User login
Amino Acid Analysis of Damaged Hair from Chemical "Relaxers"
As a follow-up to our blog about the relationship between ceramic flat iron use and trichorrhexis nodosa, we wanted to focus on the use of chemical relaxers and their association with hair damage.
Chemical relaxers have maintained their popularity over the years to make curly hair straight, especially in the African-American community. A relaxer is a chemical compound applied to curly hair to permanently break hydrogen disulfide bonds along the hair shaft to release the tight curl pattern. Typically, it is re-applied at varying intervals as new growth of unrelaxed hair occurs (Semin. Cutan. Med. Surg. 2009;28:103-8).
Relaxers have evolved from containing unusual ingredients such as lard, boiled eggs, and sodium hydroxide or lye (which is also found in many household cleaning products), to no-lye relaxers which contain guanidine hydroxide. These chemicals—whether made with or without lye—can result in hair breakage, particularly at points along the hair shaft where a new relaxer is applied to hair that has already been chemically treated.
In a recently published study, investigators performed a biochemical analysis on the hair of 30 women of African decent from Cape Town, South Africa. Of the women, 10 had natural hair (never used chemical treatments), 10 had asymptomatic relaxed hair, and 10 had symptomatic (brittle, breaking, or damaged) relaxed hair (J. Am. Acad. Dermatol. 2010; 62:402-8).
Cysteine levels were expected to be lower in chemically relaxed hair because it is estimated that 35% of cysteine changes to lanthionine during hydrolysis of the disulfide bonds (Clin. Dermatol. 1988;6:71-82).
The study found that cysteine levels were similar in proximal and distal natural hair. Levels were reduced in all relaxed hair, but were lowest in distal relaxed hair. Cysteine levels in distal and symptomatic relaxed hair were consistent with fragile, damaged hair such as that found in trichothiodystrophy.
In addition, arginine and citrulline levels were decreased, and glutamine levels were increased, in all relaxed hair when compared with natural hair. The authors noted that a decrease in arginine and citrulline has been associated with inflammation elsewhere, particularly in critically ill children, thus, relaxer use may also be associated with scalp inflammation.
However, Dr. Zoe Draelos wrote in an accompanying editorial that while cysteine levels were expected to be decreased, and this study validly confirms that, the association between decreased arginine and citrulline levels and scalp inflammation has not been as well elucidated.
Dr. Draelos, a dermatologist in High Point, N.C., also noted that prior amino acid analyses have failed to demonstrate that constituents of the body are accurately translated into the hair shaft composition in normal health. Further research is needed to elucidate whether or not relaxer use is also associated with amino acid deficiencies, which may be related to scalp inflammation, she concluded (J. Am. Acad. Dermatol. 2010;62:409-10).
As a follow-up to our blog about the relationship between ceramic flat iron use and trichorrhexis nodosa, we wanted to focus on the use of chemical relaxers and their association with hair damage.
Chemical relaxers have maintained their popularity over the years to make curly hair straight, especially in the African-American community. A relaxer is a chemical compound applied to curly hair to permanently break hydrogen disulfide bonds along the hair shaft to release the tight curl pattern. Typically, it is re-applied at varying intervals as new growth of unrelaxed hair occurs (Semin. Cutan. Med. Surg. 2009;28:103-8).
Relaxers have evolved from containing unusual ingredients such as lard, boiled eggs, and sodium hydroxide or lye (which is also found in many household cleaning products), to no-lye relaxers which contain guanidine hydroxide. These chemicals—whether made with or without lye—can result in hair breakage, particularly at points along the hair shaft where a new relaxer is applied to hair that has already been chemically treated.
In a recently published study, investigators performed a biochemical analysis on the hair of 30 women of African decent from Cape Town, South Africa. Of the women, 10 had natural hair (never used chemical treatments), 10 had asymptomatic relaxed hair, and 10 had symptomatic (brittle, breaking, or damaged) relaxed hair (J. Am. Acad. Dermatol. 2010; 62:402-8).
Cysteine levels were expected to be lower in chemically relaxed hair because it is estimated that 35% of cysteine changes to lanthionine during hydrolysis of the disulfide bonds (Clin. Dermatol. 1988;6:71-82).
The study found that cysteine levels were similar in proximal and distal natural hair. Levels were reduced in all relaxed hair, but were lowest in distal relaxed hair. Cysteine levels in distal and symptomatic relaxed hair were consistent with fragile, damaged hair such as that found in trichothiodystrophy.
In addition, arginine and citrulline levels were decreased, and glutamine levels were increased, in all relaxed hair when compared with natural hair. The authors noted that a decrease in arginine and citrulline has been associated with inflammation elsewhere, particularly in critically ill children, thus, relaxer use may also be associated with scalp inflammation.
However, Dr. Zoe Draelos wrote in an accompanying editorial that while cysteine levels were expected to be decreased, and this study validly confirms that, the association between decreased arginine and citrulline levels and scalp inflammation has not been as well elucidated.
Dr. Draelos, a dermatologist in High Point, N.C., also noted that prior amino acid analyses have failed to demonstrate that constituents of the body are accurately translated into the hair shaft composition in normal health. Further research is needed to elucidate whether or not relaxer use is also associated with amino acid deficiencies, which may be related to scalp inflammation, she concluded (J. Am. Acad. Dermatol. 2010;62:409-10).
As a follow-up to our blog about the relationship between ceramic flat iron use and trichorrhexis nodosa, we wanted to focus on the use of chemical relaxers and their association with hair damage.
Chemical relaxers have maintained their popularity over the years to make curly hair straight, especially in the African-American community. A relaxer is a chemical compound applied to curly hair to permanently break hydrogen disulfide bonds along the hair shaft to release the tight curl pattern. Typically, it is re-applied at varying intervals as new growth of unrelaxed hair occurs (Semin. Cutan. Med. Surg. 2009;28:103-8).
Relaxers have evolved from containing unusual ingredients such as lard, boiled eggs, and sodium hydroxide or lye (which is also found in many household cleaning products), to no-lye relaxers which contain guanidine hydroxide. These chemicals—whether made with or without lye—can result in hair breakage, particularly at points along the hair shaft where a new relaxer is applied to hair that has already been chemically treated.
In a recently published study, investigators performed a biochemical analysis on the hair of 30 women of African decent from Cape Town, South Africa. Of the women, 10 had natural hair (never used chemical treatments), 10 had asymptomatic relaxed hair, and 10 had symptomatic (brittle, breaking, or damaged) relaxed hair (J. Am. Acad. Dermatol. 2010; 62:402-8).
Cysteine levels were expected to be lower in chemically relaxed hair because it is estimated that 35% of cysteine changes to lanthionine during hydrolysis of the disulfide bonds (Clin. Dermatol. 1988;6:71-82).
The study found that cysteine levels were similar in proximal and distal natural hair. Levels were reduced in all relaxed hair, but were lowest in distal relaxed hair. Cysteine levels in distal and symptomatic relaxed hair were consistent with fragile, damaged hair such as that found in trichothiodystrophy.
In addition, arginine and citrulline levels were decreased, and glutamine levels were increased, in all relaxed hair when compared with natural hair. The authors noted that a decrease in arginine and citrulline has been associated with inflammation elsewhere, particularly in critically ill children, thus, relaxer use may also be associated with scalp inflammation.
However, Dr. Zoe Draelos wrote in an accompanying editorial that while cysteine levels were expected to be decreased, and this study validly confirms that, the association between decreased arginine and citrulline levels and scalp inflammation has not been as well elucidated.
Dr. Draelos, a dermatologist in High Point, N.C., also noted that prior amino acid analyses have failed to demonstrate that constituents of the body are accurately translated into the hair shaft composition in normal health. Further research is needed to elucidate whether or not relaxer use is also associated with amino acid deficiencies, which may be related to scalp inflammation, she concluded (J. Am. Acad. Dermatol. 2010;62:409-10).
ASLMS: SlimLipo Gets High Marks from Both Patients and Physicians
PHOENIX - Cosmetic results following treatment with a 924-nm laser-assisted lipolysis device achieved high patient and physician satisfaction 18 months after treatment, a single-center study demonstrated.
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss reported treatment results with the SlimLipo laser system (Palomar Medical Technologies Inc.), which he began using in April 2008.

|
This patient is shown before, and 3 months after, treatment with laser-assisted lipolysis. Photo courtesy Dr. Robert A Weiss |
The procedure involves up to three repetitions of a laser pass to melt fat and heat connective tissue followed by suction, said Dr. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md.
Data were obtained from 88 patients during follow-up visits at 1, 5, 6, 12, and 18 months. Areas treated included the abdomen (27), flanks/waist (31), thighs (14), arms (10), the submental area (12), and the knees (7). Some patients had more than one area treated.
The average fluence delivered was 28.6 kJ during the first pass, except for the submental area, which averaged 10 kJ, while the abdominal area averaged 35 kJ.
"Overall patient satisfaction was high, with 98% reporting that they were very satisfied with the results," said Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore. "Investigator assessment correlated with patient ratings, as 88% showed marked improvement at 6 and 12 months. Side effects included mild bruising in 39% of patients, which lasted for an average of 4 days." No skin burns were observed.
Dr. Weiss noted that with standard tumescent liposuction, drainage of tumescent lasts between 72 and 96 hours. With the SlimLipo, he said, duration of drainage was 12-24 hours, with a median of 14 hours. "We believe that is due to the laser channels that we make in the fat layer," he said.
Postoperative pain was rated as mild, with only five patients (6%) requiring more than nonsteroidal anti-inflammatory medications for pain control.
"No contour irregularities were noted and curved surfaces remained smooth without depressions," Dr. Weiss said. "Results achieved at 6 months were sustained for the longest follow-up at 2 years."
Dr. Weiss disclosed that he serves as a paid consultant for several medical device companies, including Palomar. He has also received speaker honoraria and research grants from the company.
