviser for and receiving honoraria from many pharmaceutical companies. He has also received research grants from AbbVie, UCB, the National Psoriasis Foundation, and the CHORD COUSIN Collaboration. No other disclosures were reported.
A version of this article first appeared on Medscape.com .
To investigate the incidence and prevalence of diagnosed vitiligo in the United States, researchers used a 15% random sample of electronic medical records from the IBM Explorys database. Two cohorts were included: 2,980,778 patients diagnosed with vitiligo between Jan. 1, 2015, and Dec. 31, 2019 (incidence analysis), and 1,057,534 patients diagnosed with vitiligo between Jan. 1 and Dec. 31, 2019 (prevalence analysis).The main outcomes were incidence (per 100,000 person-years) and prevalence of diagnosed vitiligo overall and by age, race/ethnicity, and sex. Amit Garg, MD, a dermatologist with Northwell Health, New Hyde Park, N.Y., led the study, which was published in JAMA Dermatology.
The age- and sex-adjusted overall incidence rate of diagnosed vitiligo was 22.6 per 100,000 person-years, and the prevalence was 0.16%, the authors reported. The sex-adjusted IR was highest among patients aged 60-69 years (25.3 per 100,000 person-years); prevalence was highest among patients aged 70 years or older (0.21%).
The highest age-adjusted IR was among Asian American patients (41.2 per 100,000 person-years), followed by Hispanic/Latino patients (37.3 per 100,000 PY), those reporting other or multiple races (31.1 per 100,000), Black patients (29.6 per 100,000 person-years), and White patients (18.7 per 100,000 person-years). The highest age-adjusted prevalence was among Hispanic/Latino patients (0.29%), followed by Asian American patients (0.27%), those reporting other or multiple races (0.24%), Black patients (0.22%), and White patients (0.13%).
The burden of vitiligo in the United States is poorly understood, and the findings “may support improving awareness of vitiligo disease burden in medical and public sectors, informing research agendas, improving enrollment of racial and ethnic minority populations in trials, and developing health policies,” the authors wrote.
Limitations of the study included that the analysis only captured patients who sought care in health systems included in the database, and there was the potential for underreporting, “since not all patients with vitiligo seek care,” the authors noted.
Dr. Garg reported being an adviser for and receiving honoraria from many pharmaceutical companies. He has also received research grants from AbbVie, UCB, the National Psoriasis Foundation, and the CHORD COUSIN Collaboration. No other disclosures were reported.
A version of this article first appeared on Medscape.com .
FROM JAMA DERMATOLOGY
Rheumatology summit tackles racial disparities in lupus trials
Clinical research in lupus has a mammoth diversity problem: Black individuals are most likely to develop the disease, but they’re the least likely to take part in studies. By the numbers, a 2018 analysis of randomized controlled trials in systemic lupus erythematosus from the years 1997 to 2017 found that 51% of trial participants were White and 14% were Black, even though an estimated 33% of patients with lupus were White and 43% were Black.
Are there ways to fix this disparity? The topic is getting plenty of attention, and speakers at a July 21 online conference touted research projects that aim to boost the numbers of non-White participants in lupus trials.
So far there doesn’t seem to be anything like a magic bullet. Still, the stakes are high. “While race is a social construct, genetic polymorphisms as well as environmental and social differences may influence drugs, safety, and efficacy,” Joy Buie, PhD, MSCR, research director for the Lupus Foundation of America, said at the “Engaging Diverse Participants in Lupus Clinical Trials: The Path Forward” summit held by the American College of Rheumatology (ACR).
As African American patients explained, minority populations often don’t trust the medical system and feel burned by their lengthy struggles to get diagnosed. In some cases, they don’t have full faith in their clinicians and feel unheard.
In a video presentation developed as part of a federal education campaign, Shanelle Gabriel, a poet and musician diagnosed with lupus, described her first reaction when her physician suggested she join a clinical trial. “My first reaction was no. I know my history,” she said, apparently referring to the infamous Tuskegee study that withheld proper treatment from Black men with syphilis for decades. “As an African American woman, I was scared. I didn’t want to be a guinea pig.”
Stacey Kennedy-Conner, a Chicago-area patient and advocate, told the summit audience about how patients can feel that clinical trial information can add “an extra layer of confusion” to their experience. “There’s also the mentality of, ‘If it’s not broke, don’t fix it’: If this medication regimen is working, I don’t want anybody to touch me.”
Monique Gore-Massy, a New York City patient and advocate, added that there can be a perception that patients with lupus “are stuck at home in bed.” In reality, she said, “we have jobs, we have families. Think about that, and consider everything that you’re asking from us: Is this taking me away from my family? Am I going to have to take off work? There may be incentives, but is that worth me taking time off work that I may not get paid for? These are some of the realities that we have to look at in terms of the whole entire clinical trial process.”
It’s also important to keep patients informed of progress being made in trials, she said. “You don’t want to say you just felt like a number and then not get any kind of follow-up.”
In the big picture, “there has to be something that builds up the confidence of individuals so that they are more mindful to participate in these clinical trials,” said Aleta McLean, an Atlanta patient who was diagnosed with lupus 14 years ago.
Several researchers highlighted ongoing projects at the summit. The ACR, for example, has launched a $500,000 initiative called Training to Increase Minority Enrollment in Lupus Clinical Trials with Community Engagement (TIMELY). The federally funded project aims to evaluate whether training of health care professionals can boost clinical trial participation among Black and Hispanic patients.
“We hope to disseminate the results of our project to the scientific community through abstracts, manuscripts, presentations at national meetings,” said rheumatologist Saira Z. Sheikh, MD, of the University of North Carolina at Chapel Hill. “Overall, our goal is to establish new partnerships to support the TIMELY model and advance the education and engagement of providers and community health workers.”
Pamela Payne-Foster, MD, MPH, preventive medicine/public health physician at the University of Alabama College of Community Health Sciences, Tuscaloosa, spoke about the federally funded Deep South Health Equity Project, which is paying patients to take part in an online education program and attend an online regional conference.
Other efforts are underway. The Lupus Research Alliance and its clinical affiliate Lupus Therapeutics have launched two initiatives. One is a program called Project Change (Community-based Health Action Network to Generate Trial Participation and Eliminate Disparities), and the Diversity in Lupus Research Program aims to fund scientists’ work.
Will any of this work boost diversity in clinical trials? As one audience member noted in a Q&A session, health care disparities – and knowledge about them – are nothing new: “Why are we not able to narrow the gap?”
Rear Admiral Richardae Araojo, PharmD, MS, director of the FDA’s Office of Minority Health and Health Equity and associate commissioner for minority health, replied that waves of interest in disparities come and go. “That contributes to why we may not see solutions. But ultimately, there are a lot of people doing a lot of work trying to solve the issues.”
The summit was sponsored by Bristol-Myers Squibb, Genentech, and RemeGen.
A version of this article appeared on Medscape.com.
Clinical research in lupus has a mammoth diversity problem: Black individuals are most likely to develop the disease, but they’re the least likely to take part in studies. By the numbers, a 2018 analysis of randomized controlled trials in systemic lupus erythematosus from the years 1997 to 2017 found that 51% of trial participants were White and 14% were Black, even though an estimated 33% of patients with lupus were White and 43% were Black.
Are there ways to fix this disparity? The topic is getting plenty of attention, and speakers at a July 21 online conference touted research projects that aim to boost the numbers of non-White participants in lupus trials.
So far there doesn’t seem to be anything like a magic bullet. Still, the stakes are high. “While race is a social construct, genetic polymorphisms as well as environmental and social differences may influence drugs, safety, and efficacy,” Joy Buie, PhD, MSCR, research director for the Lupus Foundation of America, said at the “Engaging Diverse Participants in Lupus Clinical Trials: The Path Forward” summit held by the American College of Rheumatology (ACR).
As African American patients explained, minority populations often don’t trust the medical system and feel burned by their lengthy struggles to get diagnosed. In some cases, they don’t have full faith in their clinicians and feel unheard.
In a video presentation developed as part of a federal education campaign, Shanelle Gabriel, a poet and musician diagnosed with lupus, described her first reaction when her physician suggested she join a clinical trial. “My first reaction was no. I know my history,” she said, apparently referring to the infamous Tuskegee study that withheld proper treatment from Black men with syphilis for decades. “As an African American woman, I was scared. I didn’t want to be a guinea pig.”
Stacey Kennedy-Conner, a Chicago-area patient and advocate, told the summit audience about how patients can feel that clinical trial information can add “an extra layer of confusion” to their experience. “There’s also the mentality of, ‘If it’s not broke, don’t fix it’: If this medication regimen is working, I don’t want anybody to touch me.”
Monique Gore-Massy, a New York City patient and advocate, added that there can be a perception that patients with lupus “are stuck at home in bed.” In reality, she said, “we have jobs, we have families. Think about that, and consider everything that you’re asking from us: Is this taking me away from my family? Am I going to have to take off work? There may be incentives, but is that worth me taking time off work that I may not get paid for? These are some of the realities that we have to look at in terms of the whole entire clinical trial process.”
It’s also important to keep patients informed of progress being made in trials, she said. “You don’t want to say you just felt like a number and then not get any kind of follow-up.”
In the big picture, “there has to be something that builds up the confidence of individuals so that they are more mindful to participate in these clinical trials,” said Aleta McLean, an Atlanta patient who was diagnosed with lupus 14 years ago.
Several researchers highlighted ongoing projects at the summit. The ACR, for example, has launched a $500,000 initiative called Training to Increase Minority Enrollment in Lupus Clinical Trials with Community Engagement (TIMELY). The federally funded project aims to evaluate whether training of health care professionals can boost clinical trial participation among Black and Hispanic patients.
“We hope to disseminate the results of our project to the scientific community through abstracts, manuscripts, presentations at national meetings,” said rheumatologist Saira Z. Sheikh, MD, of the University of North Carolina at Chapel Hill. “Overall, our goal is to establish new partnerships to support the TIMELY model and advance the education and engagement of providers and community health workers.”
Pamela Payne-Foster, MD, MPH, preventive medicine/public health physician at the University of Alabama College of Community Health Sciences, Tuscaloosa, spoke about the federally funded Deep South Health Equity Project, which is paying patients to take part in an online education program and attend an online regional conference.
Other efforts are underway. The Lupus Research Alliance and its clinical affiliate Lupus Therapeutics have launched two initiatives. One is a program called Project Change (Community-based Health Action Network to Generate Trial Participation and Eliminate Disparities), and the Diversity in Lupus Research Program aims to fund scientists’ work.
Will any of this work boost diversity in clinical trials? As one audience member noted in a Q&A session, health care disparities – and knowledge about them – are nothing new: “Why are we not able to narrow the gap?”
Rear Admiral Richardae Araojo, PharmD, MS, director of the FDA’s Office of Minority Health and Health Equity and associate commissioner for minority health, replied that waves of interest in disparities come and go. “That contributes to why we may not see solutions. But ultimately, there are a lot of people doing a lot of work trying to solve the issues.”
The summit was sponsored by Bristol-Myers Squibb, Genentech, and RemeGen.
A version of this article appeared on Medscape.com.
Clinical research in lupus has a mammoth diversity problem: Black individuals are most likely to develop the disease, but they’re the least likely to take part in studies. By the numbers, a 2018 analysis of randomized controlled trials in systemic lupus erythematosus from the years 1997 to 2017 found that 51% of trial participants were White and 14% were Black, even though an estimated 33% of patients with lupus were White and 43% were Black.
Are there ways to fix this disparity? The topic is getting plenty of attention, and speakers at a July 21 online conference touted research projects that aim to boost the numbers of non-White participants in lupus trials.
So far there doesn’t seem to be anything like a magic bullet. Still, the stakes are high. “While race is a social construct, genetic polymorphisms as well as environmental and social differences may influence drugs, safety, and efficacy,” Joy Buie, PhD, MSCR, research director for the Lupus Foundation of America, said at the “Engaging Diverse Participants in Lupus Clinical Trials: The Path Forward” summit held by the American College of Rheumatology (ACR).
As African American patients explained, minority populations often don’t trust the medical system and feel burned by their lengthy struggles to get diagnosed. In some cases, they don’t have full faith in their clinicians and feel unheard.
