User login
Study Characterizes Pathologic B-Cell Maturation in Crohn’s Disease
, according to investigators.
These findings begin to address a knowledge gap in Crohn’s disease that has been more thoroughly explored in ulcerative colitis, reported lead author Sonja Kappel-Latif, MD, PhD, of Medical University of Vienna, Vienna, Austria, and colleagues.
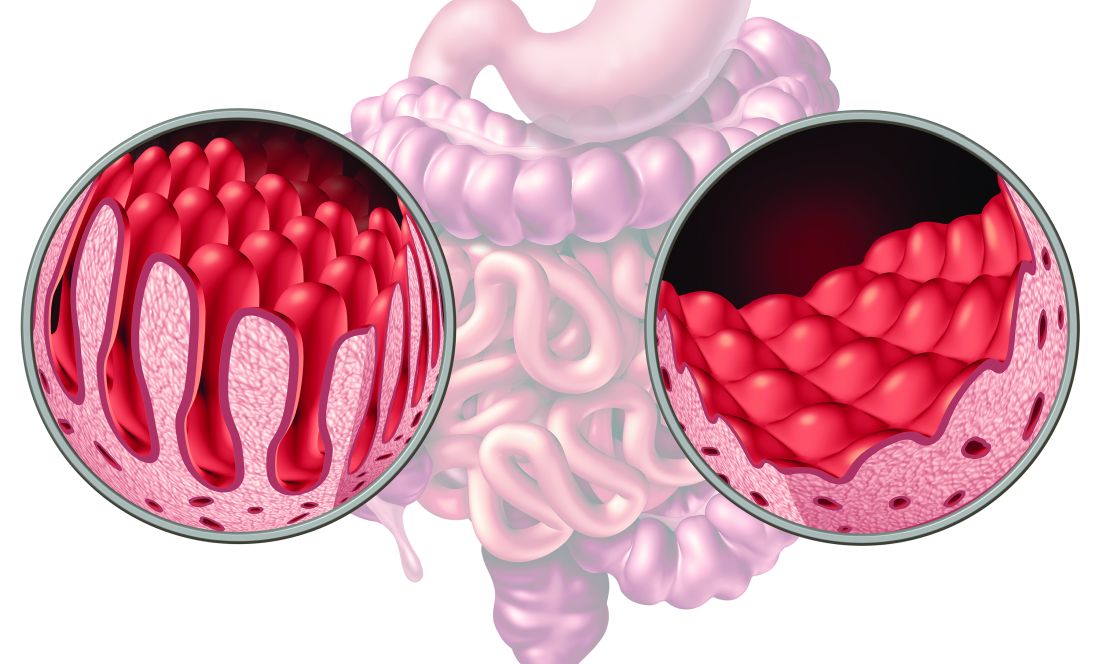
“Recent studies have investigated the role of B-cell responses in ulcerative colitis, which exclusively affects the colon, whereas data in CD, which mainly affects the terminal ileum, are insufficient,” the investigators wrote in wrote in Cellular and Molecular Gastroenterology and Hepatology. “Granuloma formation within the thickened, inflamed mesentery of patients with CD, however, is associated with significantly worse outcome, and microstructural analysis has suggested increased numbers of B cells in CD mesentery.”
Previous studies have shown that abnormal B-cell development in patients with CD leads to development of IgG targeting commensal — instead of pathogenic — gut bacteria. Yet B-cell receptor sequencing in CD has only been conducted on peripheral blood, despite awareness that anticommensal IgG antibodies can be transported across mucosal barriers in patients with ulcerative colitis, sustaining intestinal inflammation.
To better characterize local B-cell responses in CD, the investigators evaluated paired samples of draining mesenteric lymph nodes (MLNs) from both healthy and adjacently affected intestinal tissue, yielding a range of findings.
First, the investigators noted that CD19+ B cells and CD45+ leukocytes were expanded in affected MLNs, while T cells were reduced. A closer look showed that IgD-CD27- B cells were more abundant among CD19+CD45+ B cells in affected MLNs. Within this CD45+CD19+CD27+IgD- B-cell fraction, CD38- memory B cells were reduced.
The above findings suggest “ongoing antigenic stimulation within affected MLNs,” the investigators wrote.
Further comparison of paired samples showed that germinal centers (within which B cells mature) were significantly larger in affected MLNs, and contained dark and light zones. In contrast, healthy MLNs had smaller, more immature germinal centers.
Due to T-cell dependence during B-cell isotype switching within these germinal centers, the investigators next conducted immunohistochemistry staining for Bcl6, a “master regulator” of T-follicular helper cells expressed in class-switching B cells, and Ki67, which indicates cell proliferation. These analyses shows that both markers were “highly positive” within the germinal centers of affected MLNs.
Next, Dr. Kappel-Latif and colleagues conducted B-cell receptor (BCR) sequencing to characterize differences in class switching. Compared with healthy MLNs, affected MLNs showed decreased use of IGHA and IGHE alongside a significant uptick in IGHG1/2.
Further analyses showed that somatic hypermutation (SHM) frequency was significantly higher in IGHM and IGHA B cells, which was driven by mutations in complementary determining regions (CDRs) and framework regions of IGHA B cells, and mutations in the CDRs of IGHM B cells.
BCR diversity increased in the IGHG1/2 B cells, but remained unchanged in the IGHM or IGHA B cells.
“Overall, our results indicate ongoing class switching within draining MLNs of affected intestinal segments, with a shift toward IGHG1/2 BCRs,” the investigators concluded. “The lack of high SHM rates within IGHG1/2 BCRs, the difference between IGHA and IGHG1/2 BCRs in single MLNs, and increased diversity in IGHG1/2 BCRs suggests that many antigens do not result in long-lasting immunologic stimulation, and IGHA and IGHG1/2 responses may target different pathogens/commensals.”
The study was supported by the Austrian Science Fund and the Major of Vienna. The investigators disclosed no conflicts of interest.
The pathophysiology of inflammatory bowel disease (IBD) is complex and involves multiple mechanisms. Among these mechanisms, dysfunction and overactivation of the intestinal immune system are widely implicated. Dysfunctions in both the innate and adaptive immune systems have been demonstrated. However, mucosal immunology research related to IBD has long been particularly focused on T lymphocytes due to the failure of the rituximab clinical trial (anti-CD20) in ulcerative colitis (UC). Recent data have indicated modifications in the landscape of B lymphocyte subpopulations within the inflamed mucosa of patients with UC or ileal Crohn’s disease (CD).
Similarly, to what was previously shown in the inflamed colonic and ileal mucosa of IBD patients, isotype usage showed a skewing from IgA to IgG1. Further analysis of the B cell receptor (BCR) showed a very diverse repertoire of B cells, reflecting a large panel of antigenic stimulation. As we know, IBD are complex diseases that may not be explained by a single or a limited set of antigenic drivers.
Whether these changes in the B-cell compartment are a triggering event of inflammation or a bystander, reflecting the increased intestinal permeability and exposure to microbiota antigens during inflammation, remains to be explored and further studied.
Mathieu Uzzan, MD, PhD, is based in the gastroenterology department, Hopital Henri Mondor, APHP, Créteil, France. He has no relevant disclosures.
The pathophysiology of inflammatory bowel disease (IBD) is complex and involves multiple mechanisms. Among these mechanisms, dysfunction and overactivation of the intestinal immune system are widely implicated. Dysfunctions in both the innate and adaptive immune systems have been demonstrated. However, mucosal immunology research related to IBD has long been particularly focused on T lymphocytes due to the failure of the rituximab clinical trial (anti-CD20) in ulcerative colitis (UC). Recent data have indicated modifications in the landscape of B lymphocyte subpopulations within the inflamed mucosa of patients with UC or ileal Crohn’s disease (CD).
Similarly, to what was previously shown in the inflamed colonic and ileal mucosa of IBD patients, isotype usage showed a skewing from IgA to IgG1. Further analysis of the B cell receptor (BCR) showed a very diverse repertoire of B cells, reflecting a large panel of antigenic stimulation. As we know, IBD are complex diseases that may not be explained by a single or a limited set of antigenic drivers.
Whether these changes in the B-cell compartment are a triggering event of inflammation or a bystander, reflecting the increased intestinal permeability and exposure to microbiota antigens during inflammation, remains to be explored and further studied.
Mathieu Uzzan, MD, PhD, is based in the gastroenterology department, Hopital Henri Mondor, APHP, Créteil, France. He has no relevant disclosures.
The pathophysiology of inflammatory bowel disease (IBD) is complex and involves multiple mechanisms. Among these mechanisms, dysfunction and overactivation of the intestinal immune system are widely implicated. Dysfunctions in both the innate and adaptive immune systems have been demonstrated. However, mucosal immunology research related to IBD has long been particularly focused on T lymphocytes due to the failure of the rituximab clinical trial (anti-CD20) in ulcerative colitis (UC). Recent data have indicated modifications in the landscape of B lymphocyte subpopulations within the inflamed mucosa of patients with UC or ileal Crohn’s disease (CD).
Similarly, to what was previously shown in the inflamed colonic and ileal mucosa of IBD patients, isotype usage showed a skewing from IgA to IgG1. Further analysis of the B cell receptor (BCR) showed a very diverse repertoire of B cells, reflecting a large panel of antigenic stimulation. As we know, IBD are complex diseases that may not be explained by a single or a limited set of antigenic drivers.
Whether these changes in the B-cell compartment are a triggering event of inflammation or a bystander, reflecting the increased intestinal permeability and exposure to microbiota antigens during inflammation, remains to be explored and further studied.
Mathieu Uzzan, MD, PhD, is based in the gastroenterology department, Hopital Henri Mondor, APHP, Créteil, France. He has no relevant disclosures.
, according to investigators.
These findings begin to address a knowledge gap in Crohn’s disease that has been more thoroughly explored in ulcerative colitis, reported lead author Sonja Kappel-Latif, MD, PhD, of Medical University of Vienna, Vienna, Austria, and colleagues.
“Recent studies have investigated the role of B-cell responses in ulcerative colitis, which exclusively affects the colon, whereas data in CD, which mainly affects the terminal ileum, are insufficient,” the investigators wrote in wrote in Cellular and Molecular Gastroenterology and Hepatology. “Granuloma formation within the thickened, inflamed mesentery of patients with CD, however, is associated with significantly worse outcome, and microstructural analysis has suggested increased numbers of B cells in CD mesentery.”
Previous studies have shown that abnormal B-cell development in patients with CD leads to development of IgG targeting commensal — instead of pathogenic — gut bacteria. Yet B-cell receptor sequencing in CD has only been conducted on peripheral blood, despite awareness that anticommensal IgG antibodies can be transported across mucosal barriers in patients with ulcerative colitis, sustaining intestinal inflammation.
To better characterize local B-cell responses in CD, the investigators evaluated paired samples of draining mesenteric lymph nodes (MLNs) from both healthy and adjacently affected intestinal tissue, yielding a range of findings.
First, the investigators noted that CD19+ B cells and CD45+ leukocytes were expanded in affected MLNs, while T cells were reduced. A closer look showed that IgD-CD27- B cells were more abundant among CD19+CD45+ B cells in affected MLNs. Within this CD45+CD19+CD27+IgD- B-cell fraction, CD38- memory B cells were reduced.
The above findings suggest “ongoing antigenic stimulation within affected MLNs,” the investigators wrote.
Further comparison of paired samples showed that germinal centers (within which B cells mature) were significantly larger in affected MLNs, and contained dark and light zones. In contrast, healthy MLNs had smaller, more immature germinal centers.
Due to T-cell dependence during B-cell isotype switching within these germinal centers, the investigators next conducted immunohistochemistry staining for Bcl6, a “master regulator” of T-follicular helper cells expressed in class-switching B cells, and Ki67, which indicates cell proliferation. These analyses shows that both markers were “highly positive” within the germinal centers of affected MLNs.
Next, Dr. Kappel-Latif and colleagues conducted B-cell receptor (BCR) sequencing to characterize differences in class switching. Compared with healthy MLNs, affected MLNs showed decreased use of IGHA and IGHE alongside a significant uptick in IGHG1/2.
Further analyses showed that somatic hypermutation (SHM) frequency was significantly higher in IGHM and IGHA B cells, which was driven by mutations in complementary determining regions (CDRs) and framework regions of IGHA B cells, and mutations in the CDRs of IGHM B cells.
BCR diversity increased in the IGHG1/2 B cells, but remained unchanged in the IGHM or IGHA B cells.
“Overall, our results indicate ongoing class switching within draining MLNs of affected intestinal segments, with a shift toward IGHG1/2 BCRs,” the investigators concluded. “The lack of high SHM rates within IGHG1/2 BCRs, the difference between IGHA and IGHG1/2 BCRs in single MLNs, and increased diversity in IGHG1/2 BCRs suggests that many antigens do not result in long-lasting immunologic stimulation, and IGHA and IGHG1/2 responses may target different pathogens/commensals.”
The study was supported by the Austrian Science Fund and the Major of Vienna. The investigators disclosed no conflicts of interest.
, according to investigators.
These findings begin to address a knowledge gap in Crohn’s disease that has been more thoroughly explored in ulcerative colitis, reported lead author Sonja Kappel-Latif, MD, PhD, of Medical University of Vienna, Vienna, Austria, and colleagues.
“Recent studies have investigated the role of B-cell responses in ulcerative colitis, which exclusively affects the colon, whereas data in CD, which mainly affects the terminal ileum, are insufficient,” the investigators wrote in wrote in Cellular and Molecular Gastroenterology and Hepatology. “Granuloma formation within the thickened, inflamed mesentery of patients with CD, however, is associated with significantly worse outcome, and microstructural analysis has suggested increased numbers of B cells in CD mesentery.”
Previous studies have shown that abnormal B-cell development in patients with CD leads to development of IgG targeting commensal — instead of pathogenic — gut bacteria. Yet B-cell receptor sequencing in CD has only been conducted on peripheral blood, despite awareness that anticommensal IgG antibodies can be transported across mucosal barriers in patients with ulcerative colitis, sustaining intestinal inflammation.
