User login
A Case of Shortness of Breath, Abdominal Pain, and Hematuria
A48-year-old male presents with three weeks of worsening shortness of breath and pleuritic chest discomfort. A week before the onset of these symptoms, he noticed increasing fatigue, weight loss, abdominal discomfort, and persistent hematuria He was otherwise healthy and was taking no medications.
Physical examination reveals a tachypneic yet hemodynamically stable patient, with left upper quadrant fullness. CT chest and abdomen, reveal the following (see right).
You suspect that this finding is secondary to an extrapulmonary process. What unifying diagnosis most likely accounts for these findings? What is your diagnosis?
- Antiphospholipid syndrome
- Antithrombin III deficiency
- Renal cell carcinoma
- Protein C deficiency
- Prostate carcinoma
Discussion
The answer is C: Renal cell carcinoma (RCC) with caval extension causing PE; this suggests that the PE was due to tumor thrombus. The photo on p. 8 shows areas of increased attenuation in the prominent right and left pulmonary arteries, consistent with a saddle pulmonary embolism. An MRI of the abdomen (see photo above) reveals a large left renal mass extending to Gerota’s fascia and into the left renal vein, protruding slightly into the inferior vena cava (IVC).
The MRI demonstrates an occlusive thrombus in the left renal vein with propagation into the inferior vena cava. The patient underwent a left radical nephrectomy, an inferior vena cava thrombectomy, and a saddle embolectomy. Histological examination of the mass and thrombus confirmed the diagnosis. He had an uneventful recovery and was discharged from the hospital.
RCC accounts for approximately 80% of all primary renal neoplasms, and commonly is termed the “internist’s tumor.” Hematuria is the most common symptom. It is accompanied by flank pain and a palpable abdominal mass in less than 15% of cases.1 Diagnosis of RCC is often made late due to delayed clinical presentation and 20% of patients have metastatic disease at initial diagnosis.2 PE due to tumor thrombus as an initial manifestation of RCC is rare, but is a well-recognized entity leading to dyspnea, pleuritic chest pain, hypoxemia, and—in severe cases—acute cor pulmonale with hemodynamic failure.3-5
Staging CT is required in patients with suspected RCC, and MRI is needed, with transesophageal echocardiography used adjunctively, to evaluate cephalic thrombus extension when indicated.6 IVC tumor thrombus occurs in 4%-10% of all cases, most often originating in the renal vein and extending cranially, subsequently propagating to the lungs.7 Survival in local non-metastatic disease with IVC thrombus is no different whether renal vein extension occurs or not, and ranges from 40%-69%, following surgical resection and thrombectomy.8 In those with distant metastases who require venal caval thrombectomy, five-year survivals range from 0%-12.5%.2
The first case of successful removal of a PE secondary to RCC was documented in 1977.1 The goal of surgery is tumor resection and prevention of recurrent embolic events. It is the only effective means of improving survival in the presence of intravascular tumor. Preoperative anticoagulation may be warranted in patients who present with PE, but should be discontinued following definitive surgical treatment secondary to increased risks of hemorrhage.8 TH
References
- Daughtry JD, Stewart BH, Golding LAR, Groves LK. Pulmonary embolus presenting as the initial manifestation of renal cell carcinoma. Ann Thorac Surg. 1977;24:178-181.
- Goetzl MA, Goluboff ET, Murphy AM, et al. A contemporary evaluation of cytoreductive nephrectomy with tumor thrombus: morbidity and long term survival. Urol Oncol. 2004; 22:182-187.
- Kubota H, Furuse A, Kotsuka Y, et al. Successful management of massive pulmonary tumor embolism from renal cell carcinoma. Ann Thorac Surg. 1996;61:708-710.
- Gayer G, Mini S, Olchovsky D, et al. Pulmonary embolism—the initial manifestation of renal cell carcinoma in a young woman. Emerg Radiol. 2003;10:43-45.
- Eggener SE, Dalton DP. Bilateral pulmonary artery tumour emboli from renal carcinoma. Lancet Oncol. 2004;5:173.
- Tsuji Y, Goto A, Hara I, et al. Renal cell carcinoma with extension of tumor thrombus into vena cava: Surgical strategy and prognosis. J Vasc Surg. 2001;33:789-796.
- Zisman A, Pantuck AJ, Chao DH, et al. Renal cell carcinoma with tumor thrombus: is cytoreductive nephrectomy for advanced disease associated with an increased complication rate? J Urol. 2002;168:962-967.
- Nesbitt JC, Soltero ER, Dinney CPN, et al. Surgical management of renal cell carcinoma with inferior vena cava tumor thrombus. Ann Thorac Surg. 1997;63:1592-1600.
A48-year-old male presents with three weeks of worsening shortness of breath and pleuritic chest discomfort. A week before the onset of these symptoms, he noticed increasing fatigue, weight loss, abdominal discomfort, and persistent hematuria He was otherwise healthy and was taking no medications.
Physical examination reveals a tachypneic yet hemodynamically stable patient, with left upper quadrant fullness. CT chest and abdomen, reveal the following (see right).
You suspect that this finding is secondary to an extrapulmonary process. What unifying diagnosis most likely accounts for these findings? What is your diagnosis?
- Antiphospholipid syndrome
- Antithrombin III deficiency
- Renal cell carcinoma
- Protein C deficiency
- Prostate carcinoma
Discussion
The answer is C: Renal cell carcinoma (RCC) with caval extension causing PE; this suggests that the PE was due to tumor thrombus. The photo on p. 8 shows areas of increased attenuation in the prominent right and left pulmonary arteries, consistent with a saddle pulmonary embolism. An MRI of the abdomen (see photo above) reveals a large left renal mass extending to Gerota’s fascia and into the left renal vein, protruding slightly into the inferior vena cava (IVC).
The MRI demonstrates an occlusive thrombus in the left renal vein with propagation into the inferior vena cava. The patient underwent a left radical nephrectomy, an inferior vena cava thrombectomy, and a saddle embolectomy. Histological examination of the mass and thrombus confirmed the diagnosis. He had an uneventful recovery and was discharged from the hospital.
RCC accounts for approximately 80% of all primary renal neoplasms, and commonly is termed the “internist’s tumor.” Hematuria is the most common symptom. It is accompanied by flank pain and a palpable abdominal mass in less than 15% of cases.1 Diagnosis of RCC is often made late due to delayed clinical presentation and 20% of patients have metastatic disease at initial diagnosis.2 PE due to tumor thrombus as an initial manifestation of RCC is rare, but is a well-recognized entity leading to dyspnea, pleuritic chest pain, hypoxemia, and—in severe cases—acute cor pulmonale with hemodynamic failure.3-5
Staging CT is required in patients with suspected RCC, and MRI is needed, with transesophageal echocardiography used adjunctively, to evaluate cephalic thrombus extension when indicated.6 IVC tumor thrombus occurs in 4%-10% of all cases, most often originating in the renal vein and extending cranially, subsequently propagating to the lungs.7 Survival in local non-metastatic disease with IVC thrombus is no different whether renal vein extension occurs or not, and ranges from 40%-69%, following surgical resection and thrombectomy.8 In those with distant metastases who require venal caval thrombectomy, five-year survivals range from 0%-12.5%.2
The first case of successful removal of a PE secondary to RCC was documented in 1977.1 The goal of surgery is tumor resection and prevention of recurrent embolic events. It is the only effective means of improving survival in the presence of intravascular tumor. Preoperative anticoagulation may be warranted in patients who present with PE, but should be discontinued following definitive surgical treatment secondary to increased risks of hemorrhage.8 TH
References
- Daughtry JD, Stewart BH, Golding LAR, Groves LK. Pulmonary embolus presenting as the initial manifestation of renal cell carcinoma. Ann Thorac Surg. 1977;24:178-181.
- Goetzl MA, Goluboff ET, Murphy AM, et al. A contemporary evaluation of cytoreductive nephrectomy with tumor thrombus: morbidity and long term survival. Urol Oncol. 2004; 22:182-187.
- Kubota H, Furuse A, Kotsuka Y, et al. Successful management of massive pulmonary tumor embolism from renal cell carcinoma. Ann Thorac Surg. 1996;61:708-710.
- Gayer G, Mini S, Olchovsky D, et al. Pulmonary embolism—the initial manifestation of renal cell carcinoma in a young woman. Emerg Radiol. 2003;10:43-45.
- Eggener SE, Dalton DP. Bilateral pulmonary artery tumour emboli from renal carcinoma. Lancet Oncol. 2004;5:173.
- Tsuji Y, Goto A, Hara I, et al. Renal cell carcinoma with extension of tumor thrombus into vena cava: Surgical strategy and prognosis. J Vasc Surg. 2001;33:789-796.
- Zisman A, Pantuck AJ, Chao DH, et al. Renal cell carcinoma with tumor thrombus: is cytoreductive nephrectomy for advanced disease associated with an increased complication rate? J Urol. 2002;168:962-967.
- Nesbitt JC, Soltero ER, Dinney CPN, et al. Surgical management of renal cell carcinoma with inferior vena cava tumor thrombus. Ann Thorac Surg. 1997;63:1592-1600.
A48-year-old male presents with three weeks of worsening shortness of breath and pleuritic chest discomfort. A week before the onset of these symptoms, he noticed increasing fatigue, weight loss, abdominal discomfort, and persistent hematuria He was otherwise healthy and was taking no medications.
Physical examination reveals a tachypneic yet hemodynamically stable patient, with left upper quadrant fullness. CT chest and abdomen, reveal the following (see right).
You suspect that this finding is secondary to an extrapulmonary process. What unifying diagnosis most likely accounts for these findings? What is your diagnosis?
- Antiphospholipid syndrome
- Antithrombin III deficiency
- Renal cell carcinoma
- Protein C deficiency
- Prostate carcinoma
Discussion
The answer is C: Renal cell carcinoma (RCC) with caval extension causing PE; this suggests that the PE was due to tumor thrombus. The photo on p. 8 shows areas of increased attenuation in the prominent right and left pulmonary arteries, consistent with a saddle pulmonary embolism. An MRI of the abdomen (see photo above) reveals a large left renal mass extending to Gerota’s fascia and into the left renal vein, protruding slightly into the inferior vena cava (IVC).
The MRI demonstrates an occlusive thrombus in the left renal vein with propagation into the inferior vena cava. The patient underwent a left radical nephrectomy, an inferior vena cava thrombectomy, and a saddle embolectomy. Histological examination of the mass and thrombus confirmed the diagnosis. He had an uneventful recovery and was discharged from the hospital.
RCC accounts for approximately 80% of all primary renal neoplasms, and commonly is termed the “internist’s tumor.” Hematuria is the most common symptom. It is accompanied by flank pain and a palpable abdominal mass in less than 15% of cases.1 Diagnosis of RCC is often made late due to delayed clinical presentation and 20% of patients have metastatic disease at initial diagnosis.2 PE due to tumor thrombus as an initial manifestation of RCC is rare, but is a well-recognized entity leading to dyspnea, pleuritic chest pain, hypoxemia, and—in severe cases—acute cor pulmonale with hemodynamic failure.3-5
Staging CT is required in patients with suspected RCC, and MRI is needed, with transesophageal echocardiography used adjunctively, to evaluate cephalic thrombus extension when indicated.6 IVC tumor thrombus occurs in 4%-10% of all cases, most often originating in the renal vein and extending cranially, subsequently propagating to the lungs.7 Survival in local non-metastatic disease with IVC thrombus is no different whether renal vein extension occurs or not, and ranges from 40%-69%, following surgical resection and thrombectomy.8 In those with distant metastases who require venal caval thrombectomy, five-year survivals range from 0%-12.5%.2
The first case of successful removal of a PE secondary to RCC was documented in 1977.1 The goal of surgery is tumor resection and prevention of recurrent embolic events. It is the only effective means of improving survival in the presence of intravascular tumor. Preoperative anticoagulation may be warranted in patients who present with PE, but should be discontinued following definitive surgical treatment secondary to increased risks of hemorrhage.8 TH
References
- Daughtry JD, Stewart BH, Golding LAR, Groves LK. Pulmonary embolus presenting as the initial manifestation of renal cell carcinoma. Ann Thorac Surg. 1977;24:178-181.
- Goetzl MA, Goluboff ET, Murphy AM, et al. A contemporary evaluation of cytoreductive nephrectomy with tumor thrombus: morbidity and long term survival. Urol Oncol. 2004; 22:182-187.
- Kubota H, Furuse A, Kotsuka Y, et al. Successful management of massive pulmonary tumor embolism from renal cell carcinoma. Ann Thorac Surg. 1996;61:708-710.
- Gayer G, Mini S, Olchovsky D, et al. Pulmonary embolism—the initial manifestation of renal cell carcinoma in a young woman. Emerg Radiol. 2003;10:43-45.
- Eggener SE, Dalton DP. Bilateral pulmonary artery tumour emboli from renal carcinoma. Lancet Oncol. 2004;5:173.
- Tsuji Y, Goto A, Hara I, et al. Renal cell carcinoma with extension of tumor thrombus into vena cava: Surgical strategy and prognosis. J Vasc Surg. 2001;33:789-796.
- Zisman A, Pantuck AJ, Chao DH, et al. Renal cell carcinoma with tumor thrombus: is cytoreductive nephrectomy for advanced disease associated with an increased complication rate? J Urol. 2002;168:962-967.
- Nesbitt JC, Soltero ER, Dinney CPN, et al. Surgical management of renal cell carcinoma with inferior vena cava tumor thrombus. Ann Thorac Surg. 1997;63:1592-1600.
Critical Coalition
March is an important month for SHM. It is DVT Awareness Month, and once again SHM is leading a coalition of almost 40 organizations to raise the understanding of this disease. DVT causes complications that kill more people every year than AIDS and breast cancer combined. This coalition includes the American College of Physicians, the American Public Health Association, the American College of Chest Physicians, the American Society of Health System Pharmacists, the American Association of Critical Care Nurses, and many more.
The goals of the coalition are to use our knowledge and influence to inform not only the public at large, but health professionals as well. And if our success in 2005 is any measure, the DVT Awareness campaign has really had an impact.
Last year more than 400 million people saw on TV or read our message in magazines and newspapers. Utilizing the compelling story of our national spokesperson, Melanie Bloom, a mother of three girls who lost her young, athletic NBC war-correspondent husband, David, to a fatal pulmonary embolism (PE), our message was seen on “Larry King Live” on CNN, on the “Jane Pauley Show,” on “Access Hollywood,” and in Ladies Home Journal.
Often Melanie was accompanied by hospitalists such as Frank Michota, MD, the head of the Hospital Medicine Division at Cleveland Clinic. Dr. Michota answered the clinical questions in the interviews. Who can forget when Larry King turned to Dr. Michota and asked, “Are you a cardiologist?”
“No, Larry, I am a hospitalist,” said Dr. Michota.
And when Larry King asked “What is a hospitalist?” Dr. Michota spread the gospel according to hospital medicine to a nationwide audience.
