User login
Movers and Shakers in Hospital Medicine December 2015
John Carlile, MD, is the new medical director of pediatric hospitalist and intensivist services at Summerville (S.C.) Medical Center. Most recently, Dr. Carlile worked as a pediatric critical care specialist at Cox Medical Center in Springfield, Mo.

Elaine McElveen, RN, has been named director of the hospitalist program at McLeod Medical Center Dillon in Dillon, S.C. In her new role, McElveen also will oversee the case management department. She has been a practicing nurse for the McLeod Health system for 28 years.

Christine Wentt, PA, an adult hospitalist physician assistant, has been inducted into the VIP Woman of the Year Circle for 2015-2016 by the National Association of Professional Women (NAPW). Wentt works for Physicians Inpatient Care Specialists (MDICS), a private hospitalist group in Glen Burnie, Md. Wentt also serves as an adjunct professor in Drexel University’s physician assistant program.
Robert Zurcher, MD, has been appointed chief medical officer for emergency medicine at HNI Healthcare (formerly Hospitalists Now, Inc.), based in Austin, Texas. Dr. Zurcher comes to HNI Healthcare from IPC Healthcare, where he served as the administrative director for their Northwest Region. Dr. Zurcher has 27 years of practice experience and has founded and managed physician services companies in both hospital medicine and emergency medicine.
Business Moves
North Hollywood, Calif.-based IPC Healthcare recently announced its acquisition of Hospital Medicine Consultants, LLC, in Elgin, Ill., a locally owned practice serving several hospitals in the Chicago suburbs. IPC staffs hospitalist providers in more than 400 hospitals across the country.
The Schumacher Group, a private hospitalist and emergency medicine provider, announced the implementation of a new telehospitalist program at Abrom Kaplan Memorial and Acadia General Hospitals, both in Lafayette, La. The program will allow physicians to provide overnight care to the two facilities from a remote location. The Schumacher Group was founded in 1994 and currently serves more than four million patients per year.
Mike O’Neal is a freelance writer in New York City.
John Carlile, MD, is the new medical director of pediatric hospitalist and intensivist services at Summerville (S.C.) Medical Center. Most recently, Dr. Carlile worked as a pediatric critical care specialist at Cox Medical Center in Springfield, Mo.

Elaine McElveen, RN, has been named director of the hospitalist program at McLeod Medical Center Dillon in Dillon, S.C. In her new role, McElveen also will oversee the case management department. She has been a practicing nurse for the McLeod Health system for 28 years.

Christine Wentt, PA, an adult hospitalist physician assistant, has been inducted into the VIP Woman of the Year Circle for 2015-2016 by the National Association of Professional Women (NAPW). Wentt works for Physicians Inpatient Care Specialists (MDICS), a private hospitalist group in Glen Burnie, Md. Wentt also serves as an adjunct professor in Drexel University’s physician assistant program.
Robert Zurcher, MD, has been appointed chief medical officer for emergency medicine at HNI Healthcare (formerly Hospitalists Now, Inc.), based in Austin, Texas. Dr. Zurcher comes to HNI Healthcare from IPC Healthcare, where he served as the administrative director for their Northwest Region. Dr. Zurcher has 27 years of practice experience and has founded and managed physician services companies in both hospital medicine and emergency medicine.
Business Moves
North Hollywood, Calif.-based IPC Healthcare recently announced its acquisition of Hospital Medicine Consultants, LLC, in Elgin, Ill., a locally owned practice serving several hospitals in the Chicago suburbs. IPC staffs hospitalist providers in more than 400 hospitals across the country.
The Schumacher Group, a private hospitalist and emergency medicine provider, announced the implementation of a new telehospitalist program at Abrom Kaplan Memorial and Acadia General Hospitals, both in Lafayette, La. The program will allow physicians to provide overnight care to the two facilities from a remote location. The Schumacher Group was founded in 1994 and currently serves more than four million patients per year.
Mike O’Neal is a freelance writer in New York City.
John Carlile, MD, is the new medical director of pediatric hospitalist and intensivist services at Summerville (S.C.) Medical Center. Most recently, Dr. Carlile worked as a pediatric critical care specialist at Cox Medical Center in Springfield, Mo.

