User login
She Won’t Quit—But Will Her Heart?
ANSWER
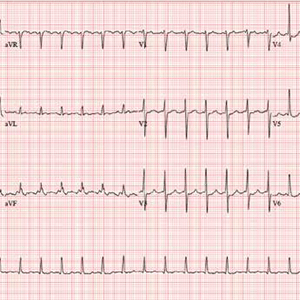
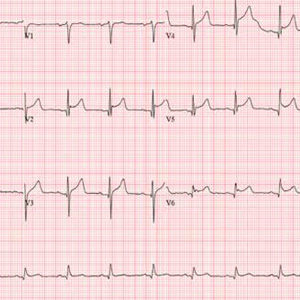
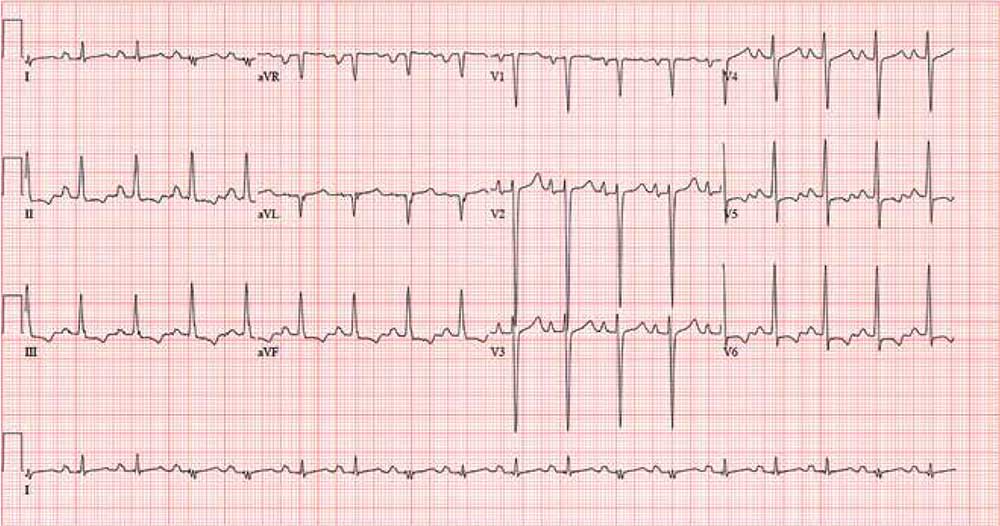
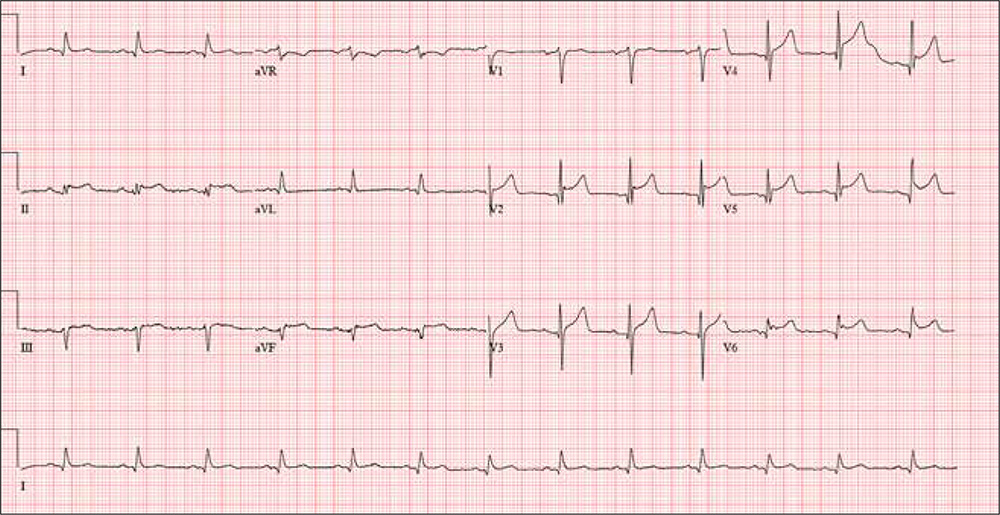
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block and possible left atrial enlargement. Criteria for sinus rhythm include a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
Criteria for a first-degree AV block include a consistent PR interval > 200 ms in all leads. Criteria for left atrial enlargement include a P-wave duration > 120 ms in lead II or a downward deflection of the P wave in lead V1 > 40 ms in length with > 1-mm negative deflection.
The P wave in leads II and V1, along with a murmur, is consistent with mitral regurgitation and a history of palpitations and paroxysmal atrial fibrillation. Left atrial enlargement should be considered. An echocardiogram was ordered and confirmed the diagnosis of left atrial enlargement in this patient.
A 58-year-old woman presents for preoperative workup for surgical repair of a distal left tibial fracture sustained while snowshoeing. She had been descending a side slope when she lost her footing. Her left snowshoe became entangled in a large granite rock, which defined the lateral wall of the path she was traversing. She has no prior orthopedic injuries.
Cardiac history is remarkable for hypertension, palpitations, and two episodes of paroxysmal atrial fibrillation. A Holter monitor, worn to help determine the etiology of her palpitations, captured the atrial fibrillation episodes, each of which was cardioverted within 48 hours of onset without complication. Following the second cardioversion, about 6 months ago, a novel oral anticoagulation agent was recommended, but she refused to take it because she felt such medication would interfere with her active lifestyle.
The patient is otherwise quite healthy and has been personally active in her preventive health maintenance.
Her current medications include lisinopril (5 mg/d) and aspirin (81 mg/d). She also takes a multivitamin daily. In the past 24 hours, she has taken two doses of acetaminophen/oxycodone (325/5 mg) for left ankle pain. She has no drug allergies.
The patient, an immigration attorney for a prominent law firm, is divorced and has no children. She works as a Zumba instructor on the weekends and has run 3 marathons within the past 2 years. She has never smoked or used recreational drugs, but she does partake in one or two glasses of wine with friends on weekends.
Family history is remarkable for hypertension in both parents and two of her three siblings. All are alive and otherwise healthy.
Review of systems reveals no current problems. She states she went through menopause about 10 years ago and was recommended to start estrogen therapy but refused this treatment.
Vital signs include a blood pressure of 118/88 mm Hg; pulse, 90 beats/min; temperature, 98.4°F; and O2 saturation, 98% on room air. Her weight is 129 lb, and her height, 64 in.
Physical exam reveals a healthy, athletic woman in no distress. She wears an orthopedic boot on her left foot, but it isn’t removed to examine the affected ankle. She wears contact lenses and has a posterior lingual brace on her lower teeth.
The HEENT exam is normal. The neck is supple without masses. There is no thyromegaly, carotid bruits, or jugular venous distention. The lungs are clear in all fields. The breasts are symmetrical without palpable nodules.
Cardiac exam is remarkable for a regular rate and rhythm at 90 beats/min. There is a soft end-systolic murmur consistent with mild mitral regurgitation. S1 and S2 are of normal intensity, and there are no extra heart sounds.
The abdomen is nontender with no organomegaly; the patient proudly shows her core strength and “a hint of a six-pack.” The genitourinary exam is deferred. Peripheral pulses are strong and equal bilaterally. The neurologic exam is grossly intact.
A preoperative chest x-ray is performed; results are pending.
