User login
Frequent, Lower Botox Dosing Best for Some Areas
Lower doses of botulinum toxin type A delivered more frequently yield better results in certain areas of the face, according to Dr. Joel L. Cohen.
While crow's feet and the glabella still do better with a higher dose and a 3- to 4-month dosing interval, there are several areas that do better with half the typical dose and half the dosing interval.
The forehead is one such area. "We use lighter doses in the forehead because we really want things to be more natural in terms of still having movement," Dr. Cohen said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "Sometimes these patients need to be dosed in the forehead every 8-10 weeks, whereas in the glabella and the crow's feet, if you're using regular doses, you might only need to inject them every 3.5 or 4 months. Sometimes they're in a cycle where they come in for Botox or Dysport in the forehead every 8 or 10 weeks and every 16 weeks or 18 weeks for the glabella and the crow's feet."
Brow lifts also do better with lower doses at shorter intervals. But Dr. Cohen, director of AboutSkin Dermatology and DermSurgery, Englewood, Colo., cautioned that brow lifts with botulinum toxin should not be attempted in patients who have a lot of sagging in the lateral brow. These patients require surgery; botulinum toxin should be reserved for patients with mild redundancy between the brow and the eyelid. Occasionally, patients with moderate sagging can benefit as well.
Around the mouth, Dr. Cohen uses 5-7 units of botulinum toxin to treat the vertical muscle columns of the upper lip and to prevent etched-in lines. At the same time, he uses 2-3 units in the lower lip, "so it doesn't feel funny." Once again, this needs to be repeated every 8-10 weeks, he said.
There is another class of patients in which low doses of perioral botulinum toxin may be beneficial. Studies have shown that healing after resurfacing procedures tends to be better after the area has previously been immobilized with botulinum toxin.
"There's decreasing contraction across the wound, so you're not imprinting lines where you already have lines," Dr. Cohen said. "And the second thing is there is decreased inflammation because there's less mobility of the area."
For one-time erbium or CO2 laser resurfacing, Dr. Cohen recommends the patient be treated with botulinum toxin a week to 10 days before. "Or you can do pretreatment a week or two before you do a fractionated ablative laser where the plan is to do three, four, or five treatments. By treating the patient with the fractionated laser every 3 weeks, you may really be able to get a session of three treatments in for every one pretreatment with Botox. The overall goal is less movement across what you're trying to heal."
Dr. Cohen acknowledged participating in clinical trials and serving as a consultant for Allergan, Medicis, Johnson and Johnson/Mentor, and Merz. SDEF and this news organization are owned by Elsevier.
Lower doses of botulinum toxin type A delivered more frequently yield better results in certain areas of the face, according to Dr. Joel L. Cohen.
While crow's feet and the glabella still do better with a higher dose and a 3- to 4-month dosing interval, there are several areas that do better with half the typical dose and half the dosing interval.
The forehead is one such area. "We use lighter doses in the forehead because we really want things to be more natural in terms of still having movement," Dr. Cohen said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "Sometimes these patients need to be dosed in the forehead every 8-10 weeks, whereas in the glabella and the crow's feet, if you're using regular doses, you might only need to inject them every 3.5 or 4 months. Sometimes they're in a cycle where they come in for Botox or Dysport in the forehead every 8 or 10 weeks and every 16 weeks or 18 weeks for the glabella and the crow's feet."
Brow lifts also do better with lower doses at shorter intervals. But Dr. Cohen, director of AboutSkin Dermatology and DermSurgery, Englewood, Colo., cautioned that brow lifts with botulinum toxin should not be attempted in patients who have a lot of sagging in the lateral brow. These patients require surgery; botulinum toxin should be reserved for patients with mild redundancy between the brow and the eyelid. Occasionally, patients with moderate sagging can benefit as well.
Around the mouth, Dr. Cohen uses 5-7 units of botulinum toxin to treat the vertical muscle columns of the upper lip and to prevent etched-in lines. At the same time, he uses 2-3 units in the lower lip, "so it doesn't feel funny." Once again, this needs to be repeated every 8-10 weeks, he said.
There is another class of patients in which low doses of perioral botulinum toxin may be beneficial. Studies have shown that healing after resurfacing procedures tends to be better after the area has previously been immobilized with botulinum toxin.
"There's decreasing contraction across the wound, so you're not imprinting lines where you already have lines," Dr. Cohen said. "And the second thing is there is decreased inflammation because there's less mobility of the area."
For one-time erbium or CO2 laser resurfacing, Dr. Cohen recommends the patient be treated with botulinum toxin a week to 10 days before. "Or you can do pretreatment a week or two before you do a fractionated ablative laser where the plan is to do three, four, or five treatments. By treating the patient with the fractionated laser every 3 weeks, you may really be able to get a session of three treatments in for every one pretreatment with Botox. The overall goal is less movement across what you're trying to heal."
Dr. Cohen acknowledged participating in clinical trials and serving as a consultant for Allergan, Medicis, Johnson and Johnson/Mentor, and Merz. SDEF and this news organization are owned by Elsevier.
Lower doses of botulinum toxin type A delivered more frequently yield better results in certain areas of the face, according to Dr. Joel L. Cohen.
While crow's feet and the glabella still do better with a higher dose and a 3- to 4-month dosing interval, there are several areas that do better with half the typical dose and half the dosing interval.
The forehead is one such area. "We use lighter doses in the forehead because we really want things to be more natural in terms of still having movement," Dr. Cohen said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "Sometimes these patients need to be dosed in the forehead every 8-10 weeks, whereas in the glabella and the crow's feet, if you're using regular doses, you might only need to inject them every 3.5 or 4 months. Sometimes they're in a cycle where they come in for Botox or Dysport in the forehead every 8 or 10 weeks and every 16 weeks or 18 weeks for the glabella and the crow's feet."
Brow lifts also do better with lower doses at shorter intervals. But Dr. Cohen, director of AboutSkin Dermatology and DermSurgery, Englewood, Colo., cautioned that brow lifts with botulinum toxin should not be attempted in patients who have a lot of sagging in the lateral brow. These patients require surgery; botulinum toxin should be reserved for patients with mild redundancy between the brow and the eyelid. Occasionally, patients with moderate sagging can benefit as well.
Around the mouth, Dr. Cohen uses 5-7 units of botulinum toxin to treat the vertical muscle columns of the upper lip and to prevent etched-in lines. At the same time, he uses 2-3 units in the lower lip, "so it doesn't feel funny." Once again, this needs to be repeated every 8-10 weeks, he said.
There is another class of patients in which low doses of perioral botulinum toxin may be beneficial. Studies have shown that healing after resurfacing procedures tends to be better after the area has previously been immobilized with botulinum toxin.
"There's decreasing contraction across the wound, so you're not imprinting lines where you already have lines," Dr. Cohen said. "And the second thing is there is decreased inflammation because there's less mobility of the area."
For one-time erbium or CO2 laser resurfacing, Dr. Cohen recommends the patient be treated with botulinum toxin a week to 10 days before. "Or you can do pretreatment a week or two before you do a fractionated ablative laser where the plan is to do three, four, or five treatments. By treating the patient with the fractionated laser every 3 weeks, you may really be able to get a session of three treatments in for every one pretreatment with Botox. The overall goal is less movement across what you're trying to heal."
Dr. Cohen acknowledged participating in clinical trials and serving as a consultant for Allergan, Medicis, Johnson and Johnson/Mentor, and Merz. SDEF and this news organization are owned by Elsevier.
Ultrasound Offers Noninvasive Skin Tightening Alternatives
Ultrasound and related radiofrequency technologies are relatively novel, effective, and noninvasive methods for body contouring and localized skin tightening, according to Dr. David J. Goldberg.
The only cosmetic ultrasound therapy currently approved by the Food and Drug Administration is the Ulthera System for skin tightening, Dr. Goldberg said at a cosmetic dermatology seminar sponsored by the Skin Disease Education Foundation in Santa Monica, Calif. The device non-specifically heats deep dermal collagen, which is thought to tighten cellulite.
In a 2008 study led by Dr. Goldberg, director of dermatologic laser research at Mount Sinai School of Medicine, New York, 30 female patients underwent six treatments with a unipolar radiofrequency device directed at cellulite on their upper thighs.
Following treatment, 27 of 30 patients had clinical improvements, with a mean decrease in thigh circumference of 2.45 cm (Dermatol. Surg. 2008;34:204-9).
The treatment was "fairly painless," he said. Side effects included post treatment erythema, which lasted for about 30-120 minutes; there were no blisters, scars, or pigmentary changes.
Another technology, known as UltraShape, delivers focused ultrasound to dissolve unwanted fat. In a recent multi-center, single-treatment, controlled study, 82% of 162 patients had measurable reductions in the circumference of their thighs, abdomens, and flanks. The decreases averaged 2 cm at 28 days, and were maintained at 84 days post treatment.
In the study, presented at the 2009 International Masters Course on Aging Skin in Paris, 76% of patients reported being satisfied with a single treatment, and 92% reported having no pain or discomfort.
According to Dr. Goldberg, UltraShape is currently used in over 57 countries. Approval has not yet been granted in the United States.