In a video presentation developed as part of a federal education campaign, Shanelle Gabriel, a poet and musician diagnosed with lupus, described her first reaction when her physician suggested she join a clinical trial. “My first reaction was no. I know my history,” she said, apparently referring to the infamous Tuskegee study that withheld proper treatment from Black men with syphilis for decades. “As an African American woman, I was scared. I didn’t want to be a guinea pig.”
Stacey Kennedy-Conner, a Chicago-area patient and advocate, told the summit audience about how patients can feel that clinical trial information can add “an extra layer of confusion” to their experience. “There’s also the mentality of, ‘If it’s not broke, don’t fix it’: If this medication regimen is working, I don’t want anybody to touch me.”
Monique Gore-Massy, a New York City patient and advocate, added that there can be a perception that patients with lupus “are stuck at home in bed.” In reality, she said, “we have jobs, we have families. Think about that, and consider everything that you’re asking from us: Is this taking me away from my family? Am I going to have to take off work? There may be incentives, but is that worth me taking time off work that I may not get paid for? These are some of the realities that we have to look at in terms of the whole entire clinical trial process.”
It’s also important to keep patients informed of progress being made in trials, she said. “You don’t want to say you just felt like a number and then not get any kind of follow-up.”
In the big picture, “there has to be something that builds up the confidence of individuals so that they are more mindful to participate in these clinical trials,” said Aleta McLean, an Atlanta patient who was diagnosed with lupus 14 years ago.
Several researchers highlighted ongoing projects at the summit. The ACR, for example, has launched a $500,000 initiative called Training to Increase Minority Enrollment in Lupus Clinical Trials with Community Engagement (TIMELY). The federally funded project aims to evaluate whether training of health care professionals can boost clinical trial participation among Black and Hispanic patients.
“We hope to disseminate the results of our project to the scientific community through abstracts, manuscripts, presentations at national meetings,” said rheumatologist Saira Z. Sheikh, MD, of the University of North Carolina at Chapel Hill. “Overall, our goal is to establish new partnerships to support the TIMELY model and advance the education and engagement of providers and community health workers.”
Pamela Payne-Foster, MD, MPH, preventive medicine/public health physician at the University of Alabama College of Community Health Sciences, Tuscaloosa, spoke about the federally funded Deep South Health Equity Project, which is paying patients to take part in an online education program and attend an online regional conference.
Other efforts are underway. The Lupus Research Alliance and its clinical affiliate Lupus Therapeutics have launched two initiatives. One is a program called Project Change (Community-based Health Action Network to Generate Trial Participation and Eliminate Disparities), and the Diversity in Lupus Research Program aims to fund scientists’ work.
Will any of this work boost diversity in clinical trials? As one audience member noted in a Q&A session, health care disparities – and knowledge about them – are nothing new: “Why are we not able to narrow the gap?”
Rear Admiral Richardae Araojo, PharmD, MS, director of the FDA’s Office of Minority Health and Health Equity and associate commissioner for minority health, replied that waves of interest in disparities come and go. “That contributes to why we may not see solutions. But ultimately, there are a lot of people doing a lot of work trying to solve the issues.”
The summit was sponsored by Bristol-Myers Squibb, Genentech, and RemeGen.
A version of this article appeared on Medscape.com.
FROM AN ACR CLINICAL TRIAL SUMMIT
Kidnapping and treatment risks come with medical tourism
In March 2023, four “medical tourists” from South Carolina who were seeking health care in Mexico were kidnapped by a drug cartel. Two were killed when they were trapped in a shootout. One of them was scheduled for tummy-tuck surgery, and others were seeking cheaper prescription drugs.
The news reached Bruce Hermann, MD, a plastic surgeon in Denton, Tex., who brought up the incident in a segment of his podcast, “Nip Talk,” in which he talked about the risks of medical tourism. But violence in foreign countries isn’t Dr. Hermann’s primary concern.
“Being the victim of a crime is lower down the risk strata,” Dr. Hermann said in an interview. “A bigger concern is the lack of regulations of doctors and facilities in countries like Mexico.”
Some employers pay for treatment at certain foreign clinics, and Blue Shield of California’s HMO plan, Access Baja, covers care in certain clinics in Mexico’s Baja peninsula. But U.S. health insurance generally does not cover medical tourism.
Despite its popularity, medical tourism is not siphoning off a significant number of patients from U.S. doctors, with the possible exception of plastic surgery. One study found that medical tourism accounts for less than 2% of U.S. spending on noncosmetic health care.
Still, as many as 1.2 million Americans travel to Mexico each year seeking health care at lower costs, particularly dental care, bariatric surgery, and cosmetic procedures.
Physicians such as Dr. Hermann see the results when things go awry. Dr. Hermann said when he takes calls at a nearby level II trauma center, he sees, on average, one patient a month with complications from plastic surgeries performed abroad.
Patients tell Dr. Hermann they often had little preoperative time with the surgeons, and some may not even see their surgeon. They have to fly back home just days after their procedures, so complications that typically arise later are missed, he said.
Who opts for medical tourism?
There are few statistics on the number of medical tourists or the clinical problems they have. Josef Woodman, CEO of Patients Beyond Borders, a medical tourism consultancy in Chapel Hill, N.C., has developed a profile of medical tourism that is based on his close contacts within the industry.
Mr. Woodman said the vast majority of U.S. medical tourists go to Mexico, which accounts for an estimated 1 million to 1.2 million medical visitors a year. He said Costa Rica is another popular destination, followed by other Latin American countries and some in the Far East, the Middle East, and Eastern Europe.
Mr. Woodman estimates that dental treatments make up 65% of all medical tourism. Cosmetic procedures come in a distant second, at 15%. Cosmetic procedures can be expensive and are rarely covered by insurance. They can be performed at half the price abroad, he said.
According to Mr. Woodman, other significant fields for medical tourism are orthopedics, which accounts for 5% of all visits, and bariatrics, with 3%-5%. Hip and knee replacements are expensive, and in the case of bariatrics, U.S. insurers often deny coverage, he said.
People also go abroad for fertility care and organ transplants, and one Jamaica company even offered dialysis vacations for U.S. tourists.
On the other hand, medical tourism does not work well for cancer treatments, because cancer care involves long periods of treatment and cannot be completed in a trip or two, Mr. Woodman said. “The media also plays up major procedures like open heart surgery, but they are in fact very rare,” he added.
What patients are looking for
Medical tourists typically pay 50%-70% of what they would pay in the United States for the same procedure, Mr. Woodman said. Prices are lower because patients pay in cash, foreign wages are lower, and expenses such as malpractice insurance are much lower.
“Many medical tourists don’t have a choice,” Mr. Woodman said. “They cannot afford the U.S. price for the procedure, even if they have health insurance, because they often have a high deductible.” In one study, the majority of medical tourists to Mexico reported an income of $25,000-$50,000 a year.
That same study also found that the average age of medical tourists was just under 65. These older patients often come for a vacation. “A sizable number of medical tourists are looking for surgery plus a vacation, a tummy-tuck and a stay at an all-inclusive resort,” said Steven P. Davison, MD, DDS, a plastic surgeon in Washington, who has written on the phenomenon.
Another large group of medical tourists are immigrants to the United States who want surgery in their country of origin, such as Brazil or Iran, Dr. Davison said, perhaps because they feel more comfortable or have family members who can act as caregivers. He said some go to places that have expertise in a certain procedure.
“For instance, they get their hair transplantation done in Turkey because surgeons there have the expertise and it’s cheaper than in the United States,” Dr. Davison said.
Arranging the trip
Patients often find foreign providers through online brokers who can arrange the flight, hotel, clinic, and physician. Brokers are not unbiased because they are usually paid by the clinic. Mr. Woodman said this arrangement works when the broker can offer a wide variety of options but not when the broker represents just a few clinics.
Mr. Woodman said patients could conceivably make their own arrangements without a broker, and some do so. “All the tools are on the Internet,” he said. “However, many people don’t trust themselves to do this work.”
Even for patients who depend on brokers, Mr. Woodman advises verifying the quality of the clinic and its doctors before signing on. Most countries have online lists of registered doctors, and patients seeking health care can research complaints against a doctor.
There is no insurance that patients can have to guard against the risks of medical tourism, Mr. Woodman said. “When you could get it, it was prohibitively expensive,” he said. “You can get travel insurance, but that just covers peripheral problems, such as flight cancellations, accidental injury, and emergency care. It has nothing to do with problems stemming from planned procedures.
“Some clinics and hospitals serving medical tourists provide warranties on their work,” he added. “However, plastic surgery clinics are less likely to offer warranties, because patients are so frequently dissatisfied.”
How things can go wrong
Mr. Woodman said medical tourists may often receive substandard care when they select a provider who offers unusually large savings, such as 80% off the U.S. price. “Those providers are likely cutting corners to get that kind of savings, and you should stay away from them,” he said.
Even when receiving care at an excellent clinic, patients can get infections if postoperative requirements are not followed, according to Darrick E. Antell, MD, a plastic surgeon in New York, who has treated medical tourists upon their return to the United States.
Typically, patients are told to stay in their rooms for several days after the operation, but friends may push them to go out and have fun, he said. Sometimes patients choose exotic arrangements that place them at risk for infection. As an example, Dr. Antell mentioned a broker who offered a safari in combination with plastic surgery.
Dr. Hermann said tummy tucks are riskier because they involve large incisions, and many such patients are overweight, which impairs healing. “Tummy-tuck patients need a longer recovery, and they often have more discomfort than other plastic surgery,” he said.
When things go wrong, medical tourists have few legal protections. “They usually don’t go to an accredited facility, there is no credentialing of physicians, and their ability to sue is extremely limited,” Dr. Davison said. Patients would have to return to the foreign country and hire a lawyer there, and even then, it is harder to win a case and to receive an award as high as in the United States, he added.
Dealing with follow-ups
An inherent flaw with medical tourism, Dr. Antell said, is that patients typically go back home before postoperative care is fully completed. “They may stay just a few days after surgery, and then fly back home,” he said.
“Patients who have complex operations abroad should stay for 8-10 days to have a proper follow-up,” he said. “But they fly back early, which can also lead to getting pulmonary embolisms on the flight.
“A checkup right after surgery doesn’t uncover many complications, because these tend to occur 7-12 days after surgery,” Dr. Hermann said.
“If they come to me within 3 months after surgery, I charge an upfront fee just to see them, because it takes an hour of my time,” Dr. Davison said. “Then I will take care of acute emergency, such as taking out an infected implant.”
Hermann said many patients wait too long to have their complications treated in the United States. “They may first try calling their doctor in Mexico, who tells them to take some antibiotics or something,” he said. “So when they finally do seek care, the infection is pretty far along.”
What U.S. doctors can do
Patients rarely tell their U.S. doctors that they are planning a trip to a foreign country to undergo medical treatment, even though they have to request a copy of their medical records for the foreign doctor, Mr. Woodman said.
Dr. Hermann said only one of his patients told him she was planning to go aboard for plastic surgery. “She was a young mom, and I tried to talk her out of it,” he said. “I don’t know what happened because she didn’t come back.”
Dr. Hermann said doctors should assume that they won’t be able to change their patients’ minds, and they should try to help their patients make the best of it.
“They should insist on seeing the doctor ahead of time and make sure they get along with them,” he said. “Ask for credentialing of the doctor and the facility, and stay there several weeks post op. But they’re probably not going to do all of this.”
A version of this article first appeared on Medscape.com.
In March 2023, four “medical tourists” from South Carolina who were seeking health care in Mexico were kidnapped by a drug cartel. Two were killed when they were trapped in a shootout. One of them was scheduled for tummy-tuck surgery, and others were seeking cheaper prescription drugs.
The news reached Bruce Hermann, MD, a plastic surgeon in Denton, Tex., who brought up the incident in a segment of his podcast, “Nip Talk,” in which he talked about the risks of medical tourism. But violence in foreign countries isn’t Dr. Hermann’s primary concern.
“Being the victim of a crime is lower down the risk strata,” Dr. Hermann said in an interview. “A bigger concern is the lack of regulations of doctors and facilities in countries like Mexico.”
Some employers pay for treatment at certain foreign clinics, and Blue Shield of California’s HMO plan, Access Baja, covers care in certain clinics in Mexico’s Baja peninsula. But U.S. health insurance generally does not cover medical tourism.
Despite its popularity, medical tourism is not siphoning off a significant number of patients from U.S. doctors, with the possible exception of plastic surgery. One study found that medical tourism accounts for less than 2% of U.S. spending on noncosmetic health care.