Elaine McElveen, RN, has been named director of the hospitalist program at McLeod Medical Center Dillon in Dillon, S.C. In her new role, McElveen also will oversee the case management department. She has been a practicing nurse for the McLeod Health system for 28 years.

Christine Wentt, PA, an adult hospitalist physician assistant, has been inducted into the VIP Woman of the Year Circle for 2015-2016 by the National Association of Professional Women (NAPW). Wentt works for Physicians Inpatient Care Specialists (MDICS), a private hospitalist group in Glen Burnie, Md. Wentt also serves as an adjunct professor in Drexel University’s physician assistant program.
Robert Zurcher, MD, has been appointed chief medical officer for emergency medicine at HNI Healthcare (formerly Hospitalists Now, Inc.), based in Austin, Texas. Dr. Zurcher comes to HNI Healthcare from IPC Healthcare, where he served as the administrative director for their Northwest Region. Dr. Zurcher has 27 years of practice experience and has founded and managed physician services companies in both hospital medicine and emergency medicine.
Business Moves
North Hollywood, Calif.-based IPC Healthcare recently announced its acquisition of Hospital Medicine Consultants, LLC, in Elgin, Ill., a locally owned practice serving several hospitals in the Chicago suburbs. IPC staffs hospitalist providers in more than 400 hospitals across the country.
The Schumacher Group, a private hospitalist and emergency medicine provider, announced the implementation of a new telehospitalist program at Abrom Kaplan Memorial and Acadia General Hospitals, both in Lafayette, La. The program will allow physicians to provide overnight care to the two facilities from a remote location. The Schumacher Group was founded in 1994 and currently serves more than four million patients per year.
Mike O’Neal is a freelance writer in New York City.
Listen Now: Society of Hospital Medicine's Student Hospitalists Discuss Future of Specialty
Two medical students who participated in SHM's inaugural Student Hospitalist program, Mimi Zander, now a second year student at Touro College of Osteopathic Medicine in New York City, and Frank Zadravecz, a second year student at the University of Illinois College of Medicine at Chicago, share their thoughts about their part in the future of hospital medicine.
Two medical students who participated in SHM's inaugural Student Hospitalist program, Mimi Zander, now a second year student at Touro College of Osteopathic Medicine in New York City, and Frank Zadravecz, a second year student at the University of Illinois College of Medicine at Chicago, share their thoughts about their part in the future of hospital medicine.
Two medical students who participated in SHM's inaugural Student Hospitalist program, Mimi Zander, now a second year student at Touro College of Osteopathic Medicine in New York City, and Frank Zadravecz, a second year student at the University of Illinois College of Medicine at Chicago, share their thoughts about their part in the future of hospital medicine.
Society of Hospital Medicine Resources Provide Quality Improvement Tips
Whether you’ve been tasked with leading a major quality improvement program or simply want to make a few things better for your patients, SHM has resources for every scale of quality improvement initiative, all created by national experts in their fields.
1. Attend an SHM Quality Improvement Webinar
The last of SHM’s live quality improvement webinars, “Elevating Provider Experience to Improve Patient Experience,” will be presented at 2 p.m. EST on Nov. 11, by Mark Rudolph, MD, SFHM. You can visit the archives of our other quality improvement webinars on topics like improving patient discharge, managing diabetes in the hospital, and general principles of quality improvement.
2. Tune in to RADEO: SHM’s New Opioid Stewardship Mentored Implementation Program
SHM has introduced RADEO: Reducing Adverse Drug Events related to Opioids, a new implementation guide and mentored implementation program designed to empower hospitalists to make opioid prescribing safer, with fewer adverse events, and much less likely to result in dangerous sedation, respiratory depression, and death.
SHM is recruiting now for participants in the mentored implementation program, and the guide is available online.
3. Download a New QI Resource