The ECG shows a ventricular rate of 89 beats/min; PR interval, 232 ms; QRS duration, 82 ms; QT/QTc interval, 364/442 ms; P axis, 86°; R axis, 23°
Beer Before Liquor Affects the Ticker
ANSWER
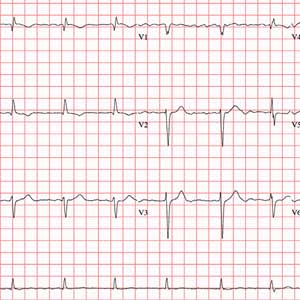
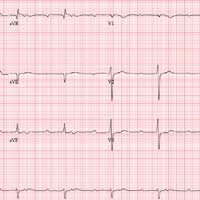
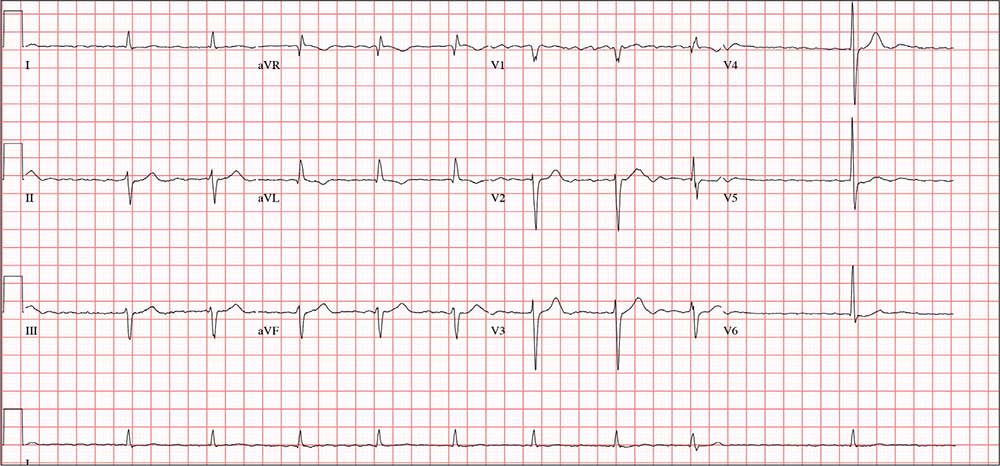
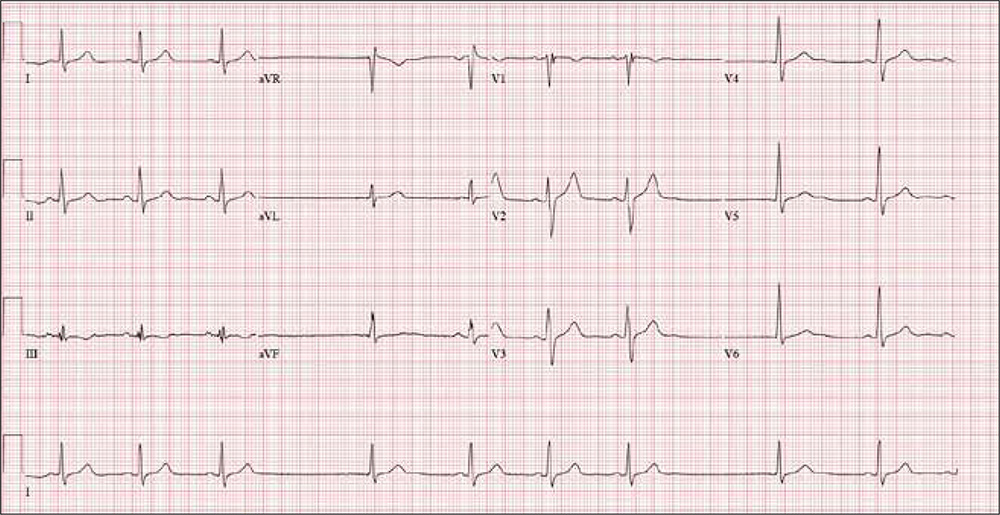
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
ANSWER
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
ANSWER
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
After a night of heavy drinking, a 34-year-old man awakens with a rapid heart rate and a fluttering sensation in his chest, which radiates up to his neck. By the time he arrives to your emergency department, he has had these symptoms for about 2 hours. He denies chest pain but reports having difficulty catching his breath. He says this is the first time he’s experienced these symptoms. He has no prior cardiac or pulmonary history.
The patient had been out with 4 old college friends, and they had between them consumed a case of beer and a fifth of whiskey. He cannot remember going home, but they all had ordered cabs ahead of time, knowing they would be drinking heavily. He denies taking any recreational drugs.
Past medical and surgical histories are remarkable only for a left tibial fracture sustained when the patient played high school football. He has no allergies and takes no medications. Although he doesn’t smoke tobacco, he admits to using marijuana sparingly; however, he says he hasn’t used it in the past 3 months. He works as a store manager at a local grocery chain. He isn’t married, has no children, and isn’t in a relationship.
Family history reveals the patient is an only child. His father has hypothyroidism, and his mother has type 2 diabetes, which is controlled with metformin. His maternal grandparents both have hypertension, which is managed with β-blockers.
The review of systems shows a recent increase in alcohol consumption following a breakup with his girlfriend 3 months ago. A 12-point review of systems is noncontributory.
Vital signs include a blood pressure of 118/62 mm Hg; pulse, 150 beats/min; and O2 saturation, 98% on room air. He is afebrile.
Physical exam reveals a thin, healthy but anxious man. His height is 72 in and his weight, 188 lb. The HEENT exam is normal. The neck is supple without thyromegaly and no jugular venous distention. The lungs are clear in all fields without wheezes, rales, or rhonchi.
Cardiac exam reveals tachycardia with a regular rate of 150 beats/min and no murmurs, extra heart sounds, or rubs. The abdomen is soft and nontender, with no palpable organomegaly. Peripheral pulses are equal bilaterally, with no palpable bruits. There is no peripheral edema, and the neurologic exam is intact.
An ECG reveals the following: a ventricular rate of 155 beats/min; PR interval, unmeasured, QRS duration, 78 ms; QT/QTc interval, 272/437 ms; P axis, unmeasured; R axis, +34°; and T axis, –50°. What is your interpretation?