Later in the year a billboard on Rockefeller Center in New York City proclaimed the DVT Awareness message along with the SHM logo. If you can make it there, you can make it anywhere.
But this campaign isn’t just about TV appearances and magazine articles. This is about using awareness to save lives. And save lives we did. More than a thousand letters and e-mails were sent to the coalition in 2005 from patients and family members with personal stories of how exposure to our campaign led them to go to their doctors or show up in an ED. They were treated early for DVT—before they developed a potentially fatal PE. They credit the DVT Awareness Campaign with saving their lives.
In 2006 SHM is back at the head of the coalition. In January at the National Press Club, I was fortunate enough to help roll out the details of our 2006 campaign. Joining me on the dais were Dr. Michota; Geno Merli, MD, from Jefferson Medical College and a frequent speaker at SHM meetings; and Sam Goldhaber, MD, from Harvard’s Brigham and Women’s in Boston.
This year we have set a goal of further engaging the public by telling our patients’ stories, by forming patient affinity groups, by providing the tools for health professionals to provide the best care for DVT and PE, and by continuing to use the media to spread our message.
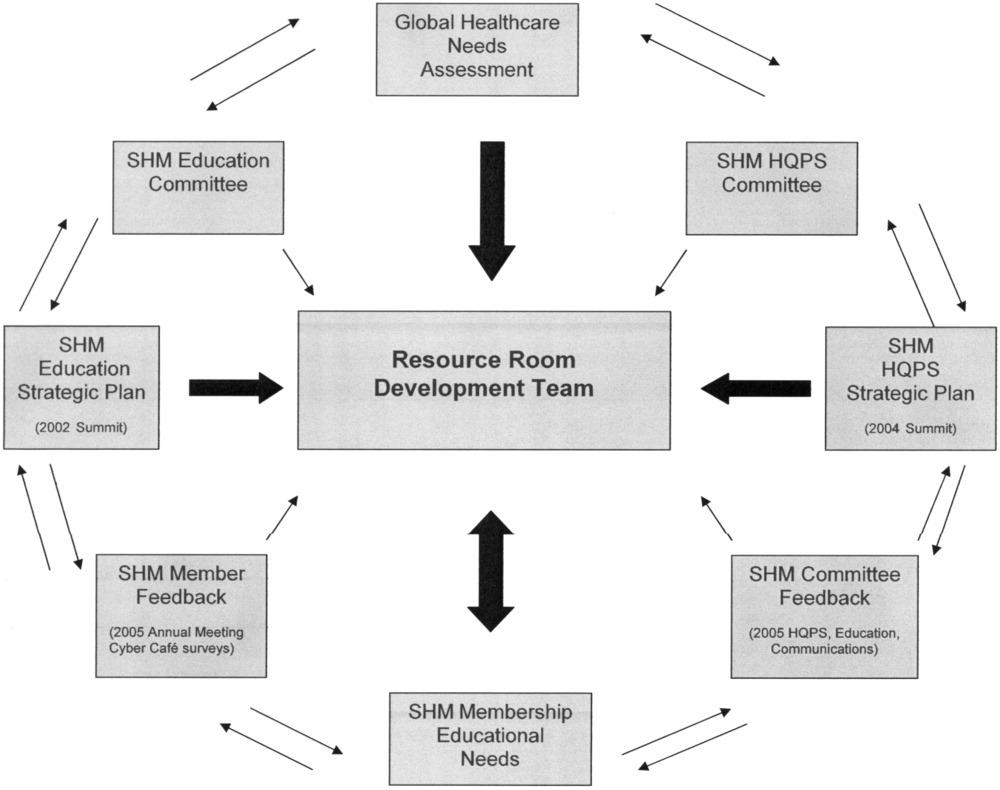
SHM has a robust set of educational and quality improvement tools in the DVT Resource Room on the SHM Web site at www.hospitalmedicine.org under the “Quality/Patient Safety” tab. There hospitalists can find an SHM DVT workbook to help measure their performance and improve their outcomes. At the SHM 2006 Annual Meeting on May 3, from 8 a.m. to 5:30 p.m., SHM will host a precourse on quality improvement, and one of the key conditions is DVT. SHM hopes to raise funds for future demonstration projects to improve patient outcomes in DVT and even to set up skilled mentors who can help hospitalists trying to affect change at their hospitals for the first time.
SHM is a young, enthusiastic organization that lacks the cynicism of entrenchment. We actually do believe with some help and support we can make quality matter, even without pay for performance and before regulated performance standards.
We see the DVT Awareness Coalition as a template for SHM’s call to action. It involves participation across the continuum involving other physicians, nurses, pharmacists, and patients. It is proactive and targeted with not only improving public knowledge, but recognizing that maybe not every doctor and nurse knows all the latest information, either. It is focused on making a tangible difference, not just writing a white paper or a guideline and declaring victory. It is about saving lives in 2005 and again in 2006. It is about multiplying the efforts of SHM by the multiple of the number of hospitals that now have hospitalists.
There is much promise to hospital medicine. Some see this as a future play with only a foundation being built today. There are surely many great things ahead for hospital medicine as we grow to more than 30,000 hospitalists at virtually every hospital in America. There are many skills left for us to learn. But hospitalists and SHM are making a difference today. We are not doing it alone, but through teamwork and coalition-building. We are proud to be a partner in the DVT Awareness Coalition and we are glad to provide leadership when asked. The payoff is in the lives we have saved and the lives we have changed for the better. TH
Dr. Wellikson has been CEO of SHM since 2000.
March is an important month for SHM. It is DVT Awareness Month, and once again SHM is leading a coalition of almost 40 organizations to raise the understanding of this disease. DVT causes complications that kill more people every year than AIDS and breast cancer combined. This coalition includes the American College of Physicians, the American Public Health Association, the American College of Chest Physicians, the American Society of Health System Pharmacists, the American Association of Critical Care Nurses, and many more.
The goals of the coalition are to use our knowledge and influence to inform not only the public at large, but health professionals as well. And if our success in 2005 is any measure, the DVT Awareness campaign has really had an impact.
Last year more than 400 million people saw on TV or read our message in magazines and newspapers. Utilizing the compelling story of our national spokesperson, Melanie Bloom, a mother of three girls who lost her young, athletic NBC war-correspondent husband, David, to a fatal pulmonary embolism (PE), our message was seen on “Larry King Live” on CNN, on the “Jane Pauley Show,” on “Access Hollywood,” and in Ladies Home Journal.
Often Melanie was accompanied by hospitalists such as Frank Michota, MD, the head of the Hospital Medicine Division at Cleveland Clinic. Dr. Michota answered the clinical questions in the interviews. Who can forget when Larry King turned to Dr. Michota and asked, “Are you a cardiologist?”
“No, Larry, I am a hospitalist,” said Dr. Michota.
And when Larry King asked “What is a hospitalist?” Dr. Michota spread the gospel according to hospital medicine to a nationwide audience.
Later in the year a billboard on Rockefeller Center in New York City proclaimed the DVT Awareness message along with the SHM logo. If you can make it there, you can make it anywhere.
But this campaign isn’t just about TV appearances and magazine articles. This is about using awareness to save lives. And save lives we did. More than a thousand letters and e-mails were sent to the coalition in 2005 from patients and family members with personal stories of how exposure to our campaign led them to go to their doctors or show up in an ED. They were treated early for DVT—before they developed a potentially fatal PE. They credit the DVT Awareness Campaign with saving their lives.
In 2006 SHM is back at the head of the coalition. In January at the National Press Club, I was fortunate enough to help roll out the details of our 2006 campaign. Joining me on the dais were Dr. Michota; Geno Merli, MD, from Jefferson Medical College and a frequent speaker at SHM meetings; and Sam Goldhaber, MD, from Harvard’s Brigham and Women’s in Boston.
This year we have set a goal of further engaging the public by telling our patients’ stories, by forming patient affinity groups, by providing the tools for health professionals to provide the best care for DVT and PE, and by continuing to use the media to spread our message.
SHM has a robust set of educational and quality improvement tools in the DVT Resource Room on the SHM Web site at www.hospitalmedicine.org under the “Quality/Patient Safety” tab. There hospitalists can find an SHM DVT workbook to help measure their performance and improve their outcomes. At the SHM 2006 Annual Meeting on May 3, from 8 a.m. to 5:30 p.m., SHM will host a precourse on quality improvement, and one of the key conditions is DVT. SHM hopes to raise funds for future demonstration projects to improve patient outcomes in DVT and even to set up skilled mentors who can help hospitalists trying to affect change at their hospitals for the first time.
SHM is a young, enthusiastic organization that lacks the cynicism of entrenchment. We actually do believe with some help and support we can make quality matter, even without pay for performance and before regulated performance standards.
We see the DVT Awareness Coalition as a template for SHM’s call to action. It involves participation across the continuum involving other physicians, nurses, pharmacists, and patients. It is proactive and targeted with not only improving public knowledge, but recognizing that maybe not every doctor and nurse knows all the latest information, either. It is focused on making a tangible difference, not just writing a white paper or a guideline and declaring victory. It is about saving lives in 2005 and again in 2006. It is about multiplying the efforts of SHM by the multiple of the number of hospitals that now have hospitalists.
There is much promise to hospital medicine. Some see this as a future play with only a foundation being built today. There are surely many great things ahead for hospital medicine as we grow to more than 30,000 hospitalists at virtually every hospital in America. There are many skills left for us to learn. But hospitalists and SHM are making a difference today. We are not doing it alone, but through teamwork and coalition-building. We are proud to be a partner in the DVT Awareness Coalition and we are glad to provide leadership when asked. The payoff is in the lives we have saved and the lives we have changed for the better. TH
Dr. Wellikson has been CEO of SHM since 2000.
March is an important month for SHM. It is DVT Awareness Month, and once again SHM is leading a coalition of almost 40 organizations to raise the understanding of this disease. DVT causes complications that kill more people every year than AIDS and breast cancer combined. This coalition includes the American College of Physicians, the American Public Health Association, the American College of Chest Physicians, the American Society of Health System Pharmacists, the American Association of Critical Care Nurses, and many more.
The goals of the coalition are to use our knowledge and influence to inform not only the public at large, but health professionals as well. And if our success in 2005 is any measure, the DVT Awareness campaign has really had an impact.
Last year more than 400 million people saw on TV or read our message in magazines and newspapers. Utilizing the compelling story of our national spokesperson, Melanie Bloom, a mother of three girls who lost her young, athletic NBC war-correspondent husband, David, to a fatal pulmonary embolism (PE), our message was seen on “Larry King Live” on CNN, on the “Jane Pauley Show,” on “Access Hollywood,” and in Ladies Home Journal.
Often Melanie was accompanied by hospitalists such as Frank Michota, MD, the head of the Hospital Medicine Division at Cleveland Clinic. Dr. Michota answered the clinical questions in the interviews. Who can forget when Larry King turned to Dr. Michota and asked, “Are you a cardiologist?”
“No, Larry, I am a hospitalist,” said Dr. Michota.
And when Larry King asked “What is a hospitalist?” Dr. Michota spread the gospel according to hospital medicine to a nationwide audience.
Later in the year a billboard on Rockefeller Center in New York City proclaimed the DVT Awareness message along with the SHM logo. If you can make it there, you can make it anywhere.
But this campaign isn’t just about TV appearances and magazine articles. This is about using awareness to save lives. And save lives we did. More than a thousand letters and e-mails were sent to the coalition in 2005 from patients and family members with personal stories of how exposure to our campaign led them to go to their doctors or show up in an ED. They were treated early for DVT—before they developed a potentially fatal PE. They credit the DVT Awareness Campaign with saving their lives.
In 2006 SHM is back at the head of the coalition. In January at the National Press Club, I was fortunate enough to help roll out the details of our 2006 campaign. Joining me on the dais were Dr. Michota; Geno Merli, MD, from Jefferson Medical College and a frequent speaker at SHM meetings; and Sam Goldhaber, MD, from Harvard’s Brigham and Women’s in Boston.
This year we have set a goal of further engaging the public by telling our patients’ stories, by forming patient affinity groups, by providing the tools for health professionals to provide the best care for DVT and PE, and by continuing to use the media to spread our message.
SHM has a robust set of educational and quality improvement tools in the DVT Resource Room on the SHM Web site at www.hospitalmedicine.org under the “Quality/Patient Safety” tab. There hospitalists can find an SHM DVT workbook to help measure their performance and improve their outcomes. At the SHM 2006 Annual Meeting on May 3, from 8 a.m. to 5:30 p.m., SHM will host a precourse on quality improvement, and one of the key conditions is DVT. SHM hopes to raise funds for future demonstration projects to improve patient outcomes in DVT and even to set up skilled mentors who can help hospitalists trying to affect change at their hospitals for the first time.
SHM is a young, enthusiastic organization that lacks the cynicism of entrenchment. We actually do believe with some help and support we can make quality matter, even without pay for performance and before regulated performance standards.
We see the DVT Awareness Coalition as a template for SHM’s call to action. It involves participation across the continuum involving other physicians, nurses, pharmacists, and patients. It is proactive and targeted with not only improving public knowledge, but recognizing that maybe not every doctor and nurse knows all the latest information, either. It is focused on making a tangible difference, not just writing a white paper or a guideline and declaring victory. It is about saving lives in 2005 and again in 2006. It is about multiplying the efforts of SHM by the multiple of the number of hospitals that now have hospitalists.
There is much promise to hospital medicine. Some see this as a future play with only a foundation being built today. There are surely many great things ahead for hospital medicine as we grow to more than 30,000 hospitalists at virtually every hospital in America. There are many skills left for us to learn. But hospitalists and SHM are making a difference today. We are not doing it alone, but through teamwork and coalition-building. We are proud to be a partner in the DVT Awareness Coalition and we are glad to provide leadership when asked. The payoff is in the lives we have saved and the lives we have changed for the better. TH
Dr. Wellikson has been CEO of SHM since 2000.
A Landmark Event
In February we experienced a landmark in the development of the field of hospital medicine with the publication of the premiere issue of the Journal of Hospital Medicine (JHM). The debut of JHM demonstrates that hospital medicine is maturing as a field and—even more importantly—that it is developing as a new field with specific issues relevant to its practice.
It is difficult to overestimate the critical role that our journal will play in the growth of our field. The content for the inaugural issue of JHM reflects the depth and breadth of hospital medicine—community acquired pneumonia, palliative care, gastrointestinal bleeding, geriatrics, and a patient’s perspective on hospital care. The many authors who submitted their manuscripts took a leap of faith that our journal would be a respected and widely read vehicle for disseminating their hard work. This leap is even greater given that JHM is not yet listed in PubMed. Nonetheless these authors believe that JHM will thrive, be well read, and influence practice and patient care.
I agree because I know the talent of hospitalists and the potential of our field. The first issue of JHM also included a supplement devoted to the core competencies in hospital medicine. These core competencies represent another milestone in the growth of our field. With the core competencies we have outlined the specific knowledge, skills, and attitudes that define who we are and what we do.
