User login
Child of The New Gastroenterologist
New and transitioning gastroenterologists face burnout too
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 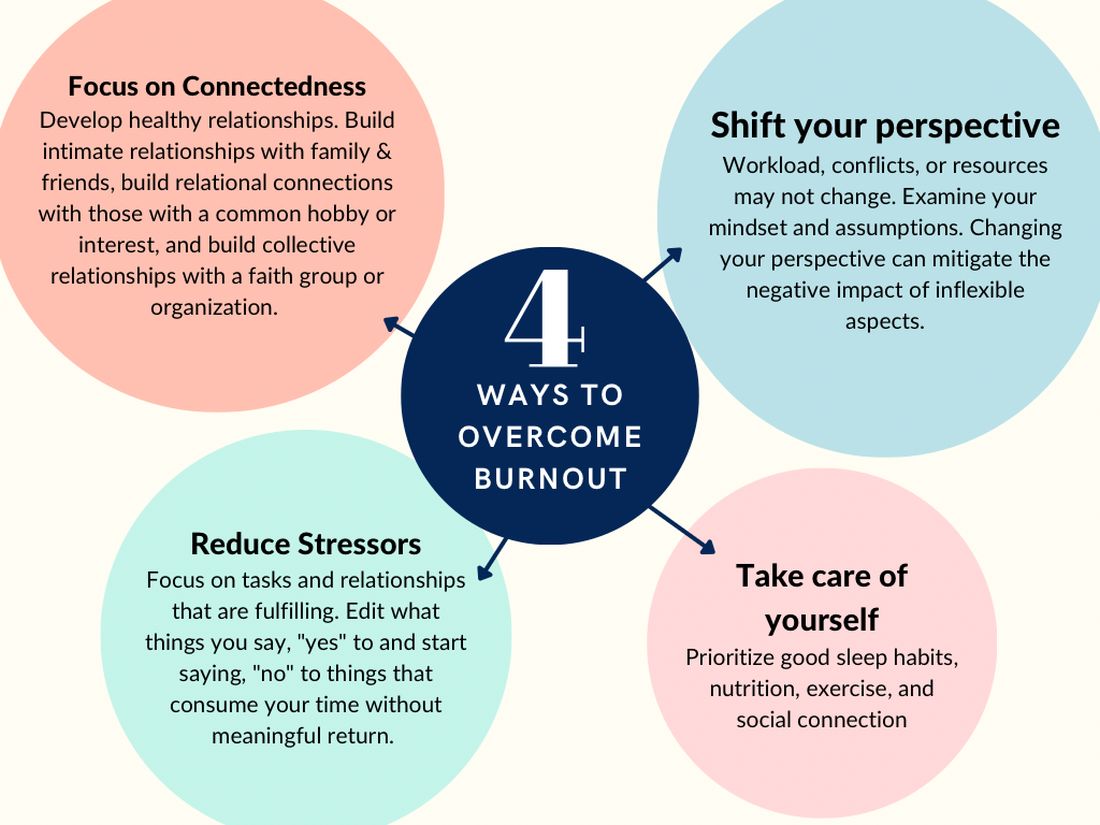
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.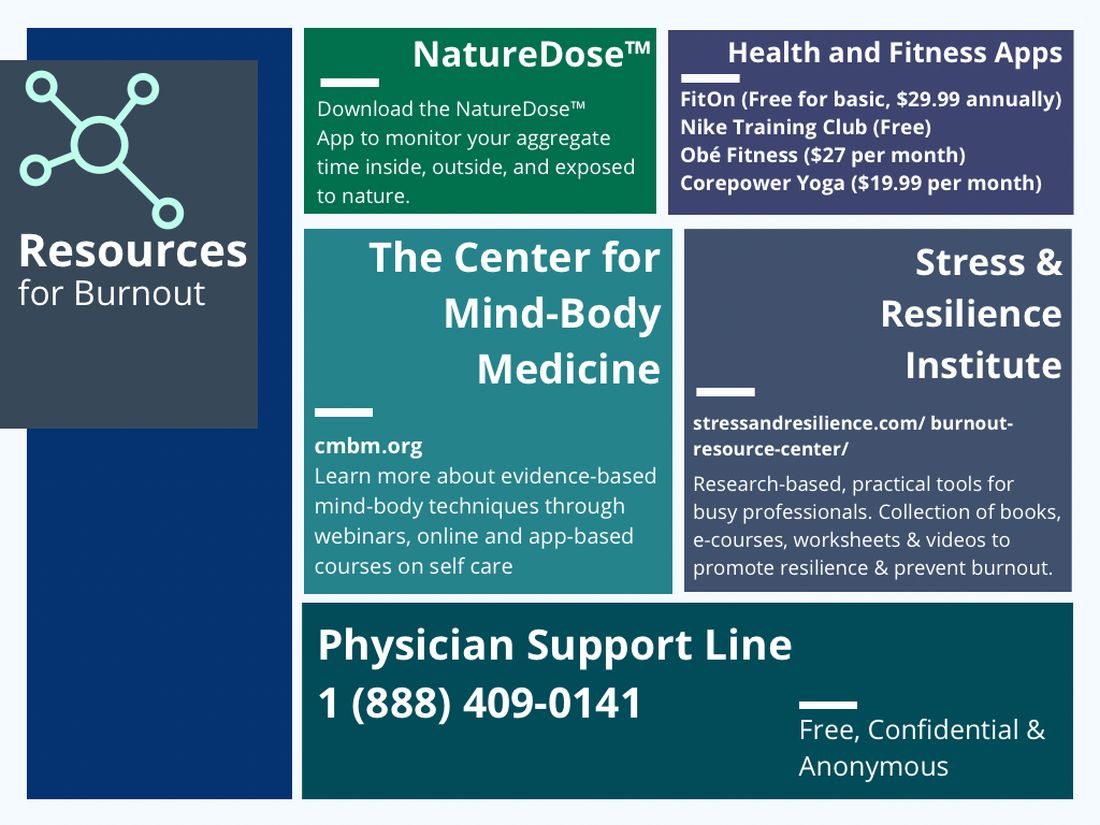
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 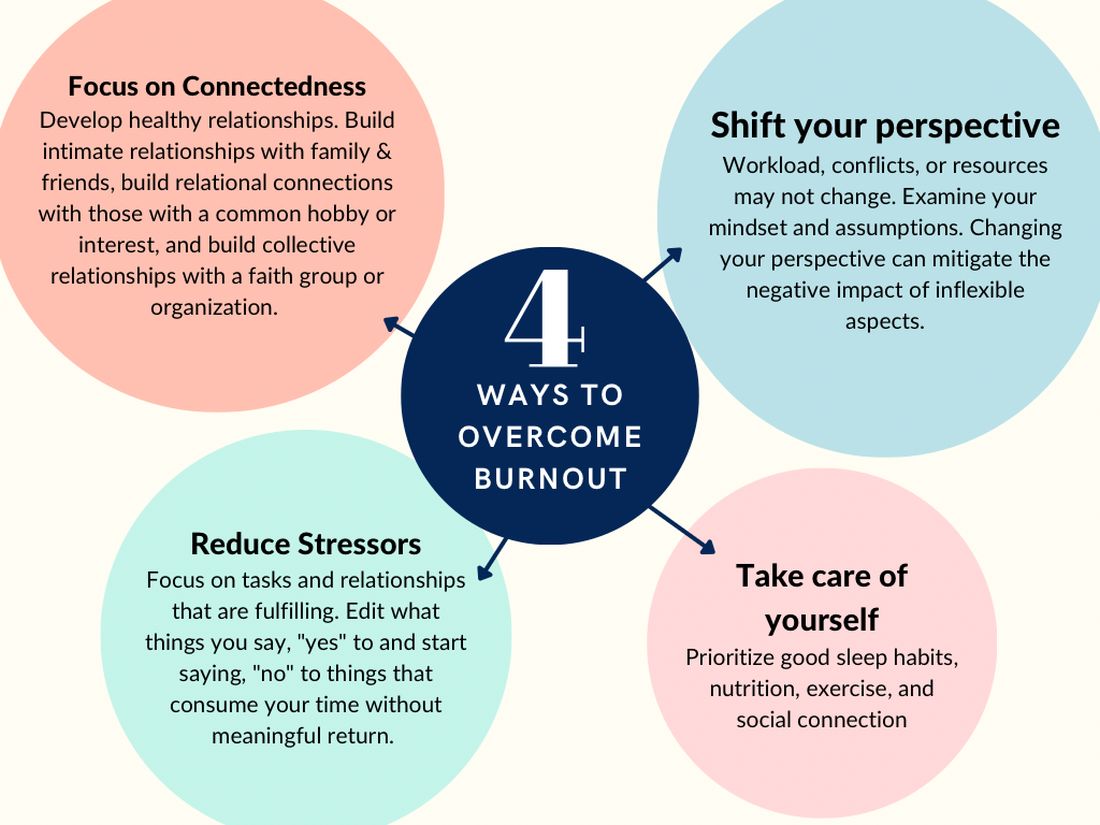
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.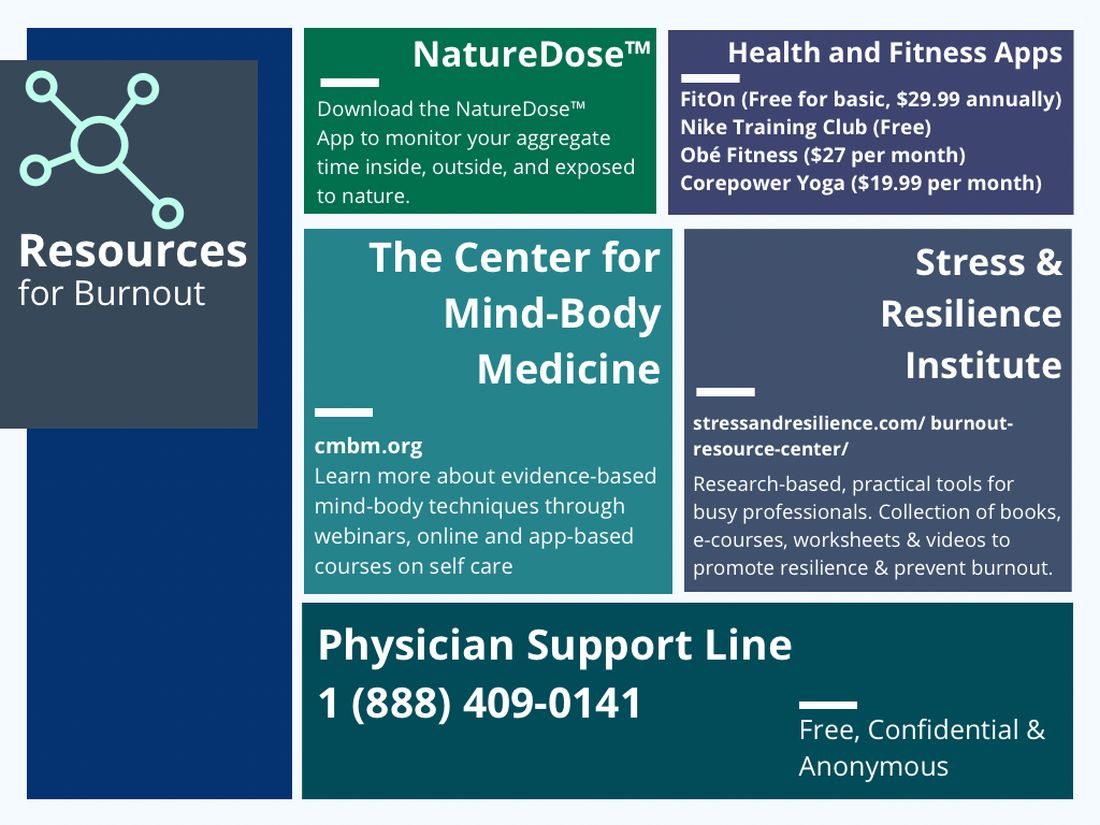
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
The field of gastroenterology can be challenging, both professionally and personally, leading to burnout, especially for new and transitioning gastroenterologists. Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.1 It is characterized by emotional fatigue, depersonalization, and a reduced sense of personal accomplishment.2,3 This condition can have severe consequences for physicians and their patients.
More than 50% of physicians report meeting the criteria for burnout, which is pervasive in all medical professions.3 Survey results of 7,288 U.S. physicians showed that burnout and dissatisfaction with work-life balance are significantly higher than among other working U.S. adults.3
The long and often irregular work hours expected of gastroenterologists significantly contribute to burnout within our field. The physically, intellectually, and technically demanding reality of managing complex patients and making high stakes decisions at all hours has far-reaching consequences.3 Most gastroenterologists work between 55 and 60 hours per week.4 This sharply contrasts the average 43-hour work week for full-time employees in the United States.5 Gastroenterologists may experience inaccurate perceptions of their commitment to patients, education, and their families based solely on time observed on each activity.4 Higher education and professional degrees usually protect against burnout.3 However, a degree in medicine (MD or DO) increases the burnout risk.3
New gastroenterologists are learning a wide range of intricate procedures and becoming proficient in diagnosing and managing gastrointestinal disorders. Extensive career demands often coincide with intense family-forming years, creating tension for a physician’s finite time and energy. The culture of medicine demanding “patients come first” while attempting to be fully human can sometimes feel irreconcilable, leading to feelings of inadequacy and anxiety.3 Gastroenterology training takes 3 years because of the complexity, danger, and need for thousands of procedures to gain proficiency and competence to recognize when complications occur. Oversight is ubiquitous during training, making this the ideal time to learn from mistakes and formulate lifelong habits of constant improvement. However, perfectionist tendencies and the Hippocratic Oath can create unrealistic self expectations.6 The risk of potential litigation, simply missing a diagnosis, or causing actual patient harm is never far from a proceduralist’s mind.
The diversity of gastroenterology requires high clinical knowledge, expertise, and emotional intelligence. Leading potentially intense end-of-life, cancer, fertility, and risk-factor discussions can be all-consuming. Keeping up with the latest research, treatments, and techniques in the field can be daunting. Furthermore, gastroenterologists spend many hours each day on electronic medical records. Constant re-documentation of interactions, seemingly endless prior authorizations, disability forms, referrals, and simply re-addressing patient and family concerns can feel low value. This uncompensated work also creates moral injury as it takes away from direct patient care.
Striking a work-life balance
New gastroenterologists are advised to find work-life balance. However, they are also plagued by the massive professional demands being constantly placed on them. The desire to find the mythical “balance” may create a mindset of significant sacrifices in their private lives as the only way to achieve professional successes.7 When gastroenterologists do not prioritize time for personal activities, including exercise, health checks, hobbies, rest, relaxation, family, and friends, they can get caught in a vicious cycle of continuing to feel poorly, resulting in overcompensating by working more in order to feel “accomplished.” The perfectionist pressure to maintain high productivity and patient satisfaction can also further contribute to burnout.