A Method to His Madness
ANSWER
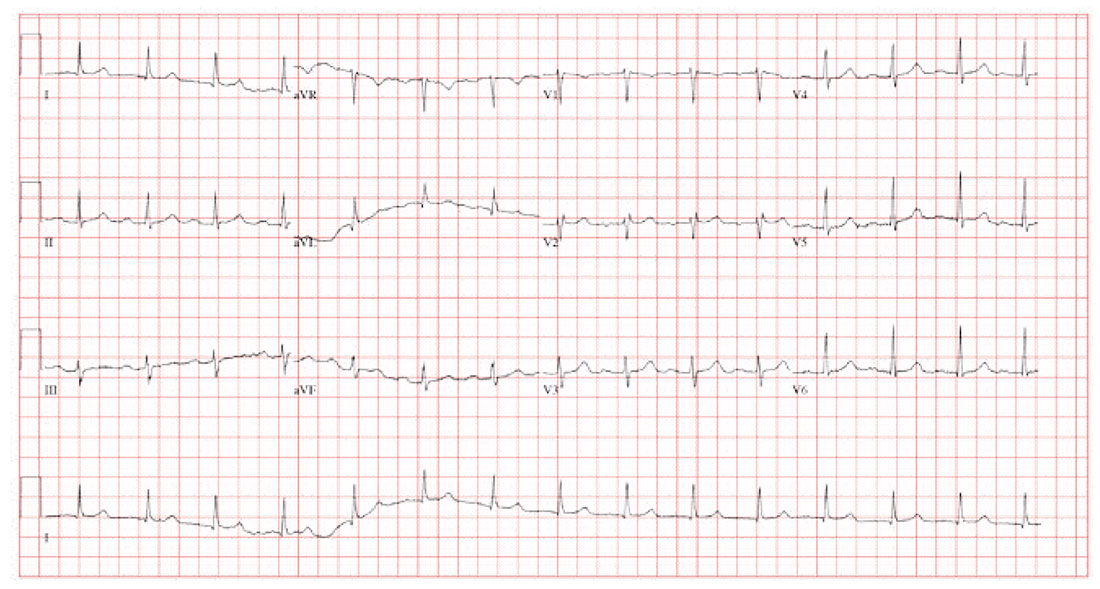
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
ANSWER
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
ANSWER
The correct interpretation includes sinus tachycardia with biatrial enlargement and ST- and T-wave abnormalities consistent with inferolateral ischemia.
Sinus tachycardia is evident from an atrial rate > 100 beats/min, with a consistent PR interval for each P and R wave.
Criteria for right atrial enlargement include tall P waves in leads II, III, and aVF, and for left atrial enlargement, P waves in lead I ≥ 110 ms with terminal negativity of the P wave in lead V1 ≥ 1 mm2. When both criteria are met, the diagnosis is biatrial enlargement.
The presence of ST elevation in lead V4 and T-wave inversions in leads V5 and V6 and limb leads II, III, and aVF suggest inferolateral ischemia.
A 34-year-old man with a history of malignant hypertension is brought to the emergency department via ACLS ambulance with substernal chest pain and a field blood pressure of 228/136 mm Hg. According to the paramedics, the patient’s symptoms include dyspnea, emotional lability, agitation, and violent behavior requiring physical restraints.
The patient is known at your institution (and many others in the area) for his frequent admissions and poor compliance with medications. Today, the patient’s agitation and paranoia prevent you from obtaining a clear history of the present illness. You do learn that he recently started working in a meth lab, where he has had free access to illicit substances.
His toxicology screen is positive for methamphetamines, cocaine, and phencyclidine. Additional lab tests indicate elevated serial troponin levels, diagnostic of non-ST-segment elevation myocardial infarction (NSTEMI), and an elevated B-type natriuretic peptide level, compatible with congestive
A review of his electronic medical record reveals allergies to sulfa and erythromycin. His medication list includes carvedilol (6.25 mg bid), furosemide (40 mg/d), and lisinopril (20 mg bid), with multiple references to noncompliance. You also note that he has had several skin and soft-tissue infections requiring both oral and IV antibiotic therapy.
The patient’s vital signs on arrival include a blood pressure of 210/140 mm Hg; pulse, 110 beats/min; respiratory rate, 20 breaths/min-1; and temperature, 38.2°C. His weight is 147 lb and his height, 69 in.
Physical exam reveals a man who appears agitated, restless, and psychotic. His skin is remarkable for multiple excoriated lesions on both upper and lower extremities. Recent needle tracks are present in both antecubital fossae.
The HEENT exam is remarkable for enlarged pupils and exophthalmos. Punctate lesions are seen on the nasal septum, and the teeth are in poor repair with multiple caries. The neck is supple, with a palpable thyroid and no evidence of jugular venous distention.
Pulmonary sounds reveal coarse rhonchi in both bases, with no evidence of wheezing. The cardiac exam reveals tachycardia with a regular rate and no extra heart sounds or murmurs. Peripheral pulses are strong and equal bilaterally. The abdominal exam is remarkable for diffuse tenderness to palpation without focal pain, as well as a firm liver edge 2 cm below the right costal margin. The neurologic exam is remarkable for agitation, paranoia, and psychosis. There are no focal cranial nerve defects.
Workup—including chest and abdominal CT, echocardiogram, and ECG—is ordered. The ECG reveals a ventricular rate of 105 beats/min; PR interval, 170 ms; QRS duration, 96 ms; QT/QTc interval, 362/478 ms; P axis, 54°; R axis, 81°; and T axis, –59°. What is your interpretation?
The Rancher, the Roof, and the Rogue Heart
ANSWER
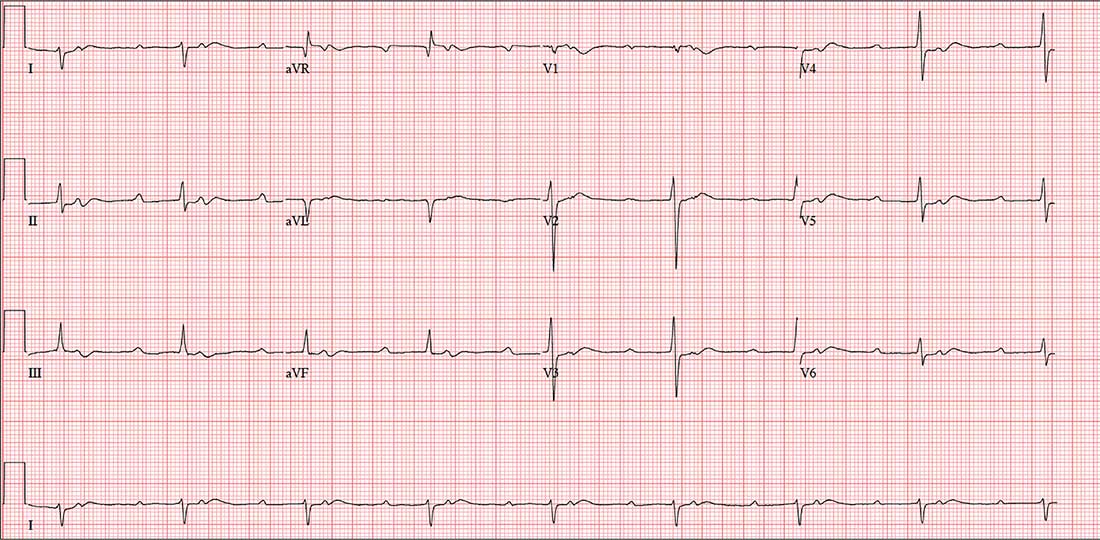
The correct interpretation of this ECG includes atrial fibrillation with variable atrioventricular (AV) block and a left-axis deviation.
Atrial fibrillation is evidenced by the absence of P waves, a consistent PR interval, and an irregularly irregular rhythm. The ventricular rate in atrial fibrillation is due to variable conduction through the AV node, and the 1.6-second pause prior to the last beat on this ECG is due to variable block in the conduction system below the AV node. Pauses such as these may result in clinical symptoms; when seen, the clinician should exercise caution in determining which method (six-second rule, 300/150/100 method) to use to measure the overall heart rate. Note that a pause of undetermined time also exists prior to the first QRS complex seen on the rhythm strip.
Finally, a left-axis deviation is evidenced by an R-wave axis between –30 and –120°.
ANSWER
The correct interpretation of this ECG includes atrial fibrillation with variable atrioventricular (AV) block and a left-axis deviation.