When you download a quality improvement toolkit or resource from SHM, you can be confident you are getting the best guidance from the national authorities on improving care for hospitalized patients.
SHM provides materials on the most pressing issues in hospital medicine, including:
- End-of-life care;
- Opioid monitoring;
- Antibiotic stewardship;
- Post-acute care;
- Veinous thromboembolism (VTE);
- Pain management; and
- Congestive heart failure (CHF).
To download, visit www.hospitalmedicine.org/qi.
Whether you’ve been tasked with leading a major quality improvement program or simply want to make a few things better for your patients, SHM has resources for every scale of quality improvement initiative, all created by national experts in their fields.
1. Attend an SHM Quality Improvement Webinar
The last of SHM’s live quality improvement webinars, “Elevating Provider Experience to Improve Patient Experience,” will be presented at 2 p.m. EST on Nov. 11, by Mark Rudolph, MD, SFHM. You can visit the archives of our other quality improvement webinars on topics like improving patient discharge, managing diabetes in the hospital, and general principles of quality improvement.
2. Tune in to RADEO: SHM’s New Opioid Stewardship Mentored Implementation Program
SHM has introduced RADEO: Reducing Adverse Drug Events related to Opioids, a new implementation guide and mentored implementation program designed to empower hospitalists to make opioid prescribing safer, with fewer adverse events, and much less likely to result in dangerous sedation, respiratory depression, and death.
SHM is recruiting now for participants in the mentored implementation program, and the guide is available online.
3. Download a New QI Resource
When you download a quality improvement toolkit or resource from SHM, you can be confident you are getting the best guidance from the national authorities on improving care for hospitalized patients.
SHM provides materials on the most pressing issues in hospital medicine, including:
- End-of-life care;
- Opioid monitoring;
- Antibiotic stewardship;
- Post-acute care;
- Veinous thromboembolism (VTE);
- Pain management; and
- Congestive heart failure (CHF).
To download, visit www.hospitalmedicine.org/qi.
Whether you’ve been tasked with leading a major quality improvement program or simply want to make a few things better for your patients, SHM has resources for every scale of quality improvement initiative, all created by national experts in their fields.
1. Attend an SHM Quality Improvement Webinar
The last of SHM’s live quality improvement webinars, “Elevating Provider Experience to Improve Patient Experience,” will be presented at 2 p.m. EST on Nov. 11, by Mark Rudolph, MD, SFHM. You can visit the archives of our other quality improvement webinars on topics like improving patient discharge, managing diabetes in the hospital, and general principles of quality improvement.
2. Tune in to RADEO: SHM’s New Opioid Stewardship Mentored Implementation Program
SHM has introduced RADEO: Reducing Adverse Drug Events related to Opioids, a new implementation guide and mentored implementation program designed to empower hospitalists to make opioid prescribing safer, with fewer adverse events, and much less likely to result in dangerous sedation, respiratory depression, and death.
SHM is recruiting now for participants in the mentored implementation program, and the guide is available online.
3. Download a New QI Resource
When you download a quality improvement toolkit or resource from SHM, you can be confident you are getting the best guidance from the national authorities on improving care for hospitalized patients.
SHM provides materials on the most pressing issues in hospital medicine, including:
- End-of-life care;
- Opioid monitoring;
- Antibiotic stewardship;
- Post-acute care;
- Veinous thromboembolism (VTE);
- Pain management; and
- Congestive heart failure (CHF).
To download, visit www.hospitalmedicine.org/qi.
Resident Education, Feedback, Incentives Improve Patient Satisfaction
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
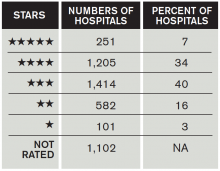
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Editor’s note: This article first appeared on SHM’s “The Hospital Leader” blog.
