User login
Time to log off: New diagnostic criteria for problematic Internet use
Many psychiatrists diagnose problematic Internet use with schemas based on substance use disorders and pathologic gambling. These predefined diagnoses, however, may lead to premature conclusions and prevent you from fully exploring other treatable diagnoses.
We propose a screening tool called “MOUSE” and diagnostic criteria for problematic Internet use, which we developed from research by our group and others. This article discusses the new criteria and answers three questions:
- How does problematic Internet use present?
- Is it an addiction or an impulse control disorder?
- How can we help those afflicted with this problem?
When Internet use goes over the line
Recognizing problematic Internet use is difficult because the Internet can serve as a tool in nearly every aspect of our lives—communication, shopping, business, travel, research, entertainment, and more. The evidence suggests that Internet use becomes a behavior disorder when:
- an individual loses the ability to control his or her use and begins to suffer distress and impaired daily function1
- and employment and relationships are jeopardized by the hours spent online2 (Box).
Relationships—particularly marriages but also parent-child relationships, dating relationships, and close friendships—appear to suffer the greatest harm. At least one-half of “Internet addicts” (53%) report that their Internet use has caused serious relationship problems.
School. Academic problems are common; one study showed 58% of students blamed Internet use for a drop in grades, missed classes, declining study habits, or being placed on probation.
Workplace. Many executives—55% in one study—complain that time spent on the Internet for non-business purposes reduces their employees’ effectiveness.
Health. Some users spend 40 to 80 hours per week online, and single sessions can last up to 20 hours. Lack of sleep results in fatigue, decreased exercise, and decreased immunity. Sitting in front of the computer for hours also increases the risk of carpal tunnel syndrome, eye strain, and back pain.
Other addictions. The more time spent on the Internet, the greater the user’s risk of exposure to other addictive activities, such as online gambling and sexual solicitations. This risk is particularly concerning in children and adolescents.
Source: Young KS. Innovations in Clin Pract 1999;17:19-31.
Case: Computer gamer out of control
Mr. A is 32 and in his fourth year of college. His psychiatric history includes obsessive-compulsive disorder (OCD), paraphilia not otherwise specified, and bipolar disorder, most recently depressed in partial remission. He has had only one manic episode 10 years ago and took lithium briefly. He experienced pleasure from masturbating in public, but his paraphilia did not meet criteria for voyeurism as he did not want to be seen. He engaged in this behavior from ages 16 to 18 and found it distressing.
He is taking no medications. The only clinically significant family history is his father’s apparent OCD, undiagnosed and untreated.
Mr. A’s excessive computer use started in high school, when he played computer games to the point where his grades suffered. He began using the Internet at age 28, just before starting college, and spent most of his time online playing multi-player, video/strategy games.
Mr. A underestimates the time he spends online at 24 hours per week, including 21 hours in nonessential use and 3 hours in essential use (required for job or school). His actual average is 35.9 hours per week—nearly equivalent to a full-time job. He divides his nonessential use among various online activities, mostly related to playing computer games:
- 35% in chat forums, communicating with gaming partners he has never met
- 25% in multi-player, video/strategy games
- 15% using e-mail
- and lesser times surfing the Web (5%), transferring files (5%), viewing pornography (5%), shopping (5%), listening to music (3%), and selling (2%).
He reports rising tension before logging on and relief after doing so. He admits to using the Internet for longer periods than intended and especially when emotionally stressed. He knows his behavior has hurt him academically, and he has tried unsuccessfully to cut down or stop his Internet use.
Internet overuse: An ‘addiction’?
Ivan Goldberg introduced the idea of Internet addiction in 1995 by posting factitious “diagnostic criteria” on a Web site as a joke.3 He was surprised at the overwhelming response he received from persons whose Internet use was interfering with their lives. The first case reports were soon published.4,5
Initially, excessive Internet use was called an “addiction”—implying a disorder similar to substance dependence. Recently, however, Internet overuse has come to be viewed as more closely resembling an impulse control disorder.5-8 Shapira et al studied 20 subjects with problematic Internet use, and all met DSM-IV criteria for an impulse control disorder, not otherwise specified. Three also met criteria for obsessive-compulsive disorder.1
As with other impulse control disorders (such as eating disorders and pathologic gambling), researchers have noticed increased depression associated with pathologic Internet use.8
Diagnostic criteria. Although Mr. A’s comorbid psychiatric illnesses complicate his presentation, his behavior clearly could be described as representing an impulse control disorder. His case also meets our proposed criteria for problematic Internet use (Table 1),9 which we define as:
- uncontrollable
- markedly distressing, time-consuming, or resulting in social, occupational, or financial difficulties
- and not solely present during mania or hypomania.
Teasing out comorbid disorders
As in Mr. A’s case, Internet overuse can serve as an expression of and a conduit for other psychiatric illnesses. Studies have found high rates of comorbidity with mood and anxiety disorders, social phobias, attention-deficit disorder with or without hyperactivity, paraphilias, insomnia, pathologic gambling, and substance use disorders.10-12
Although some researchers feel that the many comorbid and complicating factors cannot be teased out,13 most agree that compulsive Internet use or overuse can have adverse consequences and that more research is needed.
A predisposition? Are “Internet addicts” predisposed to or susceptible to Internet overuse? Researchers are exploring whether Internet overuse causes or is an effect of psychiatric illness.
Shapira et al1,14 found at least one psychiatric condition that predated the development of Internet overuse in 20 subjects. In a similar study of 21 subjects with excessive computer use, Black11 found:
- 33% had a mood disorder
- 38% had a substance use disorder
- 19% had an anxiety disorder
- 52% met criteria for at least one personality disorder.
On average, these 41 subjects were in their 20s and 30s and reported having problems with Internet use for about 3 years. They spent an average of 28 hours per week online for pleasure or recreation, and many experienced emotional distress, social impairment, and social, occupational, or financial difficulties.1,11
Table 1
PROPOSED DIAGNOSTIC CRITERIA FOR PROBLEMATIC INTERNET USE
| Maladaptive preoccupation with Internet use, as indicated by at least one of the following: |
|
|
| Source: Reprinted with permission from an article by Shapira et al9 that has been accepted for publication in Depression and Anxiety. © Copyright 2003 John Wiley & Sons. |
Isolation and depression. Increasing Internet use and withdrawal from family activities has been associated with increased depression and loneliness; Kraut et al15 hypothesized that the Internet use caused the depression. Pratarelli et al16 noted a maladaptive cycle in some persons; the more isolated they feel, the more they use the Internet and increase their social withdrawal.
In a survey of college students, individuals with “Internet addiction” were found to:
- have obsessive characteristics
- prefer online interactions to real-life interactions
- use the Internet “to feel better,” alleviate depression, and become sexually aroused.16
Personality traits. In another study, Orzack12 found that subjects viewed the computer as a means to satisfy, induce excitement, and reduce tension or induce relief. Six personality traits were identified as strong predictors of “Internet addiction disorder:”
- boredom
- private self-consciousness
- loneliness
- social anxiety
- shyness
- and low self-esteem.
Table 2
5 SCREENING QUESTIONS FOR PROBLEMATIC INTERNET USE
| More than intended time spent online? |
| Other responsibilities or activities neglected? |
| Unsuccessful attempts to cut down? |
| Significant relationship discord due to use? |
| Excessive thoughts or anxiety when not online? |
Diagnosing Internet overuse
Screening. During any psychiatric interview, ask patients how they spend their free time or what they most enjoy doing. If patients say they spend hours on the Internet or their use appears to usurp other activities, five questions—easily recalled by the mnemonic MOUSE—can help you screen for problematic Internet use (Table 2).
History. Typically, persons with problematic Internet use spend time in one Internet domain, such as chat rooms, interactive games, news groups, or search engines.17 Ask which application they use, how many hours they use it, how they rank the importance of various applications, and what they like about their preferred application.
To determine how the Internet may alter the patient’s moods, ask how he or she feels while online as opposed to offline. Keeping an hourly log and a “feelings diary” may help the patient sort through his or her emotions.17
Often patients use the Internet to escape from dissatisfaction or disappointment or to counteract a sense of personal inadequacy.17 They tend to take pride in their computer skills2 and incorporate them into their daily lives in many ways, allowing them to rationalize their excessive Internet use (“I’m using it for work, academics, travel, research, etc.”).
Chomorbidities. Given the high incidence of psychiatric comorbidity,1 it is important to complete a thorough psychiatric evaluation and treat any underlying illness. Whether the illness is primary or comorbid, it is likely exacerbating the symptoms of problematic Internet use.
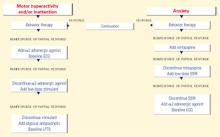
Changing problematic behaviors
Psychotherapy. Once you find the motives and possible causes of Internet overuse, what is the best form of treatment? This question warrants further study, but cognitive-behavioral therapy (CBT) is the primary treatment at this time.
The goal of CBT is for patients to disrupt their problematic computer use and reconstruct their routines with other activities. They can:
- use external timers to keep track of time online
- set goals of brief, frequent sessions online
- carry cards listing the destructive effects of their Internet use and ranking other activities they have neglected.17
Using emotion journals or mood monitoring forms may help the patient discover which dysfunctional thoughts and feelings are triggering excessive Internet use.12 Support groups and family therapy can help repair damaged relationships and engage friends and family in the treatment plan.
Drug therapy. No studies have looked at drug therapy for problematic Internet use, beyond treating comorbid psychiatric illnesses.
Treatment declined. Mr. A declined treatment for his problematic Internet use. As in many other psychiatric illnesses, insight into impulse control disorders tends to be limited. We can address the problem directly and offer to help patients change their online behaviors, but we cannot force them into treatment if they are not endangering themselves or others.
Related resources
- Computer Addiction Services. Maressa Hecht Orzack, PhD. www.computeraddiction.com; (617) 855-2908.
- Center for Online Addiction. Kimberly S. Young, PhD. www.netaddiction.com; (877) 292-3737.
1. Shapira NA, Goldsmith TG, Keck PE, Jr, Khosla UM, McElroy SL. Psychiatric features of individuals with problematic Internet use. J Affect Disord 2000;57:267-72.
2. Beard KW, Wolf EM. Modification in the proposed diagnostic criteria for Internet addiction. Cyberpsychol Behav 2001;4:377-83.
3. Goldberg I. Internet addiction. Available at http://www.cybernothing.org/jdfalk/media-coverage/archive/msg01305.html. Accessed Feb. 26, 2003.
4. Griffiths MD. Internet addiction: an issue for clinical psychology? Clin Psychol Forum 1996;97:32-6.
5. Young KS. Psychology of computer use: XL. Addictive use of the Internet: a case that breaks the stereotype. Psychol Rep 1996;79:899-902.
6. Treuer T, Fábián Z, Füredi J. Internet addiction associated with features of impulse control disorder: is it a real psychiatric disorder? J Affect Disord 2001;66:283.-
7. Young KS. Caught in the net: how to recognize the signs of Internet addiction-and a winning strategy for recovery. New York: John Wiley & Sons, Inc. 1998;8.-
8. Young KS, Rogers RC. The relationship between depression and Internet addiction. Cyberpsychol Behav 1998;1:25-8.
9. Shapira NA, Lessig MC, Goldsmith TD, et al. Problematic Internet use: proposed classification and diagnostic criteria. Depress Anxiety (in press).
10. Griffiths MD. Internet addiction: Fact or fiction? Psychologist 1999;12:246-50.
11. Black DW, Belsare G, Schlosser S. Clinical features, psychiatric comorbidity, and health-related quality of life in persons reporting compulsive computer use behavior. J Clin Psychiatry 1999;60:839-44.
12. Orzack MH. How to recognize and treat computer.com addictions. Directions in Mental Health Counseling 1999;9:13-20.
13. Stein DJ. Internet addiction, Internet psychotherapy (letter; comment). Am J Psychiatry 1997;154(6):890.-
14. Shapira NA. Unpublished data, 2000.
15. Kraut R, Lundmark V, Patterson M, Kiesler S, Mukopadhyay T, Scherlis W. Internet paradox: A social technology that reduces social involvement and psychological wellbeing? Am Psychol 1998;53:1017-31.
16. Pratarelli ME, Browne BL. Confirmatory factor analysis of Internet use and addiction. Cyberpsychol Behav 2002;5:53-64.
17. Young KS. Internet addiction: symptoms, evaluation and treatment. Innovations in Clin Pract 1999;17:19-31.
Many psychiatrists diagnose problematic Internet use with schemas based on substance use disorders and pathologic gambling. These predefined diagnoses, however, may lead to premature conclusions and prevent you from fully exploring other treatable diagnoses.
We propose a screening tool called “MOUSE” and diagnostic criteria for problematic Internet use, which we developed from research by our group and others. This article discusses the new criteria and answers three questions:
- How does problematic Internet use present?
- Is it an addiction or an impulse control disorder?
- How can we help those afflicted with this problem?
When Internet use goes over the line
Recognizing problematic Internet use is difficult because the Internet can serve as a tool in nearly every aspect of our lives—communication, shopping, business, travel, research, entertainment, and more. The evidence suggests that Internet use becomes a behavior disorder when:
- an individual loses the ability to control his or her use and begins to suffer distress and impaired daily function1
- and employment and relationships are jeopardized by the hours spent online2 (Box).
Relationships—particularly marriages but also parent-child relationships, dating relationships, and close friendships—appear to suffer the greatest harm. At least one-half of “Internet addicts” (53%) report that their Internet use has caused serious relationship problems.
School. Academic problems are common; one study showed 58% of students blamed Internet use for a drop in grades, missed classes, declining study habits, or being placed on probation.
Workplace. Many executives—55% in one study—complain that time spent on the Internet for non-business purposes reduces their employees’ effectiveness.
Health. Some users spend 40 to 80 hours per week online, and single sessions can last up to 20 hours. Lack of sleep results in fatigue, decreased exercise, and decreased immunity. Sitting in front of the computer for hours also increases the risk of carpal tunnel syndrome, eye strain, and back pain.
Other addictions. The more time spent on the Internet, the greater the user’s risk of exposure to other addictive activities, such as online gambling and sexual solicitations. This risk is particularly concerning in children and adolescents.
Source: Young KS. Innovations in Clin Pract 1999;17:19-31.
Case: Computer gamer out of control
Mr. A is 32 and in his fourth year of college. His psychiatric history includes obsessive-compulsive disorder (OCD), paraphilia not otherwise specified, and bipolar disorder, most recently depressed in partial remission. He has had only one manic episode 10 years ago and took lithium briefly. He experienced pleasure from masturbating in public, but his paraphilia did not meet criteria for voyeurism as he did not want to be seen. He engaged in this behavior from ages 16 to 18 and found it distressing.
He is taking no medications. The only clinically significant family history is his father’s apparent OCD, undiagnosed and untreated.
Mr. A’s excessive computer use started in high school, when he played computer games to the point where his grades suffered. He began using the Internet at age 28, just before starting college, and spent most of his time online playing multi-player, video/strategy games.
Mr. A underestimates the time he spends online at 24 hours per week, including 21 hours in nonessential use and 3 hours in essential use (required for job or school). His actual average is 35.9 hours per week—nearly equivalent to a full-time job. He divides his nonessential use among various online activities, mostly related to playing computer games:
- 35% in chat forums, communicating with gaming partners he has never met
- 25% in multi-player, video/strategy games
- 15% using e-mail
- and lesser times surfing the Web (5%), transferring files (5%), viewing pornography (5%), shopping (5%), listening to music (3%), and selling (2%).
He reports rising tension before logging on and relief after doing so. He admits to using the Internet for longer periods than intended and especially when emotionally stressed. He knows his behavior has hurt him academically, and he has tried unsuccessfully to cut down or stop his Internet use.
Internet overuse: An ‘addiction’?
Ivan Goldberg introduced the idea of Internet addiction in 1995 by posting factitious “diagnostic criteria” on a Web site as a joke.3 He was surprised at the overwhelming response he received from persons whose Internet use was interfering with their lives. The first case reports were soon published.4,5
Initially, excessive Internet use was called an “addiction”—implying a disorder similar to substance dependence. Recently, however, Internet overuse has come to be viewed as more closely resembling an impulse control disorder.5-8 Shapira et al studied 20 subjects with problematic Internet use, and all met DSM-IV criteria for an impulse control disorder, not otherwise specified. Three also met criteria for obsessive-compulsive disorder.1
As with other impulse control disorders (such as eating disorders and pathologic gambling), researchers have noticed increased depression associated with pathologic Internet use.8
Diagnostic criteria. Although Mr. A’s comorbid psychiatric illnesses complicate his presentation, his behavior clearly could be described as representing an impulse control disorder. His case also meets our proposed criteria for problematic Internet use (Table 1),9 which we define as:
- uncontrollable
- markedly distressing, time-consuming, or resulting in social, occupational, or financial difficulties
- and not solely present during mania or hypomania.
Teasing out comorbid disorders
As in Mr. A’s case, Internet overuse can serve as an expression of and a conduit for other psychiatric illnesses. Studies have found high rates of comorbidity with mood and anxiety disorders, social phobias, attention-deficit disorder with or without hyperactivity, paraphilias, insomnia, pathologic gambling, and substance use disorders.10-12
Although some researchers feel that the many comorbid and complicating factors cannot be teased out,13 most agree that compulsive Internet use or overuse can have adverse consequences and that more research is needed.
A predisposition? Are “Internet addicts” predisposed to or susceptible to Internet overuse? Researchers are exploring whether Internet overuse causes or is an effect of psychiatric illness.
Shapira et al1,14 found at least one psychiatric condition that predated the development of Internet overuse in 20 subjects. In a similar study of 21 subjects with excessive computer use, Black11 found:
- 33% had a mood disorder
- 38% had a substance use disorder
- 19% had an anxiety disorder
- 52% met criteria for at least one personality disorder.
On average, these 41 subjects were in their 20s and 30s and reported having problems with Internet use for about 3 years. They spent an average of 28 hours per week online for pleasure or recreation, and many experienced emotional distress, social impairment, and social, occupational, or financial difficulties.1,11
Table 1
PROPOSED DIAGNOSTIC CRITERIA FOR PROBLEMATIC INTERNET USE
| Maladaptive preoccupation with Internet use, as indicated by at least one of the following: |
|
|
| Source: Reprinted with permission from an article by Shapira et al9 that has been accepted for publication in Depression and Anxiety. © Copyright 2003 John Wiley & Sons. |
Isolation and depression. Increasing Internet use and withdrawal from family activities has been associated with increased depression and loneliness; Kraut et al15 hypothesized that the Internet use caused the depression. Pratarelli et al16 noted a maladaptive cycle in some persons; the more isolated they feel, the more they use the Internet and increase their social withdrawal.
In a survey of college students, individuals with “Internet addiction” were found to:
- have obsessive characteristics
- prefer online interactions to real-life interactions
- use the Internet “to feel better,” alleviate depression, and become sexually aroused.16
Personality traits. In another study, Orzack12 found that subjects viewed the computer as a means to satisfy, induce excitement, and reduce tension or induce relief. Six personality traits were identified as strong predictors of “Internet addiction disorder:”
- boredom
- private self-consciousness
- loneliness
- social anxiety
- shyness
- and low self-esteem.
Table 2
5 SCREENING QUESTIONS FOR PROBLEMATIC INTERNET USE
| More than intended time spent online? |
| Other responsibilities or activities neglected? |
| Unsuccessful attempts to cut down? |
| Significant relationship discord due to use? |
| Excessive thoughts or anxiety when not online? |
Diagnosing Internet overuse
Screening. During any psychiatric interview, ask patients how they spend their free time or what they most enjoy doing. If patients say they spend hours on the Internet or their use appears to usurp other activities, five questions—easily recalled by the mnemonic MOUSE—can help you screen for problematic Internet use (Table 2).
History. Typically, persons with problematic Internet use spend time in one Internet domain, such as chat rooms, interactive games, news groups, or search engines.17 Ask which application they use, how many hours they use it, how they rank the importance of various applications, and what they like about their preferred application.
To determine how the Internet may alter the patient’s moods, ask how he or she feels while online as opposed to offline. Keeping an hourly log and a “feelings diary” may help the patient sort through his or her emotions.17
Often patients use the Internet to escape from dissatisfaction or disappointment or to counteract a sense of personal inadequacy.17 They tend to take pride in their computer skills2 and incorporate them into their daily lives in many ways, allowing them to rationalize their excessive Internet use (“I’m using it for work, academics, travel, research, etc.”).
Chomorbidities. Given the high incidence of psychiatric comorbidity,1 it is important to complete a thorough psychiatric evaluation and treat any underlying illness. Whether the illness is primary or comorbid, it is likely exacerbating the symptoms of problematic Internet use.
Changing problematic behaviors
Psychotherapy. Once you find the motives and possible causes of Internet overuse, what is the best form of treatment? This question warrants further study, but cognitive-behavioral therapy (CBT) is the primary treatment at this time.
The goal of CBT is for patients to disrupt their problematic computer use and reconstruct their routines with other activities. They can:
- use external timers to keep track of time online
- set goals of brief, frequent sessions online
- carry cards listing the destructive effects of their Internet use and ranking other activities they have neglected.17
Using emotion journals or mood monitoring forms may help the patient discover which dysfunctional thoughts and feelings are triggering excessive Internet use.12 Support groups and family therapy can help repair damaged relationships and engage friends and family in the treatment plan.
Drug therapy. No studies have looked at drug therapy for problematic Internet use, beyond treating comorbid psychiatric illnesses.
Treatment declined. Mr. A declined treatment for his problematic Internet use. As in many other psychiatric illnesses, insight into impulse control disorders tends to be limited. We can address the problem directly and offer to help patients change their online behaviors, but we cannot force them into treatment if they are not endangering themselves or others.
Related resources
- Computer Addiction Services. Maressa Hecht Orzack, PhD. www.computeraddiction.com; (617) 855-2908.
- Center for Online Addiction. Kimberly S. Young, PhD. www.netaddiction.com; (877) 292-3737.
Many psychiatrists diagnose problematic Internet use with schemas based on substance use disorders and pathologic gambling. These predefined diagnoses, however, may lead to premature conclusions and prevent you from fully exploring other treatable diagnoses.
We propose a screening tool called “MOUSE” and diagnostic criteria for problematic Internet use, which we developed from research by our group and others. This article discusses the new criteria and answers three questions:
- How does problematic Internet use present?
- Is it an addiction or an impulse control disorder?
- How can we help those afflicted with this problem?
When Internet use goes over the line
Recognizing problematic Internet use is difficult because the Internet can serve as a tool in nearly every aspect of our lives—communication, shopping, business, travel, research, entertainment, and more. The evidence suggests that Internet use becomes a behavior disorder when:
- an individual loses the ability to control his or her use and begins to suffer distress and impaired daily function1
- and employment and relationships are jeopardized by the hours spent online2 (Box).
Relationships—particularly marriages but also parent-child relationships, dating relationships, and close friendships—appear to suffer the greatest harm. At least one-half of “Internet addicts” (53%) report that their Internet use has caused serious relationship problems.
School. Academic problems are common; one study showed 58% of students blamed Internet use for a drop in grades, missed classes, declining study habits, or being placed on probation.
Workplace. Many executives—55% in one study—complain that time spent on the Internet for non-business purposes reduces their employees’ effectiveness.
Health. Some users spend 40 to 80 hours per week online, and single sessions can last up to 20 hours. Lack of sleep results in fatigue, decreased exercise, and decreased immunity. Sitting in front of the computer for hours also increases the risk of carpal tunnel syndrome, eye strain, and back pain.
Other addictions. The more time spent on the Internet, the greater the user’s risk of exposure to other addictive activities, such as online gambling and sexual solicitations. This risk is particularly concerning in children and adolescents.
Source: Young KS. Innovations in Clin Pract 1999;17:19-31.
Case: Computer gamer out of control
Mr. A is 32 and in his fourth year of college. His psychiatric history includes obsessive-compulsive disorder (OCD), paraphilia not otherwise specified, and bipolar disorder, most recently depressed in partial remission. He has had only one manic episode 10 years ago and took lithium briefly. He experienced pleasure from masturbating in public, but his paraphilia did not meet criteria for voyeurism as he did not want to be seen. He engaged in this behavior from ages 16 to 18 and found it distressing.
He is taking no medications. The only clinically significant family history is his father’s apparent OCD, undiagnosed and untreated.
Mr. A’s excessive computer use started in high school, when he played computer games to the point where his grades suffered. He began using the Internet at age 28, just before starting college, and spent most of his time online playing multi-player, video/strategy games.
Mr. A underestimates the time he spends online at 24 hours per week, including 21 hours in nonessential use and 3 hours in essential use (required for job or school). His actual average is 35.9 hours per week—nearly equivalent to a full-time job. He divides his nonessential use among various online activities, mostly related to playing computer games:
- 35% in chat forums, communicating with gaming partners he has never met
- 25% in multi-player, video/strategy games
- 15% using e-mail
- and lesser times surfing the Web (5%), transferring files (5%), viewing pornography (5%), shopping (5%), listening to music (3%), and selling (2%).
He reports rising tension before logging on and relief after doing so. He admits to using the Internet for longer periods than intended and especially when emotionally stressed. He knows his behavior has hurt him academically, and he has tried unsuccessfully to cut down or stop his Internet use.
Internet overuse: An ‘addiction’?
Ivan Goldberg introduced the idea of Internet addiction in 1995 by posting factitious “diagnostic criteria” on a Web site as a joke.3 He was surprised at the overwhelming response he received from persons whose Internet use was interfering with their lives. The first case reports were soon published.4,5
Initially, excessive Internet use was called an “addiction”—implying a disorder similar to substance dependence. Recently, however, Internet overuse has come to be viewed as more closely resembling an impulse control disorder.5-8 Shapira et al studied 20 subjects with problematic Internet use, and all met DSM-IV criteria for an impulse control disorder, not otherwise specified. Three also met criteria for obsessive-compulsive disorder.1
As with other impulse control disorders (such as eating disorders and pathologic gambling), researchers have noticed increased depression associated with pathologic Internet use.8
Diagnostic criteria. Although Mr. A’s comorbid psychiatric illnesses complicate his presentation, his behavior clearly could be described as representing an impulse control disorder. His case also meets our proposed criteria for problematic Internet use (Table 1),9 which we define as:
- uncontrollable
- markedly distressing, time-consuming, or resulting in social, occupational, or financial difficulties
- and not solely present during mania or hypomania.
Teasing out comorbid disorders
As in Mr. A’s case, Internet overuse can serve as an expression of and a conduit for other psychiatric illnesses. Studies have found high rates of comorbidity with mood and anxiety disorders, social phobias, attention-deficit disorder with or without hyperactivity, paraphilias, insomnia, pathologic gambling, and substance use disorders.10-12
Although some researchers feel that the many comorbid and complicating factors cannot be teased out,13 most agree that compulsive Internet use or overuse can have adverse consequences and that more research is needed.
A predisposition? Are “Internet addicts” predisposed to or susceptible to Internet overuse? Researchers are exploring whether Internet overuse causes or is an effect of psychiatric illness.
Shapira et al1,14 found at least one psychiatric condition that predated the development of Internet overuse in 20 subjects. In a similar study of 21 subjects with excessive computer use, Black11 found:
- 33% had a mood disorder
- 38% had a substance use disorder
- 19% had an anxiety disorder
- 52% met criteria for at least one personality disorder.
On average, these 41 subjects were in their 20s and 30s and reported having problems with Internet use for about 3 years. They spent an average of 28 hours per week online for pleasure or recreation, and many experienced emotional distress, social impairment, and social, occupational, or financial difficulties.1,11
Table 1
PROPOSED DIAGNOSTIC CRITERIA FOR PROBLEMATIC INTERNET USE
| Maladaptive preoccupation with Internet use, as indicated by at least one of the following: |
|
|
| Source: Reprinted with permission from an article by Shapira et al9 that has been accepted for publication in Depression and Anxiety. © Copyright 2003 John Wiley & Sons. |
Isolation and depression. Increasing Internet use and withdrawal from family activities has been associated with increased depression and loneliness; Kraut et al15 hypothesized that the Internet use caused the depression. Pratarelli et al16 noted a maladaptive cycle in some persons; the more isolated they feel, the more they use the Internet and increase their social withdrawal.
In a survey of college students, individuals with “Internet addiction” were found to:
- have obsessive characteristics
- prefer online interactions to real-life interactions
- use the Internet “to feel better,” alleviate depression, and become sexually aroused.16
Personality traits. In another study, Orzack12 found that subjects viewed the computer as a means to satisfy, induce excitement, and reduce tension or induce relief. Six personality traits were identified as strong predictors of “Internet addiction disorder:”
- boredom
- private self-consciousness
- loneliness
- social anxiety
- shyness
- and low self-esteem.
Table 2
5 SCREENING QUESTIONS FOR PROBLEMATIC INTERNET USE
| More than intended time spent online? |
| Other responsibilities or activities neglected? |
| Unsuccessful attempts to cut down? |
| Significant relationship discord due to use? |
| Excessive thoughts or anxiety when not online? |
Diagnosing Internet overuse
Screening. During any psychiatric interview, ask patients how they spend their free time or what they most enjoy doing. If patients say they spend hours on the Internet or their use appears to usurp other activities, five questions—easily recalled by the mnemonic MOUSE—can help you screen for problematic Internet use (Table 2).
History. Typically, persons with problematic Internet use spend time in one Internet domain, such as chat rooms, interactive games, news groups, or search engines.17 Ask which application they use, how many hours they use it, how they rank the importance of various applications, and what they like about their preferred application.
To determine how the Internet may alter the patient’s moods, ask how he or she feels while online as opposed to offline. Keeping an hourly log and a “feelings diary” may help the patient sort through his or her emotions.17
Often patients use the Internet to escape from dissatisfaction or disappointment or to counteract a sense of personal inadequacy.17 They tend to take pride in their computer skills2 and incorporate them into their daily lives in many ways, allowing them to rationalize their excessive Internet use (“I’m using it for work, academics, travel, research, etc.”).
Chomorbidities. Given the high incidence of psychiatric comorbidity,1 it is important to complete a thorough psychiatric evaluation and treat any underlying illness. Whether the illness is primary or comorbid, it is likely exacerbating the symptoms of problematic Internet use.
Changing problematic behaviors
Psychotherapy. Once you find the motives and possible causes of Internet overuse, what is the best form of treatment? This question warrants further study, but cognitive-behavioral therapy (CBT) is the primary treatment at this time.
The goal of CBT is for patients to disrupt their problematic computer use and reconstruct their routines with other activities. They can:
- use external timers to keep track of time online
- set goals of brief, frequent sessions online
- carry cards listing the destructive effects of their Internet use and ranking other activities they have neglected.17
Using emotion journals or mood monitoring forms may help the patient discover which dysfunctional thoughts and feelings are triggering excessive Internet use.12 Support groups and family therapy can help repair damaged relationships and engage friends and family in the treatment plan.
Drug therapy. No studies have looked at drug therapy for problematic Internet use, beyond treating comorbid psychiatric illnesses.
Treatment declined. Mr. A declined treatment for his problematic Internet use. As in many other psychiatric illnesses, insight into impulse control disorders tends to be limited. We can address the problem directly and offer to help patients change their online behaviors, but we cannot force them into treatment if they are not endangering themselves or others.
Related resources
- Computer Addiction Services. Maressa Hecht Orzack, PhD. www.computeraddiction.com; (617) 855-2908.
- Center for Online Addiction. Kimberly S. Young, PhD. www.netaddiction.com; (877) 292-3737.
1. Shapira NA, Goldsmith TG, Keck PE, Jr, Khosla UM, McElroy SL. Psychiatric features of individuals with problematic Internet use. J Affect Disord 2000;57:267-72.
2. Beard KW, Wolf EM. Modification in the proposed diagnostic criteria for Internet addiction. Cyberpsychol Behav 2001;4:377-83.
3. Goldberg I. Internet addiction. Available at http://www.cybernothing.org/jdfalk/media-coverage/archive/msg01305.html. Accessed Feb. 26, 2003.
4. Griffiths MD. Internet addiction: an issue for clinical psychology? Clin Psychol Forum 1996;97:32-6.
5. Young KS. Psychology of computer use: XL. Addictive use of the Internet: a case that breaks the stereotype. Psychol Rep 1996;79:899-902.
6. Treuer T, Fábián Z, Füredi J. Internet addiction associated with features of impulse control disorder: is it a real psychiatric disorder? J Affect Disord 2001;66:283.-
7. Young KS. Caught in the net: how to recognize the signs of Internet addiction-and a winning strategy for recovery. New York: John Wiley & Sons, Inc. 1998;8.-
8. Young KS, Rogers RC. The relationship between depression and Internet addiction. Cyberpsychol Behav 1998;1:25-8.
9. Shapira NA, Lessig MC, Goldsmith TD, et al. Problematic Internet use: proposed classification and diagnostic criteria. Depress Anxiety (in press).
10. Griffiths MD. Internet addiction: Fact or fiction? Psychologist 1999;12:246-50.
11. Black DW, Belsare G, Schlosser S. Clinical features, psychiatric comorbidity, and health-related quality of life in persons reporting compulsive computer use behavior. J Clin Psychiatry 1999;60:839-44.
12. Orzack MH. How to recognize and treat computer.com addictions. Directions in Mental Health Counseling 1999;9:13-20.
13. Stein DJ. Internet addiction, Internet psychotherapy (letter; comment). Am J Psychiatry 1997;154(6):890.-
14. Shapira NA. Unpublished data, 2000.
15. Kraut R, Lundmark V, Patterson M, Kiesler S, Mukopadhyay T, Scherlis W. Internet paradox: A social technology that reduces social involvement and psychological wellbeing? Am Psychol 1998;53:1017-31.
16. Pratarelli ME, Browne BL. Confirmatory factor analysis of Internet use and addiction. Cyberpsychol Behav 2002;5:53-64.
17. Young KS. Internet addiction: symptoms, evaluation and treatment. Innovations in Clin Pract 1999;17:19-31.
1. Shapira NA, Goldsmith TG, Keck PE, Jr, Khosla UM, McElroy SL. Psychiatric features of individuals with problematic Internet use. J Affect Disord 2000;57:267-72.
2. Beard KW, Wolf EM. Modification in the proposed diagnostic criteria for Internet addiction. Cyberpsychol Behav 2001;4:377-83.
3. Goldberg I. Internet addiction. Available at http://www.cybernothing.org/jdfalk/media-coverage/archive/msg01305.html. Accessed Feb. 26, 2003.
4. Griffiths MD. Internet addiction: an issue for clinical psychology? Clin Psychol Forum 1996;97:32-6.
5. Young KS. Psychology of computer use: XL. Addictive use of the Internet: a case that breaks the stereotype. Psychol Rep 1996;79:899-902.
6. Treuer T, Fábián Z, Füredi J. Internet addiction associated with features of impulse control disorder: is it a real psychiatric disorder? J Affect Disord 2001;66:283.-
7. Young KS. Caught in the net: how to recognize the signs of Internet addiction-and a winning strategy for recovery. New York: John Wiley & Sons, Inc. 1998;8.-
8. Young KS, Rogers RC. The relationship between depression and Internet addiction. Cyberpsychol Behav 1998;1:25-8.
9. Shapira NA, Lessig MC, Goldsmith TD, et al. Problematic Internet use: proposed classification and diagnostic criteria. Depress Anxiety (in press).
10. Griffiths MD. Internet addiction: Fact or fiction? Psychologist 1999;12:246-50.
11. Black DW, Belsare G, Schlosser S. Clinical features, psychiatric comorbidity, and health-related quality of life in persons reporting compulsive computer use behavior. J Clin Psychiatry 1999;60:839-44.
12. Orzack MH. How to recognize and treat computer.com addictions. Directions in Mental Health Counseling 1999;9:13-20.
13. Stein DJ. Internet addiction, Internet psychotherapy (letter; comment). Am J Psychiatry 1997;154(6):890.-
14. Shapira NA. Unpublished data, 2000.
15. Kraut R, Lundmark V, Patterson M, Kiesler S, Mukopadhyay T, Scherlis W. Internet paradox: A social technology that reduces social involvement and psychological wellbeing? Am Psychol 1998;53:1017-31.
16. Pratarelli ME, Browne BL. Confirmatory factor analysis of Internet use and addiction. Cyberpsychol Behav 2002;5:53-64.
17. Young KS. Internet addiction: symptoms, evaluation and treatment. Innovations in Clin Pract 1999;17:19-31.
Atypical depression Puzzled? How to piece together symptoms and treatments
Deciding if a patient’s depressive episodes are “atypical” can be difficult because key pieces of the diagnostic puzzle are missing. Notwithstanding DSM-IV criteria, atypical depression’s definition remains unclear. This creates a therapeutic dilemma because we know that patients with atypical depression respond differently to antidepressants:
- Monoamine oxidase inhibitors (MAOIs) may be most effective, but their side effects can be troublesome.
- Tricyclics are clearly less effective than MAOIs, but the newer antidepressants’ role in treating atypical depressive symptoms has not been adequately explored.
We offer recommendations for diagnosing and treating atypical depression and address issues that may affect your clinical approach. These include possible overemphasis on mood reactivity in DSM-IV, shortcomings in studies defining the atypical depressive syndrome, and the potential role of biological markers in clarifying this challenging diagnosis.
Features of atypical depression
Atypical depression, as defined in DSM-IV,1 is characterized by mood reactivity and two or more of the following criteria:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis (heavy, leaden feeling in arms or legs)
- longstanding sensitivity to interpersonal rejection that results in significant social or occupational impairment (Table 1 ).
An estimated 16 to 23% of patients with unipolar depression present with atypical features.2 These rates are higher among patients with bipolar disorder.2,3
Distinctive features. Studies comparing atypical depression with typical or melancholic depression suggest that atypical depression may be distinct in epidemiology, family history, comorbidity, and course of illness (Table 2). Specifically, atypical depression has a higher female-to-male ratio and earlier age of onset.4 Patients with atypical depression have higher rates of comorbid panic disorder,4,5 social phobia,4,5 bipolar II disorder,5 and bulimia6 than do those with typical depression.
Family members of patients with atypical depression are more likely to have atypical features during a depressive episode than are family members of patients with melancholic depression.7 These findings suggest a genetic component to atypical depression. Atypical depressive episodes also may be more likely to become chronic.4,8
Not all patients are alike. Studies of the diagnostic stability of atypical depression over time suggest that patients exhibiting atypical features are heterogeneous.9 Some longitudinal studies report reasonable diagnostic stability, with 59% to 100% of patients with an index episode of atypical depression exhibiting atypical features 12 to 24 months later.9,10 In a follow-up study of patients in remission from an episode of atypical depression, 64% of patients suffering a relapse were again found to have atypical features.11
Table 1
MOOD EPISODES: DSM-IV CRITERIA FOR ATYPICAL FEATURES SPECIFIER
| The following criteria must be present in the last 2 weeks of the episode |
| Criterion A. Mood reactivity (ie, mood brightens in response to positive events) |
| Criterion B. Two or more of the following: Increased appetite or weight gain Hypersomnia Leaden paralysis Longstanding sensitivity to interpersonal rejection |
Although numerous studies have failed to replicate one or more of these findings,4,8 several investigators have concluded that atypical depression is a distinct and valid sub-type of major depression.4,7,8
Antidepressant dilemmas
Unlike typical or melancholic depression, atypical depression responds more robustly to MAOIs than to tricyclic antidepressants (TCAs).12 MAOIs are roughly twice as effective as TCAs (response rate 72% vs. 44%, respectively), according to a meta-analysis of six studies comparing MAOIs and TCAs in patients with atypical depression.13
Clinicians rarely use MAOIs as first-line antidepressants, however, because of side effects and potential dietary and drug interactions. A depressed patient is thus unlikely to receive MAOIs unless the clinician strongly suspects that the presentation is atypical.
SSRIs. Few studies have evaluated how patients with atypical depression respond to newer antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs). This lack of evidence creates a dilemma when treating atypical depression, as SSRIs are widely used in depressed patients, including those with atypical features.
One study found fluoxetine and phenelzine comparably effective in atypical depression,14 while another found sertraline works as well as moclobe-mide.15 However, the fluoxetine study was limited by a relatively small sample size (n=42), and both studies lacked placebo controls.
Some studies have suggested that SSRIs are less effective than MAOIs16 or as effective as TCAs in depressed patients with atypical features.17,18 However, one of these trials was limited by a small sample size (n=28),18 and only one was placebo-controlled.17
Bupropion. Studies of other antidepressants in atypical depression also are limited. In two separate trials, depressed patients with atypical features showed a greater response to bupropion than did depressed patients with typical features.19,20
Bupropion—a combined dopaminergic-noradrenergic antidepressant—appears to have stimulating properties that may help patients with hypersomnia and hyperphagia. Like MAOIs, bupropion also appears to have a greater effect on dopaminergic systems than either TCAs or SSRIs.
Recommendation. The most prudent approach appears to be using SSRIs or bupropion as first-line treatment for atypical depression and reserving MAOIs for patients who do not respond.
Attempts to define atypical depression
Although atypical depression responds differently to MAOIs than to TCAs, it is unclear which patients will respond preferentially to MAOIs. Early attempts to classify this subgroup recognized that these patients display symptom clusters, including:
- anxious depression (prominent anxiety symptoms)
- anergic depression (prominent fatigue and/or psychomotor retardation)
- and depression with reversed vegetative symptoms (hypersomnia and increased weight/appetite).7,21
Researchers have focused on patients with different combinations of these symptom profiles when defining the atypical depressive syndrome. Some have defined atypical depression as anxious temperament and reactive mood; others, as depression with reversed vegetative symptoms and severe fatigue; still others employ aspects of both profiles, as does DSM-IV.21 As a result of this confusion, investigators have demonstrated the preferential response to MAOIs in groups that exhibit different “atypical” symptoms.
Mood reactivity. The importance of mood reactivity in the diagnosis of atypical depression has been debated. DSM-IV requires mood reactivity for the diagnosis, perhaps to clearly differentiate melancholia from atypical depression.7 Yet some studies have demonstrated the preferential MAOI response in patients without this symptom.
Table 2
HOW ATYPICAL DEPRESSION COMPARES WITH MELANCHOLIC OR ‘TYPICAL’ DEPRESSION
| Feature | Atypical depression | Melancholic (MEL)/typical (TYP) depression |
|---|---|---|
| Symptom | ||
| Sleep | Increased | Decreased |
| Appetite | Increased | Decreased |
| Age of onset | Late teens to early 20s | Mid to late 30s |
| Female:male ratio | > 2:1 | Between 1:1 and 2:1 |
| Frequency of bipolar II disorder | Increased compared with MEL/TYP | |
| Duration of episodes | Increased compared with MEL/TYP | |
| Biology | ||
| HPA axis activity | Low to normal | High |
| Comorbidity | ||
| Panic disorder, social phobia, bulimia | Frequency increased compared with MEL/TYP | |
The Columbia group, from whose work the DSM-IV definition was adopted, performed several convincing studies showing clear superiority of MAOIs in patients who had reactive mood and displayed at least two additional atypical features, such as reversed vegetative symptoms and anergia.22 Patients with reactive mood and only one additional atypical symptom (classified as “probable” atypical depression) also displayed the preferential response to MAOIs, whereas patients who displayed mood reactivity alone did not.12
Thase et al,23 however, reported that reversed vegetative symptoms were more common with nonreactive mood (48%) than with reactive mood (16%) in patients with highly recurrent depression. Moreover, patients who displayed reversed vegetative symptoms without mood reactivity showed the same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Table 3
HOW ANTIDEPRESSANTS COMPARE IN CLINICAL TRIALS OF ATYPICAL DEPRESSION
| MAOIs | 8 controlled trials found MAOI > placebo 6 controlled trials found MAOI > TCA |
| TCAs | 6 controlled trials found MAOI > TCA |
| SSRIs | 2 controlled trials found SSRI = MAOI 1 trial found MAOI > SSRI 2 trials found SSRI = TCA |
| Bupropion | 1 open-label trial found bupropion more effective in atypical depression than in typical depression 1 open-label trial found bupropion effective in depression with hypersomnia 1 retrospective study found bupropion > fluoxetine in atypical depression |
| > more effective than | |
| = as effective as | |
More evidence suggests that mood reactivity should not be given the hierarchical importance it holds in the DSM-IV definition of atypical depression. In studies using latent class and cluster analyses, mood reactivity did not correlate with any other atypical feature,4,21 whereas hyperphagia, hypersomnia, leaden paralysis, and rejection sensitivity appear to be associated with one another.
Recommendation. Mood reactivity’s uncertain status in atypical depression’s definition makes it difficult to predict which patients may respond preferentially to MAOIs, as many patients present with other atypical features and nonreactive mood. Most recently, it has been suggested that atypical depression’s diagnostic criteria should be modified so that mood reactivity is not required but is one of five atypical features, of which three must be present for the diagnosis.24
Biological markers of depression
Atypical depression’s definition might be clarified if specific depressive symptoms could be linked to any biological markers. One proposed marker is decreased HPA axis activity, possibly caused by a central deficiency of corticotropin-releasing hormone (CRH),25 a potent HPA axis stimulator.
- HPA axis hyperactivity—presumably caused by increased CRH activity in the central nervous system—has been linked to melancholic depressive symptoms—particularly insomnia and reduced appetite.26
- Normal or diminished HPA axis activity—suggested by normal cortisol levels, low levels of CRH in cerebrospinal fluid, and increased frequency of dexamethasone suppression—has been associated with some atypical depressive features—specifically reversed vegetative symptoms.27-29
However, no studies have examined whether low HPA axis activity is associated with other atypical symptoms listed in DSM-IV. Research is needed to determine whether HPA axis hypoactivity is associated only with reversed vegetative symptoms or with atypical depression per se.
Obesity and eating disorders. Depressed patients who are obese or present with eating disorders may overlap with the atypical subtype and may respond better to some drug interventions than to others. Evidence suggests that depression—particularly the atypical subtype—is associated with increased rates of obesity8,29 and eating disorders.8,30
In our clinical experience, the combination of venlafaxine and bupropion can be effective for both depression and excessive eating in these patients, many of whom also exhibit other atypical features. A possible explanation is that the combined pharmacologic effect of venlafaxine and bupropion resembles that of the MAOIs (increased synaptic availability of serotonin, norepinephrine, and dopamine) without many MAOI side effects, such as weight gain.
We have, however, also observed treatment-emergent hypomania when using this drug combination, which is consistent with:
- the idea that mood reactivity and rejection sensitivity may be markers for bipolar disorder
- the often-reported high rate of bipolar II disorder among patients with atypical depression.5
In obese patients with bipolar II disorder, we have found that adding topiramate to mood stabilizer therapy can help treat both mood instability and overeating.31,32 same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Related resources
- Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs. low CRH/NE states. Mol Psychiatry 2002;7(3):254-75.
- Nierenberg AA, Alpert JE, Pava J, Rosenbaum JF, Fava M. Course and treatment of atypical depression. J Clin Psychiatry 1998;59(suppl 18):5-9.
Drug brand names
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Moclobemide • Manerix
- Phenelzine • Nardil
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor
Disclosure
Dr. Nelson receives grant/research support from Eli Lilly & Co. and Wyeth Pharmaceuticals and is on the speakers bureau of Wyeth Pharmaceuticals.
Dr. McElroy is a consultant or scientific advisor to Abbott Laboratories, Bristol-Myers Squibb Co., Elan Corp., GlaxoSmithKline, Janssen Pharmaceutica, Eli Lilly & Co., Novartis Pharmaceuticals Corp., Ortho-McNeil Pharmaceutical, UCB Pharma, and Wyeth Pharmaceuticals. She receives research support from Forest Laboratories, GlaxoSmithKline, Elan Corp., Eli Lilly & Co., Merck & Co., Ortho-McNeil Pharmaceutical, Pfizer Inc., Sanofi-Synthelabo, and UCB Pharma.
1. American Psychiatric Association. Diagnostic and statistical manual of mentab disorders (4th ed). Washington DC: American Psychiatric Association, 2000.
2. Benazzi F. Prevalence and clinical features of atypical depression in depressed outpatients: a 467-case study. Psychiatry Res 1999;86(3):259-65.
3. Benazzi F. Is atypical depression a moderate severity depression? A 536-case study. J Psychiatry Neurosci 1999;24(3):244-7.
4. Posternak MA, Zimmerman M. Partial validation of the atypical features subtype of major depressive disorder. Arch Gen Psychiatry 2002;59(1):70-6.
5. Perugi G, Akiskal HS, Lattanzi L, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry 1998;39(2):63-71.
6. Levitan RD, Kaplan AS, Brown GM, et al. Low plasma cortisol in bulimia nervosa patients with reversed neurovegetative symptoms of depression. Biol Psychiatry 1997;41(3):366-8.
7. Stewart JW, McGrath PJ, Rabkin JG, Quitkin FM. Atypical depression. A valid clinical entity? Psychiatr Clin North Am 1993;16(3):479-95.
8. Kendler KS, Eaves LJ, Walters EE, Neale MC, Heath AC, Kessler RC. The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Arch Gen Psychiatry 1996;53(5):391-9.
9. Ebert D, Barocka A. The early course of atypical depression. Eur Arch Psychiatry Clin Neurosci 1991;241(2):131-2.
10. Zubieta JK, Pande AC, Demitrack MA. Two-year follow-up of atypical depression. J Psychiatr Res 1999;33(1):23-9.
11. Nierenberg AA, Pava JA, Clancy K, Rosenbaum JF, Fava M. Are neurovegetative symptoms stable in relapsing or recurrent atypical depressive episodes? Biol Psychiatry 1996;40(8):691-6.
12. Quitkin FM, McGrath PJ, Stewart JW, et al. Phenelzine and imipramine in mood reactive depressives. Further delineation of the syndrome of atypical depression. Arch Gen Psychiatry 1989;46(9):787-93.
13. Pande AC, Birkett M, Fechner-Bates S, Haskett RF, Greden JF. Fluoxetine versus phenelzine in atypical depression. Biol Psychiatry 1996;40(10):1017-20.
14. Sogaard J, Lane R, Latimer P, et al. A 12-week study comparing moclobemide and sertraline in the treatment of outpatients with atypical depression. J Psychopharmacol 1999;13(4):406-14.
15. Lonnqvist J, Sihvo S, Syvalahti E, Kiviruusu O. Moclobemide and fluoxetine in atypical depression: a double-blind trial. J Affect Disord 1994;32(3):169-77.
16. McGrath PJ, Stewart JW, Janal MN, Petkova E, Quitkin FM, Klein DF. A placebo-controlled study of fluoxetine versus imipramine in the acute treatment of atypical depression. Am J Psychiatry 2000;157(3):344-50.
17. Stratta P, Bolino F, Cupillari M, Casacchia M. A double-blind parallel study comparing fluoxetine with imipramine in the treatment of atypical depression. Int Clin Psychopharmacol 1991;6(3):193-6.
18. Goodnick PJ, Dominguez RA, DeVane CL, Bowden CL. Bupropion slow-release response in depression: diagnosis and biochemistry. Biol Psychiatry 1998;44(7):629-32.
19. Goodnick PJ, Extein I. Bupropion and fluoxetine in depressive subtypes. Ann Clin Psychiatry 1989;1:119-22.
20. Rye DB, Dihenia B, Bliwise DL. Reversal of atypical depression, sleepiness, and REM-sleep propensity in narcolepsy with bupropion. Depress Anxiety 1998;7(2):92-5.
21. Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
22. Liebowitz MR, Quitkin FM, Stewart JW, et al. Phenelzine v imipramine in atypical depression. A preliminary report. Arch Gen Psychiatry 1984;41(7):669-77.
23. Thase ME, Carpenter L, Kupfer DJ, Frank E. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacol Bull 1991;27(1):17-22.
24. Angst J, Gamma A, Sellaro R, Zhang H, Merikangas K. Toward validation of atypical depression in the community: results of the Zurich cohort study. J Affect Disord 2002;72(2):125-38.
25. Gold PW, Chrousos GP. The endocrinology of melancholic and atypical depression: relation to neurocircuitry and somatic consequences. Proc Assoc Am Physicians 1999;111(1):22-34.
26. Garvey MJ, Schaffer C, Schaffer L, Perry PJ. Is DST status associated with depression characteristics? J Affect Disord 1989;16(2-3):159-65.
27. Geracioti TD, Jr, Loosen PT, Orth DN. Low cerebrospinal fluid corticotropin-releasing hormone concentrations in eucortisolemic depression. Biol Psychiatry 1997;42(3):165-74.
28. Casper RC, Kocsis J, Dysken M, et al. Cortisol measures in primary major depressive disorder with hypersomnia or appetite increase. J Affect Disord 1988;15(2):131-40.
29. Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry 1998;155(10):1398-406.
30. Levitan RD, Lesage A, Parikh SV, Goering P, Kennedy SH. Reversed neurovegetative symptoms of depression: a community study of Ontario. Am J Psychiatry 1997;154(7):934-40.
31. McElroy SL, Suppes T, Keck PE, Jr, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry 2000;47(12):1025-33.
32. Shapira NA, Goldsmith TD, McElroy SL. Treatment of binge-eating disorder with topiramate: a clinical case series. J Clin Psychiatry 2000;61(5):368-72.
Deciding if a patient’s depressive episodes are “atypical” can be difficult because key pieces of the diagnostic puzzle are missing. Notwithstanding DSM-IV criteria, atypical depression’s definition remains unclear. This creates a therapeutic dilemma because we know that patients with atypical depression respond differently to antidepressants:
- Monoamine oxidase inhibitors (MAOIs) may be most effective, but their side effects can be troublesome.
- Tricyclics are clearly less effective than MAOIs, but the newer antidepressants’ role in treating atypical depressive symptoms has not been adequately explored.
We offer recommendations for diagnosing and treating atypical depression and address issues that may affect your clinical approach. These include possible overemphasis on mood reactivity in DSM-IV, shortcomings in studies defining the atypical depressive syndrome, and the potential role of biological markers in clarifying this challenging diagnosis.
Features of atypical depression
Atypical depression, as defined in DSM-IV,1 is characterized by mood reactivity and two or more of the following criteria:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis (heavy, leaden feeling in arms or legs)
- longstanding sensitivity to interpersonal rejection that results in significant social or occupational impairment (Table 1 ).
An estimated 16 to 23% of patients with unipolar depression present with atypical features.2 These rates are higher among patients with bipolar disorder.2,3
Distinctive features. Studies comparing atypical depression with typical or melancholic depression suggest that atypical depression may be distinct in epidemiology, family history, comorbidity, and course of illness (Table 2). Specifically, atypical depression has a higher female-to-male ratio and earlier age of onset.4 Patients with atypical depression have higher rates of comorbid panic disorder,4,5 social phobia,4,5 bipolar II disorder,5 and bulimia6 than do those with typical depression.
Family members of patients with atypical depression are more likely to have atypical features during a depressive episode than are family members of patients with melancholic depression.7 These findings suggest a genetic component to atypical depression. Atypical depressive episodes also may be more likely to become chronic.4,8
Not all patients are alike. Studies of the diagnostic stability of atypical depression over time suggest that patients exhibiting atypical features are heterogeneous.9 Some longitudinal studies report reasonable diagnostic stability, with 59% to 100% of patients with an index episode of atypical depression exhibiting atypical features 12 to 24 months later.9,10 In a follow-up study of patients in remission from an episode of atypical depression, 64% of patients suffering a relapse were again found to have atypical features.11
Table 1
MOOD EPISODES: DSM-IV CRITERIA FOR ATYPICAL FEATURES SPECIFIER
| The following criteria must be present in the last 2 weeks of the episode |
| Criterion A. Mood reactivity (ie, mood brightens in response to positive events) |
| Criterion B. Two or more of the following: Increased appetite or weight gain Hypersomnia Leaden paralysis Longstanding sensitivity to interpersonal rejection |
Although numerous studies have failed to replicate one or more of these findings,4,8 several investigators have concluded that atypical depression is a distinct and valid sub-type of major depression.4,7,8
Antidepressant dilemmas
Unlike typical or melancholic depression, atypical depression responds more robustly to MAOIs than to tricyclic antidepressants (TCAs).12 MAOIs are roughly twice as effective as TCAs (response rate 72% vs. 44%, respectively), according to a meta-analysis of six studies comparing MAOIs and TCAs in patients with atypical depression.13
Clinicians rarely use MAOIs as first-line antidepressants, however, because of side effects and potential dietary and drug interactions. A depressed patient is thus unlikely to receive MAOIs unless the clinician strongly suspects that the presentation is atypical.
SSRIs. Few studies have evaluated how patients with atypical depression respond to newer antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs). This lack of evidence creates a dilemma when treating atypical depression, as SSRIs are widely used in depressed patients, including those with atypical features.
One study found fluoxetine and phenelzine comparably effective in atypical depression,14 while another found sertraline works as well as moclobe-mide.15 However, the fluoxetine study was limited by a relatively small sample size (n=42), and both studies lacked placebo controls.
Some studies have suggested that SSRIs are less effective than MAOIs16 or as effective as TCAs in depressed patients with atypical features.17,18 However, one of these trials was limited by a small sample size (n=28),18 and only one was placebo-controlled.17
Bupropion. Studies of other antidepressants in atypical depression also are limited. In two separate trials, depressed patients with atypical features showed a greater response to bupropion than did depressed patients with typical features.19,20
Bupropion—a combined dopaminergic-noradrenergic antidepressant—appears to have stimulating properties that may help patients with hypersomnia and hyperphagia. Like MAOIs, bupropion also appears to have a greater effect on dopaminergic systems than either TCAs or SSRIs.
Recommendation. The most prudent approach appears to be using SSRIs or bupropion as first-line treatment for atypical depression and reserving MAOIs for patients who do not respond.
Attempts to define atypical depression
Although atypical depression responds differently to MAOIs than to TCAs, it is unclear which patients will respond preferentially to MAOIs. Early attempts to classify this subgroup recognized that these patients display symptom clusters, including:
- anxious depression (prominent anxiety symptoms)
- anergic depression (prominent fatigue and/or psychomotor retardation)
- and depression with reversed vegetative symptoms (hypersomnia and increased weight/appetite).7,21
Researchers have focused on patients with different combinations of these symptom profiles when defining the atypical depressive syndrome. Some have defined atypical depression as anxious temperament and reactive mood; others, as depression with reversed vegetative symptoms and severe fatigue; still others employ aspects of both profiles, as does DSM-IV.21 As a result of this confusion, investigators have demonstrated the preferential response to MAOIs in groups that exhibit different “atypical” symptoms.
Mood reactivity. The importance of mood reactivity in the diagnosis of atypical depression has been debated. DSM-IV requires mood reactivity for the diagnosis, perhaps to clearly differentiate melancholia from atypical depression.7 Yet some studies have demonstrated the preferential MAOI response in patients without this symptom.
Table 2
HOW ATYPICAL DEPRESSION COMPARES WITH MELANCHOLIC OR ‘TYPICAL’ DEPRESSION
| Feature | Atypical depression | Melancholic (MEL)/typical (TYP) depression |
|---|---|---|
| Symptom | ||
| Sleep | Increased | Decreased |
| Appetite | Increased | Decreased |
| Age of onset | Late teens to early 20s | Mid to late 30s |
| Female:male ratio | > 2:1 | Between 1:1 and 2:1 |
| Frequency of bipolar II disorder | Increased compared with MEL/TYP | |
| Duration of episodes | Increased compared with MEL/TYP | |
| Biology | ||
| HPA axis activity | Low to normal | High |
| Comorbidity | ||
| Panic disorder, social phobia, bulimia | Frequency increased compared with MEL/TYP | |
The Columbia group, from whose work the DSM-IV definition was adopted, performed several convincing studies showing clear superiority of MAOIs in patients who had reactive mood and displayed at least two additional atypical features, such as reversed vegetative symptoms and anergia.22 Patients with reactive mood and only one additional atypical symptom (classified as “probable” atypical depression) also displayed the preferential response to MAOIs, whereas patients who displayed mood reactivity alone did not.12
Thase et al,23 however, reported that reversed vegetative symptoms were more common with nonreactive mood (48%) than with reactive mood (16%) in patients with highly recurrent depression. Moreover, patients who displayed reversed vegetative symptoms without mood reactivity showed the same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Table 3
HOW ANTIDEPRESSANTS COMPARE IN CLINICAL TRIALS OF ATYPICAL DEPRESSION
| MAOIs | 8 controlled trials found MAOI > placebo 6 controlled trials found MAOI > TCA |
| TCAs | 6 controlled trials found MAOI > TCA |
| SSRIs | 2 controlled trials found SSRI = MAOI 1 trial found MAOI > SSRI 2 trials found SSRI = TCA |
| Bupropion | 1 open-label trial found bupropion more effective in atypical depression than in typical depression 1 open-label trial found bupropion effective in depression with hypersomnia 1 retrospective study found bupropion > fluoxetine in atypical depression |
| > more effective than | |
| = as effective as | |
More evidence suggests that mood reactivity should not be given the hierarchical importance it holds in the DSM-IV definition of atypical depression. In studies using latent class and cluster analyses, mood reactivity did not correlate with any other atypical feature,4,21 whereas hyperphagia, hypersomnia, leaden paralysis, and rejection sensitivity appear to be associated with one another.
Recommendation. Mood reactivity’s uncertain status in atypical depression’s definition makes it difficult to predict which patients may respond preferentially to MAOIs, as many patients present with other atypical features and nonreactive mood. Most recently, it has been suggested that atypical depression’s diagnostic criteria should be modified so that mood reactivity is not required but is one of five atypical features, of which three must be present for the diagnosis.24
Biological markers of depression
Atypical depression’s definition might be clarified if specific depressive symptoms could be linked to any biological markers. One proposed marker is decreased HPA axis activity, possibly caused by a central deficiency of corticotropin-releasing hormone (CRH),25 a potent HPA axis stimulator.
- HPA axis hyperactivity—presumably caused by increased CRH activity in the central nervous system—has been linked to melancholic depressive symptoms—particularly insomnia and reduced appetite.26
- Normal or diminished HPA axis activity—suggested by normal cortisol levels, low levels of CRH in cerebrospinal fluid, and increased frequency of dexamethasone suppression—has been associated with some atypical depressive features—specifically reversed vegetative symptoms.27-29
However, no studies have examined whether low HPA axis activity is associated with other atypical symptoms listed in DSM-IV. Research is needed to determine whether HPA axis hypoactivity is associated only with reversed vegetative symptoms or with atypical depression per se.
Obesity and eating disorders. Depressed patients who are obese or present with eating disorders may overlap with the atypical subtype and may respond better to some drug interventions than to others. Evidence suggests that depression—particularly the atypical subtype—is associated with increased rates of obesity8,29 and eating disorders.8,30
In our clinical experience, the combination of venlafaxine and bupropion can be effective for both depression and excessive eating in these patients, many of whom also exhibit other atypical features. A possible explanation is that the combined pharmacologic effect of venlafaxine and bupropion resembles that of the MAOIs (increased synaptic availability of serotonin, norepinephrine, and dopamine) without many MAOI side effects, such as weight gain.
We have, however, also observed treatment-emergent hypomania when using this drug combination, which is consistent with:
- the idea that mood reactivity and rejection sensitivity may be markers for bipolar disorder
- the often-reported high rate of bipolar II disorder among patients with atypical depression.5
In obese patients with bipolar II disorder, we have found that adding topiramate to mood stabilizer therapy can help treat both mood instability and overeating.31,32 same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Related resources
- Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs. low CRH/NE states. Mol Psychiatry 2002;7(3):254-75.
- Nierenberg AA, Alpert JE, Pava J, Rosenbaum JF, Fava M. Course and treatment of atypical depression. J Clin Psychiatry 1998;59(suppl 18):5-9.
Drug brand names
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Moclobemide • Manerix
- Phenelzine • Nardil
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor
Disclosure
Dr. Nelson receives grant/research support from Eli Lilly & Co. and Wyeth Pharmaceuticals and is on the speakers bureau of Wyeth Pharmaceuticals.
Dr. McElroy is a consultant or scientific advisor to Abbott Laboratories, Bristol-Myers Squibb Co., Elan Corp., GlaxoSmithKline, Janssen Pharmaceutica, Eli Lilly & Co., Novartis Pharmaceuticals Corp., Ortho-McNeil Pharmaceutical, UCB Pharma, and Wyeth Pharmaceuticals. She receives research support from Forest Laboratories, GlaxoSmithKline, Elan Corp., Eli Lilly & Co., Merck & Co., Ortho-McNeil Pharmaceutical, Pfizer Inc., Sanofi-Synthelabo, and UCB Pharma.
Deciding if a patient’s depressive episodes are “atypical” can be difficult because key pieces of the diagnostic puzzle are missing. Notwithstanding DSM-IV criteria, atypical depression’s definition remains unclear. This creates a therapeutic dilemma because we know that patients with atypical depression respond differently to antidepressants:
- Monoamine oxidase inhibitors (MAOIs) may be most effective, but their side effects can be troublesome.
- Tricyclics are clearly less effective than MAOIs, but the newer antidepressants’ role in treating atypical depressive symptoms has not been adequately explored.
We offer recommendations for diagnosing and treating atypical depression and address issues that may affect your clinical approach. These include possible overemphasis on mood reactivity in DSM-IV, shortcomings in studies defining the atypical depressive syndrome, and the potential role of biological markers in clarifying this challenging diagnosis.
Features of atypical depression
Atypical depression, as defined in DSM-IV,1 is characterized by mood reactivity and two or more of the following criteria:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis (heavy, leaden feeling in arms or legs)
- longstanding sensitivity to interpersonal rejection that results in significant social or occupational impairment (Table 1 ).
An estimated 16 to 23% of patients with unipolar depression present with atypical features.2 These rates are higher among patients with bipolar disorder.2,3
Distinctive features. Studies comparing atypical depression with typical or melancholic depression suggest that atypical depression may be distinct in epidemiology, family history, comorbidity, and course of illness (Table 2). Specifically, atypical depression has a higher female-to-male ratio and earlier age of onset.4 Patients with atypical depression have higher rates of comorbid panic disorder,4,5 social phobia,4,5 bipolar II disorder,5 and bulimia6 than do those with typical depression.
Family members of patients with atypical depression are more likely to have atypical features during a depressive episode than are family members of patients with melancholic depression.7 These findings suggest a genetic component to atypical depression. Atypical depressive episodes also may be more likely to become chronic.4,8
Not all patients are alike. Studies of the diagnostic stability of atypical depression over time suggest that patients exhibiting atypical features are heterogeneous.9 Some longitudinal studies report reasonable diagnostic stability, with 59% to 100% of patients with an index episode of atypical depression exhibiting atypical features 12 to 24 months later.9,10 In a follow-up study of patients in remission from an episode of atypical depression, 64% of patients suffering a relapse were again found to have atypical features.11
Table 1
MOOD EPISODES: DSM-IV CRITERIA FOR ATYPICAL FEATURES SPECIFIER
| The following criteria must be present in the last 2 weeks of the episode |
| Criterion A. Mood reactivity (ie, mood brightens in response to positive events) |
| Criterion B. Two or more of the following: Increased appetite or weight gain Hypersomnia Leaden paralysis Longstanding sensitivity to interpersonal rejection |
Although numerous studies have failed to replicate one or more of these findings,4,8 several investigators have concluded that atypical depression is a distinct and valid sub-type of major depression.4,7,8
Antidepressant dilemmas
Unlike typical or melancholic depression, atypical depression responds more robustly to MAOIs than to tricyclic antidepressants (TCAs).12 MAOIs are roughly twice as effective as TCAs (response rate 72% vs. 44%, respectively), according to a meta-analysis of six studies comparing MAOIs and TCAs in patients with atypical depression.13
Clinicians rarely use MAOIs as first-line antidepressants, however, because of side effects and potential dietary and drug interactions. A depressed patient is thus unlikely to receive MAOIs unless the clinician strongly suspects that the presentation is atypical.
SSRIs. Few studies have evaluated how patients with atypical depression respond to newer antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs). This lack of evidence creates a dilemma when treating atypical depression, as SSRIs are widely used in depressed patients, including those with atypical features.
One study found fluoxetine and phenelzine comparably effective in atypical depression,14 while another found sertraline works as well as moclobe-mide.15 However, the fluoxetine study was limited by a relatively small sample size (n=42), and both studies lacked placebo controls.
Some studies have suggested that SSRIs are less effective than MAOIs16 or as effective as TCAs in depressed patients with atypical features.17,18 However, one of these trials was limited by a small sample size (n=28),18 and only one was placebo-controlled.17
Bupropion. Studies of other antidepressants in atypical depression also are limited. In two separate trials, depressed patients with atypical features showed a greater response to bupropion than did depressed patients with typical features.19,20
Bupropion—a combined dopaminergic-noradrenergic antidepressant—appears to have stimulating properties that may help patients with hypersomnia and hyperphagia. Like MAOIs, bupropion also appears to have a greater effect on dopaminergic systems than either TCAs or SSRIs.
Recommendation. The most prudent approach appears to be using SSRIs or bupropion as first-line treatment for atypical depression and reserving MAOIs for patients who do not respond.
Attempts to define atypical depression
Although atypical depression responds differently to MAOIs than to TCAs, it is unclear which patients will respond preferentially to MAOIs. Early attempts to classify this subgroup recognized that these patients display symptom clusters, including:
- anxious depression (prominent anxiety symptoms)
- anergic depression (prominent fatigue and/or psychomotor retardation)
- and depression with reversed vegetative symptoms (hypersomnia and increased weight/appetite).7,21
Researchers have focused on patients with different combinations of these symptom profiles when defining the atypical depressive syndrome. Some have defined atypical depression as anxious temperament and reactive mood; others, as depression with reversed vegetative symptoms and severe fatigue; still others employ aspects of both profiles, as does DSM-IV.21 As a result of this confusion, investigators have demonstrated the preferential response to MAOIs in groups that exhibit different “atypical” symptoms.
Mood reactivity. The importance of mood reactivity in the diagnosis of atypical depression has been debated. DSM-IV requires mood reactivity for the diagnosis, perhaps to clearly differentiate melancholia from atypical depression.7 Yet some studies have demonstrated the preferential MAOI response in patients without this symptom.
Table 2
HOW ATYPICAL DEPRESSION COMPARES WITH MELANCHOLIC OR ‘TYPICAL’ DEPRESSION
| Feature | Atypical depression | Melancholic (MEL)/typical (TYP) depression |
|---|---|---|
| Symptom | ||
| Sleep | Increased | Decreased |
| Appetite | Increased | Decreased |
| Age of onset | Late teens to early 20s | Mid to late 30s |
| Female:male ratio | > 2:1 | Between 1:1 and 2:1 |
| Frequency of bipolar II disorder | Increased compared with MEL/TYP | |
| Duration of episodes | Increased compared with MEL/TYP | |
| Biology | ||
| HPA axis activity | Low to normal | High |
| Comorbidity | ||
| Panic disorder, social phobia, bulimia | Frequency increased compared with MEL/TYP | |
The Columbia group, from whose work the DSM-IV definition was adopted, performed several convincing studies showing clear superiority of MAOIs in patients who had reactive mood and displayed at least two additional atypical features, such as reversed vegetative symptoms and anergia.22 Patients with reactive mood and only one additional atypical symptom (classified as “probable” atypical depression) also displayed the preferential response to MAOIs, whereas patients who displayed mood reactivity alone did not.12
Thase et al,23 however, reported that reversed vegetative symptoms were more common with nonreactive mood (48%) than with reactive mood (16%) in patients with highly recurrent depression. Moreover, patients who displayed reversed vegetative symptoms without mood reactivity showed the same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Table 3
HOW ANTIDEPRESSANTS COMPARE IN CLINICAL TRIALS OF ATYPICAL DEPRESSION
| MAOIs | 8 controlled trials found MAOI > placebo 6 controlled trials found MAOI > TCA |
| TCAs | 6 controlled trials found MAOI > TCA |
| SSRIs | 2 controlled trials found SSRI = MAOI 1 trial found MAOI > SSRI 2 trials found SSRI = TCA |
| Bupropion | 1 open-label trial found bupropion more effective in atypical depression than in typical depression 1 open-label trial found bupropion effective in depression with hypersomnia 1 retrospective study found bupropion > fluoxetine in atypical depression |
| > more effective than | |
| = as effective as | |
More evidence suggests that mood reactivity should not be given the hierarchical importance it holds in the DSM-IV definition of atypical depression. In studies using latent class and cluster analyses, mood reactivity did not correlate with any other atypical feature,4,21 whereas hyperphagia, hypersomnia, leaden paralysis, and rejection sensitivity appear to be associated with one another.
Recommendation. Mood reactivity’s uncertain status in atypical depression’s definition makes it difficult to predict which patients may respond preferentially to MAOIs, as many patients present with other atypical features and nonreactive mood. Most recently, it has been suggested that atypical depression’s diagnostic criteria should be modified so that mood reactivity is not required but is one of five atypical features, of which three must be present for the diagnosis.24
Biological markers of depression
Atypical depression’s definition might be clarified if specific depressive symptoms could be linked to any biological markers. One proposed marker is decreased HPA axis activity, possibly caused by a central deficiency of corticotropin-releasing hormone (CRH),25 a potent HPA axis stimulator.
- HPA axis hyperactivity—presumably caused by increased CRH activity in the central nervous system—has been linked to melancholic depressive symptoms—particularly insomnia and reduced appetite.26
- Normal or diminished HPA axis activity—suggested by normal cortisol levels, low levels of CRH in cerebrospinal fluid, and increased frequency of dexamethasone suppression—has been associated with some atypical depressive features—specifically reversed vegetative symptoms.27-29
However, no studies have examined whether low HPA axis activity is associated with other atypical symptoms listed in DSM-IV. Research is needed to determine whether HPA axis hypoactivity is associated only with reversed vegetative symptoms or with atypical depression per se.
Obesity and eating disorders. Depressed patients who are obese or present with eating disorders may overlap with the atypical subtype and may respond better to some drug interventions than to others. Evidence suggests that depression—particularly the atypical subtype—is associated with increased rates of obesity8,29 and eating disorders.8,30
In our clinical experience, the combination of venlafaxine and bupropion can be effective for both depression and excessive eating in these patients, many of whom also exhibit other atypical features. A possible explanation is that the combined pharmacologic effect of venlafaxine and bupropion resembles that of the MAOIs (increased synaptic availability of serotonin, norepinephrine, and dopamine) without many MAOI side effects, such as weight gain.
We have, however, also observed treatment-emergent hypomania when using this drug combination, which is consistent with:
- the idea that mood reactivity and rejection sensitivity may be markers for bipolar disorder
- the often-reported high rate of bipolar II disorder among patients with atypical depression.5
In obese patients with bipolar II disorder, we have found that adding topiramate to mood stabilizer therapy can help treat both mood instability and overeating.31,32 same preferential response to MAOIs as the mood-reactive group. Patients with typical vegetative symptoms did not show this differential response.
Related resources
- Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs. low CRH/NE states. Mol Psychiatry 2002;7(3):254-75.
- Nierenberg AA, Alpert JE, Pava J, Rosenbaum JF, Fava M. Course and treatment of atypical depression. J Clin Psychiatry 1998;59(suppl 18):5-9.
Drug brand names
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Moclobemide • Manerix
- Phenelzine • Nardil
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor
Disclosure
Dr. Nelson receives grant/research support from Eli Lilly & Co. and Wyeth Pharmaceuticals and is on the speakers bureau of Wyeth Pharmaceuticals.
Dr. McElroy is a consultant or scientific advisor to Abbott Laboratories, Bristol-Myers Squibb Co., Elan Corp., GlaxoSmithKline, Janssen Pharmaceutica, Eli Lilly & Co., Novartis Pharmaceuticals Corp., Ortho-McNeil Pharmaceutical, UCB Pharma, and Wyeth Pharmaceuticals. She receives research support from Forest Laboratories, GlaxoSmithKline, Elan Corp., Eli Lilly & Co., Merck & Co., Ortho-McNeil Pharmaceutical, Pfizer Inc., Sanofi-Synthelabo, and UCB Pharma.
1. American Psychiatric Association. Diagnostic and statistical manual of mentab disorders (4th ed). Washington DC: American Psychiatric Association, 2000.
2. Benazzi F. Prevalence and clinical features of atypical depression in depressed outpatients: a 467-case study. Psychiatry Res 1999;86(3):259-65.
3. Benazzi F. Is atypical depression a moderate severity depression? A 536-case study. J Psychiatry Neurosci 1999;24(3):244-7.
4. Posternak MA, Zimmerman M. Partial validation of the atypical features subtype of major depressive disorder. Arch Gen Psychiatry 2002;59(1):70-6.
5. Perugi G, Akiskal HS, Lattanzi L, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry 1998;39(2):63-71.
6. Levitan RD, Kaplan AS, Brown GM, et al. Low plasma cortisol in bulimia nervosa patients with reversed neurovegetative symptoms of depression. Biol Psychiatry 1997;41(3):366-8.
7. Stewart JW, McGrath PJ, Rabkin JG, Quitkin FM. Atypical depression. A valid clinical entity? Psychiatr Clin North Am 1993;16(3):479-95.
8. Kendler KS, Eaves LJ, Walters EE, Neale MC, Heath AC, Kessler RC. The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Arch Gen Psychiatry 1996;53(5):391-9.
9. Ebert D, Barocka A. The early course of atypical depression. Eur Arch Psychiatry Clin Neurosci 1991;241(2):131-2.
10. Zubieta JK, Pande AC, Demitrack MA. Two-year follow-up of atypical depression. J Psychiatr Res 1999;33(1):23-9.
11. Nierenberg AA, Pava JA, Clancy K, Rosenbaum JF, Fava M. Are neurovegetative symptoms stable in relapsing or recurrent atypical depressive episodes? Biol Psychiatry 1996;40(8):691-6.
12. Quitkin FM, McGrath PJ, Stewart JW, et al. Phenelzine and imipramine in mood reactive depressives. Further delineation of the syndrome of atypical depression. Arch Gen Psychiatry 1989;46(9):787-93.
13. Pande AC, Birkett M, Fechner-Bates S, Haskett RF, Greden JF. Fluoxetine versus phenelzine in atypical depression. Biol Psychiatry 1996;40(10):1017-20.
14. Sogaard J, Lane R, Latimer P, et al. A 12-week study comparing moclobemide and sertraline in the treatment of outpatients with atypical depression. J Psychopharmacol 1999;13(4):406-14.
15. Lonnqvist J, Sihvo S, Syvalahti E, Kiviruusu O. Moclobemide and fluoxetine in atypical depression: a double-blind trial. J Affect Disord 1994;32(3):169-77.
16. McGrath PJ, Stewart JW, Janal MN, Petkova E, Quitkin FM, Klein DF. A placebo-controlled study of fluoxetine versus imipramine in the acute treatment of atypical depression. Am J Psychiatry 2000;157(3):344-50.
17. Stratta P, Bolino F, Cupillari M, Casacchia M. A double-blind parallel study comparing fluoxetine with imipramine in the treatment of atypical depression. Int Clin Psychopharmacol 1991;6(3):193-6.
18. Goodnick PJ, Dominguez RA, DeVane CL, Bowden CL. Bupropion slow-release response in depression: diagnosis and biochemistry. Biol Psychiatry 1998;44(7):629-32.
19. Goodnick PJ, Extein I. Bupropion and fluoxetine in depressive subtypes. Ann Clin Psychiatry 1989;1:119-22.
20. Rye DB, Dihenia B, Bliwise DL. Reversal of atypical depression, sleepiness, and REM-sleep propensity in narcolepsy with bupropion. Depress Anxiety 1998;7(2):92-5.
21. Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
22. Liebowitz MR, Quitkin FM, Stewart JW, et al. Phenelzine v imipramine in atypical depression. A preliminary report. Arch Gen Psychiatry 1984;41(7):669-77.
23. Thase ME, Carpenter L, Kupfer DJ, Frank E. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacol Bull 1991;27(1):17-22.
24. Angst J, Gamma A, Sellaro R, Zhang H, Merikangas K. Toward validation of atypical depression in the community: results of the Zurich cohort study. J Affect Disord 2002;72(2):125-38.
25. Gold PW, Chrousos GP. The endocrinology of melancholic and atypical depression: relation to neurocircuitry and somatic consequences. Proc Assoc Am Physicians 1999;111(1):22-34.
26. Garvey MJ, Schaffer C, Schaffer L, Perry PJ. Is DST status associated with depression characteristics? J Affect Disord 1989;16(2-3):159-65.
27. Geracioti TD, Jr, Loosen PT, Orth DN. Low cerebrospinal fluid corticotropin-releasing hormone concentrations in eucortisolemic depression. Biol Psychiatry 1997;42(3):165-74.
28. Casper RC, Kocsis J, Dysken M, et al. Cortisol measures in primary major depressive disorder with hypersomnia or appetite increase. J Affect Disord 1988;15(2):131-40.
29. Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry 1998;155(10):1398-406.
30. Levitan RD, Lesage A, Parikh SV, Goering P, Kennedy SH. Reversed neurovegetative symptoms of depression: a community study of Ontario. Am J Psychiatry 1997;154(7):934-40.
31. McElroy SL, Suppes T, Keck PE, Jr, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry 2000;47(12):1025-33.
32. Shapira NA, Goldsmith TD, McElroy SL. Treatment of binge-eating disorder with topiramate: a clinical case series. J Clin Psychiatry 2000;61(5):368-72.
1. American Psychiatric Association. Diagnostic and statistical manual of mentab disorders (4th ed). Washington DC: American Psychiatric Association, 2000.
2. Benazzi F. Prevalence and clinical features of atypical depression in depressed outpatients: a 467-case study. Psychiatry Res 1999;86(3):259-65.
3. Benazzi F. Is atypical depression a moderate severity depression? A 536-case study. J Psychiatry Neurosci 1999;24(3):244-7.
4. Posternak MA, Zimmerman M. Partial validation of the atypical features subtype of major depressive disorder. Arch Gen Psychiatry 2002;59(1):70-6.
5. Perugi G, Akiskal HS, Lattanzi L, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry 1998;39(2):63-71.
6. Levitan RD, Kaplan AS, Brown GM, et al. Low plasma cortisol in bulimia nervosa patients with reversed neurovegetative symptoms of depression. Biol Psychiatry 1997;41(3):366-8.
7. Stewart JW, McGrath PJ, Rabkin JG, Quitkin FM. Atypical depression. A valid clinical entity? Psychiatr Clin North Am 1993;16(3):479-95.
8. Kendler KS, Eaves LJ, Walters EE, Neale MC, Heath AC, Kessler RC. The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Arch Gen Psychiatry 1996;53(5):391-9.
9. Ebert D, Barocka A. The early course of atypical depression. Eur Arch Psychiatry Clin Neurosci 1991;241(2):131-2.
10. Zubieta JK, Pande AC, Demitrack MA. Two-year follow-up of atypical depression. J Psychiatr Res 1999;33(1):23-9.
11. Nierenberg AA, Pava JA, Clancy K, Rosenbaum JF, Fava M. Are neurovegetative symptoms stable in relapsing or recurrent atypical depressive episodes? Biol Psychiatry 1996;40(8):691-6.
12. Quitkin FM, McGrath PJ, Stewart JW, et al. Phenelzine and imipramine in mood reactive depressives. Further delineation of the syndrome of atypical depression. Arch Gen Psychiatry 1989;46(9):787-93.
13. Pande AC, Birkett M, Fechner-Bates S, Haskett RF, Greden JF. Fluoxetine versus phenelzine in atypical depression. Biol Psychiatry 1996;40(10):1017-20.
14. Sogaard J, Lane R, Latimer P, et al. A 12-week study comparing moclobemide and sertraline in the treatment of outpatients with atypical depression. J Psychopharmacol 1999;13(4):406-14.
15. Lonnqvist J, Sihvo S, Syvalahti E, Kiviruusu O. Moclobemide and fluoxetine in atypical depression: a double-blind trial. J Affect Disord 1994;32(3):169-77.
16. McGrath PJ, Stewart JW, Janal MN, Petkova E, Quitkin FM, Klein DF. A placebo-controlled study of fluoxetine versus imipramine in the acute treatment of atypical depression. Am J Psychiatry 2000;157(3):344-50.
17. Stratta P, Bolino F, Cupillari M, Casacchia M. A double-blind parallel study comparing fluoxetine with imipramine in the treatment of atypical depression. Int Clin Psychopharmacol 1991;6(3):193-6.
18. Goodnick PJ, Dominguez RA, DeVane CL, Bowden CL. Bupropion slow-release response in depression: diagnosis and biochemistry. Biol Psychiatry 1998;44(7):629-32.
19. Goodnick PJ, Extein I. Bupropion and fluoxetine in depressive subtypes. Ann Clin Psychiatry 1989;1:119-22.
20. Rye DB, Dihenia B, Bliwise DL. Reversal of atypical depression, sleepiness, and REM-sleep propensity in narcolepsy with bupropion. Depress Anxiety 1998;7(2):92-5.
21. Parker G, Roy K, Mitchell P, Wilhelm K, Malhi G, Hadzi-Pavlovic D. Atypical depression: a reappraisal. Am J Psychiatry 2002;159(9):1470-9.
22. Liebowitz MR, Quitkin FM, Stewart JW, et al. Phenelzine v imipramine in atypical depression. A preliminary report. Arch Gen Psychiatry 1984;41(7):669-77.
23. Thase ME, Carpenter L, Kupfer DJ, Frank E. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacol Bull 1991;27(1):17-22.
24. Angst J, Gamma A, Sellaro R, Zhang H, Merikangas K. Toward validation of atypical depression in the community: results of the Zurich cohort study. J Affect Disord 2002;72(2):125-38.
25. Gold PW, Chrousos GP. The endocrinology of melancholic and atypical depression: relation to neurocircuitry and somatic consequences. Proc Assoc Am Physicians 1999;111(1):22-34.
26. Garvey MJ, Schaffer C, Schaffer L, Perry PJ. Is DST status associated with depression characteristics? J Affect Disord 1989;16(2-3):159-65.
27. Geracioti TD, Jr, Loosen PT, Orth DN. Low cerebrospinal fluid corticotropin-releasing hormone concentrations in eucortisolemic depression. Biol Psychiatry 1997;42(3):165-74.
28. Casper RC, Kocsis J, Dysken M, et al. Cortisol measures in primary major depressive disorder with hypersomnia or appetite increase. J Affect Disord 1988;15(2):131-40.
29. Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry 1998;155(10):1398-406.
30. Levitan RD, Lesage A, Parikh SV, Goering P, Kennedy SH. Reversed neurovegetative symptoms of depression: a community study of Ontario. Am J Psychiatry 1997;154(7):934-40.
31. McElroy SL, Suppes T, Keck PE, Jr, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry 2000;47(12):1025-33.
32. Shapira NA, Goldsmith TD, McElroy SL. Treatment of binge-eating disorder with topiramate: a clinical case series. J Clin Psychiatry 2000;61(5):368-72.
Drug therapy algorithms target autism’s problem behaviors
Aggression, irritability, repetitive phenomena, or hyperactivity can interfere with the education and treatment of patients with autism.1 To assist clinicians in selecting drug therapies to control these behaviors, we developed a medication strategy based on controlled studies and our experience in an autism specialty clinic. In this article, we:
- offer an overview with two algorithms that show how to target maladaptive behaviors in patients of all ages with autism
- and discuss the controlled clinical evidence behind this approach.
Targeting behaviors
A multimodal approach is used to manage autistic disorder. Although behavioral techniques are useful and may decrease the need for drug therapy, one or more medications are often required to target severe maladaptive behaviors. Although we recommend that you consider all interfering behaviors when selecting medications, it is important to:
- initially focus on symptoms—such as self-injurious behaviors and aggression—that acutely affect the patient’s and caregiver’s safety
- consider the patient as being pre- or postpubertal, as developmental level may affect medication response.
Figure 1 BEHAVIOR-BASED DRUG THERAPY FOR CHILDREN WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc. Aggression or self-injury. When drug therapy is needed to control severe aggression or self-injurious behavior, we recommend a trial of an atypical antipsychotic for prepubertal patients (Figure 1). Alternately, you may consider a mood stabilizer such as lithium or divalproex for an adult patient with prominent symptoms (Figure 2). However, mood stabilizer use requires monitoring by venipuncture for potential blood cell or liver function abnormalities.
Atypical antipsychotics are associated with adverse effects including sedation, weight gain, extrapyramidal symptoms, tardive dyskinesia, and hyperprolactinemia. Therefore, you may need to monitor weight, lipid profile, glucose, liver function, and cardiac function when using this class of agent.
Repetitive phenomena can be addressed with selective serotonin reuptake inhibitors (SSRIs), although SSRIs may be activating in children and tend to be better tolerated in older adolescents and adults.
Anxiety. In children with anxiety, we suggest a trial of mirtazapine—because of its calming properties—before you try an SSRI. If both the SSRI and mirtazapine are ineffective, try an α2-adrenergic agonist. A baseline ECG is recommended before starting an α2-adrenergic agonist—particularly clonidine, which has been associated with rare cardiovascular events. Overall, these agents are well tolerated.
Hyperactivity, inattention. Anecdotal evidence indicates that stimulants may worsen symptoms of aggression, hyperactivity, and irritability in individuals with autism. Therefore, we suggest you start with an α2-adrenergic agonist when target symptoms include hyperactivity and inattention. Consider a stimulant trial if the α2-adrenergic agonist does not control the symptoms.
An atypical antipsychotic is generally recommended for autistic individuals with treatment-resistant hyperactivity and inattention, anxiety, and interfering repetitive behaviors.
Drug therapy. As summarized below, controlled evidence for behavior-based drug therapy of autism (Table.) suggests a role for antipsychotics, antidepressants, mood stabilizers, and psychostimulants in managing interfering behaviors.
Antipsychotics
Risperidone. Two controlled studies have reported the effect of risperidone on autism’s related symptoms.
McDougle et al conducted a 12-week, double-blind, placebo-controlled trial of risperidone, mean 2.9 mg/d, in adults with pervasive developmental disorders.2 Repetitive behavior, aggression, anxiety, irritability, depression, and general behavioral symptoms decreased in 8 of 14 patients, as measured by Clinical Global Impressions (CGI) scale ratings of “much improved” or “very much improved.” Sixteen subjects who received placebo showed no response. Transient sedation was the most common adverse effect.
More recently, the National Institutes of Mental Health-sponsored Research Units on Pediatric Psychopharmacology (RUPP) Autism Network completed a double-blind, placebo-controlled study of risperidone, 0.5 to 3.5 mg/d (mean 1.8 mg/d), in 101 children and adolescents with autism.3 After 8 weeks, 69% of the risperidone group responded, compared with 12% of the placebo group. Response was defined as:
- at least a 25% decrease in the Irritability subscale score of the Aberrant Behavior Checklist (ABC)
- and CGI ratings of “much improved” or “very much improved.”
Risperidone was effective for treating aggression, agitation, hyperactivity, and repetitive behavior. Adverse effects included weight gain (mean 2.7 kg vs. 0.8 kg with placebo), increased appetite, sedation, dizziness, and hypersalivation.
Olanzapine. A 12-week, open-label study of olanzapine, mean 7.8 mg/d, was conducted in eight patients ages 5 to 42 diagnosed with a pervasive developmental disorder.4 Hyperactivity, social relatedness, self-injurious behavior, aggression, anxiety, and depression improved significantly in six of seven patients who completed the trial, as measured by a CGI classification of “much improved” or “very much improved.” Adverse effects included weight gain (mean 18.4 lbs) in six patients and sedation in three.
Malone et al conducted a 6-week, open-label comparison of olanzapine, mean 7.9 mg/d, versus haloperidol, mean 1.4 mg/d, in 12 children with autistic disorder.5 Five of six subjects who received olanzapine responded, compared with three of six who received haloperidol, as determined by a CGI classification of “much improved” or “very much improved.” Anger/uncooperativeness and hyperactivity were reduced significantly only in the olanzapine group. Weight gain and sedation were the most common adverse effects with both medications. Weight gain was greater with olanzapine (mean 9 lbs) than with haloperidol (mean 3.2 lbs).
Quetiapine. Only one report addresses quetiapine in children and adolescents with autism.6 Two of six patients completed this 16-week, open-label trial of quetiapine, 100 to 350 mg/d (1.6 to 5.2 mg/kg/d). The group showed no statistically significant improvement in behavioral symptoms. Two patients achieved CGI ratings of “much improved” or “very much improved.” One subject dropped out after a possible seizure during treatment, and three others withdrew because of sedation or lack of response.
Ziprasidone. McDougle et al conducted a naturalistic, open-label study of ziprasidone, 20 to 120 mg/d (mean 59.2 mg/d), in 12 subjects ages 8 to 20. Nine were diagnosed with autism and three with a pervasive developmental disorder not otherwise specified (NOS). Six subjects responded across 14 weeks of treatment, as determined by ratings of “much improved” or “very much improved” on the CGI.7
Transient sedation was the most common adverse effect. Mean weight change was −5.83 lbs (range −35 to +6 lbs). Despite ziprasidone’s reported risk of causing abnormal cardiac rhythms, no cardiovascular adverse effects were reported.
Clozapine. Three case reports but no controlled studies have addressed clozapine in autistic disorder:
- Zuddas et al used clozapine, 100 to 200 mg/d for 3 months, to treat three children ages 8 to 12.8 Previous trials of haloperidol were ineffective, but the patients’ aggression, hyperactivity, negativism, and language and communication skills improved with clozapine, as measured by the Children’s Psychiatric Rating Scale (CPRS) and the Self-Injurious Behavior Questionnaire.
- Chen et al used clozapine, 275 mg/d, to treat a 17-year-old male inpatient.9 Aggression was significantly reduced across 15 days, as determined by a 21-question modified version of the CPRS. Side effects included mild constipation and excessive salivation.
- Clozapine, 300 mg/d for 2 months, reduced aggression in an adult patient and was associated with progressive and marked improvement of aggression and social interaction, as measured by the CGI and the Visual Analog Scale (VAS). No agranulocytosis or extrapyramidal symptoms were observed across 5 years of therapy.10
Clozapine’s adverse effect profile probably explains why the literature contains so little data regarding its use in patients with autism. This drug’s propensity to lower the seizure threshold discourages its use in a population predisposed to seizures. Autistic patients also have a low tolerance for frequent venipuncture and limited ability to communicate agranulocytosis symptoms.
Antidepressants
Clomipramine—a tricyclic antidepressant with anti-obsessional properties—has shown some positive effects in treating autistic behaviors. Even so, this compound is prescribed infrequently to patients with autism because of low tolerability. In one recent double-blind, placebo-controlled, crossover study, 36 autistic patients ages 10 to 36 received:
- clomipramine, 100 to 150 mg/d (mean 128 mg/d)
- haloperidol, 1 to 1.5 mg/d (mean 1.3 mg/d)
or placebo for 7 weeks. Among patients who completed the trial, clomipramine and haloperidol were similarly effective in reducing overall autistic symptoms, irritability, and stereotypy. However, only 37.5% of those receiving clomipramine completed the study because of adverse effects, behavioral problems, and general lack of efficacy.11
Table
CONTROLLED EVIDENCE* FOR BEHAVIOR-BASED DRUG THERAPY OF AUTISM
| Medication | Behaviors improved | Significant adverse effects | Comments |
|---|---|---|---|
| Risperidone 2 | Aggression, irritability | Mild transient sedation | Conducted in adults |
| Risperidone 3 | Aggression, irritability | Weight gain, increased appetite, sedation, tremor, hypersalivation | Largest controlled study to date in children with autism |
| Clomipramine 11 | Irritability, stereotypy | Tachycardia, tremors, diaphoresis, insomnia, nausea | Conducted in children and adults |
| Fluvoxamine 12 | Aggression, repetitive phenomena | Nausea, sedation | No published controlled pediatric data; unpublished pediatric data unfavorable |
| Clonidine 24 | Hyperactivity, irritability, stereotypies, oppositional behavior, aggression, self-injury | Hypotension, sedation, decreased activity | Small number of subjects |
| Clonidine 25 | Impulsivity, self-stimulation, hyperarousal | Sedation and fatigue | Small number of subjects |
| Methylphenidate 28 | Hyperactivity, irritability | Social withdrawal and irritability | Adverse effects more common at 0.6 mg/kg/dose |
| • Double-blind, placebo-controlled studies | |||
Fluvoxamine. Only one double-blind, placebo-controlled study has examined the use of an SSRI in autistic disorder.12 In this 12-week trial, 30 adults with autism received fluvoxamine, mean 276.7 mg/d, or placebo. Eight of 15 subjects in the fluvoxamine group were categorized as “much improved” or “very much improved” on the CGI.
Fluvoxamine was much more effective than placebo in reducing repetitive thoughts and behavior, aggression, and maladaptive behavior. Adverse effects included minimal sedation and nausea.
Unpublished data of McDougle et al suggest that autistic children and adolescents respond less favorably than adults to fluvoxamine. In a 12-week, double-blind, placebocontrolled trial in patients ages 5 to 18, only 1 of 18 subjects responded to fluvoxamine at a mean dosage of 106.9 mg/d. Agitation, increased aggression, hyperactivity, and increased repetitive behavior were reported.
Fluoxetine. Seven autistic patients ages 9 to 20 were treated with fluoxetine, 20 to 80 mg/d (mean 37.1 mg/d) in an 18-month longitudinal open trial. Irritability, lethargy, and stereotypy improved, as measured by the ABC.13 Adverse effects included increased hyperactivity and transient appetite suppression.
In another open-label trial of 37 autistic children ages 2 to 7, response was rated by investigators as “excellent” in 11 and “good” in another 11 who received fluoxetine, 0.2 to 1.4 mg/kg/d. However, aggression was a frequent cause for drug discontinuation during the 21-month study.14
Sertraline. In an open-label trial, Steingard et al treated nine autistic children ages 6 to 12 with sertraline, 25 to 50 mg/d for 2 to 8 weeks. Clinical improvement was observed in irritability, transition-associated anxiety, and need for sameness in eight of the children.15
Figure 2 BEHAVIOR-BASED DRUG THERAPY FOR POSTPUBERTAL PATIENTS WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc.In an open-label trial, 42 adults with pervasive developmental disorders were treated for 12 weeks with sertraline, 50 to 200 mg/d (mean 122 mg/d). Twenty-four (57%) achieved CGI ratings of “much improved” or “very much improved” in aggressive and repetitive behavior.16
Paroxetine. Fifteen adults with profound mental retardation (including seven with pervasive developmental disorders) received paroxetine, 10 to 50 mg/d (mean 35 mg/d) in a 4-month open-label trial. Frequency and severity of aggression were rated as improved after 1 month, but not at 4 months.17
Mirtazapine. In an open-label trial, 26 patients ages 3 to 23 with pervasive developmental disorders were treated with mirtazapine, 7.5 to 45 mg/d (mean 30.3 mg/d). Aggression, self-injury, irritability, hyperactivity, anxiety, depression, and insomnia decreased in 9 patients (34%), as determined by ratings of “much improved” or “very much improved” on the CGI. Adverse effects included increased appetite and transient sedation.18
Mood stabilizers
Lithium. No recent studies of lithium in pervasive developmental disorders are known to exist, but several case reports have been published:
- two reports found lithium decreased manic symptoms in individuals with autism and a family history of bipolar disorder19,20
- one report of lithium augmentation of fluvoxamine in an adult with autistic disorder noted markedly improved aggression and impulsivity after 2 weeks of treatment, as measured by the CGI, Brown Aggression Scale, and Vineland Adaptive Behavior Scale.21
Divalproex. In an open-label trial, 14 subjects ages 5 to 40 with pervasive developmental disorders were given divalproex sodium, 125 to 2,500 mg/d (mean 768 mg/d; mean blood level 75.8 mcg/mL. Affective instability, repetitive behavior, impulsivity, and aggression improved in 10 patients (71%), as measured by CGI ratings of “much improved” or “very much improved.”22 Adverse effects included sedation, weight gain, hair loss, behavioral activation, and elevated liver enzymes.
Lamotrigine. In a 4-week, double-blind, placebo-controlled trial, lamotrigine, 5.0 mg/kg/d, was given to 14 children ages 3 to 11 with autistic disorder.23 Lamotrigine and placebo showed no significant differences in effect, as measured by the ABC, Autism Behavior Checklist, Vineland scales, Childhood Autism Rating Scale, and PreLinguistic Autism Diagnostic Observation Scale. Insomnia and hyperactivity were the most common adverse effects.
α2-adrenergic agonists
Clonidine. Jaselskis et al administered clonidine, 4 to 10 mcg/kg/d, to eight children ages 5 to 13 with autism in a 6-week, double-blind, placebo-controlled, crossover study.24 Symptoms of hyperactivity, irritability, and oppositional behavior improved, as determined by teacher ratings on the ABC, Conners Abbreviated Parent-Teacher Questionnaire, and Attention Deficit Disorder with Hyperactivity Comprehensive Teacher’s Rating Scale. Adverse effects included hypotension, sedation, and decreased activity.
Nine autistic patients ages 5 to 33 received transdermal clonidine, 0.16 to 0.48 mcg/kg/d (mean 3.6 mcg/kg/d), in a 4-week, double-blind, placebo-controlled, crossover study. Hyperarousal, impulsivity, and self-stimulation improved, as measured by the Ritvo-Freeman Real Life Rating Scale and the CGI. Sedation and fatigue were reported, especially during the first 2 weeks of treatment.25
Guanfacine. The effect of guanfacine, 0.25 to 9.0 mg/d (mean 2.6 mg/d), was examined retrospectively in 80 children and adolescents ages 3 to 18 with pervasive developmental disorders.26 Hyperactivity, inattention, and tics improved in the 19 subjects (23.8%) who were rated “much improved” or “very much improved” on the CGI. Sedation was the most frequently reported adverse effect.
Psychostimulants
Early reports showed little benefit from stimulants in pervasive developmental disorders, but more recent studies suggest a modest effect. The RUPP Autism Network is conducting a large controlled investigation of methylphenidate to better understand the role of stimulants in children and adolescents in this diagnostic cluster.
Quintana et al conducted a double-blind, crossover study of methylphenidate, 10 or 20 mg bid for 2 weeks, in 10 children ages 7 to 11 with autism.27 Although irritability and hyperactivity showed statistically significant improvement as determined by the ABC and Conners Teacher Questionnaire, the authors reported only modest clinical effects. More recently, use of methylphenidate, 0.3 and 0.6 mg/kg/dose, was associated with a 50% decrease on the Connors Hyperactivity Index in 8 of 13 autistic children ages 5 to 11.28 Adverse effects—most common with the 0.6 mg/kg/dose—included social withdrawal and irritability in this double-blind, placebo-controlled, crossover study.
Related resources
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice. New York: Oxford University Press, 2002.
- Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- National Institute of Mental Health. Autism booklet. www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America. www.autism-society.org
Drug brand names
- Clomipramine • Anafranil
- Clonidine • Catapres
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith
- Methylphenidate • Ritalin
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Ziprasidone • Geodon
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives grant support from and is a consultant to Eli Lilly & Co.
Dr. McDougle receives grant support from and is a consultant to Pfizer Inc., Eli Lilly & Co., and Janssen Pharmaceutica, and is a speaker for Pfizer Inc. and Janssen Pharmaceutica.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression Young Investigator Award (Dr. Posey), a Research Unit on Pediatric Psychopharmacology contract (N01MH70001) from the National Institute of Mental Health to Indiana University (Drs. McDougle and Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development grant (B-01-SP-IN-0200).
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: American Psychiatric Association, 2000.
2. McDougle CJ, Holmes JP, Carlson DC, Pelton GH, Cohen DJ, Price LH. A double-blind placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Arch Gen Psychiatry 1998;55:633-41.
3. Research Units on Pediatric Psychopharmacology Autism Network. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
4. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: An open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
5. Malone RP, Cater J, Sheikh RM, Choudhury MS, Delaney MA. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
6. Martin A, Koenig K, Scahill L, Bregman J. Open-label quetiapine in the treatment of children and adolescents with autistic disorder. J Child Adolesc Psychopharmacol 1999;9:99-107.
7. McDougle CJ, Kem DL, Posey DJ. Case series: use of ziprasidone for maladaptive symptoms in youths with autism. J Am Acad Child Adolesc Psychiatry 2002;41(8):921-7.
8. Zuddas A, Ledda MG, Fratta A, Muglia P, Cianchetti C. Clinical effects of clozapine on autistic disorder. Am J Psychiatry 1996;153(5):738.-
9. Chen NC, Bedair HS, McKay B, Bowers MB, Mazure C. Clozapine in the treatment of aggression in an adolescent with autistic disorder. J Clin Psychiatry 2001;62(6):479-80.
10. Gobbi G, Pulvirenti L. Long-term treatment with clozapine in an adult with autistic disorder accompanied by aggressive behaviour. J Psych Neurol 2001;26(4):340-1.
11. Remington G, Sloman L, Konstantareas M, Parker K, Gow R. Clomipramine versus haloperidol in the treatment of autistic disorder: A double-blind, placebo-controlled, crossover study. J Clin Psychopharmacol 2001;21(4):440-4.
12. McDougle CJ, Naylor ST, Cohen DJ, Volkmar FR, Heninger GR, Price LH. A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Arch Gen Psychiatry 1996;53:1001-8.
13. Fatemi SH, Realmuto GM, Khan L, Thuras P. Fluoxetine in treatment of adolescent patients with autism: a longitudinal open trial. J Autism Dev Disord 1998;28(4):303-7.
14. DeLong GR, Teague LA, Kamran MM. Effects of fluoxetine treatment in young children with idiopathic autism. Dev Med Child Neurol 1998;40:551-62.
15. Steingard RJ, Zimnitzky B, DeMaso DR, Bauman ML, Bucci JP. Sertraline treatment of transition-associated anxiety and agitation in children with autistic disorder. J Child Adolesc Psychopharmacol 1997;7(1):9-15.
16. McDougle CJ, Brodkin ES, Naylor ST, Carlson DC, Cohen DJ, Price LH. Sertraline in adults with pervasive developmental disorders: a prospective open-label investigation. J Clin Psychopharmacol 1998;18:62-6.
17. Davanzo PA, Belin TR, Widawski MH, King BH. Paroxetine treatment of aggression and self-injury in persons with mental retardation. Am J Ment Retard 1998;102(5):427-37.
18. Posey DJ, Guenin KD, Kohn AE, Swiezy NB, McDougle CJ. A naturalistic open-label study of mirtazapine in autistic and other pervasive developmental disorders. J Child Adolesc Psychopharmacol 2001;11(3):267-77.
19. Kerbeshian J, Burd L, Fisher W. Lithium carbonate in the treatment of two patients with infantile autism and atypical bipolar symptomatology. J Clin Psychopharmacol 1987;7(6):401-5.
20. Steingard R, Biederman J. Lithium-responsive manic-like symptoms in two individuals with autism and mental retardation. J Am Acad Child Adolesc Psychiatry 1987;26:932-5.
21. Epperson CN, McDougle CJ, Anand A, et al. Lithium augmentation of fluvoxamine in autistic disorder: a case report. J Child Adolesc Psychopharmacol 1994;4:201-7.
22. Hollander E, Dolgoff-Kaspar R, Cartwright C, Rawitt R, Novotny S. An open trial of divalproex sodium in autism spectrum disorders. J Clin Psychiatry 2001;62(7):530-4.
23. Belsito KM, Law PA, Kirk KS, Landa RJ, Zimmerman AW. Lamotrigine therapy for autistic disorder: a randomized, double-blind, placebo-controlled trial. J Autism Dev Disord 2001;31(2):175-81.
24. Jaselskis CA, Cook EH, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
25. Fankhauser MP, Karumanchi VC, German ML, Yates A, Karumanchi SD. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
26. Posey DJ, Decker J, Sasher TM, Kohburn A, Swiezy NB, McDougle CJ. A retrospective analysis of guanfacine in the treatment of autism. New Orleans: American Psychiatric Association annual meeting, 2001; new research abstracts no. 816.
27. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-95.
28. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
Aggression, irritability, repetitive phenomena, or hyperactivity can interfere with the education and treatment of patients with autism.1 To assist clinicians in selecting drug therapies to control these behaviors, we developed a medication strategy based on controlled studies and our experience in an autism specialty clinic. In this article, we:
- offer an overview with two algorithms that show how to target maladaptive behaviors in patients of all ages with autism
- and discuss the controlled clinical evidence behind this approach.
Targeting behaviors
A multimodal approach is used to manage autistic disorder. Although behavioral techniques are useful and may decrease the need for drug therapy, one or more medications are often required to target severe maladaptive behaviors. Although we recommend that you consider all interfering behaviors when selecting medications, it is important to:
- initially focus on symptoms—such as self-injurious behaviors and aggression—that acutely affect the patient’s and caregiver’s safety
- consider the patient as being pre- or postpubertal, as developmental level may affect medication response.
Figure 1 BEHAVIOR-BASED DRUG THERAPY FOR CHILDREN WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc. Aggression or self-injury. When drug therapy is needed to control severe aggression or self-injurious behavior, we recommend a trial of an atypical antipsychotic for prepubertal patients (Figure 1). Alternately, you may consider a mood stabilizer such as lithium or divalproex for an adult patient with prominent symptoms (Figure 2). However, mood stabilizer use requires monitoring by venipuncture for potential blood cell or liver function abnormalities.
Atypical antipsychotics are associated with adverse effects including sedation, weight gain, extrapyramidal symptoms, tardive dyskinesia, and hyperprolactinemia. Therefore, you may need to monitor weight, lipid profile, glucose, liver function, and cardiac function when using this class of agent.
Repetitive phenomena can be addressed with selective serotonin reuptake inhibitors (SSRIs), although SSRIs may be activating in children and tend to be better tolerated in older adolescents and adults.
Anxiety. In children with anxiety, we suggest a trial of mirtazapine—because of its calming properties—before you try an SSRI. If both the SSRI and mirtazapine are ineffective, try an α2-adrenergic agonist. A baseline ECG is recommended before starting an α2-adrenergic agonist—particularly clonidine, which has been associated with rare cardiovascular events. Overall, these agents are well tolerated.
Hyperactivity, inattention. Anecdotal evidence indicates that stimulants may worsen symptoms of aggression, hyperactivity, and irritability in individuals with autism. Therefore, we suggest you start with an α2-adrenergic agonist when target symptoms include hyperactivity and inattention. Consider a stimulant trial if the α2-adrenergic agonist does not control the symptoms.
An atypical antipsychotic is generally recommended for autistic individuals with treatment-resistant hyperactivity and inattention, anxiety, and interfering repetitive behaviors.
Drug therapy. As summarized below, controlled evidence for behavior-based drug therapy of autism (Table.) suggests a role for antipsychotics, antidepressants, mood stabilizers, and psychostimulants in managing interfering behaviors.
Antipsychotics
Risperidone. Two controlled studies have reported the effect of risperidone on autism’s related symptoms.
McDougle et al conducted a 12-week, double-blind, placebo-controlled trial of risperidone, mean 2.9 mg/d, in adults with pervasive developmental disorders.2 Repetitive behavior, aggression, anxiety, irritability, depression, and general behavioral symptoms decreased in 8 of 14 patients, as measured by Clinical Global Impressions (CGI) scale ratings of “much improved” or “very much improved.” Sixteen subjects who received placebo showed no response. Transient sedation was the most common adverse effect.
More recently, the National Institutes of Mental Health-sponsored Research Units on Pediatric Psychopharmacology (RUPP) Autism Network completed a double-blind, placebo-controlled study of risperidone, 0.5 to 3.5 mg/d (mean 1.8 mg/d), in 101 children and adolescents with autism.3 After 8 weeks, 69% of the risperidone group responded, compared with 12% of the placebo group. Response was defined as:
- at least a 25% decrease in the Irritability subscale score of the Aberrant Behavior Checklist (ABC)
- and CGI ratings of “much improved” or “very much improved.”
Risperidone was effective for treating aggression, agitation, hyperactivity, and repetitive behavior. Adverse effects included weight gain (mean 2.7 kg vs. 0.8 kg with placebo), increased appetite, sedation, dizziness, and hypersalivation.
Olanzapine. A 12-week, open-label study of olanzapine, mean 7.8 mg/d, was conducted in eight patients ages 5 to 42 diagnosed with a pervasive developmental disorder.4 Hyperactivity, social relatedness, self-injurious behavior, aggression, anxiety, and depression improved significantly in six of seven patients who completed the trial, as measured by a CGI classification of “much improved” or “very much improved.” Adverse effects included weight gain (mean 18.4 lbs) in six patients and sedation in three.
Malone et al conducted a 6-week, open-label comparison of olanzapine, mean 7.9 mg/d, versus haloperidol, mean 1.4 mg/d, in 12 children with autistic disorder.5 Five of six subjects who received olanzapine responded, compared with three of six who received haloperidol, as determined by a CGI classification of “much improved” or “very much improved.” Anger/uncooperativeness and hyperactivity were reduced significantly only in the olanzapine group. Weight gain and sedation were the most common adverse effects with both medications. Weight gain was greater with olanzapine (mean 9 lbs) than with haloperidol (mean 3.2 lbs).
Quetiapine. Only one report addresses quetiapine in children and adolescents with autism.6 Two of six patients completed this 16-week, open-label trial of quetiapine, 100 to 350 mg/d (1.6 to 5.2 mg/kg/d). The group showed no statistically significant improvement in behavioral symptoms. Two patients achieved CGI ratings of “much improved” or “very much improved.” One subject dropped out after a possible seizure during treatment, and three others withdrew because of sedation or lack of response.
Ziprasidone. McDougle et al conducted a naturalistic, open-label study of ziprasidone, 20 to 120 mg/d (mean 59.2 mg/d), in 12 subjects ages 8 to 20. Nine were diagnosed with autism and three with a pervasive developmental disorder not otherwise specified (NOS). Six subjects responded across 14 weeks of treatment, as determined by ratings of “much improved” or “very much improved” on the CGI.7
Transient sedation was the most common adverse effect. Mean weight change was −5.83 lbs (range −35 to +6 lbs). Despite ziprasidone’s reported risk of causing abnormal cardiac rhythms, no cardiovascular adverse effects were reported.
Clozapine. Three case reports but no controlled studies have addressed clozapine in autistic disorder:
- Zuddas et al used clozapine, 100 to 200 mg/d for 3 months, to treat three children ages 8 to 12.8 Previous trials of haloperidol were ineffective, but the patients’ aggression, hyperactivity, negativism, and language and communication skills improved with clozapine, as measured by the Children’s Psychiatric Rating Scale (CPRS) and the Self-Injurious Behavior Questionnaire.
- Chen et al used clozapine, 275 mg/d, to treat a 17-year-old male inpatient.9 Aggression was significantly reduced across 15 days, as determined by a 21-question modified version of the CPRS. Side effects included mild constipation and excessive salivation.
- Clozapine, 300 mg/d for 2 months, reduced aggression in an adult patient and was associated with progressive and marked improvement of aggression and social interaction, as measured by the CGI and the Visual Analog Scale (VAS). No agranulocytosis or extrapyramidal symptoms were observed across 5 years of therapy.10
Clozapine’s adverse effect profile probably explains why the literature contains so little data regarding its use in patients with autism. This drug’s propensity to lower the seizure threshold discourages its use in a population predisposed to seizures. Autistic patients also have a low tolerance for frequent venipuncture and limited ability to communicate agranulocytosis symptoms.
Antidepressants
Clomipramine—a tricyclic antidepressant with anti-obsessional properties—has shown some positive effects in treating autistic behaviors. Even so, this compound is prescribed infrequently to patients with autism because of low tolerability. In one recent double-blind, placebo-controlled, crossover study, 36 autistic patients ages 10 to 36 received:
- clomipramine, 100 to 150 mg/d (mean 128 mg/d)
- haloperidol, 1 to 1.5 mg/d (mean 1.3 mg/d)
or placebo for 7 weeks. Among patients who completed the trial, clomipramine and haloperidol were similarly effective in reducing overall autistic symptoms, irritability, and stereotypy. However, only 37.5% of those receiving clomipramine completed the study because of adverse effects, behavioral problems, and general lack of efficacy.11
Table
CONTROLLED EVIDENCE* FOR BEHAVIOR-BASED DRUG THERAPY OF AUTISM
| Medication | Behaviors improved | Significant adverse effects | Comments |
|---|---|---|---|
| Risperidone 2 | Aggression, irritability | Mild transient sedation | Conducted in adults |
| Risperidone 3 | Aggression, irritability | Weight gain, increased appetite, sedation, tremor, hypersalivation | Largest controlled study to date in children with autism |
| Clomipramine 11 | Irritability, stereotypy | Tachycardia, tremors, diaphoresis, insomnia, nausea | Conducted in children and adults |
| Fluvoxamine 12 | Aggression, repetitive phenomena | Nausea, sedation | No published controlled pediatric data; unpublished pediatric data unfavorable |
| Clonidine 24 | Hyperactivity, irritability, stereotypies, oppositional behavior, aggression, self-injury | Hypotension, sedation, decreased activity | Small number of subjects |
| Clonidine 25 | Impulsivity, self-stimulation, hyperarousal | Sedation and fatigue | Small number of subjects |
| Methylphenidate 28 | Hyperactivity, irritability | Social withdrawal and irritability | Adverse effects more common at 0.6 mg/kg/dose |
| • Double-blind, placebo-controlled studies | |||
Fluvoxamine. Only one double-blind, placebo-controlled study has examined the use of an SSRI in autistic disorder.12 In this 12-week trial, 30 adults with autism received fluvoxamine, mean 276.7 mg/d, or placebo. Eight of 15 subjects in the fluvoxamine group were categorized as “much improved” or “very much improved” on the CGI.
Fluvoxamine was much more effective than placebo in reducing repetitive thoughts and behavior, aggression, and maladaptive behavior. Adverse effects included minimal sedation and nausea.
Unpublished data of McDougle et al suggest that autistic children and adolescents respond less favorably than adults to fluvoxamine. In a 12-week, double-blind, placebocontrolled trial in patients ages 5 to 18, only 1 of 18 subjects responded to fluvoxamine at a mean dosage of 106.9 mg/d. Agitation, increased aggression, hyperactivity, and increased repetitive behavior were reported.
Fluoxetine. Seven autistic patients ages 9 to 20 were treated with fluoxetine, 20 to 80 mg/d (mean 37.1 mg/d) in an 18-month longitudinal open trial. Irritability, lethargy, and stereotypy improved, as measured by the ABC.13 Adverse effects included increased hyperactivity and transient appetite suppression.
In another open-label trial of 37 autistic children ages 2 to 7, response was rated by investigators as “excellent” in 11 and “good” in another 11 who received fluoxetine, 0.2 to 1.4 mg/kg/d. However, aggression was a frequent cause for drug discontinuation during the 21-month study.14
Sertraline. In an open-label trial, Steingard et al treated nine autistic children ages 6 to 12 with sertraline, 25 to 50 mg/d for 2 to 8 weeks. Clinical improvement was observed in irritability, transition-associated anxiety, and need for sameness in eight of the children.15
Figure 2 BEHAVIOR-BASED DRUG THERAPY FOR POSTPUBERTAL PATIENTS WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc.In an open-label trial, 42 adults with pervasive developmental disorders were treated for 12 weeks with sertraline, 50 to 200 mg/d (mean 122 mg/d). Twenty-four (57%) achieved CGI ratings of “much improved” or “very much improved” in aggressive and repetitive behavior.16
Paroxetine. Fifteen adults with profound mental retardation (including seven with pervasive developmental disorders) received paroxetine, 10 to 50 mg/d (mean 35 mg/d) in a 4-month open-label trial. Frequency and severity of aggression were rated as improved after 1 month, but not at 4 months.17
Mirtazapine. In an open-label trial, 26 patients ages 3 to 23 with pervasive developmental disorders were treated with mirtazapine, 7.5 to 45 mg/d (mean 30.3 mg/d). Aggression, self-injury, irritability, hyperactivity, anxiety, depression, and insomnia decreased in 9 patients (34%), as determined by ratings of “much improved” or “very much improved” on the CGI. Adverse effects included increased appetite and transient sedation.18
Mood stabilizers
Lithium. No recent studies of lithium in pervasive developmental disorders are known to exist, but several case reports have been published:
- two reports found lithium decreased manic symptoms in individuals with autism and a family history of bipolar disorder19,20
- one report of lithium augmentation of fluvoxamine in an adult with autistic disorder noted markedly improved aggression and impulsivity after 2 weeks of treatment, as measured by the CGI, Brown Aggression Scale, and Vineland Adaptive Behavior Scale.21
Divalproex. In an open-label trial, 14 subjects ages 5 to 40 with pervasive developmental disorders were given divalproex sodium, 125 to 2,500 mg/d (mean 768 mg/d; mean blood level 75.8 mcg/mL. Affective instability, repetitive behavior, impulsivity, and aggression improved in 10 patients (71%), as measured by CGI ratings of “much improved” or “very much improved.”22 Adverse effects included sedation, weight gain, hair loss, behavioral activation, and elevated liver enzymes.
Lamotrigine. In a 4-week, double-blind, placebo-controlled trial, lamotrigine, 5.0 mg/kg/d, was given to 14 children ages 3 to 11 with autistic disorder.23 Lamotrigine and placebo showed no significant differences in effect, as measured by the ABC, Autism Behavior Checklist, Vineland scales, Childhood Autism Rating Scale, and PreLinguistic Autism Diagnostic Observation Scale. Insomnia and hyperactivity were the most common adverse effects.
α2-adrenergic agonists
Clonidine. Jaselskis et al administered clonidine, 4 to 10 mcg/kg/d, to eight children ages 5 to 13 with autism in a 6-week, double-blind, placebo-controlled, crossover study.24 Symptoms of hyperactivity, irritability, and oppositional behavior improved, as determined by teacher ratings on the ABC, Conners Abbreviated Parent-Teacher Questionnaire, and Attention Deficit Disorder with Hyperactivity Comprehensive Teacher’s Rating Scale. Adverse effects included hypotension, sedation, and decreased activity.
Nine autistic patients ages 5 to 33 received transdermal clonidine, 0.16 to 0.48 mcg/kg/d (mean 3.6 mcg/kg/d), in a 4-week, double-blind, placebo-controlled, crossover study. Hyperarousal, impulsivity, and self-stimulation improved, as measured by the Ritvo-Freeman Real Life Rating Scale and the CGI. Sedation and fatigue were reported, especially during the first 2 weeks of treatment.25
Guanfacine. The effect of guanfacine, 0.25 to 9.0 mg/d (mean 2.6 mg/d), was examined retrospectively in 80 children and adolescents ages 3 to 18 with pervasive developmental disorders.26 Hyperactivity, inattention, and tics improved in the 19 subjects (23.8%) who were rated “much improved” or “very much improved” on the CGI. Sedation was the most frequently reported adverse effect.
Psychostimulants
Early reports showed little benefit from stimulants in pervasive developmental disorders, but more recent studies suggest a modest effect. The RUPP Autism Network is conducting a large controlled investigation of methylphenidate to better understand the role of stimulants in children and adolescents in this diagnostic cluster.
Quintana et al conducted a double-blind, crossover study of methylphenidate, 10 or 20 mg bid for 2 weeks, in 10 children ages 7 to 11 with autism.27 Although irritability and hyperactivity showed statistically significant improvement as determined by the ABC and Conners Teacher Questionnaire, the authors reported only modest clinical effects. More recently, use of methylphenidate, 0.3 and 0.6 mg/kg/dose, was associated with a 50% decrease on the Connors Hyperactivity Index in 8 of 13 autistic children ages 5 to 11.28 Adverse effects—most common with the 0.6 mg/kg/dose—included social withdrawal and irritability in this double-blind, placebo-controlled, crossover study.
Related resources
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice. New York: Oxford University Press, 2002.
- Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- National Institute of Mental Health. Autism booklet. www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America. www.autism-society.org
Drug brand names
- Clomipramine • Anafranil
- Clonidine • Catapres
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith
- Methylphenidate • Ritalin
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Ziprasidone • Geodon
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives grant support from and is a consultant to Eli Lilly & Co.
Dr. McDougle receives grant support from and is a consultant to Pfizer Inc., Eli Lilly & Co., and Janssen Pharmaceutica, and is a speaker for Pfizer Inc. and Janssen Pharmaceutica.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression Young Investigator Award (Dr. Posey), a Research Unit on Pediatric Psychopharmacology contract (N01MH70001) from the National Institute of Mental Health to Indiana University (Drs. McDougle and Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development grant (B-01-SP-IN-0200).
Aggression, irritability, repetitive phenomena, or hyperactivity can interfere with the education and treatment of patients with autism.1 To assist clinicians in selecting drug therapies to control these behaviors, we developed a medication strategy based on controlled studies and our experience in an autism specialty clinic. In this article, we:
- offer an overview with two algorithms that show how to target maladaptive behaviors in patients of all ages with autism
- and discuss the controlled clinical evidence behind this approach.
Targeting behaviors
A multimodal approach is used to manage autistic disorder. Although behavioral techniques are useful and may decrease the need for drug therapy, one or more medications are often required to target severe maladaptive behaviors. Although we recommend that you consider all interfering behaviors when selecting medications, it is important to:
- initially focus on symptoms—such as self-injurious behaviors and aggression—that acutely affect the patient’s and caregiver’s safety
- consider the patient as being pre- or postpubertal, as developmental level may affect medication response.
Figure 1 BEHAVIOR-BASED DRUG THERAPY FOR CHILDREN WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc. Aggression or self-injury. When drug therapy is needed to control severe aggression or self-injurious behavior, we recommend a trial of an atypical antipsychotic for prepubertal patients (Figure 1). Alternately, you may consider a mood stabilizer such as lithium or divalproex for an adult patient with prominent symptoms (Figure 2). However, mood stabilizer use requires monitoring by venipuncture for potential blood cell or liver function abnormalities.
Atypical antipsychotics are associated with adverse effects including sedation, weight gain, extrapyramidal symptoms, tardive dyskinesia, and hyperprolactinemia. Therefore, you may need to monitor weight, lipid profile, glucose, liver function, and cardiac function when using this class of agent.
Repetitive phenomena can be addressed with selective serotonin reuptake inhibitors (SSRIs), although SSRIs may be activating in children and tend to be better tolerated in older adolescents and adults.
Anxiety. In children with anxiety, we suggest a trial of mirtazapine—because of its calming properties—before you try an SSRI. If both the SSRI and mirtazapine are ineffective, try an α2-adrenergic agonist. A baseline ECG is recommended before starting an α2-adrenergic agonist—particularly clonidine, which has been associated with rare cardiovascular events. Overall, these agents are well tolerated.
Hyperactivity, inattention. Anecdotal evidence indicates that stimulants may worsen symptoms of aggression, hyperactivity, and irritability in individuals with autism. Therefore, we suggest you start with an α2-adrenergic agonist when target symptoms include hyperactivity and inattention. Consider a stimulant trial if the α2-adrenergic agonist does not control the symptoms.
An atypical antipsychotic is generally recommended for autistic individuals with treatment-resistant hyperactivity and inattention, anxiety, and interfering repetitive behaviors.
Drug therapy. As summarized below, controlled evidence for behavior-based drug therapy of autism (Table.) suggests a role for antipsychotics, antidepressants, mood stabilizers, and psychostimulants in managing interfering behaviors.
Antipsychotics
Risperidone. Two controlled studies have reported the effect of risperidone on autism’s related symptoms.
McDougle et al conducted a 12-week, double-blind, placebo-controlled trial of risperidone, mean 2.9 mg/d, in adults with pervasive developmental disorders.2 Repetitive behavior, aggression, anxiety, irritability, depression, and general behavioral symptoms decreased in 8 of 14 patients, as measured by Clinical Global Impressions (CGI) scale ratings of “much improved” or “very much improved.” Sixteen subjects who received placebo showed no response. Transient sedation was the most common adverse effect.
More recently, the National Institutes of Mental Health-sponsored Research Units on Pediatric Psychopharmacology (RUPP) Autism Network completed a double-blind, placebo-controlled study of risperidone, 0.5 to 3.5 mg/d (mean 1.8 mg/d), in 101 children and adolescents with autism.3 After 8 weeks, 69% of the risperidone group responded, compared with 12% of the placebo group. Response was defined as:
- at least a 25% decrease in the Irritability subscale score of the Aberrant Behavior Checklist (ABC)
- and CGI ratings of “much improved” or “very much improved.”
Risperidone was effective for treating aggression, agitation, hyperactivity, and repetitive behavior. Adverse effects included weight gain (mean 2.7 kg vs. 0.8 kg with placebo), increased appetite, sedation, dizziness, and hypersalivation.
Olanzapine. A 12-week, open-label study of olanzapine, mean 7.8 mg/d, was conducted in eight patients ages 5 to 42 diagnosed with a pervasive developmental disorder.4 Hyperactivity, social relatedness, self-injurious behavior, aggression, anxiety, and depression improved significantly in six of seven patients who completed the trial, as measured by a CGI classification of “much improved” or “very much improved.” Adverse effects included weight gain (mean 18.4 lbs) in six patients and sedation in three.
Malone et al conducted a 6-week, open-label comparison of olanzapine, mean 7.9 mg/d, versus haloperidol, mean 1.4 mg/d, in 12 children with autistic disorder.5 Five of six subjects who received olanzapine responded, compared with three of six who received haloperidol, as determined by a CGI classification of “much improved” or “very much improved.” Anger/uncooperativeness and hyperactivity were reduced significantly only in the olanzapine group. Weight gain and sedation were the most common adverse effects with both medications. Weight gain was greater with olanzapine (mean 9 lbs) than with haloperidol (mean 3.2 lbs).
Quetiapine. Only one report addresses quetiapine in children and adolescents with autism.6 Two of six patients completed this 16-week, open-label trial of quetiapine, 100 to 350 mg/d (1.6 to 5.2 mg/kg/d). The group showed no statistically significant improvement in behavioral symptoms. Two patients achieved CGI ratings of “much improved” or “very much improved.” One subject dropped out after a possible seizure during treatment, and three others withdrew because of sedation or lack of response.
Ziprasidone. McDougle et al conducted a naturalistic, open-label study of ziprasidone, 20 to 120 mg/d (mean 59.2 mg/d), in 12 subjects ages 8 to 20. Nine were diagnosed with autism and three with a pervasive developmental disorder not otherwise specified (NOS). Six subjects responded across 14 weeks of treatment, as determined by ratings of “much improved” or “very much improved” on the CGI.7
Transient sedation was the most common adverse effect. Mean weight change was −5.83 lbs (range −35 to +6 lbs). Despite ziprasidone’s reported risk of causing abnormal cardiac rhythms, no cardiovascular adverse effects were reported.
Clozapine. Three case reports but no controlled studies have addressed clozapine in autistic disorder:
- Zuddas et al used clozapine, 100 to 200 mg/d for 3 months, to treat three children ages 8 to 12.8 Previous trials of haloperidol were ineffective, but the patients’ aggression, hyperactivity, negativism, and language and communication skills improved with clozapine, as measured by the Children’s Psychiatric Rating Scale (CPRS) and the Self-Injurious Behavior Questionnaire.
- Chen et al used clozapine, 275 mg/d, to treat a 17-year-old male inpatient.9 Aggression was significantly reduced across 15 days, as determined by a 21-question modified version of the CPRS. Side effects included mild constipation and excessive salivation.
- Clozapine, 300 mg/d for 2 months, reduced aggression in an adult patient and was associated with progressive and marked improvement of aggression and social interaction, as measured by the CGI and the Visual Analog Scale (VAS). No agranulocytosis or extrapyramidal symptoms were observed across 5 years of therapy.10
Clozapine’s adverse effect profile probably explains why the literature contains so little data regarding its use in patients with autism. This drug’s propensity to lower the seizure threshold discourages its use in a population predisposed to seizures. Autistic patients also have a low tolerance for frequent venipuncture and limited ability to communicate agranulocytosis symptoms.
Antidepressants
Clomipramine—a tricyclic antidepressant with anti-obsessional properties—has shown some positive effects in treating autistic behaviors. Even so, this compound is prescribed infrequently to patients with autism because of low tolerability. In one recent double-blind, placebo-controlled, crossover study, 36 autistic patients ages 10 to 36 received:
- clomipramine, 100 to 150 mg/d (mean 128 mg/d)
- haloperidol, 1 to 1.5 mg/d (mean 1.3 mg/d)
or placebo for 7 weeks. Among patients who completed the trial, clomipramine and haloperidol were similarly effective in reducing overall autistic symptoms, irritability, and stereotypy. However, only 37.5% of those receiving clomipramine completed the study because of adverse effects, behavioral problems, and general lack of efficacy.11
Table
CONTROLLED EVIDENCE* FOR BEHAVIOR-BASED DRUG THERAPY OF AUTISM
| Medication | Behaviors improved | Significant adverse effects | Comments |
|---|---|---|---|
| Risperidone 2 | Aggression, irritability | Mild transient sedation | Conducted in adults |
| Risperidone 3 | Aggression, irritability | Weight gain, increased appetite, sedation, tremor, hypersalivation | Largest controlled study to date in children with autism |
| Clomipramine 11 | Irritability, stereotypy | Tachycardia, tremors, diaphoresis, insomnia, nausea | Conducted in children and adults |
| Fluvoxamine 12 | Aggression, repetitive phenomena | Nausea, sedation | No published controlled pediatric data; unpublished pediatric data unfavorable |
| Clonidine 24 | Hyperactivity, irritability, stereotypies, oppositional behavior, aggression, self-injury | Hypotension, sedation, decreased activity | Small number of subjects |
| Clonidine 25 | Impulsivity, self-stimulation, hyperarousal | Sedation and fatigue | Small number of subjects |
| Methylphenidate 28 | Hyperactivity, irritability | Social withdrawal and irritability | Adverse effects more common at 0.6 mg/kg/dose |
| • Double-blind, placebo-controlled studies | |||
Fluvoxamine. Only one double-blind, placebo-controlled study has examined the use of an SSRI in autistic disorder.12 In this 12-week trial, 30 adults with autism received fluvoxamine, mean 276.7 mg/d, or placebo. Eight of 15 subjects in the fluvoxamine group were categorized as “much improved” or “very much improved” on the CGI.
Fluvoxamine was much more effective than placebo in reducing repetitive thoughts and behavior, aggression, and maladaptive behavior. Adverse effects included minimal sedation and nausea.
Unpublished data of McDougle et al suggest that autistic children and adolescents respond less favorably than adults to fluvoxamine. In a 12-week, double-blind, placebocontrolled trial in patients ages 5 to 18, only 1 of 18 subjects responded to fluvoxamine at a mean dosage of 106.9 mg/d. Agitation, increased aggression, hyperactivity, and increased repetitive behavior were reported.
Fluoxetine. Seven autistic patients ages 9 to 20 were treated with fluoxetine, 20 to 80 mg/d (mean 37.1 mg/d) in an 18-month longitudinal open trial. Irritability, lethargy, and stereotypy improved, as measured by the ABC.13 Adverse effects included increased hyperactivity and transient appetite suppression.
In another open-label trial of 37 autistic children ages 2 to 7, response was rated by investigators as “excellent” in 11 and “good” in another 11 who received fluoxetine, 0.2 to 1.4 mg/kg/d. However, aggression was a frequent cause for drug discontinuation during the 21-month study.14
Sertraline. In an open-label trial, Steingard et al treated nine autistic children ages 6 to 12 with sertraline, 25 to 50 mg/d for 2 to 8 weeks. Clinical improvement was observed in irritability, transition-associated anxiety, and need for sameness in eight of the children.15
Figure 2 BEHAVIOR-BASED DRUG THERAPY FOR POSTPUBERTAL PATIENTS WITH AUTISM
Source: Reprinted with permission from McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, et al (eds). Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2002. Copyright © 2002 by Oxford University Press, Inc.In an open-label trial, 42 adults with pervasive developmental disorders were treated for 12 weeks with sertraline, 50 to 200 mg/d (mean 122 mg/d). Twenty-four (57%) achieved CGI ratings of “much improved” or “very much improved” in aggressive and repetitive behavior.16
Paroxetine. Fifteen adults with profound mental retardation (including seven with pervasive developmental disorders) received paroxetine, 10 to 50 mg/d (mean 35 mg/d) in a 4-month open-label trial. Frequency and severity of aggression were rated as improved after 1 month, but not at 4 months.17
Mirtazapine. In an open-label trial, 26 patients ages 3 to 23 with pervasive developmental disorders were treated with mirtazapine, 7.5 to 45 mg/d (mean 30.3 mg/d). Aggression, self-injury, irritability, hyperactivity, anxiety, depression, and insomnia decreased in 9 patients (34%), as determined by ratings of “much improved” or “very much improved” on the CGI. Adverse effects included increased appetite and transient sedation.18
Mood stabilizers
Lithium. No recent studies of lithium in pervasive developmental disorders are known to exist, but several case reports have been published:
- two reports found lithium decreased manic symptoms in individuals with autism and a family history of bipolar disorder19,20
- one report of lithium augmentation of fluvoxamine in an adult with autistic disorder noted markedly improved aggression and impulsivity after 2 weeks of treatment, as measured by the CGI, Brown Aggression Scale, and Vineland Adaptive Behavior Scale.21
Divalproex. In an open-label trial, 14 subjects ages 5 to 40 with pervasive developmental disorders were given divalproex sodium, 125 to 2,500 mg/d (mean 768 mg/d; mean blood level 75.8 mcg/mL. Affective instability, repetitive behavior, impulsivity, and aggression improved in 10 patients (71%), as measured by CGI ratings of “much improved” or “very much improved.”22 Adverse effects included sedation, weight gain, hair loss, behavioral activation, and elevated liver enzymes.
Lamotrigine. In a 4-week, double-blind, placebo-controlled trial, lamotrigine, 5.0 mg/kg/d, was given to 14 children ages 3 to 11 with autistic disorder.23 Lamotrigine and placebo showed no significant differences in effect, as measured by the ABC, Autism Behavior Checklist, Vineland scales, Childhood Autism Rating Scale, and PreLinguistic Autism Diagnostic Observation Scale. Insomnia and hyperactivity were the most common adverse effects.
α2-adrenergic agonists
Clonidine. Jaselskis et al administered clonidine, 4 to 10 mcg/kg/d, to eight children ages 5 to 13 with autism in a 6-week, double-blind, placebo-controlled, crossover study.24 Symptoms of hyperactivity, irritability, and oppositional behavior improved, as determined by teacher ratings on the ABC, Conners Abbreviated Parent-Teacher Questionnaire, and Attention Deficit Disorder with Hyperactivity Comprehensive Teacher’s Rating Scale. Adverse effects included hypotension, sedation, and decreased activity.
Nine autistic patients ages 5 to 33 received transdermal clonidine, 0.16 to 0.48 mcg/kg/d (mean 3.6 mcg/kg/d), in a 4-week, double-blind, placebo-controlled, crossover study. Hyperarousal, impulsivity, and self-stimulation improved, as measured by the Ritvo-Freeman Real Life Rating Scale and the CGI. Sedation and fatigue were reported, especially during the first 2 weeks of treatment.25
Guanfacine. The effect of guanfacine, 0.25 to 9.0 mg/d (mean 2.6 mg/d), was examined retrospectively in 80 children and adolescents ages 3 to 18 with pervasive developmental disorders.26 Hyperactivity, inattention, and tics improved in the 19 subjects (23.8%) who were rated “much improved” or “very much improved” on the CGI. Sedation was the most frequently reported adverse effect.
Psychostimulants
Early reports showed little benefit from stimulants in pervasive developmental disorders, but more recent studies suggest a modest effect. The RUPP Autism Network is conducting a large controlled investigation of methylphenidate to better understand the role of stimulants in children and adolescents in this diagnostic cluster.
Quintana et al conducted a double-blind, crossover study of methylphenidate, 10 or 20 mg bid for 2 weeks, in 10 children ages 7 to 11 with autism.27 Although irritability and hyperactivity showed statistically significant improvement as determined by the ABC and Conners Teacher Questionnaire, the authors reported only modest clinical effects. More recently, use of methylphenidate, 0.3 and 0.6 mg/kg/dose, was associated with a 50% decrease on the Connors Hyperactivity Index in 8 of 13 autistic children ages 5 to 11.28 Adverse effects—most common with the 0.6 mg/kg/dose—included social withdrawal and irritability in this double-blind, placebo-controlled, crossover study.
Related resources
- McDougle CJ, Posey DJ. Autistic and other pervasive developmental disorders. In: Martin A, Scahill L, Charney DS, Leckman JF (eds). Pediatric psychopharmacology: Principles and practice. New York: Oxford University Press, 2002.
- Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins, 2002.
- National Institute of Mental Health. Autism booklet. www.nimh.nih.gov/publicat/autism.cfm
- Autism Society of America. www.autism-society.org
Drug brand names
- Clomipramine • Anafranil
- Clonidine • Catapres
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Guanfacine • Tenex
- Lamotrigine • Lamictal
- Lithium • Eskalith
- Methylphenidate • Ritalin
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Ziprasidone • Geodon
Disclosure
Dr. Stigler reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Posey receives grant support from and is a consultant to Eli Lilly & Co.
Dr. McDougle receives grant support from and is a consultant to Pfizer Inc., Eli Lilly & Co., and Janssen Pharmaceutica, and is a speaker for Pfizer Inc. and Janssen Pharmaceutica.
Acknowledgments
This work was supported in part by a Daniel X. Freedman Psychiatric Research Fellowship Award (Dr. Posey), a National Alliance for Research in Schizophrenia and Depression Young Investigator Award (Dr. Posey), a Research Unit on Pediatric Psychopharmacology contract (N01MH70001) from the National Institute of Mental Health to Indiana University (Drs. McDougle and Posey), a National Institutes of Health Clinical Research Center grant to Indiana University (M01-RR00750), and a Department of Housing and Urban Development grant (B-01-SP-IN-0200).
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: American Psychiatric Association, 2000.
2. McDougle CJ, Holmes JP, Carlson DC, Pelton GH, Cohen DJ, Price LH. A double-blind placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Arch Gen Psychiatry 1998;55:633-41.
3. Research Units on Pediatric Psychopharmacology Autism Network. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
4. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: An open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
5. Malone RP, Cater J, Sheikh RM, Choudhury MS, Delaney MA. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
6. Martin A, Koenig K, Scahill L, Bregman J. Open-label quetiapine in the treatment of children and adolescents with autistic disorder. J Child Adolesc Psychopharmacol 1999;9:99-107.
7. McDougle CJ, Kem DL, Posey DJ. Case series: use of ziprasidone for maladaptive symptoms in youths with autism. J Am Acad Child Adolesc Psychiatry 2002;41(8):921-7.
8. Zuddas A, Ledda MG, Fratta A, Muglia P, Cianchetti C. Clinical effects of clozapine on autistic disorder. Am J Psychiatry 1996;153(5):738.-
9. Chen NC, Bedair HS, McKay B, Bowers MB, Mazure C. Clozapine in the treatment of aggression in an adolescent with autistic disorder. J Clin Psychiatry 2001;62(6):479-80.
10. Gobbi G, Pulvirenti L. Long-term treatment with clozapine in an adult with autistic disorder accompanied by aggressive behaviour. J Psych Neurol 2001;26(4):340-1.
11. Remington G, Sloman L, Konstantareas M, Parker K, Gow R. Clomipramine versus haloperidol in the treatment of autistic disorder: A double-blind, placebo-controlled, crossover study. J Clin Psychopharmacol 2001;21(4):440-4.
12. McDougle CJ, Naylor ST, Cohen DJ, Volkmar FR, Heninger GR, Price LH. A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Arch Gen Psychiatry 1996;53:1001-8.
13. Fatemi SH, Realmuto GM, Khan L, Thuras P. Fluoxetine in treatment of adolescent patients with autism: a longitudinal open trial. J Autism Dev Disord 1998;28(4):303-7.
14. DeLong GR, Teague LA, Kamran MM. Effects of fluoxetine treatment in young children with idiopathic autism. Dev Med Child Neurol 1998;40:551-62.
15. Steingard RJ, Zimnitzky B, DeMaso DR, Bauman ML, Bucci JP. Sertraline treatment of transition-associated anxiety and agitation in children with autistic disorder. J Child Adolesc Psychopharmacol 1997;7(1):9-15.
16. McDougle CJ, Brodkin ES, Naylor ST, Carlson DC, Cohen DJ, Price LH. Sertraline in adults with pervasive developmental disorders: a prospective open-label investigation. J Clin Psychopharmacol 1998;18:62-6.
17. Davanzo PA, Belin TR, Widawski MH, King BH. Paroxetine treatment of aggression and self-injury in persons with mental retardation. Am J Ment Retard 1998;102(5):427-37.
18. Posey DJ, Guenin KD, Kohn AE, Swiezy NB, McDougle CJ. A naturalistic open-label study of mirtazapine in autistic and other pervasive developmental disorders. J Child Adolesc Psychopharmacol 2001;11(3):267-77.
19. Kerbeshian J, Burd L, Fisher W. Lithium carbonate in the treatment of two patients with infantile autism and atypical bipolar symptomatology. J Clin Psychopharmacol 1987;7(6):401-5.
20. Steingard R, Biederman J. Lithium-responsive manic-like symptoms in two individuals with autism and mental retardation. J Am Acad Child Adolesc Psychiatry 1987;26:932-5.
21. Epperson CN, McDougle CJ, Anand A, et al. Lithium augmentation of fluvoxamine in autistic disorder: a case report. J Child Adolesc Psychopharmacol 1994;4:201-7.
22. Hollander E, Dolgoff-Kaspar R, Cartwright C, Rawitt R, Novotny S. An open trial of divalproex sodium in autism spectrum disorders. J Clin Psychiatry 2001;62(7):530-4.
23. Belsito KM, Law PA, Kirk KS, Landa RJ, Zimmerman AW. Lamotrigine therapy for autistic disorder: a randomized, double-blind, placebo-controlled trial. J Autism Dev Disord 2001;31(2):175-81.
24. Jaselskis CA, Cook EH, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
25. Fankhauser MP, Karumanchi VC, German ML, Yates A, Karumanchi SD. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
26. Posey DJ, Decker J, Sasher TM, Kohburn A, Swiezy NB, McDougle CJ. A retrospective analysis of guanfacine in the treatment of autism. New Orleans: American Psychiatric Association annual meeting, 2001; new research abstracts no. 816.
27. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-95.
28. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
1. American Psychiatric Association Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: American Psychiatric Association, 2000.
2. McDougle CJ, Holmes JP, Carlson DC, Pelton GH, Cohen DJ, Price LH. A double-blind placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Arch Gen Psychiatry 1998;55:633-41.
3. Research Units on Pediatric Psychopharmacology Autism Network. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347(5):314-21.
4. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: An open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
5. Malone RP, Cater J, Sheikh RM, Choudhury MS, Delaney MA. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40(8):887-94.
6. Martin A, Koenig K, Scahill L, Bregman J. Open-label quetiapine in the treatment of children and adolescents with autistic disorder. J Child Adolesc Psychopharmacol 1999;9:99-107.
7. McDougle CJ, Kem DL, Posey DJ. Case series: use of ziprasidone for maladaptive symptoms in youths with autism. J Am Acad Child Adolesc Psychiatry 2002;41(8):921-7.
8. Zuddas A, Ledda MG, Fratta A, Muglia P, Cianchetti C. Clinical effects of clozapine on autistic disorder. Am J Psychiatry 1996;153(5):738.-
9. Chen NC, Bedair HS, McKay B, Bowers MB, Mazure C. Clozapine in the treatment of aggression in an adolescent with autistic disorder. J Clin Psychiatry 2001;62(6):479-80.
10. Gobbi G, Pulvirenti L. Long-term treatment with clozapine in an adult with autistic disorder accompanied by aggressive behaviour. J Psych Neurol 2001;26(4):340-1.
11. Remington G, Sloman L, Konstantareas M, Parker K, Gow R. Clomipramine versus haloperidol in the treatment of autistic disorder: A double-blind, placebo-controlled, crossover study. J Clin Psychopharmacol 2001;21(4):440-4.
12. McDougle CJ, Naylor ST, Cohen DJ, Volkmar FR, Heninger GR, Price LH. A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Arch Gen Psychiatry 1996;53:1001-8.
13. Fatemi SH, Realmuto GM, Khan L, Thuras P. Fluoxetine in treatment of adolescent patients with autism: a longitudinal open trial. J Autism Dev Disord 1998;28(4):303-7.
14. DeLong GR, Teague LA, Kamran MM. Effects of fluoxetine treatment in young children with idiopathic autism. Dev Med Child Neurol 1998;40:551-62.
15. Steingard RJ, Zimnitzky B, DeMaso DR, Bauman ML, Bucci JP. Sertraline treatment of transition-associated anxiety and agitation in children with autistic disorder. J Child Adolesc Psychopharmacol 1997;7(1):9-15.
16. McDougle CJ, Brodkin ES, Naylor ST, Carlson DC, Cohen DJ, Price LH. Sertraline in adults with pervasive developmental disorders: a prospective open-label investigation. J Clin Psychopharmacol 1998;18:62-6.
17. Davanzo PA, Belin TR, Widawski MH, King BH. Paroxetine treatment of aggression and self-injury in persons with mental retardation. Am J Ment Retard 1998;102(5):427-37.
18. Posey DJ, Guenin KD, Kohn AE, Swiezy NB, McDougle CJ. A naturalistic open-label study of mirtazapine in autistic and other pervasive developmental disorders. J Child Adolesc Psychopharmacol 2001;11(3):267-77.
19. Kerbeshian J, Burd L, Fisher W. Lithium carbonate in the treatment of two patients with infantile autism and atypical bipolar symptomatology. J Clin Psychopharmacol 1987;7(6):401-5.
20. Steingard R, Biederman J. Lithium-responsive manic-like symptoms in two individuals with autism and mental retardation. J Am Acad Child Adolesc Psychiatry 1987;26:932-5.
21. Epperson CN, McDougle CJ, Anand A, et al. Lithium augmentation of fluvoxamine in autistic disorder: a case report. J Child Adolesc Psychopharmacol 1994;4:201-7.
22. Hollander E, Dolgoff-Kaspar R, Cartwright C, Rawitt R, Novotny S. An open trial of divalproex sodium in autism spectrum disorders. J Clin Psychiatry 2001;62(7):530-4.
23. Belsito KM, Law PA, Kirk KS, Landa RJ, Zimmerman AW. Lamotrigine therapy for autistic disorder: a randomized, double-blind, placebo-controlled trial. J Autism Dev Disord 2001;31(2):175-81.
24. Jaselskis CA, Cook EH, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. J Clin Psychopharmacol 1992;12(5):322-7.
25. Fankhauser MP, Karumanchi VC, German ML, Yates A, Karumanchi SD. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992;53(3):77-82.
26. Posey DJ, Decker J, Sasher TM, Kohburn A, Swiezy NB, McDougle CJ. A retrospective analysis of guanfacine in the treatment of autism. New Orleans: American Psychiatric Association annual meeting, 2001; new research abstracts no. 816.
27. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995;25(3):283-95.
28. Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J Autism Dev Disord 2000;30(3):245-55.
UPDATE ON ATYPICALS: Preemptive tactics to reduce weight gain
Given the efficacy and safety profiles of atypical antipsychotics, their potential to cause weight gain represents not a barrier to access but a side effect to be managed. Behavioral and/or drug interventions can help protect patients from the medical risks and social consequences of weight gain during antipsychotic treatment.
Let’s look at possible mechanisms of antipsychotic-induced weight gain and a rational strategy for controlling weight in patients taking these medications. This strategy applies to all atypical antipsychotics and psychiatric diagnoses.
Mechanisms of weight gain
Neuroleptic antipsychotics may act on the hypothalamic feeding center and directly stimulate appetite, a dynamic that was suggested 20 years ago.1 More recent evidence suggests that antagonism of serotonin (5-HT2C) or histamine (H1) receptors may play a role in antipsychotic-related weight gain. Other neurotransmitters and receptors may also be involved.
Serotonin receptor antagonism. Agents that stimulate 5-HT2C receptors—such as fenfluramine and M-chlorophenylpiperazine2 —have been associated with weight loss. Conversely, agents that antagonize these receptors have been hypothesized to increase appetite and cause weight gain.3
For example, a strain of mice craved carbohydrates and became obese after the genes for 5-HT2C receptors were removed.4 Atypical antipsychotics also antagonize 5-HT2C receptors more than the older neuroleptics do, which may explain the atypicals’ greater associated risk for weight gain.
Histamine receptor antagonism. Other researchers have suggested that antipsychotic-induced weight gain is associated less with serotonin receptors than with histamine receptor antagonism:
- Astemizole—a potent H1 receptor antagonist used to treat allergic rhinitis—was the first medication associated with weight gain by this mechanism.5
- Wirshing et al6 recently reported an exponential relationship between antipsychotics’ H1 receptor affinities and maximum weight gain.
Clozapine and olanzapine have very strong binding affinity to both 5-HT2C and H1 receptors. This characteristic may explain why patients often experience increased appetite and weight gain while taking these antipsychotics.
Other neurotransmitters. Atypical antipsychotics have diverse pharmacologic profiles, and their interactions with dopamine and other neurotransmitter receptors produce a variety of effects (Table 1). These neurotransmitter systems and receptor subtypes appear to help regulate food intake and energy homeostasis and may play a role in weight gain associated with antipsychotic use.7 For example:
- Clozapine and olanzapine have a higher affinity for serotonin receptor subtypes 5-HT2A and 5-HT2C and for H1 and muscarinic (M1) receptors than they do for D2 receptors. This preferential antagonism of 5-HT2A versus D2 receptors is a defining characteristic of novel antipsychotics and explains why they offer broader efficacy and fewer side effects than the older neuroleptics. However, 5-HT2C receptor antagonism has been implicated as a cause of increased appetite.4
- Clozapine, but not olanzapine, also has a higher affinity for adrenergic (1) receptors than for D2 receptors. Clozapine is associated with greater mean weight gain than olanzapine, risperidone, or ziprasidone.8
- Risperidone—with a lower weight gain potential than most atypicals—displays high affinity for 5-HT2A and 1 receptors and a lower affinity for 5-HT2C receptors than for D2 receptors.8
- Ziprasidone’s weight gain potential is even less than risperidone’s, and the exact mechanism is unknown.8 Some animal studies suggest that ziprasidone’s effects on the noradrenergic system may explain its low weight gain potential.9
- Aripiprazole’s long-term weight gain potential is not yet known.
Table 1
RECEPTOR BINDING AFFINITIES OF ATYPICAL ANTIPSYCHOTICS
| Drug | Dopamine | Serotonin | ∂1 adrenergic | Histamine | Muscarinic | |
|---|---|---|---|---|---|---|
| D2 | 5HT2A | 5HT2C | H1 | M1 | ||
| Clozapine | + | ++++ | +++ | +++ | ++ | |
| Olanzapine | ++ | ++++ | ++++ | − | ++ | − |
| Quetiapine | + | + | + | +++ | ++ | − |
| Risperidone | ++++ | +++++ | ++ | + | +++ | − |
| Ziprasidone | ++++ | +++++ | + | 0 | ++ | − |
A strategy for managing weight gain
Four predictors of weight gain have been identified in patients with schizophrenia:
- better clinical outcome
- low baseline body mass index
- younger age
- increase in appetite during treatment.10
When appetite increases, patients are at risk of overeating to satisfy their hunger. An average increase of 500 calories per day will cause an average weight gain of 1 lb per week. Therefore, minimizing an increase in caloric intake may minimize weight gain.
One can lose weight by reducing caloric intake or increasing caloric output, such as with exercise. Thus, behavioral interventions focusing on both nutritional education and exercise are showing benefit in minimizing antipsychotic-related weight gain. The “wellness clinic” described by Wirshing et al achieved weight loss in patients taking antipsychotics through rigorous interventions, including education, exercise classes, and group support.6
A rational approach for minimizing weight gain in patients taking antipsychotics is summarized in Table 2. This strategy combines nutritional and exercise education and drug therapy, when indicated.
Effect of behavioral interventions
Many patients who have followed behavioral interventions that emphasize nutrition and exercise have lost at least some of the weight they gained during antipsychotic treatment:
- In a study by O’Keefe, nearly 80% of patients who gained >20 lbs while taking antipsychotics then lost at least 10 lbs while in behavioral intervention programs.11
- Patients with schizophrenia or schizoaffective disorder who experienced olanzapine-related weight gain lost weight while attending a 10-week Weight Watchers program.12
- Patients who gained weight while taking antipsychotics lost weight with a step-wise behavioral approach that included increasingly intensive interventions (self-weighing, food diaries, nutrition consultation, and attendance at a “wellness clinic”).6
- 70% of 74 psychiatric inpatients lost weight across 6 to 34 months with a reduced-calorie diet, group therapy, and behavior modification.13
The effectiveness of weight management programs associated with antipsychotics may depend on the target population. In a retrospective chart review, Cohen et al found that calorie restriction did not lead to weight loss among 50 adult inpatients with mental retardation who were being treated with risperidone.14
Timing is important. During olanzapine treatment, mean weight gain has been reported to plateau after approximately 39 weeks, with the most rapid gains in the first 12 weeks.6 Thus, early weight control efforts likely would be most effective. Two small, prospective studies suggest that starting behavioral interventions before you start olanzapine therapy may be the most effective strategy to minimize weight gain.
In the first study—a randomized trial of 12 patients with schizophrenia—those who received an educational intervention prior to starting olanzapine treatment gained a mean 1 lb in 4 weeks, compared with 6.4 lbs in a standard-care group.15 The behavioral intervention included a weekly 1-hour class using educational materials on nutrition and exercise.
In the second study, our group offered 22 psychiatric outpatients a nutrition course before starting olanzapine treatment.16 We included 17 patients with psychotic disorders and 5 with nonpsychotic diagnoses—including major depressive disorder, bipolar disorder, and stuttering—to compare antipsychotic-related weight gain between psychotic and nonpsychotic populations.
We began by talking with each patient for 5 minutes about the following nutritional concepts:
- Weight gain is associated with increased appetite.
- The more you eat, the more weight you gain.
- To reduce hunger, it is better to snack on fruits, carrots, broccoli, or low-fat crackers than on high-calorie “junk food” such as potato chips, ice cream, candy, and cake.
- Drink water or diet sodas instead of sugary soft drinks.
At follow-up visits, we spent 2 minutes reinforcing the educational messages by:
- asking if patients’ appetite had increased
- re-emphasizing that they should eat low-fat snacks to reduce hunger and drink water or diet sodas instead of sugary soft drinks.
After about 7 months, the mean weight gain from olanzapine therapy was 5.27 lbs, which is 40 to 60% less than that seen in studies of olanzapine without structured interventions.6,8,17 Mean weight gain was 5 lbs for the psychotic patients and 6.2 lbs for the nonpsychotic group, which suggested that patients with schizophrenia or schizoaffective disorders may benefit from nutritional education.
Table 2
STRATEGY FOR MANAGING WEIGHT IN PATIENTS TAKING ANTIPSYCHOTICS
|
Medications for weight control
Three medications—nizatidine, topiramate, and amantadine—have shown some effect in controlling weight gain when taken concomitantly with atypical antipsychotics. These medications affect different receptors, and how they affect weight gain is not entirely understood.
Nizatidine—a selective histamine (H2) receptor antagonist—was shown to be significantly more effective than placebo in reducing olanzapine-related weight gain when given to 132 patients at 300 mg bid.18
Topiramate is believed to stimulate 5-HT2C receptors, thus suppressing the increased appetite caused by 5-HT2C antagonism. Among 13 bipolar patients with significant weight gain associated with olanzapine treatment, 73% lost weight with topiramate at 90.4 +/- 48.4 mg/d.18
Amantadine has also been shown to minimize weight gain without worsening psychotic symptoms. A case series reported a weight gain of 15.8 lbs in patients taking olanzapine alone, compared with 7.7 lbs in patients taking olanzapine plus amantadine.19
Related resources
- Wirshing DA, Wirshing WC, Ksyar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry 1999;60:358-63.
- Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry 2001;62 (suppl 7):4-10.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
Dr. Nguyen is a speaker for Eli Lilly and Co. and GlaxoSmithKline; receives research support from Eli Lilly and Co., GlaxoSmithKline, and Forest Laboratories; and is a consultant to Eli Lilly and Co., Organon, and GlaxoSmithKline.
Dr. Yu is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.; receives research/grant support from Cephalon, Inc. and Eli Lilly and Co.; and is a consultant to Eli Lilly and Co.
Dr. Maguire receives research support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
Acknowledgment
The authors wish to thank David Franklin, MS, neuroscientist; Chris Gordon, MD, resident; and Sam Truong, senior undergraduate student, University of California, Irvine, as well as Leanne Stoneking, MS, fourth-year medical student, Creighton University Medical School, for their assistance in preparing this manuscript.
1. Rockwell WJ, Ellinwood EH, Trader DW. Psychotropic drugs promoting weight gain: health risk and treatment implications. South Med J. 1983;76:1407-12.
2. Walsh AE, Smith KA, Oldman AD, et al. m-Chlorophenylpiperazine decreases food intake in a test meal. Psychopharmacology (Berl). 1994;116:120-2.
3. Garattini S, Mennini T, Samain R. Reduction of food intake by manipulation of central serotonin: current experimental results. Br J Psychiatry. 1989;155(suppl 8):41-51.
4. Tecott LH, Sun LM, Akana SF, et al. Eating disorder and epilepsy in mice lacking 5-HT2C receptors. Nature. 1995;374:542-6.
5. Howarth PH, Emanuel MB, Holgate ST. Astemizole, a potent histamine H1 receptor antagonist: effect on allergic rhinoconjunctivitis, on antigen and histamine-induced skin response and relationship to serum levels. Br J Clin Pharmacol. 1984;18:1-8.
6. Wirshing DA, Wirshing WC, Kysar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry. 1999;60:358-63.
7. Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry. 2001;62 (suppl 7):4-10.
8. Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156:1686-96.
9. Leibowitz SF. Neurochemical system of the hypothalamus control of eating and drinking and behavior and water-electrolyte excretion. In: Morgan P, Panksepp J (eds). Handbook of the hypothalamus (vol, 3). New York: Marcel Dekker, Inc., 1980;299-438.
10. Basson BR, Kinon BJ, Taylor CC, et al. Factors influencing acute weight change in patients with schizophrenia treated with olanzapine, haloperidol, or risperidone. J Clin Psychiatry. 2001;62(4):231-8.
11. O’Keefe C, et al. Reversal of weight gain associated with antipsychotic treatment (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
12. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv. 2001;52(7):967-9.
13. Knox JM. A study of weight reducing diets in psychiatric in-patients. Br J Psychiatry. 1980;136:287-9.
14. Cohen S, Glazewski R, Khan S, Khan A. Weight gain with risperidone among patients with mental retardation: effect of calorie restriction. J Clin Psychiatry. 2001;62(2):114-16.
15. Littrell KH, et al. Educational interventions for the management of antipsychotic-related weight gain (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
16. Nguyen CT, Ortiz T, Franklin D, Yu B, Maguire GA. Nutritional education in minimizing weight gain associated with antipsychotic therapy. New Orleans: American Psychiatric Association annual meeting, 2001.
17. Kinon BJ, Basson BR, Gilmore JA, Tollefson GD. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62(2):92-100.
18. Ketter TA, et al. Int J Neuropsychopharmacol. 2000;3(suppl l):S344.-
19. Floris M, Lejeune J, Deberdt W. Effect of amantadine on weight gain during olanzapine treatment. Eur Neuropsychopharmacol. 2001;11(2):181-2.
Given the efficacy and safety profiles of atypical antipsychotics, their potential to cause weight gain represents not a barrier to access but a side effect to be managed. Behavioral and/or drug interventions can help protect patients from the medical risks and social consequences of weight gain during antipsychotic treatment.
Let’s look at possible mechanisms of antipsychotic-induced weight gain and a rational strategy for controlling weight in patients taking these medications. This strategy applies to all atypical antipsychotics and psychiatric diagnoses.
Mechanisms of weight gain
Neuroleptic antipsychotics may act on the hypothalamic feeding center and directly stimulate appetite, a dynamic that was suggested 20 years ago.1 More recent evidence suggests that antagonism of serotonin (5-HT2C) or histamine (H1) receptors may play a role in antipsychotic-related weight gain. Other neurotransmitters and receptors may also be involved.
Serotonin receptor antagonism. Agents that stimulate 5-HT2C receptors—such as fenfluramine and M-chlorophenylpiperazine2 —have been associated with weight loss. Conversely, agents that antagonize these receptors have been hypothesized to increase appetite and cause weight gain.3
For example, a strain of mice craved carbohydrates and became obese after the genes for 5-HT2C receptors were removed.4 Atypical antipsychotics also antagonize 5-HT2C receptors more than the older neuroleptics do, which may explain the atypicals’ greater associated risk for weight gain.
Histamine receptor antagonism. Other researchers have suggested that antipsychotic-induced weight gain is associated less with serotonin receptors than with histamine receptor antagonism:
- Astemizole—a potent H1 receptor antagonist used to treat allergic rhinitis—was the first medication associated with weight gain by this mechanism.5
- Wirshing et al6 recently reported an exponential relationship between antipsychotics’ H1 receptor affinities and maximum weight gain.
Clozapine and olanzapine have very strong binding affinity to both 5-HT2C and H1 receptors. This characteristic may explain why patients often experience increased appetite and weight gain while taking these antipsychotics.
Other neurotransmitters. Atypical antipsychotics have diverse pharmacologic profiles, and their interactions with dopamine and other neurotransmitter receptors produce a variety of effects (Table 1). These neurotransmitter systems and receptor subtypes appear to help regulate food intake and energy homeostasis and may play a role in weight gain associated with antipsychotic use.7 For example:
- Clozapine and olanzapine have a higher affinity for serotonin receptor subtypes 5-HT2A and 5-HT2C and for H1 and muscarinic (M1) receptors than they do for D2 receptors. This preferential antagonism of 5-HT2A versus D2 receptors is a defining characteristic of novel antipsychotics and explains why they offer broader efficacy and fewer side effects than the older neuroleptics. However, 5-HT2C receptor antagonism has been implicated as a cause of increased appetite.4
- Clozapine, but not olanzapine, also has a higher affinity for adrenergic (1) receptors than for D2 receptors. Clozapine is associated with greater mean weight gain than olanzapine, risperidone, or ziprasidone.8
- Risperidone—with a lower weight gain potential than most atypicals—displays high affinity for 5-HT2A and 1 receptors and a lower affinity for 5-HT2C receptors than for D2 receptors.8
- Ziprasidone’s weight gain potential is even less than risperidone’s, and the exact mechanism is unknown.8 Some animal studies suggest that ziprasidone’s effects on the noradrenergic system may explain its low weight gain potential.9
- Aripiprazole’s long-term weight gain potential is not yet known.
Table 1
RECEPTOR BINDING AFFINITIES OF ATYPICAL ANTIPSYCHOTICS
| Drug | Dopamine | Serotonin | ∂1 adrenergic | Histamine | Muscarinic | |
|---|---|---|---|---|---|---|
| D2 | 5HT2A | 5HT2C | H1 | M1 | ||
| Clozapine | + | ++++ | +++ | +++ | ++ | |
| Olanzapine | ++ | ++++ | ++++ | − | ++ | − |
| Quetiapine | + | + | + | +++ | ++ | − |
| Risperidone | ++++ | +++++ | ++ | + | +++ | − |
| Ziprasidone | ++++ | +++++ | + | 0 | ++ | − |
A strategy for managing weight gain
Four predictors of weight gain have been identified in patients with schizophrenia:
- better clinical outcome
- low baseline body mass index
- younger age
- increase in appetite during treatment.10
When appetite increases, patients are at risk of overeating to satisfy their hunger. An average increase of 500 calories per day will cause an average weight gain of 1 lb per week. Therefore, minimizing an increase in caloric intake may minimize weight gain.
One can lose weight by reducing caloric intake or increasing caloric output, such as with exercise. Thus, behavioral interventions focusing on both nutritional education and exercise are showing benefit in minimizing antipsychotic-related weight gain. The “wellness clinic” described by Wirshing et al achieved weight loss in patients taking antipsychotics through rigorous interventions, including education, exercise classes, and group support.6
A rational approach for minimizing weight gain in patients taking antipsychotics is summarized in Table 2. This strategy combines nutritional and exercise education and drug therapy, when indicated.
Effect of behavioral interventions
Many patients who have followed behavioral interventions that emphasize nutrition and exercise have lost at least some of the weight they gained during antipsychotic treatment:
- In a study by O’Keefe, nearly 80% of patients who gained >20 lbs while taking antipsychotics then lost at least 10 lbs while in behavioral intervention programs.11
- Patients with schizophrenia or schizoaffective disorder who experienced olanzapine-related weight gain lost weight while attending a 10-week Weight Watchers program.12
- Patients who gained weight while taking antipsychotics lost weight with a step-wise behavioral approach that included increasingly intensive interventions (self-weighing, food diaries, nutrition consultation, and attendance at a “wellness clinic”).6
- 70% of 74 psychiatric inpatients lost weight across 6 to 34 months with a reduced-calorie diet, group therapy, and behavior modification.13
The effectiveness of weight management programs associated with antipsychotics may depend on the target population. In a retrospective chart review, Cohen et al found that calorie restriction did not lead to weight loss among 50 adult inpatients with mental retardation who were being treated with risperidone.14
Timing is important. During olanzapine treatment, mean weight gain has been reported to plateau after approximately 39 weeks, with the most rapid gains in the first 12 weeks.6 Thus, early weight control efforts likely would be most effective. Two small, prospective studies suggest that starting behavioral interventions before you start olanzapine therapy may be the most effective strategy to minimize weight gain.
In the first study—a randomized trial of 12 patients with schizophrenia—those who received an educational intervention prior to starting olanzapine treatment gained a mean 1 lb in 4 weeks, compared with 6.4 lbs in a standard-care group.15 The behavioral intervention included a weekly 1-hour class using educational materials on nutrition and exercise.
In the second study, our group offered 22 psychiatric outpatients a nutrition course before starting olanzapine treatment.16 We included 17 patients with psychotic disorders and 5 with nonpsychotic diagnoses—including major depressive disorder, bipolar disorder, and stuttering—to compare antipsychotic-related weight gain between psychotic and nonpsychotic populations.
We began by talking with each patient for 5 minutes about the following nutritional concepts:
- Weight gain is associated with increased appetite.
- The more you eat, the more weight you gain.
- To reduce hunger, it is better to snack on fruits, carrots, broccoli, or low-fat crackers than on high-calorie “junk food” such as potato chips, ice cream, candy, and cake.
- Drink water or diet sodas instead of sugary soft drinks.
At follow-up visits, we spent 2 minutes reinforcing the educational messages by:
- asking if patients’ appetite had increased
- re-emphasizing that they should eat low-fat snacks to reduce hunger and drink water or diet sodas instead of sugary soft drinks.
After about 7 months, the mean weight gain from olanzapine therapy was 5.27 lbs, which is 40 to 60% less than that seen in studies of olanzapine without structured interventions.6,8,17 Mean weight gain was 5 lbs for the psychotic patients and 6.2 lbs for the nonpsychotic group, which suggested that patients with schizophrenia or schizoaffective disorders may benefit from nutritional education.
Table 2
STRATEGY FOR MANAGING WEIGHT IN PATIENTS TAKING ANTIPSYCHOTICS
|
Medications for weight control
Three medications—nizatidine, topiramate, and amantadine—have shown some effect in controlling weight gain when taken concomitantly with atypical antipsychotics. These medications affect different receptors, and how they affect weight gain is not entirely understood.
Nizatidine—a selective histamine (H2) receptor antagonist—was shown to be significantly more effective than placebo in reducing olanzapine-related weight gain when given to 132 patients at 300 mg bid.18
Topiramate is believed to stimulate 5-HT2C receptors, thus suppressing the increased appetite caused by 5-HT2C antagonism. Among 13 bipolar patients with significant weight gain associated with olanzapine treatment, 73% lost weight with topiramate at 90.4 +/- 48.4 mg/d.18
Amantadine has also been shown to minimize weight gain without worsening psychotic symptoms. A case series reported a weight gain of 15.8 lbs in patients taking olanzapine alone, compared with 7.7 lbs in patients taking olanzapine plus amantadine.19
Related resources
- Wirshing DA, Wirshing WC, Ksyar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry 1999;60:358-63.
- Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry 2001;62 (suppl 7):4-10.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
Dr. Nguyen is a speaker for Eli Lilly and Co. and GlaxoSmithKline; receives research support from Eli Lilly and Co., GlaxoSmithKline, and Forest Laboratories; and is a consultant to Eli Lilly and Co., Organon, and GlaxoSmithKline.
Dr. Yu is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.; receives research/grant support from Cephalon, Inc. and Eli Lilly and Co.; and is a consultant to Eli Lilly and Co.
Dr. Maguire receives research support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
Acknowledgment
The authors wish to thank David Franklin, MS, neuroscientist; Chris Gordon, MD, resident; and Sam Truong, senior undergraduate student, University of California, Irvine, as well as Leanne Stoneking, MS, fourth-year medical student, Creighton University Medical School, for their assistance in preparing this manuscript.
Given the efficacy and safety profiles of atypical antipsychotics, their potential to cause weight gain represents not a barrier to access but a side effect to be managed. Behavioral and/or drug interventions can help protect patients from the medical risks and social consequences of weight gain during antipsychotic treatment.
Let’s look at possible mechanisms of antipsychotic-induced weight gain and a rational strategy for controlling weight in patients taking these medications. This strategy applies to all atypical antipsychotics and psychiatric diagnoses.
Mechanisms of weight gain
Neuroleptic antipsychotics may act on the hypothalamic feeding center and directly stimulate appetite, a dynamic that was suggested 20 years ago.1 More recent evidence suggests that antagonism of serotonin (5-HT2C) or histamine (H1) receptors may play a role in antipsychotic-related weight gain. Other neurotransmitters and receptors may also be involved.
Serotonin receptor antagonism. Agents that stimulate 5-HT2C receptors—such as fenfluramine and M-chlorophenylpiperazine2 —have been associated with weight loss. Conversely, agents that antagonize these receptors have been hypothesized to increase appetite and cause weight gain.3
For example, a strain of mice craved carbohydrates and became obese after the genes for 5-HT2C receptors were removed.4 Atypical antipsychotics also antagonize 5-HT2C receptors more than the older neuroleptics do, which may explain the atypicals’ greater associated risk for weight gain.
Histamine receptor antagonism. Other researchers have suggested that antipsychotic-induced weight gain is associated less with serotonin receptors than with histamine receptor antagonism:
- Astemizole—a potent H1 receptor antagonist used to treat allergic rhinitis—was the first medication associated with weight gain by this mechanism.5
- Wirshing et al6 recently reported an exponential relationship between antipsychotics’ H1 receptor affinities and maximum weight gain.
Clozapine and olanzapine have very strong binding affinity to both 5-HT2C and H1 receptors. This characteristic may explain why patients often experience increased appetite and weight gain while taking these antipsychotics.
Other neurotransmitters. Atypical antipsychotics have diverse pharmacologic profiles, and their interactions with dopamine and other neurotransmitter receptors produce a variety of effects (Table 1). These neurotransmitter systems and receptor subtypes appear to help regulate food intake and energy homeostasis and may play a role in weight gain associated with antipsychotic use.7 For example:
- Clozapine and olanzapine have a higher affinity for serotonin receptor subtypes 5-HT2A and 5-HT2C and for H1 and muscarinic (M1) receptors than they do for D2 receptors. This preferential antagonism of 5-HT2A versus D2 receptors is a defining characteristic of novel antipsychotics and explains why they offer broader efficacy and fewer side effects than the older neuroleptics. However, 5-HT2C receptor antagonism has been implicated as a cause of increased appetite.4
- Clozapine, but not olanzapine, also has a higher affinity for adrenergic (1) receptors than for D2 receptors. Clozapine is associated with greater mean weight gain than olanzapine, risperidone, or ziprasidone.8
- Risperidone—with a lower weight gain potential than most atypicals—displays high affinity for 5-HT2A and 1 receptors and a lower affinity for 5-HT2C receptors than for D2 receptors.8
- Ziprasidone’s weight gain potential is even less than risperidone’s, and the exact mechanism is unknown.8 Some animal studies suggest that ziprasidone’s effects on the noradrenergic system may explain its low weight gain potential.9
- Aripiprazole’s long-term weight gain potential is not yet known.
Table 1
RECEPTOR BINDING AFFINITIES OF ATYPICAL ANTIPSYCHOTICS
| Drug | Dopamine | Serotonin | ∂1 adrenergic | Histamine | Muscarinic | |
|---|---|---|---|---|---|---|
| D2 | 5HT2A | 5HT2C | H1 | M1 | ||
| Clozapine | + | ++++ | +++ | +++ | ++ | |
| Olanzapine | ++ | ++++ | ++++ | − | ++ | − |
| Quetiapine | + | + | + | +++ | ++ | − |
| Risperidone | ++++ | +++++ | ++ | + | +++ | − |
| Ziprasidone | ++++ | +++++ | + | 0 | ++ | − |
A strategy for managing weight gain
Four predictors of weight gain have been identified in patients with schizophrenia:
- better clinical outcome
- low baseline body mass index
- younger age
- increase in appetite during treatment.10
When appetite increases, patients are at risk of overeating to satisfy their hunger. An average increase of 500 calories per day will cause an average weight gain of 1 lb per week. Therefore, minimizing an increase in caloric intake may minimize weight gain.
One can lose weight by reducing caloric intake or increasing caloric output, such as with exercise. Thus, behavioral interventions focusing on both nutritional education and exercise are showing benefit in minimizing antipsychotic-related weight gain. The “wellness clinic” described by Wirshing et al achieved weight loss in patients taking antipsychotics through rigorous interventions, including education, exercise classes, and group support.6
A rational approach for minimizing weight gain in patients taking antipsychotics is summarized in Table 2. This strategy combines nutritional and exercise education and drug therapy, when indicated.
Effect of behavioral interventions
Many patients who have followed behavioral interventions that emphasize nutrition and exercise have lost at least some of the weight they gained during antipsychotic treatment:
- In a study by O’Keefe, nearly 80% of patients who gained >20 lbs while taking antipsychotics then lost at least 10 lbs while in behavioral intervention programs.11
- Patients with schizophrenia or schizoaffective disorder who experienced olanzapine-related weight gain lost weight while attending a 10-week Weight Watchers program.12
- Patients who gained weight while taking antipsychotics lost weight with a step-wise behavioral approach that included increasingly intensive interventions (self-weighing, food diaries, nutrition consultation, and attendance at a “wellness clinic”).6
- 70% of 74 psychiatric inpatients lost weight across 6 to 34 months with a reduced-calorie diet, group therapy, and behavior modification.13
The effectiveness of weight management programs associated with antipsychotics may depend on the target population. In a retrospective chart review, Cohen et al found that calorie restriction did not lead to weight loss among 50 adult inpatients with mental retardation who were being treated with risperidone.14
Timing is important. During olanzapine treatment, mean weight gain has been reported to plateau after approximately 39 weeks, with the most rapid gains in the first 12 weeks.6 Thus, early weight control efforts likely would be most effective. Two small, prospective studies suggest that starting behavioral interventions before you start olanzapine therapy may be the most effective strategy to minimize weight gain.
In the first study—a randomized trial of 12 patients with schizophrenia—those who received an educational intervention prior to starting olanzapine treatment gained a mean 1 lb in 4 weeks, compared with 6.4 lbs in a standard-care group.15 The behavioral intervention included a weekly 1-hour class using educational materials on nutrition and exercise.
In the second study, our group offered 22 psychiatric outpatients a nutrition course before starting olanzapine treatment.16 We included 17 patients with psychotic disorders and 5 with nonpsychotic diagnoses—including major depressive disorder, bipolar disorder, and stuttering—to compare antipsychotic-related weight gain between psychotic and nonpsychotic populations.
We began by talking with each patient for 5 minutes about the following nutritional concepts:
- Weight gain is associated with increased appetite.
- The more you eat, the more weight you gain.
- To reduce hunger, it is better to snack on fruits, carrots, broccoli, or low-fat crackers than on high-calorie “junk food” such as potato chips, ice cream, candy, and cake.
- Drink water or diet sodas instead of sugary soft drinks.
At follow-up visits, we spent 2 minutes reinforcing the educational messages by:
- asking if patients’ appetite had increased
- re-emphasizing that they should eat low-fat snacks to reduce hunger and drink water or diet sodas instead of sugary soft drinks.
After about 7 months, the mean weight gain from olanzapine therapy was 5.27 lbs, which is 40 to 60% less than that seen in studies of olanzapine without structured interventions.6,8,17 Mean weight gain was 5 lbs for the psychotic patients and 6.2 lbs for the nonpsychotic group, which suggested that patients with schizophrenia or schizoaffective disorders may benefit from nutritional education.
Table 2
STRATEGY FOR MANAGING WEIGHT IN PATIENTS TAKING ANTIPSYCHOTICS
|
Medications for weight control
Three medications—nizatidine, topiramate, and amantadine—have shown some effect in controlling weight gain when taken concomitantly with atypical antipsychotics. These medications affect different receptors, and how they affect weight gain is not entirely understood.
Nizatidine—a selective histamine (H2) receptor antagonist—was shown to be significantly more effective than placebo in reducing olanzapine-related weight gain when given to 132 patients at 300 mg bid.18
Topiramate is believed to stimulate 5-HT2C receptors, thus suppressing the increased appetite caused by 5-HT2C antagonism. Among 13 bipolar patients with significant weight gain associated with olanzapine treatment, 73% lost weight with topiramate at 90.4 +/- 48.4 mg/d.18
Amantadine has also been shown to minimize weight gain without worsening psychotic symptoms. A case series reported a weight gain of 15.8 lbs in patients taking olanzapine alone, compared with 7.7 lbs in patients taking olanzapine plus amantadine.19
Related resources
- Wirshing DA, Wirshing WC, Ksyar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry 1999;60:358-63.
- Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry 2001;62 (suppl 7):4-10.
Drug brand names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Clozapine • Clozaril
- Nizatidine • Axid
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosure
Dr. Nguyen is a speaker for Eli Lilly and Co. and GlaxoSmithKline; receives research support from Eli Lilly and Co., GlaxoSmithKline, and Forest Laboratories; and is a consultant to Eli Lilly and Co., Organon, and GlaxoSmithKline.
Dr. Yu is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.; receives research/grant support from Cephalon, Inc. and Eli Lilly and Co.; and is a consultant to Eli Lilly and Co.
Dr. Maguire receives research support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
Acknowledgment
The authors wish to thank David Franklin, MS, neuroscientist; Chris Gordon, MD, resident; and Sam Truong, senior undergraduate student, University of California, Irvine, as well as Leanne Stoneking, MS, fourth-year medical student, Creighton University Medical School, for their assistance in preparing this manuscript.
1. Rockwell WJ, Ellinwood EH, Trader DW. Psychotropic drugs promoting weight gain: health risk and treatment implications. South Med J. 1983;76:1407-12.
2. Walsh AE, Smith KA, Oldman AD, et al. m-Chlorophenylpiperazine decreases food intake in a test meal. Psychopharmacology (Berl). 1994;116:120-2.
3. Garattini S, Mennini T, Samain R. Reduction of food intake by manipulation of central serotonin: current experimental results. Br J Psychiatry. 1989;155(suppl 8):41-51.
4. Tecott LH, Sun LM, Akana SF, et al. Eating disorder and epilepsy in mice lacking 5-HT2C receptors. Nature. 1995;374:542-6.
5. Howarth PH, Emanuel MB, Holgate ST. Astemizole, a potent histamine H1 receptor antagonist: effect on allergic rhinoconjunctivitis, on antigen and histamine-induced skin response and relationship to serum levels. Br J Clin Pharmacol. 1984;18:1-8.
6. Wirshing DA, Wirshing WC, Kysar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry. 1999;60:358-63.
7. Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry. 2001;62 (suppl 7):4-10.
8. Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156:1686-96.
9. Leibowitz SF. Neurochemical system of the hypothalamus control of eating and drinking and behavior and water-electrolyte excretion. In: Morgan P, Panksepp J (eds). Handbook of the hypothalamus (vol, 3). New York: Marcel Dekker, Inc., 1980;299-438.
10. Basson BR, Kinon BJ, Taylor CC, et al. Factors influencing acute weight change in patients with schizophrenia treated with olanzapine, haloperidol, or risperidone. J Clin Psychiatry. 2001;62(4):231-8.
11. O’Keefe C, et al. Reversal of weight gain associated with antipsychotic treatment (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
12. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv. 2001;52(7):967-9.
13. Knox JM. A study of weight reducing diets in psychiatric in-patients. Br J Psychiatry. 1980;136:287-9.
14. Cohen S, Glazewski R, Khan S, Khan A. Weight gain with risperidone among patients with mental retardation: effect of calorie restriction. J Clin Psychiatry. 2001;62(2):114-16.
15. Littrell KH, et al. Educational interventions for the management of antipsychotic-related weight gain (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
16. Nguyen CT, Ortiz T, Franklin D, Yu B, Maguire GA. Nutritional education in minimizing weight gain associated with antipsychotic therapy. New Orleans: American Psychiatric Association annual meeting, 2001.
17. Kinon BJ, Basson BR, Gilmore JA, Tollefson GD. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62(2):92-100.
18. Ketter TA, et al. Int J Neuropsychopharmacol. 2000;3(suppl l):S344.-
19. Floris M, Lejeune J, Deberdt W. Effect of amantadine on weight gain during olanzapine treatment. Eur Neuropsychopharmacol. 2001;11(2):181-2.
1. Rockwell WJ, Ellinwood EH, Trader DW. Psychotropic drugs promoting weight gain: health risk and treatment implications. South Med J. 1983;76:1407-12.
2. Walsh AE, Smith KA, Oldman AD, et al. m-Chlorophenylpiperazine decreases food intake in a test meal. Psychopharmacology (Berl). 1994;116:120-2.
3. Garattini S, Mennini T, Samain R. Reduction of food intake by manipulation of central serotonin: current experimental results. Br J Psychiatry. 1989;155(suppl 8):41-51.
4. Tecott LH, Sun LM, Akana SF, et al. Eating disorder and epilepsy in mice lacking 5-HT2C receptors. Nature. 1995;374:542-6.
5. Howarth PH, Emanuel MB, Holgate ST. Astemizole, a potent histamine H1 receptor antagonist: effect on allergic rhinoconjunctivitis, on antigen and histamine-induced skin response and relationship to serum levels. Br J Clin Pharmacol. 1984;18:1-8.
6. Wirshing DA, Wirshing WC, Kysar L, et al. Novel antipsychotics: a comparison of weight gain liabilities. J Clin Psychiatry. 1999;60:358-63.
7. Casey DE, Zorn S. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry. 2001;62 (suppl 7):4-10.
8. Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156:1686-96.
9. Leibowitz SF. Neurochemical system of the hypothalamus control of eating and drinking and behavior and water-electrolyte excretion. In: Morgan P, Panksepp J (eds). Handbook of the hypothalamus (vol, 3). New York: Marcel Dekker, Inc., 1980;299-438.
10. Basson BR, Kinon BJ, Taylor CC, et al. Factors influencing acute weight change in patients with schizophrenia treated with olanzapine, haloperidol, or risperidone. J Clin Psychiatry. 2001;62(4):231-8.
11. O’Keefe C, et al. Reversal of weight gain associated with antipsychotic treatment (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
12. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv. 2001;52(7):967-9.
13. Knox JM. A study of weight reducing diets in psychiatric in-patients. Br J Psychiatry. 1980;136:287-9.
14. Cohen S, Glazewski R, Khan S, Khan A. Weight gain with risperidone among patients with mental retardation: effect of calorie restriction. J Clin Psychiatry. 2001;62(2):114-16.
15. Littrell KH, et al. Educational interventions for the management of antipsychotic-related weight gain (paper presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
16. Nguyen CT, Ortiz T, Franklin D, Yu B, Maguire GA. Nutritional education in minimizing weight gain associated with antipsychotic therapy. New Orleans: American Psychiatric Association annual meeting, 2001.
17. Kinon BJ, Basson BR, Gilmore JA, Tollefson GD. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62(2):92-100.
18. Ketter TA, et al. Int J Neuropsychopharmacol. 2000;3(suppl l):S344.-
19. Floris M, Lejeune J, Deberdt W. Effect of amantadine on weight gain during olanzapine treatment. Eur Neuropsychopharmacol. 2001;11(2):181-2.
Posttraumatic stress disorder: How to meet women’s specific needs
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
Posttraumatic stress disorder: How to meet women’s specific needs
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Posttraumatic stress disorder (PTSD) was first recognized as a diagnosis in male Vietnam War veterans, but studies since then have consistently found PTSD to be more common in women than in men. Understanding the gender-related differences in PTSD’s presentation can help us craft optimal treatment for women suffering with this persistent disorder.
Data from the National Comorbidity Survey suggest a lifetime PTSD prevalence of 10.4% in women and 5.0% in men.1 PTSD also tends to be more chronic in women. In one study of patients with PTSD, median time from symptom onset to remission was 4 years for women and 1 year for men.2
Evidence suggests that women:
- experience more or different types of trauma than men, including labor and delivery, rape, and childhood sexual abuse
- may react to trauma more often and more robustly than men because of sex hormones, cultural gender roles, or some combination of those factors.
How women experience trauma
Among studies that show gender differences in response to specific trauma, nearly all have found higher PTSD rates in women than in men. This pattern emerges early in life and is seen in children and adults.
A meta-analysis comparing PTSD symptoms in females and males of all ages after specific traumas3 found that females were much more likely than males to report PTSD symptoms after some types of trauma but not others. None of the trauma types predicted PTSD more often for males than for females.
Amount of trauma. Men are more likely than women to be exposed to traumatic events, such as violent assault, during their lifetimes.4 However, the types of trauma that women experience predominantly or exclusively—such as childhood sexual abuse, traumatic labor and delivery, pregnancy loss, severe health problems in a newborn, and prostitution—are rarely included in trauma questionnaires (Table 1). As a result, the full range of traumatic experiences in women’s lives is likely underestimated.
Instruments designed to measure trauma may inadvertently introduce gender bias in other ways.5 For example, questionnaires asking about single traumatic events may underestimate the impact of repetitive traumas, such as childhood sexual abuse and domestic violence, which are more frequently experienced by girls and women. Further, women may not acknowledge sexually linked traumas—such as childhood sexual abuse and rape—unless the questions are asked in a sensitive manner and describe specific behaviors.
Table 1
TRAUMAS THAT CAUSE PTSD PREDOMINANTLY IN WOMEN
| Rape |
| Childhood sexual abuse |
| Domestic violence |
| Pregnancy loss |
| Labor and delivery |
| Neonatal complications |
| Sexual abuse of a child |
| Prostitution |
Types of trauma. Certain types of trauma are associated with especially high conditional risk of PTSD, defined as the risk of developing PTSD after being exposed to the trauma. Childhood sexual abuse, domestic violence, and rape are among the traumas with the highest conditional risk, and women are more likely to be exposed to these trauma types than men.6
Childhood sexual abuse has a particularly high conditional risk of PTSD.7 Such abuse happens over long periods during developmentally vulnerable stages of life. Sexual abuse perpetrated by a family member creates a greater sense of betrayal than does trauma at the hands of a stranger or an impersonal force of nature. In many cases, the victims blame themselves.
Domestic violence, like sexual abuse, has a high conditional PTSD risk because of the intimate nature of the relationship and the usual pattern of multiple assaults over time.
Rape carries the highest conditional risk of any trauma,8 possibly because of the degree to which rape violates a victim’s assumptions about the world as a reasonably safe place.3 PTSD risk after rape is intensified when the victim blames himself or herself and when society—such as the family or court system—reinforces this tendency toward self-blame.9
Influence of sex hormones. Neurophysiologic systems that lie beneath stress responses are closely linked with reproductive physiology.10 Evolution may have favored this association, allowing reproductive efforts to shut down during extreme stress.
Key components of the primary stress-activated hormonal system—corticotropin-releasing hormone, adrenocorticotropic hormone, and the glucocorticoids—inhibit secretion of gonadotropin-releasing hormone and the gonadotropins, the major reproductive hormones. In turn, sex hormones modulate hypothalamic-pituitary adrenal (HPA) axis activity, stress-linked neurotransmitter changes, and behavioral responses to stress.
This intertwining of stress and reproductive hormones suggests that men’s and women’s physiologic response to trauma may differ. Women’s vulnerability to PTSD also may vary at different parts of their menstrual cycles, during pregnancy, or postpartum.
Several animal studies have shown a more intense HPA axis response to stress in females than in males’.11 To date, however, studies have not shown clear gender differences in human physiologic response to trauma. Increased sympathetic nervous system activity, enhanced dexamethasone suppression of cortisol, and hippocampal atrophy have been found in both men and women with PTSD.11,12
Some human studies suggest gender differences in PTSD-related neurophysiologic changes. For example, activation of both the sympathetic and adrenocortical systems (epinephrine and cortisol) has been seen in women with PTSD from childhood sexual abuse, whereas activation of only the sympathetic system (epinephrine but not cortisol) has been seen in men with combat-related PTSD.13 Research with improved methodology is investigating whether sex hormones modulate human response to trauma.
Gender role differences. Because of cultural expectations, women may more easily acknowledge and report distress and feelings of being traumatized.14 This behavioral difference may contribute to higher PTSD prevalence rates in women than in men. Women also may develop more negative beliefs in response to some types of trauma, such as nonsexual assault by a stranger.3
Treating PTSD in women
Drug therapy. Antidepressants—including tricyclics, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors (SSRIs)—have shown efficacy in treating PTSD. Some studies have found that women respond more robustly to SSRI antidepressants than men.15
Cognitive-behavioral therapy. Trauma victims tend to avoid reminders of the trauma. Although this coping strategy can provide short-term relief, it can also constrict a person’s life and preclude opportunities to correct distorted information. For example, a person may attribute danger to benign stimuli that were coincidentally associated with the trauma, such as fearing all men with mustaches after being raped by a man with a mustache.3
Table 2
MALADAPTIVE REACTIONS DURING LABOR AND DELIVERY
| Reaction type | Description |
|---|---|
| Fighting |
|
| Regression |
|
| Dissociation |
|
| Over-control |
|
Cognitive-behavioral therapy (CBT) for PTSD aims to activate and correct information by prolonged exposure to traumatic stimuli and to restructure incorrect cognitions. CBT approaches to PTSD include exposure therapy, cognitive therapy, cognitive processing, stress inoculation training, assertiveness training, systematic desensitization, biofeedback, and relaxation training. Of these, exposure therapy has been studied the most systematically and found to work especially well for female rape victims.16 Exposure therapy consists of confronting feared stimuli—such as returning to the scene of a rape or recalling detailed memories of childhood sexual abuse—until anxiety diminishes.
Psychodynamic therapy aims to re-engage normal adaptive mechanisms by introducing the unconscious into consciousness in tolerable doses.17 Therapy serves as a means of processing traumatic events, such as childhood sexual abuse, and exploring the psychological meanings of traumas.18 Few well-controlled studies have examined psychodynamic therapy in PTSD, in part because of the difficulty in operationally defining and assessing mechanisms of change. However, at least one relatively controlled study found reduced avoidance symptoms with psychodynamic therapy, compared with wait list and active treatment groups.19
EMDR. During eye movement desensitization and reprocessing (EMDR), the patient focuses on a disturbing image, a negative cognition, and somatic sensations associated with the trauma while tracking the movement of the clinician’s finger within her visual field.20 The procedure is repeated until the patient’s distress is reduced and she develops more adaptive thoughts about the trauma.
Most EMDR practitioners recommend its use primarily for single-event traumas, such as rape or traumatic labor and delivery. Meta-analyses have suggested that EMDR may be as effective as other exposure therapy,21 although methodologic problems in several studies limit our ability to determine EMDR’s efficacy in treating women with PTSD.22
Treating and preventing perinatal PTSD
Historically, common outcomes of giving birth included death or chronic disability. Despite advances in obstetric care, labor and delivery remains painful, frightening, and potentially dangerous. Although childbirth is a normative experience for many women, an estimated 2.8 to 5.6% of new mothers develop labor-related PTSD.23-25 Risk of PTSD is increased in women with:
- high general anxiety levels prior to labor
- a history of mental illness
- unplanned pregnancy
- absence of partner during labor and delivery
- the perception that obstetric staff is unsupportive or ineffective
- a need for obstetric interventions, including episiotomy, emergency cesarean section, or use of forceps
- a perception of lack of control.
Table 3
LABOR INTERVENTIONS FOR VICTIMS OF CHILDHOOD SEXUAL ABUSE
|
Untreated PTSD may impair the woman’s functional ability and compromise her relationship with the infant:
Avoidance can extend to subsequent health care (such as not attending the postpartum checkup), sexual relationships, caring for the baby, and future pregnancies. Some women request general anesthesia and cesarean sections for future deliveries.
Arousal may intensify postpartum sleep disturbance and fatigue and may cause a mother to be hypervigilant about her baby.
Flashbacks can influence feelings about the baby, such as when the mother has repeated, vivid memories of the newborn being limp and blue after delivery, even though the infant is healthy now.
Preventive interventions that can minimize PTSD risk after labor and dshlivery include:
- explaining to women before the onset of labor that emergency obstetric interventions might be necessary
- providing adequate social support during labor and delivery
- ensuring that the obstetric staff communicates clearly with the patient
- effectively managing pain to minimize trauma.
Postpartum, it is important to screen for PTSD symptoms among high-risk women. Prompt intervention can alleviate symptoms and minimize adverse effects on the family and the mother-infant relationship.
Role of sexual abuse in perinatal PTSD. For a woman who was sexually abused as a child, even an uncomplicated labor and delivery may trigger memories, flashbacks, and emotions associated with the abuse.26 Physical sensations associated with gynecologic examinations and labor contractions may remind her of abuse-related sensations. Some women with sexual abuse histories react adversely to the loss of control and need to depend on others during labor and delivery.
Unrecognized posttraumatic reactions during labor may result in maladaptive behaviors (Table 2).26 Obstetric staff who encounter these behaviors without being aware of their origins may think the patient is oppositional or noncompliant and may regard her as an adversary to be defeated or bypassed in order to safely deliver the baby.27 The psychiatrist can minimize this problem early in labor by alerting the staff to signs of possible sexual abuse-related PTSD. These may include:
- little or no prenatal care (due to fear of obstetric procedures)
- unusual fears of needles, intravenous lines, etc.
- recoiling when touched during obstetric examinations
- insistence on female obstetric staff
- extreme sensitivity about bodily exposure.26,28
Table 4
USE OF ANTIDEPRESSANTS FOR PTSD DURING BREAST FEEDING
| Medication | Nursling dose range* | Reported nursling side effects |
|---|---|---|
| Citalopram | 0.7 to 9.0% | Uneasy sleep |
| Fluoxetine | 1.2 to 12.0% | Vomiting, watery stools, excessive crying, difficulty sleeping, tremor, somnolence, hypotonia, decreased weight gain |
| Mirtazapine | Not known | Not known |
| Nefazodone | 0.45% | Drowsiness, poor feeding, difficulty maintaining body temperature |
| Paroxetine | 0.1 to 4.3% | None |
| Sertraline | 0.4 to 1.0% | None |
| Venlafaxine | 5.2 to 7.4% | None |
| *Weight-adjusted estimated percent of mother’s dose ingested by a nursing infant | ||
Intervention. Once abuse-related perinatal PTSD is diagnosed, the interventions in Table 3 can help a woman through labor and delivery.26,28 When successful, they can turn childbirth into a healing experience that promotes the mother’s sense of accomplishment, positive association with sexuality, and a new relationship with her body.28
Breastfeeding can also trigger flashbacks and frightening emotions in a woman who was sexually abused as a child.29 She may confuse normal sensations of skin-to-skin contact with the baby or the milk ejection reflex with unpleasant sexually-linked feelings. In such cases, it may help to:
- explain the normal sensations associated with breastfeeding and normal behaviors of breastfeeding infants
- show her how to gently redirect her baby if it does something she finds uncomfortable
- identify situations that are especially difficult for her (such as nighttime feedings) and substitute bottle feeding at those times.
These measures may promote feelings of self-efficacy and help more in the long run than prematurely giving up on breastfeeding.
Prescribing to the nursing woman. When prescribing medication for PTSD in a breast-feeding woman, minimize potential infant side effects by choosing agents that produce relatively low drug levels in breast milk (Table 4).30-34 Sertraline—the first medication to receive Food and Drug Administration approval for treating PTSD—is recommended during breastfeeding.35
Pregnancy loss. Although the prevalence of PTSD in response to miscarriage or stillbirth is unknown, some women clearly develop PTSD after pregnancy loss. The degree of associated physical trauma—and of social and professional support—influence anxiety levels in response to miscarriage36 and may also influence the likelihood of developing PTSD. Pregnancy loss after the first trimester may be more likely to result in PTSD than earlier loss, and subsequent pregnancies may exacerbate PTSD symptoms. In one study, spontaneous fetal loss after the 18th week of gestation led to high rates of PTSD symptoms in a subsequent pregnancy and up to 1 year postpartum.37
Asking a woman how she wants to grieve her pregnancy loss and helping her in that process may minimize her risk of subsequent PTSD. Couples counseling may help in some cases, as each partner may have a different grieving style.
Related resources
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
- Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002.
- Madison Institute of Medicine. Facts for Health: posttraumatic stress disorder. www.ptsd.factsforhealth.org
Drug brand names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Mirtazapine • Remeron
- Nefazodone • Serzone
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
1. Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60.
2. Breslau N, Kessler R, Chilcoat H, Schulz L, Davis G, Andreski P. Trauma and post-traumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:627-32.
3. Tolin DF, Foa EB. Gender and PTSD: a cognitive model. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;76-97.
4. Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med 1999;29:813-21.
5. Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;150-76.
6. Norris F, Foster JD, Weisshaar DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;3-42.
7. DePrince AP, Freyd JJ. The intersection of gender and betrayal in trauma. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;98-113.
8. Breslau N, Davis G, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991;48:216-22.
9. Best CL, Dansky BS, Kilpatrick DG. Medical students’ attitudes about female rape victims. J Interpersonal Violence 1992;7:175-88.
10. Rubinow DR, Schmidt PJ. The neuroendocrinology of menstrual cycle mood disorders. Ann NY Acad Sci 1995;771:648-59.
11. Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925-35.
12. Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;43-75.
13. Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosomatic Med 1995;57:105-15.
14. Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh P, Bremner JD (eds). Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon, 1999;160-79.