PHOENIX - Cosmetic results following treatment with a 924-nm laser-assisted lipolysis device achieved high patient and physician satisfaction 18 months after treatment, a single-center study demonstrated.
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss reported treatment results with the SlimLipo laser system (Palomar Medical Technologies Inc.), which he began using in April 2008.

|
This patient is shown before, and 3 months after, treatment with laser-assisted lipolysis. Photo courtesy Dr. Robert A Weiss |
The procedure involves up to three repetitions of a laser pass to melt fat and heat connective tissue followed by suction, said Dr. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md.
Data were obtained from 88 patients during follow-up visits at 1, 5, 6, 12, and 18 months. Areas treated included the abdomen (27), flanks/waist (31), thighs (14), arms (10), the submental area (12), and the knees (7). Some patients had more than one area treated.
The average fluence delivered was 28.6 kJ during the first pass, except for the submental area, which averaged 10 kJ, while the abdominal area averaged 35 kJ.
"Overall patient satisfaction was high, with 98% reporting that they were very satisfied with the results," said Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore. "Investigator assessment correlated with patient ratings, as 88% showed marked improvement at 6 and 12 months. Side effects included mild bruising in 39% of patients, which lasted for an average of 4 days." No skin burns were observed.
Dr. Weiss noted that with standard tumescent liposuction, drainage of tumescent lasts between 72 and 96 hours. With the SlimLipo, he said, duration of drainage was 12-24 hours, with a median of 14 hours. "We believe that is due to the laser channels that we make in the fat layer," he said.
Postoperative pain was rated as mild, with only five patients (6%) requiring more than nonsteroidal anti-inflammatory medications for pain control.
"No contour irregularities were noted and curved surfaces remained smooth without depressions," Dr. Weiss said. "Results achieved at 6 months were sustained for the longest follow-up at 2 years."
Dr. Weiss disclosed that he serves as a paid consultant for several medical device companies, including Palomar. He has also received speaker honoraria and research grants from the company.
PHOENIX - Cosmetic results following treatment with a 924-nm laser-assisted lipolysis device achieved high patient and physician satisfaction 18 months after treatment, a single-center study demonstrated.
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss reported treatment results with the SlimLipo laser system (Palomar Medical Technologies Inc.), which he began using in April 2008.

|
This patient is shown before, and 3 months after, treatment with laser-assisted lipolysis. Photo courtesy Dr. Robert A Weiss |
The procedure involves up to three repetitions of a laser pass to melt fat and heat connective tissue followed by suction, said Dr. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md.
Data were obtained from 88 patients during follow-up visits at 1, 5, 6, 12, and 18 months. Areas treated included the abdomen (27), flanks/waist (31), thighs (14), arms (10), the submental area (12), and the knees (7). Some patients had more than one area treated.
The average fluence delivered was 28.6 kJ during the first pass, except for the submental area, which averaged 10 kJ, while the abdominal area averaged 35 kJ.
"Overall patient satisfaction was high, with 98% reporting that they were very satisfied with the results," said Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore. "Investigator assessment correlated with patient ratings, as 88% showed marked improvement at 6 and 12 months. Side effects included mild bruising in 39% of patients, which lasted for an average of 4 days." No skin burns were observed.
Dr. Weiss noted that with standard tumescent liposuction, drainage of tumescent lasts between 72 and 96 hours. With the SlimLipo, he said, duration of drainage was 12-24 hours, with a median of 14 hours. "We believe that is due to the laser channels that we make in the fat layer," he said.
Postoperative pain was rated as mild, with only five patients (6%) requiring more than nonsteroidal anti-inflammatory medications for pain control.
"No contour irregularities were noted and curved surfaces remained smooth without depressions," Dr. Weiss said. "Results achieved at 6 months were sustained for the longest follow-up at 2 years."
Dr. Weiss disclosed that he serves as a paid consultant for several medical device companies, including Palomar. He has also received speaker honoraria and research grants from the company.
ASLMS: SmoothShapes Reduced Thigh Circumference in Controlled Study
PHOENIX - A dual-wavelength laser system with mechanical manipulation effectively reduced thigh circumference in a multicenter, 83-patient study.
The SmoothShapes system (Elemé Medical Inc.) combines a 915-nm laser with a 650-nm LED light, which is believed to stimulate collagen regeneration and to improve and restore blood and lymphatic circulation.
The system is cleared by the Food and Drug Administration for the temporary reduction in the appearance of cellulite and features contoured rollers that massage tissue and move interstitial fluid toward the lymphatic system. A vacuum enables consistent light penetration to tissue.
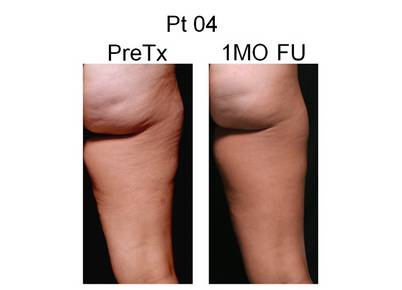
|
A study patient is shown before, and 1 month after, treatment with the SmoothShapes system for reduction of thigh circumference. Photo courtesy Dr. Robert A. Weiss |
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md., presented results from a single-blinded clinical study in which he and his associates randomly assigned women to have one thigh treated using the SmoothShapes system. The other thigh served as the control.
Each patient had circumferential measurements of the upper, mid, and lower thigh taken pre-treatment, after 4 treatments, immediately after 8 treatments, and at 1 month follow-up after completion of treatments.
Location for the measurements was determined with a laser-based device and recorded for accuracy and reproducibility. Treatment consisted of 8 twice weekly, 30-minute treatments of the entire thigh.
Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore, reported results from 83 patients treated at one of six centers. All subjects completed at least 1 month of follow-up and had no data points missing throughout the study.
The mean differences in circumferential measures on the treated and untreated thighs were consistently statistically significant at all three thigh locations (upper, mid, and lower) and at all 3 time points (after 4 treatments, immediately after 8 treatments, and at 1 month after the last treatment).
The average overall reduction among all three thigh areas treated at 1 month follow-up was 1.9 cm; the minimum loss was 0.2 cm; and the maximum loss was 8.7 cm. "We generally saw the greatest results in the upper thigh," Dr. Weiss said.
Preliminary results were similar for 47 patients who completed 3 months of follow-up, Dr. Weiss said. The average overall loss in circumference for all three thigh areas was 1.0 cm; the minimum loss was 0.1 cm; and the maximum loss was 8.7 cm.
He concluded that the SmoothShapes system "was highly effective in producing thigh circumferential reduction at each thigh location and at each evaluation time-point in the study with 1- and 3-month follow-up."
Dr. Weiss disclosed that he received equipment and consulting fees from Elemé Medical Inc. as part of the study.
PHOENIX - A dual-wavelength laser system with mechanical manipulation effectively reduced thigh circumference in a multicenter, 83-patient study.
The SmoothShapes system (Elemé Medical Inc.) combines a 915-nm laser with a 650-nm LED light, which is believed to stimulate collagen regeneration and to improve and restore blood and lymphatic circulation.
The system is cleared by the Food and Drug Administration for the temporary reduction in the appearance of cellulite and features contoured rollers that massage tissue and move interstitial fluid toward the lymphatic system. A vacuum enables consistent light penetration to tissue.
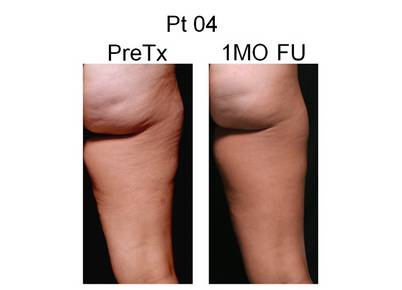
|
A study patient is shown before, and 1 month after, treatment with the SmoothShapes system for reduction of thigh circumference. Photo courtesy Dr. Robert A. Weiss |
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md., presented results from a single-blinded clinical study in which he and his associates randomly assigned women to have one thigh treated using the SmoothShapes system. The other thigh served as the control.
Each patient had circumferential measurements of the upper, mid, and lower thigh taken pre-treatment, after 4 treatments, immediately after 8 treatments, and at 1 month follow-up after completion of treatments.
Location for the measurements was determined with a laser-based device and recorded for accuracy and reproducibility. Treatment consisted of 8 twice weekly, 30-minute treatments of the entire thigh.
Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore, reported results from 83 patients treated at one of six centers. All subjects completed at least 1 month of follow-up and had no data points missing throughout the study.
The mean differences in circumferential measures on the treated and untreated thighs were consistently statistically significant at all three thigh locations (upper, mid, and lower) and at all 3 time points (after 4 treatments, immediately after 8 treatments, and at 1 month after the last treatment).
The average overall reduction among all three thigh areas treated at 1 month follow-up was 1.9 cm; the minimum loss was 0.2 cm; and the maximum loss was 8.7 cm. "We generally saw the greatest results in the upper thigh," Dr. Weiss said.
Preliminary results were similar for 47 patients who completed 3 months of follow-up, Dr. Weiss said. The average overall loss in circumference for all three thigh areas was 1.0 cm; the minimum loss was 0.1 cm; and the maximum loss was 8.7 cm.
He concluded that the SmoothShapes system "was highly effective in producing thigh circumferential reduction at each thigh location and at each evaluation time-point in the study with 1- and 3-month follow-up."
Dr. Weiss disclosed that he received equipment and consulting fees from Elemé Medical Inc. as part of the study.
PHOENIX - A dual-wavelength laser system with mechanical manipulation effectively reduced thigh circumference in a multicenter, 83-patient study.
The SmoothShapes system (Elemé Medical Inc.) combines a 915-nm laser with a 650-nm LED light, which is believed to stimulate collagen regeneration and to improve and restore blood and lymphatic circulation.
The system is cleared by the Food and Drug Administration for the temporary reduction in the appearance of cellulite and features contoured rollers that massage tissue and move interstitial fluid toward the lymphatic system. A vacuum enables consistent light penetration to tissue.