To better characterize local B-cell responses in CD, the investigators evaluated paired samples of draining mesenteric lymph nodes (MLNs) from both healthy and adjacently affected intestinal tissue, yielding a range of findings.
First, the investigators noted that CD19+ B cells and CD45+ leukocytes were expanded in affected MLNs, while T cells were reduced. A closer look showed that IgD-CD27- B cells were more abundant among CD19+CD45+ B cells in affected MLNs. Within this CD45+CD19+CD27+IgD- B-cell fraction, CD38- memory B cells were reduced.
The above findings suggest “ongoing antigenic stimulation within affected MLNs,” the investigators wrote.
Further comparison of paired samples showed that germinal centers (within which B cells mature) were significantly larger in affected MLNs, and contained dark and light zones. In contrast, healthy MLNs had smaller, more immature germinal centers.
Due to T-cell dependence during B-cell isotype switching within these germinal centers, the investigators next conducted immunohistochemistry staining for Bcl6, a “master regulator” of T-follicular helper cells expressed in class-switching B cells, and Ki67, which indicates cell proliferation. These analyses shows that both markers were “highly positive” within the germinal centers of affected MLNs.
Next, Dr. Kappel-Latif and colleagues conducted B-cell receptor (BCR) sequencing to characterize differences in class switching. Compared with healthy MLNs, affected MLNs showed decreased use of IGHA and IGHE alongside a significant uptick in IGHG1/2.
Further analyses showed that somatic hypermutation (SHM) frequency was significantly higher in IGHM and IGHA B cells, which was driven by mutations in complementary determining regions (CDRs) and framework regions of IGHA B cells, and mutations in the CDRs of IGHM B cells.
BCR diversity increased in the IGHG1/2 B cells, but remained unchanged in the IGHM or IGHA B cells.
“Overall, our results indicate ongoing class switching within draining MLNs of affected intestinal segments, with a shift toward IGHG1/2 BCRs,” the investigators concluded. “The lack of high SHM rates within IGHG1/2 BCRs, the difference between IGHA and IGHG1/2 BCRs in single MLNs, and increased diversity in IGHG1/2 BCRs suggests that many antigens do not result in long-lasting immunologic stimulation, and IGHA and IGHG1/2 responses may target different pathogens/commensals.”
The study was supported by the Austrian Science Fund and the Major of Vienna. The investigators disclosed no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
AGA Supports Fecal Microbiota Therapies for CDI but Not IBD or IBS
Addressing Clostridium difficile infection (CDI), Crohn’s disease (CD) ulcerative colitis (UC), pouchitis, and irritable bowel syndrome (IBS), the guidance supports FMT for the prevention of recurrent CDI but not for inflammatory bowel disease (IBD) or IBS — outside of clinical trials.
The AGA’s recommendations were published in Gastroenterology.
“Fecal microbiota–based therapies are effective therapy to prevent recurrent C. difficile in select patients,” the AGA guideline states. “Conventional fecal microbiota transplant is an adjuvant treatment for select adults hospitalized with severe or fulminant C. difficile infection not responding to standard of care antibiotics. Fecal microbiota transplant cannot yet be recommended in other gastrointestinal conditions.”
“We thought it was important to write this guideline because of the growing number of trials of FMT in IBD and IBS populations. It was also important with the new FDA-approved treatments on the market,” the guideline’s first author, Anne F. Peery, MD, MSCR, AGAF, told this news organization, noting that the recently approved products did not yield better results than those of conventional rectal FMT. “The guidelines will help clinicians understand the available therapies and how to use these treatments,” added Dr. Peery, associate professor in the Division of Gastroenterology and Hepatology at the University of North Carolina School of Medicine in Chapel Hill.
Although the existing evidence is of low or very low certainty, Dr. Peery acknowledged, gastroenterologists “should be comfortable with conventional FMT and also the new FDA-approved products. We spent a considerable amount of time developing implementation considerations, which is practical advice to help clinicians use the guideline recommendations.”
Designed to counteract intestinal dysbiosis and restore protective gut flora, the FMT approach includes conventional, colonoscopically delivered donor stool transplants as well as two newly approved options: rectally given fecal microbiota (live-jslm/ Rebyota) and most recently, orally delivered fecal microbiota spores (live-brpk/ Vowst).
The AGA urges careful pretreatment consideration for patients who require frequent antibiotics or long-term antibiotic prophylaxis since ongoing antibiotics may diminish the efficacy of FMT.
The guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation framework to prioritize clinical questions, identify patient-centered outcomes, and conduct an evidence synthesis, followed by the Evidence-to-Decision framework to develop recommendations for these therapies and algorithms for their implementation into clinical practice.
Recommendations
The eight-member panel suggested the following practices on behalf of the AGA Clinical Guidelines Committee:
- In immunocompetent adults with recurrent CDI, select use of FMT can be used after completion of standard-of-care antibiotics to prevent recurrence. It can be considered after the second recurrence (episode 3) of CDI or in select patients at high risk for either recurrent CDI or a morbid CDI recurrence. Recurrent CDI is defined as clinically significant diarrhea ≥ 3 unformed stools in 24 hours with a confirmatory positive test within 8 weeks of completing antibiotics. Select use includes patients who have recovered from severe, fulminant, or particularly treatment-refractory CDI and patients with significant comorbidities. Severe CDI involves a leukocyte count of ≥15 × 109 cells/L and/or creatinine ≥1.5 mg/dL, while fulminant CDI involves shock, ileus, or megacolon and can be fatal.
- In mildly or moderately immunocompromised adults with recurrent CDI, the guidance recommends select use of conventional fecal microbiota transplant.
- In severely immunocompromised adults or those undergoing cytotoxic treatment, the AGA advises against the use of any fecal microbiota-based therapies to prevent recurrent CDI.
- Conventional FMT is not advised in patients who have bowel perforation or obstruction or are severely immunocompromised.
- For CDI patients not interested in FMT, reasonable alternatives to prevent recurrence are a vancomycin taper, tapered-pulsed fidaxomicin, or bezlotoxumab.
- In adults hospitalized with severe or fulminant CDI not responding to standard-of-care antibiotics, the AGA recommends select use of conventional FM transplant.
- In the current absence of evidence, the guidance advises against the use of conventional fecal microbiota transplant as treatment for IBD or IBS except in the context of clinical trials.
“We felt the data for using FMT in the treatment of UC was promising, but there is still a lot more work to be done in IBD and IBS,” Dr. Peery said. For each disease section the guideline outlined directions for future research. It will be updated in 3-5 years as more evidence becomes available.
This guideline was fully funded by the AGA Institute. Dr. Peery and fellow panel member Dr. Benjamin Lebwohl are supported by grants the National Institute of Diabetes and Digestive and Kidney Diseases. Panel member Colleen R. Kelly, MD, is supported by the National Institute of Allergy and Infectious Diseases.
None of the panel members had any conflicts of interest to report.
Addressing Clostridium difficile infection (CDI), Crohn’s disease (CD) ulcerative colitis (UC), pouchitis, and irritable bowel syndrome (IBS), the guidance supports FMT for the prevention of recurrent CDI but not for inflammatory bowel disease (IBD) or IBS — outside of clinical trials.
The AGA’s recommendations were published in Gastroenterology.
“Fecal microbiota–based therapies are effective therapy to prevent recurrent C. difficile in select patients,” the AGA guideline states. “Conventional fecal microbiota transplant is an adjuvant treatment for select adults hospitalized with severe or fulminant C. difficile infection not responding to standard of care antibiotics. Fecal microbiota transplant cannot yet be recommended in other gastrointestinal conditions.”
“We thought it was important to write this guideline because of the growing number of trials of FMT in IBD and IBS populations. It was also important with the new FDA-approved treatments on the market,” the guideline’s first author, Anne F. Peery, MD, MSCR, AGAF, told this news organization, noting that the recently approved products did not yield better results than those of conventional rectal FMT. “The guidelines will help clinicians understand the available therapies and how to use these treatments,” added Dr. Peery, associate professor in the Division of Gastroenterology and Hepatology at the University of North Carolina School of Medicine in Chapel Hill.
Although the existing evidence is of low or very low certainty, Dr. Peery acknowledged, gastroenterologists “should be comfortable with conventional FMT and also the new FDA-approved products. We spent a considerable amount of time developing implementation considerations, which is practical advice to help clinicians use the guideline recommendations.”
Designed to counteract intestinal dysbiosis and restore protective gut flora, the FMT approach includes conventional, colonoscopically delivered donor stool transplants as well as two newly approved options: rectally given fecal microbiota (live-jslm/ Rebyota) and most recently, orally delivered fecal microbiota spores (live-brpk/ Vowst).
The AGA urges careful pretreatment consideration for patients who require frequent antibiotics or long-term antibiotic prophylaxis since ongoing antibiotics may diminish the efficacy of FMT.
The guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation framework to prioritize clinical questions, identify patient-centered outcomes, and conduct an evidence synthesis, followed by the Evidence-to-Decision framework to develop recommendations for these therapies and algorithms for their implementation into clinical practice.
Recommendations
The eight-member panel suggested the following practices on behalf of the AGA Clinical Guidelines Committee:
- In immunocompetent adults with recurrent CDI, select use of FMT can be used after completion of standard-of-care antibiotics to prevent recurrence. It can be considered after the second recurrence (episode 3) of CDI or in select patients at high risk for either recurrent CDI or a morbid CDI recurrence. Recurrent CDI is defined as clinically significant diarrhea ≥ 3 unformed stools in 24 hours with a confirmatory positive test within 8 weeks of completing antibiotics. Select use includes patients who have recovered from severe, fulminant, or particularly treatment-refractory CDI and patients with significant comorbidities. Severe CDI involves a leukocyte count of ≥15 × 109 cells/L and/or creatinine ≥1.5 mg/dL, while fulminant CDI involves shock, ileus, or megacolon and can be fatal.
- In mildly or moderately immunocompromised adults with recurrent CDI, the guidance recommends select use of conventional fecal microbiota transplant.
- In severely immunocompromised adults or those undergoing cytotoxic treatment, the AGA advises against the use of any fecal microbiota-based therapies to prevent recurrent CDI.
- Conventional FMT is not advised in patients who have bowel perforation or obstruction or are severely immunocompromised.
- For CDI patients not interested in FMT, reasonable alternatives to prevent recurrence are a vancomycin taper, tapered-pulsed fidaxomicin, or bezlotoxumab.
- In adults hospitalized with severe or fulminant CDI not responding to standard-of-care antibiotics, the AGA recommends select use of conventional FM transplant.
- In the current absence of evidence, the guidance advises against the use of conventional fecal microbiota transplant as treatment for IBD or IBS except in the context of clinical trials.
“We felt the data for using FMT in the treatment of UC was promising, but there is still a lot more work to be done in IBD and IBS,” Dr. Peery said. For each disease section the guideline outlined directions for future research. It will be updated in 3-5 years as more evidence becomes available.
This guideline was fully funded by the AGA Institute. Dr. Peery and fellow panel member Dr. Benjamin Lebwohl are supported by grants the National Institute of Diabetes and Digestive and Kidney Diseases. Panel member Colleen R. Kelly, MD, is supported by the National Institute of Allergy and Infectious Diseases.
None of the panel members had any conflicts of interest to report.
Addressing Clostridium difficile infection (CDI), Crohn’s disease (CD) ulcerative colitis (UC), pouchitis, and irritable bowel syndrome (IBS), the guidance supports FMT for the prevention of recurrent CDI but not for inflammatory bowel disease (IBD) or IBS — outside of clinical trials.
The AGA’s recommendations were published in Gastroenterology.
“Fecal microbiota–based therapies are effective therapy to prevent recurrent C. difficile in select patients,” the AGA guideline states. “Conventional fecal microbiota transplant is an adjuvant treatment for select adults hospitalized with severe or fulminant C. difficile infection not responding to standard of care antibiotics. Fecal microbiota transplant cannot yet be recommended in other gastrointestinal conditions.”
“We thought it was important to write this guideline because of the growing number of trials of FMT in IBD and IBS populations. It was also important with the new FDA-approved treatments on the market,” the guideline’s first author, Anne F. Peery, MD, MSCR, AGAF, told this news organization, noting that the recently approved products did not yield better results than those of conventional rectal FMT. “The guidelines will help clinicians understand the available therapies and how to use these treatments,” added Dr. Peery, associate professor in the Division of Gastroenterology and Hepatology at the University of North Carolina School of Medicine in Chapel Hill.
Although the existing evidence is of low or very low certainty, Dr. Peery acknowledged, gastroenterologists “should be comfortable with conventional FMT and also the new FDA-approved products. We spent a considerable amount of time developing implementation considerations, which is practical advice to help clinicians use the guideline recommendations.”
Designed to counteract intestinal dysbiosis and restore protective gut flora, the FMT approach includes conventional, colonoscopically delivered donor stool transplants as well as two newly approved options: rectally given fecal microbiota (live-jslm/ Rebyota) and most recently, orally delivered fecal microbiota spores (live-brpk/ Vowst).
The AGA urges careful pretreatment consideration for patients who require frequent antibiotics or long-term antibiotic prophylaxis since ongoing antibiotics may diminish the efficacy of FMT.
The guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation framework to prioritize clinical questions, identify patient-centered outcomes, and conduct an evidence synthesis, followed by the Evidence-to-Decision framework to develop recommendations for these therapies and algorithms for their implementation into clinical practice.
Recommendations
The eight-member panel suggested the following practices on behalf of the AGA Clinical Guidelines Committee:
- In immunocompetent adults with recurrent CDI, select use of FMT can be used after completion of standard-of-care antibiotics to prevent recurrence. It can be considered after the second recurrence (episode 3) of CDI or in select patients at high risk for either recurrent CDI or a morbid CDI recurrence. Recurrent CDI is defined as clinically significant diarrhea ≥ 3 unformed stools in 24 hours with a confirmatory positive test within 8 weeks of completing antibiotics. Select use includes patients who have recovered from severe, fulminant, or particularly treatment-refractory CDI and patients with significant comorbidities. Severe CDI involves a leukocyte count of ≥15 × 109 cells/L and/or creatinine ≥1.5 mg/dL, while fulminant CDI involves shock, ileus, or megacolon and can be fatal.
