User login
PHM17 session summary: Demonstrating teaching excellence with an educator’s portfolio
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
NASHVILLE, TENN. – Development of a medical educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process, according to an expert panel at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Promote yourself: Demonstrating teaching excellence with an educator’s portfolio
Presenters
Michael Ryan, MD, MEHP; Ashlie Tseng, MD; Jocelyn Schiller, MD; Rebecca Tenney-Soeiro, MD, MEd; Michele Long, MD; Corki Lehmann, MD, MEd; Amy Fleming, MD; and H. Barrett Fromme, MD, MHPE
Session summary
Development of an educator’s portfolio is a necessary, but daunting, task for clinician educators when they enter the promotion process. Each institution has its own specific requirements for the educator’s portfolio, but there are several general themes that should be considered for inclusion:
1. Develop an educational philosophy. This is a personal statement that frames the rest of the portfolio and describes how this philosophy is used by the educator in his/her approach to education.
2. Teaching. Include teaching activities that are both formal (i.e. lectures) and sessions that encourage more active participation (i.e. small group discussions). This can be accomplished by generating a teaching activities report, which helps to categorize these activities. This will not only demonstrate the volume of teaching experience, but also help to demonstrate the diversity of an educator’s teaching activities. In this section, an educator also should include teaching awards received.
3. Learner evaluations. A qualitative summary of comments will provide a narrative of the educator’s teaching skills. This section also may include summaries of annual reviews of teaching.
4. Curriculum development. Demonstrate the educator’s active engagement in the development of a novel curriculum or the improvement of a pre-existing curriculum and the successful outcomes of those improvements.
5. Mentoring and advising. Generating a list of advisees and highlighting their accomplishments reflects on the ability of the educator to guide and promote success in his/her learners.
6. Educational leadership and administration. This is a description of the past and present leadership roles that the educator has held, including courses or clerkships directed. This should allow the educator the opportunity to provide a narrative description of his/her involvement beyond what is typically stated on the curriculum vitae.
7. Professional development. The educator should develop a list of activities, including formal degree programs, certificate programs, and educational workshops, in which he/she has participated as a learner and have enhanced his/her skills as an educator.
8. Products of educational scholarship. Generate a list of education-related peer-reviewed publications authored, other educational products (such as a syllabus or curriculum) developed, and educational workshops that the educator was invited to give.
For clinician educators interested in developing an educator’s portfolio, there are several resources available, including the Academic Pediatric Association’s website and several MedEdPORTAL publications.
Key takeaways for Pediatric HM
• While each institution has its own specific requirements, there are general themes to consider including in an educator’s portfolio.
• Resources such as the Academic Pediatric Association’s website can help guide an educator in the development of his/her portfolio.
Dr. Player is a pediatric hospitalist at Children’s Hospital of Wisconsin and assistant professor at the Medical College of Wisconsin, Milwaukee.
At PHM 2017
PHM17 session summary: Tools for engaging learners of all levels
NASHVILLE, TENN. – Various instructional tools and techniques can help hospitalists teach medical learners at a variety of levels, according to experts who spoke at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Tools for Engaging Learners of All Levels: Multilevel Teaching Techniques & Cognitive Apprenticeship
Presenters
Session summary
Hospitalists are commonly charged with teaching learners at a variety of levels. There are various tools that can be used to accomplish this including multilevel teaching and cognitive apprenticeship.
Multilevel teaching is defined as teaching multiple levels of learners simultaneously. The goal is to maintain engagement without being boring or teaching over any learner’s head. Examples include:
1. Broadening: Change the case to make it more challenging or interesting such as asking what to do if the patient was a different age or had a comorbid condition.
2. Targeting: Target questions at specific team members depending on difficulty such as asking students common causes of bacterial meningitis and asking residents about admission criteria.
3. Novelty: Provide new data such as a recent journal article.
4. Up the Ladder: Ask the same question to all team members, starting with the most junior.
5. Student as Teacher: Ask a senior learner to teach a junior learner.
6. Multi-Answer: Seek multiple answers to one question such as asking each learner to contribute an item to a differential diagnosis.
7. No Right Answer: Ask questions that do not have a single correct answer such as how to approach a difficult conversation.
8. Teaching to the Top: Teach to the level of the most senior learner.
9. Extreme Challenge: Teach at a level above all learners on the team.
Laura Certain, MD, PhD, et al1 found that most trainees feel Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are most effective. No Right Answer, Teaching to the Top, and Extreme Challenge were felt to be least effective.
Another concept for engaging learners at all levels is cognitive apprenticeship, which is an instructional model whereby teachers make explicit their generally tacit cognitive processes. Examples include:
1. Modeling: Actively demonstrate skills such as performing a procedure while verbalizing the steps and thought processes.
2. Couching: Observe learners and provide feedback on their performance.
3. Scaffolding: Inquire about past experiences and provide opportunity for independent activities, while also providing help for activities that are difficult for learners.
4. Articulation: Ask learners to explain their thought processes.
5. Reflection: Prompt students to deliberately consider their strengths and weaknesses.
6. Exploration: Encourage students to set personal learning goals.
Coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
Key takeaways for Pediatric HM
• Multilevel teaching can be used to engage a variety of learners simultaneously. Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are effective methods to achieve this goal.
• Cognitive apprenticeship can be used in clinical teaching to make a tacit cognitive process explicit. Methods such as coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
• Regardless of the method used, teachers should demonstrate interest in the learners’ education and treat them with respect.
Dr. Rogers is assistant professor of pediatrics and Section of Hospital Medicine associate program director, Pediatric Residency Program, at the Medical College of Wisconsin, Milwaukee.
References
1. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12),e644-650. doi: 10.3109/0142159X.2011.610844.
NASHVILLE, TENN. – Various instructional tools and techniques can help hospitalists teach medical learners at a variety of levels, according to experts who spoke at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Tools for Engaging Learners of All Levels: Multilevel Teaching Techniques & Cognitive Apprenticeship
Presenters
Session summary
Hospitalists are commonly charged with teaching learners at a variety of levels. There are various tools that can be used to accomplish this including multilevel teaching and cognitive apprenticeship.
Multilevel teaching is defined as teaching multiple levels of learners simultaneously. The goal is to maintain engagement without being boring or teaching over any learner’s head. Examples include:
1. Broadening: Change the case to make it more challenging or interesting such as asking what to do if the patient was a different age or had a comorbid condition.
2. Targeting: Target questions at specific team members depending on difficulty such as asking students common causes of bacterial meningitis and asking residents about admission criteria.
3. Novelty: Provide new data such as a recent journal article.
4. Up the Ladder: Ask the same question to all team members, starting with the most junior.
5. Student as Teacher: Ask a senior learner to teach a junior learner.
6. Multi-Answer: Seek multiple answers to one question such as asking each learner to contribute an item to a differential diagnosis.
7. No Right Answer: Ask questions that do not have a single correct answer such as how to approach a difficult conversation.
8. Teaching to the Top: Teach to the level of the most senior learner.
9. Extreme Challenge: Teach at a level above all learners on the team.
Laura Certain, MD, PhD, et al1 found that most trainees feel Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are most effective. No Right Answer, Teaching to the Top, and Extreme Challenge were felt to be least effective.
Another concept for engaging learners at all levels is cognitive apprenticeship, which is an instructional model whereby teachers make explicit their generally tacit cognitive processes. Examples include:
1. Modeling: Actively demonstrate skills such as performing a procedure while verbalizing the steps and thought processes.
2. Couching: Observe learners and provide feedback on their performance.
3. Scaffolding: Inquire about past experiences and provide opportunity for independent activities, while also providing help for activities that are difficult for learners.
4. Articulation: Ask learners to explain their thought processes.
5. Reflection: Prompt students to deliberately consider their strengths and weaknesses.
6. Exploration: Encourage students to set personal learning goals.
Coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
Key takeaways for Pediatric HM
• Multilevel teaching can be used to engage a variety of learners simultaneously. Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are effective methods to achieve this goal.
• Cognitive apprenticeship can be used in clinical teaching to make a tacit cognitive process explicit. Methods such as coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
• Regardless of the method used, teachers should demonstrate interest in the learners’ education and treat them with respect.
Dr. Rogers is assistant professor of pediatrics and Section of Hospital Medicine associate program director, Pediatric Residency Program, at the Medical College of Wisconsin, Milwaukee.
References
1. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12),e644-650. doi: 10.3109/0142159X.2011.610844.
NASHVILLE, TENN. – Various instructional tools and techniques can help hospitalists teach medical learners at a variety of levels, according to experts who spoke at Pediatric Hospital Medicine 2017, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
Session
Tools for Engaging Learners of All Levels: Multilevel Teaching Techniques & Cognitive Apprenticeship
Presenters
Session summary
Hospitalists are commonly charged with teaching learners at a variety of levels. There are various tools that can be used to accomplish this including multilevel teaching and cognitive apprenticeship.
Multilevel teaching is defined as teaching multiple levels of learners simultaneously. The goal is to maintain engagement without being boring or teaching over any learner’s head. Examples include:
1. Broadening: Change the case to make it more challenging or interesting such as asking what to do if the patient was a different age or had a comorbid condition.
2. Targeting: Target questions at specific team members depending on difficulty such as asking students common causes of bacterial meningitis and asking residents about admission criteria.
3. Novelty: Provide new data such as a recent journal article.
4. Up the Ladder: Ask the same question to all team members, starting with the most junior.
5. Student as Teacher: Ask a senior learner to teach a junior learner.
6. Multi-Answer: Seek multiple answers to one question such as asking each learner to contribute an item to a differential diagnosis.
