User login
Liletta gets a new inserter: Steps for successful placement
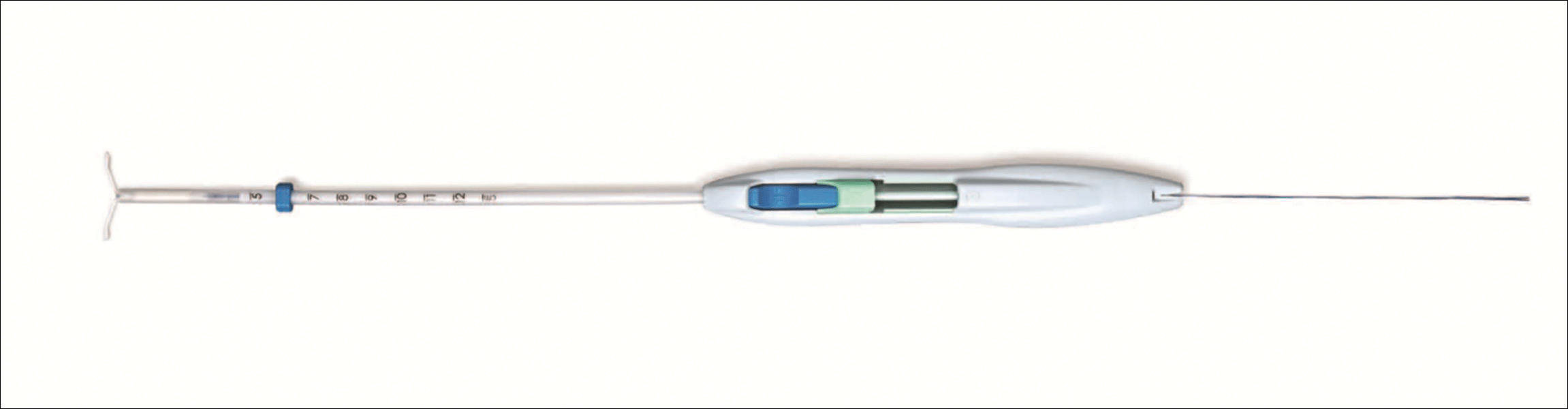
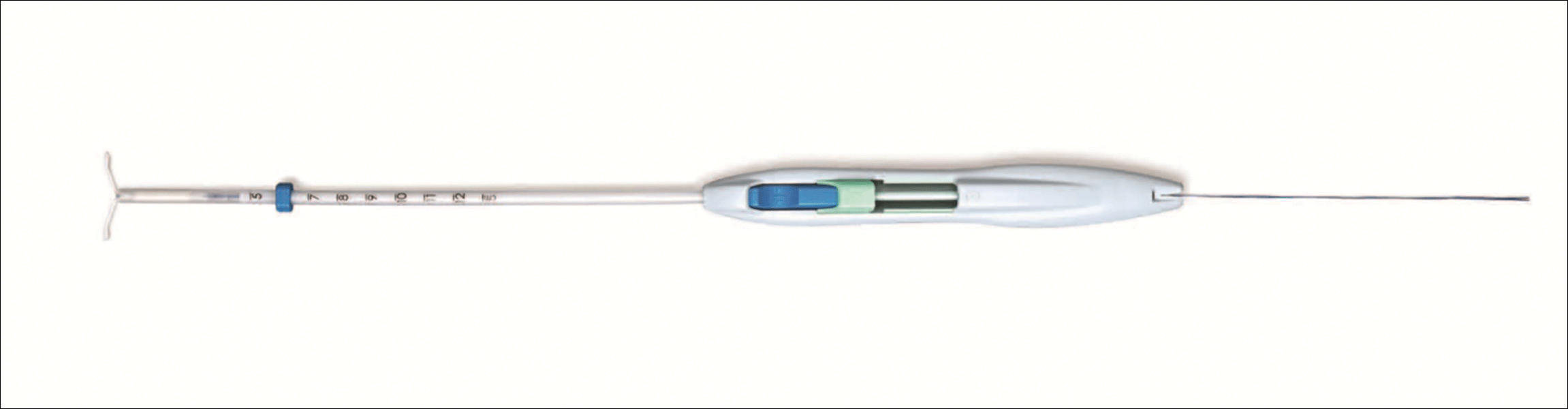
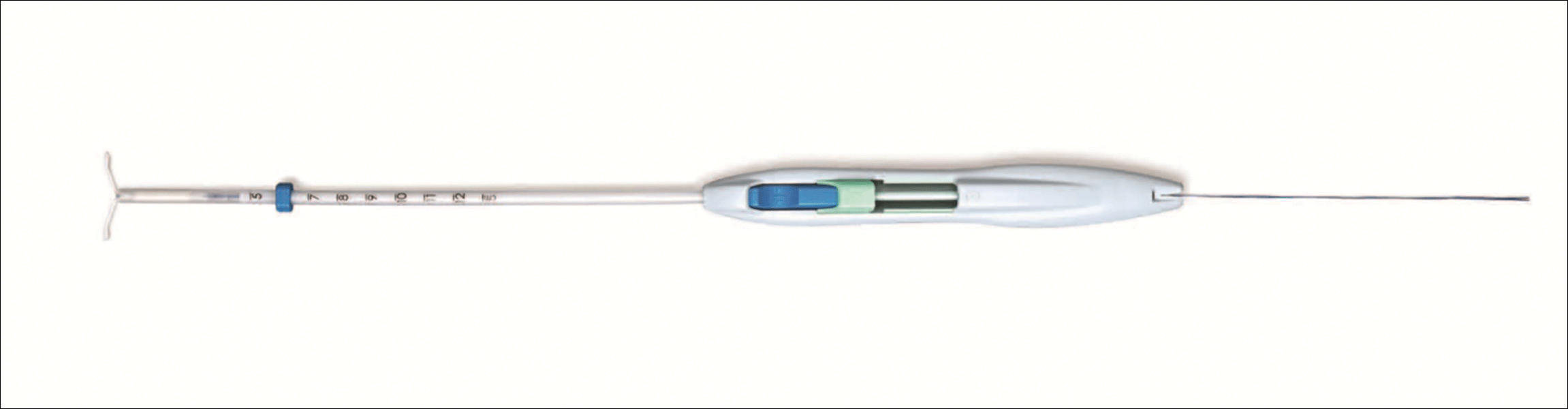
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
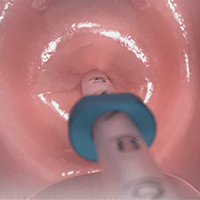
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
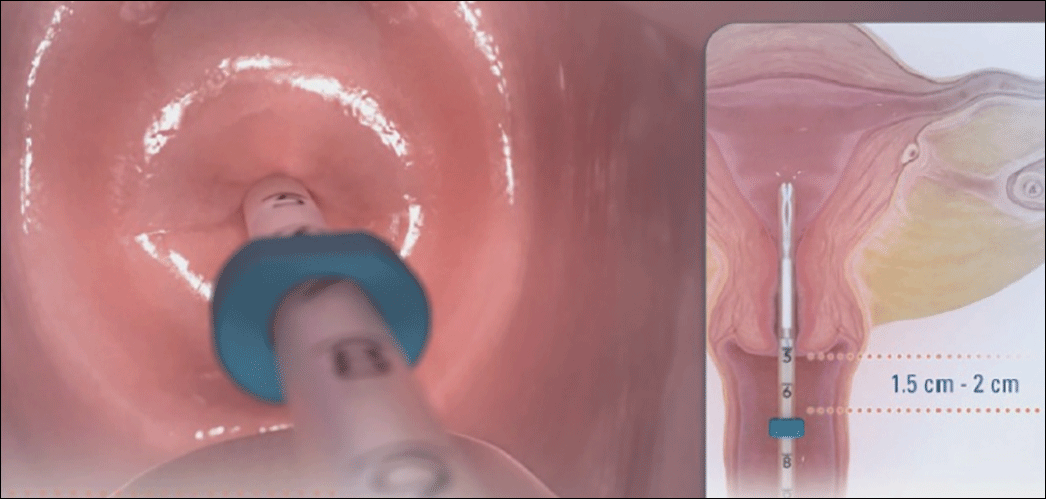 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 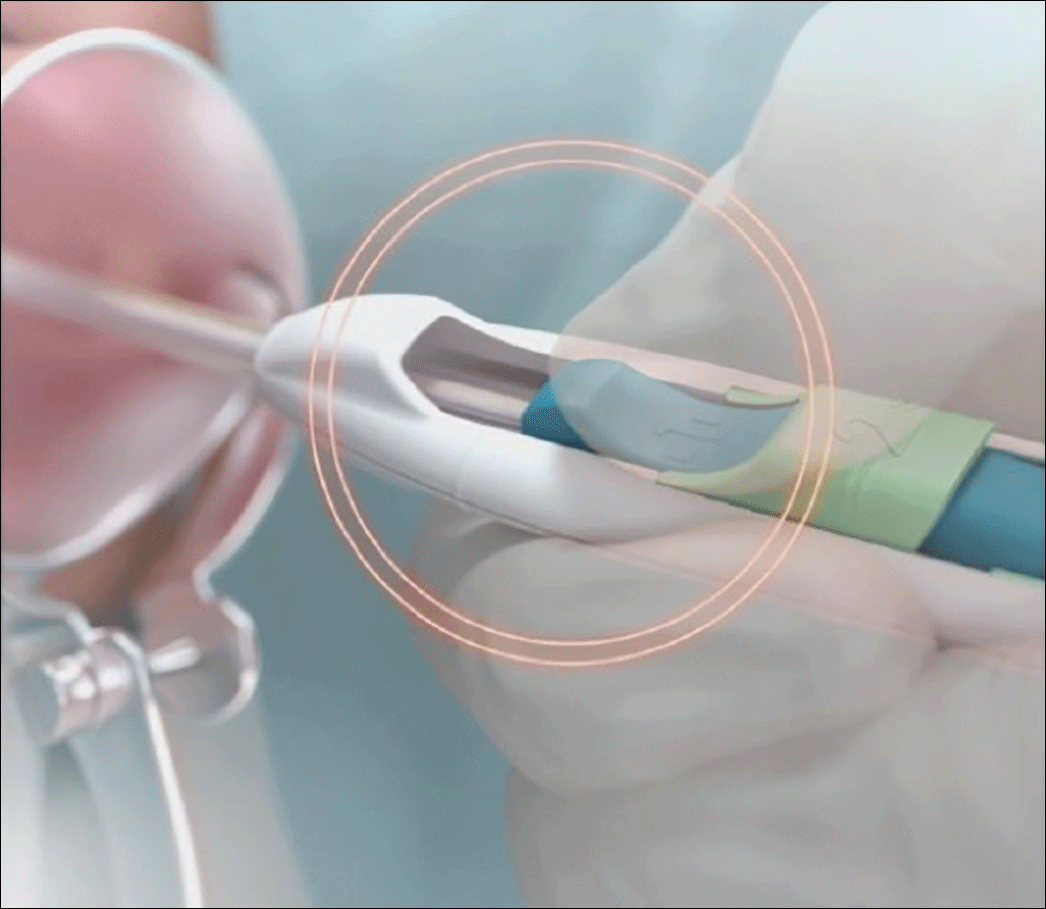 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
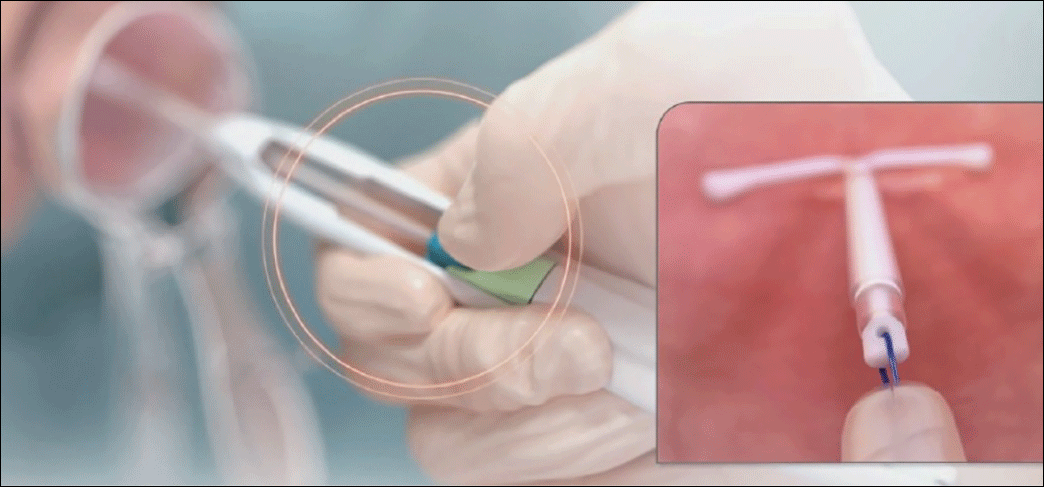 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
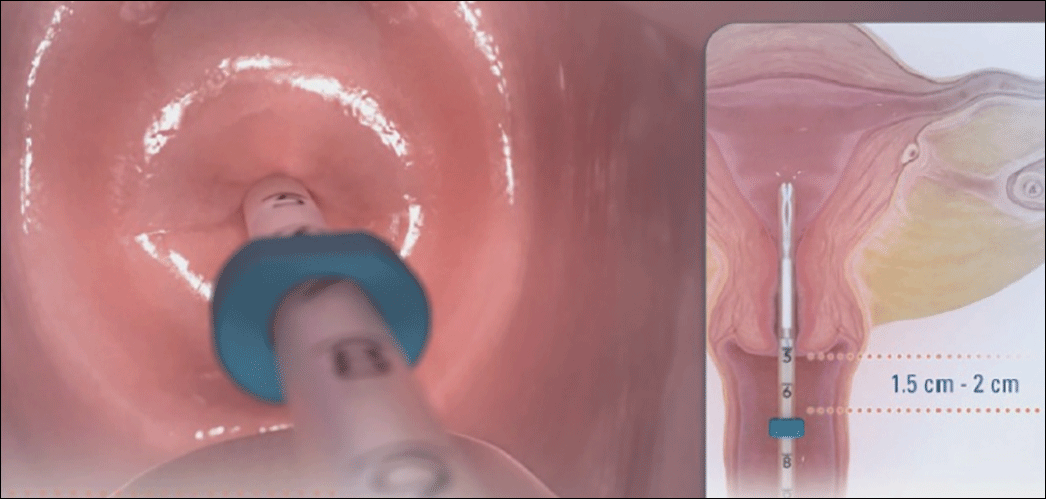 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 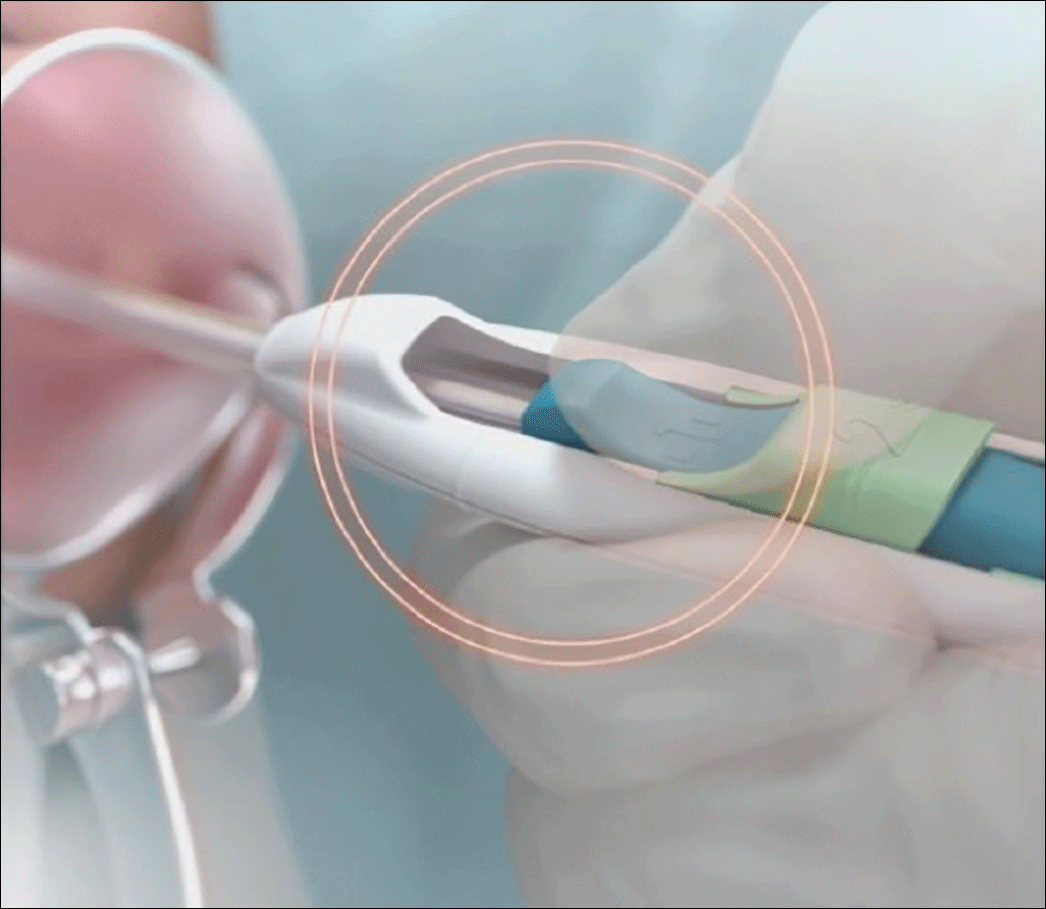 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
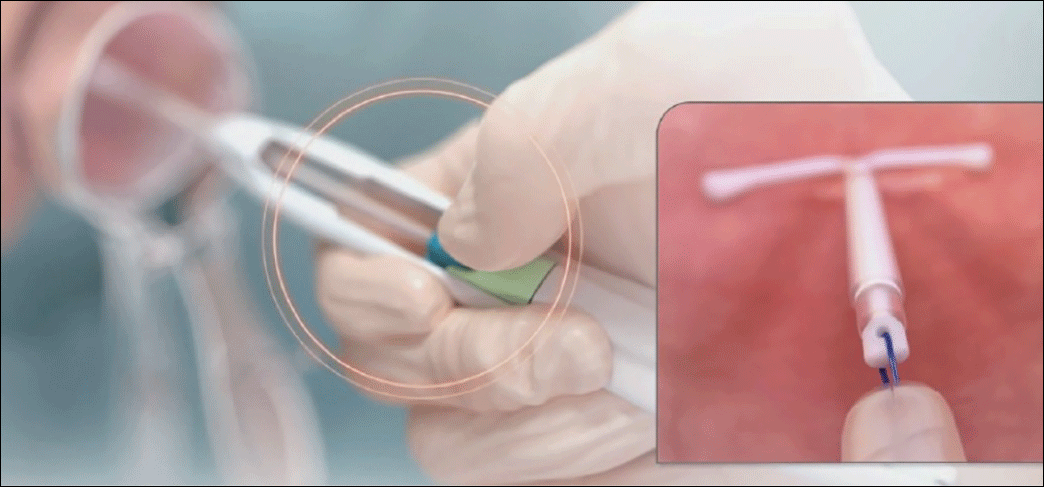 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A new single-handed inserter (SHI) for placement of Liletta has been introduced and is currently available (FIGURE 1). Liletta is a levonorgestrel 52-mg intrauterine system (IUS) that is currently approved for 3 years of use as a contraceptive in the United States. The same product in Europe, known as Levosert, is approved for both contraception and the treatment of heavy menstrual bleeding. Liletta, as a branded contraceptive, is being studied through a large Phase 3 clinical trial called ACCESS IUS, which will continue to evaluate the contraceptive efficacy of Liletta for at least 7 years of use.1 A recent publication from the study showed that the levonorgestrel release rates from Liletta are almost identical to the rates reported for the other levonorgestrel 52-mg IUS on the market (Mirena) through 5 years and supports the continued study of the IUS for at least 7 years.2
Related article:
Benefit of self-administered vaginal lidocaine gel in IUD placement
The initial marketing and distribution of Liletta used a two-handed inserter that allowed for successful placement but required multiple steps. The SHI will make loading and placement of Liletta easier for all clinicians. Features of the new SHI include:
- A double-slider mechanism in which the first slider moves into the second slider during IUS placement, providing a tactile sense for the user during the insertion process
- The ability to reload the inserter if needed before placement
- A firm but bendable tube (that is 2 cm longer than other IUS inserters on the market). This length can be helpful for obese patients or postprocedure placements.
- Depth markings to 12 cm on both sides of the insertion tube.
Related article:
2016 Update on contraception
Liletta is an important and unique product in the US market. For most public sector providers and clinics, Liletta costs only $50, significantly less than other long-acting reversible contraceptives. The price of the IUS is only one aspect of its overall cost, however, as women still need to pay for any office visit or insertion fees. Liletta is unique in its pricing. Sales of Liletta in the private sector support the low price in the public sector. As a health care community, even if we do not directly care for women in public-sector settings, we all can help poor women access affordable, effective contraception. For providers, Liletta is a highly effective and lower-cost alternative to currently available hormonal IUS products.
How to insert Liletta
Insertion can be performed using a no-touch technique. The loading and placement technique outlined below should occur after speculum and tenaculum placement, sounding of the uterus, and vaginal preparation as would be performed for any intrauterine contraceptive insertion. Never force the uterine sound or insertion tube through the cervix; if necessary, stop and dilate the cervical canal. The steps below are the main points for successful Liletta placement; see the full product label for more details.3
Related article:
In which clinical situations can the use of the 52-mg levonorgestrel-releasing IUD (Mirena) and the TCu380A copper-IUD (ParaGard) be extended?
The key steps to remember are firm-gentle-firm
- Load the device. While pushing forward firmly on the blue slider (with the number 1), load Liletta by pulling down evenly on the threads. The IUS should be laid on a flat surface in the sterile tray to keep the arms parallel to the floor while pulling on the threads. Once loaded, the threads can be pulled up or down to be locked in the cleft. The tip of the IUS will form a hemispheric dome at the top of the insertion tube.
- Adjust the flange to the measured uterine depth based on sounding using the notch in the tray.
- Place inserter into the cervix. Apply gentle traction on the tenaculum to align the cervical canal and uterine cavity. While still holding firm forward pressure on the blue slider, place the tube through the cervical canal until the flange is approximately 1.5 to 2 cm from the cervix. (FIGURE 2.) Gently slide the blue slider downward until it is flush with the green slider (with the number 2; FIGURE 3). This step will allow the IUS arms to open in the lower uterine segment; wait 10 to 15 seconds for the arms to fully unfold. By sliding gently, you will feel when to stop moving the slider.
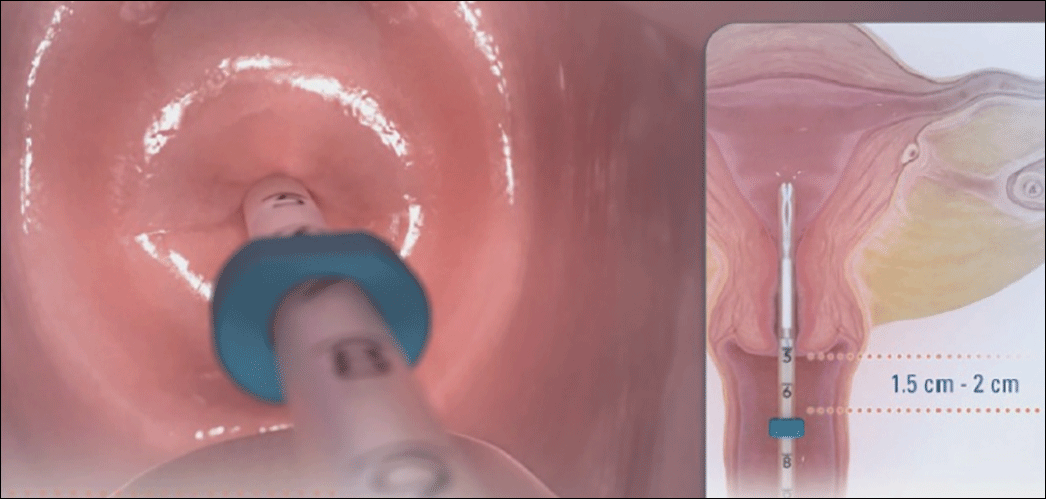 Image copyright Medicines360.
Image copyright Medicines360.Figure 2. Placing the inserter through the cervix 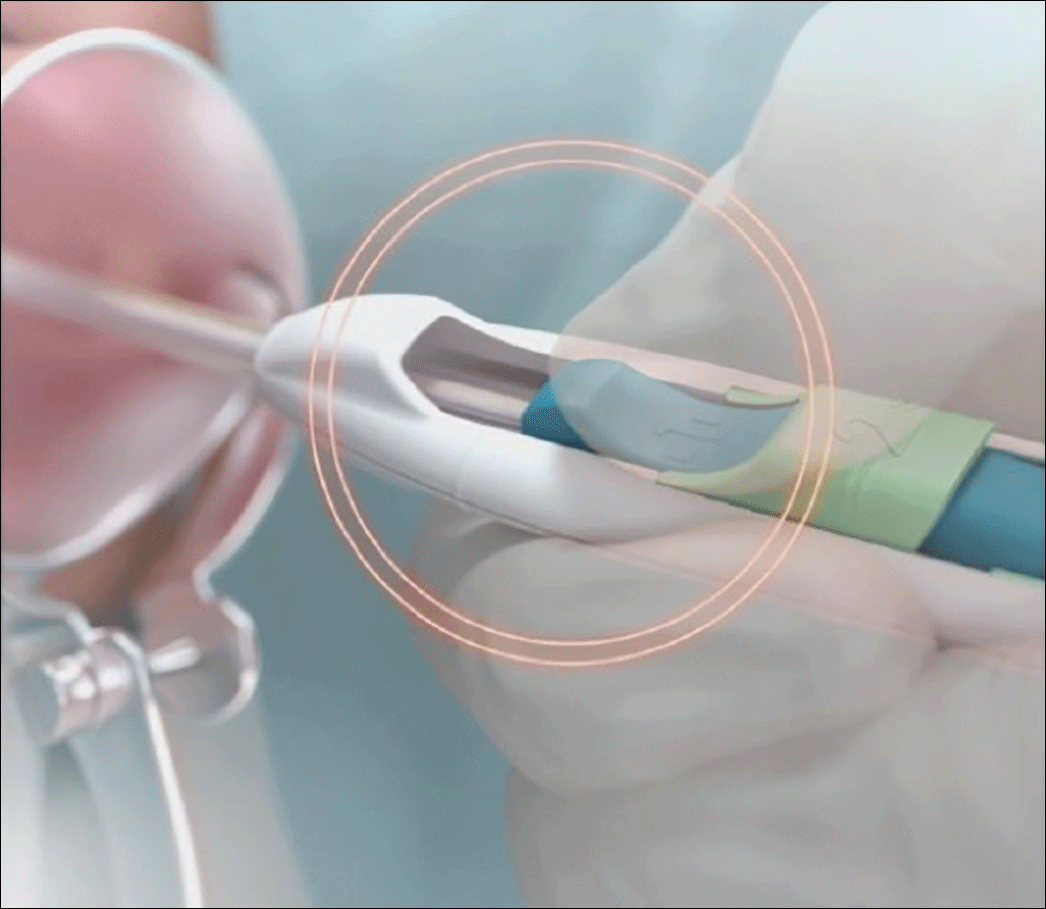 Image copyright Medicines360.
Image copyright Medicines360.Figure 3. Merging the blue and green sliders together to release the IUS arms - Advance the inserter. While holding traction on the tenaculum, advance the inserter to the fundus. You will feel slight resistance when the IUS is at the fundus and the flange should be flush against the cervix.
- Firmly slide both sliders together downward until a click is heard (FIGURE 4). A green indicator will be visible at the bottom of the handle to show that the threads have been ejected from the cleft.
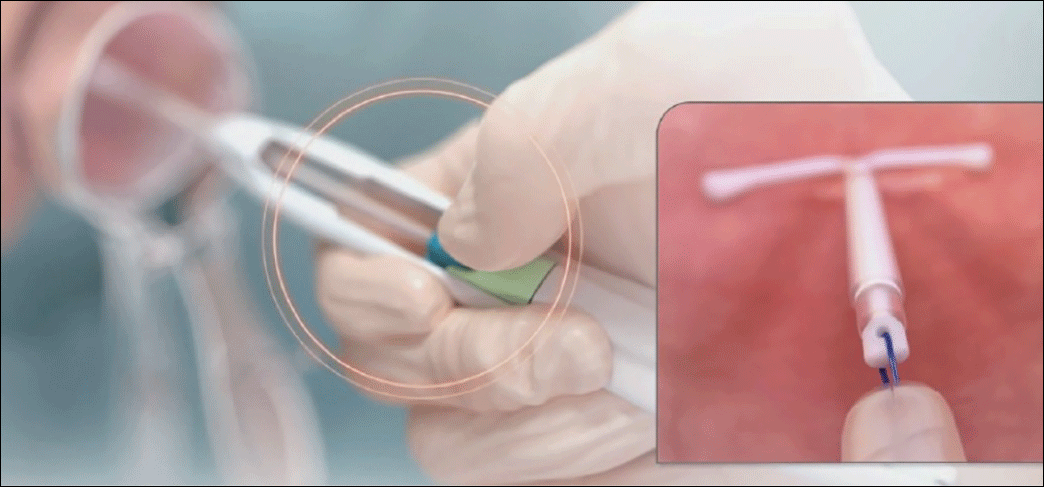 Image copyright Medicines360.
Image copyright Medicines360.Figure 4. Moving the blue and green sliders downward together to release the IUS - Withdraw the inserter from the uterus and cut the threads with blunt tipped scissors approximately 3 cm from the cervical os.
Technique video
Allergan and Medicines360 offer a video demonstrating proper Liletta insertion technique at www.lilettahcp.com. The video includes proper loading of the inserter as well as correct uterine depth measurement and release of Liletta from the inserter. Clinicians are reminded to use aseptic technique during the entire insertion procedure.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
- Eisenberg DL, Schreiber CA, Turok DK, Teal SB, Westhoff CL, Creinin MD. Three year efficacy and safety of a new 52-mg levonorgestrel-releasing intrauterine system. Contraception. 2015;92(1):10-16.
- Creinin MD, Jansen R, Starr R, Gobburu J, Gopalakrishnan M, Olariu A. Levonorgestrel release rates over 5 years with the Liletta® 52 mg intrauterine system. Contraception. 2016;94(4):353-356.
- Liletta [package insert]. Irvine, California: Allergan USA, Inc., and San Francisco, California: Medicines360; 2016.
In this article
Does one particular cesarean technique confer better maternal and neonatal outcomes?
EXPERT COMMENTARY
John M. Thorp Jr, MD, McAllister Distinguished Professor, Division Director, General Obstetrics and Gynecology, Vice Chair of Research, Department of Ob-Gyn, University of North Carolina Schools of Medicine and Public Health, Chapel Hill.
Five years ago one of our interns operating with the director of labor and delivery challenged him as to why we were not using evidenced-based surgical techniques for cesarean delivery. Bruised by the formidable (and at times misleading) club of “evidence-based medicine” that is held as sacrosanct by the modern obstetrician, the director responded to the charge by researching a systematic review on abdominal delivery that amalgamated studies of poor quality with precious few trials. He unilaterally decided that we needed an opening in the transparent portion of the drape overlying the incision site so that we might use “evidence” to prevent operative site infection. The end result: No change in the incidence of wound infections, and adhesive drapes that did not adhere well, thereby displacing the effluent of amniotic fluid and blood that are part of a cesarean delivery back into the first assistant’s socks, shoes, and clothing. It was as if the clock had been turned back to my early years as an attending when we had cloth drapes. So much for having an evidence-based protocol. I was thus elated at reading the results of the CORONIS trial.
Details of the study
The CORONIS trial, in which investigators randomly assigned almost 16,000 women from 7 countries (Argentina, Chile, Ghana, India, Kenya, Pakistan, and Sudan), used a sophisticated factorial design and followed up 13,153 (84%) of the women for 3 years. The investigators tested an array of technical questions about 5 intervention pairs used during abdominal delivery and reported the main outcomes of interest for each intervention, including:
- blunt versus sharp abdominal entry—no evidence of a difference in risk of abdominal hernias (adjusted risk ratio [RR], 0.66; 95% confidence interval [CI], 0.39–1.11)
- exteriorization of the uterus versus intra-abdominal repair—no evidence of a difference in risk of infertility (RR, 0.91; 95% CI, 0.71–1.18) or of ectopic pregnancy (RR, 0.50; CI, 0.15–1.66)
- single- versus double-layer closure of the uterus—no evidence of a difference in maternal death (RR, 0.78; 95% CI, 0.46–1.32) or a composite of pregnancy complications (RR, 1.20; 95% CI, 0.75–1.90)
- closure versus nonclosure of the peritoneum—no evidence of a difference in any outcomes relating to symptoms associated with pelvic adhesions, such as infertility (RR, 0.8; 95% CI, 0.61–1.06)
- chromic catgut versus polyglactin-910 sutures—no evidence of a difference in the main comparisons for adverse pregnancy outcomes in a subsequent pregnancy, such as uterine rupture (RR, 3.05; 95% CI, 0.32–29.29).
Strengths and limitations. The CORONIS trial included a large number of participants and had comprehensive follow-up, a rigorous data collection process, and the participation of many countries. The trial’s participating centers, however, were mostly large referral hospitals with high research interest; adverse outcomes might have been higher in other settings. As well, a lower incidence of subsequent pregnancy among participants limited the study’s power to detect differences in outcomes between the intervention pairs.
Conclusions. None of the alternative techniques produced any real benefits despite syntheses-suggested benefit reported in systematic reviews. Surgeon preference for cesarean delivery techniques likely will continue to guide clinical practice along with economic and institution factors.
A word to the wise: Evidence is not created equally, and pushing it into lumps does not increase its value.
--John M. Thorp Jr, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
John M. Thorp Jr, MD, McAllister Distinguished Professor, Division Director, General Obstetrics and Gynecology, Vice Chair of Research, Department of Ob-Gyn, University of North Carolina Schools of Medicine and Public Health, Chapel Hill.
Five years ago one of our interns operating with the director of labor and delivery challenged him as to why we were not using evidenced-based surgical techniques for cesarean delivery. Bruised by the formidable (and at times misleading) club of “evidence-based medicine” that is held as sacrosanct by the modern obstetrician, the director responded to the charge by researching a systematic review on abdominal delivery that amalgamated studies of poor quality with precious few trials. He unilaterally decided that we needed an opening in the transparent portion of the drape overlying the incision site so that we might use “evidence” to prevent operative site infection. The end result: No change in the incidence of wound infections, and adhesive drapes that did not adhere well, thereby displacing the effluent of amniotic fluid and blood that are part of a cesarean delivery back into the first assistant’s socks, shoes, and clothing. It was as if the clock had been turned back to my early years as an attending when we had cloth drapes. So much for having an evidence-based protocol. I was thus elated at reading the results of the CORONIS trial.
Details of the study
The CORONIS trial, in which investigators randomly assigned almost 16,000 women from 7 countries (Argentina, Chile, Ghana, India, Kenya, Pakistan, and Sudan), used a sophisticated factorial design and followed up 13,153 (84%) of the women for 3 years. The investigators tested an array of technical questions about 5 intervention pairs used during abdominal delivery and reported the main outcomes of interest for each intervention, including:
- blunt versus sharp abdominal entry—no evidence of a difference in risk of abdominal hernias (adjusted risk ratio [RR], 0.66; 95% confidence interval [CI], 0.39–1.11)
- exteriorization of the uterus versus intra-abdominal repair—no evidence of a difference in risk of infertility (RR, 0.91; 95% CI, 0.71–1.18) or of ectopic pregnancy (RR, 0.50; CI, 0.15–1.66)
- single- versus double-layer closure of the uterus—no evidence of a difference in maternal death (RR, 0.78; 95% CI, 0.46–1.32) or a composite of pregnancy complications (RR, 1.20; 95% CI, 0.75–1.90)
- closure versus nonclosure of the peritoneum—no evidence of a difference in any outcomes relating to symptoms associated with pelvic adhesions, such as infertility (RR, 0.8; 95% CI, 0.61–1.06)
- chromic catgut versus polyglactin-910 sutures—no evidence of a difference in the main comparisons for adverse pregnancy outcomes in a subsequent pregnancy, such as uterine rupture (RR, 3.05; 95% CI, 0.32–29.29).
Strengths and limitations. The CORONIS trial included a large number of participants and had comprehensive follow-up, a rigorous data collection process, and the participation of many countries. The trial’s participating centers, however, were mostly large referral hospitals with high research interest; adverse outcomes might have been higher in other settings. As well, a lower incidence of subsequent pregnancy among participants limited the study’s power to detect differences in outcomes between the intervention pairs.
Conclusions. None of the alternative techniques produced any real benefits despite syntheses-suggested benefit reported in systematic reviews. Surgeon preference for cesarean delivery techniques likely will continue to guide clinical practice along with economic and institution factors.
A word to the wise: Evidence is not created equally, and pushing it into lumps does not increase its value.
--John M. Thorp Jr, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
John M. Thorp Jr, MD, McAllister Distinguished Professor, Division Director, General Obstetrics and Gynecology, Vice Chair of Research, Department of Ob-Gyn, University of North Carolina Schools of Medicine and Public Health, Chapel Hill.
Five years ago one of our interns operating with the director of labor and delivery challenged him as to why we were not using evidenced-based surgical techniques for cesarean delivery. Bruised by the formidable (and at times misleading) club of “evidence-based medicine” that is held as sacrosanct by the modern obstetrician, the director responded to the charge by researching a systematic review on abdominal delivery that amalgamated studies of poor quality with precious few trials. He unilaterally decided that we needed an opening in the transparent portion of the drape overlying the incision site so that we might use “evidence” to prevent operative site infection. The end result: No change in the incidence of wound infections, and adhesive drapes that did not adhere well, thereby displacing the effluent of amniotic fluid and blood that are part of a cesarean delivery back into the first assistant’s socks, shoes, and clothing. It was as if the clock had been turned back to my early years as an attending when we had cloth drapes. So much for having an evidence-based protocol. I was thus elated at reading the results of the CORONIS trial.
Details of the study
The CORONIS trial, in which investigators randomly assigned almost 16,000 women from 7 countries (Argentina, Chile, Ghana, India, Kenya, Pakistan, and Sudan), used a sophisticated factorial design and followed up 13,153 (84%) of the women for 3 years. The investigators tested an array of technical questions about 5 intervention pairs used during abdominal delivery and reported the main outcomes of interest for each intervention, including:
- blunt versus sharp abdominal entry—no evidence of a difference in risk of abdominal hernias (adjusted risk ratio [RR], 0.66; 95% confidence interval [CI], 0.39–1.11)
- exteriorization of the uterus versus intra-abdominal repair—no evidence of a difference in risk of infertility (RR, 0.91; 95% CI, 0.71–1.18) or of ectopic pregnancy (RR, 0.50; CI, 0.15–1.66)
- single- versus double-layer closure of the uterus—no evidence of a difference in maternal death (RR, 0.78; 95% CI, 0.46–1.32) or a composite of pregnancy complications (RR, 1.20; 95% CI, 0.75–1.90)
- closure versus nonclosure of the peritoneum—no evidence of a difference in any outcomes relating to symptoms associated with pelvic adhesions, such as infertility (RR, 0.8; 95% CI, 0.61–1.06)
- chromic catgut versus polyglactin-910 sutures—no evidence of a difference in the main comparisons for adverse pregnancy outcomes in a subsequent pregnancy, such as uterine rupture (RR, 3.05; 95% CI, 0.32–29.29).
Strengths and limitations. The CORONIS trial included a large number of participants and had comprehensive follow-up, a rigorous data collection process, and the participation of many countries. The trial’s participating centers, however, were mostly large referral hospitals with high research interest; adverse outcomes might have been higher in other settings. As well, a lower incidence of subsequent pregnancy among participants limited the study’s power to detect differences in outcomes between the intervention pairs.
Conclusions. None of the alternative techniques produced any real benefits despite syntheses-suggested benefit reported in systematic reviews. Surgeon preference for cesarean delivery techniques likely will continue to guide clinical practice along with economic and institution factors.
A word to the wise: Evidence is not created equally, and pushing it into lumps does not increase its value.
--John M. Thorp Jr, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Do you utilize vasopressin in your difficult cesarean delivery surgeries?
Vasopressin is often used to reduce blood loss in gynecologic surgery. Results of randomized clinical trials indicate that its use reduces blood loss in many gynecologic surgery procedures, including hysterectomy, myomectomy, cervical conization, and second trimester pregnancy termination.1−7 In contrast to the widespread use of dilute vasopressin injection in gynecology surgery, obstetricians in the United States seldom use vasopressin to reduce blood loss in difficult cesarean delivery surgery. Although there is very little direct evidence from clinical trials on the value of vasopressin in obstetric surgery, high-quality evidence from relevant gynecologic surgery and case reports from obstetricians support its use during difficult cesarean delivery surgery.
Biology of oxytocin and vasopressin
Oxytocin and vasopressin are fraternal twin nanopeptides that differ by only two amino acids and are secreted from the posterior pituitary. The human uterus contains both oxytocin and vasopressin receptors; stimulation of either receptor causes uterine contraction. Vasopressin receptor activation also causes vasoconstriction and platelet activation.
Given the similar biochemistry of oxytocin and vasopressin it is not surprising that each hormone is capable of binding to both oxytocin and vasopressin receptors. The affinity of oxytocin for the oxytocin and vasopressin receptors as expressed as an inhibition constant is 6.8 nM and 35 nM, respectively. Vasopressin’s affinity for the oxytocin and vasopressin V1a receptors is 48 nM and 1.4 nM, respectively.8
Administering vasopressin into the uterus will achieve a high concentration of the hormone, which stimulates both the oxytocin and vasopressin receptors, resulting in uterine contraction, vasoconstriction, and platelet activation. Of particular importance to obstetricians is that following a prolonged labor or administration of oxytocin, myometrial oxytocin receptors may be downregulated, but vasopressin receptors may remain functional.9,10
Vasopressin regulates plasma volume, blood pressure, osmolality, and uterine contractility. The vasopressin V1a receptor is present on vascular smooth muscle cells, platelets, and uterine myocytes. Activating this receptor causes vasoconstriction, platelet activation, and uterine contraction.