- In mildly or moderately immunocompromised adults with recurrent CDI, the guidance recommends select use of conventional fecal microbiota transplant.
- In severely immunocompromised adults or those undergoing cytotoxic treatment, the AGA advises against the use of any fecal microbiota-based therapies to prevent recurrent CDI.
- Conventional FMT is not advised in patients who have bowel perforation or obstruction or are severely immunocompromised.
- For CDI patients not interested in FMT, reasonable alternatives to prevent recurrence are a vancomycin taper, tapered-pulsed fidaxomicin, or bezlotoxumab.
- In adults hospitalized with severe or fulminant CDI not responding to standard-of-care antibiotics, the AGA recommends select use of conventional FM transplant.
- In the current absence of evidence, the guidance advises against the use of conventional fecal microbiota transplant as treatment for IBD or IBS except in the context of clinical trials.
“We felt the data for using FMT in the treatment of UC was promising, but there is still a lot more work to be done in IBD and IBS,” Dr. Peery said. For each disease section the guideline outlined directions for future research. It will be updated in 3-5 years as more evidence becomes available.
This guideline was fully funded by the AGA Institute. Dr. Peery and fellow panel member Dr. Benjamin Lebwohl are supported by grants the National Institute of Diabetes and Digestive and Kidney Diseases. Panel member Colleen R. Kelly, MD, is supported by the National Institute of Allergy and Infectious Diseases.
None of the panel members had any conflicts of interest to report.
FROM GASTROENTEROLOGY
Global Meta-Analysis: 1 in 12 Adults May Have Fecal Incontinence
FI is more common among individuals 60 years and older, yet a considerable portion of younger people — almost 5% — may also suffer from FI, reported Isabelle Mack, PhD, of University Medical Hospital, Tübingen, Germany, and colleagues.
“Clinicians’ understanding of the prevalence and risk factors for FI have evolved with time,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Initially, FI was regarded as a symptom that predominantly affected older people, especially nursing home residents. Its prevalence among community-dwelling adults was underrecognized, possibly because persons with FI were hesitant to even disclose that they were symptomatic. Now, we recognize that FI is common in the community.”
The only previous meta-analysis of FI, published in 2006, included both community and noncommunity studies, and reported an FI prevalence of 4.3%. Two subsequent reviews put the median prevalence at 7.7%, yet neither offered geographic insights.
To address this knowledge gap, Dr. Mack and colleagues conducted a meta-analysis of 80 studies involving 548,316 community-dwelling teenagers and adults. The median response rate across the studies was 66%.
Evaluating these data revealed a pooled global prevalence of FI was 8.0%, with a lower rate of 5.4% when FI was confined to Rome criteria.
“Placed in perspective, the 8.0% prevalence of FI is lower than or similar to the global prevalence of IBS, as assessed by a meta-regression (11.2%) and by a systematic review (8.8%) using pre–Rome IV criteria, and it is twofold greater than the IBS prevalence assessed with Rome IV criteria,” the investigators wrote.
Among individuals aged 60 years and older, the FI prevalence was 9.3%, compared with 4.9% for younger people (odds ratio [OR], 1.75; 95% CI, 1.39-2.20).
“These differences are at least partly explained by age-associated declines in anorectal function (e.g., lower anal resting pressure and rectal distensibility, denervation of the external anal sphincter),” the investigators wrote.
FI was also significantly more common among women than men (9.1% vs 7.4%; OR, 1.17; 95% CI, 1.06-1.28).
“Although these differences in FI prevalence between men and women seem relatively small, most patients with FI who seek medical attention are women (unpublished data),” the investigators wrote. “We suspect that men less commonly seek medical attention for FI because they may be secretly resigned to having FI, because FI may have less of an emotional impact on men, and because health literacy with regard to FI is lower for men.”
Geographically, prevalence of FI was highest in Australia and Oceania, followed by North America, Asia, and Europe. Data were insufficient to estimates rates in the Middle East and Africa.
Dr. Mack and colleagues concluded by noting how bothersome FI is for so many individuals worldwide, which should warrant closer attention from the medical community.
“Because nearly one in four community-dwelling women with FI report that the symptom has a moderate or severe impact on one or more domains of quality of life, more resources should be devoted to research in this area,” they wrote. “Future epidemiologic studies of FI should also assess the severity of FI, risk factors for FI, and the impact of FI on quality of life. In addition, because some patients are reluctant to acknowledge or discuss FI during an in-person interview, written or internet-based surveys may be preferable.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators disclosed no conflicts of interest.
Fecal incontinence (FI) is the GI disease that remains invisible to many except its sufferers. Even in the seemingly safe confines of a physician’s office, many patients won’t admit to providers that they suffer from this socially isolating condition. This systematic review and meta-analysis by Mack et al. — like other prevalence studies before it — serves as a useful reminder just how common this hidden disease remains. While FI is common in institutionalized persons, this study importantly found that 1 in 12 community-dwelling individuals worldwide suffer from FI as well.
What should the practicing clinician take away from this study? Simply put, when it comes to FI, you need to ask: how often, how much, how urgent (or passive), and what type (solid or liquid). This disease is far too common to remain in the shadows, yet most GI fellows do not receive sufficient training on a condition that is so widespread.
Kyle Staller, MD, MPH, is director, GI Motility Laboratory at Massachusetts General Hospital and Harvard Medical School, both in Boston. He has served as a consultant for Anji, Ardelyx, GI Supply, Mahana, and Restalsis, and received research support from Ardelyx.
Fecal incontinence (FI) is the GI disease that remains invisible to many except its sufferers. Even in the seemingly safe confines of a physician’s office, many patients won’t admit to providers that they suffer from this socially isolating condition. This systematic review and meta-analysis by Mack et al. — like other prevalence studies before it — serves as a useful reminder just how common this hidden disease remains. While FI is common in institutionalized persons, this study importantly found that 1 in 12 community-dwelling individuals worldwide suffer from FI as well.
What should the practicing clinician take away from this study? Simply put, when it comes to FI, you need to ask: how often, how much, how urgent (or passive), and what type (solid or liquid). This disease is far too common to remain in the shadows, yet most GI fellows do not receive sufficient training on a condition that is so widespread.
Kyle Staller, MD, MPH, is director, GI Motility Laboratory at Massachusetts General Hospital and Harvard Medical School, both in Boston. He has served as a consultant for Anji, Ardelyx, GI Supply, Mahana, and Restalsis, and received research support from Ardelyx.
Fecal incontinence (FI) is the GI disease that remains invisible to many except its sufferers. Even in the seemingly safe confines of a physician’s office, many patients won’t admit to providers that they suffer from this socially isolating condition. This systematic review and meta-analysis by Mack et al. — like other prevalence studies before it — serves as a useful reminder just how common this hidden disease remains. While FI is common in institutionalized persons, this study importantly found that 1 in 12 community-dwelling individuals worldwide suffer from FI as well.
What should the practicing clinician take away from this study? Simply put, when it comes to FI, you need to ask: how often, how much, how urgent (or passive), and what type (solid or liquid). This disease is far too common to remain in the shadows, yet most GI fellows do not receive sufficient training on a condition that is so widespread.
Kyle Staller, MD, MPH, is director, GI Motility Laboratory at Massachusetts General Hospital and Harvard Medical School, both in Boston. He has served as a consultant for Anji, Ardelyx, GI Supply, Mahana, and Restalsis, and received research support from Ardelyx.
FI is more common among individuals 60 years and older, yet a considerable portion of younger people — almost 5% — may also suffer from FI, reported Isabelle Mack, PhD, of University Medical Hospital, Tübingen, Germany, and colleagues.
“Clinicians’ understanding of the prevalence and risk factors for FI have evolved with time,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Initially, FI was regarded as a symptom that predominantly affected older people, especially nursing home residents. Its prevalence among community-dwelling adults was underrecognized, possibly because persons with FI were hesitant to even disclose that they were symptomatic. Now, we recognize that FI is common in the community.”
The only previous meta-analysis of FI, published in 2006, included both community and noncommunity studies, and reported an FI prevalence of 4.3%. Two subsequent reviews put the median prevalence at 7.7%, yet neither offered geographic insights.
To address this knowledge gap, Dr. Mack and colleagues conducted a meta-analysis of 80 studies involving 548,316 community-dwelling teenagers and adults. The median response rate across the studies was 66%.
Evaluating these data revealed a pooled global prevalence of FI was 8.0%, with a lower rate of 5.4% when FI was confined to Rome criteria.
“Placed in perspective, the 8.0% prevalence of FI is lower than or similar to the global prevalence of IBS, as assessed by a meta-regression (11.2%) and by a systematic review (8.8%) using pre–Rome IV criteria, and it is twofold greater than the IBS prevalence assessed with Rome IV criteria,” the investigators wrote.
Among individuals aged 60 years and older, the FI prevalence was 9.3%, compared with 4.9% for younger people (odds ratio [OR], 1.75; 95% CI, 1.39-2.20).
“These differences are at least partly explained by age-associated declines in anorectal function (e.g., lower anal resting pressure and rectal distensibility, denervation of the external anal sphincter),” the investigators wrote.
FI was also significantly more common among women than men (9.1% vs 7.4%; OR, 1.17; 95% CI, 1.06-1.28).
“Although these differences in FI prevalence between men and women seem relatively small, most patients with FI who seek medical attention are women (unpublished data),” the investigators wrote. “We suspect that men less commonly seek medical attention for FI because they may be secretly resigned to having FI, because FI may have less of an emotional impact on men, and because health literacy with regard to FI is lower for men.”
Geographically, prevalence of FI was highest in Australia and Oceania, followed by North America, Asia, and Europe. Data were insufficient to estimates rates in the Middle East and Africa.
Dr. Mack and colleagues concluded by noting how bothersome FI is for so many individuals worldwide, which should warrant closer attention from the medical community.
“Because nearly one in four community-dwelling women with FI report that the symptom has a moderate or severe impact on one or more domains of quality of life, more resources should be devoted to research in this area,” they wrote. “Future epidemiologic studies of FI should also assess the severity of FI, risk factors for FI, and the impact of FI on quality of life. In addition, because some patients are reluctant to acknowledge or discuss FI during an in-person interview, written or internet-based surveys may be preferable.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators disclosed no conflicts of interest.
FI is more common among individuals 60 years and older, yet a considerable portion of younger people — almost 5% — may also suffer from FI, reported Isabelle Mack, PhD, of University Medical Hospital, Tübingen, Germany, and colleagues.
“Clinicians’ understanding of the prevalence and risk factors for FI have evolved with time,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Initially, FI was regarded as a symptom that predominantly affected older people, especially nursing home residents. Its prevalence among community-dwelling adults was underrecognized, possibly because persons with FI were hesitant to even disclose that they were symptomatic. Now, we recognize that FI is common in the community.”
The only previous meta-analysis of FI, published in 2006, included both community and noncommunity studies, and reported an FI prevalence of 4.3%. Two subsequent reviews put the median prevalence at 7.7%, yet neither offered geographic insights.
To address this knowledge gap, Dr. Mack and colleagues conducted a meta-analysis of 80 studies involving 548,316 community-dwelling teenagers and adults. The median response rate across the studies was 66%.
Evaluating these data revealed a pooled global prevalence of FI was 8.0%, with a lower rate of 5.4% when FI was confined to Rome criteria.
“Placed in perspective, the 8.0% prevalence of FI is lower than or similar to the global prevalence of IBS, as assessed by a meta-regression (11.2%) and by a systematic review (8.8%) using pre–Rome IV criteria, and it is twofold greater than the IBS prevalence assessed with Rome IV criteria,” the investigators wrote.
Among individuals aged 60 years and older, the FI prevalence was 9.3%, compared with 4.9% for younger people (odds ratio [OR], 1.75; 95% CI, 1.39-2.20).
“These differences are at least partly explained by age-associated declines in anorectal function (e.g., lower anal resting pressure and rectal distensibility, denervation of the external anal sphincter),” the investigators wrote.
FI was also significantly more common among women than men (9.1% vs 7.4%; OR, 1.17; 95% CI, 1.06-1.28).
“Although these differences in FI prevalence between men and women seem relatively small, most patients with FI who seek medical attention are women (unpublished data),” the investigators wrote. “We suspect that men less commonly seek medical attention for FI because they may be secretly resigned to having FI, because FI may have less of an emotional impact on men, and because health literacy with regard to FI is lower for men.”
Geographically, prevalence of FI was highest in Australia and Oceania, followed by North America, Asia, and Europe. Data were insufficient to estimates rates in the Middle East and Africa.
Dr. Mack and colleagues concluded by noting how bothersome FI is for so many individuals worldwide, which should warrant closer attention from the medical community.
“Because nearly one in four community-dwelling women with FI report that the symptom has a moderate or severe impact on one or more domains of quality of life, more resources should be devoted to research in this area,” they wrote. “Future epidemiologic studies of FI should also assess the severity of FI, risk factors for FI, and the impact of FI on quality of life. In addition, because some patients are reluctant to acknowledge or discuss FI during an in-person interview, written or internet-based surveys may be preferable.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators disclosed no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
The Paradox of Achalasia Symptoms
In contrast to most diseases, as achalasia progresses, the symptoms improve. Specifically, reduction of symptoms of dysphagia lulls the gastroenterologist into thinking their patients are doing well.
This improvement in dysphagia is likely due to two mechanisms. The first is that as the esophagus dilates, there is a greater capacity for food accumulation before sensation occurs. Whether this is completely a volume issue or whether there is a contribution from increased esophageal body distensibility is unclear. Similarly, as achalasia results from inflammation and destruction of the motor neurons of the myenteric plexus, sensory neurons are also damaged. As a result, the patient’s ability to sense food retention lessens. To some degree, this explains the phenomenon of patients presenting with megaesophagus; after years of initially diminishing or stable symptoms managed with patient accommodation, patients present with end-stage disease manifested by a food-impacted esophagus, nocturnal aspiration, and weight loss.
This aspect of the natural history of achalasia has led esophagologists to follow patients with achalasia after treatment at regular intervals with objective examinations such as timed esophagography to mitigate against this worsening yet symptomatically stable course.