7. No Right Answer: Ask questions that do not have a single correct answer such as how to approach a difficult conversation.
8. Teaching to the Top: Teach to the level of the most senior learner.
9. Extreme Challenge: Teach at a level above all learners on the team.
Laura Certain, MD, PhD, et al1 found that most trainees feel Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are most effective. No Right Answer, Teaching to the Top, and Extreme Challenge were felt to be least effective.
Another concept for engaging learners at all levels is cognitive apprenticeship, which is an instructional model whereby teachers make explicit their generally tacit cognitive processes. Examples include:
1. Modeling: Actively demonstrate skills such as performing a procedure while verbalizing the steps and thought processes.
2. Couching: Observe learners and provide feedback on their performance.
3. Scaffolding: Inquire about past experiences and provide opportunity for independent activities, while also providing help for activities that are difficult for learners.
4. Articulation: Ask learners to explain their thought processes.
5. Reflection: Prompt students to deliberately consider their strengths and weaknesses.
6. Exploration: Encourage students to set personal learning goals.
Coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
Key takeaways for Pediatric HM
• Multilevel teaching can be used to engage a variety of learners simultaneously. Targeting, Up the Ladder, Student as Teacher, and Multi-Answer are effective methods to achieve this goal.
• Cognitive apprenticeship can be used in clinical teaching to make a tacit cognitive process explicit. Methods such as coaching and articulation have been found to be more useful for novice learners. Reflection and exploration are more useful for advanced learners.
• Regardless of the method used, teachers should demonstrate interest in the learners’ education and treat them with respect.
Dr. Rogers is assistant professor of pediatrics and Section of Hospital Medicine associate program director, Pediatric Residency Program, at the Medical College of Wisconsin, Milwaukee.
References
1. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12),e644-650. doi: 10.3109/0142159X.2011.610844.
At PHM 2017
Student Hospitalist Scholars: Discovering a passion for research
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
When I decided to leave the business world to pursue a career in medicine, I envisioned myself in a clinic or an operating room helping the people in my community with the knowledge and skills acquired in my medical training. The thought of becoming a researcher had never even crossed my mind.
I grew up in Scottsdale, Arizona, a city which has no major academic medical centers. Prior to entering medical school, I was enrolled in a postbaccalaureate program at Johns Hopkins University, where I took the basic science classes necessary to apply. I was quite surprised to learn that, even at this level of education, I was required to participate in a research project. This experience changed the way I envisioned my entire career as a physician.
I am now a fourth year medical student and a pioneer of the “new curriculum” at Weill Cornell Medical College. In contrast to the traditional medical school curriculum, Cornell carved out 6 months of protected research time for all medical students by condensing the preclinical curriculum from 2 years to 1.5 years. I learned how much I enjoyed research at Johns Hopkins, which is one of the main reasons I applied here.
Despite my interest in research, I still struggled with the ultimate career question: What kind of doctor do I want to be?
After completing my medicine clerkship, I remember feeling intellectually stimulated in a way I hadn’t experienced in the previous years. While this may have had to do with the subject matter, I attribute much of this feeling to my clerkship director whose passion for medicine and teaching was contagious. I ultimately chose Ernie Esquivel, MD, to be my research mentor because of how much he impacted my education.
Together we came up with a project to study the utility of bone biopsies in the management of osteomyelitis. We are doing this by analyzing changes from empiric to final antibiotics after bone biopsy results become available to determine how clinicians use this information to guide their management of the disease. We were also interested in analyzing predictors of positive bone cultures in this population. The success of this project will mostly be based on our ability to perform these analyses, regardless of what the results may be. We hypothesize that, in fact, bone biopsy results are not likely to have a significant impact on antibiotic management of osteomyelitis in nonvertebral bones.
I was one of the lucky few to be awarded a grant from the Society of Hospital Medicine, which will be instrumental in the success of the project. This grant will not only support my ongoing research efforts but will also afford me the opportunity to attend the annual SHM conference and become integrated into the medical community in a way that would otherwise never be possible.
Cole Hirschfeld is originally from Phoenix, Ariz. He received undergraduate degrees in finance and entrepreneurship from the University of Arizona and went on to work in the finance industry for 2 years before deciding to change careers and attend medical school. He is now a fourth year medical student at Weill Cornell Medical College and plans to apply for residency in internal medicine.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
When I decided to leave the business world to pursue a career in medicine, I envisioned myself in a clinic or an operating room helping the people in my community with the knowledge and skills acquired in my medical training. The thought of becoming a researcher had never even crossed my mind.
I grew up in Scottsdale, Arizona, a city which has no major academic medical centers. Prior to entering medical school, I was enrolled in a postbaccalaureate program at Johns Hopkins University, where I took the basic science classes necessary to apply. I was quite surprised to learn that, even at this level of education, I was required to participate in a research project. This experience changed the way I envisioned my entire career as a physician.
I am now a fourth year medical student and a pioneer of the “new curriculum” at Weill Cornell Medical College. In contrast to the traditional medical school curriculum, Cornell carved out 6 months of protected research time for all medical students by condensing the preclinical curriculum from 2 years to 1.5 years. I learned how much I enjoyed research at Johns Hopkins, which is one of the main reasons I applied here.
Despite my interest in research, I still struggled with the ultimate career question: What kind of doctor do I want to be?
After completing my medicine clerkship, I remember feeling intellectually stimulated in a way I hadn’t experienced in the previous years. While this may have had to do with the subject matter, I attribute much of this feeling to my clerkship director whose passion for medicine and teaching was contagious. I ultimately chose Ernie Esquivel, MD, to be my research mentor because of how much he impacted my education.
Together we came up with a project to study the utility of bone biopsies in the management of osteomyelitis. We are doing this by analyzing changes from empiric to final antibiotics after bone biopsy results become available to determine how clinicians use this information to guide their management of the disease. We were also interested in analyzing predictors of positive bone cultures in this population. The success of this project will mostly be based on our ability to perform these analyses, regardless of what the results may be. We hypothesize that, in fact, bone biopsy results are not likely to have a significant impact on antibiotic management of osteomyelitis in nonvertebral bones.
I was one of the lucky few to be awarded a grant from the Society of Hospital Medicine, which will be instrumental in the success of the project. This grant will not only support my ongoing research efforts but will also afford me the opportunity to attend the annual SHM conference and become integrated into the medical community in a way that would otherwise never be possible.
Cole Hirschfeld is originally from Phoenix, Ariz. He received undergraduate degrees in finance and entrepreneurship from the University of Arizona and went on to work in the finance industry for 2 years before deciding to change careers and attend medical school. He is now a fourth year medical student at Weill Cornell Medical College and plans to apply for residency in internal medicine.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
When I decided to leave the business world to pursue a career in medicine, I envisioned myself in a clinic or an operating room helping the people in my community with the knowledge and skills acquired in my medical training. The thought of becoming a researcher had never even crossed my mind.
I grew up in Scottsdale, Arizona, a city which has no major academic medical centers. Prior to entering medical school, I was enrolled in a postbaccalaureate program at Johns Hopkins University, where I took the basic science classes necessary to apply. I was quite surprised to learn that, even at this level of education, I was required to participate in a research project. This experience changed the way I envisioned my entire career as a physician.
I am now a fourth year medical student and a pioneer of the “new curriculum” at Weill Cornell Medical College. In contrast to the traditional medical school curriculum, Cornell carved out 6 months of protected research time for all medical students by condensing the preclinical curriculum from 2 years to 1.5 years. I learned how much I enjoyed research at Johns Hopkins, which is one of the main reasons I applied here.
Despite my interest in research, I still struggled with the ultimate career question: What kind of doctor do I want to be?
After completing my medicine clerkship, I remember feeling intellectually stimulated in a way I hadn’t experienced in the previous years. While this may have had to do with the subject matter, I attribute much of this feeling to my clerkship director whose passion for medicine and teaching was contagious. I ultimately chose Ernie Esquivel, MD, to be my research mentor because of how much he impacted my education.
Together we came up with a project to study the utility of bone biopsies in the management of osteomyelitis. We are doing this by analyzing changes from empiric to final antibiotics after bone biopsy results become available to determine how clinicians use this information to guide their management of the disease. We were also interested in analyzing predictors of positive bone cultures in this population. The success of this project will mostly be based on our ability to perform these analyses, regardless of what the results may be. We hypothesize that, in fact, bone biopsy results are not likely to have a significant impact on antibiotic management of osteomyelitis in nonvertebral bones.
I was one of the lucky few to be awarded a grant from the Society of Hospital Medicine, which will be instrumental in the success of the project. This grant will not only support my ongoing research efforts but will also afford me the opportunity to attend the annual SHM conference and become integrated into the medical community in a way that would otherwise never be possible.
Cole Hirschfeld is originally from Phoenix, Ariz. He received undergraduate degrees in finance and entrepreneurship from the University of Arizona and went on to work in the finance industry for 2 years before deciding to change careers and attend medical school. He is now a fourth year medical student at Weill Cornell Medical College and plans to apply for residency in internal medicine.
Student Hospitalist Scholars: The importance of communication
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their 1st, 2nd, and 3rd years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
Quality improvement in clinical practice has recently become very important to me. What use is clinical knowledge if it cannot be appropriately used to benefit patients in a clinical setting?
Throughout my 1st year at medical school, my interest in communication continued to grow. In one of my classes, Essentials of Clinical Reasoning, we were taught to continually consider how to effectively translate our thought processes and potential diagnoses to our patients. To begin crafting effective HPIs, we created complete, whole histories from visit to visit.