Atrial fibrillation is evidenced by the absence of P waves, a consistent PR interval, and an irregularly irregular rhythm. The ventricular rate in atrial fibrillation is due to variable conduction through the AV node, and the 1.6-second pause prior to the last beat on this ECG is due to variable block in the conduction system below the AV node. Pauses such as these may result in clinical symptoms; when seen, the clinician should exercise caution in determining which method (six-second rule, 300/150/100 method) to use to measure the overall heart rate. Note that a pause of undetermined time also exists prior to the first QRS complex seen on the rhythm strip.
Finally, a left-axis deviation is evidenced by an R-wave axis between –30 and –120°.
ANSWER
The correct interpretation of this ECG includes atrial fibrillation with variable atrioventricular (AV) block and a left-axis deviation.
Atrial fibrillation is evidenced by the absence of P waves, a consistent PR interval, and an irregularly irregular rhythm. The ventricular rate in atrial fibrillation is due to variable conduction through the AV node, and the 1.6-second pause prior to the last beat on this ECG is due to variable block in the conduction system below the AV node. Pauses such as these may result in clinical symptoms; when seen, the clinician should exercise caution in determining which method (six-second rule, 300/150/100 method) to use to measure the overall heart rate. Note that a pause of undetermined time also exists prior to the first QRS complex seen on the rhythm strip.
Finally, a left-axis deviation is evidenced by an R-wave axis between –30 and –120°.
Three days ago, a 74-year-old man fell from his roof, sustaining three fractured ribs and a right-sided hemothorax. He was admitted for treatment: a chest tube to drain the hemothorax and a decortication procedure the following day. His pain has been well controlled postoperatively, and he has been ambulating with his chest tube drainage system on water seal.
This morning, the telemetry technician notices pauses on the patient’s rhythm strips and pages you for interpretation and management. Puzzled as to why this patient was placed on telemetry, you order a 12-lead ECG and review the patient’s electronic medical record (EMR).
Medical history is remarkable for chronic atrial fibrillation, hypertension, hypothyroidism, and a remote history of two transient ischemic attacks (TIAs). His CHA2DS2-VASc score is calculated to be 4, given his age and medical history. When you talk to the patient, he reports no episodes of syncope, near syncope, chest pain, or shortness of breath. He explains that he’s very active and was repairing his roof in preparation for winter when he reached too far and the ladder tipped over.
The patient’s medications include warfarin, hydrochlorothiazide, metoprolol, and propylthiouracil. He has no known drug allergies and denies recreational or homeopathic medication use.
The patient has been a rancher his entire life and doesn’t see himself retiring. He has lived alone on a 200-acre ranch since his wife died of non-Hodgkin lymphoma 12 years ago. He has two adult sons, both in good health, who visit during holidays. The patient was adopted and does not know his family history. He smoked as a young adult but says he hasn’t done so “since cigarettes reached $1.00 per pack.” He has an occasional drink when friends visit but otherwise doesn’t consume alcohol.
The review of systems is remarkable only for a resolving paronychia on his left middle finger.
According to the EMR, his vital signs as of this morning include a blood pressure of 138/94 mm Hg; heart rate, 66 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 98% on 2L of oxygen via nasal prongs. His height is 6’2” and his weight, 184 lb.
Physical exam reveals an otherwise healthy yet weathered man in no distress. He has multiple old and new areas of ecchymosis on his upper and lower extremities and his right chest. A chest tube is evident exiting the right anterior chest wall. Breath sounds are distant with rhonchi on the right chest and clear and full on the left. The cardiac exam reveals no evidence of jugular venous distention. Heart rhythm is irregularly irregular at a rate of 60 beats/min. There are no murmurs, bruits, or extra heart sounds. The abdomen is soft and scaphoid with no palpable masses. His lower extremities show no evidence of pitting edema, and pulses are strong and full bilaterally. He is alert, oriented, and conversive and does not demonstrate any focal signs.
The ECG you ordered shows an unmeasurable PR interval; QRS duration, 102 ms; QT/QTc interval, 392/397 ms; P axis, unmeasured; R axis, –61°; and T axis, 76°. What is your interpretation?
No Walk in the Park
ANSWER
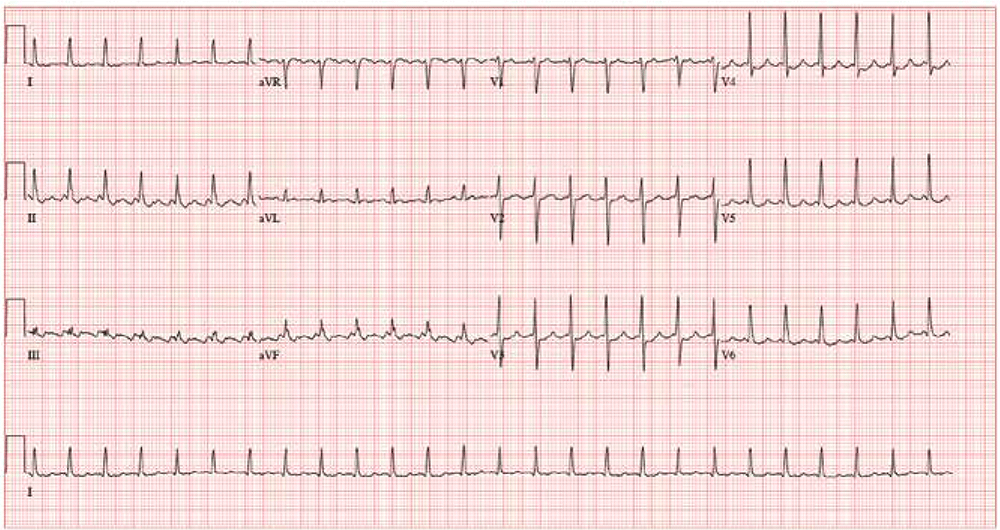
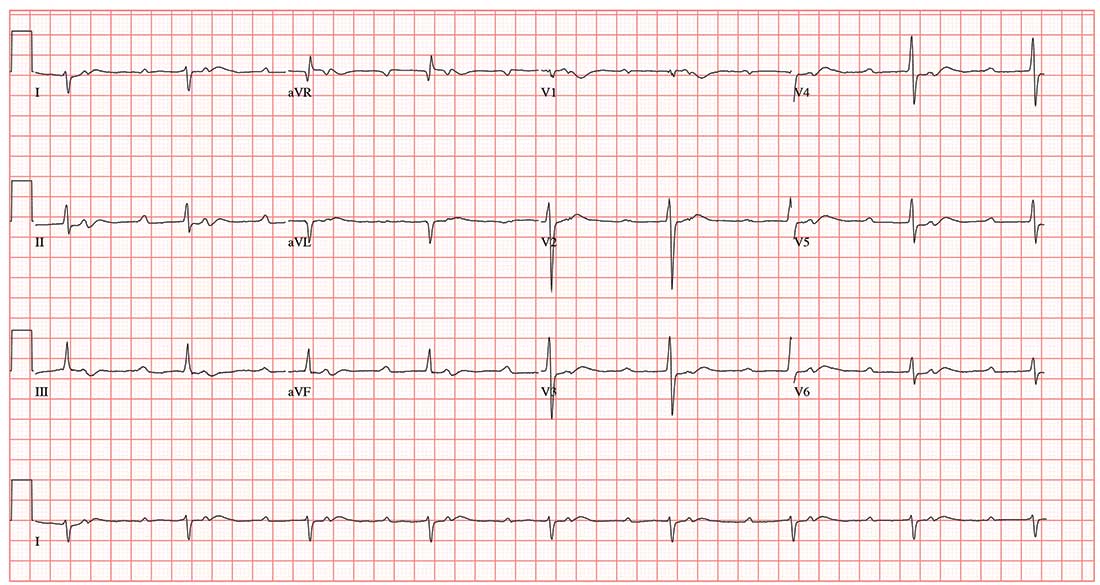
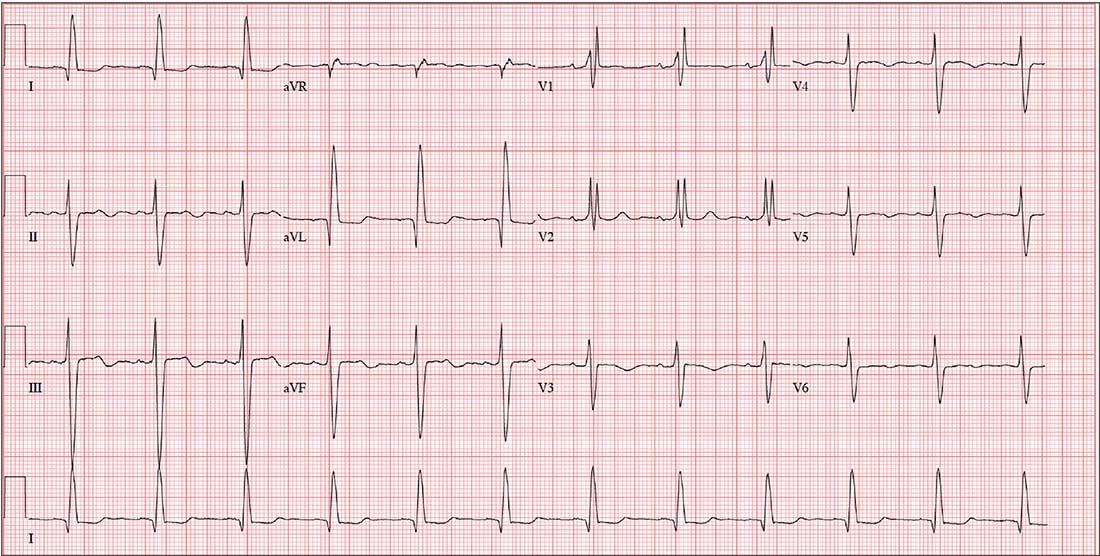
This ECG demonstrates sinus rhythm with second-degree type II block, right-axis deviation, and ST-T wave changes in the inferior leads, suggestive of ischemia. A P-P interval of 100 beats/min meets the criteria for sinus rhythm.