15. Brady KT, Back SE. Gender and the psychopharmacological treatment of PTSD. In: Kimerling R, Ouimette P, Wolfe J (eds). Gender and PTSD. New York: Guilford Publications, 2002;335-48.
16. Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23.
17. Kudler HS, Blank AS, Krupnick JL. Psychodynamic therapy. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;176-98.
18. Krupnick JL. Brief psychodynamic treatment of PTSD. J Clin Psychol 2002;58:919-32.
19. Brom D, Kleber RJ, Defares PB. Brief psychotherapy for posttraumatic stress disorders. J Consult Clin Psychol 1989;57:607-12.
20. Chemtob CM, Tolin DF, van der Kolk BA, Pitman RK. Eye movement desensitization and reprocessing. In: Foa EB, Keane TM, Friedman MJ (eds). Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000;333-5.
21. Davidson PR, Parker CH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001;69:305-16.
22. Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Publications, 2000.
23. Creedy D, Shochet I, Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth 2000;27:104-11.
24. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol 2000;39:35-51.
25. Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 2001;28:111-18.
26. Rhodes N, Hutchinson S. Labor experiences of childhood sexual abuse survivors. Birth 1994;21:213-20.
27. Josephs L. Women and trauma: a contemporary psychodynamic approach to traumatization for patients in the OB/GYN psychological consultation clinic. Bull Menninger Clin 1996;60:22-8.
28. Burian J. Helping survivors of sexual abuse through labor. MCN 1995;20:252-6.
29. Kendall-Tackett K. Breastfeeding and the sexual abuse survivor. J Hum Lact 1998;14:125-30.
30. Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol 2002;53:17-22.
31. Kristensen JH, Ilett KF, Yapp P, Paech M, Begg EJ. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br J Clin Pharmacol 1999;48:521-7.
32. Misri S, Kim J, Riggs KW, Kostaras X. Paroxetine levels in postpartum depressed women, breast milk, and infant serum. J Clin Psychiatry 2000;61:828-32.
33. Ohmann R, Hagg S, Carleborg L, Spigset O. Excretion of paroxetine into breast milk. J Clin Psychiatry 1999;60:519-23.
34. Yapp P, Ilett KF, Kristensen JH, Hackett LP, Paech MJ, Rampono J. Drowsiness and poor feeding in a breast-fed infant: association with nefazodone and its metabolites. Ann Pharmacother 2000;34:1269-72.
35. Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JR. The Expert Consensus Guideline Series. Treatment of depression in women. Postgrad Med 2001 Mar;(Spec No):1-107.
36. Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosom Res 1996;40:225-44.
37. Turton P, Hughes P, Evans CDH, Fainman D. Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 2001;178:556-60.
Handhelds: A cure for illegible prescriptions?
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Handhelds: A cure for illegible prescriptions?
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Those stale jokes about a doctor’s poor penmanship are no laughing matter when it comes to writing prescriptions.
Prescription errors are a common cause of adverse patient events.1 Illegible handwriting can lead to misinterpretations of dosage, drug name, or abbreviations. Imagine the implications for a patient with bipolar depression whose pharmacist interprets “Lamictal” as “Lamisil” on your prescription.
Replacing your Rx pad with a Palm or Pocket PC-both of which have prescription writing, printing, and processing capacities-may help you prevent such errors.
Why a handheld?
Machine-generated text usually is more readable than handwritten copy, but use of handhelds can also make prescription writing more efficient and secure.
A tap on the screen can pull a patient’s name from a database directly into the prescription. With a few more taps, you can access a list of the patient’s current medications and renew them without changes. A drug reference program allows you to check for drug-drug interactions.
To add a prescription, simply type the first letter and choose from a menu of drug names; the program narrows the choices as additional letters are typed.
Prescription-writing programs for handhelds also offer links to health plan formulary databases, so you can immediately find out whether a medication is available to the patient. This can eliminate time-consuming phone calls from the patient or pharmacy and discussions with pharmacy benefits managers. The patient also will appreciate getting needed medications with no hassle.
You can print out the prescription via the handheld’s infrared or wireless port. This will help you prevent forgery, since a printed prescription is harder to forge than a handwritten one. It is extremely difficult to align a printed document in order to add or correct existing text.
By connecting the handheld to your desktop computer, you can fax prescriptions directly to the pharmacy. Entering all prescriptions into the handheld and sending them in bulk at day’s end can save you significant time. To do this, you must create a database of pharmacies used by your patients and enter it into the handheld’s fax software.
Cellular phone networks and wireless Internet access can also facilitate handheld transmissions. Companies offering these options typically have the prescription sent to their electronic warehouses, then to the designated pharmacy. These transmissions are expedient and safe, but users should make sure that they conform to the Health Insurance Portability and Accountability Act of 1996. Users face civil penalties for failure to use these adopted standards and criminal penalties for wrongfully disclosing confidential information. Violators can be fined up to $25,000 and face as much as 10 years in prison.
Caveats
Use of handhelds entails hardware, software, and monthly service costs. Most handhelds cost around $300, with the software and service totaling around $50 per month. Several prescription solutions are on the market (See “Handheld options for writing prescriptions”) and they vary in terms of hardware compatibility, software interface, and mode of transmission. For example, ePhysician is available for Palm OS devices, but transmissions must go to the ePhysician server before they are relayed to the pharmacy. iScribe is available for Palm OS, but prescriptions must be printed on specialized paper with preset perforations.
As mentioned, fax-based transmission lets you send prescriptions en masse, but this makes it difficult to confirm that a particular faxed prescription has been received. Worse still, if the handheld device fails, all prescriptions in storage would be lost. It is better to send fax-based prescriptions as often as possible or back up the information during the day.
Pharmaceutical benefit management organizations have begun purchasing handheld-compatible prescription companies. While this could expedite claims processing for handheld users, tighter controls on out-of-formulary drug use could result. The number and types of prescriptions can be tracked, making it easier for administrators to spot non-formulary prescriptions. The impact this will have on psychiatry remains to be seen.
Finally, because both computer technology and the health care industry are constantly changing, a prescription writing solution can become obsolete within a couple of years. Specifically, when health care companies merge, some products are discontinued. For example, when Salu medical communications purchased ScanRx, the latter company’s software upgrades were stalled and continuity of service to existing customers was broken.
The future
Technology is addressing the need to reduce prescription errors in other ways.
Many hospitals use bar-code scanners attached or built into handhelds to ensure that medications reach the right patients. This capability could one day reach the practice mainstream.
Voice recognition software may one day allow physicians to dictate prescriptions onto the handheld, but will require voice imprint recognition for security.
Handheld options for writing prescriptions
Palm OS
Pocket PC OS
If you have any questions about these products or comments about Psyber Psychiatry, click here to contact Dr. Luo or e-mail to [email protected].
Disclosure:
Dr. Luo reports no financial relationship with any company whose products are mentioned in this article. The opinions expressed by Dr. Luo in this column are his own and do not necessarily reflect those of Current Psychiatry.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Reference
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000:22.
Pediatric bipolar disorder: Mood swings, irritability are cues to this diagnosis
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.
Pediatric bipolar disorder: Mood swings, irritability are cues to this diagnosis
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
Children and adolescents with bipolar disorder are often referred to psychiatrists because of disruptive behaviors at home and in school. They exhibit poor academic performance, disturbed interpersonal relationships, increased rates of substance abuse, legal difficulties, multiple hospitalizations, and high rates of suicide attempts and completions.1,2 Many have comorbid psychiatric problems—particularly attention-deficit/hyperactivity disorder (ADHD).
Although few studies have examined this complex diagnosis, we do know that bipolar disorder presents differently in children and adolescents than in adults. Prodromal symptoms can appear early—before kindergarten in some children. Early recognition therefore is key to effectively treating these sick and often complicated patients.
How often a clinician encounters a child or adolescent with bipolar disorder depends largely on the practice setting (Box).1,3,4 Wherever you practice, however, you can recognize and treat pediatric bipolar disorder if you keep in mind that its presentation and disease progression differ from the adult type.
Pediatric versus adult symptoms
Prodromal symptoms—such as episodes of depressed mood or hopelessness and excessive mood lability—have been detected in youths who later were diagnosed with bipolar disorder. More than one-half of 494 adult members of the Depression and Bipolar Support Alliance have reported that they first exhibited signs of bipolar illness before age 19, with distribution by age as follows:
- 5% before age 5
- 12% at ages 5 to 9
- 14% at ages 10 to 14
- 28% at ages 15 to 19.5
Pediatric bipolar disorder is seen much more commonly in specialized psychiatric settings than in general practice.
Overall prevalence. A large, well-designed population study of mood disorders in adolescents reported a lifetime prevalence of 1% for bipolar spectrum disorders, including bipolar I, bipolar II, and cyclothymia.1 Most adolescents in the bipolar group (84%) reported a distinct period of elevated, expansive, or irritable mood that best fit DSM-IV criteria for bipolar disorder not otherwise specified (NOS). These adolescents—who represented an overall prevalence of 5.7%—had extremely high rates of psychosocial impairment and use of mental health services, similar to those with bipolar I disorder.
In specialized settings. Bipolar disorder is seen much more frequently in specialized settings, such as a pediatric psychopharmacology clinic, than in general psychiatric practice. For example:
- Among 262 children referred consecutively to a specialty pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania.3
- In a special education class, 8 of 12 students met DSM-III-R criteria for a bipolar disorder.4
- In child and adolescent psychiatry inpatient units, it is not uncommon to find 30 to 40% of patients with a bipolar disorder.
Table 1
COMMON PRESENTING SYMPTOMS OF PEDIATRIC BIPOLAR DISORDER
| Episodes of depressed mood/hopelessness |
| Excessive mood lability |
| Periods of increased or decreased energy |
| Episodes of decreased need for sleep |
| Anger dyscontrol |
| Markedly irritable moods |
| Frequent argumentativeness |
| Bold/intrusive/demanding behaviors |
In a similar study,6 58 adult patients with bipolar I disorder reported an average interval of 9 to 12 years between the emergence of bipolar symptoms and the onset of a major affective disorder.
Common initial symptoms of pediatric bipolar disorder are listed in Table 1. Most of these symptoms occur in discrete episodes and represent a change from the child’s normal functioning.
Many children and adolescents are labeled “bipolar” without careful consideration of this disorder’s diagnostic complexities and subtypes. Bipolarity in young patients can be difficult to establish because of:
- variability of symptom expression, depending on the illness’ context and phase
- effects of development on symptom expression
- mood and behavioral effects of psychotropic medications the patient is taking.
Pediatric bipolar patients often present with a mixed or “dysphoric” picture characterized by frequent short periods of intense mood lability and irritability rather than classic euphoric mania.3,7 Clinicians who evaluate children with pediatric bipolar disorders often try to fit them into the DSM-IV “rapid cycling” subtype. This subtype does not fit bipolar children very well, however, because they often lack clear episodes of mania. Rather, researchers are reporting that bipolar children cycle far more frequently than the four episodes/year in DSM-IV’s diagnostic criteria:
- Continuous, daily cycling from mania or hypomania to euthymia or depression was seen in 81% of a well-defined group of pediatric bipolar patients.7,8
- A high rate of rapid cycling and onset of a first manic episode at mean age 7 was reported in 90 children and adolescents (mean age 11) with bipolar I disorder.9
The picture that emerges from independent research groups is that multiple daily mood swings and irritability are much more common than euphoria in prepubertal children with bipolar disorder.8,10
Making the diagnosis
DSM-IV’s diagnostic classification system for bipolar disorders is complex, involving:
- five types of episodes (manic, hypomanic, mixed, depressed, unspecified)
- four severity levels (mild, moderate, severe without psychosis, severe with psychosis)
- and three course specifiers (with or without inter-episode recovery, seasonal pattern, rapid cycling).
Table 2
PEDIATRIC BIPOLAR DISORDER SUBTYPES: DIAGNOSTIC CHARACTERISTICS AND ASSOCIATED FEATURES
| DSM-IV subtype | Minimum duration of manic symptoms | Depression symptoms | Cardinal features |
|---|---|---|---|
| Bipolar I | Pure mixed or manic 1 week (or hospitalization needed) | Major depressive disorder presentation of bipolar may be the first disorder, particularly in adolescents | Multiple daily mood swings with severe irritability (mood lability) Short periods of euphoria Decreased need for sleep Hypersexuality Grandiosity Racing thoughts Pressured speech |
| Bipolar II | Hypomania 4 days | One or more prior episodes of major depressive disorder required, each with a duration of 2 weeks | Noticeable manic symptoms that do not cause significant dysfunction or lead to hospitalization |
| Cyclothymia | Hypomania cycling with depressive symptoms 1 year | Hypomania cycling with depressive symptoms, without manic, mixed, or major depressive episodes (1 year, with symptom-free intervals <2 months) | Chronic, low-level mood cycling |
| Bipolar NOS | < 4 days of bipolar symptoms | Rapid alternation (within days) between manic depressive symptoms without full manic, mixed, or major depressive episodes | May include hypomanic and episodes (but <4 days) without intercurrent depression May also be diagnosed when clinician determines bipolar disorder is present but cannot determine whether it is primary, due to a general medical condition, or substance-induced, such as severe mood lability secondary to fetal alcohol syndrome or alcohol-related neurodevelopmental disorder |
| NOS: not otherwise specified | |||
Table 3
COMPLICATING FACTORS IN PEDIATRIC BIPOLAR DISORDER
| Medical conditions that may mimic bipolar mania |
| Temporal lobe epilepsy |
| Hyperthyroidism |
| Closed or open head injury |
| Multiple sclerosis |
| Systemic lupus erythematosus |
| Alcohol-related neurodevelopmental disorder |
| Wilson’s disease (rare progressive disease caused by defective copper metabolism) |
| Medications that may increase mood cycling |
| Tricyclic antidepressants |
| Selective serotonin reuptake inhibitors |
| Serotonin and norepinephrine reuptake inhibitors |
| Aminophylline |
| Corticosteroids |
| Sympathomimetic amines, such as pseudoephedrine |
DSM-IV criteria for mania—which were developed from data on adults with bipolar disorders—do not take into account developmental differences between bipolar adults and bipolar children and adolescents.
Diagnostic characteristics of the pediatric bipolar disorder subtypes are compared in Table 2. Generally:
- Pediatric patients with bipolar I disorder have multiple daily mood swings, a “mixed” type of episode with short periods of euphoria and longer periods of irritability, and comorbidities such as ADHD, oppositional defiant disorder, or conduct disorder.3,11,12
- Bipolar II disorder presents more typically in adolescence and is usually noticed clinically as a major depressive episode. Past episodes of hypomania may have been missed unless a careful history was taken.
- Cyclothymia is difficult to diagnose because the hypomania and depressive symptoms are not as severe as in bipolar types I or II. Prospective mood charting can help the clinician diagnose cyclothymia (see “Related Resources”).
- Bipolar disorder NOS represents the largest group of patients with bipolar symptoms. This diagnosis is made when bipolar symptoms are present but not of sufficient severity or duration to warrant a diagnosis of bipolar I, II or cyclothymia. Bipolar NOS also can be diagnosed when a bipolar disorder is secondary to a general medical condition, such as fetal alcohol syndrome or alcohol-related neurodevelopmental disorder.
Differential diagnosis. Medications and medical disorders may exacerbate or mimic pediatric bipolar symptoms (Table 3), so it is important to assess these potential confounds before initiating treatment. Psychiatric comorbidities also frequently complicate the presentation of pediatric bipolar disorder and its response to treatment (Table 4). ADHD is the most common comorbidity, with rates as high as 98% in bipolar children.3,13
Outcomes
Long-term outcomes of children and adolescents with bipolar disorders have not been well studied. In the only prospective follow-up investigation of adolescent inpatients with mania, Strober et al found that most of 54 patients (96%) recovered from an index affective episode, but nearly one-half (44%) experienced one or more relapses within 5 years.14 The rate of recovery varied according to the index episode’s polarity. Recovery was faster in patients with pure mania or mixed states, and multiple relapses occurred more frequently in those with mixed or cycling episodes. Twenty percent of the patients attempted suicide.
Recently, Geller et al reported the results of the first large, prospective, follow-up study of children with bipolar disorder.15 In 89 outpatients (mean age 11) with bipolar I disorder, comprehensive assessments at baseline and at 6, 12, 18, and 24 months showed that 65% recovered from mania but 55% relapsed after recovery. Mean time to recovery was 36 weeks, and relapse occurred after a mean of 28.6 weeks. Children living with their intact biological families were twice as likely to recover as those in other living arrangements.
The poor outcomes of these bipolar children highlight the need for earlier recognition and more effective treatments.
Treating acute mania
Many psychotropic medications used to treat adults with bipolar disorders are also used for children and adolescents. To date, only two double-blind, placebo-controlled studies13,16 and one uncontrolled maintenance treatment study17 have examined treatment of acute mania in pediatric bipolar disorder.
Lithium is the most studied medication for pediatric bipolar disorder and the only FDA-approved medication for treating acute mania and bipolar disorder in patients ages 12 to 18. Approximately 40 to 50% of children and adolescents with bipolar disorder respond to lithium monotherapy.18,19
In general, lithium should be titrated to 30 mg/kg/d in two or three divided doses; this typically produces a serum level of 0.8 to 1.2 mEq/L. Common side effects in children and adolescents include nausea, polyuria, polydipsia, tremor, acne, and weight gain. Lithium levels and thyroid function should be monitored, as in adult patients.
Only one prospective, placebo-controlled study has examined lithium use in children and adolescents with bipolar disorders. Twenty-five adolescents with comorbid bipolar and substance use disorders were treated with lithium or placebo for 6 weeks. Positive urine toxicology screens decreased significantly, and global assessment of functioning improved in 46% of those receiving lithium vs. 8% of those receiving placebo.13 This study demonstrated lithium’s efficacy in treating bipolar adolescents with comorbid substance abuse but did not measure its effect on mood.
Risk factors for poor lithium response in children and adolescents with bipolar disorder include prepubertal onset and comorbid ADHD.20
Divalproex. No placebo-controlled studies of antiepileptics in pediatric bipolar disorder have been published. Open-label studies of divalproex have reported response rates of 53 to 82% in manic adolescents.18, 21-23 Several case reports and series have described successful use of carbamazepine as monotherapy and adjunctive treatment in children and adolescents with bipolar disorder.24,25
Table 4
RATES OF COMMON COMORBIDITIES IN PEDIATRIC BIPOLAR DISORDERS
| Disorder | Children (prepubertal) | Adolescents |
|---|---|---|
| ADHD | 70 to 90% | 30 to 60% |
| Anxiety disorders | 20 to 30% | 30 to 40% |
| Conduct disorders | 20 to 30% | 30 to 50% |
| Oppositional defiant disorder | 60 to 80% | 20 to 30% |
| Substance abuse | 10% | 40 to 80% |
| Learning disabilities | 30 to 40% | 30 to 40% |
One 6-week, random-assignment, prospective study compared lithium, divalproex, and carbamazepine in treating 42 acutely manic or hypomanic patients ages 8 to 18.18 In this open study, all three mood stabilizers demonstrated efficacy in treating a mixed or manic episode in youths with bipolar I or II disorder. Response rates—based on a 50% improvement in Young Mania Rating Scale baseline scores—were divalproex 53%, lithium 38%, and carbamazepine 38%.
In general, divalproex is started at 20 mg/kg/d, which typically produces a serum level of 80 to 120 μg/ml. Common side effects in children include weight gain, nausea, sedation, and tremor.
A possible association between divalproex and polycystic ovary syndrome (PCOS) has been reported in women with epilepsy.26 The mechanism for PCOS has been hypothesized to be obesity secondary to divalproex, resulting in elevated insulin and androgen levels. Recently, Rasgon et al27 reported that epilepsy—and not the anticonvulsants used to treat it—may increase the risk of PCOS. In contrast, O’Donovan et al reported higher rates of menstrual irregularities and PCOS in women with bipolar disorder who were taking divalproex than in those who were not taking divalproex and in healthy controls.28
Until we learn more about this association, clinicians should monitor bipolar female adolescents treated with divalproex for any signs of PCOS, which include menstrual abnormalities, hirsutism, and acne.
Carbamazepine is used widely for seizure management but less commonly than divalproex in pediatric bipolar disorder. This anticonvulsant must be titrated slowly and requires frequent monitoring of blood levels, which can be a problem in children with needle phobia.
Carbamazepine is usually titrated to 15 mg/kg/d to produce a serum level of 7 to 10 μg/ml. Its most common side effects are sedation, rash, nausea, and hyponatremia. Aplastic anemia and severe dermatologic reactions, such as Stevens-Johnson syndrome, occur uncommonly.28
Atypical antipsychotics. Recent case series and open-label reports suggest that atypical antipsychotics such as clozapine,29 risperidone,30 olanzapine,31-33 and quetiapine16 are effective in treating pediatric bipolar disorder. However, clinically significant weight gain may be associated with the use of olanzapine and risperidone.34 Ziprasidone may increase QTc prolongation, and safety data are limited in children and adolescents. Therefore, ziprasidone should be used with caution in pediatric bipolar disorder, and ECGs should be monitored.
In the only double-blind, placebo-controlled study of an atypical antipsychotic in pediatric bipolar disorder, manic symptoms were more greatly reduced in 15 adolescents given quetiapine plus divalproex than in 15 patients who received divalproex alone. Quetiapine was titrated to 450 mg/d across 7 days and was well-tolerated. The findings suggest that a mood stabilizer plus an atypical antipsychotic may be more effective than a mood stabilizer alone for treating adolescent mania.16
Long-term treatment
In addition to treating acute affective episodes, lithium may also help prevent recurrent affective episodes in younger patients. In the only maintenance treatment study for pediatric bipolar disorder, Strober et al prospectively evaluated 37 adolescents whose bipolar disorder had been stabilized with lithium during hospitalization.17 After 18 months of follow-up, 35% of patients had discontinued lithium, and their relapse rate was 92% (compared with 38% in patients who were lithium-compliant.
It is reasonable to maintain a child or adolescent who has had a single manic episode on mood-stabilizing treatment for several years and then—if the patient is euthymic and asymptomatic—to slowly taper the mood stabilizer(s) over several months. If mood symptoms recur, the agent(s) should be reintroduced.
If a child with bipolar disorder does not respond or only partially responds to a mood stabilizer, it may be necessary to add a second mood stabilizer or an atypical antipsychotic. A bipolar child or adolescent with psychotic symptoms should be maintained on an antipsychotic (typical or atypical) for at least 1 month, even if the psychosis has resolved.35
Treatment of comorbid ADHD. Most children with bipolar disorder have comorbid ADHD, and mood stabilization is necessary prior to starting stimulant medications.36 In bipolar patients, sustained-release psychostimulants may reduce rebound symptoms more effectively than immediate-release formulations. Typical dosages for a child with bipolar disorder and ADHD would be Concerta, 36 mg/d, or Adderall XR, 10 to 20 mg/d.
Psychosocial interventions
Most psychotherapeutic interventions have not been systematically studied in pediatric bipolar disorder but may be beneficial. In a recent study, Fristad et al reported the efficacy of multifamily psychoeducational group therapy for treating bipolar children and adolescents and their families.37
Other useful psychosocial tactics include:
- Minimize periods of overstimulation (for example, these patients do not do well at shopping malls).
- Maintain good sleep hygiene.
- Address medication nonadherence immediately.
- Discuss the risk of substance abuse with the patient.
- Encourage mood charting by the patient and or parent.
- Mood charts appropriate for pediatric patients.
- Child and Adolescent Bipolar Foundation. www.cabf.org
- Findling RF, Kowatch RA, Post RM. Pediatric bipolar disorders: a handbook for clinicians. London, Martin Dunitz Press, 2002.
- Geller B, DelBello MP (eds). Child and early adolescent bipolar disorder: theory, assessment, and treatment. New York: Guilford Publications, 2002.
Drug brand names
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Olanzapine • Zyprexa
- Risperidone • Risperdal
- Quetiapine • Seroquel
- Ziprasidone • Geodon
Disclosure
Dr. Kowatch receives grant support from, serves as a consultant to, or is on the speakers bureau of Novartis Pharmaceuticals Corp., Abbott Laboratories, Solvay Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, GlaxoSmithKline, and AstraZeneca Pharmaceuticals.
Dr. DelBello receives grant support from, serves as a consultant to, or is on the speakers bureau of Abbott Laboratories, AstraZeneca Pharmaceuticals, Eli Lilly and Co., Ortho-McNeil Pharmaceutical, Shire Pharmaceutical Group, Janssen Pharmaceutica, Pfizer Inc., and GlaxoSmithKline.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.
1. Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 1995;34:454-63.
2. Nottelmann E. National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder. J Am Acad Child Adolesc Psychiatry 2001;40:871-8.
3. Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34(7):867-76.
4. Isaac G. Misdiagnosed bipolar disorder in adolescents in a special educational school and treatment program. J Clin Psychiatry 1992;53(4):133-6.
5. Lish JD, Dime-Meenan S, et al. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31(4):281-94.
6. Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000;39(Oct):1245-52.
7. Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord 1995;34:259-68.
8. Geller B, Zimerman B, Williams M, et al. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2000;10:157-64.
9. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
10. Wozniak J, Biederman J. Childhood mania: insights into diagnostic and treatment issues. J Assoc Acad Minor Phys 1997;8(4):78-84.
11. West SA, McElroy SL, Strakowski SM, et al. Attention-deficit/hyperactivity disorder in adolescent mania. Am J Psychiatry 1995;152(2):271-3.
12. Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995;34(6):715-23.
13. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998;37(2):171-8.
14. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995;34(6):724-31.
15. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002;159(6):927-33.
16. DelBello M, Schwiers M, Rosenberg H, Strakowski S. Quetiapine as adjunctive treatment for adolescent mania associated with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2002;41(10):1216-23.
17. Strober M, Morrell W, Lampert C, Burroughs J. Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. Am J Psychiatry 1990;147(4):457-61.
18. Kowatch RA, Suppes T, Carmody TJ, et al. Effect size of lithium, divalproex sodium and carbamazepine in children and adolescents with bipolar disorder. J Amer Acad Child Adolesc Psychiatry 2000;39(6):713-20.
19. Youngerman J, Canino IA. Lithium carbonate use in children and adolescents. A survey of the literature. Arch Gen Psychiatry 1978;35(2):216-24.
20. Strober M. Mixed mania associated with tricyclic antidepressant therapy in prepubertal delusional depression: three cases. J Child Adolesc Psychopharmacol 1998;8:181-5.
21. Wagner KD, Weller E, Biederman J, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002;41(10):1224-30.
22. West SA, Keck PE, Jr, McElroy SL, et al. Open trial of valproate in the treatment of adolescent mania. J Child Adolesc Psychopharmacol 1994;4:263-7.
23. Papatheodorou G, Kutcher SP, Katic M, Szalai JP. The efficacy and safety of divalproex sodium in the treatment of acute mania in adolescents and young adults: an open clinical trial. J Clin Psychopharmacol 1995;15(2):110-6.
24. Evans RW, Clay TH, Gualtieri CT. Carbamazepine in pediatric psychiatry. J Am Acad Child Adolesc Psychiatry 1987;26(1):2-8.
25. Puente RM. The use of carbamazepine in the treatment of behavioural disorders in children. In: Birkmayer W (ed). Epileptic seizures - behaviour - pain. Baltimore: University Park Press, 1975;243-52.
26. Isojarvi JI, Laatikainen TJ, Pakarinen AJ, Juntunen KT, Myllyla VV. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med 1993;329(19):1383-8.
27. Rasgon NL, Altshuler LL, et al. Medication status and polycystic ovary syndrome in women with bipolar disorder: a preliminary report. J Clin Psychiatry 2000;61:173-8.
28. O'Donovan C, Kusumakar V, Graves GR, Bird DC. Menstrual abnormalities and polycystic ovary syndrome in women taking valproate for bipolar mood disorder. J Clin Psychiatry 2002;63:322-30.
29. Kowatch RA, Suppes T, Gilfillan SK, et al. Clozapine treatment of children and adolescents with bipolar disorder and schizophrenia: a clinical case series. J Child Adolesc Psychopharmacol 1995;5(4):241-53.
30. Frazier J, Meyer M, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psychiatry 1999;38:960-5.
31. Soutullo C, Sorter M, Foster K, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Disord. 1999;53:279-83.
32. Khouzam H, El-Gabalawi F. Treatment of bipolar I disorder in an adolescent with olanzapine. J Child Adolesc Psychopharmacol 2000;10:147-51.
33. Chang K, Ketter T. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
34. Ratzoni G, Gothelf D, Brand-Gothelf A, et al. Weight gain associated with olanzapine and risperidone in adolescent patients: a comparative prospective study. J Am Acad Child Adolesc Psychiatry 2002;41:337-43.
35. Kafantaris V, Dicker R, et al. Adjunctive antipsychotic treatment is necessary for adolescents with psychotic mania. J Child Adolesc Psychopharmacol 2001;11:409-13.
36. Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999;9(4):247-56.
37. Fristad MA, Goldberg-Arnold JS. Working with families of children with early-onset bipolar disorder. In: Geller B, DelBello M (eds). Child and early adolescent bipolar disorder: Theory, assessment, and treatment. New York: Guilford Publications, 2002.