Patient satisfaction survey performance is becoming increasingly important for hospitals, because the ratings are being used by payers in pay-for-performance programs more and more (including the CMS Hospital Value-Based Purchasing program). CMS also recently released its “Five-Star Quality Rating System” for hospitals, which publicly grades hospitals, using one to five stars, based on their patient satisfaction scores.
How Did Hospitals Do in Medicare’s Patient Quality Ratings?
Unfortunately, there is little literature to guide physicians on exactly HOW to improve patient satisfaction scores for themselves or their groups. A recent publication in the Journal of Hospital Medicine found a feasible and effective intervention to improve patient satisfaction scores among trainees, the methodology of which could easily be applied to hospitalists.
Gaurav Banka, MD, a former internal medicine resident (and current cardiology fellow) at UCLA Hospital, was interviewed about his team’s recent publication in the Journal of Hospital Medicine. In the interview, he opined about “improving patient satisfaction through resident education, feedback, and incentives.” The study he published found that this combination of interventions among internal medicine residents improved relevant HCAHPS scores by approximately 8%.
The following are excerpts from a Q&A session I had with Dr. Banka:
Question: Can you briefly summarize the intervention(s)?
Answer: There were three total interventions put in place simultaneously: an educational conference on best practices in patient communication, a recognition-reward program (recognition within the department and a movie package for high performers), and real-time feedback to the residents from their patients via a survey. The last component was the most impactful to the residents. Patients were randomly surveyed on how their residents were communicating with them, and the results were sent to the resident for review and self-reflection within weeks.
Q: How did you become interested in resident interventions to improve HCAHPS?
A: I noticed as an intern [that] there was almost no emphasis placed on patient communication skills, and there was almost no feedback given to residents on how they were performing. I felt that this was a very important piece of feedback that residents were lacking and was very interested in creating a program that would help them learn new communication skills and get feedback on how they were doing.
Q: How should hospitalists use this study information to change their practice?
A: Hospital medicine programs should have some way to measure and give feedback to individual hospitalists on what the patient is experiencing with respect to communication. The intervention from this study should be easily scalable to any practice. There was almost no cost associated with the patient survey distribution, and it gave incredibly valuable individualized feedback about communication skills directly from the patients themselves. It should be feasible to implement this type of audit and feedback within any size hospital medicine program.
Q: Were there any unexpected findings in your study?
A: We were surprised at how much of an impact it had on HCAHPS scores. Not only did it impact physician communication ratings, but [it] also had an impressive impact on overall hospital ratings.
Q: Where does this take us with respect to future research efforts?
A: Our team is now working on expanding this program to other residency programs, as well as expanding it to attending physicians, within and outside the department of medicine.
In summary, Dr. Banka’s team found this relatively simple intervention was able to sizably improve the HCAHPS scores of recipient providers. Such interventions should be seriously considered by hospital medicine programs looking to improve their publicly reported patient satisfaction scores.
Clinical Care Conundrums Provide Learning Potential for Hospitalists
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
Hospitalist-Led Quality Initiatives Plentiful at Community Hospitals
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Movers and Shakers in Hospital Medicine September 2015
Solomon Noguera, MD, is the new assistant medical director at Serenity HospiceCare in Farmington, Mo. Dr. Noguera most recently served as a hospitalist for both St. Anthony’s Hospital in St. Louis and St. Genevieve (Mo.) Hospital. He also practices primary care at Millennium Medical PC in Festus, Mo., and attends to patients at several other St. Louis-area hospitals.


Leonard Castiglione is the new chief executive officer of Ob Hospitalist Group (OBHG). Castiglione joins the Greenville, S.C.-based company after recently serving as CEO of Florida Gulf to Bay Anesthesia Holdings, LLC, in Tampa, Fla. OBHG has been providing OB/GYN emergency and hospitalist services since 2006.


We’re always looking for hospitalists “on the move”? Send us details of your recent award, promotion, or business deal to Jason Carris.
Business Moves
Solomon Noguera, MD, is the new assistant medical director at Serenity HospiceCare in Farmington, Mo. Dr. Noguera most recently served as a hospitalist for both St. Anthony’s Hospital in St. Louis and St. Genevieve (Mo.) Hospital. He also practices primary care at Millennium Medical PC in Festus, Mo., and attends to patients at several other St. Louis-area hospitals.


Leonard Castiglione is the new chief executive officer of Ob Hospitalist Group (OBHG). Castiglione joins the Greenville, S.C.-based company after recently serving as CEO of Florida Gulf to Bay Anesthesia Holdings, LLC, in Tampa, Fla. OBHG has been providing OB/GYN emergency and hospitalist services since 2006.


We’re always looking for hospitalists “on the move”? Send us details of your recent award, promotion, or business deal to Jason Carris.
Business Moves
Solomon Noguera, MD, is the new assistant medical director at Serenity HospiceCare in Farmington, Mo. Dr. Noguera most recently served as a hospitalist for both St. Anthony’s Hospital in St. Louis and St. Genevieve (Mo.) Hospital. He also practices primary care at Millennium Medical PC in Festus, Mo., and attends to patients at several other St. Louis-area hospitals.


Leonard Castiglione is the new chief executive officer of Ob Hospitalist Group (OBHG). Castiglione joins the Greenville, S.C.-based company after recently serving as CEO of Florida Gulf to Bay Anesthesia Holdings, LLC, in Tampa, Fla. OBHG has been providing OB/GYN emergency and hospitalist services since 2006.


We’re always looking for hospitalists “on the move”? Send us details of your recent award, promotion, or business deal to Jason Carris.
Business Moves
Society of Hospital Medicine Posts Quality Improvement Resources Online

Glycemic Control Webinar
Subcutaneous Insulin Order Sets in the Inpatient Setting: Design and Implementation
Presenter: Kristi Kulasa, MD
Date: September 17
Time: 4 p.m. EDT
General QI Webinars
Quality Improvement for Hospital Medicine Groups: Self-Assessment and Self-Improvement Using the SHM Key Characteristics
Presenter: Steve Deitelzweig, MD, SFHM
Date: September 16
Time: 2 p.m. EDT
Other online resources at www.hospitalmedicine.org:
- New FREE clinical topics and guide: chronic obstructive pulmonary disease.
- Coming soon: antibiotic stewardship.
- And now, all of SHM’s popular SHMConsults modules are available on the Learning Portal.
With new quality improvement resources available online every month, Hospital Medicine is THE source for hospitalists ready to improve their hospitals.

Glycemic Control Webinar
Subcutaneous Insulin Order Sets in the Inpatient Setting: Design and Implementation
Presenter: Kristi Kulasa, MD
Date: September 17
Time: 4 p.m. EDT
General QI Webinars
Quality Improvement for Hospital Medicine Groups: Self-Assessment and Self-Improvement Using the SHM Key Characteristics
Presenter: Steve Deitelzweig, MD, SFHM
Date: September 16
Time: 2 p.m. EDT
Other online resources at www.hospitalmedicine.org:
- New FREE clinical topics and guide: chronic obstructive pulmonary disease.
- Coming soon: antibiotic stewardship.
- And now, all of SHM’s popular SHMConsults modules are available on the Learning Portal.
With new quality improvement resources available online every month, Hospital Medicine is THE source for hospitalists ready to improve their hospitals.

Glycemic Control Webinar
Subcutaneous Insulin Order Sets in the Inpatient Setting: Design and Implementation
Presenter: Kristi Kulasa, MD
Date: September 17
Time: 4 p.m. EDT
General QI Webinars
Quality Improvement for Hospital Medicine Groups: Self-Assessment and Self-Improvement Using the SHM Key Characteristics
Presenter: Steve Deitelzweig, MD, SFHM
Date: September 16
Time: 2 p.m. EDT
Other online resources at www.hospitalmedicine.org:
- New FREE clinical topics and guide: chronic obstructive pulmonary disease.
- Coming soon: antibiotic stewardship.
- And now, all of SHM’s popular SHMConsults modules are available on the Learning Portal.
With new quality improvement resources available online every month, Hospital Medicine is THE source for hospitalists ready to improve their hospitals.
LISTEN NOW: Tales from the Research, Innovations, and Clinical Vignette (RIV) Poster Competition
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
LISTEN NOW: Scott Sears, MD, MBA, Explains How GME Programs Could Be Better Aligned
SCOTT SEARS, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians, discusses how
GME programs could be better aligned with the shifting reality in medicine.
SCOTT SEARS, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians, discusses how
GME programs could be better aligned with the shifting reality in medicine.
SCOTT SEARS, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians, discusses how
GME programs could be better aligned with the shifting reality in medicine.