Gastroenterology burnout can severely affect physicians’ health status, job performance, and patient satisfaction.9 It may erode professionalism, negatively influence the quality of care, increase the risk of medical errors, and promote early retirement.3 Burnout may also correlate with adverse personal consequences for physicians, such as broken relationships, problematic alcohol use, and suicidal ideation.3 Physician burnout and professional satisfaction have strategic importance to health care organizations.10 Less burned-out physicians have patient panels with higher adherence and satisfaction with medical care.10 With more physicians becoming employees, there are opportunities for accountability of organizational leadership.10 Interestingly, healthy well-being or burnout is contagious from leaders to their teams.10 A 2015 study by Shanafelt et al. found that at the work unit level, 11% and 47% of the variation in burnout and satisfaction, correlated with the leader’s relative scores.10
So, what can be done to prevent and treat burnout in new and transitioning gastroenterologists? The gastroenterologist may implement several strategies. It is essential for individuals to take responsibility for their well-being and to prioritize self-care by setting boundaries, practicing stress management techniques, and seeking support from colleagues and mental health professionals when needed. 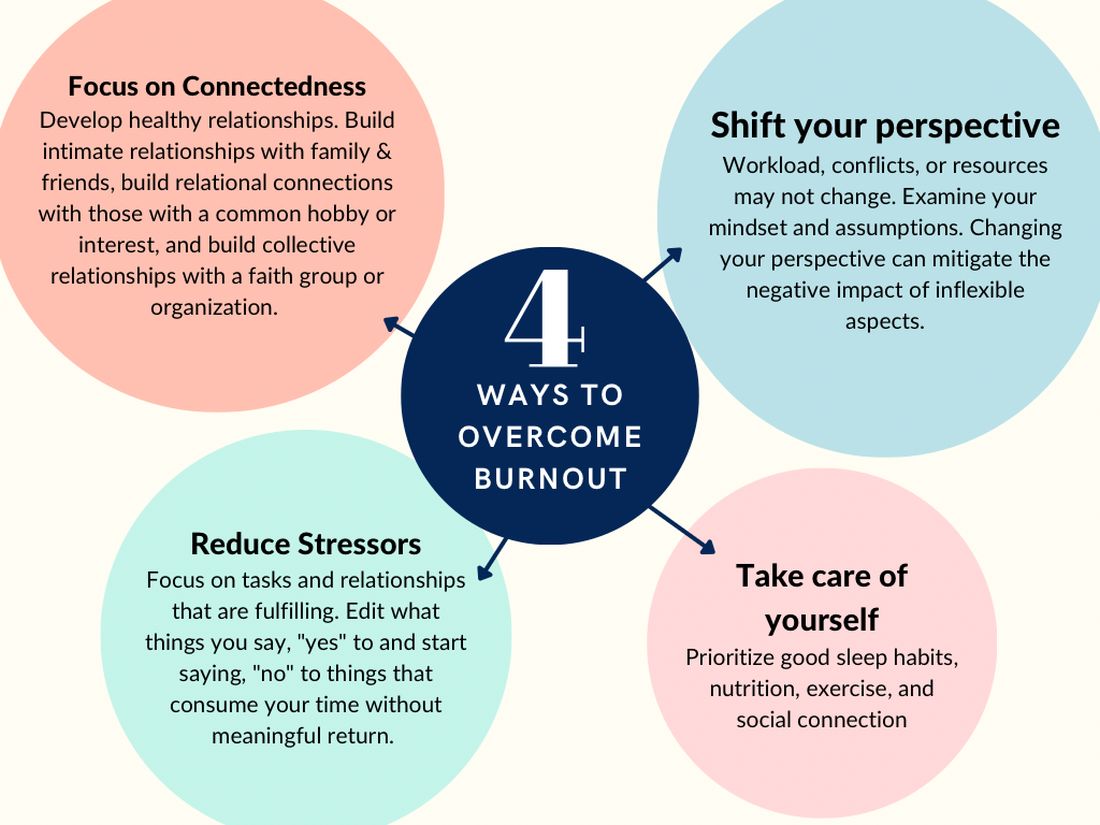
According to Dave et al. (2020), engagement in self-care practices such as mindfulness may offer advantages to gastroenterologists’ well-being and improved patient care.11
Burnout is not due to an individuals’ need for more resiliency. Instead, it developed from a systemic overwhelming of a health system near its breaking point. Recognizing that by 2033, there is a projected shortage of nearly 140,000 physicians in the United States, the U.S. Surgeon General, Dr. Vivek H. Murthy, issued a crisis advisory.12 This advisory highlights the urgent need to address the health worker burnout crisis nationwide that outlined “whole of society” efforts.12 Key components of the advisory on building a thriving health workforce included empowering health care workers, changing policies, reducing administrative burdens, prioritizing connections, and investing in our workforce.12
Provide access to mental health services
Institutions and practices would greatly benefit from providing access to mental health services, counseling, educational opportunities, potential mental health days, and mentorship programs. While the literature indicates that both individual-focused and structural or organizational strategies can result in clinically meaningful reductions in burnout among physicians, a meta-analysis revealed that corporate-led initiatives resulted in larger successes.12,13 Physicians who received support and resources from their institutions report lower levels of burnout and higher job satisfaction.2,3
New strategies to select and develop physician leaders who motivate, inspire, and effectively manage physicians may result in positive job satisfaction while decreasing employee burnout. Therefore, increased awareness of the importance of frontline leadership well-being and professional fulfillment of physicians working for a large health care organization is necessary.13 Robust and continual leadership training can ensure the entire team’s well-being, longevity, and success.13
Addressing the root causes of systemic burnout is imperative. Leadership could streamline administrative processes, optimize electronic medical records, delegate prior authorizations, and ensure staffing levels are appropriate to meet patient care demands. In a survey by Rao et al. (2017), the authors found that physicians who reported high levels of administrative burden and work overload were more likely to experience burnout.14
Institutions and practices should promote a culture of work-life balance by implementing flexible scheduling, promoting time off and vacation time, and encouraging regular exercise and healthy habits. The current compensation structure disincentivizes physicians from taking time away from patient care – this can be re-designed. Community and support mitigate burnout. Therefore, institutions and practices will benefit by intentionally providing opportunities for social connection and team building.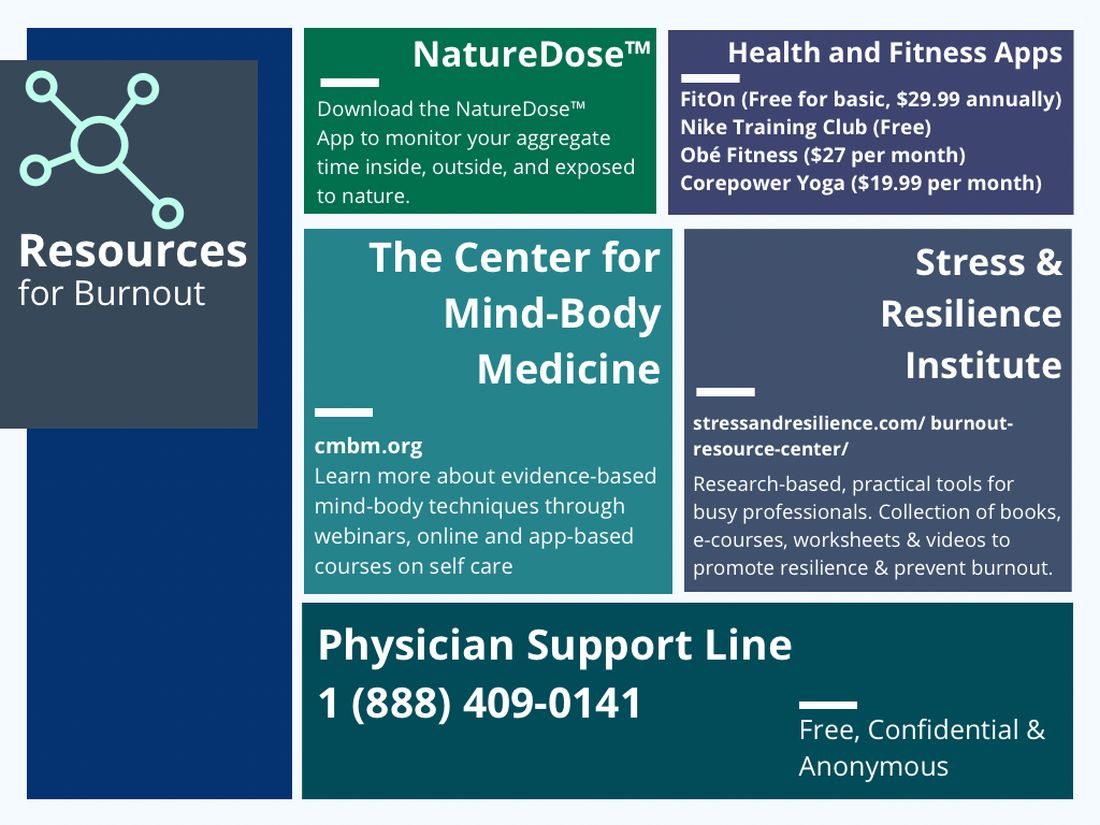
In reflection of the U.S. Surgeon General’s call for all of society to be part of the solution, we are pleased to see the Accreditation Council for Graduate Medical Education (ACGME) create mandatory 6 weeks of parental or caregiver leave for trainees.15 Continued positive pressure on overseeing agencies to minimize paperwork, preauthorizations, and non–value-added tasks to allow physicians to continue to provide medical services instead of documentation and auditing services would greatly positively impact all of health care. Therefore, communicating with legislators, policy makers, system leadership, and all health care societies to continue these improvements would be a wise use of time of resources.
In conclusion, burnout among new and transitioning gastroenterologists is a prevalent and concerning issue that can have severe consequences for both the individual and the health care system. Similar to the ergonomic considerations of being an endoscopist, A multifaceted approach to the well-being of all medical staff can help ensure the delivery of the highest quality patient care. By taking a proactive approach to preventing burnout, we can have a strong future for ourselves, our patients, and our profession.
Dr. Eboh is a gastroenterologist with Atrium Health, Charlotte, N.C.; Dr. Jaeger is with Baylor Scott & White Medical Center in Dallas. She is a gastroenterology fellow with Temple University Hospital, Philadelphia. Dr. Sears is clinical professor at Texas A&M University School of Medicine, and chief of gastroenterology at VA Central Texas Healthcare System. Dr. Sears owns GutGirlMD Consulting LLC, where she offers institutional and leadership coaching for physicians. Dr. Eboh on Instagram @Polyp.picker_EbohMD and on Twitter @PolypPicker_MD. Dr. Jaeger on Instagram @Doc.Tori.Fit and Twitter @DrToriJaeger. Dr. Sears is on Twitter @GutGirlMD.
References
1. Maslach C and Jackson S E. Maslach burnout inventory manual. Palo Alto, Calif: Consulting Psychologists Press, 1986.
2. Shanafelt TD et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015 Dec 12;90:1600-13.
3. Shanafelt TD et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85.
4. Elta G. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
5. Gallup. Work and Workplace. 2023.
6. Gawande A. When doctors make mistakes. The New Yorker. 1999 Feb 1.
7. Buscarini E et al. Burnout among gastroenterologists: How to manage and prevent it. United European Gastroenterol J. 2020 Aug;8(7):832-4.
8. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016 Nov 5;388(10057):2272-81.
9. Adarkwah CC et al. Burnout and work satisfaction are differentially associated in gastroenterologists in Germany. F1000Res. 2022 Mar 30;11:368. doi: 10.12688/f1000research.110296.3. eCollection 2022.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015 Apr;90(4):432-40.
11. Umakant D et al. Mindfulness in gastroenterology training and practice: A personal perspective. Clin Exp Gastroenterol. 2020 Nov 4;13:497-502.
12. Murthy VH. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. The U.S. Department of Health and Human Services: Office of the U.S. Surgeon General, 2022.
13. Panagioti M et al. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern Med. 2017 Feb 1;177(2):195-205.
14. Rao SK et al. The impact of administrative burden on academic physicians: Results of a hospital-wide physician survey. Acad Med. 2017 Feb;92(2):237-43.
15. ACGME. ACME Institutional Requirements 2021.
Establishing an advanced endoscopy practice: Tips for trainees and early faculty
Establishing an advanced endoscopy practice can appear challenging and overwhelming. It is often the culmination of more than a decade of education and training for advanced endoscopists and is usually their first foray into employment. all while creating a rewarding opportunity to provide a population with necessary services, which, more than likely, were not previously being offered at your institution or in your region.
Tip 1: Understand the current landscape
When joining a hospital-employed or private practice, it is important for the advanced endoscopist to gauge the current landscape of the job, beginning with gaining an understanding of the current services provided by your gastroenterology colleagues. This includes knowing the types of advanced endoscopy services previously provided, especially if you have partners or colleagues who perform these procedures, and their prior referral patterns, either within or outside their respective group. Also, it is important to understand the services that are provided locally at other institutions. This will allow you to develop a niche of the types of services you can provide that are not available in the current practice set-up.
Tip 2: Connect with peers, interspecialty collaborators, and referring physicians
It is important that you connect with your GI colleagues once you start a new job. This can differ in ease depending on the size of your group. For example, in a small group, it may be easier to familiarize yourself with your colleagues through regular interactions. If you are a part of a larger practice, however, it is necessary to be more proactive and set up introductory meetings/sessions. These interactions provide a great opportunity to share your goals and start building a relationship.
Efforts also should be made to reach out to primary care, hematology/oncology, surgical/radiation oncology, general surgery, and interventional radiology physicians, as these are the specialists with whom an advanced endoscopist typically has the most interaction. The relationship with these colleagues is bidirectional, as the majority of our patients need multidisciplinary decision-making and care. For example, the first time you speak to the colorectal surgeon at your institution should not be in the middle of a complication. The purpose of these introductions should not be solely to inform them of the services you are offering but to start developing a relationship in a true sense, because eventually those relationships will transform into excellent patient care.
Tip 3: Communication
Communication is a key principle in building a practice. Referring physicians often entrust you with managing a part of their patient’s medical problems. Patient/procedure outcomes should be relayed promptly to referring physicians, as this not only helps build the trust of the referring physician, but also enhances the patient’s trust in the health system, knowing that all physicians are communicating with the common goal of improving the patient’s disease course.
Communication with the referring physician is important not only after a procedure but also before it. Know that a consult is an “ask for help.” For example, even if you are not the correct specialist for a referral (for example, an inflammatory bowel disease patient was sent to an advanced endoscopist), it is good practice to take ownership of the patient and forward that person to the appropriate colleague.
Tip 4: Build a local reputation
Building upon this, it is also important to connect with other GI groups in the community, regardless of whether they have their own affiliated advanced endoscopists. This helps determine the advanced endoscopy services being offered regionally, which will further allow an understanding of the unmet needs of the region. In addition, building a relationship with local advanced endoscopists in the region can help establish a collaborative relationship going forward, rather than a contentious/competitive dynamic.
Tip 5: Advance your skills
As advanced endoscopy fellows are aware, completing an advanced endoscopy fellowship allows for building a strong foundation of skills, which will continue to refine and grow as you advance in your career.
Depending on your skill-set and training, the first year should focus on developing and establishing “your style” (since the training is tailored to follow the practice patterns of your mentors). The first few months are good to focus on refining endoscopic ultrasound, endoscopic retrograde cholangiopancreatography, endoscopic mucosal resection, and luminal stenting techniques. As you start to build a reputation of being “safe, thoughtful, and skilled” and depending on your interests and goals, continued engagement in the advanced endoscopy community to understand new technologies/procedures is helpful. It is important to remember that new skills and procedures can be introduced in your practice, but this should be done in a timely and patient manner. You should appropriately educate and train yourself for such procedures through educational conferences/courses, shadowing and routine engagement with mentors, and collaboration with industry partners.
Tip 6: Team building
From a procedural standpoint, certain staff members should be recognized to be part of or lead an “advanced endoscopy team,” with a goal of dedicated exposure to a high volume of complex procedures. This builds camaraderie and trust within the team of advanced endoscopy nurses and technicians going forward, which is crucial to introducing and building a high-complexity procedural service. This is also an excellent opportunity to partner with our industry colleagues to ensure that they can train your team on the use of novel devices.
Tip 7: Offering new services to your patients
Advanced endoscopy is a rapidly evolving specialty, and new procedures, technology, and devices are allowing us to provide minimally invasive options to our patients. It is important that prior to introducing new services and programs, your hospital/practice administration should be informed about any such plans. Also, all potential collaborating services (surgery, interventional radiology, etc.) should be part of the decision-making to ensure patients receive the best possible multidisciplinary care.
Tip 8: Mentorship and peer-mentorship
Establishing a network of regional and national advanced endoscopy colleagues and mentors is critical. This may be harder to develop in community-based and private practice, where one may feel that they are on an “island.” Engagement with national organizations, use of social media, and other avenues are excellent ways to build this network. Advanced endoscopic procedures also are associated with higher rates of adverse events, so having a peer-support group to provide emotional and moral support when these adverse events occur also is important. Such a network also includes those collaborating specialties to which you would refer (surgical oncology, thoracic surgery, etc.). Being involved in local tumor boards and “gut clubs” is another way of remaining engaged and not feeling isolated.