Dr. Katzka is based in the Division of Digestive and Liver Diseases, Columbia University Medical Center, New York. He receives research support from Medtronic and is an associate editor for GI & Hepatology News. Previously published in Gastro Hep Advances. 2024 Jan 19. doi: 10.1016/j.gastha.2024.01.006.
In contrast to most diseases, as achalasia progresses, the symptoms improve. Specifically, reduction of symptoms of dysphagia lulls the gastroenterologist into thinking their patients are doing well.
This improvement in dysphagia is likely due to two mechanisms. The first is that as the esophagus dilates, there is a greater capacity for food accumulation before sensation occurs. Whether this is completely a volume issue or whether there is a contribution from increased esophageal body distensibility is unclear. Similarly, as achalasia results from inflammation and destruction of the motor neurons of the myenteric plexus, sensory neurons are also damaged. As a result, the patient’s ability to sense food retention lessens. To some degree, this explains the phenomenon of patients presenting with megaesophagus; after years of initially diminishing or stable symptoms managed with patient accommodation, patients present with end-stage disease manifested by a food-impacted esophagus, nocturnal aspiration, and weight loss.
This aspect of the natural history of achalasia has led esophagologists to follow patients with achalasia after treatment at regular intervals with objective examinations such as timed esophagography to mitigate against this worsening yet symptomatically stable course.
Dr. Katzka is based in the Division of Digestive and Liver Diseases, Columbia University Medical Center, New York. He receives research support from Medtronic and is an associate editor for GI & Hepatology News. Previously published in Gastro Hep Advances. 2024 Jan 19. doi: 10.1016/j.gastha.2024.01.006.
In contrast to most diseases, as achalasia progresses, the symptoms improve. Specifically, reduction of symptoms of dysphagia lulls the gastroenterologist into thinking their patients are doing well.
This improvement in dysphagia is likely due to two mechanisms. The first is that as the esophagus dilates, there is a greater capacity for food accumulation before sensation occurs. Whether this is completely a volume issue or whether there is a contribution from increased esophageal body distensibility is unclear. Similarly, as achalasia results from inflammation and destruction of the motor neurons of the myenteric plexus, sensory neurons are also damaged. As a result, the patient’s ability to sense food retention lessens. To some degree, this explains the phenomenon of patients presenting with megaesophagus; after years of initially diminishing or stable symptoms managed with patient accommodation, patients present with end-stage disease manifested by a food-impacted esophagus, nocturnal aspiration, and weight loss.
This aspect of the natural history of achalasia has led esophagologists to follow patients with achalasia after treatment at regular intervals with objective examinations such as timed esophagography to mitigate against this worsening yet symptomatically stable course.
Dr. Katzka is based in the Division of Digestive and Liver Diseases, Columbia University Medical Center, New York. He receives research support from Medtronic and is an associate editor for GI & Hepatology News. Previously published in Gastro Hep Advances. 2024 Jan 19. doi: 10.1016/j.gastha.2024.01.006.
AGA Guides Usage of GLP-1 Receptor Agonists Before Endoscopy
The American Gastroenterological Association (AGA) has issued a rapid clinical practice update on the use of glucagon-like peptide 1 (GLP-1) receptor agonists prior to endoscopy.
The update was partly prompted by consensus-based perioperative guidance issued by the American Society of Anesthesiologists in June 2023, which advises withholding GLP-1 receptor agonists before endoscopy. This recommendation has caused some anesthesia providers to cancel or postpone endoscopic procedures, or even elect general endotracheal intubation over standard sedation.
“Many facilities and medical centers are now struggling to revise preprocedural protocols for patients taking this class of medications despite the lack of high-level evidence regarding how to proceed,” the panelists wrote in Clinical Gastroenterology and Hepatology. “Important questions include whether these preprocedural changes are necessary, if they truly mitigate periprocedural aspiration, or if the delays instituted by following this guidance might further compound the major problem currently faced nationwide: that of large numbers of patients awaiting endoscopic procedures because of delays from the COVID-19 pandemic, reduction in the recommended age threshold to start colorectal cancer screening in 2018, and workforce challenges.”
The rapid clinical practice update, commissioned and approved by the AGA, includes background on the relationship between GLP-1 receptor agonists and endoscopic procedures, followed by clinical strategies for patients taking these medications.
Lead panelist Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues began by noting that GLP-1 receptor agonists have been associated with increased gastric residue in patients with diabetes, and among nondiabetic patients, increased gastric retention of solids but not liquids. Delayed gastric emptying and increased residual gastric contents may be more common among patients on GLP-1 agonists who have vomiting, nausea, dyspepsia, or abdominal bloating, they added.
The above findings “imply an increased risk of aspiration in patients receiving GLP-1 receptor agonist medications who present for procedures that require sedation,” the panelists wrote, but more data is needed to support this hypothesis.
Yet the implications for endoscopic risk are still unclear.
Residual liquid in the stomach, at least, is “less of an issue,” according to the update, since “it is easily removed during an esophagogastroduodenoscopy, and this is the first maneuver performed by endoscopists on entering the stomach.”
While residual solids in the stomach could theoretically increase risk of aspiration, other patients with gastroparesis, such as those taking opioids, are not routinely given “special dietary precautions or medication adjustments” prior to endoscopy, Dr. Al Hashash and colleagues wrote. Even patients with severe gastroparesis who are undergoing gastric peroral endoscopic myotomy (which depends upon an empty stomach), are only required to stop ingesting solid foods the day before the procedure, they noted.
“It is appropriate that the ASA’s perioperative suggestions for patients on GLP-1 [receptor agonists] are labeled ‘consensus-based guidance on perioperative management,’ because there is clearly insufficient published evidence for a robust systematic review and guideline,” they wrote. “As such, the ASA’s suggestions are expert opinions, which may inform but should not replace clinical judgment.”
, for whom withholding these medications “might provide more risk than benefit.”
Withholding GLP-1 receptor agonists may be safe and reasonable for patients taking them solely for weight loss, but “this should not be considered mandatory or evidence-based,” as it remains unclear whether withholding one dose is enough to restore normal gastric motility.
“Generally, in patients on GLP-1 receptor agonists who have followed standard perioperative procedures (typically an 8-hour solid-food fast and a 2-hour liquid fast) and who do not have symptoms of nausea, vomiting, dyspepsia, or abdominal distention, we advise proceeding with upper and/or lower endoscopy,” the panelists concluded.
The rapid clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Apollo Endosurgery, Medtronic, Boston Scientific, and others.
The American Gastroenterological Association (AGA) has issued a rapid clinical practice update on the use of glucagon-like peptide 1 (GLP-1) receptor agonists prior to endoscopy.
The update was partly prompted by consensus-based perioperative guidance issued by the American Society of Anesthesiologists in June 2023, which advises withholding GLP-1 receptor agonists before endoscopy. This recommendation has caused some anesthesia providers to cancel or postpone endoscopic procedures, or even elect general endotracheal intubation over standard sedation.
“Many facilities and medical centers are now struggling to revise preprocedural protocols for patients taking this class of medications despite the lack of high-level evidence regarding how to proceed,” the panelists wrote in Clinical Gastroenterology and Hepatology. “Important questions include whether these preprocedural changes are necessary, if they truly mitigate periprocedural aspiration, or if the delays instituted by following this guidance might further compound the major problem currently faced nationwide: that of large numbers of patients awaiting endoscopic procedures because of delays from the COVID-19 pandemic, reduction in the recommended age threshold to start colorectal cancer screening in 2018, and workforce challenges.”
The rapid clinical practice update, commissioned and approved by the AGA, includes background on the relationship between GLP-1 receptor agonists and endoscopic procedures, followed by clinical strategies for patients taking these medications.
Lead panelist Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues began by noting that GLP-1 receptor agonists have been associated with increased gastric residue in patients with diabetes, and among nondiabetic patients, increased gastric retention of solids but not liquids. Delayed gastric emptying and increased residual gastric contents may be more common among patients on GLP-1 agonists who have vomiting, nausea, dyspepsia, or abdominal bloating, they added.
The above findings “imply an increased risk of aspiration in patients receiving GLP-1 receptor agonist medications who present for procedures that require sedation,” the panelists wrote, but more data is needed to support this hypothesis.
Yet the implications for endoscopic risk are still unclear.
Residual liquid in the stomach, at least, is “less of an issue,” according to the update, since “it is easily removed during an esophagogastroduodenoscopy, and this is the first maneuver performed by endoscopists on entering the stomach.”
While residual solids in the stomach could theoretically increase risk of aspiration, other patients with gastroparesis, such as those taking opioids, are not routinely given “special dietary precautions or medication adjustments” prior to endoscopy, Dr. Al Hashash and colleagues wrote. Even patients with severe gastroparesis who are undergoing gastric peroral endoscopic myotomy (which depends upon an empty stomach), are only required to stop ingesting solid foods the day before the procedure, they noted.
“It is appropriate that the ASA’s perioperative suggestions for patients on GLP-1 [receptor agonists] are labeled ‘consensus-based guidance on perioperative management,’ because there is clearly insufficient published evidence for a robust systematic review and guideline,” they wrote. “As such, the ASA’s suggestions are expert opinions, which may inform but should not replace clinical judgment.”
, for whom withholding these medications “might provide more risk than benefit.”
Withholding GLP-1 receptor agonists may be safe and reasonable for patients taking them solely for weight loss, but “this should not be considered mandatory or evidence-based,” as it remains unclear whether withholding one dose is enough to restore normal gastric motility.
“Generally, in patients on GLP-1 receptor agonists who have followed standard perioperative procedures (typically an 8-hour solid-food fast and a 2-hour liquid fast) and who do not have symptoms of nausea, vomiting, dyspepsia, or abdominal distention, we advise proceeding with upper and/or lower endoscopy,” the panelists concluded.
The rapid clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Apollo Endosurgery, Medtronic, Boston Scientific, and others.
The American Gastroenterological Association (AGA) has issued a rapid clinical practice update on the use of glucagon-like peptide 1 (GLP-1) receptor agonists prior to endoscopy.
The update was partly prompted by consensus-based perioperative guidance issued by the American Society of Anesthesiologists in June 2023, which advises withholding GLP-1 receptor agonists before endoscopy. This recommendation has caused some anesthesia providers to cancel or postpone endoscopic procedures, or even elect general endotracheal intubation over standard sedation.
“Many facilities and medical centers are now struggling to revise preprocedural protocols for patients taking this class of medications despite the lack of high-level evidence regarding how to proceed,” the panelists wrote in Clinical Gastroenterology and Hepatology. “Important questions include whether these preprocedural changes are necessary, if they truly mitigate periprocedural aspiration, or if the delays instituted by following this guidance might further compound the major problem currently faced nationwide: that of large numbers of patients awaiting endoscopic procedures because of delays from the COVID-19 pandemic, reduction in the recommended age threshold to start colorectal cancer screening in 2018, and workforce challenges.”
The rapid clinical practice update, commissioned and approved by the AGA, includes background on the relationship between GLP-1 receptor agonists and endoscopic procedures, followed by clinical strategies for patients taking these medications.
Lead panelist Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues began by noting that GLP-1 receptor agonists have been associated with increased gastric residue in patients with diabetes, and among nondiabetic patients, increased gastric retention of solids but not liquids. Delayed gastric emptying and increased residual gastric contents may be more common among patients on GLP-1 agonists who have vomiting, nausea, dyspepsia, or abdominal bloating, they added.
The above findings “imply an increased risk of aspiration in patients receiving GLP-1 receptor agonist medications who present for procedures that require sedation,” the panelists wrote, but more data is needed to support this hypothesis.
Yet the implications for endoscopic risk are still unclear.
Residual liquid in the stomach, at least, is “less of an issue,” according to the update, since “it is easily removed during an esophagogastroduodenoscopy, and this is the first maneuver performed by endoscopists on entering the stomach.”
While residual solids in the stomach could theoretically increase risk of aspiration, other patients with gastroparesis, such as those taking opioids, are not routinely given “special dietary precautions or medication adjustments” prior to endoscopy, Dr. Al Hashash and colleagues wrote. Even patients with severe gastroparesis who are undergoing gastric peroral endoscopic myotomy (which depends upon an empty stomach), are only required to stop ingesting solid foods the day before the procedure, they noted.
“It is appropriate that the ASA’s perioperative suggestions for patients on GLP-1 [receptor agonists] are labeled ‘consensus-based guidance on perioperative management,’ because there is clearly insufficient published evidence for a robust systematic review and guideline,” they wrote. “As such, the ASA’s suggestions are expert opinions, which may inform but should not replace clinical judgment.”
, for whom withholding these medications “might provide more risk than benefit.”
Withholding GLP-1 receptor agonists may be safe and reasonable for patients taking them solely for weight loss, but “this should not be considered mandatory or evidence-based,” as it remains unclear whether withholding one dose is enough to restore normal gastric motility.
“Generally, in patients on GLP-1 receptor agonists who have followed standard perioperative procedures (typically an 8-hour solid-food fast and a 2-hour liquid fast) and who do not have symptoms of nausea, vomiting, dyspepsia, or abdominal distention, we advise proceeding with upper and/or lower endoscopy,” the panelists concluded.
The rapid clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Apollo Endosurgery, Medtronic, Boston Scientific, and others.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA Offers Practical Advice on IBD Diets
.
The new guidance, authored by Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues, includes 12 best practices that address dietary options, enteral and parenteral nutrition, patient monitoring, and the need for multidisciplinary care.
“There is growing recognition of the role of diet in the care of patients with IBD, as both an etiopathogenic risk factor and, more recently, as a disease-modifying modality,” the update panelists wrote in Gastroenterology.
Historically, they noted, patients with IBD had been advised to avoid many different foods including fiber, but this strategy may result in unintended consequences.
“[T]hese approaches frequently led patients with IBD to avoid what are traditionally considered healthy foods, even after achieving clinical remission,” Dr. Al Hashash and colleagues wrote.
With an increasing body of data available for dietary interventions in both Crohn’s disease and ulcerative colitis, they wrote the present clinical practice update to offer some needed clarity.