At this time, I discovered the subfield of research concerning strategies surrounding handoffs as transition of care changes, with patients often suffering due to breakdowns in communication.
With my interest in handoffs, and with direction from the Society of Hospital Medicine, I reached out to Dr. Vineet Arora, a leading academic hospitalist at the University of Chicago with a highly impressive history of research concerning quality of care toward hospitalized adults. Under the supervision of Dr. Arora and Dr. Juan Rojas, a pulmonary critical care fellow, I will help investigate whether receiving floor physicians and intensive care unit physicians possess similar shared mental models in regards to the most pertinent point of care – when patients are transferred out of the ICU.
We seek to identify if there are any associations present between readmission from the general floor, the providers’ rated likelihood of the patient returning to the ICU, and whether floor and ICU physicians are on the same page concerning condition management while on the floor.
I believe the experience I gain at the University of Chicago Medical Center will be invaluable to my future as a physician. I am very excited to get to know the various clinicians at UChicago, to gain clinical experience by observing the management of the general ward, and to identify how effective physicians communicate.
Above all, I hope to use any knowledge I gain this summer to become an efficient, knowledgeable, and compassionate physician capable of providing the highest quality of care to my future patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago, Ill. He received his B.S. in Biology from Loyola University in Chicago in 2015 and his Master of Biomedical Science from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their 1st, 2nd, and 3rd years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
Quality improvement in clinical practice has recently become very important to me. What use is clinical knowledge if it cannot be appropriately used to benefit patients in a clinical setting?
Throughout my 1st year at medical school, my interest in communication continued to grow. In one of my classes, Essentials of Clinical Reasoning, we were taught to continually consider how to effectively translate our thought processes and potential diagnoses to our patients. To begin crafting effective HPIs, we created complete, whole histories from visit to visit.
At this time, I discovered the subfield of research concerning strategies surrounding handoffs as transition of care changes, with patients often suffering due to breakdowns in communication.
With my interest in handoffs, and with direction from the Society of Hospital Medicine, I reached out to Dr. Vineet Arora, a leading academic hospitalist at the University of Chicago with a highly impressive history of research concerning quality of care toward hospitalized adults. Under the supervision of Dr. Arora and Dr. Juan Rojas, a pulmonary critical care fellow, I will help investigate whether receiving floor physicians and intensive care unit physicians possess similar shared mental models in regards to the most pertinent point of care – when patients are transferred out of the ICU.
We seek to identify if there are any associations present between readmission from the general floor, the providers’ rated likelihood of the patient returning to the ICU, and whether floor and ICU physicians are on the same page concerning condition management while on the floor.
I believe the experience I gain at the University of Chicago Medical Center will be invaluable to my future as a physician. I am very excited to get to know the various clinicians at UChicago, to gain clinical experience by observing the management of the general ward, and to identify how effective physicians communicate.
Above all, I hope to use any knowledge I gain this summer to become an efficient, knowledgeable, and compassionate physician capable of providing the highest quality of care to my future patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago, Ill. He received his B.S. in Biology from Loyola University in Chicago in 2015 and his Master of Biomedical Science from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their 1st, 2nd, and 3rd years of medical school. As a part of the program, recipients are required to write about their experience on a biweekly basis.
Quality improvement in clinical practice has recently become very important to me. What use is clinical knowledge if it cannot be appropriately used to benefit patients in a clinical setting?
Throughout my 1st year at medical school, my interest in communication continued to grow. In one of my classes, Essentials of Clinical Reasoning, we were taught to continually consider how to effectively translate our thought processes and potential diagnoses to our patients. To begin crafting effective HPIs, we created complete, whole histories from visit to visit.
At this time, I discovered the subfield of research concerning strategies surrounding handoffs as transition of care changes, with patients often suffering due to breakdowns in communication.
With my interest in handoffs, and with direction from the Society of Hospital Medicine, I reached out to Dr. Vineet Arora, a leading academic hospitalist at the University of Chicago with a highly impressive history of research concerning quality of care toward hospitalized adults. Under the supervision of Dr. Arora and Dr. Juan Rojas, a pulmonary critical care fellow, I will help investigate whether receiving floor physicians and intensive care unit physicians possess similar shared mental models in regards to the most pertinent point of care – when patients are transferred out of the ICU.
We seek to identify if there are any associations present between readmission from the general floor, the providers’ rated likelihood of the patient returning to the ICU, and whether floor and ICU physicians are on the same page concerning condition management while on the floor.
I believe the experience I gain at the University of Chicago Medical Center will be invaluable to my future as a physician. I am very excited to get to know the various clinicians at UChicago, to gain clinical experience by observing the management of the general ward, and to identify how effective physicians communicate.
Above all, I hope to use any knowledge I gain this summer to become an efficient, knowledgeable, and compassionate physician capable of providing the highest quality of care to my future patients.
Anton Garazha is a medical student at Chicago Medical School at Rosalind Franklin University in North Chicago, Ill. He received his B.S. in Biology from Loyola University in Chicago in 2015 and his Master of Biomedical Science from Rosalind Franklin University in 2016. Anton is very interested in community outreach and quality improvement, and in his spare time tutors students in science-based subjects.
Student Hospitalist Scholars: Preventing unplanned PICU transfers
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Editor’s Note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the program, recipients are required to write about their experiences on a biweekly basis.
I’m a rising second year medical student working this summer on a project to determine predictors for pediatric clinical deterioration and unplanned transfers to the pediatric ICU.
We’re hoping to identify characteristics of the pediatric population that is more prone to these unplanned transfers, as well as determine what clinical signs serve as reliable warnings so that an intervention can be designed to prevent these emergency transfers.
So far, I have been searching the literature for what current interventions exist to prevent pediatric clinical deterioration. I have been reading about rapid response teams and their effectiveness in preventing codes, as well as what measures are used to evaluate the condition of a pediatric patient who is at risk for clinical deterioration. It is clear that more investigation is needed to identify reliable predictors that indicate a possible ICU transfer for the child patient.
I was interested in this project, and in quality improvement, because of its power to directly improve patient care and safety. It is vital to identify and fix problems that are preventable. It is directly related to the work of the physician, and the interprofessional collaboration aspect is key to improve communication that directly affects the patients’ outcomes.
I was introduced to the field during the past year in medical school, and this prompted me to start looking for research projects in the hospital medicine department at Cincinnati Children’s Hospital. I was connected with Patrick Brady, MD, an attending physician in the division of hospital medicine at Cincinnati Children’s, whose work involves studying patient safety. His goals of investigating how to prevent clinical deterioration in pediatric patients aligned with what I wanted to learn during my research experience.
After partnering with my primary mentor, Dr. Brady, we discussed how the Student Hospitalist Scholar Grant would be a good fit for me, so I decided to apply.
I am excited to continue this experience this summer, as I believe it would not only educate me about applying interventions to better patient care but also about medicine in general. I plan to carry on and apply these lessons learned during my third year of medical school for rotations.
Farah Hussain is a second year medical student at the University of Cincinnati and student researcher at Cincinnati Children’s Hospital Medical Center. Her research interests involve bettering patient care in vulnerable populations.
Pediatric hospital medicine marches toward subspecialty recognition
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
Pediatric hospital medicine is moving quickly toward recognition as a board-certified, fellowship-trained medical subspecialty, joining 14 other pediatric subspecialties now certified by the American Board of Pediatrics (ABP).
It was approved as a subspecialty by the American Board of Medical Specialties (ABMS) at its October 2016 board meeting in Chicago in response to a petition from the ABP. Following years of discussion within the field,1 it will take 2 more years to describe pediatric hospital medicine’s specialized knowledge base and write test questions for biannual board exams that are projected to commence in the fall of 2019.
Eventually, starting in 2025, pediatric hospitalists will need to complete a fellowship of 2 years or more if they wish to sit for the exam and become board-certified in the field. But for the next 7 years, hospitalists in current practice will be able to qualify based on their work experience. Maintenance of certification requirements likely will be similar to those in other subspecialties, and doctors certified in pediatric hospital medicine won’t be required to maintain general pediatric certification, Dr. Rauch said.
Formal eligibility criteria have not been set, but likely will include working half-time overall in pediatric-related activities, and quarter-time in clinical practice in pediatric hospital medicine for 4 years prior to qualifying for the exam. How the hours might break down between clinical and other hospital responsibilities, and between pediatric or adult patients, still needs to be determined, Dr. Rauch said. He added that the experiential pathway is likely to be defined broadly, with latitude for determinations based on percentages of time worked, rather than absolute number of hours worked. Local pediatric institutions will be granted latitude to determine how that “plays out” in real world situations, he said, “and an ABP credentialing committee will be available to hear appeals for people who have complicated life circumstances.”
“I was part of a committee that explored these issues. We were an independent group of hospitalists who decided that board certification was a good way to advance the field,” Dr. Quinonez said. “We’ve seen what subspecialty certification has done, for example, for pediatric emergency medicine and pediatric critical care medicine – advancing them tremendously from a research standpoint and helping to develop a distinct body of knowledge reflecting increased severity of illness in hospitalized children.”
Discrepancy between practicing hospitalists, fellowships
An estimated 4,000 pediatric hospitalists now practice in the United States, and 2,100 of those belong to the American Academy of Pediatrics’ Section on Hospital Medicine. There are 40 pediatric hospital medicine fellowship programs listed on the website of AAP’s Section on Hospital Medicine (http://phmfellows.org/phm-programs/), although formal training assessment criteria will be needed for the American College of Graduate Medical Education to recognize programs that qualify their fellows to sit for the PHM exam. A wide gap is anticipated between the demand for pediatric hospitalists and currently available fellowship training slots to generate new candidates for board certification, although Dr. Rauch projects that fellowship slots will double in coming years.
