User login
When is ECT indicated in psychiatric disorders?
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
When is ECT indicated in psychiatric disorders?
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
Although numerous psychotropic agents in multiple classes have emerged over the past few decades, electroconvulsive therapy (ECT) still represents an essential treatment in modern psychiatry. Its record of safety and efficacy is virtually unparalleled vis a vis pharmacological agents.
Advances in anesthetic technique, electrode placement, and electrical stimulus dosing allow ECT to be administered safely to even the most medically ill patients without excessive effects on memory, with excellent clinical benefits (Box 1). A typical course of ECT consists of 8 to 10 treatments administered 2 to 3 times per week.
The medical complications of ECT are rare, and good pre-treatment medical assessment helps ensure its safety.1 Include at minimum a medical history, physical exam, and basic laboratory tests. Specialist consultations are sometimes necessary when patients have comorbid neurologic or cardiologic illnesses (Box 2).
The most bothersome side effect of ECT is memory disturbance. This takes 3 forms: post-treatment confusion and anterograde or retrograde amnesia (Box 3). Less serious side effects include headaches, muscle soreness, and nausea. These are easily treated symptomatically with analgesics or antiemetics.
Electroconvulsive therapy (ECT) has been in use since 1938.6 It consists of the application of an electric current to the head, which causes a seizure.
Modern ECT technique involves the use of general anesthesia, usually with a barbiturate anesthetic such as methohexital, and muscular paralysis, usually with the depolarizing neuromuscular blocking agent succinylcholine. Continuous oxygenation with positive pressure ventilation, measuring of blood pressure, and monitoring with an electrocardiogram and pulse oximetry make the procedure exceedingly safe.
Efficacy and cognitive side effects may be affected by how ECT is administered. The two treatment electrodes that are placed on the head can be located on either side of the temporal fossa (the bitemporal position), on either side of the forehead (the bifrontal position), or on the right temporal fossa and just to the right of the vertex of the skull (the d’Elia unilateral position). Generally, unilateral electrode placement causes less memory impairment but has been believed to be less effective than bilateral electrode positions.6
Another technical factor receiving attention from researchers is the amount of electricity, or electrical dose, used to elicit the seizure. Generally, especially for unilateral ECT, high electrical doses are needed to attain acceptable treatment efficacy. In fact, one study indicates that if 6 times the minimum electrical seizure threshold is used for unilateral ECT, efficacy for depression is equal to that of bilateral ECT with less memory disturbance.23
Finally, treatment frequency affects ECT outcome: twice-weekly treatment schedules are associated with less memory disturbance—and only slightly slower clinical response—than thrice-weekly schedules.24
The most common indication for ECT is major depression. Using modern diagnostic criteria, most depressed patients respond to ECT. Some features that presage a particularly robust response include psychomotor retardation, psychosis, catatonia, and advanced age. Patients who have medication-resistant depression may require particularly potent forms of treatment, such as bilateral electrode placement and/or higher than usual electrical doses.
Patients with mania respond particularly well to ECT but, because of excellent responses with modern pharmacological agents, rarely need it. For patients with mania who are agitated and noncompliant, ECT may represent a life-saving option for stabilizing an acute episode. Finally, ECT may help yield stability for an acute exacerbation of schizophrenia or may extend the benefits of antipsychotic medication for those with chronic schizophrenia, in which case continuation of ECT is usually advisable.
When ECT is indicated for depression
Typical depressed patients receiving ECT have experienced functional decline and have resisted, or have not tolerated, antidepressant medication. Several specific factors affect whether ECT will help particular depressed patients:
Melancholic features From the earliest use of ECT, it seemed apparent that patients with melancholic depression respond better to ECT than do patients with atypical or mood-reactive depression. Early research seems to have borne this out. Roberts2 found that melancholic features such as psychomotor retardation and guilty ideations strongly and favorably predicted ECT response. More recent research, however, generally fails to find predictive value in ECT response in patients based on presence of melancholia.3
The medical and neurologic illnesses that place prospective ECT patients at higher than usual risk of complications include a brain tumor or other intracranial space-occupying lesion, increased intracranial pressure, unstable cardiac function, or high anesthetic risk.25
Patients with severe cardiac disease, such as congestive heart failure, coronary artery disease, or cardiac dysrhythmia, can almost always be treated with ECT safely with adequate attention to pretreatment medical stabilization and use of antihypertensive medications during the treatment to blunt the increase in myocardial oxygen demand during the seizures.
Why is this? Several factors likely explain this rather dramatic difference. First, the patients given ECT in the early decades of its use most likely suffered with a diverse range of dysphoric states (e.g., patients with “neurotic” depression, dysthymia, or personality disorders), while modern research has been limited to relatively homogeneous samples of patients with major depression defined according to strict research criteria.3 When you try to correlate a putative predictive variable such as presence vs. absence of melancholia with an outcome variable such as reduction in depression ratings, the less variability there is on the predictive variable, the less strong the correlation will be.
Another possible factor accounting for the lack of predictability is a broadened concept of melancholia. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),4 it is possible to have melancholic depression without having weight loss, psychomotor retardation, or excessive guilt—3 signs classically thought to be inherent in the melancholic syndrome. If melancholia is defined more narrowly, to include requirements for weight loss and psychomotor change, then it is probably more likely to correlate with ECT response.
A final potential reason for lack of predictability is the method of ascertaining melancholia. In modern samples, usually the Hamilton Rating Scale for Depression is used.5 Such a scale is administered in a brief interview by a research clinician not familiar with any other aspects of the patient’s mental status. In contrast, in some early studies,2 melancholic signs were ascertained by complete psychiatric history and evaluations as done in clinical practice. Such methods are likely to yield more reliable data on weight loss, guilty ideations, psychomotor activity, and other signs than is a 15-to 20-minute interview conducted by a research technician.
Along these lines, Hickie et al,6 utilizing a thorough evaluation of psychomotor activity before ECT, found that psychomotor retardation robustly predicted positive ECT response. Their scale utilized numerous items assessing agitation and retardation, and required a longer period of assessment than did the Hamilton scale; the latter scale has only 2 items for psychomotor activity, each one a global assessment of agitation or retardation.
So do you consider ECT for patients with melancholic features? Yes. Patients with classic melancholic features such as weight loss, pronounced guilt, and especially psychomotor retardation stand an excellent chance of substantial relief with a course of ECT. Additionally, patients with nonmelancholic depression have good response rates with ECT.
Patients and their families are frequently concerned about the effects of ECT on memory. The 3 types of memory disturbances to discuss are:
- Post-treatment confusion and disorientation. This state usually lasts from a few minutes to several hours or, in the case of some elderly patients after receiving numerous treatments, several days. This state is always reversible.
- Anterograde amnesia. This is the inability to recall newly learned information during and up to a few weeks after the course of treatments. During this time, any information given to the ECT patient may not be remembered. Important strategies are to write down instructions and make sure that family members are informed of the need to repeat things and monitor the patient if an outpatient. Fortunately, antero-grade amnesia is also reversible.
- Retrograde amnesia. This refers to the forgetting of personal life events and general knowledge about the world. Usually, the events and knowledge that are “wiped out” by the treatments are those from up to a few months before the treatments begin to about a month after the treatments are done. Even more remote memories may be forgotten as well. Unlike the other types of ECT-induced memory impairment, retrograde amnesia may be permanent.
Catatonic features It has been known for decades that catatonic features, regardless of etiology, respond robustly and often quickly to a course of ECT.1,7 But in recent years, the literature has documented the high rates of efficacy of benzodiazepines, usually lorazepam, in the initial treatment of catatonic signs such as mutism, stupor, waxy flexibility, posturing, stereotypies, and rigidity.
Bush et al8 treated 21 acutely catatonic patients, who were so diagnosed according to a standardized catatonia rating scale, with parenteral and oral lorazepam at doses up to 8 mg/d. Sixteen responded dramatically, usually within a day or so. Four of the lorazepam nonresponders were given ECT with excellent results, not only for the catatonic signs but also for other underlying psychopathological features.
Ungvari et al9 treated 18 catatonic patients with either lorazepam or diazepam; all patients had some degree of improvement after several days, but 9 of the 18 exhibited insufficient response. For these, ECT was administered with excellent resolution of the psychopathology, including catatonia.
A reasonable conclusion from these studies is that acutely catatonic patients should be treated first with a benzodiazepine such as parenteral and/or oral lorazepam, perhaps for up to 3 days, and then given ECT if response is insufficient. For patients with malignant catatonia—a particularly severe and life-threatening form of catatonia—ECT may need to be instituted sooner.10
Psychotic features Though the literature has been mixed on this subject, patients with psychotic depression have high response rates to an adequate course of ECT treatments. Hickie et al6 treated 81 depressed patients with ECT and performed in-depth analyses of a variety of clinical variables, including the presence of psychosis. Patients with psychotic depression were found to have a significantly higher rate of ECT response than those with nonpsychotic depression, though the latter still had high response rates.
ECT is considered a primary indication for patients with psychotic depression1,7 for two reasons:
- Response rates are uniformly high.
- If such patients were to receive pharmacotherapy, a neuroleptic with all the potential neurologic side effects inherent in such medication would be needed.
Further, clinical experience reveals that psychotically depressed patients tend to be particularly nonfunctional, to have lost weight, and to be suicidal. Thus, the rapid, definitive benefits of ECT are necessary as first-line therapy.
Age Age has been positively correlated with ECT outcome. Black et al,11 in an analysis of clinical predictors of ECT in several hundred patients, found that older patients responded more favorably to ECT than did younger ones. The study included careful assessments of pre- and post-ECT clinical status.
Tew et al,12 in a well-designed prospective study of several hundred ECT patients, found that those older than age 65 responded to ECT more favorably than those younger than 65. Possible mitigating factors in the younger group were greater medication nonresponsivity prior to ECT and longer illness severity. In another prospective study, Wilkinson et al13 also found superior response rates in patients older than 75.
At minimum, a consensus emerges from the literature that ECT response rates are at least as good in the elderly as in younger patients, an important finding given the often debilitating effects of depressive illness in this population and the high rates of medication nonresponse.
Potential for self-harm ECT is highly effective for suicidal or cachectic individuals. Decades of clinical practice have clearly established that acutely suicidal, depressed patients and those whose poor food and fluid intake has caused nutritional compromise represent urgent indications for ECT.1,7 In particular, recent research suggests that ECT response may be especially rapid in bipolar depressed patients.14
Medication resistance It is common practice for depressed patients to be given ECT after resistance to one or more medications is established. But recent research indicates that patients with medication-refractory depression respond to ECT at roughly half the rate of those who have not had an adequate antidepressant trial.15 Medication-resistant patients also have higher relapse rates post-ECT, even when they do initially respond.
Thus, particularly aggressive treatment regimens may be necessary for medication-refractory patients, including use of bilateral electrode placement and/or higher than usual electrical doses.
Another strategy would be to combine medications with ECT during the index course. While not studied prospectively, one retrospective comparison of ECT patients who were either given or not given concomitant nortriptyline suggests that such a strategy may enhance ECT efficacy.16
Personality factors Over the past few decades, patients with nonmelancholic depression have been variably referred to as neurotic, mood-reactive, hysterical, or personality-disordered. The difficulties inherent in precisely defining and measuring these variables make them difficult to apply to day-to-day practice. The more chaotic and unpredictable the patient’s emotional life, and the more mood-reactive the patient is to life events, the less the chance of substantial ECT benefit. In fact, a recent study indicates that depressed patients with personality disorders, especially from DSM-IV cluster B,4 have lower acute ECT response rates and higher post-ECT relapse rates than do depressed ECT patients without personality disorders.17
ECT: first choice for highly agitated manic patients
From the early days of ECT, it rapidly became the mainstay for treating severe, life-threatening manic states until the advent of neuroleptic drugs in the late 1950s. Large, retrospective studies have shown ECT to be highly effective for manic states.18
Two prospective, random assignment trials in particular document the modality’s efficacy. Small et al19 randomly assigned manic patients to either lithium treatment or ECT. While patients in both groups responded well, response was faster in the ECT group. Sikdar et al20 administered chlorpromazine and either real or sham ECT to manic patients and found that adding ECT to neuroleptic patients’ treatments substantially improved outcomes.
In modern practice, various anticonvulsants have become common for treating mania, and no comparative data between such agents and ECT are available. ECT is reserved for highly agitated, medication-refractory patients. The typical scenario entails a patient who does not respond to high doses of parenteral sedatives or antipsychotics, is in restraints much of the time, and is not cooperating with orally administered medications. In such circumstances, court-ordered approval for ECT is usually needed. Fortunately, in my experience bilateral ECT is almost universally effective for such patients, who are often grateful for their treatment once they achieve euthymia.
Rare uses of ECT in schizophrenia
ECT was commonly used for schizophrenia as well as mania before the advent of neuroleptics7 but is only rarely used for this indication in modern times. Here are the exceptions:1
- For acute exacerbations, especially with florid-positive symptoms such as delusions, hallucinations, disorganized thoughts and behavior, or catatonia. ECT can be remarkably effective in rendering patients compliant with oral medication. From there, patients can be discharged and can proceed with outpatient therapy.
- For the chronically ill patient, if multiple medication trials fail to achieve optimum results. When administered in combination with antipsychotic medication, a trial of ECT may extend whatever benefits accrue from medication.7 In particular, the combination of ECT and neuroleptic medication may be more effective in such cases than either ECT or medication alone.21
Especially for chronically ill patients with schizophrenia, any benefits of an acute course of ECT will likely be short-lived unless maintenance ECT is instituted. In a well-designed study of schizophrenic patients stabilized with a combination of neuroleptic medication and an acute course of ECT, Chanpattana et al22 found that those maintained for 6 months with combination continuation ECT and pharmacotherapy did much better than did those randomly assigned to either modality alone.
Related resources
- Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
- American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.:American Psychiatric Association; 2001.
- Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
Drug brand names
- Methohexital • Amidate, Brevital, Diprivan, Ethrane
- Succinylcholine • Anectine
Disclosure
The author reports no affiliation or financial arrangement with any of the companies whose products are mentioned in this article.
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
1. American Psychiatric Association. Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2nd ed. Washington, D.C.: American Psychiatric Association; 2001.
2. Roberts JM. Prognostic factors in the electroshock treatment of depressive states I. Clinical features from history and examination. J Ment Sci. 1959;105:693-702.
3. Sackeim HA, Rush AJ. Melancholia and response to ECT (letter). Am J Psychiatry. 1995;152(8):1242-1243.
4. American Psychiatric Association. Diagniositc and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
5. Sobin C, Prudic J, Devanand DP, Nobler MS, Sackeim HA. Who responds to electroconvulsive therapy? Br J Psychiatry. 1996;169:322-328.
6. Hickie I, Mason C, et al. Prediction of ECT response: validation of a refined sign-based (CORE) system for defining melancholia. Br J Psychiatry. 1996;169(1):68-74.
7. Abrams R. Electroconvulsive Therapy. 3rd ed. New York: Oxford University Press; 1997.
8. Bush G, Fink M, Petrides G, et al. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137-143.
9. Ungvari GA, Leung CM, Wong MK, Lau J. Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-288.
10. Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry and Clinical Neurosciences. 1994;6:1-13.
11. Black DW, Winokur G, Nasrallah A. A multivariate analysis of the experience of 423 depressed inpatients treated with electroconvulsive therapy. Convulsive Ther. 1993;9:112-120.
12. Tew JD, Jr, Mulsant BH, Haskett RF, et al. Acute efficacy of ECT in the treatment of major depression in the old. Am J Psychiatry. 1999;156:1865-1870.
13. Wilkinson AM, Anderson DN, Peters S. Age and the effects of ECT. Int J Geriatr Psychiatry. 1993;8:401-406.
14. Daly JJ, Prudic J, Devanand DP, et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disorders. 2001;3(2):95-104.
15. Prudic J, Haskett RF, Mulsant B, et al. Resistance to antidepressant medications and short-term clinical response to ECT. Am J Psychiatry. 1996;153(8):985-992.
16. Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convulsive Ther. 1989;5:321-329.
17. Sareen J, Enns MW, Guertin JE. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16(1):43-51.
18. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry. 1994;151:169-176.
19. Small JG, Klapper MH, et al. Electroconvulsive treatment compared with lithium in the management of manic states. Arch Gen Psychiatry. 1988;45:727-732.
20. Sikdar S, Kulhara P, Avasthi A, Singh H. Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry. 1994;164:806-810.
21. Krueger RB, Sackeim HA. Electroconvulsive therapy and schizophrenia. In Schizophrenia. SR Hirsch and D Weinberger, eds. Oxford, England: Blackwell Scientific, 1995;503-545.
22. Chanpattana W, Chakrabhand ML, Sackeim HA, et al. Continuation ECT in treatment-resistant schizophrenia: a controlled study. J ECT. 1999;15:178-192.
23. Sackeim HA, Prudic J, Devanand DP, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral ECT at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425-434.
24. Shapira B, Tubi N, Drexler H, Lidsky D, Calev A, Lerer B. Cost and benefit in the choice of ECT schedule. Twice versus three times weekly ECT. Br J Psychiatry. 1998;172:44-48.
25. Rasmussen KG, Richardson JR, Rummans TA. ECT in the medically ill. Psychiatric Clin North Amer (in press).
Pharmacotherapy of alcohol dependence: How and when to use disulfiram and naltrexone
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
Pharmacotherapy of alcohol dependence: How and when to use disulfiram and naltrexone
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
Alcohol dependence is one of the leading causes of morbidity and mortality in the United States. Approximately 10% of Americans will develop alcoholism at some point in their lives,1 and an estimated 100,000 individuals die each year due to alcohol-related medical complications, automobile accidents, and homicides.2 Alcohol dependence also costs the U.S. billions of dollars annually in health care costs, lost productivity, incarceration, and property destruction.
The search for effective pharmacologic treatments has long been a focus of research. Disulfiram, which causes an aversive reaction when combined with alcohol, was for many years the only medication in use. More recently, the opiate antagonist naltrexone has also been used to treat alcohol-dependent patients.
The homotaurine derivative, acamprosate, has recently shown great promise. Though used widely in Europe,3 it is not approved for use in this country.
This article will therefore focus on disulfiram and naltrexone: their pharmacology, efficacy, side effects, and dosing strategies. We also will present guidelines for discussing each medication with patients and for deciding which, if either, to prescribe.
Differences in pharmacology
Disulfiram Since the serendipitous discovery of its reactive property with alcohol in the 1940s, disulfiram has been used in the pharmacological treatment of alcoholism. The agent disrupts alcohol metabolism by inhibiting the action of aldehyde dehydrogenase, thus blocking the conversion of acetaldehyde to acetate. Accumulation of acetaldehyde, the first metabolite of ethanol, causes numerous unpleasant effects, including flushing, weakness, and nausea.4 In addition to acting on aldehyde dehydrogenase, disulfiram inhibits dopamine-β-hydroxylase.5
Disulfiram is absorbed from the gastrointestinal tract and is rapidly distributed to tissues and organs. It begins to affect alcohol metabolism within 1 to 2 hours, with a peak at 12 hours. It is slowly excreted from the body over the next 2 weeks, although its effects may be lost sooner as the body secretes new enzyme.4
The ethanol-disulfiram reaction is characterized by flushing, throbbing in the head and neck, respiratory difficulty, vomiting, sweating, thirst, weakness, and hypotension ( Table 1). In some cases, the reaction can be fatal.
Naltrexone Following its approval for use in treating opioid dependence in the mid-1980s, the opiate antagonist naltrexone was approved nearly a decade ago for use in treating individuals with alcohol dependence. Research interest in the use of naltrexone for this purpose grew from theories that the endogenous opiate system may be involved in the development of alcohol dependence.6 Two simultaneously published studies in 1992 showed the benefit of naltrexone in alcohol dependence;7-8 this led to its approval by the Food and Drug Administration.
Naltrexone is metabolized to its major metabolite, 6-β-naltrexol, and is then excreted in the urine as both the original compound and this metabolite.9 The half-life of naltrexone in chronic administration is approximately 10 hours; the half-life of 6-β-naltrexol is 12 to 16 hours.
Comparison of efficacy
Disulfiram Results concerning efficacy have been mixed. Initial studies showed promising effects but were limited to anecdotal evidence and case studies. More recent studies have addressed issues relating to proper control groups, compliance, and motivation in evaluating disulfiram’s effect on alcohol consumption. Early studies used placebo groups to control for the effects of counseling or regular medical monitoring. However, no controls were employed to distinguish between the psychological effects of disulfiram (e.g., fear of a reaction) and its pharmacologic effects.
Table 1
SYMPTOMS OF AN ETHANOL-DISULFIRAM REACTION
| • Flushing | • Sweating |
| • Throbbing in head and neck | • Thirst |
| • Respiratory difficulty | • Weakness |
| • Vomiting | • Hypotension |
| The intensity of the reaction is generally related to the amount of alcohol and disulfiram consumed. Because even small amounts of alcohol may cause a reaction, individuals taking disulfiram should avoid all forms of alcohol, including certain mouthwashes and cough syrups. Patients also should be instructed to read the ingredients of foods and medications they consume. | |
| While the recommended daily dose for disulfiram ranges from 125 mg to 500 mg, individuals can vary widely in their reactions. Dosages below 250 mg/d have failed to produce aversive reactions in some individuals who drink alcohol. Dosages of 250 mg/d or higher, however, may cause toxic side effects, including a more severe reaction with alcohol. Clinicians should be aware that in a few patients, the dosage needed to produce an aversive reaction may be higher than the dosage that produces toxicity.4 | |
| The authors generally prescribe 125 mg/d, which is at the low end of the usual dose range, since the fear of a reaction—not the reaction itself—is the major therapeutic action of disulfiram. Moreover, a lower dosage diminishes (but by no means eliminates) the likelihood of a highly dangerous alcohol-disulfiram reaction. | |
Fuller and Roth10 addressed this concern by designing a double-blind study that consisted of 3 groups. Group 1 received disulfiram 250 mg/d, group 2 received 1 mg/d (a pharmacologically ineffective dose), and group 3 received a placebo. Importantly, patients in both groups 1 and 2 were informed that they were receiving disulfiram and were warned of a possible ethanol-disulfiram reaction. At a 6-month follow-up, patients receiving disulfiram showed a small but significant increase in abstinence compared with those receiving placebo. Interestingly, there was no difference between patients receiving 250 mg of disulfiram and those receiving the ineffective 1 mg dose, suggesting that the primary action of disulfiram is the fear of a reaction with alcohol, not the agent’s pharmacologic effects.
A number of studies have shown that patients who agree to take disulfiram and continue taking it are generally highly motivated; such patients unsurprisingly experience better treatment outcomes.
In the largest controlled, blinded study of disulfiram performed to date, Fuller et al11 evaluated disulfiram treatment in 605 male veterans randomly assigned to disulfiram 250 mg a day, disulfiram 1 mg a day, or placebo. No significant differences were found between groups in total abstinence or time to first drink. Among patients who participated in all assessments and who drank at least once during the study, however, those receiving 250 mg had fewer drinking days than those in either control group.
The authors concluded that disulfiram may help reduce drinking frequency after a return to drinking, but does not contribute to continuous abstinence or to delay in time to first drink. Notably, despite a medication compliance rate of only 20%, a significant relationship existed between medication compliance and complete abstinence, regardless of treatment group. O’Farrell and colleagues14 have studied ways to increase compliance with disulfiram, developing the concept of the “Antabuse contract,” in which the patient takes disulfiram in front of a significant other as part of a couple’s therapy program.
How long should a patient continue taking disulfiram? Unfortunately, the ideal length of disulfiram treatment has not been established. While most randomized trials only administer disulfiram for a few months, research by Ojehagen et al15 has shown that long-term treatment (greater than 12 months) with disulfiram is significantly related to positive drinking outcomes during the 2 years following treatment.
Naltrexone The two initial landmark studies of naltrexone for alcohol dependence were published nearly a decade ago. Volpicelli et al7 conducted a double-blind, placebo-controlled trial of naltrexone 50 mg/d for 12 weeks with 70 male veterans who also received intensive psychosocial alcohol rehabilitation. Study participants who received naltrexone had fewer drinking days, less craving for alcohol, and a lower rate of full-blown relapse than did patients who received placebo. The major effect of naltrexone occurred among patients who sampled alcohol; only half of those on naltrexone progressed from first drink to a full-blown relapse, compared to a 95% rate of relapse among those who initiated drinking while receiving placebo.
O’Malley et al8 also found naltrexone to be more effective than placebo and found an interesting interaction with psychosocial treatment. Individuals who received weekly abstinence-oriented supportive therapy were more likely to be continuously abstinent from alcohol at the end of the 12-week study period. Those who received naltrexone along with cognitive behavioral coping skills therapy were least likely to progress to a full-blown relapse if they did drink.
More recently, Anton et al12 conducted a double-blind, placebo-controlled trial of naltrexone in 131 patients, all of whom received cognitive behavioral therapy (CBT). Those receiving naltrexone had a significantly longer period prior to relapse, fewer drinking days, and fewer drinks per drinking day than the placebo group. No significant differences were reported between the groups in time prior to the first drink.
These studies suggest that naltrexone may diminish the likelihood of progression from first drink to full-blown relapse. This may occur through the agent’s attenuation of the reinforcing effects of alcohol.13 While naltrexone does not fully block alcohol the way it blocks opioid drugs, the reduction in alcohol’s positive effects may help naltrexone responders to contain their “slips” and prevent progression to a full-blown relapse.
The difference in adverse effects
Disulfiram Adverse effects (see Table 2) arise from 3 main causes:
- Medical complications during an ethanol-disulfiram reaction;
- Toxicity due to disulfiram or its metabolites;
- Interactions between disulfiram and other medications.
Table 2
HOW DISULFIRAM, NALTREXONE WORK
| Disulfiram | Naltrexone | |
|---|---|---|
| Mechanism of action | Interrupts metabolism of alcohol, leads to a buildup of acetaldehyde | Opiate antagonist, may attenuate reinforcing property of alcohol |
| Recommended dose* | 25-500 mg | 50 mg |
| Side effects and adverse events | Drowsiness, impotence, headache, acne, metallic aftertaste, hepatitis, neuritis, ethanoldisulfiram reaction | Nausea, vomiting, headache, anxiety, dizziness, fatigue, insomnia, elevated liver enzymes |
| *Physicians Desk Reference 55th ed. Montvale, NJ: Medical Economics, 2001 | ||
Medical complications arising from an ethanol-disulfiram reaction can include tachycardia, hypotension, and electrocardiographic changes. Fatalities have been reported due to myocardial infarction or cerebrovascular accident.5 As a result, people with a history of severe myocardial disease should generally not be prescribed disulfiram.
Side effects from disulfiram itself include drowsiness, impotence, headache, acne, and a metallic or garlic-like aftertaste. Toxicity can also lead to psychiatric reactions such as increased depression and psychosis, possibly because of the inhibition of dopamine β–hydroxylase.5
Hepatic and neurological reactions are the most commonly reported toxic reactions.19 Disulfiram-induced hepatitis usually occurs within 2 months of initiation of treatment, but may occur up to 6 months after starting disulfiram.20 This form of liver toxicity is believed to be an allergic or hypersensitivity reaction and can lead to hepatic necrosis and death due to liver failure. Some clinicians recommend obtaining liver function tests at regular intervals (e.g., at baseline, 2 weeks, 4 weeks, then monthly for 6 months), although the optimal frequency of testing after week 2 is not well established.
Neurological reactions make up approximately 20% of the overall reported side effects from disulfiram, with the most frequent diagnosis being polyneuropathy. Other important reported adverse neurological effects include optic and peripheral neuritis.19
Disulfiram interacts with a number of medications, primarily by slowing down their metabolism and thus increasing risk of toxicity. These drugs include phenytoin, theophylline, anticoagulant drugs, isoniazid, and amitriptyline.19 Prior to starting treatment with disulfiram, phenytoin serum levels should be obtained and monitored throughout treatment. Dosage of oral anticoagulant drugs such as warfarin should also be monitored carefully.
Naltrexone The most common side effect is nausea, which typically occurs in the first week of treatment. In the largest study of naltrexone published to date, approximately 10% of naltrexone-treated subjects reported this side effect.16 Other side effects include headache, anxiety, dizziness, fatigue, vomiting, and insomnia.16
Elevated liver enzymes have been reported with use,17 so liver function should be monitored in patients receiving this medication.
It is unclear how often liver function tests should be performed. One text18 recommends baseline assessment of liver function, monthly monitoring for 3 months, then testing every 2 to 6 months afterwards if results are normal.
Other clinical considerations
Disulfiram Individuals with a history of allergy to thiuram derivatives used in rubber vulcanization or pesticides should not be given disulfiram. Caution should also be used with patients suffering from myocardial disease, diabetes mellitus, cirrhosis, hypothyroidism, seizure disorder, or impaired renal function. Finally, patients should not take disulfiram unless they have abstained from alcohol for at least 12 hours.
Naltrexone Although the recommended dosage of naltrexone for alcohol dependence is 50 mg/d, some patients who experience side effects at that dosage may tolerate 25 mg/d, so starting at this lower dose is often advisable. Some researchers are analyzing the effects of higher dosages (e.g., 100 mg/d) because of evidence that higher blood levels of 6-β-naltrexol might improve treatment outcome.9 The optimal dosage of naltrexone for alcohol dependence is currently not settled, however, and may vary among patients.
Patients should be free of opiates for at least 7 days prior to initiating naltrexone; in the case of methadone, a 10- to 14-day opiate-free interval is prudent. Clinicans should wait approximately 4 days after the patient’s last drink before initiating therapy, since starting naltrexone earlier may lead to more side effects.
Educating patients about both agents
Disulfiram This medication is not to be prescribed lightly; only patients who are fully aware of its potential risks should be taking it. Patients need to be both willing and able to avoid alcohol both in beverage and disguised forms (e.g., alcohol-laced cough syrups).
One useful question to ask patients is, “Can you imagine yourself drinking on disulfiram?” Patients who admit that disulfiram would not deter them from drinking, or who cannot commit to avoiding alcohol in any form, should not use this medication.
Naltrexone Some alcohol-dependent patients are interested in taking naltrexone because they have heard that it may diminish the likelihood of progression from initial drink to full-blown relapse, thus helping them to become controlled drinkers.
Bear in mind that naltrexone does not convert alcohol-dependent individuals into controlled drinkers. Rather, you should tell patients that naltrexone may help them return to abstinence more quickly in the event that they do slip. This statement is consistent with the data about naltrexone and helps to establish and reinforce the goal of abstinence for alcohol-dependent patients.
Which medication for which patient?
When considering which, if either, medication to prescribe for an alcohol-dependent patient, you should initially determine whether contraindications exist. (A rubber allergy would preclude disulfiram, for example.) Then obtain a medical evaluation, including liver function tests, prior to initiating either medication.
While the guidelines for adequate liver function to initiate these medications is a matter of controversy, some clinicians recommend that liver enzymes should be twice the upper limit of normal or better, and that the medications should be stopped if liver function tests are 3 times the upper limit of normal or worse. Some clinicians use more liberal or conservative guidelines, although most recommend that an elevated bilirubin contraindicates the use of either agent.
Assuming that the patient is medically able to take either one, tell the patient that there are 2 medications approved for the treatment of alcohol dependence, and briefly describe each. Then ask the patient if he or she is potentially interested in either. Many patients will opt for no pharmacotherapy, some for naltrexone, and a smaller portion for disulfiram. This choice may vary over time, however, based on the patient’s clinical status. By remaining flexible and sharing this decision-making process with the patient, you increase the likelihood of medication compliance.
Current evidence suggests that both disulfiram and naltrexone are effective only in conjunction with alcohol-focused psychosocial treatment; this may include professional alcoholism treatment, support groups such as Alcoholics Anonymous, or, ideally, a combination of the two.
Monitoring compliance and side effects is also critical. By integrating pharmacologic and psychosocial approaches for alcohol-dependent patients, outcomes can be improved for this prevalent and highly treatable population.
Related resources
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) www.niaaa.nih.gov
- American Academy of Addiction Psychiatry (AAAP) www.aaap.org
- American Society of Addiction Medicine (ASAM) www.asam.org
Drug brand names
- Acamprosate • Campral
- Disulfiram • Antabuse
- Isoniazid • Laniazid, Nydrazid
- Naltrexone • ReVia
- Warfarin • Coumadin, Miradon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
1. Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence. Alcohol Alcohol. 1995;30(2):177-186.
2. McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: A clinical review. J Clin Psychiatry. 2001;62(Suppl 20):42-48.
4. Wright C, Moore RD. Disulfiram treatment of alcoholism. Am J Medicine. 1990;88(6):647-655.
5. Sellers EM, Naranjo CA, Peachey JE. Drugs to decrease alcohol consumption. N Engl J Med. 1981;305(21):1255-1262.
6. Cohen G, Collins M. Alkaloids from catecholamines in adrenal tissue: possible role in alcoholism. Science. 1970;167:1749-1751.
7. Volpicelli JR, Alterman AI, Hayashida M, et al. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49(11):876-880.
8. O’Malley SS, Jaffe AJ, Chang G, et al. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881-887.
9. McCaul ME, Wand GS, Rohde C, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156:1758-1764.
10. Fuller RK, Roth HP. Disulfiram for the treatment of alcoholism: An evaluation of 128 men. Ann Intern Med. 1979;90(6):901-904.
11. Fuller RK, Branchey L, Brightwell DR, et al. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA. 1986;256(11):1449-1455.
12. Anton RF, Moak DH, Waid LR, et al. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. Am J Psychiatry. 1999;156(11):1758-1764.
13. Swift RM, Whelihan W, Kuznetsov O, et al. Naltrexone-induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):1463-1467.
14. O’Farrell TJ, Allen JP, Litten RZ. Disulfiram (Antabuse) contracts in treatment of alcoholism. In: Integrating behavioral therapies with medications in the treatment of drug dependence (NIDA research monograph 150). ed by JDBlaine JD and L Onken. Washington, D.C.: National Institute on Drug Abuse, 1995;65-91.
15. Ojehagen A, Skjaerris A, Berglund M. Long-term use of aversive drugs in outpatient alcoholism treatment. Acta Psychiatr Scand. 1991;84(2):185-190.
16. Croop RS, Faulkner EB, Labriola DF, et al. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. Arch Gen Psychiatry. 1997;54(12):1130-1135.
17. Atkinson RL, Berke LK, Drake CR, et al. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419-422.
18. O’Brien CP, Cornish JW. Opioids: Antagonists and partial agonists. In: The American Psychiatric Press Textbook of Substance Abuse Treatment. 2nd ed. Galanter M, Kleber HD, eds. Washington DC: American Psychiatric Press, 1999;281-294.
19. Poulsen HE, Loft S, Andersen M, Andersen JR. Disulfiram therapy—Adverse drug reactions and interactions. Acta Psychiatr Scand. 1992;86:59-66.
20. Mason NA. Disulfiram-induced hepatitis: Case report and review of the literature. DICP. 1989;23(11):872-874.
Terror-related stress: How ready are you to deal with it?
Since September 11, America has carried on under a cloud of fear. Though the cloud is lifting, it will not disappear for months or years. The terrorist attacks on New York City and Washington, DC, the resultant military action in Afghanistan, and the anthrax scare—combined with pervasive, nagging doubts about homeland security and the specter of another possible future terrorist attack—all are straining the nation’s collective emotional well-being.
Psychiatrists in America have reported new cases of terror-inspired acute stress disorder, anxiety, depression, and other illnesses, as well as recurrences of posttraumatic stress disorder (PTSD) in existing patients, in the weeks after the recent attacks and the anthrax scare. What will be the impact on psychiatric practice in the coming months and years?
“We are all at ground zero,” says Kenneth S. Thompson, MD, of Pittsburgh, an experienced disaster psychiatrist. But he and other subspecialists have identified four critical areas in which psychiatrists should be prepared:
- Identifying how terrorist attacks and scares can exacerbate symptoms in patients now in your practice;
- Diagnosing PTSD among comorbid conditions present in existing or new patients;
- Treating—and avoiding over-treatment—of patients with acute stress disorder and PTSD;
- Managing fear in your communities—in response to the Sept. 11 attacks, to the anthrax scare, or in anticipation of an impending catastrophe.
To bring you this special report, the editors of Current Psychiatry have reviewed the literature and interviewed psychiatrists nationwide and in countries such as Israel and Colombia, where terrorism has been a fact of life for years (see “PTSD lessons from Israel, Colombia,”).
Terror and your patients
Which symptoms are you most likely to see in existing patients subsequent to recent events? In the weeks following the Sept. 11 attacks, psychiatrists reported the most commonly seen symptoms as increased anxiety and worsened depression. Sleep disturbances, agoraphobia, suicidality, and severe reactions among patients with personality disorders also were reported.
Patients with previous PTSD or exposure to trauma face a high risk of new or recurrent PTSD in the wake of Sept. 11 than do those not previously exposed to trauma.1 War veterans with prior posttraumatic symptoms have been particularly prone to recurrent PTSD after the attacks. James Allen, MD, of the Department of Psychiatry and Behavioral Sciences at the University of Oklahoma Health Sciences Center, calls this the “additive effect”: patients traumatized by military service in Vietnam experience a recurrence after seeing a major disaster or atrocity. Dr. Allen, who was extensively involved with Oklahoma City’s disaster psychiatry effort after the 1995 bombing there, recalls seeing patients who were traumatized in Vietnam suffer a recurrence after the Alfred P. Murrah Building attack, and then another relapse after Sept. 11.
“The Sept. 11 attacks were very similar to the war for them,” says Juan Corvalan, MD, of the PTSD Unit of the St. Louis Veterans Administration Medical Center, referring to the numerous war veterans he treated after the atrocities. “Seeing it on TV triggered many memories.” By early November, however, many who experienced recurrent PTSD had returned to their pre-Sept. 11 mental states.
Craig Katz, MD, director of emergency psychiatry services at New York’s Mount Sinai Medical Center, says that a patient’s psychiatric history is crucial to determining risk for PTSD or other terror-related sequelae:
“You can recognize that a given person is at high risk for PTSD post-trauma, based on any combination of these factors—having a psychiatric history, past trauma, high exposure to the event, psychosocial problems pre-disaster, or lack of supports post-disaster.”
The clinical interview is a vital tool in assessing patients with suspected PTSD or posttraumatic sequelae, says Arieh Shalev, MD, of the department of psychiatry at Hadassah University Hospital in Jerusalem, Israel. “It provides the opportunity to discuss the traumatic event with the patient, and to listen to his or her perceptions of the event and its effects” in order to carefully appraise the patient’s symptoms.2
The guidelines set forth in the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) remain the gold standard for confirming a diagnosis of PTSD and discerning long-term posttraumatic sequelae from temporary acute stress disorder (Box 1). The guidelines have proved far from foolproof, however, and the existence of psychiatric comorbidities often clouds the picture.

- Exposure to a traumatic event with both of the following present:
- The traumatic event is persistently reexperienced in one or more of the following ways:
- Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three or more of the following:
- Persistent symptoms of increased arousal (not present before the trauma), as indicated by two or more of the following:
- Duration of symptoms in criteria B, C or D exceeds 1 month.
- Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Specify if; Acute: if duration of symptoms is less than 3 months.
Chronic: if symptoms persist 3 months or more.
With delayed onset: if onset of symptoms is at least 6 months after the stressor.
Acute stress disorder, whose symptom pattern is similar to that of PTSD, is distinguished from PTSD because the symptom pattern must occur and resolve within 4 weeks of the traumatic event. If the symptoms persist for more than 1 month and meet the criteria for PTSD, the diagnosis is changed from acute stress disorder to PTSD.
Differential diagnosis of PTSD
Patients with PTSD are more likely to have substantial psychiatric comorbidity than are those without the disorder.3 Possible reasons include suspected self-medication of PTSD symptoms, particularly among patients with substance abuse, and the possible overreporting of symptoms by patients. Psychiatrists should maintain a high level of suspicion for PTSD when managing a new or existing patient with psychopathology.
Citing data from the National Comorbidity Study of the Institute for Social Research at the University of Michigan, Kessler and others in 1995 noted that more than 80 percent of individuals with PTSD meet criteria for at least one other psychiatric diagnosis. Roughly half of PTSD sufferers met criteria for three or more comorbidities.3
Kathleen Brady, MD, professor of psychiatry at the Medical University of South Carolina in Charleston, noted in a 1997 study that affective disorders, other anxiety disorders, somatization, substance abuse, and dissociative disorders are common comorbidities of PTSD.5 Dr. Shalev and colleagues in one study found that a history of major depressive disorder may increase the severity of posttraumatic morbidity.6 Dr. Brady and others also have found that PTSD patients with a comorbid substance abuse disorder experience severe PTSD symptoms while in a withdrawal state.7
| Disorder | Symptoms that overlap with PTSD |
|---|---|
| Adjustment disorder | Extreme response to stressor. Stressor is not necessarily extreme in nature (e.g., spouse leaving, being fired), and the response might not meet criteria for PTSD.4 |
| Depression | Diminished interest, restricted range of affect, sleep difficulties, or poor concentration.5 |
| Dissociative disorders | Inability to recall important information about past trauma, sense of detachment from oneself, derealization, nightmares, flashbacks, startle responses, or lack of affective response (e.g., onset of dissociative fugue may be tied to past trauma).4 |
| Generalized anxiety | Irritability, hypervigilance, or increased startle reflex.5 |
| Obsessive-compulsive disorder | Recurrent intrusive thoughts (not related to trauma in obsessive-compulsive disorder).4 |
| Panic attacks | Heart palpitations or increased heart rate, sense of detachment, nausea or abdominal distress.4 |
| Psychosis | Illusions, hallucinations, or other perceptual disturbances (may be confused with flashbacks in PTSD).4 |
| Substance abuse disorder | Hallucinations, illusions, diminished interest in or avoidance of significant activities, or social estrangement.4 |

PTSD often is overlooked in the presence of other psychiatric diagnoses. Meuser et al in 1998 studied 275 patients with schizophrenia and bipolar disorder. As many as 98 percent of patients reported lifetime exposure to at least one traumatic event. The researchers found diagnosable PTSD in 119 (43 %) of the subjects, but only three (2%) had the diagnosis in their charts.8
In a later study, Dr. Brady and others cited substantial symptom overlap between PTSD and other psychiatric diagnoses, particularly major depressive disorder. This can contribute to underdiagnosis of PTSD, the researchers found.7 (Box 2).