Second-degree type II block is evidenced by two P waves for each QRS complex with a consistent PR interval. In this example, the PR interval is significantly prolonged at 415 ms. Normally, this would be a rather impressive first-degree AV block. However, a second P wave (integrated in the ST interval, best seen in the rhythm strip at the bottom) makes this second-degree type II block.
Right-axis deviation is defined by an R-wave axis of 90° to 180°; thus this patient qualifies at 131°. Finally, ST-T wave depressions are evident in leads II, III, and aVF, suggestive but not indicative of inferior ischemia. The patient was found to have a recurrent perivalvular abscess of his artificial aortic valve, as well as right lower lobe pneumonia.
ANSWER
This ECG demonstrates sinus rhythm with second-degree type II block, right-axis deviation, and ST-T wave changes in the inferior leads, suggestive of ischemia. A P-P interval of 100 beats/min meets the criteria for sinus rhythm.
Second-degree type II block is evidenced by two P waves for each QRS complex with a consistent PR interval. In this example, the PR interval is significantly prolonged at 415 ms. Normally, this would be a rather impressive first-degree AV block. However, a second P wave (integrated in the ST interval, best seen in the rhythm strip at the bottom) makes this second-degree type II block.
Right-axis deviation is defined by an R-wave axis of 90° to 180°; thus this patient qualifies at 131°. Finally, ST-T wave depressions are evident in leads II, III, and aVF, suggestive but not indicative of inferior ischemia. The patient was found to have a recurrent perivalvular abscess of his artificial aortic valve, as well as right lower lobe pneumonia.
ANSWER
This ECG demonstrates sinus rhythm with second-degree type II block, right-axis deviation, and ST-T wave changes in the inferior leads, suggestive of ischemia. A P-P interval of 100 beats/min meets the criteria for sinus rhythm.
Second-degree type II block is evidenced by two P waves for each QRS complex with a consistent PR interval. In this example, the PR interval is significantly prolonged at 415 ms. Normally, this would be a rather impressive first-degree AV block. However, a second P wave (integrated in the ST interval, best seen in the rhythm strip at the bottom) makes this second-degree type II block.
Right-axis deviation is defined by an R-wave axis of 90° to 180°; thus this patient qualifies at 131°. Finally, ST-T wave depressions are evident in leads II, III, and aVF, suggestive but not indicative of inferior ischemia. The patient was found to have a recurrent perivalvular abscess of his artificial aortic valve, as well as right lower lobe pneumonia.
A 47-year-old man is transported to your facility by ACLS ambulance after being found unresponsive in a public park. When aggressive attempts to wake him were unsuccessful, the paramedics intubated the patient. His heart rhythm was regular at 50 beats/min, and tissues were pink with good capillary refill, suggesting he was perfusing well.
On his arrival, you realize you have encountered the patient before. He has a history of chronic intravenous (IV) drug use and group B Streptococcus endocarditis; the latter was complicated by a perivalvular abscess that required replacement with a bioprosthetic aortic valve about eight months ago. His postoperative course was complicated by intermittent atrial fibrillation with conversion pauses of 4 sec. An electrophysiology consult, for possible permanent pacemaker placement, was obtained—but the patient left against medical advice before being seen. He has been lost to follow-up since.
Today’s review of the electronic medical record identifies an allergy to sulfa and IV contrast. He has been enrolled in a methadone clinic but has not been seen there for the past month. Further history, pharmacologic regimen, and review of systems are unobtainable, as the patient is sedated and intubated.
Physical examination reveals an unconscious, unresponsive, malnourished male. His blood pressure is 96/54 mm Hg; pulse, 50 beats/min; temperature, 38.6°C; respiratory rate, 16 breaths/min-1 (ventilated); and O2 saturation, 100%. He has multiple tattoos over his upper and lower extremities and torso. Examination of the extremities reveals old and new needle tracks, with dense scarring in both antecubital fossae.
The HEENT exam is remarkable for poor dentition with multiple missing teeth and a perforated nasal septum. The neck veins are distended to the angle of the jaw. Auscultation of the lungs reveals coarse, rhonchorous mechanical breath sounds with absent breath sounds in the right base.
The cardiac exam is positive for a grade IV/VI holosystolic murmur, best heard in the left upper sternal border. The abdomen is scaphoid, and a firm liver edge is palpable 2 cm below the right costal margin. The right knee is inflamed and erythematous, with palpable fluid. The neurologic exam documents that both pupils are reactive to light.
Laboratory data reveal a positive toxicology screen for cocaine, methadone, and opioids. He also has a leukocytosis level of 24,500/µL. A supine single-view chest x-ray shows consolidation of the right lower lobe and multiple perihilar nodules that were present on a previous chest x-ray.