“My message to the field is that historically, board certification has been the launching point for further development of the field,” Dr. Rauch said. “It leads to standardization of who is a subspecialist. Right now, who is a pediatric hospitalist is subject to wide variation. We need to standardize training and to create for this field the same distinction and stature as other medical subspecialties,” he said, noting that subspecialty status also has ramifications for academic settings, and for career advancement and career satisfaction for the individuals who choose to pursue it.
“I know there has been some hue and cry about this in the field, but in most cases certification will not change a pediatric hospitalist’s ability to obtain a job,” he said. “Already, you can’t become a division leader at a children’s hospital without additional training. This isn’t going to change that reality. But for people who don’t want to follow an academic career path, there will never be enough board-certified or fellowship-trained pediatric hospitalists to fill all of the pediatric positions in all the hospitals in the country. Community hospitals aren’t going to say: We won’t hire you unless you are board certified.”
Is the fellowship good for the field?
The subspecialty development process clearly is moving forward. Those in favor believe it will increase scholarship, research, and recognition for the subspecialty by the public for its specialized body of knowledge. But not everyone in the field agrees. Last fall The Hospitalist published3 an opinion piece questioning the need for fellowship-based board certification in pediatric hospital medicine. The author recommended instead retaining the current voluntary approach to fellowships and establishing a pediatric “focused practice” incorporated into residency training, much as the American Board of Internal Medicine and the American Board of Family Medicine have done for hospitalists in adult medicine.
“Will it lead to uncertainty among those currently in residency programs? If you are a pediatric resident and you want to become a board-certified pediatric hospitalist, you’ll need at least 2 years more of training. Is that going to deter qualified individuals?” Dr. Chang said. “The people this decision will impact the most are med-peds doctors – who complete a combined internal medicine and pediatrics residency – and part-timers. They may find themselves in a difficult position if the number of hours don’t add up for them to sit for the boards. For the most part, we’ll have to wait and see for answers to these questions.”
Brian Alverson, MD, FAAP, current chair of the AAP’s Section on Hospital Medicine and associate professor of pediatrics at Brown University, Providence, R.I., says he can see both sides of the debate.
But at the same time, there is a significant opportunity cost for doing 2 more years of fellowship training, Dr. Alverson said.
“We don’t know how much the board certification test will improve actual care,” he noted. “Does it truly identify higher quality doctors, or just doctors who are good at taking multiple choice exams? There are a number of people in pediatrics who do a lot of different things in their jobs, and it’s important that they not lose their ability to practice in the field. Two-thirds of our work force is in community hospitals, not academic medical centers. They work hard to provide the backbone of hospital care for young patients, and many of them are unlikely to ever do a fellowship.”
Nonetheless, Dr. Alverson believes pediatric hospitalists needn’t worry. “You still have plenty of time to figure out what’s going to happen in your hospital,” he said.
References
1. Section on Hospital Medicine. Guiding principles for pediatric hospital medicine program. Pediatrics; 2013; 132:782-786.
2. Stucky E. The Pediatric Hospital Medicine Core Competencies. Wiley-Blackwell; 2010.
3. Feldman LS, Monash B, Eniasivam A. Why required pediatric hospital medicine fellowships are unnecessary. The Hospitalist Magazine, October 8, 2016.
The role of NPs and PAs in hospital medicine programs
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
Background and growth
Hospitalist nurse practitioner (NP) and physician assistant (PA) providers have been a growing and evolving part of the inpatient medical workforce, seemingly since the inception of hospital medicine. Given the growth of these disciplines within hospital medicine, at this juncture it is helpful to look at this journey, to see what roles these providers have been serving, and to consider newer and novel trends in how NPs and PAs are being weaved into hospital medicine programs.
The drivers for growth in this provider population are not unlike those of physician hospitalists. The same milieu that provided inroads for physicians in hospital-based care have led the way for increased use of NP/PA providers. An aging physician workforce, residency work hour reforms, increasing complexity of patients and systems on the inpatient side, and the recognition that caring for inpatients is a specialty vastly different from the role of internist in primary care have all impacted the numbers of NPs and PAs in this arena.
• 2007 Today’s Hospitalist article: “Midlevels make a rocky entrance into hospital medicine”1
• 2009 ACP Hospitalist article: “When hiring midlevels, proceed with caution”2
These titles reflect the uncertainty at the time in how best to utilize NP/PA providers in hospital medicine (as well as an unfashionable vocabulary). The numbers at the time tell a similar story. In the Society of Hospital Medicine survey in 2007-2008, about 29% and 21% of hospital medicine practices utilized NPs and PAs, respectively. However, by 2014 about 50% of Veterans Affairs inpatient medical services deployed NP/PA providers, and most recent data from the Society of Hospital Medicine reveal that about 63% of groups use these advanced practice providers (APPs), with higher numbers in pediatric programs. Clearly there is evolving growth and enthusiasm for NP/PAs in hospital medicine.
Program models
Determining how best to use NP/PAs in hospital medicine programs has had a similar evolution. Reviewing past articles addressing these issues, one can see that there has been clear migration; initially NP/PAs were primarily hired to assist with late-afternoon admission surges, with about 60% of the APP workload being utilized to admit in 2007. Their role has continued to grow and change, much as hospitalist practices have; current program models consist of a few major types, with some novel models coming to the fore.
Another model is use of an NP/PA in an observation unit or with lower acuity observation patients. The majority of the management of the patients is completed and billed by the APP, with the physician available for backup. This hits the “sweet spot,” utilizing the right provider with the right skill set for the right patient. The program has to account for some reimbursement or compensation for the physician oversight time, but it is a very efficient use of APPs.
The third major deployment of APPs is with admissions. Many groups use APPs to admit into the late afternoon and evening, getting patients “tucked in,” including starting diagnostic work-ups and treatment plans. The physician hospitalist then evaluates the patient the next day and often bills for the admission. This model works in situations where the patient work-up is dependent on lab testing, imaging, or other diagnostic testing to understand and plan for the “arc” of the hospitalization; or in situations where the diagnosis is clear, but the patient needs time with treatment to determine response. The downside of this model is long-term job satisfaction for the APP (although some programs have them rotate through such a model at intervals).
Another area where APPs have made strong inroads is that of comanagement services. The NP or PA develops a long-term relationship with a surgical comanagement team, and is often highly engaged and extremely appreciated for managing chronic conditions such as hypertension and diabetes. This can be a very satisfying model for both teams. The NP/PA usually bills independently for these encounters.
APPS are also used in cross coverage and triage roles, allowing the day teams to focus on their primary patients. In a triage role, they can interface with the emergency department, providing a semi-neutral “mediator” for patient disposition.
On the more novel end of the spectrum, there is growth in more independent roles for APP hospitalists. Some groups are having success at using the paired rounding or dyad model, but having the physician see the patient every third day. This is most successful where there is strong onboarding and deep clarity for when to contact the backup physician. There are some data to support the effectiveness of this model, most recently in the Journal of Clinical Outcomes Management.3
Critical access hospitals are also having success in deploying APPs in a very independent role, staffing these hospitals at night. Smaller, rural hospitals with aging medical staff have learned to maximize the scope of practice of their APPs to remain viable and provide care for inpatients. This can be a very successful model for APPs working at the maximum scope of their practice. In addition, the use of telemedicine has been implemented to allow for remote physician backup. This may be a rapidly growing arm to hospital medicine practices in the future.
Ongoing barriers
There are many barriers to maximizing the scope of practice and efficiency of APPs in hospital medicine. They range from the “macro” to the “micro.”
On the larger stage, Medicare requires that home care orders be signed by an attending physician, which can be inefficient and difficult to accomplish. Other payers may have somewhat arcane statutes that limit billing practices, and state practice limitations vary widely. Although 22 states now allow for independent practice for NPs, other states may have a very restrictive practice environment that can impede creative care delivery models. But regardless of how liberal a practice the state allows, a hospital’s medical bylaws can still restrict the day-to-day practice of APPs. And those restrictive bylaws are emblematic of a more constant and corporeal barrier to APP practice, that of medical staff culture.
If there are physicians on the staff who fear that utilization of NP/PA providers will lead to a decay in the quality of care, or who feel threatened by the use of APPs, that can create a local stopgap to maximizing utilization of APPs. In addition, hospitalist physicians and leaders may lack knowledge or experience in APP practice. APPs take more time to successfully onboard than physicians; without clear expectations or road maps to accomplish this onboarding, leaders may feel that APP integration doesn’t work. And one bad experience can create long-term barriers for future practices.
Other barriers are the lack of standardized rigor and vigor in graduate education programs (in both educational and clinical experiences). This results in variation in the quality of NP/PA providers at graduation. Knowledge gaps may be perceived as incompetence, rather than just a lack of experience. There is a certificate for added qualification in hospital medicine for PA providers (which includes a specialty exam), and there is an acute care focus for NPs in training; however, there is no standardized licensure to ensure hospital medicine competency, creating a quagmire for hospitalist leaders who desire demonstrable competence of these providers.
Another barrier for some programs is financial; physicians may not want to give up their RVUs to an NP/PA provider. This can really inhibit a more independent role for the APP. It is important that financial incentives align with all members of the practice working at maximum scope.
Summary and future
In summary, the role of PA/NP in hospital medicine has continued to grow and evolve, to meet the needs of the industry. This includes an increase in the scope and independence of APPs, including the use of telehealth for required oversight. As a specialty, it is imperative that we continue to research APP model effectiveness, embrace innovative delivery models, and support effective onboarding and career development opportunities for our NP/PA providers.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Ms. Cardin is vice president, Advanced Practice Providers, at Sound Physicians, and is a member of SHM’s Board of Directors.
References
1. “Midlevels make a rocky entrance into hospital medicine,” by Bonnie Darves, Today’s Hospitalist, January 2007.
2. “When hiring midlevels, proceed with caution,” by Jessica Berthold, ACP Hospitalist, April 2009.
3. “A Comparison of Conventional and Expanded Physician Assistant Hospitalist Staffing Models at a Community Hospital,” J Clin Outcomes Manag. 2016 Oct 1;23[10]:455-61.
Hospitalists’ scope of services continues to evolve
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
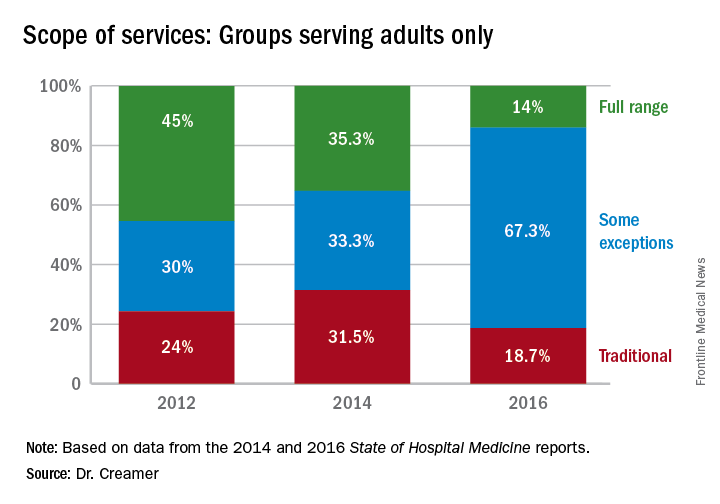
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
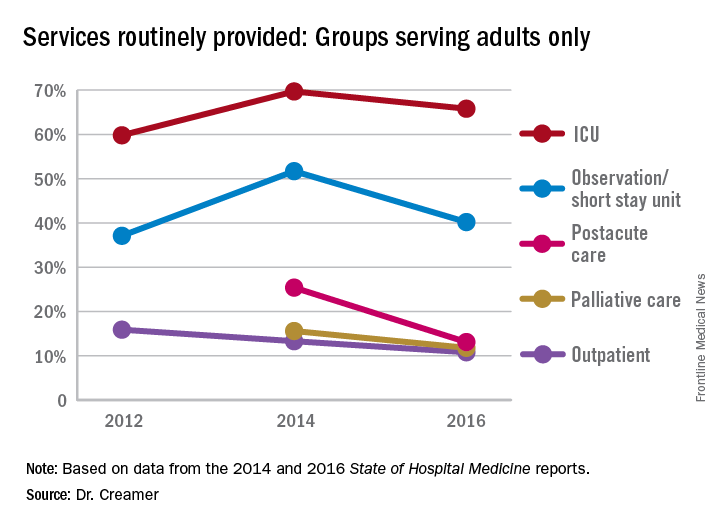
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
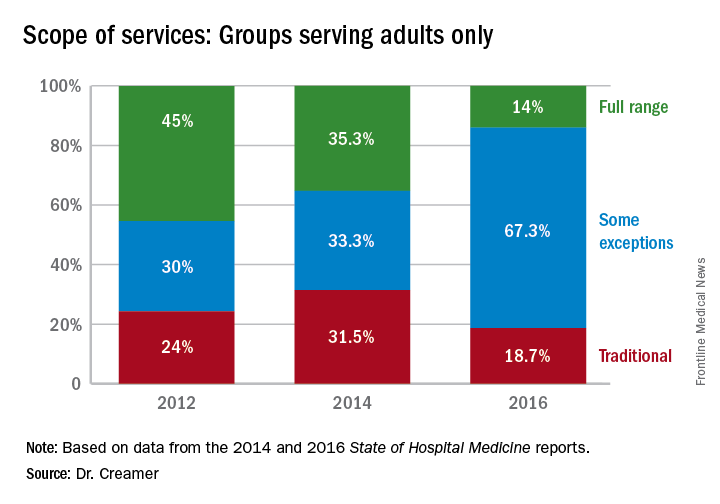
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
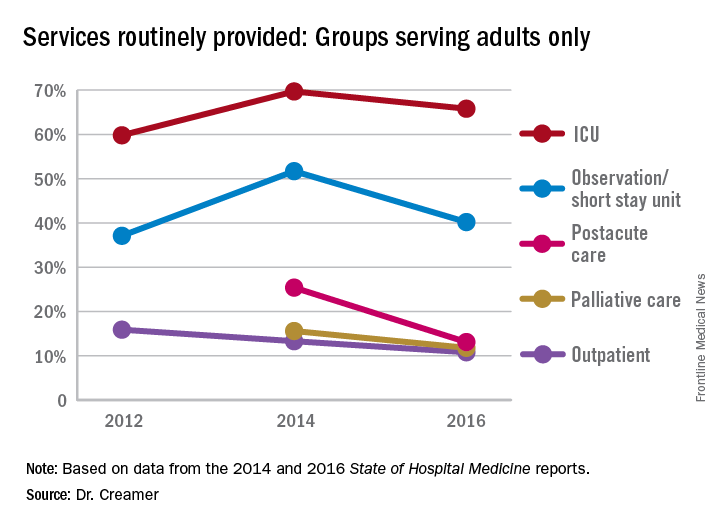
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Over the course of serial iterations of the State of Hospital Medicine (SOHM) Report, SHM has presented survey data that describe the evolving role hospitalists play in patient care. The 2016 SOHM Report shows the continuation of prior trends in hospital medicine groups’ (HMGs) scope of admittance and comanagement services. Some downturns are notable among previously increased specialty services.
The SOHM Report characterizes HMGs by their general scope of admitted patients – as admitters of purely traditional internal medicine or pediatrics hospitalized patients; full-range, nearly universal admitters who admit most patients within their age designation except OB and emergency surgery patients; or traditional admitters with some exceptions (for example, limited classically surgical patients).
As adult and adult-ped HMGs make up almost 97% of survey respondents, the predominance of the “some exceptions” category seems to represent a serious trend in much of Hospital Medicine practice. This could mean that HMGs have worked out more specific arrangements as to which patients they will admit or that the definitions are more in flux. It comes at a time when concerns figure prominently in national discussions over the stretching of hospitalists by their expanding scope of care and the need for ever more coordinated care between hospitalists and specialists.
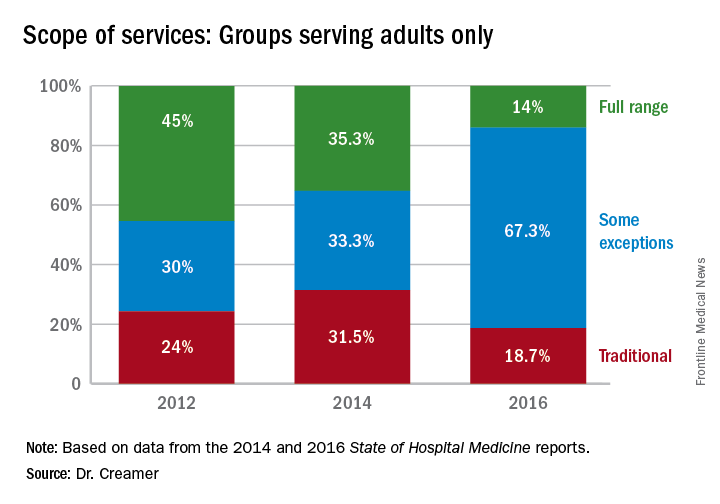
Again, with these opportunities, concerns have arisen about scope-creep and its potential deleterious effects on patient care. Hospitalists have been noted to be prodded into providing critical, geriatric, and palliative care, without specialty training in these areas.1 Interestingly, however, specialty work reported by HMGs has largely shown a downturn since 2014, when most specialty services had appeared to be on the rise.
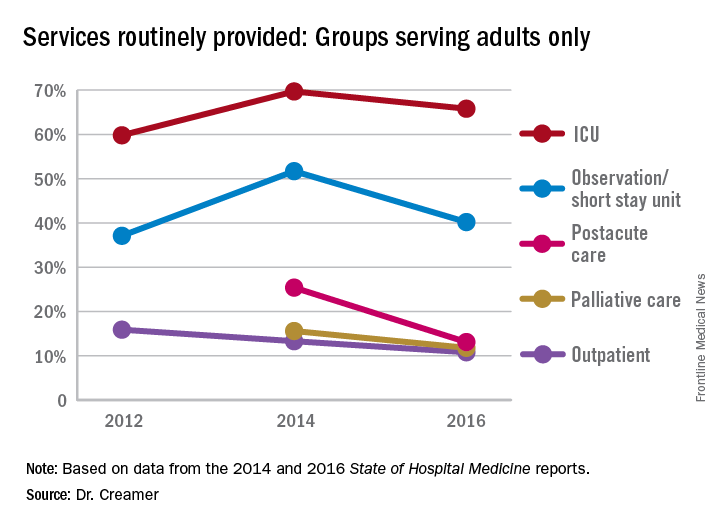
Whether this means that there is relief from scope-creep or that it is “just a blip” will remain to be seen in future data. If HMGs are able to capture the opportunity to improve outcomes through greater involvement in postacute care, this particular area may be one to watch, despite its apparent downturn since the 2014 report.
Thus, it is as imperative as ever that HMGs participate in the State of Hospital Medicine survey.
Dr. Creamer is a member of SHM’s Practice Analysis Committee. He is a hospitalist and informaticist with the MetroHealth System in Cleveland.
References
1. Wellikson, L. Hospitalists Stretched as their Responsibilities Broaden. The Hospitalist. 2016 Nov;2016(11).
Hospitalist burnout
Some things I’ve been thinking about:
- Physician well-being, morale, and burnout seem to be getting more attention in both the medical and the lay press.
- Leaders from 10 prestigious health systems and the CEO of the American Medical Association wrote a March 2017 post in the Health Affairs Blog titled “Physician Burnout is a Public Health Crisis: A Message To Our Fellow Health Care CEOs.”
- I’m now regularly hearing and reading mention of the “Quadruple Aim.” The “Triple Aim,” first described in 2008, is the pursuit of excellence in 1) patient experience – both quality of care and patient satisfaction; 2) population health; and 3) cost reduction. The November/December 2014 Annals of Family Medicine included an article recommending “that the Triple Aim be expanded to a Quadruple Aim by adding the goal of improving the work life of health care providers, including clinicians and staff.”1
- The CEO at a community hospital near me chose to make addressing physician burnout one of his top priorities and tied success in the effort to his own compensation bonus.
- In the course of my consulting work with hospitalist groups across the country, I’ve noticed a meaningful increase in the number of our colleagues who seem deeply unhappy with their work and/or burned out. The “Hospitalist Morale Index” may be a worthwhile way for a group to conduct an assessment.2
- I’m concerned that many other hospital care givers, including RNs, social workers, and others, are experiencing levels of distress and/or burnout that might be similar to that of physicians. From where I sit, they seem to be getting less attention, and I can’t tell if that is just because I’m not as immersed in their world or if it reflects reality. It’s pretty disappointing if it’s the latter.
For the most part, I think the causes of hospitalist distress and burnout are very similar to that of doctors in other specialties, and interventions to address the problem can be similar across specialties. Yet, each specialty probably differs in ways that are important to keep in mind.
Hospitalists also bear a huge burden related to observation status. Doctors in most other specialties rarely face complex decisions regarding whether observation is the right choice and are not so often the target of patient/family frustration and anger related to it.
Those seeking to address hospitalist burnout and well-being specifically should keep in mind these uniquely hospitalist issues. I think of them as a chronic disease to manage and mitigate, since “curing” them (making them go away entirely) is probably impossible for the foreseeable future.
What to do?
An Internet search on physician burnout, or other terms related to well-being, will yield more articles with advice to address the problem than you’ll ever have time to read. Trying to read all of them would likely lead to burnout! I think interventions can be divided into two broad categories: organizational efforts and personal efforts.
Like the 10 CEOs mentioned above, health care leaders should acknowledge physician distress and burnout as a meaningful issue that can impede organizational performance and that investments to address it can have a meaningful return on investment. The Health Affairs Blog post listed 11 things the CEOs committed to doing. It’s a list anyone working on this issue should review.
Doctors at The Mayo Clinic have published a great deal of research on physician burnout. In the March 7, 2017, JAMA, (summarized in a YouTube video) they describe several worthwhile organizational changes, as well as some personal strategies.3 They wrote about their experiences with interventions such as a deliberate curriculum to train doctors in self-care (self-reflection, mindfulness, etc.) in a series of one-hour lectures over several months.4 In November 2016, they published a meta-analysis of interventions to address burnout.5
In total, all of the worthwhile recommendations to address burnout leave me feeling like they’re a lot of work, and any individual intervention may not be as helpful as hoped, so that the best way to approach this is with a collection of interventions. In many ways, it is similar to the problem of readmissions: There is a lot of research out there, it’s hard to prove that any single intervention really works, and success lies in implementing a broad set of interventions. And success doesn’t equate to eliminating readmissions, only reducing them.
Coda: Is a sabbatical uniquely valuable for hospitalists?
I think a sabbatical might be a good idea for hospitalists. It also seems practical for other doctors, such as radiologists, anesthesiologists, and ED doctors, who don’t have 1:1 continuity relationships with patients. However, it is problematic for primary care doctors and specialists who need to maintain continuity relationships with patients and referring doctors that could be disrupted by a lengthy absence.
I’m not sure a sabbatical would reduce burnout much on its own, but, if properly structured, it seems very likely to reduce staffing turnover, and the sabbatical could be spent in ways that help rejuvenate interest and satisfaction in our work rather than simply taking a long vacation to travel and play golf, etc. It should probably be at least 3 months and better if it lasts a year. A common arrangement is that a doctor becomes eligible for the sabbatical after 10 years and is paid half of her usual compensation while away. I’d like to see more hospitalist groups do this.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Write to [email protected].
References
1. Bodenheimer, T and Sninsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann Fam Med. Nov/Dec 2014.
2. Chandra, S et al. Introducing the Hospitalist Morale Index: A New Tool That May Be Relevant for Improving Provider Retention. JHM. June 2016.
3. Shanafelt, T, Dyrbye, L, West, C. Addressing Physician Burnout: The Way Forward. JAMA. March 7, 2017.
4. West, C et al. Intervention to Promote Physician Well-being, Job Satisfaction, and Professionalism: A Randomized Clinical Trial. JAMA Intern Med. 2014;174(4):527-33.
5. West, C et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. The Lancet. Nov 5, 2016.
Some things I’ve been thinking about:
- Physician well-being, morale, and burnout seem to be getting more attention in both the medical and the lay press.
- Leaders from 10 prestigious health systems and the CEO of the American Medical Association wrote a March 2017 post in the Health Affairs Blog titled “Physician Burnout is a Public Health Crisis: A Message To Our Fellow Health Care CEOs.”
- I’m now regularly hearing and reading mention of the “Quadruple Aim.” The “Triple Aim,” first described in 2008, is the pursuit of excellence in 1) patient experience – both quality of care and patient satisfaction; 2) population health; and 3) cost reduction. The November/December 2014 Annals of Family Medicine included an article recommending “that the Triple Aim be expanded to a Quadruple Aim by adding the goal of improving the work life of health care providers, including clinicians and staff.”1
- The CEO at a community hospital near me chose to make addressing physician burnout one of his top priorities and tied success in the effort to his own compensation bonus.
- In the course of my consulting work with hospitalist groups across the country, I’ve noticed a meaningful increase in the number of our colleagues who seem deeply unhappy with their work and/or burned out. The “Hospitalist Morale Index” may be a worthwhile way for a group to conduct an assessment.2
- I’m concerned that many other hospital care givers, including RNs, social workers, and others, are experiencing levels of distress and/or burnout that might be similar to that of physicians. From where I sit, they seem to be getting less attention, and I can’t tell if that is just because I’m not as immersed in their world or if it reflects reality. It’s pretty disappointing if it’s the latter.
For the most part, I think the causes of hospitalist distress and burnout are very similar to that of doctors in other specialties, and interventions to address the problem can be similar across specialties. Yet, each specialty probably differs in ways that are important to keep in mind.
Hospitalists also bear a huge burden related to observation status. Doctors in most other specialties rarely face complex decisions regarding whether observation is the right choice and are not so often the target of patient/family frustration and anger related to it.
Those seeking to address hospitalist burnout and well-being specifically should keep in mind these uniquely hospitalist issues. I think of them as a chronic disease to manage and mitigate, since “curing” them (making them go away entirely) is probably impossible for the foreseeable future.
What to do?
An Internet search on physician burnout, or other terms related to well-being, will yield more articles with advice to address the problem than you’ll ever have time to read. Trying to read all of them would likely lead to burnout! I think interventions can be divided into two broad categories: organizational efforts and personal efforts.
Like the 10 CEOs mentioned above, health care leaders should acknowledge physician distress and burnout as a meaningful issue that can impede organizational performance and that investments to address it can have a meaningful return on investment. The Health Affairs Blog post listed 11 things the CEOs committed to doing. It’s a list anyone working on this issue should review.
Doctors at The Mayo Clinic have published a great deal of research on physician burnout. In the March 7, 2017, JAMA, (summarized in a YouTube video) they describe several worthwhile organizational changes, as well as some personal strategies.3 They wrote about their experiences with interventions such as a deliberate curriculum to train doctors in self-care (self-reflection, mindfulness, etc.) in a series of one-hour lectures over several months.4 In November 2016, they published a meta-analysis of interventions to address burnout.5
In total, all of the worthwhile recommendations to address burnout leave me feeling like they’re a lot of work, and any individual intervention may not be as helpful as hoped, so that the best way to approach this is with a collection of interventions. In many ways, it is similar to the problem of readmissions: There is a lot of research out there, it’s hard to prove that any single intervention really works, and success lies in implementing a broad set of interventions. And success doesn’t equate to eliminating readmissions, only reducing them.
Coda: Is a sabbatical uniquely valuable for hospitalists?
I think a sabbatical might be a good idea for hospitalists. It also seems practical for other doctors, such as radiologists, anesthesiologists, and ED doctors, who don’t have 1:1 continuity relationships with patients. However, it is problematic for primary care doctors and specialists who need to maintain continuity relationships with patients and referring doctors that could be disrupted by a lengthy absence.
I’m not sure a sabbatical would reduce burnout much on its own, but, if properly structured, it seems very likely to reduce staffing turnover, and the sabbatical could be spent in ways that help rejuvenate interest and satisfaction in our work rather than simply taking a long vacation to travel and play golf, etc. It should probably be at least 3 months and better if it lasts a year. A common arrangement is that a doctor becomes eligible for the sabbatical after 10 years and is paid half of her usual compensation while away. I’d like to see more hospitalist groups do this.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Write to [email protected].
References
1. Bodenheimer, T and Sninsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann Fam Med. Nov/Dec 2014.
2. Chandra, S et al. Introducing the Hospitalist Morale Index: A New Tool That May Be Relevant for Improving Provider Retention. JHM. June 2016.
3. Shanafelt, T, Dyrbye, L, West, C. Addressing Physician Burnout: The Way Forward. JAMA. March 7, 2017.
4. West, C et al. Intervention to Promote Physician Well-being, Job Satisfaction, and Professionalism: A Randomized Clinical Trial. JAMA Intern Med. 2014;174(4):527-33.
5. West, C et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. The Lancet. Nov 5, 2016.
Some things I’ve been thinking about:
- Physician well-being, morale, and burnout seem to be getting more attention in both the medical and the lay press.
- Leaders from 10 prestigious health systems and the CEO of the American Medical Association wrote a March 2017 post in the Health Affairs Blog titled “Physician Burnout is a Public Health Crisis: A Message To Our Fellow Health Care CEOs.”
- I’m now regularly hearing and reading mention of the “Quadruple Aim.” The “Triple Aim,” first described in 2008, is the pursuit of excellence in 1) patient experience – both quality of care and patient satisfaction; 2) population health; and 3) cost reduction. The November/December 2014 Annals of Family Medicine included an article recommending “that the Triple Aim be expanded to a Quadruple Aim by adding the goal of improving the work life of health care providers, including clinicians and staff.”1
- The CEO at a community hospital near me chose to make addressing physician burnout one of his top priorities and tied success in the effort to his own compensation bonus.
- In the course of my consulting work with hospitalist groups across the country, I’ve noticed a meaningful increase in the number of our colleagues who seem deeply unhappy with their work and/or burned out. The “Hospitalist Morale Index” may be a worthwhile way for a group to conduct an assessment.2
- I’m concerned that many other hospital care givers, including RNs, social workers, and others, are experiencing levels of distress and/or burnout that might be similar to that of physicians. From where I sit, they seem to be getting less attention, and I can’t tell if that is just because I’m not as immersed in their world or if it reflects reality. It’s pretty disappointing if it’s the latter.
For the most part, I think the causes of hospitalist distress and burnout are very similar to that of doctors in other specialties, and interventions to address the problem can be similar across specialties. Yet, each specialty probably differs in ways that are important to keep in mind.
Hospitalists also bear a huge burden related to observation status. Doctors in most other specialties rarely face complex decisions regarding whether observation is the right choice and are not so often the target of patient/family frustration and anger related to it.
Those seeking to address hospitalist burnout and well-being specifically should keep in mind these uniquely hospitalist issues. I think of them as a chronic disease to manage and mitigate, since “curing” them (making them go away entirely) is probably impossible for the foreseeable future.
What to do?
An Internet search on physician burnout, or other terms related to well-being, will yield more articles with advice to address the problem than you’ll ever have time to read. Trying to read all of them would likely lead to burnout! I think interventions can be divided into two broad categories: organizational efforts and personal efforts.
Like the 10 CEOs mentioned above, health care leaders should acknowledge physician distress and burnout as a meaningful issue that can impede organizational performance and that investments to address it can have a meaningful return on investment. The Health Affairs Blog post listed 11 things the CEOs committed to doing. It’s a list anyone working on this issue should review.
Doctors at The Mayo Clinic have published a great deal of research on physician burnout. In the March 7, 2017, JAMA, (summarized in a YouTube video) they describe several worthwhile organizational changes, as well as some personal strategies.3 They wrote about their experiences with interventions such as a deliberate curriculum to train doctors in self-care (self-reflection, mindfulness, etc.) in a series of one-hour lectures over several months.4 In November 2016, they published a meta-analysis of interventions to address burnout.5
In total, all of the worthwhile recommendations to address burnout leave me feeling like they’re a lot of work, and any individual intervention may not be as helpful as hoped, so that the best way to approach this is with a collection of interventions. In many ways, it is similar to the problem of readmissions: There is a lot of research out there, it’s hard to prove that any single intervention really works, and success lies in implementing a broad set of interventions. And success doesn’t equate to eliminating readmissions, only reducing them.
Coda: Is a sabbatical uniquely valuable for hospitalists?
I think a sabbatical might be a good idea for hospitalists. It also seems practical for other doctors, such as radiologists, anesthesiologists, and ED doctors, who don’t have 1:1 continuity relationships with patients. However, it is problematic for primary care doctors and specialists who need to maintain continuity relationships with patients and referring doctors that could be disrupted by a lengthy absence.
I’m not sure a sabbatical would reduce burnout much on its own, but, if properly structured, it seems very likely to reduce staffing turnover, and the sabbatical could be spent in ways that help rejuvenate interest and satisfaction in our work rather than simply taking a long vacation to travel and play golf, etc. It should probably be at least 3 months and better if it lasts a year. A common arrangement is that a doctor becomes eligible for the sabbatical after 10 years and is paid half of her usual compensation while away. I’d like to see more hospitalist groups do this.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Write to [email protected].
References
1. Bodenheimer, T and Sninsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann Fam Med. Nov/Dec 2014.
2. Chandra, S et al. Introducing the Hospitalist Morale Index: A New Tool That May Be Relevant for Improving Provider Retention. JHM. June 2016.
3. Shanafelt, T, Dyrbye, L, West, C. Addressing Physician Burnout: The Way Forward. JAMA. March 7, 2017.
4. West, C et al. Intervention to Promote Physician Well-being, Job Satisfaction, and Professionalism: A Randomized Clinical Trial. JAMA Intern Med. 2014;174(4):527-33.
5. West, C et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. The Lancet. Nov 5, 2016.
From hospitalist to health plan CMO
Several times a year, I’m privileged to step away from my role as chief medical officer of a health insurance company and return to a previous role I cherish – teaching.
This isn’t the clinical teaching that I used to do as a hospital medicine attending or palliative medicine consultant. These are mostly 4th-year medical students who have 90 minutes or so set aside during their primary care rotation to learn about “the business of medicine.”
I always begin by telling them that when I went to medical school, “I always intended to become a health insurance executive – NOT!” (If I get a few laughs, I know the time will fly by.) I share the history of my improbable career arc and how I wound up doing something I didn’t even know existed when I was their age. And, I still try to impart some pearls of wisdom in case they remember any of this discussion as they embark on their own personal and professional journeys, knowing that at this stage in their young careers, they will be almost totally immersed in their clinical training.
1. Do what you love
Sounds simple, but too many of us make the expedient choice, or the one expected of us. Work is hard enough without being able to find some joy and meaning every day in what you do. Every job has aspects that must be tolerated, but if you don’t find a greater purpose in practicing medicine, then find a way to get it back – or think about doing something else.
2. When opportunity knocks, be prepared to answer the door
For me, I enjoyed caring for patients one at a time, perhaps 15 or so during any particular day. Being a hospitalist is important and fulfilling work. But my experience as a hospitalist enabled me to recognize the “quality chasms” that existed in my hospital and across the “system,” namely lost opportunities to provide better end-of-life care and to better coordinate care within the hospital and across the care continuum. A new mission evolved for me: to do whatever I could to improve the safety, quality, and efficiency of the care we provided, and to make the hospital a better place to work. I taught myself the clinical skills to practice palliative medicine, and I attended courses that helped me prepare to become a service line medical director in hopes of starting a program at my hospital. I also took on the role of medical director of care management at my hospital, which in a sense allowed me to help take care of several hundred patients at a time – the beginning of my transition to population health.
3. Be a lifelong learner
When these opportunities arose, I was prepared for the challenges thanks to training opportunities I actively sought out, and thanks to the support of my mentors and my medical group to attend leadership training, such as SHM’s Leadership Academy. No matter what your role in your group or at your hospital, gaining these valuable skills outside of the usual medical training will help position you for new opportunities that can only help you create a more sustainable career. And although I never went back to school to earn another advanced degree such as an MBA or MHA, additional formal education is something to consider. You can never have too many tools in your toolkit.
4. Diversify!
It’s good advice from your financial adviser, and it’s good advice for your career. I’m not suggesting you take on a side job as a lawyer or a carpenter, but you might want to think about becoming an expert in a related field like perioperative medicine, primary palliative care, or postacute care. Or consider developing a niche as a sought-after leader for hospital-based committees, such as Quality or P&T. Or maybe consider clinical research, even if you’re not at an academic medical center. The point I’m making – and I know this may seem controversial – is that practicing medicine 100% of the time is probably no longer a sustainable plan for the entire 30- to 40-year span of your postgraduate career. Find an area that you can develop into protected, paid time apart from providing direct clinical care.
5. If you are thinking of changing jobs or even careers, run toward something – not away from something else
When I was first recruited to be a medical director at another health plan, I struggled mightily as to whether leaving full-time practice was an opportunity or a foolish, dead-end career move. Ultimately, I made my decision not to avoid night call or working every other weekend; I did it because I felt I had made a difference in the hospital where I had worked for 15 years and was ready to take on a new challenge by learning the business side of health care. It provided me the opportunity to positively impact the care of not just several hundred patients, but as many as two million! My current position now allows me to have even greater influence in pursuing my personal mission to improve the quality, safety, and affordability of health care.