Tip 9: Have fun
Advanced endoscopy can be busy, as well as physically and mentally exhausting. It is important to maintain a good work-life balance. In addition, planning scheduled retreats or social events with your advanced endoscopy team (nurses, technicians, schedulers, colleagues) is important not only to show appreciation, but also to help build camaraderie and develop relationships.
Tip 10: Remember your ‘why’
Often times, there can be stressors associated with building a practice and increasing your volume, therefore, it is always important to remember why you became a medical professional and advanced endoscopist. This will get you through the days where you had a complication or when things didn’t go as planned.
Conclusion
Lastly, it is important to keep revisiting your skill sets and practice and evaluate what is working well and what can be improved. To all the advanced endoscopists starting their careers: Be patient and have a positive attitude! The leaders in our field did not become so overnight, and an advanced endoscopy–based career resembles a marathon rather than a sprint. Mistakes during procedures and practice building can be made, but how you grow and learn from those mistakes is what determines how likely you are to succeed going forward. Respect and acknowledge your staff, your collaborating physicians, and mentors. It takes time and effort to develop an advanced endoscopy practice. Being proud of your achievements and promoting procedural and patient care advances that you have made are beneficial and encouraged. We are fortunate to be in an ever-evolving specialty, and it is an exciting time to be practicing advanced endoscopy. Good luck!
Dr. Soudagar is a gastroenterologist at Northwestern Medical Group, Lake Forest, Ill. Dr. Bilal, assistant professor of medicine at the University of Minnesota, Minneapolis, is an advanced endoscopist and gastroenterologist at Minneapolis VA Medical Center. The authors have no conflicts of interest.
Establishing an advanced endoscopy practice can appear challenging and overwhelming. It is often the culmination of more than a decade of education and training for advanced endoscopists and is usually their first foray into employment. all while creating a rewarding opportunity to provide a population with necessary services, which, more than likely, were not previously being offered at your institution or in your region.
Tip 1: Understand the current landscape
When joining a hospital-employed or private practice, it is important for the advanced endoscopist to gauge the current landscape of the job, beginning with gaining an understanding of the current services provided by your gastroenterology colleagues. This includes knowing the types of advanced endoscopy services previously provided, especially if you have partners or colleagues who perform these procedures, and their prior referral patterns, either within or outside their respective group. Also, it is important to understand the services that are provided locally at other institutions. This will allow you to develop a niche of the types of services you can provide that are not available in the current practice set-up.
Tip 2: Connect with peers, interspecialty collaborators, and referring physicians
It is important that you connect with your GI colleagues once you start a new job. This can differ in ease depending on the size of your group. For example, in a small group, it may be easier to familiarize yourself with your colleagues through regular interactions. If you are a part of a larger practice, however, it is necessary to be more proactive and set up introductory meetings/sessions. These interactions provide a great opportunity to share your goals and start building a relationship.
Efforts also should be made to reach out to primary care, hematology/oncology, surgical/radiation oncology, general surgery, and interventional radiology physicians, as these are the specialists with whom an advanced endoscopist typically has the most interaction. The relationship with these colleagues is bidirectional, as the majority of our patients need multidisciplinary decision-making and care. For example, the first time you speak to the colorectal surgeon at your institution should not be in the middle of a complication. The purpose of these introductions should not be solely to inform them of the services you are offering but to start developing a relationship in a true sense, because eventually those relationships will transform into excellent patient care.
Tip 3: Communication
Communication is a key principle in building a practice. Referring physicians often entrust you with managing a part of their patient’s medical problems. Patient/procedure outcomes should be relayed promptly to referring physicians, as this not only helps build the trust of the referring physician, but also enhances the patient’s trust in the health system, knowing that all physicians are communicating with the common goal of improving the patient’s disease course.
Communication with the referring physician is important not only after a procedure but also before it. Know that a consult is an “ask for help.” For example, even if you are not the correct specialist for a referral (for example, an inflammatory bowel disease patient was sent to an advanced endoscopist), it is good practice to take ownership of the patient and forward that person to the appropriate colleague.
Tip 4: Build a local reputation
Building upon this, it is also important to connect with other GI groups in the community, regardless of whether they have their own affiliated advanced endoscopists. This helps determine the advanced endoscopy services being offered regionally, which will further allow an understanding of the unmet needs of the region. In addition, building a relationship with local advanced endoscopists in the region can help establish a collaborative relationship going forward, rather than a contentious/competitive dynamic.
Tip 5: Advance your skills
As advanced endoscopy fellows are aware, completing an advanced endoscopy fellowship allows for building a strong foundation of skills, which will continue to refine and grow as you advance in your career.
Depending on your skill-set and training, the first year should focus on developing and establishing “your style” (since the training is tailored to follow the practice patterns of your mentors). The first few months are good to focus on refining endoscopic ultrasound, endoscopic retrograde cholangiopancreatography, endoscopic mucosal resection, and luminal stenting techniques. As you start to build a reputation of being “safe, thoughtful, and skilled” and depending on your interests and goals, continued engagement in the advanced endoscopy community to understand new technologies/procedures is helpful. It is important to remember that new skills and procedures can be introduced in your practice, but this should be done in a timely and patient manner. You should appropriately educate and train yourself for such procedures through educational conferences/courses, shadowing and routine engagement with mentors, and collaboration with industry partners.
Tip 6: Team building
From a procedural standpoint, certain staff members should be recognized to be part of or lead an “advanced endoscopy team,” with a goal of dedicated exposure to a high volume of complex procedures. This builds camaraderie and trust within the team of advanced endoscopy nurses and technicians going forward, which is crucial to introducing and building a high-complexity procedural service. This is also an excellent opportunity to partner with our industry colleagues to ensure that they can train your team on the use of novel devices.
Tip 7: Offering new services to your patients
Advanced endoscopy is a rapidly evolving specialty, and new procedures, technology, and devices are allowing us to provide minimally invasive options to our patients. It is important that prior to introducing new services and programs, your hospital/practice administration should be informed about any such plans. Also, all potential collaborating services (surgery, interventional radiology, etc.) should be part of the decision-making to ensure patients receive the best possible multidisciplinary care.
Tip 8: Mentorship and peer-mentorship
Establishing a network of regional and national advanced endoscopy colleagues and mentors is critical. This may be harder to develop in community-based and private practice, where one may feel that they are on an “island.” Engagement with national organizations, use of social media, and other avenues are excellent ways to build this network. Advanced endoscopic procedures also are associated with higher rates of adverse events, so having a peer-support group to provide emotional and moral support when these adverse events occur also is important. Such a network also includes those collaborating specialties to which you would refer (surgical oncology, thoracic surgery, etc.). Being involved in local tumor boards and “gut clubs” is another way of remaining engaged and not feeling isolated.
Tip 9: Have fun
Advanced endoscopy can be busy, as well as physically and mentally exhausting. It is important to maintain a good work-life balance. In addition, planning scheduled retreats or social events with your advanced endoscopy team (nurses, technicians, schedulers, colleagues) is important not only to show appreciation, but also to help build camaraderie and develop relationships.
Tip 10: Remember your ‘why’
Often times, there can be stressors associated with building a practice and increasing your volume, therefore, it is always important to remember why you became a medical professional and advanced endoscopist. This will get you through the days where you had a complication or when things didn’t go as planned.
Conclusion
Lastly, it is important to keep revisiting your skill sets and practice and evaluate what is working well and what can be improved. To all the advanced endoscopists starting their careers: Be patient and have a positive attitude! The leaders in our field did not become so overnight, and an advanced endoscopy–based career resembles a marathon rather than a sprint. Mistakes during procedures and practice building can be made, but how you grow and learn from those mistakes is what determines how likely you are to succeed going forward. Respect and acknowledge your staff, your collaborating physicians, and mentors. It takes time and effort to develop an advanced endoscopy practice. Being proud of your achievements and promoting procedural and patient care advances that you have made are beneficial and encouraged. We are fortunate to be in an ever-evolving specialty, and it is an exciting time to be practicing advanced endoscopy. Good luck!
Dr. Soudagar is a gastroenterologist at Northwestern Medical Group, Lake Forest, Ill. Dr. Bilal, assistant professor of medicine at the University of Minnesota, Minneapolis, is an advanced endoscopist and gastroenterologist at Minneapolis VA Medical Center. The authors have no conflicts of interest.
Establishing an advanced endoscopy practice can appear challenging and overwhelming. It is often the culmination of more than a decade of education and training for advanced endoscopists and is usually their first foray into employment. all while creating a rewarding opportunity to provide a population with necessary services, which, more than likely, were not previously being offered at your institution or in your region.
Tip 1: Understand the current landscape
When joining a hospital-employed or private practice, it is important for the advanced endoscopist to gauge the current landscape of the job, beginning with gaining an understanding of the current services provided by your gastroenterology colleagues. This includes knowing the types of advanced endoscopy services previously provided, especially if you have partners or colleagues who perform these procedures, and their prior referral patterns, either within or outside their respective group. Also, it is important to understand the services that are provided locally at other institutions. This will allow you to develop a niche of the types of services you can provide that are not available in the current practice set-up.
Tip 2: Connect with peers, interspecialty collaborators, and referring physicians
It is important that you connect with your GI colleagues once you start a new job. This can differ in ease depending on the size of your group. For example, in a small group, it may be easier to familiarize yourself with your colleagues through regular interactions. If you are a part of a larger practice, however, it is necessary to be more proactive and set up introductory meetings/sessions. These interactions provide a great opportunity to share your goals and start building a relationship.
Efforts also should be made to reach out to primary care, hematology/oncology, surgical/radiation oncology, general surgery, and interventional radiology physicians, as these are the specialists with whom an advanced endoscopist typically has the most interaction. The relationship with these colleagues is bidirectional, as the majority of our patients need multidisciplinary decision-making and care. For example, the first time you speak to the colorectal surgeon at your institution should not be in the middle of a complication. The purpose of these introductions should not be solely to inform them of the services you are offering but to start developing a relationship in a true sense, because eventually those relationships will transform into excellent patient care.
Tip 3: Communication
Communication is a key principle in building a practice. Referring physicians often entrust you with managing a part of their patient’s medical problems. Patient/procedure outcomes should be relayed promptly to referring physicians, as this not only helps build the trust of the referring physician, but also enhances the patient’s trust in the health system, knowing that all physicians are communicating with the common goal of improving the patient’s disease course.
Communication with the referring physician is important not only after a procedure but also before it. Know that a consult is an “ask for help.” For example, even if you are not the correct specialist for a referral (for example, an inflammatory bowel disease patient was sent to an advanced endoscopist), it is good practice to take ownership of the patient and forward that person to the appropriate colleague.
Tip 4: Build a local reputation
Building upon this, it is also important to connect with other GI groups in the community, regardless of whether they have their own affiliated advanced endoscopists. This helps determine the advanced endoscopy services being offered regionally, which will further allow an understanding of the unmet needs of the region. In addition, building a relationship with local advanced endoscopists in the region can help establish a collaborative relationship going forward, rather than a contentious/competitive dynamic.
Tip 5: Advance your skills
As advanced endoscopy fellows are aware, completing an advanced endoscopy fellowship allows for building a strong foundation of skills, which will continue to refine and grow as you advance in your career.
Depending on your skill-set and training, the first year should focus on developing and establishing “your style” (since the training is tailored to follow the practice patterns of your mentors). The first few months are good to focus on refining endoscopic ultrasound, endoscopic retrograde cholangiopancreatography, endoscopic mucosal resection, and luminal stenting techniques. As you start to build a reputation of being “safe, thoughtful, and skilled” and depending on your interests and goals, continued engagement in the advanced endoscopy community to understand new technologies/procedures is helpful. It is important to remember that new skills and procedures can be introduced in your practice, but this should be done in a timely and patient manner. You should appropriately educate and train yourself for such procedures through educational conferences/courses, shadowing and routine engagement with mentors, and collaboration with industry partners.
Tip 6: Team building
From a procedural standpoint, certain staff members should be recognized to be part of or lead an “advanced endoscopy team,” with a goal of dedicated exposure to a high volume of complex procedures. This builds camaraderie and trust within the team of advanced endoscopy nurses and technicians going forward, which is crucial to introducing and building a high-complexity procedural service. This is also an excellent opportunity to partner with our industry colleagues to ensure that they can train your team on the use of novel devices.
Tip 7: Offering new services to your patients
Advanced endoscopy is a rapidly evolving specialty, and new procedures, technology, and devices are allowing us to provide minimally invasive options to our patients. It is important that prior to introducing new services and programs, your hospital/practice administration should be informed about any such plans. Also, all potential collaborating services (surgery, interventional radiology, etc.) should be part of the decision-making to ensure patients receive the best possible multidisciplinary care.
Tip 8: Mentorship and peer-mentorship
Establishing a network of regional and national advanced endoscopy colleagues and mentors is critical. This may be harder to develop in community-based and private practice, where one may feel that they are on an “island.” Engagement with national organizations, use of social media, and other avenues are excellent ways to build this network. Advanced endoscopic procedures also are associated with higher rates of adverse events, so having a peer-support group to provide emotional and moral support when these adverse events occur also is important. Such a network also includes those collaborating specialties to which you would refer (surgical oncology, thoracic surgery, etc.). Being involved in local tumor boards and “gut clubs” is another way of remaining engaged and not feeling isolated.
Tip 9: Have fun
Advanced endoscopy can be busy, as well as physically and mentally exhausting. It is important to maintain a good work-life balance. In addition, planning scheduled retreats or social events with your advanced endoscopy team (nurses, technicians, schedulers, colleagues) is important not only to show appreciation, but also to help build camaraderie and develop relationships.
Tip 10: Remember your ‘why’
Often times, there can be stressors associated with building a practice and increasing your volume, therefore, it is always important to remember why you became a medical professional and advanced endoscopist. This will get you through the days where you had a complication or when things didn’t go as planned.
Conclusion
Lastly, it is important to keep revisiting your skill sets and practice and evaluate what is working well and what can be improved. To all the advanced endoscopists starting their careers: Be patient and have a positive attitude! The leaders in our field did not become so overnight, and an advanced endoscopy–based career resembles a marathon rather than a sprint. Mistakes during procedures and practice building can be made, but how you grow and learn from those mistakes is what determines how likely you are to succeed going forward. Respect and acknowledge your staff, your collaborating physicians, and mentors. It takes time and effort to develop an advanced endoscopy practice. Being proud of your achievements and promoting procedural and patient care advances that you have made are beneficial and encouraged. We are fortunate to be in an ever-evolving specialty, and it is an exciting time to be practicing advanced endoscopy. Good luck!
Dr. Soudagar is a gastroenterologist at Northwestern Medical Group, Lake Forest, Ill. Dr. Bilal, assistant professor of medicine at the University of Minnesota, Minneapolis, is an advanced endoscopist and gastroenterologist at Minneapolis VA Medical Center. The authors have no conflicts of interest.
Tips for getting involved with industry
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Introduction
The professional activity of physicians has traditionally consisted of patient care, teaching/education, and research in varying proportions. These aims, especially education and research, have traditionally been achieved in academic health settings. However, involvement with industry can afford all physicians an opportunity to increase patient referrals, gain exposure to colleagues through a variety of educational opportunities, and participate in meaningful research projects they could not initiate independently.