Dr. Goldberg disclosed receiving research grants from Alma Lasers, Thermage, Cynosure, UltraShape and Zeltiq, all makers of laser, ultrasound and radiofrequency skin-tightening and body-contouring technologies. SDEF and this news organization are owned by Elsevier.
Ultrasound and related radiofrequency technologies are relatively novel, effective, and noninvasive methods for body contouring and localized skin tightening, according to Dr. David J. Goldberg.
The only cosmetic ultrasound therapy currently approved by the Food and Drug Administration is the Ulthera System for skin tightening, Dr. Goldberg said at a cosmetic dermatology seminar sponsored by the Skin Disease Education Foundation in Santa Monica, Calif. The device non-specifically heats deep dermal collagen, which is thought to tighten cellulite.
In a 2008 study led by Dr. Goldberg, director of dermatologic laser research at Mount Sinai School of Medicine, New York, 30 female patients underwent six treatments with a unipolar radiofrequency device directed at cellulite on their upper thighs.
Following treatment, 27 of 30 patients had clinical improvements, with a mean decrease in thigh circumference of 2.45 cm (Dermatol. Surg. 2008;34:204-9).
The treatment was "fairly painless," he said. Side effects included post treatment erythema, which lasted for about 30-120 minutes; there were no blisters, scars, or pigmentary changes.
Another technology, known as UltraShape, delivers focused ultrasound to dissolve unwanted fat. In a recent multi-center, single-treatment, controlled study, 82% of 162 patients had measurable reductions in the circumference of their thighs, abdomens, and flanks. The decreases averaged 2 cm at 28 days, and were maintained at 84 days post treatment.
In the study, presented at the 2009 International Masters Course on Aging Skin in Paris, 76% of patients reported being satisfied with a single treatment, and 92% reported having no pain or discomfort.
According to Dr. Goldberg, UltraShape is currently used in over 57 countries. Approval has not yet been granted in the United States.
Dr. Goldberg disclosed receiving research grants from Alma Lasers, Thermage, Cynosure, UltraShape and Zeltiq, all makers of laser, ultrasound and radiofrequency skin-tightening and body-contouring technologies. SDEF and this news organization are owned by Elsevier.
Ultrasound and related radiofrequency technologies are relatively novel, effective, and noninvasive methods for body contouring and localized skin tightening, according to Dr. David J. Goldberg.
The only cosmetic ultrasound therapy currently approved by the Food and Drug Administration is the Ulthera System for skin tightening, Dr. Goldberg said at a cosmetic dermatology seminar sponsored by the Skin Disease Education Foundation in Santa Monica, Calif. The device non-specifically heats deep dermal collagen, which is thought to tighten cellulite.
In a 2008 study led by Dr. Goldberg, director of dermatologic laser research at Mount Sinai School of Medicine, New York, 30 female patients underwent six treatments with a unipolar radiofrequency device directed at cellulite on their upper thighs.
Following treatment, 27 of 30 patients had clinical improvements, with a mean decrease in thigh circumference of 2.45 cm (Dermatol. Surg. 2008;34:204-9).
The treatment was "fairly painless," he said. Side effects included post treatment erythema, which lasted for about 30-120 minutes; there were no blisters, scars, or pigmentary changes.
Another technology, known as UltraShape, delivers focused ultrasound to dissolve unwanted fat. In a recent multi-center, single-treatment, controlled study, 82% of 162 patients had measurable reductions in the circumference of their thighs, abdomens, and flanks. The decreases averaged 2 cm at 28 days, and were maintained at 84 days post treatment.
In the study, presented at the 2009 International Masters Course on Aging Skin in Paris, 76% of patients reported being satisfied with a single treatment, and 92% reported having no pain or discomfort.
According to Dr. Goldberg, UltraShape is currently used in over 57 countries. Approval has not yet been granted in the United States.
Dr. Goldberg disclosed receiving research grants from Alma Lasers, Thermage, Cynosure, UltraShape and Zeltiq, all makers of laser, ultrasound and radiofrequency skin-tightening and body-contouring technologies. SDEF and this news organization are owned by Elsevier.
Laser Treatment Research for Port Wine Stains Continues
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
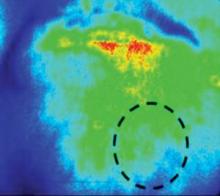
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.
Improving the appearance of port wine stains usually requires multiple laser treatments, and research is ongoing to improve results, according to Dr. Kristen Kelly.
Port wine stains (PWS) are the most common vascular malformations treated by dermatologists. About 0.3% of newborns have a PWS birthmark, which does not proliferate rapidly, but "may thicken, darken and develop nodules over time," Dr. Kelly said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Historically, treatments for PWS have included tattoos or radiation, but for almost 30 years laser therapy has been the mainstay of treatment. Although these devices have improved, 2-15 or more laser applications are needed at approximately 4-week intervals for successful treatment of these lesions, said Dr. Kelly of the University of California, Irvine, and the Beckman Laser Institute and Medical Clinic.
The pulsed dye laser is the standard of care for PWS treatment and is the laser that she and her associates use most often. However, "we use different lasers and settings over a course of treatment to try to improve our results," Dr. Kelly said in an interview. The other lasers they use include the 755-nm alexandrite laser and combined 1,064:595-nm laser system, as well as intense pulsed light.
For some patients undergoing treatment of a PWS, preparation may include use of a bleaching cream for several weeks before treatment. Sun protection of the area to be treated is recommended for all patients. She and her associates use general anesthesia for patients with large lesions and for children and infants, although this is not a universal practice among dermatologists, she pointed out.
Eye protection with a corneal shield is very important for patients if treatment involves the periorbital or eyelid area, Dr. Kelly said, noting that proper eye protection is also important for those treating the patient.
During treatment, she recommends using a 585-nm or 595-nm wavelength and 0.45-3 millisecond pulse duration--varying pulse duration and wavelength over time to achieve optimal results. Placing patients in the Trendelenburg position can increase blood flow to the area of the PWS, according to Dr. Kelly, who is also with the university's Vascular Birthmarks and Malformations Diagnostic Treatment Center.
Postoperatively, ice should be applied to the treated area, which should be elevated for the first 1-2 postoperative days. A mild analgesic like acetaminophen should be used for discomfort, she said. An emollient should be applied to the treated area, and patients should protect the treated area from sun exposure. A bleaching cream such as hydroquinone may be started 2-3 weeks after treatment for some patients.
Dr. Kelly said that most PWS birthmarks get lighter but require multiple treatments. Some lesions, however, are resistant to treatment, and complete removal is uncommon.
Research on improving results of PWS - to achieve more complete clearance over a shorter period of time - includes studies of imaging methods like laser speckle imaging (LSI), which is used intraoperatively to evaluate the impact of laser treatment on blood flow to determine if flow to the lesional blood vessel is decreased dramatically or shut down.
"Presumably, a greater reduction in flow is associated with greater damage to the blood vessels," said Dr. Kelly, who, with her associates, is studying whether a greater reduction in blood flow during treatment ultimately leads to better results. "We think it does, but we don't know that for sure yet," she said.
They also are studying whether the use of adjunctive agents after laser treatment improves results. These agents include antiangiogenic agents applied topically or administered orally or intravenously. An early study of imiquimod, an immune modulator with antiangiogenic effects, is underway, she noted.
Dr. Kelly disclosed that she has received research grants from Candela Corp. and Graceway Pharmaceuticals, and has served as a consultant to Lumenis. In addition, Graceway and Genentech have donated products for studies she is conducting.
SDEF and this news organization are both owned by Elsevier.
Pearls for Avoiding Filler Injection Danger Zones
Most dermatologists are well aware of the danger of damaging nerves during cold-steel surgery, but may be less aware of the danger zones involved in filler injection, said Dr. Howard K. Steinman at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
"Unlike the risk with a scalpel, where you're going to damage a nerve, the risk with fillers is that you may compress or occlude an artery," Dr. Steinman said in an interview. "You will get necrosis and scarring and disfigurement."
Dr. Steinman, director of dermatologic and skin cancer surgery at Texas A&M College of Medicine in College Station, offered some tips for avoiding the problem and suggestions on what to do if an occlusion occurs.
"The one everybody knows about from all the way back to the days of collagen is in the glabella," he said. If collagen is injected into the frown line, it is possible to damage the supratrochlear artery. If compressed or occluded, this artery can get a band-like area of damage extending up the forehead.
A second danger zone is at the nasolabial fold, where the angular artery runs close to the surface. Interrupting the blood flow here can cause damage to skin at the nasolabial fold and the side and tip of the nose. Although this is a relatively rare complication, the nasolabial fold is a popular site for filler injections, and physicians need to be mindful of this side effect, Dr. Steinman noted.
The third danger zone comes at the lips, where injections can interrupt flow in the labial artery.
In all cases, the symptoms are similar: There will be blanching, erythema, or edema, followed by necrosis unless the occlusion is treated promptly.
To avoid occlusion, he recommended injecting the filler perpendicular to the direction of the artery and remaining superficial but also pointed out that an artery can be indirectly occluded. According to one theory, simply injecting too much filler can compress the artery to the point of interrupting the flow.
Occlusions and compressions should be treated as soon as detected. The first step is an aggressive tapping and massaging of the area to try to break up the mass, Dr. Steinman said.
If that does not work, and the filler being used is hyaluronic acid-based, the next step is an injection of hyaluronidase, an enzyme that dissolves hyaluronic acid.
A third possibility is to apply nitroglycerin paste to the skin directly above the affected area. Typically used to keep the arteries dilated, the paste can improve flow in the case of occlusion or compression.
Unfortunately, the symptoms of an occluded artery do not always become evident immediately. "In some cases the patient won't notice this for hours after you have done the procedure," Dr. Steinman said. "They'll call you and they'll say, 'I'm having a problem.' You can certainly have them tap and massage as soon as possible, but you should meet them, even if it's at night, and start this protocol as soon as practical. It's not something you want to ignore. 'I'll see you in the morning,' is not the correct option for this."
Dr. Steinman stated that he had no conflicts of interest to disclose. SDEF and this news organization are owned by Elsevier.
Most dermatologists are well aware of the danger of damaging nerves during cold-steel surgery, but may be less aware of the danger zones involved in filler injection, said Dr. Howard K. Steinman at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
"Unlike the risk with a scalpel, where you're going to damage a nerve, the risk with fillers is that you may compress or occlude an artery," Dr. Steinman said in an interview. "You will get necrosis and scarring and disfigurement."
Dr. Steinman, director of dermatologic and skin cancer surgery at Texas A&M College of Medicine in College Station, offered some tips for avoiding the problem and suggestions on what to do if an occlusion occurs.
"The one everybody knows about from all the way back to the days of collagen is in the glabella," he said. If collagen is injected into the frown line, it is possible to damage the supratrochlear artery. If compressed or occluded, this artery can get a band-like area of damage extending up the forehead.
A second danger zone is at the nasolabial fold, where the angular artery runs close to the surface. Interrupting the blood flow here can cause damage to skin at the nasolabial fold and the side and tip of the nose. Although this is a relatively rare complication, the nasolabial fold is a popular site for filler injections, and physicians need to be mindful of this side effect, Dr. Steinman noted.
The third danger zone comes at the lips, where injections can interrupt flow in the labial artery.
In all cases, the symptoms are similar: There will be blanching, erythema, or edema, followed by necrosis unless the occlusion is treated promptly.
To avoid occlusion, he recommended injecting the filler perpendicular to the direction of the artery and remaining superficial but also pointed out that an artery can be indirectly occluded. According to one theory, simply injecting too much filler can compress the artery to the point of interrupting the flow.
Occlusions and compressions should be treated as soon as detected. The first step is an aggressive tapping and massaging of the area to try to break up the mass, Dr. Steinman said.
If that does not work, and the filler being used is hyaluronic acid-based, the next step is an injection of hyaluronidase, an enzyme that dissolves hyaluronic acid.
A third possibility is to apply nitroglycerin paste to the skin directly above the affected area. Typically used to keep the arteries dilated, the paste can improve flow in the case of occlusion or compression.
Unfortunately, the symptoms of an occluded artery do not always become evident immediately. "In some cases the patient won't notice this for hours after you have done the procedure," Dr. Steinman said. "They'll call you and they'll say, 'I'm having a problem.' You can certainly have them tap and massage as soon as possible, but you should meet them, even if it's at night, and start this protocol as soon as practical. It's not something you want to ignore. 'I'll see you in the morning,' is not the correct option for this."
Dr. Steinman stated that he had no conflicts of interest to disclose. SDEF and this news organization are owned by Elsevier.
Most dermatologists are well aware of the danger of damaging nerves during cold-steel surgery, but may be less aware of the danger zones involved in filler injection, said Dr. Howard K. Steinman at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
"Unlike the risk with a scalpel, where you're going to damage a nerve, the risk with fillers is that you may compress or occlude an artery," Dr. Steinman said in an interview. "You will get necrosis and scarring and disfigurement."
Dr. Steinman, director of dermatologic and skin cancer surgery at Texas A&M College of Medicine in College Station, offered some tips for avoiding the problem and suggestions on what to do if an occlusion occurs.
"The one everybody knows about from all the way back to the days of collagen is in the glabella," he said. If collagen is injected into the frown line, it is possible to damage the supratrochlear artery. If compressed or occluded, this artery can get a band-like area of damage extending up the forehead.
A second danger zone is at the nasolabial fold, where the angular artery runs close to the surface. Interrupting the blood flow here can cause damage to skin at the nasolabial fold and the side and tip of the nose. Although this is a relatively rare complication, the nasolabial fold is a popular site for filler injections, and physicians need to be mindful of this side effect, Dr. Steinman noted.
The third danger zone comes at the lips, where injections can interrupt flow in the labial artery.
In all cases, the symptoms are similar: There will be blanching, erythema, or edema, followed by necrosis unless the occlusion is treated promptly.
To avoid occlusion, he recommended injecting the filler perpendicular to the direction of the artery and remaining superficial but also pointed out that an artery can be indirectly occluded. According to one theory, simply injecting too much filler can compress the artery to the point of interrupting the flow.
Occlusions and compressions should be treated as soon as detected. The first step is an aggressive tapping and massaging of the area to try to break up the mass, Dr. Steinman said.
If that does not work, and the filler being used is hyaluronic acid-based, the next step is an injection of hyaluronidase, an enzyme that dissolves hyaluronic acid.
A third possibility is to apply nitroglycerin paste to the skin directly above the affected area. Typically used to keep the arteries dilated, the paste can improve flow in the case of occlusion or compression.
Unfortunately, the symptoms of an occluded artery do not always become evident immediately. "In some cases the patient won't notice this for hours after you have done the procedure," Dr. Steinman said. "They'll call you and they'll say, 'I'm having a problem.' You can certainly have them tap and massage as soon as possible, but you should meet them, even if it's at night, and start this protocol as soon as practical. It's not something you want to ignore. 'I'll see you in the morning,' is not the correct option for this."
Dr. Steinman stated that he had no conflicts of interest to disclose. SDEF and this news organization are owned by Elsevier.
Two Lasers May Be Better Than One for Hair Removal
Recent advances in laser hair removal include using combination wavelengths, longer pulses, and larger spot sizes for all skin types, and using longer wavelengths for darker skin, according to Dr. E. Victor Ross.
Better pain control and cooling techniques also can make device-based hair removal a more comfortable option for patients, Dr. Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
When using lasers for hair removal, cooling the skin before and after treatment can reduce pain and swelling, and cooling the skin during laser exposure "tends to minimize the dermal epidermal temperature," said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Historically, fair-skinned patients have been treated with a 755-nm alexandrite laser for hair removal. For dark or tanned skin, or coarser hair, a 1064-nm Nd:YAG might be more effective, but it can be more painful for patients, Dr. Ross noted.
In his experience, a blended treatment including both the 755-nm and 1064-nm lasers can be more effective for removing fine hair on the legs than either laser alone, he said, adding that some patients still prefer the 755-nm alexandrite laser because the combination therapy is more painful than the 755 nm, although it is less painful than the 1064 nm alone.
New hair removal technologies include ultrasound and microwave radiation, as well as lower-fluence intense pulsed light and diode options with suction.
Approaches using high repetition with low fluence have been applied in some settings. The advantage is less pain, but more research is needed to determine whether lower fluences at high rates of repetition are effective, and what types of treatments are effective for white hair, said Dr. Ross.
Suction devices are an option to assist with permanent hair reduction over larger areas. A larger spot size allows more photons to remain in the target area, while vacuum-assisted suction concentrates more cumulative energy at any given depth and allows for effective treatment at a lower fluence.
Dr. Ross also addressed laser-diode hair removal devices being marketed for home use. The key issues to consider when evaluating at-home devices are safety for all skin types; safety with open or closed eyes; effectiveness in removing fine, gray, or white hair; and, of course, cost.
The TRIA hair removal device from TRIA Beauty Inc. is approved by the Food and Drug Administration for home use. The device packs an 800-nm wavelength and fluences of 7, 12, or 20 J/cm2, and efficacy data on this product are promising, Dr. Ross said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron. SDEF and this news organization are both owned by Elsevier.
Recent advances in laser hair removal include using combination wavelengths, longer pulses, and larger spot sizes for all skin types, and using longer wavelengths for darker skin, according to Dr. E. Victor Ross.
Better pain control and cooling techniques also can make device-based hair removal a more comfortable option for patients, Dr. Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
When using lasers for hair removal, cooling the skin before and after treatment can reduce pain and swelling, and cooling the skin during laser exposure "tends to minimize the dermal epidermal temperature," said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Historically, fair-skinned patients have been treated with a 755-nm alexandrite laser for hair removal. For dark or tanned skin, or coarser hair, a 1064-nm Nd:YAG might be more effective, but it can be more painful for patients, Dr. Ross noted.
In his experience, a blended treatment including both the 755-nm and 1064-nm lasers can be more effective for removing fine hair on the legs than either laser alone, he said, adding that some patients still prefer the 755-nm alexandrite laser because the combination therapy is more painful than the 755 nm, although it is less painful than the 1064 nm alone.
New hair removal technologies include ultrasound and microwave radiation, as well as lower-fluence intense pulsed light and diode options with suction.
Approaches using high repetition with low fluence have been applied in some settings. The advantage is less pain, but more research is needed to determine whether lower fluences at high rates of repetition are effective, and what types of treatments are effective for white hair, said Dr. Ross.