An ECG shows a ventricular rate of 50 beats/min; PR interval, 415 ms; QRS duration, 102 ms; QT/QTc interval, 456/415 ms; P axis, 67°; R axis, 131°; and T axis, –29°. What is your interpretation?
When Life Leaves You Breathless
ANSWER
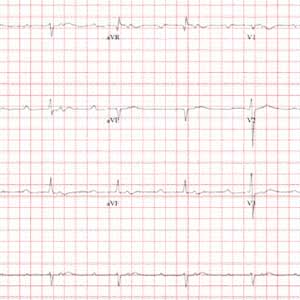
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
ANSWER
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
ANSWER
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
For the past 10 years, a 39-year-old man has experienced dyspnea on several occasions—but over the past six months, the severity has increased. The patient says he used to exercise regularly, lifting weights, running up to five miles, and swimming up to a half-mile without difficulty. Now, he can no longer run more than a half-mile without having to stop, and he has given up swimming completely. He denies syncope or near-syncope, palpitations, chest pain, and cough. There is no recent history of upper respiratory infection.
Extensive workup—including an ECG, magnetic resonance angiogram (MRA), transthoracic echocardiogram (TTE), right heart catheterization, and pulmonary function studies—is performed at an outside institution. The ECG demonstrates sinus bradycardia, MRA shows a patent foramen ovale with no shunting, and TTE shows normal left ventricular function and size with a normal ejection fraction and no valvular dysfunction. Right heart catheterization reveals pulmonary artery pressures of 30/10 mm Hg, with a mean pressure of 13 mm Hg. The cardiac output is 9.5 L/min with an arterial saturation of 99%. The Qp:Qs ratio is 1.2:1.
Medical history is positive for childhood asthma, mononucleosis, and two episodes of kidney stones. His current medications include ß-adrenergic and xanthine derivative bronchodilators. He has a true anaphylactic allergy to penicillin.
The patient is recently divorced and lives alone. He has two children, ages 4 and 6, with whom he has weekend visitation rights. He works as a sous chef at a local upscale restaurant. He does not use tobacco products, drinks one to two glasses of wine nightly, and denies recreational drug use. Family history is remarkable for asthma and COPD in both parents (who each smoke 1.5 packs/d of cigarettes).
Review of systems reveals a resolving second-degree thermal burn on the right forearm (work-related) and residual burning with urination from passage of a kidney stone approximately two weeks ago.
Vital signs include a blood pressure of 130/78 mm Hg; pulse, 50 beats/min; respiratory rate, 12 breaths/min-1; O2 saturation, 100% on room air; and temperature, 36.8°C. His weight is 172 lb and his height, 74 in.
Physical exam reveals a healthy-appearing male in no distress. There is no evidence of jugular venous distention or thyromegaly. The lungs are clear bilaterally with no wheezes, crackles, or rales. Cardiac exam reveals a regular rate and rhythm with no extra heart sounds or murmurs. The abdomen is nontender with no organomegaly or bruits. The extremities show no evidence of clubbing, cyanosis, or edema. No rashes on the skin are noted, and the patient is neurologically intact.
A repeat ECG shows a ventricular rate of 49 beats/min; PR interval, 170 ms; QRS duration, 90 ms; QT/QTc interval, 476/429 ms; P axis, 80°; R axis, 58°; and T axis, 72°. What is your interpretation?
Just Ride It Out?
ANSWER
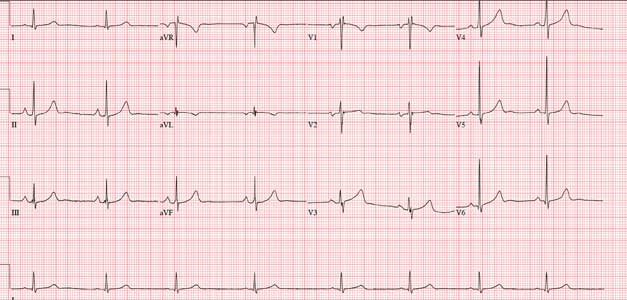
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
ANSWER
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
ANSWER
This ECG shows evidence of an acute anterior ST-elevation myocardial infarction (STEMI) and inferolateral ischemia.
STEMI criteria include a new ST-elevation in the anterior chest leads (V2–V4) at the J point (the junction of the termination of the QRS complex and the beginning of the ST segment). The American College of Cardiology/American Heart Association guidelines define cut-points for STEMI as follows: in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. In this ECG, the classic “tombstone” pattern can be seen in the T wave in leads V3 and V4.
Inferolateral ischemia is evidenced by the ST elevation and T-wave flattening in the inferior leads II, III, and aVF, as well as in lateral chest leads V5 and V6.
The patient was transferred via ACLS ambulance to a tertiary care hospital for cardiac intervention
A 61-year-old avid cyclist is training for his third triathlon this year. About a week ago, after completing a 25-mile bike ride, he developed substernal chest discomfort, which he attributed to his longstanding history of GERD and his discontinuation of omeprazole. The discomfort resolved quickly with rest, and he was symptom free until two days ago. At that time, he “just rode through” the discomfort.
Today, however, about five miles into his ride, the discomfort was so severe that he stopped to wait for it to resolve. When it did not, he slowly rode another three miles to the urgent care center to request antacids and a prescription for a proton pump inhibitor.
He describes the problem as a combination of a burning sensation and a dull ache. It does not radiate beyond the substernal area. He denies shortness of breath and is not diaphoretic. He has never had hypertension, angina, dyspnea, syncope, or near-syncope.
His medical history is remarkable only for GERD. As a child, he sustained a nondisplaced fracture of his left clavicle. He has never had a surgical procedure.
The patient, an architect, is married with two adult children. He and his wife split a bottle of wine every other day, and he says he drinks 8 to 10 cups of coffee per day on average. He has never smoked tobacco or used recreational drugs.
Family history is remarkable for type 2 diabetes (father) and hypothyroidism (mother). Both parents are alive and otherwise well. The patient’s one sibling, a brother, died in a private plane accident.
Current medications include ibuprofen and chewable antacids. He took OTC omeprazole daily for about four months, but he recently ran out and hasn’t purchased more. He has a true anaphylactic allergy to sulfa.
Review of systems is unremarkable, other than typical muscle fatigue from cycling.
Vital signs include a blood pressure of 122/64 mm Hg; pulse, 80 beats/min, respiratory rate, 12 breaths/min-1; and temperature, 97.4°F. His height is 74 in and his weight, 184 lb.
The physical exam reveals an otherwise healthy-appearing male in no acute distress. He appears frustrated that he cannot get back out on his bike. There are no pertinent findings on physical exam. The lungs are clear, and the cardiac exam reveals a regular rate and rhythm with no murmurs, gallops, rubs, or extra heart sounds. The abdomen is soft and nontender, and there is no hepatojugular reflux. Peripheral pulses are strong bilaterally, and there are no neurologic focal signs.
The ECG reveals a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; Q axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation?