Still, as many as 1.2 million Americans travel to Mexico each year seeking health care at lower costs, particularly dental care, bariatric surgery, and cosmetic procedures.
Physicians such as Dr. Hermann see the results when things go awry. Dr. Hermann said when he takes calls at a nearby level II trauma center, he sees, on average, one patient a month with complications from plastic surgeries performed abroad.
Patients tell Dr. Hermann they often had little preoperative time with the surgeons, and some may not even see their surgeon. They have to fly back home just days after their procedures, so complications that typically arise later are missed, he said.
Who opts for medical tourism?
There are few statistics on the number of medical tourists or the clinical problems they have. Josef Woodman, CEO of Patients Beyond Borders, a medical tourism consultancy in Chapel Hill, N.C., has developed a profile of medical tourism that is based on his close contacts within the industry.
Mr. Woodman said the vast majority of U.S. medical tourists go to Mexico, which accounts for an estimated 1 million to 1.2 million medical visitors a year. He said Costa Rica is another popular destination, followed by other Latin American countries and some in the Far East, the Middle East, and Eastern Europe.
Mr. Woodman estimates that dental treatments make up 65% of all medical tourism. Cosmetic procedures come in a distant second, at 15%. Cosmetic procedures can be expensive and are rarely covered by insurance. They can be performed at half the price abroad, he said.
According to Mr. Woodman, other significant fields for medical tourism are orthopedics, which accounts for 5% of all visits, and bariatrics, with 3%-5%. Hip and knee replacements are expensive, and in the case of bariatrics, U.S. insurers often deny coverage, he said.
People also go abroad for fertility care and organ transplants, and one Jamaica company even offered dialysis vacations for U.S. tourists.
On the other hand, medical tourism does not work well for cancer treatments, because cancer care involves long periods of treatment and cannot be completed in a trip or two, Mr. Woodman said. “The media also plays up major procedures like open heart surgery, but they are in fact very rare,” he added.
What patients are looking for
Medical tourists typically pay 50%-70% of what they would pay in the United States for the same procedure, Mr. Woodman said. Prices are lower because patients pay in cash, foreign wages are lower, and expenses such as malpractice insurance are much lower.
“Many medical tourists don’t have a choice,” Mr. Woodman said. “They cannot afford the U.S. price for the procedure, even if they have health insurance, because they often have a high deductible.” In one study, the majority of medical tourists to Mexico reported an income of $25,000-$50,000 a year.
That same study also found that the average age of medical tourists was just under 65. These older patients often come for a vacation. “A sizable number of medical tourists are looking for surgery plus a vacation, a tummy-tuck and a stay at an all-inclusive resort,” said Steven P. Davison, MD, DDS, a plastic surgeon in Washington, who has written on the phenomenon.
Another large group of medical tourists are immigrants to the United States who want surgery in their country of origin, such as Brazil or Iran, Dr. Davison said, perhaps because they feel more comfortable or have family members who can act as caregivers. He said some go to places that have expertise in a certain procedure.
“For instance, they get their hair transplantation done in Turkey because surgeons there have the expertise and it’s cheaper than in the United States,” Dr. Davison said.
Arranging the trip
Patients often find foreign providers through online brokers who can arrange the flight, hotel, clinic, and physician. Brokers are not unbiased because they are usually paid by the clinic. Mr. Woodman said this arrangement works when the broker can offer a wide variety of options but not when the broker represents just a few clinics.
Mr. Woodman said patients could conceivably make their own arrangements without a broker, and some do so. “All the tools are on the Internet,” he said. “However, many people don’t trust themselves to do this work.”
Even for patients who depend on brokers, Mr. Woodman advises verifying the quality of the clinic and its doctors before signing on. Most countries have online lists of registered doctors, and patients seeking health care can research complaints against a doctor.
There is no insurance that patients can have to guard against the risks of medical tourism, Mr. Woodman said. “When you could get it, it was prohibitively expensive,” he said. “You can get travel insurance, but that just covers peripheral problems, such as flight cancellations, accidental injury, and emergency care. It has nothing to do with problems stemming from planned procedures.
“Some clinics and hospitals serving medical tourists provide warranties on their work,” he added. “However, plastic surgery clinics are less likely to offer warranties, because patients are so frequently dissatisfied.”
How things can go wrong
Mr. Woodman said medical tourists may often receive substandard care when they select a provider who offers unusually large savings, such as 80% off the U.S. price. “Those providers are likely cutting corners to get that kind of savings, and you should stay away from them,” he said.
Even when receiving care at an excellent clinic, patients can get infections if postoperative requirements are not followed, according to Darrick E. Antell, MD, a plastic surgeon in New York, who has treated medical tourists upon their return to the United States.
Typically, patients are told to stay in their rooms for several days after the operation, but friends may push them to go out and have fun, he said. Sometimes patients choose exotic arrangements that place them at risk for infection. As an example, Dr. Antell mentioned a broker who offered a safari in combination with plastic surgery.
Dr. Hermann said tummy tucks are riskier because they involve large incisions, and many such patients are overweight, which impairs healing. “Tummy-tuck patients need a longer recovery, and they often have more discomfort than other plastic surgery,” he said.
When things go wrong, medical tourists have few legal protections. “They usually don’t go to an accredited facility, there is no credentialing of physicians, and their ability to sue is extremely limited,” Dr. Davison said. Patients would have to return to the foreign country and hire a lawyer there, and even then, it is harder to win a case and to receive an award as high as in the United States, he added.
Dealing with follow-ups
An inherent flaw with medical tourism, Dr. Antell said, is that patients typically go back home before postoperative care is fully completed. “They may stay just a few days after surgery, and then fly back home,” he said.
“Patients who have complex operations abroad should stay for 8-10 days to have a proper follow-up,” he said. “But they fly back early, which can also lead to getting pulmonary embolisms on the flight.
“A checkup right after surgery doesn’t uncover many complications, because these tend to occur 7-12 days after surgery,” Dr. Hermann said.
“If they come to me within 3 months after surgery, I charge an upfront fee just to see them, because it takes an hour of my time,” Dr. Davison said. “Then I will take care of acute emergency, such as taking out an infected implant.”
Hermann said many patients wait too long to have their complications treated in the United States. “They may first try calling their doctor in Mexico, who tells them to take some antibiotics or something,” he said. “So when they finally do seek care, the infection is pretty far along.”
What U.S. doctors can do
Patients rarely tell their U.S. doctors that they are planning a trip to a foreign country to undergo medical treatment, even though they have to request a copy of their medical records for the foreign doctor, Mr. Woodman said.
Dr. Hermann said only one of his patients told him she was planning to go aboard for plastic surgery. “She was a young mom, and I tried to talk her out of it,” he said. “I don’t know what happened because she didn’t come back.”
Dr. Hermann said doctors should assume that they won’t be able to change their patients’ minds, and they should try to help their patients make the best of it.
“They should insist on seeing the doctor ahead of time and make sure they get along with them,” he said. “Ask for credentialing of the doctor and the facility, and stay there several weeks post op. But they’re probably not going to do all of this.”
A version of this article first appeared on Medscape.com.
In March 2023, four “medical tourists” from South Carolina who were seeking health care in Mexico were kidnapped by a drug cartel. Two were killed when they were trapped in a shootout. One of them was scheduled for tummy-tuck surgery, and others were seeking cheaper prescription drugs.
The news reached Bruce Hermann, MD, a plastic surgeon in Denton, Tex., who brought up the incident in a segment of his podcast, “Nip Talk,” in which he talked about the risks of medical tourism. But violence in foreign countries isn’t Dr. Hermann’s primary concern.
“Being the victim of a crime is lower down the risk strata,” Dr. Hermann said in an interview. “A bigger concern is the lack of regulations of doctors and facilities in countries like Mexico.”
Some employers pay for treatment at certain foreign clinics, and Blue Shield of California’s HMO plan, Access Baja, covers care in certain clinics in Mexico’s Baja peninsula. But U.S. health insurance generally does not cover medical tourism.
Despite its popularity, medical tourism is not siphoning off a significant number of patients from U.S. doctors, with the possible exception of plastic surgery. One study found that medical tourism accounts for less than 2% of U.S. spending on noncosmetic health care.
Still, as many as 1.2 million Americans travel to Mexico each year seeking health care at lower costs, particularly dental care, bariatric surgery, and cosmetic procedures.
Physicians such as Dr. Hermann see the results when things go awry. Dr. Hermann said when he takes calls at a nearby level II trauma center, he sees, on average, one patient a month with complications from plastic surgeries performed abroad.
Patients tell Dr. Hermann they often had little preoperative time with the surgeons, and some may not even see their surgeon. They have to fly back home just days after their procedures, so complications that typically arise later are missed, he said.
Who opts for medical tourism?
There are few statistics on the number of medical tourists or the clinical problems they have. Josef Woodman, CEO of Patients Beyond Borders, a medical tourism consultancy in Chapel Hill, N.C., has developed a profile of medical tourism that is based on his close contacts within the industry.
Mr. Woodman said the vast majority of U.S. medical tourists go to Mexico, which accounts for an estimated 1 million to 1.2 million medical visitors a year. He said Costa Rica is another popular destination, followed by other Latin American countries and some in the Far East, the Middle East, and Eastern Europe.
Mr. Woodman estimates that dental treatments make up 65% of all medical tourism. Cosmetic procedures come in a distant second, at 15%. Cosmetic procedures can be expensive and are rarely covered by insurance. They can be performed at half the price abroad, he said.
According to Mr. Woodman, other significant fields for medical tourism are orthopedics, which accounts for 5% of all visits, and bariatrics, with 3%-5%. Hip and knee replacements are expensive, and in the case of bariatrics, U.S. insurers often deny coverage, he said.
People also go abroad for fertility care and organ transplants, and one Jamaica company even offered dialysis vacations for U.S. tourists.
On the other hand, medical tourism does not work well for cancer treatments, because cancer care involves long periods of treatment and cannot be completed in a trip or two, Mr. Woodman said. “The media also plays up major procedures like open heart surgery, but they are in fact very rare,” he added.
What patients are looking for
Medical tourists typically pay 50%-70% of what they would pay in the United States for the same procedure, Mr. Woodman said. Prices are lower because patients pay in cash, foreign wages are lower, and expenses such as malpractice insurance are much lower.
“Many medical tourists don’t have a choice,” Mr. Woodman said. “They cannot afford the U.S. price for the procedure, even if they have health insurance, because they often have a high deductible.” In one study, the majority of medical tourists to Mexico reported an income of $25,000-$50,000 a year.
That same study also found that the average age of medical tourists was just under 65. These older patients often come for a vacation. “A sizable number of medical tourists are looking for surgery plus a vacation, a tummy-tuck and a stay at an all-inclusive resort,” said Steven P. Davison, MD, DDS, a plastic surgeon in Washington, who has written on the phenomenon.
Another large group of medical tourists are immigrants to the United States who want surgery in their country of origin, such as Brazil or Iran, Dr. Davison said, perhaps because they feel more comfortable or have family members who can act as caregivers. He said some go to places that have expertise in a certain procedure.
“For instance, they get their hair transplantation done in Turkey because surgeons there have the expertise and it’s cheaper than in the United States,” Dr. Davison said.
Arranging the trip
Patients often find foreign providers through online brokers who can arrange the flight, hotel, clinic, and physician. Brokers are not unbiased because they are usually paid by the clinic. Mr. Woodman said this arrangement works when the broker can offer a wide variety of options but not when the broker represents just a few clinics.
Mr. Woodman said patients could conceivably make their own arrangements without a broker, and some do so. “All the tools are on the Internet,” he said. “However, many people don’t trust themselves to do this work.”
Even for patients who depend on brokers, Mr. Woodman advises verifying the quality of the clinic and its doctors before signing on. Most countries have online lists of registered doctors, and patients seeking health care can research complaints against a doctor.
There is no insurance that patients can have to guard against the risks of medical tourism, Mr. Woodman said. “When you could get it, it was prohibitively expensive,” he said. “You can get travel insurance, but that just covers peripheral problems, such as flight cancellations, accidental injury, and emergency care. It has nothing to do with problems stemming from planned procedures.
“Some clinics and hospitals serving medical tourists provide warranties on their work,” he added. “However, plastic surgery clinics are less likely to offer warranties, because patients are so frequently dissatisfied.”
How things can go wrong
Mr. Woodman said medical tourists may often receive substandard care when they select a provider who offers unusually large savings, such as 80% off the U.S. price. “Those providers are likely cutting corners to get that kind of savings, and you should stay away from them,” he said.
Even when receiving care at an excellent clinic, patients can get infections if postoperative requirements are not followed, according to Darrick E. Antell, MD, a plastic surgeon in New York, who has treated medical tourists upon their return to the United States.
Typically, patients are told to stay in their rooms for several days after the operation, but friends may push them to go out and have fun, he said. Sometimes patients choose exotic arrangements that place them at risk for infection. As an example, Dr. Antell mentioned a broker who offered a safari in combination with plastic surgery.
Dr. Hermann said tummy tucks are riskier because they involve large incisions, and many such patients are overweight, which impairs healing. “Tummy-tuck patients need a longer recovery, and they often have more discomfort than other plastic surgery,” he said.
When things go wrong, medical tourists have few legal protections. “They usually don’t go to an accredited facility, there is no credentialing of physicians, and their ability to sue is extremely limited,” Dr. Davison said. Patients would have to return to the foreign country and hire a lawyer there, and even then, it is harder to win a case and to receive an award as high as in the United States, he added.
Dealing with follow-ups
An inherent flaw with medical tourism, Dr. Antell said, is that patients typically go back home before postoperative care is fully completed. “They may stay just a few days after surgery, and then fly back home,” he said.
“Patients who have complex operations abroad should stay for 8-10 days to have a proper follow-up,” he said. “But they fly back early, which can also lead to getting pulmonary embolisms on the flight.
“A checkup right after surgery doesn’t uncover many complications, because these tend to occur 7-12 days after surgery,” Dr. Hermann said.
“If they come to me within 3 months after surgery, I charge an upfront fee just to see them, because it takes an hour of my time,” Dr. Davison said. “Then I will take care of acute emergency, such as taking out an infected implant.”
Hermann said many patients wait too long to have their complications treated in the United States. “They may first try calling their doctor in Mexico, who tells them to take some antibiotics or something,” he said. “So when they finally do seek care, the infection is pretty far along.”
What U.S. doctors can do
Patients rarely tell their U.S. doctors that they are planning a trip to a foreign country to undergo medical treatment, even though they have to request a copy of their medical records for the foreign doctor, Mr. Woodman said.
Dr. Hermann said only one of his patients told him she was planning to go aboard for plastic surgery. “She was a young mom, and I tried to talk her out of it,” he said. “I don’t know what happened because she didn’t come back.”
Dr. Hermann said doctors should assume that they won’t be able to change their patients’ minds, and they should try to help their patients make the best of it.
“They should insist on seeing the doctor ahead of time and make sure they get along with them,” he said. “Ask for credentialing of the doctor and the facility, and stay there several weeks post op. But they’re probably not going to do all of this.”
A version of this article first appeared on Medscape.com.
Chaperones for physical exams? Doctors and patients weigh in
News of physicians accused or convicted of sexually inappropriate behavior toward patients during medical exams has been frequent recently. And patient advocates have brought up the fact that many patients are uncomfortable during sensitive exams.
As a result, more
For some institutions, the movement has been toward mandating chaperones. Chaperones can be present for any examination of what are often referred to as sensitive areas, such as breasts, genitalia, and the perianal area. For example, Yale University Health requires patients to use a medical staff member as a chaperone for all sensitive exams except in emergency situations. UCLA Health, on the other hand, allows any adult or child aged 12 years or older to decline a chaperone if they wish to do so. Michigan Medicine provides a chaperone on request, although a patient can opt out.
Many physicians fully support the concept. “If a patient requests a chaperone I think we all, as practitioners, should honor that request respectfully,” said Shieva Ghofrany, MD, an ob.gyn. practicing in Stamford, Conn., and cofounder of tribecalledv, a women’s health knowledge platform. “It’s a clear sign a patient wants to ensure that they feel safe and comfortable.”
However, using a chaperone can be challenging for many primary care physicians and specialists in terms of logistics. Should a chaperone’s job be purely observational? Or should the chaperone also be a medical professional who assists during the procedure? How, specifically, should a chaperone perform their duty during an exam? Where should the chaperone stand? What about legal and ethical ramifications?
Who should be a chaperone?
The role of a chaperone is sometimes vaguely defined. It’s logical that a chaperone should have sufficient medical knowledge. Could it be a medical student? Should it be a nurse or another doctor? Would a patient representative suffice even if they aren’t a direct-care clinician?
There are no set standards about who can assume the role. However, the American Medical Association recommends that a patient chaperone be an authorized member of a health care team. For many patients, this is vital.
“As a survivor of sexual assault by an ob.gyn. while I was pregnant, I can assure you that the heinous crime committed against me and hundreds of other women would have been prevented had there been another medical professional in the room,” said Laurie Kanyok, founder of a dance company in New York City, whose former doctor was recently convicted of federal sex abuse charges and is scheduled to be sentenced in July 2023. “The chaperone should be a physician assistant, nurse or medical professional. Qualified professionals better understand the nature and protocols of an exam.”
For children and adolescents, allowing a parent to be a chaperone might be a logical and comforting choice. However, a new British study found that it’s not appropriate.
Study authors Rebecca Jane Moon and Justin Huw Davies looked at pubertal staging–related exams and contend that a chaperone should always be impartial, and a parent’s presence could conceivably open up a physician to false charges of misconduct.
The solution: A parent should have the option be present during any physical exam of their child, with a medical professional additionally acting as chaperone. This can also work for any patient who wishes to bring a trusted friend or family member to their medical appointments.
How does a chaperoned exam work?
A research team from the Medical College of Wisconsin and Louisiana State University Health conducted a recent systematic review of patient and clinician perspectives on carrying out a chaperoned urology exam. The review found that the protocol could use improvement. For example, it was reported that over one-quarter of patients didn’t feel comfortable asking for a chaperone if they were not offered one. “Patients should not have to request this,” said Diana Londoño, MD, a board-certified urologist and assistant clinical professor at City of Hope National Medical Center in Duarte, Calif.
The researchers also found that 93% of female patients preferred a chaperone of the same gender, whereas male patients were split on this issue. Key duties of a chaperone should be to ensure privacy, help interpret instructions from doctor to patient, and continually clarify that consent is being requested as a sensitive exam proceeds, the researchers report. Although clinical practice standards for chaperones aren’t uniform, keeping these important points in mind can easily be adopted by any health care provider.
Many doctors do follow their own set guidelines. “Often, we have our medical assistants be our chaperones,” explained Dr. Ghofrany. “Ideally they ‘room’ the patient – take vitals and ask the patient what specific concerns they would like to address. This helps with exam set-up.
“For example, if a patient has a breast concern versus a concern about their genital area, this would change what drapes are used. The medical assistant would then stand near me if they are helping with a Pap smear or cultures, or they may stand by the patient’s head at the bedside and offer support if needed. Some patients want to hold someone’s hand during an uncomfortable exam.”
The issue of positioning is important. A patient may feel very uneasy if it appears that the chaperone is looking at their body from the doctor’s angle, negating the point of reassurance. The key is to explain before an exam exactly how a chaperone is needed during the exam itself and whether the chaperone is a medical assistant or nurse.
“Chaperones usually stand next to me on either side or on the side of the patient facing me, depending on if they are immediately assisting me or helping the patient,” said Dr. Londoño. If a chaperone will be moving back and forth during the exam, that should be conveyed as well. For virtual visits, a chaperone can act as a third party and be present on a split screen, a process Michigan Medicine uses.
It’s also important to inform patients that a chaperone can step in and stop an exam at any point, both at the patient’s request or because of any observation of inappropriate physician behavior. Understanding this can help reluctant patients feel less worry.
When Christian Miller was diagnosed with a sleep disorder, his doctor suggested having a chaperone present during his physical exams. At first, he was apprehensive but then found the experience to be very positive. “Having someone there with me gave me an extra measure of assurance that nothing untoward would happen,” he said. “I found that having a chaperone was reassuring. The chaperone was not intrusive but stood close enough to ensure everything went smoothly and respectfully.”
Do chaperones help protect physicians legally?
Some states mandate that chaperones be present by patient request during sensitive exams, such as Texas and Oregon. For the most part, though, physicians have no legal obligation to offer chaperones, although it could be in their best interest to do so.
Ob.gyn. is one of the most litigated specialties, for example, so these physicians may find chaperones can play a key role in averting lawsuits. According to data from Physicians’ Insurance, having a reliable witness in an exam room can mitigate claims, and doctors should follow a clear practice policy regarding chaperones for all patients to further reduce liability.
Another advantage to having a chaperone present: protection for a doctor against a problematic patient. The risk for assault or aggression during an exam can of course go both ways. It’s important to be able to prove any patient misconduct through a witness, and a chaperone can lessen the prospect of violence in any form. “Having a chaperone in an exam room is about protecting the doctors as well as the patient,” said Ms. Kanyok.
A chaperone can also defuse ethical dilemmas. Consider a patient who refuses to allow a chaperone in an exam, but a chaperone is required by the physician’s health care organization. Asking a patient to state their reasons for wanting privacy with the chaperone present before the actual exam can help document the patient’s wish respectfully as well as protect a physician and organization from any potential liability if the patient refuses the exam altogether or if an exception for the patient is made.
Making a chaperone policy work best
- Have your staff inform patients of a medical chaperone policy at the time an appointment is made. Have fact sheets available for the patient before appointments fully outlining your policy.
- Inform the chaperone fully about the details of the exam and the patient’s case prior to the exam, in accordance with HIPAA.
- The chaperone can introduce themselves to the patient in the waiting room or exam room before you enter the room. The chaperone can go over the policy again verbally and answer any questions the patient may have initially. You can then clarify whether the patient understands your chaperone policy when you come in.
- Document, document, document. Write down who the chaperone was for each exam in patient notes and note the details of any interactions that are significant, such as patient questions or conflicts.
- Practice respect, above all. “A patient’s safety and level of comfort should be prioritized,” said Ms. Kanyok.
A version of this article first appeared on Medscape.com.
News of physicians accused or convicted of sexually inappropriate behavior toward patients during medical exams has been frequent recently. And patient advocates have brought up the fact that many patients are uncomfortable during sensitive exams.
As a result, more
For some institutions, the movement has been toward mandating chaperones. Chaperones can be present for any examination of what are often referred to as sensitive areas, such as breasts, genitalia, and the perianal area. For example, Yale University Health requires patients to use a medical staff member as a chaperone for all sensitive exams except in emergency situations. UCLA Health, on the other hand, allows any adult or child aged 12 years or older to decline a chaperone if they wish to do so. Michigan Medicine provides a chaperone on request, although a patient can opt out.
Many physicians fully support the concept. “If a patient requests a chaperone I think we all, as practitioners, should honor that request respectfully,” said Shieva Ghofrany, MD, an ob.gyn. practicing in Stamford, Conn., and cofounder of tribecalledv, a women’s health knowledge platform. “It’s a clear sign a patient wants to ensure that they feel safe and comfortable.”
However, using a chaperone can be challenging for many primary care physicians and specialists in terms of logistics. Should a chaperone’s job be purely observational? Or should the chaperone also be a medical professional who assists during the procedure? How, specifically, should a chaperone perform their duty during an exam? Where should the chaperone stand? What about legal and ethical ramifications?
Who should be a chaperone?
The role of a chaperone is sometimes vaguely defined. It’s logical that a chaperone should have sufficient medical knowledge. Could it be a medical student? Should it be a nurse or another doctor? Would a patient representative suffice even if they aren’t a direct-care clinician?
There are no set standards about who can assume the role. However, the American Medical Association recommends that a patient chaperone be an authorized member of a health care team. For many patients, this is vital.
“As a survivor of sexual assault by an ob.gyn. while I was pregnant, I can assure you that the heinous crime committed against me and hundreds of other women would have been prevented had there been another medical professional in the room,” said Laurie Kanyok, founder of a dance company in New York City, whose former doctor was recently convicted of federal sex abuse charges and is scheduled to be sentenced in July 2023. “The chaperone should be a physician assistant, nurse or medical professional. Qualified professionals better understand the nature and protocols of an exam.”