Suction devices are an option to assist with permanent hair reduction over larger areas. A larger spot size allows more photons to remain in the target area, while vacuum-assisted suction concentrates more cumulative energy at any given depth and allows for effective treatment at a lower fluence.
Dr. Ross also addressed laser-diode hair removal devices being marketed for home use. The key issues to consider when evaluating at-home devices are safety for all skin types; safety with open or closed eyes; effectiveness in removing fine, gray, or white hair; and, of course, cost.
The TRIA hair removal device from TRIA Beauty Inc. is approved by the Food and Drug Administration for home use. The device packs an 800-nm wavelength and fluences of 7, 12, or 20 J/cm2, and efficacy data on this product are promising, Dr. Ross said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron. SDEF and this news organization are both owned by Elsevier.
Recent advances in laser hair removal include using combination wavelengths, longer pulses, and larger spot sizes for all skin types, and using longer wavelengths for darker skin, according to Dr. E. Victor Ross.
Better pain control and cooling techniques also can make device-based hair removal a more comfortable option for patients, Dr. Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
When using lasers for hair removal, cooling the skin before and after treatment can reduce pain and swelling, and cooling the skin during laser exposure "tends to minimize the dermal epidermal temperature," said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Historically, fair-skinned patients have been treated with a 755-nm alexandrite laser for hair removal. For dark or tanned skin, or coarser hair, a 1064-nm Nd:YAG might be more effective, but it can be more painful for patients, Dr. Ross noted.
In his experience, a blended treatment including both the 755-nm and 1064-nm lasers can be more effective for removing fine hair on the legs than either laser alone, he said, adding that some patients still prefer the 755-nm alexandrite laser because the combination therapy is more painful than the 755 nm, although it is less painful than the 1064 nm alone.
New hair removal technologies include ultrasound and microwave radiation, as well as lower-fluence intense pulsed light and diode options with suction.
Approaches using high repetition with low fluence have been applied in some settings. The advantage is less pain, but more research is needed to determine whether lower fluences at high rates of repetition are effective, and what types of treatments are effective for white hair, said Dr. Ross.
Suction devices are an option to assist with permanent hair reduction over larger areas. A larger spot size allows more photons to remain in the target area, while vacuum-assisted suction concentrates more cumulative energy at any given depth and allows for effective treatment at a lower fluence.
Dr. Ross also addressed laser-diode hair removal devices being marketed for home use. The key issues to consider when evaluating at-home devices are safety for all skin types; safety with open or closed eyes; effectiveness in removing fine, gray, or white hair; and, of course, cost.
The TRIA hair removal device from TRIA Beauty Inc. is approved by the Food and Drug Administration for home use. The device packs an 800-nm wavelength and fluences of 7, 12, or 20 J/cm2, and efficacy data on this product are promising, Dr. Ross said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron. SDEF and this news organization are both owned by Elsevier.
Look Beyond Obvious When Treating Veins
On the heels of the Food and Drug Administration's recent approval of polidocanol injections for the treatment of spider and reticular veins, Dr. Margaret W. Mann is working to educate her colleagues on how to cure the more serious implications of venous disease.
An estimated 55% of American women and 45% of American men suffer from some form of vein problem. Varicose veins affect one out of two people aged 50 and older, according to the Department of Health and Human Services.
"So it is very much not a cosmetic issue," Dr. Mann said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "And it is important to treat these patients before they develop serious sequelae to their disease."
Varicose veins are often inherited. If both parents have varicose veins, a person has an 89% risk of developing the condition; if one parent is affected, the risk is 47%; and if neither parent has them, the risk decreases to 20% (J. Dermatol. Surg. Oncol. 1994;20:318-26).
"When I approach a patient with telangiectasia and varicose veins, I know that it can be just the tip of the iceberg," said Dr. Mann, codirector of the dermatologic surgery and laser center at the University of California, Irvine. Early treatment is optimal to prevent worsening of the disease.
The path to curing venous disease lies in looking beyond the visible and treating the root of problem. Patients with severe spider veins along the ankle, prominent reticular veins greater than 5 mm, or palpable varicosities likely have underlying venous insufficiency, said Dr. Mann. These patients should undergo ultrasound examination to delineate their venous anatomy prior to treatment.
"In patients with outflow obstruction, varicosities must not be ablated because they are an important bypass pathway allowing blood to flow around the obstruction," explained Dr. Mann. "Specific diagnostic tests can distinguish between patients who will benefit from ablation of dilated superficial veins and those who will be harmed by the same procedure."
In patients diagnosed with great saphenous vein insufficiency, Dr. Mann recommends minimally invasive treatment with endovenous ablation and microphlebectomy. It is essential, according to Dr. Mann, to treat their underlying disease prior to treatment of their spider veins with the mind set that "everything is connected in a hierarchal way" and "therapy must start from a top down approach."
Dr. Mann disclosed she is a paid consultant with BioForm Medical (acquired by Merz Pharmaceuticas). SDEF and this news organization are owned by Elsevier.
On the heels of the Food and Drug Administration's recent approval of polidocanol injections for the treatment of spider and reticular veins, Dr. Margaret W. Mann is working to educate her colleagues on how to cure the more serious implications of venous disease.
An estimated 55% of American women and 45% of American men suffer from some form of vein problem. Varicose veins affect one out of two people aged 50 and older, according to the Department of Health and Human Services.
"So it is very much not a cosmetic issue," Dr. Mann said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "And it is important to treat these patients before they develop serious sequelae to their disease."
Varicose veins are often inherited. If both parents have varicose veins, a person has an 89% risk of developing the condition; if one parent is affected, the risk is 47%; and if neither parent has them, the risk decreases to 20% (J. Dermatol. Surg. Oncol. 1994;20:318-26).
"When I approach a patient with telangiectasia and varicose veins, I know that it can be just the tip of the iceberg," said Dr. Mann, codirector of the dermatologic surgery and laser center at the University of California, Irvine. Early treatment is optimal to prevent worsening of the disease.
The path to curing venous disease lies in looking beyond the visible and treating the root of problem. Patients with severe spider veins along the ankle, prominent reticular veins greater than 5 mm, or palpable varicosities likely have underlying venous insufficiency, said Dr. Mann. These patients should undergo ultrasound examination to delineate their venous anatomy prior to treatment.
"In patients with outflow obstruction, varicosities must not be ablated because they are an important bypass pathway allowing blood to flow around the obstruction," explained Dr. Mann. "Specific diagnostic tests can distinguish between patients who will benefit from ablation of dilated superficial veins and those who will be harmed by the same procedure."
In patients diagnosed with great saphenous vein insufficiency, Dr. Mann recommends minimally invasive treatment with endovenous ablation and microphlebectomy. It is essential, according to Dr. Mann, to treat their underlying disease prior to treatment of their spider veins with the mind set that "everything is connected in a hierarchal way" and "therapy must start from a top down approach."
Dr. Mann disclosed she is a paid consultant with BioForm Medical (acquired by Merz Pharmaceuticas). SDEF and this news organization are owned by Elsevier.
On the heels of the Food and Drug Administration's recent approval of polidocanol injections for the treatment of spider and reticular veins, Dr. Margaret W. Mann is working to educate her colleagues on how to cure the more serious implications of venous disease.
An estimated 55% of American women and 45% of American men suffer from some form of vein problem. Varicose veins affect one out of two people aged 50 and older, according to the Department of Health and Human Services.
"So it is very much not a cosmetic issue," Dr. Mann said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif. "And it is important to treat these patients before they develop serious sequelae to their disease."
Varicose veins are often inherited. If both parents have varicose veins, a person has an 89% risk of developing the condition; if one parent is affected, the risk is 47%; and if neither parent has them, the risk decreases to 20% (J. Dermatol. Surg. Oncol. 1994;20:318-26).
"When I approach a patient with telangiectasia and varicose veins, I know that it can be just the tip of the iceberg," said Dr. Mann, codirector of the dermatologic surgery and laser center at the University of California, Irvine. Early treatment is optimal to prevent worsening of the disease.
The path to curing venous disease lies in looking beyond the visible and treating the root of problem. Patients with severe spider veins along the ankle, prominent reticular veins greater than 5 mm, or palpable varicosities likely have underlying venous insufficiency, said Dr. Mann. These patients should undergo ultrasound examination to delineate their venous anatomy prior to treatment.
"In patients with outflow obstruction, varicosities must not be ablated because they are an important bypass pathway allowing blood to flow around the obstruction," explained Dr. Mann. "Specific diagnostic tests can distinguish between patients who will benefit from ablation of dilated superficial veins and those who will be harmed by the same procedure."
In patients diagnosed with great saphenous vein insufficiency, Dr. Mann recommends minimally invasive treatment with endovenous ablation and microphlebectomy. It is essential, according to Dr. Mann, to treat their underlying disease prior to treatment of their spider veins with the mind set that "everything is connected in a hierarchal way" and "therapy must start from a top down approach."
Dr. Mann disclosed she is a paid consultant with BioForm Medical (acquired by Merz Pharmaceuticas). SDEF and this news organization are owned by Elsevier.
Stategies for Optimizing Laser Safety Outlined
Visible and infrared high-power lasers can cause permanent skin and organ damage if used inappropriately.
Patient protection measures, government and institutional guidelines, and familiarity with the physics behind laser technology are means by which dermatologists can optimize safety, Dr. E. Victor Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Mild to severe reddening, blisters, charring, depigmentation, ulceration, and scarring are among possible adverse effects when these devices are not employed safely, he said.
Even when just the skin is being treated, protective measures are warranted for the eyes, said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Visible light and some infrared-wavelength light is focused as it enters the eye, making the eyes even more susceptible to laser damage. There have been reports of severe and sometimes permanent eye injuries with lasers. One patient, for example, reported seeing a white flash and hearing a click during treatment with an Nd:YAG 1064-nm laser. The result was a dark spot in the patient's visual field resulted, he said.
Protective eyewear is of paramount importance, Dr. Ross said. Select eyewear based on the laser and the anatomic region being treated. Look for eyewear marked with the wavelengths it protects against and the degree of light energy attenuation. Caution is advised when using goggles on pediatric patients because the fit may not be ideal.
In a very practical sense, Dr. Ross also advised that staff keep cups of water or coffee off the lasers. A spill or leak can get into the device power supply and cause an "explosion." In addition, never open the part of the laser where the high voltage energy is located, said Dr. Ross.
He recommended following the American National Standards Institute's (ANSI) series of laser safety standards. The recommendations are recognized by many hospitals as the standard for guiding a laser safety program, he said.
Examples of ANSI standards include physicians acting as the safety officer, routine laser maintenance, and having a set of standard operating procedures that is kept on file. Recommendations are not just for large practices, Dr. Ross said. "Even a small clinic should have a laser safety officer."
Government safety standards for laser use are available from the Occupational Safety and Health Administration and the Food and Drug Administration's Center for Devices and Radiological Health. Having a sign posted near each device warning of potential hazards specific to that class of laser is an example of a government safety standard, he said.
There are four general safety categories for lasers:
Class 1. Low-power device that is considered safe.
Class 2. The eye blink response generally provides enough eye protection during use.
Class 3. Direct exposure of the eye to these medium-power devices has potential to cause harm.
Class 4. These high-power devices require the most caution to avoid eye and skin hazards through direct and reflected exposure. These lasers also can pose a fire hazard if nearby materials are accidentally ignited from direct or scattered beams.
Credentialing is another safety measure. All clinicians operating a laser at the Scripps Clinic, for example, must be credentialed for that specific device and wavelength. Requirements include some didactic training, supervision during three or more laser treatments, and hands-on instruction by the device manufacturer, Dr. Ross said.
As with most government standards, there is official terminology regarding laser safety. Maximal permissible exposure (MPE) is an official term, describing the amount of irradiance to which a patient can be exposed without causing eye or skin damage. It is important to note that patient discomfort is possible within the MPE limitations. The MPE is calculated using wavelength and duration of laser exposure.
Dermatologists can optimize safety with knowledge of the basic physics behind the energy delivered in laser light and how it provides benefits to the skin when delivered properly, he suggested.
Power delivered per unit area is called the irradiance. This is typically expressed as the power in watts per square centimeter. Many dermatologists and device manufacturers compare lasers and outcomes in terms of joules, which is the energy delivered per square centimeter.
On the patient end, science determines the depth to which laser light penetrates and is absorbed. This absorption coefficient varies among hemoglobin, melanin, and water, for example. Each component interacts to a different extent with laser energy, and dermatologists utilize this selective photothermolysis to optimize patient outcomes from laser treatments, he said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron.
SDEF and this news organization are owned by Elsevier.
Visible and infrared high-power lasers can cause permanent skin and organ damage if used inappropriately.
Patient protection measures, government and institutional guidelines, and familiarity with the physics behind laser technology are means by which dermatologists can optimize safety, Dr. E. Victor Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Mild to severe reddening, blisters, charring, depigmentation, ulceration, and scarring are among possible adverse effects when these devices are not employed safely, he said.
Even when just the skin is being treated, protective measures are warranted for the eyes, said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Visible light and some infrared-wavelength light is focused as it enters the eye, making the eyes even more susceptible to laser damage. There have been reports of severe and sometimes permanent eye injuries with lasers. One patient, for example, reported seeing a white flash and hearing a click during treatment with an Nd:YAG 1064-nm laser. The result was a dark spot in the patient's visual field resulted, he said.
Protective eyewear is of paramount importance, Dr. Ross said. Select eyewear based on the laser and the anatomic region being treated. Look for eyewear marked with the wavelengths it protects against and the degree of light energy attenuation. Caution is advised when using goggles on pediatric patients because the fit may not be ideal.
In a very practical sense, Dr. Ross also advised that staff keep cups of water or coffee off the lasers. A spill or leak can get into the device power supply and cause an "explosion." In addition, never open the part of the laser where the high voltage energy is located, said Dr. Ross.
He recommended following the American National Standards Institute's (ANSI) series of laser safety standards. The recommendations are recognized by many hospitals as the standard for guiding a laser safety program, he said.
Examples of ANSI standards include physicians acting as the safety officer, routine laser maintenance, and having a set of standard operating procedures that is kept on file. Recommendations are not just for large practices, Dr. Ross said. "Even a small clinic should have a laser safety officer."
Government safety standards for laser use are available from the Occupational Safety and Health Administration and the Food and Drug Administration's Center for Devices and Radiological Health. Having a sign posted near each device warning of potential hazards specific to that class of laser is an example of a government safety standard, he said.
There are four general safety categories for lasers:
Class 1. Low-power device that is considered safe.
Class 2. The eye blink response generally provides enough eye protection during use.
Class 3. Direct exposure of the eye to these medium-power devices has potential to cause harm.
Class 4. These high-power devices require the most caution to avoid eye and skin hazards through direct and reflected exposure. These lasers also can pose a fire hazard if nearby materials are accidentally ignited from direct or scattered beams.
Credentialing is another safety measure. All clinicians operating a laser at the Scripps Clinic, for example, must be credentialed for that specific device and wavelength. Requirements include some didactic training, supervision during three or more laser treatments, and hands-on instruction by the device manufacturer, Dr. Ross said.
As with most government standards, there is official terminology regarding laser safety. Maximal permissible exposure (MPE) is an official term, describing the amount of irradiance to which a patient can be exposed without causing eye or skin damage. It is important to note that patient discomfort is possible within the MPE limitations. The MPE is calculated using wavelength and duration of laser exposure.
Dermatologists can optimize safety with knowledge of the basic physics behind the energy delivered in laser light and how it provides benefits to the skin when delivered properly, he suggested.
Power delivered per unit area is called the irradiance. This is typically expressed as the power in watts per square centimeter. Many dermatologists and device manufacturers compare lasers and outcomes in terms of joules, which is the energy delivered per square centimeter.
On the patient end, science determines the depth to which laser light penetrates and is absorbed. This absorption coefficient varies among hemoglobin, melanin, and water, for example. Each component interacts to a different extent with laser energy, and dermatologists utilize this selective photothermolysis to optimize patient outcomes from laser treatments, he said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron.
SDEF and this news organization are owned by Elsevier.
Visible and infrared high-power lasers can cause permanent skin and organ damage if used inappropriately.
Patient protection measures, government and institutional guidelines, and familiarity with the physics behind laser technology are means by which dermatologists can optimize safety, Dr. E. Victor Ross said at a cosmetic dermatology seminar sponsored by Skin Disease Education Foundation in Santa Monica, Calif.
Mild to severe reddening, blisters, charring, depigmentation, ulceration, and scarring are among possible adverse effects when these devices are not employed safely, he said.
Even when just the skin is being treated, protective measures are warranted for the eyes, said Dr. Ross, director of the Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Visible light and some infrared-wavelength light is focused as it enters the eye, making the eyes even more susceptible to laser damage. There have been reports of severe and sometimes permanent eye injuries with lasers. One patient, for example, reported seeing a white flash and hearing a click during treatment with an Nd:YAG 1064-nm laser. The result was a dark spot in the patient's visual field resulted, he said.
Protective eyewear is of paramount importance, Dr. Ross said. Select eyewear based on the laser and the anatomic region being treated. Look for eyewear marked with the wavelengths it protects against and the degree of light energy attenuation. Caution is advised when using goggles on pediatric patients because the fit may not be ideal.
In a very practical sense, Dr. Ross also advised that staff keep cups of water or coffee off the lasers. A spill or leak can get into the device power supply and cause an "explosion." In addition, never open the part of the laser where the high voltage energy is located, said Dr. Ross.
He recommended following the American National Standards Institute's (ANSI) series of laser safety standards. The recommendations are recognized by many hospitals as the standard for guiding a laser safety program, he said.
Examples of ANSI standards include physicians acting as the safety officer, routine laser maintenance, and having a set of standard operating procedures that is kept on file. Recommendations are not just for large practices, Dr. Ross said. "Even a small clinic should have a laser safety officer."
Government safety standards for laser use are available from the Occupational Safety and Health Administration and the Food and Drug Administration's Center for Devices and Radiological Health. Having a sign posted near each device warning of potential hazards specific to that class of laser is an example of a government safety standard, he said.
There are four general safety categories for lasers:
Class 1. Low-power device that is considered safe.
Class 2. The eye blink response generally provides enough eye protection during use.
Class 3. Direct exposure of the eye to these medium-power devices has potential to cause harm.
Class 4. These high-power devices require the most caution to avoid eye and skin hazards through direct and reflected exposure. These lasers also can pose a fire hazard if nearby materials are accidentally ignited from direct or scattered beams.
Credentialing is another safety measure. All clinicians operating a laser at the Scripps Clinic, for example, must be credentialed for that specific device and wavelength. Requirements include some didactic training, supervision during three or more laser treatments, and hands-on instruction by the device manufacturer, Dr. Ross said.
As with most government standards, there is official terminology regarding laser safety. Maximal permissible exposure (MPE) is an official term, describing the amount of irradiance to which a patient can be exposed without causing eye or skin damage. It is important to note that patient discomfort is possible within the MPE limitations. The MPE is calculated using wavelength and duration of laser exposure.
Dermatologists can optimize safety with knowledge of the basic physics behind the energy delivered in laser light and how it provides benefits to the skin when delivered properly, he suggested.
Power delivered per unit area is called the irradiance. This is typically expressed as the power in watts per square centimeter. Many dermatologists and device manufacturers compare lasers and outcomes in terms of joules, which is the energy delivered per square centimeter.
On the patient end, science determines the depth to which laser light penetrates and is absorbed. This absorption coefficient varies among hemoglobin, melanin, and water, for example. Each component interacts to a different extent with laser energy, and dermatologists utilize this selective photothermolysis to optimize patient outcomes from laser treatments, he said.
Dr. Ross disclosed that he is a researcher for and receives funding from multiple laser companies, including Candela, Cutera, Lumenis, Sciton, and Syneron.
SDEF and this news organization are owned by Elsevier.
Dermoscopy for Pigmented Lesions
Recent studies have highlighted the rising incidence of melanoma in non-white skin. In populations with darker complexions, melanomas may appear on areas of the skin not exposed to the sun, often of the acral lentiginous type.
The stage at diagnosis is also more advanced in non-white skin. Despite increased surveillance efforts, diagnosis of melanoma in darker skin is often difficult and delayed, which affects overall prognosis and likelihood of survival. When stratified by stage of diagnosis, melanoma in non-white skin has the same prognosis as melanoma in white skin.
Pigmented skin lesions are rarely noticed and are difficult to detect by clinical examination on dark skin because of reduced visibility of melanocytic lesions.
Using a dermatoscope to examine dark skin for melanomas could help improve the chance of correct diagnosis and earlier treatment if done properly. The use of dermoscopy is increasing in favor among dermatologists to improve diagnostic accuracy.
Few studies have reviewed the use of dermoscopy in darker skinned populations. In one study investigators evaluated the utility and efficacy of dermoscopy for pigmented lesions in black populations. The authors attempted to evaluate whether darker pigmentation influences dermatoscopic features in comparison with white populations (Brit. J. Dermatol. 2006:4;695-99).
In the study, 100 clinically doubtful or equivocal pigmented skin lesions in black patients were subjected to dermatoscopic examination. The lesions were observed using dermoscopy by two groups of dermatologists, one in Brazil (in vivo) and the other blinded evaluators in Italy (on slide images), both recording dermatoscopic features. The results showed that out of 100 cases, 79 were Clark nevi, 15 seborrheic keratoses, 4 blue nevi, 1 dermatofibroma, and 1 melanoma.
The agreement between observers was statistically evaluated and there was a high level of inter-observer agreement among dermatoscopic features. Only 3 out of the 100 suspicious lesions (Clark’s nevi) required surgical excision to confirm the diagnosis.
The melanomas presented dermatoscopic characteristics similar to the melanomas appearing in white populations with a blue-whitish veil, irregular globules and streaks at the periphery.
The increased incidence of melanoma, and decreased survival of ethnic patients due to a delay in diagnosis, is a sign of caution to dermatologists to increase surveillance of pigmented lesions in dark skin. Accurate classification of pigmented lesions is difficult; however, this study showed that dermoscopy can be a useful and even necessary tool in the identification of pigmented lesions in dark skin, as naked-eye examinations may be more difficult.
More accurate diagnoses can lead to, not only earlier treatment of clinically suspicious lesions, but also to a decrease in unnecessary biopsies in skin of color, which is more prone to hypertrophic and keloidal scarring.
Recent studies have highlighted the rising incidence of melanoma in non-white skin. In populations with darker complexions, melanomas may appear on areas of the skin not exposed to the sun, often of the acral lentiginous type.
The stage at diagnosis is also more advanced in non-white skin. Despite increased surveillance efforts, diagnosis of melanoma in darker skin is often difficult and delayed, which affects overall prognosis and likelihood of survival. When stratified by stage of diagnosis, melanoma in non-white skin has the same prognosis as melanoma in white skin.
Pigmented skin lesions are rarely noticed and are difficult to detect by clinical examination on dark skin because of reduced visibility of melanocytic lesions.
Using a dermatoscope to examine dark skin for melanomas could help improve the chance of correct diagnosis and earlier treatment if done properly. The use of dermoscopy is increasing in favor among dermatologists to improve diagnostic accuracy.
Few studies have reviewed the use of dermoscopy in darker skinned populations. In one study investigators evaluated the utility and efficacy of dermoscopy for pigmented lesions in black populations. The authors attempted to evaluate whether darker pigmentation influences dermatoscopic features in comparison with white populations (Brit. J. Dermatol. 2006:4;695-99).
In the study, 100 clinically doubtful or equivocal pigmented skin lesions in black patients were subjected to dermatoscopic examination. The lesions were observed using dermoscopy by two groups of dermatologists, one in Brazil (in vivo) and the other blinded evaluators in Italy (on slide images), both recording dermatoscopic features. The results showed that out of 100 cases, 79 were Clark nevi, 15 seborrheic keratoses, 4 blue nevi, 1 dermatofibroma, and 1 melanoma.
The agreement between observers was statistically evaluated and there was a high level of inter-observer agreement among dermatoscopic features. Only 3 out of the 100 suspicious lesions (Clark’s nevi) required surgical excision to confirm the diagnosis.
The melanomas presented dermatoscopic characteristics similar to the melanomas appearing in white populations with a blue-whitish veil, irregular globules and streaks at the periphery.
The increased incidence of melanoma, and decreased survival of ethnic patients due to a delay in diagnosis, is a sign of caution to dermatologists to increase surveillance of pigmented lesions in dark skin. Accurate classification of pigmented lesions is difficult; however, this study showed that dermoscopy can be a useful and even necessary tool in the identification of pigmented lesions in dark skin, as naked-eye examinations may be more difficult.
More accurate diagnoses can lead to, not only earlier treatment of clinically suspicious lesions, but also to a decrease in unnecessary biopsies in skin of color, which is more prone to hypertrophic and keloidal scarring.
Recent studies have highlighted the rising incidence of melanoma in non-white skin. In populations with darker complexions, melanomas may appear on areas of the skin not exposed to the sun, often of the acral lentiginous type.
The stage at diagnosis is also more advanced in non-white skin. Despite increased surveillance efforts, diagnosis of melanoma in darker skin is often difficult and delayed, which affects overall prognosis and likelihood of survival. When stratified by stage of diagnosis, melanoma in non-white skin has the same prognosis as melanoma in white skin.
Pigmented skin lesions are rarely noticed and are difficult to detect by clinical examination on dark skin because of reduced visibility of melanocytic lesions.
Using a dermatoscope to examine dark skin for melanomas could help improve the chance of correct diagnosis and earlier treatment if done properly. The use of dermoscopy is increasing in favor among dermatologists to improve diagnostic accuracy.
Few studies have reviewed the use of dermoscopy in darker skinned populations. In one study investigators evaluated the utility and efficacy of dermoscopy for pigmented lesions in black populations. The authors attempted to evaluate whether darker pigmentation influences dermatoscopic features in comparison with white populations (Brit. J. Dermatol. 2006:4;695-99).
In the study, 100 clinically doubtful or equivocal pigmented skin lesions in black patients were subjected to dermatoscopic examination. The lesions were observed using dermoscopy by two groups of dermatologists, one in Brazil (in vivo) and the other blinded evaluators in Italy (on slide images), both recording dermatoscopic features. The results showed that out of 100 cases, 79 were Clark nevi, 15 seborrheic keratoses, 4 blue nevi, 1 dermatofibroma, and 1 melanoma.
The agreement between observers was statistically evaluated and there was a high level of inter-observer agreement among dermatoscopic features. Only 3 out of the 100 suspicious lesions (Clark’s nevi) required surgical excision to confirm the diagnosis.
The melanomas presented dermatoscopic characteristics similar to the melanomas appearing in white populations with a blue-whitish veil, irregular globules and streaks at the periphery.
The increased incidence of melanoma, and decreased survival of ethnic patients due to a delay in diagnosis, is a sign of caution to dermatologists to increase surveillance of pigmented lesions in dark skin. Accurate classification of pigmented lesions is difficult; however, this study showed that dermoscopy can be a useful and even necessary tool in the identification of pigmented lesions in dark skin, as naked-eye examinations may be more difficult.
More accurate diagnoses can lead to, not only earlier treatment of clinically suspicious lesions, but also to a decrease in unnecessary biopsies in skin of color, which is more prone to hypertrophic and keloidal scarring.