A Starting Point
First, the panelists advise that, unless contraindicated, all patients with IBD follow a Mediterranean diet while minimizing salt, sugar, and ultraprocessed foods.
Patients with symptomatic intestinal strictures may struggle to digest raw fruits and vegetables due to their fibrous nature, they added, so these patients should first soften these foods through cooking, steaming, or “careful chewing” before consumption.
“No diet has consistently been found to decrease the rate of flares in adults with IBD,” the update panelists noted. “A diet low in red and processed meat may reduce ulcerative colitis flares, but has not been found to reduce relapse in Crohn’s disease.”
Beyond these dietary suggestions for adults, the update advises breastfeeding for newborns and a Mediterranean diet for children, as both may reduce risk of developing IBD.
Enteral Nutrition
The update suggests that exclusive enteral nutrition is a reasonable option to induce clinical remission and endoscopic response, or as a steroid-sparing bridge, in Crohn’s disease, although this may be more effective in children than adults.
Malnourished patients may also benefit from exclusive enteral nutrition prior to elective surgery for Crohn’s disease, Dr. Al Hashash and colleagues added, as this strategy can “optimize nutritional status and reduce postoperative complications.”
A Crohn’s disease exclusion diet, which involves partial enteral nutrition therapy, may be considered in mild or moderate cases, according to the update.
“Data on the use of enteral nutrition in the treatment of active ulcerative colitis are limited,” the panelists wrote, although early data suggest it is safe and well tolerated, and can improve prealbumin levels.
Parenteral Nutrition
The update recommends short-term parenteral nutrition for patients with phlegmonous inflammation and/or an intra-abdominal abscess, as this can act as a bridge to surgical intervention.
Patients with prolonged ileus, short bowel syndrome, or high-output gastrointestinal fistula may also be candidates for parenteral nutrition, as well as those who have tried and failed both oral and enteral nutrition.
Lastly, the update encourages transition from long-term parenteral nutrition to oral intake and customized hydration management “whenever possible.”
Monitoring and Multidisciplinary Care
Dr. Al Hashash and colleagues concluded by advising that all patients with complicated IBD be comanaged by a gastroenterologist and a registered dietitian, both of whom should remain watchful for signs of malnutrition.
Using serum protein as a surrogate marker of malnutrition is no longer recommended and there are different criteria that should be utilized to identify malnutrition. Routine iron and vitamin D testing are warranted, as well as B12 testing for patients with extensive ileal disease or a history of ileal surgery.
This clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Merck, Celgene, Janssen, and others.
.
The new guidance, authored by Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues, includes 12 best practices that address dietary options, enteral and parenteral nutrition, patient monitoring, and the need for multidisciplinary care.
“There is growing recognition of the role of diet in the care of patients with IBD, as both an etiopathogenic risk factor and, more recently, as a disease-modifying modality,” the update panelists wrote in Gastroenterology.
Historically, they noted, patients with IBD had been advised to avoid many different foods including fiber, but this strategy may result in unintended consequences.
“[T]hese approaches frequently led patients with IBD to avoid what are traditionally considered healthy foods, even after achieving clinical remission,” Dr. Al Hashash and colleagues wrote.
With an increasing body of data available for dietary interventions in both Crohn’s disease and ulcerative colitis, they wrote the present clinical practice update to offer some needed clarity.
A Starting Point
First, the panelists advise that, unless contraindicated, all patients with IBD follow a Mediterranean diet while minimizing salt, sugar, and ultraprocessed foods.
Patients with symptomatic intestinal strictures may struggle to digest raw fruits and vegetables due to their fibrous nature, they added, so these patients should first soften these foods through cooking, steaming, or “careful chewing” before consumption.
“No diet has consistently been found to decrease the rate of flares in adults with IBD,” the update panelists noted. “A diet low in red and processed meat may reduce ulcerative colitis flares, but has not been found to reduce relapse in Crohn’s disease.”
Beyond these dietary suggestions for adults, the update advises breastfeeding for newborns and a Mediterranean diet for children, as both may reduce risk of developing IBD.
Enteral Nutrition
The update suggests that exclusive enteral nutrition is a reasonable option to induce clinical remission and endoscopic response, or as a steroid-sparing bridge, in Crohn’s disease, although this may be more effective in children than adults.
Malnourished patients may also benefit from exclusive enteral nutrition prior to elective surgery for Crohn’s disease, Dr. Al Hashash and colleagues added, as this strategy can “optimize nutritional status and reduce postoperative complications.”
A Crohn’s disease exclusion diet, which involves partial enteral nutrition therapy, may be considered in mild or moderate cases, according to the update.
“Data on the use of enteral nutrition in the treatment of active ulcerative colitis are limited,” the panelists wrote, although early data suggest it is safe and well tolerated, and can improve prealbumin levels.
Parenteral Nutrition
The update recommends short-term parenteral nutrition for patients with phlegmonous inflammation and/or an intra-abdominal abscess, as this can act as a bridge to surgical intervention.
Patients with prolonged ileus, short bowel syndrome, or high-output gastrointestinal fistula may also be candidates for parenteral nutrition, as well as those who have tried and failed both oral and enteral nutrition.
Lastly, the update encourages transition from long-term parenteral nutrition to oral intake and customized hydration management “whenever possible.”
Monitoring and Multidisciplinary Care
Dr. Al Hashash and colleagues concluded by advising that all patients with complicated IBD be comanaged by a gastroenterologist and a registered dietitian, both of whom should remain watchful for signs of malnutrition.
Using serum protein as a surrogate marker of malnutrition is no longer recommended and there are different criteria that should be utilized to identify malnutrition. Routine iron and vitamin D testing are warranted, as well as B12 testing for patients with extensive ileal disease or a history of ileal surgery.
This clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Merck, Celgene, Janssen, and others.
.
The new guidance, authored by Jana G. Al Hashash, MD, MSc, AGAF, of Mayo Clinic, Jacksonville, Florida, and colleagues, includes 12 best practices that address dietary options, enteral and parenteral nutrition, patient monitoring, and the need for multidisciplinary care.
“There is growing recognition of the role of diet in the care of patients with IBD, as both an etiopathogenic risk factor and, more recently, as a disease-modifying modality,” the update panelists wrote in Gastroenterology.
Historically, they noted, patients with IBD had been advised to avoid many different foods including fiber, but this strategy may result in unintended consequences.
“[T]hese approaches frequently led patients with IBD to avoid what are traditionally considered healthy foods, even after achieving clinical remission,” Dr. Al Hashash and colleagues wrote.
With an increasing body of data available for dietary interventions in both Crohn’s disease and ulcerative colitis, they wrote the present clinical practice update to offer some needed clarity.
A Starting Point
First, the panelists advise that, unless contraindicated, all patients with IBD follow a Mediterranean diet while minimizing salt, sugar, and ultraprocessed foods.
Patients with symptomatic intestinal strictures may struggle to digest raw fruits and vegetables due to their fibrous nature, they added, so these patients should first soften these foods through cooking, steaming, or “careful chewing” before consumption.
“No diet has consistently been found to decrease the rate of flares in adults with IBD,” the update panelists noted. “A diet low in red and processed meat may reduce ulcerative colitis flares, but has not been found to reduce relapse in Crohn’s disease.”
Beyond these dietary suggestions for adults, the update advises breastfeeding for newborns and a Mediterranean diet for children, as both may reduce risk of developing IBD.
Enteral Nutrition
The update suggests that exclusive enteral nutrition is a reasonable option to induce clinical remission and endoscopic response, or as a steroid-sparing bridge, in Crohn’s disease, although this may be more effective in children than adults.
Malnourished patients may also benefit from exclusive enteral nutrition prior to elective surgery for Crohn’s disease, Dr. Al Hashash and colleagues added, as this strategy can “optimize nutritional status and reduce postoperative complications.”
A Crohn’s disease exclusion diet, which involves partial enteral nutrition therapy, may be considered in mild or moderate cases, according to the update.
“Data on the use of enteral nutrition in the treatment of active ulcerative colitis are limited,” the panelists wrote, although early data suggest it is safe and well tolerated, and can improve prealbumin levels.
Parenteral Nutrition
The update recommends short-term parenteral nutrition for patients with phlegmonous inflammation and/or an intra-abdominal abscess, as this can act as a bridge to surgical intervention.
Patients with prolonged ileus, short bowel syndrome, or high-output gastrointestinal fistula may also be candidates for parenteral nutrition, as well as those who have tried and failed both oral and enteral nutrition.
Lastly, the update encourages transition from long-term parenteral nutrition to oral intake and customized hydration management “whenever possible.”
Monitoring and Multidisciplinary Care
Dr. Al Hashash and colleagues concluded by advising that all patients with complicated IBD be comanaged by a gastroenterologist and a registered dietitian, both of whom should remain watchful for signs of malnutrition.
Using serum protein as a surrogate marker of malnutrition is no longer recommended and there are different criteria that should be utilized to identify malnutrition. Routine iron and vitamin D testing are warranted, as well as B12 testing for patients with extensive ileal disease or a history of ileal surgery.
This clinical practice update was commissioned and approved by the AGA. The update panelists disclosed relationships with Merck, Celgene, Janssen, and others.
FROM GASTROENTEROLOGY
Real-World Dupilumab Wins in Treating Refractory EoE
Most patients achieved histologic, endoscopic, and symptom improvement with a median of 6 months’ treatment with the interleukin 4 and 13 blocker, and esophageal stricture diameter improved as well, according to a single-center retrospective study in Clinical Gastroenterology and Hepatology.
“Dupilumab has real-world efficacy for a severe EoE population, most of whom would not have qualified for prior clinical trials,” concluded gastroenterologists Christopher J. Lee, MD (lead author), and Evan S. Dellon, MD, MPH, AGAF, of the Center for Esophageal Diseases and Swallowing, at the University of North Carolina School of Medicine in Chapel Hill.
These real-world findings aligned with data from the group’s phase 3 clinical trial.
In addition, several case reports or series have highlighted the real-world efficacy of dupilumab, with a particular focus on pediatric patients and those with other atopic diseases.
“Despite nonresponse to prior treatments, these patients can likely expect to see results similar to what was seen in the clinical trial,” Dr. Dellon said in an interview. “However, it would be good to have similar confirmatory data from other centers, and I’m sure those data will be forthcoming as more EoE patients are treated with dupilumab.”
The placement of dupilumab in the EoE treatment algorithm is still actively being investigated. “While the phase 3 study led to [Food and Drug Administration] approval, it had strict inclusion and exclusion criteria, and some populations were ineligible,” he added. “In particular, the very severe EoE patients who either had a very narrow esophagus where the scope wouldn’t pass, or who had severe strictures and symptoms requiring esophageal dilation and who couldn’t go 6 to 12 months without dilation, couldn’t be enrolled. So the efficacy of dupilumab in this more severe group was not known.”
The group hypothesized that dupilumab would be effective in this population but did not know if the efficacy would be similar to that in the clinical trial. “The overall response rates, which were very similar to what were seen in the phase 3 trial, were surprising,“ Dr. Dellon said.”The other surprising finding was the increase in esophageal caliber, as measured by the size achieved with esophageal dilation.”
The study
The investigators identified 46 patients treated with dupilumab for refractory fibrostenotic EoE at the university’s medical center. All had failed or lost response to one or more standard therapies such as proton pump inhibitors, topical glucocorticosteroids, and a food elimination diet.
Previous treatments also included systemic steroids, cromolyn, ketotifen, montelukast, and 6-mercaptopurine, all with minimal response. Some 85% of patients had undergone an average of 9.0+ 7.0 pre-dupilumab dilations.
The biologic was initially prescribed off-label before FDA approval. Patients received it at a dose of 300 mg subcutaneously either fortnightly (n = 16) or weekly (n = 30), depending on insurance approval and timing of prescription. Length of treatment varied based on the time from prescription to first post-treatment evaluative endoscopy.
Patients showed endoscopic, histologic, and symptomatic improvement on dupilumab compared with both the worst and the pre-dupilumab esophagogastroduodenoscopies.
Among the specific findings:
- Peak eosinophil counts significantly decreased.
- Post-dupilumab histologic response rates were 80% and 57% for fewer than 15 eosinophils per high-power field, and 6 or fewer eosinophils per high-power field, respectively.
- The Endoscopic Reference Score decreased from 5.01 to 1.89 (P < .001 for all).
- Pre-dilation esophageal diameter increased from 13.9 to 16.0 mm (P < .001), although the proportion of strictures was stable.
- Global symptom improvement was reported in 91% of patients (P < .001).
Commenting on the study but not involved in it, David A. Katzka, MD, professor of medicine at Columbia University in New York City, said the findings would be of immediate use to practicing gastroenterologists.
“It’s necessary to do clinical trials, but real-world data make the clinician feel more comfortable in prescribing. Interestingly, I am seeing dupilumab being recommended not just for refractory disease but also as first-line therapy,” he said.
Dr. Dellon noted that the incidence and prevalence of EoE are rising rapidly in the US and around the world. “This increase is outpacing growing recognition of the disease,” he said. “Most likely, environmental factors are driving this change.” He called for studies to determine the long-term efficacy of dupilumab for this severe subgroup — and the potential benefit of moving dupilumab earlier into the treatment algorithm.
The latter is a controversial question, noted Dr. Katzka. “For patients with other indications such as asthma or eczema, dupilumab is the ideal medication,” he said. And it can be a first-line therapy if there are contraindications to alternatives or if compliance will be better with a once-weekly injection as opposed to a twice-daily medication or a food elimination diet. But overall, our more established therapies should be considered first.”
Dr. Katzka emphasized the need to further define EoE phenotypes in order to personalize therapy. “There’s likely a group of patients who should go straight to dupilumab, perhaps those marked by factors such as severity, progression, young age, or other atopic disorders. But we have yet to definitively identify this group.”
The authors reported no specific funding for this analysis. Dr. Dellon reported research funding and/or consulting fees from multiple pharmaceutical companies, including Regeneron/Sanofi, the developers of dupilumab. Dr. Lee had no competing interests to disclose. Dr. Katzka reported consulting for Medtronic, and is an associate editor for GI & Hepatology News.