One Heck of a Check-up
ANSWER
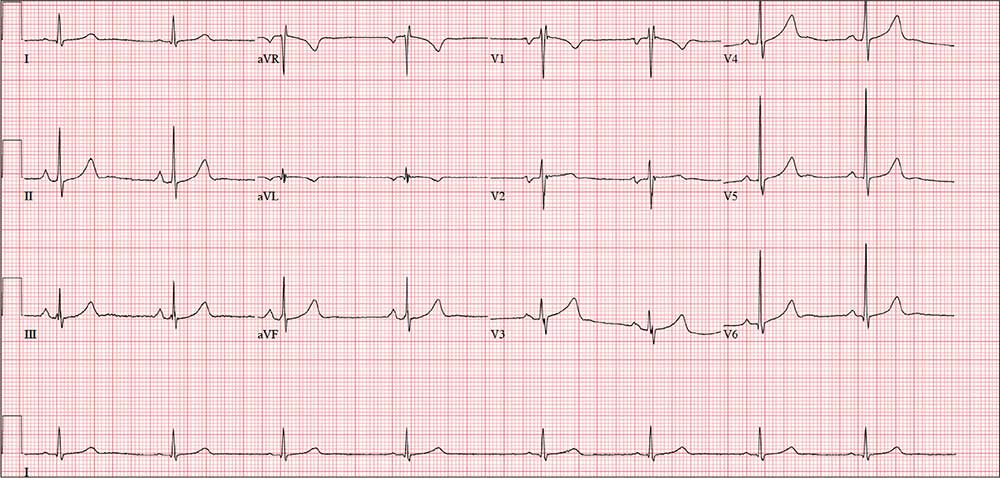
The correct interpretation includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats, and an intraventricular conduction delay.
This type of ECG is not ideal for calculating the ventricular rate via the 30/150/100 method. An easier method is to multiply the number of QRS complexes in the rhythm strip by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). In the absence of a permanent pacemaker, variation of a few beats/min from the computer reading is acceptable. In this case, multiplying 9 x 6 yields a rate of 54 beats/min (close to the computer reading of 55) and reveals sinus bradycardia.
Looking at the lead I rhythm strip, notice that while the QRS complexes in the fourth and eighth beats look similar to the others, they are not preceded by P waves; the T waves of these two beats are also not similar to the others. These represent junctional escape beats, with a possible retrograde P wave in the T-wave complex. The long pauses and the absence of a P wave prior to the fourth and eighth beats make this a sinus arrhythmia.
The diagnosis of an intraventricular conduction delay can be made by the duration of the QRS complex (122 ms), which is above normal limits. This ECG does not meet the clear criteria for a right bundle branch block (QRS ≥ 120 ms, terminal broad S wave in lead I, RSR’ in V1) or left bundle branch block (QRS ≥ 120 ms, ST depressions and inverted T waves, particularly in I, aVL, V5, and V6).
ANSWER
The correct interpretation includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats, and an intraventricular conduction delay.
This type of ECG is not ideal for calculating the ventricular rate via the 30/150/100 method. An easier method is to multiply the number of QRS complexes in the rhythm strip by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). In the absence of a permanent pacemaker, variation of a few beats/min from the computer reading is acceptable. In this case, multiplying 9 x 6 yields a rate of 54 beats/min (close to the computer reading of 55) and reveals sinus bradycardia.
Looking at the lead I rhythm strip, notice that while the QRS complexes in the fourth and eighth beats look similar to the others, they are not preceded by P waves; the T waves of these two beats are also not similar to the others. These represent junctional escape beats, with a possible retrograde P wave in the T-wave complex. The long pauses and the absence of a P wave prior to the fourth and eighth beats make this a sinus arrhythmia.
The diagnosis of an intraventricular conduction delay can be made by the duration of the QRS complex (122 ms), which is above normal limits. This ECG does not meet the clear criteria for a right bundle branch block (QRS ≥ 120 ms, terminal broad S wave in lead I, RSR’ in V1) or left bundle branch block (QRS ≥ 120 ms, ST depressions and inverted T waves, particularly in I, aVL, V5, and V6).
ANSWER
The correct interpretation includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats, and an intraventricular conduction delay.
This type of ECG is not ideal for calculating the ventricular rate via the 30/150/100 method. An easier method is to multiply the number of QRS complexes in the rhythm strip by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). In the absence of a permanent pacemaker, variation of a few beats/min from the computer reading is acceptable. In this case, multiplying 9 x 6 yields a rate of 54 beats/min (close to the computer reading of 55) and reveals sinus bradycardia.
Looking at the lead I rhythm strip, notice that while the QRS complexes in the fourth and eighth beats look similar to the others, they are not preceded by P waves; the T waves of these two beats are also not similar to the others. These represent junctional escape beats, with a possible retrograde P wave in the T-wave complex. The long pauses and the absence of a P wave prior to the fourth and eighth beats make this a sinus arrhythmia.
The diagnosis of an intraventricular conduction delay can be made by the duration of the QRS complex (122 ms), which is above normal limits. This ECG does not meet the clear criteria for a right bundle branch block (QRS ≥ 120 ms, terminal broad S wave in lead I, RSR’ in V1) or left bundle branch block (QRS ≥ 120 ms, ST depressions and inverted T waves, particularly in I, aVL, V5, and V6).
He remained stable for six years, but then his exertional angina returned. Repeat catheterization showed progressive disease in the right coronary artery (RCA) with new disease in an obtuse marginal (OM) branch of the circumflex artery. His LVEF had also diminished to 38%. Stents were placed in the RCA and OM arteries, and his ß-blocker dose was increased.
Today, he reports that over the past six months, his heart rate has been slow and often skips beats. He stopped taking his ß-blocker, hoping it would help speed up his heart; it didn’t. He says he feels fine right now (although his heart continues to skip beats). He says he can climb a flight of stairs without difficulty and denies chest pain, dyspnea, dizziness, or syncope. At night, he sleeps on one or two pillows. He denies orthopnea, paroxysmal nocturnal dyspnea, or peripheral edema.
Medical history includes type 2 diabetes (controlled with diet and exercise), degenerative joint disease, and hyperlipidemia. Surgical history includes a tonsillectomy and trigger finger repair of the left third digit. His current medications include clopidogrel, losartan, pravastatin, spironolactone, and aspirin. He has no known drug allergies.
The patient used to be a heavy smoker (> 2 packs/d) but quit after his first stent was placed. He drinks one to two glasses of wine per week and denies recreational drug use.
Family history is positive for coronary artery disease and stroke. His father died of CAD at age 60, and his mother of heart failure at 58.
A review of systems is noncontributory. Vital signs include a blood pressure of 118/80 mm Hg; pulse, 53 beats/min; temperature, 37°C; respiratory rate, 14 breaths/min-1; and O2 saturation, 96% on room air. His weight is 214 lb and his height, 70 in.
Physical exam reveals an alert, well-kept male in no distress. Pertinent findings include a regularly irregular pulse and normal S1 and S2, with no murmurs, gallops, or rubs. The lungs are clear bilaterally. The abdomen is soft and benign with no organomegaly. Peripheral pulses are 2+ bilaterally, and there is no peripheral edema or calf tenderness. Neurologic exam shows a grossly intact sensory and motor system with no focal signs.
An ECG reveals a ventricular rate of 55 beats/min; PR interval, 146 ms; QRS duration, 122 ms; QT/QTc interval, 424/405 ms; P axis, 60°; R axis, 38°; and T axis, 29°. What is your interpretation?
Woman’s Pain is Per-cyst-ent
ANSWER
The correct interpretation includes sinus tachycardia with second-degree type 2 (Mobitz II) block, 2:1 AV conduction, and a right-axis deviation.