Children also have been experiencing stress disorders since Sept. 11, says Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. Such disorders manifest as sleep disturbances, anxiety, hyperarousal/hyperactivity, and nightmares.
Young children regress and cling to their parents, and are frightened of the dark or noises, Dr, Husain notes. Those who are toilet-trained can suddenly wet the bed, become neurotic, and demand attention. School-age children are more fearful; they may not want to go to school, their schoolwork may decline, and they may have trouble paying attention. Dr. Husain suggests discussing the trauma and devising a plan of action with them in case the trauma recurs.
The media’s role in reporting on the aftermath of the attacks—and triggering traumatic reactions as an unintended consequence—cannot be overlooked. Two recent studies performed after the Oklahoma City bombing suggest that television reports of that atrocity precipitated PTSD symptoms in middle-school children 7 weeks after the bombing,23 and in geographically distant sixth-graders 2 years after the attack.12 It was not clear whether any of these students had prior PTSD or other psychopathology.
Psychiatric education in the schools is especially crucial in light of the school violence that has occurred in America in recent years. Dr. Husain believes that the children who commit violence are victims of abuse. If teachers early on can identify children who show evidence of stress disorders, they can refer them to trained psychiatrists, catching those who need help before tragedies occur. “It is the psychiatric equivalent of CPR,” Dr. Husain says.
Dr. Brady recommends that psychiatrists and primary care physicians routinely screen patients for exposure to traumatic events. Ask patients specifically about their reaction to such events and encourage them to talk about it. Patients often feel either guilty or embarrassed about the traumatic event, or do not believe it affects their presenting complaints, she notes. Other approaches may be needed to identify the risk of PTSD in children (Box 3).
Identifying a traumatic event of an extreme nature, for example, a life-threatening experience, is key to diagnosing PTSD in the presence of comorbidities, Dr. Corvalan says. “Some of the symptoms—such as avoidance, numbing, and increased arousal—are present in other disorders and may have occurred before exposure to the traumatic event.” If they did, he says, PTSD is ruled out.
Gauging the extent of the patient’s exposure to the traumatic event is critical to determining the likelihood of PTSD onset. Dr. Allen, of Oklahoma City, points to studies that show that the closer and longer the patient has been exposed to a catastrophic event, the more likely he or she will develop PTSD.9,10
Julia Frank, MD, associate professor and director of student education and psychiatry at George Washington University in Washington, DC, suggests screening for symptoms that are unique to PTSD as stated in the DSM-IV, such as nightmares, difficulty remembering the traumatic event, and extreme reactions to reminders of the trauma. She also proposes analyzing the past event and the patient’s reaction to it to confirm that it is a source of trauma.
Patients with PTSD symptoms are easily startled by loud or piercing noises. Dr. Shalev says this characteristic sets true PTSD cases apart from other psychopathology, particularly depression. In one study, Israeli combat veterans with PTSD exhibited a more pronounced heart rate and skin conductance when exposed to auditory stimuli than did combat veterans with no PTSD symptoms.11
Drs. Allen and Frank note that patients who have anthrax-related fears and no prior PTSD symptoms are not likely to develop PTSD. They may, however, manifest symptoms of chronic fatigue, fibromyalgia, and generalized anxiety disorder. Patients may be jumpy, intense, or lethargic, with autonomic instability and rapid heart rate. They may feel alienated and mistrustful of the government. A nonspecific stress disorder and mixed anxiety depression are other possible effects.
Who to treat—and how
Psychiatrists nationwide have reported increased patient presentations after the Sept. 11 attacks and throughout the anthrax scare. Studies conducted after the Oklahoma City bombing also suggest that psychiatrists could be seeing more patients in the coming months.12,13 As caseloads increase, so do the questions about who to treat, how, and how to avoid the possibility of overtreatment.
While many clinicians in the United States recently received their first taste of post-terror psychiatry, those in more violent parts of the world are well-versed in helping their patients manage fear.
Israel has repeatedly been at war throughout its 53-year history. During “peacetime,” terrorism and senseless violence have been a way of life.
“Sadly, Israel’s citizens and its medical and paramedical communities have accrued extensive experience in dealing with the ongoing threat of war and terrorist attacks and their sequelae,” says Zeev Kaplan, MD, director of the Beer-Sheva Mental Health Center and professor of psychiatry at the Ben Gurion University School of Medicine in Beer-Sheva.
Similarly, Colombia is a country long plagued by terrorist and gang violence. PTSD has been on the rise the past 5 years, according to Javier Leon-Silva, MD, chief of psychiatry at the Fundación Santafe de Bogotá. “There is not a single day without a terrorist attack in the news,” Dr. Leon-Silva notes. In addition, two major natural disasters in the last 20 years—the Armero flood and the earthquake in the coffee region—have resulted in tens of thousands of casualties.
Exposure to terror in Israel is widespread—be it direct, as a victim or witness, or secondary, as a victim’s close friend or relative. Recurrent PTSD, brought on by direct and indirect exposure, is common, Dr. Kaplan says. Holocaust survivors, almost as numerous within Israel’s population as combat veterans, have been especially prone to recurrent PTSD.
Children are particularly susceptible to PTSD. In Israel, someone’s parent, sibling or classmate often is among the casualties of a terrorist attack, Dr. Kaplan notes. In Colombia, “children grow up influenced by stories about family members or friends who have been victims of the consequences of war and terror, and by strict family security measures concerning behavior,” Dr. Leon-Silva adds.
Because of the Middle East’s volatile history, most of Israel’s psychiatric professionals have hands-on experience in treating traumatized patients in both military and civilian settings. Joseph Zohar, MD, chairman of Israel’s Consortium on PTSD, says that most psychiatrists have served at some point in the Israeli Defense Forces.
Further, as both Israel’s medical community and the public have learned more about PTSD and post-terror anxiety, physicians can now identify affected people more rapidly, and can refer them for treatment, Dr. Kaplan says. Civilians and veterans have access to five regional trauma and post trauma centers. Educators are trained to detect behavioral changes in the young, and Israel’s children are followed into adulthood to assess the long-term effects of terrorist events.
Colombia’s psychiatrists are also well-qualified to treat terror-inspired psychiatric illness, Dr. Leon-Silva says. However, most people in the impoverished nation cannot afford needed medicines, and psychiatrists are hard-pressed to reach many disaster or terror victims.
Dr. Zohar urges psychiatrists here to attend seminars and workshops on PTSD and acute stress reaction. He says such seminars in Israel have taught clinicians the long-term effects of exposure to terror and its effect on families, as well as how to help patients manage acute stress reactions.
Dr. Kaplan feels his U.S. counterparts should incorporate a multidisciplinary approach that addresses bio-medical, psychotherapeutic, familial, and social/occupational rehabilitation. He encourages national and local civic leaders to educate the public about terror-related stress.
Dr. Leon-Silva advises U.S. psychiatrists not to be ashamed to reveal their fears after a terrorist atrocity. “Sometimes expressing how the event impacts you will help the patient be more communicative and will more extensively show the patient’s symptoms.”
“In order to provide effective care to our patients it is necessary to have clear ideas on how to follow criteria for diagnosis and as a consequence for treatment,” Dr. Corvalan says. “The field at times is confusing; patients do not always follow the diagnostic criteria. The needs of the moment, limitations of recourses, intensity and variety of symptoms, urgency of the situation, etc., all conspire to make the job more difficult.”
Patients with anthrax-related anxiety should be encouraged to “try to function as normally as possible and keep an open communication with peers and those who they look to for information,” Dr. Frank notes. Dr. Allen adds that his patients with anthrax-inspired stress have responded well to breathing, meditation and other relaxation techniques.
Treatment of patients who are severely traumatized and exhibit true PTSD symptoms will vary based on severity of exposure, history of prior PTSD, and existence of comorbidities. A combination of pharmacological and psychosocial therapy is the common first-line treatment.
The selective serotonin reuptake inhibitor (SSRI) sertraline is specifically indicated for treating confirmed PTSD symptoms, and several studies have documented the agent’s effectiveness for this use.14,15 Dr. Frank recommends dosages between 50 and 200 mg/d depending on the patient’s body weight or complaint of side effects (e.g., diarrhea, nausea, or sexual dysfunction). Other SSRIs, as well as tricyclics and MAO inhibitors, are alternatives. Fluoxetine, amitriptyline, phenelzine, and imipramine have all been found more effective than a placebo;16-18 paroxetine also has been shown effective in specific populations.19
Kenneth S. Thompson, MD, a Pittsburgh-based disaster psychiatrist who helped coordinate Oklahoma City’s emergency psychiatry effort after the 1995 bombing, identified four stages that the public works through after a major disaster:
- Mobilization. Rebuilding—or just surviving—is foremost on people’s minds immediately after a traumatic event. Many people either throw themselves headfirst into the recovery and cleanup effort, or assist grieving families that have been hardest hit by the disaster. Others fear for their safety and leave town. Feelings of grief and loss are set aside to focus on the needs of the moment.
- Self-importance. As the media reports on their efforts to put their city—and their lives—back together, people at this stage tend to feel they are part of something. Those who have lost family members and coworkers seem to be coping well at this point, and feel as though they can draw ample moral support from friends and neighbors.
- Abandonment. Once the dust settles and the media coverage dies down, people who lost loved ones are left to confront their grief alone. Those who witnessed the tragedy, or who know someone who was killed or injured in the incident, must confront their demons one on one. It is at this point that PTSD and other psychiatric disorders can set in. Those who did not lose a friend or relative feel a more general sense of loss. Worse still, there may be “a disaster after the disaster,” in which a political official or emergency services officer is charged with some type of wrongdoing or abuse of power. People then feel used and betrayed.
- Acceptance. People begin to seek psychiatric or other help in dealing with the trauma, and begin to come to terms with their loss.
Benzodiazapenes also may be prescribed to manage PTSD symptoms. Patients should be counseled against taking these sedating agents in the daytime, however, as they can lead to fogginess, detachment, and trouble functioning.
Assessing the patient’s available social support also is crucial to PTSD treatment. “Do patients talk to other people about the event?” Dr. Frank asks. “Are they trying to get back to a daily routine? Can they make sense of this experience? Are they incorporating the event into a world view?”
Dr. Thompson, the Pittsburgh disaster psychiatrist, agrees. Psychiatrists should encourage their patients to talk more about their trauma and how fear is affecting their lives. “We don’t discuss with our trauma patients as much as we might what the experience has been like for them,” he says.
Small-group therapy is the most conducive approach to psychotherapy for PTSD, according to Dr. Frank, although individual counseling can work in many cases. Several studies have found group therapy effective,20,21 and 12-step group therapy has shown promise in PTSD patients with comorbid substance abuse disorder.22
Managing fear
Just as people grieve and confront death in stages, Dr. Thompson, who helped coordinate Oklahoma City’s disaster psychiatry effort, has discovered that the public usually employs a similar subconscious process to cope with a traumatic event (Box 4).
But Americans have had no time to recover. As U.S. troops seek justice in Afghanistan, back home people grapple with the threat of anthrax contamination and the prospect of another terrorist attack. The ominously enhanced presence of security at airports, major bridges, sporting and entertainment events, and in other aspects of everyday life, has further fueled the sensation that all is not right.
“The September 11 tragedy brings trauma home,” adds Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. “The anthrax scare and the Nov. 12 plane crash of American Airlines Flight 587 only further remind people of their vulnerability and fears. If the anthrax scare were an accident, people would have been relieved. Since the plane crash was ruled an accident, it has offered people a chance to feel more in control. Accidents can be fixed with better maintenance. Terrorism cannot.”
Dr. Katz of New York City and other disaster psychiatrists are urging their colleagues to help manage public fear by reaching out through community efforts.
Dr. Katz is president of the volunteer group Disaster Psychiatry Outreach, which helped coordinate the city’s post-Sept. 11 trauma psychiatry effort. Visitors waiting at New York’s Family Assistance Center, a referral and help center for people who lost family and friends in the World Trade Center attack, were approached by Dr. Katz and other colleagues to let them know that psychiatric services were available if needed. By doing this, he says, Disaster Psychiatry Outreach clinicians have identified, treated, and referred scores of patients with terror-related stress who otherwise would have gone untreated.
Joseph Dorzab, MD, of the Holt-Krock Clinic in Fort Smith, Ark., also has offered his services. Members of his clinic’s psychiatry department have made several TV appearances, and have given and coordinated area lectures. Working with the local mental health association, the department also is starting a community forum called Mental Health Mondays, an open discussion group with coffee and cookies at a local coffee shop.
In Pittsburgh, Dr. Thompson is encouraging psychiatrists to educate their communities about how traumatic events affect the public. He proposes:
- Staging community meetings to brief religious and other leaders on how to manage traumatized people;
- Informing local news editors about the nature of psychiatric disorders;
- Instructing school administrators about detecting signs of distress in children;
- Contacting local government officials to offer input in devising the town’s emergency response plan.
Psychiatrists also can educate themselves about managing public trauma, thanks to scores of studies that have been done in recent years following major man-made and natural disasters, from Mount St. Helens and Hurricane Andrew, to Chernobyl and the Yom Kippur War. Dr. Thompson urges psychiatrists to seek out the papers of prominent leaders in trauma-related psychiatry, mentioning studies by Carol North, MD, Betty Pfefferbaum, MD, and Robert Ursano, MD, as examples. Other sources include the Web sites of the American Psychiatric Association and National Center for PTSD. (See Related Resources.)
In the end, psychiatrists have been well primed for dealing with public disaster—just by treating individual patients whose psychiatric disorders emanated from everyday life, Dr. Thompson says. “Psychiatrists know more about trauma than they recognize.”
- National Center for PTSD Web site
- National Institute of Mental Health:
- Linenthal EJ. The Unfinished Bombing: Oklahoma City in American Memory. Oxford University Press, 2001.
- Norwood AE, Ursano RJ, Fullerton CS. Disaster psychiatry: principles of practice. Psychiatr Q. 2000; 71(3):207-226.
- American Psychiatric Association Web site:
- The Psychiatric Training Manual for Teachers and Mental Health Professionals
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Paroxetine • Paxil
- Phenelzine • Nardil
- Sertraline • Zoloft
1. Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902-7.
2. Shalev AY. What is posttraumtic stress disorder? J Clin Psychiatry. 2001;62(Suppl 17):4-10.
3. Kessler RC, Sonnega A, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-60
4. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association, 2000.
5. Brady KT. Posttraumatic stress disorder and comorbidity: recognizing the many faces of PTSD. J Clin Psychiatry. 1997;58 Suppl 9:12-5.
6. Shalev AY, Freedman S, Peri T, et al. Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry. 1998;155:630-7.
7. Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2000;61 Suppl 7:22-32.
8. Mueser KT, Goodman LB, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 1998;66(3):493-9.
9. Cloitre M, Cohen LR, Edelman RE, Han H. Posttraumatic stress disorder and extent of trauma exposure as correlates of medical problems and perceived health among women with childhood abuse. Women Health. 2001;34(3):1-17.
10. Hodgins GA, Creamer M, Bell R. Risk factors for posttrauma reactions in police officers: a longitudinal study. J Nerv Ment Dis. 2001;189(8):541-7.
11. Orr SP, Solomon Z, Peri T, et al. Physiologic responses to loud tones in Israeli veterans of the 1973 Yom Kippur War. Biol Psychiatry. 1997;41:319-26.
12. Pfefferbaum B, Seale TW, et al. Posttraumatic stress two years after the Oklahoma City Bombing in youths geographically distant from the explosion. Psychiatry 2000;63(4):358-370.
13. Smith DW, Christiansen EH, Vincent R, Hann N. Population effects of the bombing of Oklahoma City. J Oklahoma State Med Association. 1999;92(4):193-198.
14. Londborg PD, Hegel MT, et al. Sertraline treatment of posttraumatic stress disorder: results of 24 weeks of open-label continuation treatment. J Clin Psychiatry. 2001;62(5):325-31.
15. Davidson JR. Pharmacotherapy of generalized anxiety disorder. J Clin Psychiatry. 2001;62 Suppl 11:46-50.discussion 51-2.
16. Connor KM, Sutherland SM, et al. Fluoxetine in post-traumatic stress disorder. Randomised, double-blind study. Br J Psychiatry. 1999;175:17-22.
17. Davidson J, Kudler H, et al. Treatment of posttraumatic stress disorder with amitriptyline and placebo. Arch Gen Psychiatry. 1990;47(3):259-66.
18. Kosten TR, Frank JB, et al. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis. 1991;179(6):366-70.
19. Smajkic A, Weine S, et al. Sertraline, paroxetine, and venlafaxine in refugee posttraumatic stress disorder with depression symptoms. J Trauma Stress. 2001;14(3):445-52.
20. Wolfsdorf BA, Zlotnick C. Affect management in group therapy for women with posttraumatic stress disorder and histories of childhood sexual abuse. J Clin Psychol 2001 Feb;57(2):169-81.
21. Jones L, Brazel D, et al. Group therapy program for African-American veterans with posttraumatic stress disorder. Psychiatr Serv. 2000;51(9):1177-9.
22. Ouimette P, Humphreys K, et al. Self-help group participation among substance use disorder patients with posttraumatic stress disorder. J Subst Abuse Treat. 2001;20(1):25-32.
23. Pfefferbaum B, Nixon SJ, Tivis RD, et al. Television exposure in children after a terrorist incident. Psychiatry. 2001;64(3):202-11.
Since September 11, America has carried on under a cloud of fear. Though the cloud is lifting, it will not disappear for months or years. The terrorist attacks on New York City and Washington, DC, the resultant military action in Afghanistan, and the anthrax scare—combined with pervasive, nagging doubts about homeland security and the specter of another possible future terrorist attack—all are straining the nation’s collective emotional well-being.
Psychiatrists in America have reported new cases of terror-inspired acute stress disorder, anxiety, depression, and other illnesses, as well as recurrences of posttraumatic stress disorder (PTSD) in existing patients, in the weeks after the recent attacks and the anthrax scare. What will be the impact on psychiatric practice in the coming months and years?
“We are all at ground zero,” says Kenneth S. Thompson, MD, of Pittsburgh, an experienced disaster psychiatrist. But he and other subspecialists have identified four critical areas in which psychiatrists should be prepared:
- Identifying how terrorist attacks and scares can exacerbate symptoms in patients now in your practice;
- Diagnosing PTSD among comorbid conditions present in existing or new patients;
- Treating—and avoiding over-treatment—of patients with acute stress disorder and PTSD;
- Managing fear in your communities—in response to the Sept. 11 attacks, to the anthrax scare, or in anticipation of an impending catastrophe.
To bring you this special report, the editors of Current Psychiatry have reviewed the literature and interviewed psychiatrists nationwide and in countries such as Israel and Colombia, where terrorism has been a fact of life for years (see “PTSD lessons from Israel, Colombia,”).
Terror and your patients
Which symptoms are you most likely to see in existing patients subsequent to recent events? In the weeks following the Sept. 11 attacks, psychiatrists reported the most commonly seen symptoms as increased anxiety and worsened depression. Sleep disturbances, agoraphobia, suicidality, and severe reactions among patients with personality disorders also were reported.
Patients with previous PTSD or exposure to trauma face a high risk of new or recurrent PTSD in the wake of Sept. 11 than do those not previously exposed to trauma.1 War veterans with prior posttraumatic symptoms have been particularly prone to recurrent PTSD after the attacks. James Allen, MD, of the Department of Psychiatry and Behavioral Sciences at the University of Oklahoma Health Sciences Center, calls this the “additive effect”: patients traumatized by military service in Vietnam experience a recurrence after seeing a major disaster or atrocity. Dr. Allen, who was extensively involved with Oklahoma City’s disaster psychiatry effort after the 1995 bombing there, recalls seeing patients who were traumatized in Vietnam suffer a recurrence after the Alfred P. Murrah Building attack, and then another relapse after Sept. 11.
“The Sept. 11 attacks were very similar to the war for them,” says Juan Corvalan, MD, of the PTSD Unit of the St. Louis Veterans Administration Medical Center, referring to the numerous war veterans he treated after the atrocities. “Seeing it on TV triggered many memories.” By early November, however, many who experienced recurrent PTSD had returned to their pre-Sept. 11 mental states.
Craig Katz, MD, director of emergency psychiatry services at New York’s Mount Sinai Medical Center, says that a patient’s psychiatric history is crucial to determining risk for PTSD or other terror-related sequelae:
“You can recognize that a given person is at high risk for PTSD post-trauma, based on any combination of these factors—having a psychiatric history, past trauma, high exposure to the event, psychosocial problems pre-disaster, or lack of supports post-disaster.”
The clinical interview is a vital tool in assessing patients with suspected PTSD or posttraumatic sequelae, says Arieh Shalev, MD, of the department of psychiatry at Hadassah University Hospital in Jerusalem, Israel. “It provides the opportunity to discuss the traumatic event with the patient, and to listen to his or her perceptions of the event and its effects” in order to carefully appraise the patient’s symptoms.2
The guidelines set forth in the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) remain the gold standard for confirming a diagnosis of PTSD and discerning long-term posttraumatic sequelae from temporary acute stress disorder (Box 1). The guidelines have proved far from foolproof, however, and the existence of psychiatric comorbidities often clouds the picture.

- Exposure to a traumatic event with both of the following present:
- The traumatic event is persistently reexperienced in one or more of the following ways:
- Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three or more of the following:
- Persistent symptoms of increased arousal (not present before the trauma), as indicated by two or more of the following:
- Duration of symptoms in criteria B, C or D exceeds 1 month.
- Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Specify if; Acute: if duration of symptoms is less than 3 months.
Chronic: if symptoms persist 3 months or more.
With delayed onset: if onset of symptoms is at least 6 months after the stressor.
Acute stress disorder, whose symptom pattern is similar to that of PTSD, is distinguished from PTSD because the symptom pattern must occur and resolve within 4 weeks of the traumatic event. If the symptoms persist for more than 1 month and meet the criteria for PTSD, the diagnosis is changed from acute stress disorder to PTSD.
Differential diagnosis of PTSD
Patients with PTSD are more likely to have substantial psychiatric comorbidity than are those without the disorder.3 Possible reasons include suspected self-medication of PTSD symptoms, particularly among patients with substance abuse, and the possible overreporting of symptoms by patients. Psychiatrists should maintain a high level of suspicion for PTSD when managing a new or existing patient with psychopathology.
Citing data from the National Comorbidity Study of the Institute for Social Research at the University of Michigan, Kessler and others in 1995 noted that more than 80 percent of individuals with PTSD meet criteria for at least one other psychiatric diagnosis. Roughly half of PTSD sufferers met criteria for three or more comorbidities.3
Kathleen Brady, MD, professor of psychiatry at the Medical University of South Carolina in Charleston, noted in a 1997 study that affective disorders, other anxiety disorders, somatization, substance abuse, and dissociative disorders are common comorbidities of PTSD.5 Dr. Shalev and colleagues in one study found that a history of major depressive disorder may increase the severity of posttraumatic morbidity.6 Dr. Brady and others also have found that PTSD patients with a comorbid substance abuse disorder experience severe PTSD symptoms while in a withdrawal state.7
| Disorder | Symptoms that overlap with PTSD |
|---|---|
| Adjustment disorder | Extreme response to stressor. Stressor is not necessarily extreme in nature (e.g., spouse leaving, being fired), and the response might not meet criteria for PTSD.4 |
| Depression | Diminished interest, restricted range of affect, sleep difficulties, or poor concentration.5 |
| Dissociative disorders | Inability to recall important information about past trauma, sense of detachment from oneself, derealization, nightmares, flashbacks, startle responses, or lack of affective response (e.g., onset of dissociative fugue may be tied to past trauma).4 |
| Generalized anxiety | Irritability, hypervigilance, or increased startle reflex.5 |
| Obsessive-compulsive disorder | Recurrent intrusive thoughts (not related to trauma in obsessive-compulsive disorder).4 |
| Panic attacks | Heart palpitations or increased heart rate, sense of detachment, nausea or abdominal distress.4 |
| Psychosis | Illusions, hallucinations, or other perceptual disturbances (may be confused with flashbacks in PTSD).4 |
| Substance abuse disorder | Hallucinations, illusions, diminished interest in or avoidance of significant activities, or social estrangement.4 |

PTSD often is overlooked in the presence of other psychiatric diagnoses. Meuser et al in 1998 studied 275 patients with schizophrenia and bipolar disorder. As many as 98 percent of patients reported lifetime exposure to at least one traumatic event. The researchers found diagnosable PTSD in 119 (43 %) of the subjects, but only three (2%) had the diagnosis in their charts.8
In a later study, Dr. Brady and others cited substantial symptom overlap between PTSD and other psychiatric diagnoses, particularly major depressive disorder. This can contribute to underdiagnosis of PTSD, the researchers found.7 (Box 2).

Children also have been experiencing stress disorders since Sept. 11, says Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. Such disorders manifest as sleep disturbances, anxiety, hyperarousal/hyperactivity, and nightmares.
Young children regress and cling to their parents, and are frightened of the dark or noises, Dr, Husain notes. Those who are toilet-trained can suddenly wet the bed, become neurotic, and demand attention. School-age children are more fearful; they may not want to go to school, their schoolwork may decline, and they may have trouble paying attention. Dr. Husain suggests discussing the trauma and devising a plan of action with them in case the trauma recurs.
The media’s role in reporting on the aftermath of the attacks—and triggering traumatic reactions as an unintended consequence—cannot be overlooked. Two recent studies performed after the Oklahoma City bombing suggest that television reports of that atrocity precipitated PTSD symptoms in middle-school children 7 weeks after the bombing,23 and in geographically distant sixth-graders 2 years after the attack.12 It was not clear whether any of these students had prior PTSD or other psychopathology.
Psychiatric education in the schools is especially crucial in light of the school violence that has occurred in America in recent years. Dr. Husain believes that the children who commit violence are victims of abuse. If teachers early on can identify children who show evidence of stress disorders, they can refer them to trained psychiatrists, catching those who need help before tragedies occur. “It is the psychiatric equivalent of CPR,” Dr. Husain says.
Dr. Brady recommends that psychiatrists and primary care physicians routinely screen patients for exposure to traumatic events. Ask patients specifically about their reaction to such events and encourage them to talk about it. Patients often feel either guilty or embarrassed about the traumatic event, or do not believe it affects their presenting complaints, she notes. Other approaches may be needed to identify the risk of PTSD in children (Box 3).
Identifying a traumatic event of an extreme nature, for example, a life-threatening experience, is key to diagnosing PTSD in the presence of comorbidities, Dr. Corvalan says. “Some of the symptoms—such as avoidance, numbing, and increased arousal—are present in other disorders and may have occurred before exposure to the traumatic event.” If they did, he says, PTSD is ruled out.
Gauging the extent of the patient’s exposure to the traumatic event is critical to determining the likelihood of PTSD onset. Dr. Allen, of Oklahoma City, points to studies that show that the closer and longer the patient has been exposed to a catastrophic event, the more likely he or she will develop PTSD.9,10
Julia Frank, MD, associate professor and director of student education and psychiatry at George Washington University in Washington, DC, suggests screening for symptoms that are unique to PTSD as stated in the DSM-IV, such as nightmares, difficulty remembering the traumatic event, and extreme reactions to reminders of the trauma. She also proposes analyzing the past event and the patient’s reaction to it to confirm that it is a source of trauma.
Patients with PTSD symptoms are easily startled by loud or piercing noises. Dr. Shalev says this characteristic sets true PTSD cases apart from other psychopathology, particularly depression. In one study, Israeli combat veterans with PTSD exhibited a more pronounced heart rate and skin conductance when exposed to auditory stimuli than did combat veterans with no PTSD symptoms.11
Drs. Allen and Frank note that patients who have anthrax-related fears and no prior PTSD symptoms are not likely to develop PTSD. They may, however, manifest symptoms of chronic fatigue, fibromyalgia, and generalized anxiety disorder. Patients may be jumpy, intense, or lethargic, with autonomic instability and rapid heart rate. They may feel alienated and mistrustful of the government. A nonspecific stress disorder and mixed anxiety depression are other possible effects.
Who to treat—and how
Psychiatrists nationwide have reported increased patient presentations after the Sept. 11 attacks and throughout the anthrax scare. Studies conducted after the Oklahoma City bombing also suggest that psychiatrists could be seeing more patients in the coming months.12,13 As caseloads increase, so do the questions about who to treat, how, and how to avoid the possibility of overtreatment.
While many clinicians in the United States recently received their first taste of post-terror psychiatry, those in more violent parts of the world are well-versed in helping their patients manage fear.
Israel has repeatedly been at war throughout its 53-year history. During “peacetime,” terrorism and senseless violence have been a way of life.
“Sadly, Israel’s citizens and its medical and paramedical communities have accrued extensive experience in dealing with the ongoing threat of war and terrorist attacks and their sequelae,” says Zeev Kaplan, MD, director of the Beer-Sheva Mental Health Center and professor of psychiatry at the Ben Gurion University School of Medicine in Beer-Sheva.
Similarly, Colombia is a country long plagued by terrorist and gang violence. PTSD has been on the rise the past 5 years, according to Javier Leon-Silva, MD, chief of psychiatry at the Fundación Santafe de Bogotá. “There is not a single day without a terrorist attack in the news,” Dr. Leon-Silva notes. In addition, two major natural disasters in the last 20 years—the Armero flood and the earthquake in the coffee region—have resulted in tens of thousands of casualties.
Exposure to terror in Israel is widespread—be it direct, as a victim or witness, or secondary, as a victim’s close friend or relative. Recurrent PTSD, brought on by direct and indirect exposure, is common, Dr. Kaplan says. Holocaust survivors, almost as numerous within Israel’s population as combat veterans, have been especially prone to recurrent PTSD.
Children are particularly susceptible to PTSD. In Israel, someone’s parent, sibling or classmate often is among the casualties of a terrorist attack, Dr. Kaplan notes. In Colombia, “children grow up influenced by stories about family members or friends who have been victims of the consequences of war and terror, and by strict family security measures concerning behavior,” Dr. Leon-Silva adds.
Because of the Middle East’s volatile history, most of Israel’s psychiatric professionals have hands-on experience in treating traumatized patients in both military and civilian settings. Joseph Zohar, MD, chairman of Israel’s Consortium on PTSD, says that most psychiatrists have served at some point in the Israeli Defense Forces.
Further, as both Israel’s medical community and the public have learned more about PTSD and post-terror anxiety, physicians can now identify affected people more rapidly, and can refer them for treatment, Dr. Kaplan says. Civilians and veterans have access to five regional trauma and post trauma centers. Educators are trained to detect behavioral changes in the young, and Israel’s children are followed into adulthood to assess the long-term effects of terrorist events.
Colombia’s psychiatrists are also well-qualified to treat terror-inspired psychiatric illness, Dr. Leon-Silva says. However, most people in the impoverished nation cannot afford needed medicines, and psychiatrists are hard-pressed to reach many disaster or terror victims.
Dr. Zohar urges psychiatrists here to attend seminars and workshops on PTSD and acute stress reaction. He says such seminars in Israel have taught clinicians the long-term effects of exposure to terror and its effect on families, as well as how to help patients manage acute stress reactions.
Dr. Kaplan feels his U.S. counterparts should incorporate a multidisciplinary approach that addresses bio-medical, psychotherapeutic, familial, and social/occupational rehabilitation. He encourages national and local civic leaders to educate the public about terror-related stress.
Dr. Leon-Silva advises U.S. psychiatrists not to be ashamed to reveal their fears after a terrorist atrocity. “Sometimes expressing how the event impacts you will help the patient be more communicative and will more extensively show the patient’s symptoms.”
“In order to provide effective care to our patients it is necessary to have clear ideas on how to follow criteria for diagnosis and as a consequence for treatment,” Dr. Corvalan says. “The field at times is confusing; patients do not always follow the diagnostic criteria. The needs of the moment, limitations of recourses, intensity and variety of symptoms, urgency of the situation, etc., all conspire to make the job more difficult.”
Patients with anthrax-related anxiety should be encouraged to “try to function as normally as possible and keep an open communication with peers and those who they look to for information,” Dr. Frank notes. Dr. Allen adds that his patients with anthrax-inspired stress have responded well to breathing, meditation and other relaxation techniques.
Treatment of patients who are severely traumatized and exhibit true PTSD symptoms will vary based on severity of exposure, history of prior PTSD, and existence of comorbidities. A combination of pharmacological and psychosocial therapy is the common first-line treatment.
The selective serotonin reuptake inhibitor (SSRI) sertraline is specifically indicated for treating confirmed PTSD symptoms, and several studies have documented the agent’s effectiveness for this use.14,15 Dr. Frank recommends dosages between 50 and 200 mg/d depending on the patient’s body weight or complaint of side effects (e.g., diarrhea, nausea, or sexual dysfunction). Other SSRIs, as well as tricyclics and MAO inhibitors, are alternatives. Fluoxetine, amitriptyline, phenelzine, and imipramine have all been found more effective than a placebo;16-18 paroxetine also has been shown effective in specific populations.19
Kenneth S. Thompson, MD, a Pittsburgh-based disaster psychiatrist who helped coordinate Oklahoma City’s emergency psychiatry effort after the 1995 bombing, identified four stages that the public works through after a major disaster:
- Mobilization. Rebuilding—or just surviving—is foremost on people’s minds immediately after a traumatic event. Many people either throw themselves headfirst into the recovery and cleanup effort, or assist grieving families that have been hardest hit by the disaster. Others fear for their safety and leave town. Feelings of grief and loss are set aside to focus on the needs of the moment.
- Self-importance. As the media reports on their efforts to put their city—and their lives—back together, people at this stage tend to feel they are part of something. Those who have lost family members and coworkers seem to be coping well at this point, and feel as though they can draw ample moral support from friends and neighbors.
- Abandonment. Once the dust settles and the media coverage dies down, people who lost loved ones are left to confront their grief alone. Those who witnessed the tragedy, or who know someone who was killed or injured in the incident, must confront their demons one on one. It is at this point that PTSD and other psychiatric disorders can set in. Those who did not lose a friend or relative feel a more general sense of loss. Worse still, there may be “a disaster after the disaster,” in which a political official or emergency services officer is charged with some type of wrongdoing or abuse of power. People then feel used and betrayed.
- Acceptance. People begin to seek psychiatric or other help in dealing with the trauma, and begin to come to terms with their loss.
Benzodiazapenes also may be prescribed to manage PTSD symptoms. Patients should be counseled against taking these sedating agents in the daytime, however, as they can lead to fogginess, detachment, and trouble functioning.
Assessing the patient’s available social support also is crucial to PTSD treatment. “Do patients talk to other people about the event?” Dr. Frank asks. “Are they trying to get back to a daily routine? Can they make sense of this experience? Are they incorporating the event into a world view?”
Dr. Thompson, the Pittsburgh disaster psychiatrist, agrees. Psychiatrists should encourage their patients to talk more about their trauma and how fear is affecting their lives. “We don’t discuss with our trauma patients as much as we might what the experience has been like for them,” he says.
Small-group therapy is the most conducive approach to psychotherapy for PTSD, according to Dr. Frank, although individual counseling can work in many cases. Several studies have found group therapy effective,20,21 and 12-step group therapy has shown promise in PTSD patients with comorbid substance abuse disorder.22
Managing fear
Just as people grieve and confront death in stages, Dr. Thompson, who helped coordinate Oklahoma City’s disaster psychiatry effort, has discovered that the public usually employs a similar subconscious process to cope with a traumatic event (Box 4).
But Americans have had no time to recover. As U.S. troops seek justice in Afghanistan, back home people grapple with the threat of anthrax contamination and the prospect of another terrorist attack. The ominously enhanced presence of security at airports, major bridges, sporting and entertainment events, and in other aspects of everyday life, has further fueled the sensation that all is not right.
“The September 11 tragedy brings trauma home,” adds Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. “The anthrax scare and the Nov. 12 plane crash of American Airlines Flight 587 only further remind people of their vulnerability and fears. If the anthrax scare were an accident, people would have been relieved. Since the plane crash was ruled an accident, it has offered people a chance to feel more in control. Accidents can be fixed with better maintenance. Terrorism cannot.”
Dr. Katz of New York City and other disaster psychiatrists are urging their colleagues to help manage public fear by reaching out through community efforts.
Dr. Katz is president of the volunteer group Disaster Psychiatry Outreach, which helped coordinate the city’s post-Sept. 11 trauma psychiatry effort. Visitors waiting at New York’s Family Assistance Center, a referral and help center for people who lost family and friends in the World Trade Center attack, were approached by Dr. Katz and other colleagues to let them know that psychiatric services were available if needed. By doing this, he says, Disaster Psychiatry Outreach clinicians have identified, treated, and referred scores of patients with terror-related stress who otherwise would have gone untreated.
Joseph Dorzab, MD, of the Holt-Krock Clinic in Fort Smith, Ark., also has offered his services. Members of his clinic’s psychiatry department have made several TV appearances, and have given and coordinated area lectures. Working with the local mental health association, the department also is starting a community forum called Mental Health Mondays, an open discussion group with coffee and cookies at a local coffee shop.
In Pittsburgh, Dr. Thompson is encouraging psychiatrists to educate their communities about how traumatic events affect the public. He proposes:
- Staging community meetings to brief religious and other leaders on how to manage traumatized people;
- Informing local news editors about the nature of psychiatric disorders;
- Instructing school administrators about detecting signs of distress in children;
- Contacting local government officials to offer input in devising the town’s emergency response plan.
Psychiatrists also can educate themselves about managing public trauma, thanks to scores of studies that have been done in recent years following major man-made and natural disasters, from Mount St. Helens and Hurricane Andrew, to Chernobyl and the Yom Kippur War. Dr. Thompson urges psychiatrists to seek out the papers of prominent leaders in trauma-related psychiatry, mentioning studies by Carol North, MD, Betty Pfefferbaum, MD, and Robert Ursano, MD, as examples. Other sources include the Web sites of the American Psychiatric Association and National Center for PTSD. (See Related Resources.)
In the end, psychiatrists have been well primed for dealing with public disaster—just by treating individual patients whose psychiatric disorders emanated from everyday life, Dr. Thompson says. “Psychiatrists know more about trauma than they recognize.”
- National Center for PTSD Web site
- National Institute of Mental Health:
- Linenthal EJ. The Unfinished Bombing: Oklahoma City in American Memory. Oxford University Press, 2001.
- Norwood AE, Ursano RJ, Fullerton CS. Disaster psychiatry: principles of practice. Psychiatr Q. 2000; 71(3):207-226.
- American Psychiatric Association Web site:
- The Psychiatric Training Manual for Teachers and Mental Health Professionals
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Paroxetine • Paxil
- Phenelzine • Nardil
- Sertraline • Zoloft
Since September 11, America has carried on under a cloud of fear. Though the cloud is lifting, it will not disappear for months or years. The terrorist attacks on New York City and Washington, DC, the resultant military action in Afghanistan, and the anthrax scare—combined with pervasive, nagging doubts about homeland security and the specter of another possible future terrorist attack—all are straining the nation’s collective emotional well-being.
Psychiatrists in America have reported new cases of terror-inspired acute stress disorder, anxiety, depression, and other illnesses, as well as recurrences of posttraumatic stress disorder (PTSD) in existing patients, in the weeks after the recent attacks and the anthrax scare. What will be the impact on psychiatric practice in the coming months and years?
“We are all at ground zero,” says Kenneth S. Thompson, MD, of Pittsburgh, an experienced disaster psychiatrist. But he and other subspecialists have identified four critical areas in which psychiatrists should be prepared:
- Identifying how terrorist attacks and scares can exacerbate symptoms in patients now in your practice;
- Diagnosing PTSD among comorbid conditions present in existing or new patients;
- Treating—and avoiding over-treatment—of patients with acute stress disorder and PTSD;
- Managing fear in your communities—in response to the Sept. 11 attacks, to the anthrax scare, or in anticipation of an impending catastrophe.
To bring you this special report, the editors of Current Psychiatry have reviewed the literature and interviewed psychiatrists nationwide and in countries such as Israel and Colombia, where terrorism has been a fact of life for years (see “PTSD lessons from Israel, Colombia,”).
Terror and your patients
Which symptoms are you most likely to see in existing patients subsequent to recent events? In the weeks following the Sept. 11 attacks, psychiatrists reported the most commonly seen symptoms as increased anxiety and worsened depression. Sleep disturbances, agoraphobia, suicidality, and severe reactions among patients with personality disorders also were reported.
Patients with previous PTSD or exposure to trauma face a high risk of new or recurrent PTSD in the wake of Sept. 11 than do those not previously exposed to trauma.1 War veterans with prior posttraumatic symptoms have been particularly prone to recurrent PTSD after the attacks. James Allen, MD, of the Department of Psychiatry and Behavioral Sciences at the University of Oklahoma Health Sciences Center, calls this the “additive effect”: patients traumatized by military service in Vietnam experience a recurrence after seeing a major disaster or atrocity. Dr. Allen, who was extensively involved with Oklahoma City’s disaster psychiatry effort after the 1995 bombing there, recalls seeing patients who were traumatized in Vietnam suffer a recurrence after the Alfred P. Murrah Building attack, and then another relapse after Sept. 11.
“The Sept. 11 attacks were very similar to the war for them,” says Juan Corvalan, MD, of the PTSD Unit of the St. Louis Veterans Administration Medical Center, referring to the numerous war veterans he treated after the atrocities. “Seeing it on TV triggered many memories.” By early November, however, many who experienced recurrent PTSD had returned to their pre-Sept. 11 mental states.
Craig Katz, MD, director of emergency psychiatry services at New York’s Mount Sinai Medical Center, says that a patient’s psychiatric history is crucial to determining risk for PTSD or other terror-related sequelae:
“You can recognize that a given person is at high risk for PTSD post-trauma, based on any combination of these factors—having a psychiatric history, past trauma, high exposure to the event, psychosocial problems pre-disaster, or lack of supports post-disaster.”
The clinical interview is a vital tool in assessing patients with suspected PTSD or posttraumatic sequelae, says Arieh Shalev, MD, of the department of psychiatry at Hadassah University Hospital in Jerusalem, Israel. “It provides the opportunity to discuss the traumatic event with the patient, and to listen to his or her perceptions of the event and its effects” in order to carefully appraise the patient’s symptoms.2
The guidelines set forth in the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) remain the gold standard for confirming a diagnosis of PTSD and discerning long-term posttraumatic sequelae from temporary acute stress disorder (Box 1). The guidelines have proved far from foolproof, however, and the existence of psychiatric comorbidities often clouds the picture.

- Exposure to a traumatic event with both of the following present:
- The traumatic event is persistently reexperienced in one or more of the following ways:
- Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three or more of the following:
- Persistent symptoms of increased arousal (not present before the trauma), as indicated by two or more of the following:
- Duration of symptoms in criteria B, C or D exceeds 1 month.
- Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Specify if; Acute: if duration of symptoms is less than 3 months.
Chronic: if symptoms persist 3 months or more.
With delayed onset: if onset of symptoms is at least 6 months after the stressor.
Acute stress disorder, whose symptom pattern is similar to that of PTSD, is distinguished from PTSD because the symptom pattern must occur and resolve within 4 weeks of the traumatic event. If the symptoms persist for more than 1 month and meet the criteria for PTSD, the diagnosis is changed from acute stress disorder to PTSD.
Differential diagnosis of PTSD
Patients with PTSD are more likely to have substantial psychiatric comorbidity than are those without the disorder.3 Possible reasons include suspected self-medication of PTSD symptoms, particularly among patients with substance abuse, and the possible overreporting of symptoms by patients. Psychiatrists should maintain a high level of suspicion for PTSD when managing a new or existing patient with psychopathology.
Citing data from the National Comorbidity Study of the Institute for Social Research at the University of Michigan, Kessler and others in 1995 noted that more than 80 percent of individuals with PTSD meet criteria for at least one other psychiatric diagnosis. Roughly half of PTSD sufferers met criteria for three or more comorbidities.3
Kathleen Brady, MD, professor of psychiatry at the Medical University of South Carolina in Charleston, noted in a 1997 study that affective disorders, other anxiety disorders, somatization, substance abuse, and dissociative disorders are common comorbidities of PTSD.5 Dr. Shalev and colleagues in one study found that a history of major depressive disorder may increase the severity of posttraumatic morbidity.6 Dr. Brady and others also have found that PTSD patients with a comorbid substance abuse disorder experience severe PTSD symptoms while in a withdrawal state.7
| Disorder | Symptoms that overlap with PTSD |
|---|---|
| Adjustment disorder | Extreme response to stressor. Stressor is not necessarily extreme in nature (e.g., spouse leaving, being fired), and the response might not meet criteria for PTSD.4 |
| Depression | Diminished interest, restricted range of affect, sleep difficulties, or poor concentration.5 |
| Dissociative disorders | Inability to recall important information about past trauma, sense of detachment from oneself, derealization, nightmares, flashbacks, startle responses, or lack of affective response (e.g., onset of dissociative fugue may be tied to past trauma).4 |
| Generalized anxiety | Irritability, hypervigilance, or increased startle reflex.5 |
| Obsessive-compulsive disorder | Recurrent intrusive thoughts (not related to trauma in obsessive-compulsive disorder).4 |
| Panic attacks | Heart palpitations or increased heart rate, sense of detachment, nausea or abdominal distress.4 |
| Psychosis | Illusions, hallucinations, or other perceptual disturbances (may be confused with flashbacks in PTSD).4 |
| Substance abuse disorder | Hallucinations, illusions, diminished interest in or avoidance of significant activities, or social estrangement.4 |

PTSD often is overlooked in the presence of other psychiatric diagnoses. Meuser et al in 1998 studied 275 patients with schizophrenia and bipolar disorder. As many as 98 percent of patients reported lifetime exposure to at least one traumatic event. The researchers found diagnosable PTSD in 119 (43 %) of the subjects, but only three (2%) had the diagnosis in their charts.8
In a later study, Dr. Brady and others cited substantial symptom overlap between PTSD and other psychiatric diagnoses, particularly major depressive disorder. This can contribute to underdiagnosis of PTSD, the researchers found.7 (Box 2).

Children also have been experiencing stress disorders since Sept. 11, says Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. Such disorders manifest as sleep disturbances, anxiety, hyperarousal/hyperactivity, and nightmares.
Young children regress and cling to their parents, and are frightened of the dark or noises, Dr, Husain notes. Those who are toilet-trained can suddenly wet the bed, become neurotic, and demand attention. School-age children are more fearful; they may not want to go to school, their schoolwork may decline, and they may have trouble paying attention. Dr. Husain suggests discussing the trauma and devising a plan of action with them in case the trauma recurs.
The media’s role in reporting on the aftermath of the attacks—and triggering traumatic reactions as an unintended consequence—cannot be overlooked. Two recent studies performed after the Oklahoma City bombing suggest that television reports of that atrocity precipitated PTSD symptoms in middle-school children 7 weeks after the bombing,23 and in geographically distant sixth-graders 2 years after the attack.12 It was not clear whether any of these students had prior PTSD or other psychopathology.
Psychiatric education in the schools is especially crucial in light of the school violence that has occurred in America in recent years. Dr. Husain believes that the children who commit violence are victims of abuse. If teachers early on can identify children who show evidence of stress disorders, they can refer them to trained psychiatrists, catching those who need help before tragedies occur. “It is the psychiatric equivalent of CPR,” Dr. Husain says.
Dr. Brady recommends that psychiatrists and primary care physicians routinely screen patients for exposure to traumatic events. Ask patients specifically about their reaction to such events and encourage them to talk about it. Patients often feel either guilty or embarrassed about the traumatic event, or do not believe it affects their presenting complaints, she notes. Other approaches may be needed to identify the risk of PTSD in children (Box 3).
Identifying a traumatic event of an extreme nature, for example, a life-threatening experience, is key to diagnosing PTSD in the presence of comorbidities, Dr. Corvalan says. “Some of the symptoms—such as avoidance, numbing, and increased arousal—are present in other disorders and may have occurred before exposure to the traumatic event.” If they did, he says, PTSD is ruled out.
Gauging the extent of the patient’s exposure to the traumatic event is critical to determining the likelihood of PTSD onset. Dr. Allen, of Oklahoma City, points to studies that show that the closer and longer the patient has been exposed to a catastrophic event, the more likely he or she will develop PTSD.9,10
Julia Frank, MD, associate professor and director of student education and psychiatry at George Washington University in Washington, DC, suggests screening for symptoms that are unique to PTSD as stated in the DSM-IV, such as nightmares, difficulty remembering the traumatic event, and extreme reactions to reminders of the trauma. She also proposes analyzing the past event and the patient’s reaction to it to confirm that it is a source of trauma.
Patients with PTSD symptoms are easily startled by loud or piercing noises. Dr. Shalev says this characteristic sets true PTSD cases apart from other psychopathology, particularly depression. In one study, Israeli combat veterans with PTSD exhibited a more pronounced heart rate and skin conductance when exposed to auditory stimuli than did combat veterans with no PTSD symptoms.11
Drs. Allen and Frank note that patients who have anthrax-related fears and no prior PTSD symptoms are not likely to develop PTSD. They may, however, manifest symptoms of chronic fatigue, fibromyalgia, and generalized anxiety disorder. Patients may be jumpy, intense, or lethargic, with autonomic instability and rapid heart rate. They may feel alienated and mistrustful of the government. A nonspecific stress disorder and mixed anxiety depression are other possible effects.
Who to treat—and how
Psychiatrists nationwide have reported increased patient presentations after the Sept. 11 attacks and throughout the anthrax scare. Studies conducted after the Oklahoma City bombing also suggest that psychiatrists could be seeing more patients in the coming months.12,13 As caseloads increase, so do the questions about who to treat, how, and how to avoid the possibility of overtreatment.
While many clinicians in the United States recently received their first taste of post-terror psychiatry, those in more violent parts of the world are well-versed in helping their patients manage fear.
Israel has repeatedly been at war throughout its 53-year history. During “peacetime,” terrorism and senseless violence have been a way of life.
“Sadly, Israel’s citizens and its medical and paramedical communities have accrued extensive experience in dealing with the ongoing threat of war and terrorist attacks and their sequelae,” says Zeev Kaplan, MD, director of the Beer-Sheva Mental Health Center and professor of psychiatry at the Ben Gurion University School of Medicine in Beer-Sheva.
Similarly, Colombia is a country long plagued by terrorist and gang violence. PTSD has been on the rise the past 5 years, according to Javier Leon-Silva, MD, chief of psychiatry at the Fundación Santafe de Bogotá. “There is not a single day without a terrorist attack in the news,” Dr. Leon-Silva notes. In addition, two major natural disasters in the last 20 years—the Armero flood and the earthquake in the coffee region—have resulted in tens of thousands of casualties.
Exposure to terror in Israel is widespread—be it direct, as a victim or witness, or secondary, as a victim’s close friend or relative. Recurrent PTSD, brought on by direct and indirect exposure, is common, Dr. Kaplan says. Holocaust survivors, almost as numerous within Israel’s population as combat veterans, have been especially prone to recurrent PTSD.
Children are particularly susceptible to PTSD. In Israel, someone’s parent, sibling or classmate often is among the casualties of a terrorist attack, Dr. Kaplan notes. In Colombia, “children grow up influenced by stories about family members or friends who have been victims of the consequences of war and terror, and by strict family security measures concerning behavior,” Dr. Leon-Silva adds.
Because of the Middle East’s volatile history, most of Israel’s psychiatric professionals have hands-on experience in treating traumatized patients in both military and civilian settings. Joseph Zohar, MD, chairman of Israel’s Consortium on PTSD, says that most psychiatrists have served at some point in the Israeli Defense Forces.
Further, as both Israel’s medical community and the public have learned more about PTSD and post-terror anxiety, physicians can now identify affected people more rapidly, and can refer them for treatment, Dr. Kaplan says. Civilians and veterans have access to five regional trauma and post trauma centers. Educators are trained to detect behavioral changes in the young, and Israel’s children are followed into adulthood to assess the long-term effects of terrorist events.
Colombia’s psychiatrists are also well-qualified to treat terror-inspired psychiatric illness, Dr. Leon-Silva says. However, most people in the impoverished nation cannot afford needed medicines, and psychiatrists are hard-pressed to reach many disaster or terror victims.
Dr. Zohar urges psychiatrists here to attend seminars and workshops on PTSD and acute stress reaction. He says such seminars in Israel have taught clinicians the long-term effects of exposure to terror and its effect on families, as well as how to help patients manage acute stress reactions.
Dr. Kaplan feels his U.S. counterparts should incorporate a multidisciplinary approach that addresses bio-medical, psychotherapeutic, familial, and social/occupational rehabilitation. He encourages national and local civic leaders to educate the public about terror-related stress.
Dr. Leon-Silva advises U.S. psychiatrists not to be ashamed to reveal their fears after a terrorist atrocity. “Sometimes expressing how the event impacts you will help the patient be more communicative and will more extensively show the patient’s symptoms.”
“In order to provide effective care to our patients it is necessary to have clear ideas on how to follow criteria for diagnosis and as a consequence for treatment,” Dr. Corvalan says. “The field at times is confusing; patients do not always follow the diagnostic criteria. The needs of the moment, limitations of recourses, intensity and variety of symptoms, urgency of the situation, etc., all conspire to make the job more difficult.”
Patients with anthrax-related anxiety should be encouraged to “try to function as normally as possible and keep an open communication with peers and those who they look to for information,” Dr. Frank notes. Dr. Allen adds that his patients with anthrax-inspired stress have responded well to breathing, meditation and other relaxation techniques.
Treatment of patients who are severely traumatized and exhibit true PTSD symptoms will vary based on severity of exposure, history of prior PTSD, and existence of comorbidities. A combination of pharmacological and psychosocial therapy is the common first-line treatment.
The selective serotonin reuptake inhibitor (SSRI) sertraline is specifically indicated for treating confirmed PTSD symptoms, and several studies have documented the agent’s effectiveness for this use.14,15 Dr. Frank recommends dosages between 50 and 200 mg/d depending on the patient’s body weight or complaint of side effects (e.g., diarrhea, nausea, or sexual dysfunction). Other SSRIs, as well as tricyclics and MAO inhibitors, are alternatives. Fluoxetine, amitriptyline, phenelzine, and imipramine have all been found more effective than a placebo;16-18 paroxetine also has been shown effective in specific populations.19
Kenneth S. Thompson, MD, a Pittsburgh-based disaster psychiatrist who helped coordinate Oklahoma City’s emergency psychiatry effort after the 1995 bombing, identified four stages that the public works through after a major disaster:
- Mobilization. Rebuilding—or just surviving—is foremost on people’s minds immediately after a traumatic event. Many people either throw themselves headfirst into the recovery and cleanup effort, or assist grieving families that have been hardest hit by the disaster. Others fear for their safety and leave town. Feelings of grief and loss are set aside to focus on the needs of the moment.
- Self-importance. As the media reports on their efforts to put their city—and their lives—back together, people at this stage tend to feel they are part of something. Those who have lost family members and coworkers seem to be coping well at this point, and feel as though they can draw ample moral support from friends and neighbors.
- Abandonment. Once the dust settles and the media coverage dies down, people who lost loved ones are left to confront their grief alone. Those who witnessed the tragedy, or who know someone who was killed or injured in the incident, must confront their demons one on one. It is at this point that PTSD and other psychiatric disorders can set in. Those who did not lose a friend or relative feel a more general sense of loss. Worse still, there may be “a disaster after the disaster,” in which a political official or emergency services officer is charged with some type of wrongdoing or abuse of power. People then feel used and betrayed.
- Acceptance. People begin to seek psychiatric or other help in dealing with the trauma, and begin to come to terms with their loss.
Benzodiazapenes also may be prescribed to manage PTSD symptoms. Patients should be counseled against taking these sedating agents in the daytime, however, as they can lead to fogginess, detachment, and trouble functioning.
Assessing the patient’s available social support also is crucial to PTSD treatment. “Do patients talk to other people about the event?” Dr. Frank asks. “Are they trying to get back to a daily routine? Can they make sense of this experience? Are they incorporating the event into a world view?”
Dr. Thompson, the Pittsburgh disaster psychiatrist, agrees. Psychiatrists should encourage their patients to talk more about their trauma and how fear is affecting their lives. “We don’t discuss with our trauma patients as much as we might what the experience has been like for them,” he says.
Small-group therapy is the most conducive approach to psychotherapy for PTSD, according to Dr. Frank, although individual counseling can work in many cases. Several studies have found group therapy effective,20,21 and 12-step group therapy has shown promise in PTSD patients with comorbid substance abuse disorder.22
Managing fear
Just as people grieve and confront death in stages, Dr. Thompson, who helped coordinate Oklahoma City’s disaster psychiatry effort, has discovered that the public usually employs a similar subconscious process to cope with a traumatic event (Box 4).
But Americans have had no time to recover. As U.S. troops seek justice in Afghanistan, back home people grapple with the threat of anthrax contamination and the prospect of another terrorist attack. The ominously enhanced presence of security at airports, major bridges, sporting and entertainment events, and in other aspects of everyday life, has further fueled the sensation that all is not right.
“The September 11 tragedy brings trauma home,” adds Arshad Husain, MD, professor and chief of child and adolescent psychiatry and director of the International Center for Psychosocial Trauma at the University of Missouri-Columbia. “The anthrax scare and the Nov. 12 plane crash of American Airlines Flight 587 only further remind people of their vulnerability and fears. If the anthrax scare were an accident, people would have been relieved. Since the plane crash was ruled an accident, it has offered people a chance to feel more in control. Accidents can be fixed with better maintenance. Terrorism cannot.”
Dr. Katz of New York City and other disaster psychiatrists are urging their colleagues to help manage public fear by reaching out through community efforts.
Dr. Katz is president of the volunteer group Disaster Psychiatry Outreach, which helped coordinate the city’s post-Sept. 11 trauma psychiatry effort. Visitors waiting at New York’s Family Assistance Center, a referral and help center for people who lost family and friends in the World Trade Center attack, were approached by Dr. Katz and other colleagues to let them know that psychiatric services were available if needed. By doing this, he says, Disaster Psychiatry Outreach clinicians have identified, treated, and referred scores of patients with terror-related stress who otherwise would have gone untreated.
Joseph Dorzab, MD, of the Holt-Krock Clinic in Fort Smith, Ark., also has offered his services. Members of his clinic’s psychiatry department have made several TV appearances, and have given and coordinated area lectures. Working with the local mental health association, the department also is starting a community forum called Mental Health Mondays, an open discussion group with coffee and cookies at a local coffee shop.
In Pittsburgh, Dr. Thompson is encouraging psychiatrists to educate their communities about how traumatic events affect the public. He proposes:
- Staging community meetings to brief religious and other leaders on how to manage traumatized people;
- Informing local news editors about the nature of psychiatric disorders;
- Instructing school administrators about detecting signs of distress in children;
- Contacting local government officials to offer input in devising the town’s emergency response plan.
Psychiatrists also can educate themselves about managing public trauma, thanks to scores of studies that have been done in recent years following major man-made and natural disasters, from Mount St. Helens and Hurricane Andrew, to Chernobyl and the Yom Kippur War. Dr. Thompson urges psychiatrists to seek out the papers of prominent leaders in trauma-related psychiatry, mentioning studies by Carol North, MD, Betty Pfefferbaum, MD, and Robert Ursano, MD, as examples. Other sources include the Web sites of the American Psychiatric Association and National Center for PTSD. (See Related Resources.)
In the end, psychiatrists have been well primed for dealing with public disaster—just by treating individual patients whose psychiatric disorders emanated from everyday life, Dr. Thompson says. “Psychiatrists know more about trauma than they recognize.”
- National Center for PTSD Web site
- National Institute of Mental Health:
- Linenthal EJ. The Unfinished Bombing: Oklahoma City in American Memory. Oxford University Press, 2001.
- Norwood AE, Ursano RJ, Fullerton CS. Disaster psychiatry: principles of practice. Psychiatr Q. 2000; 71(3):207-226.
- American Psychiatric Association Web site:
- The Psychiatric Training Manual for Teachers and Mental Health Professionals
Drug brand names
- Amitriptyline • Elavil
- Bupropion • Wellbutrin
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Paroxetine • Paxil
- Phenelzine • Nardil
- Sertraline • Zoloft
1. Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902-7.
2. Shalev AY. What is posttraumtic stress disorder? J Clin Psychiatry. 2001;62(Suppl 17):4-10.
3. Kessler RC, Sonnega A, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-60
4. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association, 2000.
5. Brady KT. Posttraumatic stress disorder and comorbidity: recognizing the many faces of PTSD. J Clin Psychiatry. 1997;58 Suppl 9:12-5.
6. Shalev AY, Freedman S, Peri T, et al. Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry. 1998;155:630-7.
7. Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2000;61 Suppl 7:22-32.
8. Mueser KT, Goodman LB, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 1998;66(3):493-9.
9. Cloitre M, Cohen LR, Edelman RE, Han H. Posttraumatic stress disorder and extent of trauma exposure as correlates of medical problems and perceived health among women with childhood abuse. Women Health. 2001;34(3):1-17.
10. Hodgins GA, Creamer M, Bell R. Risk factors for posttrauma reactions in police officers: a longitudinal study. J Nerv Ment Dis. 2001;189(8):541-7.
11. Orr SP, Solomon Z, Peri T, et al. Physiologic responses to loud tones in Israeli veterans of the 1973 Yom Kippur War. Biol Psychiatry. 1997;41:319-26.
12. Pfefferbaum B, Seale TW, et al. Posttraumatic stress two years after the Oklahoma City Bombing in youths geographically distant from the explosion. Psychiatry 2000;63(4):358-370.
13. Smith DW, Christiansen EH, Vincent R, Hann N. Population effects of the bombing of Oklahoma City. J Oklahoma State Med Association. 1999;92(4):193-198.
14. Londborg PD, Hegel MT, et al. Sertraline treatment of posttraumatic stress disorder: results of 24 weeks of open-label continuation treatment. J Clin Psychiatry. 2001;62(5):325-31.
15. Davidson JR. Pharmacotherapy of generalized anxiety disorder. J Clin Psychiatry. 2001;62 Suppl 11:46-50.discussion 51-2.
16. Connor KM, Sutherland SM, et al. Fluoxetine in post-traumatic stress disorder. Randomised, double-blind study. Br J Psychiatry. 1999;175:17-22.
17. Davidson J, Kudler H, et al. Treatment of posttraumatic stress disorder with amitriptyline and placebo. Arch Gen Psychiatry. 1990;47(3):259-66.
18. Kosten TR, Frank JB, et al. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis. 1991;179(6):366-70.
19. Smajkic A, Weine S, et al. Sertraline, paroxetine, and venlafaxine in refugee posttraumatic stress disorder with depression symptoms. J Trauma Stress. 2001;14(3):445-52.
20. Wolfsdorf BA, Zlotnick C. Affect management in group therapy for women with posttraumatic stress disorder and histories of childhood sexual abuse. J Clin Psychol 2001 Feb;57(2):169-81.
21. Jones L, Brazel D, et al. Group therapy program for African-American veterans with posttraumatic stress disorder. Psychiatr Serv. 2000;51(9):1177-9.
22. Ouimette P, Humphreys K, et al. Self-help group participation among substance use disorder patients with posttraumatic stress disorder. J Subst Abuse Treat. 2001;20(1):25-32.
23. Pfefferbaum B, Nixon SJ, Tivis RD, et al. Television exposure in children after a terrorist incident. Psychiatry. 2001;64(3):202-11.
1. Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902-7.
2. Shalev AY. What is posttraumtic stress disorder? J Clin Psychiatry. 2001;62(Suppl 17):4-10.
3. Kessler RC, Sonnega A, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-60
4. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association, 2000.
5. Brady KT. Posttraumatic stress disorder and comorbidity: recognizing the many faces of PTSD. J Clin Psychiatry. 1997;58 Suppl 9:12-5.
6. Shalev AY, Freedman S, Peri T, et al. Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry. 1998;155:630-7.
7. Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2000;61 Suppl 7:22-32.
8. Mueser KT, Goodman LB, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 1998;66(3):493-9.
9. Cloitre M, Cohen LR, Edelman RE, Han H. Posttraumatic stress disorder and extent of trauma exposure as correlates of medical problems and perceived health among women with childhood abuse. Women Health. 2001;34(3):1-17.
10. Hodgins GA, Creamer M, Bell R. Risk factors for posttrauma reactions in police officers: a longitudinal study. J Nerv Ment Dis. 2001;189(8):541-7.
11. Orr SP, Solomon Z, Peri T, et al. Physiologic responses to loud tones in Israeli veterans of the 1973 Yom Kippur War. Biol Psychiatry. 1997;41:319-26.
12. Pfefferbaum B, Seale TW, et al. Posttraumatic stress two years after the Oklahoma City Bombing in youths geographically distant from the explosion. Psychiatry 2000;63(4):358-370.
13. Smith DW, Christiansen EH, Vincent R, Hann N. Population effects of the bombing of Oklahoma City. J Oklahoma State Med Association. 1999;92(4):193-198.
14. Londborg PD, Hegel MT, et al. Sertraline treatment of posttraumatic stress disorder: results of 24 weeks of open-label continuation treatment. J Clin Psychiatry. 2001;62(5):325-31.
15. Davidson JR. Pharmacotherapy of generalized anxiety disorder. J Clin Psychiatry. 2001;62 Suppl 11:46-50.discussion 51-2.
16. Connor KM, Sutherland SM, et al. Fluoxetine in post-traumatic stress disorder. Randomised, double-blind study. Br J Psychiatry. 1999;175:17-22.
17. Davidson J, Kudler H, et al. Treatment of posttraumatic stress disorder with amitriptyline and placebo. Arch Gen Psychiatry. 1990;47(3):259-66.
18. Kosten TR, Frank JB, et al. Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine. J Nerv Ment Dis. 1991;179(6):366-70.
19. Smajkic A, Weine S, et al. Sertraline, paroxetine, and venlafaxine in refugee posttraumatic stress disorder with depression symptoms. J Trauma Stress. 2001;14(3):445-52.
20. Wolfsdorf BA, Zlotnick C. Affect management in group therapy for women with posttraumatic stress disorder and histories of childhood sexual abuse. J Clin Psychol 2001 Feb;57(2):169-81.
21. Jones L, Brazel D, et al. Group therapy program for African-American veterans with posttraumatic stress disorder. Psychiatr Serv. 2000;51(9):1177-9.
22. Ouimette P, Humphreys K, et al. Self-help group participation among substance use disorder patients with posttraumatic stress disorder. J Subst Abuse Treat. 2001;20(1):25-32.
23. Pfefferbaum B, Nixon SJ, Tivis RD, et al. Television exposure in children after a terrorist incident. Psychiatry. 2001;64(3):202-11.
Excessive daytime sleepiness: Diagnosing the causes
Untreated excessive daytime sleepiness (EDS) results in compromised quality of life, reduced productivity, and public safety concerns.1 Obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, and narcolepsy are frequently underdiagnosed sleep disorders that can cause EDS. These conditions commonly go undetected and untreated for several reasons:
- Patients may not recognize sleepiness as a legitimate medical concern.
- Physicians, with few exceptions, typically have little training in sleep disorders and limited time to diagnose them.2 Screening questions regarding sleep are typically absent.
- Definitive diagnostic tests are costly.
As a result, many patients go without appropriate sleep evaluations. Instead a depressive or other psychiatric disorder may be suspected because of the sleepy patient’s poor energy, hypersomnia, amotivation, irritability, and frustration. Because of ongoing behavioral symptoms, patients with an undiagnosed primary sleep disorder are often referred to psychiatrists. Thus, a clear understanding of the differential diagnosis of EDS is crucial.
Patients with sleep issues fall into three major categories:
- Patients with EDS.
- Individuals with insomnia, another large group often seen by psychiatrists. Generally, these patients are less hesitant than patients with EDS to seek help because of the marked distress they suffer nightly when trying to sleep. Insomniacs typically experience minimal EDS.
- Patients with unusual behaviors at night that range from arm waving to violent behaviors.
Assessing the sleepy patient
When evaluating a patient with sleep complaints, several valuable sources of data come into play.
Initially, observe the patient in the waiting room or office before starting the interview. Did the patient nod off while waiting for his or her appointment? Pay attention to any patient who appears sleepy—even if he or she denies having trouble staying awake. Over time, sleepy patients may have lost their perspective on alertness. Some patients have had EDS for so many years that they no longer recall what it is like to feel fully awake.
Collateral history is often important because family members generally observe the sleeping patient. The bed partner often provides valuable information about snoring, irregular breathing leg kicks, unplanned naps, and strained interpersonal relationships due to EDS. For the patient who does not have a bed partner, ask his or her travel companion, with whom the patient may have shared accommodations.
Unfortunately, few useful screening tests exist. Most questionnaires about sleepiness are neither very reliable nor valid. One of the better questionnaires, the Epworth Sleepiness Scale, helps confirm the presence of sleepiness with a score <8, differentiating the inability to stay awake from fatigue. (Box 1 can be cut out, copied, and handed to patients). This brief questionnaire also provides a useful measure of severity.3
The value of the Epworth scale is limited, however, because patient answers often are based on a specific time and context that may not be representative. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several that focus on OSA.4
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
- 0 no chance of dozing
- 1 slight chance of dozing
- 2 moderate chance of dozing
- 3 high chance of dozing
| Chance of dozing | Situation |
|---|---|
| ○ | Sitting and reading |
| ○ | Watching TV |
| ○ | Sitting inactive in a public place (e.g., a theater or a meeting) |
| ○ | Sitting as a passenger in a car for an hour without a break |
| ○ | Lying down to rest in the afternoon when circumstances permit |
| ○ | Sitting and talking to someone |
| ○ | Sitting quietly after a lunch without alcohol |
| ○ | In a car, while stopped for a few minutes in traffic |
| Johns, M. Sleep 14:540-545, 1991. | |
Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is critical in understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep. At this time, however, no portable devices that employ EEG technology are used in clinical settings.
Additionally, none of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Even though overnight pulse oximetry has been used to screen for sleep-disordered breathing,5 the technology has limitations. For one, most pulse oximeters do not provide information about sleep stage or body position. Some patients with significant sleep-disordered breathing lack adequate oxygen desaturations but have frequent EEG arousals due to sleep issues. In this case, pulse oximetry would generate a false negative result because EEG data is not collected. The inadequate sensitivity is most likely to occur with females and thin patients.
Oximetry provides only one or two types of data (oxygen saturation plus possibly heart rate), while other physiologic processes, e.g., body movement or sleep architecture, can repetitively be disrupted during sleep.
The most critical steps in detecting sleep disorders do not require technology or specialized expertise, but rather intuition and common sense. The psychiatrist should consider the possibility of a sleep disorder and incorporate pertinent questions into the clinical interview. Figure 1 lists sequential questions that might uncover specific sleep disorders. Once suspected, the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder detected.
Diagnosing and treating OSA
Recent epidemiologic studies show that OSA affects at least 4% of men and 2% of women in the United States.6 Psychiatrists are virtually assured of seeing patients with undiagnosed OSA. The condition is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because of sleep fragmented by frequent arousals.
Figure 1 THE SLEEPY PATIENT: Possible medical and psychiatric explanations
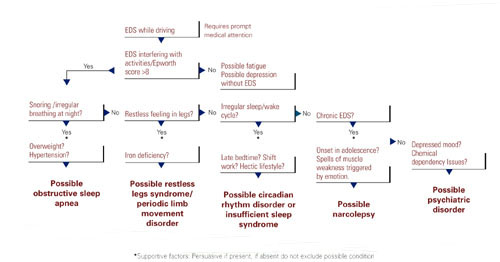
Obese patients are at higher risk than are patients at normal weight because of their body habitus. Alcohol or sedative medication use close to bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold, meaning that patients do not wake readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. New data associate OSA with multiple potential cardiovascular complications (arrhythmias, congestive heart failure, and myocardial infarction).7 Therefore, recognition and treatment are paramount.
The physical examination should focus on detecting nasal obstruction (having the patient sniff separately through each nostril can be helpful), big neck, crowded oropharynx (a low-hanging palate, reddened uvula, enlarged tonsils, large tongue size relative to oropharynx diameter) and jaw structure (particularly a small retrognathic mandible).
Referral for nocturnal polysomnography might be the next step. During a comprehensive sleep study, data is collected about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes (e.g., snoring, coughing) when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation are observed; these typically result in brief shifts in EEG frequency called arousals.
First-line interventions for OSA include avoidance of alcohol within 1 to 2 hours of bedtime, sleeping on the side instead of the back, weight loss (ideally with a regular exercise program), and nasal sprays for allergies.
If the first-line treatments for OSA are ineffective, nasal continuous positive airway pressure (CPAP) works well for almost all patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and the upper airway (Box 2). Some patients benefit from a brief trial of a sleeping medication, e.g., zolpidem or trazodone, for the first 1 to 2 weeks of nasal CPAP usage.

Nasal continuous positive airway pressure (CPAP) must be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent. CPAP can be started during the second half of a “split-night” sleep study after obstructive sleep apnea (OSA) has been diagnosed. Alternatively, the sleep laboratory might ask the patient to return for a second night for a trial of nasal CPAP.
Patients with severe OSA might notice improved sleep quality and reduced EDS, even after only a few hours of use. Such patients sometimes wish to start CPAP treatment immediately.
Overall, advances in masks and equipment have improved patient adherence to CPAP. Such innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many newer machines also have a data microchip that allows the clinician to determine the duration of usage, then use that information to counsel the patient about adherence if necessary.
Patient education also can promote CPAP adherence. Upon being first told they might need to sleep each night wearing a nasal mask, patients often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
As part of a comprehensive approach at the Mayo Sleep Disorders Center, patients watch an educational videotape, tour the sleep laboratory bedrooms before the sleep study, and are carefully fitted for masks. Ideally, the technologists interact with the patient during the sleep study to adjust the headgear and fine-tune other aspects of the equipment. The sleep specialist meets with the patient to compare the baseline diagnostic study results with changes in breathing patterns after a trial of nasal CPAP.
Other useful patient compliance tools include a CPAP informational handout, telephone access to nursing staff, and a 30-day follow-up visit.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner was likely the impetus for the appointment in the first place because of concerns about excessive snoring or apneas.
Image reprinted from Oct. 2001 Mayo Clinic Health Letter with permission of Mayo Foundation for Medical Education and Research, Rochester, MN 55905
Surgical options exist for OSA. The most common procedures are uvulopalatopharyngoplasty (UPPP) and laser-assisted uvulopalatoplasty (LAUP). Other procedures in use include tongue reduction and mandibular advancement.
The response rate to OSA surgery averages around 50% but varies on the patient’s characteristics and procedure selected.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including a deviated nasal septum, large tonsils, a low-hanging palate, and large uvula. Potential complications include nasal regurgitation, voice change, postoperative pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances have a vital niche in OSA treatment. Multiple devices have been developed that open the oropharynx by moving the mandible and tongue out of way. A growing body of data shows that oral appliances improve sleep and reduce EDS and promote patient satisfaction more effectively than nasal CPAP.10 Several studies also show that patients with mild to moderate OSA accept these devices well.
Oral devices do have drawbacks, however. In most settings, effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom fit the oral appliance; this can pose a hardship to patients who live a distance from the provider.
Restless legs syndrome, periodic limb movement disorder
The patient with restless legs syndrome typically reports a restless painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition, which affects 10% of the population, is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Patients can have childhood onset and in some cases there is a familial tendency.
Most patients with restless legs syndrome have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial. Typically, treatment is not instituted in these cases.
The history usually confirms the diagnosis without a sleep study. Sleep studies are used only if a co-existing sleep problem is suspected or if the diagnosis is not clear-cut.
One suspected mechanism of restless legs syndrome is a dopamine-deficient state. A serum ferritin level can help detect a relative iron deficiency, iron being a cofactor for dopamine synthesis.12
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics. Antidepressants have been suspected to worsen this condition but definitive studies are lacking.13
Identifying, correcting circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. Adolescents or young adults are most likely to confront these disorders.
The delayed sleep phase disorder—that is, a persistent pattern of staying up late and “sleeping in” the next morning—is the most common example. A careful assessment will reveal that the patient is getting a satisfactory amount of sleep that occurs at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients can be reluctant to acknowledge the severity of their problem, which can lead to both inaccurate sleep diaries and interviews. A portable device called a wrist actigraph provides data about limb movement, thus more objectively measuring the patient’s sleep schedule.
Psychiatrists frequently encounter patients with delayed sleep phase disorder because of a high degree of comorbidity with depressive disorders.14 The cause of this syndrome is unclear, but environmental factors including light exposure, social patterns, psychological issues, and possibly a genetic substrate, are known to contribute.
A less common circadian rhythm disorder, advanced sleep phase disorder, can also cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A recent report describes a large family with a severe form of this disorder that is linked to an abnormality on chromosome two.15
Relatively few effective treatments have been identified for circadian rhythm disorders. Some patients elect not to pursue therapy, instead selecting activities that fit around their unconventional sleep schedules. Sometimes individuals with delayed sleep phase cannot arrange their education or work hours around their atypical sleep schedules. These patients experience poor early morning academic or work performance due to sleepiness.
The internal circadian clock can be gradually readjusted with either phototherapy or gradual shifting of the major sleep period (Box 4). Stimulant or hypnotic medications generally are not utilized.
Insufficient sleep syndrome
Studies indicate that more people are attempting to burn the candle at both ends and are consequently developing a newly identified condition, insufficient sleep syndrome.16 In our 24-hour society, people often are trying to make do with less than the required 7-1/2 hours sleep per day. This may have adverse consequences to their health. When people are required to perform shift work, the problem is compounded because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek out treatment for fatigue or sleepiness because they are aware of the lifestyle choices that they have made. Still, they might develop psychologic symptoms like irritability, mood swings, and strained interpersonal relationships. These symptoms often will prompt patients to request treatment.
The most common technique is to ask the patient to establish a consistent awakening time and subsequently a regular bedtime. Initially this could be unconventional by societal standards, i.e., bedtime at 5 a.m. and arising at 2 p.m. Once this pattern is in place, the patient gradually shifts the timing by an hour a day. For most patients it is easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. This reinforcement should occur in the morning for delayed sleep phase and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to completely skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. The same modalities listed above must be used to reinforce (or “entrain”) this schedule or the patient will gradually slip back into the previous abnormal sleep-wake rhythm.
Major medical centers and North American metropolitan areas are increasingly developing sleep disorder treatment centers. Insurance companies generally cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or excessive daytime sleepiness (EDS)that jeopardizes safe driving.
The most appropriate conditions for an urgent sleep evaluation are:
- Difficulty staying alert while driving, nocturnal cardiac arrhythmias;
- Frequent observed apneas;
- EDS leading to academic or occupational problems.
Psychiatrists should take a careful history that includes a discussion of the patient’s daily and weekly schedule. Avoid psychostimulant medications. Instead, address the non-negotiable need to get adequate sleep and challenge the patients to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy, a less common sleep disorder, can lead to severe occupational, educational, and family disruption. Narcolepsy, which affects 0.05% of the population, is a potentially debilitating disease of the central nervous system that involves abnormal regulation of REM sleep. EDS is the cardinal symptom, often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which can represent inappropriate intrusion of REM phenomena.
After obtaining a history suggestive of narcolepsy, the psychiatrist should employ either the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS like sleep disorder breathing. In some cases, the REM latency on the overnight sleep study will be less than 20 minutes after sleep onset, which supports the diagnosis of narcolepsy. A multiple sleep latency test (MSLT), a diagnostic test that consists of the patient taking four to five daytime naps, is performed the following day.
Narcolepsy is confirmed if the patient has a mean initial sleep latency of less than 10 minutes during these naps plus at least two REM episodes occurring within 15 minutes after sleep onset.
Recent research shows that most patients who have narcolepsy with cataplexy have undetectable levels of a specific neuropeptide (which is called either hypocretin or orexin) in the cerebrospinal fluid.17 Hypocretin/orexin replacement therapy is a theoretical future possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
Other causes of EDS include unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in Figure 1.
Before pursuing sleep studies (polysomnography or an MSLT), eliminate medications that might confound the results. Such agents include antidepressants, which alter the timing and duration of REM sleep, and sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing. Although initial REM latency provides a potential biologic marker of major depression, this measurement is more often used in research studies than in clinical psychiatry.
Primary insomnia is a distressing inability to sleep at night or nap during the day. This suggests a hyperarousal state in several ways, and is the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also do have EDS. When evaluated, these patients typically endorse at least one of the symptoms in Figure 1. Overnight sleep studies occasionally demonstrate that the insomnia is a symptom of another underlying specific sleep disorder, such as OSA or restless legs syndrome.
Psychiatrists treating a patient with chronic insomnia may appropriately undertake several trials of behavioral interventions or sedating medications before making a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are evaluated by psychiatrists who institute an empiric trial of stimulating antidepressant medications. Use of antidepressants in these situations is unlikely to cause harm, but they might complicate diagnostic testing. When coexisting depression and a primary sleep disorder are confirmed, management of the sleepy patient optimally entails specific treatments that separately target each condition.
Related resources
- National Sleep Foundation www.sleepfoundation.org
- American Academy of Sleep Medicine www.asda.org
- American Sleep Apnea Association www.sleepapnea.org
- Restless Legs Syndrome Foundation www.rls.org
- Association for the Study of Light Therapy and Biological Rhythms www.sltbr.org
Disclosure
The author reports no affiliation or financial arrangements with any of the companies whose products are mentioned in this article.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
1. Ronald J, Delaive K, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep. 1999;22(2):225-29.
2. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc. 2000;48:228-29.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14(6):540-45.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep. 1995;18:167-71.
6. Morrell M, Finn L, Kim H, Peppard P, Badr M, Young T. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med. 2000;162(6):2091-96.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994;343(8897):572-75.
9. Lojander J, Maasilta P, Partinen M, Brander P, Salmi T, Lehtonen H. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-19.
10. Mehta A, Qian J, Petocz P, Darendeliler M, Cistulli P. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med. 2001;163(6):1457-61.
11. Chesson A, Jr, Wise M, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. Sleep. 1999;22(7):961-68.
12. Phillips B, Young T, Finn L, Asher K, Hening W, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys. 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry. 1995;152:602-08.
15. Toh K, Jones C, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science. 2001;291(5506):1040-43.
16. Yoshikawa N, Suzuki S, Ishimoto T, Matsumoto M, Miyagishi T. A case of insufficient sleep syndrome. Psychiatry Clin Neuro. 1998;52(2):200-01.
17. Nishino S, Ripley B, Overeem S, Lammers G, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc. 1990;65:869-82.
Untreated excessive daytime sleepiness (EDS) results in compromised quality of life, reduced productivity, and public safety concerns.1 Obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, and narcolepsy are frequently underdiagnosed sleep disorders that can cause EDS. These conditions commonly go undetected and untreated for several reasons:
- Patients may not recognize sleepiness as a legitimate medical concern.
- Physicians, with few exceptions, typically have little training in sleep disorders and limited time to diagnose them.2 Screening questions regarding sleep are typically absent.
- Definitive diagnostic tests are costly.
As a result, many patients go without appropriate sleep evaluations. Instead a depressive or other psychiatric disorder may be suspected because of the sleepy patient’s poor energy, hypersomnia, amotivation, irritability, and frustration. Because of ongoing behavioral symptoms, patients with an undiagnosed primary sleep disorder are often referred to psychiatrists. Thus, a clear understanding of the differential diagnosis of EDS is crucial.
Patients with sleep issues fall into three major categories:
- Patients with EDS.
- Individuals with insomnia, another large group often seen by psychiatrists. Generally, these patients are less hesitant than patients with EDS to seek help because of the marked distress they suffer nightly when trying to sleep. Insomniacs typically experience minimal EDS.
- Patients with unusual behaviors at night that range from arm waving to violent behaviors.
Assessing the sleepy patient
When evaluating a patient with sleep complaints, several valuable sources of data come into play.
Initially, observe the patient in the waiting room or office before starting the interview. Did the patient nod off while waiting for his or her appointment? Pay attention to any patient who appears sleepy—even if he or she denies having trouble staying awake. Over time, sleepy patients may have lost their perspective on alertness. Some patients have had EDS for so many years that they no longer recall what it is like to feel fully awake.
Collateral history is often important because family members generally observe the sleeping patient. The bed partner often provides valuable information about snoring, irregular breathing leg kicks, unplanned naps, and strained interpersonal relationships due to EDS. For the patient who does not have a bed partner, ask his or her travel companion, with whom the patient may have shared accommodations.
Unfortunately, few useful screening tests exist. Most questionnaires about sleepiness are neither very reliable nor valid. One of the better questionnaires, the Epworth Sleepiness Scale, helps confirm the presence of sleepiness with a score <8, differentiating the inability to stay awake from fatigue. (Box 1 can be cut out, copied, and handed to patients). This brief questionnaire also provides a useful measure of severity.3
The value of the Epworth scale is limited, however, because patient answers often are based on a specific time and context that may not be representative. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several that focus on OSA.4
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
- 0 no chance of dozing
- 1 slight chance of dozing
- 2 moderate chance of dozing
- 3 high chance of dozing
| Chance of dozing | Situation |
|---|---|
| ○ | Sitting and reading |
| ○ | Watching TV |
| ○ | Sitting inactive in a public place (e.g., a theater or a meeting) |
| ○ | Sitting as a passenger in a car for an hour without a break |
| ○ | Lying down to rest in the afternoon when circumstances permit |
| ○ | Sitting and talking to someone |
| ○ | Sitting quietly after a lunch without alcohol |
| ○ | In a car, while stopped for a few minutes in traffic |
| Johns, M. Sleep 14:540-545, 1991. | |
Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is critical in understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep. At this time, however, no portable devices that employ EEG technology are used in clinical settings.
Additionally, none of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Even though overnight pulse oximetry has been used to screen for sleep-disordered breathing,5 the technology has limitations. For one, most pulse oximeters do not provide information about sleep stage or body position. Some patients with significant sleep-disordered breathing lack adequate oxygen desaturations but have frequent EEG arousals due to sleep issues. In this case, pulse oximetry would generate a false negative result because EEG data is not collected. The inadequate sensitivity is most likely to occur with females and thin patients.
Oximetry provides only one or two types of data (oxygen saturation plus possibly heart rate), while other physiologic processes, e.g., body movement or sleep architecture, can repetitively be disrupted during sleep.
The most critical steps in detecting sleep disorders do not require technology or specialized expertise, but rather intuition and common sense. The psychiatrist should consider the possibility of a sleep disorder and incorporate pertinent questions into the clinical interview. Figure 1 lists sequential questions that might uncover specific sleep disorders. Once suspected, the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder detected.
Diagnosing and treating OSA
Recent epidemiologic studies show that OSA affects at least 4% of men and 2% of women in the United States.6 Psychiatrists are virtually assured of seeing patients with undiagnosed OSA. The condition is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because of sleep fragmented by frequent arousals.
Figure 1 THE SLEEPY PATIENT: Possible medical and psychiatric explanations
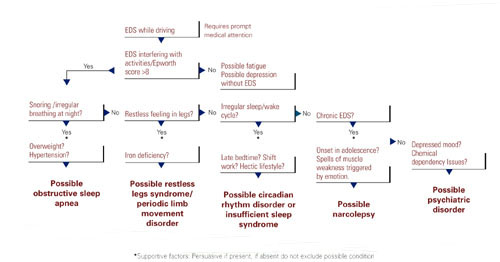
Obese patients are at higher risk than are patients at normal weight because of their body habitus. Alcohol or sedative medication use close to bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold, meaning that patients do not wake readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. New data associate OSA with multiple potential cardiovascular complications (arrhythmias, congestive heart failure, and myocardial infarction).7 Therefore, recognition and treatment are paramount.
The physical examination should focus on detecting nasal obstruction (having the patient sniff separately through each nostril can be helpful), big neck, crowded oropharynx (a low-hanging palate, reddened uvula, enlarged tonsils, large tongue size relative to oropharynx diameter) and jaw structure (particularly a small retrognathic mandible).
Referral for nocturnal polysomnography might be the next step. During a comprehensive sleep study, data is collected about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes (e.g., snoring, coughing) when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation are observed; these typically result in brief shifts in EEG frequency called arousals.
First-line interventions for OSA include avoidance of alcohol within 1 to 2 hours of bedtime, sleeping on the side instead of the back, weight loss (ideally with a regular exercise program), and nasal sprays for allergies.
If the first-line treatments for OSA are ineffective, nasal continuous positive airway pressure (CPAP) works well for almost all patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and the upper airway (Box 2). Some patients benefit from a brief trial of a sleeping medication, e.g., zolpidem or trazodone, for the first 1 to 2 weeks of nasal CPAP usage.

Nasal continuous positive airway pressure (CPAP) must be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent. CPAP can be started during the second half of a “split-night” sleep study after obstructive sleep apnea (OSA) has been diagnosed. Alternatively, the sleep laboratory might ask the patient to return for a second night for a trial of nasal CPAP.
Patients with severe OSA might notice improved sleep quality and reduced EDS, even after only a few hours of use. Such patients sometimes wish to start CPAP treatment immediately.
Overall, advances in masks and equipment have improved patient adherence to CPAP. Such innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many newer machines also have a data microchip that allows the clinician to determine the duration of usage, then use that information to counsel the patient about adherence if necessary.
Patient education also can promote CPAP adherence. Upon being first told they might need to sleep each night wearing a nasal mask, patients often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
As part of a comprehensive approach at the Mayo Sleep Disorders Center, patients watch an educational videotape, tour the sleep laboratory bedrooms before the sleep study, and are carefully fitted for masks. Ideally, the technologists interact with the patient during the sleep study to adjust the headgear and fine-tune other aspects of the equipment. The sleep specialist meets with the patient to compare the baseline diagnostic study results with changes in breathing patterns after a trial of nasal CPAP.
Other useful patient compliance tools include a CPAP informational handout, telephone access to nursing staff, and a 30-day follow-up visit.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner was likely the impetus for the appointment in the first place because of concerns about excessive snoring or apneas.
Image reprinted from Oct. 2001 Mayo Clinic Health Letter with permission of Mayo Foundation for Medical Education and Research, Rochester, MN 55905
Surgical options exist for OSA. The most common procedures are uvulopalatopharyngoplasty (UPPP) and laser-assisted uvulopalatoplasty (LAUP). Other procedures in use include tongue reduction and mandibular advancement.
The response rate to OSA surgery averages around 50% but varies on the patient’s characteristics and procedure selected.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including a deviated nasal septum, large tonsils, a low-hanging palate, and large uvula. Potential complications include nasal regurgitation, voice change, postoperative pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances have a vital niche in OSA treatment. Multiple devices have been developed that open the oropharynx by moving the mandible and tongue out of way. A growing body of data shows that oral appliances improve sleep and reduce EDS and promote patient satisfaction more effectively than nasal CPAP.10 Several studies also show that patients with mild to moderate OSA accept these devices well.
Oral devices do have drawbacks, however. In most settings, effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom fit the oral appliance; this can pose a hardship to patients who live a distance from the provider.
Restless legs syndrome, periodic limb movement disorder
The patient with restless legs syndrome typically reports a restless painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition, which affects 10% of the population, is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Patients can have childhood onset and in some cases there is a familial tendency.
Most patients with restless legs syndrome have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial. Typically, treatment is not instituted in these cases.
The history usually confirms the diagnosis without a sleep study. Sleep studies are used only if a co-existing sleep problem is suspected or if the diagnosis is not clear-cut.
One suspected mechanism of restless legs syndrome is a dopamine-deficient state. A serum ferritin level can help detect a relative iron deficiency, iron being a cofactor for dopamine synthesis.12
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics. Antidepressants have been suspected to worsen this condition but definitive studies are lacking.13
Identifying, correcting circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. Adolescents or young adults are most likely to confront these disorders.
The delayed sleep phase disorder—that is, a persistent pattern of staying up late and “sleeping in” the next morning—is the most common example. A careful assessment will reveal that the patient is getting a satisfactory amount of sleep that occurs at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients can be reluctant to acknowledge the severity of their problem, which can lead to both inaccurate sleep diaries and interviews. A portable device called a wrist actigraph provides data about limb movement, thus more objectively measuring the patient’s sleep schedule.
Psychiatrists frequently encounter patients with delayed sleep phase disorder because of a high degree of comorbidity with depressive disorders.14 The cause of this syndrome is unclear, but environmental factors including light exposure, social patterns, psychological issues, and possibly a genetic substrate, are known to contribute.
A less common circadian rhythm disorder, advanced sleep phase disorder, can also cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A recent report describes a large family with a severe form of this disorder that is linked to an abnormality on chromosome two.15
Relatively few effective treatments have been identified for circadian rhythm disorders. Some patients elect not to pursue therapy, instead selecting activities that fit around their unconventional sleep schedules. Sometimes individuals with delayed sleep phase cannot arrange their education or work hours around their atypical sleep schedules. These patients experience poor early morning academic or work performance due to sleepiness.
The internal circadian clock can be gradually readjusted with either phototherapy or gradual shifting of the major sleep period (Box 4). Stimulant or hypnotic medications generally are not utilized.
Insufficient sleep syndrome
Studies indicate that more people are attempting to burn the candle at both ends and are consequently developing a newly identified condition, insufficient sleep syndrome.16 In our 24-hour society, people often are trying to make do with less than the required 7-1/2 hours sleep per day. This may have adverse consequences to their health. When people are required to perform shift work, the problem is compounded because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek out treatment for fatigue or sleepiness because they are aware of the lifestyle choices that they have made. Still, they might develop psychologic symptoms like irritability, mood swings, and strained interpersonal relationships. These symptoms often will prompt patients to request treatment.
The most common technique is to ask the patient to establish a consistent awakening time and subsequently a regular bedtime. Initially this could be unconventional by societal standards, i.e., bedtime at 5 a.m. and arising at 2 p.m. Once this pattern is in place, the patient gradually shifts the timing by an hour a day. For most patients it is easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. This reinforcement should occur in the morning for delayed sleep phase and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to completely skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. The same modalities listed above must be used to reinforce (or “entrain”) this schedule or the patient will gradually slip back into the previous abnormal sleep-wake rhythm.
Major medical centers and North American metropolitan areas are increasingly developing sleep disorder treatment centers. Insurance companies generally cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or excessive daytime sleepiness (EDS)that jeopardizes safe driving.
The most appropriate conditions for an urgent sleep evaluation are:
- Difficulty staying alert while driving, nocturnal cardiac arrhythmias;
- Frequent observed apneas;
- EDS leading to academic or occupational problems.
Psychiatrists should take a careful history that includes a discussion of the patient’s daily and weekly schedule. Avoid psychostimulant medications. Instead, address the non-negotiable need to get adequate sleep and challenge the patients to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy, a less common sleep disorder, can lead to severe occupational, educational, and family disruption. Narcolepsy, which affects 0.05% of the population, is a potentially debilitating disease of the central nervous system that involves abnormal regulation of REM sleep. EDS is the cardinal symptom, often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which can represent inappropriate intrusion of REM phenomena.
After obtaining a history suggestive of narcolepsy, the psychiatrist should employ either the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS like sleep disorder breathing. In some cases, the REM latency on the overnight sleep study will be less than 20 minutes after sleep onset, which supports the diagnosis of narcolepsy. A multiple sleep latency test (MSLT), a diagnostic test that consists of the patient taking four to five daytime naps, is performed the following day.
Narcolepsy is confirmed if the patient has a mean initial sleep latency of less than 10 minutes during these naps plus at least two REM episodes occurring within 15 minutes after sleep onset.
Recent research shows that most patients who have narcolepsy with cataplexy have undetectable levels of a specific neuropeptide (which is called either hypocretin or orexin) in the cerebrospinal fluid.17 Hypocretin/orexin replacement therapy is a theoretical future possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
Other causes of EDS include unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in Figure 1.
Before pursuing sleep studies (polysomnography or an MSLT), eliminate medications that might confound the results. Such agents include antidepressants, which alter the timing and duration of REM sleep, and sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing. Although initial REM latency provides a potential biologic marker of major depression, this measurement is more often used in research studies than in clinical psychiatry.
Primary insomnia is a distressing inability to sleep at night or nap during the day. This suggests a hyperarousal state in several ways, and is the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also do have EDS. When evaluated, these patients typically endorse at least one of the symptoms in Figure 1. Overnight sleep studies occasionally demonstrate that the insomnia is a symptom of another underlying specific sleep disorder, such as OSA or restless legs syndrome.
Psychiatrists treating a patient with chronic insomnia may appropriately undertake several trials of behavioral interventions or sedating medications before making a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are evaluated by psychiatrists who institute an empiric trial of stimulating antidepressant medications. Use of antidepressants in these situations is unlikely to cause harm, but they might complicate diagnostic testing. When coexisting depression and a primary sleep disorder are confirmed, management of the sleepy patient optimally entails specific treatments that separately target each condition.
Related resources
- National Sleep Foundation www.sleepfoundation.org
- American Academy of Sleep Medicine www.asda.org
- American Sleep Apnea Association www.sleepapnea.org
- Restless Legs Syndrome Foundation www.rls.org
- Association for the Study of Light Therapy and Biological Rhythms www.sltbr.org
Disclosure
The author reports no affiliation or financial arrangements with any of the companies whose products are mentioned in this article.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
Untreated excessive daytime sleepiness (EDS) results in compromised quality of life, reduced productivity, and public safety concerns.1 Obstructive sleep apnea (OSA), restless legs syndrome, circadian rhythm disorders, and narcolepsy are frequently underdiagnosed sleep disorders that can cause EDS. These conditions commonly go undetected and untreated for several reasons:
- Patients may not recognize sleepiness as a legitimate medical concern.
- Physicians, with few exceptions, typically have little training in sleep disorders and limited time to diagnose them.2 Screening questions regarding sleep are typically absent.
- Definitive diagnostic tests are costly.
As a result, many patients go without appropriate sleep evaluations. Instead a depressive or other psychiatric disorder may be suspected because of the sleepy patient’s poor energy, hypersomnia, amotivation, irritability, and frustration. Because of ongoing behavioral symptoms, patients with an undiagnosed primary sleep disorder are often referred to psychiatrists. Thus, a clear understanding of the differential diagnosis of EDS is crucial.
Patients with sleep issues fall into three major categories:
- Patients with EDS.
- Individuals with insomnia, another large group often seen by psychiatrists. Generally, these patients are less hesitant than patients with EDS to seek help because of the marked distress they suffer nightly when trying to sleep. Insomniacs typically experience minimal EDS.
- Patients with unusual behaviors at night that range from arm waving to violent behaviors.
Assessing the sleepy patient
When evaluating a patient with sleep complaints, several valuable sources of data come into play.
Initially, observe the patient in the waiting room or office before starting the interview. Did the patient nod off while waiting for his or her appointment? Pay attention to any patient who appears sleepy—even if he or she denies having trouble staying awake. Over time, sleepy patients may have lost their perspective on alertness. Some patients have had EDS for so many years that they no longer recall what it is like to feel fully awake.
Collateral history is often important because family members generally observe the sleeping patient. The bed partner often provides valuable information about snoring, irregular breathing leg kicks, unplanned naps, and strained interpersonal relationships due to EDS. For the patient who does not have a bed partner, ask his or her travel companion, with whom the patient may have shared accommodations.
Unfortunately, few useful screening tests exist. Most questionnaires about sleepiness are neither very reliable nor valid. One of the better questionnaires, the Epworth Sleepiness Scale, helps confirm the presence of sleepiness with a score <8, differentiating the inability to stay awake from fatigue. (Box 1 can be cut out, copied, and handed to patients). This brief questionnaire also provides a useful measure of severity.3
The value of the Epworth scale is limited, however, because patient answers often are based on a specific time and context that may not be representative. Additional validated surveys include the Pittsburgh Sleep Quality Inventory and several that focus on OSA.4
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? Even if you have not done some of these things recently, try to work out how each situation would affect you now. Use the scale below to choose the most appropriate number for each situation:
- 0 no chance of dozing
- 1 slight chance of dozing
- 2 moderate chance of dozing
- 3 high chance of dozing
| Chance of dozing | Situation |
|---|---|
| ○ | Sitting and reading |
| ○ | Watching TV |
| ○ | Sitting inactive in a public place (e.g., a theater or a meeting) |
| ○ | Sitting as a passenger in a car for an hour without a break |
| ○ | Lying down to rest in the afternoon when circumstances permit |
| ○ | Sitting and talking to someone |
| ○ | Sitting quietly after a lunch without alcohol |
| ○ | In a car, while stopped for a few minutes in traffic |
| Johns, M. Sleep 14:540-545, 1991. | |
Electroencephalographic (EEG) monitoring can accurately measure the patient’s degree of sleep disruption. This information is critical in understanding if a patient’s EDS is caused by a physiologic condition that prevents quality nocturnal sleep. At this time, however, no portable devices that employ EEG technology are used in clinical settings.
Additionally, none of the widely used screening devices that assess leg kicks indicate the presence of possible periodic limb movements.
Even though overnight pulse oximetry has been used to screen for sleep-disordered breathing,5 the technology has limitations. For one, most pulse oximeters do not provide information about sleep stage or body position. Some patients with significant sleep-disordered breathing lack adequate oxygen desaturations but have frequent EEG arousals due to sleep issues. In this case, pulse oximetry would generate a false negative result because EEG data is not collected. The inadequate sensitivity is most likely to occur with females and thin patients.
Oximetry provides only one or two types of data (oxygen saturation plus possibly heart rate), while other physiologic processes, e.g., body movement or sleep architecture, can repetitively be disrupted during sleep.
The most critical steps in detecting sleep disorders do not require technology or specialized expertise, but rather intuition and common sense. The psychiatrist should consider the possibility of a sleep disorder and incorporate pertinent questions into the clinical interview. Figure 1 lists sequential questions that might uncover specific sleep disorders. Once suspected, the decision whether to refer the patient to a sleep disorder center for diagnostic testing depends on the type of sleep disorder detected.
Diagnosing and treating OSA
Recent epidemiologic studies show that OSA affects at least 4% of men and 2% of women in the United States.6 Psychiatrists are virtually assured of seeing patients with undiagnosed OSA. The condition is caused by repeated collapse of the soft tissues surrounding the upper airway, decreasing airflow that is restored when the patient briefly awakens. Patients develop EDS because of sleep fragmented by frequent arousals.
Figure 1 THE SLEEPY PATIENT: Possible medical and psychiatric explanations
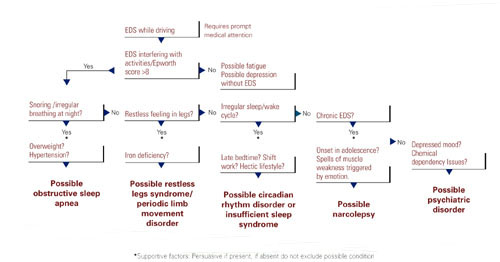
Obese patients are at higher risk than are patients at normal weight because of their body habitus. Alcohol or sedative medication use close to bedtime can aggravate OSA. These substances promote muscle relaxation and increase the arousal threshold, meaning that patients do not wake readily when apneas occur.
Long-term complications of untreated OSA include sleepiness leading to accidents, hypertension, cerebrovascular disease, and progressive obesity. New data associate OSA with multiple potential cardiovascular complications (arrhythmias, congestive heart failure, and myocardial infarction).7 Therefore, recognition and treatment are paramount.
The physical examination should focus on detecting nasal obstruction (having the patient sniff separately through each nostril can be helpful), big neck, crowded oropharynx (a low-hanging palate, reddened uvula, enlarged tonsils, large tongue size relative to oropharynx diameter) and jaw structure (particularly a small retrognathic mandible).
Referral for nocturnal polysomnography might be the next step. During a comprehensive sleep study, data is collected about respiratory, cardiovascular, and muscle activity at night, as well as the sounds the patient makes (e.g., snoring, coughing) when asleep. EEG monitoring also is performed. OSA may be diagnosed if repeated episodes of reduced airflow and oxygen desaturation are observed; these typically result in brief shifts in EEG frequency called arousals.
First-line interventions for OSA include avoidance of alcohol within 1 to 2 hours of bedtime, sleeping on the side instead of the back, weight loss (ideally with a regular exercise program), and nasal sprays for allergies.
If the first-line treatments for OSA are ineffective, nasal continuous positive airway pressure (CPAP) works well for almost all patients who adhere to the regimen.8 CPAP requires the patient to wear a nasal mask that delivers room air, splinting open the nasopharynx and the upper airway (Box 2). Some patients benefit from a brief trial of a sleeping medication, e.g., zolpidem or trazodone, for the first 1 to 2 weeks of nasal CPAP usage.

Nasal continuous positive airway pressure (CPAP) must be started in an observed setting so that the clinician can determine the optimal amount of positive pressure needed to keep the upper airway patent. CPAP can be started during the second half of a “split-night” sleep study after obstructive sleep apnea (OSA) has been diagnosed. Alternatively, the sleep laboratory might ask the patient to return for a second night for a trial of nasal CPAP.
Patients with severe OSA might notice improved sleep quality and reduced EDS, even after only a few hours of use. Such patients sometimes wish to start CPAP treatment immediately.
Overall, advances in masks and equipment have improved patient adherence to CPAP. Such innovations include auto-titrating machines, in which the pressure level can be varied depending on sleep state or body position. Many newer machines also have a data microchip that allows the clinician to determine the duration of usage, then use that information to counsel the patient about adherence if necessary.
Patient education also can promote CPAP adherence. Upon being first told they might need to sleep each night wearing a nasal mask, patients often voice well-founded concerns about comfort, claustrophobia, or sexual activity.
As part of a comprehensive approach at the Mayo Sleep Disorders Center, patients watch an educational videotape, tour the sleep laboratory bedrooms before the sleep study, and are carefully fitted for masks. Ideally, the technologists interact with the patient during the sleep study to adjust the headgear and fine-tune other aspects of the equipment. The sleep specialist meets with the patient to compare the baseline diagnostic study results with changes in breathing patterns after a trial of nasal CPAP.
Other useful patient compliance tools include a CPAP informational handout, telephone access to nursing staff, and a 30-day follow-up visit.
Obtaining the support of the bed partner by welcoming her or him to all appointments, including educational activities, is optimal. The bed partner was likely the impetus for the appointment in the first place because of concerns about excessive snoring or apneas.
Image reprinted from Oct. 2001 Mayo Clinic Health Letter with permission of Mayo Foundation for Medical Education and Research, Rochester, MN 55905
Surgical options exist for OSA. The most common procedures are uvulopalatopharyngoplasty (UPPP) and laser-assisted uvulopalatoplasty (LAUP). Other procedures in use include tongue reduction and mandibular advancement.
The response rate to OSA surgery averages around 50% but varies on the patient’s characteristics and procedure selected.9 Positive outcomes are most likely for thin patients with obvious upper airway obstruction, including a deviated nasal septum, large tonsils, a low-hanging palate, and large uvula. Potential complications include nasal regurgitation, voice change, postoperative pain, bleeding, infection, tongue numbness, and snoring without apnea (silent apnea).
Oral appliances have a vital niche in OSA treatment. Multiple devices have been developed that open the oropharynx by moving the mandible and tongue out of way. A growing body of data shows that oral appliances improve sleep and reduce EDS and promote patient satisfaction more effectively than nasal CPAP.10 Several studies also show that patients with mild to moderate OSA accept these devices well.
Oral devices do have drawbacks, however. In most settings, effectiveness cannot be observed during a “split-night” laboratory sleep study because the patient has not yet purchased the device. Also, multiple visits sometimes are required to custom fit the oral appliance; this can pose a hardship to patients who live a distance from the provider.
Restless legs syndrome, periodic limb movement disorder
The patient with restless legs syndrome typically reports a restless painful feeling in the limbs that occurs in the evening and at night, disrupting sleep. This condition, which affects 10% of the population, is associated with aging, blood loss, anemia, peripheral neuropathies, and pregnancy.11 Patients can have childhood onset and in some cases there is a familial tendency.
Most patients with restless legs syndrome have periodic limb movements (repetitive leg jerks or twitches). The clinical significance of periodic limb movements with no subjective disagreeable feelings in the limbs is controversial. Typically, treatment is not instituted in these cases.
The history usually confirms the diagnosis without a sleep study. Sleep studies are used only if a co-existing sleep problem is suspected or if the diagnosis is not clear-cut.
One suspected mechanism of restless legs syndrome is a dopamine-deficient state. A serum ferritin level can help detect a relative iron deficiency, iron being a cofactor for dopamine synthesis.12
Treatment can include iron repletion when indicated. Medications include dopaminergic agents, most notably pramipexole and levodopa/carbidopa. Other options include gabapentin, benzodiazepines, and narcotics. Antidepressants have been suspected to worsen this condition but definitive studies are lacking.13
Identifying, correcting circadian rhythm disorders
Instead of compromising the quality or quantity of sleep, circadian rhythm disorders cause sleep to occur at inappropriate times. Adolescents or young adults are most likely to confront these disorders.
The delayed sleep phase disorder—that is, a persistent pattern of staying up late and “sleeping in” the next morning—is the most common example. A careful assessment will reveal that the patient is getting a satisfactory amount of sleep that occurs at a socially unacceptable time, sometimes to the extreme that his or her nights and days are reversed.
Patients can be reluctant to acknowledge the severity of their problem, which can lead to both inaccurate sleep diaries and interviews. A portable device called a wrist actigraph provides data about limb movement, thus more objectively measuring the patient’s sleep schedule.
Psychiatrists frequently encounter patients with delayed sleep phase disorder because of a high degree of comorbidity with depressive disorders.14 The cause of this syndrome is unclear, but environmental factors including light exposure, social patterns, psychological issues, and possibly a genetic substrate, are known to contribute.
A less common circadian rhythm disorder, advanced sleep phase disorder, can also cause EDS. Patients have an inappropriately early time of sleep onset and then are fully awake in the middle of the night. A recent report describes a large family with a severe form of this disorder that is linked to an abnormality on chromosome two.15
Relatively few effective treatments have been identified for circadian rhythm disorders. Some patients elect not to pursue therapy, instead selecting activities that fit around their unconventional sleep schedules. Sometimes individuals with delayed sleep phase cannot arrange their education or work hours around their atypical sleep schedules. These patients experience poor early morning academic or work performance due to sleepiness.
The internal circadian clock can be gradually readjusted with either phototherapy or gradual shifting of the major sleep period (Box 4). Stimulant or hypnotic medications generally are not utilized.
Insufficient sleep syndrome
Studies indicate that more people are attempting to burn the candle at both ends and are consequently developing a newly identified condition, insufficient sleep syndrome.16 In our 24-hour society, people often are trying to make do with less than the required 7-1/2 hours sleep per day. This may have adverse consequences to their health. When people are required to perform shift work, the problem is compounded because of the difficulty in obtaining sufficient quality sleep during daylight hours.
Many patients do not seek out treatment for fatigue or sleepiness because they are aware of the lifestyle choices that they have made. Still, they might develop psychologic symptoms like irritability, mood swings, and strained interpersonal relationships. These symptoms often will prompt patients to request treatment.
The most common technique is to ask the patient to establish a consistent awakening time and subsequently a regular bedtime. Initially this could be unconventional by societal standards, i.e., bedtime at 5 a.m. and arising at 2 p.m. Once this pattern is in place, the patient gradually shifts the timing by an hour a day. For most patients it is easier to delay rather than advance the bedtime until it conforms to the desired time.
Reinforce this new sleep pattern with a structured daytime schedule that includes predictable mealtimes, regular exercise, social activities, and possibly bright light exposure. This reinforcement should occur in the morning for delayed sleep phase and in the evening for advanced sleep phase disorder. These interventions take time and discipline.
Another approach is for the patient to completely skip sleep one night and, in a sleep-deprived state, establish a new bedtime at the desired time. The same modalities listed above must be used to reinforce (or “entrain”) this schedule or the patient will gradually slip back into the previous abnormal sleep-wake rhythm.
Major medical centers and North American metropolitan areas are increasingly developing sleep disorder treatment centers. Insurance companies generally cover a specialty sleep evaluation, particularly if the referring physician documents a suspicion of sleep-disordered breathing or excessive daytime sleepiness (EDS)that jeopardizes safe driving.
The most appropriate conditions for an urgent sleep evaluation are:
- Difficulty staying alert while driving, nocturnal cardiac arrhythmias;
- Frequent observed apneas;
- EDS leading to academic or occupational problems.
Psychiatrists should take a careful history that includes a discussion of the patient’s daily and weekly schedule. Avoid psychostimulant medications. Instead, address the non-negotiable need to get adequate sleep and challenge the patients to prioritize his or her activities around a full night’s sleep.
When to consider narcolepsy
Narcolepsy, a less common sleep disorder, can lead to severe occupational, educational, and family disruption. Narcolepsy, which affects 0.05% of the population, is a potentially debilitating disease of the central nervous system that involves abnormal regulation of REM sleep. EDS is the cardinal symptom, often associated with cataplexy (75%), sleep paralysis (50%), vivid dreams, and insomnia, all of which can represent inappropriate intrusion of REM phenomena.
After obtaining a history suggestive of narcolepsy, the psychiatrist should employ either the history, a sleep diary, or wrist actigraphy to document whether the patient is getting adequate sleep with a consistent sleep/wake cycle. Next, consider referring the patient for polysomnography, primarily to rule out other causes of EDS like sleep disorder breathing. In some cases, the REM latency on the overnight sleep study will be less than 20 minutes after sleep onset, which supports the diagnosis of narcolepsy. A multiple sleep latency test (MSLT), a diagnostic test that consists of the patient taking four to five daytime naps, is performed the following day.
Narcolepsy is confirmed if the patient has a mean initial sleep latency of less than 10 minutes during these naps plus at least two REM episodes occurring within 15 minutes after sleep onset.
Recent research shows that most patients who have narcolepsy with cataplexy have undetectable levels of a specific neuropeptide (which is called either hypocretin or orexin) in the cerebrospinal fluid.17 Hypocretin/orexin replacement therapy is a theoretical future possibility, but for now treatment includes a combination of optimal sleep hygiene, psychostimulants, antidepressants, and hypnotics.
Other causes of EDS
Other causes of EDS include unrecognized alcohol dependence, inappropriate or excessive medication use, and depressive disorders. Overnight sleep studies are seldom indicated unless patients endorse the symptoms in Figure 1.
Before pursuing sleep studies (polysomnography or an MSLT), eliminate medications that might confound the results. Such agents include antidepressants, which alter the timing and duration of REM sleep, and sedating medications, which modify initial sleep latency and sleep efficiency and potentially aggravate sleep disordered breathing. Although initial REM latency provides a potential biologic marker of major depression, this measurement is more often used in research studies than in clinical psychiatry.
Primary insomnia is a distressing inability to sleep at night or nap during the day. This suggests a hyperarousal state in several ways, and is the opposite of EDS.18 In rare cases, however, patients who cannot sleep at night also do have EDS. When evaluated, these patients typically endorse at least one of the symptoms in Figure 1. Overnight sleep studies occasionally demonstrate that the insomnia is a symptom of another underlying specific sleep disorder, such as OSA or restless legs syndrome.
Psychiatrists treating a patient with chronic insomnia may appropriately undertake several trials of behavioral interventions or sedating medications before making a referral to a sleep disorder center. Patients can struggle with unrecognized primary sleep disorders for years, and many are evaluated by psychiatrists who institute an empiric trial of stimulating antidepressant medications. Use of antidepressants in these situations is unlikely to cause harm, but they might complicate diagnostic testing. When coexisting depression and a primary sleep disorder are confirmed, management of the sleepy patient optimally entails specific treatments that separately target each condition.
Related resources
- National Sleep Foundation www.sleepfoundation.org
- American Academy of Sleep Medicine www.asda.org
- American Sleep Apnea Association www.sleepapnea.org
- Restless Legs Syndrome Foundation www.rls.org
- Association for the Study of Light Therapy and Biological Rhythms www.sltbr.org
Disclosure
The author reports no affiliation or financial arrangements with any of the companies whose products are mentioned in this article.
Drug brand names
- Carbidopa/levodopa • Sinemet
- Gabapentin • Neurontin
- Pramipexole • Mirapex
- Trazodone • Desyrel
- Zolpidem • Ambien
1. Ronald J, Delaive K, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep. 1999;22(2):225-29.
2. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc. 2000;48:228-29.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14(6):540-45.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep. 1995;18:167-71.
6. Morrell M, Finn L, Kim H, Peppard P, Badr M, Young T. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med. 2000;162(6):2091-96.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994;343(8897):572-75.
9. Lojander J, Maasilta P, Partinen M, Brander P, Salmi T, Lehtonen H. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-19.
10. Mehta A, Qian J, Petocz P, Darendeliler M, Cistulli P. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med. 2001;163(6):1457-61.
11. Chesson A, Jr, Wise M, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. Sleep. 1999;22(7):961-68.
12. Phillips B, Young T, Finn L, Asher K, Hening W, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys. 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry. 1995;152:602-08.
15. Toh K, Jones C, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science. 2001;291(5506):1040-43.
16. Yoshikawa N, Suzuki S, Ishimoto T, Matsumoto M, Miyagishi T. A case of insufficient sleep syndrome. Psychiatry Clin Neuro. 1998;52(2):200-01.
17. Nishino S, Ripley B, Overeem S, Lammers G, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc. 1990;65:869-82.
1. Ronald J, Delaive K, et al. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep. 1999;22(2):225-29.
2. Punjabi N, Haponik E. Ask about daytime sleepiness. J Amer Geriatr Soc. 2000;48:228-29.
3. Johns M. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14(6):540-45.
4. Rowley J, Aboussouan L, Badr M. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-38.
5. Yamashiro Y, Kryger M. Nocturnal oximetry: Is it a screening tool for sleep disorders? Sleep. 1995;18:167-71.
6. Morrell M, Finn L, Kim H, Peppard P, Badr M, Young T. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Critical Care Med. 2000;162(6):2091-96.
7. Roux F, D’Ambrosio C, Mohsenin V. Sleep-related breathing disorders and cardiovascular disease. Am J Med. 2000;108:396-402.
8. Engleman H, Martin S, Deary I, Douglas N. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994;343(8897):572-75.
9. Lojander J, Maasilta P, Partinen M, Brander P, Salmi T, Lehtonen H. Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest. 1996;110(1):114-19.
10. Mehta A, Qian J, Petocz P, Darendeliler M, Cistulli P. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Critical Care Med. 2001;163(6):1457-61.
11. Chesson A, Jr, Wise M, et al. Practice parameters for the treatment of restless legs syndrome and periodic limb movement disorder. Sleep. 1999;22(7):961-68.
12. Phillips B, Young T, Finn L, Asher K, Hening W, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160(14):2137-41.
13. Thorpy M, Ehrenberg B, Hening W, et al. Restless legs syndrome: Detection and management in primary care. Amer Fam Phys. 2000;62:108-14.
14. Regestein Q, Monk T. Delayed sleep phase syndrome: A review of its clinical aspects. Am J Psychiatry. 1995;152:602-08.
15. Toh K, Jones C, et al. An hPer2 phosphorylation site mutation in familial advanced sleep phase syndrome. Science. 2001;291(5506):1040-43.
16. Yoshikawa N, Suzuki S, Ishimoto T, Matsumoto M, Miyagishi T. A case of insufficient sleep syndrome. Psychiatry Clin Neuro. 1998;52(2):200-01.
17. Nishino S, Ripley B, Overeem S, Lammers G, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39-40.
18. Hauri P, Esther M. Insomnia. Mayo Clin Proc. 1990;65:869-82.
Antipsychotics and mood disorders: A complicated alliance
Major mood disorders are challenging to diagnose and often difficult to treat. They entail unipolar depression; bipolar disorder, which includes manic, depressed, or mixed episodes; and schizoaffective disorder, which includes both depressed and bipolar subtypes. Antidepressants and mood stabilizers are the primary pharmacological treatments. They may be insufficient, however, for patients with more severe episodes, often characterized by psychosis and treatment resistance.
In these patients, antipsychotics have played an important but controversial part in management, primarily as oral or parenteral adjuncts. Literature and clinical experience now support another, unique role for the current generation of novel agents.
Compared to earlier antipsychotics, these agents produce substantially fewer neurological adverse effects, including acute extrapyramidal and tardive syndromes, and can augment antidepressants and mood stabilizers. In addition, they may:
- Possess a better antipsychotic profile, with enhanced therapeutic effects on positive, negative, cognitive, and mood symptoms
- Have a role in the acute and long-term management of these disorders when anticipated parenteral formulations become available (e.g., acute intramuscular olanzapine and ziprasidone—and long-acting intramuscular risperidone)
- Possess inherent thymoleptic properties (see “Unresolved issues with antipsychotics,” below).
- Defining what constitutes a mood stabilizer.1 Proposed definitions suggest that the drug must entail the following:
- Clarifying the mechanisms underlying the apparent mood-regulating effects of novel agents
- Ascertaining both acute and maintenance efficacy
- Clarifying the propensity of some agents to switch depressed patients into mania
- Increasing the number of well-designed studies with sufficient sample sizes, including comparison trials assessing the relative efficacy of different novel agents
- Reducing the tendency to publish only positive reports when new drugs are first available
- Introducing parenteral formulations of novel agents
- Resolving concerns about weight gain, new-onset diabetes, QT c prolongation, and sedation
- Rectifying the current level of substantially greater costs
Management of unipolar depression
Neuroleptics Delusions and hallucinations indicate a more severe form of depressive disorder, with poor short- and long-term outcomes in comparison to those without psychosis. To illustrate, Table 1 lists a summary of response rates in psychotic and nonpsychotic depressed patients given a tricyclic antidepressant (TCA). The data indicate that patients suffering from psychotic depression typically do not benefit from antidepressant monotherapy and usually require a combination of antidepressant and antipsychotic or, alternatively, electroconvulsive therapy (ECT).
There is, however, some limited clinical and neuroimaging evidence that amoxapine can be used as an effective monotherapy in this group. Amoxapine is an antidepressant whose primary active metabolite, 8-hydroxy amoxapine, may have antipsychotic properties.1 With the possible exception of amoxapine, combined antipsychotic-antidepressant treatment is the rule.
Table 1
Psychotic and nonpsychotic depressed patients’ response to monotherapy with a tricyclic antidepressant
| Psychotic | Nonpsychotic | ||||
|---|---|---|---|---|---|
| Responders (%) (n=127) | Nonresponders (%) (n=236) | Responders (%) (n=464) | Nonresponders (%) (n=227) | Difference | |
| 13 studies | 35% | 65% | 67% | 33% | 32% |
| Adapted from Chan CH, Janicak PG, Davis JM, et al. Response of psychotic and nonpsychotic depressed patients to tricyclic antidepressants. J Clin Psychiatry. 1987;48:197-200. | |||||
Historically, studies have also evaluated neuroleptic monotherapy for depressed patients. While some reported superiority over a placebo, none found conventional antipsychotics superior to imipramine. Indeed, patients with schizophrenia who are treated with a neuroleptic often develop symptoms that are difficult to distinguish from depression (e.g., secondary negative symptoms). These often improve when the neuroleptic is discontinued or the patients are switched to a novel antipsychotic such as risperidone, olanzapine, or ziprasidone, all of which have putative antidepressant effects.
When employing an antipsychotic in depressed patients, the dosage and duration of treatment are two critical considerations. To minimize neuromotor adverse effects, use low doses of a neuroleptic (e.g., haloperidol, 1 to 5 mg/d) in conjunction with the primary antidepressant therapy. The neuroleptic should then be tapered gradually after psychotic symptoms have been controlled, usually during the acute phase of treatment. Ideally, patients would then take antidepressant monotherapy through the continuation phase and, if necessary, the maintenance phase of treatment. If psychosis recurs, re-introduce the antipsychotic intermittently.
Novel antipsychotics In contrast to neuroleptics, novel antipsychotics have been reported to improve depression in various psychotic and mood disorders.
For example, ziprasidone has serotonin and noradrenergic reuptake blocking effects comparable to such classic TCAs as imipramine and amitriptyline, as well as high binding affinity at the 5-HT1A, 5-HT1D, and 5-HT2C receptors. This neuroreceptor profile indicates possible antidepressant effects.
While randomized, controlled trials with mood-disordered patients are few, there have been promising preliminary reports of augmentation of antidepressants with risperidone and olanzapine in both psychotic and nonpsychotic depressed patients.
Ostroff and Nelson2 reported the results of an open-label study of eight SSRI-nonresponsive patients (mean treatment 7.3 weeks). These patients had no psychotic features and had a dramatic reduction in depressive symptoms, as well as some improvement in sexual dysfunction, with the addition of 0.5 mg to 1.0 mg risperidone. The clinicians suggested that risperidone’s 5-HT2A antagonism might explain its augmentation of the partial SSRI response.
Olanzapine alone (n=3) or combined with an antidepressant (n=12) has also been reported to improve both depression and psychosis.3 In a double-blind, amitriptyline-controlled trial, Svestka and Synek4 found that olanzapine demonstrated antidepressant efficacy in 33 unipolar and seven bipolar depressed patients. Thirteen of these patients also had psychotic symptoms.
Shelton et al5 reported the results of a two-center, 8-week, double-blind comparison of olanzapine alone, fluoxetine alone, or their combination in 28 patients suffering from treatment-resistant, non-bipolar disorder without psychosis. They found that the combination was superior to either drug alone based on improvement in the Hamilton Depression Rating Scale (HDRS) total score. From their preliminary data, it also appears that the doses required were relatively low, reducing the risk of side effects.
Their findings, however, need to be replicated in more controlled studies with combinations, addressing possible adverse effects, the potential for clinically relevant drug interactions, decreased compliance rates, and increased cost of treatment. Earlier reports raised concern about the potential of these agents to increase switching to hypomania or mania. But in more recent reports, this has not emerged as a significant problem.7
Finally, several case reports and case series indicate that agents such as clozapine and risperidone may augment ECT in particularly severe, treatment-resistant depressive episodes.7
Management of bipolar and schizoaffective depressed episodes
Neuroleptics Antipsychotics are frequently used to manage more severe, usually psychotic episodes of bipolar and schizoaffective depression. Reports indicate that affectively ill patients receiving neuroleptics may be more prone to develop neuromotor adverse effects than are those suffering from schizophrenia. Thus, their use for such patients must be well justified, limited in dosage and duration, and carefully monitored for the emergence of acute and tardive neurological events.
Novel antipsychotics Novel antipsychotics have demonstrated fewer propensities than have neuroleptics in worsening depression or negative symptoms in schizophrenic patients, and have possible antidepressant effects. In support of this hypothesis, and reminiscent of data from earlier risperidone and olanzapine trials, ziprasidone was observed to improve the Montgomery Asberg Rating Scale (MADRS) and Brief Psychotic Rating Scale (BPRS) depressive cluster scores in three clinical trials with schizophrenic and schizoaffective patients.8,9
Vieta et al reported the efficacy and safety of risperidone add-on therapy for treating various episodes of bipolar (n=358) and schizoaffective (n=183) disorders.6 In this multicenter, open study, 33 patients (6.1%) suffered a depressed episode and received a mean risperidone dose of 1.6 (± 2.3) mg/d added to their ongoing but ineffective drug regimen. Mean HDRS declined significantly over the 6-month course. Further, switch rates were low and in the expected range for spontaneous fluctuations seen in these disorders.
The results of a 6-week, double-blind, controlled trial of risperidone versus haloperidol in 62 patients with schizoaffective disorder, bipolar or depressed subtype, were published.10 Risperidone (average dose of 5.5 mg/d) was comparable to haloperidol (average dose of 10.8 mg/d) in reducing the mean in the Positive and Negative Syndrome Scale and Clinician-Administered Rating Scale for Mania change scores.
In those patients with baseline HDRS scores ≥ 20, risperidone produced a significantly greater reduction in mean change scores than did haloperidol. In addition, patients had no mood switches with risperidone or haloperidol; there was a significantly higher incidence of patients who had extra-pyramidal symptoms with haloperidol than among those taking risperidone; and six patients in the group taking haloperidol dropped out after experiencing adverse effects. None of the patients taking risperidone dropped out.
Table 2
Lithium versus antipsychotics for acute mania
| Lithium | Antipsychotics | ||||
|---|---|---|---|---|---|
| Responders (%) (n=64) | Nonresponders (%) (n=10) | Responders (%) (n=38) | Nonresponders (%) (n=33) | Difference | |
| 5 studies | 89% | 11% | 54% | 46% | 35% |
| Adapted from Janicak PG, Newman RH, Davis JM. Advances in the treatment of mania and related disorders: a reappraisal. Psychiatric Ann. 1992;22(2):94. | |||||
Management of bipolar manic or mixed episodes
Up to 80% of all bipolar patients receive an antipsychotic drug during the acute and/or maintenance phase of their illness, even though loading doses of valproate and benzodiazepines may also be used during an exacerbation and pose much less risk, especially in terms of adverse neurological effects.
Neuroleptics Shortly after their introduction, neuroleptics were found to reduce mortality secondary to dehydration and exhaustion in many highly agitated patients during an acute manic episode such as lethal catatonia.7
While earlier controlled studies found these agents to be effective in the treatment of acute mania, they are clearly less efficacious than lithium for core manic symptoms.11Table 2 demonstrates a meta-analysis of five well-controlled, double-blind studies documenting the statistical superiority of lithium over neuroleptics. These agents, however, offer the advantage of a more rapid onset of action, particularly when given in the acute parenteral formulation, and are superior to lithium in the initial control of agitation. Further, long-acting depot formulations of neuroleptics may be the only viable strategy for chronic, recurrent, noncompliant patients.
As with psychotic depression, dosing and duration of neuroleptic treatment are important concerns. In this context, Rifkin et al demonstrated that 10 mg of haloperidol per day had comparable efficacy but fewer adverse effects than did 30 or 80 mg per day in a group of acutely manic patients.12 Despite such data, high chlorpromazine-equivalent doses are often administered acutely and maintained for sustained periods. This can be a significant problem given the apparent great sensitivity of bipolar patients to the neurological sequelae of these antipsychotic agents.
Novel antipsychotics Early case series reports indicated that clozapine may benefit treatment-refractory bipolar patients. Given the inherent drawbacks of clozapine (e.g., agranulocytosis and seizure induction), attention now focuses on other novel agents with more benign adverse effect profiles than clopazine. Controlled trials with olanzapine and risperidone serve to reinforce the usefulness of these as well as other novel agents.
Tohen et al published the results of a 3-week, double-blind, placebo-controlled trial of olanzapine in 139 patients experiencing an acute bipolar manic or mixed episode.13 Olanzapine produced a statistically greater mean improvement than did the placebo on the Young Mania Rating Scale (YMRS) change scores. Further, 49% of the olanzapine-treated group (n=70) met the a priori criteria for response versus only 24% of the placebo-treated group (n=69). A second study using a higher starting dose of olanzapine, less rescue medication, and longer treatment duration than the first study resulted in a similar outcome.14
Sachs et al reported on the results of a 3-week, double-blind, placebo-controlled trial involving 156 patients with bipolar manic or mixed subtype who received a mood stabilizer (lithium or valproate) plus a placebo, risperidone (1 to 6 mg/d), or haloperidol (2 to 12 mg/d).15 The clinicians concluded that risperidone plus a mood stabilizer was statistically superior to a placebo plus a mood stabilizer, and produced more rapid reduction in manic symptoms, regardless of whether psychosis was present.
Sajatovic et al16 published the results of a prospective, open trial with quetiapine (mean dose = 203 ± 124 mg/d) as add-on therapy in 20 patients (10 bipolar, 10 schizoaffective; 19 male, 1 female) insufficiently responsive to their mood stabilizer or antipsychotic. Pre-post assessments indicated significant improvement in the BPRS, Mania Rating Scale (MRS), and HDRS scores. While the combination was generally well tolerated, there was a mean weight gain of 4.9 kg (10.8 lb). This raises the specter of complications associated with substantial weight gain produced by several of the novel antipsychotics.
A recent report indicates that ziprasidone may also be an effective antimanic agent. In a randomized, double-blind, placebo-controlled, multicenter trial involving 210 bipolar (manic or mixed episodes) patients, ziprasidone (80 to 160 mg/d; n=140) was compared to a placebo (n=70) for 3 weeks.17 By day 2 and all subsequent time points, ziprasidone was superior in terms of mean change scores from the baseline MRS; produced a more rapid and significantly greater improvement in overall psychopathology in both positive and negative symptoms; and did not produce significant adverse effects (including relevant ECG parameter changes) when compared with the placebo. Similar trials are being conducted for risperidone, aripiprazole, and iloperidone.
Finally, Meehan et al18 reported on the results of an acute parenteral formulation of olanzapine used to manage agitation in an acute manic or mixed episode. This was a 24-hour, double-blind, placebo-controlled trial comparing intramuscular olanzapine to intramuscular lorazepam. The following results were indicated:
- Olanzapine (doses of 5 to 10 mg) produced a significantly greater reduction in excitation than did the placebo or lorazepam at 30 minutes post-injection.
- Twice as many patients receiving lorazepam or a placebo versus olanzapine required more than one injection.
- Except for olanzapine-induced tachycardia in one patient, there were no significant changes in vital signs, ECG parameters, or laboratory assays among the three groups.
- Somnolence (13%) and dizziness (9%) were the most frequent side effects in the olanzapine group.
Treatment strategies for depression and mania
Considering the existing research data, clinical experience, and the risk/benefit ratio, treatment strategies that emphasize the role of antipsychotics in managing severe mood disorders are presented in the algorithms in Figures 1 and 2.
Figure 1 emphasizes the role of antipsychotics in the pharmacological management of patients with major depression. For unipolar depression with psychotic symptoms, options include an antidepressant plus an antipsychotic; amoxapine monotherapy; and possibly monotherapy with a novel agent such as ziprasidone. For bipolar depression with psychosis or schizoaffective disorder with depression, combining a mood stabilizer such as lithium plus an antipsychotic may be sufficient, but often an antidepressant must also be added. If the response is insufficient, consider switching to a novel antipsychotic (e.g., olanzapine or risperidone) plus a mood stabilizer (± antidepressant). In more serious exacerbations (e.g., high suicidality), ECT may be most appropriate. Secondary choices include clozapine with or without an antidepressant or novel antipsychotic such as risperidone combined with ECT.
Figure 2 describes the use of antipsychotics in patients with mania. If response to a primary mood stabilizer such as lithium, valproate, or their combination in the context of a bipolar or schizoaffective disorder is insufficient—or if patients have severe manic or psychotic symptoms—an antipsychotic may be added to the primary mood stabilizer.
Alternatively, when mood stabilizers are not tolerated or a clinical situation such as pregnancy precludes their use, a novel agent such as olanzapine or risperidone may be given as monotherapy. While the safety of these agents in pregnancy is not clearly established, clinical experience thus far indicates they may be safer than agents such as valproate or carbamazepine. These agents would be the first choice given their diminished propensity for extrapyramidal symptoms; absence of clozapine-related adverse effects such as agranulocytosis and seizures; and growing evidence of possible mood stabilizing effects.
Figure 1 ANTIPSYCHOTICS IN THE TREATMENT OF MAJOR DEPRESSION
Figure 2 ANTIPSYCHOTICS IN THE TREATMENT OF MANIA
For patients who remain nonresponsive, clozapine should be considered either as monotherapy or combined with valproate and/or lithium. Combining this agent with carbamazepine is not recommended because of the possibility of an increased risk of hematotoxicity.
Electroconvulsive therapy may be used safely and effectively in patients who are severely ill (e.g., those with manic delirium); pose an immediate danger because of their potential for violence; are in medical crisis; or have medical contraindications to pharmacotherapy. There is preliminary evidence that ECT can be safely administered with novel antipsychotics such as clozapine, risperidone, or olanzapine to produce additional benefit in patients insufficiently responsive to either therapy alone.
Related resources
- International Society for Bipolar Disorders www.isbd.org
Drug brand names
- Amitriptyline • Elavil
- Amoxapine • Asendin
- Aripiprazole • (in development)
- Carbamazepine • Tegretol, Epitol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Iloperidone • (in development)
- Imipramine • Tofranil
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproate sodium • Depacon
- Ziprasidone • Geodon
Disclosure
The author reports that he receives research/grant support from, serves as a consultant for, and on the speaker’s bureau of Janssen Pharmaceutica. He also receives research/grant support from Genentech Inc. and Bristol-Myers Squibb Co.; serves as a consultant for Pfizer Inc., Sepracor, and Novartis Pharmaceuticals Corp.; and is on the speaker’s bureau of Abbott Laboratories, Eli Lilly and Co., Pfizer Inc., Forest Pharmaceuticals, Bristol-Myers Squibb Co., and Wyeth-Ayerst Pharmaceuticals.
1. Kapur S, Cho R, Jones C, et al. Is amoxapine an atypical antipsychotic? Positronemission tomography investigation of its dopamine2 and serotonin2 occupancy. Biol Psychiatry. 1999;45:1217-1220.
2. Ostroff RB, Nelson JC. Risperidone augmentation of selective serotonin reuptake inhibitors in major depression. J Clin Psychiatry. 1999;60:256-259.
3. Rothschild AJ, Bates KS, Boehringer KL, Syed A. Olanzapine response in psychotic depression. J Clin Psychiatry. 1999;60:116-118.
4. Svestka J, Synek O. Does olanzapine have antidepressant effect? A double-blind amitriptyline-controlled study [abstract]. Int J Neuropsychopharmacol. 2000;3(suppl 1):S251.-
5. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158:131-134.
6. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 5-month, multicenter, open study. J Clin Psychiatry. 2001;62(10):818.-
7. Janicak PG, Davis JM, et al. Principles and Practice of Psychopharmacotherapy. 3rd ed. Philadelphia, Pa: Lippincott-Williams & Wilkins; 2001.
8. Daniel DG, Zimbroff DL, et al. for the Ziprasidone Study Group Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Neuropsychopharmacol. 1999;20(5):491-505.
9. Keck PE, Jr, Buffenstein A, Ferguson J, et al. Ziprasidone 40 and 120 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 4-week placebo-controlled trial. Psychopharmacol. 1998;140:173-184.
10. Janicak PG, Keck PE, Jr, Davis JM, et al. A double-blind, randomized, prospective evaluation of the efficacy and safety of risperidone versus haloperidol in the treatment of schizoaffective disorder. J Clin Psychopharmacol. 2001;21:360-368.
11. Keck PE, Welge JA, McElroy SL, et al. Placebo effect in randomized, controlled studies of acute bipolar mania and depression. Biol Psychiatry. 2000;47(8):756-761.
12. Rifkin A, Doddi S, Karajgi B, et al. Dosage of haloperidol for mania. Br J Psychiatry. 1994;165:113-116.
13. Tohen M, Sanger TM, McElroy SL, et al. Olanzipine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry. 1999;156:702-709.
14. Tohen M, Jacobs TG, Grundy SL, et al. Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. The Olanzipine HGGW Study Group. Arch Gen Psychiatry. 2000;57:841-849.
15. Sachs G, Ghaemi N, Grossman F, Bowden C. Risperidone plus mood stabilizer vs. placebo plus mood stabilizer for acute mania of bipolar disorder: a double-blind comparison of efficacy and safety. International Congress on Bipolar Disorders. Pittsburgh, Pa. June 14-16, 2001.
16. Sajatovic M, Briscan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry. 2001;62:728-732.
17. Giller E, Mandel FS, Keck P. Ziprasidone in the acute treatment of mania: a double-blind, placebo-controlled, randomized trial. Schizophr Res. 2001;49(suppl 1-2):229.-
18. Meehan K, Zhang F, David S, Tohen N, Janicak PG, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular (IM) olanzapine versus IM lorazepam and IM placebo in acutely agitated patients diagnosed with mania associated with bipolar disorder. J Clin Psychopharmacol 2001;21:389-397.
Major mood disorders are challenging to diagnose and often difficult to treat. They entail unipolar depression; bipolar disorder, which includes manic, depressed, or mixed episodes; and schizoaffective disorder, which includes both depressed and bipolar subtypes. Antidepressants and mood stabilizers are the primary pharmacological treatments. They may be insufficient, however, for patients with more severe episodes, often characterized by psychosis and treatment resistance.
In these patients, antipsychotics have played an important but controversial part in management, primarily as oral or parenteral adjuncts. Literature and clinical experience now support another, unique role for the current generation of novel agents.
Compared to earlier antipsychotics, these agents produce substantially fewer neurological adverse effects, including acute extrapyramidal and tardive syndromes, and can augment antidepressants and mood stabilizers. In addition, they may:
- Possess a better antipsychotic profile, with enhanced therapeutic effects on positive, negative, cognitive, and mood symptoms
- Have a role in the acute and long-term management of these disorders when anticipated parenteral formulations become available (e.g., acute intramuscular olanzapine and ziprasidone—and long-acting intramuscular risperidone)
- Possess inherent thymoleptic properties (see “Unresolved issues with antipsychotics,” below).
- Defining what constitutes a mood stabilizer.1 Proposed definitions suggest that the drug must entail the following:
- Clarifying the mechanisms underlying the apparent mood-regulating effects of novel agents
- Ascertaining both acute and maintenance efficacy
- Clarifying the propensity of some agents to switch depressed patients into mania
- Increasing the number of well-designed studies with sufficient sample sizes, including comparison trials assessing the relative efficacy of different novel agents
- Reducing the tendency to publish only positive reports when new drugs are first available
- Introducing parenteral formulations of novel agents
- Resolving concerns about weight gain, new-onset diabetes, QT c prolongation, and sedation
- Rectifying the current level of substantially greater costs
Management of unipolar depression
Neuroleptics Delusions and hallucinations indicate a more severe form of depressive disorder, with poor short- and long-term outcomes in comparison to those without psychosis. To illustrate, Table 1 lists a summary of response rates in psychotic and nonpsychotic depressed patients given a tricyclic antidepressant (TCA). The data indicate that patients suffering from psychotic depression typically do not benefit from antidepressant monotherapy and usually require a combination of antidepressant and antipsychotic or, alternatively, electroconvulsive therapy (ECT).
There is, however, some limited clinical and neuroimaging evidence that amoxapine can be used as an effective monotherapy in this group. Amoxapine is an antidepressant whose primary active metabolite, 8-hydroxy amoxapine, may have antipsychotic properties.1 With the possible exception of amoxapine, combined antipsychotic-antidepressant treatment is the rule.
Table 1
Psychotic and nonpsychotic depressed patients’ response to monotherapy with a tricyclic antidepressant
| Psychotic | Nonpsychotic | ||||
|---|---|---|---|---|---|
| Responders (%) (n=127) | Nonresponders (%) (n=236) | Responders (%) (n=464) | Nonresponders (%) (n=227) | Difference | |
| 13 studies | 35% | 65% | 67% | 33% | 32% |
| Adapted from Chan CH, Janicak PG, Davis JM, et al. Response of psychotic and nonpsychotic depressed patients to tricyclic antidepressants. J Clin Psychiatry. 1987;48:197-200. | |||||
Historically, studies have also evaluated neuroleptic monotherapy for depressed patients. While some reported superiority over a placebo, none found conventional antipsychotics superior to imipramine. Indeed, patients with schizophrenia who are treated with a neuroleptic often develop symptoms that are difficult to distinguish from depression (e.g., secondary negative symptoms). These often improve when the neuroleptic is discontinued or the patients are switched to a novel antipsychotic such as risperidone, olanzapine, or ziprasidone, all of which have putative antidepressant effects.
When employing an antipsychotic in depressed patients, the dosage and duration of treatment are two critical considerations. To minimize neuromotor adverse effects, use low doses of a neuroleptic (e.g., haloperidol, 1 to 5 mg/d) in conjunction with the primary antidepressant therapy. The neuroleptic should then be tapered gradually after psychotic symptoms have been controlled, usually during the acute phase of treatment. Ideally, patients would then take antidepressant monotherapy through the continuation phase and, if necessary, the maintenance phase of treatment. If psychosis recurs, re-introduce the antipsychotic intermittently.
Novel antipsychotics In contrast to neuroleptics, novel antipsychotics have been reported to improve depression in various psychotic and mood disorders.
For example, ziprasidone has serotonin and noradrenergic reuptake blocking effects comparable to such classic TCAs as imipramine and amitriptyline, as well as high binding affinity at the 5-HT1A, 5-HT1D, and 5-HT2C receptors. This neuroreceptor profile indicates possible antidepressant effects.
While randomized, controlled trials with mood-disordered patients are few, there have been promising preliminary reports of augmentation of antidepressants with risperidone and olanzapine in both psychotic and nonpsychotic depressed patients.
Ostroff and Nelson2 reported the results of an open-label study of eight SSRI-nonresponsive patients (mean treatment 7.3 weeks). These patients had no psychotic features and had a dramatic reduction in depressive symptoms, as well as some improvement in sexual dysfunction, with the addition of 0.5 mg to 1.0 mg risperidone. The clinicians suggested that risperidone’s 5-HT2A antagonism might explain its augmentation of the partial SSRI response.
Olanzapine alone (n=3) or combined with an antidepressant (n=12) has also been reported to improve both depression and psychosis.3 In a double-blind, amitriptyline-controlled trial, Svestka and Synek4 found that olanzapine demonstrated antidepressant efficacy in 33 unipolar and seven bipolar depressed patients. Thirteen of these patients also had psychotic symptoms.
Shelton et al5 reported the results of a two-center, 8-week, double-blind comparison of olanzapine alone, fluoxetine alone, or their combination in 28 patients suffering from treatment-resistant, non-bipolar disorder without psychosis. They found that the combination was superior to either drug alone based on improvement in the Hamilton Depression Rating Scale (HDRS) total score. From their preliminary data, it also appears that the doses required were relatively low, reducing the risk of side effects.
Their findings, however, need to be replicated in more controlled studies with combinations, addressing possible adverse effects, the potential for clinically relevant drug interactions, decreased compliance rates, and increased cost of treatment. Earlier reports raised concern about the potential of these agents to increase switching to hypomania or mania. But in more recent reports, this has not emerged as a significant problem.7
Finally, several case reports and case series indicate that agents such as clozapine and risperidone may augment ECT in particularly severe, treatment-resistant depressive episodes.7
Management of bipolar and schizoaffective depressed episodes
Neuroleptics Antipsychotics are frequently used to manage more severe, usually psychotic episodes of bipolar and schizoaffective depression. Reports indicate that affectively ill patients receiving neuroleptics may be more prone to develop neuromotor adverse effects than are those suffering from schizophrenia. Thus, their use for such patients must be well justified, limited in dosage and duration, and carefully monitored for the emergence of acute and tardive neurological events.
Novel antipsychotics Novel antipsychotics have demonstrated fewer propensities than have neuroleptics in worsening depression or negative symptoms in schizophrenic patients, and have possible antidepressant effects. In support of this hypothesis, and reminiscent of data from earlier risperidone and olanzapine trials, ziprasidone was observed to improve the Montgomery Asberg Rating Scale (MADRS) and Brief Psychotic Rating Scale (BPRS) depressive cluster scores in three clinical trials with schizophrenic and schizoaffective patients.8,9
Vieta et al reported the efficacy and safety of risperidone add-on therapy for treating various episodes of bipolar (n=358) and schizoaffective (n=183) disorders.6 In this multicenter, open study, 33 patients (6.1%) suffered a depressed episode and received a mean risperidone dose of 1.6 (± 2.3) mg/d added to their ongoing but ineffective drug regimen. Mean HDRS declined significantly over the 6-month course. Further, switch rates were low and in the expected range for spontaneous fluctuations seen in these disorders.
The results of a 6-week, double-blind, controlled trial of risperidone versus haloperidol in 62 patients with schizoaffective disorder, bipolar or depressed subtype, were published.10 Risperidone (average dose of 5.5 mg/d) was comparable to haloperidol (average dose of 10.8 mg/d) in reducing the mean in the Positive and Negative Syndrome Scale and Clinician-Administered Rating Scale for Mania change scores.
In those patients with baseline HDRS scores ≥ 20, risperidone produced a significantly greater reduction in mean change scores than did haloperidol. In addition, patients had no mood switches with risperidone or haloperidol; there was a significantly higher incidence of patients who had extra-pyramidal symptoms with haloperidol than among those taking risperidone; and six patients in the group taking haloperidol dropped out after experiencing adverse effects. None of the patients taking risperidone dropped out.
Table 2
Lithium versus antipsychotics for acute mania
| Lithium | Antipsychotics | ||||
|---|---|---|---|---|---|
| Responders (%) (n=64) | Nonresponders (%) (n=10) | Responders (%) (n=38) | Nonresponders (%) (n=33) | Difference | |
| 5 studies | 89% | 11% | 54% | 46% | 35% |
| Adapted from Janicak PG, Newman RH, Davis JM. Advances in the treatment of mania and related disorders: a reappraisal. Psychiatric Ann. 1992;22(2):94. | |||||
Management of bipolar manic or mixed episodes
Up to 80% of all bipolar patients receive an antipsychotic drug during the acute and/or maintenance phase of their illness, even though loading doses of valproate and benzodiazepines may also be used during an exacerbation and pose much less risk, especially in terms of adverse neurological effects.
Neuroleptics Shortly after their introduction, neuroleptics were found to reduce mortality secondary to dehydration and exhaustion in many highly agitated patients during an acute manic episode such as lethal catatonia.7
While earlier controlled studies found these agents to be effective in the treatment of acute mania, they are clearly less efficacious than lithium for core manic symptoms.11Table 2 demonstrates a meta-analysis of five well-controlled, double-blind studies documenting the statistical superiority of lithium over neuroleptics. These agents, however, offer the advantage of a more rapid onset of action, particularly when given in the acute parenteral formulation, and are superior to lithium in the initial control of agitation. Further, long-acting depot formulations of neuroleptics may be the only viable strategy for chronic, recurrent, noncompliant patients.
As with psychotic depression, dosing and duration of neuroleptic treatment are important concerns. In this context, Rifkin et al demonstrated that 10 mg of haloperidol per day had comparable efficacy but fewer adverse effects than did 30 or 80 mg per day in a group of acutely manic patients.12 Despite such data, high chlorpromazine-equivalent doses are often administered acutely and maintained for sustained periods. This can be a significant problem given the apparent great sensitivity of bipolar patients to the neurological sequelae of these antipsychotic agents.
Novel antipsychotics Early case series reports indicated that clozapine may benefit treatment-refractory bipolar patients. Given the inherent drawbacks of clozapine (e.g., agranulocytosis and seizure induction), attention now focuses on other novel agents with more benign adverse effect profiles than clopazine. Controlled trials with olanzapine and risperidone serve to reinforce the usefulness of these as well as other novel agents.
Tohen et al published the results of a 3-week, double-blind, placebo-controlled trial of olanzapine in 139 patients experiencing an acute bipolar manic or mixed episode.13 Olanzapine produced a statistically greater mean improvement than did the placebo on the Young Mania Rating Scale (YMRS) change scores. Further, 49% of the olanzapine-treated group (n=70) met the a priori criteria for response versus only 24% of the placebo-treated group (n=69). A second study using a higher starting dose of olanzapine, less rescue medication, and longer treatment duration than the first study resulted in a similar outcome.14
Sachs et al reported on the results of a 3-week, double-blind, placebo-controlled trial involving 156 patients with bipolar manic or mixed subtype who received a mood stabilizer (lithium or valproate) plus a placebo, risperidone (1 to 6 mg/d), or haloperidol (2 to 12 mg/d).15 The clinicians concluded that risperidone plus a mood stabilizer was statistically superior to a placebo plus a mood stabilizer, and produced more rapid reduction in manic symptoms, regardless of whether psychosis was present.
Sajatovic et al16 published the results of a prospective, open trial with quetiapine (mean dose = 203 ± 124 mg/d) as add-on therapy in 20 patients (10 bipolar, 10 schizoaffective; 19 male, 1 female) insufficiently responsive to their mood stabilizer or antipsychotic. Pre-post assessments indicated significant improvement in the BPRS, Mania Rating Scale (MRS), and HDRS scores. While the combination was generally well tolerated, there was a mean weight gain of 4.9 kg (10.8 lb). This raises the specter of complications associated with substantial weight gain produced by several of the novel antipsychotics.
A recent report indicates that ziprasidone may also be an effective antimanic agent. In a randomized, double-blind, placebo-controlled, multicenter trial involving 210 bipolar (manic or mixed episodes) patients, ziprasidone (80 to 160 mg/d; n=140) was compared to a placebo (n=70) for 3 weeks.17 By day 2 and all subsequent time points, ziprasidone was superior in terms of mean change scores from the baseline MRS; produced a more rapid and significantly greater improvement in overall psychopathology in both positive and negative symptoms; and did not produce significant adverse effects (including relevant ECG parameter changes) when compared with the placebo. Similar trials are being conducted for risperidone, aripiprazole, and iloperidone.
Finally, Meehan et al18 reported on the results of an acute parenteral formulation of olanzapine used to manage agitation in an acute manic or mixed episode. This was a 24-hour, double-blind, placebo-controlled trial comparing intramuscular olanzapine to intramuscular lorazepam. The following results were indicated:
- Olanzapine (doses of 5 to 10 mg) produced a significantly greater reduction in excitation than did the placebo or lorazepam at 30 minutes post-injection.
- Twice as many patients receiving lorazepam or a placebo versus olanzapine required more than one injection.
- Except for olanzapine-induced tachycardia in one patient, there were no significant changes in vital signs, ECG parameters, or laboratory assays among the three groups.
- Somnolence (13%) and dizziness (9%) were the most frequent side effects in the olanzapine group.
Treatment strategies for depression and mania
Considering the existing research data, clinical experience, and the risk/benefit ratio, treatment strategies that emphasize the role of antipsychotics in managing severe mood disorders are presented in the algorithms in Figures 1 and 2.
Figure 1 emphasizes the role of antipsychotics in the pharmacological management of patients with major depression. For unipolar depression with psychotic symptoms, options include an antidepressant plus an antipsychotic; amoxapine monotherapy; and possibly monotherapy with a novel agent such as ziprasidone. For bipolar depression with psychosis or schizoaffective disorder with depression, combining a mood stabilizer such as lithium plus an antipsychotic may be sufficient, but often an antidepressant must also be added. If the response is insufficient, consider switching to a novel antipsychotic (e.g., olanzapine or risperidone) plus a mood stabilizer (± antidepressant). In more serious exacerbations (e.g., high suicidality), ECT may be most appropriate. Secondary choices include clozapine with or without an antidepressant or novel antipsychotic such as risperidone combined with ECT.
Figure 2 describes the use of antipsychotics in patients with mania. If response to a primary mood stabilizer such as lithium, valproate, or their combination in the context of a bipolar or schizoaffective disorder is insufficient—or if patients have severe manic or psychotic symptoms—an antipsychotic may be added to the primary mood stabilizer.
Alternatively, when mood stabilizers are not tolerated or a clinical situation such as pregnancy precludes their use, a novel agent such as olanzapine or risperidone may be given as monotherapy. While the safety of these agents in pregnancy is not clearly established, clinical experience thus far indicates they may be safer than agents such as valproate or carbamazepine. These agents would be the first choice given their diminished propensity for extrapyramidal symptoms; absence of clozapine-related adverse effects such as agranulocytosis and seizures; and growing evidence of possible mood stabilizing effects.
Figure 1 ANTIPSYCHOTICS IN THE TREATMENT OF MAJOR DEPRESSION
Figure 2 ANTIPSYCHOTICS IN THE TREATMENT OF MANIA
For patients who remain nonresponsive, clozapine should be considered either as monotherapy or combined with valproate and/or lithium. Combining this agent with carbamazepine is not recommended because of the possibility of an increased risk of hematotoxicity.
Electroconvulsive therapy may be used safely and effectively in patients who are severely ill (e.g., those with manic delirium); pose an immediate danger because of their potential for violence; are in medical crisis; or have medical contraindications to pharmacotherapy. There is preliminary evidence that ECT can be safely administered with novel antipsychotics such as clozapine, risperidone, or olanzapine to produce additional benefit in patients insufficiently responsive to either therapy alone.
Related resources
- International Society for Bipolar Disorders www.isbd.org
Drug brand names
- Amitriptyline • Elavil
- Amoxapine • Asendin
- Aripiprazole • (in development)
- Carbamazepine • Tegretol, Epitol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Iloperidone • (in development)
- Imipramine • Tofranil
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproate sodium • Depacon
- Ziprasidone • Geodon
Disclosure
The author reports that he receives research/grant support from, serves as a consultant for, and on the speaker’s bureau of Janssen Pharmaceutica. He also receives research/grant support from Genentech Inc. and Bristol-Myers Squibb Co.; serves as a consultant for Pfizer Inc., Sepracor, and Novartis Pharmaceuticals Corp.; and is on the speaker’s bureau of Abbott Laboratories, Eli Lilly and Co., Pfizer Inc., Forest Pharmaceuticals, Bristol-Myers Squibb Co., and Wyeth-Ayerst Pharmaceuticals.
Major mood disorders are challenging to diagnose and often difficult to treat. They entail unipolar depression; bipolar disorder, which includes manic, depressed, or mixed episodes; and schizoaffective disorder, which includes both depressed and bipolar subtypes. Antidepressants and mood stabilizers are the primary pharmacological treatments. They may be insufficient, however, for patients with more severe episodes, often characterized by psychosis and treatment resistance.
In these patients, antipsychotics have played an important but controversial part in management, primarily as oral or parenteral adjuncts. Literature and clinical experience now support another, unique role for the current generation of novel agents.
Compared to earlier antipsychotics, these agents produce substantially fewer neurological adverse effects, including acute extrapyramidal and tardive syndromes, and can augment antidepressants and mood stabilizers. In addition, they may:
- Possess a better antipsychotic profile, with enhanced therapeutic effects on positive, negative, cognitive, and mood symptoms
- Have a role in the acute and long-term management of these disorders when anticipated parenteral formulations become available (e.g., acute intramuscular olanzapine and ziprasidone—and long-acting intramuscular risperidone)
- Possess inherent thymoleptic properties (see “Unresolved issues with antipsychotics,” below).
- Defining what constitutes a mood stabilizer.1 Proposed definitions suggest that the drug must entail the following:
- Clarifying the mechanisms underlying the apparent mood-regulating effects of novel agents
- Ascertaining both acute and maintenance efficacy
- Clarifying the propensity of some agents to switch depressed patients into mania
- Increasing the number of well-designed studies with sufficient sample sizes, including comparison trials assessing the relative efficacy of different novel agents
- Reducing the tendency to publish only positive reports when new drugs are first available
- Introducing parenteral formulations of novel agents
- Resolving concerns about weight gain, new-onset diabetes, QT c prolongation, and sedation
- Rectifying the current level of substantially greater costs
Management of unipolar depression
Neuroleptics Delusions and hallucinations indicate a more severe form of depressive disorder, with poor short- and long-term outcomes in comparison to those without psychosis. To illustrate, Table 1 lists a summary of response rates in psychotic and nonpsychotic depressed patients given a tricyclic antidepressant (TCA). The data indicate that patients suffering from psychotic depression typically do not benefit from antidepressant monotherapy and usually require a combination of antidepressant and antipsychotic or, alternatively, electroconvulsive therapy (ECT).
There is, however, some limited clinical and neuroimaging evidence that amoxapine can be used as an effective monotherapy in this group. Amoxapine is an antidepressant whose primary active metabolite, 8-hydroxy amoxapine, may have antipsychotic properties.1 With the possible exception of amoxapine, combined antipsychotic-antidepressant treatment is the rule.
Table 1
Psychotic and nonpsychotic depressed patients’ response to monotherapy with a tricyclic antidepressant
| Psychotic | Nonpsychotic | ||||
|---|---|---|---|---|---|
| Responders (%) (n=127) | Nonresponders (%) (n=236) | Responders (%) (n=464) | Nonresponders (%) (n=227) | Difference | |
| 13 studies | 35% | 65% | 67% | 33% | 32% |
| Adapted from Chan CH, Janicak PG, Davis JM, et al. Response of psychotic and nonpsychotic depressed patients to tricyclic antidepressants. J Clin Psychiatry. 1987;48:197-200. | |||||
Historically, studies have also evaluated neuroleptic monotherapy for depressed patients. While some reported superiority over a placebo, none found conventional antipsychotics superior to imipramine. Indeed, patients with schizophrenia who are treated with a neuroleptic often develop symptoms that are difficult to distinguish from depression (e.g., secondary negative symptoms). These often improve when the neuroleptic is discontinued or the patients are switched to a novel antipsychotic such as risperidone, olanzapine, or ziprasidone, all of which have putative antidepressant effects.
When employing an antipsychotic in depressed patients, the dosage and duration of treatment are two critical considerations. To minimize neuromotor adverse effects, use low doses of a neuroleptic (e.g., haloperidol, 1 to 5 mg/d) in conjunction with the primary antidepressant therapy. The neuroleptic should then be tapered gradually after psychotic symptoms have been controlled, usually during the acute phase of treatment. Ideally, patients would then take antidepressant monotherapy through the continuation phase and, if necessary, the maintenance phase of treatment. If psychosis recurs, re-introduce the antipsychotic intermittently.
Novel antipsychotics In contrast to neuroleptics, novel antipsychotics have been reported to improve depression in various psychotic and mood disorders.
For example, ziprasidone has serotonin and noradrenergic reuptake blocking effects comparable to such classic TCAs as imipramine and amitriptyline, as well as high binding affinity at the 5-HT1A, 5-HT1D, and 5-HT2C receptors. This neuroreceptor profile indicates possible antidepressant effects.
While randomized, controlled trials with mood-disordered patients are few, there have been promising preliminary reports of augmentation of antidepressants with risperidone and olanzapine in both psychotic and nonpsychotic depressed patients.
Ostroff and Nelson2 reported the results of an open-label study of eight SSRI-nonresponsive patients (mean treatment 7.3 weeks). These patients had no psychotic features and had a dramatic reduction in depressive symptoms, as well as some improvement in sexual dysfunction, with the addition of 0.5 mg to 1.0 mg risperidone. The clinicians suggested that risperidone’s 5-HT2A antagonism might explain its augmentation of the partial SSRI response.
Olanzapine alone (n=3) or combined with an antidepressant (n=12) has also been reported to improve both depression and psychosis.3 In a double-blind, amitriptyline-controlled trial, Svestka and Synek4 found that olanzapine demonstrated antidepressant efficacy in 33 unipolar and seven bipolar depressed patients. Thirteen of these patients also had psychotic symptoms.
Shelton et al5 reported the results of a two-center, 8-week, double-blind comparison of olanzapine alone, fluoxetine alone, or their combination in 28 patients suffering from treatment-resistant, non-bipolar disorder without psychosis. They found that the combination was superior to either drug alone based on improvement in the Hamilton Depression Rating Scale (HDRS) total score. From their preliminary data, it also appears that the doses required were relatively low, reducing the risk of side effects.
Their findings, however, need to be replicated in more controlled studies with combinations, addressing possible adverse effects, the potential for clinically relevant drug interactions, decreased compliance rates, and increased cost of treatment. Earlier reports raised concern about the potential of these agents to increase switching to hypomania or mania. But in more recent reports, this has not emerged as a significant problem.7
Finally, several case reports and case series indicate that agents such as clozapine and risperidone may augment ECT in particularly severe, treatment-resistant depressive episodes.7
Management of bipolar and schizoaffective depressed episodes
Neuroleptics Antipsychotics are frequently used to manage more severe, usually psychotic episodes of bipolar and schizoaffective depression. Reports indicate that affectively ill patients receiving neuroleptics may be more prone to develop neuromotor adverse effects than are those suffering from schizophrenia. Thus, their use for such patients must be well justified, limited in dosage and duration, and carefully monitored for the emergence of acute and tardive neurological events.
Novel antipsychotics Novel antipsychotics have demonstrated fewer propensities than have neuroleptics in worsening depression or negative symptoms in schizophrenic patients, and have possible antidepressant effects. In support of this hypothesis, and reminiscent of data from earlier risperidone and olanzapine trials, ziprasidone was observed to improve the Montgomery Asberg Rating Scale (MADRS) and Brief Psychotic Rating Scale (BPRS) depressive cluster scores in three clinical trials with schizophrenic and schizoaffective patients.8,9
Vieta et al reported the efficacy and safety of risperidone add-on therapy for treating various episodes of bipolar (n=358) and schizoaffective (n=183) disorders.6 In this multicenter, open study, 33 patients (6.1%) suffered a depressed episode and received a mean risperidone dose of 1.6 (± 2.3) mg/d added to their ongoing but ineffective drug regimen. Mean HDRS declined significantly over the 6-month course. Further, switch rates were low and in the expected range for spontaneous fluctuations seen in these disorders.
The results of a 6-week, double-blind, controlled trial of risperidone versus haloperidol in 62 patients with schizoaffective disorder, bipolar or depressed subtype, were published.10 Risperidone (average dose of 5.5 mg/d) was comparable to haloperidol (average dose of 10.8 mg/d) in reducing the mean in the Positive and Negative Syndrome Scale and Clinician-Administered Rating Scale for Mania change scores.
In those patients with baseline HDRS scores ≥ 20, risperidone produced a significantly greater reduction in mean change scores than did haloperidol. In addition, patients had no mood switches with risperidone or haloperidol; there was a significantly higher incidence of patients who had extra-pyramidal symptoms with haloperidol than among those taking risperidone; and six patients in the group taking haloperidol dropped out after experiencing adverse effects. None of the patients taking risperidone dropped out.
Table 2
Lithium versus antipsychotics for acute mania
| Lithium | Antipsychotics | ||||
|---|---|---|---|---|---|
| Responders (%) (n=64) | Nonresponders (%) (n=10) | Responders (%) (n=38) | Nonresponders (%) (n=33) | Difference | |
| 5 studies | 89% | 11% | 54% | 46% | 35% |
| Adapted from Janicak PG, Newman RH, Davis JM. Advances in the treatment of mania and related disorders: a reappraisal. Psychiatric Ann. 1992;22(2):94. | |||||
Management of bipolar manic or mixed episodes
Up to 80% of all bipolar patients receive an antipsychotic drug during the acute and/or maintenance phase of their illness, even though loading doses of valproate and benzodiazepines may also be used during an exacerbation and pose much less risk, especially in terms of adverse neurological effects.
Neuroleptics Shortly after their introduction, neuroleptics were found to reduce mortality secondary to dehydration and exhaustion in many highly agitated patients during an acute manic episode such as lethal catatonia.7
While earlier controlled studies found these agents to be effective in the treatment of acute mania, they are clearly less efficacious than lithium for core manic symptoms.11Table 2 demonstrates a meta-analysis of five well-controlled, double-blind studies documenting the statistical superiority of lithium over neuroleptics. These agents, however, offer the advantage of a more rapid onset of action, particularly when given in the acute parenteral formulation, and are superior to lithium in the initial control of agitation. Further, long-acting depot formulations of neuroleptics may be the only viable strategy for chronic, recurrent, noncompliant patients.
As with psychotic depression, dosing and duration of neuroleptic treatment are important concerns. In this context, Rifkin et al demonstrated that 10 mg of haloperidol per day had comparable efficacy but fewer adverse effects than did 30 or 80 mg per day in a group of acutely manic patients.12 Despite such data, high chlorpromazine-equivalent doses are often administered acutely and maintained for sustained periods. This can be a significant problem given the apparent great sensitivity of bipolar patients to the neurological sequelae of these antipsychotic agents.
Novel antipsychotics Early case series reports indicated that clozapine may benefit treatment-refractory bipolar patients. Given the inherent drawbacks of clozapine (e.g., agranulocytosis and seizure induction), attention now focuses on other novel agents with more benign adverse effect profiles than clopazine. Controlled trials with olanzapine and risperidone serve to reinforce the usefulness of these as well as other novel agents.
Tohen et al published the results of a 3-week, double-blind, placebo-controlled trial of olanzapine in 139 patients experiencing an acute bipolar manic or mixed episode.13 Olanzapine produced a statistically greater mean improvement than did the placebo on the Young Mania Rating Scale (YMRS) change scores. Further, 49% of the olanzapine-treated group (n=70) met the a priori criteria for response versus only 24% of the placebo-treated group (n=69). A second study using a higher starting dose of olanzapine, less rescue medication, and longer treatment duration than the first study resulted in a similar outcome.14
Sachs et al reported on the results of a 3-week, double-blind, placebo-controlled trial involving 156 patients with bipolar manic or mixed subtype who received a mood stabilizer (lithium or valproate) plus a placebo, risperidone (1 to 6 mg/d), or haloperidol (2 to 12 mg/d).15 The clinicians concluded that risperidone plus a mood stabilizer was statistically superior to a placebo plus a mood stabilizer, and produced more rapid reduction in manic symptoms, regardless of whether psychosis was present.
Sajatovic et al16 published the results of a prospective, open trial with quetiapine (mean dose = 203 ± 124 mg/d) as add-on therapy in 20 patients (10 bipolar, 10 schizoaffective; 19 male, 1 female) insufficiently responsive to their mood stabilizer or antipsychotic. Pre-post assessments indicated significant improvement in the BPRS, Mania Rating Scale (MRS), and HDRS scores. While the combination was generally well tolerated, there was a mean weight gain of 4.9 kg (10.8 lb). This raises the specter of complications associated with substantial weight gain produced by several of the novel antipsychotics.
A recent report indicates that ziprasidone may also be an effective antimanic agent. In a randomized, double-blind, placebo-controlled, multicenter trial involving 210 bipolar (manic or mixed episodes) patients, ziprasidone (80 to 160 mg/d; n=140) was compared to a placebo (n=70) for 3 weeks.17 By day 2 and all subsequent time points, ziprasidone was superior in terms of mean change scores from the baseline MRS; produced a more rapid and significantly greater improvement in overall psychopathology in both positive and negative symptoms; and did not produce significant adverse effects (including relevant ECG parameter changes) when compared with the placebo. Similar trials are being conducted for risperidone, aripiprazole, and iloperidone.
Finally, Meehan et al18 reported on the results of an acute parenteral formulation of olanzapine used to manage agitation in an acute manic or mixed episode. This was a 24-hour, double-blind, placebo-controlled trial comparing intramuscular olanzapine to intramuscular lorazepam. The following results were indicated:
- Olanzapine (doses of 5 to 10 mg) produced a significantly greater reduction in excitation than did the placebo or lorazepam at 30 minutes post-injection.
- Twice as many patients receiving lorazepam or a placebo versus olanzapine required more than one injection.
- Except for olanzapine-induced tachycardia in one patient, there were no significant changes in vital signs, ECG parameters, or laboratory assays among the three groups.
- Somnolence (13%) and dizziness (9%) were the most frequent side effects in the olanzapine group.
Treatment strategies for depression and mania
Considering the existing research data, clinical experience, and the risk/benefit ratio, treatment strategies that emphasize the role of antipsychotics in managing severe mood disorders are presented in the algorithms in Figures 1 and 2.
Figure 1 emphasizes the role of antipsychotics in the pharmacological management of patients with major depression. For unipolar depression with psychotic symptoms, options include an antidepressant plus an antipsychotic; amoxapine monotherapy; and possibly monotherapy with a novel agent such as ziprasidone. For bipolar depression with psychosis or schizoaffective disorder with depression, combining a mood stabilizer such as lithium plus an antipsychotic may be sufficient, but often an antidepressant must also be added. If the response is insufficient, consider switching to a novel antipsychotic (e.g., olanzapine or risperidone) plus a mood stabilizer (± antidepressant). In more serious exacerbations (e.g., high suicidality), ECT may be most appropriate. Secondary choices include clozapine with or without an antidepressant or novel antipsychotic such as risperidone combined with ECT.
Figure 2 describes the use of antipsychotics in patients with mania. If response to a primary mood stabilizer such as lithium, valproate, or their combination in the context of a bipolar or schizoaffective disorder is insufficient—or if patients have severe manic or psychotic symptoms—an antipsychotic may be added to the primary mood stabilizer.
Alternatively, when mood stabilizers are not tolerated or a clinical situation such as pregnancy precludes their use, a novel agent such as olanzapine or risperidone may be given as monotherapy. While the safety of these agents in pregnancy is not clearly established, clinical experience thus far indicates they may be safer than agents such as valproate or carbamazepine. These agents would be the first choice given their diminished propensity for extrapyramidal symptoms; absence of clozapine-related adverse effects such as agranulocytosis and seizures; and growing evidence of possible mood stabilizing effects.
Figure 1 ANTIPSYCHOTICS IN THE TREATMENT OF MAJOR DEPRESSION
Figure 2 ANTIPSYCHOTICS IN THE TREATMENT OF MANIA
For patients who remain nonresponsive, clozapine should be considered either as monotherapy or combined with valproate and/or lithium. Combining this agent with carbamazepine is not recommended because of the possibility of an increased risk of hematotoxicity.
Electroconvulsive therapy may be used safely and effectively in patients who are severely ill (e.g., those with manic delirium); pose an immediate danger because of their potential for violence; are in medical crisis; or have medical contraindications to pharmacotherapy. There is preliminary evidence that ECT can be safely administered with novel antipsychotics such as clozapine, risperidone, or olanzapine to produce additional benefit in patients insufficiently responsive to either therapy alone.
Related resources
- International Society for Bipolar Disorders www.isbd.org
Drug brand names
- Amitriptyline • Elavil
- Amoxapine • Asendin
- Aripiprazole • (in development)
- Carbamazepine • Tegretol, Epitol
- Clozapine • Clozaril
- Haloperidol • Haldol
- Iloperidone • (in development)
- Imipramine • Tofranil
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproate sodium • Depacon
- Ziprasidone • Geodon
Disclosure
The author reports that he receives research/grant support from, serves as a consultant for, and on the speaker’s bureau of Janssen Pharmaceutica. He also receives research/grant support from Genentech Inc. and Bristol-Myers Squibb Co.; serves as a consultant for Pfizer Inc., Sepracor, and Novartis Pharmaceuticals Corp.; and is on the speaker’s bureau of Abbott Laboratories, Eli Lilly and Co., Pfizer Inc., Forest Pharmaceuticals, Bristol-Myers Squibb Co., and Wyeth-Ayerst Pharmaceuticals.
1. Kapur S, Cho R, Jones C, et al. Is amoxapine an atypical antipsychotic? Positronemission tomography investigation of its dopamine2 and serotonin2 occupancy. Biol Psychiatry. 1999;45:1217-1220.
2. Ostroff RB, Nelson JC. Risperidone augmentation of selective serotonin reuptake inhibitors in major depression. J Clin Psychiatry. 1999;60:256-259.
3. Rothschild AJ, Bates KS, Boehringer KL, Syed A. Olanzapine response in psychotic depression. J Clin Psychiatry. 1999;60:116-118.
4. Svestka J, Synek O. Does olanzapine have antidepressant effect? A double-blind amitriptyline-controlled study [abstract]. Int J Neuropsychopharmacol. 2000;3(suppl 1):S251.-
5. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158:131-134.
6. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 5-month, multicenter, open study. J Clin Psychiatry. 2001;62(10):818.-
7. Janicak PG, Davis JM, et al. Principles and Practice of Psychopharmacotherapy. 3rd ed. Philadelphia, Pa: Lippincott-Williams & Wilkins; 2001.
8. Daniel DG, Zimbroff DL, et al. for the Ziprasidone Study Group Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Neuropsychopharmacol. 1999;20(5):491-505.
9. Keck PE, Jr, Buffenstein A, Ferguson J, et al. Ziprasidone 40 and 120 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 4-week placebo-controlled trial. Psychopharmacol. 1998;140:173-184.
10. Janicak PG, Keck PE, Jr, Davis JM, et al. A double-blind, randomized, prospective evaluation of the efficacy and safety of risperidone versus haloperidol in the treatment of schizoaffective disorder. J Clin Psychopharmacol. 2001;21:360-368.
11. Keck PE, Welge JA, McElroy SL, et al. Placebo effect in randomized, controlled studies of acute bipolar mania and depression. Biol Psychiatry. 2000;47(8):756-761.
12. Rifkin A, Doddi S, Karajgi B, et al. Dosage of haloperidol for mania. Br J Psychiatry. 1994;165:113-116.
13. Tohen M, Sanger TM, McElroy SL, et al. Olanzipine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry. 1999;156:702-709.
14. Tohen M, Jacobs TG, Grundy SL, et al. Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. The Olanzipine HGGW Study Group. Arch Gen Psychiatry. 2000;57:841-849.
15. Sachs G, Ghaemi N, Grossman F, Bowden C. Risperidone plus mood stabilizer vs. placebo plus mood stabilizer for acute mania of bipolar disorder: a double-blind comparison of efficacy and safety. International Congress on Bipolar Disorders. Pittsburgh, Pa. June 14-16, 2001.
16. Sajatovic M, Briscan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry. 2001;62:728-732.
17. Giller E, Mandel FS, Keck P. Ziprasidone in the acute treatment of mania: a double-blind, placebo-controlled, randomized trial. Schizophr Res. 2001;49(suppl 1-2):229.-
18. Meehan K, Zhang F, David S, Tohen N, Janicak PG, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular (IM) olanzapine versus IM lorazepam and IM placebo in acutely agitated patients diagnosed with mania associated with bipolar disorder. J Clin Psychopharmacol 2001;21:389-397.
1. Kapur S, Cho R, Jones C, et al. Is amoxapine an atypical antipsychotic? Positronemission tomography investigation of its dopamine2 and serotonin2 occupancy. Biol Psychiatry. 1999;45:1217-1220.
2. Ostroff RB, Nelson JC. Risperidone augmentation of selective serotonin reuptake inhibitors in major depression. J Clin Psychiatry. 1999;60:256-259.
3. Rothschild AJ, Bates KS, Boehringer KL, Syed A. Olanzapine response in psychotic depression. J Clin Psychiatry. 1999;60:116-118.
4. Svestka J, Synek O. Does olanzapine have antidepressant effect? A double-blind amitriptyline-controlled study [abstract]. Int J Neuropsychopharmacol. 2000;3(suppl 1):S251.-
5. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158:131-134.
6. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 5-month, multicenter, open study. J Clin Psychiatry. 2001;62(10):818.-
7. Janicak PG, Davis JM, et al. Principles and Practice of Psychopharmacotherapy. 3rd ed. Philadelphia, Pa: Lippincott-Williams & Wilkins; 2001.
8. Daniel DG, Zimbroff DL, et al. for the Ziprasidone Study Group Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Neuropsychopharmacol. 1999;20(5):491-505.
9. Keck PE, Jr, Buffenstein A, Ferguson J, et al. Ziprasidone 40 and 120 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 4-week placebo-controlled trial. Psychopharmacol. 1998;140:173-184.
10. Janicak PG, Keck PE, Jr, Davis JM, et al. A double-blind, randomized, prospective evaluation of the efficacy and safety of risperidone versus haloperidol in the treatment of schizoaffective disorder. J Clin Psychopharmacol. 2001;21:360-368.
11. Keck PE, Welge JA, McElroy SL, et al. Placebo effect in randomized, controlled studies of acute bipolar mania and depression. Biol Psychiatry. 2000;47(8):756-761.
12. Rifkin A, Doddi S, Karajgi B, et al. Dosage of haloperidol for mania. Br J Psychiatry. 1994;165:113-116.
13. Tohen M, Sanger TM, McElroy SL, et al. Olanzipine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry. 1999;156:702-709.
14. Tohen M, Jacobs TG, Grundy SL, et al. Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. The Olanzipine HGGW Study Group. Arch Gen Psychiatry. 2000;57:841-849.
15. Sachs G, Ghaemi N, Grossman F, Bowden C. Risperidone plus mood stabilizer vs. placebo plus mood stabilizer for acute mania of bipolar disorder: a double-blind comparison of efficacy and safety. International Congress on Bipolar Disorders. Pittsburgh, Pa. June 14-16, 2001.
16. Sajatovic M, Briscan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry. 2001;62:728-732.
17. Giller E, Mandel FS, Keck P. Ziprasidone in the acute treatment of mania: a double-blind, placebo-controlled, randomized trial. Schizophr Res. 2001;49(suppl 1-2):229.-
18. Meehan K, Zhang F, David S, Tohen N, Janicak PG, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular (IM) olanzapine versus IM lorazepam and IM placebo in acutely agitated patients diagnosed with mania associated with bipolar disorder. J Clin Psychopharmacol 2001;21:389-397.
Safe and effective care for your patients with diabetes
Type 2 diabetes mellitus is one of the most common and costly chronic diseases, afflicting 16 million people nationwide. According to American Diabetes Association statistics, the disease each year costs the United States more than $100 billion in health-care expenses and lost productivity.
Diabetes is associated with many psychiatric conditions, yet psychiatrists may not be aware that patients under treatment for mental disorders are suffering from diabetes or have problems related to their psychopharmacologic therapy. With changing criteria for the diagnosis of diabetes, new evidence about the prevention and treatment of this disease, and a growing link between diabetes and psychiatric issues, the practicing psychiatrist should be knowledgeable about such possible interactions.
The following three cases illustrate these challenges and offer pearls for patient management.
Type 1 diabetes is caused by an autoimmune phenomenon leading to beta-cell failure and absolute deficiency in insulin. Type 2 diabetes is characterized by tissue receptor resistance to insulin (aggravated by genetic factors, obesity, aging, and other problems), beta cell dysfunction (with defects in the timing and amount of insulin secretion), and changes in hepatic glucose output and glucose transport. Patients with type 2 diabetes will initially lose phase one (early) insulin secretion in response to a glucose load.
Unregulated production of hepatic glucose ultimately leads to abnormal fasting blood sugars. The beta cells will initially compensate, but will eventually fail. Thus, postprandial blood sugars will increase, reflecting the loss of early insulin secretion, but return relatively rapidly to normal. Gradually, fasting blood sugars will also rise as insulin resistance becomes more pronounced and the imbalance in hepatic glucogenesis occurs. Eventually, with absolute beta cell failure, patients with type 2 diabetes will require insulin to offset their insulinopenic state.
Case 1: Diabetes and depression
L.S., age 54, has a five-year history of type 2 diabetes. On referral, he presents with increasing lethargy, difficulty concentrating, and irritability. His mental status examination discloses anhedonia, moderate irritability, depressed mood, loss of appetite, and overall lethargy. He emphatically denies suicidal thoughts, but feels “overwhelmed with life.” His referring physician notes that he also suffers from hyperlipidemia and hypertension, and continues to smoke one pack per day. His current medications include atorvastatin, enalapril, glucophage, and one baby aspirin per day. His weight is 247 pounds. Other than mild background retinopathy and mild peripheral neuropathy, his last physical examination was normal. His last HbA1c was 8.8%, and his creatinine was 1.7.
How do you manage this patient?
The challenge Type 2 diabetes mellitus affects more than one in 17 persons in the U.S., and physicians diagnose approximately 800,000 cases yearly. Yet one third of individuals with diabetes are undiagnosed, and multiple studies suggest we are falling short of accepted guidelines for care. Diabetes remains the leading cause of blindness, renal failure, and non-traumatic amputation in adults. While care for patients with diabetes will largely fall to primary care physicians (it is the third most common problem seen by family physicians) and endocrinologists, psychiatrists will often also see these patients.
Case 1 concluded While this patient’s history clearly suggests major depressive disorder, the possibility of other medical complications (e.g., worsening renal function or lactic acidosis from metformin therapy) should be entertained. A serum lactate level was normal and a metabolic panel, including renal function, was stable. The patient responded well to the addition of a selective serotonin reuptake inhibitor (SSRI) for his major depressive disorder.
Comment Many patients with diabetes will present with symptoms and signs suggestive of depression and anxiety. Patients with diabetes are more likely to develop depression, a disorder that worsens the outcomes for such individuals. These patients are likely to take multiple medications and have many medical comorbidities. Therapy of psychiatric disorders in patients with diabetes may be complicated by drug-drug and drug-disease interactions. When patients with diabetes present with symptoms of a mental disorder, a careful assessment is essential.
The diagnosis of diabetes depends on the demonstration of either fasting glucose intolerance (plasma glucose 126) or abnormal response to glucose challenge (plasma glucose 200 following a 75 gm glucose challenge). Testing is repeated and not done at a time of stress, such as during an acute illness. The HbA1c is not recommended for the diagnosis of diabetes.
Risk factors for type 2 diabetes mellitus include:
- Obesity
- Family history of diabetes
- Race/ethnicity (African-American, Hispanic, Asian-American, Pacific Islander)
- Age ≥ 45
- Sedentary lifestyle
- Previous history of impaired glucose tolerance
- History of gestational diabetes or birth weight of child of 4 kg or more
- Hypertension
- HDL 35 ≤ mg per dL or triglyceride 250 ≥ mg per dL
Case 2: A patient on risperidone who develops diabetes
G.L., 47, has a longstanding history of schizophrenia. She has been on risperidone for one year and has done well, but has gained 14 pounds and now weighs 212 pounds. G.L. complains of difficulty seeing and returns for assessment. What next?
Psychiatric drug use and diabetes The incidence of mental health problems is increased in individuals with diabetes and psychiatric disorders may increase diabetic morbidity. Certain medications commonly used by psychiatrists may trigger diabetic complications and some hypoglycemic agents may be associated with potential drug-drug interactions or other difficulties (Tables 1 and 2).
Approximately 40% of patients with type 2 diabetes remain undiagnosed. It is estimated that diagnosis is delayed by 4 to 7 years after the development of their disease, and patients frequently present with established retinopathy, renal disease, or macrovascular disease. As the diagnostic criteria have changed and more patients are obese and lead sedentary lifestyles, the prevalence of recognized diabetes is increasing.
Table 1
Therapeutic options for type 2 diabetes treatment
| Class | Representative agents | Mechanism of action | Side effects, cautions, and notes | Common uses |
|---|---|---|---|---|
| First-generation sulfonylureas | Tolbutamide (Orinase), chlorpropamide (Diabinese), tolazamide (Tolinase) | Stimulate insulin secretion | Weight gain, hypoglycemia, fever, disulfiram type reaction. Caution: if significant hepaticor renal impairment; MAOIs may exacerbate hypoglycemia | Generic versions are least expensive oral hypoglycemics |
| Newer-generation sulfonylureas | Glipizide (Glucotrol, Glucotrol XL), glyburide (DiaBeta, Glynase), glimepiride (Amaryl) | Stimulate insulin secretion | Weight gain, hypoglycemia. Caution: with significant hepatic impairment; glyburide has active metabolite that may accumulate with renal dysfunction; MAOIs may exacerbate hypoglycemia | More potent; glipizide may lack some of the side effects of first-generation agents; common initial monotherapy |
| Metglitinides | Repaglinide (Prandin), nateglinide (Starlix) | Stimulate insulin secretion | Very short half life—must be given right before meals; metabolized by CYP-450 3A4 (may be induced by medications such as carbamazepine); highly protein bound; contraindicated in pregnancy | May help patients who have transient loss of diet control, postprandial hyperglycemia |
| Biguanides | Metformin (Glucophage, Glucophage XR) | Reduce hepatic glucose output and enhance insulin sensitivity | Gastrointestinal problems common initially; must be withheld before imaging with contrast media; lactic acidosis; contraindicated if renal or hepatic dysfunction, CHF, dehydration, hypoxemia; metallic taste | Overweight patients; favorable effects on lipids; fasting hyperglycemia |
| Thiazolidinediones | Pioglitazone (Actos), rosiglitazone (Avandia) | Enhance insulin sensitivity (cellular uptake of insulin) and inhibit hepatic glucose production | Hepatic toxicity; delayed onset of action; weight gain and fluid retention; contraindicated with CHF, liver disease | Useful as monotherapy or in combination; does not cause hypoglycemia and might ameliorate hyperlipidemia |
| Alpha-glucosidase inhibitors | Acarbose (Precose), miglitol (Glyset) | Inhibit breakdown and absorption of carbohydrates | Flatulence; need for high carbohydrate diet; cannot correct hypoglycemia with sucrose, maltose, or starch (but do not cause hypoglycemia on their own); contraindicated in patients with substantive renal and hepatic disease | Early in treatment for postprandial hyperglycemia; less potent than other agents |
| Combination agents | Glyburide/metformin (Glucovance) | As above | As above | Failure to meet goals on one agent alone; may reduce side effects of higher doses of either agent alone |
| Insulin | Short acting (Lispro and regular—aspart pending release); intermediate (NPH and Lente); long-acting (Ultralente and glargine) | Replace insulin, reduce hepatic glucose production, increase glucose uptake | Hypoglycemia; weight gain; must currently be injected | Failure to meet goals with oral agents or unable to take oral agents or to overcome glucose toxicity |
Table 2
Selected psychiatric drugs that interact with diabetes agents and patients with diabetes
| Drug Class | Effect |
|---|---|
| MAOIs | Hypoglycemia; may displace metglitinides and other protein-bound agents from serum proteins and cause hypoglycemia |
| SSRIs | Hypoglycemic unawareness |
| Tricyclics | May exacerbate autonomic neuropathy, orthostatic hypotension |
| Nefazodone | Highly protein bound and metabolized by CYP-3A4 (may effect metglitinide metabolism) |
| Bupropion | Liver metabolism |
| Carbamazepine | CYP-3A4 metabolized; may induce metglitinide metabolism |
| Valproate | Highly protein bound |
| Phenytoin | May decrease hypoglycemic effect of sulfonylureas |
| Benzodiazepines | Some (e.g., triazolam, alprazolam) metabolized by CYP/liver |
| Buspirone | Protein bound; CYP-3A4 metabolism |
| Antipsychotics | Weight gain may exacerbate or precipitate diabetes; liver metabolized |
| Note: Except for case reports, most of these agents are only theoretically implicated in the above drug-drug interactions (DDIs) or drug-disease interactions. Remember to assess all medications used in persons with diabetes, many of which do have substantial potential for DDIs. | |
The growing association of impaired glucose tolerance with progression to diabetes, the availability of effective interventions, and the high burden of morbidity for unrecognized diabetes suggest that more aggressive screening may be warranted.
Case 2 concluded Weight gain associated with atypical antipsychotic agents is all too common, and will often tip a patient “over the edge” from impaired glucose tolerance to type 2 diabetes. G.L. was referred to her primary care physician for assessment. Her fasting blood glucose Commonly used psychiatric medications may cause weight gain that exacerbates or precipitates type 2 diabetes was 312. Repeat FBG was 299. An ophthalmologic evaluation disclosed background changes consistent with diabetic retinopathy. Type 2 diabetes was diagnosed.
This patient deserves aggressive attention to modifiable risk factors, and warrants therapy for diabetes. Appropriate modification of diet, exercise, smoking and other risk factors—and medical comanagement—are critical. This includes attention to the psychotropic drugs she is taking.
Comment Medications commonly used by psychiatrists (e.g., atypical antipsychotics) may be associated with weight gain that exacerbates or precipitates type 2 diabetes.
The psychiatrist also must be aware of other potential medical comorbidities of treatment. Drug-drug interactions may occur with agents that are hepatic metabolized, including commonly used therapies for bipolar disorder (Table 2).
Metglitinides are metabolized by the CYP-3A4 system and drugs such as barbiturates and carbamazepine may induce this enzyme and reduce effectiveness. MAO inhibitors are associated with hypoglycemia with a number of agents, including sulfonylureas, and highly protein-bound agents such as the MAO inhibitors may displace repaglinide and increase its hypoglycemic activity. Fluoxetine and other SSRIs may cause hypoglycemic unawareness. Oral hypoglycemia agents themselves can be associated with hypoglycemia, and the onset may be confused with anxiety or panic attacks. The older sulfonylureas may cause inappropriate ADH (SIADH). Biguanides are occasionally associated with potentially catastrophic lactic acidosis.
Case 3: Disordered eating in an adolescent with type 1 diabetes
B.C., a 17-year-old with type 1 diabetes mellitus, is referred to a psychiatrist for a possible eating disorder. She was diagnosed with diabetes when she was 4. Over the past year her diabetes self-care has become increasingly erratic. B.C.’s mother notes that the patient often skips her insulin altogether, is preoccupied with her weight, and consumes large amounts of junk food. B.C. also admits to purging when she has been particularly lax with her diet.
Interaction between psychiatric and endocrine disorders Disordered eating appears to be frequent in adolescent girls and women with diabetes. Conscious underdosing of insulin and irregular eating habits may occur when patients are concerned about their body image, feel a stigma about using insulin, or fear they won’t fit in with friends.
Diabetes treatment requires a comprehensive approach embracing education, regular history and physical examinations, routine laboratory evaluations, and establishment of counseling goals. The foundation of care lies on appropriate diet and exercise.
Increasingly, a “stepped care approach” to medication is being advocated based on the patient’s stage of disease. For individuals with early type 2 diabetes, risk factor modification, diet, and exercise may be sufficient. Later, as further insulin resistance occurs, oral hypoglycemic agents must be added. A number of therapeutic options are available (Table 1). Finally, late in the course of type 2 diabetes, as absolute insulin deficiency occurs, combination therapy and insulin are used. Insulin is also often required for initial therapy to “rescue” the overstressed beta cells and overcome “glucose toxicity.”
Little evidence exists to guide the choice of treatment of type 2 diabetes, and nuances of therapy are beyond the scope of this article. However, several points are worth reinforcing:
- Ideal treatment is geared to normalizing the blood sugar at all times and achieving a near normal A1c (6.5% to 7%).
- Lifestyle modifications are important, and even relatively small changes in weight can substantially increase insulin sensitivity.
- Risk factor modification (e.g., smoking, lipids, hypertension) is extremely important.
- Therapy for type 2 diabetes is not static. As the disease progresses, more aggressive therapy is often required.
It also appears that depression may be associated with diabetes, perhaps through an intervening effect on diet and exercise. The incidence of depression in patients with diabetes is up to 28%, and women with diabetes appear to have a greater risk for depression than men. Patients with diabetes who are depressed are less likely to adhere to their diabetes program and more likely to have worse glycemic control and increasing risk of complications.
Of course, prevention is the best treatment of diabetes, and promising data are emerging. Increased physical activity (irrespective of BMI) and weight control appear to reduce both the risk of developing type 2 diabetes and the risk of progression from impaired glucose tolerance to overt diabetes. Smoking cessation may also play a role by improving insulin sensitivity. The Diabetes Prevention Program, a multicenter trial sponsored by the National Institutes of Health, should provide definitive data on primary prevention; recommendations based on the initial results of this trial are being developed.
The value of secondary prevention (screening) for type 2 diabetes has been debated. The American Diabetes Association recommends screening all individuals age 45 and older, while the U.S. Preventive Services Task Force suggests there is insufficient evidence to recommend for or against routine screening.
The all-cause mortality rate is doubled for individuals with diabetes. Good data from controlled trials suggest that improved glycemic control diminishes the microvascular complications of diabetes (e.g., retinopathy). A goal of a normal or near normal HbA1c (6.5% to 7.0%) is recommended.
The leading causes of mortality in patients with type 2 diabetes include coronary heart disease and complications of diabetes. The influence on macrovascular complications such as myocardial infarction is less clear. Thus, cardiac risk factors must be managed aggressively.
Diabetic retinopathy is the leading cause of blindness, diabetic nephropathy is the most common reason for end-stage renal disease, and diabetic neuropathy is the most frequent origin of amputation in the United States. Tertiary screening is directed toward early detection and treatment of these complications.
Case 3 concluded B.C. is concerned about weight gain, her friends making fun of her need for injections, and hypoglycemic reactions while playing varsity volleyball. Her concerns are explored and intensive counseling is undertaken. At the same time, she is referred to an endocrinologist for further evaluation, and the diabetes care team initiates therapy with an insulin pump.
After an initial rocky period, B.C.’s therapy is stabilized and her hypoglycemic episodes reduced. B.C. discusses her concerns with other teens in a diabetes support group and is introduced at the local college to a star volleyball player (who also suffers from diabetes). As B.C. graduates, she is offered a scholarship at a top university. Her HbA1c is at normal levels.
Comment Younger individuals with diabetes face substantial challenges in adjusting to their disease. The incidence of disordered eating, depression, anxiety, and adjustment disorders is increased.
What’s more, diabetes in children and adolescents affects the whole family. Parents and siblings are often stressed over the patient’s care needs and mood swings, and may also present with mental disorders.
Related resources Oriented to mental health issues
- Wirshing DA. Adverse effects of atypical antipschotics. J Clin Psych. 2001;62:(suppl 21)7-10.
- Goodnick PJ, Henry JH, Buki VMV. Treatment of depression in patients with diabetes mellitus. J Clin Psych. 1995;56:4,128-136.
- Carney C. Diabetes mellitus and major depressive disorder: an overview of prevalence, complications, and treatment. Depression Anxiety. 1998;7:149-157.
- Jacobson AM. The psychological care of patients with insulin-dependent diabetes mellitus. N Engl J Med. 1996;334(19), 1249-53.
- Glasgow RE, Fisher EB, Anderson BJ, et al. Behavioral science in diabetes. Contribution and opportunities. Diabetes Care. 1999;22(5):832-43.
- Hoffman RP. Eating disorders in adolescents with type 1 diabetes. Postgrad Med. 2001;109(4)67-74.
- Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care. 2000;23(10):1556-62.
- Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol. 2001;57(4):457-78.
- Golden MP. Special problems with children and adolescents with diabetes. Primary Care Clin. 1999; 26(4):885-94.
Drug brand names
- Alprazolam • Xanax
- Atorvastatin • Lipitor
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Carbamazepine • Tegretol, Epitol, Atretol
- Enalapril • Vasotec
- Fluoxetine • Prozac
- Nefazodone • Serzone
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Triazolam • Halcion
- Valproate • Depacon
Disclosure
The author reports that he has been a speaker or consultant for SmithKline Beecham, Organon, Wyeth-Ayerst Pharmaceuticals, and Pfizer.
General on diabetes
• Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:997-
• United Kingdom Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837-53.
• Reasner CA, Defronzo RA. Treatment of type 2 diabetes mellitus: a rational approach based on its pathophysiology. Am Fam Phys. 2001;63(9):1687-92.
• Clark CM, Fradkin JE, Hiss RG, et al. Promoting early diagnosis and treatment of type 2 diabetes. JAMA. 2000;284(3):363-4
• Evans RM, Brown EF, Krosnick A. eds. Managing diabetes. A CME program for primary care physicians. Chicago: American Medical Association, 2001.
Type 2 diabetes mellitus is one of the most common and costly chronic diseases, afflicting 16 million people nationwide. According to American Diabetes Association statistics, the disease each year costs the United States more than $100 billion in health-care expenses and lost productivity.
Diabetes is associated with many psychiatric conditions, yet psychiatrists may not be aware that patients under treatment for mental disorders are suffering from diabetes or have problems related to their psychopharmacologic therapy. With changing criteria for the diagnosis of diabetes, new evidence about the prevention and treatment of this disease, and a growing link between diabetes and psychiatric issues, the practicing psychiatrist should be knowledgeable about such possible interactions.
The following three cases illustrate these challenges and offer pearls for patient management.
Type 1 diabetes is caused by an autoimmune phenomenon leading to beta-cell failure and absolute deficiency in insulin. Type 2 diabetes is characterized by tissue receptor resistance to insulin (aggravated by genetic factors, obesity, aging, and other problems), beta cell dysfunction (with defects in the timing and amount of insulin secretion), and changes in hepatic glucose output and glucose transport. Patients with type 2 diabetes will initially lose phase one (early) insulin secretion in response to a glucose load.
Unregulated production of hepatic glucose ultimately leads to abnormal fasting blood sugars. The beta cells will initially compensate, but will eventually fail. Thus, postprandial blood sugars will increase, reflecting the loss of early insulin secretion, but return relatively rapidly to normal. Gradually, fasting blood sugars will also rise as insulin resistance becomes more pronounced and the imbalance in hepatic glucogenesis occurs. Eventually, with absolute beta cell failure, patients with type 2 diabetes will require insulin to offset their insulinopenic state.
Case 1: Diabetes and depression
L.S., age 54, has a five-year history of type 2 diabetes. On referral, he presents with increasing lethargy, difficulty concentrating, and irritability. His mental status examination discloses anhedonia, moderate irritability, depressed mood, loss of appetite, and overall lethargy. He emphatically denies suicidal thoughts, but feels “overwhelmed with life.” His referring physician notes that he also suffers from hyperlipidemia and hypertension, and continues to smoke one pack per day. His current medications include atorvastatin, enalapril, glucophage, and one baby aspirin per day. His weight is 247 pounds. Other than mild background retinopathy and mild peripheral neuropathy, his last physical examination was normal. His last HbA1c was 8.8%, and his creatinine was 1.7.
How do you manage this patient?
The challenge Type 2 diabetes mellitus affects more than one in 17 persons in the U.S., and physicians diagnose approximately 800,000 cases yearly. Yet one third of individuals with diabetes are undiagnosed, and multiple studies suggest we are falling short of accepted guidelines for care. Diabetes remains the leading cause of blindness, renal failure, and non-traumatic amputation in adults. While care for patients with diabetes will largely fall to primary care physicians (it is the third most common problem seen by family physicians) and endocrinologists, psychiatrists will often also see these patients.
Case 1 concluded While this patient’s history clearly suggests major depressive disorder, the possibility of other medical complications (e.g., worsening renal function or lactic acidosis from metformin therapy) should be entertained. A serum lactate level was normal and a metabolic panel, including renal function, was stable. The patient responded well to the addition of a selective serotonin reuptake inhibitor (SSRI) for his major depressive disorder.
Comment Many patients with diabetes will present with symptoms and signs suggestive of depression and anxiety. Patients with diabetes are more likely to develop depression, a disorder that worsens the outcomes for such individuals. These patients are likely to take multiple medications and have many medical comorbidities. Therapy of psychiatric disorders in patients with diabetes may be complicated by drug-drug and drug-disease interactions. When patients with diabetes present with symptoms of a mental disorder, a careful assessment is essential.
The diagnosis of diabetes depends on the demonstration of either fasting glucose intolerance (plasma glucose 126) or abnormal response to glucose challenge (plasma glucose 200 following a 75 gm glucose challenge). Testing is repeated and not done at a time of stress, such as during an acute illness. The HbA1c is not recommended for the diagnosis of diabetes.
Risk factors for type 2 diabetes mellitus include:
- Obesity
- Family history of diabetes
- Race/ethnicity (African-American, Hispanic, Asian-American, Pacific Islander)
- Age ≥ 45
- Sedentary lifestyle
- Previous history of impaired glucose tolerance
- History of gestational diabetes or birth weight of child of 4 kg or more
- Hypertension
- HDL 35 ≤ mg per dL or triglyceride 250 ≥ mg per dL
Case 2: A patient on risperidone who develops diabetes
G.L., 47, has a longstanding history of schizophrenia. She has been on risperidone for one year and has done well, but has gained 14 pounds and now weighs 212 pounds. G.L. complains of difficulty seeing and returns for assessment. What next?
Psychiatric drug use and diabetes The incidence of mental health problems is increased in individuals with diabetes and psychiatric disorders may increase diabetic morbidity. Certain medications commonly used by psychiatrists may trigger diabetic complications and some hypoglycemic agents may be associated with potential drug-drug interactions or other difficulties (Tables 1 and 2).
Approximately 40% of patients with type 2 diabetes remain undiagnosed. It is estimated that diagnosis is delayed by 4 to 7 years after the development of their disease, and patients frequently present with established retinopathy, renal disease, or macrovascular disease. As the diagnostic criteria have changed and more patients are obese and lead sedentary lifestyles, the prevalence of recognized diabetes is increasing.
Table 1
Therapeutic options for type 2 diabetes treatment
| Class | Representative agents | Mechanism of action | Side effects, cautions, and notes | Common uses |
|---|---|---|---|---|
| First-generation sulfonylureas | Tolbutamide (Orinase), chlorpropamide (Diabinese), tolazamide (Tolinase) | Stimulate insulin secretion | Weight gain, hypoglycemia, fever, disulfiram type reaction. Caution: if significant hepaticor renal impairment; MAOIs may exacerbate hypoglycemia | Generic versions are least expensive oral hypoglycemics |
| Newer-generation sulfonylureas | Glipizide (Glucotrol, Glucotrol XL), glyburide (DiaBeta, Glynase), glimepiride (Amaryl) | Stimulate insulin secretion | Weight gain, hypoglycemia. Caution: with significant hepatic impairment; glyburide has active metabolite that may accumulate with renal dysfunction; MAOIs may exacerbate hypoglycemia | More potent; glipizide may lack some of the side effects of first-generation agents; common initial monotherapy |
| Metglitinides | Repaglinide (Prandin), nateglinide (Starlix) | Stimulate insulin secretion | Very short half life—must be given right before meals; metabolized by CYP-450 3A4 (may be induced by medications such as carbamazepine); highly protein bound; contraindicated in pregnancy | May help patients who have transient loss of diet control, postprandial hyperglycemia |
| Biguanides | Metformin (Glucophage, Glucophage XR) | Reduce hepatic glucose output and enhance insulin sensitivity | Gastrointestinal problems common initially; must be withheld before imaging with contrast media; lactic acidosis; contraindicated if renal or hepatic dysfunction, CHF, dehydration, hypoxemia; metallic taste | Overweight patients; favorable effects on lipids; fasting hyperglycemia |
| Thiazolidinediones | Pioglitazone (Actos), rosiglitazone (Avandia) | Enhance insulin sensitivity (cellular uptake of insulin) and inhibit hepatic glucose production | Hepatic toxicity; delayed onset of action; weight gain and fluid retention; contraindicated with CHF, liver disease | Useful as monotherapy or in combination; does not cause hypoglycemia and might ameliorate hyperlipidemia |
| Alpha-glucosidase inhibitors | Acarbose (Precose), miglitol (Glyset) | Inhibit breakdown and absorption of carbohydrates | Flatulence; need for high carbohydrate diet; cannot correct hypoglycemia with sucrose, maltose, or starch (but do not cause hypoglycemia on their own); contraindicated in patients with substantive renal and hepatic disease | Early in treatment for postprandial hyperglycemia; less potent than other agents |
| Combination agents | Glyburide/metformin (Glucovance) | As above | As above | Failure to meet goals on one agent alone; may reduce side effects of higher doses of either agent alone |
| Insulin | Short acting (Lispro and regular—aspart pending release); intermediate (NPH and Lente); long-acting (Ultralente and glargine) | Replace insulin, reduce hepatic glucose production, increase glucose uptake | Hypoglycemia; weight gain; must currently be injected | Failure to meet goals with oral agents or unable to take oral agents or to overcome glucose toxicity |
Table 2
Selected psychiatric drugs that interact with diabetes agents and patients with diabetes
| Drug Class | Effect |
|---|---|
| MAOIs | Hypoglycemia; may displace metglitinides and other protein-bound agents from serum proteins and cause hypoglycemia |
| SSRIs | Hypoglycemic unawareness |
| Tricyclics | May exacerbate autonomic neuropathy, orthostatic hypotension |
| Nefazodone | Highly protein bound and metabolized by CYP-3A4 (may effect metglitinide metabolism) |
| Bupropion | Liver metabolism |
| Carbamazepine | CYP-3A4 metabolized; may induce metglitinide metabolism |
| Valproate | Highly protein bound |
| Phenytoin | May decrease hypoglycemic effect of sulfonylureas |
| Benzodiazepines | Some (e.g., triazolam, alprazolam) metabolized by CYP/liver |
| Buspirone | Protein bound; CYP-3A4 metabolism |
| Antipsychotics | Weight gain may exacerbate or precipitate diabetes; liver metabolized |
| Note: Except for case reports, most of these agents are only theoretically implicated in the above drug-drug interactions (DDIs) or drug-disease interactions. Remember to assess all medications used in persons with diabetes, many of which do have substantial potential for DDIs. | |
The growing association of impaired glucose tolerance with progression to diabetes, the availability of effective interventions, and the high burden of morbidity for unrecognized diabetes suggest that more aggressive screening may be warranted.
Case 2 concluded Weight gain associated with atypical antipsychotic agents is all too common, and will often tip a patient “over the edge” from impaired glucose tolerance to type 2 diabetes. G.L. was referred to her primary care physician for assessment. Her fasting blood glucose Commonly used psychiatric medications may cause weight gain that exacerbates or precipitates type 2 diabetes was 312. Repeat FBG was 299. An ophthalmologic evaluation disclosed background changes consistent with diabetic retinopathy. Type 2 diabetes was diagnosed.
This patient deserves aggressive attention to modifiable risk factors, and warrants therapy for diabetes. Appropriate modification of diet, exercise, smoking and other risk factors—and medical comanagement—are critical. This includes attention to the psychotropic drugs she is taking.
Comment Medications commonly used by psychiatrists (e.g., atypical antipsychotics) may be associated with weight gain that exacerbates or precipitates type 2 diabetes.
The psychiatrist also must be aware of other potential medical comorbidities of treatment. Drug-drug interactions may occur with agents that are hepatic metabolized, including commonly used therapies for bipolar disorder (Table 2).
Metglitinides are metabolized by the CYP-3A4 system and drugs such as barbiturates and carbamazepine may induce this enzyme and reduce effectiveness. MAO inhibitors are associated with hypoglycemia with a number of agents, including sulfonylureas, and highly protein-bound agents such as the MAO inhibitors may displace repaglinide and increase its hypoglycemic activity. Fluoxetine and other SSRIs may cause hypoglycemic unawareness. Oral hypoglycemia agents themselves can be associated with hypoglycemia, and the onset may be confused with anxiety or panic attacks. The older sulfonylureas may cause inappropriate ADH (SIADH). Biguanides are occasionally associated with potentially catastrophic lactic acidosis.
Case 3: Disordered eating in an adolescent with type 1 diabetes
B.C., a 17-year-old with type 1 diabetes mellitus, is referred to a psychiatrist for a possible eating disorder. She was diagnosed with diabetes when she was 4. Over the past year her diabetes self-care has become increasingly erratic. B.C.’s mother notes that the patient often skips her insulin altogether, is preoccupied with her weight, and consumes large amounts of junk food. B.C. also admits to purging when she has been particularly lax with her diet.
Interaction between psychiatric and endocrine disorders Disordered eating appears to be frequent in adolescent girls and women with diabetes. Conscious underdosing of insulin and irregular eating habits may occur when patients are concerned about their body image, feel a stigma about using insulin, or fear they won’t fit in with friends.
Diabetes treatment requires a comprehensive approach embracing education, regular history and physical examinations, routine laboratory evaluations, and establishment of counseling goals. The foundation of care lies on appropriate diet and exercise.
Increasingly, a “stepped care approach” to medication is being advocated based on the patient’s stage of disease. For individuals with early type 2 diabetes, risk factor modification, diet, and exercise may be sufficient. Later, as further insulin resistance occurs, oral hypoglycemic agents must be added. A number of therapeutic options are available (Table 1). Finally, late in the course of type 2 diabetes, as absolute insulin deficiency occurs, combination therapy and insulin are used. Insulin is also often required for initial therapy to “rescue” the overstressed beta cells and overcome “glucose toxicity.”
Little evidence exists to guide the choice of treatment of type 2 diabetes, and nuances of therapy are beyond the scope of this article. However, several points are worth reinforcing:
- Ideal treatment is geared to normalizing the blood sugar at all times and achieving a near normal A1c (6.5% to 7%).
- Lifestyle modifications are important, and even relatively small changes in weight can substantially increase insulin sensitivity.
- Risk factor modification (e.g., smoking, lipids, hypertension) is extremely important.
- Therapy for type 2 diabetes is not static. As the disease progresses, more aggressive therapy is often required.
It also appears that depression may be associated with diabetes, perhaps through an intervening effect on diet and exercise. The incidence of depression in patients with diabetes is up to 28%, and women with diabetes appear to have a greater risk for depression than men. Patients with diabetes who are depressed are less likely to adhere to their diabetes program and more likely to have worse glycemic control and increasing risk of complications.
Of course, prevention is the best treatment of diabetes, and promising data are emerging. Increased physical activity (irrespective of BMI) and weight control appear to reduce both the risk of developing type 2 diabetes and the risk of progression from impaired glucose tolerance to overt diabetes. Smoking cessation may also play a role by improving insulin sensitivity. The Diabetes Prevention Program, a multicenter trial sponsored by the National Institutes of Health, should provide definitive data on primary prevention; recommendations based on the initial results of this trial are being developed.
The value of secondary prevention (screening) for type 2 diabetes has been debated. The American Diabetes Association recommends screening all individuals age 45 and older, while the U.S. Preventive Services Task Force suggests there is insufficient evidence to recommend for or against routine screening.
The all-cause mortality rate is doubled for individuals with diabetes. Good data from controlled trials suggest that improved glycemic control diminishes the microvascular complications of diabetes (e.g., retinopathy). A goal of a normal or near normal HbA1c (6.5% to 7.0%) is recommended.
The leading causes of mortality in patients with type 2 diabetes include coronary heart disease and complications of diabetes. The influence on macrovascular complications such as myocardial infarction is less clear. Thus, cardiac risk factors must be managed aggressively.
Diabetic retinopathy is the leading cause of blindness, diabetic nephropathy is the most common reason for end-stage renal disease, and diabetic neuropathy is the most frequent origin of amputation in the United States. Tertiary screening is directed toward early detection and treatment of these complications.
Case 3 concluded B.C. is concerned about weight gain, her friends making fun of her need for injections, and hypoglycemic reactions while playing varsity volleyball. Her concerns are explored and intensive counseling is undertaken. At the same time, she is referred to an endocrinologist for further evaluation, and the diabetes care team initiates therapy with an insulin pump.
After an initial rocky period, B.C.’s therapy is stabilized and her hypoglycemic episodes reduced. B.C. discusses her concerns with other teens in a diabetes support group and is introduced at the local college to a star volleyball player (who also suffers from diabetes). As B.C. graduates, she is offered a scholarship at a top university. Her HbA1c is at normal levels.
Comment Younger individuals with diabetes face substantial challenges in adjusting to their disease. The incidence of disordered eating, depression, anxiety, and adjustment disorders is increased.
What’s more, diabetes in children and adolescents affects the whole family. Parents and siblings are often stressed over the patient’s care needs and mood swings, and may also present with mental disorders.
Related resources Oriented to mental health issues
- Wirshing DA. Adverse effects of atypical antipschotics. J Clin Psych. 2001;62:(suppl 21)7-10.
- Goodnick PJ, Henry JH, Buki VMV. Treatment of depression in patients with diabetes mellitus. J Clin Psych. 1995;56:4,128-136.
- Carney C. Diabetes mellitus and major depressive disorder: an overview of prevalence, complications, and treatment. Depression Anxiety. 1998;7:149-157.
- Jacobson AM. The psychological care of patients with insulin-dependent diabetes mellitus. N Engl J Med. 1996;334(19), 1249-53.
- Glasgow RE, Fisher EB, Anderson BJ, et al. Behavioral science in diabetes. Contribution and opportunities. Diabetes Care. 1999;22(5):832-43.
- Hoffman RP. Eating disorders in adolescents with type 1 diabetes. Postgrad Med. 2001;109(4)67-74.
- Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care. 2000;23(10):1556-62.
- Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol. 2001;57(4):457-78.
- Golden MP. Special problems with children and adolescents with diabetes. Primary Care Clin. 1999; 26(4):885-94.
Drug brand names
- Alprazolam • Xanax
- Atorvastatin • Lipitor
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Carbamazepine • Tegretol, Epitol, Atretol
- Enalapril • Vasotec
- Fluoxetine • Prozac
- Nefazodone • Serzone
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Triazolam • Halcion
- Valproate • Depacon
Disclosure
The author reports that he has been a speaker or consultant for SmithKline Beecham, Organon, Wyeth-Ayerst Pharmaceuticals, and Pfizer.
Type 2 diabetes mellitus is one of the most common and costly chronic diseases, afflicting 16 million people nationwide. According to American Diabetes Association statistics, the disease each year costs the United States more than $100 billion in health-care expenses and lost productivity.
Diabetes is associated with many psychiatric conditions, yet psychiatrists may not be aware that patients under treatment for mental disorders are suffering from diabetes or have problems related to their psychopharmacologic therapy. With changing criteria for the diagnosis of diabetes, new evidence about the prevention and treatment of this disease, and a growing link between diabetes and psychiatric issues, the practicing psychiatrist should be knowledgeable about such possible interactions.
The following three cases illustrate these challenges and offer pearls for patient management.
Type 1 diabetes is caused by an autoimmune phenomenon leading to beta-cell failure and absolute deficiency in insulin. Type 2 diabetes is characterized by tissue receptor resistance to insulin (aggravated by genetic factors, obesity, aging, and other problems), beta cell dysfunction (with defects in the timing and amount of insulin secretion), and changes in hepatic glucose output and glucose transport. Patients with type 2 diabetes will initially lose phase one (early) insulin secretion in response to a glucose load.
Unregulated production of hepatic glucose ultimately leads to abnormal fasting blood sugars. The beta cells will initially compensate, but will eventually fail. Thus, postprandial blood sugars will increase, reflecting the loss of early insulin secretion, but return relatively rapidly to normal. Gradually, fasting blood sugars will also rise as insulin resistance becomes more pronounced and the imbalance in hepatic glucogenesis occurs. Eventually, with absolute beta cell failure, patients with type 2 diabetes will require insulin to offset their insulinopenic state.
Case 1: Diabetes and depression
L.S., age 54, has a five-year history of type 2 diabetes. On referral, he presents with increasing lethargy, difficulty concentrating, and irritability. His mental status examination discloses anhedonia, moderate irritability, depressed mood, loss of appetite, and overall lethargy. He emphatically denies suicidal thoughts, but feels “overwhelmed with life.” His referring physician notes that he also suffers from hyperlipidemia and hypertension, and continues to smoke one pack per day. His current medications include atorvastatin, enalapril, glucophage, and one baby aspirin per day. His weight is 247 pounds. Other than mild background retinopathy and mild peripheral neuropathy, his last physical examination was normal. His last HbA1c was 8.8%, and his creatinine was 1.7.
How do you manage this patient?
The challenge Type 2 diabetes mellitus affects more than one in 17 persons in the U.S., and physicians diagnose approximately 800,000 cases yearly. Yet one third of individuals with diabetes are undiagnosed, and multiple studies suggest we are falling short of accepted guidelines for care. Diabetes remains the leading cause of blindness, renal failure, and non-traumatic amputation in adults. While care for patients with diabetes will largely fall to primary care physicians (it is the third most common problem seen by family physicians) and endocrinologists, psychiatrists will often also see these patients.
Case 1 concluded While this patient’s history clearly suggests major depressive disorder, the possibility of other medical complications (e.g., worsening renal function or lactic acidosis from metformin therapy) should be entertained. A serum lactate level was normal and a metabolic panel, including renal function, was stable. The patient responded well to the addition of a selective serotonin reuptake inhibitor (SSRI) for his major depressive disorder.
Comment Many patients with diabetes will present with symptoms and signs suggestive of depression and anxiety. Patients with diabetes are more likely to develop depression, a disorder that worsens the outcomes for such individuals. These patients are likely to take multiple medications and have many medical comorbidities. Therapy of psychiatric disorders in patients with diabetes may be complicated by drug-drug and drug-disease interactions. When patients with diabetes present with symptoms of a mental disorder, a careful assessment is essential.
The diagnosis of diabetes depends on the demonstration of either fasting glucose intolerance (plasma glucose 126) or abnormal response to glucose challenge (plasma glucose 200 following a 75 gm glucose challenge). Testing is repeated and not done at a time of stress, such as during an acute illness. The HbA1c is not recommended for the diagnosis of diabetes.
Risk factors for type 2 diabetes mellitus include:
- Obesity
- Family history of diabetes
- Race/ethnicity (African-American, Hispanic, Asian-American, Pacific Islander)
- Age ≥ 45
- Sedentary lifestyle
- Previous history of impaired glucose tolerance
- History of gestational diabetes or birth weight of child of 4 kg or more
- Hypertension
- HDL 35 ≤ mg per dL or triglyceride 250 ≥ mg per dL
Case 2: A patient on risperidone who develops diabetes
G.L., 47, has a longstanding history of schizophrenia. She has been on risperidone for one year and has done well, but has gained 14 pounds and now weighs 212 pounds. G.L. complains of difficulty seeing and returns for assessment. What next?
Psychiatric drug use and diabetes The incidence of mental health problems is increased in individuals with diabetes and psychiatric disorders may increase diabetic morbidity. Certain medications commonly used by psychiatrists may trigger diabetic complications and some hypoglycemic agents may be associated with potential drug-drug interactions or other difficulties (Tables 1 and 2).
Approximately 40% of patients with type 2 diabetes remain undiagnosed. It is estimated that diagnosis is delayed by 4 to 7 years after the development of their disease, and patients frequently present with established retinopathy, renal disease, or macrovascular disease. As the diagnostic criteria have changed and more patients are obese and lead sedentary lifestyles, the prevalence of recognized diabetes is increasing.
Table 1
Therapeutic options for type 2 diabetes treatment
| Class | Representative agents | Mechanism of action | Side effects, cautions, and notes | Common uses |
|---|---|---|---|---|
| First-generation sulfonylureas | Tolbutamide (Orinase), chlorpropamide (Diabinese), tolazamide (Tolinase) | Stimulate insulin secretion | Weight gain, hypoglycemia, fever, disulfiram type reaction. Caution: if significant hepaticor renal impairment; MAOIs may exacerbate hypoglycemia | Generic versions are least expensive oral hypoglycemics |
| Newer-generation sulfonylureas | Glipizide (Glucotrol, Glucotrol XL), glyburide (DiaBeta, Glynase), glimepiride (Amaryl) | Stimulate insulin secretion | Weight gain, hypoglycemia. Caution: with significant hepatic impairment; glyburide has active metabolite that may accumulate with renal dysfunction; MAOIs may exacerbate hypoglycemia | More potent; glipizide may lack some of the side effects of first-generation agents; common initial monotherapy |
| Metglitinides | Repaglinide (Prandin), nateglinide (Starlix) | Stimulate insulin secretion | Very short half life—must be given right before meals; metabolized by CYP-450 3A4 (may be induced by medications such as carbamazepine); highly protein bound; contraindicated in pregnancy | May help patients who have transient loss of diet control, postprandial hyperglycemia |
| Biguanides | Metformin (Glucophage, Glucophage XR) | Reduce hepatic glucose output and enhance insulin sensitivity | Gastrointestinal problems common initially; must be withheld before imaging with contrast media; lactic acidosis; contraindicated if renal or hepatic dysfunction, CHF, dehydration, hypoxemia; metallic taste | Overweight patients; favorable effects on lipids; fasting hyperglycemia |
| Thiazolidinediones | Pioglitazone (Actos), rosiglitazone (Avandia) | Enhance insulin sensitivity (cellular uptake of insulin) and inhibit hepatic glucose production | Hepatic toxicity; delayed onset of action; weight gain and fluid retention; contraindicated with CHF, liver disease | Useful as monotherapy or in combination; does not cause hypoglycemia and might ameliorate hyperlipidemia |
| Alpha-glucosidase inhibitors | Acarbose (Precose), miglitol (Glyset) | Inhibit breakdown and absorption of carbohydrates | Flatulence; need for high carbohydrate diet; cannot correct hypoglycemia with sucrose, maltose, or starch (but do not cause hypoglycemia on their own); contraindicated in patients with substantive renal and hepatic disease | Early in treatment for postprandial hyperglycemia; less potent than other agents |
| Combination agents | Glyburide/metformin (Glucovance) | As above | As above | Failure to meet goals on one agent alone; may reduce side effects of higher doses of either agent alone |
| Insulin | Short acting (Lispro and regular—aspart pending release); intermediate (NPH and Lente); long-acting (Ultralente and glargine) | Replace insulin, reduce hepatic glucose production, increase glucose uptake | Hypoglycemia; weight gain; must currently be injected | Failure to meet goals with oral agents or unable to take oral agents or to overcome glucose toxicity |
Table 2
Selected psychiatric drugs that interact with diabetes agents and patients with diabetes
| Drug Class | Effect |
|---|---|
| MAOIs | Hypoglycemia; may displace metglitinides and other protein-bound agents from serum proteins and cause hypoglycemia |
| SSRIs | Hypoglycemic unawareness |
| Tricyclics | May exacerbate autonomic neuropathy, orthostatic hypotension |
| Nefazodone | Highly protein bound and metabolized by CYP-3A4 (may effect metglitinide metabolism) |
| Bupropion | Liver metabolism |
| Carbamazepine | CYP-3A4 metabolized; may induce metglitinide metabolism |
| Valproate | Highly protein bound |
| Phenytoin | May decrease hypoglycemic effect of sulfonylureas |
| Benzodiazepines | Some (e.g., triazolam, alprazolam) metabolized by CYP/liver |
| Buspirone | Protein bound; CYP-3A4 metabolism |
| Antipsychotics | Weight gain may exacerbate or precipitate diabetes; liver metabolized |
| Note: Except for case reports, most of these agents are only theoretically implicated in the above drug-drug interactions (DDIs) or drug-disease interactions. Remember to assess all medications used in persons with diabetes, many of which do have substantial potential for DDIs. | |
The growing association of impaired glucose tolerance with progression to diabetes, the availability of effective interventions, and the high burden of morbidity for unrecognized diabetes suggest that more aggressive screening may be warranted.
Case 2 concluded Weight gain associated with atypical antipsychotic agents is all too common, and will often tip a patient “over the edge” from impaired glucose tolerance to type 2 diabetes. G.L. was referred to her primary care physician for assessment. Her fasting blood glucose Commonly used psychiatric medications may cause weight gain that exacerbates or precipitates type 2 diabetes was 312. Repeat FBG was 299. An ophthalmologic evaluation disclosed background changes consistent with diabetic retinopathy. Type 2 diabetes was diagnosed.
This patient deserves aggressive attention to modifiable risk factors, and warrants therapy for diabetes. Appropriate modification of diet, exercise, smoking and other risk factors—and medical comanagement—are critical. This includes attention to the psychotropic drugs she is taking.
Comment Medications commonly used by psychiatrists (e.g., atypical antipsychotics) may be associated with weight gain that exacerbates or precipitates type 2 diabetes.
The psychiatrist also must be aware of other potential medical comorbidities of treatment. Drug-drug interactions may occur with agents that are hepatic metabolized, including commonly used therapies for bipolar disorder (Table 2).
Metglitinides are metabolized by the CYP-3A4 system and drugs such as barbiturates and carbamazepine may induce this enzyme and reduce effectiveness. MAO inhibitors are associated with hypoglycemia with a number of agents, including sulfonylureas, and highly protein-bound agents such as the MAO inhibitors may displace repaglinide and increase its hypoglycemic activity. Fluoxetine and other SSRIs may cause hypoglycemic unawareness. Oral hypoglycemia agents themselves can be associated with hypoglycemia, and the onset may be confused with anxiety or panic attacks. The older sulfonylureas may cause inappropriate ADH (SIADH). Biguanides are occasionally associated with potentially catastrophic lactic acidosis.
Case 3: Disordered eating in an adolescent with type 1 diabetes
B.C., a 17-year-old with type 1 diabetes mellitus, is referred to a psychiatrist for a possible eating disorder. She was diagnosed with diabetes when she was 4. Over the past year her diabetes self-care has become increasingly erratic. B.C.’s mother notes that the patient often skips her insulin altogether, is preoccupied with her weight, and consumes large amounts of junk food. B.C. also admits to purging when she has been particularly lax with her diet.
Interaction between psychiatric and endocrine disorders Disordered eating appears to be frequent in adolescent girls and women with diabetes. Conscious underdosing of insulin and irregular eating habits may occur when patients are concerned about their body image, feel a stigma about using insulin, or fear they won’t fit in with friends.
Diabetes treatment requires a comprehensive approach embracing education, regular history and physical examinations, routine laboratory evaluations, and establishment of counseling goals. The foundation of care lies on appropriate diet and exercise.
Increasingly, a “stepped care approach” to medication is being advocated based on the patient’s stage of disease. For individuals with early type 2 diabetes, risk factor modification, diet, and exercise may be sufficient. Later, as further insulin resistance occurs, oral hypoglycemic agents must be added. A number of therapeutic options are available (Table 1). Finally, late in the course of type 2 diabetes, as absolute insulin deficiency occurs, combination therapy and insulin are used. Insulin is also often required for initial therapy to “rescue” the overstressed beta cells and overcome “glucose toxicity.”
Little evidence exists to guide the choice of treatment of type 2 diabetes, and nuances of therapy are beyond the scope of this article. However, several points are worth reinforcing:
- Ideal treatment is geared to normalizing the blood sugar at all times and achieving a near normal A1c (6.5% to 7%).
- Lifestyle modifications are important, and even relatively small changes in weight can substantially increase insulin sensitivity.
- Risk factor modification (e.g., smoking, lipids, hypertension) is extremely important.
- Therapy for type 2 diabetes is not static. As the disease progresses, more aggressive therapy is often required.
It also appears that depression may be associated with diabetes, perhaps through an intervening effect on diet and exercise. The incidence of depression in patients with diabetes is up to 28%, and women with diabetes appear to have a greater risk for depression than men. Patients with diabetes who are depressed are less likely to adhere to their diabetes program and more likely to have worse glycemic control and increasing risk of complications.
Of course, prevention is the best treatment of diabetes, and promising data are emerging. Increased physical activity (irrespective of BMI) and weight control appear to reduce both the risk of developing type 2 diabetes and the risk of progression from impaired glucose tolerance to overt diabetes. Smoking cessation may also play a role by improving insulin sensitivity. The Diabetes Prevention Program, a multicenter trial sponsored by the National Institutes of Health, should provide definitive data on primary prevention; recommendations based on the initial results of this trial are being developed.
The value of secondary prevention (screening) for type 2 diabetes has been debated. The American Diabetes Association recommends screening all individuals age 45 and older, while the U.S. Preventive Services Task Force suggests there is insufficient evidence to recommend for or against routine screening.
The all-cause mortality rate is doubled for individuals with diabetes. Good data from controlled trials suggest that improved glycemic control diminishes the microvascular complications of diabetes (e.g., retinopathy). A goal of a normal or near normal HbA1c (6.5% to 7.0%) is recommended.
The leading causes of mortality in patients with type 2 diabetes include coronary heart disease and complications of diabetes. The influence on macrovascular complications such as myocardial infarction is less clear. Thus, cardiac risk factors must be managed aggressively.
Diabetic retinopathy is the leading cause of blindness, diabetic nephropathy is the most common reason for end-stage renal disease, and diabetic neuropathy is the most frequent origin of amputation in the United States. Tertiary screening is directed toward early detection and treatment of these complications.
Case 3 concluded B.C. is concerned about weight gain, her friends making fun of her need for injections, and hypoglycemic reactions while playing varsity volleyball. Her concerns are explored and intensive counseling is undertaken. At the same time, she is referred to an endocrinologist for further evaluation, and the diabetes care team initiates therapy with an insulin pump.
After an initial rocky period, B.C.’s therapy is stabilized and her hypoglycemic episodes reduced. B.C. discusses her concerns with other teens in a diabetes support group and is introduced at the local college to a star volleyball player (who also suffers from diabetes). As B.C. graduates, she is offered a scholarship at a top university. Her HbA1c is at normal levels.
Comment Younger individuals with diabetes face substantial challenges in adjusting to their disease. The incidence of disordered eating, depression, anxiety, and adjustment disorders is increased.
What’s more, diabetes in children and adolescents affects the whole family. Parents and siblings are often stressed over the patient’s care needs and mood swings, and may also present with mental disorders.
Related resources Oriented to mental health issues
- Wirshing DA. Adverse effects of atypical antipschotics. J Clin Psych. 2001;62:(suppl 21)7-10.
- Goodnick PJ, Henry JH, Buki VMV. Treatment of depression in patients with diabetes mellitus. J Clin Psych. 1995;56:4,128-136.
- Carney C. Diabetes mellitus and major depressive disorder: an overview of prevalence, complications, and treatment. Depression Anxiety. 1998;7:149-157.
- Jacobson AM. The psychological care of patients with insulin-dependent diabetes mellitus. N Engl J Med. 1996;334(19), 1249-53.
- Glasgow RE, Fisher EB, Anderson BJ, et al. Behavioral science in diabetes. Contribution and opportunities. Diabetes Care. 1999;22(5):832-43.
- Hoffman RP. Eating disorders in adolescents with type 1 diabetes. Postgrad Med. 2001;109(4)67-74.
- Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care. 2000;23(10):1556-62.
- Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol. 2001;57(4):457-78.
- Golden MP. Special problems with children and adolescents with diabetes. Primary Care Clin. 1999; 26(4):885-94.
Drug brand names
- Alprazolam • Xanax
- Atorvastatin • Lipitor
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Carbamazepine • Tegretol, Epitol, Atretol
- Enalapril • Vasotec
- Fluoxetine • Prozac
- Nefazodone • Serzone
- Phenytoin • Dilantin
- Risperidone • Risperdal
- Triazolam • Halcion
- Valproate • Depacon
Disclosure
The author reports that he has been a speaker or consultant for SmithKline Beecham, Organon, Wyeth-Ayerst Pharmaceuticals, and Pfizer.
General on diabetes
• Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:997-
• United Kingdom Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837-53.
• Reasner CA, Defronzo RA. Treatment of type 2 diabetes mellitus: a rational approach based on its pathophysiology. Am Fam Phys. 2001;63(9):1687-92.
• Clark CM, Fradkin JE, Hiss RG, et al. Promoting early diagnosis and treatment of type 2 diabetes. JAMA. 2000;284(3):363-4
• Evans RM, Brown EF, Krosnick A. eds. Managing diabetes. A CME program for primary care physicians. Chicago: American Medical Association, 2001.
General on diabetes
• Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:997-
• United Kingdom Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837-53.
• Reasner CA, Defronzo RA. Treatment of type 2 diabetes mellitus: a rational approach based on its pathophysiology. Am Fam Phys. 2001;63(9):1687-92.
• Clark CM, Fradkin JE, Hiss RG, et al. Promoting early diagnosis and treatment of type 2 diabetes. JAMA. 2000;284(3):363-4
• Evans RM, Brown EF, Krosnick A. eds. Managing diabetes. A CME program for primary care physicians. Chicago: American Medical Association, 2001.
Antiepileptic drugs for bipolar disorder: Are there any clear winners?
The newer antiepileptic drugs pose a sometimes bewildering range of options for bipolar disorder treatment. Which work best for acute bipolar I mania? Which are best suited for maintenance in patients with mixed episodes, or for those with a history of rapid cycling? What about prevention of depressive episodes? And how do the antiepileptics compare with lithium?
For many patients with bipolar disorder, lithium is still the drug of choice. For others, however, an increasing body of evidence supports the efficacy of some antiepileptics and atypical antipsychotics.
The mood-stabilizing properties of two antiepileptic agents, carbamazepine and valproate, were demonstrated some years ago in randomized controlled trials in patients with bipolar disorder. Since then, there has been considerable interest in the potential thymoleptic properties of the new antiepileptic drugs.1 In recent years gabapentin, lamotrigine, topiramate, oxcarbazepine, zonisamide, tiagabine, and levetiracetam have been approved in the United States for the treatment of various types of epilepsy. These medications have diverse pharmacological properties that distinguish them from earlier agents and from one another.
Do these new agents have anything to offer patients? For the most part, the evidence is not yet in hand, but we will examine what’s available, starting with the most recent trial data regarding the efficacy of valproate and carbamazepine.
Carbamazepine for bipolar mania
Five randomized, controlled trials2 have shown the efficacy of carbamazepine in patients with acute bipolar I mania. Carbamazepine was superior to placebo and comparable to chlorpromazine and lithium. Pooled data reveal an overall response rate (defined as the proportion of patients experiencing > 50% reduction in manic symptoms) of 50% for carbamazepine, 56% for lithium, and 61% for chlorpromazine (differences in overall response rates are not significant).
Until recently, the efficacy of carbamazepine as a maintenance therapy for bipolar disorder was controversial.3 However, two recent large randomized, controlled maintenance studies that compared carbamazepine with lithium validated use of the agent for that purpose.4,5
In the first study, 144 patients received either drug and were followed for up to 2 1/2 years.4 The study showed no significant differences between the two groups in time-to-mood episode recurrence or hospitalization. However, significantly more patients receiving carbamazepine required treatment discontinuation for side effects and additional medications for breakthrough symptoms than did the patients receiving lithium.
Patients without both comorbid disorders and mood-incongruent delusions responded better to lithium, whereas those with mixed episodes and bipolar II disorder or NOS appeared to respond better to carbamazepine.
In the second trial, 52 patients with bipolar I or II disorders received either lithium or carbamazepine for one year, crossed over to the alternate drug the second year, and received both drugs during the third year.5 No significant differences were reported in relapse rates during the first year between lithium (31%) and carbamazepine (37%), or in the percentage of patients who experienced a moderate or better response: 33% on lithium, 31% on carbamazepine, and 55% on the combination. On a variety of other measures, lithium was superior to carbamazepine. But patients with a history of rapid cycling responded significantly better to the combination (56%) than to lithium (28%) or carbamazepine (19%) alone.
As in the previous study, a higher proportion of patients receiving carbamazepine withdrew after experiencing side effects. Both studies found that while carbamazepine is efficacious, lithium is superior overall. But since neither study included a placebo group, carbamazepine’s efficacy in maintenance treatment cannot be determined.
Carbamazepine also was evaluated in three randomized, controlled trials in patients with bipolar depression.2 These small trials suggest that carbamazepine’s antidepressant activity may be less robust than its antimanic effects. Response rates (>50% improvement in depressive symptoms) ranged from 32% to 34%, although many patients who participated had treatment-resistant bipolar depression.
Comparing the known efficacy of antiepileptic agents in bipolar disorder
| Drug | Mania | Depression | Maintenance | Comments |
|---|---|---|---|---|
| Valproate | ◊◊◊◊ | ◊ | ◊◊◊ | New Depakote ER formulation |
| Carbamazepine | ◊◊◊ | ◊◊ | ◊◊◊ | 2 new maintenance studies v. lithium |
| Gabapentin | – | ◊ | ◊ | 2 negative placebo-controlled studies in mania |
| Lamotrigine | × | ◊◊◊ | ◊◊◊ | Antidepressant activity in several controlled trials |
| Topiramate | ◊ | ◊ | ◊ | Dose-related weight loss |
| Oxcarbazepine | ◊◊ | ◊ | ◊ | Improved tolerability & pharmacokinetics |
| Zonisamide | ◊ | ND | ND | May produce weight loss in some patients |
| Tiagabine | × | ND | ND | More data needed regarding tolerability and efficacy |
| Levetiracetam | ND | ND | ND | Data needed regarding efficacy and tolerability |
Key
◊◊◊◊ efficacy demonstrated in ≥2 placebo-controlled trials
◊◊◊ efficacy demonstrated in one placebo-controlled or two large, active comparator trials
◊◊ efficacy in two small or one large active comparator trial
◊ efficacy only in open trials and case series
× conflicting evidence of efficacy in available studies
– lack of efficacy demonstrated in randomized, controlled trials
ND no data presently available
Based on the studies reviewed above, carbamazepine is considered a second-line agent for bipolar mania and maintenance treatment with very limited data regarding its antidepressant effects.6
Valproate: For patients with mixed and mood episodes
The evidence seems to point to valproate as a suitable agent for patients with mixed and mood episodes.
Two earlier randomized, controlled studies7,8 showed that the divalproex sodium formulation of valproate was superior to a placebo, leading to the indication of divalproex for treatment of acute mania in patients with bipolar disorder. Additional analyses of data from the second controlled trial8 indicated that patients with prominent depressive symptoms during mania (mixed episodes) responded better to divalproex than lithium. Further, multiple prior mood episodes were associated with poor lithium response but not with divalproex response.
Two recent randomized, controlled trials compared the antimanic efficacy and tolerability of divalproex and olanzapine.9,10 The design of these two studies differed in two important ways: sample size and starting doses. This may explain the different results of the two trials.
In the first study, 248 patients received starting doses of either divalproex 750 mg/d with upward titration to therapeutic concentrations, or olanzapine 15 mg/d with titration if clinically indicated.9 Olanzapine was found to be superior in the mean reduction of manic symptoms and in the proportion of patients who either responded to treatment or were in remission.
In the second study, the number of patients (N=120) randomized was not sufficient to detect a statistically significant difference between treatment groups.10 Initial dosing consisted of rapid divalproex loading (20 mg/kg/d) versus olanzapine (10 mg/d) with upward titration as clinically indicated. This trial revealed no significant differences in efficacy on any outcome measure and the mean valproic acid plasma concentration was higher than in the first trial.
Differences in side effects between the two agents were similar in both studies. Olanzapine was associated with greater sedation, appetite stimulation, and weight gain, and divalproex with greater gastrointestinal symptoms. Taken together, these two studies indicate that olanzapine is at least as efficacious as divalproex in treating acute mania and that divalproex should be titrated to plasma concentrations well within the therapeutic range consistent with response and tolerability.
The efficacy of divalproex as a maintenance therapy for patients with bipolar disorder has been studied in four trials to date:
- A randomized, open comparison of lithium and divalproex found generally good efficacy for both drugs across 18 months.
- A second naturalistic, pharmacoeconomic, one-year open comparison also found both lithium and divalproex fairly equal in efficacy.
- A large, prospective, randomized one-year maintenance trial showed little difference in relapse rates among patients receiving divalproex (24%), lithium (31%), and a placebo (38%).11
- A recently completed one-year comparison of relapse rates between divalproex and olanzapine showed little difference between the two drugs.12
The overall results suggest that divalproex helps prevent mood episodes in patients with bipolar disorder, but the data are less substantial and conclusive than from placebo-controlled trials of lithium.
The antidepressant effects of divalproex in treating acute bipolar depression have not been studied in randomized controlled trials. Impressions from case reports and case series suggest that divalproex may exert some antidepressant activity, but that this action may be less robust than its antimanic effects.
Divalproex is now available in a once-daily extended release (ER) formulation. This appears to have improved tolerability, especially regarding gastrointestinal side effects. (Clinical experience suggests that the immediate release formulation of divalproex can also be given once daily.) The ER formulation is not bioequivalent to its immediate-release counterpart; it produces plasma concentrations of approximately 80% of those achieved with immediate release. Thus, switching a patient to the ER formulation might require a dose increase.
Lamotrigine for bipolar depression
Several recent randomized controlled trials indicate that lamotrigine has important thymoleptic properties.14-17
Three studies addressed the efficacy of lamotrigine in treating patients with acute bipolar mania. In two small trials, lamotrigine did not display superior efficacy over placebo in reducing manic symptoms.14 A third trial revealed differences between lithium and lamotrigine in reducing manic symptoms, but this study lacked sufficient power to detect potential differences in efficacy.
Two placebo-controlled maintenance studies of lamotrigine were recently reported.15,16 The first found no significant differences in relapse rates in patients with rapid cycling bipolar I and II disorders randomized to lamotrigine or placebo after initial stabilization on lamotrigine.15 However, in a post hoc analysis among bipolar II (but not bipolar I) patients, lamotrigine was significantly more efficacious than placebo in time-to-study dropout and considerably better (P=0.07) in time to need for additional medication.
In the second randomized, placebo-controlled trial, patients with bipolar I disorder who had recently experienced a manic episode were treated with lamotrigine 100-200 mg/d during an open-label phase (8-16 weeks) while other psychotropic agents were tapered and discontinued.16 Patients (N = 171) who remained stable were then randomized to lamotrigine 200-400 mg/d, lithium, or placebo for up to 18 months.
The lamotrigine-treated group showed significantly lower relapse rates than placebo-treated patients in time-to-study dropout, time to intervention for a mood episode, and time to intervention for depressive relapse. Differences between the lamotrigine and placebo groups in time to intervention for manic relapse were insignificant. Lithium was superior to a placebo in time to relapse for any mood episode and time to intervention for a manic episode. Lithium also outperformed lamotrigine in that manic symptoms did not worsen as quickly from baseline to endpoint.
The results here are consistent with those of the rapid cycling study: Lamotrigine helps prevent recurrence of depressive symptoms and episodes. Evidence of prophylaxis against manic recurrences was not compelling, however.
The findings of these two maintenance trials are consistent with the results of a placebo-controlled, randomized, 6-week acute treatment trial of lamotrigine (50 mg/d and 200 mg/d) in patients with bipolar depression.17 Seventeen lamotrigine-treated patients in both dosage groups saw more-significantly reduced depressive symptoms than did placebo-treated patients on the MADRS (but not the HAMD) total score and on the CGI. The 200 mg/d group tended to have greater improvement than the 50 mg/d group. There was little difference among the three treatment groups in the incidence of switching into hypomania or mania.
These studies indicate that lamotrigine has acute and prophylactic efficacy against bipolar depression. In contrast, evidence of the agent’s acute or prophylactic efficacy in mania is lacking.
Other new antiepileptics: More testing needed
Use of the six other newer antiepileptics in patients with bipolar disorder is still being explored. (See “Comparing the known efficacy of antiepileptic agents in bipolar disorder,”) Let’s look at what we know about these agents to this point.
Gabapentin A number of case reports and case series published in recent years suggest that gabapentin may have mood-stabilizing properties. In two randomized, controlled trials, however, gabapentin did not display significantly greater efficacy than a placebo in treating acute mania.13,14 Gabapentin has not been studied in controlled trials as a maintenance treatment or for bipolar depression.
In contrast to these negative studies, gabapentin was superior to placebo in studies of patients with panic disorder, social anxiety disorder, and neuropathic pain. Overall, these studies suggest that gabapentin is not a bona fide mood stabilizer for most patients.
Topiramate More than 10 case reports and case series suggest that topiramate may have mood-stabilizing properties. A number of open trials also have found significant dose-related weight loss in patients with weight gain associated with other psychotropic agents.18 These observations have sparked interest in topiramate’s potential role as an obesity treatment.
Only one randomized, controlled trial of topiramate for bipolar disorder has appeared to date.19 An interim analysis of a placebo-controlled, randomized trial of two doses of topiramate (approximately 250 mg/d and 500 mg/d) in 97 hospitalized patients with acute bipolar I mania revealed strong trends toward reduced manic symptoms for both topiramate groups over placebo. These differences were not significant by the time the study was concluded, however.
Lamotrigine is a novel drug that blocks voltage-sensitive sodium channels, thereby indirectly inhibiting the release of excitatory neurotransmitters, particularly glutamate and aspartate.
Gabapentin was developed to mimic the synaptic effects of gamma-aminobutyric acid (GABA); it does not appear to appreciably interact with GABA receptors, however, and its mechanism of action in epilepsy remains unknown. It has several attractive pharmacokinetic properties, including lack of protein binding, renal clearance rather than hepatic metabolism, and few known drug-drug interactions.
Topiramate is a sulfamate-substituted monosaccharide with a number of possible mechanisms of action, including blockade of voltage-gated sodium channels, antagonism of the kainate/AMPA glutamate receptor subtype, enhancement of GABA activity at the GABA A receptor via interaction with a nonbenzodiazepine receptor site, and carbonic anhydrase inhibition.
Oxcarbazepine is the 10-keto analogue of carbamazepine, a chemical difference that translates into a number of safety advantages over carbamazepine. Oxcarbazepine is converted to an active 10-hydroxy metabolite rather than to the 10,11-epoxide metabolite of carbamazepine. The 10,11-epoxide metabolite of carbamazepine is associated with neurological side effects. Oxcarbazepine is a weak inducer of the CYP450 system, appears to have fewer drug-drug interactions, and offers better overall tolerability.
Zonisamide, a sulfonamide derivative, blocks voltage-sensitive sodium channels and T-type calcium currents, modulates GABAergic and dopaminergic neurotransmission, and is a free-radical scavenger.
Tiagabine is a selective GABA reuptake inhibitor.
Levetiracetam is the S-enantiomer of the ethyl analogue of the nootropic agent piracetam. Its mechanism of action in treating epilepsy is unknown. It does not appear to interact significantly with voltage-sensitive sodium channels or T-type calcium channels, nor does it significantly alter levels of GABA, glutamate, or glutamine in the central nervous system.
When patients with mania associated with recent antidepressant use were excluded from post hocanalysis, topiramate’s superiority over placebo was re-established. These tantalizing results require further study. Similarly, studies of topiramate’s potential efficacy in acute bipolar depression and as a maintenance treatment are needed.
Oxcarbazepine Oxcarbazepine is a relative newcomer to the United States, but has been available abroad for some time.
While numerous studies have tested carbamazepine in treating various aspects of bipolar disorder, few controlled trials have tested oxcarbazepine for this use.20
Oxcarbazepine as a treatment for acute bipolar mania was comparable to haloperidol in two small randomized, controlled trials and to lithium in one small trial. None of these studies had adequate power to detect potential differences in efficacy. Similarly, two very small maintenance studies (total N=25) found no differences in efficacy between oxcarbazepine and lithium.20
Additionally, to our knowledge oxcarbazepine has not been formally tested as a treatment for acute bipolar depression. So while oxcarbazepine is an attractive alternative to carbamazepine for pharmacokinetic and pharmacodynamic reasons, data supporting oxcarbazepine’s efficacy in bipolar disorder are far less substantial.
Zonisamide The only report of zonisamide as a bipolar disorder treatment so far is a case series of 15 patients who received the drug adjunctively for manic symptoms. Of these patients, 80% showed at least moderate improvement and 33% were rated as markedly improved. These preliminary observations require further study. Like topiramate, zonisamide may also be associated with weight loss in some patients.
Tiagabine A few case reports and case series describe tiagabine’s effects in patients with bipolar disorder. Conflicting results have been reported to date and some reports of poor tolerability have emerged. Fundamental safety and efficacy data for this agent in bipolar disorder are needed.
Levetiracetam Studies of levetiracetam for treatment of bipolar disorder are just under way. The Stanley Foundation Bipolar Treatment Network, a program of the National Alliance for the Mentally Ill Research Institute, is investigating its potential thymoleptic properties.
Related resources
- Joffe RT, Calabrese JR. Anticonvulsants in Mood Disorders. New York: Marcel Dekker Inc., 1994.
- Modigh K, Robak OH, Vestergaard P. Anticonvulsants in Psychiatry. Bristol, Pa: Wrightson Biomedical Publishing, Ltd., 1994.
- Schatzberg AF, Nemeroff CB. Textbook of Psychopharmacology, 2 nd ed. Washington, DC: American Psychiatric Press, 1998.
- Nathan P, Gorman J. A Guide to Treatments that Work, 2 nd ed. New York: Oxford University Press, 2001.
- Janicak PG, Davis JM, Preskorn SH, Ayd FJ, Jr. Principles and Practice of Psychopharmacotherapy, 2 nd ed. Baltimore, MD: Williams & Wilkins, 1997.
Drug brand names
- Carbamazepine • Tegretol, Epitol, Atretol
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levetiracetam • Keppra
- Oxcarbazepine • Trileptal
- Tiagabine • Gabatril
- Topiramate • Topamax
- Valproate-divalproex sodium • Depakote, Depakote ER
- Zonisamide • Zonegran
Disclosure
Dr. Keck reports that he receives grant/research support from and serves as a consultant to Abbott Laboratories, AstraZeneca, Pfizer Inc., and Eli Lilly and Co. He also receives grant/research support from Merck and Co. and Otsuka America Pharmaceutical, and serves as a consultant to Bristol-Myers Squibb Co., GlaxoSmithKline, and Janssen Pharmaceutica.
Dr. McElroy reports that she receives grant/research support from and serves as a consultant to Abbott Laboratories, Elan Pharmaceuticals, Cephalon Inc. GlaxoSmithKline, and Eli Lilly and Co. She also receives grant/research support from Forest Pharmaceuticals and Solvay Pharmaceuticals, and serves as a consultant to Bristol-Myers Squibb Co., Ortho-McNeil Pharmaceutical, and Janssen Pharmaceutica.
1. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry. 1998;59(Suppl 6):74-81.
2. McElroy SL, Keck PE, Jr. Pharmacologic agents for the treatment of acute bipolar mania. Biol Psychiatry. 2000;48:539-557.
3. Post RM, Denicoff KD, Frye MA, Leverich GS. Re-evaluating carbamazepine prophylaxis in bipolar disorder. Br J Psychiatry. 1997;170:202-204.
4. Greil W, Ludwig-Mayerhofer W, Erazon-Scheichlin C, Schmidt S, Engel RR, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders–a randomized study. J Affect Disorders. 1997;43:151-161.
5. Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO, Leverich GS, Post RM. Comparative prophylactic efficacy of lithium, carbamazepine and the combination in bipolar disorder. J Clin Psychiatry. 1997;58:470-478.
6. Suppes T, Swann AC, Dennehy EB, Habermacher ED, Mason M, Crismon ML, Toprac MG, Rush AJ, Shon SP, Altshuler KZ. Texas Medication Algorithm Project: development and feasibility testing of a treatment algorithm for patients with bipolar disorder. J Clin Psychiatry. 2001;62:439-447.
7. Pope HG, Jr, McElroy SL, Keck PE, Jr, Hudson JI. Valproate in the treatment of acute mania: a placebo-controlled study. Arch Gen Psychiatry. 1991;48:62-68.
8. Bowden CL, Brugger AM, Swann AC, Calabrese JR, Janicak PG, Petty F, et al. Efficacy of divalproex sodium vs. lithium and placebo in the treatment of mania. JAMA. 1994;271:915-924.
9. Tohen M, Baker RW, Milton DR, Risser RC, Gilmore JA, Davis AR, et al. Olanzapine versus divalproex sodium for the treatment of acute mania. Bipolar Disorders. 2001;3(Suppl 1):60-61.
10. Zajecka J. Divalproex versus olanzapine in the treatment of acute mania. Presented at the 39 th Annual Meeting of the American College of Neuropsychopharmacology. San Juan, Puerto Rico, Dec. 10-14, 2000.
11. Bowden CL, Calabrese JR, McElroy SL, Hirschfeld RMA, Petty F, Gyulai LL, Pope HG, Jr, et al. Efficacy of divalproex versus lithium and placebo in maintenance treatment of bipolar disorder. Arch Gen Psychiatry. 2000;57:481-489.
12. Tohen M, Baker RW, Altshuler LL, Zarate CA, Suppes T, Ketter T, et al. Olanzapine versus divalproex for bipolar mania: a 47-week study. Presented at the European College of Neuropsychopharmacology Meeting, Istanbul, Turkey, Oct. 15, 2001.
13. Pande AD, Crockatt JG, Janney CA, Werth JL, Tsaaroucha G. and the Gabapentin Bipolar Disorder Study Group. Bipolar Disorders. 2000;2:249-255.
14. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol. 2000;24:205-212.
15. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in rapid-cycling bipolar disorder. J Clin Psychiatry. 2000;61:841-850.
16. Bowden CL, Calabrese JR, Akthar S, Olajossy M, Montgomery S, Ascher J, et al. Lamotrigine demonstrates long-term mood stabilization in manic patients. Bipolar Disorders. 2001;3(Suppl 1):27-28.
17. Calabrese JR, Bowden CL, Sachs GS, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. J Clin Psychiatry. 1999;60:79-88.
18. McElroy SL, Suppes T, Keck PE, Jr, Frye MA, Denicoff KD, Altshuler LL, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry. 2000;47:1025-1033.
19. Calabrese JR. A double-blind, placebo-controlled trial of topiramate monotherapy in the treatment of acute mania. Presented at the Annual Meeting of the European College of Neuropsychopharmacology. Munich, Germany, Sept. 9-13, 2000.
20. Emrich H, Schiwy W, Silverstone T. eds. Carbamazepine and Oxcarbazepine in Psychiatry. London: CNS Publishers, 1990.
The newer antiepileptic drugs pose a sometimes bewildering range of options for bipolar disorder treatment. Which work best for acute bipolar I mania? Which are best suited for maintenance in patients with mixed episodes, or for those with a history of rapid cycling? What about prevention of depressive episodes? And how do the antiepileptics compare with lithium?
For many patients with bipolar disorder, lithium is still the drug of choice. For others, however, an increasing body of evidence supports the efficacy of some antiepileptics and atypical antipsychotics.
The mood-stabilizing properties of two antiepileptic agents, carbamazepine and valproate, were demonstrated some years ago in randomized controlled trials in patients with bipolar disorder. Since then, there has been considerable interest in the potential thymoleptic properties of the new antiepileptic drugs.1 In recent years gabapentin, lamotrigine, topiramate, oxcarbazepine, zonisamide, tiagabine, and levetiracetam have been approved in the United States for the treatment of various types of epilepsy. These medications have diverse pharmacological properties that distinguish them from earlier agents and from one another.
Do these new agents have anything to offer patients? For the most part, the evidence is not yet in hand, but we will examine what’s available, starting with the most recent trial data regarding the efficacy of valproate and carbamazepine.
Carbamazepine for bipolar mania
Five randomized, controlled trials2 have shown the efficacy of carbamazepine in patients with acute bipolar I mania. Carbamazepine was superior to placebo and comparable to chlorpromazine and lithium. Pooled data reveal an overall response rate (defined as the proportion of patients experiencing > 50% reduction in manic symptoms) of 50% for carbamazepine, 56% for lithium, and 61% for chlorpromazine (differences in overall response rates are not significant).
Until recently, the efficacy of carbamazepine as a maintenance therapy for bipolar disorder was controversial.3 However, two recent large randomized, controlled maintenance studies that compared carbamazepine with lithium validated use of the agent for that purpose.4,5
In the first study, 144 patients received either drug and were followed for up to 2 1/2 years.4 The study showed no significant differences between the two groups in time-to-mood episode recurrence or hospitalization. However, significantly more patients receiving carbamazepine required treatment discontinuation for side effects and additional medications for breakthrough symptoms than did the patients receiving lithium.
Patients without both comorbid disorders and mood-incongruent delusions responded better to lithium, whereas those with mixed episodes and bipolar II disorder or NOS appeared to respond better to carbamazepine.
In the second trial, 52 patients with bipolar I or II disorders received either lithium or carbamazepine for one year, crossed over to the alternate drug the second year, and received both drugs during the third year.5 No significant differences were reported in relapse rates during the first year between lithium (31%) and carbamazepine (37%), or in the percentage of patients who experienced a moderate or better response: 33% on lithium, 31% on carbamazepine, and 55% on the combination. On a variety of other measures, lithium was superior to carbamazepine. But patients with a history of rapid cycling responded significantly better to the combination (56%) than to lithium (28%) or carbamazepine (19%) alone.
As in the previous study, a higher proportion of patients receiving carbamazepine withdrew after experiencing side effects. Both studies found that while carbamazepine is efficacious, lithium is superior overall. But since neither study included a placebo group, carbamazepine’s efficacy in maintenance treatment cannot be determined.
Carbamazepine also was evaluated in three randomized, controlled trials in patients with bipolar depression.2 These small trials suggest that carbamazepine’s antidepressant activity may be less robust than its antimanic effects. Response rates (>50% improvement in depressive symptoms) ranged from 32% to 34%, although many patients who participated had treatment-resistant bipolar depression.
Comparing the known efficacy of antiepileptic agents in bipolar disorder
| Drug | Mania | Depression | Maintenance | Comments |
|---|---|---|---|---|
| Valproate | ◊◊◊◊ | ◊ | ◊◊◊ | New Depakote ER formulation |
| Carbamazepine | ◊◊◊ | ◊◊ | ◊◊◊ | 2 new maintenance studies v. lithium |
| Gabapentin | – | ◊ | ◊ | 2 negative placebo-controlled studies in mania |
| Lamotrigine | × | ◊◊◊ | ◊◊◊ | Antidepressant activity in several controlled trials |
| Topiramate | ◊ | ◊ | ◊ | Dose-related weight loss |
| Oxcarbazepine | ◊◊ | ◊ | ◊ | Improved tolerability & pharmacokinetics |
| Zonisamide | ◊ | ND | ND | May produce weight loss in some patients |
| Tiagabine | × | ND | ND | More data needed regarding tolerability and efficacy |
| Levetiracetam | ND | ND | ND | Data needed regarding efficacy and tolerability |
Key
◊◊◊◊ efficacy demonstrated in ≥2 placebo-controlled trials
◊◊◊ efficacy demonstrated in one placebo-controlled or two large, active comparator trials
◊◊ efficacy in two small or one large active comparator trial
◊ efficacy only in open trials and case series
× conflicting evidence of efficacy in available studies
– lack of efficacy demonstrated in randomized, controlled trials
ND no data presently available
Based on the studies reviewed above, carbamazepine is considered a second-line agent for bipolar mania and maintenance treatment with very limited data regarding its antidepressant effects.6
Valproate: For patients with mixed and mood episodes
The evidence seems to point to valproate as a suitable agent for patients with mixed and mood episodes.
Two earlier randomized, controlled studies7,8 showed that the divalproex sodium formulation of valproate was superior to a placebo, leading to the indication of divalproex for treatment of acute mania in patients with bipolar disorder. Additional analyses of data from the second controlled trial8 indicated that patients with prominent depressive symptoms during mania (mixed episodes) responded better to divalproex than lithium. Further, multiple prior mood episodes were associated with poor lithium response but not with divalproex response.
Two recent randomized, controlled trials compared the antimanic efficacy and tolerability of divalproex and olanzapine.9,10 The design of these two studies differed in two important ways: sample size and starting doses. This may explain the different results of the two trials.
In the first study, 248 patients received starting doses of either divalproex 750 mg/d with upward titration to therapeutic concentrations, or olanzapine 15 mg/d with titration if clinically indicated.9 Olanzapine was found to be superior in the mean reduction of manic symptoms and in the proportion of patients who either responded to treatment or were in remission.
In the second study, the number of patients (N=120) randomized was not sufficient to detect a statistically significant difference between treatment groups.10 Initial dosing consisted of rapid divalproex loading (20 mg/kg/d) versus olanzapine (10 mg/d) with upward titration as clinically indicated. This trial revealed no significant differences in efficacy on any outcome measure and the mean valproic acid plasma concentration was higher than in the first trial.
Differences in side effects between the two agents were similar in both studies. Olanzapine was associated with greater sedation, appetite stimulation, and weight gain, and divalproex with greater gastrointestinal symptoms. Taken together, these two studies indicate that olanzapine is at least as efficacious as divalproex in treating acute mania and that divalproex should be titrated to plasma concentrations well within the therapeutic range consistent with response and tolerability.
The efficacy of divalproex as a maintenance therapy for patients with bipolar disorder has been studied in four trials to date:
- A randomized, open comparison of lithium and divalproex found generally good efficacy for both drugs across 18 months.
- A second naturalistic, pharmacoeconomic, one-year open comparison also found both lithium and divalproex fairly equal in efficacy.
- A large, prospective, randomized one-year maintenance trial showed little difference in relapse rates among patients receiving divalproex (24%), lithium (31%), and a placebo (38%).11
- A recently completed one-year comparison of relapse rates between divalproex and olanzapine showed little difference between the two drugs.12
The overall results suggest that divalproex helps prevent mood episodes in patients with bipolar disorder, but the data are less substantial and conclusive than from placebo-controlled trials of lithium.
The antidepressant effects of divalproex in treating acute bipolar depression have not been studied in randomized controlled trials. Impressions from case reports and case series suggest that divalproex may exert some antidepressant activity, but that this action may be less robust than its antimanic effects.
Divalproex is now available in a once-daily extended release (ER) formulation. This appears to have improved tolerability, especially regarding gastrointestinal side effects. (Clinical experience suggests that the immediate release formulation of divalproex can also be given once daily.) The ER formulation is not bioequivalent to its immediate-release counterpart; it produces plasma concentrations of approximately 80% of those achieved with immediate release. Thus, switching a patient to the ER formulation might require a dose increase.
Lamotrigine for bipolar depression
Several recent randomized controlled trials indicate that lamotrigine has important thymoleptic properties.14-17
Three studies addressed the efficacy of lamotrigine in treating patients with acute bipolar mania. In two small trials, lamotrigine did not display superior efficacy over placebo in reducing manic symptoms.14 A third trial revealed differences between lithium and lamotrigine in reducing manic symptoms, but this study lacked sufficient power to detect potential differences in efficacy.
Two placebo-controlled maintenance studies of lamotrigine were recently reported.15,16 The first found no significant differences in relapse rates in patients with rapid cycling bipolar I and II disorders randomized to lamotrigine or placebo after initial stabilization on lamotrigine.15 However, in a post hoc analysis among bipolar II (but not bipolar I) patients, lamotrigine was significantly more efficacious than placebo in time-to-study dropout and considerably better (P=0.07) in time to need for additional medication.
In the second randomized, placebo-controlled trial, patients with bipolar I disorder who had recently experienced a manic episode were treated with lamotrigine 100-200 mg/d during an open-label phase (8-16 weeks) while other psychotropic agents were tapered and discontinued.16 Patients (N = 171) who remained stable were then randomized to lamotrigine 200-400 mg/d, lithium, or placebo for up to 18 months.
The lamotrigine-treated group showed significantly lower relapse rates than placebo-treated patients in time-to-study dropout, time to intervention for a mood episode, and time to intervention for depressive relapse. Differences between the lamotrigine and placebo groups in time to intervention for manic relapse were insignificant. Lithium was superior to a placebo in time to relapse for any mood episode and time to intervention for a manic episode. Lithium also outperformed lamotrigine in that manic symptoms did not worsen as quickly from baseline to endpoint.
The results here are consistent with those of the rapid cycling study: Lamotrigine helps prevent recurrence of depressive symptoms and episodes. Evidence of prophylaxis against manic recurrences was not compelling, however.
The findings of these two maintenance trials are consistent with the results of a placebo-controlled, randomized, 6-week acute treatment trial of lamotrigine (50 mg/d and 200 mg/d) in patients with bipolar depression.17 Seventeen lamotrigine-treated patients in both dosage groups saw more-significantly reduced depressive symptoms than did placebo-treated patients on the MADRS (but not the HAMD) total score and on the CGI. The 200 mg/d group tended to have greater improvement than the 50 mg/d group. There was little difference among the three treatment groups in the incidence of switching into hypomania or mania.
These studies indicate that lamotrigine has acute and prophylactic efficacy against bipolar depression. In contrast, evidence of the agent’s acute or prophylactic efficacy in mania is lacking.
Other new antiepileptics: More testing needed
Use of the six other newer antiepileptics in patients with bipolar disorder is still being explored. (See “Comparing the known efficacy of antiepileptic agents in bipolar disorder,”) Let’s look at what we know about these agents to this point.
Gabapentin A number of case reports and case series published in recent years suggest that gabapentin may have mood-stabilizing properties. In two randomized, controlled trials, however, gabapentin did not display significantly greater efficacy than a placebo in treating acute mania.13,14 Gabapentin has not been studied in controlled trials as a maintenance treatment or for bipolar depression.
In contrast to these negative studies, gabapentin was superior to placebo in studies of patients with panic disorder, social anxiety disorder, and neuropathic pain. Overall, these studies suggest that gabapentin is not a bona fide mood stabilizer for most patients.
Topiramate More than 10 case reports and case series suggest that topiramate may have mood-stabilizing properties. A number of open trials also have found significant dose-related weight loss in patients with weight gain associated with other psychotropic agents.18 These observations have sparked interest in topiramate’s potential role as an obesity treatment.
Only one randomized, controlled trial of topiramate for bipolar disorder has appeared to date.19 An interim analysis of a placebo-controlled, randomized trial of two doses of topiramate (approximately 250 mg/d and 500 mg/d) in 97 hospitalized patients with acute bipolar I mania revealed strong trends toward reduced manic symptoms for both topiramate groups over placebo. These differences were not significant by the time the study was concluded, however.
Lamotrigine is a novel drug that blocks voltage-sensitive sodium channels, thereby indirectly inhibiting the release of excitatory neurotransmitters, particularly glutamate and aspartate.
Gabapentin was developed to mimic the synaptic effects of gamma-aminobutyric acid (GABA); it does not appear to appreciably interact with GABA receptors, however, and its mechanism of action in epilepsy remains unknown. It has several attractive pharmacokinetic properties, including lack of protein binding, renal clearance rather than hepatic metabolism, and few known drug-drug interactions.
Topiramate is a sulfamate-substituted monosaccharide with a number of possible mechanisms of action, including blockade of voltage-gated sodium channels, antagonism of the kainate/AMPA glutamate receptor subtype, enhancement of GABA activity at the GABA A receptor via interaction with a nonbenzodiazepine receptor site, and carbonic anhydrase inhibition.
Oxcarbazepine is the 10-keto analogue of carbamazepine, a chemical difference that translates into a number of safety advantages over carbamazepine. Oxcarbazepine is converted to an active 10-hydroxy metabolite rather than to the 10,11-epoxide metabolite of carbamazepine. The 10,11-epoxide metabolite of carbamazepine is associated with neurological side effects. Oxcarbazepine is a weak inducer of the CYP450 system, appears to have fewer drug-drug interactions, and offers better overall tolerability.
Zonisamide, a sulfonamide derivative, blocks voltage-sensitive sodium channels and T-type calcium currents, modulates GABAergic and dopaminergic neurotransmission, and is a free-radical scavenger.
Tiagabine is a selective GABA reuptake inhibitor.
Levetiracetam is the S-enantiomer of the ethyl analogue of the nootropic agent piracetam. Its mechanism of action in treating epilepsy is unknown. It does not appear to interact significantly with voltage-sensitive sodium channels or T-type calcium channels, nor does it significantly alter levels of GABA, glutamate, or glutamine in the central nervous system.
When patients with mania associated with recent antidepressant use were excluded from post hocanalysis, topiramate’s superiority over placebo was re-established. These tantalizing results require further study. Similarly, studies of topiramate’s potential efficacy in acute bipolar depression and as a maintenance treatment are needed.
Oxcarbazepine Oxcarbazepine is a relative newcomer to the United States, but has been available abroad for some time.
While numerous studies have tested carbamazepine in treating various aspects of bipolar disorder, few controlled trials have tested oxcarbazepine for this use.20
Oxcarbazepine as a treatment for acute bipolar mania was comparable to haloperidol in two small randomized, controlled trials and to lithium in one small trial. None of these studies had adequate power to detect potential differences in efficacy. Similarly, two very small maintenance studies (total N=25) found no differences in efficacy between oxcarbazepine and lithium.20
Additionally, to our knowledge oxcarbazepine has not been formally tested as a treatment for acute bipolar depression. So while oxcarbazepine is an attractive alternative to carbamazepine for pharmacokinetic and pharmacodynamic reasons, data supporting oxcarbazepine’s efficacy in bipolar disorder are far less substantial.
Zonisamide The only report of zonisamide as a bipolar disorder treatment so far is a case series of 15 patients who received the drug adjunctively for manic symptoms. Of these patients, 80% showed at least moderate improvement and 33% were rated as markedly improved. These preliminary observations require further study. Like topiramate, zonisamide may also be associated with weight loss in some patients.
Tiagabine A few case reports and case series describe tiagabine’s effects in patients with bipolar disorder. Conflicting results have been reported to date and some reports of poor tolerability have emerged. Fundamental safety and efficacy data for this agent in bipolar disorder are needed.
Levetiracetam Studies of levetiracetam for treatment of bipolar disorder are just under way. The Stanley Foundation Bipolar Treatment Network, a program of the National Alliance for the Mentally Ill Research Institute, is investigating its potential thymoleptic properties.
Related resources
- Joffe RT, Calabrese JR. Anticonvulsants in Mood Disorders. New York: Marcel Dekker Inc., 1994.
- Modigh K, Robak OH, Vestergaard P. Anticonvulsants in Psychiatry. Bristol, Pa: Wrightson Biomedical Publishing, Ltd., 1994.
- Schatzberg AF, Nemeroff CB. Textbook of Psychopharmacology, 2 nd ed. Washington, DC: American Psychiatric Press, 1998.
- Nathan P, Gorman J. A Guide to Treatments that Work, 2 nd ed. New York: Oxford University Press, 2001.
- Janicak PG, Davis JM, Preskorn SH, Ayd FJ, Jr. Principles and Practice of Psychopharmacotherapy, 2 nd ed. Baltimore, MD: Williams & Wilkins, 1997.
Drug brand names
- Carbamazepine • Tegretol, Epitol, Atretol
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levetiracetam • Keppra
- Oxcarbazepine • Trileptal
- Tiagabine • Gabatril
- Topiramate • Topamax
- Valproate-divalproex sodium • Depakote, Depakote ER
- Zonisamide • Zonegran
Disclosure
Dr. Keck reports that he receives grant/research support from and serves as a consultant to Abbott Laboratories, AstraZeneca, Pfizer Inc., and Eli Lilly and Co. He also receives grant/research support from Merck and Co. and Otsuka America Pharmaceutical, and serves as a consultant to Bristol-Myers Squibb Co., GlaxoSmithKline, and Janssen Pharmaceutica.
Dr. McElroy reports that she receives grant/research support from and serves as a consultant to Abbott Laboratories, Elan Pharmaceuticals, Cephalon Inc. GlaxoSmithKline, and Eli Lilly and Co. She also receives grant/research support from Forest Pharmaceuticals and Solvay Pharmaceuticals, and serves as a consultant to Bristol-Myers Squibb Co., Ortho-McNeil Pharmaceutical, and Janssen Pharmaceutica.
The newer antiepileptic drugs pose a sometimes bewildering range of options for bipolar disorder treatment. Which work best for acute bipolar I mania? Which are best suited for maintenance in patients with mixed episodes, or for those with a history of rapid cycling? What about prevention of depressive episodes? And how do the antiepileptics compare with lithium?
For many patients with bipolar disorder, lithium is still the drug of choice. For others, however, an increasing body of evidence supports the efficacy of some antiepileptics and atypical antipsychotics.
The mood-stabilizing properties of two antiepileptic agents, carbamazepine and valproate, were demonstrated some years ago in randomized controlled trials in patients with bipolar disorder. Since then, there has been considerable interest in the potential thymoleptic properties of the new antiepileptic drugs.1 In recent years gabapentin, lamotrigine, topiramate, oxcarbazepine, zonisamide, tiagabine, and levetiracetam have been approved in the United States for the treatment of various types of epilepsy. These medications have diverse pharmacological properties that distinguish them from earlier agents and from one another.
Do these new agents have anything to offer patients? For the most part, the evidence is not yet in hand, but we will examine what’s available, starting with the most recent trial data regarding the efficacy of valproate and carbamazepine.
Carbamazepine for bipolar mania
Five randomized, controlled trials2 have shown the efficacy of carbamazepine in patients with acute bipolar I mania. Carbamazepine was superior to placebo and comparable to chlorpromazine and lithium. Pooled data reveal an overall response rate (defined as the proportion of patients experiencing > 50% reduction in manic symptoms) of 50% for carbamazepine, 56% for lithium, and 61% for chlorpromazine (differences in overall response rates are not significant).
Until recently, the efficacy of carbamazepine as a maintenance therapy for bipolar disorder was controversial.3 However, two recent large randomized, controlled maintenance studies that compared carbamazepine with lithium validated use of the agent for that purpose.4,5
In the first study, 144 patients received either drug and were followed for up to 2 1/2 years.4 The study showed no significant differences between the two groups in time-to-mood episode recurrence or hospitalization. However, significantly more patients receiving carbamazepine required treatment discontinuation for side effects and additional medications for breakthrough symptoms than did the patients receiving lithium.
Patients without both comorbid disorders and mood-incongruent delusions responded better to lithium, whereas those with mixed episodes and bipolar II disorder or NOS appeared to respond better to carbamazepine.
In the second trial, 52 patients with bipolar I or II disorders received either lithium or carbamazepine for one year, crossed over to the alternate drug the second year, and received both drugs during the third year.5 No significant differences were reported in relapse rates during the first year between lithium (31%) and carbamazepine (37%), or in the percentage of patients who experienced a moderate or better response: 33% on lithium, 31% on carbamazepine, and 55% on the combination. On a variety of other measures, lithium was superior to carbamazepine. But patients with a history of rapid cycling responded significantly better to the combination (56%) than to lithium (28%) or carbamazepine (19%) alone.
As in the previous study, a higher proportion of patients receiving carbamazepine withdrew after experiencing side effects. Both studies found that while carbamazepine is efficacious, lithium is superior overall. But since neither study included a placebo group, carbamazepine’s efficacy in maintenance treatment cannot be determined.
Carbamazepine also was evaluated in three randomized, controlled trials in patients with bipolar depression.2 These small trials suggest that carbamazepine’s antidepressant activity may be less robust than its antimanic effects. Response rates (>50% improvement in depressive symptoms) ranged from 32% to 34%, although many patients who participated had treatment-resistant bipolar depression.
Comparing the known efficacy of antiepileptic agents in bipolar disorder
| Drug | Mania | Depression | Maintenance | Comments |
|---|---|---|---|---|
| Valproate | ◊◊◊◊ | ◊ | ◊◊◊ | New Depakote ER formulation |
| Carbamazepine | ◊◊◊ | ◊◊ | ◊◊◊ | 2 new maintenance studies v. lithium |
| Gabapentin | – | ◊ | ◊ | 2 negative placebo-controlled studies in mania |
| Lamotrigine | × | ◊◊◊ | ◊◊◊ | Antidepressant activity in several controlled trials |
| Topiramate | ◊ | ◊ | ◊ | Dose-related weight loss |
| Oxcarbazepine | ◊◊ | ◊ | ◊ | Improved tolerability & pharmacokinetics |
| Zonisamide | ◊ | ND | ND | May produce weight loss in some patients |
| Tiagabine | × | ND | ND | More data needed regarding tolerability and efficacy |
| Levetiracetam | ND | ND | ND | Data needed regarding efficacy and tolerability |
Key
◊◊◊◊ efficacy demonstrated in ≥2 placebo-controlled trials
◊◊◊ efficacy demonstrated in one placebo-controlled or two large, active comparator trials
◊◊ efficacy in two small or one large active comparator trial
◊ efficacy only in open trials and case series
× conflicting evidence of efficacy in available studies
– lack of efficacy demonstrated in randomized, controlled trials
ND no data presently available
Based on the studies reviewed above, carbamazepine is considered a second-line agent for bipolar mania and maintenance treatment with very limited data regarding its antidepressant effects.6
Valproate: For patients with mixed and mood episodes
The evidence seems to point to valproate as a suitable agent for patients with mixed and mood episodes.
Two earlier randomized, controlled studies7,8 showed that the divalproex sodium formulation of valproate was superior to a placebo, leading to the indication of divalproex for treatment of acute mania in patients with bipolar disorder. Additional analyses of data from the second controlled trial8 indicated that patients with prominent depressive symptoms during mania (mixed episodes) responded better to divalproex than lithium. Further, multiple prior mood episodes were associated with poor lithium response but not with divalproex response.
Two recent randomized, controlled trials compared the antimanic efficacy and tolerability of divalproex and olanzapine.9,10 The design of these two studies differed in two important ways: sample size and starting doses. This may explain the different results of the two trials.
In the first study, 248 patients received starting doses of either divalproex 750 mg/d with upward titration to therapeutic concentrations, or olanzapine 15 mg/d with titration if clinically indicated.9 Olanzapine was found to be superior in the mean reduction of manic symptoms and in the proportion of patients who either responded to treatment or were in remission.
In the second study, the number of patients (N=120) randomized was not sufficient to detect a statistically significant difference between treatment groups.10 Initial dosing consisted of rapid divalproex loading (20 mg/kg/d) versus olanzapine (10 mg/d) with upward titration as clinically indicated. This trial revealed no significant differences in efficacy on any outcome measure and the mean valproic acid plasma concentration was higher than in the first trial.
Differences in side effects between the two agents were similar in both studies. Olanzapine was associated with greater sedation, appetite stimulation, and weight gain, and divalproex with greater gastrointestinal symptoms. Taken together, these two studies indicate that olanzapine is at least as efficacious as divalproex in treating acute mania and that divalproex should be titrated to plasma concentrations well within the therapeutic range consistent with response and tolerability.
The efficacy of divalproex as a maintenance therapy for patients with bipolar disorder has been studied in four trials to date:
- A randomized, open comparison of lithium and divalproex found generally good efficacy for both drugs across 18 months.
- A second naturalistic, pharmacoeconomic, one-year open comparison also found both lithium and divalproex fairly equal in efficacy.
- A large, prospective, randomized one-year maintenance trial showed little difference in relapse rates among patients receiving divalproex (24%), lithium (31%), and a placebo (38%).11
- A recently completed one-year comparison of relapse rates between divalproex and olanzapine showed little difference between the two drugs.12
The overall results suggest that divalproex helps prevent mood episodes in patients with bipolar disorder, but the data are less substantial and conclusive than from placebo-controlled trials of lithium.
The antidepressant effects of divalproex in treating acute bipolar depression have not been studied in randomized controlled trials. Impressions from case reports and case series suggest that divalproex may exert some antidepressant activity, but that this action may be less robust than its antimanic effects.
Divalproex is now available in a once-daily extended release (ER) formulation. This appears to have improved tolerability, especially regarding gastrointestinal side effects. (Clinical experience suggests that the immediate release formulation of divalproex can also be given once daily.) The ER formulation is not bioequivalent to its immediate-release counterpart; it produces plasma concentrations of approximately 80% of those achieved with immediate release. Thus, switching a patient to the ER formulation might require a dose increase.
Lamotrigine for bipolar depression
Several recent randomized controlled trials indicate that lamotrigine has important thymoleptic properties.14-17
Three studies addressed the efficacy of lamotrigine in treating patients with acute bipolar mania. In two small trials, lamotrigine did not display superior efficacy over placebo in reducing manic symptoms.14 A third trial revealed differences between lithium and lamotrigine in reducing manic symptoms, but this study lacked sufficient power to detect potential differences in efficacy.
Two placebo-controlled maintenance studies of lamotrigine were recently reported.15,16 The first found no significant differences in relapse rates in patients with rapid cycling bipolar I and II disorders randomized to lamotrigine or placebo after initial stabilization on lamotrigine.15 However, in a post hoc analysis among bipolar II (but not bipolar I) patients, lamotrigine was significantly more efficacious than placebo in time-to-study dropout and considerably better (P=0.07) in time to need for additional medication.
In the second randomized, placebo-controlled trial, patients with bipolar I disorder who had recently experienced a manic episode were treated with lamotrigine 100-200 mg/d during an open-label phase (8-16 weeks) while other psychotropic agents were tapered and discontinued.16 Patients (N = 171) who remained stable were then randomized to lamotrigine 200-400 mg/d, lithium, or placebo for up to 18 months.
The lamotrigine-treated group showed significantly lower relapse rates than placebo-treated patients in time-to-study dropout, time to intervention for a mood episode, and time to intervention for depressive relapse. Differences between the lamotrigine and placebo groups in time to intervention for manic relapse were insignificant. Lithium was superior to a placebo in time to relapse for any mood episode and time to intervention for a manic episode. Lithium also outperformed lamotrigine in that manic symptoms did not worsen as quickly from baseline to endpoint.
The results here are consistent with those of the rapid cycling study: Lamotrigine helps prevent recurrence of depressive symptoms and episodes. Evidence of prophylaxis against manic recurrences was not compelling, however.
The findings of these two maintenance trials are consistent with the results of a placebo-controlled, randomized, 6-week acute treatment trial of lamotrigine (50 mg/d and 200 mg/d) in patients with bipolar depression.17 Seventeen lamotrigine-treated patients in both dosage groups saw more-significantly reduced depressive symptoms than did placebo-treated patients on the MADRS (but not the HAMD) total score and on the CGI. The 200 mg/d group tended to have greater improvement than the 50 mg/d group. There was little difference among the three treatment groups in the incidence of switching into hypomania or mania.
These studies indicate that lamotrigine has acute and prophylactic efficacy against bipolar depression. In contrast, evidence of the agent’s acute or prophylactic efficacy in mania is lacking.
Other new antiepileptics: More testing needed
Use of the six other newer antiepileptics in patients with bipolar disorder is still being explored. (See “Comparing the known efficacy of antiepileptic agents in bipolar disorder,”) Let’s look at what we know about these agents to this point.
Gabapentin A number of case reports and case series published in recent years suggest that gabapentin may have mood-stabilizing properties. In two randomized, controlled trials, however, gabapentin did not display significantly greater efficacy than a placebo in treating acute mania.13,14 Gabapentin has not been studied in controlled trials as a maintenance treatment or for bipolar depression.
In contrast to these negative studies, gabapentin was superior to placebo in studies of patients with panic disorder, social anxiety disorder, and neuropathic pain. Overall, these studies suggest that gabapentin is not a bona fide mood stabilizer for most patients.
Topiramate More than 10 case reports and case series suggest that topiramate may have mood-stabilizing properties. A number of open trials also have found significant dose-related weight loss in patients with weight gain associated with other psychotropic agents.18 These observations have sparked interest in topiramate’s potential role as an obesity treatment.
Only one randomized, controlled trial of topiramate for bipolar disorder has appeared to date.19 An interim analysis of a placebo-controlled, randomized trial of two doses of topiramate (approximately 250 mg/d and 500 mg/d) in 97 hospitalized patients with acute bipolar I mania revealed strong trends toward reduced manic symptoms for both topiramate groups over placebo. These differences were not significant by the time the study was concluded, however.
Lamotrigine is a novel drug that blocks voltage-sensitive sodium channels, thereby indirectly inhibiting the release of excitatory neurotransmitters, particularly glutamate and aspartate.
Gabapentin was developed to mimic the synaptic effects of gamma-aminobutyric acid (GABA); it does not appear to appreciably interact with GABA receptors, however, and its mechanism of action in epilepsy remains unknown. It has several attractive pharmacokinetic properties, including lack of protein binding, renal clearance rather than hepatic metabolism, and few known drug-drug interactions.
Topiramate is a sulfamate-substituted monosaccharide with a number of possible mechanisms of action, including blockade of voltage-gated sodium channels, antagonism of the kainate/AMPA glutamate receptor subtype, enhancement of GABA activity at the GABA A receptor via interaction with a nonbenzodiazepine receptor site, and carbonic anhydrase inhibition.
Oxcarbazepine is the 10-keto analogue of carbamazepine, a chemical difference that translates into a number of safety advantages over carbamazepine. Oxcarbazepine is converted to an active 10-hydroxy metabolite rather than to the 10,11-epoxide metabolite of carbamazepine. The 10,11-epoxide metabolite of carbamazepine is associated with neurological side effects. Oxcarbazepine is a weak inducer of the CYP450 system, appears to have fewer drug-drug interactions, and offers better overall tolerability.
Zonisamide, a sulfonamide derivative, blocks voltage-sensitive sodium channels and T-type calcium currents, modulates GABAergic and dopaminergic neurotransmission, and is a free-radical scavenger.
Tiagabine is a selective GABA reuptake inhibitor.
Levetiracetam is the S-enantiomer of the ethyl analogue of the nootropic agent piracetam. Its mechanism of action in treating epilepsy is unknown. It does not appear to interact significantly with voltage-sensitive sodium channels or T-type calcium channels, nor does it significantly alter levels of GABA, glutamate, or glutamine in the central nervous system.
When patients with mania associated with recent antidepressant use were excluded from post hocanalysis, topiramate’s superiority over placebo was re-established. These tantalizing results require further study. Similarly, studies of topiramate’s potential efficacy in acute bipolar depression and as a maintenance treatment are needed.
Oxcarbazepine Oxcarbazepine is a relative newcomer to the United States, but has been available abroad for some time.
While numerous studies have tested carbamazepine in treating various aspects of bipolar disorder, few controlled trials have tested oxcarbazepine for this use.20
Oxcarbazepine as a treatment for acute bipolar mania was comparable to haloperidol in two small randomized, controlled trials and to lithium in one small trial. None of these studies had adequate power to detect potential differences in efficacy. Similarly, two very small maintenance studies (total N=25) found no differences in efficacy between oxcarbazepine and lithium.20
Additionally, to our knowledge oxcarbazepine has not been formally tested as a treatment for acute bipolar depression. So while oxcarbazepine is an attractive alternative to carbamazepine for pharmacokinetic and pharmacodynamic reasons, data supporting oxcarbazepine’s efficacy in bipolar disorder are far less substantial.
Zonisamide The only report of zonisamide as a bipolar disorder treatment so far is a case series of 15 patients who received the drug adjunctively for manic symptoms. Of these patients, 80% showed at least moderate improvement and 33% were rated as markedly improved. These preliminary observations require further study. Like topiramate, zonisamide may also be associated with weight loss in some patients.
Tiagabine A few case reports and case series describe tiagabine’s effects in patients with bipolar disorder. Conflicting results have been reported to date and some reports of poor tolerability have emerged. Fundamental safety and efficacy data for this agent in bipolar disorder are needed.
Levetiracetam Studies of levetiracetam for treatment of bipolar disorder are just under way. The Stanley Foundation Bipolar Treatment Network, a program of the National Alliance for the Mentally Ill Research Institute, is investigating its potential thymoleptic properties.
Related resources
- Joffe RT, Calabrese JR. Anticonvulsants in Mood Disorders. New York: Marcel Dekker Inc., 1994.
- Modigh K, Robak OH, Vestergaard P. Anticonvulsants in Psychiatry. Bristol, Pa: Wrightson Biomedical Publishing, Ltd., 1994.
- Schatzberg AF, Nemeroff CB. Textbook of Psychopharmacology, 2 nd ed. Washington, DC: American Psychiatric Press, 1998.
- Nathan P, Gorman J. A Guide to Treatments that Work, 2 nd ed. New York: Oxford University Press, 2001.
- Janicak PG, Davis JM, Preskorn SH, Ayd FJ, Jr. Principles and Practice of Psychopharmacotherapy, 2 nd ed. Baltimore, MD: Williams & Wilkins, 1997.
Drug brand names
- Carbamazepine • Tegretol, Epitol, Atretol
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levetiracetam • Keppra
- Oxcarbazepine • Trileptal
- Tiagabine • Gabatril
- Topiramate • Topamax
- Valproate-divalproex sodium • Depakote, Depakote ER
- Zonisamide • Zonegran
Disclosure
Dr. Keck reports that he receives grant/research support from and serves as a consultant to Abbott Laboratories, AstraZeneca, Pfizer Inc., and Eli Lilly and Co. He also receives grant/research support from Merck and Co. and Otsuka America Pharmaceutical, and serves as a consultant to Bristol-Myers Squibb Co., GlaxoSmithKline, and Janssen Pharmaceutica.
Dr. McElroy reports that she receives grant/research support from and serves as a consultant to Abbott Laboratories, Elan Pharmaceuticals, Cephalon Inc. GlaxoSmithKline, and Eli Lilly and Co. She also receives grant/research support from Forest Pharmaceuticals and Solvay Pharmaceuticals, and serves as a consultant to Bristol-Myers Squibb Co., Ortho-McNeil Pharmaceutical, and Janssen Pharmaceutica.
1. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry. 1998;59(Suppl 6):74-81.
2. McElroy SL, Keck PE, Jr. Pharmacologic agents for the treatment of acute bipolar mania. Biol Psychiatry. 2000;48:539-557.
3. Post RM, Denicoff KD, Frye MA, Leverich GS. Re-evaluating carbamazepine prophylaxis in bipolar disorder. Br J Psychiatry. 1997;170:202-204.
4. Greil W, Ludwig-Mayerhofer W, Erazon-Scheichlin C, Schmidt S, Engel RR, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders–a randomized study. J Affect Disorders. 1997;43:151-161.
5. Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO, Leverich GS, Post RM. Comparative prophylactic efficacy of lithium, carbamazepine and the combination in bipolar disorder. J Clin Psychiatry. 1997;58:470-478.
6. Suppes T, Swann AC, Dennehy EB, Habermacher ED, Mason M, Crismon ML, Toprac MG, Rush AJ, Shon SP, Altshuler KZ. Texas Medication Algorithm Project: development and feasibility testing of a treatment algorithm for patients with bipolar disorder. J Clin Psychiatry. 2001;62:439-447.
7. Pope HG, Jr, McElroy SL, Keck PE, Jr, Hudson JI. Valproate in the treatment of acute mania: a placebo-controlled study. Arch Gen Psychiatry. 1991;48:62-68.
8. Bowden CL, Brugger AM, Swann AC, Calabrese JR, Janicak PG, Petty F, et al. Efficacy of divalproex sodium vs. lithium and placebo in the treatment of mania. JAMA. 1994;271:915-924.
9. Tohen M, Baker RW, Milton DR, Risser RC, Gilmore JA, Davis AR, et al. Olanzapine versus divalproex sodium for the treatment of acute mania. Bipolar Disorders. 2001;3(Suppl 1):60-61.
10. Zajecka J. Divalproex versus olanzapine in the treatment of acute mania. Presented at the 39 th Annual Meeting of the American College of Neuropsychopharmacology. San Juan, Puerto Rico, Dec. 10-14, 2000.
11. Bowden CL, Calabrese JR, McElroy SL, Hirschfeld RMA, Petty F, Gyulai LL, Pope HG, Jr, et al. Efficacy of divalproex versus lithium and placebo in maintenance treatment of bipolar disorder. Arch Gen Psychiatry. 2000;57:481-489.
12. Tohen M, Baker RW, Altshuler LL, Zarate CA, Suppes T, Ketter T, et al. Olanzapine versus divalproex for bipolar mania: a 47-week study. Presented at the European College of Neuropsychopharmacology Meeting, Istanbul, Turkey, Oct. 15, 2001.
13. Pande AD, Crockatt JG, Janney CA, Werth JL, Tsaaroucha G. and the Gabapentin Bipolar Disorder Study Group. Bipolar Disorders. 2000;2:249-255.
14. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol. 2000;24:205-212.
15. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in rapid-cycling bipolar disorder. J Clin Psychiatry. 2000;61:841-850.
16. Bowden CL, Calabrese JR, Akthar S, Olajossy M, Montgomery S, Ascher J, et al. Lamotrigine demonstrates long-term mood stabilization in manic patients. Bipolar Disorders. 2001;3(Suppl 1):27-28.
17. Calabrese JR, Bowden CL, Sachs GS, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. J Clin Psychiatry. 1999;60:79-88.
18. McElroy SL, Suppes T, Keck PE, Jr, Frye MA, Denicoff KD, Altshuler LL, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry. 2000;47:1025-1033.
19. Calabrese JR. A double-blind, placebo-controlled trial of topiramate monotherapy in the treatment of acute mania. Presented at the Annual Meeting of the European College of Neuropsychopharmacology. Munich, Germany, Sept. 9-13, 2000.
20. Emrich H, Schiwy W, Silverstone T. eds. Carbamazepine and Oxcarbazepine in Psychiatry. London: CNS Publishers, 1990.
1. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry. 1998;59(Suppl 6):74-81.
2. McElroy SL, Keck PE, Jr. Pharmacologic agents for the treatment of acute bipolar mania. Biol Psychiatry. 2000;48:539-557.
3. Post RM, Denicoff KD, Frye MA, Leverich GS. Re-evaluating carbamazepine prophylaxis in bipolar disorder. Br J Psychiatry. 1997;170:202-204.
4. Greil W, Ludwig-Mayerhofer W, Erazon-Scheichlin C, Schmidt S, Engel RR, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders–a randomized study. J Affect Disorders. 1997;43:151-161.
5. Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO, Leverich GS, Post RM. Comparative prophylactic efficacy of lithium, carbamazepine and the combination in bipolar disorder. J Clin Psychiatry. 1997;58:470-478.
6. Suppes T, Swann AC, Dennehy EB, Habermacher ED, Mason M, Crismon ML, Toprac MG, Rush AJ, Shon SP, Altshuler KZ. Texas Medication Algorithm Project: development and feasibility testing of a treatment algorithm for patients with bipolar disorder. J Clin Psychiatry. 2001;62:439-447.
7. Pope HG, Jr, McElroy SL, Keck PE, Jr, Hudson JI. Valproate in the treatment of acute mania: a placebo-controlled study. Arch Gen Psychiatry. 1991;48:62-68.
8. Bowden CL, Brugger AM, Swann AC, Calabrese JR, Janicak PG, Petty F, et al. Efficacy of divalproex sodium vs. lithium and placebo in the treatment of mania. JAMA. 1994;271:915-924.
9. Tohen M, Baker RW, Milton DR, Risser RC, Gilmore JA, Davis AR, et al. Olanzapine versus divalproex sodium for the treatment of acute mania. Bipolar Disorders. 2001;3(Suppl 1):60-61.
10. Zajecka J. Divalproex versus olanzapine in the treatment of acute mania. Presented at the 39 th Annual Meeting of the American College of Neuropsychopharmacology. San Juan, Puerto Rico, Dec. 10-14, 2000.
11. Bowden CL, Calabrese JR, McElroy SL, Hirschfeld RMA, Petty F, Gyulai LL, Pope HG, Jr, et al. Efficacy of divalproex versus lithium and placebo in maintenance treatment of bipolar disorder. Arch Gen Psychiatry. 2000;57:481-489.
12. Tohen M, Baker RW, Altshuler LL, Zarate CA, Suppes T, Ketter T, et al. Olanzapine versus divalproex for bipolar mania: a 47-week study. Presented at the European College of Neuropsychopharmacology Meeting, Istanbul, Turkey, Oct. 15, 2001.
13. Pande AD, Crockatt JG, Janney CA, Werth JL, Tsaaroucha G. and the Gabapentin Bipolar Disorder Study Group. Bipolar Disorders. 2000;2:249-255.
14. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol. 2000;24:205-212.
15. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in rapid-cycling bipolar disorder. J Clin Psychiatry. 2000;61:841-850.
16. Bowden CL, Calabrese JR, Akthar S, Olajossy M, Montgomery S, Ascher J, et al. Lamotrigine demonstrates long-term mood stabilization in manic patients. Bipolar Disorders. 2001;3(Suppl 1):27-28.
17. Calabrese JR, Bowden CL, Sachs GS, et al. A double-blind, placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. J Clin Psychiatry. 1999;60:79-88.
18. McElroy SL, Suppes T, Keck PE, Jr, Frye MA, Denicoff KD, Altshuler LL, et al. Open-label adjunctive topiramate in the treatment of bipolar disorders. Biol Psychiatry. 2000;47:1025-1033.
19. Calabrese JR. A double-blind, placebo-controlled trial of topiramate monotherapy in the treatment of acute mania. Presented at the Annual Meeting of the European College of Neuropsychopharmacology. Munich, Germany, Sept. 9-13, 2000.
20. Emrich H, Schiwy W, Silverstone T. eds. Carbamazepine and Oxcarbazepine in Psychiatry. London: CNS Publishers, 1990.
‘I’m as ugly as the elephant man’: How to recognize and treat body dysmorphic disorder
A 52-year-old man becomes intoxicated with alcohol so he can lie in his backyard and get a tan. Convinced that his skin is too pale and that he looks “like a ghost,” he is so self-conscious about how he looks that he can’t go outside without drinking excessively.
An attractive 23-year-old woman dropped out of the 10th grade because of her “hideous” appearance and has hidden in her bedroom in her parents’ house ever since. She leaves her room no more than once a month, only after covering her face with a veil, not letting even her family see her face.
A middle-aged man cuts his nose open with a razor blade, trying to remove his nasal cartilage and replace it with chicken cartilage, in the desired shape.
These patients have body dysmorphic disorder (BDD), a somatoform disorder that the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) defines as a preoccupation with an imagined defect in appearance; if a slight physical anomaly is present, the person's concern is markedly excessive. The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning that are not attributed to another mental disorder.
Most of us are dissatisfied with some aspect of how we look. In fact, more than half of all women and nearly half of all men in the United States are dissatisfied with their overall appearance.1 As the preceding cases illustrate, however, BDD does not consist simply of normal appearance concerns.
BDD is a relatively common disorder2 (Box 1) that occurs in children as well as adults. It usually begins during the early teenage years.2 BDD has been described around the world for more than a century.3 It causes notable distress and impaired functioning, and can lead to suicide.4 This disorder typically goes undiagnosed in clinical settings, however, in part because many patients are too embarrassed and ashamed to discuss their symptoms with their physicians unless specifically asked.2,5 BDD often masquerades as other psychiatric disorders, and misdiagnosis appears common6 (Table 1). Diagnosing BDD is usually straightforward, however, and can be achieved using the questions in Box 2.4 Clues to the presence of BDD are presented in Box 3; patients who present with any of them should be carefully evaluated for BDD.
- 1 in 8 psychiatric inpatients (13%)
- 1 in 7 to nearly half of outpatients with atypical major depression (14%-42%)
- 1 in 8 to 9 outpatients with social phobia (11%-13%)
- 1 in 3 to 12 outpatients with obsessive-compulsive disorder (8%-37%)
- 1 in 8 patients seeking dermatologic treatment (12%)
- 1 in 7 to 15 patients seeking cosmetic surgery (6%-15%)
- Nearly 1 in 100 to more than 1 in 50 people in the general population (0.7%-2.3%)
Perceptions of patients with BDD
Individuals with BDD obsess that there is something wrong with their appearance when in fact they look fine; the perceived flaw is actually minimal or nonexistent.7 Prior to treatment, insight is usually poor or absent, however, so that most patients are convinced or fairly certain that they look abnormal.2,8 They may describe the perceived flaw as unattractive or deformed, or they may even say that they look like a freak, a monster, or the “elephant man” (Box 4). Individuals with this disorder think about the perceived appearance flaws, on average, for 3 to 8 hours a day, and they usually find the thoughts difficult to resist or control.9 Diagnostic errors that cause BDD to be missed
Table 1
Diagnostic errors that cause BDD to be missed
| Misdiagnosis | Diagnostic error | How to avoid the error |
|---|---|---|
| Depression | The depressive symptoms that often coexist with BDD are diagnosed and BDD is missed; or BDD symptoms are considered a symptom of depression. In the author’s clinical experience, this is the most common diagnostic error. | Look for BDD in all depressed patients; appearance concerns may not be simply a symptom of depression. |
| Social phobia | Social anxiety is a common consequence of BDD, which may be misdiagnosed as social phobia or avoidant personality disorder. | Explore the cause of social anxiety or avoidance and determine whether it is secondary to BDD. |
| Agoraphobia | Many BDD patients are housebound at some point, which may be misdiagnosed as agoraphobia. | Explore the cause of avoidance and determine whether it is due to BDD. |
| OCD | BDD’s prominent obsessions and compulsive behaviors may be misdiagnosed as OCD. | If the obsessions and behaviors focus on physical appearance, BDD is the more accurate diagnosis. |
| Panic disorder | Panic attacks that occur when looking in the mirror or experiencing referential thinking can be misdiagnosed as panic disorder. | Determine whether panic attacks have BDD-related triggers; if so, BDD should be diagnosed. |
| Trichotillomania | Some BDD patients remove their body, head, or facial hair in an effort to improve their appearance, which may be misdiagnosed as trichotillomania. | Determine whether hair removal reflects thoughts that the hair does not look right and is intended to improve appearance; if so, the patient may have BDD. |
| Schizophrenia. | Because BDD beliefs are often delusional, and many patients have referential thinking, occasionally patients are misdiagnosed with Schizophrenia | If psychotic symptoms are largely limited to a nonbizarre delusional belief about one’s physical appearance and/or related delusions of reference, BDD is the more accurate diagnosis. |
Although repetitive behaviors are not part of BDD’s diagnostic criteria, virtually all patients perform such behaviors, usually in an attempt to improve, hide, examine, or be reassured about the perceived flaw.7,9 (See Box 3 for a partial listing.) These behaviors are usually time-consuming, occurring for many hours a day, and, like the preoccupations, are typically difficult to resist or control. With the exception of camouflaging, however, they often do not diminish appearance concerns. In fact, some of them (e.g., mirror checking) may actually increase anxiety about the perceived flaw.
Comorbidity is common in patients seen in clinical settings.2,8 Major depression is the most frequent comorbid disorder, which often appears secondary to BDD.10 Other common comorbidities include substance-use disorders, obsessive-compulsive disorder (OCD), social phobia, and personality disorders (most often, avoidant personality disorder).
Individuals with BDD are distressed over their appearance, many to the point of contemplating, attempting, or completing suicide.4,5 Nearly one quarter of patients seen in a clinical setting have attempted suicide.9 Although some patients appear to function reasonably well, they usually function below their capacity—for example, by avoiding social situations or meetings at work where others will see them. Others are completely incapacitated by their BDD symptoms, unable to work or socialize, and may be housebound for years.2,8,9 In a study that used the SF-36 to measure health-related quality of life, outpatients with BDD scored notably worse in all mental health domains than did the general U.S. population and patients with depression, type II diabetes, or a recent myocardial infarction.2
- Are you worried about your appearance in any way? If yes: What is your concern? OR Are you unhappy with how you look? If yes: What is your concern?
- Does this concern preoccupy you? That is, do you think about it a lot and wish you could worry about it less? OR If you add up all the time you spend each day thinking about your appearance, how much time would you estimate you spend?
- What effect has this preoccupation with your appearance had on your life? Has it:
BDD is diagnosed in patients who 1) are concerned about a minimal or nonexistent appearance flaw, 2) are preoccupied with the “flaw” (e.g., think about it for at least an hour a day), and 3) experience clinically significant distress or impairment in functioning as a result of their concern.
- Mirror checking or avoidance, or checking other reflective surfaces, such as windows, car bumpers, or the backs of spoons
- Reassurance seeking, that is, asking other people how they look or insisting that they look bad
- Skin picking, which may be manifested by skin lesions or scarring
- Excessive grooming, for example hair styling, applying makeup, shaving, tweezing hair, or cutting hair or wigs
- Camouflaging with a hat, toupee, makeup, sunglasses, clothes, or body position
- Excessive tanning, to darken “pale” skin
- Ideas or delusions of reference, thinking others take special notice of the “flaw” in a negative way (e.g., mock it or stare at it)
- Treatment-resistant anxiety, especially social anxiety, or depression
- Social avoidance or being housebound
- Unnecessary surgery, dermatologic treatment, or other nonpsychiatric treatment (e.g., electrolysis)
Guidelines for treating BDD
- Establish trust. It is important to convey that you take the patient’s appearance concerns seriously. Many patients with BDD fear being considered silly or vain and do not divulge their symptoms. It is usually best to avoid reassuring patients that they look fine, since they usually do not believe the reassurance and can interpret it as trivializing their concerns.
- Provide psychoeducation. Explain to patients that they have a relatively common and treatable body image disorder. To decrease the patient’s reluctance to accept the diagnosis and treatment, it can be helpful to emphasize the excessive preoccupation, distress, and other problems their symptoms are causing. Discussions about whether the defect is “real” are usually fruitless, unless the patient already has good insight, which is rare. Several educational books and Web sites for patients are available. See Related Resources.
- Target BDD symptoms in treatment. Ignoring BDD symptoms and focusing treatment on other symptoms only may be unsuccessful because effective treatment for BDD differs in some important ways from that of most other psychiatric disorders, such as depression.10 It appears, for example, that non-selective serotonin reuptake inhibitor (SSRI) antidepressants are generally ineffective for BDD, unless used at higher SSRI doses than are often needed for depression. BDD symptoms also do not necessarily improve in concert with symptoms of other disorders, such as depression or OCD.10
- Avoid nonpsychiatric medical treatment. Although no one can predict how an individual patient will respond to nonpsychiatric treatment, (e.g., surgery or dermatologic treatment), explain that as best we know, such treatment usually appears to be ineffective for BDD and even can make the symptoms worse.11
Which psychopharmaceuticals should you consider?
Although BDD’s response to pharmacotherapy has received far less investigation than that of many other psychiatric disorders, research on this treatment approach has dramatically increased in recent years. The following strategies are suggested on the basis of evidence from controlled studies, open-label trials, and the author’s clinical experience (Figure 1):2,6,8,12-17
‘I’m as ugly as the elephant man’

Chris is a shy, anxious-appearing, 31-year-old man who was hospitalized after attempting suicide. He wears a baseball cap pulled down over his forehead and partially covering his eyes. It is difficult for him to reveal the reason for his suicide attempt: “It’s really hard to talk about this. I don’t know if I can. It’s too embarrassing.” Then he adds, “Well I guess I should tell you—after all, I’m in the hospital because of it. It’s my nose—these huge pock marks on my nose. They’re grotesque! I look like a monster. I’m as ugly as the elephant man!
“These marks on my nose are all I can think about. I’ve thought about them for hours a day every day for the past 15 years. I even have nightmares about them. And I think that everyone can see them and that they laugh at me because of them. That’s why I wear this hat all the time. And that’s why I couldn’t talk to you in a bright room. You’d notice the marks and see how ugly I am.” Chris actually appeared entirely normal, but no one could convince him of this.
“This has affected me in a lot of ways,” Chris adds. “This may be hard for you to believe, but this problem has ruined my life. All I can think about is my face, and I spend hours a day looking at the marks in the mirror. I just can’t resist. I thought I looked so ugly that I started missing more and more work, and I stopped going out with my friends and my girlfriend. I got so anxious when people looked at me that I started staying in the house most of the time. Sometimes when I did go out, I went through red lights so I wouldn’t have to sit at the light, where people might be staring at me. The hat helped a little, but it didn’t cover all the marks. I tried covering them with makeup for a while, but I thought people could see the makeup so that didn’t really help. The only time I really felt comfortable is when I wore my nephew’s Batman mask on Halloween—then no one could see the marks.
I finally missed so much work that I was fired. My girlfriend stuck it out with me for a long time, but finally she couldn’t take it any more. One thing that was really hard for her was that I started asking her about 50 times a day whether I looked OK and whether she could see the marks—I think that was the final straw. If I had a choice, I’d rather have cancer. It must be less painful. This is like an arrow through my heart.”
Chris had a notable, although only partial, response to fluoxetine 100 mg/d and buspirone 60 mg/d (higher doses of fluoxetine and buspirone were tried but were not more effective). Adding clonazepam was helpful for severe anxiety. Clomipramine, venlafaxine, lithium, mirtazapine, and various antipsychotics were sequentially added to this regimen, with minimal success, although a second trial of olanzapine, at a higher dose (15 mg/d) than he had been willing to try previously, further decreased Chris’ BDD and depressive symptoms. The addition of bupropion was somewhat helpful for depression but not for BDD.
Figure 1 Proposed pharmacotherapy for treating BDD
- Use an SSRI as a first-line approach. Other medications, including other antidepressants, appear less effective than SSRIs or clomipramine.2,8,9,13,15 An SSRI or clomipramine is also recommended for patients with delusional BDD (those who are completely convinced that they look abnormal and cannot be convinced otherwise), as Proposed pharmacotherapy for treating BDD these patients appear to respond to SSRIs as well as nondelusional patients do.12-17
- Use the maximum recommended or tolerated SSRI dose if lower doses are ineffective. Although no studies have compared different SSRI dosages, BDD appears to often require higher doses than those that are typically used for depression.
In a chart-review study of 90 patients with BDD treated in the author’s clinical practice, the mean SSRI doses used were fluoxetine 66.7 ±23.5 mg/d, fluvoxamine 308.3 ±49.2 mg/d, paroxetine 55.0 ± 12.9 mg/d, sertraline 202.1 ± 45.8 mg/d, and clomipramine 203.3 ±52.5 mg/d.17 Some patients respond only to doses higher than the maximum recommended dose (for example, 80-100 mg/d of citalopram or paroxetine).
- Treat for 12 to 16 weeks with an SSRI before concluding that the medication is ineffective. The average time to response is between 6 to 9 weeks.12,14,16 Clinical experience suggests that with continued treatment, relapse is rare and many patients further improve.
- Try sequential SSRIs if the first or second one does not work. A substantial percentage of patients who fail an initial SSRI trial will respond to a subsequent SSRI.17
- Continue an effective SSRI for at least 1 year before discontinuing it, as relapse appears likely with discontinuation.17 Severely ill patients may require treatment for life.
- Several SSRI augmentation and combination strategies might be helpful (Figure 1).16,17 If clomipramine is used in combination with an SSRI, the clomipramine level should be monitored.
What is the role of psychotherapy?
Although research on psychotherapy for BDD is limited, findings from clinical series and studies using waiting-list controls indicate that cognitive-behavioral therapy (CBT) is often effective.18-20 In contrast, supportive psychotherapy and insight-oriented and psychodynamic psychotherapy alone appear to be ineffective.9 CBT usually consists of a cognitive element (e.g., changing distorted views of the appearance “flaw”), exposure to feared and avoided situations (often social), and response prevention, avoiding repetitive behaviors such as excessive grooming.
- Consider using CBT as a first-line approach for milder BDD without significant comorbidity requiring pharmacotherapy.
- Use more intensive CBT treatment including frequent sessions and use of homework rather than less intensive treatment, although the optimal number and frequency of sessions is unknown.
- Consider maintenance and booster sessions for patients with more severe BDD following treatment to prevent relapse.
- Consider combining CBT and an SSRI. Although it is not known whether a combination of these treatments is more effective than either one alone, they are compatible and their combination may benefit certain patients. For patients with severe BDD, especially very depressed or suicidal patients, it is probably best to use CBT in combination with medication only, as sicker patients may not be able to tolerate or participate in CBT without first experiencing some improvement with medication.
- Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
- Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
- Phillips KA, Van Noppen B, Shapiro L. Learning to Live with Body Dysmorphic Disorder. Milford, Conn: Obsessive-Compulsive Foundation, 1997.
- Body Dysmorphic Disorder (BDD)and Body Image Program Homepage at Butler Hospital (Providence, RI). http://www.bodyimageprogram.com
Drug brand names
- Bupropion • Wellbutrin, Zyban
- Buspirone • Buspar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Ativan, Diastat, Halcion
- Fluoxetine • Prozac, Sarafem
- Fluvoxamine • Luvox
- Mirtazapine • Remeron, Remeron Solitab
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The author reports that she receives grant support and occasional speaking honoraria from Eli Lilly and Co.; receives grant support from Forest Pharmaceuticals and Gate Pharmaceuticals; is on the speakers' bureau of Solvay Pharmaceuticals; and serves as a consultant for Wyeth-Ayerst Pharmaceuticals.
1. Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
2. Phillips KA. Body dysmorphic disorder. In: Phillips KA, ed. Somatoform and Factitious Disorders. Washington DC: American Psychiatric Publishing, 2001.
3. Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. Am J Psychiatry. 1991;148:1138-1149.
4. Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
5. Grant JE, et al. Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. J Clin Psychiatry. 2001;62:517-522.
6. Phillips KA. Body dysmorphic disorder: diagnostic controversies and treatment challenges. Bull Menninger Clin. 2000;64:18-35.
7. Hollander E, Cohen LJ, Simeon D. Body dysmorphic disorder. Psychiatric Annals. 1993;23:359-364.
8. Phillips KA, Castle DJ. Body dysmorphic disorder. In: Castle DJ, Phillips KA, eds. Disorders of Body Image. Hampshire, England: Wrightson Biomedical, in press.
9. Phillips KA, McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry. 1993;150:302-308.
10. Phillips KA: Body dysmorphic disorder and depression: theoretical considerations and treatment strategies. Psychiatry Quart. 1999;70:313-331.
11. Phillips KA, Grant JD, Siniscalchi J, Albertini RS. Surgical and nonpsychiatric medical treatment of patients with body dysmorphic disorder. Psychosomatics, in press.
12. Phillips KA, Dwight MM, McElroy SL. Efficacy and safety of fluvoxamine in body dysmorphic disorder. J Clin Psychiatry. 1998;59:165-171.
13. Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, Simeon D. Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch Gen Psychiatry. 1999;56:1033-1039.
14. Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry, in press.
15. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: review of the evidence and a recommended treatment approach. CNS Spectrums, in press.
16. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: a review of empirical data and a proposed treatment algorithm. Psychiatric Clin North Am. 2000;7:59-82.
17. Phillips KA, Albertini RS, Siniscalchi J, Khan A, Robinson M. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. J Clin Psychiatry. 2001;721-727.
18. Neziroglu FA, Yaryura-Tobias JA. Exposure, response prevention, and cognitive therapy in the treatment of body dysmorphic disorder. Behav Ther. 1993;24:431-438.
19. Veale D, Gournay K, Dryden W, Boocock A, Shah F, Willson R, Walburn J. Body dysmorphic disorder: a cognitive behavioural model and pilot randomized controlled trial. Behav Res Therapeut. 1996;34:717-729.
20. Wilhelm S, Otto MW, Lohr B, Deckersback T. Cognitive behavior group therapy for body dysmorphic disorder: a case series. Behav Res Ther. 1999;37:71-75.
A 52-year-old man becomes intoxicated with alcohol so he can lie in his backyard and get a tan. Convinced that his skin is too pale and that he looks “like a ghost,” he is so self-conscious about how he looks that he can’t go outside without drinking excessively.
An attractive 23-year-old woman dropped out of the 10th grade because of her “hideous” appearance and has hidden in her bedroom in her parents’ house ever since. She leaves her room no more than once a month, only after covering her face with a veil, not letting even her family see her face.
A middle-aged man cuts his nose open with a razor blade, trying to remove his nasal cartilage and replace it with chicken cartilage, in the desired shape.
These patients have body dysmorphic disorder (BDD), a somatoform disorder that the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) defines as a preoccupation with an imagined defect in appearance; if a slight physical anomaly is present, the person's concern is markedly excessive. The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning that are not attributed to another mental disorder.
Most of us are dissatisfied with some aspect of how we look. In fact, more than half of all women and nearly half of all men in the United States are dissatisfied with their overall appearance.1 As the preceding cases illustrate, however, BDD does not consist simply of normal appearance concerns.
BDD is a relatively common disorder2 (Box 1) that occurs in children as well as adults. It usually begins during the early teenage years.2 BDD has been described around the world for more than a century.3 It causes notable distress and impaired functioning, and can lead to suicide.4 This disorder typically goes undiagnosed in clinical settings, however, in part because many patients are too embarrassed and ashamed to discuss their symptoms with their physicians unless specifically asked.2,5 BDD often masquerades as other psychiatric disorders, and misdiagnosis appears common6 (Table 1). Diagnosing BDD is usually straightforward, however, and can be achieved using the questions in Box 2.4 Clues to the presence of BDD are presented in Box 3; patients who present with any of them should be carefully evaluated for BDD.
- 1 in 8 psychiatric inpatients (13%)
- 1 in 7 to nearly half of outpatients with atypical major depression (14%-42%)
- 1 in 8 to 9 outpatients with social phobia (11%-13%)
- 1 in 3 to 12 outpatients with obsessive-compulsive disorder (8%-37%)
- 1 in 8 patients seeking dermatologic treatment (12%)
- 1 in 7 to 15 patients seeking cosmetic surgery (6%-15%)
- Nearly 1 in 100 to more than 1 in 50 people in the general population (0.7%-2.3%)
Perceptions of patients with BDD
Individuals with BDD obsess that there is something wrong with their appearance when in fact they look fine; the perceived flaw is actually minimal or nonexistent.7 Prior to treatment, insight is usually poor or absent, however, so that most patients are convinced or fairly certain that they look abnormal.2,8 They may describe the perceived flaw as unattractive or deformed, or they may even say that they look like a freak, a monster, or the “elephant man” (Box 4). Individuals with this disorder think about the perceived appearance flaws, on average, for 3 to 8 hours a day, and they usually find the thoughts difficult to resist or control.9 Diagnostic errors that cause BDD to be missed
Table 1
Diagnostic errors that cause BDD to be missed
| Misdiagnosis | Diagnostic error | How to avoid the error |
|---|---|---|
| Depression | The depressive symptoms that often coexist with BDD are diagnosed and BDD is missed; or BDD symptoms are considered a symptom of depression. In the author’s clinical experience, this is the most common diagnostic error. | Look for BDD in all depressed patients; appearance concerns may not be simply a symptom of depression. |
| Social phobia | Social anxiety is a common consequence of BDD, which may be misdiagnosed as social phobia or avoidant personality disorder. | Explore the cause of social anxiety or avoidance and determine whether it is secondary to BDD. |
| Agoraphobia | Many BDD patients are housebound at some point, which may be misdiagnosed as agoraphobia. | Explore the cause of avoidance and determine whether it is due to BDD. |
| OCD | BDD’s prominent obsessions and compulsive behaviors may be misdiagnosed as OCD. | If the obsessions and behaviors focus on physical appearance, BDD is the more accurate diagnosis. |
| Panic disorder | Panic attacks that occur when looking in the mirror or experiencing referential thinking can be misdiagnosed as panic disorder. | Determine whether panic attacks have BDD-related triggers; if so, BDD should be diagnosed. |
| Trichotillomania | Some BDD patients remove their body, head, or facial hair in an effort to improve their appearance, which may be misdiagnosed as trichotillomania. | Determine whether hair removal reflects thoughts that the hair does not look right and is intended to improve appearance; if so, the patient may have BDD. |
| Schizophrenia. | Because BDD beliefs are often delusional, and many patients have referential thinking, occasionally patients are misdiagnosed with Schizophrenia | If psychotic symptoms are largely limited to a nonbizarre delusional belief about one’s physical appearance and/or related delusions of reference, BDD is the more accurate diagnosis. |
Although repetitive behaviors are not part of BDD’s diagnostic criteria, virtually all patients perform such behaviors, usually in an attempt to improve, hide, examine, or be reassured about the perceived flaw.7,9 (See Box 3 for a partial listing.) These behaviors are usually time-consuming, occurring for many hours a day, and, like the preoccupations, are typically difficult to resist or control. With the exception of camouflaging, however, they often do not diminish appearance concerns. In fact, some of them (e.g., mirror checking) may actually increase anxiety about the perceived flaw.
Comorbidity is common in patients seen in clinical settings.2,8 Major depression is the most frequent comorbid disorder, which often appears secondary to BDD.10 Other common comorbidities include substance-use disorders, obsessive-compulsive disorder (OCD), social phobia, and personality disorders (most often, avoidant personality disorder).
Individuals with BDD are distressed over their appearance, many to the point of contemplating, attempting, or completing suicide.4,5 Nearly one quarter of patients seen in a clinical setting have attempted suicide.9 Although some patients appear to function reasonably well, they usually function below their capacity—for example, by avoiding social situations or meetings at work where others will see them. Others are completely incapacitated by their BDD symptoms, unable to work or socialize, and may be housebound for years.2,8,9 In a study that used the SF-36 to measure health-related quality of life, outpatients with BDD scored notably worse in all mental health domains than did the general U.S. population and patients with depression, type II diabetes, or a recent myocardial infarction.2
- Are you worried about your appearance in any way? If yes: What is your concern? OR Are you unhappy with how you look? If yes: What is your concern?
- Does this concern preoccupy you? That is, do you think about it a lot and wish you could worry about it less? OR If you add up all the time you spend each day thinking about your appearance, how much time would you estimate you spend?
- What effect has this preoccupation with your appearance had on your life? Has it:
BDD is diagnosed in patients who 1) are concerned about a minimal or nonexistent appearance flaw, 2) are preoccupied with the “flaw” (e.g., think about it for at least an hour a day), and 3) experience clinically significant distress or impairment in functioning as a result of their concern.
- Mirror checking or avoidance, or checking other reflective surfaces, such as windows, car bumpers, or the backs of spoons
- Reassurance seeking, that is, asking other people how they look or insisting that they look bad
- Skin picking, which may be manifested by skin lesions or scarring
- Excessive grooming, for example hair styling, applying makeup, shaving, tweezing hair, or cutting hair or wigs
- Camouflaging with a hat, toupee, makeup, sunglasses, clothes, or body position
- Excessive tanning, to darken “pale” skin
- Ideas or delusions of reference, thinking others take special notice of the “flaw” in a negative way (e.g., mock it or stare at it)
- Treatment-resistant anxiety, especially social anxiety, or depression
- Social avoidance or being housebound
- Unnecessary surgery, dermatologic treatment, or other nonpsychiatric treatment (e.g., electrolysis)
Guidelines for treating BDD
- Establish trust. It is important to convey that you take the patient’s appearance concerns seriously. Many patients with BDD fear being considered silly or vain and do not divulge their symptoms. It is usually best to avoid reassuring patients that they look fine, since they usually do not believe the reassurance and can interpret it as trivializing their concerns.
- Provide psychoeducation. Explain to patients that they have a relatively common and treatable body image disorder. To decrease the patient’s reluctance to accept the diagnosis and treatment, it can be helpful to emphasize the excessive preoccupation, distress, and other problems their symptoms are causing. Discussions about whether the defect is “real” are usually fruitless, unless the patient already has good insight, which is rare. Several educational books and Web sites for patients are available. See Related Resources.
- Target BDD symptoms in treatment. Ignoring BDD symptoms and focusing treatment on other symptoms only may be unsuccessful because effective treatment for BDD differs in some important ways from that of most other psychiatric disorders, such as depression.10 It appears, for example, that non-selective serotonin reuptake inhibitor (SSRI) antidepressants are generally ineffective for BDD, unless used at higher SSRI doses than are often needed for depression. BDD symptoms also do not necessarily improve in concert with symptoms of other disorders, such as depression or OCD.10
- Avoid nonpsychiatric medical treatment. Although no one can predict how an individual patient will respond to nonpsychiatric treatment, (e.g., surgery or dermatologic treatment), explain that as best we know, such treatment usually appears to be ineffective for BDD and even can make the symptoms worse.11
Which psychopharmaceuticals should you consider?
Although BDD’s response to pharmacotherapy has received far less investigation than that of many other psychiatric disorders, research on this treatment approach has dramatically increased in recent years. The following strategies are suggested on the basis of evidence from controlled studies, open-label trials, and the author’s clinical experience (Figure 1):2,6,8,12-17
‘I’m as ugly as the elephant man’