Most patients achieved histologic, endoscopic, and symptom improvement with a median of 6 months’ treatment with the interleukin 4 and 13 blocker, and esophageal stricture diameter improved as well, according to a single-center retrospective study in Clinical Gastroenterology and Hepatology.
“Dupilumab has real-world efficacy for a severe EoE population, most of whom would not have qualified for prior clinical trials,” concluded gastroenterologists Christopher J. Lee, MD (lead author), and Evan S. Dellon, MD, MPH, AGAF, of the Center for Esophageal Diseases and Swallowing, at the University of North Carolina School of Medicine in Chapel Hill.
These real-world findings aligned with data from the group’s phase 3 clinical trial.
In addition, several case reports or series have highlighted the real-world efficacy of dupilumab, with a particular focus on pediatric patients and those with other atopic diseases.
“Despite nonresponse to prior treatments, these patients can likely expect to see results similar to what was seen in the clinical trial,” Dr. Dellon said in an interview. “However, it would be good to have similar confirmatory data from other centers, and I’m sure those data will be forthcoming as more EoE patients are treated with dupilumab.”
The placement of dupilumab in the EoE treatment algorithm is still actively being investigated. “While the phase 3 study led to [Food and Drug Administration] approval, it had strict inclusion and exclusion criteria, and some populations were ineligible,” he added. “In particular, the very severe EoE patients who either had a very narrow esophagus where the scope wouldn’t pass, or who had severe strictures and symptoms requiring esophageal dilation and who couldn’t go 6 to 12 months without dilation, couldn’t be enrolled. So the efficacy of dupilumab in this more severe group was not known.”
The group hypothesized that dupilumab would be effective in this population but did not know if the efficacy would be similar to that in the clinical trial. “The overall response rates, which were very similar to what were seen in the phase 3 trial, were surprising,“ Dr. Dellon said.”The other surprising finding was the increase in esophageal caliber, as measured by the size achieved with esophageal dilation.”
The study
The investigators identified 46 patients treated with dupilumab for refractory fibrostenotic EoE at the university’s medical center. All had failed or lost response to one or more standard therapies such as proton pump inhibitors, topical glucocorticosteroids, and a food elimination diet.
Previous treatments also included systemic steroids, cromolyn, ketotifen, montelukast, and 6-mercaptopurine, all with minimal response. Some 85% of patients had undergone an average of 9.0+ 7.0 pre-dupilumab dilations.
The biologic was initially prescribed off-label before FDA approval. Patients received it at a dose of 300 mg subcutaneously either fortnightly (n = 16) or weekly (n = 30), depending on insurance approval and timing of prescription. Length of treatment varied based on the time from prescription to first post-treatment evaluative endoscopy.
Patients showed endoscopic, histologic, and symptomatic improvement on dupilumab compared with both the worst and the pre-dupilumab esophagogastroduodenoscopies.
Among the specific findings:
- Peak eosinophil counts significantly decreased.
- Post-dupilumab histologic response rates were 80% and 57% for fewer than 15 eosinophils per high-power field, and 6 or fewer eosinophils per high-power field, respectively.
- The Endoscopic Reference Score decreased from 5.01 to 1.89 (P < .001 for all).
- Pre-dilation esophageal diameter increased from 13.9 to 16.0 mm (P < .001), although the proportion of strictures was stable.
- Global symptom improvement was reported in 91% of patients (P < .001).
Commenting on the study but not involved in it, David A. Katzka, MD, professor of medicine at Columbia University in New York City, said the findings would be of immediate use to practicing gastroenterologists.
“It’s necessary to do clinical trials, but real-world data make the clinician feel more comfortable in prescribing. Interestingly, I am seeing dupilumab being recommended not just for refractory disease but also as first-line therapy,” he said.
Dr. Dellon noted that the incidence and prevalence of EoE are rising rapidly in the US and around the world. “This increase is outpacing growing recognition of the disease,” he said. “Most likely, environmental factors are driving this change.” He called for studies to determine the long-term efficacy of dupilumab for this severe subgroup — and the potential benefit of moving dupilumab earlier into the treatment algorithm.
The latter is a controversial question, noted Dr. Katzka. “For patients with other indications such as asthma or eczema, dupilumab is the ideal medication,” he said. And it can be a first-line therapy if there are contraindications to alternatives or if compliance will be better with a once-weekly injection as opposed to a twice-daily medication or a food elimination diet. But overall, our more established therapies should be considered first.”
Dr. Katzka emphasized the need to further define EoE phenotypes in order to personalize therapy. “There’s likely a group of patients who should go straight to dupilumab, perhaps those marked by factors such as severity, progression, young age, or other atopic disorders. But we have yet to definitively identify this group.”
The authors reported no specific funding for this analysis. Dr. Dellon reported research funding and/or consulting fees from multiple pharmaceutical companies, including Regeneron/Sanofi, the developers of dupilumab. Dr. Lee had no competing interests to disclose. Dr. Katzka reported consulting for Medtronic, and is an associate editor for GI & Hepatology News.
Most patients achieved histologic, endoscopic, and symptom improvement with a median of 6 months’ treatment with the interleukin 4 and 13 blocker, and esophageal stricture diameter improved as well, according to a single-center retrospective study in Clinical Gastroenterology and Hepatology.
“Dupilumab has real-world efficacy for a severe EoE population, most of whom would not have qualified for prior clinical trials,” concluded gastroenterologists Christopher J. Lee, MD (lead author), and Evan S. Dellon, MD, MPH, AGAF, of the Center for Esophageal Diseases and Swallowing, at the University of North Carolina School of Medicine in Chapel Hill.
These real-world findings aligned with data from the group’s phase 3 clinical trial.
In addition, several case reports or series have highlighted the real-world efficacy of dupilumab, with a particular focus on pediatric patients and those with other atopic diseases.
“Despite nonresponse to prior treatments, these patients can likely expect to see results similar to what was seen in the clinical trial,” Dr. Dellon said in an interview. “However, it would be good to have similar confirmatory data from other centers, and I’m sure those data will be forthcoming as more EoE patients are treated with dupilumab.”
The placement of dupilumab in the EoE treatment algorithm is still actively being investigated. “While the phase 3 study led to [Food and Drug Administration] approval, it had strict inclusion and exclusion criteria, and some populations were ineligible,” he added. “In particular, the very severe EoE patients who either had a very narrow esophagus where the scope wouldn’t pass, or who had severe strictures and symptoms requiring esophageal dilation and who couldn’t go 6 to 12 months without dilation, couldn’t be enrolled. So the efficacy of dupilumab in this more severe group was not known.”
The group hypothesized that dupilumab would be effective in this population but did not know if the efficacy would be similar to that in the clinical trial. “The overall response rates, which were very similar to what were seen in the phase 3 trial, were surprising,“ Dr. Dellon said.”The other surprising finding was the increase in esophageal caliber, as measured by the size achieved with esophageal dilation.”
The study
The investigators identified 46 patients treated with dupilumab for refractory fibrostenotic EoE at the university’s medical center. All had failed or lost response to one or more standard therapies such as proton pump inhibitors, topical glucocorticosteroids, and a food elimination diet.
Previous treatments also included systemic steroids, cromolyn, ketotifen, montelukast, and 6-mercaptopurine, all with minimal response. Some 85% of patients had undergone an average of 9.0+ 7.0 pre-dupilumab dilations.
The biologic was initially prescribed off-label before FDA approval. Patients received it at a dose of 300 mg subcutaneously either fortnightly (n = 16) or weekly (n = 30), depending on insurance approval and timing of prescription. Length of treatment varied based on the time from prescription to first post-treatment evaluative endoscopy.
Patients showed endoscopic, histologic, and symptomatic improvement on dupilumab compared with both the worst and the pre-dupilumab esophagogastroduodenoscopies.
Among the specific findings:
- Peak eosinophil counts significantly decreased.
- Post-dupilumab histologic response rates were 80% and 57% for fewer than 15 eosinophils per high-power field, and 6 or fewer eosinophils per high-power field, respectively.
- The Endoscopic Reference Score decreased from 5.01 to 1.89 (P < .001 for all).
- Pre-dilation esophageal diameter increased from 13.9 to 16.0 mm (P < .001), although the proportion of strictures was stable.
- Global symptom improvement was reported in 91% of patients (P < .001).
Commenting on the study but not involved in it, David A. Katzka, MD, professor of medicine at Columbia University in New York City, said the findings would be of immediate use to practicing gastroenterologists.
“It’s necessary to do clinical trials, but real-world data make the clinician feel more comfortable in prescribing. Interestingly, I am seeing dupilumab being recommended not just for refractory disease but also as first-line therapy,” he said.
Dr. Dellon noted that the incidence and prevalence of EoE are rising rapidly in the US and around the world. “This increase is outpacing growing recognition of the disease,” he said. “Most likely, environmental factors are driving this change.” He called for studies to determine the long-term efficacy of dupilumab for this severe subgroup — and the potential benefit of moving dupilumab earlier into the treatment algorithm.
The latter is a controversial question, noted Dr. Katzka. “For patients with other indications such as asthma or eczema, dupilumab is the ideal medication,” he said. And it can be a first-line therapy if there are contraindications to alternatives or if compliance will be better with a once-weekly injection as opposed to a twice-daily medication or a food elimination diet. But overall, our more established therapies should be considered first.”
Dr. Katzka emphasized the need to further define EoE phenotypes in order to personalize therapy. “There’s likely a group of patients who should go straight to dupilumab, perhaps those marked by factors such as severity, progression, young age, or other atopic disorders. But we have yet to definitively identify this group.”
The authors reported no specific funding for this analysis. Dr. Dellon reported research funding and/or consulting fees from multiple pharmaceutical companies, including Regeneron/Sanofi, the developers of dupilumab. Dr. Lee had no competing interests to disclose. Dr. Katzka reported consulting for Medtronic, and is an associate editor for GI & Hepatology News.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
How to Optimize EHR Use in Gastroenterology Practices
, a new practice management article suggests.
Michelle Kang Kim, MD, PhD, AGAF, chair of gastroenterology at Cleveland Clinic, Ohio, and colleagues provide EHR improvement strategies and examples that can be adapted for use in a variety of gastroenterology clinic settings.
Their article, which was published online in Clinical Gastroenterology and Hepatology , includes the following suggestions, among others:
- Develop optimization teams. An example is SPRINT, a short, intensive team-based intervention at the University of Colorado Health, Aurora, Colorado, that developed specialty-specific tools, provided EHR efficiency training, and helped streamline workflows. The optimization project increased EHR satisfaction scores and reduced documentation time.
- Reroute low-acuity messages. Low-risk medication refills or appointment requests can be handled by nurses and medical assistants. This strategy has helped reduce the inbox burden.
- Create order sets for complex treatment dosing. One example is Cleveland Clinic’s Helicobacter pylori order set, which enables clinicians to quickly place orders with built-in dosages.
- Personalize EHR drop-down menus. Incorporate inflammatory bowel disease (IBD) severity scores, biopsy sampling, resection protocols, specimen container numbering, and other workflow-specific documentation into the EHR.
- Employ medical scribes. These professionals can serve as personal assistants, supporting care teams and reducing clinician documentation time. Alternatively, clinical support staff, such as nurses, can assist with documentation and messages, helping to reduce physician burnout. “These models could be particularly useful in GI specialties that require a multidisciplinary approach, for example, IBD and hepatology,” the authors write.
- Provide real-time training on best practices. There is no widely accepted EHR training curriculum for students, and experienced physicians face time constraints in learning new practices. Real-time training can help clinicians at all levels optimize their time outside the clinic.
In addition, the authors addressed novel tools and strategies that have been recently deployed and/or are in development, which are based largely on artificial intelligence (AI), natural language processing, and speech recognition. For now, these tools are digitizing data to help automate some EHR tasks, supporting communications with patients, and assisting in clinical decision making.
However, the authors note that although current optimization tools are promising, “there is still a lack of knowledge about their usability and effects on provider and patient well-being. More research is needed to evaluate current methodologies and design intelligent tools for the future that will help GI providers overcome the EHR-related obstacles specific to our field and harness the enormous potential of AI in optimizing the busy GI practice.”
This work received no external funding, and the authors disclosed no conflicts.
A version of this article appeared on Medscape.com.
, a new practice management article suggests.
Michelle Kang Kim, MD, PhD, AGAF, chair of gastroenterology at Cleveland Clinic, Ohio, and colleagues provide EHR improvement strategies and examples that can be adapted for use in a variety of gastroenterology clinic settings.
Their article, which was published online in Clinical Gastroenterology and Hepatology , includes the following suggestions, among others:
- Develop optimization teams. An example is SPRINT, a short, intensive team-based intervention at the University of Colorado Health, Aurora, Colorado, that developed specialty-specific tools, provided EHR efficiency training, and helped streamline workflows. The optimization project increased EHR satisfaction scores and reduced documentation time.
- Reroute low-acuity messages. Low-risk medication refills or appointment requests can be handled by nurses and medical assistants. This strategy has helped reduce the inbox burden.
- Create order sets for complex treatment dosing. One example is Cleveland Clinic’s Helicobacter pylori order set, which enables clinicians to quickly place orders with built-in dosages.
- Personalize EHR drop-down menus. Incorporate inflammatory bowel disease (IBD) severity scores, biopsy sampling, resection protocols, specimen container numbering, and other workflow-specific documentation into the EHR.
- Employ medical scribes. These professionals can serve as personal assistants, supporting care teams and reducing clinician documentation time. Alternatively, clinical support staff, such as nurses, can assist with documentation and messages, helping to reduce physician burnout. “These models could be particularly useful in GI specialties that require a multidisciplinary approach, for example, IBD and hepatology,” the authors write.
- Provide real-time training on best practices. There is no widely accepted EHR training curriculum for students, and experienced physicians face time constraints in learning new practices. Real-time training can help clinicians at all levels optimize their time outside the clinic.
In addition, the authors addressed novel tools and strategies that have been recently deployed and/or are in development, which are based largely on artificial intelligence (AI), natural language processing, and speech recognition. For now, these tools are digitizing data to help automate some EHR tasks, supporting communications with patients, and assisting in clinical decision making.
However, the authors note that although current optimization tools are promising, “there is still a lack of knowledge about their usability and effects on provider and patient well-being. More research is needed to evaluate current methodologies and design intelligent tools for the future that will help GI providers overcome the EHR-related obstacles specific to our field and harness the enormous potential of AI in optimizing the busy GI practice.”
This work received no external funding, and the authors disclosed no conflicts.
A version of this article appeared on Medscape.com.
, a new practice management article suggests.
Michelle Kang Kim, MD, PhD, AGAF, chair of gastroenterology at Cleveland Clinic, Ohio, and colleagues provide EHR improvement strategies and examples that can be adapted for use in a variety of gastroenterology clinic settings.
Their article, which was published online in Clinical Gastroenterology and Hepatology , includes the following suggestions, among others:
- Develop optimization teams. An example is SPRINT, a short, intensive team-based intervention at the University of Colorado Health, Aurora, Colorado, that developed specialty-specific tools, provided EHR efficiency training, and helped streamline workflows. The optimization project increased EHR satisfaction scores and reduced documentation time.
- Reroute low-acuity messages. Low-risk medication refills or appointment requests can be handled by nurses and medical assistants. This strategy has helped reduce the inbox burden.
- Create order sets for complex treatment dosing. One example is Cleveland Clinic’s Helicobacter pylori order set, which enables clinicians to quickly place orders with built-in dosages.
- Personalize EHR drop-down menus. Incorporate inflammatory bowel disease (IBD) severity scores, biopsy sampling, resection protocols, specimen container numbering, and other workflow-specific documentation into the EHR.
- Employ medical scribes. These professionals can serve as personal assistants, supporting care teams and reducing clinician documentation time. Alternatively, clinical support staff, such as nurses, can assist with documentation and messages, helping to reduce physician burnout. “These models could be particularly useful in GI specialties that require a multidisciplinary approach, for example, IBD and hepatology,” the authors write.
- Provide real-time training on best practices. There is no widely accepted EHR training curriculum for students, and experienced physicians face time constraints in learning new practices. Real-time training can help clinicians at all levels optimize their time outside the clinic.
In addition, the authors addressed novel tools and strategies that have been recently deployed and/or are in development, which are based largely on artificial intelligence (AI), natural language processing, and speech recognition. For now, these tools are digitizing data to help automate some EHR tasks, supporting communications with patients, and assisting in clinical decision making.
However, the authors note that although current optimization tools are promising, “there is still a lack of knowledge about their usability and effects on provider and patient well-being. More research is needed to evaluate current methodologies and design intelligent tools for the future that will help GI providers overcome the EHR-related obstacles specific to our field and harness the enormous potential of AI in optimizing the busy GI practice.”
This work received no external funding, and the authors disclosed no conflicts.
A version of this article appeared on Medscape.com.
No-Biopsy Approach to Celiac Disease Diagnosis Appears Effective for Select Adult Patients
Select adult patients with immunoglobulin A-tissue transglutaminase antibody levels (IgA-tTG) greater than or equal to 10 times the upper limit of normal (ULN) and a moderate-to-high pretest probability of celiac disease could be diagnosed without undergoing invasive endoscopy and duodenal biopsy, according to a new study.
, the authors wrote.
“Our study confirms the high accuracy of serology-based diagnosis of coeliac disease in select adult patients,” said Mohamed G. Shiha, MBBCh, MRCP, lead author and a clinical research fellow in gastroenterology at Sheffield Teaching Hospitals in the United Kingdom.
“This no-biopsy approach could lead to a shorter time to diagnosis, increased patient satisfaction, and reduced healthcare costs,” he said.
The study was published online in Gastroenterology.
Evaluating the No-Biopsy Approach
Dr. Shiha and colleagues conducted a systematic review and meta-analysis to evaluate to the accuracy of a no-biopsy approach for diagnosing celiac disease in adults. They looked for studies that reported the sensitivity and specificity of IgA-tTG ≥10xULN compared with duodenal biopsies (with a Marsh grade ≥2) in adults with suspected celiac disease.
The research team used a bivariate random-effects model to calculate the summary estimates of sensitivity, specificity, and positive and negative likelihood ratios. Then the positive and negative likelihood ratios were used to calculate the positive predictive value (PPV) of the no-biopsy approach across different pretest probabilities of celiac disease.
Among 18 studies with 12,103 participants from 15 countries, the pooled prevalence of biopsy-proven celiac disease was 62%. The proportion of patients with IgA-tTG ≥10xULN was 32%.
The summary sensitivity of IgA-tTG ≥10xULN was 51%, and the summary specificity was 100% for the diagnosis of celiac disease. The positive and negative likelihood ratios were 183.42 and .49, respectively. The area under the summary receiver operating characteristic curve was .83.
Overall, the PPV of IgA-tTG ≥10xULN to identify patients with celiac disease was 98%, which varied according to pretest probability of celiac disease in the studied population. Specifically, the PPV was 65%, 88%, 95%, and 99% if celiac disease prevalence was 1%, 4%, 10%, and 40%, respectively. The 40% prevalence represents the lower confidence interval of the pooled prevalence from the included studies, the authors noted.
“We provided PPV estimates of IgA-tTG ≥10xULN for common pretest probabilities of coeliac disease to aid clinicians and patients in reaching an informed decision on a no-biopsy diagnosis based on the best available evidence,” the authors wrote.
Considering Additional Factors
Due to the increased accuracy of serological tests, pediatric guidelines have adopted a no-biopsy approach, the authors wrote. Children with IgA-tTG ≥10xULN and positive serum endomysial antibodies (EMA) can be diagnosed with celiac disease without biopsy.
However, the no-biopsy approach remains controversial for diagnosing adult patients and requires additional study, the authors wrote. They noted a limitation that all included studies were conducted in secondary and tertiary care settings and excluded patients with known celiac disease or on a gluten-free diet, so the results may not be generalizable to primary care settings.
In addition, relying on serology testing alone could lead to potential false-positive diagnoses, unnecessary dietary restriction, and negative effects on patients’ quality of life, the authors wrote.
At the same time, duodenal biopsy may not always be accurate due to inadequate sampling and could result in false-negative histology. The no-biopsy approach could mitigate this potential risk, the authors noted.
“This study systematically collates the growing data supporting the accuracy of antibody testing to diagnose celiac disease,” said Benjamin Lebwohl, MD, AGAF, professor of medicine and epidemiology at Columbia University Medical Center and director of clinical research for the Celiac Disease Center at Columbia University, New York. Dr. Lebwohl wasn’t involved with this study.
“We have historically relied on duodenal biopsy to confirm the diagnosis of celiac disease, and the biopsy will still have a central role in most cases in the foreseeable future,” he said. “But as we hone our understanding of antibody testing, one day we may be able to accept or even recommend a biopsy-free approach in select patients.”
Two authors reported grant support from the National Institute for Health and Care Research and National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Shiha reported speaker honorarium from Thermo Fisher. Dr. Lebwohl reported no relevant disclosures.
Select adult patients with immunoglobulin A-tissue transglutaminase antibody levels (IgA-tTG) greater than or equal to 10 times the upper limit of normal (ULN) and a moderate-to-high pretest probability of celiac disease could be diagnosed without undergoing invasive endoscopy and duodenal biopsy, according to a new study.
, the authors wrote.
“Our study confirms the high accuracy of serology-based diagnosis of coeliac disease in select adult patients,” said Mohamed G. Shiha, MBBCh, MRCP, lead author and a clinical research fellow in gastroenterology at Sheffield Teaching Hospitals in the United Kingdom.
“This no-biopsy approach could lead to a shorter time to diagnosis, increased patient satisfaction, and reduced healthcare costs,” he said.
The study was published online in Gastroenterology.
Evaluating the No-Biopsy Approach
Dr. Shiha and colleagues conducted a systematic review and meta-analysis to evaluate to the accuracy of a no-biopsy approach for diagnosing celiac disease in adults. They looked for studies that reported the sensitivity and specificity of IgA-tTG ≥10xULN compared with duodenal biopsies (with a Marsh grade ≥2) in adults with suspected celiac disease.
The research team used a bivariate random-effects model to calculate the summary estimates of sensitivity, specificity, and positive and negative likelihood ratios. Then the positive and negative likelihood ratios were used to calculate the positive predictive value (PPV) of the no-biopsy approach across different pretest probabilities of celiac disease.
Among 18 studies with 12,103 participants from 15 countries, the pooled prevalence of biopsy-proven celiac disease was 62%. The proportion of patients with IgA-tTG ≥10xULN was 32%.
The summary sensitivity of IgA-tTG ≥10xULN was 51%, and the summary specificity was 100% for the diagnosis of celiac disease. The positive and negative likelihood ratios were 183.42 and .49, respectively. The area under the summary receiver operating characteristic curve was .83.
Overall, the PPV of IgA-tTG ≥10xULN to identify patients with celiac disease was 98%, which varied according to pretest probability of celiac disease in the studied population. Specifically, the PPV was 65%, 88%, 95%, and 99% if celiac disease prevalence was 1%, 4%, 10%, and 40%, respectively. The 40% prevalence represents the lower confidence interval of the pooled prevalence from the included studies, the authors noted.
“We provided PPV estimates of IgA-tTG ≥10xULN for common pretest probabilities of coeliac disease to aid clinicians and patients in reaching an informed decision on a no-biopsy diagnosis based on the best available evidence,” the authors wrote.
Considering Additional Factors
Due to the increased accuracy of serological tests, pediatric guidelines have adopted a no-biopsy approach, the authors wrote. Children with IgA-tTG ≥10xULN and positive serum endomysial antibodies (EMA) can be diagnosed with celiac disease without biopsy.
However, the no-biopsy approach remains controversial for diagnosing adult patients and requires additional study, the authors wrote. They noted a limitation that all included studies were conducted in secondary and tertiary care settings and excluded patients with known celiac disease or on a gluten-free diet, so the results may not be generalizable to primary care settings.
In addition, relying on serology testing alone could lead to potential false-positive diagnoses, unnecessary dietary restriction, and negative effects on patients’ quality of life, the authors wrote.
At the same time, duodenal biopsy may not always be accurate due to inadequate sampling and could result in false-negative histology. The no-biopsy approach could mitigate this potential risk, the authors noted.
“This study systematically collates the growing data supporting the accuracy of antibody testing to diagnose celiac disease,” said Benjamin Lebwohl, MD, AGAF, professor of medicine and epidemiology at Columbia University Medical Center and director of clinical research for the Celiac Disease Center at Columbia University, New York. Dr. Lebwohl wasn’t involved with this study.
“We have historically relied on duodenal biopsy to confirm the diagnosis of celiac disease, and the biopsy will still have a central role in most cases in the foreseeable future,” he said. “But as we hone our understanding of antibody testing, one day we may be able to accept or even recommend a biopsy-free approach in select patients.”
Two authors reported grant support from the National Institute for Health and Care Research and National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Shiha reported speaker honorarium from Thermo Fisher. Dr. Lebwohl reported no relevant disclosures.
Select adult patients with immunoglobulin A-tissue transglutaminase antibody levels (IgA-tTG) greater than or equal to 10 times the upper limit of normal (ULN) and a moderate-to-high pretest probability of celiac disease could be diagnosed without undergoing invasive endoscopy and duodenal biopsy, according to a new study.
, the authors wrote.
“Our study confirms the high accuracy of serology-based diagnosis of coeliac disease in select adult patients,” said Mohamed G. Shiha, MBBCh, MRCP, lead author and a clinical research fellow in gastroenterology at Sheffield Teaching Hospitals in the United Kingdom.
“This no-biopsy approach could lead to a shorter time to diagnosis, increased patient satisfaction, and reduced healthcare costs,” he said.
The study was published online in Gastroenterology.
Evaluating the No-Biopsy Approach
Dr. Shiha and colleagues conducted a systematic review and meta-analysis to evaluate to the accuracy of a no-biopsy approach for diagnosing celiac disease in adults. They looked for studies that reported the sensitivity and specificity of IgA-tTG ≥10xULN compared with duodenal biopsies (with a Marsh grade ≥2) in adults with suspected celiac disease.
The research team used a bivariate random-effects model to calculate the summary estimates of sensitivity, specificity, and positive and negative likelihood ratios. Then the positive and negative likelihood ratios were used to calculate the positive predictive value (PPV) of the no-biopsy approach across different pretest probabilities of celiac disease.
Among 18 studies with 12,103 participants from 15 countries, the pooled prevalence of biopsy-proven celiac disease was 62%. The proportion of patients with IgA-tTG ≥10xULN was 32%.
The summary sensitivity of IgA-tTG ≥10xULN was 51%, and the summary specificity was 100% for the diagnosis of celiac disease. The positive and negative likelihood ratios were 183.42 and .49, respectively. The area under the summary receiver operating characteristic curve was .83.
Overall, the PPV of IgA-tTG ≥10xULN to identify patients with celiac disease was 98%, which varied according to pretest probability of celiac disease in the studied population. Specifically, the PPV was 65%, 88%, 95%, and 99% if celiac disease prevalence was 1%, 4%, 10%, and 40%, respectively. The 40% prevalence represents the lower confidence interval of the pooled prevalence from the included studies, the authors noted.
“We provided PPV estimates of IgA-tTG ≥10xULN for common pretest probabilities of coeliac disease to aid clinicians and patients in reaching an informed decision on a no-biopsy diagnosis based on the best available evidence,” the authors wrote.
Considering Additional Factors
Due to the increased accuracy of serological tests, pediatric guidelines have adopted a no-biopsy approach, the authors wrote. Children with IgA-tTG ≥10xULN and positive serum endomysial antibodies (EMA) can be diagnosed with celiac disease without biopsy.
However, the no-biopsy approach remains controversial for diagnosing adult patients and requires additional study, the authors wrote. They noted a limitation that all included studies were conducted in secondary and tertiary care settings and excluded patients with known celiac disease or on a gluten-free diet, so the results may not be generalizable to primary care settings.
In addition, relying on serology testing alone could lead to potential false-positive diagnoses, unnecessary dietary restriction, and negative effects on patients’ quality of life, the authors wrote.
At the same time, duodenal biopsy may not always be accurate due to inadequate sampling and could result in false-negative histology. The no-biopsy approach could mitigate this potential risk, the authors noted.
“This study systematically collates the growing data supporting the accuracy of antibody testing to diagnose celiac disease,” said Benjamin Lebwohl, MD, AGAF, professor of medicine and epidemiology at Columbia University Medical Center and director of clinical research for the Celiac Disease Center at Columbia University, New York. Dr. Lebwohl wasn’t involved with this study.
“We have historically relied on duodenal biopsy to confirm the diagnosis of celiac disease, and the biopsy will still have a central role in most cases in the foreseeable future,” he said. “But as we hone our understanding of antibody testing, one day we may be able to accept or even recommend a biopsy-free approach in select patients.”
Two authors reported grant support from the National Institute for Health and Care Research and National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Shiha reported speaker honorarium from Thermo Fisher. Dr. Lebwohl reported no relevant disclosures.
FROM GASTROENTEROLOGY
Automated ADR Software Shows Promise
, according to investigators.
The new software, which automatically integrates endoscopy and pathology reports across a variety of practice settings, delivered an ADR on par with manual review, supporting its accuracy and feasibility for real-world usage, reported Todd A. Brenner, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“ADR calculation is resource-intensive, often requiring manual collation of endoscopy and pathology data across multiple reporting modalities, making it an impractical tool for frequent quality audits at many centers,” the investigators wrote in Techniques and Innovations in Gastrointestinal Endoscopy.
Although others have tried to streamline ADR calculation, most efforts have relied upon manual entry of pathology data, while approaches using artificial intelligence tend to be costly and clumsy to implement across different databases, according to the investigators.
“Thus, there is a substantial demand for a novel tool to extract and analyze colonoscopy indicators from text-based reports that provides accurate data extraction in a package that is easily implemented and modified by clinicians,” they wrote.
Dr. Brenner and colleagues developed a web-based platform to meet these goals.
Following colonoscopy, the system gathers procedural and histopathology results, extracts and classifies relevant data, then outputs ADR, along with cecal intubation rate, Boston Bowel Preparation Score (BBPS), and withdrawal time.
The software was evaluated using endoscopy and pathology reports from 3,809 colonoscopies performed at six centers over 3 months. Six months later, the investigators manually reviewed data from a validation cohort of 1384 colonoscopies conducted over a 1-month period.
Comparing the automated versus manual approach revealed high congruity, with an ADR of 45.1% for the automated system vs 44.3% for manual review. The software also correctly identified most ADR-qualifying screening colonoscopies (sensitivity, 0.918; specificity, 1.0).
“The discrepancy between manual and automated ADR calculations was exclusively attributable to missed (i.e., false negative) identification of ADR-qualifying procedures,” the investigators wrote.
Of these 43 mislabeled cases, about half involved pending pathology results or erroneous pathology sample entries, while the remainder were due to spelling and/or syntax issues that stumped the system.
Still, Dr. Brenner and colleagues suggested that additional programming can overcome these kinds of issues and allow for generalizability across institutions. They noted that search terms can be edited to match local practice patterns, while the web-based reporting platform can be customized to deliver desired quality metrics.
The publication includes a screenshot of one such dashboard, including a readout of ADR, a comparison of ADR across sexes, a pie chart of BBPS score distribution, and gauge charts for cecal intubation rate and mean withdrawal time.
“Further development of this Internet-based colonoscopy quality reporting platform will focus on integrating additional metrics, such as adenomas per colonoscopy, as well as novel metrics, such as a size-stratified ADR, location-stratified ADR, or ADR stratified by polyp histology,” the investigators wrote.
They predicted that automating data collection in this way could help determine which metrics provide clinically meaningful insights, potentially expanding the roster of standard performance benchmarks.
“We further intend to study the integration of this platform into colonoscopy quality improvement and transparency programs to better characterize the impact of frequent, on-demand ADR feedback on colonoscopy performance,” Dr. Brenner and colleagues concluded.The investigators disclosed relationships with Olympus, Medtronic, Apollo Endosurgery, and others.
Adenoma detection rate (ADR) has proven to be a useful metric for the evaluation of quality in screening colonoscopies. Outside of its proven inverse associations with interval colon cancer, ADR also can facilitate quality improvement interventions aimed at improving colonoscopy quality among low performing endoscopists. By focusing on this metric, healthcare providers can identify areas for improvement, ensuring a higher standard of care and ensuring maximum benefit of screening colonoscopies for patients.
Brenner and colleagues describe an automated system importing smart-phrase–based pathology reports into the endoscopy reporting software allowing for the subsequent calculation of an endoscopist-specific ADR. The automated reporting system provided a high level of agreement against manual review and correlated with average withdrawal time. Additional available quality metrics included cecal intubation rate and individual endoscopist procedural volumes.
The added methodology for developing endoscopist and site-specific ADR is an exciting and potentially more generalizable tool that will allow for widespread adoption of this quality metric. Site-specific data limitations and the use of smart-phrase–based reporting systems may limit the utility of this methodology, but it can also encourage more uniform reporting in pathologic and endoscopic reports. Regular service intervals may be required to inspect the quality of the reporting when initially implementing systems at a variety of practice settings.
Vijaya L. Rao, MD, is Assistant Professor of Medicine in the Division of Digestive Diseases & Nutrition at Rush University Medical Center, Chicago. She reports no conflicts of interest.
Adenoma detection rate (ADR) has proven to be a useful metric for the evaluation of quality in screening colonoscopies. Outside of its proven inverse associations with interval colon cancer, ADR also can facilitate quality improvement interventions aimed at improving colonoscopy quality among low performing endoscopists. By focusing on this metric, healthcare providers can identify areas for improvement, ensuring a higher standard of care and ensuring maximum benefit of screening colonoscopies for patients.
Brenner and colleagues describe an automated system importing smart-phrase–based pathology reports into the endoscopy reporting software allowing for the subsequent calculation of an endoscopist-specific ADR. The automated reporting system provided a high level of agreement against manual review and correlated with average withdrawal time. Additional available quality metrics included cecal intubation rate and individual endoscopist procedural volumes.
The added methodology for developing endoscopist and site-specific ADR is an exciting and potentially more generalizable tool that will allow for widespread adoption of this quality metric. Site-specific data limitations and the use of smart-phrase–based reporting systems may limit the utility of this methodology, but it can also encourage more uniform reporting in pathologic and endoscopic reports. Regular service intervals may be required to inspect the quality of the reporting when initially implementing systems at a variety of practice settings.
Vijaya L. Rao, MD, is Assistant Professor of Medicine in the Division of Digestive Diseases & Nutrition at Rush University Medical Center, Chicago. She reports no conflicts of interest.
Adenoma detection rate (ADR) has proven to be a useful metric for the evaluation of quality in screening colonoscopies. Outside of its proven inverse associations with interval colon cancer, ADR also can facilitate quality improvement interventions aimed at improving colonoscopy quality among low performing endoscopists. By focusing on this metric, healthcare providers can identify areas for improvement, ensuring a higher standard of care and ensuring maximum benefit of screening colonoscopies for patients.
Brenner and colleagues describe an automated system importing smart-phrase–based pathology reports into the endoscopy reporting software allowing for the subsequent calculation of an endoscopist-specific ADR. The automated reporting system provided a high level of agreement against manual review and correlated with average withdrawal time. Additional available quality metrics included cecal intubation rate and individual endoscopist procedural volumes.
The added methodology for developing endoscopist and site-specific ADR is an exciting and potentially more generalizable tool that will allow for widespread adoption of this quality metric. Site-specific data limitations and the use of smart-phrase–based reporting systems may limit the utility of this methodology, but it can also encourage more uniform reporting in pathologic and endoscopic reports. Regular service intervals may be required to inspect the quality of the reporting when initially implementing systems at a variety of practice settings.
Vijaya L. Rao, MD, is Assistant Professor of Medicine in the Division of Digestive Diseases & Nutrition at Rush University Medical Center, Chicago. She reports no conflicts of interest.
, according to investigators.
The new software, which automatically integrates endoscopy and pathology reports across a variety of practice settings, delivered an ADR on par with manual review, supporting its accuracy and feasibility for real-world usage, reported Todd A. Brenner, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“ADR calculation is resource-intensive, often requiring manual collation of endoscopy and pathology data across multiple reporting modalities, making it an impractical tool for frequent quality audits at many centers,” the investigators wrote in Techniques and Innovations in Gastrointestinal Endoscopy.
Although others have tried to streamline ADR calculation, most efforts have relied upon manual entry of pathology data, while approaches using artificial intelligence tend to be costly and clumsy to implement across different databases, according to the investigators.
“Thus, there is a substantial demand for a novel tool to extract and analyze colonoscopy indicators from text-based reports that provides accurate data extraction in a package that is easily implemented and modified by clinicians,” they wrote.
Dr. Brenner and colleagues developed a web-based platform to meet these goals.
Following colonoscopy, the system gathers procedural and histopathology results, extracts and classifies relevant data, then outputs ADR, along with cecal intubation rate, Boston Bowel Preparation Score (BBPS), and withdrawal time.
The software was evaluated using endoscopy and pathology reports from 3,809 colonoscopies performed at six centers over 3 months. Six months later, the investigators manually reviewed data from a validation cohort of 1384 colonoscopies conducted over a 1-month period.
Comparing the automated versus manual approach revealed high congruity, with an ADR of 45.1% for the automated system vs 44.3% for manual review. The software also correctly identified most ADR-qualifying screening colonoscopies (sensitivity, 0.918; specificity, 1.0).
“The discrepancy between manual and automated ADR calculations was exclusively attributable to missed (i.e., false negative) identification of ADR-qualifying procedures,” the investigators wrote.
Of these 43 mislabeled cases, about half involved pending pathology results or erroneous pathology sample entries, while the remainder were due to spelling and/or syntax issues that stumped the system.
Still, Dr. Brenner and colleagues suggested that additional programming can overcome these kinds of issues and allow for generalizability across institutions. They noted that search terms can be edited to match local practice patterns, while the web-based reporting platform can be customized to deliver desired quality metrics.
The publication includes a screenshot of one such dashboard, including a readout of ADR, a comparison of ADR across sexes, a pie chart of BBPS score distribution, and gauge charts for cecal intubation rate and mean withdrawal time.
“Further development of this Internet-based colonoscopy quality reporting platform will focus on integrating additional metrics, such as adenomas per colonoscopy, as well as novel metrics, such as a size-stratified ADR, location-stratified ADR, or ADR stratified by polyp histology,” the investigators wrote.
They predicted that automating data collection in this way could help determine which metrics provide clinically meaningful insights, potentially expanding the roster of standard performance benchmarks.
“We further intend to study the integration of this platform into colonoscopy quality improvement and transparency programs to better characterize the impact of frequent, on-demand ADR feedback on colonoscopy performance,” Dr. Brenner and colleagues concluded.The investigators disclosed relationships with Olympus, Medtronic, Apollo Endosurgery, and others.
, according to investigators.
The new software, which automatically integrates endoscopy and pathology reports across a variety of practice settings, delivered an ADR on par with manual review, supporting its accuracy and feasibility for real-world usage, reported Todd A. Brenner, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“ADR calculation is resource-intensive, often requiring manual collation of endoscopy and pathology data across multiple reporting modalities, making it an impractical tool for frequent quality audits at many centers,” the investigators wrote in Techniques and Innovations in Gastrointestinal Endoscopy.
Although others have tried to streamline ADR calculation, most efforts have relied upon manual entry of pathology data, while approaches using artificial intelligence tend to be costly and clumsy to implement across different databases, according to the investigators.
“Thus, there is a substantial demand for a novel tool to extract and analyze colonoscopy indicators from text-based reports that provides accurate data extraction in a package that is easily implemented and modified by clinicians,” they wrote.
Dr. Brenner and colleagues developed a web-based platform to meet these goals.
Following colonoscopy, the system gathers procedural and histopathology results, extracts and classifies relevant data, then outputs ADR, along with cecal intubation rate, Boston Bowel Preparation Score (BBPS), and withdrawal time.
The software was evaluated using endoscopy and pathology reports from 3,809 colonoscopies performed at six centers over 3 months. Six months later, the investigators manually reviewed data from a validation cohort of 1384 colonoscopies conducted over a 1-month period.
Comparing the automated versus manual approach revealed high congruity, with an ADR of 45.1% for the automated system vs 44.3% for manual review. The software also correctly identified most ADR-qualifying screening colonoscopies (sensitivity, 0.918; specificity, 1.0).
“The discrepancy between manual and automated ADR calculations was exclusively attributable to missed (i.e., false negative) identification of ADR-qualifying procedures,” the investigators wrote.
Of these 43 mislabeled cases, about half involved pending pathology results or erroneous pathology sample entries, while the remainder were due to spelling and/or syntax issues that stumped the system.
Still, Dr. Brenner and colleagues suggested that additional programming can overcome these kinds of issues and allow for generalizability across institutions. They noted that search terms can be edited to match local practice patterns, while the web-based reporting platform can be customized to deliver desired quality metrics.
The publication includes a screenshot of one such dashboard, including a readout of ADR, a comparison of ADR across sexes, a pie chart of BBPS score distribution, and gauge charts for cecal intubation rate and mean withdrawal time.
“Further development of this Internet-based colonoscopy quality reporting platform will focus on integrating additional metrics, such as adenomas per colonoscopy, as well as novel metrics, such as a size-stratified ADR, location-stratified ADR, or ADR stratified by polyp histology,” the investigators wrote.
They predicted that automating data collection in this way could help determine which metrics provide clinically meaningful insights, potentially expanding the roster of standard performance benchmarks.
“We further intend to study the integration of this platform into colonoscopy quality improvement and transparency programs to better characterize the impact of frequent, on-demand ADR feedback on colonoscopy performance,” Dr. Brenner and colleagues concluded.The investigators disclosed relationships with Olympus, Medtronic, Apollo Endosurgery, and others.
FROM TECHNIQUES AND INNOVATIONS IN GASTROINTESTINAL ENDOSCOPY