Bringing a journal from concept to reality takes a Herculean effort by many people. I especially want to thank Mark Williams, MD, editor of JHM, for his leadership and grand vision for JHM that reflects our society and field so well. I also want to thank the associate editors and editorial board for giving their time, energy, and expertise to our journal.
I want to share my gratitude and appreciation for Larry Wellikson, MD, the CEO of SHM, who took an idea and mandate presented by the SHM Board of Directors and “operationalized” it in the most effective way. Finally, I want to thank Vickie Thaw, associate publisher at John Wiley & Sons, and her publishing team who have been such great partners in this endeavor.
Growth in Research at the SHM
Papers published in JHM represent only the tip of the iceberg of research in hospital medicine. This year we had 176 abstracts submitted for presentation at our annual meeting in May. These abstracts in research, innovations, and vignettes reflect the enthusiasm, interest, and dedication of many hospitalists. I am always impressed as I read the abstracts and wander through the poster session at the amount of work and creativity represented.
What is even more impressive about these abstracts is that they reflect the breadth of hospital medicine—adult medicine and pediatrics; academic and community hospitals; clinical work and administration; internal medicine, family practice, and pediatrics; disease-specific treatments; and system approaches to care. This year for the first time we will publish the abstracts in a supplement to both The Hospitalist and JHM. All hospitalists who have an abstract accepted for the meeting will be able to cite their work. The supplement marks another advance for our society and field.
I hope that many of you who have submitted abstracts will consider turning them into manuscripts and submitting to JHM. Abstracts whet the appetite to know more, and papers provide the details to improve care.
The Importance of Pursuing Research at SHM
These efforts are critical to our field and represent one visible way that SHM pursues research. SHM must pursue research because it helps define our field. We must ensure that the questions asked are relevant to hospital medicine and that the interventions tested and solutions advocated reflect the real world.
While we welcome anyone to pursue research in hospital medicine and how to improve the care of hospitalized patients, we must ensure that hospitalists play a key role in conducting this research. Research conducted by non-hospitalists may advocate for unrealistic interventions or result in research that is not representative of our field. As the organization that represents hospitalists, SHM can also ensure that research asks the right questions and finds practical solutions with real-world applicability.
For example, SHM should promote:
- Research about best practices, innovations in care delivery, and implementation of known beneficial treatments;
- New approaches to system issues, including error reduction, inpatient-outpatient communication, information systems and transitions; and
- Clinical trials of common inpatient conditions, such as pneumonia and acute decompensated heart failure.
By playing a central role in research, SHM can also advocate for community-based initiatives that ensure research occurs where the majority of patients are cared for.
If we fail to lead in research someone else will, and others will be able to define best practices in hospital medicine. We should not let others define hospital medicine. We took a critical step in defining our field by developing and publishing the core competencies in hospital medicine. Research will be another important way for us to delineate our field. Finally, if SHM does not pursue research we risk losing our academic credentials as a society and a field. Ultimately it will be difficult to succeed as a field and specialty if we do not succeed in academic centers because that is where students and residents—the hospitalists of tomorrow—choose their careers. Hospitalists are great teachers and role models for students and residents. However, in order to ensure that the role models and teachers flourish, we need to pursue research so hospital medicine remains a legitimate part of the academic mission.
SHM Research Initiatives
Although JHM may be the most visible sign of research at SHM, it is not the only one. Research projects directly sponsored by SHM include a demonstration project evaluating interventions to improve care of patients with heart failure, a planned survey of hospitalist involvement in managing heart failure in the emergency department and observation units, and a project to develop and evaluate a tool kit to support discharge planning for elders.
I am especially proud that each of these projects involves community and academic hospitalist programs. The SHM Research Committee, chaired by Andy Auerbach, MD, has played a key role in defining a vision for research at the SHM, and I thank Dr. Auerbach and the committee for their efforts and guidance. I am also delighted that SHM recently hired Kathleen Kerr as a senior advisor for research. Kerr’s extensive experience with hospitalists, quality improvement, and research at the University of California, San Francisco, makes her the ideal person to help spearhead this important initiative at SHM. Taken together we have a strong foundation for our research initiative and ensuring that SHM plays a key role in helping to define and shepherd research in hospital medicine.
The Future of Research at SHM
As difficult as it is to publish the first issue of a new journal, the real challenge will be to publish the second issue and beyond. Sustaining the quality and breadth reflected in the first issue will take the combined efforts of the entire editorial staff at JHM, all hospitalists, and all others interested in improving the care of hospitalized patients.
The good news is that, as reflected in our abstract submissions, there is a deep pool of good work in hospital medicine to write about and publish. The other good news is that our field is one in which many of the best innovations and much of the important research comes from community settings and not just academic centers. In fact our strength in research comes from the fact that we can draw from both academic and community programs to create new, “generalizable” knowledge. An even greater strength is when these programs collaborate to take advantage of the best that each has to offer to research.
I encourage each of us to think about the work we are doing and to think about what innovative, creative, or successful program should be shared and implore each of us to submit our work to JHM. Help make JHM the best source for innovation and best practices in hospital medicine. Help shape JHM into the best possible journal it can be—the one you open right away and read through because it is so relevant to your practice.
As our field grows we will look back on this moment as a critical landmark in the development of our field. Hold on to your first issue: It may be a valuable collector’s item when volume 50 is being published and JHM is one of the world’s leading journals. What practices will we look back on and laugh at? What practices will have survived years of scrutiny? What will our field look like? Only time will tell. Read JHM to find out. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
In February we experienced a landmark in the development of the field of hospital medicine with the publication of the premiere issue of the Journal of Hospital Medicine (JHM). The debut of JHM demonstrates that hospital medicine is maturing as a field and—even more importantly—that it is developing as a new field with specific issues relevant to its practice.
It is difficult to overestimate the critical role that our journal will play in the growth of our field. The content for the inaugural issue of JHM reflects the depth and breadth of hospital medicine—community acquired pneumonia, palliative care, gastrointestinal bleeding, geriatrics, and a patient’s perspective on hospital care. The many authors who submitted their manuscripts took a leap of faith that our journal would be a respected and widely read vehicle for disseminating their hard work. This leap is even greater given that JHM is not yet listed in PubMed. Nonetheless these authors believe that JHM will thrive, be well read, and influence practice and patient care.
I agree because I know the talent of hospitalists and the potential of our field. The first issue of JHM also included a supplement devoted to the core competencies in hospital medicine. These core competencies represent another milestone in the growth of our field. With the core competencies we have outlined the specific knowledge, skills, and attitudes that define who we are and what we do.
Bringing a journal from concept to reality takes a Herculean effort by many people. I especially want to thank Mark Williams, MD, editor of JHM, for his leadership and grand vision for JHM that reflects our society and field so well. I also want to thank the associate editors and editorial board for giving their time, energy, and expertise to our journal.
I want to share my gratitude and appreciation for Larry Wellikson, MD, the CEO of SHM, who took an idea and mandate presented by the SHM Board of Directors and “operationalized” it in the most effective way. Finally, I want to thank Vickie Thaw, associate publisher at John Wiley & Sons, and her publishing team who have been such great partners in this endeavor.
Growth in Research at the SHM
Papers published in JHM represent only the tip of the iceberg of research in hospital medicine. This year we had 176 abstracts submitted for presentation at our annual meeting in May. These abstracts in research, innovations, and vignettes reflect the enthusiasm, interest, and dedication of many hospitalists. I am always impressed as I read the abstracts and wander through the poster session at the amount of work and creativity represented.
What is even more impressive about these abstracts is that they reflect the breadth of hospital medicine—adult medicine and pediatrics; academic and community hospitals; clinical work and administration; internal medicine, family practice, and pediatrics; disease-specific treatments; and system approaches to care. This year for the first time we will publish the abstracts in a supplement to both The Hospitalist and JHM. All hospitalists who have an abstract accepted for the meeting will be able to cite their work. The supplement marks another advance for our society and field.
I hope that many of you who have submitted abstracts will consider turning them into manuscripts and submitting to JHM. Abstracts whet the appetite to know more, and papers provide the details to improve care.
The Importance of Pursuing Research at SHM
These efforts are critical to our field and represent one visible way that SHM pursues research. SHM must pursue research because it helps define our field. We must ensure that the questions asked are relevant to hospital medicine and that the interventions tested and solutions advocated reflect the real world.
While we welcome anyone to pursue research in hospital medicine and how to improve the care of hospitalized patients, we must ensure that hospitalists play a key role in conducting this research. Research conducted by non-hospitalists may advocate for unrealistic interventions or result in research that is not representative of our field. As the organization that represents hospitalists, SHM can also ensure that research asks the right questions and finds practical solutions with real-world applicability.
For example, SHM should promote:
- Research about best practices, innovations in care delivery, and implementation of known beneficial treatments;
- New approaches to system issues, including error reduction, inpatient-outpatient communication, information systems and transitions; and
- Clinical trials of common inpatient conditions, such as pneumonia and acute decompensated heart failure.
By playing a central role in research, SHM can also advocate for community-based initiatives that ensure research occurs where the majority of patients are cared for.
If we fail to lead in research someone else will, and others will be able to define best practices in hospital medicine. We should not let others define hospital medicine. We took a critical step in defining our field by developing and publishing the core competencies in hospital medicine. Research will be another important way for us to delineate our field. Finally, if SHM does not pursue research we risk losing our academic credentials as a society and a field. Ultimately it will be difficult to succeed as a field and specialty if we do not succeed in academic centers because that is where students and residents—the hospitalists of tomorrow—choose their careers. Hospitalists are great teachers and role models for students and residents. However, in order to ensure that the role models and teachers flourish, we need to pursue research so hospital medicine remains a legitimate part of the academic mission.
SHM Research Initiatives
Although JHM may be the most visible sign of research at SHM, it is not the only one. Research projects directly sponsored by SHM include a demonstration project evaluating interventions to improve care of patients with heart failure, a planned survey of hospitalist involvement in managing heart failure in the emergency department and observation units, and a project to develop and evaluate a tool kit to support discharge planning for elders.
I am especially proud that each of these projects involves community and academic hospitalist programs. The SHM Research Committee, chaired by Andy Auerbach, MD, has played a key role in defining a vision for research at the SHM, and I thank Dr. Auerbach and the committee for their efforts and guidance. I am also delighted that SHM recently hired Kathleen Kerr as a senior advisor for research. Kerr’s extensive experience with hospitalists, quality improvement, and research at the University of California, San Francisco, makes her the ideal person to help spearhead this important initiative at SHM. Taken together we have a strong foundation for our research initiative and ensuring that SHM plays a key role in helping to define and shepherd research in hospital medicine.
The Future of Research at SHM
As difficult as it is to publish the first issue of a new journal, the real challenge will be to publish the second issue and beyond. Sustaining the quality and breadth reflected in the first issue will take the combined efforts of the entire editorial staff at JHM, all hospitalists, and all others interested in improving the care of hospitalized patients.
The good news is that, as reflected in our abstract submissions, there is a deep pool of good work in hospital medicine to write about and publish. The other good news is that our field is one in which many of the best innovations and much of the important research comes from community settings and not just academic centers. In fact our strength in research comes from the fact that we can draw from both academic and community programs to create new, “generalizable” knowledge. An even greater strength is when these programs collaborate to take advantage of the best that each has to offer to research.
I encourage each of us to think about the work we are doing and to think about what innovative, creative, or successful program should be shared and implore each of us to submit our work to JHM. Help make JHM the best source for innovation and best practices in hospital medicine. Help shape JHM into the best possible journal it can be—the one you open right away and read through because it is so relevant to your practice.
As our field grows we will look back on this moment as a critical landmark in the development of our field. Hold on to your first issue: It may be a valuable collector’s item when volume 50 is being published and JHM is one of the world’s leading journals. What practices will we look back on and laugh at? What practices will have survived years of scrutiny? What will our field look like? Only time will tell. Read JHM to find out. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
In February we experienced a landmark in the development of the field of hospital medicine with the publication of the premiere issue of the Journal of Hospital Medicine (JHM). The debut of JHM demonstrates that hospital medicine is maturing as a field and—even more importantly—that it is developing as a new field with specific issues relevant to its practice.
It is difficult to overestimate the critical role that our journal will play in the growth of our field. The content for the inaugural issue of JHM reflects the depth and breadth of hospital medicine—community acquired pneumonia, palliative care, gastrointestinal bleeding, geriatrics, and a patient’s perspective on hospital care. The many authors who submitted their manuscripts took a leap of faith that our journal would be a respected and widely read vehicle for disseminating their hard work. This leap is even greater given that JHM is not yet listed in PubMed. Nonetheless these authors believe that JHM will thrive, be well read, and influence practice and patient care.
I agree because I know the talent of hospitalists and the potential of our field. The first issue of JHM also included a supplement devoted to the core competencies in hospital medicine. These core competencies represent another milestone in the growth of our field. With the core competencies we have outlined the specific knowledge, skills, and attitudes that define who we are and what we do.
Bringing a journal from concept to reality takes a Herculean effort by many people. I especially want to thank Mark Williams, MD, editor of JHM, for his leadership and grand vision for JHM that reflects our society and field so well. I also want to thank the associate editors and editorial board for giving their time, energy, and expertise to our journal.
I want to share my gratitude and appreciation for Larry Wellikson, MD, the CEO of SHM, who took an idea and mandate presented by the SHM Board of Directors and “operationalized” it in the most effective way. Finally, I want to thank Vickie Thaw, associate publisher at John Wiley & Sons, and her publishing team who have been such great partners in this endeavor.
Growth in Research at the SHM
Papers published in JHM represent only the tip of the iceberg of research in hospital medicine. This year we had 176 abstracts submitted for presentation at our annual meeting in May. These abstracts in research, innovations, and vignettes reflect the enthusiasm, interest, and dedication of many hospitalists. I am always impressed as I read the abstracts and wander through the poster session at the amount of work and creativity represented.
What is even more impressive about these abstracts is that they reflect the breadth of hospital medicine—adult medicine and pediatrics; academic and community hospitals; clinical work and administration; internal medicine, family practice, and pediatrics; disease-specific treatments; and system approaches to care. This year for the first time we will publish the abstracts in a supplement to both The Hospitalist and JHM. All hospitalists who have an abstract accepted for the meeting will be able to cite their work. The supplement marks another advance for our society and field.
I hope that many of you who have submitted abstracts will consider turning them into manuscripts and submitting to JHM. Abstracts whet the appetite to know more, and papers provide the details to improve care.
The Importance of Pursuing Research at SHM
These efforts are critical to our field and represent one visible way that SHM pursues research. SHM must pursue research because it helps define our field. We must ensure that the questions asked are relevant to hospital medicine and that the interventions tested and solutions advocated reflect the real world.
While we welcome anyone to pursue research in hospital medicine and how to improve the care of hospitalized patients, we must ensure that hospitalists play a key role in conducting this research. Research conducted by non-hospitalists may advocate for unrealistic interventions or result in research that is not representative of our field. As the organization that represents hospitalists, SHM can also ensure that research asks the right questions and finds practical solutions with real-world applicability.