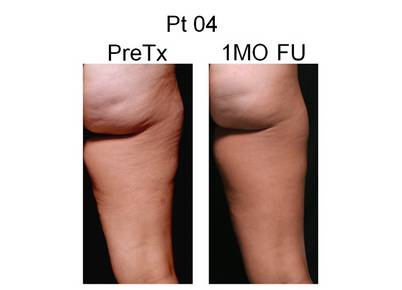
|
A study patient is shown before, and 1 month after, treatment with the SmoothShapes system for reduction of thigh circumference. Photo courtesy Dr. Robert A. Weiss |
At the annual meeting of the American Society for Laser Medicine and Surgery, Dr. Robert A. Weiss, director of the Maryland Laser, Skin, and Vein Institute in Hunt Valley, Md., presented results from a single-blinded clinical study in which he and his associates randomly assigned women to have one thigh treated using the SmoothShapes system. The other thigh served as the control.
Each patient had circumferential measurements of the upper, mid, and lower thigh taken pre-treatment, after 4 treatments, immediately after 8 treatments, and at 1 month follow-up after completion of treatments.
Location for the measurements was determined with a laser-based device and recorded for accuracy and reproducibility. Treatment consisted of 8 twice weekly, 30-minute treatments of the entire thigh.
Dr. Weiss, also of the department of dermatology at Johns Hopkins University in Baltimore, reported results from 83 patients treated at one of six centers. All subjects completed at least 1 month of follow-up and had no data points missing throughout the study.
The mean differences in circumferential measures on the treated and untreated thighs were consistently statistically significant at all three thigh locations (upper, mid, and lower) and at all 3 time points (after 4 treatments, immediately after 8 treatments, and at 1 month after the last treatment).
The average overall reduction among all three thigh areas treated at 1 month follow-up was 1.9 cm; the minimum loss was 0.2 cm; and the maximum loss was 8.7 cm. "We generally saw the greatest results in the upper thigh," Dr. Weiss said.
Preliminary results were similar for 47 patients who completed 3 months of follow-up, Dr. Weiss said. The average overall loss in circumference for all three thigh areas was 1.0 cm; the minimum loss was 0.1 cm; and the maximum loss was 8.7 cm.
He concluded that the SmoothShapes system "was highly effective in producing thigh circumferential reduction at each thigh location and at each evaluation time-point in the study with 1- and 3-month follow-up."
Dr. Weiss disclosed that he received equipment and consulting fees from Elemé Medical Inc. as part of the study.
ASLMS: Expert Reframes Skin of Color to "Skin of Cultures"
PHOENIX - Using laser technology to treat patients requires not only paying attention to the color of their skin, but also to the patient's ethnicity, according to Dr. Eliot F. Battle Jr.
"In my practice we don't just talk about skin of color anymore," Dr. Battle said at the annual meeting of the American Society for Laser Medicine and Surgery. "We talk about skin of cultures. It's not just their skin color but their ethnicity also makes a difference."
He explained that African Americans "have different combinations of black, white, Latin, Spanish, and Indian. Is my ethnicity a mixture of Nigerian, Italian, and Cherokee Indian, or am I a mixture of Cameroonian, Spanish, and Creek Indian? The future of this field, to improve the way we treat people, is going to appreciate more ethnicity as it relates to skin of color."
Brown skin "competes for the light of the laser, because melanin is absorbed across most of the photobiological spectrum, and we are a diverse population of people," said Dr. Battle, who said that he is a mix of Saharan African, Indo-European, and Asian. "To safely treat skin of color we have to use lower wavelengths, lower fluences, lower pulse durations, and aggressive epidermal cooling."
When he treats skin of color, Dr. Battle, a cosmetic dermatologist and laser
surgeon who is director of Cultura Cosmetic Medical Spa in Washington, normally favors an integrated approach and often combines laser treatments, medical skin care, and facial injectables.
For safe laser-hair removal in patients with Fitzpatrick skin types V and VI, Dr. Battle recommends using a long-pulsed diode laser and the long-pulsed Nd:YAG laser.
Safe lasers for complexion blending and skin rejuvenation to improve texture include the microsecond Nd:YAG laser, fractional therapy, the excimer laser, the Q-switched Nd:YAG laser, and the potassium-titanyl-phosphate (KTP) laser, while safe lasers for skin tightening include infrared lasers and radiofrequency technology.
"There are many lasers we can use for skin of color," he said. "The key is to find a laser that you're comfortable with. Become an expert with that laser and go forward. I don't treat skin of color with vascular lasers, resurfacing lasers, or with intense pulsed light. I don't trust most parameters supplied by the manufacturers. I find my own, safe parameters. I treat more conservatively, and I do not cause erythema or edema."
Aggressive skin cooling is key, he said, and can include ice packs, cold gel, cold liquid, cold air flow, a copper plate, and sapphire windows. "We all get side effects when our skin temperature goes past 45° C," said Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "By using longer pulse durations, and thus pouring the energy in slower, I'm able to remove heat from the skin more effectively and more efficiently. Longer pulse durations are by far the safest way to treat skin of color."
More than two-thirds of Dr. Battle's patients have darker skin. Between 2002 and 2009, the two most popular nonsurgical procedures in his practice were laser hair removal and laser complexion blending, followed by Botox injections, laser skin rejuvenation, fillers, and laser skin tightening.
Lasers "have come a long way in the last decade," he said.
If side effects occur "show compassion and empathy," Dr. Battle noted. "Allow time to help, and always be available to your patients, even if it means giving them your cell phone number."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from a number of medical device companies.
PHOENIX - Using laser technology to treat patients requires not only paying attention to the color of their skin, but also to the patient's ethnicity, according to Dr. Eliot F. Battle Jr.
"In my practice we don't just talk about skin of color anymore," Dr. Battle said at the annual meeting of the American Society for Laser Medicine and Surgery. "We talk about skin of cultures. It's not just their skin color but their ethnicity also makes a difference."
He explained that African Americans "have different combinations of black, white, Latin, Spanish, and Indian. Is my ethnicity a mixture of Nigerian, Italian, and Cherokee Indian, or am I a mixture of Cameroonian, Spanish, and Creek Indian? The future of this field, to improve the way we treat people, is going to appreciate more ethnicity as it relates to skin of color."
Brown skin "competes for the light of the laser, because melanin is absorbed across most of the photobiological spectrum, and we are a diverse population of people," said Dr. Battle, who said that he is a mix of Saharan African, Indo-European, and Asian. "To safely treat skin of color we have to use lower wavelengths, lower fluences, lower pulse durations, and aggressive epidermal cooling."
When he treats skin of color, Dr. Battle, a cosmetic dermatologist and laser
surgeon who is director of Cultura Cosmetic Medical Spa in Washington, normally favors an integrated approach and often combines laser treatments, medical skin care, and facial injectables.
For safe laser-hair removal in patients with Fitzpatrick skin types V and VI, Dr. Battle recommends using a long-pulsed diode laser and the long-pulsed Nd:YAG laser.
Safe lasers for complexion blending and skin rejuvenation to improve texture include the microsecond Nd:YAG laser, fractional therapy, the excimer laser, the Q-switched Nd:YAG laser, and the potassium-titanyl-phosphate (KTP) laser, while safe lasers for skin tightening include infrared lasers and radiofrequency technology.
"There are many lasers we can use for skin of color," he said. "The key is to find a laser that you're comfortable with. Become an expert with that laser and go forward. I don't treat skin of color with vascular lasers, resurfacing lasers, or with intense pulsed light. I don't trust most parameters supplied by the manufacturers. I find my own, safe parameters. I treat more conservatively, and I do not cause erythema or edema."
Aggressive skin cooling is key, he said, and can include ice packs, cold gel, cold liquid, cold air flow, a copper plate, and sapphire windows. "We all get side effects when our skin temperature goes past 45° C," said Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "By using longer pulse durations, and thus pouring the energy in slower, I'm able to remove heat from the skin more effectively and more efficiently. Longer pulse durations are by far the safest way to treat skin of color."
More than two-thirds of Dr. Battle's patients have darker skin. Between 2002 and 2009, the two most popular nonsurgical procedures in his practice were laser hair removal and laser complexion blending, followed by Botox injections, laser skin rejuvenation, fillers, and laser skin tightening.
Lasers "have come a long way in the last decade," he said.
If side effects occur "show compassion and empathy," Dr. Battle noted. "Allow time to help, and always be available to your patients, even if it means giving them your cell phone number."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from a number of medical device companies.
PHOENIX - Using laser technology to treat patients requires not only paying attention to the color of their skin, but also to the patient's ethnicity, according to Dr. Eliot F. Battle Jr.
"In my practice we don't just talk about skin of color anymore," Dr. Battle said at the annual meeting of the American Society for Laser Medicine and Surgery. "We talk about skin of cultures. It's not just their skin color but their ethnicity also makes a difference."
He explained that African Americans "have different combinations of black, white, Latin, Spanish, and Indian. Is my ethnicity a mixture of Nigerian, Italian, and Cherokee Indian, or am I a mixture of Cameroonian, Spanish, and Creek Indian? The future of this field, to improve the way we treat people, is going to appreciate more ethnicity as it relates to skin of color."
Brown skin "competes for the light of the laser, because melanin is absorbed across most of the photobiological spectrum, and we are a diverse population of people," said Dr. Battle, who said that he is a mix of Saharan African, Indo-European, and Asian. "To safely treat skin of color we have to use lower wavelengths, lower fluences, lower pulse durations, and aggressive epidermal cooling."
When he treats skin of color, Dr. Battle, a cosmetic dermatologist and laser
surgeon who is director of Cultura Cosmetic Medical Spa in Washington, normally favors an integrated approach and often combines laser treatments, medical skin care, and facial injectables.
For safe laser-hair removal in patients with Fitzpatrick skin types V and VI, Dr. Battle recommends using a long-pulsed diode laser and the long-pulsed Nd:YAG laser.