Vasopressin reduces surgical blood loss in two ways. The first major mechanism is through vasoconstriction.11 Second, in uterine surgery specifically, vasopressin stimulates uterine contraction. The hormone exerts its antidiuretic action through the V2 receptor in the kidney.
Optimal vasopressin dose
In gynecologic surgery, the vasopressin doses utilized to reduce blood loss range from 5 U to 20 U diluted in 20 mL to 200 mL of saline. Randomized trial results indicate that a vasopressin dose of 4 U is effective in reducing blood loss during second trimester pregnancy termination,7 and a dose of 3 U is effective in reducing blood loss during cervical conization.5,6 There is insufficient obstetric literature to determine the optimal dose of vasopressin to reduce blood loss in difficult cesarean delivery sur- gery, but doses similar to those used in gynecologic surgery should be considered.
Possible effects of vasopressin overdosing. In gynecologic surgery, injection of vasopressin has been reported to cause bradycardia, hypotension, myocardial infarction, and cardiovascular collapse.12 Given that multiple vasoactive medications may be given to a patient undergoing a complex cesarean delivery, including oxytocin, methergine, and ephedrine, it is important for the obstetrician to use the lowest effective dose of vasopressin necessary to facilitate control of blood loss. The obstetrician needs to communicate with the anesthesiologist and coordinate the use of dilute vasopressin with other vasoactive medications.
Avoid intravascular injection of vasopressin. I prefer to inject vasopressin in the subserosa of the uterus rather than to inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.
Vasopressin reduces blood loss during hysterectomy
One randomized trial has reported that the administration of 10 U of vasopressin diluted in saline into the lower uterine segment reduced blood loss at abdominal hysterectomy in nonpregnant women compared with an injection of saline alone (445 mL vs 748 mL of blood loss, respectively).1 There are no clinical trials of the use of vasopressin in cesarean hysterectomy. However, abdominal hysterectomy procedures and cesarean hysterectomy are similar, and vasopressin likely helps to reduce blood loss at cesarean hysterectomy.
Vasopressin reduces blood loss during myomectomy
Authors of 3 small, randomized clinical trials in nonpregnant women have reported that the intramyometrial injection of dilute vasopressin reduces blood loss during myomectomy surgery.2−4 The vasopressin doses in the 3 trials ranged from 5 U of vasopressin in 100 mL of saline to 20 U of vasopressin in 20 mL of saline. A Cochrane meta-analyis of the 3 studies concluded that, at myomectomy, the intramyometrial injection of dilute vasopressin was associated with a significant reduction in blood loss compared with placebo (246 mL vs 483 mL, respectively).13
There are great similarities between myomectomy in the nonpregnant and pregnant uterus. Given the clinical trials data that support the use of vasopressin to reduce blood loss during myomectomy in the nonpregnant uterus, it is likely that vasopressin also would reduce blood loss during myomectomy performed at the time of a cesarean delivery.
At cesarean delivery, elective myomectomy of intramural fibroids is generally not recommended because of the risk of massive blood loss. Clinicians often remove large pedunculated fibroids because this surgery does not usually cause massive bleeding. However, on occasion it may be necessary to perform a myomectomy on intramural myoma(s) in order to close a hysterotomy incision.
For myomectomy surgery performed at the time of cesarean delivery, many techniques have been utilized to reduce blood loss, including:
- intravenous oxytocin infusion14,15
- injection of oxytocin into the myoma pseudocapsule15
- electrosurgery16−18
- argon beam coagulator19
- uterine tourniquet20
- premyomectomy placement of a uterine U stitch21 or purse string suture22
- O’Leary sutures23,24
- temporary balloon occlusion of pelvic arteries25
- vasopressin injection.26
Given the widespread use of vasopressin injection in gynecologic surgery to reduce blood loss at myomectomy, obstetricians should consider using vasopressin in their cesarean myomectomy surgery.
Use of vasopressin during cesarean delivery for placenta previa may reduce blood loss
Women with a complete placenta previa require a cesarean delivery to safely birth their baby. Cesarean deliveries performed for this indication are associated with an increased risk of hemorrhage. In one case series of 59 patients with placenta previa undergoing cesarean delivery, 4 U of vasopressin diluted in 20 mL of saline was injected into the placental implantation site to reduce blood loss. Among the patients receiving vasopressin in- jection, the blood loss was 1,149 mL. Among 50 women with placenta previa who did not receive vasopressin injection, the blood loss was 1,634 mL.27
Obstetric surgery and vasopressin: The time has come
As obstetricians and gynecologists we constantly strive to improve the effectiveness of our surgical procedures and reduce adverse outcomes, including infection and blood loss. The use of vasopressin is widely accepted in gynecologic surgery as an adjuvant that reduces blood loss. The time has come to expand the use of vasopressin in difficult obstetric surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Okin CR, Guido RS, Meyn LA, Ramanathan S. Vasopressin during abdominal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2001;97:867–872.
- Frederick J, Fletcher H, Simeon D, Mullings A, Hardie M. Intramyometrial vasopressin as a haemostatic agent during myomectomy. Brit J Obstet Gynaecol. 1994;101:435–437.
- Assaf A. Adhesions after laparoscopic myomectomy effect of the technique used. Gynaecol Endosc. 1999;8(4):225–229.
- Zhao F, Jiao Y, Guo Z, Hou R, Wang M. Evaluation of loop ligation of larger myoma pseudocapsule combined with vasopressin on laparoscopic myomectomy. Fertil Steril. 2011;95(2):762–766.
- Sabol ED, Gibson JL, Bowes WA Jr. Vasopressin injection in cervical conization. A double-blind study. Obstet Gynecol. 1971;37(4):596–601.
- Martin-Hirsch PP, Keep SL, Bryant A. Interventions for preventing blood loss during the treatment of cervical intraepithelial neoplasia. Cochrane Database Syst Rev. 2010;(6):CD001421.
- Schulz KE, Grimes DA, Christensen DD. Vasopressin reduces blood loss from second trimester dilatation and evacuation abortion. Lancet. 1985;2(8451):353–356.
- Akerlund M, Bossmar T, Brouard R, et al. Receptor binding of oxytocin and vasopressin antagonists and inhibitory effects in isolated myometrium from preterm and term pregnant women. Br J Obstet Gynaecol. 1999;106(10):1047–1053.
- Akerlund M. Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog Brain Res. 2002;139:359–365.
- Helmer H, Hacki T, Schneeberger C, et al. Oxytocinand vasopressin 1a receptor gene expression in the cycling or pregnant human uterus. Am J Obstet Gynecol. 1998;179(6 pt 1):1572–1578.
- Wing DA, Goharkhay N, Felix JC, Rostamkhani M, Naidu YM, Kovacs BW. Expression of the oxytocin and V1a vasopressin receptors in human myometrium during differing physiological states and following misoprostol administration. Gynecol Obstet Invest. 2006;62(4):181–185.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014; (8):CD005355.
- Tinelli A, Malvasi A, Mynbaev OA, et al. The surgical outcome of intracapsular cesarean myomectomy. A match control study. J Matern Fetal Neonatal Med. 2014;27(1):66–71.
- Brown D, Fletcher HM, Myrie MO, Reid M. Caesarean myomectomy—a safe procedure. A retrospective case controlled study. J Obstet Gynaecol. 1999;19(2):139–141.
- Kaymak O, Ustunyrt E, Okyay RE, Kalyoncu S, Mollamahmutoglu L. Myomectomy during cesarean section. Int J Gynaecol Obstet. 2005;89(2):90–93.
- Park BJ, Kim YW. Safety of cesarean myomectomy. J Obstet Gynaecol Res. 2009;35(5):906–911.
- Kim YS, Choi SD, Bae DH. Risk factors for complications in patients undergoing myomectomy at the time of cesarean section. J Obstet Gynaecol Res. 2010;36(3):550–554.
- Ortac F, Gungor M, Sonmezer M. Myomectomy during cesarean section. Int J Gynecol Obstet. 1999;67(3):189–190.
- Incebiyik A, Hilali NG, Camuzcuoglu A, Vural M, Camuzcuoglu H. Myomectomy during caesarean: a retrospective evaluation of 6 cases. Arch Gynecol Obstet. 2014;289(3):569–573.
- Cobellis L, Pecori E, Cobellis G. Hemostatic technique for myomectomy during cesarean section. Int J Gynaecol Obstet. 2002;79(3):261–262.
- Lee JH, Cho DH. Myomectomy using purse-string suture during cesarean section. Arch Gynecol Obstet. 2011;283(suppl 1):S35–S37.
- Desai BR, Patted SS, Pujar YV, Sheriqar BY, Das SR, Ruge JC. A novel technique of selective uterine devascularization before myomectomy at the time of cesarean section: a pilot study. Fertil Steril. 2010;94(1):362–364.
- Sapmaz E, Celik H, Altungul A. Bilateral ascending uterine artery ligation vs. tourniquet use for hemostasis in cesarean myomectomy. A comparison. J Reprod Med. 2003;48(12):950–954.
- Sparic R, Malvasi A, Kadija S, Babovic I, Nejkovic L, Tinelli A. Cesarean myomectomy trends and controveries: an appraisal [published online ahead of print July 17, 2016]. J Matern Fetal Neonatal Med. doi:10.1080/14767058.2016.1205024.
- Lin JY, Lee WL, Wang PH, et al. Uterine artery occlusion and myomectomy for treatment of pregnant women with uterine leiomyomas who are undergoing cesarean section. J Obstet Gynaecol Res. 2010;36(2):284–290.
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
Vasopressin is often used to reduce blood loss in gynecologic surgery. Results of randomized clinical trials indicate that its use reduces blood loss in many gynecologic surgery procedures, including hysterectomy, myomectomy, cervical conization, and second trimester pregnancy termination.1−7 In contrast to the widespread use of dilute vasopressin injection in gynecology surgery, obstetricians in the United States seldom use vasopressin to reduce blood loss in difficult cesarean delivery surgery. Although there is very little direct evidence from clinical trials on the value of vasopressin in obstetric surgery, high-quality evidence from relevant gynecologic surgery and case reports from obstetricians support its use during difficult cesarean delivery surgery.
Biology of oxytocin and vasopressin
Oxytocin and vasopressin are fraternal twin nanopeptides that differ by only two amino acids and are secreted from the posterior pituitary. The human uterus contains both oxytocin and vasopressin receptors; stimulation of either receptor causes uterine contraction. Vasopressin receptor activation also causes vasoconstriction and platelet activation.
Given the similar biochemistry of oxytocin and vasopressin it is not surprising that each hormone is capable of binding to both oxytocin and vasopressin receptors. The affinity of oxytocin for the oxytocin and vasopressin receptors as expressed as an inhibition constant is 6.8 nM and 35 nM, respectively. Vasopressin’s affinity for the oxytocin and vasopressin V1a receptors is 48 nM and 1.4 nM, respectively.8
Administering vasopressin into the uterus will achieve a high concentration of the hormone, which stimulates both the oxytocin and vasopressin receptors, resulting in uterine contraction, vasoconstriction, and platelet activation. Of particular importance to obstetricians is that following a prolonged labor or administration of oxytocin, myometrial oxytocin receptors may be downregulated, but vasopressin receptors may remain functional.9,10
Vasopressin regulates plasma volume, blood pressure, osmolality, and uterine contractility. The vasopressin V1a receptor is present on vascular smooth muscle cells, platelets, and uterine myocytes. Activating this receptor causes vasoconstriction, platelet activation, and uterine contraction.
Vasopressin reduces surgical blood loss in two ways. The first major mechanism is through vasoconstriction.11 Second, in uterine surgery specifically, vasopressin stimulates uterine contraction. The hormone exerts its antidiuretic action through the V2 receptor in the kidney.
Optimal vasopressin dose
In gynecologic surgery, the vasopressin doses utilized to reduce blood loss range from 5 U to 20 U diluted in 20 mL to 200 mL of saline. Randomized trial results indicate that a vasopressin dose of 4 U is effective in reducing blood loss during second trimester pregnancy termination,7 and a dose of 3 U is effective in reducing blood loss during cervical conization.5,6 There is insufficient obstetric literature to determine the optimal dose of vasopressin to reduce blood loss in difficult cesarean delivery sur- gery, but doses similar to those used in gynecologic surgery should be considered.
Possible effects of vasopressin overdosing. In gynecologic surgery, injection of vasopressin has been reported to cause bradycardia, hypotension, myocardial infarction, and cardiovascular collapse.12 Given that multiple vasoactive medications may be given to a patient undergoing a complex cesarean delivery, including oxytocin, methergine, and ephedrine, it is important for the obstetrician to use the lowest effective dose of vasopressin necessary to facilitate control of blood loss. The obstetrician needs to communicate with the anesthesiologist and coordinate the use of dilute vasopressin with other vasoactive medications.
Avoid intravascular injection of vasopressin. I prefer to inject vasopressin in the subserosa of the uterus rather than to inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.
Vasopressin reduces blood loss during hysterectomy
One randomized trial has reported that the administration of 10 U of vasopressin diluted in saline into the lower uterine segment reduced blood loss at abdominal hysterectomy in nonpregnant women compared with an injection of saline alone (445 mL vs 748 mL of blood loss, respectively).1 There are no clinical trials of the use of vasopressin in cesarean hysterectomy. However, abdominal hysterectomy procedures and cesarean hysterectomy are similar, and vasopressin likely helps to reduce blood loss at cesarean hysterectomy.
Vasopressin reduces blood loss during myomectomy
Authors of 3 small, randomized clinical trials in nonpregnant women have reported that the intramyometrial injection of dilute vasopressin reduces blood loss during myomectomy surgery.2−4 The vasopressin doses in the 3 trials ranged from 5 U of vasopressin in 100 mL of saline to 20 U of vasopressin in 20 mL of saline. A Cochrane meta-analyis of the 3 studies concluded that, at myomectomy, the intramyometrial injection of dilute vasopressin was associated with a significant reduction in blood loss compared with placebo (246 mL vs 483 mL, respectively).13
There are great similarities between myomectomy in the nonpregnant and pregnant uterus. Given the clinical trials data that support the use of vasopressin to reduce blood loss during myomectomy in the nonpregnant uterus, it is likely that vasopressin also would reduce blood loss during myomectomy performed at the time of a cesarean delivery.
At cesarean delivery, elective myomectomy of intramural fibroids is generally not recommended because of the risk of massive blood loss. Clinicians often remove large pedunculated fibroids because this surgery does not usually cause massive bleeding. However, on occasion it may be necessary to perform a myomectomy on intramural myoma(s) in order to close a hysterotomy incision.
For myomectomy surgery performed at the time of cesarean delivery, many techniques have been utilized to reduce blood loss, including:
- intravenous oxytocin infusion14,15
- injection of oxytocin into the myoma pseudocapsule15
- electrosurgery16−18
- argon beam coagulator19
- uterine tourniquet20
- premyomectomy placement of a uterine U stitch21 or purse string suture22
- O’Leary sutures23,24
- temporary balloon occlusion of pelvic arteries25
- vasopressin injection.26
Given the widespread use of vasopressin injection in gynecologic surgery to reduce blood loss at myomectomy, obstetricians should consider using vasopressin in their cesarean myomectomy surgery.
Use of vasopressin during cesarean delivery for placenta previa may reduce blood loss
Women with a complete placenta previa require a cesarean delivery to safely birth their baby. Cesarean deliveries performed for this indication are associated with an increased risk of hemorrhage. In one case series of 59 patients with placenta previa undergoing cesarean delivery, 4 U of vasopressin diluted in 20 mL of saline was injected into the placental implantation site to reduce blood loss. Among the patients receiving vasopressin in- jection, the blood loss was 1,149 mL. Among 50 women with placenta previa who did not receive vasopressin injection, the blood loss was 1,634 mL.27
Obstetric surgery and vasopressin: The time has come
As obstetricians and gynecologists we constantly strive to improve the effectiveness of our surgical procedures and reduce adverse outcomes, including infection and blood loss. The use of vasopressin is widely accepted in gynecologic surgery as an adjuvant that reduces blood loss. The time has come to expand the use of vasopressin in difficult obstetric surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Vasopressin is often used to reduce blood loss in gynecologic surgery. Results of randomized clinical trials indicate that its use reduces blood loss in many gynecologic surgery procedures, including hysterectomy, myomectomy, cervical conization, and second trimester pregnancy termination.1−7 In contrast to the widespread use of dilute vasopressin injection in gynecology surgery, obstetricians in the United States seldom use vasopressin to reduce blood loss in difficult cesarean delivery surgery. Although there is very little direct evidence from clinical trials on the value of vasopressin in obstetric surgery, high-quality evidence from relevant gynecologic surgery and case reports from obstetricians support its use during difficult cesarean delivery surgery.
Biology of oxytocin and vasopressin
Oxytocin and vasopressin are fraternal twin nanopeptides that differ by only two amino acids and are secreted from the posterior pituitary. The human uterus contains both oxytocin and vasopressin receptors; stimulation of either receptor causes uterine contraction. Vasopressin receptor activation also causes vasoconstriction and platelet activation.
Given the similar biochemistry of oxytocin and vasopressin it is not surprising that each hormone is capable of binding to both oxytocin and vasopressin receptors. The affinity of oxytocin for the oxytocin and vasopressin receptors as expressed as an inhibition constant is 6.8 nM and 35 nM, respectively. Vasopressin’s affinity for the oxytocin and vasopressin V1a receptors is 48 nM and 1.4 nM, respectively.8
Administering vasopressin into the uterus will achieve a high concentration of the hormone, which stimulates both the oxytocin and vasopressin receptors, resulting in uterine contraction, vasoconstriction, and platelet activation. Of particular importance to obstetricians is that following a prolonged labor or administration of oxytocin, myometrial oxytocin receptors may be downregulated, but vasopressin receptors may remain functional.9,10
Vasopressin regulates plasma volume, blood pressure, osmolality, and uterine contractility. The vasopressin V1a receptor is present on vascular smooth muscle cells, platelets, and uterine myocytes. Activating this receptor causes vasoconstriction, platelet activation, and uterine contraction.
Vasopressin reduces surgical blood loss in two ways. The first major mechanism is through vasoconstriction.11 Second, in uterine surgery specifically, vasopressin stimulates uterine contraction. The hormone exerts its antidiuretic action through the V2 receptor in the kidney.
Optimal vasopressin dose
In gynecologic surgery, the vasopressin doses utilized to reduce blood loss range from 5 U to 20 U diluted in 20 mL to 200 mL of saline. Randomized trial results indicate that a vasopressin dose of 4 U is effective in reducing blood loss during second trimester pregnancy termination,7 and a dose of 3 U is effective in reducing blood loss during cervical conization.5,6 There is insufficient obstetric literature to determine the optimal dose of vasopressin to reduce blood loss in difficult cesarean delivery sur- gery, but doses similar to those used in gynecologic surgery should be considered.
Possible effects of vasopressin overdosing. In gynecologic surgery, injection of vasopressin has been reported to cause bradycardia, hypotension, myocardial infarction, and cardiovascular collapse.12 Given that multiple vasoactive medications may be given to a patient undergoing a complex cesarean delivery, including oxytocin, methergine, and ephedrine, it is important for the obstetrician to use the lowest effective dose of vasopressin necessary to facilitate control of blood loss. The obstetrician needs to communicate with the anesthesiologist and coordinate the use of dilute vasopressin with other vasoactive medications.
Avoid intravascular injection of vasopressin. I prefer to inject vasopressin in the subserosa of the uterus rather than to inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.
Vasopressin reduces blood loss during hysterectomy
One randomized trial has reported that the administration of 10 U of vasopressin diluted in saline into the lower uterine segment reduced blood loss at abdominal hysterectomy in nonpregnant women compared with an injection of saline alone (445 mL vs 748 mL of blood loss, respectively).1 There are no clinical trials of the use of vasopressin in cesarean hysterectomy. However, abdominal hysterectomy procedures and cesarean hysterectomy are similar, and vasopressin likely helps to reduce blood loss at cesarean hysterectomy.
Vasopressin reduces blood loss during myomectomy
Authors of 3 small, randomized clinical trials in nonpregnant women have reported that the intramyometrial injection of dilute vasopressin reduces blood loss during myomectomy surgery.2−4 The vasopressin doses in the 3 trials ranged from 5 U of vasopressin in 100 mL of saline to 20 U of vasopressin in 20 mL of saline. A Cochrane meta-analyis of the 3 studies concluded that, at myomectomy, the intramyometrial injection of dilute vasopressin was associated with a significant reduction in blood loss compared with placebo (246 mL vs 483 mL, respectively).13
There are great similarities between myomectomy in the nonpregnant and pregnant uterus. Given the clinical trials data that support the use of vasopressin to reduce blood loss during myomectomy in the nonpregnant uterus, it is likely that vasopressin also would reduce blood loss during myomectomy performed at the time of a cesarean delivery.
At cesarean delivery, elective myomectomy of intramural fibroids is generally not recommended because of the risk of massive blood loss. Clinicians often remove large pedunculated fibroids because this surgery does not usually cause massive bleeding. However, on occasion it may be necessary to perform a myomectomy on intramural myoma(s) in order to close a hysterotomy incision.
For myomectomy surgery performed at the time of cesarean delivery, many techniques have been utilized to reduce blood loss, including:
- intravenous oxytocin infusion14,15
- injection of oxytocin into the myoma pseudocapsule15
- electrosurgery16−18
- argon beam coagulator19
- uterine tourniquet20
- premyomectomy placement of a uterine U stitch21 or purse string suture22
- O’Leary sutures23,24
- temporary balloon occlusion of pelvic arteries25
- vasopressin injection.26
Given the widespread use of vasopressin injection in gynecologic surgery to reduce blood loss at myomectomy, obstetricians should consider using vasopressin in their cesarean myomectomy surgery.
Use of vasopressin during cesarean delivery for placenta previa may reduce blood loss
Women with a complete placenta previa require a cesarean delivery to safely birth their baby. Cesarean deliveries performed for this indication are associated with an increased risk of hemorrhage. In one case series of 59 patients with placenta previa undergoing cesarean delivery, 4 U of vasopressin diluted in 20 mL of saline was injected into the placental implantation site to reduce blood loss. Among the patients receiving vasopressin in- jection, the blood loss was 1,149 mL. Among 50 women with placenta previa who did not receive vasopressin injection, the blood loss was 1,634 mL.27
Obstetric surgery and vasopressin: The time has come
As obstetricians and gynecologists we constantly strive to improve the effectiveness of our surgical procedures and reduce adverse outcomes, including infection and blood loss. The use of vasopressin is widely accepted in gynecologic surgery as an adjuvant that reduces blood loss. The time has come to expand the use of vasopressin in difficult obstetric surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Okin CR, Guido RS, Meyn LA, Ramanathan S. Vasopressin during abdominal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2001;97:867–872.
- Frederick J, Fletcher H, Simeon D, Mullings A, Hardie M. Intramyometrial vasopressin as a haemostatic agent during myomectomy. Brit J Obstet Gynaecol. 1994;101:435–437.
- Assaf A. Adhesions after laparoscopic myomectomy effect of the technique used. Gynaecol Endosc. 1999;8(4):225–229.
- Zhao F, Jiao Y, Guo Z, Hou R, Wang M. Evaluation of loop ligation of larger myoma pseudocapsule combined with vasopressin on laparoscopic myomectomy. Fertil Steril. 2011;95(2):762–766.
- Sabol ED, Gibson JL, Bowes WA Jr. Vasopressin injection in cervical conization. A double-blind study. Obstet Gynecol. 1971;37(4):596–601.
- Martin-Hirsch PP, Keep SL, Bryant A. Interventions for preventing blood loss during the treatment of cervical intraepithelial neoplasia. Cochrane Database Syst Rev. 2010;(6):CD001421.
- Schulz KE, Grimes DA, Christensen DD. Vasopressin reduces blood loss from second trimester dilatation and evacuation abortion. Lancet. 1985;2(8451):353–356.
- Akerlund M, Bossmar T, Brouard R, et al. Receptor binding of oxytocin and vasopressin antagonists and inhibitory effects in isolated myometrium from preterm and term pregnant women. Br J Obstet Gynaecol. 1999;106(10):1047–1053.
- Akerlund M. Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog Brain Res. 2002;139:359–365.
- Helmer H, Hacki T, Schneeberger C, et al. Oxytocinand vasopressin 1a receptor gene expression in the cycling or pregnant human uterus. Am J Obstet Gynecol. 1998;179(6 pt 1):1572–1578.
- Wing DA, Goharkhay N, Felix JC, Rostamkhani M, Naidu YM, Kovacs BW. Expression of the oxytocin and V1a vasopressin receptors in human myometrium during differing physiological states and following misoprostol administration. Gynecol Obstet Invest. 2006;62(4):181–185.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014; (8):CD005355.
- Tinelli A, Malvasi A, Mynbaev OA, et al. The surgical outcome of intracapsular cesarean myomectomy. A match control study. J Matern Fetal Neonatal Med. 2014;27(1):66–71.
- Brown D, Fletcher HM, Myrie MO, Reid M. Caesarean myomectomy—a safe procedure. A retrospective case controlled study. J Obstet Gynaecol. 1999;19(2):139–141.
- Kaymak O, Ustunyrt E, Okyay RE, Kalyoncu S, Mollamahmutoglu L. Myomectomy during cesarean section. Int J Gynaecol Obstet. 2005;89(2):90–93.
- Park BJ, Kim YW. Safety of cesarean myomectomy. J Obstet Gynaecol Res. 2009;35(5):906–911.
- Kim YS, Choi SD, Bae DH. Risk factors for complications in patients undergoing myomectomy at the time of cesarean section. J Obstet Gynaecol Res. 2010;36(3):550–554.
- Ortac F, Gungor M, Sonmezer M. Myomectomy during cesarean section. Int J Gynecol Obstet. 1999;67(3):189–190.
- Incebiyik A, Hilali NG, Camuzcuoglu A, Vural M, Camuzcuoglu H. Myomectomy during caesarean: a retrospective evaluation of 6 cases. Arch Gynecol Obstet. 2014;289(3):569–573.
- Cobellis L, Pecori E, Cobellis G. Hemostatic technique for myomectomy during cesarean section. Int J Gynaecol Obstet. 2002;79(3):261–262.
- Lee JH, Cho DH. Myomectomy using purse-string suture during cesarean section. Arch Gynecol Obstet. 2011;283(suppl 1):S35–S37.
- Desai BR, Patted SS, Pujar YV, Sheriqar BY, Das SR, Ruge JC. A novel technique of selective uterine devascularization before myomectomy at the time of cesarean section: a pilot study. Fertil Steril. 2010;94(1):362–364.
- Sapmaz E, Celik H, Altungul A. Bilateral ascending uterine artery ligation vs. tourniquet use for hemostasis in cesarean myomectomy. A comparison. J Reprod Med. 2003;48(12):950–954.
- Sparic R, Malvasi A, Kadija S, Babovic I, Nejkovic L, Tinelli A. Cesarean myomectomy trends and controveries: an appraisal [published online ahead of print July 17, 2016]. J Matern Fetal Neonatal Med. doi:10.1080/14767058.2016.1205024.
- Lin JY, Lee WL, Wang PH, et al. Uterine artery occlusion and myomectomy for treatment of pregnant women with uterine leiomyomas who are undergoing cesarean section. J Obstet Gynaecol Res. 2010;36(2):284–290.
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
- Okin CR, Guido RS, Meyn LA, Ramanathan S. Vasopressin during abdominal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2001;97:867–872.
- Frederick J, Fletcher H, Simeon D, Mullings A, Hardie M. Intramyometrial vasopressin as a haemostatic agent during myomectomy. Brit J Obstet Gynaecol. 1994;101:435–437.
- Assaf A. Adhesions after laparoscopic myomectomy effect of the technique used. Gynaecol Endosc. 1999;8(4):225–229.
- Zhao F, Jiao Y, Guo Z, Hou R, Wang M. Evaluation of loop ligation of larger myoma pseudocapsule combined with vasopressin on laparoscopic myomectomy. Fertil Steril. 2011;95(2):762–766.
- Sabol ED, Gibson JL, Bowes WA Jr. Vasopressin injection in cervical conization. A double-blind study. Obstet Gynecol. 1971;37(4):596–601.
- Martin-Hirsch PP, Keep SL, Bryant A. Interventions for preventing blood loss during the treatment of cervical intraepithelial neoplasia. Cochrane Database Syst Rev. 2010;(6):CD001421.
- Schulz KE, Grimes DA, Christensen DD. Vasopressin reduces blood loss from second trimester dilatation and evacuation abortion. Lancet. 1985;2(8451):353–356.
- Akerlund M, Bossmar T, Brouard R, et al. Receptor binding of oxytocin and vasopressin antagonists and inhibitory effects in isolated myometrium from preterm and term pregnant women. Br J Obstet Gynaecol. 1999;106(10):1047–1053.
- Akerlund M. Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog Brain Res. 2002;139:359–365.
- Helmer H, Hacki T, Schneeberger C, et al. Oxytocinand vasopressin 1a receptor gene expression in the cycling or pregnant human uterus. Am J Obstet Gynecol. 1998;179(6 pt 1):1572–1578.
- Wing DA, Goharkhay N, Felix JC, Rostamkhani M, Naidu YM, Kovacs BW. Expression of the oxytocin and V1a vasopressin receptors in human myometrium during differing physiological states and following misoprostol administration. Gynecol Obstet Invest. 2006;62(4):181–185.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014; (8):CD005355.
- Tinelli A, Malvasi A, Mynbaev OA, et al. The surgical outcome of intracapsular cesarean myomectomy. A match control study. J Matern Fetal Neonatal Med. 2014;27(1):66–71.
- Brown D, Fletcher HM, Myrie MO, Reid M. Caesarean myomectomy—a safe procedure. A retrospective case controlled study. J Obstet Gynaecol. 1999;19(2):139–141.
- Kaymak O, Ustunyrt E, Okyay RE, Kalyoncu S, Mollamahmutoglu L. Myomectomy during cesarean section. Int J Gynaecol Obstet. 2005;89(2):90–93.
- Park BJ, Kim YW. Safety of cesarean myomectomy. J Obstet Gynaecol Res. 2009;35(5):906–911.
- Kim YS, Choi SD, Bae DH. Risk factors for complications in patients undergoing myomectomy at the time of cesarean section. J Obstet Gynaecol Res. 2010;36(3):550–554.
- Ortac F, Gungor M, Sonmezer M. Myomectomy during cesarean section. Int J Gynecol Obstet. 1999;67(3):189–190.
- Incebiyik A, Hilali NG, Camuzcuoglu A, Vural M, Camuzcuoglu H. Myomectomy during caesarean: a retrospective evaluation of 6 cases. Arch Gynecol Obstet. 2014;289(3):569–573.
- Cobellis L, Pecori E, Cobellis G. Hemostatic technique for myomectomy during cesarean section. Int J Gynaecol Obstet. 2002;79(3):261–262.
- Lee JH, Cho DH. Myomectomy using purse-string suture during cesarean section. Arch Gynecol Obstet. 2011;283(suppl 1):S35–S37.
- Desai BR, Patted SS, Pujar YV, Sheriqar BY, Das SR, Ruge JC. A novel technique of selective uterine devascularization before myomectomy at the time of cesarean section: a pilot study. Fertil Steril. 2010;94(1):362–364.
- Sapmaz E, Celik H, Altungul A. Bilateral ascending uterine artery ligation vs. tourniquet use for hemostasis in cesarean myomectomy. A comparison. J Reprod Med. 2003;48(12):950–954.
- Sparic R, Malvasi A, Kadija S, Babovic I, Nejkovic L, Tinelli A. Cesarean myomectomy trends and controveries: an appraisal [published online ahead of print July 17, 2016]. J Matern Fetal Neonatal Med. doi:10.1080/14767058.2016.1205024.
- Lin JY, Lee WL, Wang PH, et al. Uterine artery occlusion and myomectomy for treatment of pregnant women with uterine leiomyomas who are undergoing cesarean section. J Obstet Gynaecol Res. 2010;36(2):284–290.
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
A Quick Lesson on Bundled Payments
The Centers for Medicare & Medicaid Services (CMS) has too many new payment models for a practicing doctor to keep up with them all. But there are three that I think are most important for hospitalists to know something about: hospital value-based purchasing, MACRA-related models, and bundled payments. Here, I’ll focus on the latter, which unlike the first two, influences payment to both hospitals and physicians (as well as other providers).
Bundles for Different Diagnoses
Bundled payment programs are the most visible of CMS’s episode payment models (EPMs). There are currently voluntary bundle models (called Bundled Payments for Care Improvement, or BPCI) across many different diagnoses. And in some locales, there is a mandatory bundle program for hip and knee replacements that began in March 2016 (called Comprehensive Care for Joint Replacement, or CCJR or just CJR).
These programs are set to expand significantly in the next few years. The Surgical Hip and Femur Fracture Treatment (SHFFT) becomes active in 2017 in some locales. It will essentially add hip and femur fractures requiring surgery to the existing CJR program. New bundles for acute myocardial infarction, either managed medically or with percutaneous coronary intervention (PCI), and coronary bypass surgery will become mandatory in some parts of the country beginning July 2017.
How the Programs Work
CMS totals all Medicare dollars paid per patient historically for the relevant bundle. This includes payments to the hospital (e.g., the DRG payment) and all fees paid to physicians, therapists, visiting nurses, skilled nursing facilities, etc., from the time of hospital admission through 90 days after discharge. It then sets a target spend (or price) for that diagnosis that is about 3% below the historical average. Because it is based on the past track record of a hospital and its market (or region), the price will vary from place to place.
If, going forward, the Medicare spend for each patient is below the target, CMS pays that amount to the hospital. But if the spend is above the target, the hospital pays some or all of that amount to CMS. Presumably, hospitals will have negotiated with others, such as physicians, how such an “upside” or penalty payment will be divided between them.
It’s worth noting that all parties continue to bill, and are paid by Medicare, via the same fee-for-service arrangements currently in place. It is only at the time of a “true up” that an upside is paid or penalty assessed. And hospitals are eligible for upside payments only if they perform above a threshold on a few quality and patient satisfaction metrics.
The details of these programs are incredibly complicated, and I’m intentionally providing a very simple description of them here. I think that nearly all practicing clinicians should not try to learn and keep up with all of the precise details. They change often! Instead, it’s best to focus on the big picture only and rely on others at the hospital to keep track of the details.
Ways to Lower the Spend
These programs are intended to provide a significant financial incentive to find lower-cost ways to care for patients while still ensuring good care. Any successful effort to lower the cost should start by analyzing just what Medicare spends on each element of care over the more than 90 days each patient is in the bundle. For example, for hip and knee replacement patients, nearly half of the spend goes toward post-hospital services such as a skilled nursing facility and home nursing visits. So the best opportunity to reduce the spend may be to reduce utilization of these services where appropriate.
For patients in the bundles for coronary artery bypass grafting and acute myocardial infarction treated with PCI, only about 10% of the total spend goes to post-hospital services. For these, it might be more effective to focus cost reductions on other things.
Each organization will need to make its own decisions regarding where to focus cost-reduction efforts across the bundle. For many of us, that will mean moving away from a focus on traditional hospitalist-related cost-containment efforts like length of stay or pharmacy costs and instead looking at the bigger picture, including use of post-hospital services.
Some Things to Watch
I expect there will be a number of side effects of these payment models that hospitalists will care about. Doctors in different specialties, for example, might change their minds about whether they want to serve as attending physicians for “bundle patients.” One scenario is that if orthopedists have an opportunity to realize a significant financial upside, they may prefer to serve as attendings for hip fracture patients rather than leaving to hospitalists financially important decisions such as whether patients are discharged to a skilled nursing facility or home. We’ll just have to see how that plays out and be prepared to advocate for our position if different from other specialties.
Successful performance in bundles requires effective coordination of care across settings, and I’m hopeful this will benefit patients. Hospitals and skilled nursing facilities, for example, will need to work together more effectively to curb unnecessary days in the facilities and to reduce readmissions. Many hospitals have already begun developing a preferred network of skilled nursing facilities for referrals that is based on demonstrating good care and low returns to the hospital. Your hospital has probably already started doing this work even if you haven’t heard about it yet.
For me, one of the most concerning outcomes of bundles is the negotiations between providers regarding how an upside or penalty is to be shared among them. I suspect this won’t be contentious initially, but as the dollars at stake grow, it could lead to increasingly stressful negotiations and relationships.
And, lastly, like any payment model, bundles are “gameable,” especially bundles for medical diagnoses such as congestive heart failure or pneumonia, which can be gamed by lowering the threshold for admitting less-sick patients to inpatient status. The spend for these patients, who are less likely to require expensive post-hospital services or be readmitted, will lower the average spend in the bundle, increasing the chance of an upside payment for the providers. TH

The Centers for Medicare & Medicaid Services (CMS) has too many new payment models for a practicing doctor to keep up with them all. But there are three that I think are most important for hospitalists to know something about: hospital value-based purchasing, MACRA-related models, and bundled payments. Here, I’ll focus on the latter, which unlike the first two, influences payment to both hospitals and physicians (as well as other providers).
Bundles for Different Diagnoses
Bundled payment programs are the most visible of CMS’s episode payment models (EPMs). There are currently voluntary bundle models (called Bundled Payments for Care Improvement, or BPCI) across many different diagnoses. And in some locales, there is a mandatory bundle program for hip and knee replacements that began in March 2016 (called Comprehensive Care for Joint Replacement, or CCJR or just CJR).
These programs are set to expand significantly in the next few years. The Surgical Hip and Femur Fracture Treatment (SHFFT) becomes active in 2017 in some locales. It will essentially add hip and femur fractures requiring surgery to the existing CJR program. New bundles for acute myocardial infarction, either managed medically or with percutaneous coronary intervention (PCI), and coronary bypass surgery will become mandatory in some parts of the country beginning July 2017.
How the Programs Work
CMS totals all Medicare dollars paid per patient historically for the relevant bundle. This includes payments to the hospital (e.g., the DRG payment) and all fees paid to physicians, therapists, visiting nurses, skilled nursing facilities, etc., from the time of hospital admission through 90 days after discharge. It then sets a target spend (or price) for that diagnosis that is about 3% below the historical average. Because it is based on the past track record of a hospital and its market (or region), the price will vary from place to place.
If, going forward, the Medicare spend for each patient is below the target, CMS pays that amount to the hospital. But if the spend is above the target, the hospital pays some or all of that amount to CMS. Presumably, hospitals will have negotiated with others, such as physicians, how such an “upside” or penalty payment will be divided between them.
It’s worth noting that all parties continue to bill, and are paid by Medicare, via the same fee-for-service arrangements currently in place. It is only at the time of a “true up” that an upside is paid or penalty assessed. And hospitals are eligible for upside payments only if they perform above a threshold on a few quality and patient satisfaction metrics.
The details of these programs are incredibly complicated, and I’m intentionally providing a very simple description of them here. I think that nearly all practicing clinicians should not try to learn and keep up with all of the precise details. They change often! Instead, it’s best to focus on the big picture only and rely on others at the hospital to keep track of the details.
Ways to Lower the Spend
These programs are intended to provide a significant financial incentive to find lower-cost ways to care for patients while still ensuring good care. Any successful effort to lower the cost should start by analyzing just what Medicare spends on each element of care over the more than 90 days each patient is in the bundle. For example, for hip and knee replacement patients, nearly half of the spend goes toward post-hospital services such as a skilled nursing facility and home nursing visits. So the best opportunity to reduce the spend may be to reduce utilization of these services where appropriate.
For patients in the bundles for coronary artery bypass grafting and acute myocardial infarction treated with PCI, only about 10% of the total spend goes to post-hospital services. For these, it might be more effective to focus cost reductions on other things.
Each organization will need to make its own decisions regarding where to focus cost-reduction efforts across the bundle. For many of us, that will mean moving away from a focus on traditional hospitalist-related cost-containment efforts like length of stay or pharmacy costs and instead looking at the bigger picture, including use of post-hospital services.
Some Things to Watch
I expect there will be a number of side effects of these payment models that hospitalists will care about. Doctors in different specialties, for example, might change their minds about whether they want to serve as attending physicians for “bundle patients.” One scenario is that if orthopedists have an opportunity to realize a significant financial upside, they may prefer to serve as attendings for hip fracture patients rather than leaving to hospitalists financially important decisions such as whether patients are discharged to a skilled nursing facility or home. We’ll just have to see how that plays out and be prepared to advocate for our position if different from other specialties.
Successful performance in bundles requires effective coordination of care across settings, and I’m hopeful this will benefit patients. Hospitals and skilled nursing facilities, for example, will need to work together more effectively to curb unnecessary days in the facilities and to reduce readmissions. Many hospitals have already begun developing a preferred network of skilled nursing facilities for referrals that is based on demonstrating good care and low returns to the hospital. Your hospital has probably already started doing this work even if you haven’t heard about it yet.
For me, one of the most concerning outcomes of bundles is the negotiations between providers regarding how an upside or penalty is to be shared among them. I suspect this won’t be contentious initially, but as the dollars at stake grow, it could lead to increasingly stressful negotiations and relationships.
And, lastly, like any payment model, bundles are “gameable,” especially bundles for medical diagnoses such as congestive heart failure or pneumonia, which can be gamed by lowering the threshold for admitting less-sick patients to inpatient status. The spend for these patients, who are less likely to require expensive post-hospital services or be readmitted, will lower the average spend in the bundle, increasing the chance of an upside payment for the providers. TH

The Centers for Medicare & Medicaid Services (CMS) has too many new payment models for a practicing doctor to keep up with them all. But there are three that I think are most important for hospitalists to know something about: hospital value-based purchasing, MACRA-related models, and bundled payments. Here, I’ll focus on the latter, which unlike the first two, influences payment to both hospitals and physicians (as well as other providers).
Bundles for Different Diagnoses
Bundled payment programs are the most visible of CMS’s episode payment models (EPMs). There are currently voluntary bundle models (called Bundled Payments for Care Improvement, or BPCI) across many different diagnoses. And in some locales, there is a mandatory bundle program for hip and knee replacements that began in March 2016 (called Comprehensive Care for Joint Replacement, or CCJR or just CJR).
These programs are set to expand significantly in the next few years. The Surgical Hip and Femur Fracture Treatment (SHFFT) becomes active in 2017 in some locales. It will essentially add hip and femur fractures requiring surgery to the existing CJR program. New bundles for acute myocardial infarction, either managed medically or with percutaneous coronary intervention (PCI), and coronary bypass surgery will become mandatory in some parts of the country beginning July 2017.
How the Programs Work
CMS totals all Medicare dollars paid per patient historically for the relevant bundle. This includes payments to the hospital (e.g., the DRG payment) and all fees paid to physicians, therapists, visiting nurses, skilled nursing facilities, etc., from the time of hospital admission through 90 days after discharge. It then sets a target spend (or price) for that diagnosis that is about 3% below the historical average. Because it is based on the past track record of a hospital and its market (or region), the price will vary from place to place.
If, going forward, the Medicare spend for each patient is below the target, CMS pays that amount to the hospital. But if the spend is above the target, the hospital pays some or all of that amount to CMS. Presumably, hospitals will have negotiated with others, such as physicians, how such an “upside” or penalty payment will be divided between them.
It’s worth noting that all parties continue to bill, and are paid by Medicare, via the same fee-for-service arrangements currently in place. It is only at the time of a “true up” that an upside is paid or penalty assessed. And hospitals are eligible for upside payments only if they perform above a threshold on a few quality and patient satisfaction metrics.
The details of these programs are incredibly complicated, and I’m intentionally providing a very simple description of them here. I think that nearly all practicing clinicians should not try to learn and keep up with all of the precise details. They change often! Instead, it’s best to focus on the big picture only and rely on others at the hospital to keep track of the details.
Ways to Lower the Spend
These programs are intended to provide a significant financial incentive to find lower-cost ways to care for patients while still ensuring good care. Any successful effort to lower the cost should start by analyzing just what Medicare spends on each element of care over the more than 90 days each patient is in the bundle. For example, for hip and knee replacement patients, nearly half of the spend goes toward post-hospital services such as a skilled nursing facility and home nursing visits. So the best opportunity to reduce the spend may be to reduce utilization of these services where appropriate.
For patients in the bundles for coronary artery bypass grafting and acute myocardial infarction treated with PCI, only about 10% of the total spend goes to post-hospital services. For these, it might be more effective to focus cost reductions on other things.
Each organization will need to make its own decisions regarding where to focus cost-reduction efforts across the bundle. For many of us, that will mean moving away from a focus on traditional hospitalist-related cost-containment efforts like length of stay or pharmacy costs and instead looking at the bigger picture, including use of post-hospital services.
Some Things to Watch
I expect there will be a number of side effects of these payment models that hospitalists will care about. Doctors in different specialties, for example, might change their minds about whether they want to serve as attending physicians for “bundle patients.” One scenario is that if orthopedists have an opportunity to realize a significant financial upside, they may prefer to serve as attendings for hip fracture patients rather than leaving to hospitalists financially important decisions such as whether patients are discharged to a skilled nursing facility or home. We’ll just have to see how that plays out and be prepared to advocate for our position if different from other specialties.
Successful performance in bundles requires effective coordination of care across settings, and I’m hopeful this will benefit patients. Hospitals and skilled nursing facilities, for example, will need to work together more effectively to curb unnecessary days in the facilities and to reduce readmissions. Many hospitals have already begun developing a preferred network of skilled nursing facilities for referrals that is based on demonstrating good care and low returns to the hospital. Your hospital has probably already started doing this work even if you haven’t heard about it yet.
For me, one of the most concerning outcomes of bundles is the negotiations between providers regarding how an upside or penalty is to be shared among them. I suspect this won’t be contentious initially, but as the dollars at stake grow, it could lead to increasingly stressful negotiations and relationships.
And, lastly, like any payment model, bundles are “gameable,” especially bundles for medical diagnoses such as congestive heart failure or pneumonia, which can be gamed by lowering the threshold for admitting less-sick patients to inpatient status. The spend for these patients, who are less likely to require expensive post-hospital services or be readmitted, will lower the average spend in the bundle, increasing the chance of an upside payment for the providers. TH

Surveys Are Not the Most Effective Way to Improve Patient Satisfaction
What started with a car dealership survey has become a near avalanche of surveys from my credit card, bank, airlines, hotels, and other businesses. Each starts by assuring me that it will take only a minute or two to complete the survey, but if I completed every survey sent my way, it would add up to a significant amount of time. So I’ve stopped responding to nearly all of them, not so much as a form of protest but as part of my overall time-management efforts.
I imagine many of our patients see surveys from hospitals and other healthcare providers similarly: just another one to add to the pile. Patients in their 80s and 90s—a significant portion of hospitalist patients—probably interact a lot less with companies that send satisfaction surveys and so might be more attentive to ones from healthcare organizations. But I suspect that a reasonable portion of older patients rely on a family member to complete them, and this person, often a son or daughter, probably does get a lot of similar surveys. Surely, survey fatigue is influencing the results at least a little.
Healthcare Surveys: HCAHPS
For all the surveying going on, I find it pretty difficult to use HCAHPS results to guide patient-satisfaction improvement efforts. Sure, I can see how individual doctors or different physician groups score compared to one another and try to model my behaviors after the high performers. That is a really valuable thing to do, but it doesn’t get to the granular level I’d like.
One would hope the three physician-specific HCAHPS questions would support drilling down to more actionable information. But every hospitalist group I’ve seen always has the same pattern, scoring from lowest to highest as follows:
- How often did doctors explain things in a way you could understand?
- How often did doctors listen carefully to you?
- How often did doctors treat you with courtesy and respect?
So I don’t think the difference in scores on these questions is very useful in guiding improvement efforts.
Looking beyond HCAHPS
For a few years, our hospitalist group added a very short survey to the brochure describing the practice. I still think that was good idea to ensure accurate attribution and more granular information, but it didn’t yield much value in practice because of a low response rate. Ultimately, we stopped using it because of our hospital risk manager’s concern any such survey could be construed as “coaching” patients in their HCAHPS responses, something the Centers for Medicare & Medicaid Services forbids.
Mark Rudolph, MD, vice president of physician development and patient experience at Sound Physicians, told me about their experience with their employed RNs using tablet computers to survey every patient the day following hospital admission (i.e., while patients were still in the hospital). It seems to me this could be a really valuable tool to provide very granular feedback at the outset of a patient stay when there is still time to address areas in which the patient is less satisfied. They found that for about 30% of patients, the survey uncovered something that could be fixed, such as providing another blanket, determining what time a test was likely to be done, etc. I bet for most patients the fact that a nurse cared enough to ask how things are going and try to remedy problems improved their HCAPHS scores.
Yet after some experience with this approach, Sound Physicians found that, for a number of reasons, this wasn’t as valuable as hoped. They now survey a smaller sample of patients and sometimes adjust the questions based on the known or suspected strengths and weaknesses of individual providers. For one doctor, for example, the survey might ask whether the doctor spent enough time with the patient; for another, it might ask if the doctor spoke clearly, etc.
Dr. Rudolph thinks having someone such as the lead hospitalist observe the doctor while on rounds might ultimately prove more valuable than administering a survey. It will be interesting to see how his group and others around the country evolve their approach to better understand each provider’s strengths and weaknesses and most effective ways to improve patient satisfaction.
How to Improve Patient Satisfaction?
In my April 2012 column, I wrote about several things for hospitalists to consider including in their patient-satisfaction improvement plan. And, of course, there are a lot of additional sources of ideas available just by searching the Internet.
I find it difficult to consistently implement a bundle of multiple different habits, such as always sitting or always rounding with the patient’s bedside nurse, etc. I acknowledge these are proven valuable strategies to improve scores, but I still find it hard to do them consistently.
For some of us, it might be better to pick one thing to focus on. And while I don’t have research data to prove it, I think the single most valuable thing to improve patient satisfaction with hospitalists is to phone patients after discharge. It isn’t as difficult as most assume, and it often leads patients (or the family member you reach) to thank you profusely for the call. I think hospitalists can really benefit from more expressions of gratitude from patients and families, and these calls often provide it.
I’ve learned a few lessons about making post-discharge calls that are detailed in my August 2012 column. TH

What started with a car dealership survey has become a near avalanche of surveys from my credit card, bank, airlines, hotels, and other businesses. Each starts by assuring me that it will take only a minute or two to complete the survey, but if I completed every survey sent my way, it would add up to a significant amount of time. So I’ve stopped responding to nearly all of them, not so much as a form of protest but as part of my overall time-management efforts.
I imagine many of our patients see surveys from hospitals and other healthcare providers similarly: just another one to add to the pile. Patients in their 80s and 90s—a significant portion of hospitalist patients—probably interact a lot less with companies that send satisfaction surveys and so might be more attentive to ones from healthcare organizations. But I suspect that a reasonable portion of older patients rely on a family member to complete them, and this person, often a son or daughter, probably does get a lot of similar surveys. Surely, survey fatigue is influencing the results at least a little.
Healthcare Surveys: HCAHPS
For all the surveying going on, I find it pretty difficult to use HCAHPS results to guide patient-satisfaction improvement efforts. Sure, I can see how individual doctors or different physician groups score compared to one another and try to model my behaviors after the high performers. That is a really valuable thing to do, but it doesn’t get to the granular level I’d like.
One would hope the three physician-specific HCAHPS questions would support drilling down to more actionable information. But every hospitalist group I’ve seen always has the same pattern, scoring from lowest to highest as follows:
- How often did doctors explain things in a way you could understand?
- How often did doctors listen carefully to you?
- How often did doctors treat you with courtesy and respect?
So I don’t think the difference in scores on these questions is very useful in guiding improvement efforts.
Looking beyond HCAHPS
For a few years, our hospitalist group added a very short survey to the brochure describing the practice. I still think that was good idea to ensure accurate attribution and more granular information, but it didn’t yield much value in practice because of a low response rate. Ultimately, we stopped using it because of our hospital risk manager’s concern any such survey could be construed as “coaching” patients in their HCAHPS responses, something the Centers for Medicare & Medicaid Services forbids.
Mark Rudolph, MD, vice president of physician development and patient experience at Sound Physicians, told me about their experience with their employed RNs using tablet computers to survey every patient the day following hospital admission (i.e., while patients were still in the hospital). It seems to me this could be a really valuable tool to provide very granular feedback at the outset of a patient stay when there is still time to address areas in which the patient is less satisfied. They found that for about 30% of patients, the survey uncovered something that could be fixed, such as providing another blanket, determining what time a test was likely to be done, etc. I bet for most patients the fact that a nurse cared enough to ask how things are going and try to remedy problems improved their HCAPHS scores.
Yet after some experience with this approach, Sound Physicians found that, for a number of reasons, this wasn’t as valuable as hoped. They now survey a smaller sample of patients and sometimes adjust the questions based on the known or suspected strengths and weaknesses of individual providers. For one doctor, for example, the survey might ask whether the doctor spent enough time with the patient; for another, it might ask if the doctor spoke clearly, etc.
Dr. Rudolph thinks having someone such as the lead hospitalist observe the doctor while on rounds might ultimately prove more valuable than administering a survey. It will be interesting to see how his group and others around the country evolve their approach to better understand each provider’s strengths and weaknesses and most effective ways to improve patient satisfaction.
How to Improve Patient Satisfaction?
In my April 2012 column, I wrote about several things for hospitalists to consider including in their patient-satisfaction improvement plan. And, of course, there are a lot of additional sources of ideas available just by searching the Internet.
I find it difficult to consistently implement a bundle of multiple different habits, such as always sitting or always rounding with the patient’s bedside nurse, etc. I acknowledge these are proven valuable strategies to improve scores, but I still find it hard to do them consistently.
For some of us, it might be better to pick one thing to focus on. And while I don’t have research data to prove it, I think the single most valuable thing to improve patient satisfaction with hospitalists is to phone patients after discharge. It isn’t as difficult as most assume, and it often leads patients (or the family member you reach) to thank you profusely for the call. I think hospitalists can really benefit from more expressions of gratitude from patients and families, and these calls often provide it.
I’ve learned a few lessons about making post-discharge calls that are detailed in my August 2012 column. TH

What started with a car dealership survey has become a near avalanche of surveys from my credit card, bank, airlines, hotels, and other businesses. Each starts by assuring me that it will take only a minute or two to complete the survey, but if I completed every survey sent my way, it would add up to a significant amount of time. So I’ve stopped responding to nearly all of them, not so much as a form of protest but as part of my overall time-management efforts.
I imagine many of our patients see surveys from hospitals and other healthcare providers similarly: just another one to add to the pile. Patients in their 80s and 90s—a significant portion of hospitalist patients—probably interact a lot less with companies that send satisfaction surveys and so might be more attentive to ones from healthcare organizations. But I suspect that a reasonable portion of older patients rely on a family member to complete them, and this person, often a son or daughter, probably does get a lot of similar surveys. Surely, survey fatigue is influencing the results at least a little.
Healthcare Surveys: HCAHPS
For all the surveying going on, I find it pretty difficult to use HCAHPS results to guide patient-satisfaction improvement efforts. Sure, I can see how individual doctors or different physician groups score compared to one another and try to model my behaviors after the high performers. That is a really valuable thing to do, but it doesn’t get to the granular level I’d like.
One would hope the three physician-specific HCAHPS questions would support drilling down to more actionable information. But every hospitalist group I’ve seen always has the same pattern, scoring from lowest to highest as follows:
- How often did doctors explain things in a way you could understand?
- How often did doctors listen carefully to you?
- How often did doctors treat you with courtesy and respect?
So I don’t think the difference in scores on these questions is very useful in guiding improvement efforts.
Looking beyond HCAHPS
For a few years, our hospitalist group added a very short survey to the brochure describing the practice. I still think that was good idea to ensure accurate attribution and more granular information, but it didn’t yield much value in practice because of a low response rate. Ultimately, we stopped using it because of our hospital risk manager’s concern any such survey could be construed as “coaching” patients in their HCAHPS responses, something the Centers for Medicare & Medicaid Services forbids.
Mark Rudolph, MD, vice president of physician development and patient experience at Sound Physicians, told me about their experience with their employed RNs using tablet computers to survey every patient the day following hospital admission (i.e., while patients were still in the hospital). It seems to me this could be a really valuable tool to provide very granular feedback at the outset of a patient stay when there is still time to address areas in which the patient is less satisfied. They found that for about 30% of patients, the survey uncovered something that could be fixed, such as providing another blanket, determining what time a test was likely to be done, etc. I bet for most patients the fact that a nurse cared enough to ask how things are going and try to remedy problems improved their HCAPHS scores.
Yet after some experience with this approach, Sound Physicians found that, for a number of reasons, this wasn’t as valuable as hoped. They now survey a smaller sample of patients and sometimes adjust the questions based on the known or suspected strengths and weaknesses of individual providers. For one doctor, for example, the survey might ask whether the doctor spent enough time with the patient; for another, it might ask if the doctor spoke clearly, etc.
Dr. Rudolph thinks having someone such as the lead hospitalist observe the doctor while on rounds might ultimately prove more valuable than administering a survey. It will be interesting to see how his group and others around the country evolve their approach to better understand each provider’s strengths and weaknesses and most effective ways to improve patient satisfaction.
How to Improve Patient Satisfaction?
In my April 2012 column, I wrote about several things for hospitalists to consider including in their patient-satisfaction improvement plan. And, of course, there are a lot of additional sources of ideas available just by searching the Internet.
I find it difficult to consistently implement a bundle of multiple different habits, such as always sitting or always rounding with the patient’s bedside nurse, etc. I acknowledge these are proven valuable strategies to improve scores, but I still find it hard to do them consistently.
For some of us, it might be better to pick one thing to focus on. And while I don’t have research data to prove it, I think the single most valuable thing to improve patient satisfaction with hospitalists is to phone patients after discharge. It isn’t as difficult as most assume, and it often leads patients (or the family member you reach) to thank you profusely for the call. I think hospitalists can really benefit from more expressions of gratitude from patients and families, and these calls often provide it.
I’ve learned a few lessons about making post-discharge calls that are detailed in my August 2012 column. TH

Strategies for maintaining resilience to the burnout threat
It sometimes seems that the pace of life, and its stresses, have spiraled out of control: There just never seems to be enough time to deal with all the directions in which we are pulled. This easily can lead to the exhaustion of physical or emotional strength or motivation, otherwise known as “burnout.” Burnout is physical or mental collapse caused by overwork or stress and we are all at risk of suffering it. Conflicting demands on our time, loss of control (real or imagined), and a diminishing sense of worth grind at us from every direction.
In general, having some control over schedule and hours worked is associated with reductions in burnout and improved job satisfaction.1 But this is not always the case. Well-intentioned efforts to reduce workload, such as the electronic medical records or physician order entry systems, have actually made the problem worse.2 The seeming level of control that comes with being the chair of an obstetrics and gynecology department does not necessarily reduce burnout rates,3 and neither does the perceived resilience of mental health professionals, who still report burnout rates that approach 25%.4
This article continues the focus on recalibrating work/life balance that began last month with “ObGyn burnout: ACOG takes aim,” by Lucia DiVenere, MA, and the peer-to-peer audiocast with Ms. DiVenere and myself titled “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?” Here, I identify the causes and symptoms of burnout and provide specific tools to help you develop resilience.
Who is most at risk for burnout?
Estimates range from 40% to 75% of ObGyns currently suffer from professional burnout, making the lifetime risk a virtual certainty.1−3 The idea of professional burnout is not new, but wider recognition of the alarming rates of burnout is very current.4,5 A recent survey of gynecologic oncologists6 found that of those studied 30% scored high for emotional exhaustion, 10% high for depersonalization, and 11% low for personal accomplishment. Overall, 32% of physicians had scores indicating burnout. More worrisome was that 33% screened positive for depression, 13% had a history of suicidal ideation, 15% screened positive for alcohol abuse, and 34% reported impaired quality of life. Almost 40% would not encourage their children to enter medicine and more than 10% said that they would not enter medicine again if they had to do it over.
Residents and those at mid-career are particularly vulnerable,7 with resident burnout rates reported to be as high as 75%.8 Of surveyed residents in a 2012 study, 13% satisfied all 3 subscale scores for high burnout and greater than 50% had high levels of depersonalization and emotional exhaustion. Those with high levels of emotional exhaustion were less satisfied with their careers, regretted choosing obstetrics and gynecology, and had higher rates of depression—all findings consistent with older studies.
9,10
References
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed July 7, 2016.
- Shanafelt TD, Boone, S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385.
- Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240–242.
- Lee YY, Medford AR, Halim AS. Burnout in physicians. J R Coll Physicians Edinb. 2015;45(2):104–107.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Rath KS, Huffman LB, Phillips GS, Carpenter KM, Fowler JM. Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol. 2015;213(6):824.e1–e9.
- Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–395.
- Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195(5):1444–1449.
- Castelo-Branco C, Figueras F, Eixarch E, et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114(1):94–98
Why burnout occurs
Simply identifying ourselves as professionals and the same attributes that make us successful as physicians (type-A behavior, obsessive-compulsive commitment to our profession) put us at risk for professional burnout (see “Who is most at risk for burnout?”). Those predilections combine with the forces from the world in which we live and practice to increase this threat (TABLE 1). Conditions in which there are weak retention rates, high turnover, heavy workloads, and low staffing levels or staffing shortages increase the risk of burnout and, when burnout is present, are associated with a degraded quality of care.5
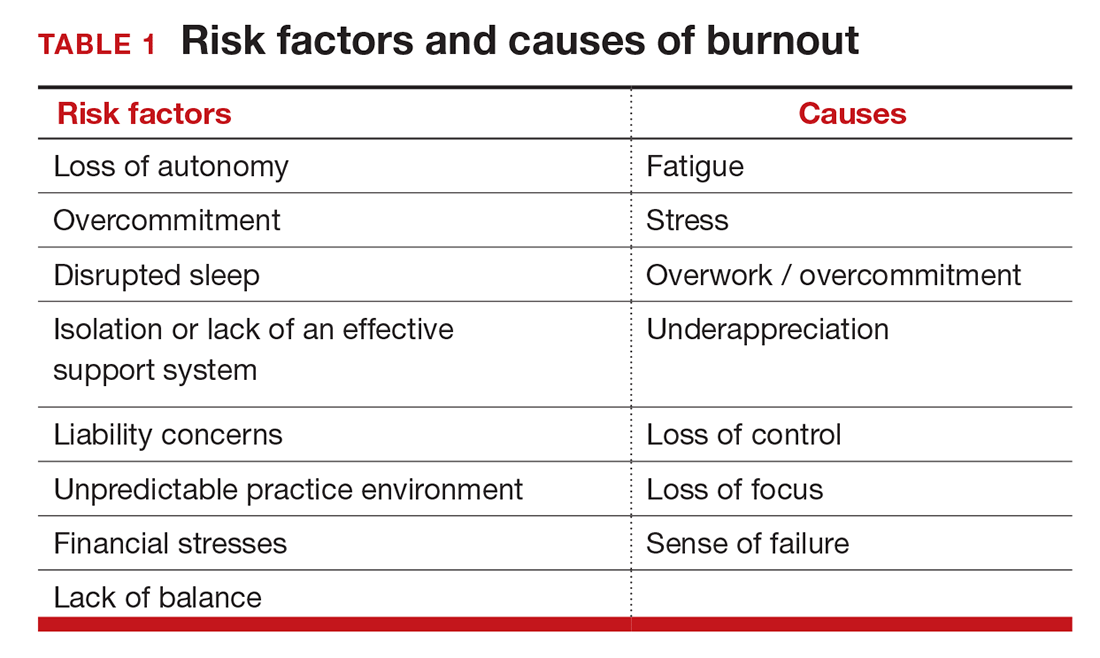
Does stress cause burnout?
Stress is often seen as the reason for burnout. Research shows that there is no single source of burnout,6 however, and a number of factors combine to cause this physical or mental collapse. Stress can be a positive or negative factor in our performance. Too little stress and we feel underutilized; too much stress and we collapse from the strain.
There is a middle ground where stress and expectations keep us focused and at peak productivity (FIGURE 1). The key is the balance between control and demand: When we have a greater level of control, we can handle high demands (FIGURE 2). It is when we lack that control that high demands result in what has been called “toxic stress,” and we collapse under the strain.
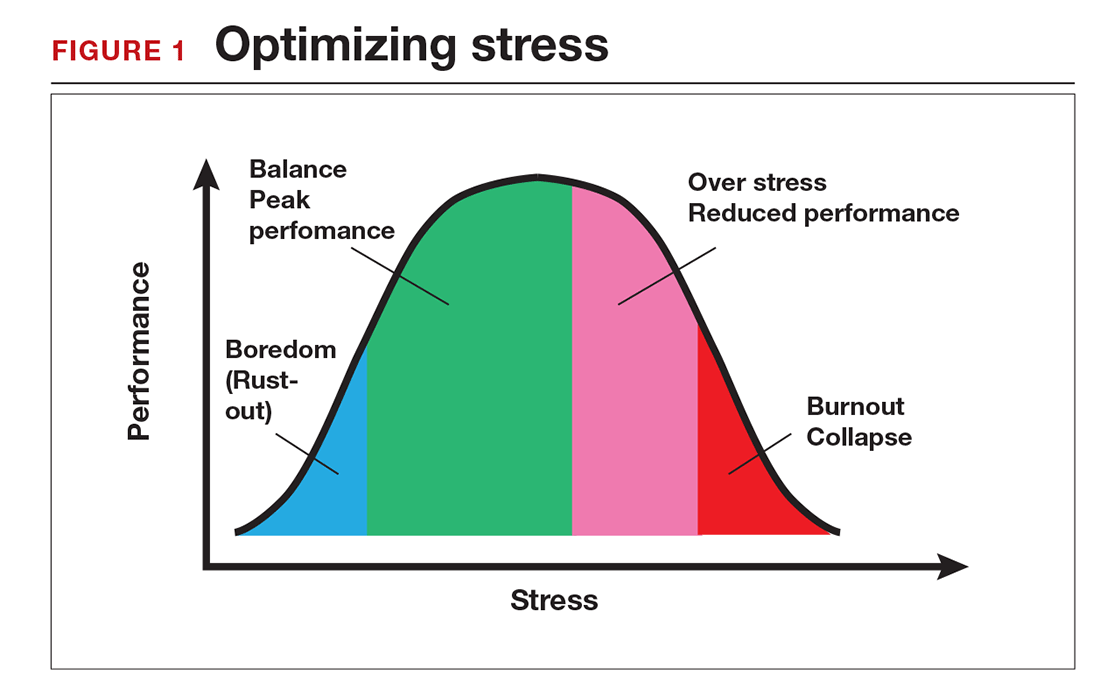
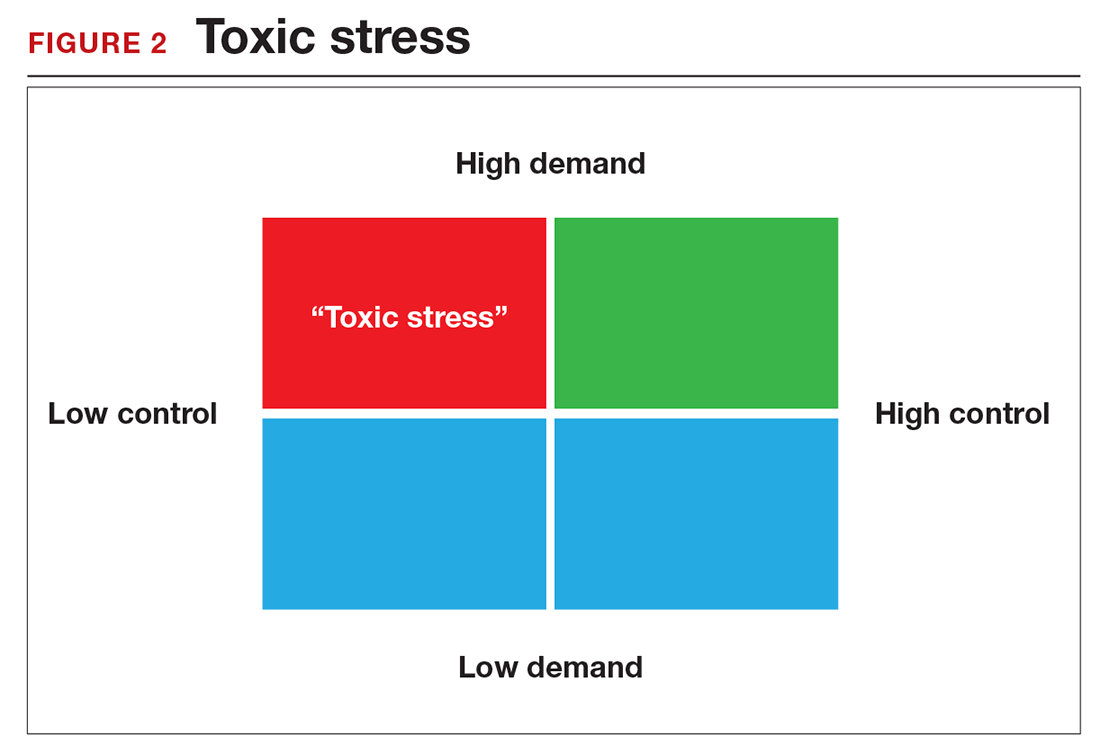
The impact of burnout
Burnout is associated with reduced performance and job satisfaction, increased rates of illness and absenteeism, accidents, premature retirement, and even premature death. Physically, stress induces the dry mouth, dilated pupils, and release of adrenalin and noradrenalin associated with the “fight-or-flight” reaction. The degree to which the physical, emotional, and professional symptoms are manifest depends on the depth or stage of burnout present (TABLE 2). Overall, burnout is associated with an increased risk for physical illness.7 Economically, the impact of physician burnout (for physicians practicing in Canada) has been estimated to be $213.1 million,8 which includes $185.2 million due to early retirement and $27.9 million due to reduced clinical hours.
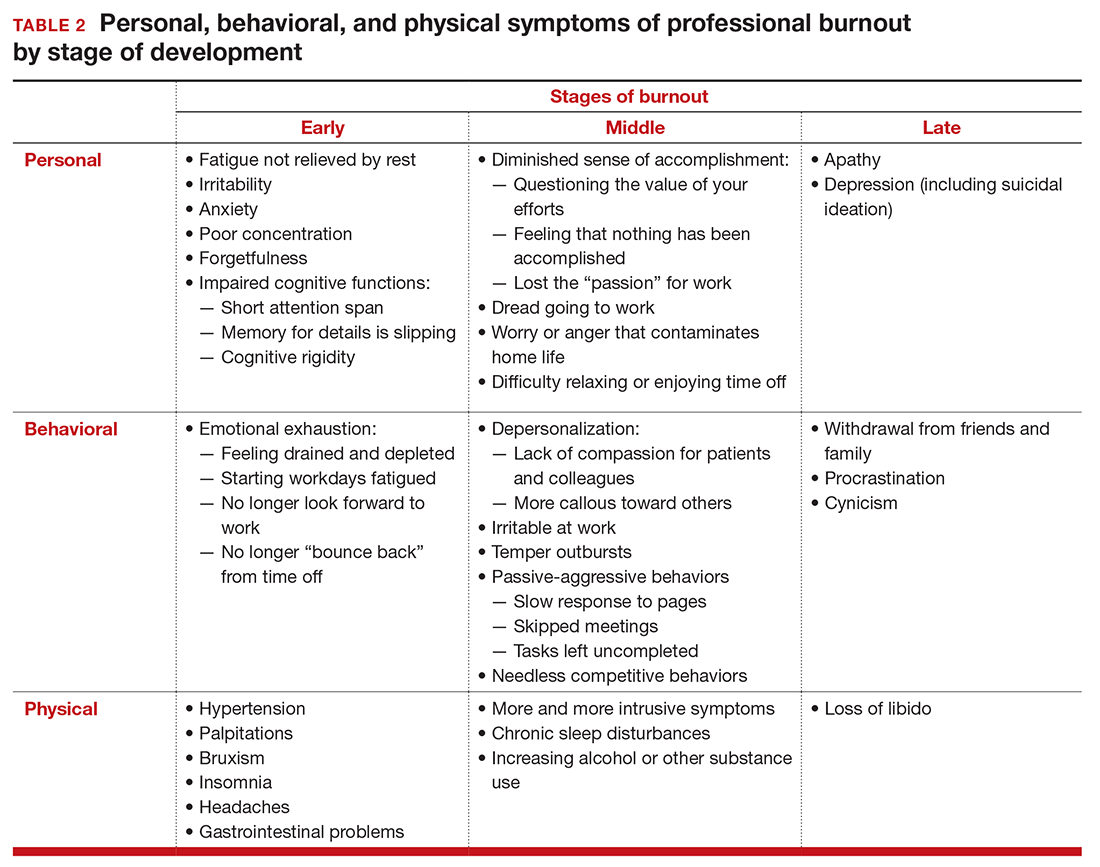
“Do I have burnout?”
We all suffer from fatigue and have stress, but do we have burnout? With so many myths surrounding stress and burnout, it is sometimes hard to know where the truth lies. Some of those myths say that:
- you can leave your troubles at home
- mental stress does not affect physical performance
- stress is only for wimps
- stress and burnout are chemical imbalances that can be treated with medications
- stress is always bad
- burnout will get better if you just give it more time.
Maslach Burnout Inventory. The effective “gold standard” for diagnosing burnout is the Maslach Burnout Inventory,9 which operationalizes burnout as a 3-dimensional syndrome made up of exhaustion, cynicism, and inefficacy. Other diagnostic tools have been introduced10 but have not gained the wide acceptance of the Maslach Inventory. Some authors have argued that burnout and depression represent different, closely spaced points along a spectrum and that any effort to separate them may be artificial.11,12
The Maslach Burnout Inventory consists of a survey of 22 items; it requires a fee to take and is interpreted by a qualified individual. A simpler screening test consists of 10 questions (TABLE 3). If you answer “yes” to 5 or more of the questions, you probably have burnout. An even quicker test is to see, when you go on vacation, if your symptoms disappear. If so, you are not depressed; you have burnout. (If you cannot even go on vacation, then it is almost certain.)
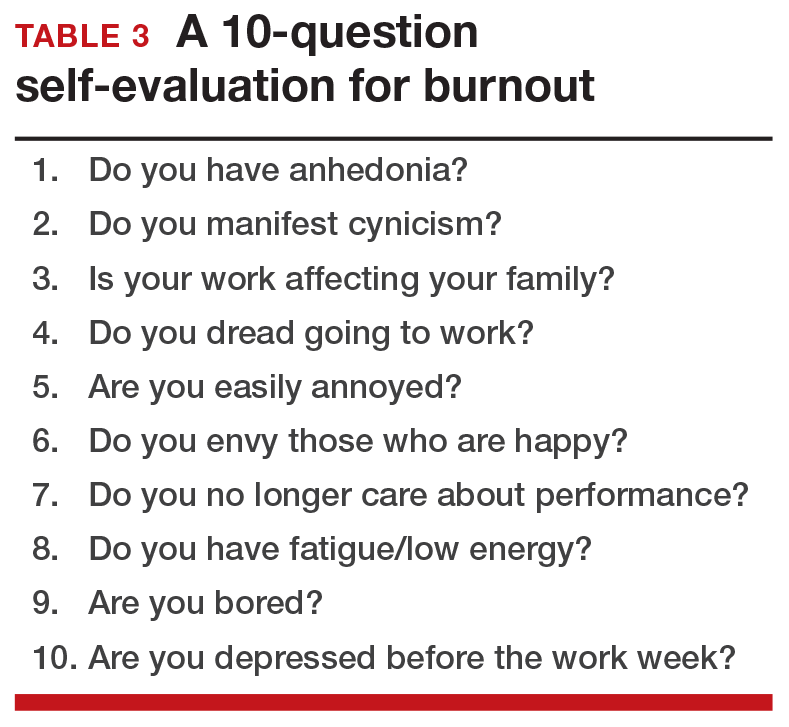
12 stages of burnout. Psychologists Herbert Freudenberger and Gail North have theorized that the burnout process can be divided into 12 phases (TABLE 4).13 These stages are not necessarily sequential—some may be absent and others may present simultaneously. It is easy to see how these can represent stages in a potentially spiraling series of behaviors and changes that result in complete dysfunction. It is also easy to understand that the characteristics that are associated with success in medical school, clinical training, and practice, such as high expectations, placing the needs of others above our own, and a desire to prove oneself, virtually define the first 3 stages.
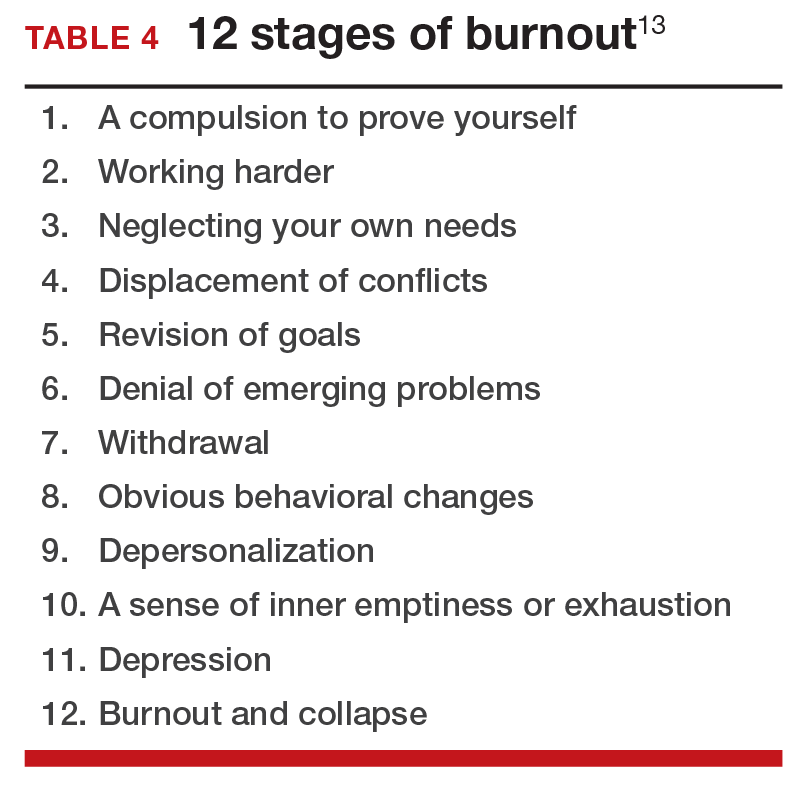
Approaches for burnout control and prevention
There are some simple steps we can take to reduce the risk of burnout or to reverse its effects. Because fatigue and stress are 2 of the greatest risk factors, reducing these is a good place to start.
Prioritize sleep. When it comes to fatigue, that one is easy: get some sleep. Physicians tend to sleep fewer hours than the general population and what we get is often not the type that is restful and restorative.14 Just reducing the number of hours worked is not enough, as a number of studies have found.15 The rest must result in relaxation.
e Stress reduction may seem a more difficult goal than getting more sleep. In reality, there are several simple approaches to use to reduce stress:
- Even though we all have busy clinical schedules, take short breaks to rest, sing, laugh, and exercise. Even breaks as short as 10 minutes can be effective.16
- Separate work from private life by taking a short break to resolve issues before heading home. Avoiding “baggage” or homework will go a long way to giving you the perspective you need from your time off. This may also mean that you have to delegate tasks, share chores, or get carry-out for dinner.
- Set meaningful and realistic goals for yourself professionally and personally. Do not expect or demand more than is possible. This will mean setting priorities and recognizing that some tasks may have to wait.
- Finally, do not forget to pay yourself with hobbies and activities that you enjoy.
Take action
If you feel the effects of burnout tugging at your coattails, you can reduce the effects, deal with the sources, and improve your attitude (TABLE 5). Rest and relaxation will go a long way to helping, but do not forget to take care of your physical well-being with a healthy diet, exercise, and health checkups. Deal with the sources of burnout by identifying the stressors, setting realistic priorities, and practicing good time management.
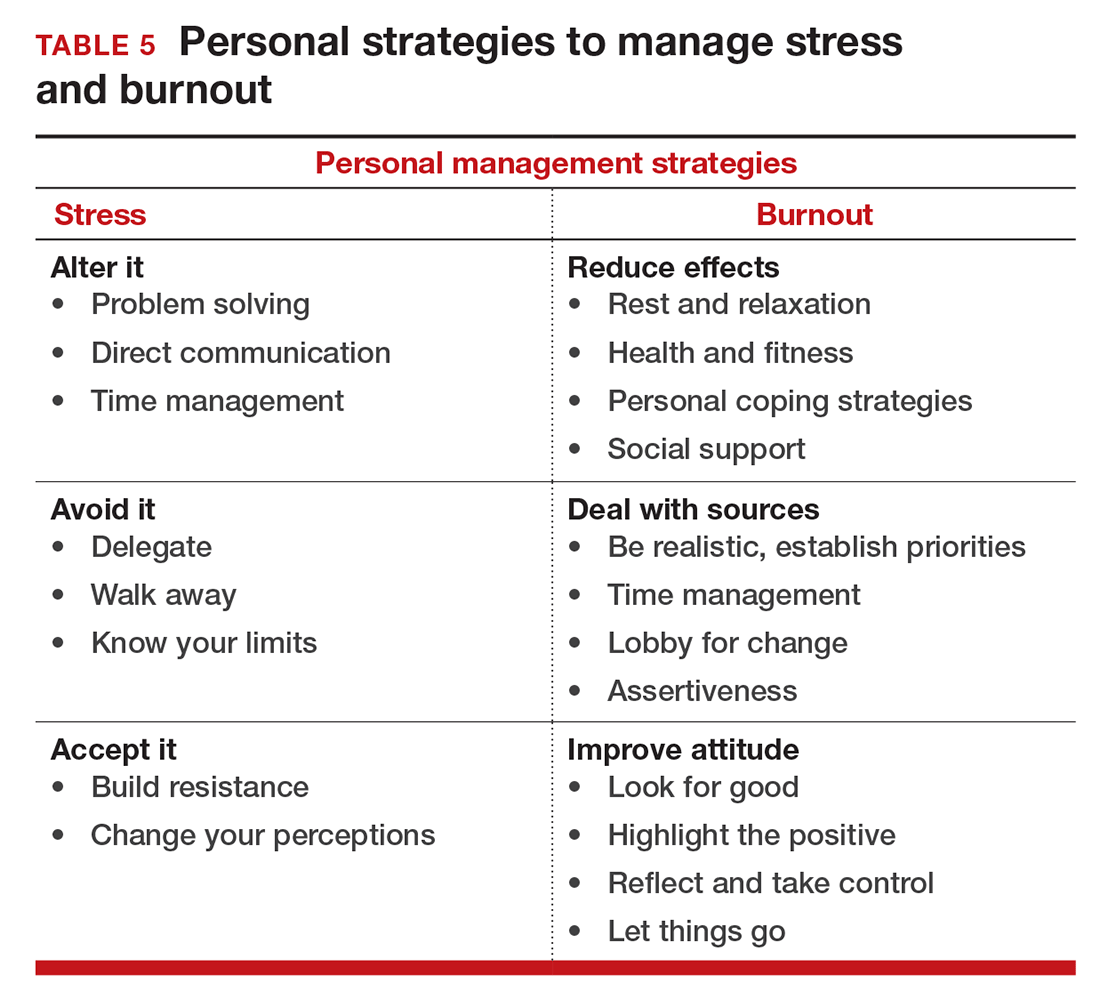
You also should lobby for changes that will increase your control and reduce unnecessary obstacles to completing your goals. Be your own best advocate. Look for the good and try to identify at least one instance during the day where your presence or acts made a difference. In the end, it is like Smokey the Bear says, “Only you can prevent burnout.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007;109(4):949-955.
- Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848.
- Gabbe SG, Melville J, Mandel L, Walker E. Burnout in chairs of obstetrics and gynecology: diagnosis, treatment, and prevention. Am J Obstet Gynecol. 2002;186(4):601-612.
- Kok BC, Herrell RK, Grossman SH, West JC, Wilk JE. Prevalence of professional burnout among military mental health service providers. Psychiatr Serv. 2016;67(1):137-140.
- Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, McGee H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293-307.
- Streu R, Hansen J, Abrahamse P, Alderman AK. Professional burnout among US plastic surgeons: results of a national survey. Ann Plast Surg. 2014;72(3):346-350.
- Honkonen T, Ahola K, Pertovaara M, et al. The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61(1):59-66.
- Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014;14:254.
- Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory Manual. Palo Alto, California: Consulting Psychologists Press, 1996.
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress. 2005;19(3):192-207.
- Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E. Comparative symptomatology of burnout and depression. J Health Psychol. 2013;18(6):782-787.
- Bianchi R, Schonfeld I S, Laurent E. Is burnout a depressive disorder? A re-examination with special focus on atypical depression. Intl J Stress Manag. 2014;21(4):307-324.
- Freudenberger HJ, North G. Women's burnout: How to spot it, how to reverse it, and how to prevent it. New York, New York: Doubleday, 1985.
- Abrams RM. Sleep deprivation. Obstet Gynecol Clin North Am. 2015;42(3):493-506.
- Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47-54.
- Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: The personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255(4):625-633.
It sometimes seems that the pace of life, and its stresses, have spiraled out of control: There just never seems to be enough time to deal with all the directions in which we are pulled. This easily can lead to the exhaustion of physical or emotional strength or motivation, otherwise known as “burnout.” Burnout is physical or mental collapse caused by overwork or stress and we are all at risk of suffering it. Conflicting demands on our time, loss of control (real or imagined), and a diminishing sense of worth grind at us from every direction.
In general, having some control over schedule and hours worked is associated with reductions in burnout and improved job satisfaction.1 But this is not always the case. Well-intentioned efforts to reduce workload, such as the electronic medical records or physician order entry systems, have actually made the problem worse.2 The seeming level of control that comes with being the chair of an obstetrics and gynecology department does not necessarily reduce burnout rates,3 and neither does the perceived resilience of mental health professionals, who still report burnout rates that approach 25%.4
This article continues the focus on recalibrating work/life balance that began last month with “ObGyn burnout: ACOG takes aim,” by Lucia DiVenere, MA, and the peer-to-peer audiocast with Ms. DiVenere and myself titled “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?” Here, I identify the causes and symptoms of burnout and provide specific tools to help you develop resilience.
Who is most at risk for burnout?
Estimates range from 40% to 75% of ObGyns currently suffer from professional burnout, making the lifetime risk a virtual certainty.1−3 The idea of professional burnout is not new, but wider recognition of the alarming rates of burnout is very current.4,5 A recent survey of gynecologic oncologists6 found that of those studied 30% scored high for emotional exhaustion, 10% high for depersonalization, and 11% low for personal accomplishment. Overall, 32% of physicians had scores indicating burnout. More worrisome was that 33% screened positive for depression, 13% had a history of suicidal ideation, 15% screened positive for alcohol abuse, and 34% reported impaired quality of life. Almost 40% would not encourage their children to enter medicine and more than 10% said that they would not enter medicine again if they had to do it over.
Residents and those at mid-career are particularly vulnerable,7 with resident burnout rates reported to be as high as 75%.8 Of surveyed residents in a 2012 study, 13% satisfied all 3 subscale scores for high burnout and greater than 50% had high levels of depersonalization and emotional exhaustion. Those with high levels of emotional exhaustion were less satisfied with their careers, regretted choosing obstetrics and gynecology, and had higher rates of depression—all findings consistent with older studies.
9,10
References
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed July 7, 2016.
- Shanafelt TD, Boone, S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385.
- Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240–242.
- Lee YY, Medford AR, Halim AS. Burnout in physicians. J R Coll Physicians Edinb. 2015;45(2):104–107.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Rath KS, Huffman LB, Phillips GS, Carpenter KM, Fowler JM. Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol. 2015;213(6):824.e1–e9.
- Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–395.
- Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195(5):1444–1449.
- Castelo-Branco C, Figueras F, Eixarch E, et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114(1):94–98
Why burnout occurs
Simply identifying ourselves as professionals and the same attributes that make us successful as physicians (type-A behavior, obsessive-compulsive commitment to our profession) put us at risk for professional burnout (see “Who is most at risk for burnout?”). Those predilections combine with the forces from the world in which we live and practice to increase this threat (TABLE 1). Conditions in which there are weak retention rates, high turnover, heavy workloads, and low staffing levels or staffing shortages increase the risk of burnout and, when burnout is present, are associated with a degraded quality of care.5
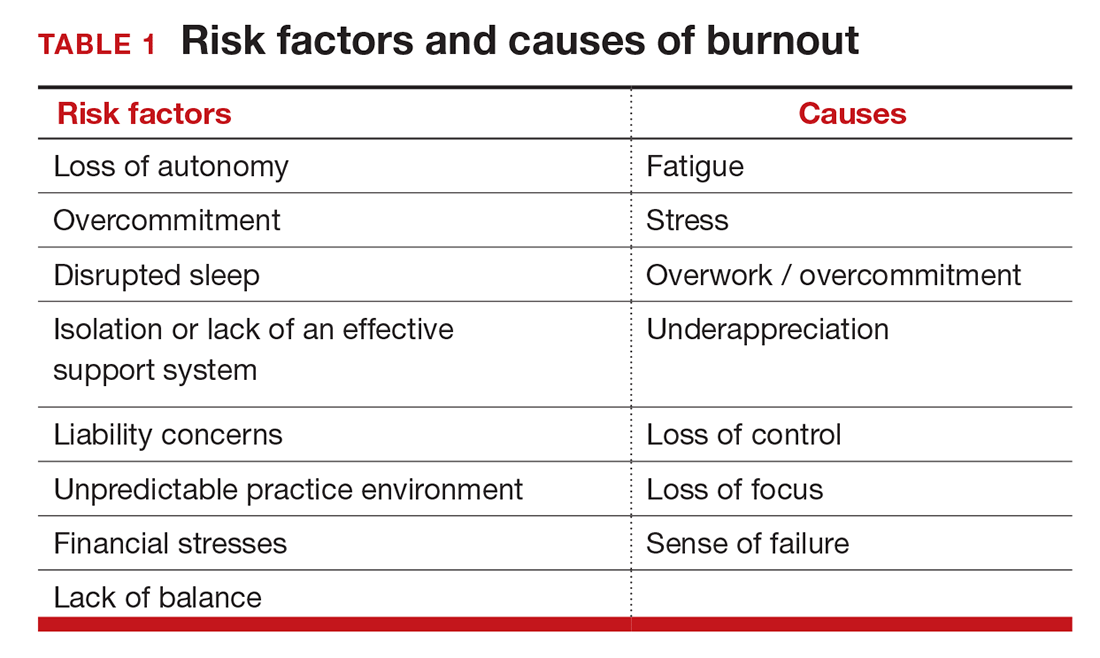
Does stress cause burnout?
Stress is often seen as the reason for burnout. Research shows that there is no single source of burnout,6 however, and a number of factors combine to cause this physical or mental collapse. Stress can be a positive or negative factor in our performance. Too little stress and we feel underutilized; too much stress and we collapse from the strain.
There is a middle ground where stress and expectations keep us focused and at peak productivity (FIGURE 1). The key is the balance between control and demand: When we have a greater level of control, we can handle high demands (FIGURE 2). It is when we lack that control that high demands result in what has been called “toxic stress,” and we collapse under the strain.
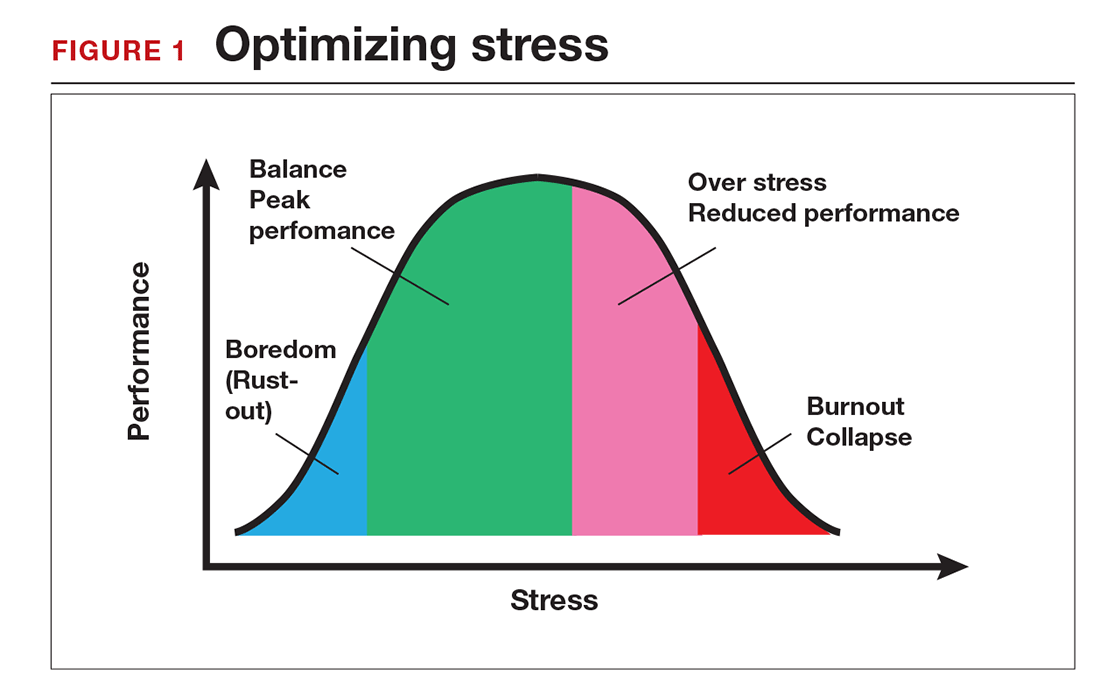
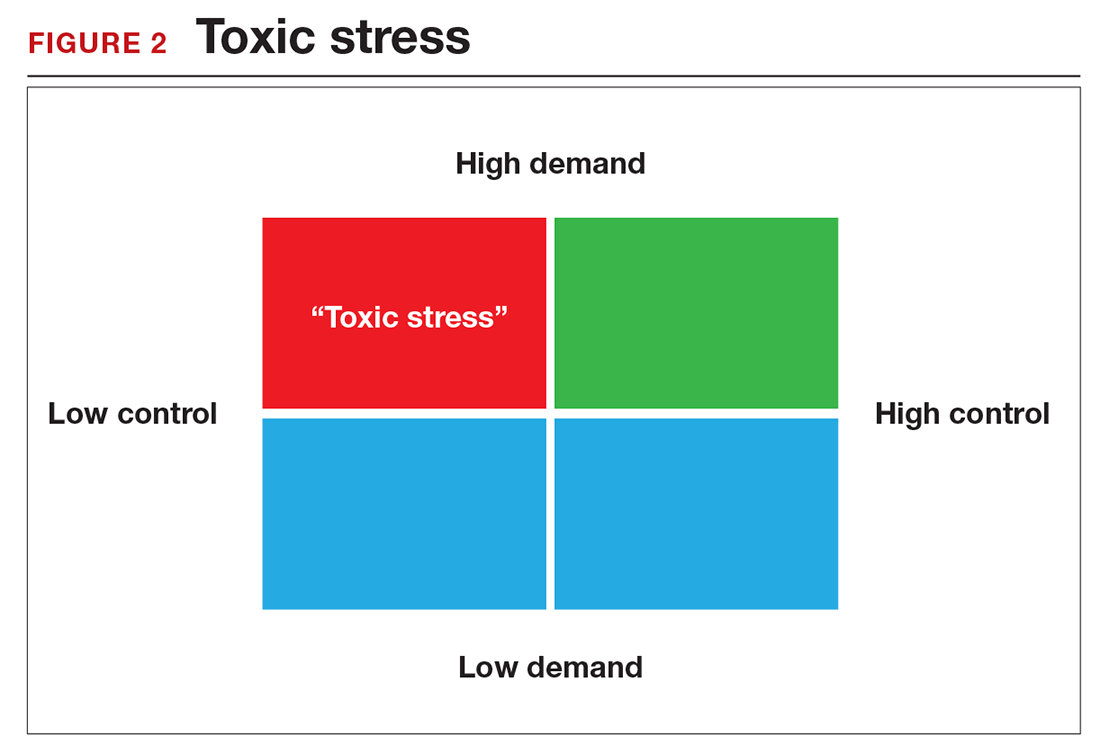
The impact of burnout
Burnout is associated with reduced performance and job satisfaction, increased rates of illness and absenteeism, accidents, premature retirement, and even premature death. Physically, stress induces the dry mouth, dilated pupils, and release of adrenalin and noradrenalin associated with the “fight-or-flight” reaction. The degree to which the physical, emotional, and professional symptoms are manifest depends on the depth or stage of burnout present (TABLE 2). Overall, burnout is associated with an increased risk for physical illness.7 Economically, the impact of physician burnout (for physicians practicing in Canada) has been estimated to be $213.1 million,8 which includes $185.2 million due to early retirement and $27.9 million due to reduced clinical hours.
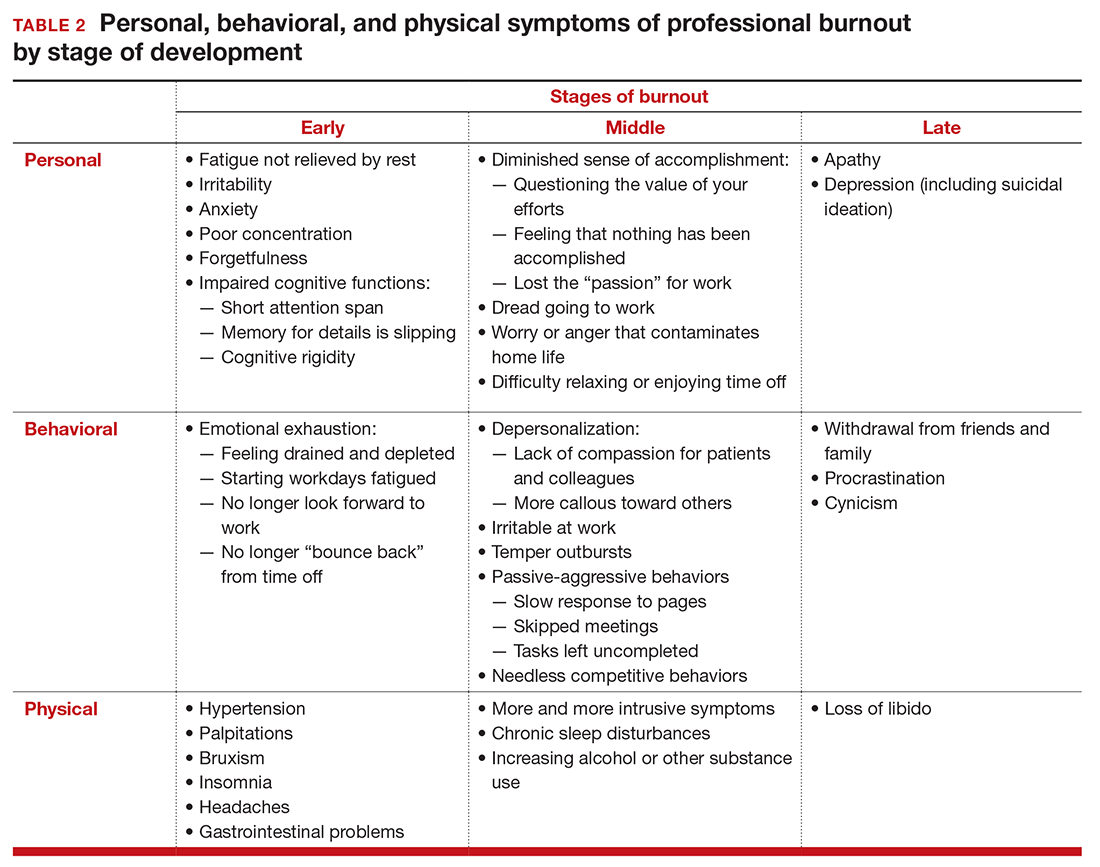
“Do I have burnout?”
We all suffer from fatigue and have stress, but do we have burnout? With so many myths surrounding stress and burnout, it is sometimes hard to know where the truth lies. Some of those myths say that:
- you can leave your troubles at home
- mental stress does not affect physical performance
- stress is only for wimps
- stress and burnout are chemical imbalances that can be treated with medications
- stress is always bad
- burnout will get better if you just give it more time.
Maslach Burnout Inventory. The effective “gold standard” for diagnosing burnout is the Maslach Burnout Inventory,9 which operationalizes burnout as a 3-dimensional syndrome made up of exhaustion, cynicism, and inefficacy. Other diagnostic tools have been introduced10 but have not gained the wide acceptance of the Maslach Inventory. Some authors have argued that burnout and depression represent different, closely spaced points along a spectrum and that any effort to separate them may be artificial.11,12
The Maslach Burnout Inventory consists of a survey of 22 items; it requires a fee to take and is interpreted by a qualified individual. A simpler screening test consists of 10 questions (TABLE 3). If you answer “yes” to 5 or more of the questions, you probably have burnout. An even quicker test is to see, when you go on vacation, if your symptoms disappear. If so, you are not depressed; you have burnout. (If you cannot even go on vacation, then it is almost certain.)
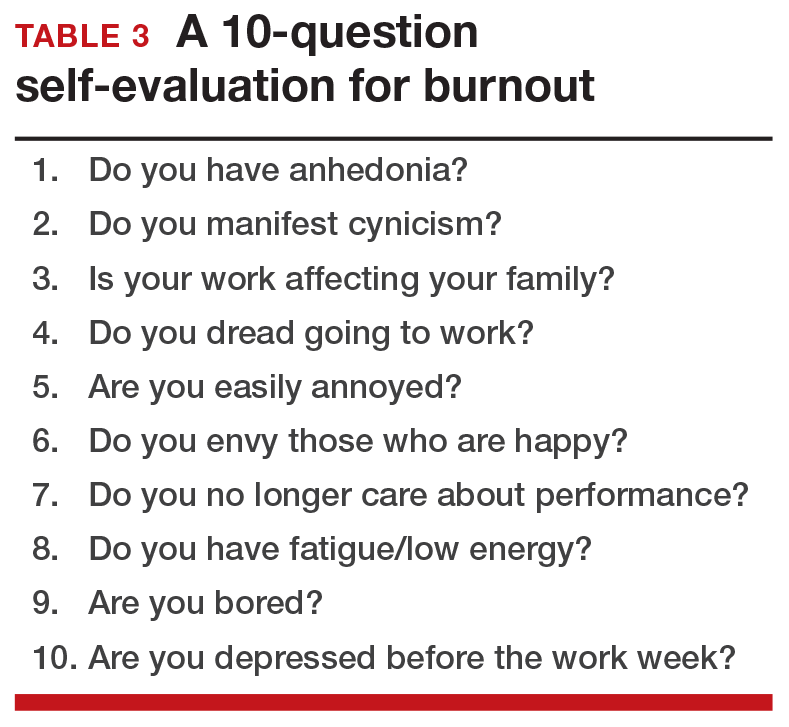
12 stages of burnout. Psychologists Herbert Freudenberger and Gail North have theorized that the burnout process can be divided into 12 phases (TABLE 4).13 These stages are not necessarily sequential—some may be absent and others may present simultaneously. It is easy to see how these can represent stages in a potentially spiraling series of behaviors and changes that result in complete dysfunction. It is also easy to understand that the characteristics that are associated with success in medical school, clinical training, and practice, such as high expectations, placing the needs of others above our own, and a desire to prove oneself, virtually define the first 3 stages.
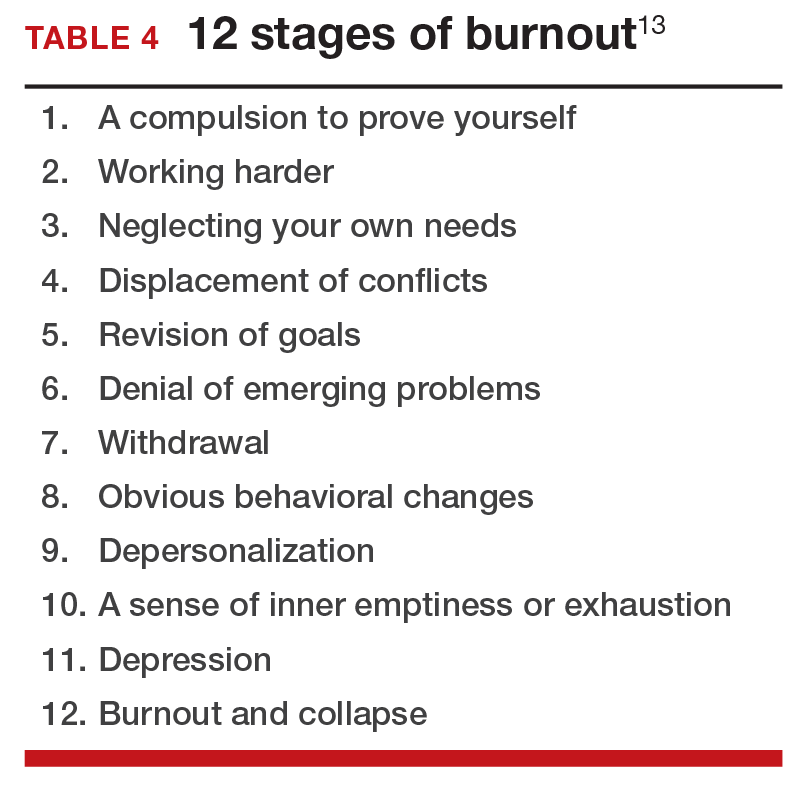
Approaches for burnout control and prevention
There are some simple steps we can take to reduce the risk of burnout or to reverse its effects. Because fatigue and stress are 2 of the greatest risk factors, reducing these is a good place to start.