The P-P interval is 100 beats/min—twice the rate of the QRS complexes. A consistent PR interval > 200 ms supports the diagnosis of first-degree AV block, as the ratio of two P waves for every QRS does for 2:1 AV conduction. Finally, a right-axis deviation is evidenced by an axis > 90°.
These findings are suggestive of AV nodal disease and may explain the patient’s recent increase in fatigue (noted in the review of systems).
ANSWER
The correct interpretation includes sinus tachycardia with second-degree type 2 (Mobitz II) block, 2:1 AV conduction, and a right-axis deviation.
The P-P interval is 100 beats/min—twice the rate of the QRS complexes. A consistent PR interval > 200 ms supports the diagnosis of first-degree AV block, as the ratio of two P waves for every QRS does for 2:1 AV conduction. Finally, a right-axis deviation is evidenced by an axis > 90°.
These findings are suggestive of AV nodal disease and may explain the patient’s recent increase in fatigue (noted in the review of systems).
ANSWER
The correct interpretation includes sinus tachycardia with second-degree type 2 (Mobitz II) block, 2:1 AV conduction, and a right-axis deviation.
The P-P interval is 100 beats/min—twice the rate of the QRS complexes. A consistent PR interval > 200 ms supports the diagnosis of first-degree AV block, as the ratio of two P waves for every QRS does for 2:1 AV conduction. Finally, a right-axis deviation is evidenced by an axis > 90°.
These findings are suggestive of AV nodal disease and may explain the patient’s recent increase in fatigue (noted in the review of systems).
In the past six to eight months, a 58-year-old woman has experienced abnormal vaginal bleeding and a “heavy” feeling in her lower abdomen. She has also noticed pelvic pain with intercourse. About two months ago, she began having difficulty emptying her bladder. Abdominal CT and MRI revealed a 3-cm cyst of the right ovary. She is scheduled for laparoscopic surgery to remove it and presents for preoperative assessment.
The patient is G3P2A1 and transitioned through menopause at age 53. Medical history is remarkable for gestational diabetes during her second pregnancy; she has had no further symptoms or findings to support the diagnosis since. Both children were delivered by uncomplicated vaginal delivery. During her third pregnancy, she miscarried at 12 weeks.
She has no history of cardiac or pulmonary disease. Surgical history is remarkable for an open reduction internal fixation of a left high ankle fracture at age 18 and for dilation and curettage following her miscarriage.
Social history reveals a 30-year marriage and employment as a tax accountant. The patient drinks one to two glasses of wine nightly and has never smoked. She did try marijuana briefly during college but hasn’t used any illicit substances since.
Family history is positive for coronary artery disease (father) and hypothyroidism (mother). Her children, now adults, are alive and well, with no known medical problems.
Current medications include ibuprofen for abdominal discomfort and diazepam for anxiety; she started the latter after receiving her CT and MRI results. She has no known drug or food allergies.
Review of systems reveals a two-month history of decreased energy and stamina. She denies palpitations or skipped heart beats and shortness of breath or dyspnea on exertion. She does say that she fatigues more easily than she did three months ago. The remainder of the review is uneventful.
Vital signs include a blood pressure of 108/72 mm Hg; pulse, 50 beats/min; respiratory rate, 14 breaths/min-1; temperature, 97.6°F; and O2 saturation, 98% on room air. Her weight is 158 lb and her height, 66 in.
Physical exam reveals an anxious but alert woman in no apparent distress. Corrective lenses are present. There is no evidence of thyromegaly or jugular venous distention. The lungs are clear in all fields. The cardiac exam reveals a regular rate of 50 beats/min with a regular rhythm. There are no murmurs, rubs, or extra heart sounds.
The breasts are well developed and symmetrical, with no discharge. The abdomen is soft and nontender. She states that palpation of the right lower quadrant is uncomfortable but not painful. The ovarian mass is not palpable. Vaginal and rectal exams are deferred.
Her extremities reveal full range of motion with strong peripheral pulses bilaterally. A well-healed surgical scar is present on the lateral aspect of her left lower leg. The neurologic exam is grossly intact, without focal signs.
A preoperative ECG shows a ventricular rate of 50 beats/min; PR interval, 432 ms; QRS duration, 102 ms; QT/QTc interval, 456/415 ms; P axis, 67°; R axis, 131°; and T axis, –29°. What is your interpretation?
This Evaluation Is a Heart-stopper
ANSWER
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
ANSWER
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
ANSWER
The correct interpretation includes normal sinus rhythm with left-axis deviation, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB).
Normal sinus rhythm is evidenced by a P for every QRS and a QRS for every P, with a consistent PR interval and a rate between 60 and 100 beats/min.
A left-axis deviation is indicated by an R-wave axis of –48°, which is less than the upper limit of normal (–30°).
Criteria for an RBBB include a QRS duration ≥ 120 ms with an RSR’ complex in lead V1. A terminal broad S wave in lead I, often seen with RBBB, is not evident in this ECG.
Finally, the criteria for LAFB include S waves > R waves in leads I, II, and aVF, which are well illustrated in this ECG. The combination of an RBBB and an LAFB is consistent with bifascicular block and places the patient at increased risk for complete heart block
A 79-year-old man with a history of aortic stenosis presents for preoperative evaluation for aortic valve replacement versus transcatheter aortic valve placement. Over the past three months, he has developed worsening shortness of breath, dyspnea on exertion, chest tightness, and lightheadedness, but no frank syncope. One month ago, he was hospitalized for heart failure, which improved with IV diuresis.
An echocardiogram performed one week ago showed an aortic valve area of 0.5 cm, with a peak velocity of 5.4 m/s and a mean gradient of 64 mm Hg. The left ventricular function was normal, with an ejection fraction of 72%. The pulmonary artery pressure measured 40 mm Hg. Other findings included mild-to-moderate mitral and tricuspid valve regurgitation.
Cardiac history is also positive for coronary artery disease, with a recent coronary angiogram showing 60% stenosis in the proximal left anterior descending artery and 80% stenosis of the mid-portion of the right coronary artery.
Medical history is positive for hypertension, type 2 diabetes, and osteoarthritis. Surgical history includes bilateral knee replacements. Current medications include aspirin, furosemide, metformin, atorvastatin, and metoprolol. The patient is allergic to sulfa-containing medications.
Social history reveals that he is a retired police officer who is married and has three adult children. He does not smoke, enjoys an occasional beer, and denies recreational drug use. Family history is notable for coronary artery disease, hypertension, and diabetes.
Review of systems reveals no additional complaints. It is noted that he wears hearing aids and glasses.
Vital signs include a blood pressure of 110/64 mm Hg; pulse, 70 beats/min; and respiratory rate, 14 breaths/min-1. O2 saturation is 96% on room air. His weight is 214 lb and his height, 74 in.
On physical exam, you find a congenial but inquisitive male in no distress, with jugular venous distention at 8 cm, clear lung fields, and a regular heart rate and rhythm. There is a grade 3/6 systolic ejection murmur at the right upper sternal border but no extra heart sounds or rubs. The abdomen is soft and nontender. Peripheral pulses are 2+ bilaterally without femoral bruits, and surgical scars are present over both knees. There is trace pitting edema bilaterally in the lower extremities. The neurologic exam is intact, without focal signs.
An ECG, obtained as part of his preoperative workup, reveals a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation?