User login
Wife is Worried That Her Husband's Condition is Contagious
ANSWER
The correct answer is petaloid seborrheic dermatitis (choice “d”), named for the flowerlike appearance of its polycyclic borders. Psoriasis (choice “a”) can present in this area, but tends to be scalier and usually involves multiple areas (eg, elbows, knees, and nails).
Rashes like this patient’s are often termed yeast infection (choice “b”). However, while a commensal yeast (Pityrosporum) can play a role in its formation, it appears that seborrhea represents an idiosyncratic reaction to increased numbers of this organism, rather than an actual infection.
Bowen’s disease (choice “c”) is a superficial squamous cell carcinoma, usually caused by overexposure to sunlight. Its lesions will be fixed, slowly growing larger with time, while seborrheic dermatitis will typically come and go. Biopsy is sometimes necessary to distinguish one from the other.
DISCUSSION
Seborrheic dermatitis (SD, aka seborrhea) is common, affecting up to 5% of the population. Dandruff is its usual manifestation, but it affects numerous other areas (as in this case), including the axillae, groin, beard, and genitals.
Presenting with scaling on an erythematous base, SD often flares and remits with the season (especially winter), with stress, and with increases in alcohol intake. Although it is usually mild, some cases can be severe. SD is associated with or accentuated by several other conditions, including Parkinson’s, stroke, and HIV. Severe SD in infants raises the possibility of Langerhans cell histiocytosis, especially when the presentation is atypical.
The diagnosis of SD can be difficult when it appears elsewhere than the scalp and face (eg, as an axillary or genital rash). Likewise, sternal petaloid SD is mystifying, unless other corroboratory manifestations are sought and found.
A few patients show signs of SD and psoriasis such that a definitive diagnosis cannot be made. Such overlap cases are sometimes termed sebopsoriasis. But psoriasis will usually exhibit signs not seen with SD, such as pitting of the nails, involvement of extensor surfaces of elbows and knees, and characteristic signs of psoriatic arthropathy in about 20% of cases. Pinpoint bleeding caused by peeling away scale, called the Auspitz sign, is seen with psoriasis and not with SD.
TREATMENT
This patient’s chest involvement responded rapidly to topical betamethasone foam, quickly tapered to avoid thinning the skin. Less powerful steroid creams, lotions, or gels (eg, triamcinolone 0.025%) can be used on other areas, such as ears and face. The daily use of an OTC dandruff shampoo (containing selenium sulfide, zinc pyrithione, tar, or ketoconazole) is an effective approach to controlling scalp involvement, but the product should be changed weekly.
Once the initial inflammation is controlled, topical antiyeast/antifungal preparations (eg, ketoconazole cream or any of the imidazoles, such as clotrimazole or oxiconazole) can be useful.
Finally, emphasis must be placed on educating the patient to expect control of the condition but not a cure.
ANSWER
The correct answer is petaloid seborrheic dermatitis (choice “d”), named for the flowerlike appearance of its polycyclic borders. Psoriasis (choice “a”) can present in this area, but tends to be scalier and usually involves multiple areas (eg, elbows, knees, and nails).
Rashes like this patient’s are often termed yeast infection (choice “b”). However, while a commensal yeast (Pityrosporum) can play a role in its formation, it appears that seborrhea represents an idiosyncratic reaction to increased numbers of this organism, rather than an actual infection.
Bowen’s disease (choice “c”) is a superficial squamous cell carcinoma, usually caused by overexposure to sunlight. Its lesions will be fixed, slowly growing larger with time, while seborrheic dermatitis will typically come and go. Biopsy is sometimes necessary to distinguish one from the other.
DISCUSSION
Seborrheic dermatitis (SD, aka seborrhea) is common, affecting up to 5% of the population. Dandruff is its usual manifestation, but it affects numerous other areas (as in this case), including the axillae, groin, beard, and genitals.
Presenting with scaling on an erythematous base, SD often flares and remits with the season (especially winter), with stress, and with increases in alcohol intake. Although it is usually mild, some cases can be severe. SD is associated with or accentuated by several other conditions, including Parkinson’s, stroke, and HIV. Severe SD in infants raises the possibility of Langerhans cell histiocytosis, especially when the presentation is atypical.
The diagnosis of SD can be difficult when it appears elsewhere than the scalp and face (eg, as an axillary or genital rash). Likewise, sternal petaloid SD is mystifying, unless other corroboratory manifestations are sought and found.
A few patients show signs of SD and psoriasis such that a definitive diagnosis cannot be made. Such overlap cases are sometimes termed sebopsoriasis. But psoriasis will usually exhibit signs not seen with SD, such as pitting of the nails, involvement of extensor surfaces of elbows and knees, and characteristic signs of psoriatic arthropathy in about 20% of cases. Pinpoint bleeding caused by peeling away scale, called the Auspitz sign, is seen with psoriasis and not with SD.
TREATMENT
This patient’s chest involvement responded rapidly to topical betamethasone foam, quickly tapered to avoid thinning the skin. Less powerful steroid creams, lotions, or gels (eg, triamcinolone 0.025%) can be used on other areas, such as ears and face. The daily use of an OTC dandruff shampoo (containing selenium sulfide, zinc pyrithione, tar, or ketoconazole) is an effective approach to controlling scalp involvement, but the product should be changed weekly.
Once the initial inflammation is controlled, topical antiyeast/antifungal preparations (eg, ketoconazole cream or any of the imidazoles, such as clotrimazole or oxiconazole) can be useful.
Finally, emphasis must be placed on educating the patient to expect control of the condition but not a cure.
ANSWER
The correct answer is petaloid seborrheic dermatitis (choice “d”), named for the flowerlike appearance of its polycyclic borders. Psoriasis (choice “a”) can present in this area, but tends to be scalier and usually involves multiple areas (eg, elbows, knees, and nails).
Rashes like this patient’s are often termed yeast infection (choice “b”). However, while a commensal yeast (Pityrosporum) can play a role in its formation, it appears that seborrhea represents an idiosyncratic reaction to increased numbers of this organism, rather than an actual infection.
Bowen’s disease (choice “c”) is a superficial squamous cell carcinoma, usually caused by overexposure to sunlight. Its lesions will be fixed, slowly growing larger with time, while seborrheic dermatitis will typically come and go. Biopsy is sometimes necessary to distinguish one from the other.
DISCUSSION
Seborrheic dermatitis (SD, aka seborrhea) is common, affecting up to 5% of the population. Dandruff is its usual manifestation, but it affects numerous other areas (as in this case), including the axillae, groin, beard, and genitals.
Presenting with scaling on an erythematous base, SD often flares and remits with the season (especially winter), with stress, and with increases in alcohol intake. Although it is usually mild, some cases can be severe. SD is associated with or accentuated by several other conditions, including Parkinson’s, stroke, and HIV. Severe SD in infants raises the possibility of Langerhans cell histiocytosis, especially when the presentation is atypical.
The diagnosis of SD can be difficult when it appears elsewhere than the scalp and face (eg, as an axillary or genital rash). Likewise, sternal petaloid SD is mystifying, unless other corroboratory manifestations are sought and found.
A few patients show signs of SD and psoriasis such that a definitive diagnosis cannot be made. Such overlap cases are sometimes termed sebopsoriasis. But psoriasis will usually exhibit signs not seen with SD, such as pitting of the nails, involvement of extensor surfaces of elbows and knees, and characteristic signs of psoriatic arthropathy in about 20% of cases. Pinpoint bleeding caused by peeling away scale, called the Auspitz sign, is seen with psoriasis and not with SD.
TREATMENT
This patient’s chest involvement responded rapidly to topical betamethasone foam, quickly tapered to avoid thinning the skin. Less powerful steroid creams, lotions, or gels (eg, triamcinolone 0.025%) can be used on other areas, such as ears and face. The daily use of an OTC dandruff shampoo (containing selenium sulfide, zinc pyrithione, tar, or ketoconazole) is an effective approach to controlling scalp involvement, but the product should be changed weekly.
Once the initial inflammation is controlled, topical antiyeast/antifungal preparations (eg, ketoconazole cream or any of the imidazoles, such as clotrimazole or oxiconazole) can be useful.
Finally, emphasis must be placed on educating the patient to expect control of the condition but not a cure.

A 70-year-old man presents with a slightly itchy rash on his sternum that has appeared intermittently for years. Told it is “ringworm” by his primary care provider, the patient tried tolnaftate cream, to no avail. He is seeking additional consultation primarily because his wife is concerned she will catch the “infection.” The patient denies other skin problems, but then remembers that he has dandruff that flares from time to time, as well as a curious scaly red rash that “comes and goes” between his eyes, in his nasolabial folds, and behind his ears, especially in the winter. His father had similar problems. The patient is otherwise healthy, except for mild hypertension. The rash, located on the lower right sternum, measures about 6 cm at its largest dimension. Faintly pink, it has a papulosquamous surface, especially on its pol-ycyclic borders. Results of a KOH prep are negative for fungal elements. Elsewhere, a faintly scaly, orange-red rash is seen in the glabellar area and behind both ears. The man’s knees, elbows, and nails are free of any changes.