Safe lasers for complexion blending and skin rejuvenation to improve texture include the microsecond Nd:YAG laser, fractional therapy, the excimer laser, the Q-switched Nd:YAG laser, and the potassium-titanyl-phosphate (KTP) laser, while safe lasers for skin tightening include infrared lasers and radiofrequency technology.
"There are many lasers we can use for skin of color," he said. "The key is to find a laser that you're comfortable with. Become an expert with that laser and go forward. I don't treat skin of color with vascular lasers, resurfacing lasers, or with intense pulsed light. I don't trust most parameters supplied by the manufacturers. I find my own, safe parameters. I treat more conservatively, and I do not cause erythema or edema."
Aggressive skin cooling is key, he said, and can include ice packs, cold gel, cold liquid, cold air flow, a copper plate, and sapphire windows. "We all get side effects when our skin temperature goes past 45° C," said Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "By using longer pulse durations, and thus pouring the energy in slower, I'm able to remove heat from the skin more effectively and more efficiently. Longer pulse durations are by far the safest way to treat skin of color."
More than two-thirds of Dr. Battle's patients have darker skin. Between 2002 and 2009, the two most popular nonsurgical procedures in his practice were laser hair removal and laser complexion blending, followed by Botox injections, laser skin rejuvenation, fillers, and laser skin tightening.
Lasers "have come a long way in the last decade," he said.
If side effects occur "show compassion and empathy," Dr. Battle noted. "Allow time to help, and always be available to your patients, even if it means giving them your cell phone number."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from a number of medical device companies.
ASLMS: New Device Shrinks Upper Arms in Small Study
PHOENIX - Treatment with a radiofrequency-assisted liposuction device resulted in improved reduction of upper arm circumference up to 12 weeks post treatment, results from a small single-center study showed.

| |
A patient was treated with 20 W to 30 W of power, with a total energy of 31.5 kj per arm. |
"Traditional liposuction of the upper arms has been a challenge for patients, in particular for those with great volumes or a great amount of laxity," Dr. Lori Brightman said at the annual meeting of the American Society for Laser Medicine and Surgery. "This is a concern … for patients who want reduction of their upper arms or abdomen, because we're concerned about the loose skin that can result after removing the volume."
Dr. Brightman, of the Laser and Skin Surgery Center of New York, and her associates enrolled seven female patients with Fitzpatrick skin types II-IV to undergo treatment with BodyTite, a novel, bipolar, radiofrequency-assisted liposuction device with coagulation and simultaneous aspiration.
Manufactured by Invasix, the investigational device delivers radiofrequency energy from an internal electrode to an external electrode, which results in coagulation of adipose, vascular, and fibrous tissue, as well as heating of the soft-tissue matrix.
BodyTite features online monitoring of skin temperature, as well as monitoring of power and tissue impedance. It is powered by a 50- and 75-watt bipolar radiofrequency output system.

|
At baseline, the arm circumference was 39 cm. It reduced to 34 cm at week 12. Images courtesy Dr. Lori Brightman, Laser and Skin Surgery Center of New York |
The patients were 21-58 years old. They received one treatment on each upper arm and were assessed at 1, 3, 6, and 12 weeks. Assessments included the patient's body weight, standardized circumference tape measurements, two- and three-dimensional photography, caliper measurements, and biomechanical tissue characterization (BTC), which is an assessment of skin elasticity.
After standard tumescent anesthesia, the investigators treated the deeper planes of the upper arm skin, followed by the superficial planes; they treated to the loss of resistance at each level. The target epidermal temperature ranged from 38° C to 40° C, the radiofrequency energy ranged from 20 W to 35 W, and the total energy per zone ranged from 20.7 kJ to 30.4 kJ.
Dr. Brightman reported that the mean circumferential reduction among six of the seven patients who achieved a 6-week follow-up was 2.7 cm. Of the five patients who achieved a 12-week follow-up, the mean circumferential reduction was 4.3 cm.
The reduction in skinfold thickness (as measured by calipers) increased over time - from 7.5 mm between baseline and 3 weeks to 13.5 mm between baseline and 12 weeks. Mean skin laxity as measured by BTC went from 68% at 3 weeks to 58% at 12 weeks. Reduction in upper arm circumference was also evident on two- and three-dimensional photographs, Dr. Brightman said.
"You can improve and reduce the size of these larger arms with greater laxity with this bipolar radiofrequency device," she concluded.
Dr. Brightman disclosed that she is a clinical investigator for a number of device companies, including Invasix. She also holds stock options in the company.
PHOENIX - Treatment with a radiofrequency-assisted liposuction device resulted in improved reduction of upper arm circumference up to 12 weeks post treatment, results from a small single-center study showed.

| |
A patient was treated with 20 W to 30 W of power, with a total energy of 31.5 kj per arm. |
"Traditional liposuction of the upper arms has been a challenge for patients, in particular for those with great volumes or a great amount of laxity," Dr. Lori Brightman said at the annual meeting of the American Society for Laser Medicine and Surgery. "This is a concern … for patients who want reduction of their upper arms or abdomen, because we're concerned about the loose skin that can result after removing the volume."
Dr. Brightman, of the Laser and Skin Surgery Center of New York, and her associates enrolled seven female patients with Fitzpatrick skin types II-IV to undergo treatment with BodyTite, a novel, bipolar, radiofrequency-assisted liposuction device with coagulation and simultaneous aspiration.
Manufactured by Invasix, the investigational device delivers radiofrequency energy from an internal electrode to an external electrode, which results in coagulation of adipose, vascular, and fibrous tissue, as well as heating of the soft-tissue matrix.
BodyTite features online monitoring of skin temperature, as well as monitoring of power and tissue impedance. It is powered by a 50- and 75-watt bipolar radiofrequency output system.

|
At baseline, the arm circumference was 39 cm. It reduced to 34 cm at week 12. Images courtesy Dr. Lori Brightman, Laser and Skin Surgery Center of New York |
The patients were 21-58 years old. They received one treatment on each upper arm and were assessed at 1, 3, 6, and 12 weeks. Assessments included the patient's body weight, standardized circumference tape measurements, two- and three-dimensional photography, caliper measurements, and biomechanical tissue characterization (BTC), which is an assessment of skin elasticity.
After standard tumescent anesthesia, the investigators treated the deeper planes of the upper arm skin, followed by the superficial planes; they treated to the loss of resistance at each level. The target epidermal temperature ranged from 38° C to 40° C, the radiofrequency energy ranged from 20 W to 35 W, and the total energy per zone ranged from 20.7 kJ to 30.4 kJ.
Dr. Brightman reported that the mean circumferential reduction among six of the seven patients who achieved a 6-week follow-up was 2.7 cm. Of the five patients who achieved a 12-week follow-up, the mean circumferential reduction was 4.3 cm.
The reduction in skinfold thickness (as measured by calipers) increased over time - from 7.5 mm between baseline and 3 weeks to 13.5 mm between baseline and 12 weeks. Mean skin laxity as measured by BTC went from 68% at 3 weeks to 58% at 12 weeks. Reduction in upper arm circumference was also evident on two- and three-dimensional photographs, Dr. Brightman said.
"You can improve and reduce the size of these larger arms with greater laxity with this bipolar radiofrequency device," she concluded.
Dr. Brightman disclosed that she is a clinical investigator for a number of device companies, including Invasix. She also holds stock options in the company.
PHOENIX - Treatment with a radiofrequency-assisted liposuction device resulted in improved reduction of upper arm circumference up to 12 weeks post treatment, results from a small single-center study showed.

| |
A patient was treated with 20 W to 30 W of power, with a total energy of 31.5 kj per arm. |
"Traditional liposuction of the upper arms has been a challenge for patients, in particular for those with great volumes or a great amount of laxity," Dr. Lori Brightman said at the annual meeting of the American Society for Laser Medicine and Surgery. "This is a concern … for patients who want reduction of their upper arms or abdomen, because we're concerned about the loose skin that can result after removing the volume."
Dr. Brightman, of the Laser and Skin Surgery Center of New York, and her associates enrolled seven female patients with Fitzpatrick skin types II-IV to undergo treatment with BodyTite, a novel, bipolar, radiofrequency-assisted liposuction device with coagulation and simultaneous aspiration.
Manufactured by Invasix, the investigational device delivers radiofrequency energy from an internal electrode to an external electrode, which results in coagulation of adipose, vascular, and fibrous tissue, as well as heating of the soft-tissue matrix.
BodyTite features online monitoring of skin temperature, as well as monitoring of power and tissue impedance. It is powered by a 50- and 75-watt bipolar radiofrequency output system.

|
At baseline, the arm circumference was 39 cm. It reduced to 34 cm at week 12. Images courtesy Dr. Lori Brightman, Laser and Skin Surgery Center of New York |
The patients were 21-58 years old. They received one treatment on each upper arm and were assessed at 1, 3, 6, and 12 weeks. Assessments included the patient's body weight, standardized circumference tape measurements, two- and three-dimensional photography, caliper measurements, and biomechanical tissue characterization (BTC), which is an assessment of skin elasticity.
After standard tumescent anesthesia, the investigators treated the deeper planes of the upper arm skin, followed by the superficial planes; they treated to the loss of resistance at each level. The target epidermal temperature ranged from 38° C to 40° C, the radiofrequency energy ranged from 20 W to 35 W, and the total energy per zone ranged from 20.7 kJ to 30.4 kJ.
Dr. Brightman reported that the mean circumferential reduction among six of the seven patients who achieved a 6-week follow-up was 2.7 cm. Of the five patients who achieved a 12-week follow-up, the mean circumferential reduction was 4.3 cm.
The reduction in skinfold thickness (as measured by calipers) increased over time - from 7.5 mm between baseline and 3 weeks to 13.5 mm between baseline and 12 weeks. Mean skin laxity as measured by BTC went from 68% at 3 weeks to 58% at 12 weeks. Reduction in upper arm circumference was also evident on two- and three-dimensional photographs, Dr. Brightman said.