How to initiate relationships with industry
Here are several ways to initiate a collaboration with industry. A few of the most common ways are to become a site investigator of a multicenter device or pharmaceutical trial, participate as a member of a speaker’s bureau, or obtain training on a new technology and subsequently incorporate it into your clinical practice. To find out what trials are enrolling and looking for additional sites or new studies that are being planned, I would suggest contacting the company’s local representative and have them put you in touch the appropriate personnel in the clinical trials division. For individuals who become involved in trials, this can be a great way to improve your understanding of how to design and conduct clinical trials as well as gain exposure to colleagues with similar clinical and research interests. Some of my closest long-term collaborators and friends have been individuals who I initially met as part of industry trials at investigator meetings. Another approach is to participate in a speaker’s bureau, which can be an excellent way to improve one’s presentation skills as well as gain knowledge with respect to a specific disease state. It is also a great way to network, meet colleagues, and develop a local and regional reputation as a content expert on a specific topic. Methods to find out about such opportunities include touring the exhibit halls during educational meetings and reading scientific journals to identify new products that are launching. I have found these sorts of opportunities can significantly increase topic-based referrals. Finally, obtaining training on a new diagnostic or therapeutic technology (usually through an industry-sponsored course) can allow individuals an opportunity to offer a unique or distinctive service to their community. In addition, as further clinical expertise is gained, the relationship can be expanded to offer local, regional, or even national training courses to colleagues via either on-site or virtual courses. Similarly, opportunities to speak about or demonstrate the technology/technique at educational courses may also follow.
Navigating and expanding the relationship
Once an individual establishes a relationship with a company or has established a reputation as a key opinion leader, additional opportunities for engagement may become available. These include serving as a consultant, becoming a member of an advisory board, participating or directing educational courses for trainees/practitioners, or serving as the principal investigator of a future clinical trial. Serving as a consultant can be quite rewarding as it can highlight clinical needs, identify where product improvement can be achieved, and focus where research and development funds should be directed. Serving on the advisory board can afford an even higher level of influence where corporate strategy can be influenced. Such input is particularly impactful with smaller companies looking to enter a new field or expand a limited market share. There are also a variety of educational opportunities offered by industry including local, regional, and national courses that focus on utilizing a new technology or education concerning a specific disease state. These courses can be held locally at the physician’s clinical site or off site to attract the desired target audience. Finally, being involved in research studies, especially early-stage projects, can be critical as many small companies have limited capital, and it is essential for them to design studies with appropriate endpoints that will ideally achieve both regulatory approval as well as payor coverage. Of note, in addition to relationships directly involving industry, the American Gastroenterological Association Center for GI Innovation and Technology (CGIT) also offers the opportunity to be part of key opinion leader meetings arranged and organized by the AGA. This may allow for some individuals to participate who may be restricted from direct relationships with industry partners. The industry services offered by the CGIT also include clinical trial design and registry management services.
Entrepreneurship/intellectual property
A less commonly explored opportunity with industry involves the development of one’s own intellectual property. Some of the most impactful technologies in my advanced endoscopy clinical practice have been developed from the ideas of gastroenterology colleagues that have been successfully commercialized. These include radiofrequency ablation technology to treat Barrett’s esophagus and the development of lumen-apposing stents. There are several options for physicians with an idea for an innovation. These can include working with a university technology transfer department if they are in an academic setting, creation of their own company, or collaborating with industry to develop the device through a licensing/royalty agreement. The AGA CGIT offers extensive resources to physicians with new ideas on how to secure their intellectual property as well as to evaluate the feasibility of the aforementioned options to choose which may be most appropriate for them.
Important caveats
It is important that physicians with industry relations be aware of their local institutional policies. Some institutions may prohibit such activities while others may limit the types of relationships or the amount of income that can be received. It is the physician’s responsibility to be aware of their institution’s guidelines prior to formalizing industry agreements. If intellectual property is involved, it is essential to know the specific rules regarding physician remuneration, especially pertaining to royalty or equity agreements. Furthermore, with regard to presentations and publications, it is required to acknowledge industry relations and potential conflicts of interest. Failure to do so may adversely affect an individual’s reputation as well as lead to additional consequences such as the potential for retraction of publications or restrictions regarding future educational speaking opportunities. In addition, key opinion leaders often consult for several companies that may be in competition with each other. Therefore, it is essential that there is no disclosure of confidential proprietary information among companies. Finally, the financial incentives resulting from industry collaboration should never influence physician judgment when interpreting or speaking about data regarding product efficacy or safety.
Conclusions
In summary, there are numerous opportunities for physicians to collaborate with industry. These relationships can be very rewarding and can serve to expedite the introduction of new diagnostic or treatment modalities and provide the opportunity to network and interact with colleagues as well as to participate in important research that improves clinical practice. The nature of these relationships should always be transparent, and it is the physician’s responsibility to ensure that the types of relationships that are engaged in are permitted by their employer. Over the course of my career, I have participated in nearly all forms of these relationships and have seen that participation lead to important publications, changes in corporate strategy, the fostering of acquisitions, and the rapid development and utilization of new endoscopic technologies. It is my personal belief than industry relationships can improve professional satisfaction, enhance one’s brand, and most importantly, expedite clinical innovation to improve patient care.
Dr. Muthusamy is professor of clinical medicine at the University of California, Los Angeles, and medical director of endoscopy, UCLA Health System. He disclosed ties with Medtronic, Boston Scientific, Motus GI, Endogastric Solutions, and Capsovision.
Becoming an AGA committee chair as an early-career physician
One of the cornerstones of member engagement within the American Gastroenterological Association is its committees, which provide a platform for AGA members to network, effect change at the institutional level, and obtain leadership positions. For many within the AGA, exposure to these committees occurs during training. Both of us were first introduced to the possibility of serving on an AGA committee by faculty members at our institution. Each year, applications for available committee positions open in the fall and are due on Nov. 1. While you can be nominated by other members, self-nomination is common and encouraged. Truthfully, neither of us was quite certain what committee membership would entail. However, we both applied to several committees because we knew that it would be an excellent opportunity to network with leading gastroenterologists across the country and to have the ability to become involved in key AGA programs.
We were selected to serve 2-year terms as trainee members on the Government Affairs and Publication Committees, respectively, which gave us a deeper understanding of how an organization with both a full-time professional staff and group of volunteer members functions. A unique feature of the AGA is its Trainee and Early Career (TEC) Committee, which mainly comprises trainee members who serve on other committees. By virtue of our roles with the other committees, we also became full-fledged members of the TEC committee, which is dedicated to enhancing the experience for trainees and those who are within 5 years of graduation.
One of the most innovative programs developed by the TEC committee is Career Development Workshops, which is a webinar series focused on important topics not covered in fellowship, such as different career paths, personal finance, and how to increase the number of underrepresented individuals in the field. The predecessor of the Career Development Workshops was the in-person Regional Practice Skills Workshop, and we both took on the responsibility of planning and organizing separate workshops. For one of us (Stephanie), that involved enlisting our fellowship program to host the event. For the other (Peter), it meant collaborating with our local gastroenterology society to cosponsor the workshop. It was extremely rewarding to organize the workshops, which allowed us to work closely with AGA staff and local gastroenterology faculty, as well as our peers, to bring the events to fruition. For both of us, the success of the Regional Practice Skills Workshop was one of the highlights of our tenure on the TEC committee.
Although we were not aware of it at the time, volunteering to plan a workshop and assisting with other projects and subcommittees were signs of enthusiasm and leadership that the AGA recognized and valued. Our advice on becoming a committee chair is to not only show an interest in committee projects but also to turn that interest into action. A committee member who is strongly interested in a leadership position cannot expect to transition into that role by being a “silent but present” member. You need to do more than just show up. You should actively participate in projects, engage in discussions, and devote your time and energy to ensure the success of committee programs. However, you should also make sure to have sufficient bandwidth to make meaningful contributions to each project and not commit to tasks that you cannot complete. To set yourself apart on a committee, it is important to be actively engaged and committed to a project (or two) that allows for professional growth and visibility. Ideally, you will become an integral part of a committee that sparks your drive to serve.
Applying to become a committee chair follows the same process and timeline as for any other committee position, and you can be nominated or self-nominate. Although previous experience on that specific committee is not a prerequisite for most chair positions, having previously served on any AGA committee or task force is generally required. Successful applicants serve for 1 year as chair-elect, during which they work closely with the outgoing chair and staff to ensure a smooth transition when their 3-year term as chair officially begins in June.
Each committee has a guiding mission statement and a staff liaison who provides institutional knowledge and logistical support. However, the committee members, and especially the chair, have considerable latitude to develop and implement new initiatives or retire old ones. The entire committee meets twice per year, once in September in Washington, D.C., and once at DDW. Between the meetings, working groups are formed to move the various programs forward. In addition to the Career Development Workshops, the TEC committee organizes the Young Delegates program (which allows any AGA member to volunteer on small, time-limited projects), a symposium at DDW focused on trainee and early career issues, and a networking event at DDW. Moreover, we collaborate with other committees and provide input from the perspective of younger members on larger initiatives such as the AGA Equity Project and Career Compass.
As chair, we lead the twice-yearly meetings as well as the working groups. We strongly encourage all committee members to participate on at least one working group, which develops leadership skills and provides the opportunity to moderate sessions for the Career Development Workshops and DDW symposium. Moreover, we solicit feedback on ways to improve current programming, start new initiatives, and work with other committees that the TEC committee members are part of. Trainees and early career members are seen as a key constituency group within the AGA, and we take the responsibility of increasing the value of membership for this group seriously.
As early-career physicians ourselves, we also view the chance to serve as a committee chair as a great career development opportunity. It allows us to expand our professional networks, help shape an organization that is a leading voice and advocate for digestive health, and meet the needs of young members who are the future of the AGA.
There is no doubt that all of you have achieved amazing things on the way to becoming a trainee or early career professional in the competitive fields of gastroenterology and hepatology. The AGA is constantly looking for bright, motivated individuals to serve as volunteers and future leaders. Our experience shows that with a bit of persistence to get in the door – through Young Delegates or a committee – along with lots of hard work along the way, you will be in a great position to rise through the ranks and help lead an organization at the vanguard of our field.
Dr. Liang is assistant professor of medicine and population health, New York University Langone Health, and a staff physician at VA New York Harbor Health Care System. Dr. Pointer is a founder and managing partner of Digestive and Liver Health Specialists. She is on staff as a clinical gastroenterologist at Tristar Hendersonville (Tenn.) Medical Center. They have no conflicts of interest.
One of the cornerstones of member engagement within the American Gastroenterological Association is its committees, which provide a platform for AGA members to network, effect change at the institutional level, and obtain leadership positions. For many within the AGA, exposure to these committees occurs during training. Both of us were first introduced to the possibility of serving on an AGA committee by faculty members at our institution. Each year, applications for available committee positions open in the fall and are due on Nov. 1. While you can be nominated by other members, self-nomination is common and encouraged. Truthfully, neither of us was quite certain what committee membership would entail. However, we both applied to several committees because we knew that it would be an excellent opportunity to network with leading gastroenterologists across the country and to have the ability to become involved in key AGA programs.
We were selected to serve 2-year terms as trainee members on the Government Affairs and Publication Committees, respectively, which gave us a deeper understanding of how an organization with both a full-time professional staff and group of volunteer members functions. A unique feature of the AGA is its Trainee and Early Career (TEC) Committee, which mainly comprises trainee members who serve on other committees. By virtue of our roles with the other committees, we also became full-fledged members of the TEC committee, which is dedicated to enhancing the experience for trainees and those who are within 5 years of graduation.
One of the most innovative programs developed by the TEC committee is Career Development Workshops, which is a webinar series focused on important topics not covered in fellowship, such as different career paths, personal finance, and how to increase the number of underrepresented individuals in the field. The predecessor of the Career Development Workshops was the in-person Regional Practice Skills Workshop, and we both took on the responsibility of planning and organizing separate workshops. For one of us (Stephanie), that involved enlisting our fellowship program to host the event. For the other (Peter), it meant collaborating with our local gastroenterology society to cosponsor the workshop. It was extremely rewarding to organize the workshops, which allowed us to work closely with AGA staff and local gastroenterology faculty, as well as our peers, to bring the events to fruition. For both of us, the success of the Regional Practice Skills Workshop was one of the highlights of our tenure on the TEC committee.
Although we were not aware of it at the time, volunteering to plan a workshop and assisting with other projects and subcommittees were signs of enthusiasm and leadership that the AGA recognized and valued. Our advice on becoming a committee chair is to not only show an interest in committee projects but also to turn that interest into action. A committee member who is strongly interested in a leadership position cannot expect to transition into that role by being a “silent but present” member. You need to do more than just show up. You should actively participate in projects, engage in discussions, and devote your time and energy to ensure the success of committee programs. However, you should also make sure to have sufficient bandwidth to make meaningful contributions to each project and not commit to tasks that you cannot complete. To set yourself apart on a committee, it is important to be actively engaged and committed to a project (or two) that allows for professional growth and visibility. Ideally, you will become an integral part of a committee that sparks your drive to serve.
Applying to become a committee chair follows the same process and timeline as for any other committee position, and you can be nominated or self-nominate. Although previous experience on that specific committee is not a prerequisite for most chair positions, having previously served on any AGA committee or task force is generally required. Successful applicants serve for 1 year as chair-elect, during which they work closely with the outgoing chair and staff to ensure a smooth transition when their 3-year term as chair officially begins in June.
Each committee has a guiding mission statement and a staff liaison who provides institutional knowledge and logistical support. However, the committee members, and especially the chair, have considerable latitude to develop and implement new initiatives or retire old ones. The entire committee meets twice per year, once in September in Washington, D.C., and once at DDW. Between the meetings, working groups are formed to move the various programs forward. In addition to the Career Development Workshops, the TEC committee organizes the Young Delegates program (which allows any AGA member to volunteer on small, time-limited projects), a symposium at DDW focused on trainee and early career issues, and a networking event at DDW. Moreover, we collaborate with other committees and provide input from the perspective of younger members on larger initiatives such as the AGA Equity Project and Career Compass.
As chair, we lead the twice-yearly meetings as well as the working groups. We strongly encourage all committee members to participate on at least one working group, which develops leadership skills and provides the opportunity to moderate sessions for the Career Development Workshops and DDW symposium. Moreover, we solicit feedback on ways to improve current programming, start new initiatives, and work with other committees that the TEC committee members are part of. Trainees and early career members are seen as a key constituency group within the AGA, and we take the responsibility of increasing the value of membership for this group seriously.
As early-career physicians ourselves, we also view the chance to serve as a committee chair as a great career development opportunity. It allows us to expand our professional networks, help shape an organization that is a leading voice and advocate for digestive health, and meet the needs of young members who are the future of the AGA.
There is no doubt that all of you have achieved amazing things on the way to becoming a trainee or early career professional in the competitive fields of gastroenterology and hepatology. The AGA is constantly looking for bright, motivated individuals to serve as volunteers and future leaders. Our experience shows that with a bit of persistence to get in the door – through Young Delegates or a committee – along with lots of hard work along the way, you will be in a great position to rise through the ranks and help lead an organization at the vanguard of our field.
Dr. Liang is assistant professor of medicine and population health, New York University Langone Health, and a staff physician at VA New York Harbor Health Care System. Dr. Pointer is a founder and managing partner of Digestive and Liver Health Specialists. She is on staff as a clinical gastroenterologist at Tristar Hendersonville (Tenn.) Medical Center. They have no conflicts of interest.
One of the cornerstones of member engagement within the American Gastroenterological Association is its committees, which provide a platform for AGA members to network, effect change at the institutional level, and obtain leadership positions. For many within the AGA, exposure to these committees occurs during training. Both of us were first introduced to the possibility of serving on an AGA committee by faculty members at our institution. Each year, applications for available committee positions open in the fall and are due on Nov. 1. While you can be nominated by other members, self-nomination is common and encouraged. Truthfully, neither of us was quite certain what committee membership would entail. However, we both applied to several committees because we knew that it would be an excellent opportunity to network with leading gastroenterologists across the country and to have the ability to become involved in key AGA programs.
We were selected to serve 2-year terms as trainee members on the Government Affairs and Publication Committees, respectively, which gave us a deeper understanding of how an organization with both a full-time professional staff and group of volunteer members functions. A unique feature of the AGA is its Trainee and Early Career (TEC) Committee, which mainly comprises trainee members who serve on other committees. By virtue of our roles with the other committees, we also became full-fledged members of the TEC committee, which is dedicated to enhancing the experience for trainees and those who are within 5 years of graduation.
One of the most innovative programs developed by the TEC committee is Career Development Workshops, which is a webinar series focused on important topics not covered in fellowship, such as different career paths, personal finance, and how to increase the number of underrepresented individuals in the field. The predecessor of the Career Development Workshops was the in-person Regional Practice Skills Workshop, and we both took on the responsibility of planning and organizing separate workshops. For one of us (Stephanie), that involved enlisting our fellowship program to host the event. For the other (Peter), it meant collaborating with our local gastroenterology society to cosponsor the workshop. It was extremely rewarding to organize the workshops, which allowed us to work closely with AGA staff and local gastroenterology faculty, as well as our peers, to bring the events to fruition. For both of us, the success of the Regional Practice Skills Workshop was one of the highlights of our tenure on the TEC committee.
Although we were not aware of it at the time, volunteering to plan a workshop and assisting with other projects and subcommittees were signs of enthusiasm and leadership that the AGA recognized and valued. Our advice on becoming a committee chair is to not only show an interest in committee projects but also to turn that interest into action. A committee member who is strongly interested in a leadership position cannot expect to transition into that role by being a “silent but present” member. You need to do more than just show up. You should actively participate in projects, engage in discussions, and devote your time and energy to ensure the success of committee programs. However, you should also make sure to have sufficient bandwidth to make meaningful contributions to each project and not commit to tasks that you cannot complete. To set yourself apart on a committee, it is important to be actively engaged and committed to a project (or two) that allows for professional growth and visibility. Ideally, you will become an integral part of a committee that sparks your drive to serve.
Applying to become a committee chair follows the same process and timeline as for any other committee position, and you can be nominated or self-nominate. Although previous experience on that specific committee is not a prerequisite for most chair positions, having previously served on any AGA committee or task force is generally required. Successful applicants serve for 1 year as chair-elect, during which they work closely with the outgoing chair and staff to ensure a smooth transition when their 3-year term as chair officially begins in June.
Each committee has a guiding mission statement and a staff liaison who provides institutional knowledge and logistical support. However, the committee members, and especially the chair, have considerable latitude to develop and implement new initiatives or retire old ones. The entire committee meets twice per year, once in September in Washington, D.C., and once at DDW. Between the meetings, working groups are formed to move the various programs forward. In addition to the Career Development Workshops, the TEC committee organizes the Young Delegates program (which allows any AGA member to volunteer on small, time-limited projects), a symposium at DDW focused on trainee and early career issues, and a networking event at DDW. Moreover, we collaborate with other committees and provide input from the perspective of younger members on larger initiatives such as the AGA Equity Project and Career Compass.
As chair, we lead the twice-yearly meetings as well as the working groups. We strongly encourage all committee members to participate on at least one working group, which develops leadership skills and provides the opportunity to moderate sessions for the Career Development Workshops and DDW symposium. Moreover, we solicit feedback on ways to improve current programming, start new initiatives, and work with other committees that the TEC committee members are part of. Trainees and early career members are seen as a key constituency group within the AGA, and we take the responsibility of increasing the value of membership for this group seriously.
As early-career physicians ourselves, we also view the chance to serve as a committee chair as a great career development opportunity. It allows us to expand our professional networks, help shape an organization that is a leading voice and advocate for digestive health, and meet the needs of young members who are the future of the AGA.
There is no doubt that all of you have achieved amazing things on the way to becoming a trainee or early career professional in the competitive fields of gastroenterology and hepatology. The AGA is constantly looking for bright, motivated individuals to serve as volunteers and future leaders. Our experience shows that with a bit of persistence to get in the door – through Young Delegates or a committee – along with lots of hard work along the way, you will be in a great position to rise through the ranks and help lead an organization at the vanguard of our field.
Dr. Liang is assistant professor of medicine and population health, New York University Langone Health, and a staff physician at VA New York Harbor Health Care System. Dr. Pointer is a founder and managing partner of Digestive and Liver Health Specialists. She is on staff as a clinical gastroenterologist at Tristar Hendersonville (Tenn.) Medical Center. They have no conflicts of interest.
Become a highly effective endoscopy teacher, from start to finish
When I first became an attending, I was struck by how difficult it was to teach endoscopy effectively. As a fellow, I saw the various teaching styles of my attendings, and it was easy to pick out the best teachers from the group. But when the roles switched, and suddenly I was the supervising faculty member, it was hard to recall exactly what those teachers were doing to create an optimal learning environment in the endoscopy suite. Not only did I lack a framework on how to teach endoscopy, I also was still building confidence in my own endoscopic skills while feeling the pressure to keep my room running on time. All in all, although I loved the opportunity to teach, I found the experience to be quite stressful.
Hoping to find some guidance, I turned to the literature and was fortunate to find some great pieces on how to teach endoscopy effectively. I learned of cognitive load theory – the idea that short-term or “working memory” can manage only a few pieces of information at a time – and how excess feedback or other external distractions (e.g., pagers) during a procedure can overwhelm a learner and lead to declining performance.1 I also read about the pursuit of “conscious competence,” where an endoscopist can verbalize the steps of a maneuver so that a trainee can remain on the scope and maximize hands-on participation.2
Motivated to bring these key concepts together in an evidence-based framework, I helped lead a Delphi study of GI fellowship program directors and endoscopy education experts to reach consensus on the best practices of teaching endoscopy.3 After two rounds of surveys, the participants identified 10 essential endoscopy teaching practices, which I will summarize in the next sections. What I found most helpful was how these practices were distributed throughout the endoscopy learning experience. By breaking down the complicated task of teaching endoscopy to three discrete parts – prior to the procedure, during the procedure, and after the procedure – I now had a framework to take back to the endoscopy suite.
Prior to the procedure
With a busy endoscopy schedule and increasing clinical demands, it is tempting to use the time between cases to complete documentation, address patient messages, and review emails. While this is great for efficiency, make sure to also reserve time to set the stage for your fellow. One of the key practices during this phase is to assess your fellow’s current procedural competency. I start open-ended by asking my fellows how they have been doing with colonoscopy and then ask if they are working on a specific skill. With this information, I have a sense of how much hands-on assistance they will need, what realistic goals to set for them (e.g., navigate out of the sigmoid colon for an early learner vs. efficiently and independently completing the entire case for a later learner), and the areas to focus my observation to provide feedback after the procedure.
During this preparatory time, faculty should also discuss the patient history and indications for the procedure. Reviewing information such as prior sedation requirements and confirming plans for the procedure (e.g., random colon biopsies in a patient with chronic diarrhea and concern for microscopic colitis) helps ensure a proper plan is in place for the patient while also presenting opportunities for learning. Faculty can take this time to review the steps of a more complicated procedure (e.g., PEG placement) and establish ground rules such as when the attending will take the scope from the trainee. Lastly, make sure that the patient understands the role of the fellow and the supervision you will be providing throughout the case.
During the procedure
Once the procedure starts, your most important task is to maintain attention throughout the case – if you do, the other best practices generally fall into place. I am most attentive when I am gowned and positioned next to the fellow. From this vantage point, I can see the patient, the fellow’s hands, and the endoscopy screen, which allows me to readily assist if needed while directly observing the fellow’s performance.
If I need to provide feedback in the moment, I often ask the fellows to pause what they are doing and first listen to my feedback. Taking this “timeout” helps manage their cognitive load such that they can actually hear the feedback. As a general rule, however, I try to reserve the bulk of my feedback for when the procedure is complete (see next section). Another way to manage your fellow’s cognitive load is by using standardized endoscopic language throughout the procedure. For example, rather than say “go to the left” during a colonoscopy, try saying “tip left” or “torque counterclockwise” to provide more clear instructions to the fellow. Holding your fellow’s pager during the procedure is a kind gesture that also helps minimize extraneous cognitive load so that the fellow can focus on the procedure.
If your fellows get to a point where they cannot complete the task despite your giving appropriate feedback, or if patient safety concerns arise, then it is time for you to take hands-on control of the scope. In my experience, most fellows welcome the hands-on assistance as they are overloaded by the difficulty of the procedure. Setting this expectation ahead of time, as noted above, makes for a smoother transition. While assuming control of the scope, try to narrate what you are doing differently so that the fellow can still learn while watching. Once you complete the difficult portion of the procedure (e.g., reducing a loop to reach the cecum), return the scope to the fellow to maximize the hands-on participation (if time permits).
After the procedure
In the third and final stage of the endoscopy teaching experience, faculty should take the time to confirm the findings of the procedure with the fellow and discuss next steps in management for the patient. Finding these teachable moments helps solidify the cognitive learning for the fellow while also ensuring the patient receives the appropriate postprocedure recommendations. As part of this process, make sure to review the procedure note drafted by the fellow, and if you need to make any substantive edits, review the changes with the fellow so that he or she can learn for future cases.
To wrap up the session, provide feedback to the fellow on performance based on your direct observation. Make sure to name this process aloud – “Let’s do some feedback” – and start by asking how the fellow felt about the performance, both in terms of what went well and what the fellow would like to improve. Then provide your feedback on the performance and be specific, such as, “I really like how you identified a loop and then reduced around the hepatic flexure.” Conclude by having the fellow set a plan for improvement and make sure to ask for feedback on your own teaching performance.
In conclusion, teaching endoscopy is hard – especially as a junior attending. By breaking down the endoscopy teaching experience into its three components, however, and committing to teaching from start to finish, you can provide high-quality endoscopy education to your fellows while ensuring the best care for your patients.
Dr. Kumar is associate medicine clerkship director at Harvard Medical School, and associate physician in the division of gastroenterology at Brigham and Women’s Hospital, both in Boston. He disclosed having no conflicts of interest. He is on Twitter @NavinKumarMD.
References
1. Dilly CK and Sewell JL. 2017 Sep;153(3):632-36.
2. Waschke KA et al. Best Pract Res Clin Gastroenterol. 2016 Jun;30(3):409-19.
3. Kumar NL et al. Clin Gastroenterol Hepatol. 2020 Mar;18(3):574-79.
When I first became an attending, I was struck by how difficult it was to teach endoscopy effectively. As a fellow, I saw the various teaching styles of my attendings, and it was easy to pick out the best teachers from the group. But when the roles switched, and suddenly I was the supervising faculty member, it was hard to recall exactly what those teachers were doing to create an optimal learning environment in the endoscopy suite. Not only did I lack a framework on how to teach endoscopy, I also was still building confidence in my own endoscopic skills while feeling the pressure to keep my room running on time. All in all, although I loved the opportunity to teach, I found the experience to be quite stressful.
Hoping to find some guidance, I turned to the literature and was fortunate to find some great pieces on how to teach endoscopy effectively. I learned of cognitive load theory – the idea that short-term or “working memory” can manage only a few pieces of information at a time – and how excess feedback or other external distractions (e.g., pagers) during a procedure can overwhelm a learner and lead to declining performance.1 I also read about the pursuit of “conscious competence,” where an endoscopist can verbalize the steps of a maneuver so that a trainee can remain on the scope and maximize hands-on participation.2
Motivated to bring these key concepts together in an evidence-based framework, I helped lead a Delphi study of GI fellowship program directors and endoscopy education experts to reach consensus on the best practices of teaching endoscopy.3 After two rounds of surveys, the participants identified 10 essential endoscopy teaching practices, which I will summarize in the next sections. What I found most helpful was how these practices were distributed throughout the endoscopy learning experience. By breaking down the complicated task of teaching endoscopy to three discrete parts – prior to the procedure, during the procedure, and after the procedure – I now had a framework to take back to the endoscopy suite.
Prior to the procedure
With a busy endoscopy schedule and increasing clinical demands, it is tempting to use the time between cases to complete documentation, address patient messages, and review emails. While this is great for efficiency, make sure to also reserve time to set the stage for your fellow. One of the key practices during this phase is to assess your fellow’s current procedural competency. I start open-ended by asking my fellows how they have been doing with colonoscopy and then ask if they are working on a specific skill. With this information, I have a sense of how much hands-on assistance they will need, what realistic goals to set for them (e.g., navigate out of the sigmoid colon for an early learner vs. efficiently and independently completing the entire case for a later learner), and the areas to focus my observation to provide feedback after the procedure.
During this preparatory time, faculty should also discuss the patient history and indications for the procedure. Reviewing information such as prior sedation requirements and confirming plans for the procedure (e.g., random colon biopsies in a patient with chronic diarrhea and concern for microscopic colitis) helps ensure a proper plan is in place for the patient while also presenting opportunities for learning. Faculty can take this time to review the steps of a more complicated procedure (e.g., PEG placement) and establish ground rules such as when the attending will take the scope from the trainee. Lastly, make sure that the patient understands the role of the fellow and the supervision you will be providing throughout the case.
During the procedure
Once the procedure starts, your most important task is to maintain attention throughout the case – if you do, the other best practices generally fall into place. I am most attentive when I am gowned and positioned next to the fellow. From this vantage point, I can see the patient, the fellow’s hands, and the endoscopy screen, which allows me to readily assist if needed while directly observing the fellow’s performance.
If I need to provide feedback in the moment, I often ask the fellows to pause what they are doing and first listen to my feedback. Taking this “timeout” helps manage their cognitive load such that they can actually hear the feedback. As a general rule, however, I try to reserve the bulk of my feedback for when the procedure is complete (see next section). Another way to manage your fellow’s cognitive load is by using standardized endoscopic language throughout the procedure. For example, rather than say “go to the left” during a colonoscopy, try saying “tip left” or “torque counterclockwise” to provide more clear instructions to the fellow. Holding your fellow’s pager during the procedure is a kind gesture that also helps minimize extraneous cognitive load so that the fellow can focus on the procedure.
If your fellows get to a point where they cannot complete the task despite your giving appropriate feedback, or if patient safety concerns arise, then it is time for you to take hands-on control of the scope. In my experience, most fellows welcome the hands-on assistance as they are overloaded by the difficulty of the procedure. Setting this expectation ahead of time, as noted above, makes for a smoother transition. While assuming control of the scope, try to narrate what you are doing differently so that the fellow can still learn while watching. Once you complete the difficult portion of the procedure (e.g., reducing a loop to reach the cecum), return the scope to the fellow to maximize the hands-on participation (if time permits).
After the procedure
In the third and final stage of the endoscopy teaching experience, faculty should take the time to confirm the findings of the procedure with the fellow and discuss next steps in management for the patient. Finding these teachable moments helps solidify the cognitive learning for the fellow while also ensuring the patient receives the appropriate postprocedure recommendations. As part of this process, make sure to review the procedure note drafted by the fellow, and if you need to make any substantive edits, review the changes with the fellow so that he or she can learn for future cases.
To wrap up the session, provide feedback to the fellow on performance based on your direct observation. Make sure to name this process aloud – “Let’s do some feedback” – and start by asking how the fellow felt about the performance, both in terms of what went well and what the fellow would like to improve. Then provide your feedback on the performance and be specific, such as, “I really like how you identified a loop and then reduced around the hepatic flexure.” Conclude by having the fellow set a plan for improvement and make sure to ask for feedback on your own teaching performance.
In conclusion, teaching endoscopy is hard – especially as a junior attending. By breaking down the endoscopy teaching experience into its three components, however, and committing to teaching from start to finish, you can provide high-quality endoscopy education to your fellows while ensuring the best care for your patients.
Dr. Kumar is associate medicine clerkship director at Harvard Medical School, and associate physician in the division of gastroenterology at Brigham and Women’s Hospital, both in Boston. He disclosed having no conflicts of interest. He is on Twitter @NavinKumarMD.
References
1. Dilly CK and Sewell JL. 2017 Sep;153(3):632-36.
2. Waschke KA et al. Best Pract Res Clin Gastroenterol. 2016 Jun;30(3):409-19.
3. Kumar NL et al. Clin Gastroenterol Hepatol. 2020 Mar;18(3):574-79.
When I first became an attending, I was struck by how difficult it was to teach endoscopy effectively. As a fellow, I saw the various teaching styles of my attendings, and it was easy to pick out the best teachers from the group. But when the roles switched, and suddenly I was the supervising faculty member, it was hard to recall exactly what those teachers were doing to create an optimal learning environment in the endoscopy suite. Not only did I lack a framework on how to teach endoscopy, I also was still building confidence in my own endoscopic skills while feeling the pressure to keep my room running on time. All in all, although I loved the opportunity to teach, I found the experience to be quite stressful.
Hoping to find some guidance, I turned to the literature and was fortunate to find some great pieces on how to teach endoscopy effectively. I learned of cognitive load theory – the idea that short-term or “working memory” can manage only a few pieces of information at a time – and how excess feedback or other external distractions (e.g., pagers) during a procedure can overwhelm a learner and lead to declining performance.1 I also read about the pursuit of “conscious competence,” where an endoscopist can verbalize the steps of a maneuver so that a trainee can remain on the scope and maximize hands-on participation.2
Motivated to bring these key concepts together in an evidence-based framework, I helped lead a Delphi study of GI fellowship program directors and endoscopy education experts to reach consensus on the best practices of teaching endoscopy.3 After two rounds of surveys, the participants identified 10 essential endoscopy teaching practices, which I will summarize in the next sections. What I found most helpful was how these practices were distributed throughout the endoscopy learning experience. By breaking down the complicated task of teaching endoscopy to three discrete parts – prior to the procedure, during the procedure, and after the procedure – I now had a framework to take back to the endoscopy suite.
Prior to the procedure
With a busy endoscopy schedule and increasing clinical demands, it is tempting to use the time between cases to complete documentation, address patient messages, and review emails. While this is great for efficiency, make sure to also reserve time to set the stage for your fellow. One of the key practices during this phase is to assess your fellow’s current procedural competency. I start open-ended by asking my fellows how they have been doing with colonoscopy and then ask if they are working on a specific skill. With this information, I have a sense of how much hands-on assistance they will need, what realistic goals to set for them (e.g., navigate out of the sigmoid colon for an early learner vs. efficiently and independently completing the entire case for a later learner), and the areas to focus my observation to provide feedback after the procedure.
During this preparatory time, faculty should also discuss the patient history and indications for the procedure. Reviewing information such as prior sedation requirements and confirming plans for the procedure (e.g., random colon biopsies in a patient with chronic diarrhea and concern for microscopic colitis) helps ensure a proper plan is in place for the patient while also presenting opportunities for learning. Faculty can take this time to review the steps of a more complicated procedure (e.g., PEG placement) and establish ground rules such as when the attending will take the scope from the trainee. Lastly, make sure that the patient understands the role of the fellow and the supervision you will be providing throughout the case.
During the procedure
Once the procedure starts, your most important task is to maintain attention throughout the case – if you do, the other best practices generally fall into place. I am most attentive when I am gowned and positioned next to the fellow. From this vantage point, I can see the patient, the fellow’s hands, and the endoscopy screen, which allows me to readily assist if needed while directly observing the fellow’s performance.
If I need to provide feedback in the moment, I often ask the fellows to pause what they are doing and first listen to my feedback. Taking this “timeout” helps manage their cognitive load such that they can actually hear the feedback. As a general rule, however, I try to reserve the bulk of my feedback for when the procedure is complete (see next section). Another way to manage your fellow’s cognitive load is by using standardized endoscopic language throughout the procedure. For example, rather than say “go to the left” during a colonoscopy, try saying “tip left” or “torque counterclockwise” to provide more clear instructions to the fellow. Holding your fellow’s pager during the procedure is a kind gesture that also helps minimize extraneous cognitive load so that the fellow can focus on the procedure.
If your fellows get to a point where they cannot complete the task despite your giving appropriate feedback, or if patient safety concerns arise, then it is time for you to take hands-on control of the scope. In my experience, most fellows welcome the hands-on assistance as they are overloaded by the difficulty of the procedure. Setting this expectation ahead of time, as noted above, makes for a smoother transition. While assuming control of the scope, try to narrate what you are doing differently so that the fellow can still learn while watching. Once you complete the difficult portion of the procedure (e.g., reducing a loop to reach the cecum), return the scope to the fellow to maximize the hands-on participation (if time permits).
After the procedure
In the third and final stage of the endoscopy teaching experience, faculty should take the time to confirm the findings of the procedure with the fellow and discuss next steps in management for the patient. Finding these teachable moments helps solidify the cognitive learning for the fellow while also ensuring the patient receives the appropriate postprocedure recommendations. As part of this process, make sure to review the procedure note drafted by the fellow, and if you need to make any substantive edits, review the changes with the fellow so that he or she can learn for future cases.
To wrap up the session, provide feedback to the fellow on performance based on your direct observation. Make sure to name this process aloud – “Let’s do some feedback” – and start by asking how the fellow felt about the performance, both in terms of what went well and what the fellow would like to improve. Then provide your feedback on the performance and be specific, such as, “I really like how you identified a loop and then reduced around the hepatic flexure.” Conclude by having the fellow set a plan for improvement and make sure to ask for feedback on your own teaching performance.
In conclusion, teaching endoscopy is hard – especially as a junior attending. By breaking down the endoscopy teaching experience into its three components, however, and committing to teaching from start to finish, you can provide high-quality endoscopy education to your fellows while ensuring the best care for your patients.
Dr. Kumar is associate medicine clerkship director at Harvard Medical School, and associate physician in the division of gastroenterology at Brigham and Women’s Hospital, both in Boston. He disclosed having no conflicts of interest. He is on Twitter @NavinKumarMD.
References
1. Dilly CK and Sewell JL. 2017 Sep;153(3):632-36.
2. Waschke KA et al. Best Pract Res Clin Gastroenterol. 2016 Jun;30(3):409-19.
3. Kumar NL et al. Clin Gastroenterol Hepatol. 2020 Mar;18(3):574-79.
Top 12 tips for research success in fellowship and early academic faculty years
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Congratulations! You have matched in a competitive medical subspecialty or you have secured your first faculty position. But what do you do now? Success in your early career – as a new fellow or a new attending – requires both hard work and perseverance. We present our top 12 tips for how to be successful as you transition into your new position.
Tip #1: Be kind to yourself
As you transition from medical resident to GI fellow or from GI fellow to first-time attending, it is important to recognize that you are going through a major career transition (not as major as fourth year to intern, but probably a close second). First and foremost, remember to be kind to yourself and set reasonable expectations. You need to allow yourself time to transition to a new role which may also be in a new city or state. Take care of yourself – don’t forget to exercise, eat well, and sleep. You are in the long game now. Work to get yourself in a routine that is sustainable. Block out time to exercise, explore your new city, meal plan, and pursue your interests outside of medicine.
Tip #2: Set up for success
Since you are going through this major life/career transition, it is really helpful if you can set yourself up for success by having some projects that are easily completed during this challenging time so that you can demonstrate success. If you have projects in different stages of development, you will always have something you can work on when some projects are delayed for reasons outside of your control. In particular, it is great to have a few papers ready to go during late fellowship so they are published during your first year as an academic attending! This will allow you to continue your research trajectory as you learn the ropes of your new position.
Tip #3: Ask for help
It turns out you cannot do everything on your own! Make sure you are getting help professionally and personally so that you are set up for success. It’s okay to feel overwhelmed or confused; we all do at some point or another. Fellowship and early academic faculty years are stressful and nobody expects you to do it alone. Chances are your mentors or cofellows have had similar struggles, and in opening up, this dialogue may help you both.
Tip #4: Write out your 5-year plan
You need to know where you are going before you can figure out how to get there. Take some time for “soul searching”: Think about where you would like to be in 5 years and work backward (along with help from your mentors; see Tip #5) to determine how best to get there. If you think a career in academia might be for you, it’s never too soon to start networking and involving yourself in research. If a specific institution or clinical position draws your attention, check out the current faculty. You can use their CVs as a roadmap of types of experiences and honors that should be on your radar throughout these 5 years. Remember that your 5-year plan is not written in stone – this is something that you should re-evaluate as your interests and priorities change throughout your career.
Tip #5: Develop your personal ‘Board of Directors’
Instead of trying to find the perfect mentor, we suggest you seek out a personal “Board of Directors” who can serve as your mentoring team. There will never be a single perfect mentor for you and it is likely that you will need separate mentors to help guide you on different aspects of your career. I personally have separate individuals serving as my clinical mentor, my research content mentor, my research methods mentor, my career mentor, and my personal/life mentor. Having multiple mentors allows you to maximize the impact of your different mentors’ strengths across each component of your career. Further, your mentors themselves may have past histories of collaboration that you may then leverage to buoy your own fledgling career. When deciding on who to choose as a mentor, it is important to talk to prior mentees about their experiences with a mentor to help you decide if you may be a good match.
Tip #6: Master the art of “Menteering”
Now that you have identified mentors, you need to do your part in nurturing this mentee-mentor relationship. Be an excellent mentee: Show up, stick to a timeline, bring ideas and enthusiasm, and make it easy for your mentor. Your mentors want to see you succeed and sometimes this requires you to help them help you. If you know your own learning style and how you like to interact, have that conversation with your mentor upfront (for example, you may need strict deadlines or you may prefer having more time to develop ideas). Having these conversations before you start a project or a relationship will help set the expectations and ensure effective communication with your mentor. If you find that your mentor is doing something that hinders your progress, such as asking for updates too often or not checking in enough, have a constructive conversation with them about how you feel. Come prepared for meetings with your mentor with an agenda and timeline. Be specific if there is something you need from your mentor and be respectful of their other commitments. For example, if you would like your mentor to review your grant application, let them know the grant deadline and find out when you need to get them a draft so that they will have time to provide meaningful feedback.
Tip #7: Identify sponsors
Equally, if not more important than your mentoring team, are sponsors. These are people in positions of power who will promote you and help push your career forward. Sponsors can be people more senior to you, cofellows, or even acquaintances in industry or pharmaceuticals. Your mentor may also be your sponsor, but not always. As early academic faculty, it is important to get your name out there with speaking engagements related to your clinical and research niche, and that is one way a sponsor can help bolster your career.
Tip #8: Develop your personal brand – what is on your T-shirt?
As medicine becomes more and more subspecialized, finding your brand is becoming increasingly important. A brand could be anything from your academic niche to social justice, or even social media utilization. Your brand should encompass what you are naturally excited by within your field. Finding your brand will not only distinguish you from your peers but will also provide you with expertise which you can then offer to your colleagues, near and far. Practice the “elevator pitch” of your personal brand so that you can effectively (and efficiently) describe yourself and your interests when meeting new people and networking.
Tip #9: Meet thought leaders in your field
Think of the top five or six most prominent and influential people in your area of clinical or research interest and introduce yourself. This can be done at a national meeting or simply over email, though in person is always best if possible. Although thought leaders are busy, in my experience, if you are persistent, you can always find a few minutes to make an introduction. I’ve shared cab rides just to get a few minutes of someone’s time. In my first few years on faculty, I met with most of the thought leaders in my field; some of these meetings led to fruitful collaborations and important introductions (see tip #7). Meet others at your career level too. They can be great to bounce ideas off, and they will be future leaders in the field. Inviting thought leaders to come to your institution to give talks (in-person or virtually) is another great way to show your interest in their work and also find time to introduce yourself.
Tip #10: Apply, apply, apply
Remember that feedback is a gift and the best way to receive feedback is to apply to as many opportunities as you can. Any successful person in GI will have a ‘CV of failures’ far longer than their actual CV documenting their successes. I applied to 8 grants before landing my first one, but I received invaluable feedback and improved my writing skills in the process. Success in fellowship and early faculty takes immense grit – work on building a thick skin and finding the learning opportunity within any outcome.
Tip #11: Don’t get sucked into the email abyss
It is easy to fill your time completing low priority, but easy to complete, tasks such as responding to emails. Time management is key and you need to make sure that you dedicate time to more time-consuming tasks – such as writing and developing projects/grants – that have a high reward. Dedicate time on your calendar for high-priority tasks and make sure you don’t open your email during this time. Turn off the email pop-up window and do emails at the end of the day (or whenever you are done writing and thinking). Limiting distractions will help get your creative juices flowing.
Tip #12: Don’t always say yes
In fact, don’t ever say yes to a career or research opportunity within the first 24 hours to allow yourself time to weigh the pros and cons of the commitment, to assess the timeline feasibility, and to decide it fits into your 5-year plan. You can say you need to talk to your mentor about it first. If you decide you cannot accept an opportunity, a great way to mitigate that is to simply say “I’d love to, but my mentor says no.” Act as a sponsor to someone else by suggesting a potential colleague who might be interested in the opportunity. As you accept more responsibilities, think about what you might be able to give up to give yourself time to be successful in this new opportunity (and not distract from yourself or your 5-year plan).
Conclusion
Success in research and early academic faculty years takes planning and determination. We hope these tips provide a broad outline for what to think about and how to approach planning your future career. First and foremost, you must put in the time to think about what you really want and what will make you happy in the long run. Academic success is a broad term that each of us defines differently. What does it mean to you? Once you figure that out, make your 5-year plan and run with it!
Dr. Rebello and Dr. Long are with section of gastroenterology at Boston Medical Center and Boston University. They have no conflicts to report.
Microaggressions, racism, and antiracism: The role of gastroenterology
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
On a busy call day, Oviea (a second-year gastroenterology fellow), paused in the hallway to listen to a conversation between an endoscopy nurse and a patient. The nurse was requesting the patient’s permission for a gastroenterology fellow to participate in their care and the patient, well acquainted with the role from prior procedures, immediately agreed. Oviea entered the patient’s room, introduced himself as “Dr. Akpotaire, the gastroenterology fellow,” as he had with hundreds of other patients during his fellowship, and completed the informed consent. The interaction was brief but pleasant. As Oviea was leaving the room, the patient asked: “When will I meet the doctor”?
This question was familiar to Oviea. Despite always introducing himself by title and wearing matching identification, many patients had dismissed his credentials since graduating from medical school. His answer was equally familiar: “I am a doctor, and Dr. X, the supervising physician, will meet you soon.” With the patient seemingly placated, Oviea delivered the consent form to the procedure room. Minutes later, he was surprised to learn that the patient specifically requested that he not be allowed to participate in their care. This in combination with the patient’s initial dismissal of Oviea’s credentials, left a sting. While none of the other team members outwardly questioned the reason for the patient’s change of heart, Oviea continued to wonder if the patient’s decision was because of his race.
Beyond gastroenterology, similar experiences are common in other spheres. The Twitter thread #BlackintheIvory recounts stories of microaggressions and structural racism in medicine and academia. The cumulative toll of these experiences leads to departures of Black physicians including Uché Blackstock, MD;1 Aysha Khoury, MD, MPH;2 Ben Danielson, MD;3 Princess Dennar, MD;4 and others.
Microaggressions as proxy for bias
The term microaggression was coined by Chester Pierce, MD, the first Black tenured professor at Massachusetts General Hospital in the 1970’s, to describe the frequent, yet subtle dismissals Black Americans experienced in society. Over time, the term has been expanded to include “brief and commonplace daily verbal, behavioral, or environmental indignities, intentional or unintentional, that communicate hostile, derogatory, or negative slights and insults” to any marginalized group.5
While the term microaggressions is useful in contextualizing individual experiences, it narrowly focuses on conscious or unconscious interpersonal prejudices. In medicine, this misdirects attention away from the policies and practices that create and reinforce prejudices; these policies and practices do so by systematically excluding underrepresented minority (URM) physicians,6 defined by the American Association of Medical Colleges as physicians who are Black, Hispanic, Native Americans, and Alaska Natives,7 from the medical workforce. Ultimately, this leads to and exacerbates poor health outcomes for racial and ethnic minority patients.
Microaggressions represent our society’s deepest and oldest biases and are rooted in structural racism, as well as misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.8 For URM physicians, experiences like the example above are frequently caused by structural racism.
