User login
How to prevent serotonin syndrome from drug-drug interactions
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
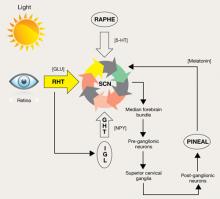
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
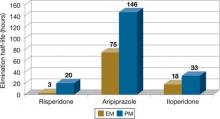
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
• Know which drugs are associated with serotonin syndrome.
• Understand the types of drug interactions that may precipitate serotonin syndrome and use drug information resources such as Micromedex, Lexicomp, Physicians’ Desk Reference, AHFS Drug Information, and Facts and Comparisons.
• Know what prescription medications your patient is receiving from other providers as well as any over-the-counter and illicit drugs they may be using.
Ms. B, age 22, is brought to the emergency department (ED) by her roommate for evaluation of confusion. Ms. B has a history of migraines and major depressive disorder and has been taking fluoxetine, 40 mg/d, for 1 year. A week ago, she started amitriptyline, 50 mg/d, when her migraines became more frequent. According to her roommate, Ms. B experienced a migraine early in the morning and had taken 2 doses of sumatriptan, 50 mg. She later complained of nausea and vomiting, and when her roommate returned from work that evening Ms. B was disoriented and her leg muscles would not stop twitching.
In the ED, Ms. B is diaphoretic and increasingly agitated. Blood alcohol and urine drug screens are negative. Blood glucose is 95 mg/dL. Complete blood count, basic metabolic panel, liver function, and kidney function tests are within normal limits. Her physical examination reveals a blood pressure of 130/85 mm Hg, heart rate of 130 beats per minute, respiratory rate of 21 breaths per minute, and body temperature of 38.6°C (101. 4°F). Myoclonus and hyperreflexia affect her lower extremities. Ms. B is admitted with a preliminary diagnosis of serotonin (5-HT) syndrome.
Serotonin syndrome: What is it?
Serotonin syndrome is a rare but potentially serious adverse event resulting from excess serotonergic activity at central and peripheral 5-HT2A and 5-HT1A receptors. Serotonin syndrome toxicity ranges from relatively mild to severe, and may be lethal. Symptoms develop rapidly—within hours—and may include altered mental status, clonus, tremor, hyperthermia, diaphoresis, tachycardia, mydriasis, and akathisia ( Table 1 ).1-3 Fortunately, if recognized promptly and offending agents are discontinued, serotonin syndrome often resolves within a couple of days.
The differential diagnosis includes neuroleptic malignant syndrome (NMS), anticholinergic toxicity, and malignant hyperthermia.1 Differentiating serotonin syndrome from NMS can be difficult. NMS results from dopamine blockade; however, many NMS symptoms are similar to those experienced with serotonin syndrome. Obtaining a history of recent medication and/or illicit drug use, conducting a physical exam, and evaluating the patient’s clinical course help clarify a likely diagnosis. NMS generally has a slower onset—within days—and patients demonstrate neuromuscular rigidity and bradykinesia rather than the neuromuscular hyperreactivity (myoclonus, hyperreflexia) seen with serotonin syndrome.
Table 1
Characteristics of serotonin syndrome*
| Recent addition or dose increase of a serotonergic agent |
| Tremor plus hyperreflexia |
| Muscle rigidity plus fever plus clonus |
| Spontaneous clonus |
| Ocular clonus plus agitation or diaphoresis |
| Inducible clonus plus agitation or diaphoresis |
| *A combination of these characteristics may indicate serotonin syndrome |
| Source: References 1-3 |
Interactions that increase risk
A drug interaction is a pharmacologic or clinical response to a combination of medications that differs from the agents’ known effects if given on their own. In the context of serotonin syndrome, the serotonergic activity of a drug can be increased as a result of a pharmacokinetic (PK) interaction, a pharmacodynamic (PD) interaction, or a combination of both.
PK interactions may result from the coadministration of a drug that alters absorption, distribution, metabolism, or elimination parameters of \>1 other drugs. Serotonergic antidepressants usually are metabolized by cytochrome P450 (CYP450) enzymes. Any drug that inhibits a CYP450 enzyme responsible for biotransformation of 1 of these antidepressants may increase exposure to the antidepressant and raise the risk of serotonin syndrome. CYP450 inhibitors include prescription medications as well as seemingly benign over-the-counter (OTC) drugs.
PD interactions may result from an additive or synergistic pharmacologic effect caused by coadministration of 2 agents that produce the same or similar end result. In Ms. B’s case, agents inhibiting 5-HT reuptake (fluoxetine and amitriptyline) were combined with a direct 5-HT agonist (sumatriptan). The resulting potentiation of 5-HT via 2 distinct mechanisms increased Ms. B’s risk of serotonin syndrome. Similarly, simultaneous use of 2 agents potentiating 5-HT through identical mechanisms, such as combining 2 serotonin reuptake inhibitors, also may increase the risk of serotonin syndrome ( Table 2 ).1
A combination of PK and PD interactions also may increase the risk of serotonin syndrome. For example, Ms. B is taking fluoxetine and amitriptyline for different therapeutic reasons. Both of these agents inhibit 5-HT reuptake, potentiating 5-HT. In addition, amitriptyline is a substrate for CYP2D6 and fluoxetine is a robust CYP2D6 inhibitor. The coadministration of fluoxetine with tricyclic antidepressants (TCAs) results in a 4- to 5-fold increase in TCA exposure, which may increase the risk of serotonin syndrome and other sequelae from TCA toxicity.4,5
Table 2
Drugs associated with serotonin syndrome
| Drugs that increase 5-HT release | Amphetamine, cocaine, MDMA (ecstasy), mirtazapine, phentermine, reserpine |
| Drugs that inhibit 5-HT reuptake | Amitriptyline, amphetamine, bupropion, Citalopram, clomipramine, cocaine, desipramine, dextromethorphan, doxepin, duloxetine, escitalopram, fentanyl, fluoxetine, fluvoxamine, Hypericum perforatum (St. John’s wort), imipramine, MDMA, meperidine, nefazodone, nortriptyline, paroxetine, protriptyline, sertraline, tramadol, trazodone, venlafaxine |
| Drugs that decrease 5-HT metabolism | Isocarboxazid, linezolid, phenelzine, selegiline, tranylcypromine |
| Drugs that are direct 5-HT agonists | Almotriptan, buspirone, dihydroergotamine, eletriptan, frovatriptan, LSD, naratriptan, rizatriptan, sumatriptan, zolmitriptan |
| Others | L-tryptophan, carbamazepine, carisoprodol, droperidol, levodopa, lithium, metoclopramide, pentazocine, phenylpropanolamine |
| 5-HT: serotonin; LSD: lysergic acid; MDMA: methylenedioxymethamphetamine | |
| Source: Reference 1 | |
Preventing serotonin syndrome
The warnings highlighted in drug interaction references or pharmacy databases often mean that clinicians have to evaluate whether the risk of combining medications outweighs the therapeutic benefits. It is unknown why some patients tolerate multiple agents potentiating 5-HT, and practitioners cannot predict when and in whom serotonin syndrome may occur. However, the following strategies may help minimize these risks:
Know which drugs are associated with serotonin syndrome. Concomitant use of these drugs and agents that inhibit metabolism of these drugs increases risk.
Know which drugs your patient is taking. Patients may see several prescribers, which makes it essential to ask what they are receiving from other practitioners. Also inquire about OTC and illicit drug use.
Check for interactions. If you are unfamiliar with a new drug or drug-drug combination, check multiple resources for potential interactions. The potential severity of an interaction and the detail in which interactions are described—such as class effects vs documented cases or studies—differs among drug interaction resources, which means a potential interaction may be “flagged” in 1 source but not another. Electronic resources such as Micromedex and Lexicomp often have detailed literature summaries and citations so clinicians can review primary literature that lead to the categorization of an interaction. Using multiple sources is helpful when trying to translate warnings in the context of a clinical scenario.
Weigh the risks and benefits. Prescribers know that not all treatments are benign, but not treating a condition also may be detrimental. Identify potential alternative pharmacologic or nonpharmacologic treatments when possible. Discuss the risks and benefits of drug therapy with patients.
Counsel your patients. Although it is not possible to predict who may experience serotonin syndrome, educate patients on what symptoms to look for. Instruct them to call their prescriber or pharmacist if they show symptoms that may be consistent with serotonin syndrome.
Related Resource
• MedWatch: The FDA Safety Information and Adverse Event Reporting Program. www.fda.gov/Safety/MedWatch.
Drug Brand Names
- Aripiprazole • Abilify
- Almotriptan • Axert
- Amitriptyline • Elavil
- Bupropion • Wellbutrin, Zyban
- Buspirone • BuSpar
- Carbamazepine • Carbatrol, Equetro, others
- Carisoprodol • Soma
- Citalopram • Celexa
- Desipramine • Norpramin
- Dihydroergotamine • Migranal
- Doxepin • Adapin, Silenor
- Droperidol • Inapsine
- Duloxetine • Cymbalta
- Eletriptan • Relpax
- Escitalopram • Lexapro
- Fentanyl • Sublimaze, others
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Frovatriptan • Frova
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Levodopa • Dopar, Larodopa, others
- Linezolid • Zyvox
- Lithium • Eskalith, Lithobid
- Meperidine • Demerol
- Metoclopramide • Reglan, Metozol
- Mirtazapine • Remeron
- Naratriptan • Amerge
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Paroxetine • Paxil
- Pentazocine • Talwin
- Phenelzine • Nardil
- Phentermine • Fastin, Adipex-P
- Protriptyline • Vivactil
- Reserpine • Serpasil
- Rizatriptan • Maxalt
- Selegiline • Carbex, Eldepryl, others
- Sertraline • Zoloft
- Sumatriptan • Imitrex, Alsuma
- Tramadol • Ultram, Ultracet, others
- Tranylcypromine • Parnate
- Trazodone • Desyrel, Oleptro
- Venlafaxine • Effexor
- Zolmitriptan • Zomig
Disclosures
Dr. Jeffrey Bishop receives grant/research support from Ortho-McNeil-Janssen.
Dr. Danielle Bishop reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
1. Beyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352:1112-1120.
2. Dunkley EJ, Isbister GK, Sibbritt D, et al. The TTunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96:635-642.
3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991;148:705-713.
4. Preskorn SH, Beber JH, Faul JC, et al. Serious adverse effects of combining fluoxetine and tricyclic antidepressants. Am J Psychiatry. 1990;147-532.
5. Preskorn SH, Alderman J, Chung M, et al. Pharmacokinetics of desipramine coadministered with sertraline or fluoxetine. J Clin Psychopharmacol. 1994;14:90-98.
The surgeon who operated on himself
CASE: Self-surgery
Dr. T (a pseudonym), a middle-aged male surgeon, arrives in the emergency department (ED) by ambulance after vomiting and losing consciousness at his office. Paramedics place him on an involuntary psychiatric hold, which is permitted in California, after learning that he had been performing surgery on himself.
Dr. T has developed medical complications after attempting to repair his own umbilical hernia. He states that the hernia resulted from weakened periumbilical abdominal muscles after multiple abdominal liposuctions, during which he inserted a cannula through the umbilicus. Dr. T initially repaired the hernia 4 months ago, but the wound margins had dehisced. He had performed the procedure at his ambulatory care surgical suite with help from his surgical assistant. Dr. T says he has performed many procedures on himself, including abdominal and chest liposuction, dermal filler injections, and skin laser resurfacing to improve perceived blemishes and remove hair. These procedures often resulted in poor cosmetic outcomes.
The authors’ observations
Clinical interviews confirmed that Dr. T met DSM-IV-TR criteria for BDD (Table 1).1 He is excessively preoccupied with perceived physical defects, which cause clinically significant distress, and this preoccupation is not better accounted for by another mental disorder.
Although Dr. T denied any psychotic symptoms during clinical interviews and Mini-Mental State Exam assessment, a reported 77% of BDD patients meet criteria for delusional disorder, somatic type (Table 2).1,2 Both disorders can be diagnosed concurrently if a patient meets criteria for both disorders.1 Phillips et al3 have suggested that delusional and non-delusional BDD may constitute the same disorder, spanning a continuum of insight. This hypothesis is supported by reports that selective serotonin reuptake inhibitors (SSRIs) work equally well for both BDD variants.4
Table 1
DSM-IV-TR criteria for body dysmorphic disorder
| A. | Preoccupation with an imagined defect in appearance. If a slight physical anomaly is present, the person’s concern is markedly excessive |
| B. | The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| C. | The preoccupation is not better accounted for by another mental disorder (eg, dissatisfaction with body shape and size in anorexia nervosa) |
| Source: Reference 1 | |
Table 2
DSM-IV-TR criteria for delusional disorder
| A. | Nonbizarre delusions (ie, involving situations that occur in real life, such as being followed, poisoned, infected, loved at a distance, or deceived by spouse or lover, or having a disease) of at least 1 month’s duration |
| B. | Criterion A for schizophrenia has never been met |
| C. | Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired and behavior is not obviously odd or bizarre |
| D. | If mood episodes have occurred concurrently with delusions, their total duration has been brief relative to the duration of the delusional periods |
| E. | The disturbance is not due to the direct physiological effects of a substance (eg, a drug of abuse, a medication) or a general medical condition |
| Somatic Type: This subtype applies when the central theme of the delusion involves bodily functions or sensations. Somatic delusions can occur in several forms. Most common are the person’s conviction that he or she emits a foul odor from the skin, mouth, rectum, or vagina; that there is an infestation of insects on or in the skin; that there is an internal parasite; that certain parts of the body are definitely (contrary to all evidence) misshapen or ugly; or that parts of the body (eg, the large intestine) are not functioning | |
| Source: Reference 1 | |
HISTORY: Accomplishment, anxiety
When we ask Dr. T why he operated on himself, he replies that he did not have time to go to another surgeon. He disagrees when we suggest that he feared that his privacy and professional reputation might be compromised. Dr. T states, “Doctors with walking pneumonia prescribe pills for themselves; this is the same in principle” and “There is no law against operating on oneself.” When we ask if he regrets his actions, he says “I was just overconfident. I did them under local anesthesia and I have a high pain tolerance.” He denies enjoying the pain. He reports that his friends and significant other consider him “courageous” for operating on himself. He denies further plans to perform surgery on himself.
Dr. T has no history of psychiatric hospitalizations or suicide attempts. He has a history of “situational anxiety” and over 3 years his general practitioner prescribed unknown dosages of sertraline, alprazolam, and propranolol, but he did not take these medications regularly and denies taking any other medications. Except for impaired judgment, his mental status exam is within normal limits. He has no other medical problems. He denies alcohol or illicit drug use or a desire to harm himself or others. Dr. T states that as a younger man he was an accomplished athlete and is now an avid body builder who exercises daily and is proud of the intensity and rigor of his workouts.
The authors’ observations
Dr. T does not meet DSM-IV-TR criteria for a current mood or anxiety disorder; however, he has taken medications for what he described as “situational anxiety.” This pattern is consistent with data suggesting that BDD patients feel an unusually high degree of stress in their lives.5 Crerand et al6 found that >60% of BDD patients had a lifetime history of an anxiety disorder.
Dr. T’s history highlights traits often observed in patients with BDD. As is common in men with BDD, he follows a rigorous exercise regimen.7 He also was a competitive athlete, and hypercompetitiveness has significant positive correlation with BDD symptoms.8 He is preoccupied with excessive body hair, which is more prevalent in men than in women with BDD.9 Dr. T’s work required a keen sense of aesthetics, and it has been observed that individuals with BDD have increased aesthetic sensitivity.10,11
Although many individuals with BDD struggle socially and financially, some BDD patients are successful and quite accomplished. In a study of 156 Pakistani medical students, 5.8% met criteria for BDD.12 In The broken mirror,13 BDD expert Dr. Katharine Phillips describes caring for many high-functioning health care professionals who suffer from BDD, yet “they provide their patients with superb care … many with this disorder are productive, some are very high achievers.”
EVALUATION: Bad scars
Dr. T has multiple surgical scars on his chest and abdomen (Photo), ecchymoses, and tenderness on palpation. His vital signs are within normal limits and he is otherwise medically healthy. Notable laboratory findings include elevated white blood cell count and platelets, and decreased hemoglobin.
A CT scan shows a large hematoma over the anterior abdominal wall extending toward the flanks with extensive subcutaneous emphysema. The peritoneum is intact. These findings raise the medical team’s concern about possible infection and vascular instability. The involuntary psychiatric hold for observation is continued after evaluation in the ED.
Photo Dr. T’s chest and abdomen during presentation to the ED
Note the asymmetry of the nipples and scarring from prior self-surgeries
The authors’ observations
There is a disconnect between Dr. T’s perception of his physical attributes and the treatment team’s observations. He perceives himself as marred by physical defects, while the treatment team sees him as a handsome and attractive person— excluding his scars from self-surgery.
Patients with BDD frequently are concerned about perceived physical defects that objective observers would consider slight or not noticeable. Three-quarters of individuals with BDD seek surgery or other medical treatment for their perceived physical flaws.4 Many patients minimize their BDD symptoms and their distress when talking with health care professionals.14 Approximately 20% of cosmetic surgery patients report ongoing psychiatric treatment at the time of surgery.15 Eighty-four percent of cosmetic surgeons state they have refused to operate on a patient because of BDD.16 However, it may be difficult for surgeons to distinguish a “perfectionist” from a patient with BDD.17 Even “positive” cosmetic surgery outcomes do not ameliorate BDD symptoms because most patients develop new areas of concern. In a small study of patients with minimal defects who requested cosmetic surgery, surgery did not reduce symptoms of BDD, disability, or psychiatric comorbidity in 6 out of 7 patients at 5-year follow up.18
Specialized medical equipment, such as surgical instruments and dermabrasion or laser hair removal devices, can be purchased on the Internet, which may increase the likelihood of individuals attempting procedures on themselves. Veale14 published a retrospective case series of patients who were turned down or unable to afford cosmetic surgery who performed self-surgery. These efforts did not lead to the desired effect, and patients continued to be plagued by their original concerns as well as self-inflicted scarring and damage.
Dr. T had the training and resources to perform cosmetic procedures on himself. Unfortunately, these efforts led to disfigurement. Phillips13 states that although self-surgery appears infrequently, it reflects the severe emotional pain and desperation felt by some patients with BDD. Self-surgery is associated with an increased rate of serious suicide attempts.14 Carefully monitor any BDD patient for suicidal ideation, intent, or plans.
TREATMENT: Refuses follow-up
Dr. T is admitted to the medical service and stabilized with IV fluids and antibiotics. The consultation-liaison service followed him during hospitalization. Because repeated interviews do not uncover grave disability or an imminent danger to himself or others, the involuntary psychiatric hold is discontinued. Dr. T declines psychiatric follow-up care, but says he would consider seeing a mental health professional in the future.
The authors’ observations
This case involves challenging ethical, legal, and countertransference issues. One of the first dilemmas the treatment team encountered was the decision to continue the involuntary hold for observation and assessment. The ED physician and psychiatric resident were faced with telling a fellow physician that he had to remain in the hospital despite his adamant desire to leave. Dr. T’s articulate arguments against staying in the hospital were addressed in order to deliver needed medical treatment. The psychiatric, surgical, and internal medicine teams discussed these countertransference concerns extensively during Dr. T’s hospitalization.
Clearly, Dr. T demonstrated poor judgment by operating on himself, and we aimed to ensure that he received appropriate psychiatric follow-up, but it could not be mandated. After intense and strongly debated ethical and legal discussions with the hospital’s ethicists and risk management team, we determined that we could not file a report with the state medical board because there was no evidence of incompetence, malpractice, or imminent risk to patients. A detailed description of these discussions is omitted from this article to preserve Dr. T’s confidentiality. However, Dr. T will have to disclose and explain the involuntary psychiatric hold on his next medical license renewal.
Our decision was influenced by Phillips,13 who found that although patients with BDD may have minimal insight into their illness, “their judgment remains intact in areas unrelated to their body image problem. Attention span and memory are well preserved, and physical and neurologic examinations are normal.” Although Dr. T meets criteria for BDD, mental illness in physicians is not synonymous with impairment.19
BDD treatment options
With medications and psychotherapy, patients with BDD generally have a good prognosis. A recent meta-analysis found that SSRIs and cognitive-behavioral therapy are effective treatments for BDD.20 In general, higher doses of SSRIs are needed to treat BDD compared with depression. Other medications with evidence of efficacy for BDD include the serotonin norepinephrine reuptake inhibitor venlafaxine21 and the anticonvulsant levetiracetam.22 However, clinicians often don’t have the opportunity to try these approaches because BDD patients are difficult to engage in treatment, as is evident in Dr. T’s case. Innovative approaches that combine practical and evidence-based strategies have been manualized.23 These approaches can help clinicians engage BDD patients in treatment and recognize underlying issues of distorted body image.
Related Resources
- BDD Central. www.bddcentral.com.
- Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
Drug Brand Names
- Alprazolam • Xanax
- Levetiracetam • Keppra
- Propranolol • Inderal
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Rapaport receives grant/research support from the National Institute of Mental Health and the National Center for Complementary and Alternative Medicine and is a consultant for Affectis Pharmaceuticals, Methylation Sciences, PAX Pharmaceuticals, and Johnson and Johnson Pharmaceuticals.
Drs. Rafin and Pimstone report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors wish to thank Dr. Kristine Andrade for editorial assistance. We also wish to thank the Institutional Review Board at Cedars-Sinai Medical Center for its review and approval of this case report, and Dr. T for his consent to publish it.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Phillips KA, Menard W, Fay C, et al. Demographic characteristics, phenomenology, comorbidity, and family history in 200 individuals with body dysmorphic disorder. Psychosomatics. 2005;46:317-325.
3. Phillips KA, McElroy SL, Keck PE, Jr, et al. A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases. Psychopharmacol Bull. 1994;30:179-186.
4. Crerand CE, Franklin ME, Sarwer DB. Patient safety: body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2008;122(4S):1-15.
5. DeMarco LM, Li LC, Phillips KA, et al. Perceived stress in body dysmorphic disorder. J Nerv Ment Dis. 1998;186(11):724-726.
6. Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2006;118(7):167-180.
7. Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185(9):570-577.
8. Woodie DS, Fromuth ME. The relationship of hypercompetitiveness and gender roles with body dysmorphic disorder symptoms in a nonclinical sample. Body Image. 2009;6(4):318-321.
9. Perugi G, Akiskal HS, Giannotti D, et al. Gender-related differences in body dysmorphic disorder (dysmorphophobia). J Nerv Ment Dis. 1997;185(9):578-582.
10. Veale D, Ennis M, Lambrou C. Possible association of body dysmorphic disorder with an occupation or education in art and design. Am J Psychiatry. 2002;159(10):1788-1790.
11. Phillips KA, Menard W. Body dysmorphic disorder and art background. Am J Psychiatry. 2004;161:927-928.
12. Ather MT, Mehrine S, Saqib GA, et al. Body dysmorphic disorder: gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry. 2008;8:20.
13. Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
14. Veale D. Outcome of cosmetic surgery and ‘DIY’ surgery in patients with body dysmorphic disorder. Psychiatric Bulletin. 2000;24:218-220.
15. Sarwer DB, Zanville HA, LaRossa D, et al. Mental health histories and psychiatric medication usage among persons who sought cosmetic surgery. Plast Reconstr Surg. 2004;114:1927-1933.
16. Sarwer DB. Awareness and identification of body dysmorphic disorder by aesthetic surgeons: results of a survey of American Society for Aesthetic Plastic Surgery members. Aesthet Surg J. 2002;22:531-535.
17. Glaser DA, Kaminer MS. Body dysmorphic disorder and the liposuction patient. Dermatol Surg. 2005;31(5):559-560.
18. Tignol J, Biraben-Gotzamanis L, Martin-Guehl C, et al. Body dysmorphic disorder and cosmetic surgery: evolution of 24 subjects with a minimal defect in appearance 5 years after their request for cosmetic surgery. Eur Psychiatry. 2007;22(8):520-524.
19. Myers MF. The psychiatrist’s role in the management of impaired colleagues. Directions in Psychiatry. 1995;15:1-8.
20. Ipser JC, Sander C, Stein DJ. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database Syst Rev. 2009;(1):CD005332.
21. Allen A, Hadley SJ, Kaplan A, et al. An open-label trial of venlafaxine in body dysmorphic disorder. CNS Spectr. 2008;13(2):138-144.
22. Phillips KA, Menard W. A prospective pilot study of levetiracetam for body dysmorphic disorder. CNS Spectr. 2009;14(5):252-260.
23. Veale D, Neziroglu F. Body dysmorphic disorder: a treatment manual. West Sussex, United Kingdom: Wiley-Blackwell; 2010.
CASE: Self-surgery
Dr. T (a pseudonym), a middle-aged male surgeon, arrives in the emergency department (ED) by ambulance after vomiting and losing consciousness at his office. Paramedics place him on an involuntary psychiatric hold, which is permitted in California, after learning that he had been performing surgery on himself.
Dr. T has developed medical complications after attempting to repair his own umbilical hernia. He states that the hernia resulted from weakened periumbilical abdominal muscles after multiple abdominal liposuctions, during which he inserted a cannula through the umbilicus. Dr. T initially repaired the hernia 4 months ago, but the wound margins had dehisced. He had performed the procedure at his ambulatory care surgical suite with help from his surgical assistant. Dr. T says he has performed many procedures on himself, including abdominal and chest liposuction, dermal filler injections, and skin laser resurfacing to improve perceived blemishes and remove hair. These procedures often resulted in poor cosmetic outcomes.
The authors’ observations
Clinical interviews confirmed that Dr. T met DSM-IV-TR criteria for BDD (Table 1).1 He is excessively preoccupied with perceived physical defects, which cause clinically significant distress, and this preoccupation is not better accounted for by another mental disorder.
Although Dr. T denied any psychotic symptoms during clinical interviews and Mini-Mental State Exam assessment, a reported 77% of BDD patients meet criteria for delusional disorder, somatic type (Table 2).1,2 Both disorders can be diagnosed concurrently if a patient meets criteria for both disorders.1 Phillips et al3 have suggested that delusional and non-delusional BDD may constitute the same disorder, spanning a continuum of insight. This hypothesis is supported by reports that selective serotonin reuptake inhibitors (SSRIs) work equally well for both BDD variants.4
Table 1
DSM-IV-TR criteria for body dysmorphic disorder
| A. | Preoccupation with an imagined defect in appearance. If a slight physical anomaly is present, the person’s concern is markedly excessive |
| B. | The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| C. | The preoccupation is not better accounted for by another mental disorder (eg, dissatisfaction with body shape and size in anorexia nervosa) |
| Source: Reference 1 | |
Table 2
DSM-IV-TR criteria for delusional disorder
| A. | Nonbizarre delusions (ie, involving situations that occur in real life, such as being followed, poisoned, infected, loved at a distance, or deceived by spouse or lover, or having a disease) of at least 1 month’s duration |
| B. | Criterion A for schizophrenia has never been met |
| C. | Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired and behavior is not obviously odd or bizarre |
| D. | If mood episodes have occurred concurrently with delusions, their total duration has been brief relative to the duration of the delusional periods |
| E. | The disturbance is not due to the direct physiological effects of a substance (eg, a drug of abuse, a medication) or a general medical condition |
| Somatic Type: This subtype applies when the central theme of the delusion involves bodily functions or sensations. Somatic delusions can occur in several forms. Most common are the person’s conviction that he or she emits a foul odor from the skin, mouth, rectum, or vagina; that there is an infestation of insects on or in the skin; that there is an internal parasite; that certain parts of the body are definitely (contrary to all evidence) misshapen or ugly; or that parts of the body (eg, the large intestine) are not functioning | |
| Source: Reference 1 | |
HISTORY: Accomplishment, anxiety
When we ask Dr. T why he operated on himself, he replies that he did not have time to go to another surgeon. He disagrees when we suggest that he feared that his privacy and professional reputation might be compromised. Dr. T states, “Doctors with walking pneumonia prescribe pills for themselves; this is the same in principle” and “There is no law against operating on oneself.” When we ask if he regrets his actions, he says “I was just overconfident. I did them under local anesthesia and I have a high pain tolerance.” He denies enjoying the pain. He reports that his friends and significant other consider him “courageous” for operating on himself. He denies further plans to perform surgery on himself.
Dr. T has no history of psychiatric hospitalizations or suicide attempts. He has a history of “situational anxiety” and over 3 years his general practitioner prescribed unknown dosages of sertraline, alprazolam, and propranolol, but he did not take these medications regularly and denies taking any other medications. Except for impaired judgment, his mental status exam is within normal limits. He has no other medical problems. He denies alcohol or illicit drug use or a desire to harm himself or others. Dr. T states that as a younger man he was an accomplished athlete and is now an avid body builder who exercises daily and is proud of the intensity and rigor of his workouts.
The authors’ observations
Dr. T does not meet DSM-IV-TR criteria for a current mood or anxiety disorder; however, he has taken medications for what he described as “situational anxiety.” This pattern is consistent with data suggesting that BDD patients feel an unusually high degree of stress in their lives.5 Crerand et al6 found that >60% of BDD patients had a lifetime history of an anxiety disorder.
Dr. T’s history highlights traits often observed in patients with BDD. As is common in men with BDD, he follows a rigorous exercise regimen.7 He also was a competitive athlete, and hypercompetitiveness has significant positive correlation with BDD symptoms.8 He is preoccupied with excessive body hair, which is more prevalent in men than in women with BDD.9 Dr. T’s work required a keen sense of aesthetics, and it has been observed that individuals with BDD have increased aesthetic sensitivity.10,11
Although many individuals with BDD struggle socially and financially, some BDD patients are successful and quite accomplished. In a study of 156 Pakistani medical students, 5.8% met criteria for BDD.12 In The broken mirror,13 BDD expert Dr. Katharine Phillips describes caring for many high-functioning health care professionals who suffer from BDD, yet “they provide their patients with superb care … many with this disorder are productive, some are very high achievers.”
EVALUATION: Bad scars
Dr. T has multiple surgical scars on his chest and abdomen (Photo), ecchymoses, and tenderness on palpation. His vital signs are within normal limits and he is otherwise medically healthy. Notable laboratory findings include elevated white blood cell count and platelets, and decreased hemoglobin.
A CT scan shows a large hematoma over the anterior abdominal wall extending toward the flanks with extensive subcutaneous emphysema. The peritoneum is intact. These findings raise the medical team’s concern about possible infection and vascular instability. The involuntary psychiatric hold for observation is continued after evaluation in the ED.
Photo Dr. T’s chest and abdomen during presentation to the ED
Note the asymmetry of the nipples and scarring from prior self-surgeries
The authors’ observations
There is a disconnect between Dr. T’s perception of his physical attributes and the treatment team’s observations. He perceives himself as marred by physical defects, while the treatment team sees him as a handsome and attractive person— excluding his scars from self-surgery.
Patients with BDD frequently are concerned about perceived physical defects that objective observers would consider slight or not noticeable. Three-quarters of individuals with BDD seek surgery or other medical treatment for their perceived physical flaws.4 Many patients minimize their BDD symptoms and their distress when talking with health care professionals.14 Approximately 20% of cosmetic surgery patients report ongoing psychiatric treatment at the time of surgery.15 Eighty-four percent of cosmetic surgeons state they have refused to operate on a patient because of BDD.16 However, it may be difficult for surgeons to distinguish a “perfectionist” from a patient with BDD.17 Even “positive” cosmetic surgery outcomes do not ameliorate BDD symptoms because most patients develop new areas of concern. In a small study of patients with minimal defects who requested cosmetic surgery, surgery did not reduce symptoms of BDD, disability, or psychiatric comorbidity in 6 out of 7 patients at 5-year follow up.18
Specialized medical equipment, such as surgical instruments and dermabrasion or laser hair removal devices, can be purchased on the Internet, which may increase the likelihood of individuals attempting procedures on themselves. Veale14 published a retrospective case series of patients who were turned down or unable to afford cosmetic surgery who performed self-surgery. These efforts did not lead to the desired effect, and patients continued to be plagued by their original concerns as well as self-inflicted scarring and damage.
Dr. T had the training and resources to perform cosmetic procedures on himself. Unfortunately, these efforts led to disfigurement. Phillips13 states that although self-surgery appears infrequently, it reflects the severe emotional pain and desperation felt by some patients with BDD. Self-surgery is associated with an increased rate of serious suicide attempts.14 Carefully monitor any BDD patient for suicidal ideation, intent, or plans.
TREATMENT: Refuses follow-up
Dr. T is admitted to the medical service and stabilized with IV fluids and antibiotics. The consultation-liaison service followed him during hospitalization. Because repeated interviews do not uncover grave disability or an imminent danger to himself or others, the involuntary psychiatric hold is discontinued. Dr. T declines psychiatric follow-up care, but says he would consider seeing a mental health professional in the future.
The authors’ observations
This case involves challenging ethical, legal, and countertransference issues. One of the first dilemmas the treatment team encountered was the decision to continue the involuntary hold for observation and assessment. The ED physician and psychiatric resident were faced with telling a fellow physician that he had to remain in the hospital despite his adamant desire to leave. Dr. T’s articulate arguments against staying in the hospital were addressed in order to deliver needed medical treatment. The psychiatric, surgical, and internal medicine teams discussed these countertransference concerns extensively during Dr. T’s hospitalization.
Clearly, Dr. T demonstrated poor judgment by operating on himself, and we aimed to ensure that he received appropriate psychiatric follow-up, but it could not be mandated. After intense and strongly debated ethical and legal discussions with the hospital’s ethicists and risk management team, we determined that we could not file a report with the state medical board because there was no evidence of incompetence, malpractice, or imminent risk to patients. A detailed description of these discussions is omitted from this article to preserve Dr. T’s confidentiality. However, Dr. T will have to disclose and explain the involuntary psychiatric hold on his next medical license renewal.
Our decision was influenced by Phillips,13 who found that although patients with BDD may have minimal insight into their illness, “their judgment remains intact in areas unrelated to their body image problem. Attention span and memory are well preserved, and physical and neurologic examinations are normal.” Although Dr. T meets criteria for BDD, mental illness in physicians is not synonymous with impairment.19
BDD treatment options
With medications and psychotherapy, patients with BDD generally have a good prognosis. A recent meta-analysis found that SSRIs and cognitive-behavioral therapy are effective treatments for BDD.20 In general, higher doses of SSRIs are needed to treat BDD compared with depression. Other medications with evidence of efficacy for BDD include the serotonin norepinephrine reuptake inhibitor venlafaxine21 and the anticonvulsant levetiracetam.22 However, clinicians often don’t have the opportunity to try these approaches because BDD patients are difficult to engage in treatment, as is evident in Dr. T’s case. Innovative approaches that combine practical and evidence-based strategies have been manualized.23 These approaches can help clinicians engage BDD patients in treatment and recognize underlying issues of distorted body image.
Related Resources
- BDD Central. www.bddcentral.com.
- Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
Drug Brand Names
- Alprazolam • Xanax
- Levetiracetam • Keppra
- Propranolol • Inderal
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Rapaport receives grant/research support from the National Institute of Mental Health and the National Center for Complementary and Alternative Medicine and is a consultant for Affectis Pharmaceuticals, Methylation Sciences, PAX Pharmaceuticals, and Johnson and Johnson Pharmaceuticals.
Drs. Rafin and Pimstone report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors wish to thank Dr. Kristine Andrade for editorial assistance. We also wish to thank the Institutional Review Board at Cedars-Sinai Medical Center for its review and approval of this case report, and Dr. T for his consent to publish it.
CASE: Self-surgery
Dr. T (a pseudonym), a middle-aged male surgeon, arrives in the emergency department (ED) by ambulance after vomiting and losing consciousness at his office. Paramedics place him on an involuntary psychiatric hold, which is permitted in California, after learning that he had been performing surgery on himself.
Dr. T has developed medical complications after attempting to repair his own umbilical hernia. He states that the hernia resulted from weakened periumbilical abdominal muscles after multiple abdominal liposuctions, during which he inserted a cannula through the umbilicus. Dr. T initially repaired the hernia 4 months ago, but the wound margins had dehisced. He had performed the procedure at his ambulatory care surgical suite with help from his surgical assistant. Dr. T says he has performed many procedures on himself, including abdominal and chest liposuction, dermal filler injections, and skin laser resurfacing to improve perceived blemishes and remove hair. These procedures often resulted in poor cosmetic outcomes.
The authors’ observations
Clinical interviews confirmed that Dr. T met DSM-IV-TR criteria for BDD (Table 1).1 He is excessively preoccupied with perceived physical defects, which cause clinically significant distress, and this preoccupation is not better accounted for by another mental disorder.
Although Dr. T denied any psychotic symptoms during clinical interviews and Mini-Mental State Exam assessment, a reported 77% of BDD patients meet criteria for delusional disorder, somatic type (Table 2).1,2 Both disorders can be diagnosed concurrently if a patient meets criteria for both disorders.1 Phillips et al3 have suggested that delusional and non-delusional BDD may constitute the same disorder, spanning a continuum of insight. This hypothesis is supported by reports that selective serotonin reuptake inhibitors (SSRIs) work equally well for both BDD variants.4
Table 1
DSM-IV-TR criteria for body dysmorphic disorder
| A. | Preoccupation with an imagined defect in appearance. If a slight physical anomaly is present, the person’s concern is markedly excessive |
| B. | The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| C. | The preoccupation is not better accounted for by another mental disorder (eg, dissatisfaction with body shape and size in anorexia nervosa) |
| Source: Reference 1 | |
Table 2
DSM-IV-TR criteria for delusional disorder
| A. | Nonbizarre delusions (ie, involving situations that occur in real life, such as being followed, poisoned, infected, loved at a distance, or deceived by spouse or lover, or having a disease) of at least 1 month’s duration |
| B. | Criterion A for schizophrenia has never been met |
| C. | Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired and behavior is not obviously odd or bizarre |
| D. | If mood episodes have occurred concurrently with delusions, their total duration has been brief relative to the duration of the delusional periods |
| E. | The disturbance is not due to the direct physiological effects of a substance (eg, a drug of abuse, a medication) or a general medical condition |
| Somatic Type: This subtype applies when the central theme of the delusion involves bodily functions or sensations. Somatic delusions can occur in several forms. Most common are the person’s conviction that he or she emits a foul odor from the skin, mouth, rectum, or vagina; that there is an infestation of insects on or in the skin; that there is an internal parasite; that certain parts of the body are definitely (contrary to all evidence) misshapen or ugly; or that parts of the body (eg, the large intestine) are not functioning | |
| Source: Reference 1 | |
HISTORY: Accomplishment, anxiety
When we ask Dr. T why he operated on himself, he replies that he did not have time to go to another surgeon. He disagrees when we suggest that he feared that his privacy and professional reputation might be compromised. Dr. T states, “Doctors with walking pneumonia prescribe pills for themselves; this is the same in principle” and “There is no law against operating on oneself.” When we ask if he regrets his actions, he says “I was just overconfident. I did them under local anesthesia and I have a high pain tolerance.” He denies enjoying the pain. He reports that his friends and significant other consider him “courageous” for operating on himself. He denies further plans to perform surgery on himself.
Dr. T has no history of psychiatric hospitalizations or suicide attempts. He has a history of “situational anxiety” and over 3 years his general practitioner prescribed unknown dosages of sertraline, alprazolam, and propranolol, but he did not take these medications regularly and denies taking any other medications. Except for impaired judgment, his mental status exam is within normal limits. He has no other medical problems. He denies alcohol or illicit drug use or a desire to harm himself or others. Dr. T states that as a younger man he was an accomplished athlete and is now an avid body builder who exercises daily and is proud of the intensity and rigor of his workouts.
The authors’ observations
Dr. T does not meet DSM-IV-TR criteria for a current mood or anxiety disorder; however, he has taken medications for what he described as “situational anxiety.” This pattern is consistent with data suggesting that BDD patients feel an unusually high degree of stress in their lives.5 Crerand et al6 found that >60% of BDD patients had a lifetime history of an anxiety disorder.
Dr. T’s history highlights traits often observed in patients with BDD. As is common in men with BDD, he follows a rigorous exercise regimen.7 He also was a competitive athlete, and hypercompetitiveness has significant positive correlation with BDD symptoms.8 He is preoccupied with excessive body hair, which is more prevalent in men than in women with BDD.9 Dr. T’s work required a keen sense of aesthetics, and it has been observed that individuals with BDD have increased aesthetic sensitivity.10,11
Although many individuals with BDD struggle socially and financially, some BDD patients are successful and quite accomplished. In a study of 156 Pakistani medical students, 5.8% met criteria for BDD.12 In The broken mirror,13 BDD expert Dr. Katharine Phillips describes caring for many high-functioning health care professionals who suffer from BDD, yet “they provide their patients with superb care … many with this disorder are productive, some are very high achievers.”
EVALUATION: Bad scars
Dr. T has multiple surgical scars on his chest and abdomen (Photo), ecchymoses, and tenderness on palpation. His vital signs are within normal limits and he is otherwise medically healthy. Notable laboratory findings include elevated white blood cell count and platelets, and decreased hemoglobin.
A CT scan shows a large hematoma over the anterior abdominal wall extending toward the flanks with extensive subcutaneous emphysema. The peritoneum is intact. These findings raise the medical team’s concern about possible infection and vascular instability. The involuntary psychiatric hold for observation is continued after evaluation in the ED.
Photo Dr. T’s chest and abdomen during presentation to the ED
Note the asymmetry of the nipples and scarring from prior self-surgeries
The authors’ observations
There is a disconnect between Dr. T’s perception of his physical attributes and the treatment team’s observations. He perceives himself as marred by physical defects, while the treatment team sees him as a handsome and attractive person— excluding his scars from self-surgery.
Patients with BDD frequently are concerned about perceived physical defects that objective observers would consider slight or not noticeable. Three-quarters of individuals with BDD seek surgery or other medical treatment for their perceived physical flaws.4 Many patients minimize their BDD symptoms and their distress when talking with health care professionals.14 Approximately 20% of cosmetic surgery patients report ongoing psychiatric treatment at the time of surgery.15 Eighty-four percent of cosmetic surgeons state they have refused to operate on a patient because of BDD.16 However, it may be difficult for surgeons to distinguish a “perfectionist” from a patient with BDD.17 Even “positive” cosmetic surgery outcomes do not ameliorate BDD symptoms because most patients develop new areas of concern. In a small study of patients with minimal defects who requested cosmetic surgery, surgery did not reduce symptoms of BDD, disability, or psychiatric comorbidity in 6 out of 7 patients at 5-year follow up.18
Specialized medical equipment, such as surgical instruments and dermabrasion or laser hair removal devices, can be purchased on the Internet, which may increase the likelihood of individuals attempting procedures on themselves. Veale14 published a retrospective case series of patients who were turned down or unable to afford cosmetic surgery who performed self-surgery. These efforts did not lead to the desired effect, and patients continued to be plagued by their original concerns as well as self-inflicted scarring and damage.
Dr. T had the training and resources to perform cosmetic procedures on himself. Unfortunately, these efforts led to disfigurement. Phillips13 states that although self-surgery appears infrequently, it reflects the severe emotional pain and desperation felt by some patients with BDD. Self-surgery is associated with an increased rate of serious suicide attempts.14 Carefully monitor any BDD patient for suicidal ideation, intent, or plans.
TREATMENT: Refuses follow-up
Dr. T is admitted to the medical service and stabilized with IV fluids and antibiotics. The consultation-liaison service followed him during hospitalization. Because repeated interviews do not uncover grave disability or an imminent danger to himself or others, the involuntary psychiatric hold is discontinued. Dr. T declines psychiatric follow-up care, but says he would consider seeing a mental health professional in the future.
The authors’ observations
This case involves challenging ethical, legal, and countertransference issues. One of the first dilemmas the treatment team encountered was the decision to continue the involuntary hold for observation and assessment. The ED physician and psychiatric resident were faced with telling a fellow physician that he had to remain in the hospital despite his adamant desire to leave. Dr. T’s articulate arguments against staying in the hospital were addressed in order to deliver needed medical treatment. The psychiatric, surgical, and internal medicine teams discussed these countertransference concerns extensively during Dr. T’s hospitalization.
Clearly, Dr. T demonstrated poor judgment by operating on himself, and we aimed to ensure that he received appropriate psychiatric follow-up, but it could not be mandated. After intense and strongly debated ethical and legal discussions with the hospital’s ethicists and risk management team, we determined that we could not file a report with the state medical board because there was no evidence of incompetence, malpractice, or imminent risk to patients. A detailed description of these discussions is omitted from this article to preserve Dr. T’s confidentiality. However, Dr. T will have to disclose and explain the involuntary psychiatric hold on his next medical license renewal.
Our decision was influenced by Phillips,13 who found that although patients with BDD may have minimal insight into their illness, “their judgment remains intact in areas unrelated to their body image problem. Attention span and memory are well preserved, and physical and neurologic examinations are normal.” Although Dr. T meets criteria for BDD, mental illness in physicians is not synonymous with impairment.19
BDD treatment options
With medications and psychotherapy, patients with BDD generally have a good prognosis. A recent meta-analysis found that SSRIs and cognitive-behavioral therapy are effective treatments for BDD.20 In general, higher doses of SSRIs are needed to treat BDD compared with depression. Other medications with evidence of efficacy for BDD include the serotonin norepinephrine reuptake inhibitor venlafaxine21 and the anticonvulsant levetiracetam.22 However, clinicians often don’t have the opportunity to try these approaches because BDD patients are difficult to engage in treatment, as is evident in Dr. T’s case. Innovative approaches that combine practical and evidence-based strategies have been manualized.23 These approaches can help clinicians engage BDD patients in treatment and recognize underlying issues of distorted body image.
Related Resources
- BDD Central. www.bddcentral.com.
- Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
Drug Brand Names
- Alprazolam • Xanax
- Levetiracetam • Keppra
- Propranolol • Inderal
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Rapaport receives grant/research support from the National Institute of Mental Health and the National Center for Complementary and Alternative Medicine and is a consultant for Affectis Pharmaceuticals, Methylation Sciences, PAX Pharmaceuticals, and Johnson and Johnson Pharmaceuticals.
Drs. Rafin and Pimstone report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors wish to thank Dr. Kristine Andrade for editorial assistance. We also wish to thank the Institutional Review Board at Cedars-Sinai Medical Center for its review and approval of this case report, and Dr. T for his consent to publish it.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Phillips KA, Menard W, Fay C, et al. Demographic characteristics, phenomenology, comorbidity, and family history in 200 individuals with body dysmorphic disorder. Psychosomatics. 2005;46:317-325.
3. Phillips KA, McElroy SL, Keck PE, Jr, et al. A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases. Psychopharmacol Bull. 1994;30:179-186.
4. Crerand CE, Franklin ME, Sarwer DB. Patient safety: body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2008;122(4S):1-15.
5. DeMarco LM, Li LC, Phillips KA, et al. Perceived stress in body dysmorphic disorder. J Nerv Ment Dis. 1998;186(11):724-726.
6. Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2006;118(7):167-180.
7. Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185(9):570-577.
8. Woodie DS, Fromuth ME. The relationship of hypercompetitiveness and gender roles with body dysmorphic disorder symptoms in a nonclinical sample. Body Image. 2009;6(4):318-321.
9. Perugi G, Akiskal HS, Giannotti D, et al. Gender-related differences in body dysmorphic disorder (dysmorphophobia). J Nerv Ment Dis. 1997;185(9):578-582.
10. Veale D, Ennis M, Lambrou C. Possible association of body dysmorphic disorder with an occupation or education in art and design. Am J Psychiatry. 2002;159(10):1788-1790.
11. Phillips KA, Menard W. Body dysmorphic disorder and art background. Am J Psychiatry. 2004;161:927-928.
12. Ather MT, Mehrine S, Saqib GA, et al. Body dysmorphic disorder: gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry. 2008;8:20.
13. Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
14. Veale D. Outcome of cosmetic surgery and ‘DIY’ surgery in patients with body dysmorphic disorder. Psychiatric Bulletin. 2000;24:218-220.
15. Sarwer DB, Zanville HA, LaRossa D, et al. Mental health histories and psychiatric medication usage among persons who sought cosmetic surgery. Plast Reconstr Surg. 2004;114:1927-1933.
16. Sarwer DB. Awareness and identification of body dysmorphic disorder by aesthetic surgeons: results of a survey of American Society for Aesthetic Plastic Surgery members. Aesthet Surg J. 2002;22:531-535.
17. Glaser DA, Kaminer MS. Body dysmorphic disorder and the liposuction patient. Dermatol Surg. 2005;31(5):559-560.
18. Tignol J, Biraben-Gotzamanis L, Martin-Guehl C, et al. Body dysmorphic disorder and cosmetic surgery: evolution of 24 subjects with a minimal defect in appearance 5 years after their request for cosmetic surgery. Eur Psychiatry. 2007;22(8):520-524.
19. Myers MF. The psychiatrist’s role in the management of impaired colleagues. Directions in Psychiatry. 1995;15:1-8.
20. Ipser JC, Sander C, Stein DJ. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database Syst Rev. 2009;(1):CD005332.
21. Allen A, Hadley SJ, Kaplan A, et al. An open-label trial of venlafaxine in body dysmorphic disorder. CNS Spectr. 2008;13(2):138-144.
22. Phillips KA, Menard W. A prospective pilot study of levetiracetam for body dysmorphic disorder. CNS Spectr. 2009;14(5):252-260.
23. Veale D, Neziroglu F. Body dysmorphic disorder: a treatment manual. West Sussex, United Kingdom: Wiley-Blackwell; 2010.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
2. Phillips KA, Menard W, Fay C, et al. Demographic characteristics, phenomenology, comorbidity, and family history in 200 individuals with body dysmorphic disorder. Psychosomatics. 2005;46:317-325.
3. Phillips KA, McElroy SL, Keck PE, Jr, et al. A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases. Psychopharmacol Bull. 1994;30:179-186.
4. Crerand CE, Franklin ME, Sarwer DB. Patient safety: body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2008;122(4S):1-15.
5. DeMarco LM, Li LC, Phillips KA, et al. Perceived stress in body dysmorphic disorder. J Nerv Ment Dis. 1998;186(11):724-726.
6. Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2006;118(7):167-180.
7. Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185(9):570-577.
8. Woodie DS, Fromuth ME. The relationship of hypercompetitiveness and gender roles with body dysmorphic disorder symptoms in a nonclinical sample. Body Image. 2009;6(4):318-321.
9. Perugi G, Akiskal HS, Giannotti D, et al. Gender-related differences in body dysmorphic disorder (dysmorphophobia). J Nerv Ment Dis. 1997;185(9):578-582.
10. Veale D, Ennis M, Lambrou C. Possible association of body dysmorphic disorder with an occupation or education in art and design. Am J Psychiatry. 2002;159(10):1788-1790.
11. Phillips KA, Menard W. Body dysmorphic disorder and art background. Am J Psychiatry. 2004;161:927-928.
12. Ather MT, Mehrine S, Saqib GA, et al. Body dysmorphic disorder: gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry. 2008;8:20.
13. Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New York, NY: Oxford University Press; 2005.
14. Veale D. Outcome of cosmetic surgery and ‘DIY’ surgery in patients with body dysmorphic disorder. Psychiatric Bulletin. 2000;24:218-220.
15. Sarwer DB, Zanville HA, LaRossa D, et al. Mental health histories and psychiatric medication usage among persons who sought cosmetic surgery. Plast Reconstr Surg. 2004;114:1927-1933.
16. Sarwer DB. Awareness and identification of body dysmorphic disorder by aesthetic surgeons: results of a survey of American Society for Aesthetic Plastic Surgery members. Aesthet Surg J. 2002;22:531-535.
17. Glaser DA, Kaminer MS. Body dysmorphic disorder and the liposuction patient. Dermatol Surg. 2005;31(5):559-560.
18. Tignol J, Biraben-Gotzamanis L, Martin-Guehl C, et al. Body dysmorphic disorder and cosmetic surgery: evolution of 24 subjects with a minimal defect in appearance 5 years after their request for cosmetic surgery. Eur Psychiatry. 2007;22(8):520-524.
19. Myers MF. The psychiatrist’s role in the management of impaired colleagues. Directions in Psychiatry. 1995;15:1-8.
20. Ipser JC, Sander C, Stein DJ. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database Syst Rev. 2009;(1):CD005332.
21. Allen A, Hadley SJ, Kaplan A, et al. An open-label trial of venlafaxine in body dysmorphic disorder. CNS Spectr. 2008;13(2):138-144.
22. Phillips KA, Menard W. A prospective pilot study of levetiracetam for body dysmorphic disorder. CNS Spectr. 2009;14(5):252-260.
23. Veale D, Neziroglu F. Body dysmorphic disorder: a treatment manual. West Sussex, United Kingdom: Wiley-Blackwell; 2010.
A case of returning psychosis
CASE: Agitated and violent
Police bring Ms. Y, age 42, to the emergency room (ER) after her boyfriend calls 911 because she is physically aggressive. The police note that the home is in disarray and several windows are broken. Ms. Y is threatening and violent—she bites and spits at her boyfriend and the police. The ER assessment reports that she is “agitated, confused, and not making sense.” She receives IV haloperidol, 5 mg, for agitation and aggressive behavior, but does not improve and receives a second dose of haloperidol approximately 1 hour later.
On examination she is afebrile. Laboratory results are notable for elevated blood urea nitrogen (27 mg/dL) and creatinine (2.3 mg/dL), suggesting renal failure. Her white blood cell (WBC) count is elevated at 14.7 K/μL with increased neutrophil count. Her creatine phosphokinase (CPK) also is elevated at 2,778 U/L. Other lab results, including liver function tests and a rapid plasma reagin, are within normal limits. Urinalysis reveals WBC >50 and leukocyte esterase 3+ WBC/μL. Urine drug screen is negative for barbiturates, benzodiazepines, opiates, and cocaine and her blood alcohol level is <10 mg/dL. She is overweight, but not obese. Ms. Y is admitted to the medical service for workup of rhabdomyolysis and altered mental status.
When the psychiatric consultation-liaison (CL) service evaluates Ms. Y 12 hours after presentation, she is disheveled, drowsy, and lying in bed, with multiple superficial lacerations on her forearms. She is cooperative but claims to have no recollection of the events leading up to her admission. Her speech is soft with a lack of spontaneity, and she demonstrates substantial psychomotor retardation. Her mood is irritable and affect is restricted. She has a latency of thought and difficulty recalling basic historic information. Ms. Y appears confused and frequently responds to questions with “I don’t remember.” She seems frustrated and distressed by her inability to answer questions. She denies suicidal or homicidal ideation and auditory or visual hallucinations, although she appears to be responding to internal stimuli. We cannot complete a Mini-Mental State Exam because she becomes uncooperative. After 10 minutes, Ms. Y ends the interview, stating that too much is being “demanded” of her.
The authors’ observations
Ms. Y’s acute-onset agitation and confusion could be caused by an infection, such as a urinary tract infection, a frequent culprit in delirium or transient psychosis. Seizure activity with postictal confusion also has to be included in the differential, as well as an endogenous psychotic disorder such as schizophrenia or a manic bipolar episode. Ms. Y’s boyfriend of 16 months indicated that Ms. Y uses alcohol but cannot quantify the amount or frequency. We considered and ruled out other intoxicant use as a potential cause of her transient psychosis. An extended drug screen was negative and her lab values did not suggest heavy alcohol use.
HISTORY: Past psychotic episodes
Ms. Y’s boyfriend reports that she had 2 psychiatric hospitalizations approximately 30 years ago, which were precipitated by psychotic symptoms that she developed while abusing drugs. To the best of his knowledge Ms. Y had not used these agents recently. He stated that Ms. Y did not appear to have ongoing psychotic symptoms and had not received psychiatric treatment since she was a teenager until 6 months ago. He describes the current hospitalization as being “just like 6 months ago.”
Medical records reveal that Ms. Y was admitted to our hospital 6 months ago because she was acting violently and combative. She was “talking out of context,” “stated that she was God,” and had auditory hallucinations. She was admitted to the medical service for rhabdomyolysis, which was thought to be caused by hyperactivity or exertion. Ms. Y indicated that she was taking food supplements, including L-carnitine, to help lose weight. Her psychotic symptoms cleared within 24 hours and she was discharged without any psychiatric medications. Her behavioral disturbance was attributed to ingesting excessive amounts of carnitine supplements, and Ms. Y was counseled to abstain from them.
The authors’ observations
Carnitine is a common dietary supplement that is advertised as being safe and effective.1 It is purported to increase fat oxidation or reduce fat synthesis; however, no trials demonstrate that L-carnitine is effective for weight loss (Box).2-7 Evidence from well-designed randomized, controlled clinical trials indicates that the safe upper limit of long-term intake is 2,000 mg/d of L-carnitine equivalents.8 The data for doses >2,000 mg/d are not sufficient to make a confident conclusion on long-term safety.8
Further evaluation for possible causes of Ms. Y’s symptoms include a chest radiography and blood and urine cultures, which are unremarkable. Results of a lumbar puncture are within normal limits. Computed tomography of the head reveals confluent periventricular hypodensities compatible with moderate to severe non-specific white matter disease.
Carnitine is derived from an amino acid and found in nearly all cells of the body. “Carnitine” is used to refer to several compounds, including L-carnitine, acetyl-L-carnitine, and propionyl-L-carnitine. The natural form and the only one with biologic activity is the geometric isomer L-carnitine. Most endogenous L-carnitine is derived from diet— meat and dairy are the primary sources—and the remainder is synthesized.2-4
Carnitine transports long-chain fatty acids into the mitochondria so they can be oxidized to produce energy and transports toxic compounds out of the mitochondria to prevent them from accumulating. Carnitine is concentrated in tissues that use fatty acids as a dietary fuel, such as skeletal and cardiac muscle.2-4 The body makes enough carnitine to meet most person’s needs and supplementation typically is not required. Some drugs, such as valproic acid and carbamazepine, can reduce carnitine blood concentrations.2
Because of its role in fatty acid oxidation, carnitine often is promoted as a weight loss aid. In addition, it is purported to improve exercise performance and enhance well-being.3,4 However, there is no consistent evidence that carnitine supplements can improve physical performance in healthy individuals.5
At doses of approximately 3 g/d, carnitine supplements can cause nausea, vomiting, abdominal cramps, diarrhea, and a “fishy” body odor. Rare side effects include muscle weakness in uremic patients and seizures in those with a seizure disorder.2-4
In animal studies, carnitine persistently increases dopamine outflow in the nucleus accumbens.6 Dopamine dysregulation in this pathway has been shown to cause psychotic symptoms.7
TREATMENT: Rapid improvement
Ms. Y’s renal dysfunction resolves within 24 hours with aggressive hydration and supportive therapy. Her WBC count normalizes and her CPK decreases.
When Ms. Y becomes more cooperative, the CL team pieces together more of her story with further interviews and collateral information from her cousin. Ms. Y’s family history includes an aunt with schizophrenia. Three years ago Ms. Y moved from the Midwest to a large Southern city with her husband, from whom she is divorced. She has 2 children who were removed from her custody when she was a teenager for unclear reasons. At admission, she lives with her boyfriend, whom she plans on marrying.
Ms. Y says she was taking carnitine to improve her energy and lose weight. She recalls that her physicians advised her to discontinue carnitine supplements, but she continued to take “4 or 5 a day” in an ongoing attempt to lose weight. When asked about other supplements, Ms. Y reports regularly consuming 16-ounce energy drinks, including the day before admission. The label on this drink lists L-carnitine and caffeine as main ingredients. She denies regularly drinking other caffeine-containing beverages, including coffee, tea, or soda.
The authors’ observations
Supplements for weight loss may appeal to people’s desire for a “quick fix” that is less demanding than diets and increased physical activity. Supplements are available without a prescription and despite reports of adverse reactions generally are perceived as being safe and having few side effects. These supplements may be marketed as “natural,” which can be misinterpreted as an assurance of safety and efficacy.
Given the similarities of the current admission to the one 6 months ago, we suspect Ms. Y is experiencing transient psychosis secondary to carnitine intoxication. Based on Ms. Y’s boyfriend’s report and the product labeling, we estimate that Ms. Y took approximately 4,000 mg of carnitine in the 24 hours before admission.
Other causes of transient psychosis, such as infectious, metabolic, and neoplastic processes, were considered and ruled out. Seizures with postictal confusion also was ruled out because Ms. Y does not have a history of seizures and there is no evidence of convulsive activity, incontinence, or buccal lacerations. Given Ms. Y’s family history of schizophrenia and reported history of psychotic symptoms as a teenager we considered that she may have an endogenous psychotic disorder. However, her psychotic symptoms were transient, and Ms. Y returned to her baseline level of functioning between episodes.
OUTCOME: Advice to stop
We start Ms. Y on risperidone, 2 mg/d, at bedtime for her psychotic symptoms. Her psychotic symptoms quickly improve. She seems to return to her baseline state approximately 36 hours after admission and is medically cleared for discharge. Risperidone is discontinued after only 1 dose.
Ms. Y is remorseful over her recent aggressive behavior, and fears that her boyfriend will leave her. She denies suicidal and homicidal ideation and does not require inpatient psychiatric hospitalization. We strongly advise her to discontinue carnitine supplements and energy drinks and to limit her caffeine intake. Because Ms. Y’s had continued to use carnitine supplements despite adverse consequences and against medical advice, we refer her for substance abuse treatment.
The authors’ observations
Although temporal coincidence does not necessarily imply causality, in Ms. Y’s case, the relationship between carnitine ingestion and psychiatric symptoms cannot be ignored. Individuals predisposed to mania or psychosis may be more likely to respond adversely after ingesting nutritional supplements or energy drinks.9 Ms. Y’s past psychotic episodes suggest that she could be vulnerable to future episodes. She also might have a biologic predisposition to psychosis because of her family history of schizophrenia.
The literature contains at least 1 other reported case of carnitine-induced psychosis. A patient with a history of bipolar disorder presented with auditory hallucinations, persecutory delusions, and verbally threatening and physically assaultive behavior 5 days after beginning nutritional supplements containing carnitine.1 There also are reports of patients who experienced acute changes in mental status after consuming other nutritional weight loss supplements (Table).9-17 Chelben et al9 describe 3 patients with known psychiatric illness who showed clinical deterioration leading to psychiatric hospitalization after ingesting nutraceutical preparations. This may be a common but unrecognized cause of decompensation in psychiatric patients who take supplements.
This case highlights the importance of being aware of patients’ use of alternative medications or nutritional supplements. Physicians should routinely inquire about the use of weight loss products, energy drinks, and supplements, and patients should be educated about the risks, including potential to exacerbate pre-existing psychiatric disorders.
Table
Psychiatric effects of common weight loss supplements
| Supplement | Psychiatric effects |
|---|---|
| Caffeine | Depression, anxiety, agitation, aggression, psychosis10-12 |
| Ephedra* | Psychosis, severe depression, mania or agitation, hallucinations, sleep disturbance, suicidal ideation13 |
| Panax (ginseng) | Euphoria, mania14 |
| Amino acid-containing drinks (taurine and inositol) | Euphoria, hypervigilance, insomnia, verbal and physical aggression, impulsive behavior9,15 |
| Hypericum (St. John’s wort) | Mania,16 psychosis17 |
| *FDA removed ephedra from the market in 2003 because of adverse events | |
Related Resources
- National Library of Medicine. Dietary supplements labels database. http://dietarysupplements.nlm.nih.gov/dietary.
- Grossberg G, Fox B. The essential herb-drug-vitamin interaction guide. New York, NY: Broadway Books; 2007.
Drug Brand Names
- Carbamazepine • Tegretol
- Haloperidol • Haldol
- Risperidone • Risperdal
- Valproic acid • Depakene
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Evcimen H, Mania I, Mathews M, et al. Psychosis precipitated by acetyl-L-carnitine in a patient with bipolar disorder. Prim Care Companion J Clin Psychiatry. 2007;9(1):71-72.
2. Office of Dietary Supplements National Institutes of Health. Dietary supplement fact sheet: carnitine. Available at: http://ods.od.nih.gov/factsheets/carnitine.asp. Accessed November 22, 2010.
3. Carnitine: lessons from one hundred years of research Ann NY Acad Sci. 2004;1033:ix-xi.
4. Rebouche CJ, Carnitine. In: Shils ME, Olson JA, Shike M, et al, eds. Modern nutrition in health and disease. 9th ed. Baltimore, MD: Lippincott Williams and Wilkins; 1999: 505-512.
5. Brass EP. Carnitine and sports medicine: use or abuse? Ann NY Acad Sci. 2004;1033:67-78.
6. Scheggi S, Rauggi R, Nanni G, et al. Repeated acetyl-L-carnitine administration increases phosphor-Thr34 DARPP-32 levels and antagonizes cocaine-induced increase in Cdk5 and phosphor-Thr75 DARPP-32 levels in rat striatum. Eur J Neurosci. 2004;19:1609-1620.
7. Howes OD, McDonald C, Cannon M, et al. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7(suppl 1):S7-S13.
8. Hathcock JN, Shao A. Risk assessment for carnitine. Regul Toxicol Pharmacol. 2006;46:23-28.
9. Chelben J, Piccone-Sapir A, Ianco I, et al. Effects of amino acid energy drinks leading to hospitalization in individuals with mental illness. Gen Hosp Psychiatry. 2008;30(2):187-189.
10. Hedges DW, Woon FL, Hoopes SP. Caffeine-induced psychosis. CNS Spectr. 2009;14:127-129.
11. Broderick P, Benjamin AB. Caffeine and psychiatric symptoms: a review. J Okla State Med Assoc. 2004;97(12):538-542.
12. Cerimele JM, Stern AP, Jutras-Aswad D. Psychosis following excessive ingestion of energy drinks in a patient with schizophrenia. Am J Psychiatry. 2010;167(3):353.-
13. Maglione M, Miotto K, Iguchi M, et al. Psychiatric effects of ephedra use: an analysis of Food and Drug Administration reports of adverse events. Am J Psychiatry. 2005;162(1):189-191.
14. Engelberg D, McCutcheon A, Wiseman S. A case of ginseng-induced mania. J Clin Psychopharmacol. 2001;21(5):535-537.
15. Machado-Vieira R, Viale CI, Kapczinski F. Mania associated with an energy drink: the possible role of caffeine, taurine and inositol. Can J Psychiatry. 2001;46:454-455.
16. Fahmi M, Huang C, Schweitzer I. A case of mania induced by hypericum. World J Biol Psychiatry. 2002;3(1):58-59.
17. Stevinson C, Ernst E. Can St. John’s wort trigger psychoses? Int J Clin Pharmacol Ther. 2004;42(9):473-480.
CASE: Agitated and violent
Police bring Ms. Y, age 42, to the emergency room (ER) after her boyfriend calls 911 because she is physically aggressive. The police note that the home is in disarray and several windows are broken. Ms. Y is threatening and violent—she bites and spits at her boyfriend and the police. The ER assessment reports that she is “agitated, confused, and not making sense.” She receives IV haloperidol, 5 mg, for agitation and aggressive behavior, but does not improve and receives a second dose of haloperidol approximately 1 hour later.
On examination she is afebrile. Laboratory results are notable for elevated blood urea nitrogen (27 mg/dL) and creatinine (2.3 mg/dL), suggesting renal failure. Her white blood cell (WBC) count is elevated at 14.7 K/μL with increased neutrophil count. Her creatine phosphokinase (CPK) also is elevated at 2,778 U/L. Other lab results, including liver function tests and a rapid plasma reagin, are within normal limits. Urinalysis reveals WBC >50 and leukocyte esterase 3+ WBC/μL. Urine drug screen is negative for barbiturates, benzodiazepines, opiates, and cocaine and her blood alcohol level is <10 mg/dL. She is overweight, but not obese. Ms. Y is admitted to the medical service for workup of rhabdomyolysis and altered mental status.
When the psychiatric consultation-liaison (CL) service evaluates Ms. Y 12 hours after presentation, she is disheveled, drowsy, and lying in bed, with multiple superficial lacerations on her forearms. She is cooperative but claims to have no recollection of the events leading up to her admission. Her speech is soft with a lack of spontaneity, and she demonstrates substantial psychomotor retardation. Her mood is irritable and affect is restricted. She has a latency of thought and difficulty recalling basic historic information. Ms. Y appears confused and frequently responds to questions with “I don’t remember.” She seems frustrated and distressed by her inability to answer questions. She denies suicidal or homicidal ideation and auditory or visual hallucinations, although she appears to be responding to internal stimuli. We cannot complete a Mini-Mental State Exam because she becomes uncooperative. After 10 minutes, Ms. Y ends the interview, stating that too much is being “demanded” of her.
The authors’ observations
Ms. Y’s acute-onset agitation and confusion could be caused by an infection, such as a urinary tract infection, a frequent culprit in delirium or transient psychosis. Seizure activity with postictal confusion also has to be included in the differential, as well as an endogenous psychotic disorder such as schizophrenia or a manic bipolar episode. Ms. Y’s boyfriend of 16 months indicated that Ms. Y uses alcohol but cannot quantify the amount or frequency. We considered and ruled out other intoxicant use as a potential cause of her transient psychosis. An extended drug screen was negative and her lab values did not suggest heavy alcohol use.
HISTORY: Past psychotic episodes
Ms. Y’s boyfriend reports that she had 2 psychiatric hospitalizations approximately 30 years ago, which were precipitated by psychotic symptoms that she developed while abusing drugs. To the best of his knowledge Ms. Y had not used these agents recently. He stated that Ms. Y did not appear to have ongoing psychotic symptoms and had not received psychiatric treatment since she was a teenager until 6 months ago. He describes the current hospitalization as being “just like 6 months ago.”
Medical records reveal that Ms. Y was admitted to our hospital 6 months ago because she was acting violently and combative. She was “talking out of context,” “stated that she was God,” and had auditory hallucinations. She was admitted to the medical service for rhabdomyolysis, which was thought to be caused by hyperactivity or exertion. Ms. Y indicated that she was taking food supplements, including L-carnitine, to help lose weight. Her psychotic symptoms cleared within 24 hours and she was discharged without any psychiatric medications. Her behavioral disturbance was attributed to ingesting excessive amounts of carnitine supplements, and Ms. Y was counseled to abstain from them.
The authors’ observations
Carnitine is a common dietary supplement that is advertised as being safe and effective.1 It is purported to increase fat oxidation or reduce fat synthesis; however, no trials demonstrate that L-carnitine is effective for weight loss (Box).2-7 Evidence from well-designed randomized, controlled clinical trials indicates that the safe upper limit of long-term intake is 2,000 mg/d of L-carnitine equivalents.8 The data for doses >2,000 mg/d are not sufficient to make a confident conclusion on long-term safety.8
Further evaluation for possible causes of Ms. Y’s symptoms include a chest radiography and blood and urine cultures, which are unremarkable. Results of a lumbar puncture are within normal limits. Computed tomography of the head reveals confluent periventricular hypodensities compatible with moderate to severe non-specific white matter disease.
Carnitine is derived from an amino acid and found in nearly all cells of the body. “Carnitine” is used to refer to several compounds, including L-carnitine, acetyl-L-carnitine, and propionyl-L-carnitine. The natural form and the only one with biologic activity is the geometric isomer L-carnitine. Most endogenous L-carnitine is derived from diet— meat and dairy are the primary sources—and the remainder is synthesized.2-4
Carnitine transports long-chain fatty acids into the mitochondria so they can be oxidized to produce energy and transports toxic compounds out of the mitochondria to prevent them from accumulating. Carnitine is concentrated in tissues that use fatty acids as a dietary fuel, such as skeletal and cardiac muscle.2-4 The body makes enough carnitine to meet most person’s needs and supplementation typically is not required. Some drugs, such as valproic acid and carbamazepine, can reduce carnitine blood concentrations.2
Because of its role in fatty acid oxidation, carnitine often is promoted as a weight loss aid. In addition, it is purported to improve exercise performance and enhance well-being.3,4 However, there is no consistent evidence that carnitine supplements can improve physical performance in healthy individuals.5
At doses of approximately 3 g/d, carnitine supplements can cause nausea, vomiting, abdominal cramps, diarrhea, and a “fishy” body odor. Rare side effects include muscle weakness in uremic patients and seizures in those with a seizure disorder.2-4
In animal studies, carnitine persistently increases dopamine outflow in the nucleus accumbens.6 Dopamine dysregulation in this pathway has been shown to cause psychotic symptoms.7
TREATMENT: Rapid improvement
Ms. Y’s renal dysfunction resolves within 24 hours with aggressive hydration and supportive therapy. Her WBC count normalizes and her CPK decreases.
When Ms. Y becomes more cooperative, the CL team pieces together more of her story with further interviews and collateral information from her cousin. Ms. Y’s family history includes an aunt with schizophrenia. Three years ago Ms. Y moved from the Midwest to a large Southern city with her husband, from whom she is divorced. She has 2 children who were removed from her custody when she was a teenager for unclear reasons. At admission, she lives with her boyfriend, whom she plans on marrying.
Ms. Y says she was taking carnitine to improve her energy and lose weight. She recalls that her physicians advised her to discontinue carnitine supplements, but she continued to take “4 or 5 a day” in an ongoing attempt to lose weight. When asked about other supplements, Ms. Y reports regularly consuming 16-ounce energy drinks, including the day before admission. The label on this drink lists L-carnitine and caffeine as main ingredients. She denies regularly drinking other caffeine-containing beverages, including coffee, tea, or soda.
The authors’ observations
Supplements for weight loss may appeal to people’s desire for a “quick fix” that is less demanding than diets and increased physical activity. Supplements are available without a prescription and despite reports of adverse reactions generally are perceived as being safe and having few side effects. These supplements may be marketed as “natural,” which can be misinterpreted as an assurance of safety and efficacy.
Given the similarities of the current admission to the one 6 months ago, we suspect Ms. Y is experiencing transient psychosis secondary to carnitine intoxication. Based on Ms. Y’s boyfriend’s report and the product labeling, we estimate that Ms. Y took approximately 4,000 mg of carnitine in the 24 hours before admission.
Other causes of transient psychosis, such as infectious, metabolic, and neoplastic processes, were considered and ruled out. Seizures with postictal confusion also was ruled out because Ms. Y does not have a history of seizures and there is no evidence of convulsive activity, incontinence, or buccal lacerations. Given Ms. Y’s family history of schizophrenia and reported history of psychotic symptoms as a teenager we considered that she may have an endogenous psychotic disorder. However, her psychotic symptoms were transient, and Ms. Y returned to her baseline level of functioning between episodes.
OUTCOME: Advice to stop
We start Ms. Y on risperidone, 2 mg/d, at bedtime for her psychotic symptoms. Her psychotic symptoms quickly improve. She seems to return to her baseline state approximately 36 hours after admission and is medically cleared for discharge. Risperidone is discontinued after only 1 dose.
Ms. Y is remorseful over her recent aggressive behavior, and fears that her boyfriend will leave her. She denies suicidal and homicidal ideation and does not require inpatient psychiatric hospitalization. We strongly advise her to discontinue carnitine supplements and energy drinks and to limit her caffeine intake. Because Ms. Y’s had continued to use carnitine supplements despite adverse consequences and against medical advice, we refer her for substance abuse treatment.
The authors’ observations
Although temporal coincidence does not necessarily imply causality, in Ms. Y’s case, the relationship between carnitine ingestion and psychiatric symptoms cannot be ignored. Individuals predisposed to mania or psychosis may be more likely to respond adversely after ingesting nutritional supplements or energy drinks.9 Ms. Y’s past psychotic episodes suggest that she could be vulnerable to future episodes. She also might have a biologic predisposition to psychosis because of her family history of schizophrenia.
The literature contains at least 1 other reported case of carnitine-induced psychosis. A patient with a history of bipolar disorder presented with auditory hallucinations, persecutory delusions, and verbally threatening and physically assaultive behavior 5 days after beginning nutritional supplements containing carnitine.1 There also are reports of patients who experienced acute changes in mental status after consuming other nutritional weight loss supplements (Table).9-17 Chelben et al9 describe 3 patients with known psychiatric illness who showed clinical deterioration leading to psychiatric hospitalization after ingesting nutraceutical preparations. This may be a common but unrecognized cause of decompensation in psychiatric patients who take supplements.
This case highlights the importance of being aware of patients’ use of alternative medications or nutritional supplements. Physicians should routinely inquire about the use of weight loss products, energy drinks, and supplements, and patients should be educated about the risks, including potential to exacerbate pre-existing psychiatric disorders.
Table
Psychiatric effects of common weight loss supplements
| Supplement | Psychiatric effects |
|---|---|
| Caffeine | Depression, anxiety, agitation, aggression, psychosis10-12 |
| Ephedra* | Psychosis, severe depression, mania or agitation, hallucinations, sleep disturbance, suicidal ideation13 |
| Panax (ginseng) | Euphoria, mania14 |
| Amino acid-containing drinks (taurine and inositol) | Euphoria, hypervigilance, insomnia, verbal and physical aggression, impulsive behavior9,15 |
| Hypericum (St. John’s wort) | Mania,16 psychosis17 |
| *FDA removed ephedra from the market in 2003 because of adverse events | |
Related Resources
- National Library of Medicine. Dietary supplements labels database. http://dietarysupplements.nlm.nih.gov/dietary.
- Grossberg G, Fox B. The essential herb-drug-vitamin interaction guide. New York, NY: Broadway Books; 2007.
Drug Brand Names
- Carbamazepine • Tegretol
- Haloperidol • Haldol
- Risperidone • Risperdal
- Valproic acid • Depakene
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Agitated and violent
Police bring Ms. Y, age 42, to the emergency room (ER) after her boyfriend calls 911 because she is physically aggressive. The police note that the home is in disarray and several windows are broken. Ms. Y is threatening and violent—she bites and spits at her boyfriend and the police. The ER assessment reports that she is “agitated, confused, and not making sense.” She receives IV haloperidol, 5 mg, for agitation and aggressive behavior, but does not improve and receives a second dose of haloperidol approximately 1 hour later.
On examination she is afebrile. Laboratory results are notable for elevated blood urea nitrogen (27 mg/dL) and creatinine (2.3 mg/dL), suggesting renal failure. Her white blood cell (WBC) count is elevated at 14.7 K/μL with increased neutrophil count. Her creatine phosphokinase (CPK) also is elevated at 2,778 U/L. Other lab results, including liver function tests and a rapid plasma reagin, are within normal limits. Urinalysis reveals WBC >50 and leukocyte esterase 3+ WBC/μL. Urine drug screen is negative for barbiturates, benzodiazepines, opiates, and cocaine and her blood alcohol level is <10 mg/dL. She is overweight, but not obese. Ms. Y is admitted to the medical service for workup of rhabdomyolysis and altered mental status.
When the psychiatric consultation-liaison (CL) service evaluates Ms. Y 12 hours after presentation, she is disheveled, drowsy, and lying in bed, with multiple superficial lacerations on her forearms. She is cooperative but claims to have no recollection of the events leading up to her admission. Her speech is soft with a lack of spontaneity, and she demonstrates substantial psychomotor retardation. Her mood is irritable and affect is restricted. She has a latency of thought and difficulty recalling basic historic information. Ms. Y appears confused and frequently responds to questions with “I don’t remember.” She seems frustrated and distressed by her inability to answer questions. She denies suicidal or homicidal ideation and auditory or visual hallucinations, although she appears to be responding to internal stimuli. We cannot complete a Mini-Mental State Exam because she becomes uncooperative. After 10 minutes, Ms. Y ends the interview, stating that too much is being “demanded” of her.
The authors’ observations
Ms. Y’s acute-onset agitation and confusion could be caused by an infection, such as a urinary tract infection, a frequent culprit in delirium or transient psychosis. Seizure activity with postictal confusion also has to be included in the differential, as well as an endogenous psychotic disorder such as schizophrenia or a manic bipolar episode. Ms. Y’s boyfriend of 16 months indicated that Ms. Y uses alcohol but cannot quantify the amount or frequency. We considered and ruled out other intoxicant use as a potential cause of her transient psychosis. An extended drug screen was negative and her lab values did not suggest heavy alcohol use.
HISTORY: Past psychotic episodes
Ms. Y’s boyfriend reports that she had 2 psychiatric hospitalizations approximately 30 years ago, which were precipitated by psychotic symptoms that she developed while abusing drugs. To the best of his knowledge Ms. Y had not used these agents recently. He stated that Ms. Y did not appear to have ongoing psychotic symptoms and had not received psychiatric treatment since she was a teenager until 6 months ago. He describes the current hospitalization as being “just like 6 months ago.”
Medical records reveal that Ms. Y was admitted to our hospital 6 months ago because she was acting violently and combative. She was “talking out of context,” “stated that she was God,” and had auditory hallucinations. She was admitted to the medical service for rhabdomyolysis, which was thought to be caused by hyperactivity or exertion. Ms. Y indicated that she was taking food supplements, including L-carnitine, to help lose weight. Her psychotic symptoms cleared within 24 hours and she was discharged without any psychiatric medications. Her behavioral disturbance was attributed to ingesting excessive amounts of carnitine supplements, and Ms. Y was counseled to abstain from them.
The authors’ observations
Carnitine is a common dietary supplement that is advertised as being safe and effective.1 It is purported to increase fat oxidation or reduce fat synthesis; however, no trials demonstrate that L-carnitine is effective for weight loss (Box).2-7 Evidence from well-designed randomized, controlled clinical trials indicates that the safe upper limit of long-term intake is 2,000 mg/d of L-carnitine equivalents.8 The data for doses >2,000 mg/d are not sufficient to make a confident conclusion on long-term safety.8
Further evaluation for possible causes of Ms. Y’s symptoms include a chest radiography and blood and urine cultures, which are unremarkable. Results of a lumbar puncture are within normal limits. Computed tomography of the head reveals confluent periventricular hypodensities compatible with moderate to severe non-specific white matter disease.
Carnitine is derived from an amino acid and found in nearly all cells of the body. “Carnitine” is used to refer to several compounds, including L-carnitine, acetyl-L-carnitine, and propionyl-L-carnitine. The natural form and the only one with biologic activity is the geometric isomer L-carnitine. Most endogenous L-carnitine is derived from diet— meat and dairy are the primary sources—and the remainder is synthesized.2-4
Carnitine transports long-chain fatty acids into the mitochondria so they can be oxidized to produce energy and transports toxic compounds out of the mitochondria to prevent them from accumulating. Carnitine is concentrated in tissues that use fatty acids as a dietary fuel, such as skeletal and cardiac muscle.2-4 The body makes enough carnitine to meet most person’s needs and supplementation typically is not required. Some drugs, such as valproic acid and carbamazepine, can reduce carnitine blood concentrations.2
Because of its role in fatty acid oxidation, carnitine often is promoted as a weight loss aid. In addition, it is purported to improve exercise performance and enhance well-being.3,4 However, there is no consistent evidence that carnitine supplements can improve physical performance in healthy individuals.5
At doses of approximately 3 g/d, carnitine supplements can cause nausea, vomiting, abdominal cramps, diarrhea, and a “fishy” body odor. Rare side effects include muscle weakness in uremic patients and seizures in those with a seizure disorder.2-4
In animal studies, carnitine persistently increases dopamine outflow in the nucleus accumbens.6 Dopamine dysregulation in this pathway has been shown to cause psychotic symptoms.7
TREATMENT: Rapid improvement
Ms. Y’s renal dysfunction resolves within 24 hours with aggressive hydration and supportive therapy. Her WBC count normalizes and her CPK decreases.
When Ms. Y becomes more cooperative, the CL team pieces together more of her story with further interviews and collateral information from her cousin. Ms. Y’s family history includes an aunt with schizophrenia. Three years ago Ms. Y moved from the Midwest to a large Southern city with her husband, from whom she is divorced. She has 2 children who were removed from her custody when she was a teenager for unclear reasons. At admission, she lives with her boyfriend, whom she plans on marrying.
Ms. Y says she was taking carnitine to improve her energy and lose weight. She recalls that her physicians advised her to discontinue carnitine supplements, but she continued to take “4 or 5 a day” in an ongoing attempt to lose weight. When asked about other supplements, Ms. Y reports regularly consuming 16-ounce energy drinks, including the day before admission. The label on this drink lists L-carnitine and caffeine as main ingredients. She denies regularly drinking other caffeine-containing beverages, including coffee, tea, or soda.
The authors’ observations
Supplements for weight loss may appeal to people’s desire for a “quick fix” that is less demanding than diets and increased physical activity. Supplements are available without a prescription and despite reports of adverse reactions generally are perceived as being safe and having few side effects. These supplements may be marketed as “natural,” which can be misinterpreted as an assurance of safety and efficacy.
Given the similarities of the current admission to the one 6 months ago, we suspect Ms. Y is experiencing transient psychosis secondary to carnitine intoxication. Based on Ms. Y’s boyfriend’s report and the product labeling, we estimate that Ms. Y took approximately 4,000 mg of carnitine in the 24 hours before admission.
Other causes of transient psychosis, such as infectious, metabolic, and neoplastic processes, were considered and ruled out. Seizures with postictal confusion also was ruled out because Ms. Y does not have a history of seizures and there is no evidence of convulsive activity, incontinence, or buccal lacerations. Given Ms. Y’s family history of schizophrenia and reported history of psychotic symptoms as a teenager we considered that she may have an endogenous psychotic disorder. However, her psychotic symptoms were transient, and Ms. Y returned to her baseline level of functioning between episodes.
OUTCOME: Advice to stop
We start Ms. Y on risperidone, 2 mg/d, at bedtime for her psychotic symptoms. Her psychotic symptoms quickly improve. She seems to return to her baseline state approximately 36 hours after admission and is medically cleared for discharge. Risperidone is discontinued after only 1 dose.
Ms. Y is remorseful over her recent aggressive behavior, and fears that her boyfriend will leave her. She denies suicidal and homicidal ideation and does not require inpatient psychiatric hospitalization. We strongly advise her to discontinue carnitine supplements and energy drinks and to limit her caffeine intake. Because Ms. Y’s had continued to use carnitine supplements despite adverse consequences and against medical advice, we refer her for substance abuse treatment.
The authors’ observations
Although temporal coincidence does not necessarily imply causality, in Ms. Y’s case, the relationship between carnitine ingestion and psychiatric symptoms cannot be ignored. Individuals predisposed to mania or psychosis may be more likely to respond adversely after ingesting nutritional supplements or energy drinks.9 Ms. Y’s past psychotic episodes suggest that she could be vulnerable to future episodes. She also might have a biologic predisposition to psychosis because of her family history of schizophrenia.
The literature contains at least 1 other reported case of carnitine-induced psychosis. A patient with a history of bipolar disorder presented with auditory hallucinations, persecutory delusions, and verbally threatening and physically assaultive behavior 5 days after beginning nutritional supplements containing carnitine.1 There also are reports of patients who experienced acute changes in mental status after consuming other nutritional weight loss supplements (Table).9-17 Chelben et al9 describe 3 patients with known psychiatric illness who showed clinical deterioration leading to psychiatric hospitalization after ingesting nutraceutical preparations. This may be a common but unrecognized cause of decompensation in psychiatric patients who take supplements.
This case highlights the importance of being aware of patients’ use of alternative medications or nutritional supplements. Physicians should routinely inquire about the use of weight loss products, energy drinks, and supplements, and patients should be educated about the risks, including potential to exacerbate pre-existing psychiatric disorders.
Table
Psychiatric effects of common weight loss supplements
| Supplement | Psychiatric effects |
|---|---|
| Caffeine | Depression, anxiety, agitation, aggression, psychosis10-12 |
| Ephedra* | Psychosis, severe depression, mania or agitation, hallucinations, sleep disturbance, suicidal ideation13 |
| Panax (ginseng) | Euphoria, mania14 |
| Amino acid-containing drinks (taurine and inositol) | Euphoria, hypervigilance, insomnia, verbal and physical aggression, impulsive behavior9,15 |
| Hypericum (St. John’s wort) | Mania,16 psychosis17 |
| *FDA removed ephedra from the market in 2003 because of adverse events | |
Related Resources
- National Library of Medicine. Dietary supplements labels database. http://dietarysupplements.nlm.nih.gov/dietary.
- Grossberg G, Fox B. The essential herb-drug-vitamin interaction guide. New York, NY: Broadway Books; 2007.
Drug Brand Names
- Carbamazepine • Tegretol
- Haloperidol • Haldol
- Risperidone • Risperdal
- Valproic acid • Depakene
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Evcimen H, Mania I, Mathews M, et al. Psychosis precipitated by acetyl-L-carnitine in a patient with bipolar disorder. Prim Care Companion J Clin Psychiatry. 2007;9(1):71-72.
2. Office of Dietary Supplements National Institutes of Health. Dietary supplement fact sheet: carnitine. Available at: http://ods.od.nih.gov/factsheets/carnitine.asp. Accessed November 22, 2010.
3. Carnitine: lessons from one hundred years of research Ann NY Acad Sci. 2004;1033:ix-xi.
4. Rebouche CJ, Carnitine. In: Shils ME, Olson JA, Shike M, et al, eds. Modern nutrition in health and disease. 9th ed. Baltimore, MD: Lippincott Williams and Wilkins; 1999: 505-512.
5. Brass EP. Carnitine and sports medicine: use or abuse? Ann NY Acad Sci. 2004;1033:67-78.
6. Scheggi S, Rauggi R, Nanni G, et al. Repeated acetyl-L-carnitine administration increases phosphor-Thr34 DARPP-32 levels and antagonizes cocaine-induced increase in Cdk5 and phosphor-Thr75 DARPP-32 levels in rat striatum. Eur J Neurosci. 2004;19:1609-1620.
7. Howes OD, McDonald C, Cannon M, et al. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7(suppl 1):S7-S13.
8. Hathcock JN, Shao A. Risk assessment for carnitine. Regul Toxicol Pharmacol. 2006;46:23-28.
9. Chelben J, Piccone-Sapir A, Ianco I, et al. Effects of amino acid energy drinks leading to hospitalization in individuals with mental illness. Gen Hosp Psychiatry. 2008;30(2):187-189.
10. Hedges DW, Woon FL, Hoopes SP. Caffeine-induced psychosis. CNS Spectr. 2009;14:127-129.
11. Broderick P, Benjamin AB. Caffeine and psychiatric symptoms: a review. J Okla State Med Assoc. 2004;97(12):538-542.
12. Cerimele JM, Stern AP, Jutras-Aswad D. Psychosis following excessive ingestion of energy drinks in a patient with schizophrenia. Am J Psychiatry. 2010;167(3):353.-
13. Maglione M, Miotto K, Iguchi M, et al. Psychiatric effects of ephedra use: an analysis of Food and Drug Administration reports of adverse events. Am J Psychiatry. 2005;162(1):189-191.
14. Engelberg D, McCutcheon A, Wiseman S. A case of ginseng-induced mania. J Clin Psychopharmacol. 2001;21(5):535-537.
15. Machado-Vieira R, Viale CI, Kapczinski F. Mania associated with an energy drink: the possible role of caffeine, taurine and inositol. Can J Psychiatry. 2001;46:454-455.
16. Fahmi M, Huang C, Schweitzer I. A case of mania induced by hypericum. World J Biol Psychiatry. 2002;3(1):58-59.
17. Stevinson C, Ernst E. Can St. John’s wort trigger psychoses? Int J Clin Pharmacol Ther. 2004;42(9):473-480.
1. Evcimen H, Mania I, Mathews M, et al. Psychosis precipitated by acetyl-L-carnitine in a patient with bipolar disorder. Prim Care Companion J Clin Psychiatry. 2007;9(1):71-72.
2. Office of Dietary Supplements National Institutes of Health. Dietary supplement fact sheet: carnitine. Available at: http://ods.od.nih.gov/factsheets/carnitine.asp. Accessed November 22, 2010.
3. Carnitine: lessons from one hundred years of research Ann NY Acad Sci. 2004;1033:ix-xi.
4. Rebouche CJ, Carnitine. In: Shils ME, Olson JA, Shike M, et al, eds. Modern nutrition in health and disease. 9th ed. Baltimore, MD: Lippincott Williams and Wilkins; 1999: 505-512.
5. Brass EP. Carnitine and sports medicine: use or abuse? Ann NY Acad Sci. 2004;1033:67-78.
6. Scheggi S, Rauggi R, Nanni G, et al. Repeated acetyl-L-carnitine administration increases phosphor-Thr34 DARPP-32 levels and antagonizes cocaine-induced increase in Cdk5 and phosphor-Thr75 DARPP-32 levels in rat striatum. Eur J Neurosci. 2004;19:1609-1620.
7. Howes OD, McDonald C, Cannon M, et al. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7(suppl 1):S7-S13.
8. Hathcock JN, Shao A. Risk assessment for carnitine. Regul Toxicol Pharmacol. 2006;46:23-28.
9. Chelben J, Piccone-Sapir A, Ianco I, et al. Effects of amino acid energy drinks leading to hospitalization in individuals with mental illness. Gen Hosp Psychiatry. 2008;30(2):187-189.
10. Hedges DW, Woon FL, Hoopes SP. Caffeine-induced psychosis. CNS Spectr. 2009;14:127-129.
11. Broderick P, Benjamin AB. Caffeine and psychiatric symptoms: a review. J Okla State Med Assoc. 2004;97(12):538-542.
12. Cerimele JM, Stern AP, Jutras-Aswad D. Psychosis following excessive ingestion of energy drinks in a patient with schizophrenia. Am J Psychiatry. 2010;167(3):353.-
13. Maglione M, Miotto K, Iguchi M, et al. Psychiatric effects of ephedra use: an analysis of Food and Drug Administration reports of adverse events. Am J Psychiatry. 2005;162(1):189-191.
14. Engelberg D, McCutcheon A, Wiseman S. A case of ginseng-induced mania. J Clin Psychopharmacol. 2001;21(5):535-537.
15. Machado-Vieira R, Viale CI, Kapczinski F. Mania associated with an energy drink: the possible role of caffeine, taurine and inositol. Can J Psychiatry. 2001;46:454-455.
16. Fahmi M, Huang C, Schweitzer I. A case of mania induced by hypericum. World J Biol Psychiatry. 2002;3(1):58-59.
17. Stevinson C, Ernst E. Can St. John’s wort trigger psychoses? Int J Clin Pharmacol Ther. 2004;42(9):473-480.
The heart of depression: Treating patients who have cardiovascular disease
Mrs. T, age 59, sustained an ST-elevation myocardial infarction (MI) 6 weeks ago. She has a history of hypertension, hyperlipidemia, and major depressive disorder (MDD). Before her MI, Mrs. T’s MDD was well managed with cognitive-behavioral therapy (CBT). She states that her depressive symptoms have worsened since her MI, and clinicians determine that she is experiencing an acute depressive episode severe enough to require pharmacotherapy. Past medication trials for her depression include sertraline, up to 150 mg/d, and duloxetine, 60 mg/d, but her provider determined they were ineffective after an adequate trial duration. Her hypertension is well controlled on her current regimen, which includes lisinopril, 20 mg/d, metoprolol, 50 mg/d, simvastatin, 40 mg/d, and clopidogrel, 75 mg/d. Her father experienced sudden cardiac death and her mother and younger brother have a history of severe MDD.
- Selective serotonin reuptake inhibitors, particularly citalopram and sertraline, are generally well tolerated, effective, and safe to use in patients with cardiovascular disease (CVD), although clinicians must be aware of the risk of drug-drug interactions with these agents.
- Tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated in patients with CVD.
- The FDA warns against using desipramine in patients with cardiovascular disease; fluoxetine and other CYP2C19 inhibitors may reduce the efficacy of clopidogrel.
- Whether pharmacologic or nonpharmacologic treatment of depression improves long-term cardiac outcomes needs to be clarified with sufficiently powered studies.
Depression is more prevalent in patients with cardiovascular disease (CVD) than in the general population, with estimates as high as 23%.1 Possible mechanisms to help explain the relationship between CVD and depression are summarized in Table 1.2 Appropriate antidepressant selection and depression management strategies in patients with CVD, particularly after MI, may reduce the risk for additional cardiac events and reduce mortality.1,2
Table 1
The link between depression and cardiovascular disease
Depressed patients with CVD often exhibit:
|
Other factors that impact cardiovascular risk in patients with depression include:
|
| CRP: C-reactive protein; CVD: cardiovascular disease; TNF: tumor necrosis factor Source: Reference 2 |
Antidepressant choices by class
Many older antidepressants, including tricyclic antidepressants (TCAs), are:
- contraindicated during acute recovery from MI
- cardiotoxic
- lethal in overdose
- not recommended for patients with CVD.1,3
The FDA recently mandated additional labeling for desipramine to alert health care providers to the risk of using this agent in patients with CVD or a family history of sudden death, arrhythmias, or conduction abnormalities.3 Similar to TCAs, monoamine oxidase inhibitors (MAOIs) generally are not recommended for use in this population because of the risk of hypertensive crisis, orthostatic hypotension, tachycardia, and increased QTc interval.2 Trazodone, which might help relieve insomnia, is associated with orthostasis and tachycardia. These effects may occur more frequently in patients with cardiac disease.4
Selective serotonin reuptake inhibitors (SSRIs) are effective antidepressants post-MI, have antiplatelet activity, and may improve surrogate markers of cardiac risk, although further research is needed.5,6 Individual SSRIs vary in their effects on the cytochrome P450 (CYP450) system, and therefore carry different risks of drug-drug interactions (see Related Resources).
The cardiovascular impact of serotonin-norepinephrine reuptake inhibitors is unknown. These agents may be associated with hypertension and tachycardia.7 Additional research on the use of bupropion and mirtazapine in patients with CVD also is warranted. However, bupropion has been used to help patients with CVD stop smoking and likely is safe, although it may be associated with an increase in blood pressure.2,7 Bupropion and mirtazapine also can affect appetite and weight, which require monitoring in CVD patients. The Myocardial Infarction and Depression-Intervention Trial (MIND-IT) reveals that antidepressant treatment with mirtazapine or citalopram does not increase the incidence of cardiac events and does not improve long-term depression status compared with treatment as usual in depressed post-MI patients.8 Orthostatic hypotension is a possible adverse effect of mirtazapine,7 and this antidepressant may reduce the antihypertensive effect of clonidine.
Monitor for interactions
Drug interaction databases—including Micromedex, Lexi-Comp, or Facts and Comparisons—can differ with regard to identifying and classifying drug interactions. Therefore, individual clinicians often carry the burden of recognizing potential drug-drug interactions. Preskorn and Flockhart9 suggest developing a “personal formulary” of the medications clinicians regularly prescribe to minimize drug-drug interactions. This formulary includes knowledge of a drug’s:
- enzymes responsible for elimination
- half-life
- relevant clinical trials
- receptor affinities
- common adverse effects.
Following these recommendations reveals several considerations when selecting an antidepressant for Mrs. T:
- Studies of SSRIs have shown them to be safe and well tolerated in post-MI patients. Because Mrs. T failed only 1 previous SSRI trial (sertraline), it would be reasonable to select an alternate agent within this class.
- An FDA alert highlights the risk of using clopidogrel in combination with drugs such as omeprazole, ketoconazole, fluoxetine, and fluvoxamine.10 These medications are CYP2C19 inhibitors, which can reduce clopidogrel’s effect by inhibiting conversion of the parent drug to its active metabolite.
- Adding a strong CYP2D6 inhibitor, such as fluoxetine or paroxetine, could increase the effects of metoprolol, which is a CYP2D6 substrate.11
Cardiac outcomes
Evidence is insufficient to ascertain whether pharmacologic management of depression can reduce the risk of future cardiac events. Data evaluating SSRIs’ effects on cardiac outcomes are equivocal5,12,13 and limited by inadequate power.14,15 Preliminary evidence suggests patients who respond to antidepressant treatment may have improved cardiovascular outcomes.16,17 Evidence obtained from the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) trial, and the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial suggest the SSRIs sertraline and citalopram can be used safely, with minimal bleeding risk, to treat depression in CVD patients (Table 2).14,15,18 When treating depressed patients who have CVD, remember to include nonpharmacologic options, such as psychotherapy, in the treatment plan, although studies have not yet shown improved cardiovascular mortality rates in patients receiving CBT.8,17,18
Although other SSRIs may be helpful for Mrs. T, citalopram is one of the best-studied agents post-MI, with the CREATE study supporting its efficacy and tolerability in this population. Citalopram has negligible drug interactions, although it is a weak inhibitor of CYP2D6 and the possibility of increasing metoprolol’s effects should be monitored. All SSRIs are associated with an increased risk of bleeding in patients receiving antiplatelet therapy; however, in Mrs. T’s case the risks are minimal, which makes citalopram a reasonable option. CBT also could be resumed to optimize Mrs. T’s treatment.
Table 2
SSRIs and cardiovascular disease: Results from RCTs
| Study | Design | Results |
|---|---|---|
| SADHART14 | Randomized, double-blind trial of sertraline vs placebo for 24 weeks for depression following MI or unstable angina (N=369) | Sertraline was more effective than placebo as measured by CGI-I, but not HAM-D in the total sample; both measures demonstrated statistical significance in patients with a history of MDD and those with HAM-D score >18 with 2 past episodes of MDD; incidence of severe cardiovascular events was 14.5% with sertraline and 22.4% with placebo (P=NS) |
| ENRICHD18 | Randomized, double-blind, controlled trial of early CBT supplemented with SSRI (usually sertraline) if necessary vs usual care for depression and low perceived social support after MI (N=2,481) | Intervention had a modest effect on depressive symptoms; antidepressant use reduced the risk of death or nonfatal MI |
| CREATE15 | Randomized, controlled, 12-week, parallel-group trial of 284 depressed patients with coronary artery disease first randomized to weekly interpersonal psychotherapy for 12 weeks plus clinical management or clinical management only, then randomized to citalopram or placebo for 12 weeks | Although the effect size was small, citalopram was more effective for depression than placebo and did not differ in effect on cardiac parameters, such as blood pressure, heart rate, or ECG change (P=.005) |
| CBT: cognitive-behavioral therapy; CGI-I: Clinical Global Impressions-Improvement scale; CREATE: Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy; ENRICHD: Enhancing Recovery in Coronary Heart Disease Patients; HAM-D: Hamilton Depression Rating Scale; MDD: major depressive disorder; MI: myocardial infarction; NS: nonsignificant; RCT: randomized controlled trial; SADHART: Sertraline Antidepressant Heart Attack Randomized Trial; SSRI: selective serotonin reuptake inhibitor | ||
- Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
- Indiana University School of Medicine. P450 drug interaction table. Indiana University School of Medicine. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Citalopram • Celexa
- Clopidogrel • Plavix
- Desipramine • Norpramin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketoconazole • Nizoral
- Lisinopril • Prinivil, Zestril
- Metoprolol • Lopressor, Toprol
- Mirtazapine • Remeron
- Omeprazole • Prilosec
- Paroxetine • Paxil
- Sertraline • Zoloft
- Simvastatin • Zocor
- Trazodone • Desyrel
Disclosure
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580-592.
2. Carney RM, Freedland KE. Depression in patients with coronary heart disease. Am J Med. 2008;121(11 suppl 2):S20-27.
3. Norpramin [package insert]. Bridgewater, NJ: sanofi-aventis; 2009.
4. American Psychiatric Association. Treatment of patients with major depressive disorder, 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed December 2, 2010.
5. Bush DE, Ziegelstein RC, Patel UV, et al. Post-myocardial infarction depression. Summary, evidence report/ technology assessment: number 123. Rockville, MD: Agency for Healthcare Research and Quality; May 2005. AHRQ publication 05-E018-1.
6. Roose SP, Miyazaki M. Pharmacologic treatment of depression in patients with heart disease. Psychosom Med. 2005;(67 suppl 1):S54-57.
7. Alvarez W Jr, Pickworth KK. Safety of antidepressant drugs in the patient with cardiac disease: a review of the literature. Pharmacotherapy. 2003;23:754-771.
8. van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry. 2007;190:460-466.
9. Preskorn SH, Flockhart D. 2006 guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
10. U.S. Food and Drug Administration. Information for healthcare professionals: update to the labeling of clopidogrel bisulfate (marketed as Plavix) to alert healthcare professionals about a drug interaction with omeprazole (marketed as Prilosec and Prilosec OTC). Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
DrugSafetyInformationforHeathcareProfessionals/ucm190787.htm. Accessed January 24, 2010.
11. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30:1206-1227.
12. Von Ruden AE, Adson DE, Kotlyar M. Effect of selective serotonin reuptake inhibitors on cardiovascular morbidity and mortality. J Cardiovasc Pharmacol Ther. 2008;13(1):32-40.
13. Glassman A. Depression and cardiovascular disease. Pharmacopsychiatry. 2008;41(6):221-225.
14. Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701-709.
15. Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367-379.
16. de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry. 2007;164:1371-1378.
17. Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
18. Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 2003;289:3106-3116.
Mrs. T, age 59, sustained an ST-elevation myocardial infarction (MI) 6 weeks ago. She has a history of hypertension, hyperlipidemia, and major depressive disorder (MDD). Before her MI, Mrs. T’s MDD was well managed with cognitive-behavioral therapy (CBT). She states that her depressive symptoms have worsened since her MI, and clinicians determine that she is experiencing an acute depressive episode severe enough to require pharmacotherapy. Past medication trials for her depression include sertraline, up to 150 mg/d, and duloxetine, 60 mg/d, but her provider determined they were ineffective after an adequate trial duration. Her hypertension is well controlled on her current regimen, which includes lisinopril, 20 mg/d, metoprolol, 50 mg/d, simvastatin, 40 mg/d, and clopidogrel, 75 mg/d. Her father experienced sudden cardiac death and her mother and younger brother have a history of severe MDD.
- Selective serotonin reuptake inhibitors, particularly citalopram and sertraline, are generally well tolerated, effective, and safe to use in patients with cardiovascular disease (CVD), although clinicians must be aware of the risk of drug-drug interactions with these agents.
- Tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated in patients with CVD.
- The FDA warns against using desipramine in patients with cardiovascular disease; fluoxetine and other CYP2C19 inhibitors may reduce the efficacy of clopidogrel.
- Whether pharmacologic or nonpharmacologic treatment of depression improves long-term cardiac outcomes needs to be clarified with sufficiently powered studies.
Depression is more prevalent in patients with cardiovascular disease (CVD) than in the general population, with estimates as high as 23%.1 Possible mechanisms to help explain the relationship between CVD and depression are summarized in Table 1.2 Appropriate antidepressant selection and depression management strategies in patients with CVD, particularly after MI, may reduce the risk for additional cardiac events and reduce mortality.1,2
Table 1
The link between depression and cardiovascular disease
Depressed patients with CVD often exhibit:
|
Other factors that impact cardiovascular risk in patients with depression include:
|
| CRP: C-reactive protein; CVD: cardiovascular disease; TNF: tumor necrosis factor Source: Reference 2 |
Antidepressant choices by class
Many older antidepressants, including tricyclic antidepressants (TCAs), are:
- contraindicated during acute recovery from MI
- cardiotoxic
- lethal in overdose
- not recommended for patients with CVD.1,3
The FDA recently mandated additional labeling for desipramine to alert health care providers to the risk of using this agent in patients with CVD or a family history of sudden death, arrhythmias, or conduction abnormalities.3 Similar to TCAs, monoamine oxidase inhibitors (MAOIs) generally are not recommended for use in this population because of the risk of hypertensive crisis, orthostatic hypotension, tachycardia, and increased QTc interval.2 Trazodone, which might help relieve insomnia, is associated with orthostasis and tachycardia. These effects may occur more frequently in patients with cardiac disease.4
Selective serotonin reuptake inhibitors (SSRIs) are effective antidepressants post-MI, have antiplatelet activity, and may improve surrogate markers of cardiac risk, although further research is needed.5,6 Individual SSRIs vary in their effects on the cytochrome P450 (CYP450) system, and therefore carry different risks of drug-drug interactions (see Related Resources).
The cardiovascular impact of serotonin-norepinephrine reuptake inhibitors is unknown. These agents may be associated with hypertension and tachycardia.7 Additional research on the use of bupropion and mirtazapine in patients with CVD also is warranted. However, bupropion has been used to help patients with CVD stop smoking and likely is safe, although it may be associated with an increase in blood pressure.2,7 Bupropion and mirtazapine also can affect appetite and weight, which require monitoring in CVD patients. The Myocardial Infarction and Depression-Intervention Trial (MIND-IT) reveals that antidepressant treatment with mirtazapine or citalopram does not increase the incidence of cardiac events and does not improve long-term depression status compared with treatment as usual in depressed post-MI patients.8 Orthostatic hypotension is a possible adverse effect of mirtazapine,7 and this antidepressant may reduce the antihypertensive effect of clonidine.
Monitor for interactions
Drug interaction databases—including Micromedex, Lexi-Comp, or Facts and Comparisons—can differ with regard to identifying and classifying drug interactions. Therefore, individual clinicians often carry the burden of recognizing potential drug-drug interactions. Preskorn and Flockhart9 suggest developing a “personal formulary” of the medications clinicians regularly prescribe to minimize drug-drug interactions. This formulary includes knowledge of a drug’s:
- enzymes responsible for elimination
- half-life
- relevant clinical trials
- receptor affinities
- common adverse effects.
Following these recommendations reveals several considerations when selecting an antidepressant for Mrs. T:
- Studies of SSRIs have shown them to be safe and well tolerated in post-MI patients. Because Mrs. T failed only 1 previous SSRI trial (sertraline), it would be reasonable to select an alternate agent within this class.
- An FDA alert highlights the risk of using clopidogrel in combination with drugs such as omeprazole, ketoconazole, fluoxetine, and fluvoxamine.10 These medications are CYP2C19 inhibitors, which can reduce clopidogrel’s effect by inhibiting conversion of the parent drug to its active metabolite.
- Adding a strong CYP2D6 inhibitor, such as fluoxetine or paroxetine, could increase the effects of metoprolol, which is a CYP2D6 substrate.11
Cardiac outcomes
Evidence is insufficient to ascertain whether pharmacologic management of depression can reduce the risk of future cardiac events. Data evaluating SSRIs’ effects on cardiac outcomes are equivocal5,12,13 and limited by inadequate power.14,15 Preliminary evidence suggests patients who respond to antidepressant treatment may have improved cardiovascular outcomes.16,17 Evidence obtained from the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) trial, and the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial suggest the SSRIs sertraline and citalopram can be used safely, with minimal bleeding risk, to treat depression in CVD patients (Table 2).14,15,18 When treating depressed patients who have CVD, remember to include nonpharmacologic options, such as psychotherapy, in the treatment plan, although studies have not yet shown improved cardiovascular mortality rates in patients receiving CBT.8,17,18
Although other SSRIs may be helpful for Mrs. T, citalopram is one of the best-studied agents post-MI, with the CREATE study supporting its efficacy and tolerability in this population. Citalopram has negligible drug interactions, although it is a weak inhibitor of CYP2D6 and the possibility of increasing metoprolol’s effects should be monitored. All SSRIs are associated with an increased risk of bleeding in patients receiving antiplatelet therapy; however, in Mrs. T’s case the risks are minimal, which makes citalopram a reasonable option. CBT also could be resumed to optimize Mrs. T’s treatment.
Table 2
SSRIs and cardiovascular disease: Results from RCTs
| Study | Design | Results |
|---|---|---|
| SADHART14 | Randomized, double-blind trial of sertraline vs placebo for 24 weeks for depression following MI or unstable angina (N=369) | Sertraline was more effective than placebo as measured by CGI-I, but not HAM-D in the total sample; both measures demonstrated statistical significance in patients with a history of MDD and those with HAM-D score >18 with 2 past episodes of MDD; incidence of severe cardiovascular events was 14.5% with sertraline and 22.4% with placebo (P=NS) |
| ENRICHD18 | Randomized, double-blind, controlled trial of early CBT supplemented with SSRI (usually sertraline) if necessary vs usual care for depression and low perceived social support after MI (N=2,481) | Intervention had a modest effect on depressive symptoms; antidepressant use reduced the risk of death or nonfatal MI |
| CREATE15 | Randomized, controlled, 12-week, parallel-group trial of 284 depressed patients with coronary artery disease first randomized to weekly interpersonal psychotherapy for 12 weeks plus clinical management or clinical management only, then randomized to citalopram or placebo for 12 weeks | Although the effect size was small, citalopram was more effective for depression than placebo and did not differ in effect on cardiac parameters, such as blood pressure, heart rate, or ECG change (P=.005) |
| CBT: cognitive-behavioral therapy; CGI-I: Clinical Global Impressions-Improvement scale; CREATE: Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy; ENRICHD: Enhancing Recovery in Coronary Heart Disease Patients; HAM-D: Hamilton Depression Rating Scale; MDD: major depressive disorder; MI: myocardial infarction; NS: nonsignificant; RCT: randomized controlled trial; SADHART: Sertraline Antidepressant Heart Attack Randomized Trial; SSRI: selective serotonin reuptake inhibitor | ||
- Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
- Indiana University School of Medicine. P450 drug interaction table. Indiana University School of Medicine. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Citalopram • Celexa
- Clopidogrel • Plavix
- Desipramine • Norpramin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketoconazole • Nizoral
- Lisinopril • Prinivil, Zestril
- Metoprolol • Lopressor, Toprol
- Mirtazapine • Remeron
- Omeprazole • Prilosec
- Paroxetine • Paxil
- Sertraline • Zoloft
- Simvastatin • Zocor
- Trazodone • Desyrel
Disclosure
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Mrs. T, age 59, sustained an ST-elevation myocardial infarction (MI) 6 weeks ago. She has a history of hypertension, hyperlipidemia, and major depressive disorder (MDD). Before her MI, Mrs. T’s MDD was well managed with cognitive-behavioral therapy (CBT). She states that her depressive symptoms have worsened since her MI, and clinicians determine that she is experiencing an acute depressive episode severe enough to require pharmacotherapy. Past medication trials for her depression include sertraline, up to 150 mg/d, and duloxetine, 60 mg/d, but her provider determined they were ineffective after an adequate trial duration. Her hypertension is well controlled on her current regimen, which includes lisinopril, 20 mg/d, metoprolol, 50 mg/d, simvastatin, 40 mg/d, and clopidogrel, 75 mg/d. Her father experienced sudden cardiac death and her mother and younger brother have a history of severe MDD.
- Selective serotonin reuptake inhibitors, particularly citalopram and sertraline, are generally well tolerated, effective, and safe to use in patients with cardiovascular disease (CVD), although clinicians must be aware of the risk of drug-drug interactions with these agents.
- Tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated in patients with CVD.
- The FDA warns against using desipramine in patients with cardiovascular disease; fluoxetine and other CYP2C19 inhibitors may reduce the efficacy of clopidogrel.
- Whether pharmacologic or nonpharmacologic treatment of depression improves long-term cardiac outcomes needs to be clarified with sufficiently powered studies.
Depression is more prevalent in patients with cardiovascular disease (CVD) than in the general population, with estimates as high as 23%.1 Possible mechanisms to help explain the relationship between CVD and depression are summarized in Table 1.2 Appropriate antidepressant selection and depression management strategies in patients with CVD, particularly after MI, may reduce the risk for additional cardiac events and reduce mortality.1,2
Table 1
The link between depression and cardiovascular disease
Depressed patients with CVD often exhibit:
|
Other factors that impact cardiovascular risk in patients with depression include:
|
| CRP: C-reactive protein; CVD: cardiovascular disease; TNF: tumor necrosis factor Source: Reference 2 |
Antidepressant choices by class
Many older antidepressants, including tricyclic antidepressants (TCAs), are:
- contraindicated during acute recovery from MI
- cardiotoxic
- lethal in overdose
- not recommended for patients with CVD.1,3
The FDA recently mandated additional labeling for desipramine to alert health care providers to the risk of using this agent in patients with CVD or a family history of sudden death, arrhythmias, or conduction abnormalities.3 Similar to TCAs, monoamine oxidase inhibitors (MAOIs) generally are not recommended for use in this population because of the risk of hypertensive crisis, orthostatic hypotension, tachycardia, and increased QTc interval.2 Trazodone, which might help relieve insomnia, is associated with orthostasis and tachycardia. These effects may occur more frequently in patients with cardiac disease.4
Selective serotonin reuptake inhibitors (SSRIs) are effective antidepressants post-MI, have antiplatelet activity, and may improve surrogate markers of cardiac risk, although further research is needed.5,6 Individual SSRIs vary in their effects on the cytochrome P450 (CYP450) system, and therefore carry different risks of drug-drug interactions (see Related Resources).
The cardiovascular impact of serotonin-norepinephrine reuptake inhibitors is unknown. These agents may be associated with hypertension and tachycardia.7 Additional research on the use of bupropion and mirtazapine in patients with CVD also is warranted. However, bupropion has been used to help patients with CVD stop smoking and likely is safe, although it may be associated with an increase in blood pressure.2,7 Bupropion and mirtazapine also can affect appetite and weight, which require monitoring in CVD patients. The Myocardial Infarction and Depression-Intervention Trial (MIND-IT) reveals that antidepressant treatment with mirtazapine or citalopram does not increase the incidence of cardiac events and does not improve long-term depression status compared with treatment as usual in depressed post-MI patients.8 Orthostatic hypotension is a possible adverse effect of mirtazapine,7 and this antidepressant may reduce the antihypertensive effect of clonidine.
Monitor for interactions
Drug interaction databases—including Micromedex, Lexi-Comp, or Facts and Comparisons—can differ with regard to identifying and classifying drug interactions. Therefore, individual clinicians often carry the burden of recognizing potential drug-drug interactions. Preskorn and Flockhart9 suggest developing a “personal formulary” of the medications clinicians regularly prescribe to minimize drug-drug interactions. This formulary includes knowledge of a drug’s:
- enzymes responsible for elimination
- half-life
- relevant clinical trials
- receptor affinities
- common adverse effects.
Following these recommendations reveals several considerations when selecting an antidepressant for Mrs. T:
- Studies of SSRIs have shown them to be safe and well tolerated in post-MI patients. Because Mrs. T failed only 1 previous SSRI trial (sertraline), it would be reasonable to select an alternate agent within this class.
- An FDA alert highlights the risk of using clopidogrel in combination with drugs such as omeprazole, ketoconazole, fluoxetine, and fluvoxamine.10 These medications are CYP2C19 inhibitors, which can reduce clopidogrel’s effect by inhibiting conversion of the parent drug to its active metabolite.
- Adding a strong CYP2D6 inhibitor, such as fluoxetine or paroxetine, could increase the effects of metoprolol, which is a CYP2D6 substrate.11
Cardiac outcomes
Evidence is insufficient to ascertain whether pharmacologic management of depression can reduce the risk of future cardiac events. Data evaluating SSRIs’ effects on cardiac outcomes are equivocal5,12,13 and limited by inadequate power.14,15 Preliminary evidence suggests patients who respond to antidepressant treatment may have improved cardiovascular outcomes.16,17 Evidence obtained from the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) trial, and the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial suggest the SSRIs sertraline and citalopram can be used safely, with minimal bleeding risk, to treat depression in CVD patients (Table 2).14,15,18 When treating depressed patients who have CVD, remember to include nonpharmacologic options, such as psychotherapy, in the treatment plan, although studies have not yet shown improved cardiovascular mortality rates in patients receiving CBT.8,17,18
Although other SSRIs may be helpful for Mrs. T, citalopram is one of the best-studied agents post-MI, with the CREATE study supporting its efficacy and tolerability in this population. Citalopram has negligible drug interactions, although it is a weak inhibitor of CYP2D6 and the possibility of increasing metoprolol’s effects should be monitored. All SSRIs are associated with an increased risk of bleeding in patients receiving antiplatelet therapy; however, in Mrs. T’s case the risks are minimal, which makes citalopram a reasonable option. CBT also could be resumed to optimize Mrs. T’s treatment.
Table 2
SSRIs and cardiovascular disease: Results from RCTs
| Study | Design | Results |
|---|---|---|
| SADHART14 | Randomized, double-blind trial of sertraline vs placebo for 24 weeks for depression following MI or unstable angina (N=369) | Sertraline was more effective than placebo as measured by CGI-I, but not HAM-D in the total sample; both measures demonstrated statistical significance in patients with a history of MDD and those with HAM-D score >18 with 2 past episodes of MDD; incidence of severe cardiovascular events was 14.5% with sertraline and 22.4% with placebo (P=NS) |
| ENRICHD18 | Randomized, double-blind, controlled trial of early CBT supplemented with SSRI (usually sertraline) if necessary vs usual care for depression and low perceived social support after MI (N=2,481) | Intervention had a modest effect on depressive symptoms; antidepressant use reduced the risk of death or nonfatal MI |
| CREATE15 | Randomized, controlled, 12-week, parallel-group trial of 284 depressed patients with coronary artery disease first randomized to weekly interpersonal psychotherapy for 12 weeks plus clinical management or clinical management only, then randomized to citalopram or placebo for 12 weeks | Although the effect size was small, citalopram was more effective for depression than placebo and did not differ in effect on cardiac parameters, such as blood pressure, heart rate, or ECG change (P=.005) |
| CBT: cognitive-behavioral therapy; CGI-I: Clinical Global Impressions-Improvement scale; CREATE: Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy; ENRICHD: Enhancing Recovery in Coronary Heart Disease Patients; HAM-D: Hamilton Depression Rating Scale; MDD: major depressive disorder; MI: myocardial infarction; NS: nonsignificant; RCT: randomized controlled trial; SADHART: Sertraline Antidepressant Heart Attack Randomized Trial; SSRI: selective serotonin reuptake inhibitor | ||
- Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
- Indiana University School of Medicine. P450 drug interaction table. Indiana University School of Medicine. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Citalopram • Celexa
- Clopidogrel • Plavix
- Desipramine • Norpramin
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Ketoconazole • Nizoral
- Lisinopril • Prinivil, Zestril
- Metoprolol • Lopressor, Toprol
- Mirtazapine • Remeron
- Omeprazole • Prilosec
- Paroxetine • Paxil
- Sertraline • Zoloft
- Simvastatin • Zocor
- Trazodone • Desyrel
Disclosure
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580-592.
2. Carney RM, Freedland KE. Depression in patients with coronary heart disease. Am J Med. 2008;121(11 suppl 2):S20-27.
3. Norpramin [package insert]. Bridgewater, NJ: sanofi-aventis; 2009.
4. American Psychiatric Association. Treatment of patients with major depressive disorder, 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed December 2, 2010.
5. Bush DE, Ziegelstein RC, Patel UV, et al. Post-myocardial infarction depression. Summary, evidence report/ technology assessment: number 123. Rockville, MD: Agency for Healthcare Research and Quality; May 2005. AHRQ publication 05-E018-1.
6. Roose SP, Miyazaki M. Pharmacologic treatment of depression in patients with heart disease. Psychosom Med. 2005;(67 suppl 1):S54-57.
7. Alvarez W Jr, Pickworth KK. Safety of antidepressant drugs in the patient with cardiac disease: a review of the literature. Pharmacotherapy. 2003;23:754-771.
8. van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry. 2007;190:460-466.
9. Preskorn SH, Flockhart D. 2006 guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
10. U.S. Food and Drug Administration. Information for healthcare professionals: update to the labeling of clopidogrel bisulfate (marketed as Plavix) to alert healthcare professionals about a drug interaction with omeprazole (marketed as Prilosec and Prilosec OTC). Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
DrugSafetyInformationforHeathcareProfessionals/ucm190787.htm. Accessed January 24, 2010.
11. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30:1206-1227.
12. Von Ruden AE, Adson DE, Kotlyar M. Effect of selective serotonin reuptake inhibitors on cardiovascular morbidity and mortality. J Cardiovasc Pharmacol Ther. 2008;13(1):32-40.
13. Glassman A. Depression and cardiovascular disease. Pharmacopsychiatry. 2008;41(6):221-225.
14. Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701-709.
15. Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367-379.
16. de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry. 2007;164:1371-1378.
17. Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
18. Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 2003;289:3106-3116.
1. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580-592.
2. Carney RM, Freedland KE. Depression in patients with coronary heart disease. Am J Med. 2008;121(11 suppl 2):S20-27.
3. Norpramin [package insert]. Bridgewater, NJ: sanofi-aventis; 2009.
4. American Psychiatric Association. Treatment of patients with major depressive disorder, 3rd ed. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideChapToc_7.aspx. Accessed December 2, 2010.
5. Bush DE, Ziegelstein RC, Patel UV, et al. Post-myocardial infarction depression. Summary, evidence report/ technology assessment: number 123. Rockville, MD: Agency for Healthcare Research and Quality; May 2005. AHRQ publication 05-E018-1.
6. Roose SP, Miyazaki M. Pharmacologic treatment of depression in patients with heart disease. Psychosom Med. 2005;(67 suppl 1):S54-57.
7. Alvarez W Jr, Pickworth KK. Safety of antidepressant drugs in the patient with cardiac disease: a review of the literature. Pharmacotherapy. 2003;23:754-771.
8. van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry. 2007;190:460-466.
9. Preskorn SH, Flockhart D. 2006 guide to psychiatric drug interactions. Primary Psychiatry. 2006;13(4):35-64.
10. U.S. Food and Drug Administration. Information for healthcare professionals: update to the labeling of clopidogrel bisulfate (marketed as Plavix) to alert healthcare professionals about a drug interaction with omeprazole (marketed as Prilosec and Prilosec OTC). Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
DrugSafetyInformationforHeathcareProfessionals/ucm190787.htm. Accessed January 24, 2010.
11. Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30:1206-1227.
12. Von Ruden AE, Adson DE, Kotlyar M. Effect of selective serotonin reuptake inhibitors on cardiovascular morbidity and mortality. J Cardiovasc Pharmacol Ther. 2008;13(1):32-40.
13. Glassman A. Depression and cardiovascular disease. Pharmacopsychiatry. 2008;41(6):221-225.
14. Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701-709.
15. Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367-379.
16. de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry. 2007;164:1371-1378.
17. Summers KM, Martin KE, Watson K. Impact and clinical management of depression in patients with coronary artery disease. Pharmacotherapy. 2010;30:304-322.
18. Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 2003;289:3106-3116.
Immobile, mute, and at risk
CASE: Nude and mute
Mr. M, age 45, is found naked outside his apartment. He has a history of schizophrenia, paranoid type, hypertension, and diet-controlled type 2 diabetes mellitus. His schizophrenia has been treated with ziprasidone, 160 mg/d, but 2 months ago he stopped taking his medication and seeing his psychiatrist. He does not respond to questions from police and is taken to a local emergency department for medical workup of altered mental status.
Mr. M is noted to have bilateral conjunctival discharge and a white blood cell (WBC) count of 15,000/mm3. Vital signs, physical examination, laboratory studies, and head CT are otherwise within normal limits. Mr. M is medically cleared for his 15th admission to our inpatient psychiatric facility in the last 7 years. He is divorced, has 2 adult sons, and receives Social Security disability benefits.
Mr. M is alert but guarded and mute and appears to be internally preoccupied. His mood is euthymic and his facial expressions do not vary much and are similar to a blank stare. His grooming and hygiene are poor, but there is no evidence of delusions or suicidal or homicidal ideation. He paces around the unit or sits in his bed staring straight ahead, occasionally mouthing inaudible words but remaining nonverbal.
Mr. M is restarted on his previous dose of ziprasidone and referred to the primary care physician in our inpatient psychiatric facility for further evaluation. His admission vitals and laboratory values show a platelet count of 124,000/mm3, glucose of 113 mg/dL, triglycerides of 160 mg/dL, high-density lipoprotein of 37 mg/dL, and hemoglobin A1c of 6%. Mr. M needs help drinking fluids but resists solid foods as well as medications, including lorazepam, 3 mg/d, and most scheduled doses of ziprasidone. On day 3, Mr. M’s extremities are rigid and he has poor oral intake. We diagnose Mr. M with catatonia based on his immobility, negativity, and mutism.
The authors’ observations
The literature describes >40 signs of catatonia.1-11 According to DSM-IV-TR, catatonia may occur in the context of schizophrenia, a mood disorder, or a general medical condition. DSM-IV-TR criteria for catatonia include:
- motor immobility as evidenced by catalepsy or stupor
- excessive motor activity
- extreme negativism or mutism
- peculiarities of voluntary movements as evidenced by posturing, stereotypic movements, or grimacing
- echolalia or echopraxia.12
Only 2 signs are necessary to meet the diagnostic criteria for catatonia.11,12 Several catatonia rating scales—including the Bush-Francis Catatonia Rating Scale (BFCRS)—have been found to be highly reliable for screening for and rating the severity of catatonia. Such tools also can be used serially to monitor treatment efficacy. The BFCRS takes 5 minutes to administer; the screen is considered positive if ≥2 of the first 14 items on the scale are present.13 Mr. M exhibits immobility and mutism, which are the most common signs of catatonia.
In patients with catatonia, poor oral intake may result in malnutrition that often requires parenteral nutrition or intravenous fluids1,10 and dehydration that may lead to dental caries, gum disease, constipation, and ileus.1 Pneumonia may occur secondary to atelectasis or buildup of respiratory secretions and possibly aspiration.7 Vaginal infections may develop secondary to poor hygiene.1 Immobility and malnutrition may lead to infection and decubitus ulcers.1 Finally, immobility also may cause urinary incontinence,2,10 nerve palsies, flexion contractions, and rhabdomyolysis.1
EVALUATION: Venous complications
On day 3, Mr. M is referred to a local emergency department, where he is assessed for delirium and dehydration because of increased WBC count and diaphoresis. The medical staff finds bilateral pulmonary embolisms and a deep vein thrombosis (DVT) of his left lower leg.
The authors’ observations
Catatonia is associated with an increased risk of venous thromboembolism because of the increased risk of venous stasis and hypercoagulability, both elements of Virchow’s triad for thrombogenesis.1-10,14,15 The third element of Virchow’s triad, vascular injury, does not appear to directly increase the risk for thromboembolic events in catatonic states.
Catatonia-specific causes for venous stasis include immobility, prolonged use of physical restraints, and sedation as a side effect of antipsychotic use.16
Causes for hypercoagulability during catatonic states include:
- increased catecholamine levels during excited states3
- hyperhomocysteinemia secondary to poor diet, smoking, and/or high caffeine consumption16
- increased anticardiolipin and/or anti-phospholipid antibody levels secondary to use of specific antipsychotics, such as chlorpromazine and clozapine16
- increased platelet aggregation secondary to hyperprolactinemia caused by low-potency conventional antipsychotics, such as chlorpromazine16,17
- increased platelet activation caused by altered levels of platelet serotonin in depressed patients.18
Patients taking low-potency conventional antipsychotics may have a 7-fold greater risk for thromboembolic events compared with those who do not use these medications.16
Reducing thromboembolic risk
Diagnose catatonia early. Treating symptoms of catatonia early with benzodiazepines (and, in refractory cases, with electroconvulsive therapy) prevents immobility, thereby decreasing the risk of thromboembolic events.3,11 It may be useful to minimize antipsychotic use.
Monitor activity levels. Fatal thromboembolic events may appear early in the course of catatonia before risk factors associated with thromboembolic events are evident.4 However, these events may be more common when the patient resumes movement.3 Monitor patients’ activity status and encourage ambulation throughout treatment.
Monitor vital signs for signs of pulmonary embolism, including hypoxia, tachycardia, tachypnea, and fever. Take serial pulse oximetry and, if indicated, arterial blood gas measurements to monitor hemoglobin oxygen saturation. Be vigilant for other signs and symptoms of pulmonary embolism and DVT (Table).
Consider prophylactic treatment. Some studies recommend prophylaxis against thromboembolic events in catatonic patients.3-6,10,15 These measures include:
- intravenous fluids
- nasogastric tube feeding
- physical examinations to assess for signs of DVT
- support stockings
- sequential/pneumatic compression devices
- physical therapy or range-of-motion exercises
- complete anticoagulation during immobility, although there are no data that support using anticoagulation medications in catatonic patients who have not yet experienced a thromboembolic event.
Consider prophylactic antithrombotic treatment in catatonic patients and other immobile inpatients who have risk factors for thromboembolic events.9,16 Although it has not been rigorously tested, the Algorithm suggested by Malý et al15 can serve as a guideline for determining the need for prophylaxis against venous thromboembolism in psychiatric inpatient settings.
Table
Signs and symptoms of deep vein thrombosis and pulmonary embolism
| Deep vein thrombosis |
| Swelling of the leg or along a vein in the leg |
| Pain or tenderness in the leg, which may be felt only when standing or walking |
| Increased warmth in the area of the leg that is swollen or in pain |
| Red or discolored skin on the leg |
| Pulmonary embolism |
| Unexplained shortness of breath or pain with deep breathing |
| Chest pain |
| Coughing or coughing up blood |
| Arrhythmia |
| Source: National Heart, Lung, and Blood Institute. What are the signs and symptoms of deep vein thrombosis? Available at: www.nhlbi.nih.gov/health/dci/Diseases/Dvt/DVT_ SignsAndSymptoms.html. Accessed November 8, 2010 |
Algorithm
Does my patient need venous thromboembolism prophylaxis?
| Step 1. Assess risk factors for venous thromboembolism and determine risk level score | |
|---|---|
| Risk factor | Score |
| Consensus-based | |
| Immobilization | 1 |
| Hormone therapy | 1 |
| Obesity (BMI ≥30 kg/m2) | 1 |
| Age 60 to 74 | 1 |
| Varicose veins/venous insufficiency | 1 |
| Dehydration | 1 |
| Thrombophilia | 1 |
| Expert opinion | |
| Treatment with antipsychotics | 1 |
| Evidence-based | |
| History of deep vein thrombosis or pulmonary embolism | 2 |
| Cancer (active/treated) | 2 |
| Age ≥75 | 2 |
| Acute infection/respiratory disease | 2 |
| TOTAL | |
| BMI: body mass index | |
| Step 2. Determine recommended prophylaxis based on risk level score | |
| Risk level score | Recommended prophylaxis |
| All risk levels | Regular physical exercise of lower extremities, sufficient hydration, graduated compression stockings |
| Medium risk (4 to 7 points) and/or physical restraint ≥8 hours | Heparin, 5,000 units every 12 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| High risk (≥8 points) | Heparin, 5,000 units every 8 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| Source: Adapted from reference 15 | |
OUTCOME: Stable and speaking
In the hospital, Mr. M remains immobile and mute for several days. The hospital’s psychiatric consult team recommends lorazepam, 3 mg/d, to address his catatonia. Mr. M improves and begins speaking and eating after starting lorazepam, but becomes agitated, banging his head against walls and threatening to jump out the window. Because this puts him at risk for trauma, Mr. M is not a good candidate for warfarin therapy, and an inferior vena cava filter is placed on an emergency basis. Later, a Dobhoff tube is placed for feeding and administering oral medications.
Mr. M’s catatonic state gradually improves and he begins to respond to the staff with short phrases, eats all of his food, and accepts oral medications. He is transferred back to our inpatient psychiatric facility with haloperidol, 10 mg/d, lorazepam, 3 mg/d, and benztro-pine, 2 mg/d, in addition to sulfacetamide eye drops for bilateral conjunctivitis. At our facility, we start him on warfarin, 5 mg/d, and closely monitor his international normalized ratio levels, with a plan to remove the inferior vena cava filter after 6 months of anticoagulation therapy. Mr. M remains at our facility for 3 weeks to stabilize his medications and is discharged to his apartment.
Six months after being discharged from our facility, Mr. M is stable at an intensive outpatient mental health program.
Related Resources
- Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge, United Kingdom: Cambridge University Press; 2003.
- Snow V, Qaseem A, Barry P, et al, and American College of Physicians; American Academy of Family Physicians Panel on Deep Venous Thrombosis/Pulmonary Embolism. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146(3):204-210.
Drug Brand Names
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Sulfacetamide • Sulamyd
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Caroff SN, Mann SC, Francis A, et al. eds. Catatonia: from psychopathology to neurobiology. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
2. Gangadhar BN, Keshavan MS, Goswami U, et al. Cortical venous thrombosis presenting as catatonia: a clinicopathologic report. J Clin Psychiatry. 1983;44:109-110.
3. McCall WV, Mann SC, Shelp FE, et al. Fatal pulmonary embolism in the catatonic syndrome: two case reports and a literature review. J Clin Psychiatry. 1995;51:21-25.
4. Morioka H, Nagatomo I, Yamada K, et al. Deep venous thrombosis of the leg due to psychiatric stupor. Psychiatry Clin Neurosci. 1997;51:323-326.
5. Lachner C, Sandson NB. Medical complications of catatonia: a case of catatonia-induced deep venous thrombosis. Psychosomatics. 2003;44:512-514.
6. Woo BK. Basal ganglia calcification and pulmonary embolism in catatonia. J Neuropsychiatry Clin Neurosci. 2007;19:472-473.
7. Regestein QR, Alpert JS, Reich P. Sudden catatonic stupor with disastrous outcome. JAMA. 1977;238:618-620.
8. Suzuki K, Takamatsu K, Takano T, et al. Safety of electroconvulsive therapy in psychiatric patients shortly after the occurrence of pulmonary embolism. J ECT. 2008;24:286-288.
9. Tsao C, Nusbaum A. Successful ECT course for catatonia after large pulmonary embolism and placement of inferior vena cava filter. Gen Hosp Psychiatry. 2007;29:374.-
10. Barbuto J. Preventing sudden death during a catatonic episode. Hosp Community Psychiatry. 1983;34:72-73.
11. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160:1233-1241.
12. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
13. Bush G, Fink M, Petrides G, et al. Catatonia I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
14. Lal S, Bleiman M, Brown GN. Pulmonary embolism in psychiatric patients. J Am Geriatr Soc. 1966;14:1138-1143.
15. Malý R, Masopust J, Hosák L, et al. Assessment of risk of venous thromboembolism and its possible prevention in psychiatric patients. Psychiatry Clin Neurosci. 2008;62:3-8.
16. Higg S, Jönsson AK, Spigset O. Risk of venous thromboembolism due to antipsychotic drug therapy. Expert Opin Drug Saf. 2009;8:537-547.
17. Wallaschofski H, Eigenthaler M, Kiefer M, et al. Hyperprolactinemia in patients on antipsychotic drugs causes ADP-stimulated platelet activation that might explain the increased risk for venous thromboembolism: pilot study. J Clin Psychopharmacol. 2003;23(5):479-483.
18. Arnone D, Hansen L, Davies G. Pulmonary embolism and severe depression. Am J Psychiatry. 2009;159:873-874.
CASE: Nude and mute
Mr. M, age 45, is found naked outside his apartment. He has a history of schizophrenia, paranoid type, hypertension, and diet-controlled type 2 diabetes mellitus. His schizophrenia has been treated with ziprasidone, 160 mg/d, but 2 months ago he stopped taking his medication and seeing his psychiatrist. He does not respond to questions from police and is taken to a local emergency department for medical workup of altered mental status.
Mr. M is noted to have bilateral conjunctival discharge and a white blood cell (WBC) count of 15,000/mm3. Vital signs, physical examination, laboratory studies, and head CT are otherwise within normal limits. Mr. M is medically cleared for his 15th admission to our inpatient psychiatric facility in the last 7 years. He is divorced, has 2 adult sons, and receives Social Security disability benefits.
Mr. M is alert but guarded and mute and appears to be internally preoccupied. His mood is euthymic and his facial expressions do not vary much and are similar to a blank stare. His grooming and hygiene are poor, but there is no evidence of delusions or suicidal or homicidal ideation. He paces around the unit or sits in his bed staring straight ahead, occasionally mouthing inaudible words but remaining nonverbal.
Mr. M is restarted on his previous dose of ziprasidone and referred to the primary care physician in our inpatient psychiatric facility for further evaluation. His admission vitals and laboratory values show a platelet count of 124,000/mm3, glucose of 113 mg/dL, triglycerides of 160 mg/dL, high-density lipoprotein of 37 mg/dL, and hemoglobin A1c of 6%. Mr. M needs help drinking fluids but resists solid foods as well as medications, including lorazepam, 3 mg/d, and most scheduled doses of ziprasidone. On day 3, Mr. M’s extremities are rigid and he has poor oral intake. We diagnose Mr. M with catatonia based on his immobility, negativity, and mutism.
The authors’ observations
The literature describes >40 signs of catatonia.1-11 According to DSM-IV-TR, catatonia may occur in the context of schizophrenia, a mood disorder, or a general medical condition. DSM-IV-TR criteria for catatonia include:
- motor immobility as evidenced by catalepsy or stupor
- excessive motor activity
- extreme negativism or mutism
- peculiarities of voluntary movements as evidenced by posturing, stereotypic movements, or grimacing
- echolalia or echopraxia.12
Only 2 signs are necessary to meet the diagnostic criteria for catatonia.11,12 Several catatonia rating scales—including the Bush-Francis Catatonia Rating Scale (BFCRS)—have been found to be highly reliable for screening for and rating the severity of catatonia. Such tools also can be used serially to monitor treatment efficacy. The BFCRS takes 5 minutes to administer; the screen is considered positive if ≥2 of the first 14 items on the scale are present.13 Mr. M exhibits immobility and mutism, which are the most common signs of catatonia.
In patients with catatonia, poor oral intake may result in malnutrition that often requires parenteral nutrition or intravenous fluids1,10 and dehydration that may lead to dental caries, gum disease, constipation, and ileus.1 Pneumonia may occur secondary to atelectasis or buildup of respiratory secretions and possibly aspiration.7 Vaginal infections may develop secondary to poor hygiene.1 Immobility and malnutrition may lead to infection and decubitus ulcers.1 Finally, immobility also may cause urinary incontinence,2,10 nerve palsies, flexion contractions, and rhabdomyolysis.1
EVALUATION: Venous complications
On day 3, Mr. M is referred to a local emergency department, where he is assessed for delirium and dehydration because of increased WBC count and diaphoresis. The medical staff finds bilateral pulmonary embolisms and a deep vein thrombosis (DVT) of his left lower leg.
The authors’ observations
Catatonia is associated with an increased risk of venous thromboembolism because of the increased risk of venous stasis and hypercoagulability, both elements of Virchow’s triad for thrombogenesis.1-10,14,15 The third element of Virchow’s triad, vascular injury, does not appear to directly increase the risk for thromboembolic events in catatonic states.
Catatonia-specific causes for venous stasis include immobility, prolonged use of physical restraints, and sedation as a side effect of antipsychotic use.16
Causes for hypercoagulability during catatonic states include:
- increased catecholamine levels during excited states3
- hyperhomocysteinemia secondary to poor diet, smoking, and/or high caffeine consumption16
- increased anticardiolipin and/or anti-phospholipid antibody levels secondary to use of specific antipsychotics, such as chlorpromazine and clozapine16
- increased platelet aggregation secondary to hyperprolactinemia caused by low-potency conventional antipsychotics, such as chlorpromazine16,17
- increased platelet activation caused by altered levels of platelet serotonin in depressed patients.18
Patients taking low-potency conventional antipsychotics may have a 7-fold greater risk for thromboembolic events compared with those who do not use these medications.16
Reducing thromboembolic risk
Diagnose catatonia early. Treating symptoms of catatonia early with benzodiazepines (and, in refractory cases, with electroconvulsive therapy) prevents immobility, thereby decreasing the risk of thromboembolic events.3,11 It may be useful to minimize antipsychotic use.
Monitor activity levels. Fatal thromboembolic events may appear early in the course of catatonia before risk factors associated with thromboembolic events are evident.4 However, these events may be more common when the patient resumes movement.3 Monitor patients’ activity status and encourage ambulation throughout treatment.
Monitor vital signs for signs of pulmonary embolism, including hypoxia, tachycardia, tachypnea, and fever. Take serial pulse oximetry and, if indicated, arterial blood gas measurements to monitor hemoglobin oxygen saturation. Be vigilant for other signs and symptoms of pulmonary embolism and DVT (Table).
Consider prophylactic treatment. Some studies recommend prophylaxis against thromboembolic events in catatonic patients.3-6,10,15 These measures include:
- intravenous fluids
- nasogastric tube feeding
- physical examinations to assess for signs of DVT
- support stockings
- sequential/pneumatic compression devices
- physical therapy or range-of-motion exercises
- complete anticoagulation during immobility, although there are no data that support using anticoagulation medications in catatonic patients who have not yet experienced a thromboembolic event.
Consider prophylactic antithrombotic treatment in catatonic patients and other immobile inpatients who have risk factors for thromboembolic events.9,16 Although it has not been rigorously tested, the Algorithm suggested by Malý et al15 can serve as a guideline for determining the need for prophylaxis against venous thromboembolism in psychiatric inpatient settings.
Table
Signs and symptoms of deep vein thrombosis and pulmonary embolism
| Deep vein thrombosis |
| Swelling of the leg or along a vein in the leg |
| Pain or tenderness in the leg, which may be felt only when standing or walking |
| Increased warmth in the area of the leg that is swollen or in pain |
| Red or discolored skin on the leg |
| Pulmonary embolism |
| Unexplained shortness of breath or pain with deep breathing |
| Chest pain |
| Coughing or coughing up blood |
| Arrhythmia |
| Source: National Heart, Lung, and Blood Institute. What are the signs and symptoms of deep vein thrombosis? Available at: www.nhlbi.nih.gov/health/dci/Diseases/Dvt/DVT_ SignsAndSymptoms.html. Accessed November 8, 2010 |
Algorithm
Does my patient need venous thromboembolism prophylaxis?
| Step 1. Assess risk factors for venous thromboembolism and determine risk level score | |
|---|---|
| Risk factor | Score |
| Consensus-based | |
| Immobilization | 1 |
| Hormone therapy | 1 |
| Obesity (BMI ≥30 kg/m2) | 1 |
| Age 60 to 74 | 1 |
| Varicose veins/venous insufficiency | 1 |
| Dehydration | 1 |
| Thrombophilia | 1 |
| Expert opinion | |
| Treatment with antipsychotics | 1 |
| Evidence-based | |
| History of deep vein thrombosis or pulmonary embolism | 2 |
| Cancer (active/treated) | 2 |
| Age ≥75 | 2 |
| Acute infection/respiratory disease | 2 |
| TOTAL | |
| BMI: body mass index | |
| Step 2. Determine recommended prophylaxis based on risk level score | |
| Risk level score | Recommended prophylaxis |
| All risk levels | Regular physical exercise of lower extremities, sufficient hydration, graduated compression stockings |
| Medium risk (4 to 7 points) and/or physical restraint ≥8 hours | Heparin, 5,000 units every 12 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| High risk (≥8 points) | Heparin, 5,000 units every 8 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| Source: Adapted from reference 15 | |
OUTCOME: Stable and speaking
In the hospital, Mr. M remains immobile and mute for several days. The hospital’s psychiatric consult team recommends lorazepam, 3 mg/d, to address his catatonia. Mr. M improves and begins speaking and eating after starting lorazepam, but becomes agitated, banging his head against walls and threatening to jump out the window. Because this puts him at risk for trauma, Mr. M is not a good candidate for warfarin therapy, and an inferior vena cava filter is placed on an emergency basis. Later, a Dobhoff tube is placed for feeding and administering oral medications.
Mr. M’s catatonic state gradually improves and he begins to respond to the staff with short phrases, eats all of his food, and accepts oral medications. He is transferred back to our inpatient psychiatric facility with haloperidol, 10 mg/d, lorazepam, 3 mg/d, and benztro-pine, 2 mg/d, in addition to sulfacetamide eye drops for bilateral conjunctivitis. At our facility, we start him on warfarin, 5 mg/d, and closely monitor his international normalized ratio levels, with a plan to remove the inferior vena cava filter after 6 months of anticoagulation therapy. Mr. M remains at our facility for 3 weeks to stabilize his medications and is discharged to his apartment.
Six months after being discharged from our facility, Mr. M is stable at an intensive outpatient mental health program.
Related Resources
- Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge, United Kingdom: Cambridge University Press; 2003.
- Snow V, Qaseem A, Barry P, et al, and American College of Physicians; American Academy of Family Physicians Panel on Deep Venous Thrombosis/Pulmonary Embolism. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146(3):204-210.
Drug Brand Names
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Sulfacetamide • Sulamyd
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Nude and mute
Mr. M, age 45, is found naked outside his apartment. He has a history of schizophrenia, paranoid type, hypertension, and diet-controlled type 2 diabetes mellitus. His schizophrenia has been treated with ziprasidone, 160 mg/d, but 2 months ago he stopped taking his medication and seeing his psychiatrist. He does not respond to questions from police and is taken to a local emergency department for medical workup of altered mental status.
Mr. M is noted to have bilateral conjunctival discharge and a white blood cell (WBC) count of 15,000/mm3. Vital signs, physical examination, laboratory studies, and head CT are otherwise within normal limits. Mr. M is medically cleared for his 15th admission to our inpatient psychiatric facility in the last 7 years. He is divorced, has 2 adult sons, and receives Social Security disability benefits.
Mr. M is alert but guarded and mute and appears to be internally preoccupied. His mood is euthymic and his facial expressions do not vary much and are similar to a blank stare. His grooming and hygiene are poor, but there is no evidence of delusions or suicidal or homicidal ideation. He paces around the unit or sits in his bed staring straight ahead, occasionally mouthing inaudible words but remaining nonverbal.
Mr. M is restarted on his previous dose of ziprasidone and referred to the primary care physician in our inpatient psychiatric facility for further evaluation. His admission vitals and laboratory values show a platelet count of 124,000/mm3, glucose of 113 mg/dL, triglycerides of 160 mg/dL, high-density lipoprotein of 37 mg/dL, and hemoglobin A1c of 6%. Mr. M needs help drinking fluids but resists solid foods as well as medications, including lorazepam, 3 mg/d, and most scheduled doses of ziprasidone. On day 3, Mr. M’s extremities are rigid and he has poor oral intake. We diagnose Mr. M with catatonia based on his immobility, negativity, and mutism.
The authors’ observations
The literature describes >40 signs of catatonia.1-11 According to DSM-IV-TR, catatonia may occur in the context of schizophrenia, a mood disorder, or a general medical condition. DSM-IV-TR criteria for catatonia include:
- motor immobility as evidenced by catalepsy or stupor
- excessive motor activity
- extreme negativism or mutism
- peculiarities of voluntary movements as evidenced by posturing, stereotypic movements, or grimacing
- echolalia or echopraxia.12
Only 2 signs are necessary to meet the diagnostic criteria for catatonia.11,12 Several catatonia rating scales—including the Bush-Francis Catatonia Rating Scale (BFCRS)—have been found to be highly reliable for screening for and rating the severity of catatonia. Such tools also can be used serially to monitor treatment efficacy. The BFCRS takes 5 minutes to administer; the screen is considered positive if ≥2 of the first 14 items on the scale are present.13 Mr. M exhibits immobility and mutism, which are the most common signs of catatonia.
In patients with catatonia, poor oral intake may result in malnutrition that often requires parenteral nutrition or intravenous fluids1,10 and dehydration that may lead to dental caries, gum disease, constipation, and ileus.1 Pneumonia may occur secondary to atelectasis or buildup of respiratory secretions and possibly aspiration.7 Vaginal infections may develop secondary to poor hygiene.1 Immobility and malnutrition may lead to infection and decubitus ulcers.1 Finally, immobility also may cause urinary incontinence,2,10 nerve palsies, flexion contractions, and rhabdomyolysis.1
EVALUATION: Venous complications
On day 3, Mr. M is referred to a local emergency department, where he is assessed for delirium and dehydration because of increased WBC count and diaphoresis. The medical staff finds bilateral pulmonary embolisms and a deep vein thrombosis (DVT) of his left lower leg.
The authors’ observations
Catatonia is associated with an increased risk of venous thromboembolism because of the increased risk of venous stasis and hypercoagulability, both elements of Virchow’s triad for thrombogenesis.1-10,14,15 The third element of Virchow’s triad, vascular injury, does not appear to directly increase the risk for thromboembolic events in catatonic states.
Catatonia-specific causes for venous stasis include immobility, prolonged use of physical restraints, and sedation as a side effect of antipsychotic use.16
Causes for hypercoagulability during catatonic states include:
- increased catecholamine levels during excited states3
- hyperhomocysteinemia secondary to poor diet, smoking, and/or high caffeine consumption16
- increased anticardiolipin and/or anti-phospholipid antibody levels secondary to use of specific antipsychotics, such as chlorpromazine and clozapine16
- increased platelet aggregation secondary to hyperprolactinemia caused by low-potency conventional antipsychotics, such as chlorpromazine16,17
- increased platelet activation caused by altered levels of platelet serotonin in depressed patients.18
Patients taking low-potency conventional antipsychotics may have a 7-fold greater risk for thromboembolic events compared with those who do not use these medications.16
Reducing thromboembolic risk
Diagnose catatonia early. Treating symptoms of catatonia early with benzodiazepines (and, in refractory cases, with electroconvulsive therapy) prevents immobility, thereby decreasing the risk of thromboembolic events.3,11 It may be useful to minimize antipsychotic use.
Monitor activity levels. Fatal thromboembolic events may appear early in the course of catatonia before risk factors associated with thromboembolic events are evident.4 However, these events may be more common when the patient resumes movement.3 Monitor patients’ activity status and encourage ambulation throughout treatment.
Monitor vital signs for signs of pulmonary embolism, including hypoxia, tachycardia, tachypnea, and fever. Take serial pulse oximetry and, if indicated, arterial blood gas measurements to monitor hemoglobin oxygen saturation. Be vigilant for other signs and symptoms of pulmonary embolism and DVT (Table).
Consider prophylactic treatment. Some studies recommend prophylaxis against thromboembolic events in catatonic patients.3-6,10,15 These measures include:
- intravenous fluids
- nasogastric tube feeding
- physical examinations to assess for signs of DVT
- support stockings
- sequential/pneumatic compression devices
- physical therapy or range-of-motion exercises
- complete anticoagulation during immobility, although there are no data that support using anticoagulation medications in catatonic patients who have not yet experienced a thromboembolic event.
Consider prophylactic antithrombotic treatment in catatonic patients and other immobile inpatients who have risk factors for thromboembolic events.9,16 Although it has not been rigorously tested, the Algorithm suggested by Malý et al15 can serve as a guideline for determining the need for prophylaxis against venous thromboembolism in psychiatric inpatient settings.
Table
Signs and symptoms of deep vein thrombosis and pulmonary embolism
| Deep vein thrombosis |
| Swelling of the leg or along a vein in the leg |
| Pain or tenderness in the leg, which may be felt only when standing or walking |
| Increased warmth in the area of the leg that is swollen or in pain |
| Red or discolored skin on the leg |
| Pulmonary embolism |
| Unexplained shortness of breath or pain with deep breathing |
| Chest pain |
| Coughing or coughing up blood |
| Arrhythmia |
| Source: National Heart, Lung, and Blood Institute. What are the signs and symptoms of deep vein thrombosis? Available at: www.nhlbi.nih.gov/health/dci/Diseases/Dvt/DVT_ SignsAndSymptoms.html. Accessed November 8, 2010 |
Algorithm
Does my patient need venous thromboembolism prophylaxis?
| Step 1. Assess risk factors for venous thromboembolism and determine risk level score | |
|---|---|
| Risk factor | Score |
| Consensus-based | |
| Immobilization | 1 |
| Hormone therapy | 1 |
| Obesity (BMI ≥30 kg/m2) | 1 |
| Age 60 to 74 | 1 |
| Varicose veins/venous insufficiency | 1 |
| Dehydration | 1 |
| Thrombophilia | 1 |
| Expert opinion | |
| Treatment with antipsychotics | 1 |
| Evidence-based | |
| History of deep vein thrombosis or pulmonary embolism | 2 |
| Cancer (active/treated) | 2 |
| Age ≥75 | 2 |
| Acute infection/respiratory disease | 2 |
| TOTAL | |
| BMI: body mass index | |
| Step 2. Determine recommended prophylaxis based on risk level score | |
| Risk level score | Recommended prophylaxis |
| All risk levels | Regular physical exercise of lower extremities, sufficient hydration, graduated compression stockings |
| Medium risk (4 to 7 points) and/or physical restraint ≥8 hours | Heparin, 5,000 units every 12 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| High risk (≥8 points) | Heparin, 5,000 units every 8 hours, or low molecular weight heparin equivalent until patient is fully mobilized |
| Source: Adapted from reference 15 | |
OUTCOME: Stable and speaking
In the hospital, Mr. M remains immobile and mute for several days. The hospital’s psychiatric consult team recommends lorazepam, 3 mg/d, to address his catatonia. Mr. M improves and begins speaking and eating after starting lorazepam, but becomes agitated, banging his head against walls and threatening to jump out the window. Because this puts him at risk for trauma, Mr. M is not a good candidate for warfarin therapy, and an inferior vena cava filter is placed on an emergency basis. Later, a Dobhoff tube is placed for feeding and administering oral medications.
Mr. M’s catatonic state gradually improves and he begins to respond to the staff with short phrases, eats all of his food, and accepts oral medications. He is transferred back to our inpatient psychiatric facility with haloperidol, 10 mg/d, lorazepam, 3 mg/d, and benztro-pine, 2 mg/d, in addition to sulfacetamide eye drops for bilateral conjunctivitis. At our facility, we start him on warfarin, 5 mg/d, and closely monitor his international normalized ratio levels, with a plan to remove the inferior vena cava filter after 6 months of anticoagulation therapy. Mr. M remains at our facility for 3 weeks to stabilize his medications and is discharged to his apartment.
Six months after being discharged from our facility, Mr. M is stable at an intensive outpatient mental health program.
Related Resources
- Fink M, Taylor MA. Catatonia: a clinician’s guide to diagnosis and treatment. Cambridge, United Kingdom: Cambridge University Press; 2003.
- Snow V, Qaseem A, Barry P, et al, and American College of Physicians; American Academy of Family Physicians Panel on Deep Venous Thrombosis/Pulmonary Embolism. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146(3):204-210.
Drug Brand Names
- Benztropine • Cogentin
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Sulfacetamide • Sulamyd
- Warfarin • Coumadin
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Caroff SN, Mann SC, Francis A, et al. eds. Catatonia: from psychopathology to neurobiology. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
2. Gangadhar BN, Keshavan MS, Goswami U, et al. Cortical venous thrombosis presenting as catatonia: a clinicopathologic report. J Clin Psychiatry. 1983;44:109-110.
3. McCall WV, Mann SC, Shelp FE, et al. Fatal pulmonary embolism in the catatonic syndrome: two case reports and a literature review. J Clin Psychiatry. 1995;51:21-25.
4. Morioka H, Nagatomo I, Yamada K, et al. Deep venous thrombosis of the leg due to psychiatric stupor. Psychiatry Clin Neurosci. 1997;51:323-326.
5. Lachner C, Sandson NB. Medical complications of catatonia: a case of catatonia-induced deep venous thrombosis. Psychosomatics. 2003;44:512-514.
6. Woo BK. Basal ganglia calcification and pulmonary embolism in catatonia. J Neuropsychiatry Clin Neurosci. 2007;19:472-473.
7. Regestein QR, Alpert JS, Reich P. Sudden catatonic stupor with disastrous outcome. JAMA. 1977;238:618-620.
8. Suzuki K, Takamatsu K, Takano T, et al. Safety of electroconvulsive therapy in psychiatric patients shortly after the occurrence of pulmonary embolism. J ECT. 2008;24:286-288.
9. Tsao C, Nusbaum A. Successful ECT course for catatonia after large pulmonary embolism and placement of inferior vena cava filter. Gen Hosp Psychiatry. 2007;29:374.-
10. Barbuto J. Preventing sudden death during a catatonic episode. Hosp Community Psychiatry. 1983;34:72-73.
11. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160:1233-1241.
12. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
13. Bush G, Fink M, Petrides G, et al. Catatonia I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
14. Lal S, Bleiman M, Brown GN. Pulmonary embolism in psychiatric patients. J Am Geriatr Soc. 1966;14:1138-1143.
15. Malý R, Masopust J, Hosák L, et al. Assessment of risk of venous thromboembolism and its possible prevention in psychiatric patients. Psychiatry Clin Neurosci. 2008;62:3-8.
16. Higg S, Jönsson AK, Spigset O. Risk of venous thromboembolism due to antipsychotic drug therapy. Expert Opin Drug Saf. 2009;8:537-547.
17. Wallaschofski H, Eigenthaler M, Kiefer M, et al. Hyperprolactinemia in patients on antipsychotic drugs causes ADP-stimulated platelet activation that might explain the increased risk for venous thromboembolism: pilot study. J Clin Psychopharmacol. 2003;23(5):479-483.
18. Arnone D, Hansen L, Davies G. Pulmonary embolism and severe depression. Am J Psychiatry. 2009;159:873-874.
1. Caroff SN, Mann SC, Francis A, et al. eds. Catatonia: from psychopathology to neurobiology. Arlington, VA: American Psychiatric Publishing, Inc.; 2004.
2. Gangadhar BN, Keshavan MS, Goswami U, et al. Cortical venous thrombosis presenting as catatonia: a clinicopathologic report. J Clin Psychiatry. 1983;44:109-110.
3. McCall WV, Mann SC, Shelp FE, et al. Fatal pulmonary embolism in the catatonic syndrome: two case reports and a literature review. J Clin Psychiatry. 1995;51:21-25.
4. Morioka H, Nagatomo I, Yamada K, et al. Deep venous thrombosis of the leg due to psychiatric stupor. Psychiatry Clin Neurosci. 1997;51:323-326.
5. Lachner C, Sandson NB. Medical complications of catatonia: a case of catatonia-induced deep venous thrombosis. Psychosomatics. 2003;44:512-514.
6. Woo BK. Basal ganglia calcification and pulmonary embolism in catatonia. J Neuropsychiatry Clin Neurosci. 2007;19:472-473.
7. Regestein QR, Alpert JS, Reich P. Sudden catatonic stupor with disastrous outcome. JAMA. 1977;238:618-620.
8. Suzuki K, Takamatsu K, Takano T, et al. Safety of electroconvulsive therapy in psychiatric patients shortly after the occurrence of pulmonary embolism. J ECT. 2008;24:286-288.
9. Tsao C, Nusbaum A. Successful ECT course for catatonia after large pulmonary embolism and placement of inferior vena cava filter. Gen Hosp Psychiatry. 2007;29:374.-
10. Barbuto J. Preventing sudden death during a catatonic episode. Hosp Community Psychiatry. 1983;34:72-73.
11. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160:1233-1241.
12. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
13. Bush G, Fink M, Petrides G, et al. Catatonia I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
14. Lal S, Bleiman M, Brown GN. Pulmonary embolism in psychiatric patients. J Am Geriatr Soc. 1966;14:1138-1143.
15. Malý R, Masopust J, Hosák L, et al. Assessment of risk of venous thromboembolism and its possible prevention in psychiatric patients. Psychiatry Clin Neurosci. 2008;62:3-8.
16. Higg S, Jönsson AK, Spigset O. Risk of venous thromboembolism due to antipsychotic drug therapy. Expert Opin Drug Saf. 2009;8:537-547.
17. Wallaschofski H, Eigenthaler M, Kiefer M, et al. Hyperprolactinemia in patients on antipsychotic drugs causes ADP-stimulated platelet activation that might explain the increased risk for venous thromboembolism: pilot study. J Clin Psychopharmacol. 2003;23(5):479-483.
18. Arnone D, Hansen L, Davies G. Pulmonary embolism and severe depression. Am J Psychiatry. 2009;159:873-874.
Descent after a missed flight
CASE: Psychotic and sleepless
Mr. F, age 30, is referred to our psychiatric outpatient clinic for follow-up care after hospitalization to treat a psychotic episode. His psychotic symptoms started 2 years ago without an identifiable trigger. Mr. F complains of episodic mood symptoms, such as depression, irritability, and angry outbursts; persistent auditory hallucinations (voices calling him names); and persecutory delusions. While in the hospital he was diagnosed with psychotic disorder not otherwise specified and started on olanzapine titrated to 30 mg/d.
During evaluation, Mr. F is depressed and exhibits motor retardation, slow speech, bland affect, impaired short-term memory, and auditory hallucinations. He describes social anxiety and has ideas of reference and problems interpreting facial expressions. He is guarded and suspicious. Although auditory hallucinations and depression affect Mr. F’s daily activities, he is attempting to find a job.
Mr. F has used alcohol since age 16 to escape social difficulties. He says he last used alcohol 1 year ago, but refuses to provide details about how much alcohol he typically consumed. Sporadic cannabis use also started when Mr. F was in his teens.
Mr. F’s symptoms improve with olanzapine, but he complains of weight gain and sedation, so we switch him to aripiprazole, 10 mg/d. Two weeks later he reports feeling jittery and anxious, so we discontinue aripiprazole and start loxapine, 25 mg/d at night, and propranolol, 60 mg/d, for residual akathisia. Despite limited clinical improvement, Mr. F irrationally says he wants to join the Navy. After a week, his psychotic symptoms improve but anxiety persists, so we start clonazepam, 1 mg/d, and oxcarbazepine, 600 mg/d. After 2 weeks he says he feels calmer, but has gained 20 lbs and is constantly tired. Against our advice, Mr. F decides to discontinue loxapine and propranolol, but continues clonazepam and oxcarbazepine.
At his next visit 4 weeks later, Mr. F is in good spirits. He says he is looking for a job as a dental assistant, and shows no apparent signs of psychosis. Mr. F misses his next appointment but returns 3 months later with evident deterioration in his general appearance. He says he is having difficulty sleeping and is depressed, stating “I just lay in bed; I don’t want to deal with life.” He is withdrawn and unwilling to elaborate on his personal problems but asks for a refill of clonazepam and oxcarbazepine, which we provide.
The authors’ observations
Sleep disturbances, including poor sleep efficiency, increased sleep-onset latency, decreased rapid eye movement (REM) sleep latency, and decreased stage 4 of non-REM sleep, occur in 16% to 30% of patients with schizophrenia and are associated with reduced quality of life and poor coping skills.1 Sleep-onset and sleep maintenance problems and sleep-wake reversal generally persist despite antipsychotic treatment.2,3
Slow-wave sleep deficiency can lead to negative symptoms and memory deficits in patients with schizophrenia because4:
- declarative and procedural memory consolidation are associated with slow-wave and stage 2 sleep, respectively
- procedural learning and visual spatial memory are correlated with delta power in slow-wave sleep.3,8
Acute psychosis exacerbations are associated with restless, agitated sleep. Insomnia often is an early warning sign of clinical relapse.5 The etiology of sleep dysfunction in schizophrenia is unknown, but glutamatergic action through N-methyl-d-aspartate receptors, the GABA system,6 and the serotonin system7 have been implicated.
Relapse to alcohol could trigger an exacerbation of Mr. F’s illness; however, he continues to deny alcohol or drug use and we could not identify any evidence of alcohol use at his last visit.
HISTORY: Strange behavior
Mr. F is a first-generation immigrant from Venezuela. He has a general educational development diploma and an associate’s degree. He says he has worked as a dental assistant but lost his job after a driving under the influence charge a year ago. Subsequently, he could not remain employed for long. He lives with his parents.
When Mr. F returns to the clinic 5 months later, he has lost 20 lbs and complains of anxiety and lack of sleep. With stooped posture, slow movements, and a mood-incongruent smile, he admits he ran out of medications and asks for refills, which we provide. He appears somewhat bizarre, wearing a loosely fitting baseball cap that covers his direct field of vision. Mr. F admits that he has been pulling out his hair. His thought process is impoverished and his answers are guarded and evasive. He rejects our recommendation of an antipsychotic; the only medications he is willing to continue are oxcarbazepine and clonazepam.
The authors’ observations
Treatment strategies for sleep disorders in patients with schizophrenia mainly target behavioral aspects of sleep, such as sleep onset and total sleep time, and rarely correct polysomnographic disturbances. Commonly used medications include atypical antipsychotics, benzodiazepines, zolpidem, zopiclone, and antidepressants with sedative properties (Table 1).1 However, new insights on sleep architecture patterns in these individuals have directed focus on other medications. Although antipsychotics, GABAA modulators, and melatonin provide some sleep benefits, none of these agents fully address characteristic sleep disturbances found in patients with schizophrenia.
Recent research has looked at GABAB modulators because of their unique function. GABAB receptors are located on pre-synaptic dopaminergic terminals and inhibit dopamine release and modulate glutamatergic regulation of dopamine. In the glutamate hypofunction model of psychosis, a GABAB agonist would cause disinhibition of glutamate modulation of mesolimbic dopamine and reversal of GABA transmission in the ventral tegmental area.9 Baclofen and γ-hydroxybutyric acid (GHB) currently are the only FDA-approved GABAB receptor agonists. Overall, trials of baclofen have not shown benefit for sleep disturbances in patients with schizophrenia,10,11 perhaps because of the drug’s poor liposolubility and consequent inability to cross the blood-brain barrier. Although hydrophilic like baclofen, GHB, which is also known as sodium oxybate and is FDA-approved for cataplexy due to narcolepsy, might have an advantage because of carrier-mediated transfer across the blood-brain barrier. GHB is thought to act directly as a neurotransmitter but also interacts with dopamine via the GHB receptor and with the GABAB receptor after it is converted to extracellular GABA.
Table 1
Schizophrenia and sleep dysfunction: The effect of psychotropics
| Medication/class | Comments |
|---|---|
| Atypical antipsychotics | In the CATIE study, a large proportion of patients had sleep problems despite antipsychotic treatment Atypicals may improve sleep acutely, but do not normalize it The long-term effects of atypicals on sleep architecture in schizophrenia are unclear; some studies show improved slow-wave sleep but in others slow-wave sleep is reduced |
| GABAA modulators (benzodiazepines, zolpidem, zopiclone) | Decrease sleep latency and nocturnal awakening Do not increase slow-wave sleep and overall sleep quality Decrease slow-wave sleep and REM sleep in rats May impair sleep architecture and cognition |
| Melatonin and modafinil | Melatonin may be useful for improving subjective sleep in patients with schizophrenia, although it does not improve slow-wave sleep parameters Modafinil may enhance cognition |
| GABAB receptor agonists | Few trials in humans but animal studies support a potential therapeutic role Minimal impact on REM sleep Increase slow-wave sleep Human studies with the GABAB agonist GHB show improvement in sleep architecture and subjective sleep |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness; GHB: γ-hydroxybutyric acid; REM: rapid eye movement | |
| Source:Reference 1 | |
OUTCOME: A trip cut short
Mr. F does not return to the clinic as scheduled, but 2 months later the U.S. consulate of a Western European country contacts us because Mr. F had a bottle of oxcarbazepine with our contact information. After Mr. F returns to the United States, he tells us his story.
After his last outpatient visit, Mr. F relapsed on alcohol, became despondent over his weakness, and searched for a way to escape his alcohol cravings. He came up with a plan to relocate to an Islamic Middle Eastern country where alcohol is banned and its use heavily punished. Mr. F bought a one-way airplane ticket through a Western Europe connection and departed 7 days later without notifying his family or psychiatrist.
Mr. F’s flight to Western Europe was uneventful. After landing for a connecting flight, his mood improved, his outlook became hopeful, and his auditory hallucinations changed from derogatory to supportive. However, Mr. F became despondent after being barred from his next flight because he did not have a return ticket. He was stranded in the airport with little money and no extra clothing, only his passport and laptop. He slept in the airport and after 3 days set off into the city. Mr. F navigated subway stations, ate at soup kitchens, and sought shelter in hotel lobbies and churches. One week after Mr. F left the airport, the police detained him for disorganized behavior and refusing to vacate a church. He was transported to a hospital, admitted to the psychiatric unit for catatonia, and stabilized on olanzapine, 20 mg/d.
After 1 week, Mr. F was returned to the United States and hospitalized for further evaluation and treatment. On his first day back, Mr. F’s disorganized process appeared to improve. He was euthymic and reported good sleep, tolerable anxiety, and infrequent derogatory auditory hallucinations that were low in volume. On day 3, Mr. F’s mood deteriorated moderately. He became depressed and again experienced derogatory auditory hallucinations. He was internally preoccupied and showed reduced affect and psychomotor activity. Mr. F was discharged the next day to a state-run respite program with a structured plan for psychiatric follow-up, social services, and sobriety maintenance. He remained on olanzapine, 20 mg/d, because we anticipated he would need an adjustment period after his uncommon journey.
The authors’ observations
Psychotic symptoms occurring during long-distance trips have been well described in psychiatric literature. Westbound travel could exacerbate depression. Emerging mania has been documented in eastbound flights, which could be related to sleep deprivation.12,13 The incidence of psychotic exacerbations is correlated with the number of time zones crossed.12
A change in environment, unfamiliar surroundings, presence of strangers, physical inactivity, and a sense of isolation all contribute to jet lag syndrome. Long-distance air travel also disrupts zeitgebers, environmental cues that induce adjustments in the internal body clock.12,14 The body clock is controlled mainly by the SCN in the hypothalamus, which is primarily regulated by the light/dark cycle via melatonin secretion (Figure).
Endogenous changes in circadian rhythms and melatonin secretion abnormalities are present in the pathophysiological mechanism of several psychiatric disorders, including depression, bipolar disorder, and schizophrenia. Trbovic hypothesized that in essence schizophrenia could be a sleep disorder and SCN dysfunction may contribute to the pathogenesis of schizophrenia.15 Several research findings support this hypothesis (Table 2). Recent evidence suggests that abnormal circadian melatonin metabolism may be directly related to the schizophrenia pathophysiology.16 Because melatonin production is regulated by the SCN and jet lag resets the melatonin cycle, a defective SCN may not respond well to such adjustments.
Mr. F’s symptomatology is illustrative of the jet lag scenario. His auditory hallucinations became “more supportive” and helpful during his eastbound flight, whereas after his return to the United States, depression was the predominant mood symptom. Psychotic exacerbation also was noticeable after his return.
There are no recommended treatments for psychosis related to jet lag. Antipsychotics often are used, although there is no accepted agent of choice. Treatment of jet lag includes addressing sleep loss and desynchronization.17 Medications suggested for treatment of sleep loss are antihistamines (H1 receptor antagonists), benzodiazepines, and imidazopyridines (zolpidem, zopiclone). Light therapy or administration of melatonin, ramelteon, or agomelatine can help jet-lagged patients resynchronize with the environment.
Figure: Pathways for light: Circadian timing system
Photic information reaches the suprachiasmatic nucleus (SCN) through the retinohypothalamic tract (RHT), which uses glutamate (GLU) as a neurotransmitter. A multisynaptic indirect pathway also carries photic information to the SCN. This indirect route arises from the RHT, projects through the intergeniculate leaflet (IGL) of the lateral geniculate nucleus, and finally, the geniculohypothalamic tract (GHT). Neuropeptide Y (NPY) is the neurotransmitter of the GHT. Serotoninergic (5-HT) input to the SCN arrives from the dorsal raphe nuclei. Melatonin, produced in the pineal gland, exerts its effect on circadian timing by feeding back onto the SCN.
Source: Reprinted with permission from reference 14Table 2
Suprachiasmatic nucleus dysfunction may have a role in schizophrenia
| Consequences of SCN dysfunction | Findings relevant to schizophrenia |
|---|---|
| Circadian pattern abnormalities | Individuals with schizophrenia do not have a characteristic circadian pattern of melatonin secretiona Actigraphic studies confirm that patients with schizophrenia have abnormal circadian rhythm activitiesb-d |
| Dopaminergic system abnormalities | The fetal dopaminergic system and D1 dopamine receptors may be involved in the process of synchronizing the SCNe,f |
| Jet lag symptomatology | Jet lag can exacerbate psychiatric disorders,g which suggests that in these patients the SCN is not capable of adjustment |
| Pathologic daytime sleep | Saccadic eye movements in patients with schizophrenia suggest they may be experiencing remnants of REM sleep, supporting the notion that these patients may have dream states during wakefulness |
| REM: rapid eye movement; SCN: suprachiasmatic nucleus | |
| Source: a. Bersani G, Mameli M, Garavini A, et al. Reduction of night/day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Neuro Endocrinol Lett. 2003;24(3-4):181-184. b. Poyurovsky M, Nave R, Epstein R, et al. Actigraphic monitoring (actigraphy) of circadian locomotor activity in schizophrenic patients with acute neuroleptic-induced akathisia. Eur Neuropsychopharmacol. 2000;10(3):171-176. c. Haug HJ, Wirz-Justice A, Rössler W. Actigraphy to measure day structure as a therapeutic variable in the treatment of schizophrenic patients. Acta Psychiatr Scand Suppl. 2000;(407):91-95. d. Martin JL, Jeste DV, Ancoli-Israel S. Older schizophrenia patients have more disrupted sleep and circadian rhythms than age-matched comparison subjects. J Psychiatr Res. 2005;39(3):251-259. e. Strother WN, Norman AB, Lehman MN. D1-dopamine receptor binding and tyrosine hydroxylase-immunoreactivity in the fetal and neonatal hamster suprachiasmatic nucleus. Brain Res Dev Brain Res. 1998;106(1-2):137-144. f. Viswanathan N, Weaver DR, Reppert SM, et al. Entrainment of the fetal hamster circadian pacemaker by prenatal injections of the dopamine agonist SKF 38393. J Neurosci. 1994;14(9):5393-5398. g. Katz G, Durst R, Zislin J, et al. Jet lag causing or exacerbating psychiatric disorders. Harefuah. 2000;138(10):809-812, 912. | |
Related Resources
- Klein DC, Moore R, Reppert SM, eds. Suprachiasmatic nucleus: the mind’s clock. New York, NY: Oxford University Press; 1991.
- Hofstetter JR, Lysaker PH, Mayeda AR. Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry. 2005;5:13.
Drug Brand Names
- Agomelatine • Valdoxan
- Aripiprazole • Abilify
- Baclofen • Lioresal
- Clonazepam • Klonopin
- γ-hydroxybutyric acid, sodium oxybate • Xyrem
- Loxapine • Loxitane
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Propranolol • Inderal
- Ramelteon • Rozerem
- Zolpidem • Ambien
- Zoplicone • Lunesta
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kantrowitz J, Citrome L, Javitt D. GABA(B) receptors, schizophrenia and sleep dysfunction: a review of the relationship and its potential clinical and therapeutic implications. CNS Drugs. 2009;23(8):631-669.
2. Poulin J, Daoust AM, Forest G, et al. Sleep architecture and its clinical correlates in first episode and neuroleptic-naïve patients with schizophrenia. Schizophr Res. 2003;62:147-153.
3. Ferrarelli F, Huber R, Peterson MJ. Reduced sleep spindle activity in schizophrenia patients. Am J Psychiatry. 2007;164(3):483-492.
4. Cohrs S. Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs. 2008;22(11):939-962.
5. Haffmans P, Hoencamp E, Knegtering HJ, et al. Sleep disturbance in schizophrenia. Br J Psychiatry. 1994;165(5):697-698.
6. Wisor J, Morairty S, Huynh N, et al. Gene expression in the rat cerebral cortex: comparison of recovery sleep and hypnotic-induced sleep. Neuroscience. 2006;141(1):371-378.
7. Benson KL, Faull KF, Zarcone VP. Evidence for the role of serotonin in the regulation of slow wave sleep in schizophrenia. Sleep. 1991;14(2):133-139.
8. Göder R, Boigs M, Braun S, et al. Impairment of visuospatial memory is associated with decreased slow wave sleep in schizophrenia. J Psychiatr Res. 2004;38:591-599.
9. Harte M, O’Connor WT. Evidence for a selective prefrontal cortical GABA(B) receptor mediated inhibition of glutamate release in the ventral tegmental area: a dual probe microdialysis study in the awake rat. Neuroscience. 2005;130(1):215-222.
10. Garbutt JC, van Kammen DP. The interaction between GABA and dopamine: implications for schizophrenia. Schizophr Bull. 1983;9(3):336-353.
11. Finnimore A, Roebuck M, Sajkov D, et al. The effects of the GABA agonist, baclofen, on sleep and breathing. Eur Respir J. 1995;8(2):230-234.
12. Jahuar P, Weller MP. Psychiatric morbidity and time zone changes: a study of patients from Heathrow airport. Br J Psychiatry. 1982;140:231-234.
13. Katz G, Durst R, Zislin Y, et al. Psychiatric aspects of jet lag: review and hypothesis. Med Hypotheses. 2001;56(1):20-23.
14. Waterhouse J, Reilly T, Atkinson G. Jet-lag. Lancet. 1997;350:1611-1616.
15. Trbovic SM. Schizophrenia as a possible dysfunction of the suprachiasmatic nucleus. Med Hypotheses. 2010;74:127-131.
16. Bersani G, Mameli M, Garavini A, et al. Reduction of night/ day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Nuero Endocrinol Lett. 2003;24(3-4):181-184.
17. Brown GM, Pandi-Perumal SR, Trakht I, et al. Melatonin and its relevance to jet lag. Travel Med Infect Dis. 2009;7:69-81.
CASE: Psychotic and sleepless
Mr. F, age 30, is referred to our psychiatric outpatient clinic for follow-up care after hospitalization to treat a psychotic episode. His psychotic symptoms started 2 years ago without an identifiable trigger. Mr. F complains of episodic mood symptoms, such as depression, irritability, and angry outbursts; persistent auditory hallucinations (voices calling him names); and persecutory delusions. While in the hospital he was diagnosed with psychotic disorder not otherwise specified and started on olanzapine titrated to 30 mg/d.
During evaluation, Mr. F is depressed and exhibits motor retardation, slow speech, bland affect, impaired short-term memory, and auditory hallucinations. He describes social anxiety and has ideas of reference and problems interpreting facial expressions. He is guarded and suspicious. Although auditory hallucinations and depression affect Mr. F’s daily activities, he is attempting to find a job.
Mr. F has used alcohol since age 16 to escape social difficulties. He says he last used alcohol 1 year ago, but refuses to provide details about how much alcohol he typically consumed. Sporadic cannabis use also started when Mr. F was in his teens.
Mr. F’s symptoms improve with olanzapine, but he complains of weight gain and sedation, so we switch him to aripiprazole, 10 mg/d. Two weeks later he reports feeling jittery and anxious, so we discontinue aripiprazole and start loxapine, 25 mg/d at night, and propranolol, 60 mg/d, for residual akathisia. Despite limited clinical improvement, Mr. F irrationally says he wants to join the Navy. After a week, his psychotic symptoms improve but anxiety persists, so we start clonazepam, 1 mg/d, and oxcarbazepine, 600 mg/d. After 2 weeks he says he feels calmer, but has gained 20 lbs and is constantly tired. Against our advice, Mr. F decides to discontinue loxapine and propranolol, but continues clonazepam and oxcarbazepine.
At his next visit 4 weeks later, Mr. F is in good spirits. He says he is looking for a job as a dental assistant, and shows no apparent signs of psychosis. Mr. F misses his next appointment but returns 3 months later with evident deterioration in his general appearance. He says he is having difficulty sleeping and is depressed, stating “I just lay in bed; I don’t want to deal with life.” He is withdrawn and unwilling to elaborate on his personal problems but asks for a refill of clonazepam and oxcarbazepine, which we provide.
The authors’ observations
Sleep disturbances, including poor sleep efficiency, increased sleep-onset latency, decreased rapid eye movement (REM) sleep latency, and decreased stage 4 of non-REM sleep, occur in 16% to 30% of patients with schizophrenia and are associated with reduced quality of life and poor coping skills.1 Sleep-onset and sleep maintenance problems and sleep-wake reversal generally persist despite antipsychotic treatment.2,3
Slow-wave sleep deficiency can lead to negative symptoms and memory deficits in patients with schizophrenia because4:
- declarative and procedural memory consolidation are associated with slow-wave and stage 2 sleep, respectively
- procedural learning and visual spatial memory are correlated with delta power in slow-wave sleep.3,8
Acute psychosis exacerbations are associated with restless, agitated sleep. Insomnia often is an early warning sign of clinical relapse.5 The etiology of sleep dysfunction in schizophrenia is unknown, but glutamatergic action through N-methyl-d-aspartate receptors, the GABA system,6 and the serotonin system7 have been implicated.
Relapse to alcohol could trigger an exacerbation of Mr. F’s illness; however, he continues to deny alcohol or drug use and we could not identify any evidence of alcohol use at his last visit.
HISTORY: Strange behavior
Mr. F is a first-generation immigrant from Venezuela. He has a general educational development diploma and an associate’s degree. He says he has worked as a dental assistant but lost his job after a driving under the influence charge a year ago. Subsequently, he could not remain employed for long. He lives with his parents.
When Mr. F returns to the clinic 5 months later, he has lost 20 lbs and complains of anxiety and lack of sleep. With stooped posture, slow movements, and a mood-incongruent smile, he admits he ran out of medications and asks for refills, which we provide. He appears somewhat bizarre, wearing a loosely fitting baseball cap that covers his direct field of vision. Mr. F admits that he has been pulling out his hair. His thought process is impoverished and his answers are guarded and evasive. He rejects our recommendation of an antipsychotic; the only medications he is willing to continue are oxcarbazepine and clonazepam.
The authors’ observations
Treatment strategies for sleep disorders in patients with schizophrenia mainly target behavioral aspects of sleep, such as sleep onset and total sleep time, and rarely correct polysomnographic disturbances. Commonly used medications include atypical antipsychotics, benzodiazepines, zolpidem, zopiclone, and antidepressants with sedative properties (Table 1).1 However, new insights on sleep architecture patterns in these individuals have directed focus on other medications. Although antipsychotics, GABAA modulators, and melatonin provide some sleep benefits, none of these agents fully address characteristic sleep disturbances found in patients with schizophrenia.
Recent research has looked at GABAB modulators because of their unique function. GABAB receptors are located on pre-synaptic dopaminergic terminals and inhibit dopamine release and modulate glutamatergic regulation of dopamine. In the glutamate hypofunction model of psychosis, a GABAB agonist would cause disinhibition of glutamate modulation of mesolimbic dopamine and reversal of GABA transmission in the ventral tegmental area.9 Baclofen and γ-hydroxybutyric acid (GHB) currently are the only FDA-approved GABAB receptor agonists. Overall, trials of baclofen have not shown benefit for sleep disturbances in patients with schizophrenia,10,11 perhaps because of the drug’s poor liposolubility and consequent inability to cross the blood-brain barrier. Although hydrophilic like baclofen, GHB, which is also known as sodium oxybate and is FDA-approved for cataplexy due to narcolepsy, might have an advantage because of carrier-mediated transfer across the blood-brain barrier. GHB is thought to act directly as a neurotransmitter but also interacts with dopamine via the GHB receptor and with the GABAB receptor after it is converted to extracellular GABA.
Table 1
Schizophrenia and sleep dysfunction: The effect of psychotropics
| Medication/class | Comments |
|---|---|
| Atypical antipsychotics | In the CATIE study, a large proportion of patients had sleep problems despite antipsychotic treatment Atypicals may improve sleep acutely, but do not normalize it The long-term effects of atypicals on sleep architecture in schizophrenia are unclear; some studies show improved slow-wave sleep but in others slow-wave sleep is reduced |
| GABAA modulators (benzodiazepines, zolpidem, zopiclone) | Decrease sleep latency and nocturnal awakening Do not increase slow-wave sleep and overall sleep quality Decrease slow-wave sleep and REM sleep in rats May impair sleep architecture and cognition |
| Melatonin and modafinil | Melatonin may be useful for improving subjective sleep in patients with schizophrenia, although it does not improve slow-wave sleep parameters Modafinil may enhance cognition |
| GABAB receptor agonists | Few trials in humans but animal studies support a potential therapeutic role Minimal impact on REM sleep Increase slow-wave sleep Human studies with the GABAB agonist GHB show improvement in sleep architecture and subjective sleep |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness; GHB: γ-hydroxybutyric acid; REM: rapid eye movement | |
| Source:Reference 1 | |
OUTCOME: A trip cut short
Mr. F does not return to the clinic as scheduled, but 2 months later the U.S. consulate of a Western European country contacts us because Mr. F had a bottle of oxcarbazepine with our contact information. After Mr. F returns to the United States, he tells us his story.
After his last outpatient visit, Mr. F relapsed on alcohol, became despondent over his weakness, and searched for a way to escape his alcohol cravings. He came up with a plan to relocate to an Islamic Middle Eastern country where alcohol is banned and its use heavily punished. Mr. F bought a one-way airplane ticket through a Western Europe connection and departed 7 days later without notifying his family or psychiatrist.
Mr. F’s flight to Western Europe was uneventful. After landing for a connecting flight, his mood improved, his outlook became hopeful, and his auditory hallucinations changed from derogatory to supportive. However, Mr. F became despondent after being barred from his next flight because he did not have a return ticket. He was stranded in the airport with little money and no extra clothing, only his passport and laptop. He slept in the airport and after 3 days set off into the city. Mr. F navigated subway stations, ate at soup kitchens, and sought shelter in hotel lobbies and churches. One week after Mr. F left the airport, the police detained him for disorganized behavior and refusing to vacate a church. He was transported to a hospital, admitted to the psychiatric unit for catatonia, and stabilized on olanzapine, 20 mg/d.
After 1 week, Mr. F was returned to the United States and hospitalized for further evaluation and treatment. On his first day back, Mr. F’s disorganized process appeared to improve. He was euthymic and reported good sleep, tolerable anxiety, and infrequent derogatory auditory hallucinations that were low in volume. On day 3, Mr. F’s mood deteriorated moderately. He became depressed and again experienced derogatory auditory hallucinations. He was internally preoccupied and showed reduced affect and psychomotor activity. Mr. F was discharged the next day to a state-run respite program with a structured plan for psychiatric follow-up, social services, and sobriety maintenance. He remained on olanzapine, 20 mg/d, because we anticipated he would need an adjustment period after his uncommon journey.
The authors’ observations
Psychotic symptoms occurring during long-distance trips have been well described in psychiatric literature. Westbound travel could exacerbate depression. Emerging mania has been documented in eastbound flights, which could be related to sleep deprivation.12,13 The incidence of psychotic exacerbations is correlated with the number of time zones crossed.12
A change in environment, unfamiliar surroundings, presence of strangers, physical inactivity, and a sense of isolation all contribute to jet lag syndrome. Long-distance air travel also disrupts zeitgebers, environmental cues that induce adjustments in the internal body clock.12,14 The body clock is controlled mainly by the SCN in the hypothalamus, which is primarily regulated by the light/dark cycle via melatonin secretion (Figure).
Endogenous changes in circadian rhythms and melatonin secretion abnormalities are present in the pathophysiological mechanism of several psychiatric disorders, including depression, bipolar disorder, and schizophrenia. Trbovic hypothesized that in essence schizophrenia could be a sleep disorder and SCN dysfunction may contribute to the pathogenesis of schizophrenia.15 Several research findings support this hypothesis (Table 2). Recent evidence suggests that abnormal circadian melatonin metabolism may be directly related to the schizophrenia pathophysiology.16 Because melatonin production is regulated by the SCN and jet lag resets the melatonin cycle, a defective SCN may not respond well to such adjustments.
Mr. F’s symptomatology is illustrative of the jet lag scenario. His auditory hallucinations became “more supportive” and helpful during his eastbound flight, whereas after his return to the United States, depression was the predominant mood symptom. Psychotic exacerbation also was noticeable after his return.
There are no recommended treatments for psychosis related to jet lag. Antipsychotics often are used, although there is no accepted agent of choice. Treatment of jet lag includes addressing sleep loss and desynchronization.17 Medications suggested for treatment of sleep loss are antihistamines (H1 receptor antagonists), benzodiazepines, and imidazopyridines (zolpidem, zopiclone). Light therapy or administration of melatonin, ramelteon, or agomelatine can help jet-lagged patients resynchronize with the environment.
Figure: Pathways for light: Circadian timing system
Photic information reaches the suprachiasmatic nucleus (SCN) through the retinohypothalamic tract (RHT), which uses glutamate (GLU) as a neurotransmitter. A multisynaptic indirect pathway also carries photic information to the SCN. This indirect route arises from the RHT, projects through the intergeniculate leaflet (IGL) of the lateral geniculate nucleus, and finally, the geniculohypothalamic tract (GHT). Neuropeptide Y (NPY) is the neurotransmitter of the GHT. Serotoninergic (5-HT) input to the SCN arrives from the dorsal raphe nuclei. Melatonin, produced in the pineal gland, exerts its effect on circadian timing by feeding back onto the SCN.
Source: Reprinted with permission from reference 14Table 2
Suprachiasmatic nucleus dysfunction may have a role in schizophrenia
| Consequences of SCN dysfunction | Findings relevant to schizophrenia |
|---|---|
| Circadian pattern abnormalities | Individuals with schizophrenia do not have a characteristic circadian pattern of melatonin secretiona Actigraphic studies confirm that patients with schizophrenia have abnormal circadian rhythm activitiesb-d |
| Dopaminergic system abnormalities | The fetal dopaminergic system and D1 dopamine receptors may be involved in the process of synchronizing the SCNe,f |
| Jet lag symptomatology | Jet lag can exacerbate psychiatric disorders,g which suggests that in these patients the SCN is not capable of adjustment |
| Pathologic daytime sleep | Saccadic eye movements in patients with schizophrenia suggest they may be experiencing remnants of REM sleep, supporting the notion that these patients may have dream states during wakefulness |
| REM: rapid eye movement; SCN: suprachiasmatic nucleus | |
| Source: a. Bersani G, Mameli M, Garavini A, et al. Reduction of night/day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Neuro Endocrinol Lett. 2003;24(3-4):181-184. b. Poyurovsky M, Nave R, Epstein R, et al. Actigraphic monitoring (actigraphy) of circadian locomotor activity in schizophrenic patients with acute neuroleptic-induced akathisia. Eur Neuropsychopharmacol. 2000;10(3):171-176. c. Haug HJ, Wirz-Justice A, Rössler W. Actigraphy to measure day structure as a therapeutic variable in the treatment of schizophrenic patients. Acta Psychiatr Scand Suppl. 2000;(407):91-95. d. Martin JL, Jeste DV, Ancoli-Israel S. Older schizophrenia patients have more disrupted sleep and circadian rhythms than age-matched comparison subjects. J Psychiatr Res. 2005;39(3):251-259. e. Strother WN, Norman AB, Lehman MN. D1-dopamine receptor binding and tyrosine hydroxylase-immunoreactivity in the fetal and neonatal hamster suprachiasmatic nucleus. Brain Res Dev Brain Res. 1998;106(1-2):137-144. f. Viswanathan N, Weaver DR, Reppert SM, et al. Entrainment of the fetal hamster circadian pacemaker by prenatal injections of the dopamine agonist SKF 38393. J Neurosci. 1994;14(9):5393-5398. g. Katz G, Durst R, Zislin J, et al. Jet lag causing or exacerbating psychiatric disorders. Harefuah. 2000;138(10):809-812, 912. | |
Related Resources
- Klein DC, Moore R, Reppert SM, eds. Suprachiasmatic nucleus: the mind’s clock. New York, NY: Oxford University Press; 1991.
- Hofstetter JR, Lysaker PH, Mayeda AR. Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry. 2005;5:13.
Drug Brand Names
- Agomelatine • Valdoxan
- Aripiprazole • Abilify
- Baclofen • Lioresal
- Clonazepam • Klonopin
- γ-hydroxybutyric acid, sodium oxybate • Xyrem
- Loxapine • Loxitane
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Propranolol • Inderal
- Ramelteon • Rozerem
- Zolpidem • Ambien
- Zoplicone • Lunesta
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Psychotic and sleepless
Mr. F, age 30, is referred to our psychiatric outpatient clinic for follow-up care after hospitalization to treat a psychotic episode. His psychotic symptoms started 2 years ago without an identifiable trigger. Mr. F complains of episodic mood symptoms, such as depression, irritability, and angry outbursts; persistent auditory hallucinations (voices calling him names); and persecutory delusions. While in the hospital he was diagnosed with psychotic disorder not otherwise specified and started on olanzapine titrated to 30 mg/d.
During evaluation, Mr. F is depressed and exhibits motor retardation, slow speech, bland affect, impaired short-term memory, and auditory hallucinations. He describes social anxiety and has ideas of reference and problems interpreting facial expressions. He is guarded and suspicious. Although auditory hallucinations and depression affect Mr. F’s daily activities, he is attempting to find a job.
Mr. F has used alcohol since age 16 to escape social difficulties. He says he last used alcohol 1 year ago, but refuses to provide details about how much alcohol he typically consumed. Sporadic cannabis use also started when Mr. F was in his teens.
Mr. F’s symptoms improve with olanzapine, but he complains of weight gain and sedation, so we switch him to aripiprazole, 10 mg/d. Two weeks later he reports feeling jittery and anxious, so we discontinue aripiprazole and start loxapine, 25 mg/d at night, and propranolol, 60 mg/d, for residual akathisia. Despite limited clinical improvement, Mr. F irrationally says he wants to join the Navy. After a week, his psychotic symptoms improve but anxiety persists, so we start clonazepam, 1 mg/d, and oxcarbazepine, 600 mg/d. After 2 weeks he says he feels calmer, but has gained 20 lbs and is constantly tired. Against our advice, Mr. F decides to discontinue loxapine and propranolol, but continues clonazepam and oxcarbazepine.
At his next visit 4 weeks later, Mr. F is in good spirits. He says he is looking for a job as a dental assistant, and shows no apparent signs of psychosis. Mr. F misses his next appointment but returns 3 months later with evident deterioration in his general appearance. He says he is having difficulty sleeping and is depressed, stating “I just lay in bed; I don’t want to deal with life.” He is withdrawn and unwilling to elaborate on his personal problems but asks for a refill of clonazepam and oxcarbazepine, which we provide.
The authors’ observations
Sleep disturbances, including poor sleep efficiency, increased sleep-onset latency, decreased rapid eye movement (REM) sleep latency, and decreased stage 4 of non-REM sleep, occur in 16% to 30% of patients with schizophrenia and are associated with reduced quality of life and poor coping skills.1 Sleep-onset and sleep maintenance problems and sleep-wake reversal generally persist despite antipsychotic treatment.2,3
Slow-wave sleep deficiency can lead to negative symptoms and memory deficits in patients with schizophrenia because4:
- declarative and procedural memory consolidation are associated with slow-wave and stage 2 sleep, respectively
- procedural learning and visual spatial memory are correlated with delta power in slow-wave sleep.3,8
Acute psychosis exacerbations are associated with restless, agitated sleep. Insomnia often is an early warning sign of clinical relapse.5 The etiology of sleep dysfunction in schizophrenia is unknown, but glutamatergic action through N-methyl-d-aspartate receptors, the GABA system,6 and the serotonin system7 have been implicated.
Relapse to alcohol could trigger an exacerbation of Mr. F’s illness; however, he continues to deny alcohol or drug use and we could not identify any evidence of alcohol use at his last visit.
HISTORY: Strange behavior
Mr. F is a first-generation immigrant from Venezuela. He has a general educational development diploma and an associate’s degree. He says he has worked as a dental assistant but lost his job after a driving under the influence charge a year ago. Subsequently, he could not remain employed for long. He lives with his parents.
When Mr. F returns to the clinic 5 months later, he has lost 20 lbs and complains of anxiety and lack of sleep. With stooped posture, slow movements, and a mood-incongruent smile, he admits he ran out of medications and asks for refills, which we provide. He appears somewhat bizarre, wearing a loosely fitting baseball cap that covers his direct field of vision. Mr. F admits that he has been pulling out his hair. His thought process is impoverished and his answers are guarded and evasive. He rejects our recommendation of an antipsychotic; the only medications he is willing to continue are oxcarbazepine and clonazepam.
The authors’ observations
Treatment strategies for sleep disorders in patients with schizophrenia mainly target behavioral aspects of sleep, such as sleep onset and total sleep time, and rarely correct polysomnographic disturbances. Commonly used medications include atypical antipsychotics, benzodiazepines, zolpidem, zopiclone, and antidepressants with sedative properties (Table 1).1 However, new insights on sleep architecture patterns in these individuals have directed focus on other medications. Although antipsychotics, GABAA modulators, and melatonin provide some sleep benefits, none of these agents fully address characteristic sleep disturbances found in patients with schizophrenia.
Recent research has looked at GABAB modulators because of their unique function. GABAB receptors are located on pre-synaptic dopaminergic terminals and inhibit dopamine release and modulate glutamatergic regulation of dopamine. In the glutamate hypofunction model of psychosis, a GABAB agonist would cause disinhibition of glutamate modulation of mesolimbic dopamine and reversal of GABA transmission in the ventral tegmental area.9 Baclofen and γ-hydroxybutyric acid (GHB) currently are the only FDA-approved GABAB receptor agonists. Overall, trials of baclofen have not shown benefit for sleep disturbances in patients with schizophrenia,10,11 perhaps because of the drug’s poor liposolubility and consequent inability to cross the blood-brain barrier. Although hydrophilic like baclofen, GHB, which is also known as sodium oxybate and is FDA-approved for cataplexy due to narcolepsy, might have an advantage because of carrier-mediated transfer across the blood-brain barrier. GHB is thought to act directly as a neurotransmitter but also interacts with dopamine via the GHB receptor and with the GABAB receptor after it is converted to extracellular GABA.
Table 1
Schizophrenia and sleep dysfunction: The effect of psychotropics
| Medication/class | Comments |
|---|---|
| Atypical antipsychotics | In the CATIE study, a large proportion of patients had sleep problems despite antipsychotic treatment Atypicals may improve sleep acutely, but do not normalize it The long-term effects of atypicals on sleep architecture in schizophrenia are unclear; some studies show improved slow-wave sleep but in others slow-wave sleep is reduced |
| GABAA modulators (benzodiazepines, zolpidem, zopiclone) | Decrease sleep latency and nocturnal awakening Do not increase slow-wave sleep and overall sleep quality Decrease slow-wave sleep and REM sleep in rats May impair sleep architecture and cognition |
| Melatonin and modafinil | Melatonin may be useful for improving subjective sleep in patients with schizophrenia, although it does not improve slow-wave sleep parameters Modafinil may enhance cognition |
| GABAB receptor agonists | Few trials in humans but animal studies support a potential therapeutic role Minimal impact on REM sleep Increase slow-wave sleep Human studies with the GABAB agonist GHB show improvement in sleep architecture and subjective sleep |
| CATIE: Clinical Antipsychotic Trials of Intervention Effectiveness; GHB: γ-hydroxybutyric acid; REM: rapid eye movement | |
| Source:Reference 1 | |
OUTCOME: A trip cut short
Mr. F does not return to the clinic as scheduled, but 2 months later the U.S. consulate of a Western European country contacts us because Mr. F had a bottle of oxcarbazepine with our contact information. After Mr. F returns to the United States, he tells us his story.
After his last outpatient visit, Mr. F relapsed on alcohol, became despondent over his weakness, and searched for a way to escape his alcohol cravings. He came up with a plan to relocate to an Islamic Middle Eastern country where alcohol is banned and its use heavily punished. Mr. F bought a one-way airplane ticket through a Western Europe connection and departed 7 days later without notifying his family or psychiatrist.
Mr. F’s flight to Western Europe was uneventful. After landing for a connecting flight, his mood improved, his outlook became hopeful, and his auditory hallucinations changed from derogatory to supportive. However, Mr. F became despondent after being barred from his next flight because he did not have a return ticket. He was stranded in the airport with little money and no extra clothing, only his passport and laptop. He slept in the airport and after 3 days set off into the city. Mr. F navigated subway stations, ate at soup kitchens, and sought shelter in hotel lobbies and churches. One week after Mr. F left the airport, the police detained him for disorganized behavior and refusing to vacate a church. He was transported to a hospital, admitted to the psychiatric unit for catatonia, and stabilized on olanzapine, 20 mg/d.
After 1 week, Mr. F was returned to the United States and hospitalized for further evaluation and treatment. On his first day back, Mr. F’s disorganized process appeared to improve. He was euthymic and reported good sleep, tolerable anxiety, and infrequent derogatory auditory hallucinations that were low in volume. On day 3, Mr. F’s mood deteriorated moderately. He became depressed and again experienced derogatory auditory hallucinations. He was internally preoccupied and showed reduced affect and psychomotor activity. Mr. F was discharged the next day to a state-run respite program with a structured plan for psychiatric follow-up, social services, and sobriety maintenance. He remained on olanzapine, 20 mg/d, because we anticipated he would need an adjustment period after his uncommon journey.
The authors’ observations
Psychotic symptoms occurring during long-distance trips have been well described in psychiatric literature. Westbound travel could exacerbate depression. Emerging mania has been documented in eastbound flights, which could be related to sleep deprivation.12,13 The incidence of psychotic exacerbations is correlated with the number of time zones crossed.12
A change in environment, unfamiliar surroundings, presence of strangers, physical inactivity, and a sense of isolation all contribute to jet lag syndrome. Long-distance air travel also disrupts zeitgebers, environmental cues that induce adjustments in the internal body clock.12,14 The body clock is controlled mainly by the SCN in the hypothalamus, which is primarily regulated by the light/dark cycle via melatonin secretion (Figure).
Endogenous changes in circadian rhythms and melatonin secretion abnormalities are present in the pathophysiological mechanism of several psychiatric disorders, including depression, bipolar disorder, and schizophrenia. Trbovic hypothesized that in essence schizophrenia could be a sleep disorder and SCN dysfunction may contribute to the pathogenesis of schizophrenia.15 Several research findings support this hypothesis (Table 2). Recent evidence suggests that abnormal circadian melatonin metabolism may be directly related to the schizophrenia pathophysiology.16 Because melatonin production is regulated by the SCN and jet lag resets the melatonin cycle, a defective SCN may not respond well to such adjustments.
Mr. F’s symptomatology is illustrative of the jet lag scenario. His auditory hallucinations became “more supportive” and helpful during his eastbound flight, whereas after his return to the United States, depression was the predominant mood symptom. Psychotic exacerbation also was noticeable after his return.
There are no recommended treatments for psychosis related to jet lag. Antipsychotics often are used, although there is no accepted agent of choice. Treatment of jet lag includes addressing sleep loss and desynchronization.17 Medications suggested for treatment of sleep loss are antihistamines (H1 receptor antagonists), benzodiazepines, and imidazopyridines (zolpidem, zopiclone). Light therapy or administration of melatonin, ramelteon, or agomelatine can help jet-lagged patients resynchronize with the environment.
Figure: Pathways for light: Circadian timing system
Photic information reaches the suprachiasmatic nucleus (SCN) through the retinohypothalamic tract (RHT), which uses glutamate (GLU) as a neurotransmitter. A multisynaptic indirect pathway also carries photic information to the SCN. This indirect route arises from the RHT, projects through the intergeniculate leaflet (IGL) of the lateral geniculate nucleus, and finally, the geniculohypothalamic tract (GHT). Neuropeptide Y (NPY) is the neurotransmitter of the GHT. Serotoninergic (5-HT) input to the SCN arrives from the dorsal raphe nuclei. Melatonin, produced in the pineal gland, exerts its effect on circadian timing by feeding back onto the SCN.
Source: Reprinted with permission from reference 14Table 2
Suprachiasmatic nucleus dysfunction may have a role in schizophrenia
| Consequences of SCN dysfunction | Findings relevant to schizophrenia |
|---|---|
| Circadian pattern abnormalities | Individuals with schizophrenia do not have a characteristic circadian pattern of melatonin secretiona Actigraphic studies confirm that patients with schizophrenia have abnormal circadian rhythm activitiesb-d |
| Dopaminergic system abnormalities | The fetal dopaminergic system and D1 dopamine receptors may be involved in the process of synchronizing the SCNe,f |
| Jet lag symptomatology | Jet lag can exacerbate psychiatric disorders,g which suggests that in these patients the SCN is not capable of adjustment |
| Pathologic daytime sleep | Saccadic eye movements in patients with schizophrenia suggest they may be experiencing remnants of REM sleep, supporting the notion that these patients may have dream states during wakefulness |
| REM: rapid eye movement; SCN: suprachiasmatic nucleus | |
| Source: a. Bersani G, Mameli M, Garavini A, et al. Reduction of night/day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Neuro Endocrinol Lett. 2003;24(3-4):181-184. b. Poyurovsky M, Nave R, Epstein R, et al. Actigraphic monitoring (actigraphy) of circadian locomotor activity in schizophrenic patients with acute neuroleptic-induced akathisia. Eur Neuropsychopharmacol. 2000;10(3):171-176. c. Haug HJ, Wirz-Justice A, Rössler W. Actigraphy to measure day structure as a therapeutic variable in the treatment of schizophrenic patients. Acta Psychiatr Scand Suppl. 2000;(407):91-95. d. Martin JL, Jeste DV, Ancoli-Israel S. Older schizophrenia patients have more disrupted sleep and circadian rhythms than age-matched comparison subjects. J Psychiatr Res. 2005;39(3):251-259. e. Strother WN, Norman AB, Lehman MN. D1-dopamine receptor binding and tyrosine hydroxylase-immunoreactivity in the fetal and neonatal hamster suprachiasmatic nucleus. Brain Res Dev Brain Res. 1998;106(1-2):137-144. f. Viswanathan N, Weaver DR, Reppert SM, et al. Entrainment of the fetal hamster circadian pacemaker by prenatal injections of the dopamine agonist SKF 38393. J Neurosci. 1994;14(9):5393-5398. g. Katz G, Durst R, Zislin J, et al. Jet lag causing or exacerbating psychiatric disorders. Harefuah. 2000;138(10):809-812, 912. | |
Related Resources
- Klein DC, Moore R, Reppert SM, eds. Suprachiasmatic nucleus: the mind’s clock. New York, NY: Oxford University Press; 1991.
- Hofstetter JR, Lysaker PH, Mayeda AR. Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry. 2005;5:13.
Drug Brand Names
- Agomelatine • Valdoxan
- Aripiprazole • Abilify
- Baclofen • Lioresal
- Clonazepam • Klonopin
- γ-hydroxybutyric acid, sodium oxybate • Xyrem
- Loxapine • Loxitane
- Modafinil • Provigil
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Propranolol • Inderal
- Ramelteon • Rozerem
- Zolpidem • Ambien
- Zoplicone • Lunesta
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kantrowitz J, Citrome L, Javitt D. GABA(B) receptors, schizophrenia and sleep dysfunction: a review of the relationship and its potential clinical and therapeutic implications. CNS Drugs. 2009;23(8):631-669.
2. Poulin J, Daoust AM, Forest G, et al. Sleep architecture and its clinical correlates in first episode and neuroleptic-naïve patients with schizophrenia. Schizophr Res. 2003;62:147-153.
3. Ferrarelli F, Huber R, Peterson MJ. Reduced sleep spindle activity in schizophrenia patients. Am J Psychiatry. 2007;164(3):483-492.
4. Cohrs S. Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs. 2008;22(11):939-962.
5. Haffmans P, Hoencamp E, Knegtering HJ, et al. Sleep disturbance in schizophrenia. Br J Psychiatry. 1994;165(5):697-698.
6. Wisor J, Morairty S, Huynh N, et al. Gene expression in the rat cerebral cortex: comparison of recovery sleep and hypnotic-induced sleep. Neuroscience. 2006;141(1):371-378.
7. Benson KL, Faull KF, Zarcone VP. Evidence for the role of serotonin in the regulation of slow wave sleep in schizophrenia. Sleep. 1991;14(2):133-139.
8. Göder R, Boigs M, Braun S, et al. Impairment of visuospatial memory is associated with decreased slow wave sleep in schizophrenia. J Psychiatr Res. 2004;38:591-599.
9. Harte M, O’Connor WT. Evidence for a selective prefrontal cortical GABA(B) receptor mediated inhibition of glutamate release in the ventral tegmental area: a dual probe microdialysis study in the awake rat. Neuroscience. 2005;130(1):215-222.
10. Garbutt JC, van Kammen DP. The interaction between GABA and dopamine: implications for schizophrenia. Schizophr Bull. 1983;9(3):336-353.
11. Finnimore A, Roebuck M, Sajkov D, et al. The effects of the GABA agonist, baclofen, on sleep and breathing. Eur Respir J. 1995;8(2):230-234.
12. Jahuar P, Weller MP. Psychiatric morbidity and time zone changes: a study of patients from Heathrow airport. Br J Psychiatry. 1982;140:231-234.
13. Katz G, Durst R, Zislin Y, et al. Psychiatric aspects of jet lag: review and hypothesis. Med Hypotheses. 2001;56(1):20-23.
14. Waterhouse J, Reilly T, Atkinson G. Jet-lag. Lancet. 1997;350:1611-1616.
15. Trbovic SM. Schizophrenia as a possible dysfunction of the suprachiasmatic nucleus. Med Hypotheses. 2010;74:127-131.
16. Bersani G, Mameli M, Garavini A, et al. Reduction of night/ day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Nuero Endocrinol Lett. 2003;24(3-4):181-184.
17. Brown GM, Pandi-Perumal SR, Trakht I, et al. Melatonin and its relevance to jet lag. Travel Med Infect Dis. 2009;7:69-81.
1. Kantrowitz J, Citrome L, Javitt D. GABA(B) receptors, schizophrenia and sleep dysfunction: a review of the relationship and its potential clinical and therapeutic implications. CNS Drugs. 2009;23(8):631-669.
2. Poulin J, Daoust AM, Forest G, et al. Sleep architecture and its clinical correlates in first episode and neuroleptic-naïve patients with schizophrenia. Schizophr Res. 2003;62:147-153.
3. Ferrarelli F, Huber R, Peterson MJ. Reduced sleep spindle activity in schizophrenia patients. Am J Psychiatry. 2007;164(3):483-492.
4. Cohrs S. Sleep disturbances in patients with schizophrenia: impact and effect of antipsychotics. CNS Drugs. 2008;22(11):939-962.
5. Haffmans P, Hoencamp E, Knegtering HJ, et al. Sleep disturbance in schizophrenia. Br J Psychiatry. 1994;165(5):697-698.
6. Wisor J, Morairty S, Huynh N, et al. Gene expression in the rat cerebral cortex: comparison of recovery sleep and hypnotic-induced sleep. Neuroscience. 2006;141(1):371-378.
7. Benson KL, Faull KF, Zarcone VP. Evidence for the role of serotonin in the regulation of slow wave sleep in schizophrenia. Sleep. 1991;14(2):133-139.
8. Göder R, Boigs M, Braun S, et al. Impairment of visuospatial memory is associated with decreased slow wave sleep in schizophrenia. J Psychiatr Res. 2004;38:591-599.
9. Harte M, O’Connor WT. Evidence for a selective prefrontal cortical GABA(B) receptor mediated inhibition of glutamate release in the ventral tegmental area: a dual probe microdialysis study in the awake rat. Neuroscience. 2005;130(1):215-222.
10. Garbutt JC, van Kammen DP. The interaction between GABA and dopamine: implications for schizophrenia. Schizophr Bull. 1983;9(3):336-353.
11. Finnimore A, Roebuck M, Sajkov D, et al. The effects of the GABA agonist, baclofen, on sleep and breathing. Eur Respir J. 1995;8(2):230-234.
12. Jahuar P, Weller MP. Psychiatric morbidity and time zone changes: a study of patients from Heathrow airport. Br J Psychiatry. 1982;140:231-234.
13. Katz G, Durst R, Zislin Y, et al. Psychiatric aspects of jet lag: review and hypothesis. Med Hypotheses. 2001;56(1):20-23.
14. Waterhouse J, Reilly T, Atkinson G. Jet-lag. Lancet. 1997;350:1611-1616.
15. Trbovic SM. Schizophrenia as a possible dysfunction of the suprachiasmatic nucleus. Med Hypotheses. 2010;74:127-131.
16. Bersani G, Mameli M, Garavini A, et al. Reduction of night/ day difference in melatonin blood levels as a possible disease-related index in schizophrenia. Nuero Endocrinol Lett. 2003;24(3-4):181-184.
17. Brown GM, Pandi-Perumal SR, Trakht I, et al. Melatonin and its relevance to jet lag. Travel Med Infect Dis. 2009;7:69-81.
Antidepressants in geriatric patients: Reduce the risk of GI bleeding
Mr. M, age 70, presents to the emergency department (ED) complaining of new-onset fatigue, dizziness, and black, tarry stools. He is anemic (hemoglobin 8.9 g/dL) and his stool is positive for occult blood. Mr. M denies having any symptoms until 1 week ago and reports taking his medications as prescribed. An upper endoscopy reveals a gastrointestinal (GI) bleed and his physician stops his antiplatelet medications. Mr. M’s medical history includes hypertension, hyperlipidemia, and placement of a drug-eluding coronary artery stent 9 months ago. Before presenting to the ED, he had been maintained on lisinopril, 20 mg/d, simvastatin, 40 mg/d, aspirin, 325 mg/d, clopidogrel, 75 mg/d, and a daily multivitamin. Three weeks ago, Mr. M was started on citalopram, 20 mg/d, for depressed mood that he has had since his wife died a year ago.
The psychiatry service is consulted after Mr. M admits he has had thoughts of suicide and a few weeks ago was planning to take an overdose of his medications. He denies taking any extra medications and reports feeling more positive since starting citalopram. The psychiatrist discontinues citalopram, however, because of a possible drug interaction with antiplatelet medications, starts Mr. M on bupropion, 150 mg/d, and recommends he follow up with his primary care physician for management of his depressive symptoms.
- Geriatric patients who take multiple medications for various disease states are at increased risk for drug-drug interactions.
- Serotonergic antidepressants inhibit platelet aggregation, which may increase a patient’s risk of bleeding or bruising.
- Closely monitor patients receiving serotonergic antidepressants concomitantly with other medications that may increase bleeding risk.
- Consider prophylactic acid suppressive therapy for patients at high risk for GI bleeding who receive concomitant SSRIs.
Older patients frequently take multiple medications for various disease states, which increases their risk of drug-drug interactions. In addition, physiologic changes associated with aging alter how patients respond to medications. Drugs may interact pharmacokinetically and pharmacodynamically. Pharmacokinetic interactions are well understood and represent changes in absorption, distribution, metabolism, and elimination of specific medications. Pharmacodynamic drug-drug interactions, on the other hand, are less recognized and represent changes in medications’ mechanism of action. A clinician who understands pharmacodynamic interactions will be able to better identify potential drug-drug interactions and could avoid adverse events.1
Antidepressants and bleeding
In Mr. M’s case, a pharmacodynamic drug-drug interaction among citalopram, aspirin, and clopidogrel caused a GI bleed. This type of interaction may be overlooked because of the relatively safe drug-drug interaction profile of selective serotonin reuptake inhibitors (SSRIs). However, any antidepressant that increases serotonin concentration, including serotonin-norepinephrine reuptake inhibitors, may cause this pharmacodynamic interaction.1
Platelets release serotonin to promote aggregation, but do not produce it themselves and are dependent on the serotonin transporter system (reuptake pump) to acquire serotonin. Because SSRIs act on serotonin transporters found on platelet cell membranes, these drugs deplete platelets’ supply of serotonin, leading to diminished platelet aggregation. This effect may propagate the action of other medications that inhibit platelet aggregation, which may increase a patient’s risk of bruising and/or bleeding. This increased risk of bleeding is not associated with non-serotonergic antidepressants such as bupropion, and seems to decrease when SSRIs are discontinued.2
A modest increase in bleeding risk with SSRIs when used alone and with other platelet-inhibiting therapies has been described in case reports, case controlled studies, and chart reviews.2-4 The agents studied include aspirin and clopidogrel, which Mr. M was receiving, but also other, often-overlooked medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, calcium channel blockers, and systemic corticosteroids. Patient factors and diseases—including a history of peptic ulcer disease, previous bleeding, heavy alcohol use, and older age—also may increase bleeding risk (Table).2-5
Serotonin reuptake inhibitor medications have been associated with various bleeding events.5 Most case-control and cohort analyses have examined the risk of GI bleeding with SSRIs; however, serotonergic antidepressants also have been associated with an increased risk of uterine bleeding and perioperative blood loss and transfusions in various surgical procedures.6 Some reports have suggested that there may be a small increase in the incidence of hemorrhagic and fatal stroke with SSRI use5,7; however, many studies have not found an association between SSRI use and increased risk of intracranial hemorrhage stroke.8 The Women’s Health Initiative Study, which reviewed cardiovascular morbidity and mortality data, showed that antidepressant use in postmenopausal women was associated with an increased risk of all-cause mortality, but not coronary heart disease.7 SSRI use was associated with an increased risk of stroke, specifically hemorrhagic stroke, although the absolute event risks were low and cannot be used to predict risk.
Table
Risk factors for gastrointestinal bleeding
| Medications | Corticosteroids, anticoagulants (warfarin), antiplatelets (clopidogrel), NSAIDs (including aspirin), calcium channel blockers, SSRIs, SNRIs, tricyclic antidepressants |
| Disease state/patient factors | Age (elderly are at higher risk), history of ulcer, chronic alcohol use, peptic ulcer disease, esophageal varices, gastric or colorectal cancer, gastritis, liver disease, coagulopathy |
| NSAIDs: nonsteroidal anti-inflammatory drugs; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors | |
| Source: References 2-5 | |
Reducing bleeding risk
In a case-control study, de Abajo et al4 found that patients taking acid-suppressing drugs—proton pump inhibitors and histamine H2 receptor antagonists—had a lower risk of upper GI tract bleeding associated with serotonergic antidepressants compared with those not taking acid-suppressing medications. These drugs further reduced the risk of bleeding in patients taking NSAIDs or antiplatelet medications concomitantly with SSRIs. We suggest initiating prophylactic acid suppression therapy for any patient who is considered at high risk for a GI bleed and is taking an SSRI with or without other medications that inhibit platelet aggregation. Specifically, start with an H2 antagonist because of these medications’ faster onset of action and lower cost vs proton pump inhibitors.
Although the association between SSRIs and bleeding have been described in observational studies, it is impossible to rule out alternate causes and potential confounders that may have contributed to these events. Due diligence and therapeutic drug monitoring of all known and predicted drug-drug interactions is warranted for all patients taking serotonergic antidepressants in combination with medications known to increase bleeding risk.
Related Resources
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
- Hansten PD, Horn JR. The top 100 drug interactions: a guide to patient management. Edmonds, WA: H&H Publications; 2010.
Drug Brand Names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clopidogrel • Plavix
- Lisinopril • Zestril, Prinivil
- Simvastatin • Zocor
- Warfarin • Coumadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
2. Targownik LE, Bolton JM, Metge CJ, et al. Selective serotonin reuptake inhibitors are associated with a modest increase in the risk of upper gastrointestinal bleeding. Am J Gastroenterol. 2009;104:1475-1482.
3. Opatrny L, Delaney JA, Suissa S. Gastro-intestinal haemorrhage risks of selective serotonin receptor antagonist therapy: a new look. Br J Clin Pharmacol. 2008;66(1):76-81.
4. de Abajo FJ, García-Rodríguez LA. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry. 2008;65(7):795-803.
5. Looper KJ. Potential medical and surgical complications of serotonergic antidepressant medications. Psychosomatics. 2007;48:1-9.
6. Gärtner R, Cronin-Fenton D, Hundborg HH, et al. Use of selective serotonin reuptake inhibitors and risk of re-operation due to post-surgical bleeding in breast cancer patients: a Danish population-based cohort study. BMC Surg. 2010;10:3.-
7. Smoller JW, Allison M, Cochrane BB, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative Study. Arch Intern Med. 2009;169(22):2128-2139.
8. Chen Y, Guo JJ, Patel NC. Hemorrhagic stroke associated with antidepressant use in patients with depression: does degree of serotonin reuptake inhibition matter? Pharmacoepidemiol Drug Saf. 2009;18(3):196-202.
Mr. M, age 70, presents to the emergency department (ED) complaining of new-onset fatigue, dizziness, and black, tarry stools. He is anemic (hemoglobin 8.9 g/dL) and his stool is positive for occult blood. Mr. M denies having any symptoms until 1 week ago and reports taking his medications as prescribed. An upper endoscopy reveals a gastrointestinal (GI) bleed and his physician stops his antiplatelet medications. Mr. M’s medical history includes hypertension, hyperlipidemia, and placement of a drug-eluding coronary artery stent 9 months ago. Before presenting to the ED, he had been maintained on lisinopril, 20 mg/d, simvastatin, 40 mg/d, aspirin, 325 mg/d, clopidogrel, 75 mg/d, and a daily multivitamin. Three weeks ago, Mr. M was started on citalopram, 20 mg/d, for depressed mood that he has had since his wife died a year ago.
The psychiatry service is consulted after Mr. M admits he has had thoughts of suicide and a few weeks ago was planning to take an overdose of his medications. He denies taking any extra medications and reports feeling more positive since starting citalopram. The psychiatrist discontinues citalopram, however, because of a possible drug interaction with antiplatelet medications, starts Mr. M on bupropion, 150 mg/d, and recommends he follow up with his primary care physician for management of his depressive symptoms.
- Geriatric patients who take multiple medications for various disease states are at increased risk for drug-drug interactions.
- Serotonergic antidepressants inhibit platelet aggregation, which may increase a patient’s risk of bleeding or bruising.
- Closely monitor patients receiving serotonergic antidepressants concomitantly with other medications that may increase bleeding risk.
- Consider prophylactic acid suppressive therapy for patients at high risk for GI bleeding who receive concomitant SSRIs.
Older patients frequently take multiple medications for various disease states, which increases their risk of drug-drug interactions. In addition, physiologic changes associated with aging alter how patients respond to medications. Drugs may interact pharmacokinetically and pharmacodynamically. Pharmacokinetic interactions are well understood and represent changes in absorption, distribution, metabolism, and elimination of specific medications. Pharmacodynamic drug-drug interactions, on the other hand, are less recognized and represent changes in medications’ mechanism of action. A clinician who understands pharmacodynamic interactions will be able to better identify potential drug-drug interactions and could avoid adverse events.1
Antidepressants and bleeding
In Mr. M’s case, a pharmacodynamic drug-drug interaction among citalopram, aspirin, and clopidogrel caused a GI bleed. This type of interaction may be overlooked because of the relatively safe drug-drug interaction profile of selective serotonin reuptake inhibitors (SSRIs). However, any antidepressant that increases serotonin concentration, including serotonin-norepinephrine reuptake inhibitors, may cause this pharmacodynamic interaction.1
Platelets release serotonin to promote aggregation, but do not produce it themselves and are dependent on the serotonin transporter system (reuptake pump) to acquire serotonin. Because SSRIs act on serotonin transporters found on platelet cell membranes, these drugs deplete platelets’ supply of serotonin, leading to diminished platelet aggregation. This effect may propagate the action of other medications that inhibit platelet aggregation, which may increase a patient’s risk of bruising and/or bleeding. This increased risk of bleeding is not associated with non-serotonergic antidepressants such as bupropion, and seems to decrease when SSRIs are discontinued.2
A modest increase in bleeding risk with SSRIs when used alone and with other platelet-inhibiting therapies has been described in case reports, case controlled studies, and chart reviews.2-4 The agents studied include aspirin and clopidogrel, which Mr. M was receiving, but also other, often-overlooked medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, calcium channel blockers, and systemic corticosteroids. Patient factors and diseases—including a history of peptic ulcer disease, previous bleeding, heavy alcohol use, and older age—also may increase bleeding risk (Table).2-5
Serotonin reuptake inhibitor medications have been associated with various bleeding events.5 Most case-control and cohort analyses have examined the risk of GI bleeding with SSRIs; however, serotonergic antidepressants also have been associated with an increased risk of uterine bleeding and perioperative blood loss and transfusions in various surgical procedures.6 Some reports have suggested that there may be a small increase in the incidence of hemorrhagic and fatal stroke with SSRI use5,7; however, many studies have not found an association between SSRI use and increased risk of intracranial hemorrhage stroke.8 The Women’s Health Initiative Study, which reviewed cardiovascular morbidity and mortality data, showed that antidepressant use in postmenopausal women was associated with an increased risk of all-cause mortality, but not coronary heart disease.7 SSRI use was associated with an increased risk of stroke, specifically hemorrhagic stroke, although the absolute event risks were low and cannot be used to predict risk.
Table
Risk factors for gastrointestinal bleeding
| Medications | Corticosteroids, anticoagulants (warfarin), antiplatelets (clopidogrel), NSAIDs (including aspirin), calcium channel blockers, SSRIs, SNRIs, tricyclic antidepressants |
| Disease state/patient factors | Age (elderly are at higher risk), history of ulcer, chronic alcohol use, peptic ulcer disease, esophageal varices, gastric or colorectal cancer, gastritis, liver disease, coagulopathy |
| NSAIDs: nonsteroidal anti-inflammatory drugs; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors | |
| Source: References 2-5 | |
Reducing bleeding risk
In a case-control study, de Abajo et al4 found that patients taking acid-suppressing drugs—proton pump inhibitors and histamine H2 receptor antagonists—had a lower risk of upper GI tract bleeding associated with serotonergic antidepressants compared with those not taking acid-suppressing medications. These drugs further reduced the risk of bleeding in patients taking NSAIDs or antiplatelet medications concomitantly with SSRIs. We suggest initiating prophylactic acid suppression therapy for any patient who is considered at high risk for a GI bleed and is taking an SSRI with or without other medications that inhibit platelet aggregation. Specifically, start with an H2 antagonist because of these medications’ faster onset of action and lower cost vs proton pump inhibitors.
Although the association between SSRIs and bleeding have been described in observational studies, it is impossible to rule out alternate causes and potential confounders that may have contributed to these events. Due diligence and therapeutic drug monitoring of all known and predicted drug-drug interactions is warranted for all patients taking serotonergic antidepressants in combination with medications known to increase bleeding risk.
Related Resources
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
- Hansten PD, Horn JR. The top 100 drug interactions: a guide to patient management. Edmonds, WA: H&H Publications; 2010.
Drug Brand Names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clopidogrel • Plavix
- Lisinopril • Zestril, Prinivil
- Simvastatin • Zocor
- Warfarin • Coumadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Mr. M, age 70, presents to the emergency department (ED) complaining of new-onset fatigue, dizziness, and black, tarry stools. He is anemic (hemoglobin 8.9 g/dL) and his stool is positive for occult blood. Mr. M denies having any symptoms until 1 week ago and reports taking his medications as prescribed. An upper endoscopy reveals a gastrointestinal (GI) bleed and his physician stops his antiplatelet medications. Mr. M’s medical history includes hypertension, hyperlipidemia, and placement of a drug-eluding coronary artery stent 9 months ago. Before presenting to the ED, he had been maintained on lisinopril, 20 mg/d, simvastatin, 40 mg/d, aspirin, 325 mg/d, clopidogrel, 75 mg/d, and a daily multivitamin. Three weeks ago, Mr. M was started on citalopram, 20 mg/d, for depressed mood that he has had since his wife died a year ago.
The psychiatry service is consulted after Mr. M admits he has had thoughts of suicide and a few weeks ago was planning to take an overdose of his medications. He denies taking any extra medications and reports feeling more positive since starting citalopram. The psychiatrist discontinues citalopram, however, because of a possible drug interaction with antiplatelet medications, starts Mr. M on bupropion, 150 mg/d, and recommends he follow up with his primary care physician for management of his depressive symptoms.
- Geriatric patients who take multiple medications for various disease states are at increased risk for drug-drug interactions.
- Serotonergic antidepressants inhibit platelet aggregation, which may increase a patient’s risk of bleeding or bruising.
- Closely monitor patients receiving serotonergic antidepressants concomitantly with other medications that may increase bleeding risk.
- Consider prophylactic acid suppressive therapy for patients at high risk for GI bleeding who receive concomitant SSRIs.
Older patients frequently take multiple medications for various disease states, which increases their risk of drug-drug interactions. In addition, physiologic changes associated with aging alter how patients respond to medications. Drugs may interact pharmacokinetically and pharmacodynamically. Pharmacokinetic interactions are well understood and represent changes in absorption, distribution, metabolism, and elimination of specific medications. Pharmacodynamic drug-drug interactions, on the other hand, are less recognized and represent changes in medications’ mechanism of action. A clinician who understands pharmacodynamic interactions will be able to better identify potential drug-drug interactions and could avoid adverse events.1
Antidepressants and bleeding
In Mr. M’s case, a pharmacodynamic drug-drug interaction among citalopram, aspirin, and clopidogrel caused a GI bleed. This type of interaction may be overlooked because of the relatively safe drug-drug interaction profile of selective serotonin reuptake inhibitors (SSRIs). However, any antidepressant that increases serotonin concentration, including serotonin-norepinephrine reuptake inhibitors, may cause this pharmacodynamic interaction.1
Platelets release serotonin to promote aggregation, but do not produce it themselves and are dependent on the serotonin transporter system (reuptake pump) to acquire serotonin. Because SSRIs act on serotonin transporters found on platelet cell membranes, these drugs deplete platelets’ supply of serotonin, leading to diminished platelet aggregation. This effect may propagate the action of other medications that inhibit platelet aggregation, which may increase a patient’s risk of bruising and/or bleeding. This increased risk of bleeding is not associated with non-serotonergic antidepressants such as bupropion, and seems to decrease when SSRIs are discontinued.2
A modest increase in bleeding risk with SSRIs when used alone and with other platelet-inhibiting therapies has been described in case reports, case controlled studies, and chart reviews.2-4 The agents studied include aspirin and clopidogrel, which Mr. M was receiving, but also other, often-overlooked medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2 inhibitors, calcium channel blockers, and systemic corticosteroids. Patient factors and diseases—including a history of peptic ulcer disease, previous bleeding, heavy alcohol use, and older age—also may increase bleeding risk (Table).2-5
Serotonin reuptake inhibitor medications have been associated with various bleeding events.5 Most case-control and cohort analyses have examined the risk of GI bleeding with SSRIs; however, serotonergic antidepressants also have been associated with an increased risk of uterine bleeding and perioperative blood loss and transfusions in various surgical procedures.6 Some reports have suggested that there may be a small increase in the incidence of hemorrhagic and fatal stroke with SSRI use5,7; however, many studies have not found an association between SSRI use and increased risk of intracranial hemorrhage stroke.8 The Women’s Health Initiative Study, which reviewed cardiovascular morbidity and mortality data, showed that antidepressant use in postmenopausal women was associated with an increased risk of all-cause mortality, but not coronary heart disease.7 SSRI use was associated with an increased risk of stroke, specifically hemorrhagic stroke, although the absolute event risks were low and cannot be used to predict risk.
Table
Risk factors for gastrointestinal bleeding
| Medications | Corticosteroids, anticoagulants (warfarin), antiplatelets (clopidogrel), NSAIDs (including aspirin), calcium channel blockers, SSRIs, SNRIs, tricyclic antidepressants |
| Disease state/patient factors | Age (elderly are at higher risk), history of ulcer, chronic alcohol use, peptic ulcer disease, esophageal varices, gastric or colorectal cancer, gastritis, liver disease, coagulopathy |
| NSAIDs: nonsteroidal anti-inflammatory drugs; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors | |
| Source: References 2-5 | |
Reducing bleeding risk
In a case-control study, de Abajo et al4 found that patients taking acid-suppressing drugs—proton pump inhibitors and histamine H2 receptor antagonists—had a lower risk of upper GI tract bleeding associated with serotonergic antidepressants compared with those not taking acid-suppressing medications. These drugs further reduced the risk of bleeding in patients taking NSAIDs or antiplatelet medications concomitantly with SSRIs. We suggest initiating prophylactic acid suppression therapy for any patient who is considered at high risk for a GI bleed and is taking an SSRI with or without other medications that inhibit platelet aggregation. Specifically, start with an H2 antagonist because of these medications’ faster onset of action and lower cost vs proton pump inhibitors.
Although the association between SSRIs and bleeding have been described in observational studies, it is impossible to rule out alternate causes and potential confounders that may have contributed to these events. Due diligence and therapeutic drug monitoring of all known and predicted drug-drug interactions is warranted for all patients taking serotonergic antidepressants in combination with medications known to increase bleeding risk.
Related Resources
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
- Hansten PD, Horn JR. The top 100 drug interactions: a guide to patient management. Edmonds, WA: H&H Publications; 2010.
Drug Brand Names
- Bupropion • Wellbutrin
- Citalopram • Celexa
- Clopidogrel • Plavix
- Lisinopril • Zestril, Prinivil
- Simvastatin • Zocor
- Warfarin • Coumadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
2. Targownik LE, Bolton JM, Metge CJ, et al. Selective serotonin reuptake inhibitors are associated with a modest increase in the risk of upper gastrointestinal bleeding. Am J Gastroenterol. 2009;104:1475-1482.
3. Opatrny L, Delaney JA, Suissa S. Gastro-intestinal haemorrhage risks of selective serotonin receptor antagonist therapy: a new look. Br J Clin Pharmacol. 2008;66(1):76-81.
4. de Abajo FJ, García-Rodríguez LA. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry. 2008;65(7):795-803.
5. Looper KJ. Potential medical and surgical complications of serotonergic antidepressant medications. Psychosomatics. 2007;48:1-9.
6. Gärtner R, Cronin-Fenton D, Hundborg HH, et al. Use of selective serotonin reuptake inhibitors and risk of re-operation due to post-surgical bleeding in breast cancer patients: a Danish population-based cohort study. BMC Surg. 2010;10:3.-
7. Smoller JW, Allison M, Cochrane BB, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative Study. Arch Intern Med. 2009;169(22):2128-2139.
8. Chen Y, Guo JJ, Patel NC. Hemorrhagic stroke associated with antidepressant use in patients with depression: does degree of serotonin reuptake inhibition matter? Pharmacoepidemiol Drug Saf. 2009;18(3):196-202.
1. Kutscher EC, Alexander B. A review of drug interactions with psychiatric medicines for the pharmacy practitioner. J Pharm Pract. 2007;20(4):327-333.
2. Targownik LE, Bolton JM, Metge CJ, et al. Selective serotonin reuptake inhibitors are associated with a modest increase in the risk of upper gastrointestinal bleeding. Am J Gastroenterol. 2009;104:1475-1482.
3. Opatrny L, Delaney JA, Suissa S. Gastro-intestinal haemorrhage risks of selective serotonin receptor antagonist therapy: a new look. Br J Clin Pharmacol. 2008;66(1):76-81.
4. de Abajo FJ, García-Rodríguez LA. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry. 2008;65(7):795-803.
5. Looper KJ. Potential medical and surgical complications of serotonergic antidepressant medications. Psychosomatics. 2007;48:1-9.
6. Gärtner R, Cronin-Fenton D, Hundborg HH, et al. Use of selective serotonin reuptake inhibitors and risk of re-operation due to post-surgical bleeding in breast cancer patients: a Danish population-based cohort study. BMC Surg. 2010;10:3.-
7. Smoller JW, Allison M, Cochrane BB, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative Study. Arch Intern Med. 2009;169(22):2128-2139.
8. Chen Y, Guo JJ, Patel NC. Hemorrhagic stroke associated with antidepressant use in patients with depression: does degree of serotonin reuptake inhibition matter? Pharmacoepidemiol Drug Saf. 2009;18(3):196-202.
Gasping for relief
CASE: Food issues
Ms. A, age 62, has a 40-year history of paranoid schizophrenia, which has been well controlled with olanzapine, 20 mg/d, for many years. Two weeks ago, she stops taking her medication and is brought to a state-run psychiatric hospital by law enforcement officers because of worsening paranoia and hostility. She is disheveled, intermittently denudative, and confused. Ms. A has type II diabetes, gastroesophageal reflux disease, obesity (body mass index of 34.75 kg/m2), and poor dentition. She has no history of substance abuse.
During the first 2 days in the hospital Ms. A refuses to eat, stating that the food is “poisoned,” but accepts 1 oral dose of aripiprazole, 25 mg. On hospital day 3, Ms. A is less hostile and eats dinner with the other patients. A few minutes after beginning her meal, Ms. A abruptly stands up and puts her hands to her throat. She looks frightened, and cannot speak.
A staff member asks Ms. A if she is choking and she nods. Because the psychiatric hospital does not have an emergency room, the staff call 911, and a staff member gives Ms. A back blows, but no food is forced out. Next, nursing staff start abdominal thrusts (Heimlich maneuver) without success. Ms. A then loses consciousness and the staff lowers her to the ground. The nurse looks in Ms. A’s mouth, but can’t see what is blocking her throat. Attempts to provide rescue breathing are unproductive because a foreign body obstructs Ms. A’s airway. A staff member continues abdominal thrusts once Ms. A is on the ground. She has no pulse, and CPR is initiated.
Emergency medical technicians arrive within 7 minutes and suction a piece of hot dog from Ms. A’s trachea. She is then taken to a nearby emergency department, where neurologic examination reveals signs of brain death.
Ms. A dies a few days later. The cause of death is respiratory and cardiac failure secondary to choking and foreign body obstruction. A review of Ms. A’s history reveals she had past episodes of choking and a habit of rapidly ingesting large amounts of food (tachyphagia).
The authors’ observations
The term “café coronary” describes sudden unexpected death caused by airway obstruction by food.1 In 1975, Henry Heimlich described the abdominal thrusting maneuver recommended to prevent these fatalities.2 For more than a century, choking has been recognized as a cause of death in individuals with severe mental illness.3 An analysis of sudden deaths among psychiatric in-patients in Ireland found that choking accounted for 10% of deaths over 10 years.4 An Australian study reported that individuals with schizophrenia had 20-fold greater risk of death by choking than the general population.5 Another study found the mortality rate attributable to choking was 8-fold higher for psychiatric inpatients than the general population,6 and a study in the United States reported that for every 1,000 deaths among psychiatric inpatients, 0.6 were caused by asphyxia,7 which is 100 times greater than the general population reported in the same time.8
Physiological mechanisms associated with impaired swallowing include:
- dopamine blockade, which could produce central and peripheral impairment of swallowing9
- anticholinergic effect leading to impaired esophageal motility
- impaired gag reflex.10
Multiple factors increase mentally ill individuals’ risk of death by choking (Table 1).11 Patients with schizophrenia may exhibit impaired swallowing mechanism, irrespective of psychotropic medications.12 Schizophrenia patients also could exhibit pica behavior—persistent and culturally and developmentally inappropriate ingestion of non-nutritive substances. Examples of pica behavior include ingesting rolled can lids13 and coins14,15 and coprophagia.16 Pica behavior increases the risk for choking, and has been implicated in deaths of individuals with schizophrenia.17
Medications with dopamine blocking and anticholinergic effects may increase choking risk.18 These medications could produce extrapyramidal side effects and parkinsonism, which might impair swallowing. Psychotropic medications could increase appetite and food craving, which in turn may lead to overeating and tachyphagia. In addition, many individuals suffering from severe mental illness have poor dentition, which could make chewing food difficult.19 Psychiatric patients are more likely to be obese, which also increases the risk of choking.
Table 1
Risk factors for choking in mentally ill patients
| Age (>60) |
| Impaired swallowing (schizophrenia patients are at greater risk) |
| Parkinsonism |
| Poor dentition |
| Schizophrenia |
| Tachyphagia (rapid eating) |
| Tardive dyskinesia |
| Obesity |
| Source: Reference 11 |
OUTCOME: Prevention strategies
New Hampshire Hospital’s administration implemented a plan to increase the staff’s awareness of choking risks in mentally ill patients. Nurses complete nutrition screens along with the initial nursing database assessment on all patients during the admission process, and are encouraged to contact registered dieticians for a nutrition review and assessment if a psychiatric patient is thought to be at risk for choking. Registered dieticians work with nursing staff to promptly complete nutrition assessments and address eating-related problems.
Direct care staff were reminded that all inpatient units have a battery-powered, portable compact suction unit available that can be used in a choking emergency. The hospital’s cardiopulmonary resuscitation instructors emphasize the importance of the abdominal thrust maneuver during all staff training sessions.
The hospital’s administration and staff did not reach a consensus on whether physicians should attempt a tracheotomy when other measures to dislodge a foreign object from a patient’s throat fail. Instead, the focus remains on assessing and treating the clinical emergency and obtaining rapid intervention by emergency medical technicians.
The authors’ observations
The following recommendations may help minimize or prevent choking events in inpatient units:
- Ensure all staff who care for patients are trained regularly on emergency first aid for choking victims, including proper use of abdominal thrusts (Heimlich maneuver) (Table 2).20
- Educate staff about which patients may be at higher risk for choking.
- Assess for a history of choking incidents and/or the presence of swallowing problems in patients at risk for choking.
- Supervise meals and instruct staff to look for patients who display dysphagia.
- Consider ordering a swallowing evaluation performed by a speech therapist in patients who manifest dysphagia.
- Avoid polypharmacy of drugs with anticholinergic and/or potent dopamine blocking effects, such as olanzapine, risperidone, or haloperidol.
- Teach safe eating habits to patients who are at risk for choking.
- Contact outpatient care providers of patients at risk for choking and inform them of the need for further education on safe eating habits, a dietary evaluation, and/or a swallowing evaluation.
Implementing these measures may reduce choking incidents and could save lives.
Table 2
American Red Cross guidelines for treating a conscious, choking adult
| Send someone to call 911 |
| Lean person forward and give 5 back blows with heel of your hand |
| Give 5 quick abdominal thrusts by placing the thumbside of your fist against the middle of the victim’s abdomen, just above the navel. Grab your fist with the other hand. In obese or pregnant adults, place your fist in the middle of the breastbone |
| Continue giving 5 back blows and 5 abdominal thrusts until the object is forced out or the person breathes or coughs on his or her own |
| Source: Reference 20 |
Related Resources
- Hwang SJ, Tsai SJ, Chen IJ, et al. Choking incidents among psychiatric inpatients: a retrospective study in Chutung Veterans General Hospital. J Chin Med Assoc. 2010;73(8):419-424.
- American College of Emergency Physicians Foundation. What to do in a medical emergency. Choking. www.emergencycareforyou.org/EmergencyManual/WhatToDoInMedicalEmergency/Default.aspx?id=224.
Drug Brand Names
- Aripiprazole • Abilify
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosures
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Folks is a consultant and speaker for Pfizer Inc., a speaker for Forest Pharmaceuticals, and has received a research grant from Janssen Pharmaceuticals.
1. Haugen RK. The café coronary: sudden deaths in restaurants. JAMA. 1963;186:142-143.
2. Heimlich HJ. A life-saving maneuver to prevent food-choking. JAMA. 1975;234:398-401.
3. Hammond WA. A treatise on insanity and its medical relations. New York, NY: D. Appleton and Company; 1883:724.
4. Corcoran E, Walsh D. Obstructive asphyxia: a cause of excess mortality in psychiatric patients. Ir J Psychol Med. 2003;20:88-90.
5. Ruschena D, Mullen PE, Palmer S, et al. Choking deaths: the role of antipsychotic medication. Br J Psychiatry. 2003;183:446-450.
6. Yim PHW, Chong CSY. Choking in psychiatric patients: associations and outcomes. Hong Kong Journal of Psychiatry. 2009;19:145-149.
7. Craig TJ. Medication use and deaths attributed to asphyxia among psychiatric patients. Am J Psychiatry. 1980;137:1366-1373.
8. Mittleman RE, Wetli CV. The fatal café coronary. Foreign-body airway obstruction. JAMA. 1982;247:1285-1288.
9. Bieger D, Giles SA, Hockman CH. Dopaminergic influences on swallowing. Neuropharmacology. 1977;16:243-252.
10. Bettarello A, Tuttle SG, Grossman MI. Effects of autonomic drugs on gastroesophageal reflux. Gastroenterology. 1960;39:340-346.
11. Fioritti A, Giaccotto L, Melega V. Choking incidents among psychiatric patients: retrospective analysis of thirty-one cases from the west Bologna psychiatric wards. Can J Psychiatry. 1997;42:515-520.
12. Hussar AE, Bragg DG. The effect of chlorpromazine on the swallowing function in schizophrenic patients. Am J Psychiatry. 1969;126:570-573.
13. Abraham B, Alao AO. An unusual body ingestion in a schizophrenic patient: case report. Int J Psychiatry Med. 2005;35(3):313-318.
14. Beecroft N, Bach L, Tunstall N, et al. An unusual case of pica. Int J Geriatr Psychiatry. 1998;13(9):638-641.
15. Pawa S, Khalifa AJ, Ehrinpreis MN, et al. Zinc toxicity from massive and prolonged coin ingestion in an adult. Am J Med Sci. 2008;336(5):430-433.
16. Beck DA, Frohberg NR. Coprophagia in an elderly man: a case report and review of the literature. Int J Psychiatry Med. 2005;35(4):417-427.
17. Dumaguing NI, Singh I, Sethi M, et al. Pica in the geriatric mentally ill: unrelenting and potentially fatal. J Geriatr Psychiatry Neurol. 2003;16(3):189-191.
18. Bazemore H, Tonkonogy J, Ananth R. Dysphagia in psychiatric patients: clinical videofluoroscopic study. Dysphagia. 1991;6:62-65.
19. von Brauchitsch H, May W. Deaths from aspiration and asphyxiation in a mental hospital. Arch Gen Psych. 1968;18:129-136.
20. American Red Cross. Treatment for a conscious choking adult. Available at: http://www.redcross.org/flash/brr/English-html/conscious-choking.asp. Accessed August 27, 2010.
CASE: Food issues
Ms. A, age 62, has a 40-year history of paranoid schizophrenia, which has been well controlled with olanzapine, 20 mg/d, for many years. Two weeks ago, she stops taking her medication and is brought to a state-run psychiatric hospital by law enforcement officers because of worsening paranoia and hostility. She is disheveled, intermittently denudative, and confused. Ms. A has type II diabetes, gastroesophageal reflux disease, obesity (body mass index of 34.75 kg/m2), and poor dentition. She has no history of substance abuse.
During the first 2 days in the hospital Ms. A refuses to eat, stating that the food is “poisoned,” but accepts 1 oral dose of aripiprazole, 25 mg. On hospital day 3, Ms. A is less hostile and eats dinner with the other patients. A few minutes after beginning her meal, Ms. A abruptly stands up and puts her hands to her throat. She looks frightened, and cannot speak.
A staff member asks Ms. A if she is choking and she nods. Because the psychiatric hospital does not have an emergency room, the staff call 911, and a staff member gives Ms. A back blows, but no food is forced out. Next, nursing staff start abdominal thrusts (Heimlich maneuver) without success. Ms. A then loses consciousness and the staff lowers her to the ground. The nurse looks in Ms. A’s mouth, but can’t see what is blocking her throat. Attempts to provide rescue breathing are unproductive because a foreign body obstructs Ms. A’s airway. A staff member continues abdominal thrusts once Ms. A is on the ground. She has no pulse, and CPR is initiated.
Emergency medical technicians arrive within 7 minutes and suction a piece of hot dog from Ms. A’s trachea. She is then taken to a nearby emergency department, where neurologic examination reveals signs of brain death.
Ms. A dies a few days later. The cause of death is respiratory and cardiac failure secondary to choking and foreign body obstruction. A review of Ms. A’s history reveals she had past episodes of choking and a habit of rapidly ingesting large amounts of food (tachyphagia).
The authors’ observations
The term “café coronary” describes sudden unexpected death caused by airway obstruction by food.1 In 1975, Henry Heimlich described the abdominal thrusting maneuver recommended to prevent these fatalities.2 For more than a century, choking has been recognized as a cause of death in individuals with severe mental illness.3 An analysis of sudden deaths among psychiatric in-patients in Ireland found that choking accounted for 10% of deaths over 10 years.4 An Australian study reported that individuals with schizophrenia had 20-fold greater risk of death by choking than the general population.5 Another study found the mortality rate attributable to choking was 8-fold higher for psychiatric inpatients than the general population,6 and a study in the United States reported that for every 1,000 deaths among psychiatric inpatients, 0.6 were caused by asphyxia,7 which is 100 times greater than the general population reported in the same time.8
Physiological mechanisms associated with impaired swallowing include:
- dopamine blockade, which could produce central and peripheral impairment of swallowing9
- anticholinergic effect leading to impaired esophageal motility
- impaired gag reflex.10
Multiple factors increase mentally ill individuals’ risk of death by choking (Table 1).11 Patients with schizophrenia may exhibit impaired swallowing mechanism, irrespective of psychotropic medications.12 Schizophrenia patients also could exhibit pica behavior—persistent and culturally and developmentally inappropriate ingestion of non-nutritive substances. Examples of pica behavior include ingesting rolled can lids13 and coins14,15 and coprophagia.16 Pica behavior increases the risk for choking, and has been implicated in deaths of individuals with schizophrenia.17
Medications with dopamine blocking and anticholinergic effects may increase choking risk.18 These medications could produce extrapyramidal side effects and parkinsonism, which might impair swallowing. Psychotropic medications could increase appetite and food craving, which in turn may lead to overeating and tachyphagia. In addition, many individuals suffering from severe mental illness have poor dentition, which could make chewing food difficult.19 Psychiatric patients are more likely to be obese, which also increases the risk of choking.
Table 1
Risk factors for choking in mentally ill patients
| Age (>60) |
| Impaired swallowing (schizophrenia patients are at greater risk) |
| Parkinsonism |
| Poor dentition |
| Schizophrenia |
| Tachyphagia (rapid eating) |
| Tardive dyskinesia |
| Obesity |
| Source: Reference 11 |
OUTCOME: Prevention strategies
New Hampshire Hospital’s administration implemented a plan to increase the staff’s awareness of choking risks in mentally ill patients. Nurses complete nutrition screens along with the initial nursing database assessment on all patients during the admission process, and are encouraged to contact registered dieticians for a nutrition review and assessment if a psychiatric patient is thought to be at risk for choking. Registered dieticians work with nursing staff to promptly complete nutrition assessments and address eating-related problems.
Direct care staff were reminded that all inpatient units have a battery-powered, portable compact suction unit available that can be used in a choking emergency. The hospital’s cardiopulmonary resuscitation instructors emphasize the importance of the abdominal thrust maneuver during all staff training sessions.
The hospital’s administration and staff did not reach a consensus on whether physicians should attempt a tracheotomy when other measures to dislodge a foreign object from a patient’s throat fail. Instead, the focus remains on assessing and treating the clinical emergency and obtaining rapid intervention by emergency medical technicians.
The authors’ observations
The following recommendations may help minimize or prevent choking events in inpatient units:
- Ensure all staff who care for patients are trained regularly on emergency first aid for choking victims, including proper use of abdominal thrusts (Heimlich maneuver) (Table 2).20
- Educate staff about which patients may be at higher risk for choking.
- Assess for a history of choking incidents and/or the presence of swallowing problems in patients at risk for choking.
- Supervise meals and instruct staff to look for patients who display dysphagia.
- Consider ordering a swallowing evaluation performed by a speech therapist in patients who manifest dysphagia.
- Avoid polypharmacy of drugs with anticholinergic and/or potent dopamine blocking effects, such as olanzapine, risperidone, or haloperidol.
- Teach safe eating habits to patients who are at risk for choking.
- Contact outpatient care providers of patients at risk for choking and inform them of the need for further education on safe eating habits, a dietary evaluation, and/or a swallowing evaluation.
Implementing these measures may reduce choking incidents and could save lives.
Table 2
American Red Cross guidelines for treating a conscious, choking adult
| Send someone to call 911 |
| Lean person forward and give 5 back blows with heel of your hand |
| Give 5 quick abdominal thrusts by placing the thumbside of your fist against the middle of the victim’s abdomen, just above the navel. Grab your fist with the other hand. In obese or pregnant adults, place your fist in the middle of the breastbone |
| Continue giving 5 back blows and 5 abdominal thrusts until the object is forced out or the person breathes or coughs on his or her own |
| Source: Reference 20 |
Related Resources
- Hwang SJ, Tsai SJ, Chen IJ, et al. Choking incidents among psychiatric inpatients: a retrospective study in Chutung Veterans General Hospital. J Chin Med Assoc. 2010;73(8):419-424.
- American College of Emergency Physicians Foundation. What to do in a medical emergency. Choking. www.emergencycareforyou.org/EmergencyManual/WhatToDoInMedicalEmergency/Default.aspx?id=224.
Drug Brand Names
- Aripiprazole • Abilify
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosures
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Folks is a consultant and speaker for Pfizer Inc., a speaker for Forest Pharmaceuticals, and has received a research grant from Janssen Pharmaceuticals.
CASE: Food issues
Ms. A, age 62, has a 40-year history of paranoid schizophrenia, which has been well controlled with olanzapine, 20 mg/d, for many years. Two weeks ago, she stops taking her medication and is brought to a state-run psychiatric hospital by law enforcement officers because of worsening paranoia and hostility. She is disheveled, intermittently denudative, and confused. Ms. A has type II diabetes, gastroesophageal reflux disease, obesity (body mass index of 34.75 kg/m2), and poor dentition. She has no history of substance abuse.
During the first 2 days in the hospital Ms. A refuses to eat, stating that the food is “poisoned,” but accepts 1 oral dose of aripiprazole, 25 mg. On hospital day 3, Ms. A is less hostile and eats dinner with the other patients. A few minutes after beginning her meal, Ms. A abruptly stands up and puts her hands to her throat. She looks frightened, and cannot speak.
A staff member asks Ms. A if she is choking and she nods. Because the psychiatric hospital does not have an emergency room, the staff call 911, and a staff member gives Ms. A back blows, but no food is forced out. Next, nursing staff start abdominal thrusts (Heimlich maneuver) without success. Ms. A then loses consciousness and the staff lowers her to the ground. The nurse looks in Ms. A’s mouth, but can’t see what is blocking her throat. Attempts to provide rescue breathing are unproductive because a foreign body obstructs Ms. A’s airway. A staff member continues abdominal thrusts once Ms. A is on the ground. She has no pulse, and CPR is initiated.
Emergency medical technicians arrive within 7 minutes and suction a piece of hot dog from Ms. A’s trachea. She is then taken to a nearby emergency department, where neurologic examination reveals signs of brain death.
Ms. A dies a few days later. The cause of death is respiratory and cardiac failure secondary to choking and foreign body obstruction. A review of Ms. A’s history reveals she had past episodes of choking and a habit of rapidly ingesting large amounts of food (tachyphagia).
The authors’ observations
The term “café coronary” describes sudden unexpected death caused by airway obstruction by food.1 In 1975, Henry Heimlich described the abdominal thrusting maneuver recommended to prevent these fatalities.2 For more than a century, choking has been recognized as a cause of death in individuals with severe mental illness.3 An analysis of sudden deaths among psychiatric in-patients in Ireland found that choking accounted for 10% of deaths over 10 years.4 An Australian study reported that individuals with schizophrenia had 20-fold greater risk of death by choking than the general population.5 Another study found the mortality rate attributable to choking was 8-fold higher for psychiatric inpatients than the general population,6 and a study in the United States reported that for every 1,000 deaths among psychiatric inpatients, 0.6 were caused by asphyxia,7 which is 100 times greater than the general population reported in the same time.8
Physiological mechanisms associated with impaired swallowing include:
- dopamine blockade, which could produce central and peripheral impairment of swallowing9
- anticholinergic effect leading to impaired esophageal motility
- impaired gag reflex.10
Multiple factors increase mentally ill individuals’ risk of death by choking (Table 1).11 Patients with schizophrenia may exhibit impaired swallowing mechanism, irrespective of psychotropic medications.12 Schizophrenia patients also could exhibit pica behavior—persistent and culturally and developmentally inappropriate ingestion of non-nutritive substances. Examples of pica behavior include ingesting rolled can lids13 and coins14,15 and coprophagia.16 Pica behavior increases the risk for choking, and has been implicated in deaths of individuals with schizophrenia.17
Medications with dopamine blocking and anticholinergic effects may increase choking risk.18 These medications could produce extrapyramidal side effects and parkinsonism, which might impair swallowing. Psychotropic medications could increase appetite and food craving, which in turn may lead to overeating and tachyphagia. In addition, many individuals suffering from severe mental illness have poor dentition, which could make chewing food difficult.19 Psychiatric patients are more likely to be obese, which also increases the risk of choking.
Table 1
Risk factors for choking in mentally ill patients
| Age (>60) |
| Impaired swallowing (schizophrenia patients are at greater risk) |
| Parkinsonism |
| Poor dentition |
| Schizophrenia |
| Tachyphagia (rapid eating) |
| Tardive dyskinesia |
| Obesity |
| Source: Reference 11 |
OUTCOME: Prevention strategies
New Hampshire Hospital’s administration implemented a plan to increase the staff’s awareness of choking risks in mentally ill patients. Nurses complete nutrition screens along with the initial nursing database assessment on all patients during the admission process, and are encouraged to contact registered dieticians for a nutrition review and assessment if a psychiatric patient is thought to be at risk for choking. Registered dieticians work with nursing staff to promptly complete nutrition assessments and address eating-related problems.
Direct care staff were reminded that all inpatient units have a battery-powered, portable compact suction unit available that can be used in a choking emergency. The hospital’s cardiopulmonary resuscitation instructors emphasize the importance of the abdominal thrust maneuver during all staff training sessions.
The hospital’s administration and staff did not reach a consensus on whether physicians should attempt a tracheotomy when other measures to dislodge a foreign object from a patient’s throat fail. Instead, the focus remains on assessing and treating the clinical emergency and obtaining rapid intervention by emergency medical technicians.
The authors’ observations
The following recommendations may help minimize or prevent choking events in inpatient units:
- Ensure all staff who care for patients are trained regularly on emergency first aid for choking victims, including proper use of abdominal thrusts (Heimlich maneuver) (Table 2).20
- Educate staff about which patients may be at higher risk for choking.
- Assess for a history of choking incidents and/or the presence of swallowing problems in patients at risk for choking.
- Supervise meals and instruct staff to look for patients who display dysphagia.
- Consider ordering a swallowing evaluation performed by a speech therapist in patients who manifest dysphagia.
- Avoid polypharmacy of drugs with anticholinergic and/or potent dopamine blocking effects, such as olanzapine, risperidone, or haloperidol.
- Teach safe eating habits to patients who are at risk for choking.
- Contact outpatient care providers of patients at risk for choking and inform them of the need for further education on safe eating habits, a dietary evaluation, and/or a swallowing evaluation.
Implementing these measures may reduce choking incidents and could save lives.
Table 2
American Red Cross guidelines for treating a conscious, choking adult
| Send someone to call 911 |
| Lean person forward and give 5 back blows with heel of your hand |
| Give 5 quick abdominal thrusts by placing the thumbside of your fist against the middle of the victim’s abdomen, just above the navel. Grab your fist with the other hand. In obese or pregnant adults, place your fist in the middle of the breastbone |
| Continue giving 5 back blows and 5 abdominal thrusts until the object is forced out or the person breathes or coughs on his or her own |
| Source: Reference 20 |
Related Resources
- Hwang SJ, Tsai SJ, Chen IJ, et al. Choking incidents among psychiatric inpatients: a retrospective study in Chutung Veterans General Hospital. J Chin Med Assoc. 2010;73(8):419-424.
- American College of Emergency Physicians Foundation. What to do in a medical emergency. Choking. www.emergencycareforyou.org/EmergencyManual/WhatToDoInMedicalEmergency/Default.aspx?id=224.
Drug Brand Names
- Aripiprazole • Abilify
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Risperidone • Risperdal
Disclosures
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Folks is a consultant and speaker for Pfizer Inc., a speaker for Forest Pharmaceuticals, and has received a research grant from Janssen Pharmaceuticals.
1. Haugen RK. The café coronary: sudden deaths in restaurants. JAMA. 1963;186:142-143.
2. Heimlich HJ. A life-saving maneuver to prevent food-choking. JAMA. 1975;234:398-401.
3. Hammond WA. A treatise on insanity and its medical relations. New York, NY: D. Appleton and Company; 1883:724.
4. Corcoran E, Walsh D. Obstructive asphyxia: a cause of excess mortality in psychiatric patients. Ir J Psychol Med. 2003;20:88-90.
5. Ruschena D, Mullen PE, Palmer S, et al. Choking deaths: the role of antipsychotic medication. Br J Psychiatry. 2003;183:446-450.
6. Yim PHW, Chong CSY. Choking in psychiatric patients: associations and outcomes. Hong Kong Journal of Psychiatry. 2009;19:145-149.
7. Craig TJ. Medication use and deaths attributed to asphyxia among psychiatric patients. Am J Psychiatry. 1980;137:1366-1373.
8. Mittleman RE, Wetli CV. The fatal café coronary. Foreign-body airway obstruction. JAMA. 1982;247:1285-1288.
9. Bieger D, Giles SA, Hockman CH. Dopaminergic influences on swallowing. Neuropharmacology. 1977;16:243-252.
10. Bettarello A, Tuttle SG, Grossman MI. Effects of autonomic drugs on gastroesophageal reflux. Gastroenterology. 1960;39:340-346.
11. Fioritti A, Giaccotto L, Melega V. Choking incidents among psychiatric patients: retrospective analysis of thirty-one cases from the west Bologna psychiatric wards. Can J Psychiatry. 1997;42:515-520.
12. Hussar AE, Bragg DG. The effect of chlorpromazine on the swallowing function in schizophrenic patients. Am J Psychiatry. 1969;126:570-573.
13. Abraham B, Alao AO. An unusual body ingestion in a schizophrenic patient: case report. Int J Psychiatry Med. 2005;35(3):313-318.
14. Beecroft N, Bach L, Tunstall N, et al. An unusual case of pica. Int J Geriatr Psychiatry. 1998;13(9):638-641.
15. Pawa S, Khalifa AJ, Ehrinpreis MN, et al. Zinc toxicity from massive and prolonged coin ingestion in an adult. Am J Med Sci. 2008;336(5):430-433.
16. Beck DA, Frohberg NR. Coprophagia in an elderly man: a case report and review of the literature. Int J Psychiatry Med. 2005;35(4):417-427.
17. Dumaguing NI, Singh I, Sethi M, et al. Pica in the geriatric mentally ill: unrelenting and potentially fatal. J Geriatr Psychiatry Neurol. 2003;16(3):189-191.
18. Bazemore H, Tonkonogy J, Ananth R. Dysphagia in psychiatric patients: clinical videofluoroscopic study. Dysphagia. 1991;6:62-65.
19. von Brauchitsch H, May W. Deaths from aspiration and asphyxiation in a mental hospital. Arch Gen Psych. 1968;18:129-136.
20. American Red Cross. Treatment for a conscious choking adult. Available at: http://www.redcross.org/flash/brr/English-html/conscious-choking.asp. Accessed August 27, 2010.
1. Haugen RK. The café coronary: sudden deaths in restaurants. JAMA. 1963;186:142-143.
2. Heimlich HJ. A life-saving maneuver to prevent food-choking. JAMA. 1975;234:398-401.
3. Hammond WA. A treatise on insanity and its medical relations. New York, NY: D. Appleton and Company; 1883:724.
4. Corcoran E, Walsh D. Obstructive asphyxia: a cause of excess mortality in psychiatric patients. Ir J Psychol Med. 2003;20:88-90.
5. Ruschena D, Mullen PE, Palmer S, et al. Choking deaths: the role of antipsychotic medication. Br J Psychiatry. 2003;183:446-450.
6. Yim PHW, Chong CSY. Choking in psychiatric patients: associations and outcomes. Hong Kong Journal of Psychiatry. 2009;19:145-149.
7. Craig TJ. Medication use and deaths attributed to asphyxia among psychiatric patients. Am J Psychiatry. 1980;137:1366-1373.
8. Mittleman RE, Wetli CV. The fatal café coronary. Foreign-body airway obstruction. JAMA. 1982;247:1285-1288.
9. Bieger D, Giles SA, Hockman CH. Dopaminergic influences on swallowing. Neuropharmacology. 1977;16:243-252.
10. Bettarello A, Tuttle SG, Grossman MI. Effects of autonomic drugs on gastroesophageal reflux. Gastroenterology. 1960;39:340-346.
11. Fioritti A, Giaccotto L, Melega V. Choking incidents among psychiatric patients: retrospective analysis of thirty-one cases from the west Bologna psychiatric wards. Can J Psychiatry. 1997;42:515-520.
12. Hussar AE, Bragg DG. The effect of chlorpromazine on the swallowing function in schizophrenic patients. Am J Psychiatry. 1969;126:570-573.
13. Abraham B, Alao AO. An unusual body ingestion in a schizophrenic patient: case report. Int J Psychiatry Med. 2005;35(3):313-318.
14. Beecroft N, Bach L, Tunstall N, et al. An unusual case of pica. Int J Geriatr Psychiatry. 1998;13(9):638-641.
15. Pawa S, Khalifa AJ, Ehrinpreis MN, et al. Zinc toxicity from massive and prolonged coin ingestion in an adult. Am J Med Sci. 2008;336(5):430-433.
16. Beck DA, Frohberg NR. Coprophagia in an elderly man: a case report and review of the literature. Int J Psychiatry Med. 2005;35(4):417-427.
17. Dumaguing NI, Singh I, Sethi M, et al. Pica in the geriatric mentally ill: unrelenting and potentially fatal. J Geriatr Psychiatry Neurol. 2003;16(3):189-191.
18. Bazemore H, Tonkonogy J, Ananth R. Dysphagia in psychiatric patients: clinical videofluoroscopic study. Dysphagia. 1991;6:62-65.
19. von Brauchitsch H, May W. Deaths from aspiration and asphyxiation in a mental hospital. Arch Gen Psych. 1968;18:129-136.
20. American Red Cross. Treatment for a conscious choking adult. Available at: http://www.redcross.org/flash/brr/English-html/conscious-choking.asp. Accessed August 27, 2010.
The psychotic pot smoker
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
CASE: Scared and confused
Mr. C, age 28, presents to the emergency department (ED) in police custody with agitation and altered mental status. Earlier that evening, Mr. C’s girlfriend noticed he was talking to himself while watching television. A few hours later, Mr. C thought someone was breaking into his house. Mr. C ran out of the house screaming for help, broke his neighbor’s window, and eventually called the police. When the police arrived Mr. C was wearing only his underwear, shaking, and bleeding from his hands. He said he was afraid and refused to respond to police instructions. Police officers used an electronic stun gun to facilitate transport to the hospital.
Mr. C admits to smoking 3 to 4 marijuana joints daily for the past 16 years. His last drug use was 2 hours before his symptoms began. Mr. C suggests that someone may have adulterated his marijuana joint but he has no factual basis for this accusation. He denies using alcohol and other illicit drugs and has no personal or family psychiatric history. He denies recent fever, loss of consciousness, chest pain, weakness, myalgia, or headache. Medically stable, his only complaint is mild hand pain.
Mr. C is alert, awake, and oriented to his name, and he responds properly to questions. He is tachycardic (101 bpm), his blood pressure is 149/57 mm Hg with normal S1 and S2 sounds, and he has no meningismus or nystagmus. Glasgow Coma Scale score is 15. He has increased deep tendon reflexes on the right upper and lower limb with good hand-grip and multiple abrasions and lacerations on his hands.
The authors’ observations
New-onset psychosis can have a wide differential diagnosis, particularly when reliable history is not available. Mr. C’s allegation that someone tampered with his marijuana raises 2 possibilities: embalming fluid (form-aldehyde) toxicity or PCP intoxication.
Embalming fluid toxicity can cause:
- agitation and sudden unpredictable behavior
- confusion or toxic delirium
- coma or seizure
- cerebral and pulmonary edema or death in severe cases.
The terms “wet,” “sherm,” “fly,” “amp,” or “illy” are used to describe a marijuana cigarette that has been dipped into embalming fluid, dried, and then smoked.1 The effect is similar to that of PCP and causes extreme hallucinations. Reported highs last 30 minutes to 1 hour.2
Symptomatology of PCP intoxication may be indistinguishable from functional psychosis (Table 1).3 Visual, auditory, and tactile misperceptions are common and highly changeable disorientation often is accompanied by alternating periods of lethargy and fearful agitation. These patients typically show catatonic posturing and/or stereotyped movement. Somatic sensations appear to be disassociated; patients may misperceive pain, distance, and time. Patients taking PCP rarely admit to true hallucinations; however their thinking usually is grossly disoriented.4 Symptoms of delirium may last from 30 minutes to 6 hours in 80% of cases; 12% of patients may remain symptomatic for 12 hours. Violent behavior and agitation usually lasts only a few hours.5
Long-term marijuana abuse can lead to psychosis6 but acute onset is not typical, and recent prospective trials raised doubts that cannabis would be a sole factor.7 Instead, cannabis may be 1 of several factors that contribute to psychosis, particularly in patients who are predisposed.
Table 1
Phencyclidine (PCP) intoxication: What to look for
| Findings | Percentage of cases |
|---|---|
| Nystagmus | 57.4% |
| Hypertension | 57.0% |
| Delirium | 36.9% |
| Violent behavior | 35.4% |
| Agitation | 34.0% |
| Tachycardia | 30.0% |
| Bizarre behavior | 28.5% |
| Hallucinations/delusions | 18.5% |
| Unconsciousness | 10.6% |
| Lethargy/stupor | 6.6% |
| Hypothermia | 6.4% |
| Generalized rigidity | 5.2% |
| Profuse sweating | 3.9% |
| No behavior effect | 3.5% |
| Grand mal seizure | 3.1% |
| Source: Reference 3 | |
Possible neurologic causes
Complex partial seizures—also known as psychomotor epilepsy—are caused by a surge of electrical activity in the brain. Seizures often involve 1 of the brain’s temporal lobes but can affect any brain region. Symptoms include:
- impaired social interaction
- inability to control one’s movements
- alogia
- amnesia.
Episodes typically start with a blank stare followed by automatisms. The actions and movements often are unorganized or confused. Motor symptoms typically last for 1 to 2 minutes and confusion persists for another 1 to 2 minutes.8 In rare cases, a patient may become agitated or engage in behaviors such as undressing. Complex partial seizures may cause a person to run in apparent fear, cry out, or repeat a phrase.9 Electroencephalogram, CT, MRI, or positron-emission tomography scan could reveal any intracranial focus of complex partial seizures.
We suspect PCP or embalming fluid intoxication and initiate supportive therapy.
EVALUATION: Still confused
Initial baseline labs include a urine drug screen (UDS), chest radiography, ECG, and head CT. Mr. C’s UDS is positive for cannabis. A specific PCP assay is negative. White blood cell count (WBC) is 22,000/μL with high neutrophil count (88%), creatine kinase (CK) is 458 U/L, and urinalyis reveals protein 75 mg/dL and ketone 50 mg/dL. Head CT is negative for any acute process (click here for detailed description of Mr. C�s hospital course while in the ED).
During psychiatric evaluation 7 hours after presentation, Mr. C’s speech is loose and somewhat pressured, but intelligible. He cannot follow commands. Mr. C is delusional and appears to be hallucinating. He can repeat 3 words immediately but not after 3 minutes. We start Mr. C on divalproex, 1,500 mg/d, haloperidol, 6 mg/d, and IV lorazepam, 2 mg as needed for agitation. Although mildly disoriented, he gradually becomes less agitated.
The authors’ observations
At this point further evaluation is needed. Mr. C’s elevated WBC count could explain his fluctuating symptoms. He cannot provide further history and his family denies any past psychiatric episodes. Thyroid-stimulating hormone, B12, and folate levels are within normal limits. A negative LP rules out meningitic infection. We give Mr. C a diagnosis of psychosis NOS (Table 2).10
Table 2
DSM-IV-TR criteria for psychotic disorder, not otherwise specified
| This category includes psychotic symptomatology (ie, delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior) about which there is inadequate information to make a specific diagnosis or about which there is contradictory information, or disorders with psychotic symptoms that do not meet the criteria for any specific psychotic disorder. Examples include: |
|
| Source: Reference 10 |
TREATMENT: Medication choices
After 8 hours in the ED, Mr. C is transferred to the medical unit, where he becomes agitated and complains of auditory and visual hallucinations. He receives divalproex, 750 mg, haloperidol, 3 mg, and IM diphenhydramine, 50 mg, to calm him. He remains agitated but not violent until bedtime. At midnight he is agitated and violent and receives another dose of haloperidol and IM diphenhydramine with IV lorazepam, 2 mg. These medications calm him and he is able to sleep until morning.
Morning labs reveal CK is 674 U/L and WBC decreased to 13,200/μL. Mr. C denies any distress but after the fourth dose of haloperidol, he develops dystonia of his arms so we discontinue this medication. We start aripiprazole, 10 mg/d gradually increased to 30 mg/d, and Mr. C receives 1 injection of diphenhydramine. He responds well to the treatment.
The next few hours are uneventful but then Mr. C becomes verbally abusive to his relatives and sitter; physical restraints are ordered and he receives IM ziprasidone, 20 mg, and IV lorazepam, 2 mg. He remains awake and babbling. His perception continues to wax and wane and his words are jumbled. He remains calm until the next morning (click here for detailed description of Mr. C�s hospital course while on the medical unit).
After 4 days on the medical unit Mr. C is transferred to the psychiatry unit, where he is angry, belligerent, and hostile, but not placed in restraints. His symptoms resolve in 2 days without any further episodes of violent behavior.
OUTCOME: Solving the puzzle
When Mr. C becomes cooperative, he gives a detailed history. He repeats his suspicion of smoking adulterated marijuana, but during detailed questioning, he admits to using alprazolam, which he purchased illegally, to sleep for the past 6 to 7 months. He started with 1 or 2 “footballs” (1 to 2 mg) and gradually increased to 3 or 4 “bars” (6 to 8 mg) each day. Mr. C could no longer afford the drug and last took alprazolam 6 days before his symptoms began. He says that after stopping alprazolam he felt anxious and could not sleep. His girlfriend adds that he was irritable and “he had not been acting himself” several days before admission. She says he complained of hearing the voice of God, particularly when he was not taking alprazolam.
Mr. C’s hand wounds heal and his vitals are normal during his 1-week stay on the psychiatric unit. His interactions with staff and peers improve. Aripiprazole is tapered and discontinued; divalproex is reduced to 1,000 mg/d. Mr. C is discharged 11 days after presentation and prescribed divalproex, 1,000 mg/d, with instructions to taper the drug over several days to prevent withdrawal seizures before stopping it in 1 week.
Mr. C does not return for his follow-up appointment; however, in a telephone follow-up 6 months later, he denies experiencing withdrawal symptoms after discharge. Mr. C is now undergoing drug rehabilitation.
The authors’ observations
Benzodiazepine withdrawal symptoms occur 7 to 10 days after abrupt cessation (Table 3).10 Symptoms are similar to those of alcohol withdrawal and include tachycardia, hypertension, clouding of consciousness, and auditory and visual hallucinations.11 Serious reactions to benzodiazepine withdrawal include seizures and death.12
Because of the high prevalence of poly-substance misuse, obtain a detailed substance use history in patients undergoing benzodiazepine withdrawal to determine the likelihood of polysubstance withdrawal.13 A cross-tolerant sedative such as clonazepam could prevent withdrawal symptoms as the dose is gradually decreased. Long-acting benzodiazepines such as clonazepam or diazepam are recommended.14
In Mr. C’s case, minor withdrawal symptoms, such as disturbed sleep and irritability, began 3 to 4 days after discontinuing benzodiazepines15 and preceded development of psychosis. Withdrawal symptoms usually resolve after 2 weeks.16 Mr. C responded only partially to IV lorazepam because he did not receive the total replacement dose. Had we known he was experiencing benzodiazepine withdrawal, Mr. C could have been managed with detoxi"cation of the primary drug, alprazolam, with diazepam substitution and tapering over 3 weeks.17
Table 3
Criteria for sedative, hypnotic, or anxiolytic withdrawal
| A. Cessation of (or reduction in) sedative, hypnotic, or anxiolytic use that has been heavy and prolonged |
B. Two (or more) of the following, developing within several hours to a few days after Criterion A:
|
| C. The symptoms in Criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder |
| Source: Reference 10 |
Related Resource
- Vikander B, Koechling UM, Borg S, et al. Benzodiazepine tapering: a prospective study. Nord J Psychiatry. 2010; 64(4):273-282.
Drug Brand Names
- Alprazolam • Xanax
- Aripiprazole • Abilify
- Chlordiazepoxide • Librium
- Diazepam • Valium
- Diphenhydramine • Diphenhydramine injection
- Divalproex • Depakote
- Haloperidol • Haldol
- Lorazepam • Ativan
- Ziprasidone • Geodon
Acknowledgements
The authors wish to thank Reena Kumar, MD, and Sonja Gennuso, fourth-year medical student at Louisiana State University Health Sciences Center, Shreveport, for their help in preparing this manuscript.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 1
Mr. C’s hospital course in the emergency department
| Time after presentation | Description |
|---|---|
| 2 hours | Mr. C is alert and oriented to his name and place. He rests comfortably but asks questions about his girlfriend and uncle, falsely believing they are in the emergency department |
| 4 hours | Hand lacerations are repaired, but Mr. C continues to dig in his wounds with the opposite hand and place it over his mouth despite constant redirection. He reports hearing his uncle’s voice behind the curtain. He then uses the pulse oximeter as a telephone and holds a conversation with his uncle on the other side of the curtain. On redirection, Mr. C replies that the pulse oximeter looks like a telephone and begins mumbling to himself |
| 5 hours | Mr. C continues to mumble but responds when directly questioned. He keeps insisting that the pulse oximeter is a telephone and that he can tell his uncle to come over from the other side of the curtain. He continues to act inappropriately despite the presence of family members but he is aware of their identities |
| 6 hours | Mr. C becomes disoriented and agitated and pulls out his IV line. Because of the high WBC count, we order blood cultures and a urine culture and give him IV antibiotics |
| WBC: white blood cell count | |
Table 2
Mr. C’s hospital course on the medical unit
| Time after presentation | Description |
|---|---|
| 54 hours | He is oriented to person and place. Staff notices he is talking to someone in the room but no one is present. Mr. C appears to be responding to visual hallucinations, but upon questioning he denies any symptoms. Restraints are discontinued. Divalproex is increased to 2,000 mg/d |
| 62 hours | Mr. C remains calm for several hours but later begins hallucinating and calls to his mother and others when no one is in the room. He receives IV lorazepam, 2 mg, without much response. Again he is placed in restraints and receives another dose of IV lorazepam, 3 mg, and IM ziprasidone, 20 mg. He becomes calmer. Restraints are continued as a precautionary measure. Mr. C calms down after several hours but cannot sleep |
| 78 hours | The next morning, Mr. C remains agitated and aggressive with loud speech. He denies any further hallucinations but talks to an invisible person. He remains in restraints and receives his routine medications. His blood pressure is 141/99 mm Hg and pulse is 110. Pulse rate normalizes during the day and he becomes calmer but seclusive |
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
1. Office of National Drug Control Policy. Street terms: drugs and the drug trade. Available at:http://www.whitehousedrugpolicy.gov/streetterms/ByType.asp?intTypeID=1. Accessed July 26, 2010.
2. Elwood WN. TCADA research brief: “Fry:” a study of adolescents’ use of embalming fluid with marijuana and tobacco. Texas Commission on Alcohol and Drug Abuse. 1998. Available at:http://www.dshs.state.tx.us/sa/research/populations/fry.pdf. Accessed August 9, 2010.
3. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10(5):237-242.
4. Aniline O, Pitts FN, Jr. Phencyclidine (PCP): a review and perspectives. Crit Rev Toxicol. 1982;10(2):145-177.
5. McCarron MM, Schulze BW, Thomson GA, et al. Acute phencyclidine intoxication: clinical patterns, complications, and treatment. Ann Emerg Med. 1981;10(6):290-297.
6. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187-194.
7. Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4(3):191-196.
8. Carroll E, Benbadis SR. Complex partial seizures. eMedicine. April 21, 2010. Available at:http://emedicine.medscape.com/article/1183962-overview. Accessed July 20, 2010.
9. Epilepsy.com. Complex partial seizures. Available at: http://www.epilepsy.com/epilepsy/seizure_complexpartial. Accessed July 20, 2010.
10. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Mellor CS, Jain VK. Diazepam withdrawal syndrome: its prolonged and changing nature. Can Med Assoc J. 1982;127(11):1093-1096.
12. Lann MA, Molina DK. A fatal case of benzodiazepine withdrawal. Am J Forensic Med Pathol. 2009;30(2):177-179.
13. Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16(1):51-57.
14. Franklin JE, Jr., Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:400–401.
15. Preskorn SH, Denner LJ. Benzodiazepines and withdrawal psychosis. Report of three cases. JAMA. 1977;237(1):36-38.
16. Miller F, Nulsen J. Single case study. Diazepam (valium) detoxification. J Nerv Ment Dis. 1979;167:637-638.
17. Seivewright N, Dougal W. Withdrawal symptoms from high dose benzodiazepines in poly drug users. Drug Alcohol Depend. 1993;32(1):15-23.
Should you order genetic testing to identify how patients metabolize antipsychotics?
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Two months ago, Mr. P, age 20, experienced paranoid thoughts, anxiety, agitation, and auditory hallucinations. During a brief hospitalization 1 month later, he received IM haloperidol, 2 mg, which he said “made his neck stiff.” After he was discharged, Mr. P, who is White, stopped taking his antipsychotics. During a recent outpatient evaluation, the clinician gives Mr. P a working diagnosis of schizophrenia and prescribes risperidone, 2 mg/d, with plans to titrate to 4 mg/d in the next 2 weeks. However, a week later, Mr. P complains of extreme sedation and feeling “knocked out” and does not want to continue taking the medication. Physical exam reveals slight cogwheel rigidity. His delusional thought content is not improved. The treating physician considers ordering a genetic test to determine Mr. P’s cytochrome P450 (CYP) 2D6 metabolizer status.
Studies investigating relationships among genetic variants thought to impact pharmacokinetics and pharmacodynamics of psychotropic medications have had mixed results.1 Metabolism of most antipsychotics depends on the CYP450 enzyme system, which is expressed predominantly in the liver (Table 1). CYP2D6 is one of these enzymes and may be responsible for metabolizing approximately 20% to 50% of all medications, including a number of antipsychotics.2 Genetic variations of CYP2D6 are common and the frequencies of these variants differ among racial groups.3
The half-life and other pharmacokinetic parameters of an antipsychotic metabolized by CYP2D6 may differ based on whether someone is a poor metabolizer (PM), intermediate metabolizer (IM), extensive metabolizer (EM), or ultrarapid metabolizer (UM).4 Regarding CYP2D6 metabolism among Whites, 3% to 5% are UMs, 70% to 80% are EMs, 10% to 17% are IMs, and 5% to 10% are PMs.5 By contrast, the percentage of PMs and UMs in the Asian population is low—about 1% for each phenotype; the IM phenotype is more common (65% to 70% in the Chinese population).5,6 The percentage of PMs in African Americans is roughly 2% to 6%.2
- Genetic variants of CYP2D6 may result in decreased or increased metabolism of some drugs, including risperidone, iloperidone, perphenazine, haloperidol, and thioridazine.
- The effect of reduced CYP2D6 activity may increase a patient’s risk for dose-related adverse effects.
- It is currently unknown if clinical genotyping for CYP2D6 variants and using this information to guide drug selection or dosing improves patient outcomes.
The clinical effect of altered metabolizer status depends on the extent the metabolism of a given agent is dependent on CYP2D6. PM status results in an approximately 2- to 6-fold increase in elimination half-life and overall exposure of aripiprazole,7 risperidone,8 and iloperidone9 (Figure). On the other end of the spectrum are UMs. Because of gene duplication, patients who fall into this category have enhanced metabolic activity. As a result, the therapeutic effect of several medications may be decreased because of faster clearance from the body, leading some physicians to label them as treatment-resistant.
Because side effects of many antipsychotics are dose-dependent, genotyping may be valuable for patients taking agents that are primarily metabolized by CYP2D6.10 Clinicians now have access to laboratory resources and FDA-approved methods for assessing CYP2D6 gene variants.11 It is debatable, however, whether this testing—which is expensive (≥$400) and may not be covered by health insurance—improves patient outcomes. In Mr. P’s case, if he had been genotyped as a CYP2D6 PM before treatment, his physicians might not have prescribed haloperidol and could have prevented a mild dystonic reaction. Also, they could have lowered the initial risperidone dose or chosen an antipsychotic such as ziprasidone, paliperidone, or quetiapine where the pharmacokinetic consequences of 2D6 poor metabolism are not as severe. Theoretically, one may argue that this could have reduced the risk for antipsychotic-associated side effects that now are a barrier to Mr. P’s desire to continue antipsychotics. On the other hand one may also reasonably argue that there may be other/additional reasons (genetic or non-genetic) that make some patients more sensitive to the side effects of antipsychotics and that simply assessing CYP2D6 status is not enough to guide drug selection and dosing.
Table 1
Cytochrome P450 (CYP) metabolism of commonly used antipsychotics*
| Drug | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4/5 |
|---|---|---|---|---|---|
| Aripiprazole | X | X | |||
| Asenapine | X | X | X | ||
| Chlorpromazine | X | X | X | ||
| Clozapine | X | X | X | X | X |
| Fluphenazine | X | ||||
| Haloperidol | X | X | X | ||
| Iloperidone | X | X | |||
| Olanzapine | X | X | |||
| Paliperidone | X† | X† | |||
| Perphenazine | X | X | X | X | X |
| Quetiapine | X | X | |||
| Risperidone | X | X | |||
| Thioridazine | X | X | |||
| Ziprasidone | X | X | |||
| *Information obtained from the most recent prescribing information available from each drug’s manufacturer †According to paliperidone’s prescribing information, in vitro studies identify that CYP2D6 and CYP3A4 may be involved in paliperidone metabolism, but in vivo studies indicate that their role in eliminating paliperidone is minimal | |||||
Figure: Effects of CYP2D6 poor metabolizer status on the half-life of risperidone, aripiprazole, and iloperidone
EM: extensive metabolizer; PM: poor metabolizer
Source: References 7-9
Use in clinical practice
Proposed expert guidelines recommend halving the normal target dose of risperidone and avoiding haloperidol and phenothiazine antipsychotics in CYP2D6 PMs.12 These guidelines are based on expert review of the pharmacokinetic effects of CYP2D6 PM status as well as case reports and studies associating CYP2D6 with poor outcomes, usually side effects. Although these studies suggest that determining metabolizer status may be clinically important, many other studies—some very large—have not found evidence for associations between drug metabolizing enzyme variants and clinical outcomes from antipsychotics.13
There are 2 clinical scenarios in which one may consider obtaining CYP2D6 genotype information:
- before initiating treatment (Table 2)
- after trying ≥1 agent primarily dependent on CYP2D6 with evidence of dose-related side effect (Table 3).
Identifying PMs could influence drug selection and dosing if this information is available before antipsychotic exposure. Studies have found evidence that CYP2D6 PMs may be at greater risk of experiencing adverse reactions to risperidone compared with other metabolizer groups.14 Also, prescribing information for aripiprazole and iloperidone recommends halving the dose of these drugs in the presence of CYP2D6 inhibitors, a condition that pharmacokinetically mimics PM status.
Knowing genotype information after ≥1 drugs have been tried may not be as useful. Clinicians often base drug switches or dose titrations on a patient’s experience with present or past doses of the antipsychotic. Examples include slowing titrations or reducing a target dose when a patient, such as Mr. P, experiences side effects, or selecting non-2D6 substrate agents after detecting a pattern of drug sensitivity.
Table 2
CYP2D6 testing before initiating antipsychotics: Benefits vs drawbacks
| Benefits | Drawbacks |
|---|---|
| Clinicians could avoid 2D6 substrate drugs with high likelihood for ADEs or increased risk of 2D6-based interactions in PMs | No empiric evidence shows that routine genotyping produces better clinical outcomes (eg, fewer side effects and better treatment adherence) |
| May lower initial dose, slow titration, and lower initial target dose to minimize risk of side effects in PMs | Many clinicians titrate slowly or adjust titration schedule and target doses based on initial tolerability as part of routine practice |
| The test would need to be done only once and the information may be useful for other therapy decisions | Patients who need immediate drug therapy may not be able to wait for test results |
| Testing may not be covered by a patient’s health insurance | |
| ADEs: adverse drug events; PMs: poor metabolizers | |
Table 3
Genotype testing after a patient experiences side effects
| Benefits |
| Identifying a biologic reason for side effect sensitivity may aid choice and dosing of subsequent antipsychotics and other medications |
| Drawbacks |
| In clinical practice, antipsychotic switching because of tolerability (and response) often is guided by outcomes experienced from previously used agents. In general, patients with a history of experiencing side effects at lower doses of antipsychotics are likely to be initiated at lower doses and titrated more cautiously during subsequent therapy choices regardless of whether side effects were caused by metabolizer status or other factor(s) |
Better patient outcomes?
It is not known if obtaining genotype information will provide better outcomes than a “trial and error” approach. Currently, obtaining genotype information before antipsychotic treatment is not standard clinical practice. Because this testing is expensive and requires prior approval from third party payers or out-of-pocket financial resources, testing is not recommended for all patients at this time.
However, a growing body of evidence suggests that knowing metabolizer status could be useful in drug selection or dosing for antipsychotics. This scientific knowledge continues to accumulate, and CYP2D6 genotyping may some day be integrated into routine clinical care. Currently, for patients and physicians with the resources to obtain and the ability to appropriately interpret the test results, this information may prove useful on an individual basis. However, additional studies are needed to support better outcomes from dosing and drug selection based on CYP2D6 genotype information.
Related Resources
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP). www.egappreviews.org.
- Pharmacogenomics Knowledge Base. www.pharmgkb.org.
- Indiana University School of Medicine. P450 drug interaction table. http://medicine.iupui.edu/clinpharm/ddis/table.asp.
Drug Brand Names
- Aripiprazole • Abilify
- Asenapine • Saphris
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Fluphenazine • Prolixin
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Perphenazine • Trilafon
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Bishop receives grant/research support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil-Janssen and has received honoraria from Eli Lilly and Company.
Ms. Chae reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.
1. Leckband SG, Bishop JR, Ellingrod VL. Pharmacogenomics in psychiatry. J Pharm Pract. 2007;20:252-264.
2. Neafsey P, Ginsberg G, Hattis D, et al. Genetic polymorphism in cytochrome P450 2D6 (CYP2D6): population distribution of CYP2D6 activity. J Toxicol Environ Health B Crit Rev. 2009;12(5-6):334-361.
3. Bradford LD, Gaedigk A, Leeder JS. High frequency of CYP2D6 poor and “intermediate” metabolizers in black populations: a review and preliminary data. Psychopharmacol Bull. 1998;34:797-804.
4. Gaedigk A, Simon SD, Pearce RE, et al. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234-242.
5. Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761-804.
6. Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest. 2003;33(suppl 2):17-22.
7. Risperdal [package insert]. Titusville, NJ: Janssen; 2010.
8. Abilify [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co.; 2009.
9. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals, Inc.; 2009.
10. Kirchheiner J, Rodriguez-Antona C. Cytochrome P450 2D6 genotyping: potential role in improving treatment outcomes in psychiatric disorders. CNS Drugs. 2009;23:181-191.
11. de Leon J, Susce MT, Murray-Carmichael E. The AmpliChip CYP450 genotyping test: integrating a new clinical tool. Mol Diagn Ther. 2006;10:135-151.
12. de Leon J, Armstrong SC, Cozza KL. Clinical guidelines for psychiatrists for the use of pharmacogenetic testing for CYP450 2D6 and CYP450 2C19. Psychosomatics. 2006;47:75-85.
13. Grossman I, Sullivan PF, Walley N, et al. Genetic determinants of variable metabolism have little impact on the clinical use of leading antipsychotics in the CATIE study. Genet Med. 2008;10:720-729.
14. Rodriguez-Antona C, Gurwitz D, de Leon J, et al. CYP2D6 genotyping for psychiatric patients treated with risperidone: considerations for cost-effectiveness studies. Pharmacogenomics. 2009;10:685-699.