For children and adolescents, allowing a parent to be a chaperone might be a logical and comforting choice. However, a new British study found that it’s not appropriate.
Study authors Rebecca Jane Moon and Justin Huw Davies looked at pubertal staging–related exams and contend that a chaperone should always be impartial, and a parent’s presence could conceivably open up a physician to false charges of misconduct.
The solution: A parent should have the option be present during any physical exam of their child, with a medical professional additionally acting as chaperone. This can also work for any patient who wishes to bring a trusted friend or family member to their medical appointments.
How does a chaperoned exam work?
A research team from the Medical College of Wisconsin and Louisiana State University Health conducted a recent systematic review of patient and clinician perspectives on carrying out a chaperoned urology exam. The review found that the protocol could use improvement. For example, it was reported that over one-quarter of patients didn’t feel comfortable asking for a chaperone if they were not offered one. “Patients should not have to request this,” said Diana Londoño, MD, a board-certified urologist and assistant clinical professor at City of Hope National Medical Center in Duarte, Calif.
The researchers also found that 93% of female patients preferred a chaperone of the same gender, whereas male patients were split on this issue. Key duties of a chaperone should be to ensure privacy, help interpret instructions from doctor to patient, and continually clarify that consent is being requested as a sensitive exam proceeds, the researchers report. Although clinical practice standards for chaperones aren’t uniform, keeping these important points in mind can easily be adopted by any health care provider.
Many doctors do follow their own set guidelines. “Often, we have our medical assistants be our chaperones,” explained Dr. Ghofrany. “Ideally they ‘room’ the patient – take vitals and ask the patient what specific concerns they would like to address. This helps with exam set-up.
“For example, if a patient has a breast concern versus a concern about their genital area, this would change what drapes are used. The medical assistant would then stand near me if they are helping with a Pap smear or cultures, or they may stand by the patient’s head at the bedside and offer support if needed. Some patients want to hold someone’s hand during an uncomfortable exam.”
The issue of positioning is important. A patient may feel very uneasy if it appears that the chaperone is looking at their body from the doctor’s angle, negating the point of reassurance. The key is to explain before an exam exactly how a chaperone is needed during the exam itself and whether the chaperone is a medical assistant or nurse.
“Chaperones usually stand next to me on either side or on the side of the patient facing me, depending on if they are immediately assisting me or helping the patient,” said Dr. Londoño. If a chaperone will be moving back and forth during the exam, that should be conveyed as well. For virtual visits, a chaperone can act as a third party and be present on a split screen, a process Michigan Medicine uses.
It’s also important to inform patients that a chaperone can step in and stop an exam at any point, both at the patient’s request or because of any observation of inappropriate physician behavior. Understanding this can help reluctant patients feel less worry.
When Christian Miller was diagnosed with a sleep disorder, his doctor suggested having a chaperone present during his physical exams. At first, he was apprehensive but then found the experience to be very positive. “Having someone there with me gave me an extra measure of assurance that nothing untoward would happen,” he said. “I found that having a chaperone was reassuring. The chaperone was not intrusive but stood close enough to ensure everything went smoothly and respectfully.”
Do chaperones help protect physicians legally?
Some states mandate that chaperones be present by patient request during sensitive exams, such as Texas and Oregon. For the most part, though, physicians have no legal obligation to offer chaperones, although it could be in their best interest to do so.
Ob.gyn. is one of the most litigated specialties, for example, so these physicians may find chaperones can play a key role in averting lawsuits. According to data from Physicians’ Insurance, having a reliable witness in an exam room can mitigate claims, and doctors should follow a clear practice policy regarding chaperones for all patients to further reduce liability.
Another advantage to having a chaperone present: protection for a doctor against a problematic patient. The risk for assault or aggression during an exam can of course go both ways. It’s important to be able to prove any patient misconduct through a witness, and a chaperone can lessen the prospect of violence in any form. “Having a chaperone in an exam room is about protecting the doctors as well as the patient,” said Ms. Kanyok.
A chaperone can also defuse ethical dilemmas. Consider a patient who refuses to allow a chaperone in an exam, but a chaperone is required by the physician’s health care organization. Asking a patient to state their reasons for wanting privacy with the chaperone present before the actual exam can help document the patient’s wish respectfully as well as protect a physician and organization from any potential liability if the patient refuses the exam altogether or if an exception for the patient is made.
Making a chaperone policy work best
- Have your staff inform patients of a medical chaperone policy at the time an appointment is made. Have fact sheets available for the patient before appointments fully outlining your policy.
- Inform the chaperone fully about the details of the exam and the patient’s case prior to the exam, in accordance with HIPAA.
- The chaperone can introduce themselves to the patient in the waiting room or exam room before you enter the room. The chaperone can go over the policy again verbally and answer any questions the patient may have initially. You can then clarify whether the patient understands your chaperone policy when you come in.
- Document, document, document. Write down who the chaperone was for each exam in patient notes and note the details of any interactions that are significant, such as patient questions or conflicts.
- Practice respect, above all. “A patient’s safety and level of comfort should be prioritized,” said Ms. Kanyok.
A version of this article first appeared on Medscape.com.
News of physicians accused or convicted of sexually inappropriate behavior toward patients during medical exams has been frequent recently. And patient advocates have brought up the fact that many patients are uncomfortable during sensitive exams.
As a result, more
For some institutions, the movement has been toward mandating chaperones. Chaperones can be present for any examination of what are often referred to as sensitive areas, such as breasts, genitalia, and the perianal area. For example, Yale University Health requires patients to use a medical staff member as a chaperone for all sensitive exams except in emergency situations. UCLA Health, on the other hand, allows any adult or child aged 12 years or older to decline a chaperone if they wish to do so. Michigan Medicine provides a chaperone on request, although a patient can opt out.
Many physicians fully support the concept. “If a patient requests a chaperone I think we all, as practitioners, should honor that request respectfully,” said Shieva Ghofrany, MD, an ob.gyn. practicing in Stamford, Conn., and cofounder of tribecalledv, a women’s health knowledge platform. “It’s a clear sign a patient wants to ensure that they feel safe and comfortable.”
However, using a chaperone can be challenging for many primary care physicians and specialists in terms of logistics. Should a chaperone’s job be purely observational? Or should the chaperone also be a medical professional who assists during the procedure? How, specifically, should a chaperone perform their duty during an exam? Where should the chaperone stand? What about legal and ethical ramifications?
Who should be a chaperone?
The role of a chaperone is sometimes vaguely defined. It’s logical that a chaperone should have sufficient medical knowledge. Could it be a medical student? Should it be a nurse or another doctor? Would a patient representative suffice even if they aren’t a direct-care clinician?
There are no set standards about who can assume the role. However, the American Medical Association recommends that a patient chaperone be an authorized member of a health care team. For many patients, this is vital.
“As a survivor of sexual assault by an ob.gyn. while I was pregnant, I can assure you that the heinous crime committed against me and hundreds of other women would have been prevented had there been another medical professional in the room,” said Laurie Kanyok, founder of a dance company in New York City, whose former doctor was recently convicted of federal sex abuse charges and is scheduled to be sentenced in July 2023. “The chaperone should be a physician assistant, nurse or medical professional. Qualified professionals better understand the nature and protocols of an exam.”
For children and adolescents, allowing a parent to be a chaperone might be a logical and comforting choice. However, a new British study found that it’s not appropriate.
Study authors Rebecca Jane Moon and Justin Huw Davies looked at pubertal staging–related exams and contend that a chaperone should always be impartial, and a parent’s presence could conceivably open up a physician to false charges of misconduct.
The solution: A parent should have the option be present during any physical exam of their child, with a medical professional additionally acting as chaperone. This can also work for any patient who wishes to bring a trusted friend or family member to their medical appointments.
How does a chaperoned exam work?
A research team from the Medical College of Wisconsin and Louisiana State University Health conducted a recent systematic review of patient and clinician perspectives on carrying out a chaperoned urology exam. The review found that the protocol could use improvement. For example, it was reported that over one-quarter of patients didn’t feel comfortable asking for a chaperone if they were not offered one. “Patients should not have to request this,” said Diana Londoño, MD, a board-certified urologist and assistant clinical professor at City of Hope National Medical Center in Duarte, Calif.
The researchers also found that 93% of female patients preferred a chaperone of the same gender, whereas male patients were split on this issue. Key duties of a chaperone should be to ensure privacy, help interpret instructions from doctor to patient, and continually clarify that consent is being requested as a sensitive exam proceeds, the researchers report. Although clinical practice standards for chaperones aren’t uniform, keeping these important points in mind can easily be adopted by any health care provider.
Many doctors do follow their own set guidelines. “Often, we have our medical assistants be our chaperones,” explained Dr. Ghofrany. “Ideally they ‘room’ the patient – take vitals and ask the patient what specific concerns they would like to address. This helps with exam set-up.
“For example, if a patient has a breast concern versus a concern about their genital area, this would change what drapes are used. The medical assistant would then stand near me if they are helping with a Pap smear or cultures, or they may stand by the patient’s head at the bedside and offer support if needed. Some patients want to hold someone’s hand during an uncomfortable exam.”
The issue of positioning is important. A patient may feel very uneasy if it appears that the chaperone is looking at their body from the doctor’s angle, negating the point of reassurance. The key is to explain before an exam exactly how a chaperone is needed during the exam itself and whether the chaperone is a medical assistant or nurse.
“Chaperones usually stand next to me on either side or on the side of the patient facing me, depending on if they are immediately assisting me or helping the patient,” said Dr. Londoño. If a chaperone will be moving back and forth during the exam, that should be conveyed as well. For virtual visits, a chaperone can act as a third party and be present on a split screen, a process Michigan Medicine uses.
It’s also important to inform patients that a chaperone can step in and stop an exam at any point, both at the patient’s request or because of any observation of inappropriate physician behavior. Understanding this can help reluctant patients feel less worry.
When Christian Miller was diagnosed with a sleep disorder, his doctor suggested having a chaperone present during his physical exams. At first, he was apprehensive but then found the experience to be very positive. “Having someone there with me gave me an extra measure of assurance that nothing untoward would happen,” he said. “I found that having a chaperone was reassuring. The chaperone was not intrusive but stood close enough to ensure everything went smoothly and respectfully.”
Do chaperones help protect physicians legally?
Some states mandate that chaperones be present by patient request during sensitive exams, such as Texas and Oregon. For the most part, though, physicians have no legal obligation to offer chaperones, although it could be in their best interest to do so.
Ob.gyn. is one of the most litigated specialties, for example, so these physicians may find chaperones can play a key role in averting lawsuits. According to data from Physicians’ Insurance, having a reliable witness in an exam room can mitigate claims, and doctors should follow a clear practice policy regarding chaperones for all patients to further reduce liability.
Another advantage to having a chaperone present: protection for a doctor against a problematic patient. The risk for assault or aggression during an exam can of course go both ways. It’s important to be able to prove any patient misconduct through a witness, and a chaperone can lessen the prospect of violence in any form. “Having a chaperone in an exam room is about protecting the doctors as well as the patient,” said Ms. Kanyok.
A chaperone can also defuse ethical dilemmas. Consider a patient who refuses to allow a chaperone in an exam, but a chaperone is required by the physician’s health care organization. Asking a patient to state their reasons for wanting privacy with the chaperone present before the actual exam can help document the patient’s wish respectfully as well as protect a physician and organization from any potential liability if the patient refuses the exam altogether or if an exception for the patient is made.
Making a chaperone policy work best
- Have your staff inform patients of a medical chaperone policy at the time an appointment is made. Have fact sheets available for the patient before appointments fully outlining your policy.
- Inform the chaperone fully about the details of the exam and the patient’s case prior to the exam, in accordance with HIPAA.
- The chaperone can introduce themselves to the patient in the waiting room or exam room before you enter the room. The chaperone can go over the policy again verbally and answer any questions the patient may have initially. You can then clarify whether the patient understands your chaperone policy when you come in.
- Document, document, document. Write down who the chaperone was for each exam in patient notes and note the details of any interactions that are significant, such as patient questions or conflicts.
- Practice respect, above all. “A patient’s safety and level of comfort should be prioritized,” said Ms. Kanyok.
A version of this article first appeared on Medscape.com.
Over-the-counter switches improve access but come with risks
On July 13, the Food and Drug Administration approved the first over-the-counter (OTC) norgestrel birth control pill (Opill). The daily oral contraceptive was approved for prescription use 5 decades ago, providing regulators with a half-century of data to show that the progestin-only drug can be used safely without a prescription.