For example, SHM should promote:
- Research about best practices, innovations in care delivery, and implementation of known beneficial treatments;
- New approaches to system issues, including error reduction, inpatient-outpatient communication, information systems and transitions; and
- Clinical trials of common inpatient conditions, such as pneumonia and acute decompensated heart failure.
By playing a central role in research, SHM can also advocate for community-based initiatives that ensure research occurs where the majority of patients are cared for.
If we fail to lead in research someone else will, and others will be able to define best practices in hospital medicine. We should not let others define hospital medicine. We took a critical step in defining our field by developing and publishing the core competencies in hospital medicine. Research will be another important way for us to delineate our field. Finally, if SHM does not pursue research we risk losing our academic credentials as a society and a field. Ultimately it will be difficult to succeed as a field and specialty if we do not succeed in academic centers because that is where students and residents—the hospitalists of tomorrow—choose their careers. Hospitalists are great teachers and role models for students and residents. However, in order to ensure that the role models and teachers flourish, we need to pursue research so hospital medicine remains a legitimate part of the academic mission.
SHM Research Initiatives
Although JHM may be the most visible sign of research at SHM, it is not the only one. Research projects directly sponsored by SHM include a demonstration project evaluating interventions to improve care of patients with heart failure, a planned survey of hospitalist involvement in managing heart failure in the emergency department and observation units, and a project to develop and evaluate a tool kit to support discharge planning for elders.
I am especially proud that each of these projects involves community and academic hospitalist programs. The SHM Research Committee, chaired by Andy Auerbach, MD, has played a key role in defining a vision for research at the SHM, and I thank Dr. Auerbach and the committee for their efforts and guidance. I am also delighted that SHM recently hired Kathleen Kerr as a senior advisor for research. Kerr’s extensive experience with hospitalists, quality improvement, and research at the University of California, San Francisco, makes her the ideal person to help spearhead this important initiative at SHM. Taken together we have a strong foundation for our research initiative and ensuring that SHM plays a key role in helping to define and shepherd research in hospital medicine.
The Future of Research at SHM
As difficult as it is to publish the first issue of a new journal, the real challenge will be to publish the second issue and beyond. Sustaining the quality and breadth reflected in the first issue will take the combined efforts of the entire editorial staff at JHM, all hospitalists, and all others interested in improving the care of hospitalized patients.
The good news is that, as reflected in our abstract submissions, there is a deep pool of good work in hospital medicine to write about and publish. The other good news is that our field is one in which many of the best innovations and much of the important research comes from community settings and not just academic centers. In fact our strength in research comes from the fact that we can draw from both academic and community programs to create new, “generalizable” knowledge. An even greater strength is when these programs collaborate to take advantage of the best that each has to offer to research.
I encourage each of us to think about the work we are doing and to think about what innovative, creative, or successful program should be shared and implore each of us to submit our work to JHM. Help make JHM the best source for innovation and best practices in hospital medicine. Help shape JHM into the best possible journal it can be—the one you open right away and read through because it is so relevant to your practice.
As our field grows we will look back on this moment as a critical landmark in the development of our field. Hold on to your first issue: It may be a valuable collector’s item when volume 50 is being published and JHM is one of the world’s leading journals. What practices will we look back on and laugh at? What practices will have survived years of scrutiny? What will our field look like? Only time will tell. Read JHM to find out. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
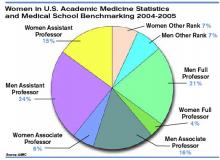
The Gender Factor
In 1980 women physicians represented 11.6% of all U.S. physicians. In 2003 they represented 26% of the total physician population.1 Drawing from the ranks of internal medicine and pediatrics, in which women physicians represent 41.8% and 65.6% of all residents, hospital medicine will likely reap the benefits of these increasing numbers.2 Indeed, hospital medicine appears to offer many advantages for women: an intrinsically collaborative working environment, flexible work hours, and the opportunity to participate in forming the structure for a new specialty. But do enough opportunities for advancement exist in this relatively young specialty?
The Hospitalist recently talked with women hospitalists, SHM leadership, and a researcher on gender discrimination in academic medicine. All shared their perceptions about how hospital medicine fares regarding inclusion of women—both in the ranks and in leadership positions.
A Career that Works
“As a woman hospitalist, I’ve had many opportunities to advocate for patient safety and quality being the primary guiding principle in reorganizing care,” says Lakshmi Halasyamani, MD, associate chair, Department of Internal Medicine and an academic hospitalist at St. Joseph Mercy Hospital, Ann Arbor, Mich. “I think as women we do juggle a lot of responsibilities, but I think those skills probably uniquely position us to be very effective in managing groups and being members and leaders of teams.”
As a mother of two young children, Dr. Halasyamani enjoys the flexibility of her current position. “I have a very busy life, but I make sure I have time to do the other parts of my life because those will never come back to me. Today, I went to my daughter’s school and helped her class with some of their math problems, and I chair a multicultural committee at her school as well.”
She finds that she brings the same type of organizational skills to both her working and family life. “Whether it’s preparing for a school assembly or preparing for a patient safety committee meeting,” explains Dr. Halasyamani, “there just isn’t time to focus on what is not important or to come unprepared. Every minute is incredibly precious.”
Like Dr. Halasyamani, Sheri Chernetsky Tejedor, MD, a clinical instructor of medicine at Emory University School of Medicine in Atlanta, has also been able to carve out a clinical and academic track that suits her present needs for family time. Under a supportive supervisor, Mark Williams, MD, FACP, professor of medicine and director, Emory Hospital Medicine Unit, and editor of the Journal of Hospital Medicine, Dr. Tejedor has worked part time as a hospitalist in a nearby community hospital; has worked in academia, including writing and research in quality improvement; and essentially has been a full-time mother when she is home. “I haven’t felt that any doors have closed, and the only ones that have closed are ones that I’ve closed myself—just accepting that I can’t do everything,” says Dr. Tejedor.
According to the AMA, 62.6% of all women physicians fall within the specialties of internal medicine, pediatrics, family medicine, obstetrics/gynecology, psychiatry, and anesthesiology.1 That is one reason the numbers of women in hospital medicine are also increasing, says Larry Wellikson, MD, FACP, CEO of SHM.
“Because hospitalists come from the ranks of pediatricians and internists, as those specialties attract more women, I think they will also find hospital medicine very attractive as they are looking for their career choice,” says Dr. Wellikson.

—Lakshmi Halasyamani, MD
Approaching Parity?
Although SHM does not currently keep statistics on percentages of women in the organization, many hospitalist services point to increasing numbers of women in their departments. For instance, SHM Past President Robert Wachter, MD, FACP, director of the hospitalist group at the University of California, San Francisco, reports that 57% (12 out of 21) of the hospitalists in his group are women. This majority does not stem from deliberate recruiting on his part.
“My goal here has been to recruit and retain the best people. I couldn’t care less whether they are women or men,” says Dr. Wachter. “I would begin to care if we were so skewed in one direction or the other that it might indicate that we weren’t providing a positive environment for either women or men. But our group has grown organically and it has just turned out that we’ve ended up with more women than men.”
Leadership Opportunities in Medicine
While overall increases in the numbers of women physicians can be seen as a hopeful sign, these percentages may mask the reality for women trying to achieve parity in leadership roles. In fact, the percentages of women in leadership positions in academic medicine remain low: For example, only 11% of department chairs in medical schools are women, and 10% of medical school deans are women.1
A higher percentage of women in a particular specialty does not necessarily translate into better advancement opportunities, according to statistician Arlene S. Ash, PhD, a research professor in the Department of General Internal Medicine at the Boston University School of Medicine. “Sadly,” she says, “the main thing you can predict about a specialty with more women is that it will be less well-paid overall.”
Many committee assignments and semi-leadership positions in the academic medicine arena are informally awarded, and they often go to men. “Often these are innocent decisions,” explains Dr. Ash. “The positions carry perks, and perhaps some regular funding, and can be stepping stones to later promotion, but they usually go to the person who pops into the mind of the administrator making the decision.”
It takes “incredible vigilance,” says Dr. Ash, “to see your way past the prejudiced lens with which we all, having grown up in this society, view the relative value of men’s and women’s contributions.”
To achieve more parity for women, Dr. Ash believes it’s necessary to more closely scrutinize and to set standards for leadership selection processes. Currently, she explains, “There is no comprehensive attempt to cast a wide net, to consider all who might be appropriate, and to ensure a non-sexist, non-biased process for choosing people to get such positions. Even in departments with more than 50% women, and even where the problem is recognized, most of these ‘gateway’ opportunities still go to guys.”
Hospitalists Breaking the Mold?
Those interviewed believe hospital medicine, as a new specialty, may have a chance to break the traditional molds established by more entrenched medical school specialties.
“We’re inventing this entire thing [the hospital medicine specialty] as we go along, so we have not had time to develop an ‘old boys’ network,’” quips Dr. Wachter. “The hope is that if you start a field now, it will not develop along those lines. As we look at those holding leadership roles at individual hospitals and in the society, you find that talented people rise to the top. If you start with a neutral playing field without the tradition and history of the smoke-filled room, it turns out that people sort out on their skills and their interests.”
“I think hospital medicine is a very accessible profession for women on a number of levels,” says Dr. Wellikson. “This is a young, growing, evolving field—as opposed to some of the more static fields in medicine, like orthopedics or thoracic surgery. One of the hallmarks of hospital medicine is creating true teams of health professionals. Women come in as equals, with good ideas, and I think this is mirrored on the SHM Board.”
Currently, four of the 12 SHM board members are women; Jean Huddleston, MD, of the Mayo Clinic is a past president; and the incoming president, Mary Jo Gorman, MD, of IPC, is also a woman. “We [the Society of Hospital Medicine] are very much an open tent,” remarks Dr. Wellikson.
According to Sylvia Cheney McKean, MD, FACP, medical director of the Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston, there are pros and cons to hospital medicine being a new specialty.
“In some ways, because [hospital medicine] is a new specialty, women may have been given the opportunity to lead hospitalist programs because early hospitalist services—at least initially—were viewed as experimental,” she says. “Many hospital leaders hired hospitalists to function as ‘super residents’ rather than as leaders. So, therefore, academic institutions didn’t really feel that they had much to lose by hiring women versus men, and many hospitalist leaders—male and female—found themselves functioning as middle managers without necessarily having much input into their job descriptions.
“Even in 2006 some physician administrators hire hospitalists with the expectation that turnover is inevitable as physicians advance to other specialties,” continues Dr. McKean. “Hospital administrators and residency directors may not understand the evolving role of hospitalists as change agents in the hospital setting and may not recognize that hospitalists offer special expertise in addition to on-site availability. So it’s a two-edged sword. A lot of hospital medicine programs, because they have not only young physician leaders, but also proportionately more female physician leaders, may find that they really cannot have the same amount of clout as other established specialties within the department of medicine hierarchy.”
Dr. Halasyamani believes that the male hierarchy may be changing. In hospital medicine, she notes, “because the emphasis in inpatient care delivery is so team focused, the leaders in hospital medicine who are able to best meet those goals and have those skills are really the ones who are being given the most opportunity. If the structures within organizations are very hierarchical, then care delivery ends up looking that way. But if the leadership and decision-making structures are more collaborative, then I think care reflects that.”
At her institution, Dr. Halasyamani has had numerous opportunities to help build some of those new structures. For example, in the past year, she helped form an institutional quality and patient safety collaborative practice team, which she chaired jointly with the head of nursing. The team “brings together people who touch the patient; they identify the barriers in delivering the type of care that we want to be proud of every time, and to help solve those problems.”
Possible Pitfalls
Can hospital medicine, in fact, succeed in developing new leadership paradigms? Much will depend on consciously constructing new systems for nurturing talent and leaders. “You really have to think through your mechanisms for recognizing and rewarding achievement and ask if those mechanisms encourage the behaviors you want to encourage, or do they disadvantage people who do the work that you most want done?” says Dr. Ash.
For example, she says, the collaborative nature of hospital medicine can create problems with career advancement. “To do something meaningful, you may need to involve 20 people on a five-year project,” she explains. “How do you ensure that those people don’t get punished for choosing that work?”
Dr. Ash, together with Boston University colleague Phyllis L. Carr, MD, and Linda Pololi, MD, from Brandeis University (the principal investigator) has started a Josiah Macy Jr. Foundation-funded project to “try to change the culture of academic medicine so that it will better encourage and reward collaborative research,” she says. “This change should benefit the entire academic enterprise—although its immediate goal is to make a common career track for women more viable.
“I want to fix a generic problem about the failure to reward certain kinds of highly desirable activities,” says Dr. Ash. “The current reward system hurts women more than men, but I’m not the slightest bit unhappy—it would be a wonderful thing, actually—for men who do collaborative research to also get the career benefits they deserve.”
Advice for Leaders and Women
Are opportunities for women hospitalists improving? Dr. McKean thinks that “hierarchies exist in hospitals, where surgeons are more powerful than physicians in the department of medicine, which has its own internal hierarchy. I see many more women interviewing for internal medicine slots. And, you could say, that’s great, it’s equalizing out. But I wonder if all it’s going to mean is that the pay scale will go down. I think that’s a real consideration. What we’re seeing now is that the starting salary for physician assistants in the hospital may be more than the starting salary for some physicians in primary care. Adding more women [to a specialty] may not change inequalities. The key is adding more women in the highest leadership positions.”
“The whole process of growing talent needs to be done in a take-control sort of way,” says Dr. Ash. There is a predictable, ongoing need to fill leadership positions, she notes, and “not enough good thought about how to systematically reach out to the entire potential talent pool.”
“Mentorship is very important,” emphasizes Dr. McKean. Her own career as a physician was characterized early on, she says, by a lack of support and mentorship. Twenty-five years later, she hopes things are beginning to change and hospital medicine may in fact set the standard for other specialties for both male and female physicians.
“Medicine is always going to be unpredictable,” she continues. “It will always be stressful. There will be acutely ill patients, and people will return [to the hospital] with unanticipated problems. You cannot change this reality. But you can change how things are structured. The more the Society of Hospital Medicine can give people the tools to identify modifiable risk factors in their own practices, help leaders of the hospitalist services analyze what works and what doesn’t work, and allow for as much diversity as possible within each service, I think that a career in hospital medicine will be sustainable and extremely satisfying, and that people will get promoted. They will find different niches in which they are expert.”
To that end, with Win Whitcomb, MD (SHM co-founder), Dr. McKean approached the SHM to charge a task force to identify what makes for a long and satisfying career in hospital medicine and to develop practice standards. The job-person fit is important, and she advises young women hospitalists to take a look at themselves, define what is important, and then “tailor a schedule around that. If it is important to you to be teaching residents, for example, then you need to be in an academic program. If it is more important to have time off, and to work shifts, then you might want to work at a community hospital. There are a lot of different models,” she says “so you have to look at yourself and your husband and the other issues you have to grapple with in addition to your career.”