Woman with Discomfort and Discoloration on Back
ANSWER
The correct answer is erythema ab igne (choice “a”) caused, of course, by the effects of the heating pad. The reticular pattern and acute onset are quite characteristic of this unusual condition.
Contact dermatitis (choice “b”) would not have presented in this reticular pattern and would typically have itched intensely.
Cellulitis (choice “c”) represents a superficial infection usually caused by strep and/or staph. It would not have been reticular, would have been painful, and would have required a break in the skin for the offending organism to gain entrance.
Poikiloderma vasculare atrophicans (PVA; choice “d”) describes vascular changes seen focally in patches that evolve slowly over months or even years. It is significant because of its reported potential to evolve into cutaneous T-cell lymphoma; however, PVA does not present with a reticular pattern, nor does it appear acutely.
DISCUSSION
The superficial vascular plexus, configured in a reticular pattern and normally invisible, is sensitive to repeated exposure to the infrared portion of the magnetic spectrum (wavelength 700 to 1,100 nm). This exposure initially produces erythema, which over time turns livid, then permanently hyperpigmented.
Erythema ab igne (EAI) was classically seen in those sitting close to an open fire or stove (producing temperatures of 43°C to 47°C) for extended periods, often for hours each day. With the advent of central heating, other triggers of EAI evolved, including prolonged use of laptop computers, heating fans, and as in this case, heating pads. It can even be due to occupational exposure to intense heat, as with glassblowers, bakers, and steelworkers.
Most of the skin changes seen with EAI resemble those seen with chronic sun damage, including vasodilatation and melanin incontinence with melanophages in the upper dermis.
This particular patient had only one exposure to the heating pad, but had turned it on high and lain on it all night. This produced the changes seen, which will likely become permanently etched in her skin in the exact pattern of the causative heating pad. Months of dexamethasone therapy may also have contributed to the problem, by thinning the patient’s skin enough to render her susceptible to this single exposure to heat.
With EAI patients in general, thought needs to be given to possible underlying issues, such as the source of pain being treated with the heating pad—most commonly, on the low back—or the possible reason for constantly feeling cold, such as anemia or hypothyroidism.
Treatment choices include the application of tretinoin cream or 5-fluorouracil cream, or ablation with laser (YAG, ruby, alexandrite).
ANSWER
The correct answer is erythema ab igne (choice “a”) caused, of course, by the effects of the heating pad. The reticular pattern and acute onset are quite characteristic of this unusual condition.
Contact dermatitis (choice “b”) would not have presented in this reticular pattern and would typically have itched intensely.
Cellulitis (choice “c”) represents a superficial infection usually caused by strep and/or staph. It would not have been reticular, would have been painful, and would have required a break in the skin for the offending organism to gain entrance.
Poikiloderma vasculare atrophicans (PVA; choice “d”) describes vascular changes seen focally in patches that evolve slowly over months or even years. It is significant because of its reported potential to evolve into cutaneous T-cell lymphoma; however, PVA does not present with a reticular pattern, nor does it appear acutely.
DISCUSSION
The superficial vascular plexus, configured in a reticular pattern and normally invisible, is sensitive to repeated exposure to the infrared portion of the magnetic spectrum (wavelength 700 to 1,100 nm). This exposure initially produces erythema, which over time turns livid, then permanently hyperpigmented.
Erythema ab igne (EAI) was classically seen in those sitting close to an open fire or stove (producing temperatures of 43°C to 47°C) for extended periods, often for hours each day. With the advent of central heating, other triggers of EAI evolved, including prolonged use of laptop computers, heating fans, and as in this case, heating pads. It can even be due to occupational exposure to intense heat, as with glassblowers, bakers, and steelworkers.
Most of the skin changes seen with EAI resemble those seen with chronic sun damage, including vasodilatation and melanin incontinence with melanophages in the upper dermis.
This particular patient had only one exposure to the heating pad, but had turned it on high and lain on it all night. This produced the changes seen, which will likely become permanently etched in her skin in the exact pattern of the causative heating pad. Months of dexamethasone therapy may also have contributed to the problem, by thinning the patient’s skin enough to render her susceptible to this single exposure to heat.
With EAI patients in general, thought needs to be given to possible underlying issues, such as the source of pain being treated with the heating pad—most commonly, on the low back—or the possible reason for constantly feeling cold, such as anemia or hypothyroidism.
Treatment choices include the application of tretinoin cream or 5-fluorouracil cream, or ablation with laser (YAG, ruby, alexandrite).