Chris is a shy, anxious-appearing, 31-year-old man who was hospitalized after attempting suicide. He wears a baseball cap pulled down over his forehead and partially covering his eyes. It is difficult for him to reveal the reason for his suicide attempt: “It’s really hard to talk about this. I don’t know if I can. It’s too embarrassing.” Then he adds, “Well I guess I should tell you—after all, I’m in the hospital because of it. It’s my nose—these huge pock marks on my nose. They’re grotesque! I look like a monster. I’m as ugly as the elephant man!
“These marks on my nose are all I can think about. I’ve thought about them for hours a day every day for the past 15 years. I even have nightmares about them. And I think that everyone can see them and that they laugh at me because of them. That’s why I wear this hat all the time. And that’s why I couldn’t talk to you in a bright room. You’d notice the marks and see how ugly I am.” Chris actually appeared entirely normal, but no one could convince him of this.
“This has affected me in a lot of ways,” Chris adds. “This may be hard for you to believe, but this problem has ruined my life. All I can think about is my face, and I spend hours a day looking at the marks in the mirror. I just can’t resist. I thought I looked so ugly that I started missing more and more work, and I stopped going out with my friends and my girlfriend. I got so anxious when people looked at me that I started staying in the house most of the time. Sometimes when I did go out, I went through red lights so I wouldn’t have to sit at the light, where people might be staring at me. The hat helped a little, but it didn’t cover all the marks. I tried covering them with makeup for a while, but I thought people could see the makeup so that didn’t really help. The only time I really felt comfortable is when I wore my nephew’s Batman mask on Halloween—then no one could see the marks.
I finally missed so much work that I was fired. My girlfriend stuck it out with me for a long time, but finally she couldn’t take it any more. One thing that was really hard for her was that I started asking her about 50 times a day whether I looked OK and whether she could see the marks—I think that was the final straw. If I had a choice, I’d rather have cancer. It must be less painful. This is like an arrow through my heart.”
Chris had a notable, although only partial, response to fluoxetine 100 mg/d and buspirone 60 mg/d (higher doses of fluoxetine and buspirone were tried but were not more effective). Adding clonazepam was helpful for severe anxiety. Clomipramine, venlafaxine, lithium, mirtazapine, and various antipsychotics were sequentially added to this regimen, with minimal success, although a second trial of olanzapine, at a higher dose (15 mg/d) than he had been willing to try previously, further decreased Chris’ BDD and depressive symptoms. The addition of bupropion was somewhat helpful for depression but not for BDD.
Figure 1 Proposed pharmacotherapy for treating BDD
- Use an SSRI as a first-line approach. Other medications, including other antidepressants, appear less effective than SSRIs or clomipramine.2,8,9,13,15 An SSRI or clomipramine is also recommended for patients with delusional BDD (those who are completely convinced that they look abnormal and cannot be convinced otherwise), as Proposed pharmacotherapy for treating BDD these patients appear to respond to SSRIs as well as nondelusional patients do.12-17
- Use the maximum recommended or tolerated SSRI dose if lower doses are ineffective. Although no studies have compared different SSRI dosages, BDD appears to often require higher doses than those that are typically used for depression.
In a chart-review study of 90 patients with BDD treated in the author’s clinical practice, the mean SSRI doses used were fluoxetine 66.7 ±23.5 mg/d, fluvoxamine 308.3 ±49.2 mg/d, paroxetine 55.0 ± 12.9 mg/d, sertraline 202.1 ± 45.8 mg/d, and clomipramine 203.3 ±52.5 mg/d.17 Some patients respond only to doses higher than the maximum recommended dose (for example, 80-100 mg/d of citalopram or paroxetine).
- Treat for 12 to 16 weeks with an SSRI before concluding that the medication is ineffective. The average time to response is between 6 to 9 weeks.12,14,16 Clinical experience suggests that with continued treatment, relapse is rare and many patients further improve.
- Try sequential SSRIs if the first or second one does not work. A substantial percentage of patients who fail an initial SSRI trial will respond to a subsequent SSRI.17
- Continue an effective SSRI for at least 1 year before discontinuing it, as relapse appears likely with discontinuation.17 Severely ill patients may require treatment for life.
- Several SSRI augmentation and combination strategies might be helpful (Figure 1).16,17 If clomipramine is used in combination with an SSRI, the clomipramine level should be monitored.
What is the role of psychotherapy?
Although research on psychotherapy for BDD is limited, findings from clinical series and studies using waiting-list controls indicate that cognitive-behavioral therapy (CBT) is often effective.18-20 In contrast, supportive psychotherapy and insight-oriented and psychodynamic psychotherapy alone appear to be ineffective.9 CBT usually consists of a cognitive element (e.g., changing distorted views of the appearance “flaw”), exposure to feared and avoided situations (often social), and response prevention, avoiding repetitive behaviors such as excessive grooming.
- Consider using CBT as a first-line approach for milder BDD without significant comorbidity requiring pharmacotherapy.
- Use more intensive CBT treatment including frequent sessions and use of homework rather than less intensive treatment, although the optimal number and frequency of sessions is unknown.
- Consider maintenance and booster sessions for patients with more severe BDD following treatment to prevent relapse.
- Consider combining CBT and an SSRI. Although it is not known whether a combination of these treatments is more effective than either one alone, they are compatible and their combination may benefit certain patients. For patients with severe BDD, especially very depressed or suicidal patients, it is probably best to use CBT in combination with medication only, as sicker patients may not be able to tolerate or participate in CBT without first experiencing some improvement with medication.
- Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
- Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
- Phillips KA, Van Noppen B, Shapiro L. Learning to Live with Body Dysmorphic Disorder. Milford, Conn: Obsessive-Compulsive Foundation, 1997.
- Body Dysmorphic Disorder (BDD)and Body Image Program Homepage at Butler Hospital (Providence, RI). http://www.bodyimageprogram.com
Drug brand names
- Bupropion • Wellbutrin, Zyban
- Buspirone • Buspar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Ativan, Diastat, Halcion
- Fluoxetine • Prozac, Sarafem
- Fluvoxamine • Luvox
- Mirtazapine • Remeron, Remeron Solitab
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The author reports that she receives grant support and occasional speaking honoraria from Eli Lilly and Co.; receives grant support from Forest Pharmaceuticals and Gate Pharmaceuticals; is on the speakers' bureau of Solvay Pharmaceuticals; and serves as a consultant for Wyeth-Ayerst Pharmaceuticals.
A 52-year-old man becomes intoxicated with alcohol so he can lie in his backyard and get a tan. Convinced that his skin is too pale and that he looks “like a ghost,” he is so self-conscious about how he looks that he can’t go outside without drinking excessively.
An attractive 23-year-old woman dropped out of the 10th grade because of her “hideous” appearance and has hidden in her bedroom in her parents’ house ever since. She leaves her room no more than once a month, only after covering her face with a veil, not letting even her family see her face.
A middle-aged man cuts his nose open with a razor blade, trying to remove his nasal cartilage and replace it with chicken cartilage, in the desired shape.
These patients have body dysmorphic disorder (BDD), a somatoform disorder that the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) defines as a preoccupation with an imagined defect in appearance; if a slight physical anomaly is present, the person's concern is markedly excessive. The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning that are not attributed to another mental disorder.
Most of us are dissatisfied with some aspect of how we look. In fact, more than half of all women and nearly half of all men in the United States are dissatisfied with their overall appearance.1 As the preceding cases illustrate, however, BDD does not consist simply of normal appearance concerns.
BDD is a relatively common disorder2 (Box 1) that occurs in children as well as adults. It usually begins during the early teenage years.2 BDD has been described around the world for more than a century.3 It causes notable distress and impaired functioning, and can lead to suicide.4 This disorder typically goes undiagnosed in clinical settings, however, in part because many patients are too embarrassed and ashamed to discuss their symptoms with their physicians unless specifically asked.2,5 BDD often masquerades as other psychiatric disorders, and misdiagnosis appears common6 (Table 1). Diagnosing BDD is usually straightforward, however, and can be achieved using the questions in Box 2.4 Clues to the presence of BDD are presented in Box 3; patients who present with any of them should be carefully evaluated for BDD.
- 1 in 8 psychiatric inpatients (13%)
- 1 in 7 to nearly half of outpatients with atypical major depression (14%-42%)
- 1 in 8 to 9 outpatients with social phobia (11%-13%)
- 1 in 3 to 12 outpatients with obsessive-compulsive disorder (8%-37%)
- 1 in 8 patients seeking dermatologic treatment (12%)
- 1 in 7 to 15 patients seeking cosmetic surgery (6%-15%)
- Nearly 1 in 100 to more than 1 in 50 people in the general population (0.7%-2.3%)
Perceptions of patients with BDD
Individuals with BDD obsess that there is something wrong with their appearance when in fact they look fine; the perceived flaw is actually minimal or nonexistent.7 Prior to treatment, insight is usually poor or absent, however, so that most patients are convinced or fairly certain that they look abnormal.2,8 They may describe the perceived flaw as unattractive or deformed, or they may even say that they look like a freak, a monster, or the “elephant man” (Box 4). Individuals with this disorder think about the perceived appearance flaws, on average, for 3 to 8 hours a day, and they usually find the thoughts difficult to resist or control.9 Diagnostic errors that cause BDD to be missed
Table 1
Diagnostic errors that cause BDD to be missed
| Misdiagnosis | Diagnostic error | How to avoid the error |
|---|---|---|
| Depression | The depressive symptoms that often coexist with BDD are diagnosed and BDD is missed; or BDD symptoms are considered a symptom of depression. In the author’s clinical experience, this is the most common diagnostic error. | Look for BDD in all depressed patients; appearance concerns may not be simply a symptom of depression. |
| Social phobia | Social anxiety is a common consequence of BDD, which may be misdiagnosed as social phobia or avoidant personality disorder. | Explore the cause of social anxiety or avoidance and determine whether it is secondary to BDD. |
| Agoraphobia | Many BDD patients are housebound at some point, which may be misdiagnosed as agoraphobia. | Explore the cause of avoidance and determine whether it is due to BDD. |
| OCD | BDD’s prominent obsessions and compulsive behaviors may be misdiagnosed as OCD. | If the obsessions and behaviors focus on physical appearance, BDD is the more accurate diagnosis. |
| Panic disorder | Panic attacks that occur when looking in the mirror or experiencing referential thinking can be misdiagnosed as panic disorder. | Determine whether panic attacks have BDD-related triggers; if so, BDD should be diagnosed. |
| Trichotillomania | Some BDD patients remove their body, head, or facial hair in an effort to improve their appearance, which may be misdiagnosed as trichotillomania. | Determine whether hair removal reflects thoughts that the hair does not look right and is intended to improve appearance; if so, the patient may have BDD. |
| Schizophrenia. | Because BDD beliefs are often delusional, and many patients have referential thinking, occasionally patients are misdiagnosed with Schizophrenia | If psychotic symptoms are largely limited to a nonbizarre delusional belief about one’s physical appearance and/or related delusions of reference, BDD is the more accurate diagnosis. |
Although repetitive behaviors are not part of BDD’s diagnostic criteria, virtually all patients perform such behaviors, usually in an attempt to improve, hide, examine, or be reassured about the perceived flaw.7,9 (See Box 3 for a partial listing.) These behaviors are usually time-consuming, occurring for many hours a day, and, like the preoccupations, are typically difficult to resist or control. With the exception of camouflaging, however, they often do not diminish appearance concerns. In fact, some of them (e.g., mirror checking) may actually increase anxiety about the perceived flaw.
Comorbidity is common in patients seen in clinical settings.2,8 Major depression is the most frequent comorbid disorder, which often appears secondary to BDD.10 Other common comorbidities include substance-use disorders, obsessive-compulsive disorder (OCD), social phobia, and personality disorders (most often, avoidant personality disorder).
Individuals with BDD are distressed over their appearance, many to the point of contemplating, attempting, or completing suicide.4,5 Nearly one quarter of patients seen in a clinical setting have attempted suicide.9 Although some patients appear to function reasonably well, they usually function below their capacity—for example, by avoiding social situations or meetings at work where others will see them. Others are completely incapacitated by their BDD symptoms, unable to work or socialize, and may be housebound for years.2,8,9 In a study that used the SF-36 to measure health-related quality of life, outpatients with BDD scored notably worse in all mental health domains than did the general U.S. population and patients with depression, type II diabetes, or a recent myocardial infarction.2
- Are you worried about your appearance in any way? If yes: What is your concern? OR Are you unhappy with how you look? If yes: What is your concern?
- Does this concern preoccupy you? That is, do you think about it a lot and wish you could worry about it less? OR If you add up all the time you spend each day thinking about your appearance, how much time would you estimate you spend?
- What effect has this preoccupation with your appearance had on your life? Has it:
BDD is diagnosed in patients who 1) are concerned about a minimal or nonexistent appearance flaw, 2) are preoccupied with the “flaw” (e.g., think about it for at least an hour a day), and 3) experience clinically significant distress or impairment in functioning as a result of their concern.
- Mirror checking or avoidance, or checking other reflective surfaces, such as windows, car bumpers, or the backs of spoons
- Reassurance seeking, that is, asking other people how they look or insisting that they look bad
- Skin picking, which may be manifested by skin lesions or scarring
- Excessive grooming, for example hair styling, applying makeup, shaving, tweezing hair, or cutting hair or wigs
- Camouflaging with a hat, toupee, makeup, sunglasses, clothes, or body position
- Excessive tanning, to darken “pale” skin
- Ideas or delusions of reference, thinking others take special notice of the “flaw” in a negative way (e.g., mock it or stare at it)
- Treatment-resistant anxiety, especially social anxiety, or depression
- Social avoidance or being housebound
- Unnecessary surgery, dermatologic treatment, or other nonpsychiatric treatment (e.g., electrolysis)
Guidelines for treating BDD
- Establish trust. It is important to convey that you take the patient’s appearance concerns seriously. Many patients with BDD fear being considered silly or vain and do not divulge their symptoms. It is usually best to avoid reassuring patients that they look fine, since they usually do not believe the reassurance and can interpret it as trivializing their concerns.
- Provide psychoeducation. Explain to patients that they have a relatively common and treatable body image disorder. To decrease the patient’s reluctance to accept the diagnosis and treatment, it can be helpful to emphasize the excessive preoccupation, distress, and other problems their symptoms are causing. Discussions about whether the defect is “real” are usually fruitless, unless the patient already has good insight, which is rare. Several educational books and Web sites for patients are available. See Related Resources.
- Target BDD symptoms in treatment. Ignoring BDD symptoms and focusing treatment on other symptoms only may be unsuccessful because effective treatment for BDD differs in some important ways from that of most other psychiatric disorders, such as depression.10 It appears, for example, that non-selective serotonin reuptake inhibitor (SSRI) antidepressants are generally ineffective for BDD, unless used at higher SSRI doses than are often needed for depression. BDD symptoms also do not necessarily improve in concert with symptoms of other disorders, such as depression or OCD.10
- Avoid nonpsychiatric medical treatment. Although no one can predict how an individual patient will respond to nonpsychiatric treatment, (e.g., surgery or dermatologic treatment), explain that as best we know, such treatment usually appears to be ineffective for BDD and even can make the symptoms worse.11
Which psychopharmaceuticals should you consider?
Although BDD’s response to pharmacotherapy has received far less investigation than that of many other psychiatric disorders, research on this treatment approach has dramatically increased in recent years. The following strategies are suggested on the basis of evidence from controlled studies, open-label trials, and the author’s clinical experience (Figure 1):2,6,8,12-17
‘I’m as ugly as the elephant man’