Above all Dr. McKean urges women (as well as men) to be receptive to advocates or mentors within their organizations.
Going Forward
Overall, Dr. Wachter sees “the nature of the field [of hospital medicine] as one that involves a lot of collaboration and multidisciplinary work seems to draw a certain kind of person. The kind of person who is most happy and successful in our field is one who likes working closely with nurses, physical therapists, social workers, and hospital administrators, and recognizes that the quality of care and patients’ outcomes are going to be, in large part, dependent on how well that team functions.”
Many younger women and men hospitalists are finding that the job-person fit contributes to a fulfilling work/life balance.
“I chose this field because I was interested in inpatient care,” says Dr. Tejedor, and the flexibility offered by her institution has reinforced that choice. “This [hospital medicine] is a great way to have the best of everything.” TH
Writer Gretchen Henkel is based in California.
References
- Women in Medicine Statistics. Prepared by the Women Physicians Congress from Physician Characteristics and Distribution in the US, 2005 ed., Chicago. AMA Press. Available at www.ama-assn.org/ama1/pub/upload/mm/19/wimstats2005.pdf. Last accessed January 9, 2005.
- Table 2. Distribution of Residents by Specialty, 1994 Compared to 2004. Women in U.S. Academic Medicine: Statistics and Medical School Benchmarking, 2004-2005. Association of American Medical Colleges; page 12. Available at www.aamc.org/members/wim/statistics/stats05/wimstats2005.pdf. Last accessed January 9, 2005.
In 1980 women physicians represented 11.6% of all U.S. physicians. In 2003 they represented 26% of the total physician population.1 Drawing from the ranks of internal medicine and pediatrics, in which women physicians represent 41.8% and 65.6% of all residents, hospital medicine will likely reap the benefits of these increasing numbers.2 Indeed, hospital medicine appears to offer many advantages for women: an intrinsically collaborative working environment, flexible work hours, and the opportunity to participate in forming the structure for a new specialty. But do enough opportunities for advancement exist in this relatively young specialty?
The Hospitalist recently talked with women hospitalists, SHM leadership, and a researcher on gender discrimination in academic medicine. All shared their perceptions about how hospital medicine fares regarding inclusion of women—both in the ranks and in leadership positions.
A Career that Works
“As a woman hospitalist, I’ve had many opportunities to advocate for patient safety and quality being the primary guiding principle in reorganizing care,” says Lakshmi Halasyamani, MD, associate chair, Department of Internal Medicine and an academic hospitalist at St. Joseph Mercy Hospital, Ann Arbor, Mich. “I think as women we do juggle a lot of responsibilities, but I think those skills probably uniquely position us to be very effective in managing groups and being members and leaders of teams.”
As a mother of two young children, Dr. Halasyamani enjoys the flexibility of her current position. “I have a very busy life, but I make sure I have time to do the other parts of my life because those will never come back to me. Today, I went to my daughter’s school and helped her class with some of their math problems, and I chair a multicultural committee at her school as well.”
She finds that she brings the same type of organizational skills to both her working and family life. “Whether it’s preparing for a school assembly or preparing for a patient safety committee meeting,” explains Dr. Halasyamani, “there just isn’t time to focus on what is not important or to come unprepared. Every minute is incredibly precious.”
Like Dr. Halasyamani, Sheri Chernetsky Tejedor, MD, a clinical instructor of medicine at Emory University School of Medicine in Atlanta, has also been able to carve out a clinical and academic track that suits her present needs for family time. Under a supportive supervisor, Mark Williams, MD, FACP, professor of medicine and director, Emory Hospital Medicine Unit, and editor of the Journal of Hospital Medicine, Dr. Tejedor has worked part time as a hospitalist in a nearby community hospital; has worked in academia, including writing and research in quality improvement; and essentially has been a full-time mother when she is home. “I haven’t felt that any doors have closed, and the only ones that have closed are ones that I’ve closed myself—just accepting that I can’t do everything,” says Dr. Tejedor.
According to the AMA, 62.6% of all women physicians fall within the specialties of internal medicine, pediatrics, family medicine, obstetrics/gynecology, psychiatry, and anesthesiology.1 That is one reason the numbers of women in hospital medicine are also increasing, says Larry Wellikson, MD, FACP, CEO of SHM.
“Because hospitalists come from the ranks of pediatricians and internists, as those specialties attract more women, I think they will also find hospital medicine very attractive as they are looking for their career choice,” says Dr. Wellikson.

—Lakshmi Halasyamani, MD
Approaching Parity?
Although SHM does not currently keep statistics on percentages of women in the organization, many hospitalist services point to increasing numbers of women in their departments. For instance, SHM Past President Robert Wachter, MD, FACP, director of the hospitalist group at the University of California, San Francisco, reports that 57% (12 out of 21) of the hospitalists in his group are women. This majority does not stem from deliberate recruiting on his part.
“My goal here has been to recruit and retain the best people. I couldn’t care less whether they are women or men,” says Dr. Wachter. “I would begin to care if we were so skewed in one direction or the other that it might indicate that we weren’t providing a positive environment for either women or men. But our group has grown organically and it has just turned out that we’ve ended up with more women than men.”
Leadership Opportunities in Medicine
While overall increases in the numbers of women physicians can be seen as a hopeful sign, these percentages may mask the reality for women trying to achieve parity in leadership roles. In fact, the percentages of women in leadership positions in academic medicine remain low: For example, only 11% of department chairs in medical schools are women, and 10% of medical school deans are women.1
A higher percentage of women in a particular specialty does not necessarily translate into better advancement opportunities, according to statistician Arlene S. Ash, PhD, a research professor in the Department of General Internal Medicine at the Boston University School of Medicine. “Sadly,” she says, “the main thing you can predict about a specialty with more women is that it will be less well-paid overall.”
Many committee assignments and semi-leadership positions in the academic medicine arena are informally awarded, and they often go to men. “Often these are innocent decisions,” explains Dr. Ash. “The positions carry perks, and perhaps some regular funding, and can be stepping stones to later promotion, but they usually go to the person who pops into the mind of the administrator making the decision.”
It takes “incredible vigilance,” says Dr. Ash, “to see your way past the prejudiced lens with which we all, having grown up in this society, view the relative value of men’s and women’s contributions.”
To achieve more parity for women, Dr. Ash believes it’s necessary to more closely scrutinize and to set standards for leadership selection processes. Currently, she explains, “There is no comprehensive attempt to cast a wide net, to consider all who might be appropriate, and to ensure a non-sexist, non-biased process for choosing people to get such positions. Even in departments with more than 50% women, and even where the problem is recognized, most of these ‘gateway’ opportunities still go to guys.”
Hospitalists Breaking the Mold?
Those interviewed believe hospital medicine, as a new specialty, may have a chance to break the traditional molds established by more entrenched medical school specialties.
“We’re inventing this entire thing [the hospital medicine specialty] as we go along, so we have not had time to develop an ‘old boys’ network,’” quips Dr. Wachter. “The hope is that if you start a field now, it will not develop along those lines. As we look at those holding leadership roles at individual hospitals and in the society, you find that talented people rise to the top. If you start with a neutral playing field without the tradition and history of the smoke-filled room, it turns out that people sort out on their skills and their interests.”
“I think hospital medicine is a very accessible profession for women on a number of levels,” says Dr. Wellikson. “This is a young, growing, evolving field—as opposed to some of the more static fields in medicine, like orthopedics or thoracic surgery. One of the hallmarks of hospital medicine is creating true teams of health professionals. Women come in as equals, with good ideas, and I think this is mirrored on the SHM Board.”
Currently, four of the 12 SHM board members are women; Jean Huddleston, MD, of the Mayo Clinic is a past president; and the incoming president, Mary Jo Gorman, MD, of IPC, is also a woman. “We [the Society of Hospital Medicine] are very much an open tent,” remarks Dr. Wellikson.
According to Sylvia Cheney McKean, MD, FACP, medical director of the Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston, there are pros and cons to hospital medicine being a new specialty.
“In some ways, because [hospital medicine] is a new specialty, women may have been given the opportunity to lead hospitalist programs because early hospitalist services—at least initially—were viewed as experimental,” she says. “Many hospital leaders hired hospitalists to function as ‘super residents’ rather than as leaders. So, therefore, academic institutions didn’t really feel that they had much to lose by hiring women versus men, and many hospitalist leaders—male and female—found themselves functioning as middle managers without necessarily having much input into their job descriptions.
“Even in 2006 some physician administrators hire hospitalists with the expectation that turnover is inevitable as physicians advance to other specialties,” continues Dr. McKean. “Hospital administrators and residency directors may not understand the evolving role of hospitalists as change agents in the hospital setting and may not recognize that hospitalists offer special expertise in addition to on-site availability. So it’s a two-edged sword. A lot of hospital medicine programs, because they have not only young physician leaders, but also proportionately more female physician leaders, may find that they really cannot have the same amount of clout as other established specialties within the department of medicine hierarchy.”
Dr. Halasyamani believes that the male hierarchy may be changing. In hospital medicine, she notes, “because the emphasis in inpatient care delivery is so team focused, the leaders in hospital medicine who are able to best meet those goals and have those skills are really the ones who are being given the most opportunity. If the structures within organizations are very hierarchical, then care delivery ends up looking that way. But if the leadership and decision-making structures are more collaborative, then I think care reflects that.”
At her institution, Dr. Halasyamani has had numerous opportunities to help build some of those new structures. For example, in the past year, she helped form an institutional quality and patient safety collaborative practice team, which she chaired jointly with the head of nursing. The team “brings together people who touch the patient; they identify the barriers in delivering the type of care that we want to be proud of every time, and to help solve those problems.”
Possible Pitfalls
Can hospital medicine, in fact, succeed in developing new leadership paradigms? Much will depend on consciously constructing new systems for nurturing talent and leaders. “You really have to think through your mechanisms for recognizing and rewarding achievement and ask if those mechanisms encourage the behaviors you want to encourage, or do they disadvantage people who do the work that you most want done?” says Dr. Ash.
For example, she says, the collaborative nature of hospital medicine can create problems with career advancement. “To do something meaningful, you may need to involve 20 people on a five-year project,” she explains. “How do you ensure that those people don’t get punished for choosing that work?”
Dr. Ash, together with Boston University colleague Phyllis L. Carr, MD, and Linda Pololi, MD, from Brandeis University (the principal investigator) has started a Josiah Macy Jr. Foundation-funded project to “try to change the culture of academic medicine so that it will better encourage and reward collaborative research,” she says. “This change should benefit the entire academic enterprise—although its immediate goal is to make a common career track for women more viable.
“I want to fix a generic problem about the failure to reward certain kinds of highly desirable activities,” says Dr. Ash. “The current reward system hurts women more than men, but I’m not the slightest bit unhappy—it would be a wonderful thing, actually—for men who do collaborative research to also get the career benefits they deserve.”
Advice for Leaders and Women
Are opportunities for women hospitalists improving? Dr. McKean thinks that “hierarchies exist in hospitals, where surgeons are more powerful than physicians in the department of medicine, which has its own internal hierarchy. I see many more women interviewing for internal medicine slots. And, you could say, that’s great, it’s equalizing out. But I wonder if all it’s going to mean is that the pay scale will go down. I think that’s a real consideration. What we’re seeing now is that the starting salary for physician assistants in the hospital may be more than the starting salary for some physicians in primary care. Adding more women [to a specialty] may not change inequalities. The key is adding more women in the highest leadership positions.”
“The whole process of growing talent needs to be done in a take-control sort of way,” says Dr. Ash. There is a predictable, ongoing need to fill leadership positions, she notes, and “not enough good thought about how to systematically reach out to the entire potential talent pool.”
“Mentorship is very important,” emphasizes Dr. McKean. Her own career as a physician was characterized early on, she says, by a lack of support and mentorship. Twenty-five years later, she hopes things are beginning to change and hospital medicine may in fact set the standard for other specialties for both male and female physicians.
“Medicine is always going to be unpredictable,” she continues. “It will always be stressful. There will be acutely ill patients, and people will return [to the hospital] with unanticipated problems. You cannot change this reality. But you can change how things are structured. The more the Society of Hospital Medicine can give people the tools to identify modifiable risk factors in their own practices, help leaders of the hospitalist services analyze what works and what doesn’t work, and allow for as much diversity as possible within each service, I think that a career in hospital medicine will be sustainable and extremely satisfying, and that people will get promoted. They will find different niches in which they are expert.”
To that end, with Win Whitcomb, MD (SHM co-founder), Dr. McKean approached the SHM to charge a task force to identify what makes for a long and satisfying career in hospital medicine and to develop practice standards. The job-person fit is important, and she advises young women hospitalists to take a look at themselves, define what is important, and then “tailor a schedule around that. If it is important to you to be teaching residents, for example, then you need to be in an academic program. If it is more important to have time off, and to work shifts, then you might want to work at a community hospital. There are a lot of different models,” she says “so you have to look at yourself and your husband and the other issues you have to grapple with in addition to your career.”
Above all Dr. McKean urges women (as well as men) to be receptive to advocates or mentors within their organizations.
Going Forward
Overall, Dr. Wachter sees “the nature of the field [of hospital medicine] as one that involves a lot of collaboration and multidisciplinary work seems to draw a certain kind of person. The kind of person who is most happy and successful in our field is one who likes working closely with nurses, physical therapists, social workers, and hospital administrators, and recognizes that the quality of care and patients’ outcomes are going to be, in large part, dependent on how well that team functions.”
Many younger women and men hospitalists are finding that the job-person fit contributes to a fulfilling work/life balance.
“I chose this field because I was interested in inpatient care,” says Dr. Tejedor, and the flexibility offered by her institution has reinforced that choice. “This [hospital medicine] is a great way to have the best of everything.” TH
Writer Gretchen Henkel is based in California.
References
- Women in Medicine Statistics. Prepared by the Women Physicians Congress from Physician Characteristics and Distribution in the US, 2005 ed., Chicago. AMA Press. Available at www.ama-assn.org/ama1/pub/upload/mm/19/wimstats2005.pdf. Last accessed January 9, 2005.
- Table 2. Distribution of Residents by Specialty, 1994 Compared to 2004. Women in U.S. Academic Medicine: Statistics and Medical School Benchmarking, 2004-2005. Association of American Medical Colleges; page 12. Available at www.aamc.org/members/wim/statistics/stats05/wimstats2005.pdf. Last accessed January 9, 2005.
In 1980 women physicians represented 11.6% of all U.S. physicians. In 2003 they represented 26% of the total physician population.1 Drawing from the ranks of internal medicine and pediatrics, in which women physicians represent 41.8% and 65.6% of all residents, hospital medicine will likely reap the benefits of these increasing numbers.2 Indeed, hospital medicine appears to offer many advantages for women: an intrinsically collaborative working environment, flexible work hours, and the opportunity to participate in forming the structure for a new specialty. But do enough opportunities for advancement exist in this relatively young specialty?