Structural racism in medicine
Structural racism refers to the policies, practices, cultural representations, and norms that reinforce inequities by providing privileges to White people at the disadvantage of non-White people.9 In 1910, Abraham Flexner, commissioned by the Carnegie Foundation and the American Medical Association, wrote that African American physicians should be trained in hygiene rather than surgery and should primarily serve as “sanitarians” whose purpose was to “protect Whites” from common diseases like tuberculosis.10 The 1910 Flexner Report also emphasized the importance of prerequisite basic sciences education and recommended that only two of the seven existing Black medical schools remain open because Flexner believed that only these schools had the potential to meet the new requirements for medical education.11 A recent analysis found that, had the other five medical schools affiliated with historically Black colleges and universities remained open, this would have resulted in an additional 33,315 Black medical school graduates by 2019.12 Structural racism explains why the majority of practicing physicians, medical educators, National Institutes of Health–funded researchers, and hospital executives are White and, similarly, why White patients are overrepresented in clinical trials, have better health outcomes, and live longer lives than several racial and ethnic minority groups.13
The murders of Ahmaud Arbery, Breonna Taylor, and George Floyd and the inequitable toll of the COVID-19 pandemic on Black, Hispanic, and Native American people renewed the dialogue regarding structural racism in America. Beyond criminal justice and police reform, the current social justice movement demands that structural racism is examined in all spheres. In medicine and health care, acknowledging the history of exclusion and exploitation of Black people and other URM groups is an important first step, but this must be followed by a commitment to an antiracist future for the benefit of all medical professionals and patients.14,15
Antiracism as a path forward
Antiracism refers to actions and policies that seek to dismantle structural racism. While individuals can and should engage in antiracist actions, it is equally important for organizations and government to actively participate in this process as well.
Individual and interpersonal levels
Gastroenterologists should advocate an end to racist practices within their organizations (e.g., unjustified use of race-based corrections in diagnostic algorithms and practice guidelines),16 and interrupt microaggressions and racist actions in real time (e.g., overpolicing of underrepresented groups in health care settings).17 Gastroenterologists from underrepresented groups may also need to unlearn internalized racism, which is defined as acceptance by members of disadvantaged races of the negative messages about their own abilities and intrinsic worth.18
Organizational level
Gastroenterology divisions and practices must ensure that the entire workforce, including leadership, reflects the diversity of our country. Underrepresented groups represent 33% of the U.S. population, but only 9.1% of gastroenterology fellows and 10% of gastroenterology faculty are from underrepresented groups.19 In addition to diversifying the field of gastroenterology through financial and operational support of pipeline educational programs, organizations should also promote the scholarship of URM groups, whose work is often undervalued, and redistribute power by elevating voices that have been historically absent.20 Gastroenterology practices should also collect high-quality patient data disaggregated by demographic factors. Doing so will enable rapid identification of disparate health outcomes by demographic variables and inform interventions to eliminate identified disparities.
Government level
The “Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government” issued by President Biden on Jan. 20, 2021, is an example of how government can promote antiracism.21 The executive order states that domestic policies cause group inequities and calls for the removal of systemic barriers in current and future domestic policies. The executive order outlines several additional ways to improve equity in current and future policy, including engagement, consultation, and coordination with members of underserved communities. The details outlined in the executive order should serve as the foundation for establishing new standards at the state, county, and city levels as well. Gastroenterologists can influence government by voting for officials at all levels that support and promote these standards.
Conclusion
Beyond calling out microaggressions in real time, we must also interrogate the biases, policies, and practices that support them in medicine and beyond. As Black gastroenterologists who have experienced microaggressions and overt acts of racism, we ground Oviea’s experience in structural racism and offer strategies that individuals, organizations, and governing institutions can adopt toward an antiracist future. This model can be applied to experiences rooted in misogyny, homophobia, transphobia, xenophobia, ableism, and other prejudices.
As a nation, we must make an active and collective choice to address structural racism. In health care, doing so will strengthen communities, enhance the lived experiences of URM physician colleagues, and save patient lives. Gastroenterologists, as trusted health care providers, are uniquely positioned to lead the way.
Dr. Akpotaire is a second-year GI fellow in the division of gastroenterology at the University of Washington, Seattle. Dr. Issaka is an assistant professor with both the Fred Hutchinson Cancer Research Center, Seattle, and the division of gastroenterology at the University of Washington.
References
1. Blackstock U. “Why Black doctors like me are leaving faculty positions in academic medical centers.” STAT News, 2020.
2. Asare JG. “One Doctor Shares Her Story of Racism in Medicine.” Forbes. 2021 Feb 1.
3. Kroman D. “Revered doctor steps down, accusing Seattle Children’s Hospital of racism.” Crosscut. 2020 Dec 31.
4. United States District Court Eastern District of Louisiana. Princess Dennar, M.D. v. The Administrators of the Tulane Educational Fund, 2020.
5. Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. Hoboken, N.J.: Wiley, 2010.
6. Boyd RW. Lancet. 2019 Jun 22;393(10190):2484-5.
7. AAMC. Diversity in Medicine Facts and Figures 2019. Washington, D.C., 2019.
8. Overland MK et al. PM R. 2019 Sep;11(9):1004-12.
9. Jones CP. Ethn Dis. 2018 Aug 9;28(Suppl 1):231-4.
10. Hlavinka E. “Racial Bias in Flexner Report Permeates Medical Education Today.” Medpage Today. 2020 Jun 18.
11. Flexner A. Medical Education in the United States and Canada. New York: 1910. Republished: Bull World Health Organ. 2002;80(7):594-602.
12. Campbell KM et al. JAMA Netw Open. 2020 Aug 3;3(8):e2015220.
13. Malat J et al. Soc Sci Med. 2018 Feb;199:148-56.
14. Kendi IX. How to be an antiracist. New York: Random House Books, 2019.
15. Gray DM 2nd et al. Nat Rev Gastroenterol Hepatol. 2020 Oct;17(10):589-90.
16. Vyas DA et al. N Engl J Med. 2020 Aug 27;383(9):874-82.
17. Green CR et al. J Natl Med Assoc. 2018 Feb;110(1):37-43.
18. Jones CP. Am J Public Health. 2000 Aug;90(8):1212-5.
19. Anyane-Yeboa A et al. Am J Gastroenterol. 2020 Aug;115(8):1147-9.
20. Issaka RB. JAMA. 2020 Aug 11;324(6):556-7.
21. Biden JR. Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, D.C.: The White House, 2021.
Impostor syndrome: Implications for medical professionals
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
A few years ago, I was asked to give a talk on impostor syndrome at a national conference. My initial thought was “I am not even remotely qualified to give this talk.” Upon reflection, I think that was the first time I acknowledged that I, too, suffer from this syndrome.
There are many definitions and designations (e.g., impostor phenomenon or fraud syndrome), but the one I use most often is high-achieving individuals who are marked by an inability to internalize their accomplishments and a persistent fear of being exposed as a fraud. They live in fear that their incompetence will be exposed and they will be revealed as a fraud both intellectually and within their job or role. First described by Clance and Imes in 1978,1 the original authors observed that many highly respected and accomplished women did not experience an internal sense of success despite their education and evidence of academic achievement. Based in part on previous observations regarding the differential attribution of success in men and women,2 the authors suggested that two general principles were found to be at the heart of this syndrome. The first was that an unexpected performance outcome will be attributed to a temporary cause. The second was that an expected performance outcome will be attributed to a stable cause. As such, the authors originally suggested that women tended to explain failure with lack of ability, whereas men attributed failure to luck or task difficulty. Furthermore, the authors emphasized environmental factors – such as mentorship, competition, and isolation – as the primary influence in the development of these tendencies.
Although originally described in women, this phenomenon can also affect men, as well as a wide variety of people from different occupations and cultures.3-6 Furthermore, although environmental factors were originally linked as the primary driver of these tendencies, further research has suggested that personality factors play a larger role, and that up to 70% of people may experience this phenomenon in their lifetime.7 Personality traits such as perfectionism and neuroticism may be linked to the development of this phenomenon.3,8
There are several online screening questionnaires that can be used to gauge whether individuals experience some or most of these traits. On one such questionnaire, the Clance IP Scale,9 poses such questions as: “I have often succeeded on a test or task even though I was afraid that I would not do well before I undertook the task” and “I am afraid people important to me may find out that I am not as capable as they think I am.” There are 20 questions scored from 1 to 5 and a score of 40 or below suggests few impostor tendencies, while a score of 80 or above suggests the respondent often has intense IP experiences. The higher the score, the more frequently and seriously the impostor syndrome interferes in a person’s life. What is unclear is whether this worsens, improves, or stays the same throughout one’s career. Of interest is that my personal score at this time is 43; however, it would have been 89 had I taken the test during college and medical school. What is unclear to me from the literature is what factors may play a role in a person’s perception of their abilities and their personal confidence over time.
Why is this important? Given that we are all professionals, impostor tendencies appear to have significant impact in the context of our work. This may have impact on us both as employers and as employees.10 Individuals with impostor syndrome tendencies often characterize themselves negatively and perform poorly on self-appraisals.11 In a study of 201 Belgian white-collar workers, Vergauwe and colleagues found that impostor syndrome tendencies were negatively related to job satisfaction and organizational citizenship behavior; both of which could be influenced by a high degree of social support.10 Individuals with impostor syndrome tendencies do less career planning, explore career options less frequently, and are less inclined to lead.12,13 These tendencies can be detrimental as the most qualified people for a position or opportunity may not step forward for consideration. Employers may tend to overlook these individuals for promotions or for pay raises which could negatively influence future earnings. Furthermore, a person may experience increased burnout as they continuously try to overcompensate for what they perceive as their shortcomings. They may feel concerned they are letting others down or not performing to standards. They may derive less enjoyment from life because of the constant focus on feelings of inadequacy.14 Research along these lines suggest impostor syndrome tendencies can have adverse personal and health-related consequences and may increase social anxiety, depression, and overall psychological distress.15,16
What can we do about it? In a very interesting study by Zanchetta and colleagues, the authors studied 103 young employees and randomized them to receive coaching, training, or no intervention.17 Their findings showed that coaching was an effective mindset intervention which resulted in reduced impostor syndrome scores. Furthermore, fear of negative evaluation and the effect of coaching appeared to be significantly associated with a reduction in the impostor syndrome scores. Coaching appeared to improve self-enhancing attributions and self-efficacy with a reduction in the tendency of subjects to fear negative evaluation. The authors concluded that fostering a mindset shift by reducing the fear of negative evaluations through coaching demonstrated measurable and sustained improvements in overall impostor syndrome scores for participants.17
What do I suggest? It is clear this affects a significant percentage of physicians, health care professionals, and professionals in general. Harboring these tendencies can have a negative impact on health, professional achievement, income, and happiness. It is important to self-reflect, identify if you are at risk, and if so, take the opportunity to explore solutions. My recommendations are:
- Name it: Take the test and see how you score.
- Be mindful: Self-reflection will help you identify the behaviors that are interfering with your happiness and success.
- Write it down: Be strategic and document your plan for success to reinforce your accomplishments.
- Create a feedback group: Friends and colleagues can help to mitigate the negative effects of impostor syndrome tendencies.
- Speak up: Ask for help; coaching has been documented to reduce impostor syndrome scores and help lessen the burden of these tendencies.
- Step out of your comfort zone: Develop a mantra, break bigger challenges into smaller pieces, and acknowledge little wins along the way.
In conclusion, impostor syndrome appears to be highly prevalent in professionals including those of us in medicine. The experience can adversely affect our careers and ability to secure key leadership positions. As managers, we also must keep in mind our role in mentoring others and recognizing the potential impact of impostor syndrome on those who report to us. Recognition of this phenomenon – and understanding of the effects on oneself – is the first step in overcoming the negative effects and moving toward realization of one’s potential.
Dr. Brown is a professor of medicine at Wayne State University, division chief of gastroenterology and hepatology at Henry Ford Hospital, and associate medical director at the Henry Ford Hospital Transplant Institute, all in Detroit.
References
1. Clance PR, Imes S. Psychother Theory Res Pract. 1978 Fall;15(3):1-7.
2. Deaux D. In J.H.Harvey, W.J.Ickes and R.F. Kidd (Eds). New directions in attribution research. Vol. 1. New York: Halsted Press Division, Wiley. 1976; p 335-42.
3. Bernard NS et al. J Pers Assess. 2002;78(2):321-33.
4. Topping ME et al. Acad Psychol Bull. 1985;(7):213-26.
5. Langford J et al. Psychotherapy. 1993;30(3):495-501.
6. Chae JH et al. J Pers Assess. 1995;65(3):468-85.
7. Harvey JC et al. If I’m successful, why do I feel like a fake? New York: Random House, 1985.
8. Ross SR et al. Pers Individ Diff. 2001;31:1347-55.
9. Clance PR. The impostor phenomenon: When success makes you feel like a fake. Toronto: Bantam Books, 1985; p 20-2.
10. Vergauwe J et al. J Bus Psychol. 2015;30:565-81.
11. Leary MR et al. J Pers. 2000;68(4):725-56.
12. Neureiter M et al. Front Psychol. 2016;7:48.
13. Neureiter M et al. J Vocat Behav. 2017;98:56-69.
14. Duhigg C. The power of habit: Why we do what we do in life and business. New York: Random House, 2012.
15. Henning K et al. Med Educ. 1998 Sep;32(5):456-64.
16. Oriel K et al. Fam Med. 2004 Apr;36(4):248-52.
17. Zanchetta M et al. Front Psychol. 2020 May 15;11:405.
@GiJournal: An online platform to discuss the latest gastroenterology and hepatology publications
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
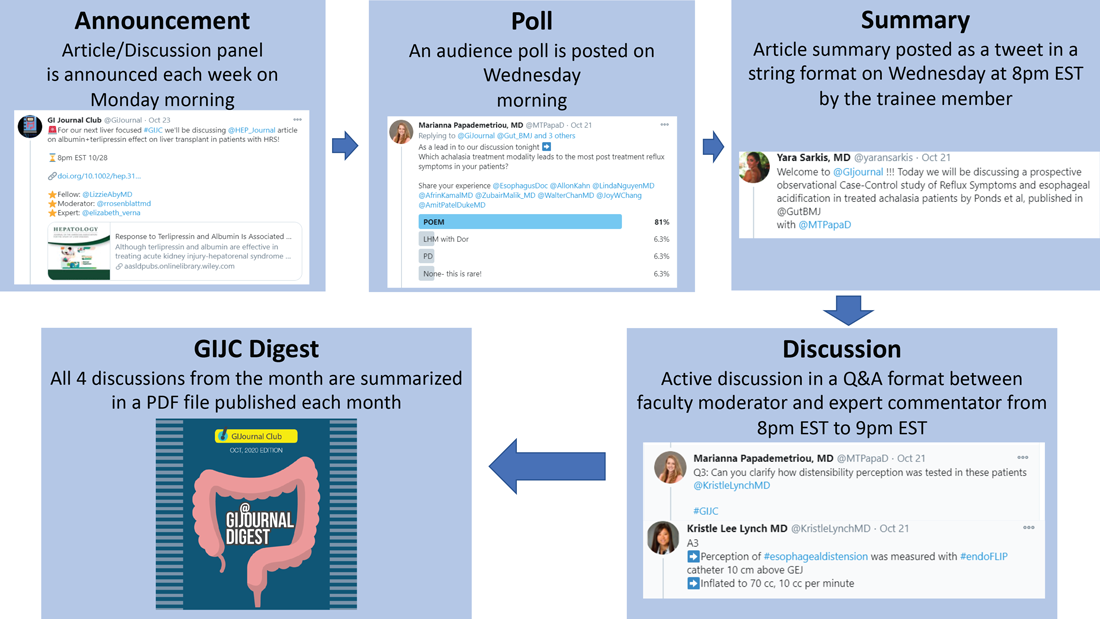
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
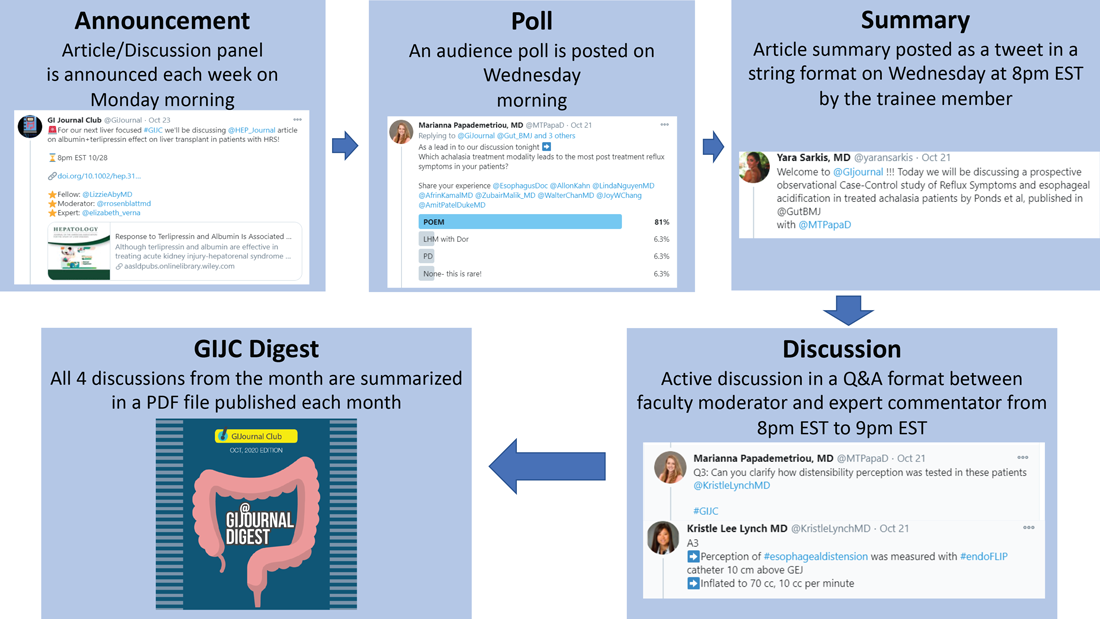
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
The last decade has seen an increased focus on the use of social media for medical education. Twitter, with over 330 million active users, is the most popular social media platform for medical education. We describe here our recent initiative to establish a weekly online gastroenterology-focused journal club on Twitter.