Chris is a shy, anxious-appearing, 31-year-old man who was hospitalized after attempting suicide. He wears a baseball cap pulled down over his forehead and partially covering his eyes. It is difficult for him to reveal the reason for his suicide attempt: “It’s really hard to talk about this. I don’t know if I can. It’s too embarrassing.” Then he adds, “Well I guess I should tell you—after all, I’m in the hospital because of it. It’s my nose—these huge pock marks on my nose. They’re grotesque! I look like a monster. I’m as ugly as the elephant man!
“These marks on my nose are all I can think about. I’ve thought about them for hours a day every day for the past 15 years. I even have nightmares about them. And I think that everyone can see them and that they laugh at me because of them. That’s why I wear this hat all the time. And that’s why I couldn’t talk to you in a bright room. You’d notice the marks and see how ugly I am.” Chris actually appeared entirely normal, but no one could convince him of this.
“This has affected me in a lot of ways,” Chris adds. “This may be hard for you to believe, but this problem has ruined my life. All I can think about is my face, and I spend hours a day looking at the marks in the mirror. I just can’t resist. I thought I looked so ugly that I started missing more and more work, and I stopped going out with my friends and my girlfriend. I got so anxious when people looked at me that I started staying in the house most of the time. Sometimes when I did go out, I went through red lights so I wouldn’t have to sit at the light, where people might be staring at me. The hat helped a little, but it didn’t cover all the marks. I tried covering them with makeup for a while, but I thought people could see the makeup so that didn’t really help. The only time I really felt comfortable is when I wore my nephew’s Batman mask on Halloween—then no one could see the marks.
I finally missed so much work that I was fired. My girlfriend stuck it out with me for a long time, but finally she couldn’t take it any more. One thing that was really hard for her was that I started asking her about 50 times a day whether I looked OK and whether she could see the marks—I think that was the final straw. If I had a choice, I’d rather have cancer. It must be less painful. This is like an arrow through my heart.”
Chris had a notable, although only partial, response to fluoxetine 100 mg/d and buspirone 60 mg/d (higher doses of fluoxetine and buspirone were tried but were not more effective). Adding clonazepam was helpful for severe anxiety. Clomipramine, venlafaxine, lithium, mirtazapine, and various antipsychotics were sequentially added to this regimen, with minimal success, although a second trial of olanzapine, at a higher dose (15 mg/d) than he had been willing to try previously, further decreased Chris’ BDD and depressive symptoms. The addition of bupropion was somewhat helpful for depression but not for BDD.
Figure 1 Proposed pharmacotherapy for treating BDD
- Use an SSRI as a first-line approach. Other medications, including other antidepressants, appear less effective than SSRIs or clomipramine.2,8,9,13,15 An SSRI or clomipramine is also recommended for patients with delusional BDD (those who are completely convinced that they look abnormal and cannot be convinced otherwise), as Proposed pharmacotherapy for treating BDD these patients appear to respond to SSRIs as well as nondelusional patients do.12-17
- Use the maximum recommended or tolerated SSRI dose if lower doses are ineffective. Although no studies have compared different SSRI dosages, BDD appears to often require higher doses than those that are typically used for depression.
In a chart-review study of 90 patients with BDD treated in the author’s clinical practice, the mean SSRI doses used were fluoxetine 66.7 ±23.5 mg/d, fluvoxamine 308.3 ±49.2 mg/d, paroxetine 55.0 ± 12.9 mg/d, sertraline 202.1 ± 45.8 mg/d, and clomipramine 203.3 ±52.5 mg/d.17 Some patients respond only to doses higher than the maximum recommended dose (for example, 80-100 mg/d of citalopram or paroxetine).
- Treat for 12 to 16 weeks with an SSRI before concluding that the medication is ineffective. The average time to response is between 6 to 9 weeks.12,14,16 Clinical experience suggests that with continued treatment, relapse is rare and many patients further improve.
- Try sequential SSRIs if the first or second one does not work. A substantial percentage of patients who fail an initial SSRI trial will respond to a subsequent SSRI.17
- Continue an effective SSRI for at least 1 year before discontinuing it, as relapse appears likely with discontinuation.17 Severely ill patients may require treatment for life.
- Several SSRI augmentation and combination strategies might be helpful (Figure 1).16,17 If clomipramine is used in combination with an SSRI, the clomipramine level should be monitored.
What is the role of psychotherapy?
Although research on psychotherapy for BDD is limited, findings from clinical series and studies using waiting-list controls indicate that cognitive-behavioral therapy (CBT) is often effective.18-20 In contrast, supportive psychotherapy and insight-oriented and psychodynamic psychotherapy alone appear to be ineffective.9 CBT usually consists of a cognitive element (e.g., changing distorted views of the appearance “flaw”), exposure to feared and avoided situations (often social), and response prevention, avoiding repetitive behaviors such as excessive grooming.
- Consider using CBT as a first-line approach for milder BDD without significant comorbidity requiring pharmacotherapy.
- Use more intensive CBT treatment including frequent sessions and use of homework rather than less intensive treatment, although the optimal number and frequency of sessions is unknown.
- Consider maintenance and booster sessions for patients with more severe BDD following treatment to prevent relapse.
- Consider combining CBT and an SSRI. Although it is not known whether a combination of these treatments is more effective than either one alone, they are compatible and their combination may benefit certain patients. For patients with severe BDD, especially very depressed or suicidal patients, it is probably best to use CBT in combination with medication only, as sicker patients may not be able to tolerate or participate in CBT without first experiencing some improvement with medication.
- Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
- Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
- Phillips KA, Van Noppen B, Shapiro L. Learning to Live with Body Dysmorphic Disorder. Milford, Conn: Obsessive-Compulsive Foundation, 1997.
- Body Dysmorphic Disorder (BDD)and Body Image Program Homepage at Butler Hospital (Providence, RI). http://www.bodyimageprogram.com
Drug brand names
- Bupropion • Wellbutrin, Zyban
- Buspirone • Buspar
- Citalopram • Celexa
- Clomipramine • Anafranil
- Clonazepam • Ativan, Diastat, Halcion
- Fluoxetine • Prozac, Sarafem
- Fluvoxamine • Luvox
- Mirtazapine • Remeron, Remeron Solitab
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
The author reports that she receives grant support and occasional speaking honoraria from Eli Lilly and Co.; receives grant support from Forest Pharmaceuticals and Gate Pharmaceuticals; is on the speakers' bureau of Solvay Pharmaceuticals; and serves as a consultant for Wyeth-Ayerst Pharmaceuticals.
1. Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
2. Phillips KA. Body dysmorphic disorder. In: Phillips KA, ed. Somatoform and Factitious Disorders. Washington DC: American Psychiatric Publishing, 2001.
3. Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. Am J Psychiatry. 1991;148:1138-1149.
4. Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
5. Grant JE, et al. Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. J Clin Psychiatry. 2001;62:517-522.
6. Phillips KA. Body dysmorphic disorder: diagnostic controversies and treatment challenges. Bull Menninger Clin. 2000;64:18-35.
7. Hollander E, Cohen LJ, Simeon D. Body dysmorphic disorder. Psychiatric Annals. 1993;23:359-364.
8. Phillips KA, Castle DJ. Body dysmorphic disorder. In: Castle DJ, Phillips KA, eds. Disorders of Body Image. Hampshire, England: Wrightson Biomedical, in press.
9. Phillips KA, McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry. 1993;150:302-308.
10. Phillips KA: Body dysmorphic disorder and depression: theoretical considerations and treatment strategies. Psychiatry Quart. 1999;70:313-331.
11. Phillips KA, Grant JD, Siniscalchi J, Albertini RS. Surgical and nonpsychiatric medical treatment of patients with body dysmorphic disorder. Psychosomatics, in press.
12. Phillips KA, Dwight MM, McElroy SL. Efficacy and safety of fluvoxamine in body dysmorphic disorder. J Clin Psychiatry. 1998;59:165-171.
13. Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, Simeon D. Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch Gen Psychiatry. 1999;56:1033-1039.
14. Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry, in press.
15. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: review of the evidence and a recommended treatment approach. CNS Spectrums, in press.
16. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: a review of empirical data and a proposed treatment algorithm. Psychiatric Clin North Am. 2000;7:59-82.
17. Phillips KA, Albertini RS, Siniscalchi J, Khan A, Robinson M. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. J Clin Psychiatry. 2001;721-727.
18. Neziroglu FA, Yaryura-Tobias JA. Exposure, response prevention, and cognitive therapy in the treatment of body dysmorphic disorder. Behav Ther. 1993;24:431-438.
19. Veale D, Gournay K, Dryden W, Boocock A, Shah F, Willson R, Walburn J. Body dysmorphic disorder: a cognitive behavioural model and pilot randomized controlled trial. Behav Res Therapeut. 1996;34:717-729.
20. Wilhelm S, Otto MW, Lohr B, Deckersback T. Cognitive behavior group therapy for body dysmorphic disorder: a case series. Behav Res Ther. 1999;37:71-75.
1. Pope HG, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY: The Free Press, 2000.
2. Phillips KA. Body dysmorphic disorder. In: Phillips KA, ed. Somatoform and Factitious Disorders. Washington DC: American Psychiatric Publishing, 2001.
3. Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. Am J Psychiatry. 1991;148:1138-1149.
4. Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York, NY: Oxford University Press, 1996.
5. Grant JE, et al. Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. J Clin Psychiatry. 2001;62:517-522.
6. Phillips KA. Body dysmorphic disorder: diagnostic controversies and treatment challenges. Bull Menninger Clin. 2000;64:18-35.
7. Hollander E, Cohen LJ, Simeon D. Body dysmorphic disorder. Psychiatric Annals. 1993;23:359-364.
8. Phillips KA, Castle DJ. Body dysmorphic disorder. In: Castle DJ, Phillips KA, eds. Disorders of Body Image. Hampshire, England: Wrightson Biomedical, in press.
9. Phillips KA, McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry. 1993;150:302-308.
10. Phillips KA: Body dysmorphic disorder and depression: theoretical considerations and treatment strategies. Psychiatry Quart. 1999;70:313-331.
11. Phillips KA, Grant JD, Siniscalchi J, Albertini RS. Surgical and nonpsychiatric medical treatment of patients with body dysmorphic disorder. Psychosomatics, in press.
12. Phillips KA, Dwight MM, McElroy SL. Efficacy and safety of fluvoxamine in body dysmorphic disorder. J Clin Psychiatry. 1998;59:165-171.
13. Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, Simeon D. Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch Gen Psychiatry. 1999;56:1033-1039.
14. Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry, in press.
15. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: review of the evidence and a recommended treatment approach. CNS Spectrums, in press.
16. Phillips KA. Pharmacologic treatment of body dysmorphic disorder: a review of empirical data and a proposed treatment algorithm. Psychiatric Clin North Am. 2000;7:59-82.
17. Phillips KA, Albertini RS, Siniscalchi J, Khan A, Robinson M. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. J Clin Psychiatry. 2001;721-727.
18. Neziroglu FA, Yaryura-Tobias JA. Exposure, response prevention, and cognitive therapy in the treatment of body dysmorphic disorder. Behav Ther. 1993;24:431-438.
19. Veale D, Gournay K, Dryden W, Boocock A, Shah F, Willson R, Walburn J. Body dysmorphic disorder: a cognitive behavioural model and pilot randomized controlled trial. Behav Res Therapeut. 1996;34:717-729.
20. Wilhelm S, Otto MW, Lohr B, Deckersback T. Cognitive behavior group therapy for body dysmorphic disorder: a case series. Behav Res Ther. 1999;37:71-75.