The Hospitalist recently talked with women hospitalists, SHM leadership, and a researcher on gender discrimination in academic medicine. All shared their perceptions about how hospital medicine fares regarding inclusion of women—both in the ranks and in leadership positions.
A Career that Works
“As a woman hospitalist, I’ve had many opportunities to advocate for patient safety and quality being the primary guiding principle in reorganizing care,” says Lakshmi Halasyamani, MD, associate chair, Department of Internal Medicine and an academic hospitalist at St. Joseph Mercy Hospital, Ann Arbor, Mich. “I think as women we do juggle a lot of responsibilities, but I think those skills probably uniquely position us to be very effective in managing groups and being members and leaders of teams.”
As a mother of two young children, Dr. Halasyamani enjoys the flexibility of her current position. “I have a very busy life, but I make sure I have time to do the other parts of my life because those will never come back to me. Today, I went to my daughter’s school and helped her class with some of their math problems, and I chair a multicultural committee at her school as well.”
She finds that she brings the same type of organizational skills to both her working and family life. “Whether it’s preparing for a school assembly or preparing for a patient safety committee meeting,” explains Dr. Halasyamani, “there just isn’t time to focus on what is not important or to come unprepared. Every minute is incredibly precious.”
Like Dr. Halasyamani, Sheri Chernetsky Tejedor, MD, a clinical instructor of medicine at Emory University School of Medicine in Atlanta, has also been able to carve out a clinical and academic track that suits her present needs for family time. Under a supportive supervisor, Mark Williams, MD, FACP, professor of medicine and director, Emory Hospital Medicine Unit, and editor of the Journal of Hospital Medicine, Dr. Tejedor has worked part time as a hospitalist in a nearby community hospital; has worked in academia, including writing and research in quality improvement; and essentially has been a full-time mother when she is home. “I haven’t felt that any doors have closed, and the only ones that have closed are ones that I’ve closed myself—just accepting that I can’t do everything,” says Dr. Tejedor.
According to the AMA, 62.6% of all women physicians fall within the specialties of internal medicine, pediatrics, family medicine, obstetrics/gynecology, psychiatry, and anesthesiology.1 That is one reason the numbers of women in hospital medicine are also increasing, says Larry Wellikson, MD, FACP, CEO of SHM.
“Because hospitalists come from the ranks of pediatricians and internists, as those specialties attract more women, I think they will also find hospital medicine very attractive as they are looking for their career choice,” says Dr. Wellikson.

—Lakshmi Halasyamani, MD
Approaching Parity?
Although SHM does not currently keep statistics on percentages of women in the organization, many hospitalist services point to increasing numbers of women in their departments. For instance, SHM Past President Robert Wachter, MD, FACP, director of the hospitalist group at the University of California, San Francisco, reports that 57% (12 out of 21) of the hospitalists in his group are women. This majority does not stem from deliberate recruiting on his part.
“My goal here has been to recruit and retain the best people. I couldn’t care less whether they are women or men,” says Dr. Wachter. “I would begin to care if we were so skewed in one direction or the other that it might indicate that we weren’t providing a positive environment for either women or men. But our group has grown organically and it has just turned out that we’ve ended up with more women than men.”
Leadership Opportunities in Medicine
While overall increases in the numbers of women physicians can be seen as a hopeful sign, these percentages may mask the reality for women trying to achieve parity in leadership roles. In fact, the percentages of women in leadership positions in academic medicine remain low: For example, only 11% of department chairs in medical schools are women, and 10% of medical school deans are women.1
A higher percentage of women in a particular specialty does not necessarily translate into better advancement opportunities, according to statistician Arlene S. Ash, PhD, a research professor in the Department of General Internal Medicine at the Boston University School of Medicine. “Sadly,” she says, “the main thing you can predict about a specialty with more women is that it will be less well-paid overall.”
Many committee assignments and semi-leadership positions in the academic medicine arena are informally awarded, and they often go to men. “Often these are innocent decisions,” explains Dr. Ash. “The positions carry perks, and perhaps some regular funding, and can be stepping stones to later promotion, but they usually go to the person who pops into the mind of the administrator making the decision.”
It takes “incredible vigilance,” says Dr. Ash, “to see your way past the prejudiced lens with which we all, having grown up in this society, view the relative value of men’s and women’s contributions.”
To achieve more parity for women, Dr. Ash believes it’s necessary to more closely scrutinize and to set standards for leadership selection processes. Currently, she explains, “There is no comprehensive attempt to cast a wide net, to consider all who might be appropriate, and to ensure a non-sexist, non-biased process for choosing people to get such positions. Even in departments with more than 50% women, and even where the problem is recognized, most of these ‘gateway’ opportunities still go to guys.”
Hospitalists Breaking the Mold?
Those interviewed believe hospital medicine, as a new specialty, may have a chance to break the traditional molds established by more entrenched medical school specialties.
“We’re inventing this entire thing [the hospital medicine specialty] as we go along, so we have not had time to develop an ‘old boys’ network,’” quips Dr. Wachter. “The hope is that if you start a field now, it will not develop along those lines. As we look at those holding leadership roles at individual hospitals and in the society, you find that talented people rise to the top. If you start with a neutral playing field without the tradition and history of the smoke-filled room, it turns out that people sort out on their skills and their interests.”
“I think hospital medicine is a very accessible profession for women on a number of levels,” says Dr. Wellikson. “This is a young, growing, evolving field—as opposed to some of the more static fields in medicine, like orthopedics or thoracic surgery. One of the hallmarks of hospital medicine is creating true teams of health professionals. Women come in as equals, with good ideas, and I think this is mirrored on the SHM Board.”
Currently, four of the 12 SHM board members are women; Jean Huddleston, MD, of the Mayo Clinic is a past president; and the incoming president, Mary Jo Gorman, MD, of IPC, is also a woman. “We [the Society of Hospital Medicine] are very much an open tent,” remarks Dr. Wellikson.
According to Sylvia Cheney McKean, MD, FACP, medical director of the Brigham and Women’s Hospital/Faulkner Hospitalist Service in Boston, there are pros and cons to hospital medicine being a new specialty.
“In some ways, because [hospital medicine] is a new specialty, women may have been given the opportunity to lead hospitalist programs because early hospitalist services—at least initially—were viewed as experimental,” she says. “Many hospital leaders hired hospitalists to function as ‘super residents’ rather than as leaders. So, therefore, academic institutions didn’t really feel that they had much to lose by hiring women versus men, and many hospitalist leaders—male and female—found themselves functioning as middle managers without necessarily having much input into their job descriptions.
“Even in 2006 some physician administrators hire hospitalists with the expectation that turnover is inevitable as physicians advance to other specialties,” continues Dr. McKean. “Hospital administrators and residency directors may not understand the evolving role of hospitalists as change agents in the hospital setting and may not recognize that hospitalists offer special expertise in addition to on-site availability. So it’s a two-edged sword. A lot of hospital medicine programs, because they have not only young physician leaders, but also proportionately more female physician leaders, may find that they really cannot have the same amount of clout as other established specialties within the department of medicine hierarchy.”
Dr. Halasyamani believes that the male hierarchy may be changing. In hospital medicine, she notes, “because the emphasis in inpatient care delivery is so team focused, the leaders in hospital medicine who are able to best meet those goals and have those skills are really the ones who are being given the most opportunity. If the structures within organizations are very hierarchical, then care delivery ends up looking that way. But if the leadership and decision-making structures are more collaborative, then I think care reflects that.”
At her institution, Dr. Halasyamani has had numerous opportunities to help build some of those new structures. For example, in the past year, she helped form an institutional quality and patient safety collaborative practice team, which she chaired jointly with the head of nursing. The team “brings together people who touch the patient; they identify the barriers in delivering the type of care that we want to be proud of every time, and to help solve those problems.”
Possible Pitfalls
Can hospital medicine, in fact, succeed in developing new leadership paradigms? Much will depend on consciously constructing new systems for nurturing talent and leaders. “You really have to think through your mechanisms for recognizing and rewarding achievement and ask if those mechanisms encourage the behaviors you want to encourage, or do they disadvantage people who do the work that you most want done?” says Dr. Ash.
For example, she says, the collaborative nature of hospital medicine can create problems with career advancement. “To do something meaningful, you may need to involve 20 people on a five-year project,” she explains. “How do you ensure that those people don’t get punished for choosing that work?”
Dr. Ash, together with Boston University colleague Phyllis L. Carr, MD, and Linda Pololi, MD, from Brandeis University (the principal investigator) has started a Josiah Macy Jr. Foundation-funded project to “try to change the culture of academic medicine so that it will better encourage and reward collaborative research,” she says. “This change should benefit the entire academic enterprise—although its immediate goal is to make a common career track for women more viable.
“I want to fix a generic problem about the failure to reward certain kinds of highly desirable activities,” says Dr. Ash. “The current reward system hurts women more than men, but I’m not the slightest bit unhappy—it would be a wonderful thing, actually—for men who do collaborative research to also get the career benefits they deserve.”
Advice for Leaders and Women
Are opportunities for women hospitalists improving? Dr. McKean thinks that “hierarchies exist in hospitals, where surgeons are more powerful than physicians in the department of medicine, which has its own internal hierarchy. I see many more women interviewing for internal medicine slots. And, you could say, that’s great, it’s equalizing out. But I wonder if all it’s going to mean is that the pay scale will go down. I think that’s a real consideration. What we’re seeing now is that the starting salary for physician assistants in the hospital may be more than the starting salary for some physicians in primary care. Adding more women [to a specialty] may not change inequalities. The key is adding more women in the highest leadership positions.”
“The whole process of growing talent needs to be done in a take-control sort of way,” says Dr. Ash. There is a predictable, ongoing need to fill leadership positions, she notes, and “not enough good thought about how to systematically reach out to the entire potential talent pool.”
“Mentorship is very important,” emphasizes Dr. McKean. Her own career as a physician was characterized early on, she says, by a lack of support and mentorship. Twenty-five years later, she hopes things are beginning to change and hospital medicine may in fact set the standard for other specialties for both male and female physicians.
“Medicine is always going to be unpredictable,” she continues. “It will always be stressful. There will be acutely ill patients, and people will return [to the hospital] with unanticipated problems. You cannot change this reality. But you can change how things are structured. The more the Society of Hospital Medicine can give people the tools to identify modifiable risk factors in their own practices, help leaders of the hospitalist services analyze what works and what doesn’t work, and allow for as much diversity as possible within each service, I think that a career in hospital medicine will be sustainable and extremely satisfying, and that people will get promoted. They will find different niches in which they are expert.”
To that end, with Win Whitcomb, MD (SHM co-founder), Dr. McKean approached the SHM to charge a task force to identify what makes for a long and satisfying career in hospital medicine and to develop practice standards. The job-person fit is important, and she advises young women hospitalists to take a look at themselves, define what is important, and then “tailor a schedule around that. If it is important to you to be teaching residents, for example, then you need to be in an academic program. If it is more important to have time off, and to work shifts, then you might want to work at a community hospital. There are a lot of different models,” she says “so you have to look at yourself and your husband and the other issues you have to grapple with in addition to your career.”
Above all Dr. McKean urges women (as well as men) to be receptive to advocates or mentors within their organizations.
Going Forward
Overall, Dr. Wachter sees “the nature of the field [of hospital medicine] as one that involves a lot of collaboration and multidisciplinary work seems to draw a certain kind of person. The kind of person who is most happy and successful in our field is one who likes working closely with nurses, physical therapists, social workers, and hospital administrators, and recognizes that the quality of care and patients’ outcomes are going to be, in large part, dependent on how well that team functions.”
Many younger women and men hospitalists are finding that the job-person fit contributes to a fulfilling work/life balance.
“I chose this field because I was interested in inpatient care,” says Dr. Tejedor, and the flexibility offered by her institution has reinforced that choice. “This [hospital medicine] is a great way to have the best of everything.” TH
Writer Gretchen Henkel is based in California.
References
- Women in Medicine Statistics. Prepared by the Women Physicians Congress from Physician Characteristics and Distribution in the US, 2005 ed., Chicago. AMA Press. Available at www.ama-assn.org/ama1/pub/upload/mm/19/wimstats2005.pdf. Last accessed January 9, 2005.
- Table 2. Distribution of Residents by Specialty, 1994 Compared to 2004. Women in U.S. Academic Medicine: Statistics and Medical School Benchmarking, 2004-2005. Association of American Medical Colleges; page 12. Available at www.aamc.org/members/wim/statistics/stats05/wimstats2005.pdf. Last accessed January 9, 2005.
Proceedings of the Perioperative Medicine Summit
Summit Co-Directors and Co-Editors:
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD
Contents
Foreword: Why perioperative medicine matters more than ever
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The preoperative evaluation and use of laboratory testing
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The surgical burden: How to prevent a crisis in perioperative medicine
Michael F. Roizen, MD, Cleveland Clinic Foundation, Cleveland, OH
Anesthetics and anesthesia techniques: Impact on perioperative management and postoperative outcomes
Brian M. Parker, MD, Cleveland Clinic Foundation, Cleveland, OH
Cardiac risk stratification before noncardiac surgery
Steven L. Cohn, MD, FACP, SUNY Downstate Medical Center, Brooklyn, NY
Perioperative cardiac risk reduction: Doing it right
Andrew D. Auerbach, MD, MPH, University of California, San Francisco, CA
Quality measurement: Who is measuring outcomes and what are patients being told?
Walter G. Maurer, MD, and Christopher J. Hebert, MD, Cleveland Clinic Foundation, Cleveland, OH
Preoperative pulmonary evaluation: Identifying and reducing risks for pulmonary complications
Gerald W. Smetana, MD, Beth Israel Deaconess Medicine Center and Harvard Medical School, Boston, MA
Antibiotic prophylaxis against postoperative wound infections
Steven M. Gordon, MD, Cleveland Clinic Foundation, Cleveland, OH
Managing perioperative risk in the hip fracture patient
Wael K. Barsoum, MD; Robert Helfand, MD; Viktor Krebs, MD; and Christopher Whinney, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of the bariatric surgery patient: Focus on cardiac and anesthesia considerations
Bipan Chand, MD; David Gugliotti, MD; Philip Schauer, MD; and Karen Steckner, MD, Cleveland Clinic Foundation, Cleveland, OH
Ambulatory anesthesia: Preventing perioperative and postoperative complications
Raymond G. Borkowski, MD, Cleveland Clinic Foundation, Cleveland, OH
Evaluating postoperative fever: A focused approach
James C. Pile, MD, MetroHealth Medical Center, Cleveland, OH
Septic shock in the postoperative patient: Three important management decisions
Ali Jahan, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing postoperative pain management
R. Michael Ritchey, MD, Cleveland Clinic Foundation, Cleveland, OH
Nutritional issues in the surgical patient
Douglas L. Seidner, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative medication management: A case-based review of general principles
Wael Saber, MD, Cleveland Clinic Foundation, Cleveland, OH
Preventing venous thromboembolism in surgical patients
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of diabetes mellitus: How should we act on the limited evidence?
Byron J. Hoogwerf, MD, Cleveland Clinic Foundation, Cleveland, OH
Anticoagulation management strategies for patients on warfarin who need surgery
Amir K. Jaffer, MD, FHM, Cleveland Clinic Foundation, Cleveland, OH
Perioperative care of the elderly patient
Robert M. Palmer, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing the preoperative evaluation of patients with aortic stenosis or congestive heart failure prior to noncardiac surgery
Curtis M. Rimmerman, MD, MBA, Cleveland Clinic Foundation, Cleveland, OH
Minimizing perioperative complications in patients with renal insufficiency
Martin J. Schreiber, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Summit Co-Directors and Co-Editors:
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD
Contents
Foreword: Why perioperative medicine matters more than ever
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The preoperative evaluation and use of laboratory testing
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The surgical burden: How to prevent a crisis in perioperative medicine
Michael F. Roizen, MD, Cleveland Clinic Foundation, Cleveland, OH
Anesthetics and anesthesia techniques: Impact on perioperative management and postoperative outcomes
Brian M. Parker, MD, Cleveland Clinic Foundation, Cleveland, OH
Cardiac risk stratification before noncardiac surgery
Steven L. Cohn, MD, FACP, SUNY Downstate Medical Center, Brooklyn, NY
Perioperative cardiac risk reduction: Doing it right
Andrew D. Auerbach, MD, MPH, University of California, San Francisco, CA
Quality measurement: Who is measuring outcomes and what are patients being told?
Walter G. Maurer, MD, and Christopher J. Hebert, MD, Cleveland Clinic Foundation, Cleveland, OH
Preoperative pulmonary evaluation: Identifying and reducing risks for pulmonary complications
Gerald W. Smetana, MD, Beth Israel Deaconess Medicine Center and Harvard Medical School, Boston, MA
Antibiotic prophylaxis against postoperative wound infections
Steven M. Gordon, MD, Cleveland Clinic Foundation, Cleveland, OH
Managing perioperative risk in the hip fracture patient
Wael K. Barsoum, MD; Robert Helfand, MD; Viktor Krebs, MD; and Christopher Whinney, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of the bariatric surgery patient: Focus on cardiac and anesthesia considerations
Bipan Chand, MD; David Gugliotti, MD; Philip Schauer, MD; and Karen Steckner, MD, Cleveland Clinic Foundation, Cleveland, OH
Ambulatory anesthesia: Preventing perioperative and postoperative complications
Raymond G. Borkowski, MD, Cleveland Clinic Foundation, Cleveland, OH
Evaluating postoperative fever: A focused approach
James C. Pile, MD, MetroHealth Medical Center, Cleveland, OH
Septic shock in the postoperative patient: Three important management decisions
Ali Jahan, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing postoperative pain management
R. Michael Ritchey, MD, Cleveland Clinic Foundation, Cleveland, OH
Nutritional issues in the surgical patient
Douglas L. Seidner, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative medication management: A case-based review of general principles
Wael Saber, MD, Cleveland Clinic Foundation, Cleveland, OH
Preventing venous thromboembolism in surgical patients
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of diabetes mellitus: How should we act on the limited evidence?
Byron J. Hoogwerf, MD, Cleveland Clinic Foundation, Cleveland, OH
Anticoagulation management strategies for patients on warfarin who need surgery
Amir K. Jaffer, MD, FHM, Cleveland Clinic Foundation, Cleveland, OH
Perioperative care of the elderly patient
Robert M. Palmer, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing the preoperative evaluation of patients with aortic stenosis or congestive heart failure prior to noncardiac surgery
Curtis M. Rimmerman, MD, MBA, Cleveland Clinic Foundation, Cleveland, OH
Minimizing perioperative complications in patients with renal insufficiency
Martin J. Schreiber, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Summit Co-Directors and Co-Editors:
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD
Contents
Foreword: Why perioperative medicine matters more than ever
Amir K. Jaffer, MD, and Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The preoperative evaluation and use of laboratory testing
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
The surgical burden: How to prevent a crisis in perioperative medicine
Michael F. Roizen, MD, Cleveland Clinic Foundation, Cleveland, OH
Anesthetics and anesthesia techniques: Impact on perioperative management and postoperative outcomes
Brian M. Parker, MD, Cleveland Clinic Foundation, Cleveland, OH
Cardiac risk stratification before noncardiac surgery
Steven L. Cohn, MD, FACP, SUNY Downstate Medical Center, Brooklyn, NY
Perioperative cardiac risk reduction: Doing it right
Andrew D. Auerbach, MD, MPH, University of California, San Francisco, CA
Quality measurement: Who is measuring outcomes and what are patients being told?
Walter G. Maurer, MD, and Christopher J. Hebert, MD, Cleveland Clinic Foundation, Cleveland, OH
Preoperative pulmonary evaluation: Identifying and reducing risks for pulmonary complications
Gerald W. Smetana, MD, Beth Israel Deaconess Medicine Center and Harvard Medical School, Boston, MA
Antibiotic prophylaxis against postoperative wound infections
Steven M. Gordon, MD, Cleveland Clinic Foundation, Cleveland, OH
Managing perioperative risk in the hip fracture patient
Wael K. Barsoum, MD; Robert Helfand, MD; Viktor Krebs, MD; and Christopher Whinney, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of the bariatric surgery patient: Focus on cardiac and anesthesia considerations
Bipan Chand, MD; David Gugliotti, MD; Philip Schauer, MD; and Karen Steckner, MD, Cleveland Clinic Foundation, Cleveland, OH
Ambulatory anesthesia: Preventing perioperative and postoperative complications
Raymond G. Borkowski, MD, Cleveland Clinic Foundation, Cleveland, OH
Evaluating postoperative fever: A focused approach
James C. Pile, MD, MetroHealth Medical Center, Cleveland, OH
Septic shock in the postoperative patient: Three important management decisions
Ali Jahan, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing postoperative pain management
R. Michael Ritchey, MD, Cleveland Clinic Foundation, Cleveland, OH
Nutritional issues in the surgical patient
Douglas L. Seidner, MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative medication management: A case-based review of general principles
Wael Saber, MD, Cleveland Clinic Foundation, Cleveland, OH
Preventing venous thromboembolism in surgical patients
Franklin A. Michota, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Perioperative management of diabetes mellitus: How should we act on the limited evidence?
Byron J. Hoogwerf, MD, Cleveland Clinic Foundation, Cleveland, OH
Anticoagulation management strategies for patients on warfarin who need surgery
Amir K. Jaffer, MD, FHM, Cleveland Clinic Foundation, Cleveland, OH
Perioperative care of the elderly patient
Robert M. Palmer, MD, Cleveland Clinic Foundation, Cleveland, OH
Optimizing the preoperative evaluation of patients with aortic stenosis or congestive heart failure prior to noncardiac surgery
Curtis M. Rimmerman, MD, MBA, Cleveland Clinic Foundation, Cleveland, OH
Minimizing perioperative complications in patients with renal insufficiency
Martin J. Schreiber, Jr., MD, Cleveland Clinic Foundation, Cleveland, OH
Foreword: Why perioperative medicine matters more than ever
Managing perioperative risk in the hip fracture patient
Aldosterone receptor antagonists for heart failure: Current status, future indications
Glutamatergic TB drug ‘cools off’ anxiety disorders
Think of anxiety disorders as an overactive brain alarm that psychotropics and exposure therapy quiet via separate mechanisms. Psychotropics “cool off” the alarm by curtailing excitability of the amygdala, brainstem nuclei, and hypothalamus.1 Psychological treatments, particularly exposure therapy, seek to teach the brain not to fear the dreaded object.2
One would assume that combining medication and exposure therapy for anxiety would be beneficial, but results have been disappointing.3 Anxiolytics do not enhance—and many impede—learning that occurs during psychotherapy. When the medications are tapered, patients who receive psychotherapy plus placebo typically experience more-enduring benefit than those receiving psychotherapy plus active medication.4-6
An unlikely candidate—a glutamatergic tuberculosis (TB) drug—may offer a solution. The drug and others in its class may potentiate psychotherapy’s effects by enhancing learning rather than relief.7
Glutamate/learning link
Glutamate neurons have 3 types of glutamatergic receptors, with the NMDA and AMPA types perceived as most important because of their possible role in memory development. Creating new memories may involve strengthening signals between glutamate neurons. The exact cellular mechanism is unknown, but it may involve greater release of neurotransmitters or formation of new synapses.
Stronger signaling—and hence learning—may depend on opening the NMDA receptor to enhance postsynaptic potential.8 Opening both NMDA and AMPA receptors generates a stronger signal and allows calcium influx, compared with opening the AMPA receptor alone (Figure). This combination can activate genes that control protein synthesis and result in structural changes necessary for developing long-term memories.
D-cycloserine—a partial agonist at the NMDA receptor—is usually used as an antibiotic to treat TB. The drug also has been shown to enhance the learning process that underlies fear extinction in rats. A group at Emory University studied the effect of adding the medication to exposure therapy in humans with acrophobia.7
FigureNMDA receptor agonists may enhance learning in psychotherapy
Normally, only glutamate neurons’ AMPA receptors activate in response to glutamate release (A). Both AMPA and NMDA receptors open in response to NMDA receptor agonists like D-cycloserine (B). Consequent stronger signaling may improve memory.
Going ‘up’
The researchers developed a virtual reality exposure system in which participants felt as if they were standing in an elevator, watching the floors recede as they rose 19 stories. Exposure therapy—seven weekly 35- to 45-minute sessions—has been shown to reduce the fear patients with acrophobia experience in virtual elevators.
Of 27 subjects, 10 received placebo and 17 received D-cycloserine, 50 mg or 500 mg. Subjects took their pills 2 to 4 hours before an exposure session. All participants experienced 2 virtual exposure sessions 1 to 2 weeks apart, which is considered suboptimal treatment for acrophobia.
Three months after the study, the D-cycloserine groups showed a markedly reduced fear of heights on the virtual elevator, while the placebo group showed no change from baseline. Fear levels were measured by subjective report of discomfort at each “floor.” D-cycloserine subjects also reported significantly greater reductions in measures of acrophobia in their daily lives.
Interestingly, both the D-cycloserine and placebo groups were equally frightened during virtual reality exposure. Only later did the D-cycloserine groups report less fear when exposed to heights, indicating that D-cycloserine enhanced learning that occurred during exposure therapy.
It’s exciting to think that medications could enhance and accelerate healing by activating the appropriate receptors during psychotherapy and give patients enduring benefits without the need for continued treatment.
If shown to be effective in larger studies, glutamatergic medications plus psychotherapy could provide more effective therapy for anxiety disorder. This approach is reported to be under investigation for treating anorexia nervosa, social phobia, panic disorder, and obsessive-compulsive disorder.9
1. Lydiard RB. Break the ‘fear circuit’ in resistant panic disorder. Current Psychiatry 2003;2(11):12-22.
2. Tynes LL, Tynes SF. Panic attacks: help sufferers recover with cognitive-behavioral therapy. Current Psychiatry 2005;4(11):51-60.
3. Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: review and analysis. Clinical Psychology: Science & Practice 2005;12(1):72-86.
4. Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283(19):2529-36.
5. Haug TT, Blomhoff S, Hellstrom K, et al. Exposure therapy and sertraline in social phobia: I-year follow-up of a randomised controlled trial. Br J Psychiatry 2003;182:312-8.
6. Marks IM, Swinson RP, Basoglu M, et al. Alprazolam and exposure alone and combined in panic disorder with agoraphobia. A controlled study in London and Toronto. Br J Psychiatry 1993;162:776-87.
7. Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry 2004;61(11):1136-44.
8. Purves D, Augustine GJ, Fitzpatrick D, et al. Plasticity of mature synapses and circuits. In: Neuroscience (3rd ed). Sunderland, MA: Sinauer; 2004:575-610.
9. O’Connor A. A pill that helps ease grip of irrational fears. New York Times March 22, 2005.
Think of anxiety disorders as an overactive brain alarm that psychotropics and exposure therapy quiet via separate mechanisms. Psychotropics “cool off” the alarm by curtailing excitability of the amygdala, brainstem nuclei, and hypothalamus.1 Psychological treatments, particularly exposure therapy, seek to teach the brain not to fear the dreaded object.2
One would assume that combining medication and exposure therapy for anxiety would be beneficial, but results have been disappointing.3 Anxiolytics do not enhance—and many impede—learning that occurs during psychotherapy. When the medications are tapered, patients who receive psychotherapy plus placebo typically experience more-enduring benefit than those receiving psychotherapy plus active medication.4-6
An unlikely candidate—a glutamatergic tuberculosis (TB) drug—may offer a solution. The drug and others in its class may potentiate psychotherapy’s effects by enhancing learning rather than relief.7
Glutamate/learning link
Glutamate neurons have 3 types of glutamatergic receptors, with the NMDA and AMPA types perceived as most important because of their possible role in memory development. Creating new memories may involve strengthening signals between glutamate neurons. The exact cellular mechanism is unknown, but it may involve greater release of neurotransmitters or formation of new synapses.
Stronger signaling—and hence learning—may depend on opening the NMDA receptor to enhance postsynaptic potential.8 Opening both NMDA and AMPA receptors generates a stronger signal and allows calcium influx, compared with opening the AMPA receptor alone (Figure). This combination can activate genes that control protein synthesis and result in structural changes necessary for developing long-term memories.
D-cycloserine—a partial agonist at the NMDA receptor—is usually used as an antibiotic to treat TB. The drug also has been shown to enhance the learning process that underlies fear extinction in rats. A group at Emory University studied the effect of adding the medication to exposure therapy in humans with acrophobia.7
FigureNMDA receptor agonists may enhance learning in psychotherapy
Normally, only glutamate neurons’ AMPA receptors activate in response to glutamate release (A). Both AMPA and NMDA receptors open in response to NMDA receptor agonists like D-cycloserine (B). Consequent stronger signaling may improve memory.
Going ‘up’
The researchers developed a virtual reality exposure system in which participants felt as if they were standing in an elevator, watching the floors recede as they rose 19 stories. Exposure therapy—seven weekly 35- to 45-minute sessions—has been shown to reduce the fear patients with acrophobia experience in virtual elevators.
Of 27 subjects, 10 received placebo and 17 received D-cycloserine, 50 mg or 500 mg. Subjects took their pills 2 to 4 hours before an exposure session. All participants experienced 2 virtual exposure sessions 1 to 2 weeks apart, which is considered suboptimal treatment for acrophobia.
Three months after the study, the D-cycloserine groups showed a markedly reduced fear of heights on the virtual elevator, while the placebo group showed no change from baseline. Fear levels were measured by subjective report of discomfort at each “floor.” D-cycloserine subjects also reported significantly greater reductions in measures of acrophobia in their daily lives.
Interestingly, both the D-cycloserine and placebo groups were equally frightened during virtual reality exposure. Only later did the D-cycloserine groups report less fear when exposed to heights, indicating that D-cycloserine enhanced learning that occurred during exposure therapy.
It’s exciting to think that medications could enhance and accelerate healing by activating the appropriate receptors during psychotherapy and give patients enduring benefits without the need for continued treatment.
If shown to be effective in larger studies, glutamatergic medications plus psychotherapy could provide more effective therapy for anxiety disorder. This approach is reported to be under investigation for treating anorexia nervosa, social phobia, panic disorder, and obsessive-compulsive disorder.9
Think of anxiety disorders as an overactive brain alarm that psychotropics and exposure therapy quiet via separate mechanisms. Psychotropics “cool off” the alarm by curtailing excitability of the amygdala, brainstem nuclei, and hypothalamus.1 Psychological treatments, particularly exposure therapy, seek to teach the brain not to fear the dreaded object.2
One would assume that combining medication and exposure therapy for anxiety would be beneficial, but results have been disappointing.3 Anxiolytics do not enhance—and many impede—learning that occurs during psychotherapy. When the medications are tapered, patients who receive psychotherapy plus placebo typically experience more-enduring benefit than those receiving psychotherapy plus active medication.4-6
An unlikely candidate—a glutamatergic tuberculosis (TB) drug—may offer a solution. The drug and others in its class may potentiate psychotherapy’s effects by enhancing learning rather than relief.7
Glutamate/learning link
Glutamate neurons have 3 types of glutamatergic receptors, with the NMDA and AMPA types perceived as most important because of their possible role in memory development. Creating new memories may involve strengthening signals between glutamate neurons. The exact cellular mechanism is unknown, but it may involve greater release of neurotransmitters or formation of new synapses.
Stronger signaling—and hence learning—may depend on opening the NMDA receptor to enhance postsynaptic potential.8 Opening both NMDA and AMPA receptors generates a stronger signal and allows calcium influx, compared with opening the AMPA receptor alone (Figure). This combination can activate genes that control protein synthesis and result in structural changes necessary for developing long-term memories.
D-cycloserine—a partial agonist at the NMDA receptor—is usually used as an antibiotic to treat TB. The drug also has been shown to enhance the learning process that underlies fear extinction in rats. A group at Emory University studied the effect of adding the medication to exposure therapy in humans with acrophobia.7
FigureNMDA receptor agonists may enhance learning in psychotherapy
Normally, only glutamate neurons’ AMPA receptors activate in response to glutamate release (A). Both AMPA and NMDA receptors open in response to NMDA receptor agonists like D-cycloserine (B). Consequent stronger signaling may improve memory.
Going ‘up’
The researchers developed a virtual reality exposure system in which participants felt as if they were standing in an elevator, watching the floors recede as they rose 19 stories. Exposure therapy—seven weekly 35- to 45-minute sessions—has been shown to reduce the fear patients with acrophobia experience in virtual elevators.
Of 27 subjects, 10 received placebo and 17 received D-cycloserine, 50 mg or 500 mg. Subjects took their pills 2 to 4 hours before an exposure session. All participants experienced 2 virtual exposure sessions 1 to 2 weeks apart, which is considered suboptimal treatment for acrophobia.
Three months after the study, the D-cycloserine groups showed a markedly reduced fear of heights on the virtual elevator, while the placebo group showed no change from baseline. Fear levels were measured by subjective report of discomfort at each “floor.” D-cycloserine subjects also reported significantly greater reductions in measures of acrophobia in their daily lives.
Interestingly, both the D-cycloserine and placebo groups were equally frightened during virtual reality exposure. Only later did the D-cycloserine groups report less fear when exposed to heights, indicating that D-cycloserine enhanced learning that occurred during exposure therapy.
It’s exciting to think that medications could enhance and accelerate healing by activating the appropriate receptors during psychotherapy and give patients enduring benefits without the need for continued treatment.
If shown to be effective in larger studies, glutamatergic medications plus psychotherapy could provide more effective therapy for anxiety disorder. This approach is reported to be under investigation for treating anorexia nervosa, social phobia, panic disorder, and obsessive-compulsive disorder.9
1. Lydiard RB. Break the ‘fear circuit’ in resistant panic disorder. Current Psychiatry 2003;2(11):12-22.
2. Tynes LL, Tynes SF. Panic attacks: help sufferers recover with cognitive-behavioral therapy. Current Psychiatry 2005;4(11):51-60.
3. Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: review and analysis. Clinical Psychology: Science & Practice 2005;12(1):72-86.
4. Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283(19):2529-36.
5. Haug TT, Blomhoff S, Hellstrom K, et al. Exposure therapy and sertraline in social phobia: I-year follow-up of a randomised controlled trial. Br J Psychiatry 2003;182:312-8.
6. Marks IM, Swinson RP, Basoglu M, et al. Alprazolam and exposure alone and combined in panic disorder with agoraphobia. A controlled study in London and Toronto. Br J Psychiatry 1993;162:776-87.
7. Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry 2004;61(11):1136-44.
8. Purves D, Augustine GJ, Fitzpatrick D, et al. Plasticity of mature synapses and circuits. In: Neuroscience (3rd ed). Sunderland, MA: Sinauer; 2004:575-610.
9. O’Connor A. A pill that helps ease grip of irrational fears. New York Times March 22, 2005.
1. Lydiard RB. Break the ‘fear circuit’ in resistant panic disorder. Current Psychiatry 2003;2(11):12-22.
2. Tynes LL, Tynes SF. Panic attacks: help sufferers recover with cognitive-behavioral therapy. Current Psychiatry 2005;4(11):51-60.
3. Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: review and analysis. Clinical Psychology: Science & Practice 2005;12(1):72-86.
4. Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283(19):2529-36.
5. Haug TT, Blomhoff S, Hellstrom K, et al. Exposure therapy and sertraline in social phobia: I-year follow-up of a randomised controlled trial. Br J Psychiatry 2003;182:312-8.
6. Marks IM, Swinson RP, Basoglu M, et al. Alprazolam and exposure alone and combined in panic disorder with agoraphobia. A controlled study in London and Toronto. Br J Psychiatry 1993;162:776-87.
7. Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry 2004;61(11):1136-44.
8. Purves D, Augustine GJ, Fitzpatrick D, et al. Plasticity of mature synapses and circuits. In: Neuroscience (3rd ed). Sunderland, MA: Sinauer; 2004:575-610.
9. O’Connor A. A pill that helps ease grip of irrational fears. New York Times March 22, 2005.
How to use the core competencies in hospital medicine: A framework for curriculum development
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
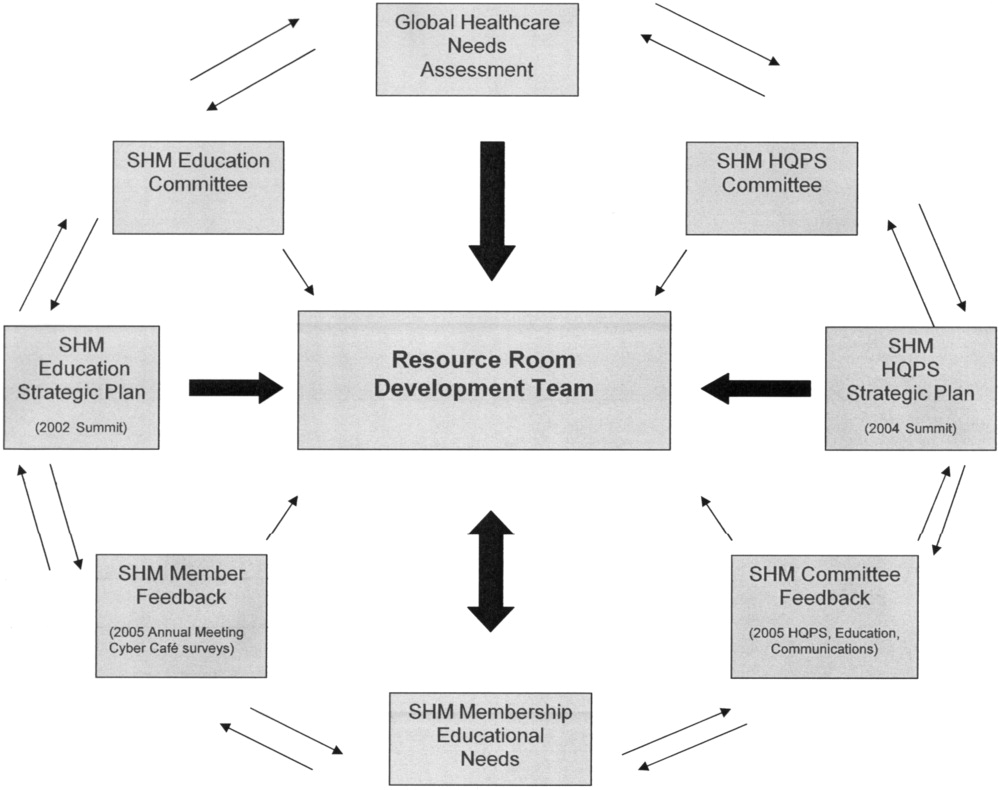
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
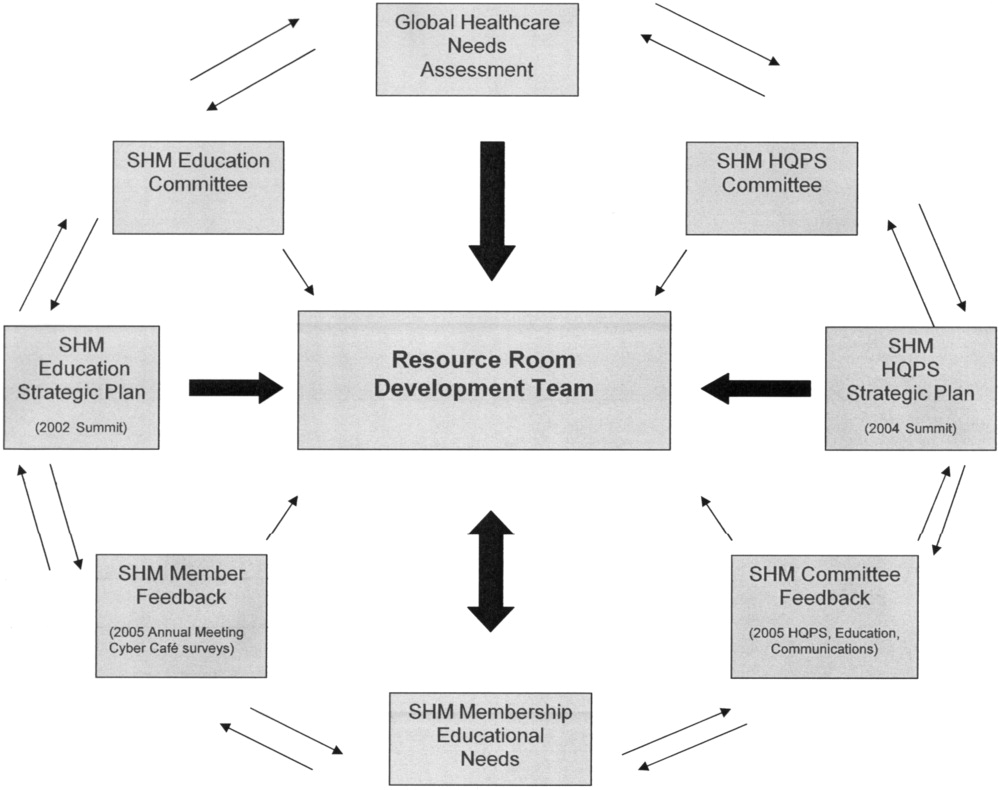
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
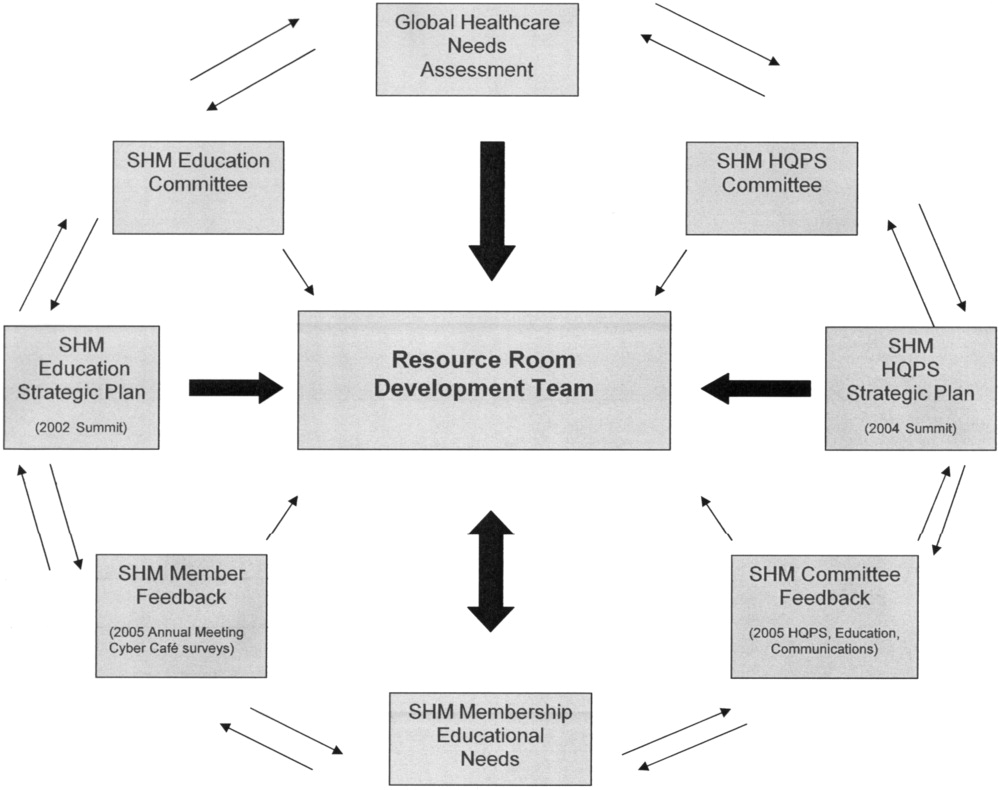
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: The focus of traditional medical education. |
| How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. | |
| Didactic lectures on the pathophysiology of VTE .rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional research | Research Questions |
| Identifying barriers to VTE prophylaxis in the hospital setting. | |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for improvement | Quality issues in the transfer of care. |
| Failure to review radiographic study. | |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other members of the inpatient team | The Current Approach: Inherent discontinuities of inpatient care. |
| ACGME legislated work hours: resident shifts. | |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for additional research | Research Questions |
| What are the key components of the sign‐out process? | |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members of the inpatient team | The Current Approach: Problems with the work environment |
| Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. | |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- Pistoria MJ, Amin AN, Dressler DD, McKean SCW, Budnitz TL, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org [accessed November2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org [accessed November2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL: http://www.med‐ed‐online.org/pdf/f0000040.pdf [accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org [accessed November2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
Copyright © 2006 Society of Hospital Medicine