ANSWER
The correct answer is erythema ab igne (choice “a”) caused, of course, by the effects of the heating pad. The reticular pattern and acute onset are quite characteristic of this unusual condition.
Contact dermatitis (choice “b”) would not have presented in this reticular pattern and would typically have itched intensely.
Cellulitis (choice “c”) represents a superficial infection usually caused by strep and/or staph. It would not have been reticular, would have been painful, and would have required a break in the skin for the offending organism to gain entrance.
Poikiloderma vasculare atrophicans (PVA; choice “d”) describes vascular changes seen focally in patches that evolve slowly over months or even years. It is significant because of its reported potential to evolve into cutaneous T-cell lymphoma; however, PVA does not present with a reticular pattern, nor does it appear acutely.
DISCUSSION
The superficial vascular plexus, configured in a reticular pattern and normally invisible, is sensitive to repeated exposure to the infrared portion of the magnetic spectrum (wavelength 700 to 1,100 nm). This exposure initially produces erythema, which over time turns livid, then permanently hyperpigmented.
Erythema ab igne (EAI) was classically seen in those sitting close to an open fire or stove (producing temperatures of 43°C to 47°C) for extended periods, often for hours each day. With the advent of central heating, other triggers of EAI evolved, including prolonged use of laptop computers, heating fans, and as in this case, heating pads. It can even be due to occupational exposure to intense heat, as with glassblowers, bakers, and steelworkers.
Most of the skin changes seen with EAI resemble those seen with chronic sun damage, including vasodilatation and melanin incontinence with melanophages in the upper dermis.
This particular patient had only one exposure to the heating pad, but had turned it on high and lain on it all night. This produced the changes seen, which will likely become permanently etched in her skin in the exact pattern of the causative heating pad. Months of dexamethasone therapy may also have contributed to the problem, by thinning the patient’s skin enough to render her susceptible to this single exposure to heat.
With EAI patients in general, thought needs to be given to possible underlying issues, such as the source of pain being treated with the heating pad—most commonly, on the low back—or the possible reason for constantly feeling cold, such as anemia or hypothyroidism.
Treatment choices include the application of tretinoin cream or 5-fluorouracil cream, or ablation with laser (YAG, ruby, alexandrite).

A 42-year-old woman presents with discoloration and discomfort involving her back. The discomfort, which started less than 24 hours ago, is not severe, but she is worried about the changes in color she can see in the mirror. Her history is significant for metastatic melanoma. She has been undergoing treatment with chemotherapy and localized radiation and for several months has been taking systemic steroids for intracerebral edema. Additional history taking reveals that the night before the appearance of the skin changes, she fell asleep lying on a heating pad because she was cold. She denies doing this habitually. Examination reveals a large patch of reticular erythema covering the entire central back, sharply sparing the area under the bra strap. The erythema is bounded laterally by sharply demarcated linear margins that mimic the exact shape and size of the heating pad in question. Focal blisters can be seen within the erythema, but the overall effect is macular (flat). Neither tenderness nor increased warmth is noted on palpation.
Skin Change and Fatigue Forces Woman to Take Leave of Absence
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
ANSWER
The correct answer is dermatomyositis (choice “c”), thought to be a vasculopathy mediated by the deposition of complement and lysis of capillaries in skin and muscle.
Carcinoid (choice “a”) is a rare tumor that can release vasoactive peptides, which cause episodic flushing, and if prolonged, can cause permanent changes in the skin. But carcinoid involves neither muscle weakness nor the particular skin changes seen with dermatomyositis.
Lupus erythematosus (choice “b”) can present with similar symptoms. However, when it affects the fingers, it specifically affects the interphalangeal skin, sharply sparing the knuckles. Both lupus erythematosus and mixed connective tissue disease (MCTD; choice “d”) can present with similar changes in the cuticles, but neither present with such profound muscle weakness.
DISCUSSION
Dermatomyositis is one of three main conditions that present with characteristic changes in the cuticular vasculature (the other two being scleroderma and MCTD). The definitive diagnosis is usually made by a rheumatologist, who is able to distinguish dermatomyositis from the rest of the differential—a process that can be rather complex.
The first diagnostic step is to identify the changes to the cuticular vasculature. These must be specifically sought; they are not always as obvious as in this case. Fortunately, magnification can easily be carried out with either an ophthalmoscope or dermatoscope, an examination enhanced by the application of oil first.