The drug is the latest in a series of medications that have made the switch from behind the pharmacy counter to retail shelves.
Why switch?
When a drug manufacturer submits a proposal for a switch to OTC, the key question that the FDA considers is patient safety. Some risks can be mitigated by approving OTC drugs at lower doses than what is available as the prescription version.
“There is no drug that doesn’t have risks,” said Almut G. Winterstein, RPh, PhD, a distinguished professor in pharmaceutical outcomes and policy and director of the Center for Drug Evaluation and Safety at the University of Florida, Gainesville. “Risks are mitigated by putting specific constraints around access to those medications.”
Dr. Winterstein, a former chair of the FDA’s Drug Safety and Risk Management Advisory Committee, said that nonprescription drugs are unnecessary in a functional health care system.
Many patients may struggle with accessing health clinicians, so making medications available OTC fills gaps left by not being able to get a prescription, according to Dr. Winterstein.
A 2012 paper funded by the Consumer Healthcare Products Association (CHPA), the organization representing manufacturers and distributors of OTC medications, estimated that one quarter of people who bought OTC drugs would not otherwise seek treatment if these treatments were available only via prescription. The CHPA notes that the number of those who experience allergies who use nonprescription antihistamines and allergy-relief drugs increased by about 10% between 2009 and 2015.
Cholesterol drugs
Approximately 80 million U.S. adults are eligible for cholesterol-lowering medications, particularly statins, but nearly half don’t take them, according to the Centers for Disease Control and Prevention.
Fear of side effects is the most common reason people might avoid taking these drugs. But eliminating the need for a refill may encourage uptake of the statins.
“It’s refill, refill, refill,” said Allen J. Taylor, MD, chairman of cardiology at MedStar Heart and Vascular Institute, in Washington. “We spend a ton of time refilling statins and it’s a headache for patients, too.”
The need to secure regular prescriptions for the drug, “doesn’t put enough trust and faith in pharmacists and doesn’t put enough trust and faith in patients,” Dr. Taylor said.
Moving statins to the front end of a pharmacy might not be the best move given the potential for drug interactions, but a nonprescription behind-the-counter approach could work, according to Dr. Taylor.
“The concerns are modest at most, to where they can be monitored by a pharmacist,” he said. “There’s probably more people that would take a statin if they had that kind of access.”
Many statin manufacturers have attempted to make the prescription-to-OTC switch. In 2005, an FDA advisory panel rejected Merck’s proposal for OTC sales of lovastatin after reviewing a study that found only 55% of OTC purchases would have been medically appropriate.
In 2015, Pfizer pulled its application to make the cholesterol drug atorvastatin available to patients OTC because patients were not using the drug correctly. AstraZeneca is investigating an online platform that would allow patients to self-assess their eligibility for rosuvastatin.
Asthma inhalers
Inhalers are the main rescue therapy for asthma aside from a visit to the ED.
The only inhaler available OTC is epinephrine sold under the brand name Primatene Mist, but this type of medicine device is not recommended as a first-line therapy for acute asthma symptoms, according to the American Medical Association.
“It’s been around for a long time and has stayed over the counter even though newer, safer agents have come onto the market which aren’t available over the counter,” said William B. Feldman, MD, DPhil, MPH, a pulmonologist at Brigham and Women’s Hospital, Boston.
Patients who have a hard time getting to a doctor or patients who lack insurance often face barriers accessing albuterol inhalers and beta agonist–corticosteroid combinations, according to Dr. Feldman. A switch to OTC distribution would widen access.
“What we’re advocating is, if they’re going to have access to Primatene Mist, wouldn’t it be sensible to have access to a safer and more effective therapy?” Dr. Feldman said.
Triptans
Migraines affect an estimated 39 million people in the United States, according to the American Migraine Foundation. Several drugs to treat migraine are available OTC, including nonsteroidal anti-inflammatory drugs, aspirin, and acetaminophen. Triptans, drugs used for the short-term treatment of acute symptoms, are prescription-only in the United States.
But in the United Kingdom, triptans first became available in retail stores in 2006, leading to reduced costs for patients, employers, and the government. One study found that government health expenditures would be reduced by $84 million annually if the OTC switch were made in six European countries.
However, overuse of the drug and potential contraindications have been cited as concerns with OTC access.
For Dr. Winterstein, the decision to switch isn’t just about the freedom to buy a drug; it comes down to weighing potential risks and benefits.
“Drugs are only as good as if they’re used in the context of how they should be used,” Dr. Winterstein said. “It’s not candy.”
A version of this article first appeared on Medscape.com.
On July 13, the Food and Drug Administration approved the first over-the-counter (OTC) norgestrel birth control pill (Opill). The daily oral contraceptive was approved for prescription use 5 decades ago, providing regulators with a half-century of data to show that the progestin-only drug can be used safely without a prescription.
The drug is the latest in a series of medications that have made the switch from behind the pharmacy counter to retail shelves.
Why switch?
When a drug manufacturer submits a proposal for a switch to OTC, the key question that the FDA considers is patient safety. Some risks can be mitigated by approving OTC drugs at lower doses than what is available as the prescription version.
“There is no drug that doesn’t have risks,” said Almut G. Winterstein, RPh, PhD, a distinguished professor in pharmaceutical outcomes and policy and director of the Center for Drug Evaluation and Safety at the University of Florida, Gainesville. “Risks are mitigated by putting specific constraints around access to those medications.”
Dr. Winterstein, a former chair of the FDA’s Drug Safety and Risk Management Advisory Committee, said that nonprescription drugs are unnecessary in a functional health care system.
Many patients may struggle with accessing health clinicians, so making medications available OTC fills gaps left by not being able to get a prescription, according to Dr. Winterstein.
A 2012 paper funded by the Consumer Healthcare Products Association (CHPA), the organization representing manufacturers and distributors of OTC medications, estimated that one quarter of people who bought OTC drugs would not otherwise seek treatment if these treatments were available only via prescription. The CHPA notes that the number of those who experience allergies who use nonprescription antihistamines and allergy-relief drugs increased by about 10% between 2009 and 2015.
Cholesterol drugs
Approximately 80 million U.S. adults are eligible for cholesterol-lowering medications, particularly statins, but nearly half don’t take them, according to the Centers for Disease Control and Prevention.
Fear of side effects is the most common reason people might avoid taking these drugs. But eliminating the need for a refill may encourage uptake of the statins.
“It’s refill, refill, refill,” said Allen J. Taylor, MD, chairman of cardiology at MedStar Heart and Vascular Institute, in Washington. “We spend a ton of time refilling statins and it’s a headache for patients, too.”
The need to secure regular prescriptions for the drug, “doesn’t put enough trust and faith in pharmacists and doesn’t put enough trust and faith in patients,” Dr. Taylor said.
Moving statins to the front end of a pharmacy might not be the best move given the potential for drug interactions, but a nonprescription behind-the-counter approach could work, according to Dr. Taylor.
“The concerns are modest at most, to where they can be monitored by a pharmacist,” he said. “There’s probably more people that would take a statin if they had that kind of access.”
Many statin manufacturers have attempted to make the prescription-to-OTC switch. In 2005, an FDA advisory panel rejected Merck’s proposal for OTC sales of lovastatin after reviewing a study that found only 55% of OTC purchases would have been medically appropriate.
In 2015, Pfizer pulled its application to make the cholesterol drug atorvastatin available to patients OTC because patients were not using the drug correctly. AstraZeneca is investigating an online platform that would allow patients to self-assess their eligibility for rosuvastatin.
Asthma inhalers
Inhalers are the main rescue therapy for asthma aside from a visit to the ED.
The only inhaler available OTC is epinephrine sold under the brand name Primatene Mist, but this type of medicine device is not recommended as a first-line therapy for acute asthma symptoms, according to the American Medical Association.
“It’s been around for a long time and has stayed over the counter even though newer, safer agents have come onto the market which aren’t available over the counter,” said William B. Feldman, MD, DPhil, MPH, a pulmonologist at Brigham and Women’s Hospital, Boston.
Patients who have a hard time getting to a doctor or patients who lack insurance often face barriers accessing albuterol inhalers and beta agonist–corticosteroid combinations, according to Dr. Feldman. A switch to OTC distribution would widen access.
“What we’re advocating is, if they’re going to have access to Primatene Mist, wouldn’t it be sensible to have access to a safer and more effective therapy?” Dr. Feldman said.
Triptans
Migraines affect an estimated 39 million people in the United States, according to the American Migraine Foundation. Several drugs to treat migraine are available OTC, including nonsteroidal anti-inflammatory drugs, aspirin, and acetaminophen. Triptans, drugs used for the short-term treatment of acute symptoms, are prescription-only in the United States.
But in the United Kingdom, triptans first became available in retail stores in 2006, leading to reduced costs for patients, employers, and the government. One study found that government health expenditures would be reduced by $84 million annually if the OTC switch were made in six European countries.
However, overuse of the drug and potential contraindications have been cited as concerns with OTC access.
For Dr. Winterstein, the decision to switch isn’t just about the freedom to buy a drug; it comes down to weighing potential risks and benefits.
“Drugs are only as good as if they’re used in the context of how they should be used,” Dr. Winterstein said. “It’s not candy.”
A version of this article first appeared on Medscape.com.
On July 13, the Food and Drug Administration approved the first over-the-counter (OTC) norgestrel birth control pill (Opill). The daily oral contraceptive was approved for prescription use 5 decades ago, providing regulators with a half-century of data to show that the progestin-only drug can be used safely without a prescription.
The drug is the latest in a series of medications that have made the switch from behind the pharmacy counter to retail shelves.
Why switch?
When a drug manufacturer submits a proposal for a switch to OTC, the key question that the FDA considers is patient safety. Some risks can be mitigated by approving OTC drugs at lower doses than what is available as the prescription version.
“There is no drug that doesn’t have risks,” said Almut G. Winterstein, RPh, PhD, a distinguished professor in pharmaceutical outcomes and policy and director of the Center for Drug Evaluation and Safety at the University of Florida, Gainesville. “Risks are mitigated by putting specific constraints around access to those medications.”
Dr. Winterstein, a former chair of the FDA’s Drug Safety and Risk Management Advisory Committee, said that nonprescription drugs are unnecessary in a functional health care system.
Many patients may struggle with accessing health clinicians, so making medications available OTC fills gaps left by not being able to get a prescription, according to Dr. Winterstein.
A 2012 paper funded by the Consumer Healthcare Products Association (CHPA), the organization representing manufacturers and distributors of OTC medications, estimated that one quarter of people who bought OTC drugs would not otherwise seek treatment if these treatments were available only via prescription. The CHPA notes that the number of those who experience allergies who use nonprescription antihistamines and allergy-relief drugs increased by about 10% between 2009 and 2015.
Cholesterol drugs
Approximately 80 million U.S. adults are eligible for cholesterol-lowering medications, particularly statins, but nearly half don’t take them, according to the Centers for Disease Control and Prevention.
Fear of side effects is the most common reason people might avoid taking these drugs. But eliminating the need for a refill may encourage uptake of the statins.
“It’s refill, refill, refill,” said Allen J. Taylor, MD, chairman of cardiology at MedStar Heart and Vascular Institute, in Washington. “We spend a ton of time refilling statins and it’s a headache for patients, too.”
The need to secure regular prescriptions for the drug, “doesn’t put enough trust and faith in pharmacists and doesn’t put enough trust and faith in patients,” Dr. Taylor said.
Moving statins to the front end of a pharmacy might not be the best move given the potential for drug interactions, but a nonprescription behind-the-counter approach could work, according to Dr. Taylor.
“The concerns are modest at most, to where they can be monitored by a pharmacist,” he said. “There’s probably more people that would take a statin if they had that kind of access.”
Many statin manufacturers have attempted to make the prescription-to-OTC switch. In 2005, an FDA advisory panel rejected Merck’s proposal for OTC sales of lovastatin after reviewing a study that found only 55% of OTC purchases would have been medically appropriate.
In 2015, Pfizer pulled its application to make the cholesterol drug atorvastatin available to patients OTC because patients were not using the drug correctly. AstraZeneca is investigating an online platform that would allow patients to self-assess their eligibility for rosuvastatin.
Asthma inhalers
Inhalers are the main rescue therapy for asthma aside from a visit to the ED.
The only inhaler available OTC is epinephrine sold under the brand name Primatene Mist, but this type of medicine device is not recommended as a first-line therapy for acute asthma symptoms, according to the American Medical Association.
“It’s been around for a long time and has stayed over the counter even though newer, safer agents have come onto the market which aren’t available over the counter,” said William B. Feldman, MD, DPhil, MPH, a pulmonologist at Brigham and Women’s Hospital, Boston.
Patients who have a hard time getting to a doctor or patients who lack insurance often face barriers accessing albuterol inhalers and beta agonist–corticosteroid combinations, according to Dr. Feldman. A switch to OTC distribution would widen access.
“What we’re advocating is, if they’re going to have access to Primatene Mist, wouldn’t it be sensible to have access to a safer and more effective therapy?” Dr. Feldman said.
Triptans
Migraines affect an estimated 39 million people in the United States, according to the American Migraine Foundation. Several drugs to treat migraine are available OTC, including nonsteroidal anti-inflammatory drugs, aspirin, and acetaminophen. Triptans, drugs used for the short-term treatment of acute symptoms, are prescription-only in the United States.
But in the United Kingdom, triptans first became available in retail stores in 2006, leading to reduced costs for patients, employers, and the government. One study found that government health expenditures would be reduced by $84 million annually if the OTC switch were made in six European countries.
However, overuse of the drug and potential contraindications have been cited as concerns with OTC access.
For Dr. Winterstein, the decision to switch isn’t just about the freedom to buy a drug; it comes down to weighing potential risks and benefits.
“Drugs are only as good as if they’re used in the context of how they should be used,” Dr. Winterstein said. “It’s not candy.”
A version of this article first appeared on Medscape.com.
Intermittent fasting vs. calorie counting for weight loss
BOSTON –
For the study, 57 overweight and obese participants with type 2 diabetes were randomly assigned to three different groups: The first group ate between noon and 8 p.m., the second was asked to reduce caloric intake by 25% of maintenance calories, and the third, a control group, continued eating normally.
The calorie-restriction group tracked intake on MyFitnessPal, an app that logs the calorie content of different foods. Both the intermittent-fasting and calorie-restriction groups were assigned a dietitian to help with adherence.
After 6 months, participants in the intermittent-fasting group lost about 4.3% of body weight – the equivalent of 10 pounds of weight loss for a person weighing 230 pounds – whereas participants in the calorie-restriction group lost about 2.5% of body weight.
The difference between the two groups was not significant, so one approach isn’t necessarily better than the other for weight loss.
“Let’s not think of this as an approach that’s better than calorie restriction,” William Yancy, MD, MHS, an internist and weight management specialist at Duke Lifestyle and Weight Management Center, Durham, N.C., said in an interview. “It’s an alternative approach to calorie restriction.”
Participants’ willingness to adhere to the diet likely accounted for the percentage difference between the groups, study author Vasiliki Pavlou, RDN, told this news organization. Ms. Pavlou presented the findings at the Nutrition 2023 conference.
“People that have type 2 diabetes, they’ve already been to the doctor, they’ve already been told to count calories,” said Ms. Pavlou, a doctoral student at the University of Illinois at Chicago. “There were many weeks where they came to us with nothing on MyFitnessPal and we’d have to encourage them to start tracking again.”
The intermittent-fasting group adhered to the eating time window 6 out of 7 days of the week, with a 1-hour grace period for the noon-to-8-p.m. window. In comparison, one-third of the calorie-restriction group didn’t stay within 200 calories of the goal, according to Ms. Pavlou.
That meant the fasting group cut about 100 calories more per day than the calorie-restriction group, which was reflected in their weight loss, Ms. Pavlou said.
A1c levels dropped by about 1% in both the intermittent-fasting and calorie-restriction groups – a meaningful decrease, said Dr. Yancy. “I think a 0.5% difference would have some clinical significance in terms of complications from diabetes,” he said. “So 1% would be even more clinically meaningful.”
However, fewer participants taking insulin in the calorie-restriction group could explain the difference, according to Ms. Pavlou. “Usually, when someone goes on insulin, their pancreas is already not functioning as well,” she said. “And it’s way harder to see improvements in their A1c and glycemic control.”
Up to 90% of people with type 2 diabetes are overweight or obese. Weight loss is one of the major components of type 2 diabetes care, according to the American Diabetes Association, and studies have shown that even a 5% reduction in body weight can reduce blood glucose concentration and A1c. Some studies suggest diabetes remission can occur after a 10% loss in body weight, but Dr. Yancy said it depends on the person.
“It depends on the individual, their metabolic situation, how long they’ve had diabetes, what kind of approach they’re following, maybe what medicines they’re taking,” Dr. Yancy said. “There’s a lot of different factors involved in remission.”
The study cohort generally had advanced diabetes and was taking a mix of medications, so the results might not be applicable to people with a more recent diabetes diagnosis, according to Ms. Pavlou.
Dr. Yancy said intermittent fasting could work well for the right person. The success of the approach could depend on a person’s eating habits and whether their meals usually fall outside the time-restricted window, or it could depend on how well a person follows rules, according to Dr. Yancy.
“Some people might not eat much after 8 o’clock, and some people might skip breakfast,” Dr. Yancy said. “And if that’s the case, then it’s not going to make a big impact on their weight probably.”
Medication is also an important consideration. Not eating can be dangerous for patients taking short-acting insulin or sulfonylureas, according to Dr. Yancy.
Ms. Pavlou said these findings show intermittent fasting is another option for patients with type 2 diabetes trying to lose weight. “If you’ve tried calorie counting, that’s not working for you or if you’re kind of burnt out, this is something else that you could try,” she said.
“We have a lot of patients that need to lose weight, and we have patients who respond differently to different approaches,” said Dr. Yancy. “So having various approaches is really valuable.”
The manuscript is currently under review at JAMA Internal Medicine, said Ms. Pavlou.
A version of this article appeared on Medscape.com.
BOSTON –
For the study, 57 overweight and obese participants with type 2 diabetes were randomly assigned to three different groups: The first group ate between noon and 8 p.m., the second was asked to reduce caloric intake by 25% of maintenance calories, and the third, a control group, continued eating normally.
The calorie-restriction group tracked intake on MyFitnessPal, an app that logs the calorie content of different foods. Both the intermittent-fasting and calorie-restriction groups were assigned a dietitian to help with adherence.
After 6 months, participants in the intermittent-fasting group lost about 4.3% of body weight – the equivalent of 10 pounds of weight loss for a person weighing 230 pounds – whereas participants in the calorie-restriction group lost about 2.5% of body weight.
The difference between the two groups was not significant, so one approach isn’t necessarily better than the other for weight loss.
“Let’s not think of this as an approach that’s better than calorie restriction,” William Yancy, MD, MHS, an internist and weight management specialist at Duke Lifestyle and Weight Management Center, Durham, N.C., said in an interview. “It’s an alternative approach to calorie restriction.”
Participants’ willingness to adhere to the diet likely accounted for the percentage difference between the groups, study author Vasiliki Pavlou, RDN, told this news organization. Ms. Pavlou presented the findings at the Nutrition 2023 conference.
“People that have type 2 diabetes, they’ve already been to the doctor, they’ve already been told to count calories,” said Ms. Pavlou, a doctoral student at the University of Illinois at Chicago. “There were many weeks where they came to us with nothing on MyFitnessPal and we’d have to encourage them to start tracking again.”
The intermittent-fasting group adhered to the eating time window 6 out of 7 days of the week, with a 1-hour grace period for the noon-to-8-p.m. window. In comparison, one-third of the calorie-restriction group didn’t stay within 200 calories of the goal, according to Ms. Pavlou.
That meant the fasting group cut about 100 calories more per day than the calorie-restriction group, which was reflected in their weight loss, Ms. Pavlou said.
A1c levels dropped by about 1% in both the intermittent-fasting and calorie-restriction groups – a meaningful decrease, said Dr. Yancy. “I think a 0.5% difference would have some clinical significance in terms of complications from diabetes,” he said. “So 1% would be even more clinically meaningful.”
However, fewer participants taking insulin in the calorie-restriction group could explain the difference, according to Ms. Pavlou. “Usually, when someone goes on insulin, their pancreas is already not functioning as well,” she said. “And it’s way harder to see improvements in their A1c and glycemic control.”
Up to 90% of people with type 2 diabetes are overweight or obese. Weight loss is one of the major components of type 2 diabetes care, according to the American Diabetes Association, and studies have shown that even a 5% reduction in body weight can reduce blood glucose concentration and A1c. Some studies suggest diabetes remission can occur after a 10% loss in body weight, but Dr. Yancy said it depends on the person.
“It depends on the individual, their metabolic situation, how long they’ve had diabetes, what kind of approach they’re following, maybe what medicines they’re taking,” Dr. Yancy said. “There’s a lot of different factors involved in remission.”
The study cohort generally had advanced diabetes and was taking a mix of medications, so the results might not be applicable to people with a more recent diabetes diagnosis, according to Ms. Pavlou.
Dr. Yancy said intermittent fasting could work well for the right person. The success of the approach could depend on a person’s eating habits and whether their meals usually fall outside the time-restricted window, or it could depend on how well a person follows rules, according to Dr. Yancy.
“Some people might not eat much after 8 o’clock, and some people might skip breakfast,” Dr. Yancy said. “And if that’s the case, then it’s not going to make a big impact on their weight probably.”
Medication is also an important consideration. Not eating can be dangerous for patients taking short-acting insulin or sulfonylureas, according to Dr. Yancy.
Ms. Pavlou said these findings show intermittent fasting is another option for patients with type 2 diabetes trying to lose weight. “If you’ve tried calorie counting, that’s not working for you or if you’re kind of burnt out, this is something else that you could try,” she said.
“We have a lot of patients that need to lose weight, and we have patients who respond differently to different approaches,” said Dr. Yancy. “So having various approaches is really valuable.”
The manuscript is currently under review at JAMA Internal Medicine, said Ms. Pavlou.
A version of this article appeared on Medscape.com.
BOSTON –
For the study, 57 overweight and obese participants with type 2 diabetes were randomly assigned to three different groups: The first group ate between noon and 8 p.m., the second was asked to reduce caloric intake by 25% of maintenance calories, and the third, a control group, continued eating normally.
The calorie-restriction group tracked intake on MyFitnessPal, an app that logs the calorie content of different foods. Both the intermittent-fasting and calorie-restriction groups were assigned a dietitian to help with adherence.
After 6 months, participants in the intermittent-fasting group lost about 4.3% of body weight – the equivalent of 10 pounds of weight loss for a person weighing 230 pounds – whereas participants in the calorie-restriction group lost about 2.5% of body weight.
The difference between the two groups was not significant, so one approach isn’t necessarily better than the other for weight loss.
“Let’s not think of this as an approach that’s better than calorie restriction,” William Yancy, MD, MHS, an internist and weight management specialist at Duke Lifestyle and Weight Management Center, Durham, N.C., said in an interview. “It’s an alternative approach to calorie restriction.”
Participants’ willingness to adhere to the diet likely accounted for the percentage difference between the groups, study author Vasiliki Pavlou, RDN, told this news organization. Ms. Pavlou presented the findings at the Nutrition 2023 conference.
“People that have type 2 diabetes, they’ve already been to the doctor, they’ve already been told to count calories,” said Ms. Pavlou, a doctoral student at the University of Illinois at Chicago. “There were many weeks where they came to us with nothing on MyFitnessPal and we’d have to encourage them to start tracking again.”
The intermittent-fasting group adhered to the eating time window 6 out of 7 days of the week, with a 1-hour grace period for the noon-to-8-p.m. window. In comparison, one-third of the calorie-restriction group didn’t stay within 200 calories of the goal, according to Ms. Pavlou.
That meant the fasting group cut about 100 calories more per day than the calorie-restriction group, which was reflected in their weight loss, Ms. Pavlou said.
A1c levels dropped by about 1% in both the intermittent-fasting and calorie-restriction groups – a meaningful decrease, said Dr. Yancy. “I think a 0.5% difference would have some clinical significance in terms of complications from diabetes,” he said. “So 1% would be even more clinically meaningful.”
However, fewer participants taking insulin in the calorie-restriction group could explain the difference, according to Ms. Pavlou. “Usually, when someone goes on insulin, their pancreas is already not functioning as well,” she said. “And it’s way harder to see improvements in their A1c and glycemic control.”
Up to 90% of people with type 2 diabetes are overweight or obese. Weight loss is one of the major components of type 2 diabetes care, according to the American Diabetes Association, and studies have shown that even a 5% reduction in body weight can reduce blood glucose concentration and A1c. Some studies suggest diabetes remission can occur after a 10% loss in body weight, but Dr. Yancy said it depends on the person.
“It depends on the individual, their metabolic situation, how long they’ve had diabetes, what kind of approach they’re following, maybe what medicines they’re taking,” Dr. Yancy said. “There’s a lot of different factors involved in remission.”
The study cohort generally had advanced diabetes and was taking a mix of medications, so the results might not be applicable to people with a more recent diabetes diagnosis, according to Ms. Pavlou.
Dr. Yancy said intermittent fasting could work well for the right person. The success of the approach could depend on a person’s eating habits and whether their meals usually fall outside the time-restricted window, or it could depend on how well a person follows rules, according to Dr. Yancy.
“Some people might not eat much after 8 o’clock, and some people might skip breakfast,” Dr. Yancy said. “And if that’s the case, then it’s not going to make a big impact on their weight probably.”
Medication is also an important consideration. Not eating can be dangerous for patients taking short-acting insulin or sulfonylureas, according to Dr. Yancy.
Ms. Pavlou said these findings show intermittent fasting is another option for patients with type 2 diabetes trying to lose weight. “If you’ve tried calorie counting, that’s not working for you or if you’re kind of burnt out, this is something else that you could try,” she said.
“We have a lot of patients that need to lose weight, and we have patients who respond differently to different approaches,” said Dr. Yancy. “So having various approaches is really valuable.”
The manuscript is currently under review at JAMA Internal Medicine, said Ms. Pavlou.
A version of this article appeared on Medscape.com.
AT NUTRITION 2023
CDC offers guidance on RSV vaccines for adults
Two newly approved respiratory syncytial virus (RSV) vaccines for adults aged 60 years and older may be able to prevent illness in those at risk for severe RSV disease.
Most adult RSV illness occurs among the older age group and results in an estimated 60,000-160,000 hospitalizations and 6,000-10,000 deaths per year among people aged at least 65 years.
Older adults deciding whether to get the vaccines should weigh risks and their own preferences and make the decision in consultation with their clinicians, said authors of a Centers for Disease Control and Prevention report.
Michael Melgar, MD, with the Coronavirus and Other Respiratory Viruses Division at the CDC, was lead author on the report, published in the Morbidity and Mortality Weekly Report.
Two new vaccines
In May, the Food and Drug Administration approved the first of two vaccines for preventing RSV lower respiratory tract disease for adults aged at least 60 years.
On June 21, the Advisory Committee on Immunization Practices (ACIP) recommended that people in that age group receive a single dose of RSV vaccine using shared decision-making.
The recommendation for shared decision-making makes the ACIP decision different from routine and risk-based vaccine recommendations. Rather than targeting all in a particular age group or risk group, the decision calls for consideration of a patients’ risk for disease and their characteristics, preferences, and values; the health care professional’s clinical discretion; and performance of the vaccine.
Dr. Melgar and colleagues reported that vaccination with one dose of the GSK or Pfizer RSV vaccines has proved moderately to highly effective in preventing symptomatic RSV-associated lower respiratory tract disease over two consecutive RSV seasons among people aged 60 and older.
The trials that led to approval weren’t powered to gauge efficacy against RSV-associated hospitalization and death. However, the authors wrote, the prevention of lower respiratory tract disease, including medically attended illness, suggests that the shots might prevent considerable morbidity from RSV disease among those aged 60 and older.
Both vaccines were generally well tolerated with a good safety profile. However, six cases of inflammatory neurologic events (including Guillain-Barré Syndrome, acute disseminated encephalomyelitis, and others) were reported in clinical trials after RSV vaccination.
“Whether these events occurred due to chance, or whether RSV vaccination increases the risk for inflammatory neurologic events, is currently unknown,” the authors wrote.
Postmarketing surveillance may help clarify the existence of any potential risk, but until those results are clearer, the CDC researchers said, RSV vaccinations should be targeted to older adults at highest risk for severe RSV and those most likely to benefit from the shots.
At higher risk
Some adults with certain medical conditions have a higher risk for RSV-associated hospitalization, according to the report.
Those conditions include chronic obstructive pulmonary disease, asthma, heart failure, coronary artery disease, cerebrovascular disease, diabetes mellitus, and chronic kidney disease.
People who are frail and of advanced age also are at higher risk for RSV hospitalization. That risk increases with age and the highest risk is for people aged at least 75 years.
The researchers added that RSV can cause severe disease in those with compromised immunity, including people who have received hematopoietic stem cell transplants and patients taking immunosuppressive drugs such as those used with solid organ transplants, cancer treatment, or other conditions.
As for when physicians should offer the vaccinations, shots are optimally given before the start of the RSV season.
However, the COVID-19 pandemic interrupted the seasonality and the timing has not yet returned to prepandemic patterns.
For the 2023-24 season, this report states, clinicians should offer RSV vaccination to adults aged at least 60 years using shared clinical decision-making as early as vaccine supply is available and should continue to offer vaccination to eligible adults who remain unvaccinated.
RSV vaccines can be administered with other adult vaccines during the same visit, the authors confirmed.
A version of this article first appeared on Medscape.com.
Two newly approved respiratory syncytial virus (RSV) vaccines for adults aged 60 years and older may be able to prevent illness in those at risk for severe RSV disease.
Most adult RSV illness occurs among the older age group and results in an estimated 60,000-160,000 hospitalizations and 6,000-10,000 deaths per year among people aged at least 65 years.
Older adults deciding whether to get the vaccines should weigh risks and their own preferences and make the decision in consultation with their clinicians, said authors of a Centers for Disease Control and Prevention report.
Michael Melgar, MD, with the Coronavirus and Other Respiratory Viruses Division at the CDC, was lead author on the report, published in the Morbidity and Mortality Weekly Report.
Two new vaccines
In May, the Food and Drug Administration approved the first of two vaccines for preventing RSV lower respiratory tract disease for adults aged at least 60 years.
On June 21, the Advisory Committee on Immunization Practices (ACIP) recommended that people in that age group receive a single dose of RSV vaccine using shared decision-making.
The recommendation for shared decision-making makes the ACIP decision different from routine and risk-based vaccine recommendations. Rather than targeting all in a particular age group or risk group, the decision calls for consideration of a patients’ risk for disease and their characteristics, preferences, and values; the health care professional’s clinical discretion; and performance of the vaccine.
Dr. Melgar and colleagues reported that vaccination with one dose of the GSK or Pfizer RSV vaccines has proved moderately to highly effective in preventing symptomatic RSV-associated lower respiratory tract disease over two consecutive RSV seasons among people aged 60 and older.
The trials that led to approval weren’t powered to gauge efficacy against RSV-associated hospitalization and death. However, the authors wrote, the prevention of lower respiratory tract disease, including medically attended illness, suggests that the shots might prevent considerable morbidity from RSV disease among those aged 60 and older.
Both vaccines were generally well tolerated with a good safety profile. However, six cases of inflammatory neurologic events (including Guillain-Barré Syndrome, acute disseminated encephalomyelitis, and others) were reported in clinical trials after RSV vaccination.
“Whether these events occurred due to chance, or whether RSV vaccination increases the risk for inflammatory neurologic events, is currently unknown,” the authors wrote.
Postmarketing surveillance may help clarify the existence of any potential risk, but until those results are clearer, the CDC researchers said, RSV vaccinations should be targeted to older adults at highest risk for severe RSV and those most likely to benefit from the shots.
At higher risk
Some adults with certain medical conditions have a higher risk for RSV-associated hospitalization, according to the report.
Those conditions include chronic obstructive pulmonary disease, asthma, heart failure, coronary artery disease, cerebrovascular disease, diabetes mellitus, and chronic kidney disease.
People who are frail and of advanced age also are at higher risk for RSV hospitalization. That risk increases with age and the highest risk is for people aged at least 75 years.
The researchers added that RSV can cause severe disease in those with compromised immunity, including people who have received hematopoietic stem cell transplants and patients taking immunosuppressive drugs such as those used with solid organ transplants, cancer treatment, or other conditions.
As for when physicians should offer the vaccinations, shots are optimally given before the start of the RSV season.
However, the COVID-19 pandemic interrupted the seasonality and the timing has not yet returned to prepandemic patterns.
For the 2023-24 season, this report states, clinicians should offer RSV vaccination to adults aged at least 60 years using shared clinical decision-making as early as vaccine supply is available and should continue to offer vaccination to eligible adults who remain unvaccinated.
RSV vaccines can be administered with other adult vaccines during the same visit, the authors confirmed.
A version of this article first appeared on Medscape.com.
Two newly approved respiratory syncytial virus (RSV) vaccines for adults aged 60 years and older may be able to prevent illness in those at risk for severe RSV disease.
Most adult RSV illness occurs among the older age group and results in an estimated 60,000-160,000 hospitalizations and 6,000-10,000 deaths per year among people aged at least 65 years.
Older adults deciding whether to get the vaccines should weigh risks and their own preferences and make the decision in consultation with their clinicians, said authors of a Centers for Disease Control and Prevention report.
Michael Melgar, MD, with the Coronavirus and Other Respiratory Viruses Division at the CDC, was lead author on the report, published in the Morbidity and Mortality Weekly Report.
Two new vaccines
In May, the Food and Drug Administration approved the first of two vaccines for preventing RSV lower respiratory tract disease for adults aged at least 60 years.
On June 21, the Advisory Committee on Immunization Practices (ACIP) recommended that people in that age group receive a single dose of RSV vaccine using shared decision-making.
The recommendation for shared decision-making makes the ACIP decision different from routine and risk-based vaccine recommendations. Rather than targeting all in a particular age group or risk group, the decision calls for consideration of a patients’ risk for disease and their characteristics, preferences, and values; the health care professional’s clinical discretion; and performance of the vaccine.
Dr. Melgar and colleagues reported that vaccination with one dose of the GSK or Pfizer RSV vaccines has proved moderately to highly effective in preventing symptomatic RSV-associated lower respiratory tract disease over two consecutive RSV seasons among people aged 60 and older.
The trials that led to approval weren’t powered to gauge efficacy against RSV-associated hospitalization and death. However, the authors wrote, the prevention of lower respiratory tract disease, including medically attended illness, suggests that the shots might prevent considerable morbidity from RSV disease among those aged 60 and older.
Both vaccines were generally well tolerated with a good safety profile. However, six cases of inflammatory neurologic events (including Guillain-Barré Syndrome, acute disseminated encephalomyelitis, and others) were reported in clinical trials after RSV vaccination.
“Whether these events occurred due to chance, or whether RSV vaccination increases the risk for inflammatory neurologic events, is currently unknown,” the authors wrote.
Postmarketing surveillance may help clarify the existence of any potential risk, but until those results are clearer, the CDC researchers said, RSV vaccinations should be targeted to older adults at highest risk for severe RSV and those most likely to benefit from the shots.
At higher risk
Some adults with certain medical conditions have a higher risk for RSV-associated hospitalization, according to the report.
Those conditions include chronic obstructive pulmonary disease, asthma, heart failure, coronary artery disease, cerebrovascular disease, diabetes mellitus, and chronic kidney disease.
People who are frail and of advanced age also are at higher risk for RSV hospitalization. That risk increases with age and the highest risk is for people aged at least 75 years.
The researchers added that RSV can cause severe disease in those with compromised immunity, including people who have received hematopoietic stem cell transplants and patients taking immunosuppressive drugs such as those used with solid organ transplants, cancer treatment, or other conditions.
As for when physicians should offer the vaccinations, shots are optimally given before the start of the RSV season.
However, the COVID-19 pandemic interrupted the seasonality and the timing has not yet returned to prepandemic patterns.
For the 2023-24 season, this report states, clinicians should offer RSV vaccination to adults aged at least 60 years using shared clinical decision-making as early as vaccine supply is available and should continue to offer vaccination to eligible adults who remain unvaccinated.
RSV vaccines can be administered with other adult vaccines during the same visit, the authors confirmed.
A version of this article first appeared on Medscape.com.
FROM THE MMWR