Cryolipolysis Appears Safe for Fat Reduction
PHOENIX - Using noninvasive cryolipolysis for fat-layer reduction in the flanks and back fat pads caused no serious adverse events and no reports of skin damage or pigment changes up to 6 months after treatment, results from a large multicenter study showed.
Side effects included "mostly erythema and edema, numbness/tingling, and a little blanching," Dr. A. Jay Burns said at the annual meeting of the American Society for Laser Medicine and Surgery. "Occasionally there was bruising on the treatment site as well, but all side effects resolved by 6 months."
Invented by Dr. Dieter Manstein and Dr. R. Rox Anderson at Massachusetts General Hospital and Harvard Medical School in Boston, cryolipolysis is noninvasive way to cool fat cells to induce lipolysis without damage to other tissue. Pleasanton, Calif.-based Zeltiq currently owns exclusive rights to the technology and markets a cryolipolysis device known as the Zeltiq system.
The Zeltiq system is cleared in the European Union and Canada for noninvasive fat-layer reduction through cold-assisted lipolysis. It is also cleared by the Food and Drug Administration for various applications related to skin cooling during dermatologic treatments, with a pending application for noninvasive fat-layer reduction. The system is available for sale on a limited basis to physicians in the European Union, Canada, and the United States and other selected international markets.
At the meeting, Dr. Burns reported side effect data from two prospective, controlled clinical studies in which researchers at 16 centers used the Zeltiq system to treat 341 patients on their flanks and back fat pads. Efficacy was evaluated by ultrasound, comparison of pre- and post-treatment photographs, and physician assessment. Final follow-up occurred at 6 months or less.
"There were no reports of serious adverse effects, and all side effects were transient," said Dr. Burns, a plastic surgeon in Dallas who is also with the University of Texas Southwestern Medical Center. The most common post-treatment side effect was erythema, followed by hypoesthesia/tingling, edema, bruising, temperature sensation, blanching, and pressure at the treatment site.
PHOENIX - Using noninvasive cryolipolysis for fat-layer reduction in the flanks and back fat pads caused no serious adverse events and no reports of skin damage or pigment changes up to 6 months after treatment, results from a large multicenter study showed.
Side effects included "mostly erythema and edema, numbness/tingling, and a little blanching," Dr. A. Jay Burns said at the annual meeting of the American Society for Laser Medicine and Surgery. "Occasionally there was bruising on the treatment site as well, but all side effects resolved by 6 months."
Invented by Dr. Dieter Manstein and Dr. R. Rox Anderson at Massachusetts General Hospital and Harvard Medical School in Boston, cryolipolysis is noninvasive way to cool fat cells to induce lipolysis without damage to other tissue. Pleasanton, Calif.-based Zeltiq currently owns exclusive rights to the technology and markets a cryolipolysis device known as the Zeltiq system.
The Zeltiq system is cleared in the European Union and Canada for noninvasive fat-layer reduction through cold-assisted lipolysis. It is also cleared by the Food and Drug Administration for various applications related to skin cooling during dermatologic treatments, with a pending application for noninvasive fat-layer reduction. The system is available for sale on a limited basis to physicians in the European Union, Canada, and the United States and other selected international markets.
At the meeting, Dr. Burns reported side effect data from two prospective, controlled clinical studies in which researchers at 16 centers used the Zeltiq system to treat 341 patients on their flanks and back fat pads. Efficacy was evaluated by ultrasound, comparison of pre- and post-treatment photographs, and physician assessment. Final follow-up occurred at 6 months or less.
"There were no reports of serious adverse effects, and all side effects were transient," said Dr. Burns, a plastic surgeon in Dallas who is also with the University of Texas Southwestern Medical Center. The most common post-treatment side effect was erythema, followed by hypoesthesia/tingling, edema, bruising, temperature sensation, blanching, and pressure at the treatment site.
PHOENIX - Using noninvasive cryolipolysis for fat-layer reduction in the flanks and back fat pads caused no serious adverse events and no reports of skin damage or pigment changes up to 6 months after treatment, results from a large multicenter study showed.
Side effects included "mostly erythema and edema, numbness/tingling, and a little blanching," Dr. A. Jay Burns said at the annual meeting of the American Society for Laser Medicine and Surgery. "Occasionally there was bruising on the treatment site as well, but all side effects resolved by 6 months."
Invented by Dr. Dieter Manstein and Dr. R. Rox Anderson at Massachusetts General Hospital and Harvard Medical School in Boston, cryolipolysis is noninvasive way to cool fat cells to induce lipolysis without damage to other tissue. Pleasanton, Calif.-based Zeltiq currently owns exclusive rights to the technology and markets a cryolipolysis device known as the Zeltiq system.
The Zeltiq system is cleared in the European Union and Canada for noninvasive fat-layer reduction through cold-assisted lipolysis. It is also cleared by the Food and Drug Administration for various applications related to skin cooling during dermatologic treatments, with a pending application for noninvasive fat-layer reduction. The system is available for sale on a limited basis to physicians in the European Union, Canada, and the United States and other selected international markets.
At the meeting, Dr. Burns reported side effect data from two prospective, controlled clinical studies in which researchers at 16 centers used the Zeltiq system to treat 341 patients on their flanks and back fat pads. Efficacy was evaluated by ultrasound, comparison of pre- and post-treatment photographs, and physician assessment. Final follow-up occurred at 6 months or less.
"There were no reports of serious adverse effects, and all side effects were transient," said Dr. Burns, a plastic surgeon in Dallas who is also with the University of Texas Southwestern Medical Center. The most common post-treatment side effect was erythema, followed by hypoesthesia/tingling, edema, bruising, temperature sensation, blanching, and pressure at the treatment site.
ASLMS: Tips for Effective Laser Hair Removal in Darker Skin
PHOENIX - When performing laser hair removal in patients with Fitzpatrick skin types IV-VI, keep in mind that darker skin contains more melanin in the epidermis, which acts as a competing chromophore, "so the risk for epidermal injury is higher," Dr. Andrew F. Alexis said.
Other tips to remember when treating this patient population include the melanocytes' tendency "to be labile in response to injury and inflammation, so there is an increased risk of dyschromia," Dr. Alexis said at the annual meeting of the American Society for Laser Medicine and Surgery. "This can manifest as hyperpigmentation or hypopigmentation following laser hair removal procedures."
He went on to note that fibroblasts in the dermis "are also more reactive to injury, so there is an increased risk of hypertrophic scars and keloids when performing surgical or some cosmetic procedures. In addition, having curved follicles [which are primarily seen in people of African descent] is associated with an increased prevalence of a number of follicular disorders."
His guidelines for performing laser hair removal safely on skin of color include longer wavelengths, lower fluences, longer pulse durations, and increased epidermal cooling.
"You want longer wavelengths because we're trying to maximize the ratio of follicular bulb temperature to epidermal temperature," explained Dr. Alexis, director of the Skin of Color Center at St. Luke's & Roosevelt Hospitals, New York, and assistant professor of dermatology at Columbia University.
"Using wavelengths in the near infrared range, we are at a lower point on the melanin absorption curve and therefore are compromising some efficacy, but this is the range that is considered safest for darker skin types," he noted.
A review found that the long-pulsed 1064-nm laser had the lowest incidence of adverse events in dark-skinned patients, followed by the long-pulsed 800-nm or 810-nm diode laser (J. Drugs Dermatol. 2007;6:40-6).
"For patients with type IV or V skin, the diode laser is appropriate, as long as you are using long pulse durations," he said, "but for the darker skin types, particularly type VI, the 1064-nm Nd:YAG laser is the best choice for safety reasons."
In one study, researchers used a 1064-nm laser with contact cooling to treat pseudofolliculitis barbae in 37 patients with skin types IV, V, and VI. They found that the highest fluences tolerated by the epidermis were 50 J/cm2 for skin type VI and 100 J/cm2 for skin types IV and V (J. Am. Acad. Dermatol. 2002;47:263-70).
In another study, researchers used a 1064-nm laser with contact cooling for hair removal in 36 patients with skin types I-VI (Dermatol. Surg. 2004;30:13-7). Patients underwent three consecutive treatments at 4- to 6-week intervals. For skin types V-VI, investigators used a 30-millisecond pulse duration and a fluence of 30-45 J/cm2 on the face and 35-50 J/cm2 on nonfacial sites. Six months post treatment, the mean facial hair reduction ranged from 41% to 46%, while the mean hair reduction on the body ranged from 48% to 53%.
Based on the results of these and other studies, and from his own clinical experience, Dr. Alexis recommends a pulse duration of 100 milliseconds or 400 milliseconds when using a 810-nm diode laser and a duration of 20-30 milliseconds when using a 1064-nm Nd:YAG laser with contact cooling.
One recent study used a 1064-nm Nd:YAG laser with lower than traditional fluences for treating 22 patients with skin types IV-VI who had pseudofolliculitis barbae (Dermatol. Surg. 2009;35:98-107). Patients underwent five weekly treatments on the neck with a fluence of 12 J/cm2 and a pulse duration of 20 milliseconds and a spot size of 10 mm. At 4 weeks follow-up, the papule count had been reduced by a mean of 91% and dyspigmentation by a mean of 60%.