These findings, along with sunburn-like eruptions on the neck and face, should prompt laboratory testing. Significant results would include a positive antinuclear antibody test and elevations of the muscle enzymes creatine kinase and aldolase. Skin biopsy is helpful, though not diagnostic by itself. Additional studies might include a barium swallow, which would show weak pharyngeal muscles, and either an electromyography or MRI, which would demonstrate characteristic muscle changes secondary to inflammation.
Perhaps the most important aspect of dermatomyositis is its connection to cancer. A significant percentage of adults diagnosed with dermatomyositis will also have an associated and often occult malignancy, which may be found before, during, or after the diagnosis of dermatomyositis. (Juvenile dermatomyositis is not associated with malignancy.)
Patient age, constitutional symptoms, rapidity of onset, high level of serum muscle enzymes, grossly elevated erythrocyte sedimentation rate, and severity of dermatomyositis are all factors that would prompt an aggressive search for malignancies, the types of which mirror those seen in the general population. In such cases, surgical and/or medical cures of causative cancer usually stop the dermatomyositis as well.
The workup on this particular patient is still underway, but she is already responding to therapy with prednisone (1 mg/kg/d), to be taken until muscle enzymes are normal. This can take months, with dosage reduced as symptoms respond. Steroid-sparing agents, such as methotrexate or azathioprine, are often begun as prednisone levels are reduced.
SUGGESTED READING
James WD, Berger T, Elston D. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders; 2005:166-170.
Bergman R, Sharony L, Schapira D, et al. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8): 1027-1030.
A three-month history of muscle weakness, fatigue, and skin changes prompts a 59-year-old woman to self-refer to dermatology. Otherwise healthy prior to the onset of these symptoms, she has had to take a leave of absence from work due to her inability to carry out her duties, which include light lifting and prolonged periods of time on her feet as a clerk in a pharmacy. She first consulted her primary care provider (PCP), who informed her that she was not anemic and did not have thyroid disease; the PCP felt that stress was probably a factor. She then purchased a number of products from her health food store, which she started taking until the skin on her hands began to change. On examination, atrophic pinkish red planar plaques are noted on 10/10 fingers, confined to the dorsal aspects of her joints and sharply sparing the interphalangeal spaces. The cuticles demonstrate the presence of dilated and irregularly shaped capillary loops. Several of her cuticles are also overgrown and frayed. Examination of the rest of the patient’s skin reveals a blanchable, faintly sunburned appearance to her anterior neck.
Immunosuppressed Woman with Lesion on Her Thumb
ANSWER
The correct answer is basal cell carcinoma (choice “d”), which only rarely affects the hands; it is far more common on more directly sun-exposed skin (eg, face, neck, and back).
Immunosuppressed individuals are at increased risk for squamous cell carcinoma (SCC; choice “a”), particularly those cancers associated with the human papillomavirus. These can present as odd plaques on the hands, so SCC belongs in the differential.
Mycobacterial infection (choice “b”) will demonstrate caseating (necrotic) granulomas and positive stains for acid-fast bacilli such as M marinum or M fortuitum; however, it can manifest with plaques.
Sarcoid (choice “c”) can be lesional and is thought to represent a reaction to an unknown antigen. Often reddish brown in color with plaquish morphology, sarcoid also demonstrates granulomatous changes microscopically; however, these are noncaseating epithelioid granulomas with no palisading.
DISCUSSION
Since granuloma annulare (GA) is notorious for appearing as papules and plaques on the extremities of females, this diagnosis was not a surprise. Often, GA is so obvious that a biopsy is unnecessary. However, given the patient’s immunosuppressed state and the many serious diagnostic possibilities to be ruled out (cancer was a possibility, and had the lesion represented sarcoidosis, it could have been the tip of a serious iceberg involving the liver, lung, or even heart), biopsy was the only option. As is often the case, thought was given to the site selected, in order to avoid damage to local structures or the creation of nonhealing wounds.
GA can occur in several forms, this patient’s case representing the most common one. It can also present as a generalized eruption, in a subcutaneous form, or even with blistering. At one time, it was thought that having GA meant that the patient had or was about to develop diabetes, but that assertion has long since been disproven.
Once diagnosed, GA does not really require treatment since it is self-limiting. However, treatment choices for this form include class 2 steroid creams or liquid nitrogen. This patient opted to do nothing, but she was very relieved to have ruled out more serious disease.
ANSWER
The correct answer is basal cell carcinoma (choice “d”), which only rarely affects the hands; it is far more common on more directly sun-exposed skin (eg, face, neck, and back).
Immunosuppressed individuals are at increased risk for squamous cell carcinoma (SCC; choice “a”), particularly those cancers associated with the human papillomavirus. These can present as odd plaques on the hands, so SCC belongs in the differential.
Mycobacterial infection (choice “b”) will demonstrate caseating (necrotic) granulomas and positive stains for acid-fast bacilli such as M marinum or M fortuitum; however, it can manifest with plaques.
Sarcoid (choice “c”) can be lesional and is thought to represent a reaction to an unknown antigen. Often reddish brown in color with plaquish morphology, sarcoid also demonstrates granulomatous changes microscopically; however, these are noncaseating epithelioid granulomas with no palisading.
DISCUSSION
Since granuloma annulare (GA) is notorious for appearing as papules and plaques on the extremities of females, this diagnosis was not a surprise. Often, GA is so obvious that a biopsy is unnecessary. However, given the patient’s immunosuppressed state and the many serious diagnostic possibilities to be ruled out (cancer was a possibility, and had the lesion represented sarcoidosis, it could have been the tip of a serious iceberg involving the liver, lung, or even heart), biopsy was the only option. As is often the case, thought was given to the site selected, in order to avoid damage to local structures or the creation of nonhealing wounds.
GA can occur in several forms, this patient’s case representing the most common one. It can also present as a generalized eruption, in a subcutaneous form, or even with blistering. At one time, it was thought that having GA meant that the patient had or was about to develop diabetes, but that assertion has long since been disproven.
Once diagnosed, GA does not really require treatment since it is self-limiting. However, treatment choices for this form include class 2 steroid creams or liquid nitrogen. This patient opted to do nothing, but she was very relieved to have ruled out more serious disease.
ANSWER
The correct answer is basal cell carcinoma (choice “d”), which only rarely affects the hands; it is far more common on more directly sun-exposed skin (eg, face, neck, and back).
Immunosuppressed individuals are at increased risk for squamous cell carcinoma (SCC; choice “a”), particularly those cancers associated with the human papillomavirus. These can present as odd plaques on the hands, so SCC belongs in the differential.
Mycobacterial infection (choice “b”) will demonstrate caseating (necrotic) granulomas and positive stains for acid-fast bacilli such as M marinum or M fortuitum; however, it can manifest with plaques.
Sarcoid (choice “c”) can be lesional and is thought to represent a reaction to an unknown antigen. Often reddish brown in color with plaquish morphology, sarcoid also demonstrates granulomatous changes microscopically; however, these are noncaseating epithelioid granulomas with no palisading.
DISCUSSION
Since granuloma annulare (GA) is notorious for appearing as papules and plaques on the extremities of females, this diagnosis was not a surprise. Often, GA is so obvious that a biopsy is unnecessary. However, given the patient’s immunosuppressed state and the many serious diagnostic possibilities to be ruled out (cancer was a possibility, and had the lesion represented sarcoidosis, it could have been the tip of a serious iceberg involving the liver, lung, or even heart), biopsy was the only option. As is often the case, thought was given to the site selected, in order to avoid damage to local structures or the creation of nonhealing wounds.
GA can occur in several forms, this patient’s case representing the most common one. It can also present as a generalized eruption, in a subcutaneous form, or even with blistering. At one time, it was thought that having GA meant that the patient had or was about to develop diabetes, but that assertion has long since been disproven.
Once diagnosed, GA does not really require treatment since it is self-limiting. However, treatment choices for this form include class 2 steroid creams or liquid nitrogen. This patient opted to do nothing, but she was very relieved to have ruled out more serious disease.

Referred by her primary care provider, a 63-year-old woman presents to dermatology for evaluation of an asymptomatic lesion on her thumb. The lesion has slowly grown over a period of years and has persisted despite attempted treatment with topical steroid creams, antifungal cream, and cryotherapy. She denies any other similar occurrences or indeed any skin problems in general. She has a dense medical history, mostly revolving around a heart transplant several years ago that necessitated ongoing immune suppression. This apparently played a role in the development of two squamous cell carcinomas (one on the face, the other on an arm), both successfully dealt with surgically. She admits that as a teenager she tanned and sunburned repeatedly. She specifically denies having diabetes. On examination, the lesion proves to be a reddish brown, roughly ovoid plaque measuring about 3 x 2 cm, located on the medial right thumb. Its surface is smooth and nontender to touch, with no focal papularity and no scaling. Given the failure of previous treatments and the patient’s immunosuppressed state, the decision is made to perform punch biopsy on the site. Care is taken to avoid the neurovascular bundle on the mid-lateral aspect of the digit, and the 3-mm defect is closed with a single nylon suture. The pathology report shows foci of degenerative collagen associated with palisaded granulomatous inflammation.
Dandruff Provides Clue for Rash
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.

A 64-year-old man self-refers to dermatology for evaluation of an asymptomatic rash that has been present on his groin for more than a year. He has tried a number of topical antifungal creams (terbinafine, tolnaftate, and miconazole) and oral antifungal medications (terbinafine and ketoconazole), none of which produced any beneficial effect. The rash, which has been constant and limited to the groin, started around the same time his mother became ill. She eventually succumbed to cancer, leaving a number of stressful tasks for the patient to complete. As a result, the patient had to leave his job and spend a good deal of time away from home, repairing and then selling his mother’s home and possessions. At his first visit to dermatology, the groin rash is bright orange-red, covers both crural areas, and exhibits sharply defined margins that are faintly scaly. However, a KOH prep fails to demonstrate fungal elements, and since a number of antifungal treatments have already been tried without success, a provisional diagnosis of erythrasma is made. The patient is given topical clindamycin solution and oral cephalexin (500 mg tid for a week). Neither of these treatments changes the rash at all, so the man returns for a second visit. Since the rash is asymptomatic, you are not inclined to biopsy it. Clearly, the rash is neither fungal nor bacterial in origin, but in an effort to try something, you go to the supply room seeking samples of a mild steroid cream. When you return to the exam room, you find the man’s wife closely examining his scalp. When you ask what she is looking at, she says she is checking his dandruff, which has been flaring for months. When you look, you see that he does indeed have a brisk case of dandruff. Checking elsewhere, you notice that his external auditory meati are scaly and red, as are the eyebrow, postauricular sulci, and perinasilar areas. There are focally scaly, salmon-pink sites in his beard.
Man with History of Intense Sun Exposure
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
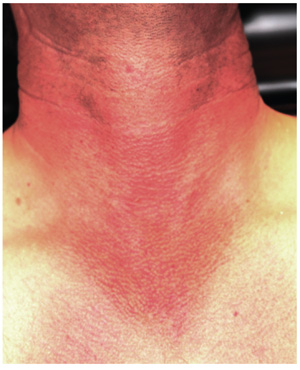
A 36-year-old man urgently self-refers to dermatology for evaluation of skin changes that a friend recently noticed and promptly insisted he seek care for. The patient denies symptoms and has never had any previous medical provider comment on his skin.
He has a long history of overexposure to the sun, as an oil field worker and as a professional bass fisherman on weekends. “If the sun is up, chances are I’m out in it, seven days a week,” is how the patient puts it, adding that he knows he needs sunscreen but has just never bothered with it. At work, he is required to wear a hardhat; in his leisure time, he wears short sleeves and a ball cap, if anything, on his head.
Overall, the patient looks easily 10 years older than his stated age, with splotchy, weathered skin and a very red face on which multiple actinic keratoses are readily noted. With the patient’s shirt off, the primary reason for his visit is apparent: an intensely red, sharply demarcated, blanchable macular V-shaped patch of skin that roughly coincides with the area not usually covered by his shirt. This same process extends onto his anterior neck and cheeks, becoming slightly less intense on posterior neck skin. The U-shaped area of his anterior neck (directly under his chin) is spared, with sharply defined margins between red and white skin.
Examination with 10x magnification reveals a dense mat of fine telangiectatic, blanchable blood vessels comprising the bulk of the erythema. On both sides of the anterolateral neck, rows of sharply defined, 1- to 1.5-mm whitish yellow papules can be seen, virtually covering the area. These gradually thin out, then end, as normal skin is encountered on the upper chest.
Woman Goes Gray - Not Her Hair, Her Face
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
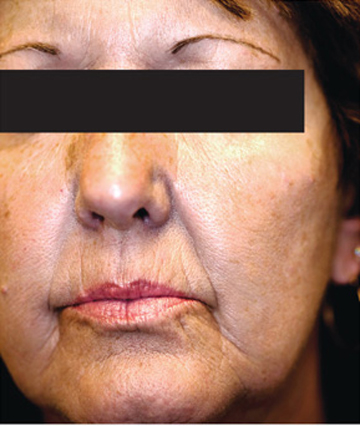
A 61-year-old woman presents with marked changes in her skin that she first noted several months ago. These have become so noticeable that friends and family, growing alarmed, urged her to seek medical evaluation. The patient, who is a hospital nurse, denies taking any prescription medicines (eg, minocycline, amiodarone) during this time. She further denies having any accompanying symptoms in her facial skin. On examination, the patient’s face and neck are markedly discolored—a uniform shade of slate gray. The problem affects her whole body, but is more evident in sun-exposed areas. The discoloration is not blanchable, nor can it be removed by scrubbing the skin with an alcohol-soaked pad. Oral mucosal surfaces, including the gums, are also affected, but less so than the facial skin. These findings prompt additional history taking, with a particular focus on nonprescription medications. As a result, the patient recalls taking an oral colloidal silver–containing solution from the health food store for several months, for reasons she cannot recall.