6. Seek balance in life
Again, sounds trite, but think about it. Most health care professionals, especially physicians, have spent most of their adult lives focused on a single goal – and that often comes at a great cost, both financially and personally. (By the way, I say “seek” because at this point in my career, I doubt any of us ever really find balance.) The best you can hope for is to be wise enough to know that amongst all the balls we are juggling, there are a few that you just can’t let drop without possibly breaking without repair.
As I conclude my talks, I tell those young medical students to practice resiliency; the only constant is change. Remain inquisitive, open yourself to whatever life may bring and enjoy the ride. With a specialty as dynamic and diverse as hospital medicine, you never know where it will take you.
Dr. Epstein is executive vice president & chief medical officer at PreferredOne, and adjunct assistant professor of medicine at the University of Minnesota, Minneapolis. He also serves as Board Secretary of SHM.
Several times a year, I’m privileged to step away from my role as chief medical officer of a health insurance company and return to a previous role I cherish – teaching.
This isn’t the clinical teaching that I used to do as a hospital medicine attending or palliative medicine consultant. These are mostly 4th-year medical students who have 90 minutes or so set aside during their primary care rotation to learn about “the business of medicine.”
I always begin by telling them that when I went to medical school, “I always intended to become a health insurance executive – NOT!” (If I get a few laughs, I know the time will fly by.) I share the history of my improbable career arc and how I wound up doing something I didn’t even know existed when I was their age. And, I still try to impart some pearls of wisdom in case they remember any of this discussion as they embark on their own personal and professional journeys, knowing that at this stage in their young careers, they will be almost totally immersed in their clinical training.
1. Do what you love
Sounds simple, but too many of us make the expedient choice, or the one expected of us. Work is hard enough without being able to find some joy and meaning every day in what you do. Every job has aspects that must be tolerated, but if you don’t find a greater purpose in practicing medicine, then find a way to get it back – or think about doing something else.
2. When opportunity knocks, be prepared to answer the door
For me, I enjoyed caring for patients one at a time, perhaps 15 or so during any particular day. Being a hospitalist is important and fulfilling work. But my experience as a hospitalist enabled me to recognize the “quality chasms” that existed in my hospital and across the “system,” namely lost opportunities to provide better end-of-life care and to better coordinate care within the hospital and across the care continuum. A new mission evolved for me: to do whatever I could to improve the safety, quality, and efficiency of the care we provided, and to make the hospital a better place to work. I taught myself the clinical skills to practice palliative medicine, and I attended courses that helped me prepare to become a service line medical director in hopes of starting a program at my hospital. I also took on the role of medical director of care management at my hospital, which in a sense allowed me to help take care of several hundred patients at a time – the beginning of my transition to population health.
3. Be a lifelong learner
When these opportunities arose, I was prepared for the challenges thanks to training opportunities I actively sought out, and thanks to the support of my mentors and my medical group to attend leadership training, such as SHM’s Leadership Academy. No matter what your role in your group or at your hospital, gaining these valuable skills outside of the usual medical training will help position you for new opportunities that can only help you create a more sustainable career. And although I never went back to school to earn another advanced degree such as an MBA or MHA, additional formal education is something to consider. You can never have too many tools in your toolkit.
4. Diversify!
It’s good advice from your financial adviser, and it’s good advice for your career. I’m not suggesting you take on a side job as a lawyer or a carpenter, but you might want to think about becoming an expert in a related field like perioperative medicine, primary palliative care, or postacute care. Or consider developing a niche as a sought-after leader for hospital-based committees, such as Quality or P&T. Or maybe consider clinical research, even if you’re not at an academic medical center. The point I’m making – and I know this may seem controversial – is that practicing medicine 100% of the time is probably no longer a sustainable plan for the entire 30- to 40-year span of your postgraduate career. Find an area that you can develop into protected, paid time apart from providing direct clinical care.
5. If you are thinking of changing jobs or even careers, run toward something – not away from something else
When I was first recruited to be a medical director at another health plan, I struggled mightily as to whether leaving full-time practice was an opportunity or a foolish, dead-end career move. Ultimately, I made my decision not to avoid night call or working every other weekend; I did it because I felt I had made a difference in the hospital where I had worked for 15 years and was ready to take on a new challenge by learning the business side of health care. It provided me the opportunity to positively impact the care of not just several hundred patients, but as many as two million! My current position now allows me to have even greater influence in pursuing my personal mission to improve the quality, safety, and affordability of health care.
6. Seek balance in life
Again, sounds trite, but think about it. Most health care professionals, especially physicians, have spent most of their adult lives focused on a single goal – and that often comes at a great cost, both financially and personally. (By the way, I say “seek” because at this point in my career, I doubt any of us ever really find balance.) The best you can hope for is to be wise enough to know that amongst all the balls we are juggling, there are a few that you just can’t let drop without possibly breaking without repair.
As I conclude my talks, I tell those young medical students to practice resiliency; the only constant is change. Remain inquisitive, open yourself to whatever life may bring and enjoy the ride. With a specialty as dynamic and diverse as hospital medicine, you never know where it will take you.
Dr. Epstein is executive vice president & chief medical officer at PreferredOne, and adjunct assistant professor of medicine at the University of Minnesota, Minneapolis. He also serves as Board Secretary of SHM.
Several times a year, I’m privileged to step away from my role as chief medical officer of a health insurance company and return to a previous role I cherish – teaching.
This isn’t the clinical teaching that I used to do as a hospital medicine attending or palliative medicine consultant. These are mostly 4th-year medical students who have 90 minutes or so set aside during their primary care rotation to learn about “the business of medicine.”
I always begin by telling them that when I went to medical school, “I always intended to become a health insurance executive – NOT!” (If I get a few laughs, I know the time will fly by.) I share the history of my improbable career arc and how I wound up doing something I didn’t even know existed when I was their age. And, I still try to impart some pearls of wisdom in case they remember any of this discussion as they embark on their own personal and professional journeys, knowing that at this stage in their young careers, they will be almost totally immersed in their clinical training.
1. Do what you love
Sounds simple, but too many of us make the expedient choice, or the one expected of us. Work is hard enough without being able to find some joy and meaning every day in what you do. Every job has aspects that must be tolerated, but if you don’t find a greater purpose in practicing medicine, then find a way to get it back – or think about doing something else.
2. When opportunity knocks, be prepared to answer the door
For me, I enjoyed caring for patients one at a time, perhaps 15 or so during any particular day. Being a hospitalist is important and fulfilling work. But my experience as a hospitalist enabled me to recognize the “quality chasms” that existed in my hospital and across the “system,” namely lost opportunities to provide better end-of-life care and to better coordinate care within the hospital and across the care continuum. A new mission evolved for me: to do whatever I could to improve the safety, quality, and efficiency of the care we provided, and to make the hospital a better place to work. I taught myself the clinical skills to practice palliative medicine, and I attended courses that helped me prepare to become a service line medical director in hopes of starting a program at my hospital. I also took on the role of medical director of care management at my hospital, which in a sense allowed me to help take care of several hundred patients at a time – the beginning of my transition to population health.
3. Be a lifelong learner
When these opportunities arose, I was prepared for the challenges thanks to training opportunities I actively sought out, and thanks to the support of my mentors and my medical group to attend leadership training, such as SHM’s Leadership Academy. No matter what your role in your group or at your hospital, gaining these valuable skills outside of the usual medical training will help position you for new opportunities that can only help you create a more sustainable career. And although I never went back to school to earn another advanced degree such as an MBA or MHA, additional formal education is something to consider. You can never have too many tools in your toolkit.
4. Diversify!
It’s good advice from your financial adviser, and it’s good advice for your career. I’m not suggesting you take on a side job as a lawyer or a carpenter, but you might want to think about becoming an expert in a related field like perioperative medicine, primary palliative care, or postacute care. Or consider developing a niche as a sought-after leader for hospital-based committees, such as Quality or P&T. Or maybe consider clinical research, even if you’re not at an academic medical center. The point I’m making – and I know this may seem controversial – is that practicing medicine 100% of the time is probably no longer a sustainable plan for the entire 30- to 40-year span of your postgraduate career. Find an area that you can develop into protected, paid time apart from providing direct clinical care.
5. If you are thinking of changing jobs or even careers, run toward something – not away from something else
When I was first recruited to be a medical director at another health plan, I struggled mightily as to whether leaving full-time practice was an opportunity or a foolish, dead-end career move. Ultimately, I made my decision not to avoid night call or working every other weekend; I did it because I felt I had made a difference in the hospital where I had worked for 15 years and was ready to take on a new challenge by learning the business side of health care. It provided me the opportunity to positively impact the care of not just several hundred patients, but as many as two million! My current position now allows me to have even greater influence in pursuing my personal mission to improve the quality, safety, and affordability of health care.
6. Seek balance in life
Again, sounds trite, but think about it. Most health care professionals, especially physicians, have spent most of their adult lives focused on a single goal – and that often comes at a great cost, both financially and personally. (By the way, I say “seek” because at this point in my career, I doubt any of us ever really find balance.) The best you can hope for is to be wise enough to know that amongst all the balls we are juggling, there are a few that you just can’t let drop without possibly breaking without repair.
As I conclude my talks, I tell those young medical students to practice resiliency; the only constant is change. Remain inquisitive, open yourself to whatever life may bring and enjoy the ride. With a specialty as dynamic and diverse as hospital medicine, you never know where it will take you.
Dr. Epstein is executive vice president & chief medical officer at PreferredOne, and adjunct assistant professor of medicine at the University of Minnesota, Minneapolis. He also serves as Board Secretary of SHM.