In another recent development, researchers studying a novel diode laser with a fluence of 5-10 J/cm2 used at a repetition rate of 10 Hz found that it resulted in less pain, faster treatment, and fewer adverse events compared with one pass of a high-fluence diode laser at 25-40 J/cm2 in Fitzpatrick skin types I-V (J. Drugs Dermatol. 2009;8:s14-7).
Options for epidermal cooling include cold gel, contact cryogen or forced air, and post treatment with ice packs for 10-15 minutes. Devices for contact cooling feature either a sapphire tip or chilled copper plate. Regardless of which type of contact cooling chosen, Dr. Alexis suggested "using a slower treatment speed in order to ensure adequate cooling before delivering pulse."
Dr. Alexis said that he had no relevant financial conflicts.
PHOENIX - When performing laser hair removal in patients with Fitzpatrick skin types IV-VI, keep in mind that darker skin contains more melanin in the epidermis, which acts as a competing chromophore, "so the risk for epidermal injury is higher," Dr. Andrew F. Alexis said.
Other tips to remember when treating this patient population include the melanocytes' tendency "to be labile in response to injury and inflammation, so there is an increased risk of dyschromia," Dr. Alexis said at the annual meeting of the American Society for Laser Medicine and Surgery. "This can manifest as hyperpigmentation or hypopigmentation following laser hair removal procedures."
He went on to note that fibroblasts in the dermis "are also more reactive to injury, so there is an increased risk of hypertrophic scars and keloids when performing surgical or some cosmetic procedures. In addition, having curved follicles [which are primarily seen in people of African descent] is associated with an increased prevalence of a number of follicular disorders."
His guidelines for performing laser hair removal safely on skin of color include longer wavelengths, lower fluences, longer pulse durations, and increased epidermal cooling.
"You want longer wavelengths because we're trying to maximize the ratio of follicular bulb temperature to epidermal temperature," explained Dr. Alexis, director of the Skin of Color Center at St. Luke's & Roosevelt Hospitals, New York, and assistant professor of dermatology at Columbia University.
"Using wavelengths in the near infrared range, we are at a lower point on the melanin absorption curve and therefore are compromising some efficacy, but this is the range that is considered safest for darker skin types," he noted.
A review found that the long-pulsed 1064-nm laser had the lowest incidence of adverse events in dark-skinned patients, followed by the long-pulsed 800-nm or 810-nm diode laser (J. Drugs Dermatol. 2007;6:40-6).
"For patients with type IV or V skin, the diode laser is appropriate, as long as you are using long pulse durations," he said, "but for the darker skin types, particularly type VI, the 1064-nm Nd:YAG laser is the best choice for safety reasons."
In one study, researchers used a 1064-nm laser with contact cooling to treat pseudofolliculitis barbae in 37 patients with skin types IV, V, and VI. They found that the highest fluences tolerated by the epidermis were 50 J/cm2 for skin type VI and 100 J/cm2 for skin types IV and V (J. Am. Acad. Dermatol. 2002;47:263-70).
In another study, researchers used a 1064-nm laser with contact cooling for hair removal in 36 patients with skin types I-VI (Dermatol. Surg. 2004;30:13-7). Patients underwent three consecutive treatments at 4- to 6-week intervals. For skin types V-VI, investigators used a 30-millisecond pulse duration and a fluence of 30-45 J/cm2 on the face and 35-50 J/cm2 on nonfacial sites. Six months post treatment, the mean facial hair reduction ranged from 41% to 46%, while the mean hair reduction on the body ranged from 48% to 53%.
Based on the results of these and other studies, and from his own clinical experience, Dr. Alexis recommends a pulse duration of 100 milliseconds or 400 milliseconds when using a 810-nm diode laser and a duration of 20-30 milliseconds when using a 1064-nm Nd:YAG laser with contact cooling.
One recent study used a 1064-nm Nd:YAG laser with lower than traditional fluences for treating 22 patients with skin types IV-VI who had pseudofolliculitis barbae (Dermatol. Surg. 2009;35:98-107). Patients underwent five weekly treatments on the neck with a fluence of 12 J/cm2 and a pulse duration of 20 milliseconds and a spot size of 10 mm. At 4 weeks follow-up, the papule count had been reduced by a mean of 91% and dyspigmentation by a mean of 60%.
In another recent development, researchers studying a novel diode laser with a fluence of 5-10 J/cm2 used at a repetition rate of 10 Hz found that it resulted in less pain, faster treatment, and fewer adverse events compared with one pass of a high-fluence diode laser at 25-40 J/cm2 in Fitzpatrick skin types I-V (J. Drugs Dermatol. 2009;8:s14-7).
Options for epidermal cooling include cold gel, contact cryogen or forced air, and post treatment with ice packs for 10-15 minutes. Devices for contact cooling feature either a sapphire tip or chilled copper plate. Regardless of which type of contact cooling chosen, Dr. Alexis suggested "using a slower treatment speed in order to ensure adequate cooling before delivering pulse."
Dr. Alexis said that he had no relevant financial conflicts.
PHOENIX - When performing laser hair removal in patients with Fitzpatrick skin types IV-VI, keep in mind that darker skin contains more melanin in the epidermis, which acts as a competing chromophore, "so the risk for epidermal injury is higher," Dr. Andrew F. Alexis said.
Other tips to remember when treating this patient population include the melanocytes' tendency "to be labile in response to injury and inflammation, so there is an increased risk of dyschromia," Dr. Alexis said at the annual meeting of the American Society for Laser Medicine and Surgery. "This can manifest as hyperpigmentation or hypopigmentation following laser hair removal procedures."
He went on to note that fibroblasts in the dermis "are also more reactive to injury, so there is an increased risk of hypertrophic scars and keloids when performing surgical or some cosmetic procedures. In addition, having curved follicles [which are primarily seen in people of African descent] is associated with an increased prevalence of a number of follicular disorders."
His guidelines for performing laser hair removal safely on skin of color include longer wavelengths, lower fluences, longer pulse durations, and increased epidermal cooling.
"You want longer wavelengths because we're trying to maximize the ratio of follicular bulb temperature to epidermal temperature," explained Dr. Alexis, director of the Skin of Color Center at St. Luke's & Roosevelt Hospitals, New York, and assistant professor of dermatology at Columbia University.
"Using wavelengths in the near infrared range, we are at a lower point on the melanin absorption curve and therefore are compromising some efficacy, but this is the range that is considered safest for darker skin types," he noted.
A review found that the long-pulsed 1064-nm laser had the lowest incidence of adverse events in dark-skinned patients, followed by the long-pulsed 800-nm or 810-nm diode laser (J. Drugs Dermatol. 2007;6:40-6).
"For patients with type IV or V skin, the diode laser is appropriate, as long as you are using long pulse durations," he said, "but for the darker skin types, particularly type VI, the 1064-nm Nd:YAG laser is the best choice for safety reasons."
In one study, researchers used a 1064-nm laser with contact cooling to treat pseudofolliculitis barbae in 37 patients with skin types IV, V, and VI. They found that the highest fluences tolerated by the epidermis were 50 J/cm2 for skin type VI and 100 J/cm2 for skin types IV and V (J. Am. Acad. Dermatol. 2002;47:263-70).
In another study, researchers used a 1064-nm laser with contact cooling for hair removal in 36 patients with skin types I-VI (Dermatol. Surg. 2004;30:13-7). Patients underwent three consecutive treatments at 4- to 6-week intervals. For skin types V-VI, investigators used a 30-millisecond pulse duration and a fluence of 30-45 J/cm2 on the face and 35-50 J/cm2 on nonfacial sites. Six months post treatment, the mean facial hair reduction ranged from 41% to 46%, while the mean hair reduction on the body ranged from 48% to 53%.
Based on the results of these and other studies, and from his own clinical experience, Dr. Alexis recommends a pulse duration of 100 milliseconds or 400 milliseconds when using a 810-nm diode laser and a duration of 20-30 milliseconds when using a 1064-nm Nd:YAG laser with contact cooling.
One recent study used a 1064-nm Nd:YAG laser with lower than traditional fluences for treating 22 patients with skin types IV-VI who had pseudofolliculitis barbae (Dermatol. Surg. 2009;35:98-107). Patients underwent five weekly treatments on the neck with a fluence of 12 J/cm2 and a pulse duration of 20 milliseconds and a spot size of 10 mm. At 4 weeks follow-up, the papule count had been reduced by a mean of 91% and dyspigmentation by a mean of 60%.
In another recent development, researchers studying a novel diode laser with a fluence of 5-10 J/cm2 used at a repetition rate of 10 Hz found that it resulted in less pain, faster treatment, and fewer adverse events compared with one pass of a high-fluence diode laser at 25-40 J/cm2 in Fitzpatrick skin types I-V (J. Drugs Dermatol. 2009;8:s14-7).
Options for epidermal cooling include cold gel, contact cryogen or forced air, and post treatment with ice packs for 10-15 minutes. Devices for contact cooling feature either a sapphire tip or chilled copper plate. Regardless of which type of contact cooling chosen, Dr. Alexis suggested "using a slower treatment speed in order to ensure adequate cooling before delivering pulse."
Dr. Alexis said that he had no relevant financial conflicts.