How was the idea conceived?
Sultan Mahmood, MD (@SultanMahmoodMD)
I joined #GITwitter at the end of 2019 and started following some of the leading experts in the field of gastroenterology and hepatology. It was a pleasant surprise to see how easy it was to engage with them and get expert opinions from across the world in real time. #MondayNightIBD, led by Aline Charabaty, MD, had become a phenomenon in the GI community and changed the perception of medical education in the digital world. There were online journal clubs for different medical subspecialties, including #NephroJC, #HOJournalClub, and #DermJC, but none for gastroenterology. Realizing this opportunity, and with guidance from Dr. Charabaty, we started @GiJournal in December of 2019 with weekly discussions.
@GiJournal started off as an informal discussion in which we would post a summary of the article and invite an expert in the field to comment. However, the interest in the journal club quickly took off as we gained more followers and a worldwide audience joined our journal club discussions on a weekly basis. As the COVID-19 pandemic took hold and endoscopy suites around the word closed, interest in online medical education grew. @GIJournal provided a platform for trainees and practicing physicians alike to stay up to date with the latest publications from the comfort of their homes. Needless to say, the journal club has evolved since its inception in that we now work with a team of experts and trainees who run the journal club on a rotating basis.
How does @GiJournal work?
Ijlal Akbar Ali, MD (@IjlalAkbar)
We have a large editorial board with volunteer faculty and trainees, all divided into four special interest groups (general GI/inflammatory bowel disease, interventional endoscopy/bariatric endoscopy, hepatology, and esophageal/motility disorders). Each week, a faculty member and a trainee pick a recently published article from a high-impact GI-focused journal. We also try to invite an expert of international repute (often the authors of the article themselves!) to engage as well. The faculty moderator and invited expert then work with the trainee to plan the session content. We post the topic and article on Monday. At 8 p.m. EST on Wednesday, the trainee posts a series of six to eight tweets summarizing the article. The faculty then asks the invited expert (and audience at large) a series of predetermined questions. Anyone can respond, share their opinion, and direct their own questions toward the moderator and expert who continually check their notifications and respond in real time. This brews into an hour-long discussion which covers not only the methodologic aspects of the article, but clinical practice in general. Discussions often trickle into the next day as people from different time zones participate. Everyone uses #GIJC at the end of their tweets which assists those following the article and facilitates indexing for future review. For those who miss or want to review sessions, we conveniently summarize all articles and corresponding discussions in a monthly publication, @GiJournal Digest, that is posted on Twitter for anyone to download, read and enjoy (Figure 1).
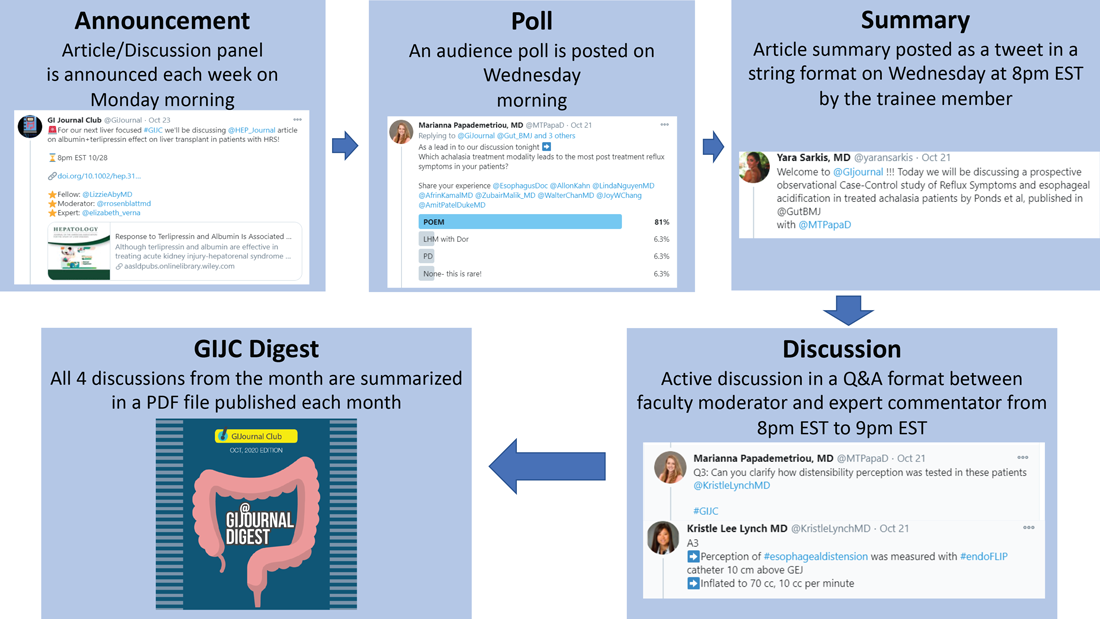
How is this different from any other journal club?
Atoosa Rabiee, MD (@AtoosaRabiee)
@GiJournal is unique in that it provides trainees and practicing gastroenterologists access to interactive discussions with both authors and world-renowned experts in the field. Online journal clubs operate with a flattened hierarchy; as such, they inherently break down access barriers to both the researchers who performed the study and key opinion leaders who commonly participate. There is no boundary as far as institutions or even countries. As a result, our platform has uncovered an unexpected degree of interest in live online discussion, and we have enjoyed collaborating and learning from experts from all over the world. @GiJournal also differs from conventional journal clubs by allowing trainees the opportunity to collaborate and engage with mentors from other institutions. As such, trainees develop relationships with experts in the field outside their home institutions, experts with whom they may not have had contact otherwise.
Although worldwide participation is a key strength of the online @GiJournal platform, it may be challenging for some members to attend the live discussion based on time difference. We account for this in two ways. First, participants are encouraged to continue with comments and questions afterward at their convenience, which allows experts and moderators to continue the conversation, often for several days. Second, to promote inclusivity, we have created a unique, customized publication to summarize and present the key points of conversation for each session. This asynchronous access is a quality not found in more traditional journal club formats. Finally, studies have shown that articles shared on social media tend to have increased citations and higher Altmetric scores.
What are the opportunities for trainees and recent graduates?
Sunil Amin, MD, MPH (@SunilAminMD)
Our surveys have shown that 30%-45% of the @GiJournal discussion participants are trainees. Both gastroenterology fellows and internal medicine residents from around the world are an integral part of each specialty panel for the weekly @GIjournal discussions. Trainees are paired up with a specific faculty mentor and together they choose an article for discussion, create a summary, informal twitter poll, and questions for the discussion. This direct access provides an opportunity for trainees to interact, ask questions, and learn from faculty in an informal atmosphere.
We have heard from multiple trainees who have developed long-term relationships with the experts and faculty mentors they worked with and are now also working on research projects. Additionally, trainees can bring the expertise they have now acquired back to their home institutions to pick articles, add specific teaching points, and enrich their local journal club discussions. Finally, trainees who present on the @GiJournal platform are given unique visibility to the many faculty members and opinion leaders participating in each discussion. This may facilitate future networking opportunities and enhance their CVs for future fellowship or employment applications.
Plans for the future?
Allon Kahn, MD (@AllonKahn)
Despite significant evolution and growth in @GiJournal over the past year, we are still actively working to expand our platform. Modes of online medical education, specifically Twitter-based GI journal club discussions, remain in their infancy. We see this @GiJournal as an opportunity for innovation as we plan for the year ahead. Our top priority for the upcoming year includes obtaining CME approval, which we are currently developing with Integrity CE (an Accreditation Council for Continuing Medical Education–accredited provider of CME for health care professionals). This will give an opportunity for the participants to be awarded CME credit when they participate in our weekly discussions. Other options being explored include starting a podcast and translation of @GiJournal Digest in different languages to reach a wider international audience. Furthermore, with the continued expansion of GI leaders and experts joining and engaging in Twitter, our options for unique and multidisciplinary discussion topics will continue to grow.
How can you join the @GiJournal discussions?
@SultanMahmoodMD
Joining the journal club discussion is easy. Just follow the @GiJournal handle on Twitter and turn on the notifications icon. Although we encourage everyone to “actively” participate in the discussion by asking questions or sharing your personal experience, joining the discussion as an “observer” is also a great way to learn. The discussion starts at 8 p.m. EST every Wednesday. Follow the #GIJC and the @GiJournal handle as questions are posted by the faculty moderator and answered by the experts. Even if you miss the discussion, the @GiJournal Digest is a great way to recap the discussions in an easy-to-read PDF format. The @GiJournal Digest is a monthly publication that archives the four @GiJournal club discussions in the previous month. Follow the link below to access the recent publications: http://ow.ly/uu2550C3RXX
Conclusion
In summary, we believe Twitter-based journal clubs offer an engaging way of virtual learning from the comfort of one’s home and a convenient way to directly interact with the experts. The success of @GiJournal highlights the importance of social media for medical education in the field of gastroenterology and hepatology and we look forward to developing this endeavor further.
Dr. Mahmood is clinical assistant professor of medicine, co–program director of the GI fellowship program, UB division of gastroenterology, hepatology & nutrition, State University of New York at Buffalo; Dr. Rabiee is assistant professor of medicine, director of hepatology, division of gastroenterology and hepatology, Washington DC VA Medical Center, Washington; Dr. Amin is assistant professor of medicine, director of endoscopy, The Lennar Foundation Medical Center, division of digestive health and liver disease, department of medicine, University of Miami; Dr. Kahn is assistant professor of medicine, division of gastroenterology & hepatology, Mayo Clinic, Scottsdale, Ariz.; and Dr. Akbar Ali is a gastroenterology fellow in the division of digestive diseases and nutrition, University of Oklahoma Health Sciences Center, Oklahoma City.
Coaching in medicine: A perspective
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.
Coaching is a new topic in medicine. I first heard about coaching several years ago and met the term with skepticism. I was unsure how coaching was different than mentoring or advising and I wondered about its usefulness. However, the reason that I even started to learn about coaching was because I was struggling. I had finally arrived in my career, I had my dream job with two healthy kids, a perfect house, and good marriage. I kept hearing the refrain in my head: “Is this all there is?” I had this arrival fallacy that after all this striving and straining that I would finally be content. I felt unfulfilled and was dissatisfied with where I was that was affecting all parts of my life.
As I was wrestling with these thoughts, I had an opportunity to become a coach to residents around the country through the Association of Women Surgeons. I discussed with them what fills them up, what gets them down, how to set goals, and what their goals were for the year, as well as imposter syndrome. Impostor syndrome is defined as a pattern in which an individual doubts their accomplishments or talents and has a persistent internalized fear of being exposed as a “fraud.” Despite external evidence of their competence, those experiencing this phenomenon remain convinced that they are fooling everyone around them and do not deserve all they have achieved. Individuals incorrectly attribute their success to luck or interpret it as a result of deceiving others into thinking they are more intelligent than they perceive themselves to be. Imposter syndrome is prevalent and deep in medicine. As perfectionists, we are especially vulnerable to imposter syndrome as we set unrealistic ideals for ourselves. When we fail to reach these ideals, we feel like frauds, setting up this cycle of self-doubt that is toxic. When we feel that we can’t achieve the goals that we are striving for we will always find ourselves lacking. There is a slow, insidious erosion of self over the years. Imposter syndrome is well documented in medicine and is even felt as early as medical school.1,2
When I began coaching these residents the most profound thing that came out of these sessions was that my life was getting better – I knew what filled me up, what got me down, what my goals were for the year, and how I still deal with imposter syndrome. Coaching gave me a framework for helping determine what I wanted for the rest of my life. As I began coaching, I started learning all the ways in which I could figure out my values, my personal and professional goals, and perhaps most importantly, my relationships with myself and others.
Another perspective on coaching is to look at a professional athlete such as Tom Brady, one of the greatest quarterbacks of all time. He has a quarterback coach. No coach is going to be a better quarterback than Tom Brady. A coach for him is to be there as an advocate, break his fundamentals down technically, and help him improve upon what he already knows. A coach also identifies strengths and weaknesses, and helps him capitalize on both by bringing awareness, reflection, accountability, and support. If world-class athletes still want and benefit from coaching in a sport they have already mastered, coaching for physicians is just another tool to help us improve our abilities in and out of medicine.
Coaching is more encompassing than advising or mentoring. It is about examining deeply held beliefs to see if they are really serving us, if they are in line with our values and how we want to live our lives.
Coaching has also been validated in medicine in several papers. In an article by Dyrbye et al. in JAMA Internal Medicine, measures of emotional exhaustion and burnout decreased in physicians who were coached and increased in those who were not.3 In another study from this year by McGonagle et al., a randomized, controlled trial showed that primary care physicians who had sessions (as short as 6 weeks) to address burnout, psychological capital, and job satisfaction experienced an improvement in measures which persisted for 6 months after intervention.4 Numerous other articles in medicine also exist to demonstrate the effect of coaching on mitigating burnout at an institutional level.
Physicians are inherently driven by their love of learning. As physicians, we love getting to the root cause of any problem and coming up with creative solutions. Any challenge we have, or just wanting to improve the quality of our lives, can be addressed with coaching. As perpetual students we can use coaching to truly master ourselves.
Dr. Shah is associate professor of surgery, Rush University Medical Center, Chicago. Instagram: ami.shahmdcoaching.
References
1. Gottlieb M et al. Med Educ. 2020 Feb;54(2):116-24.
2. Villwock JA et al. Int J Med Educ. 2016 Oct 31;7:364-9.
3. Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5;179(10):1406-14.
4. McGonagle AK et al. J Occup Health Psychol. 2020 Apr 16. doi: 10.1037/ocp0000180.