"You can improve and reduce the size of these larger arms with greater laxity with this bipolar radiofrequency device," she concluded.
Dr. Brightman disclosed that she is a clinical investigator for a number of device companies, including Invasix. She also holds stock options in the company.
ASLMS: Complexion Blending Tops Hair Removal in Skin of Color Practice
PHOENIX - In the last 2 years, complexion blending has been the most sought-after procedure in Dr. Eliot F. Battle Jr.'s practice.
One of his favorite devices for treating dark spots, melasma, postinflammatory hyperpigmentation, and scarring is the microsecond Nd:YAG laser. With this device, "we're driving heat down deep and trying to break up pigment … that's been encapsulated by membranes," Dr. Battle said. "For a dark spot to last for months or years, we know there is a pigment problem in the dermis. Fractional technology has also been used, but we treat conservatively. I don't ever use the manufacturer's parameters. I don't cause erythema or edema. I'm always under the threshold of redness and swelling."
Speaking during the annual meeting of the American Society for Laser Medicine and Surgery on laser treatment for skin of color patients, Dr. Battle's take-home advice was to reduce conventional parameters and fluences to avoid erythema and edema.
"There are many lasers to use on Caucasians for complexion blending," he said.
"For skin of color, we're limited to the microsecond Nd:YAG, Q-switched Nd:YAG, KTP [potassium-titanyl-phosphate], and infrared lasers."
Prior to treatment he asks patients about their ethnic background because ethnicity plays as much a role in how their skin reacts as their skin color, he said.
He also gets a sun protection history to find out whether he will be treating brown skin that is sun protected, as is the case with some people of Pacific-Asian ancestry, or whether he will be treating brown skin that has been suntanned, as is the case with some people of African-American ancestry.
"Don't make assumptions," he said. "Don't think that the person in front of you, who has the same skin color as the person you just treated, has the same response to lasers, because the ethnicity of the patient dictates how the skin reacts as much as their skin color."
He also recommends investing in an imaging system, such as the VISIA Complexion Analysis system, "that allows us to see what we're treating."
To maximize results of complexion blending, consider concomitant nonlaser "old-school" treatments, such as aesthetic peels, hydroquinone, and a hyfrecator, he said.
"The true art of cosmetic therapy is integrating spa treatments, cosmeceuticals,
prescription medications, and lasers all together," remarked Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "Lasers don't speak for themselves, particularly when treating pigmented lesions such as melasma and dark spots. We really have to take advantage of the product side of this, also. We have most of our patients on alpha hydroxy acids, Retin A, vitamin C, and we use hydroquinone bleaching cream up to 12%. I'm not bashful with hydroquinone. I monitor them very closely, but I think our patients can benefit from a higher strength."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from numerous medical device companies, including Canfield.
PHOENIX - In the last 2 years, complexion blending has been the most sought-after procedure in Dr. Eliot F. Battle Jr.'s practice.
One of his favorite devices for treating dark spots, melasma, postinflammatory hyperpigmentation, and scarring is the microsecond Nd:YAG laser. With this device, "we're driving heat down deep and trying to break up pigment … that's been encapsulated by membranes," Dr. Battle said. "For a dark spot to last for months or years, we know there is a pigment problem in the dermis. Fractional technology has also been used, but we treat conservatively. I don't ever use the manufacturer's parameters. I don't cause erythema or edema. I'm always under the threshold of redness and swelling."
Speaking during the annual meeting of the American Society for Laser Medicine and Surgery on laser treatment for skin of color patients, Dr. Battle's take-home advice was to reduce conventional parameters and fluences to avoid erythema and edema.
"There are many lasers to use on Caucasians for complexion blending," he said.
"For skin of color, we're limited to the microsecond Nd:YAG, Q-switched Nd:YAG, KTP [potassium-titanyl-phosphate], and infrared lasers."
Prior to treatment he asks patients about their ethnic background because ethnicity plays as much a role in how their skin reacts as their skin color, he said.
He also gets a sun protection history to find out whether he will be treating brown skin that is sun protected, as is the case with some people of Pacific-Asian ancestry, or whether he will be treating brown skin that has been suntanned, as is the case with some people of African-American ancestry.
"Don't make assumptions," he said. "Don't think that the person in front of you, who has the same skin color as the person you just treated, has the same response to lasers, because the ethnicity of the patient dictates how the skin reacts as much as their skin color."
He also recommends investing in an imaging system, such as the VISIA Complexion Analysis system, "that allows us to see what we're treating."
To maximize results of complexion blending, consider concomitant nonlaser "old-school" treatments, such as aesthetic peels, hydroquinone, and a hyfrecator, he said.
"The true art of cosmetic therapy is integrating spa treatments, cosmeceuticals,
prescription medications, and lasers all together," remarked Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "Lasers don't speak for themselves, particularly when treating pigmented lesions such as melasma and dark spots. We really have to take advantage of the product side of this, also. We have most of our patients on alpha hydroxy acids, Retin A, vitamin C, and we use hydroquinone bleaching cream up to 12%. I'm not bashful with hydroquinone. I monitor them very closely, but I think our patients can benefit from a higher strength."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from numerous medical device companies, including Canfield.
PHOENIX - In the last 2 years, complexion blending has been the most sought-after procedure in Dr. Eliot F. Battle Jr.'s practice.
One of his favorite devices for treating dark spots, melasma, postinflammatory hyperpigmentation, and scarring is the microsecond Nd:YAG laser. With this device, "we're driving heat down deep and trying to break up pigment … that's been encapsulated by membranes," Dr. Battle said. "For a dark spot to last for months or years, we know there is a pigment problem in the dermis. Fractional technology has also been used, but we treat conservatively. I don't ever use the manufacturer's parameters. I don't cause erythema or edema. I'm always under the threshold of redness and swelling."
Speaking during the annual meeting of the American Society for Laser Medicine and Surgery on laser treatment for skin of color patients, Dr. Battle's take-home advice was to reduce conventional parameters and fluences to avoid erythema and edema.
"There are many lasers to use on Caucasians for complexion blending," he said.
"For skin of color, we're limited to the microsecond Nd:YAG, Q-switched Nd:YAG, KTP [potassium-titanyl-phosphate], and infrared lasers."
Prior to treatment he asks patients about their ethnic background because ethnicity plays as much a role in how their skin reacts as their skin color, he said.
He also gets a sun protection history to find out whether he will be treating brown skin that is sun protected, as is the case with some people of Pacific-Asian ancestry, or whether he will be treating brown skin that has been suntanned, as is the case with some people of African-American ancestry.
"Don't make assumptions," he said. "Don't think that the person in front of you, who has the same skin color as the person you just treated, has the same response to lasers, because the ethnicity of the patient dictates how the skin reacts as much as their skin color."
He also recommends investing in an imaging system, such as the VISIA Complexion Analysis system, "that allows us to see what we're treating."
To maximize results of complexion blending, consider concomitant nonlaser "old-school" treatments, such as aesthetic peels, hydroquinone, and a hyfrecator, he said.
"The true art of cosmetic therapy is integrating spa treatments, cosmeceuticals,
prescription medications, and lasers all together," remarked Dr. Battle, who is also on the dermatology faculty at Howard University, Washington. "Lasers don't speak for themselves, particularly when treating pigmented lesions such as melasma and dark spots. We really have to take advantage of the product side of this, also. We have most of our patients on alpha hydroxy acids, Retin A, vitamin C, and we use hydroquinone bleaching cream up to 12%. I'm not bashful with hydroquinone. I monitor them very closely, but I think our patients can benefit from a higher strength."
Dr. Battle disclosed that he has received equipment, discounts, and honoraria from numerous medical device companies, including Canfield.
Pseudofolliculitis Barbae Treatment Solutions
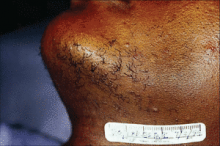
Pseudofolliculitis barbae is a common complaint among darker-skinned patients with coarse, curly hair. Patients present with follicular papules in the beard area from ingrown hairs that can eventually result in post-inflammatory pigmentary alteration and scarring. While PFB is more common in men, women may also present with symptoms.
For dermatologists who do not regularly treat skin of color patients, here are tips for treating (pseudofolliculitis barbae).
- If your male patients don’t mind having a beard, suggest they grow one! The chances of having ingrown hairs that stimulate this condition are less likely if the hairs are not plucked or shaved. It also helps if they are kept at least a few millimeters long.
- If shaving is a must, advise your skin of color patients to:
- Apply warm compresses to the beard area for a few minutes prior to shaving. A mild exfoliant, loofah, or toothbrush can be used (in a circular motion) to help ingrown hairs be more easily plucked or released at the skin surface.
- Use a shaving gel and a sharp razor each time they shave.
- Do not pull the skin taut.
- Do not shave against the grain or direction of hair growth.
- Take short strokes and do not shave back and forth over the same areas.
- Use a soothing aftershave or hydrocortisone 1% lotion after each shave.
- If hair removal is a must, treatment options include:
- Using a shave protector mist or lotion to help soften the skin and reduce irritation.
- Using a self-cleaning electric razor (replacing the blades at least every 2 years).
- Using a thick shaving gel with either a single or twin blade razor or a chemical depilatory.
- Undergoing laser hair removal. Longer pulsed lasers (1064 nm or 810 nm) may work best in darker skinned patients.
- Using an enzyme inhibitor (has been shown to work synergistically with laser hair removal).
- Undergoing electrolysis. This may also be helpful if there are hairs that do not respond to laser hair removal with longer pulsed lasers.
- Products like PFB Vanish or A+ Skin Care products, that contain salicylic, glycolic, or lactic acid, can help prevent ingrown hairs after hair removal.
- If there are inflammatory papules or pustules, a combination benzoyl peroxide and clindamycin gel (such as BenzaClin or Duac) can be prescribed, but patients with severe inflammation may require oral antibiotics.
- The use of a topical retinoid at night, or a combination retinoid product with hydroquinone (such as Tri-Luma), may reduce post-inflammatory hyperpigmentation. Caution should be taken when treating darker skin with topical retinoids, however, because irritation from the products can lead to post-inflammatory pigmentary alteration. Advise patients to avoid using drying products, such as toners, if topical retinoids are being used.
- For severe or refractory post-inflammatory hyperpigmentation or inflammatory papules, consider chemical peels with 20%-30% salicylic acid.
For dermatologists who have worked with this type of condition before, what are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients. Please take a moment to respond to this blog.
Pseudofolliculitis barbae is a common complaint among darker-skinned patients with coarse, curly hair. Patients present with follicular papules in the beard area from ingrown hairs that can eventually result in post-inflammatory pigmentary alteration and scarring. While PFB is more common in men, women may also present with symptoms.
For dermatologists who do not regularly treat skin of color patients, here are tips for treating (pseudofolliculitis barbae).
- If your male patients don’t mind having a beard, suggest they grow one! The chances of having ingrown hairs that stimulate this condition are less likely if the hairs are not plucked or shaved. It also helps if they are kept at least a few millimeters long.
- If shaving is a must, advise your skin of color patients to:
- Apply warm compresses to the beard area for a few minutes prior to shaving. A mild exfoliant, loofah, or toothbrush can be used (in a circular motion) to help ingrown hairs be more easily plucked or released at the skin surface.
- Use a shaving gel and a sharp razor each time they shave.
- Do not pull the skin taut.
- Do not shave against the grain or direction of hair growth.
- Take short strokes and do not shave back and forth over the same areas.
- Use a soothing aftershave or hydrocortisone 1% lotion after each shave.
- If hair removal is a must, treatment options include:
- Using a shave protector mist or lotion to help soften the skin and reduce irritation.
- Using a self-cleaning electric razor (replacing the blades at least every 2 years).
- Using a thick shaving gel with either a single or twin blade razor or a chemical depilatory.
- Undergoing laser hair removal. Longer pulsed lasers (1064 nm or 810 nm) may work best in darker skinned patients.
- Using an enzyme inhibitor (has been shown to work synergistically with laser hair removal).
- Undergoing electrolysis. This may also be helpful if there are hairs that do not respond to laser hair removal with longer pulsed lasers.
- Products like PFB Vanish or A+ Skin Care products, that contain salicylic, glycolic, or lactic acid, can help prevent ingrown hairs after hair removal.
- If there are inflammatory papules or pustules, a combination benzoyl peroxide and clindamycin gel (such as BenzaClin or Duac) can be prescribed, but patients with severe inflammation may require oral antibiotics.
- The use of a topical retinoid at night, or a combination retinoid product with hydroquinone (such as Tri-Luma), may reduce post-inflammatory hyperpigmentation. Caution should be taken when treating darker skin with topical retinoids, however, because irritation from the products can lead to post-inflammatory pigmentary alteration. Advise patients to avoid using drying products, such as toners, if topical retinoids are being used.
- For severe or refractory post-inflammatory hyperpigmentation or inflammatory papules, consider chemical peels with 20%-30% salicylic acid.
For dermatologists who have worked with this type of condition before, what are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients. Please take a moment to respond to this blog.
Pseudofolliculitis barbae is a common complaint among darker-skinned patients with coarse, curly hair. Patients present with follicular papules in the beard area from ingrown hairs that can eventually result in post-inflammatory pigmentary alteration and scarring. While PFB is more common in men, women may also present with symptoms.
For dermatologists who do not regularly treat skin of color patients, here are tips for treating (pseudofolliculitis barbae).
- If your male patients don’t mind having a beard, suggest they grow one! The chances of having ingrown hairs that stimulate this condition are less likely if the hairs are not plucked or shaved. It also helps if they are kept at least a few millimeters long.
- If shaving is a must, advise your skin of color patients to:
- Apply warm compresses to the beard area for a few minutes prior to shaving. A mild exfoliant, loofah, or toothbrush can be used (in a circular motion) to help ingrown hairs be more easily plucked or released at the skin surface.
- Use a shaving gel and a sharp razor each time they shave.
- Do not pull the skin taut.
- Do not shave against the grain or direction of hair growth.
- Take short strokes and do not shave back and forth over the same areas.
- Use a soothing aftershave or hydrocortisone 1% lotion after each shave.
- If hair removal is a must, treatment options include:
- Using a shave protector mist or lotion to help soften the skin and reduce irritation.
- Using a self-cleaning electric razor (replacing the blades at least every 2 years).
- Using a thick shaving gel with either a single or twin blade razor or a chemical depilatory.
- Undergoing laser hair removal. Longer pulsed lasers (1064 nm or 810 nm) may work best in darker skinned patients.
- Using an enzyme inhibitor (has been shown to work synergistically with laser hair removal).
- Undergoing electrolysis. This may also be helpful if there are hairs that do not respond to laser hair removal with longer pulsed lasers.
- Products like PFB Vanish or A+ Skin Care products, that contain salicylic, glycolic, or lactic acid, can help prevent ingrown hairs after hair removal.
- If there are inflammatory papules or pustules, a combination benzoyl peroxide and clindamycin gel (such as BenzaClin or Duac) can be prescribed, but patients with severe inflammation may require oral antibiotics.
- The use of a topical retinoid at night, or a combination retinoid product with hydroquinone (such as Tri-Luma), may reduce post-inflammatory hyperpigmentation. Caution should be taken when treating darker skin with topical retinoids, however, because irritation from the products can lead to post-inflammatory pigmentary alteration. Advise patients to avoid using drying products, such as toners, if topical retinoids are being used.
- For severe or refractory post-inflammatory hyperpigmentation or inflammatory papules, consider chemical peels with 20%-30% salicylic acid.
For dermatologists who have worked with this type of condition before, what are your PFB solutions? The more we share our clinical insights, the better we will be able to achieve improved treatment results for our patients. Please take a moment to respond to this blog.
Natural Products Prove Effectiveness for Skin
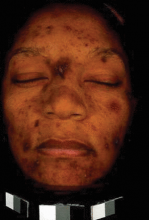
WAIKOLOA, Hawaii -- Natural ingredients in over-the-counter products with proven effectiveness work through tyrosinase inhibition or by curbing melanosome transfer to keratinocytes, according to Dr. Susan C. Taylor (photographed below).
The substances are supported by studies showing evidence of efficacy for skin brightening and improvement in photoaging; however, the studies are often of lesser quality than dermatologists are accustomed to for prescription drugs approved by the Food and Drug Administration, said Dr. Taylor, founding director of the Skin of Color Center at St. Luke's-Roosevelt Hospital Center in New York.
Rest assured, though, that these natural ingredients have known mechanisms of action, are backed by some evidence of improvement in pigmentation, and can be incorporated as adjuncts to more potent standard therapies, Dr. Taylor said.
She discussed several products in detail:
- P Olay Definity. One of the most rigorous scientific evaluations for any of the natural products for skin brightening was conducted by Dr. Alexa B. Kimball of the department of dermatology at Harvard Medical School, Boston, and coworkers.
They conducted a randomized, double-blind trial of Olay Definity (4% niacinamide and 2% N-acetylglucosamine) or its cream vehicle for reduction of facial hyperpigmentation in 202 middle-aged women (Skin & Allergy News, "N-Acetylglucosamine Reduces Hyperpigmentation," December 2006, p. 54).
By all outcome measures, Definity was significantly more effective in reducing the detectable areas of facial spots, as well as hypermelanization and other manifestations of irregular pigmentation, in the Procter & Gamble-funded trial (Br. J. Dermatol. 2010;162:435-41).
- P Arbutin. This glycosylated hydroquinone is derived from cranberry, blueberry, and bearberry leaves, noted Dr. Taylor. In a 50-patient study, the blinded expert consensus was that deoxyarbutin achieved a significant improvement in solar lentigines, but only in the 34 white women (Exp. Dermatol. 2005;14:601-8).
- P Liquiritin. A cream containing liquiritin--a licorice extract derived from the Glycyrrhiza inflata plant of northwest China--was compared with a vehicle in 20 patients with melasma.
Investigators rated 80% of liquiritin-treated areas as showing excellent response in terms of reduced pigment intensity and size, while the other 20% were rated as having a good response. In contrast, no vehicle-treated areas were rated as having a good or excellent response (Int. J. Dermatol. 2000;39:299-302).
- P Soy. Fresh soy, which contains essential fatty acids, saponins, lecithin, and oleic acid, has a salutary effect on hyperpigmentation. Fermented soy contains isoflavones having an estrogenic effect; it is of no value in skin brightening, Dr. Taylor said. Researchers at Johnson & Johnson conducted a double-blind, vehicle-controlled trial of a soy moisturizer in 65 women with moderate facial photoaging. The group treated with the moisturizer showed significantly greater improvement than controls in terms of reduced mottled hyperpigmentation, blotchiness, fine lines, and tactile roughness (J. Drugs Dermatol. 2007;6:512-22).n
Disclosures: Dr. Taylor has served as an investigator, speaker, and/or advisory board member for Allergan, Beiersdorf, Johnson & Johnson, Medicis, Procter & Gamble, Stiefel, and T2 Skin Care. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, Hawaii -- Natural ingredients in over-the-counter products with proven effectiveness work through tyrosinase inhibition or by curbing melanosome transfer to keratinocytes, according to Dr. Susan C. Taylor (photographed below).
The substances are supported by studies showing evidence of efficacy for skin brightening and improvement in photoaging; however, the studies are often of lesser quality than dermatologists are accustomed to for prescription drugs approved by the Food and Drug Administration, said Dr. Taylor, founding director of the Skin of Color Center at St. Luke's-Roosevelt Hospital Center in New York.
Rest assured, though, that these natural ingredients have known mechanisms of action, are backed by some evidence of improvement in pigmentation, and can be incorporated as adjuncts to more potent standard therapies, Dr. Taylor said.
She discussed several products in detail:
- P Olay Definity. One of the most rigorous scientific evaluations for any of the natural products for skin brightening was conducted by Dr. Alexa B. Kimball of the department of dermatology at Harvard Medical School, Boston, and coworkers.
They conducted a randomized, double-blind trial of Olay Definity (4% niacinamide and 2% N-acetylglucosamine) or its cream vehicle for reduction of facial hyperpigmentation in 202 middle-aged women (Skin & Allergy News, "N-Acetylglucosamine Reduces Hyperpigmentation," December 2006, p. 54).
By all outcome measures, Definity was significantly more effective in reducing the detectable areas of facial spots, as well as hypermelanization and other manifestations of irregular pigmentation, in the Procter & Gamble-funded trial (Br. J. Dermatol. 2010;162:435-41).
- P Arbutin. This glycosylated hydroquinone is derived from cranberry, blueberry, and bearberry leaves, noted Dr. Taylor. In a 50-patient study, the blinded expert consensus was that deoxyarbutin achieved a significant improvement in solar lentigines, but only in the 34 white women (Exp. Dermatol. 2005;14:601-8).
- P Liquiritin. A cream containing liquiritin--a licorice extract derived from the Glycyrrhiza inflata plant of northwest China--was compared with a vehicle in 20 patients with melasma.
Investigators rated 80% of liquiritin-treated areas as showing excellent response in terms of reduced pigment intensity and size, while the other 20% were rated as having a good response. In contrast, no vehicle-treated areas were rated as having a good or excellent response (Int. J. Dermatol. 2000;39:299-302).
- P Soy. Fresh soy, which contains essential fatty acids, saponins, lecithin, and oleic acid, has a salutary effect on hyperpigmentation. Fermented soy contains isoflavones having an estrogenic effect; it is of no value in skin brightening, Dr. Taylor said. Researchers at Johnson & Johnson conducted a double-blind, vehicle-controlled trial of a soy moisturizer in 65 women with moderate facial photoaging. The group treated with the moisturizer showed significantly greater improvement than controls in terms of reduced mottled hyperpigmentation, blotchiness, fine lines, and tactile roughness (J. Drugs Dermatol. 2007;6:512-22).n
Disclosures: Dr. Taylor has served as an investigator, speaker, and/or advisory board member for Allergan, Beiersdorf, Johnson & Johnson, Medicis, Procter & Gamble, Stiefel, and T2 Skin Care. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, Hawaii -- Natural ingredients in over-the-counter products with proven effectiveness work through tyrosinase inhibition or by curbing melanosome transfer to keratinocytes, according to Dr. Susan C. Taylor (photographed below).
The substances are supported by studies showing evidence of efficacy for skin brightening and improvement in photoaging; however, the studies are often of lesser quality than dermatologists are accustomed to for prescription drugs approved by the Food and Drug Administration, said Dr. Taylor, founding director of the Skin of Color Center at St. Luke's-Roosevelt Hospital Center in New York.
Rest assured, though, that these natural ingredients have known mechanisms of action, are backed by some evidence of improvement in pigmentation, and can be incorporated as adjuncts to more potent standard therapies, Dr. Taylor said.
She discussed several products in detail:
- P Olay Definity. One of the most rigorous scientific evaluations for any of the natural products for skin brightening was conducted by Dr. Alexa B. Kimball of the department of dermatology at Harvard Medical School, Boston, and coworkers.
They conducted a randomized, double-blind trial of Olay Definity (4% niacinamide and 2% N-acetylglucosamine) or its cream vehicle for reduction of facial hyperpigmentation in 202 middle-aged women (Skin & Allergy News, "N-Acetylglucosamine Reduces Hyperpigmentation," December 2006, p. 54).
By all outcome measures, Definity was significantly more effective in reducing the detectable areas of facial spots, as well as hypermelanization and other manifestations of irregular pigmentation, in the Procter & Gamble-funded trial (Br. J. Dermatol. 2010;162:435-41).
- P Arbutin. This glycosylated hydroquinone is derived from cranberry, blueberry, and bearberry leaves, noted Dr. Taylor. In a 50-patient study, the blinded expert consensus was that deoxyarbutin achieved a significant improvement in solar lentigines, but only in the 34 white women (Exp. Dermatol. 2005;14:601-8).
- P Liquiritin. A cream containing liquiritin--a licorice extract derived from the Glycyrrhiza inflata plant of northwest China--was compared with a vehicle in 20 patients with melasma.
Investigators rated 80% of liquiritin-treated areas as showing excellent response in terms of reduced pigment intensity and size, while the other 20% were rated as having a good response. In contrast, no vehicle-treated areas were rated as having a good or excellent response (Int. J. Dermatol. 2000;39:299-302).
- P Soy. Fresh soy, which contains essential fatty acids, saponins, lecithin, and oleic acid, has a salutary effect on hyperpigmentation. Fermented soy contains isoflavones having an estrogenic effect; it is of no value in skin brightening, Dr. Taylor said. Researchers at Johnson & Johnson conducted a double-blind, vehicle-controlled trial of a soy moisturizer in 65 women with moderate facial photoaging. The group treated with the moisturizer showed significantly greater improvement than controls in terms of reduced mottled hyperpigmentation, blotchiness, fine lines, and tactile roughness (J. Drugs Dermatol. 2007;6:512-22).n
Disclosures: Dr. Taylor has served as an investigator, speaker, and/or advisory board member for Allergan, Beiersdorf, Johnson & Johnson, Medicis, Procter & Gamble, Stiefel, and T2 Skin Care. SDEF and this news organization are owned by Elsevier.
Medical Tourism Q & A: Are Cost Savings Worth the Risks?
Dr. Michael McGuire, president of the American Society of Plastic Surgeons, shares his views on medical tourism, the potential risks involved in seeking surgery abroad, and the ethical obligations of physicians once patients return for care in this country.
Question: Why does medical tourism seem to be so popular right now?
Dr. McGuire: I think probably the most recent impetus has been the recession and the layoffs that have resulted in a loss of health care coverage. Obviously, if you need to have surgery and you don’t have insurance, it can be extremely expensive to pay for it on your own. But patients also need to understand that the cheapest surgery is not going to be the best surgery. If they were to seek the top surgeons around the world, they wouldn’t save much money. The savings comes in going to lesser trained surgeons, often in lesser qualified hospitals.
Question: What are the risks involved in getting surgery abroad?
Dr. McGuire: I divide the risks into three components: the preoperative phase, the interoperative phase, and the postoperative phase, each of which presents significant logistical and safety issues for patients. The major challenge in the preoperative phase is how to find a qualified surgeon. But even if you find the right surgeon, that still doesn’t mean that the rest of the surgical team will be up to the same standard. For example, in many less developed countries, nursing training is little more than a high school–level course, and the nurse may not speak English.
During the interoperative phase, patients are faced with making a long trip, which raises the risk of blood clots and pulmonary embolism. Adding to that risk, patients preparing for surgery can’t be on anticoagulants.
Then there’s the postoperative phase. The medical tourism industry often paints a picture of a patient recovering from surgery on an exotic beach. Unfortunately, that’s not the reality. Patients recovering from hip replacement, coronary bypass surgery, or cosmetic surgery have a lot of healing to do and should not be exposing themselves to possible infections and other contamination problems they could face while traveling. Perhaps even more important, once they get home, patients must face the issue of who will take care of them if they experience a complication from surgery.
Question: If a patient does return with a complication from surgery, what’s the ethical responsibility of the U.S. surgeon?
Dr. McGuire: It is a real challenge. I think if it’s a true emergency, you must take care of the patient without question. But if it’s something more elective, you have to be very cautious. I think it has to be done on a case-by-case basis, evaluating the patient and trying to minimize your exposure to liability.
There are obviously agreements that you can make, such as developing a “hold harmless” contract so that the patient understands that you cannot assume liability for all that’s happened before. That can minimize the exposure risk. But again, it depends on whether this is a patient whom you know and one who will have realistic expectations. In that case, I think it’s certainly possible to work something out, but you have to be careful.
Question: What about insurance? Is that becoming a driver at all? Are insurers creating packages where people can go abroad for surgery?
Dr. McGuire: Insurance companies were beginning to get involved in medical tourism, but that has really declined recently. In speaking to some insurers, I have pointed out that once they encourage or incentivize people to have surgery abroad, they are no longer functioning as an insurance company. And as a result, they assume liability if the patient does not have a good outcome. Needless to say, the malpractice attorneys are very anxious to have a deep pocket like an insurance company that they can sue. So that has put a significant damper on the insurance industry’s enthusiasm for promoting this.
Question: Do you think medical tourism will continue to grow?
Dr. McGuire: In terms of aesthetic surgery, I see it as plateauing. I don’t see it as dramatically increasing, because the real costs involved are so significant that it’s not going to be enough of a savings for most people. And most people who are interested in aesthetic surgery are not looking for bargains.
In terms of insurance-covered procedures, I think it depends entirely on how much health care reform minimizes the number of people without insurance. As the economy improves and more people gain insurance, I think that’s going to be the major driver in terms of the growth of insurance-covered medical tourism. Right now, I think we’re seeing a bit of a spike simply because there are more and more people without insurance. Once that trend changes, I think the number of people going abroad will significantly decline. Virtually nobody is going abroad if they have insurance coverage.
Dr. Michael McGuire, president of the American Society of Plastic Surgeons, shares his views on medical tourism, the potential risks involved in seeking surgery abroad, and the ethical obligations of physicians once patients return for care in this country.
Question: Why does medical tourism seem to be so popular right now?
Dr. McGuire: I think probably the most recent impetus has been the recession and the layoffs that have resulted in a loss of health care coverage. Obviously, if you need to have surgery and you don’t have insurance, it can be extremely expensive to pay for it on your own. But patients also need to understand that the cheapest surgery is not going to be the best surgery. If they were to seek the top surgeons around the world, they wouldn’t save much money. The savings comes in going to lesser trained surgeons, often in lesser qualified hospitals.
Question: What are the risks involved in getting surgery abroad?
Dr. McGuire: I divide the risks into three components: the preoperative phase, the interoperative phase, and the postoperative phase, each of which presents significant logistical and safety issues for patients. The major challenge in the preoperative phase is how to find a qualified surgeon. But even if you find the right surgeon, that still doesn’t mean that the rest of the surgical team will be up to the same standard. For example, in many less developed countries, nursing training is little more than a high school–level course, and the nurse may not speak English.
During the interoperative phase, patients are faced with making a long trip, which raises the risk of blood clots and pulmonary embolism. Adding to that risk, patients preparing for surgery can’t be on anticoagulants.
Then there’s the postoperative phase. The medical tourism industry often paints a picture of a patient recovering from surgery on an exotic beach. Unfortunately, that’s not the reality. Patients recovering from hip replacement, coronary bypass surgery, or cosmetic surgery have a lot of healing to do and should not be exposing themselves to possible infections and other contamination problems they could face while traveling. Perhaps even more important, once they get home, patients must face the issue of who will take care of them if they experience a complication from surgery.
Question: If a patient does return with a complication from surgery, what’s the ethical responsibility of the U.S. surgeon?
Dr. McGuire: It is a real challenge. I think if it’s a true emergency, you must take care of the patient without question. But if it’s something more elective, you have to be very cautious. I think it has to be done on a case-by-case basis, evaluating the patient and trying to minimize your exposure to liability.
There are obviously agreements that you can make, such as developing a “hold harmless” contract so that the patient understands that you cannot assume liability for all that’s happened before. That can minimize the exposure risk. But again, it depends on whether this is a patient whom you know and one who will have realistic expectations. In that case, I think it’s certainly possible to work something out, but you have to be careful.
Question: What about insurance? Is that becoming a driver at all? Are insurers creating packages where people can go abroad for surgery?
Dr. McGuire: Insurance companies were beginning to get involved in medical tourism, but that has really declined recently. In speaking to some insurers, I have pointed out that once they encourage or incentivize people to have surgery abroad, they are no longer functioning as an insurance company. And as a result, they assume liability if the patient does not have a good outcome. Needless to say, the malpractice attorneys are very anxious to have a deep pocket like an insurance company that they can sue. So that has put a significant damper on the insurance industry’s enthusiasm for promoting this.
Question: Do you think medical tourism will continue to grow?
Dr. McGuire: In terms of aesthetic surgery, I see it as plateauing. I don’t see it as dramatically increasing, because the real costs involved are so significant that it’s not going to be enough of a savings for most people. And most people who are interested in aesthetic surgery are not looking for bargains.
In terms of insurance-covered procedures, I think it depends entirely on how much health care reform minimizes the number of people without insurance. As the economy improves and more people gain insurance, I think that’s going to be the major driver in terms of the growth of insurance-covered medical tourism. Right now, I think we’re seeing a bit of a spike simply because there are more and more people without insurance. Once that trend changes, I think the number of people going abroad will significantly decline. Virtually nobody is going abroad if they have insurance coverage.
Dr. Michael McGuire, president of the American Society of Plastic Surgeons, shares his views on medical tourism, the potential risks involved in seeking surgery abroad, and the ethical obligations of physicians once patients return for care in this country.
Question: Why does medical tourism seem to be so popular right now?
Dr. McGuire: I think probably the most recent impetus has been the recession and the layoffs that have resulted in a loss of health care coverage. Obviously, if you need to have surgery and you don’t have insurance, it can be extremely expensive to pay for it on your own. But patients also need to understand that the cheapest surgery is not going to be the best surgery. If they were to seek the top surgeons around the world, they wouldn’t save much money. The savings comes in going to lesser trained surgeons, often in lesser qualified hospitals.
Question: What are the risks involved in getting surgery abroad?
Dr. McGuire: I divide the risks into three components: the preoperative phase, the interoperative phase, and the postoperative phase, each of which presents significant logistical and safety issues for patients. The major challenge in the preoperative phase is how to find a qualified surgeon. But even if you find the right surgeon, that still doesn’t mean that the rest of the surgical team will be up to the same standard. For example, in many less developed countries, nursing training is little more than a high school–level course, and the nurse may not speak English.
During the interoperative phase, patients are faced with making a long trip, which raises the risk of blood clots and pulmonary embolism. Adding to that risk, patients preparing for surgery can’t be on anticoagulants.
Then there’s the postoperative phase. The medical tourism industry often paints a picture of a patient recovering from surgery on an exotic beach. Unfortunately, that’s not the reality. Patients recovering from hip replacement, coronary bypass surgery, or cosmetic surgery have a lot of healing to do and should not be exposing themselves to possible infections and other contamination problems they could face while traveling. Perhaps even more important, once they get home, patients must face the issue of who will take care of them if they experience a complication from surgery.
Question: If a patient does return with a complication from surgery, what’s the ethical responsibility of the U.S. surgeon?
Dr. McGuire: It is a real challenge. I think if it’s a true emergency, you must take care of the patient without question. But if it’s something more elective, you have to be very cautious. I think it has to be done on a case-by-case basis, evaluating the patient and trying to minimize your exposure to liability.
There are obviously agreements that you can make, such as developing a “hold harmless” contract so that the patient understands that you cannot assume liability for all that’s happened before. That can minimize the exposure risk. But again, it depends on whether this is a patient whom you know and one who will have realistic expectations. In that case, I think it’s certainly possible to work something out, but you have to be careful.
Question: What about insurance? Is that becoming a driver at all? Are insurers creating packages where people can go abroad for surgery?
Dr. McGuire: Insurance companies were beginning to get involved in medical tourism, but that has really declined recently. In speaking to some insurers, I have pointed out that once they encourage or incentivize people to have surgery abroad, they are no longer functioning as an insurance company. And as a result, they assume liability if the patient does not have a good outcome. Needless to say, the malpractice attorneys are very anxious to have a deep pocket like an insurance company that they can sue. So that has put a significant damper on the insurance industry’s enthusiasm for promoting this.
Question: Do you think medical tourism will continue to grow?
Dr. McGuire: In terms of aesthetic surgery, I see it as plateauing. I don’t see it as dramatically increasing, because the real costs involved are so significant that it’s not going to be enough of a savings for most people. And most people who are interested in aesthetic surgery are not looking for bargains.
In terms of insurance-covered procedures, I think it depends entirely on how much health care reform minimizes the number of people without insurance. As the economy improves and more people gain insurance, I think that’s going to be the major driver in terms of the growth of insurance-covered medical tourism. Right now, I think we’re seeing a bit of a spike simply because there are more and more people without insurance. Once that trend changes, I think the number of people going abroad will significantly decline. Virtually nobody is going abroad if they have insurance coverage.
Lasers: Coming Soon to a Home Near You
From the annual meeting of the American Society for Laser Medicine and Surgery.
Expect an increasing number of laser devices intended for home use to enter the market over the next decade, Dr. R. Rox Anderson, the outgoing president of ASLMS, predicted during a press briefing.
As a co-inventor of permanent laser hair removal about 15 years ago, Dr. Anderson recalled working with “great big lasers that cost a lot of money [and] took up a lot of space. There are now three or four of those devices that are approved and cleared by the FDA for home use. It’s fascinating that something as powerful as a laser can be safe enough for consumer use. We’re going to see a lot more of this in the next 5-10 years. Believe me, you will have laser devices at home and I think you’ll find them to be useful and user friendly, but we have to make sure we do it right so nobody gets hurt.”
Dr. Anderson, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, also predicted that lasers will play a key role in improving diagnostics. For example, instead of subjecting patients to an invasive skin biopsy for a suspicious lesion, “we’re getting to the point where lasers for making microscopic images in living people are becoming practical,” he said. “I think we’ll be able to do that through fiber optics inside your body.”
Stay tuned.
–Doug Brunk
From the annual meeting of the American Society for Laser Medicine and Surgery.
Expect an increasing number of laser devices intended for home use to enter the market over the next decade, Dr. R. Rox Anderson, the outgoing president of ASLMS, predicted during a press briefing.
As a co-inventor of permanent laser hair removal about 15 years ago, Dr. Anderson recalled working with “great big lasers that cost a lot of money [and] took up a lot of space. There are now three or four of those devices that are approved and cleared by the FDA for home use. It’s fascinating that something as powerful as a laser can be safe enough for consumer use. We’re going to see a lot more of this in the next 5-10 years. Believe me, you will have laser devices at home and I think you’ll find them to be useful and user friendly, but we have to make sure we do it right so nobody gets hurt.”
Dr. Anderson, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, also predicted that lasers will play a key role in improving diagnostics. For example, instead of subjecting patients to an invasive skin biopsy for a suspicious lesion, “we’re getting to the point where lasers for making microscopic images in living people are becoming practical,” he said. “I think we’ll be able to do that through fiber optics inside your body.”
Stay tuned.
–Doug Brunk
From the annual meeting of the American Society for Laser Medicine and Surgery.
Expect an increasing number of laser devices intended for home use to enter the market over the next decade, Dr. R. Rox Anderson, the outgoing president of ASLMS, predicted during a press briefing.
As a co-inventor of permanent laser hair removal about 15 years ago, Dr. Anderson recalled working with “great big lasers that cost a lot of money [and] took up a lot of space. There are now three or four of those devices that are approved and cleared by the FDA for home use. It’s fascinating that something as powerful as a laser can be safe enough for consumer use. We’re going to see a lot more of this in the next 5-10 years. Believe me, you will have laser devices at home and I think you’ll find them to be useful and user friendly, but we have to make sure we do it right so nobody gets hurt.”
Dr. Anderson, director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, also predicted that lasers will play a key role in improving diagnostics. For example, instead of subjecting patients to an invasive skin biopsy for a suspicious lesion, “we’re getting to the point where lasers for making microscopic images in living people are becoming practical,” he said. “I think we’ll be able to do that through fiber optics inside your body.”
Stay tuned.
–Doug Brunk