Patient's Condition is "All Thumbs"
ANSWER
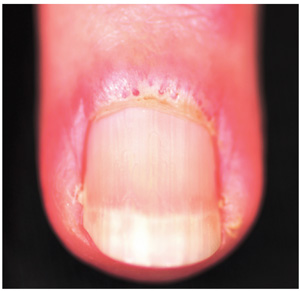
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.
ANSWER
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.
ANSWER
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.

A 56-year-old man is referred to dermatology for evaluation of a “fungal infection” that has affected both thumbnails for at least 20 years. While the condition produces no symptoms, it has nonetheless been a source of constant embarrassment to him. He denies having any such problems with his toenails. Furthermore, he says the problem has persisted despite the use of numerous topical and oral medications, including topical miconazole, clotrimazole, oil of eucalyptus, bleach, and the oral antifungals terbinafine and griseofulvin. None of these has had any effect. Additional history taking reveals that the patient is highly allergy-prone; he had seasonal allergies and asthma as a child. He also has a history of extremely dry and sensitive skin. On examination, the problems with the patient’s thumbnails are obvious, with traumatic absence of cuticles, widening and deepening of the cuticular sulcus, and deep parallel transverse lines involving the entire visible nail plates. Scattered subungual patches of brown discoloration are also seen beneath the lines. None of the patient’s other nails are abnormal in any way.
Pruritic Rash on Both Soles
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.

A 62-year-old woman is referred to dermatology for evaluation of a pruritic rash that has been present on both soles for more than two years. Attempts to treat it with different OTC topical creams (eg, clotrimazole, miconazole), prescription antifungal creams (oxiconazole and nystatin), and even a combination cream (clotrimazole/betamethasone) have been unsuccessful. The last eased her symptoms but yielded no lasting relief. Her primary care provider had prescribed a month-long course of oral terbinafine (250 mg/d). When that did not help, a two-week course of oral antibiotic (cephalexin 500 mg qid) was tried. Neither had any salutary effect, so the patient was referred first to a podiatrist, who quickly sent her to dermatology. Complaining bitterly of itching on these areas, she explains that the condition began with tiny pustules, then tiny blisters that gradually covered both insteps. She denies having any such rash elsewhere (eg, on elbows or knees or in the scalp). There is no known family history of skin problems, and no personal history of arthritis. Just prior to the onset of this problem, she had received a diagnosis of bipolar affective disorder, which forced her to leave her job and start taking lithium. Although the lithium has helped, she remains unable to work. On examination, the skin of both insteps is covered with discrete and confluent papules and tiny pustules on an erythematous and hyperpigmented (brown), sharply demarcated, and highly symmetrical base. As the patient said, her skin, nails, and scalp elsewhere are free of any such lesions. Given her Hispanic ancestry, her skin is phototype IV/VI. Punch biopsy is performed and shows almost no spongiosis or edema, relatively tortuous capillary loops, and collections of neutrophils above foci of parakeratosis. Special stain for fungal elements fails to identify any sign of that family of organisms.
Is A Common Illness The Cause of This Man's Rash?
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.

A 44-year-old man presents with an asymptomatic rash that manifested several weeks ago. His primary care provider called it “ringworm,” but it has been unresponsive to topical antifungal creams, including clotrimazole and tolnaftate. The patient also sought evaluation in an urgent care setting, where the provider diagnosed “psoriasis” and prescribed triamcinolone, which didn’t seem to help. Additional history taking reveals that, two weeks before the lesions appeared, the patient received a diagnosis of strep throat and subsequently was treated with amoxicillin. The patient is otherwise healthy, taking no medications regularly. On examination, the rash is quite striking—brightly erythematous, with annular margins on which the skin is red. But just behind the advancing margin is a parallel band of scaling. At its largest dimension, the papulosquamous patch is slightly in excess of 8 cm. Microscopic examination of scrapings from the lesion’s scale is negative for fungal elements. The rest of the patient’s skin, with particular attention to the feet and groin, is well within normal limits. Punch biopsy of the lesion shows intense lymphohistiocytic cuffing around superficial and deep dermal vessels, with no epidermal involvement. Stains for fungal elements are negative.