Prioritize sleep. When it comes to fatigue, that one is easy: get some sleep. Physicians tend to sleep fewer hours than the general population and what we get is often not the type that is restful and restorative.14 Just reducing the number of hours worked is not enough, as a number of studies have found.15 The rest must result in relaxation.
e Stress reduction may seem a more difficult goal than getting more sleep. In reality, there are several simple approaches to use to reduce stress:
- Even though we all have busy clinical schedules, take short breaks to rest, sing, laugh, and exercise. Even breaks as short as 10 minutes can be effective.16
- Separate work from private life by taking a short break to resolve issues before heading home. Avoiding “baggage” or homework will go a long way to giving you the perspective you need from your time off. This may also mean that you have to delegate tasks, share chores, or get carry-out for dinner.
- Set meaningful and realistic goals for yourself professionally and personally. Do not expect or demand more than is possible. This will mean setting priorities and recognizing that some tasks may have to wait.
- Finally, do not forget to pay yourself with hobbies and activities that you enjoy.
Take action
If you feel the effects of burnout tugging at your coattails, you can reduce the effects, deal with the sources, and improve your attitude (TABLE 5). Rest and relaxation will go a long way to helping, but do not forget to take care of your physical well-being with a healthy diet, exercise, and health checkups. Deal with the sources of burnout by identifying the stressors, setting realistic priorities, and practicing good time management.
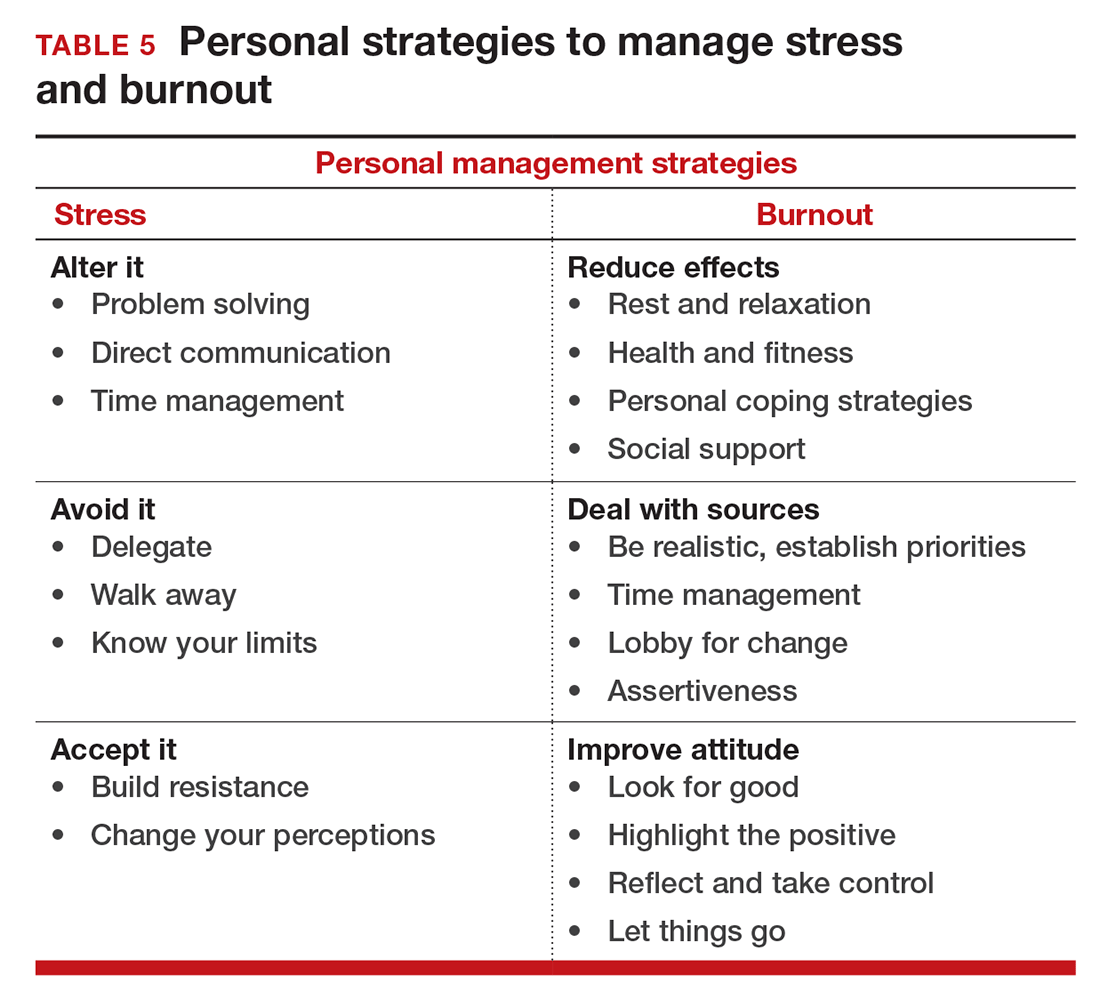
You also should lobby for changes that will increase your control and reduce unnecessary obstacles to completing your goals. Be your own best advocate. Look for the good and try to identify at least one instance during the day where your presence or acts made a difference. In the end, it is like Smokey the Bear says, “Only you can prevent burnout.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
It sometimes seems that the pace of life, and its stresses, have spiraled out of control: There just never seems to be enough time to deal with all the directions in which we are pulled. This easily can lead to the exhaustion of physical or emotional strength or motivation, otherwise known as “burnout.” Burnout is physical or mental collapse caused by overwork or stress and we are all at risk of suffering it. Conflicting demands on our time, loss of control (real or imagined), and a diminishing sense of worth grind at us from every direction.
In general, having some control over schedule and hours worked is associated with reductions in burnout and improved job satisfaction.1 But this is not always the case. Well-intentioned efforts to reduce workload, such as the electronic medical records or physician order entry systems, have actually made the problem worse.2 The seeming level of control that comes with being the chair of an obstetrics and gynecology department does not necessarily reduce burnout rates,3 and neither does the perceived resilience of mental health professionals, who still report burnout rates that approach 25%.4
This article continues the focus on recalibrating work/life balance that began last month with “ObGyn burnout: ACOG takes aim,” by Lucia DiVenere, MA, and the peer-to-peer audiocast with Ms. DiVenere and myself titled “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?” Here, I identify the causes and symptoms of burnout and provide specific tools to help you develop resilience.
Who is most at risk for burnout?
Estimates range from 40% to 75% of ObGyns currently suffer from professional burnout, making the lifetime risk a virtual certainty.1−3 The idea of professional burnout is not new, but wider recognition of the alarming rates of burnout is very current.4,5 A recent survey of gynecologic oncologists6 found that of those studied 30% scored high for emotional exhaustion, 10% high for depersonalization, and 11% low for personal accomplishment. Overall, 32% of physicians had scores indicating burnout. More worrisome was that 33% screened positive for depression, 13% had a history of suicidal ideation, 15% screened positive for alcohol abuse, and 34% reported impaired quality of life. Almost 40% would not encourage their children to enter medicine and more than 10% said that they would not enter medicine again if they had to do it over.
Residents and those at mid-career are particularly vulnerable,7 with resident burnout rates reported to be as high as 75%.8 Of surveyed residents in a 2012 study, 13% satisfied all 3 subscale scores for high burnout and greater than 50% had high levels of depersonalization and emotional exhaustion. Those with high levels of emotional exhaustion were less satisfied with their careers, regretted choosing obstetrics and gynecology, and had higher rates of depression—all findings consistent with older studies.
9,10
References
- Peckham C. Medscape Lifestyle Report 2016: Bias and Burnout. Medscape website. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed July 7, 2016.
- Shanafelt TD, Boone, S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385.
- Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240–242.
- Lee YY, Medford AR, Halim AS. Burnout in physicians. J R Coll Physicians Edinb. 2015;45(2):104–107.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Rath KS, Huffman LB, Phillips GS, Carpenter KM, Fowler JM. Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol. 2015;213(6):824.e1–e9.
- Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367.
- Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–395.
- Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195(5):1444–1449.
- Castelo-Branco C, Figueras F, Eixarch E, et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114(1):94–98
Why burnout occurs
Simply identifying ourselves as professionals and the same attributes that make us successful as physicians (type-A behavior, obsessive-compulsive commitment to our profession) put us at risk for professional burnout (see “Who is most at risk for burnout?”). Those predilections combine with the forces from the world in which we live and practice to increase this threat (TABLE 1). Conditions in which there are weak retention rates, high turnover, heavy workloads, and low staffing levels or staffing shortages increase the risk of burnout and, when burnout is present, are associated with a degraded quality of care.5
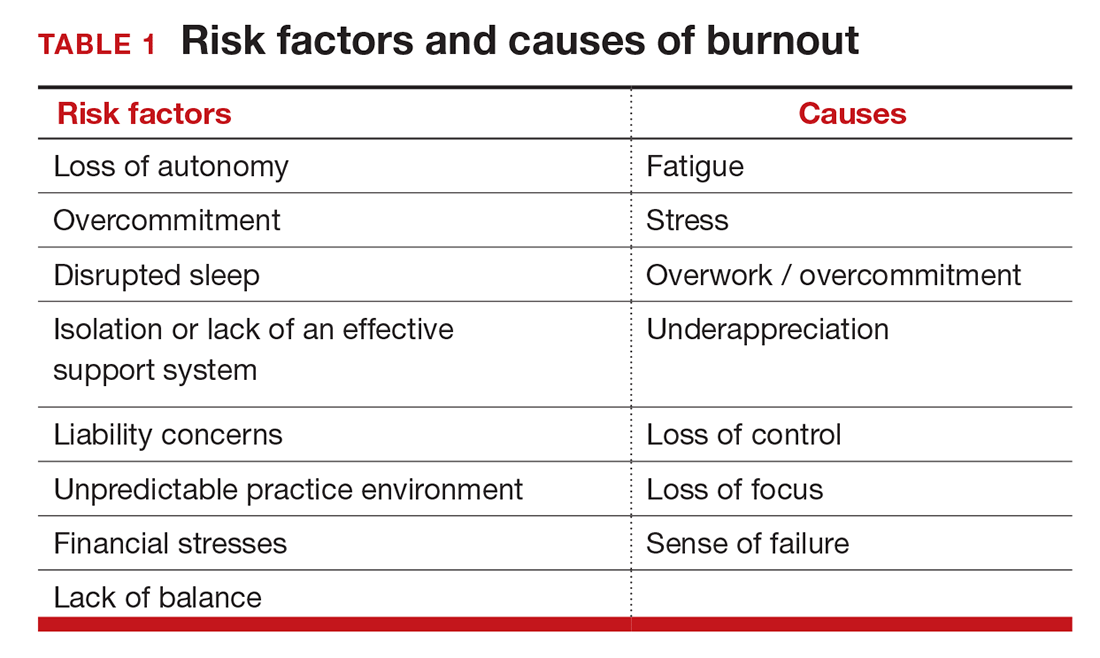
Does stress cause burnout?
Stress is often seen as the reason for burnout. Research shows that there is no single source of burnout,6 however, and a number of factors combine to cause this physical or mental collapse. Stress can be a positive or negative factor in our performance. Too little stress and we feel underutilized; too much stress and we collapse from the strain.
There is a middle ground where stress and expectations keep us focused and at peak productivity (FIGURE 1). The key is the balance between control and demand: When we have a greater level of control, we can handle high demands (FIGURE 2). It is when we lack that control that high demands result in what has been called “toxic stress,” and we collapse under the strain.
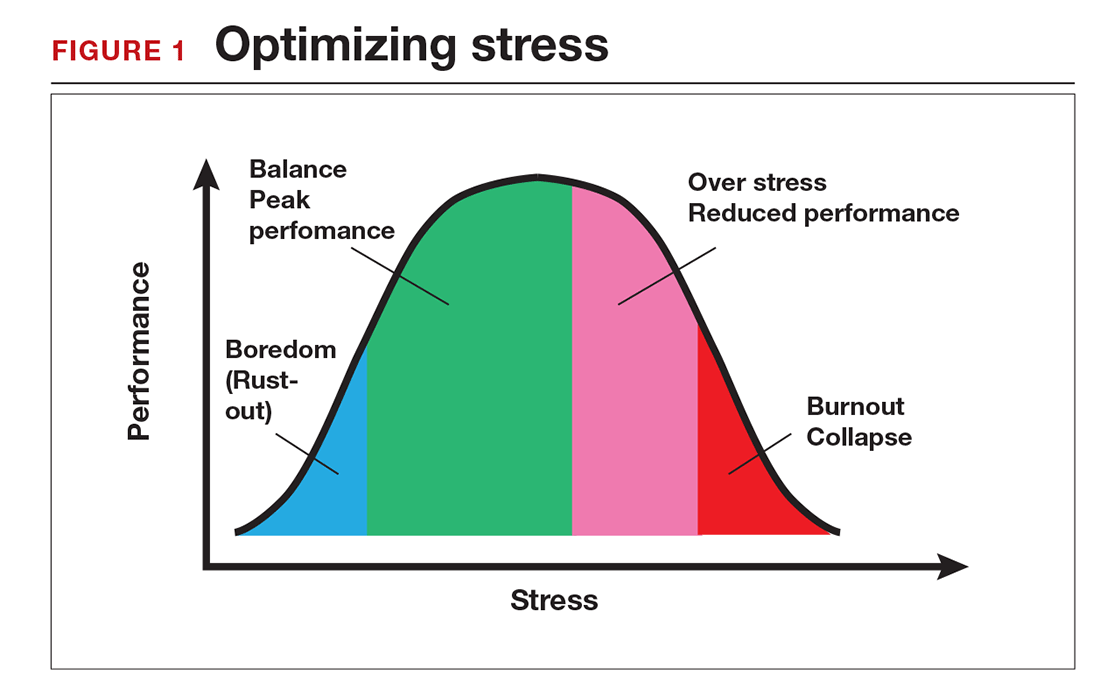
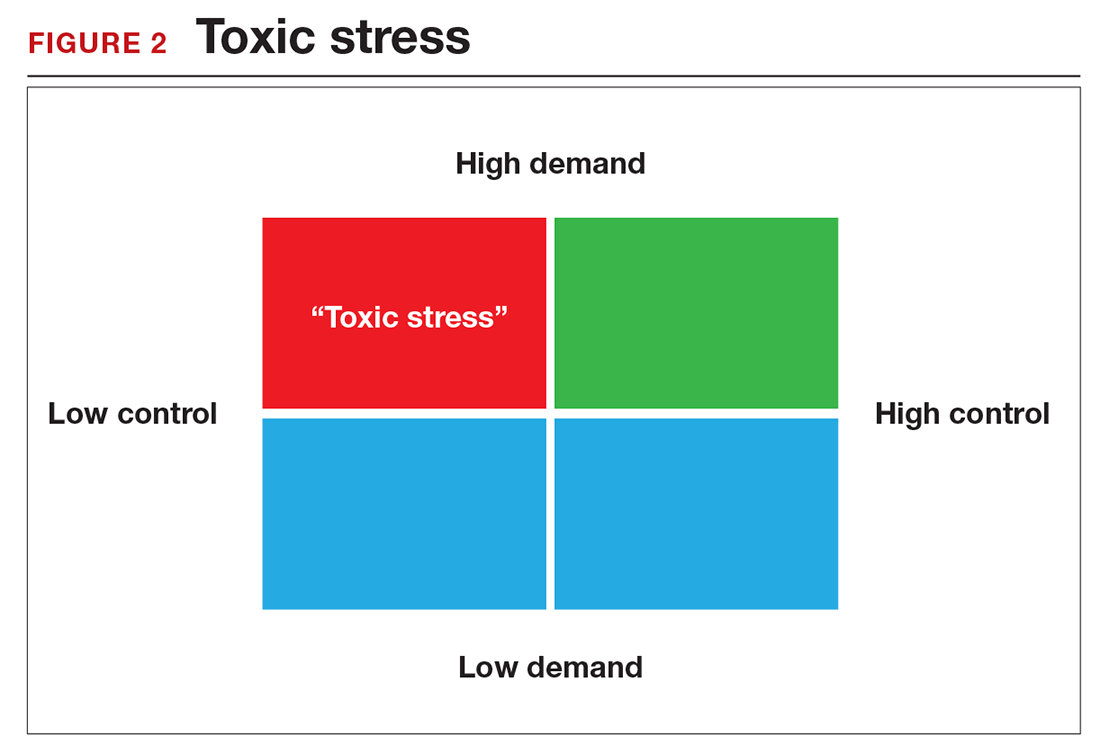
The impact of burnout
Burnout is associated with reduced performance and job satisfaction, increased rates of illness and absenteeism, accidents, premature retirement, and even premature death. Physically, stress induces the dry mouth, dilated pupils, and release of adrenalin and noradrenalin associated with the “fight-or-flight” reaction. The degree to which the physical, emotional, and professional symptoms are manifest depends on the depth or stage of burnout present (TABLE 2). Overall, burnout is associated with an increased risk for physical illness.7 Economically, the impact of physician burnout (for physicians practicing in Canada) has been estimated to be $213.1 million,8 which includes $185.2 million due to early retirement and $27.9 million due to reduced clinical hours.
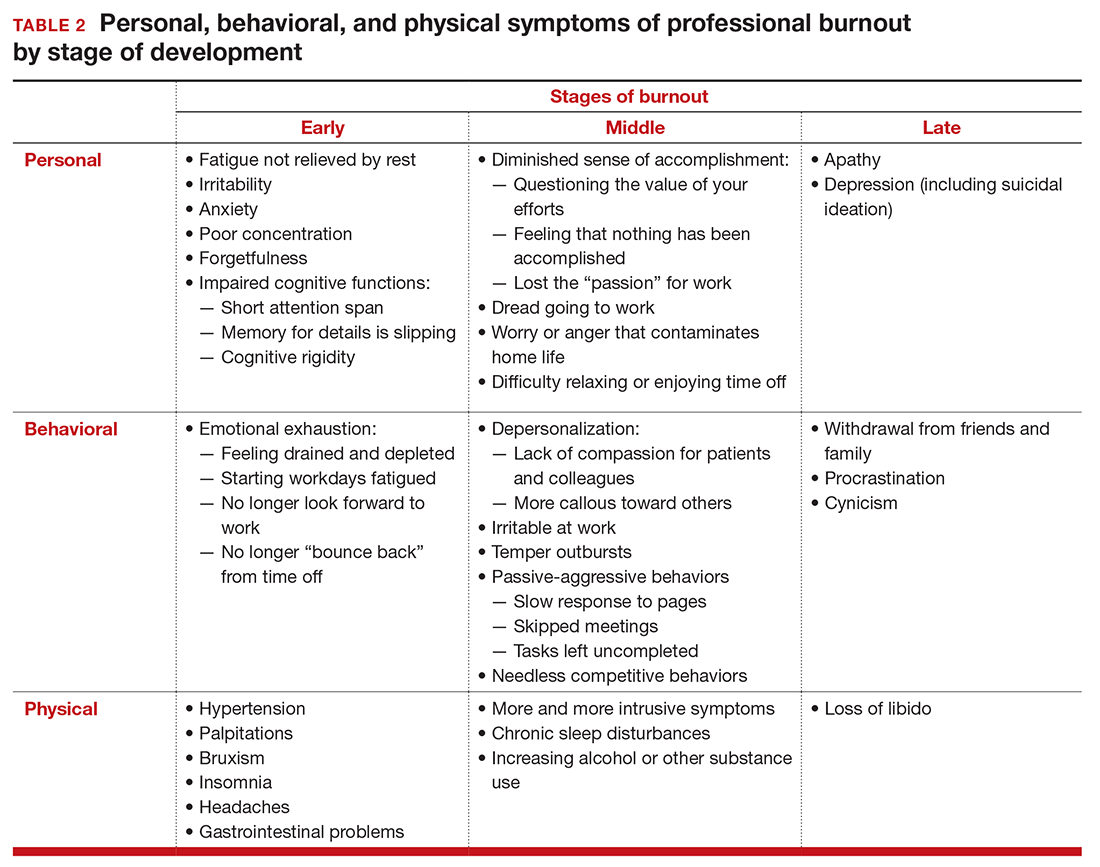
“Do I have burnout?”
We all suffer from fatigue and have stress, but do we have burnout? With so many myths surrounding stress and burnout, it is sometimes hard to know where the truth lies. Some of those myths say that:
- you can leave your troubles at home
- mental stress does not affect physical performance
- stress is only for wimps
- stress and burnout are chemical imbalances that can be treated with medications
- stress is always bad
- burnout will get better if you just give it more time.
Maslach Burnout Inventory. The effective “gold standard” for diagnosing burnout is the Maslach Burnout Inventory,9 which operationalizes burnout as a 3-dimensional syndrome made up of exhaustion, cynicism, and inefficacy. Other diagnostic tools have been introduced10 but have not gained the wide acceptance of the Maslach Inventory. Some authors have argued that burnout and depression represent different, closely spaced points along a spectrum and that any effort to separate them may be artificial.11,12
The Maslach Burnout Inventory consists of a survey of 22 items; it requires a fee to take and is interpreted by a qualified individual. A simpler screening test consists of 10 questions (TABLE 3). If you answer “yes” to 5 or more of the questions, you probably have burnout. An even quicker test is to see, when you go on vacation, if your symptoms disappear. If so, you are not depressed; you have burnout. (If you cannot even go on vacation, then it is almost certain.)
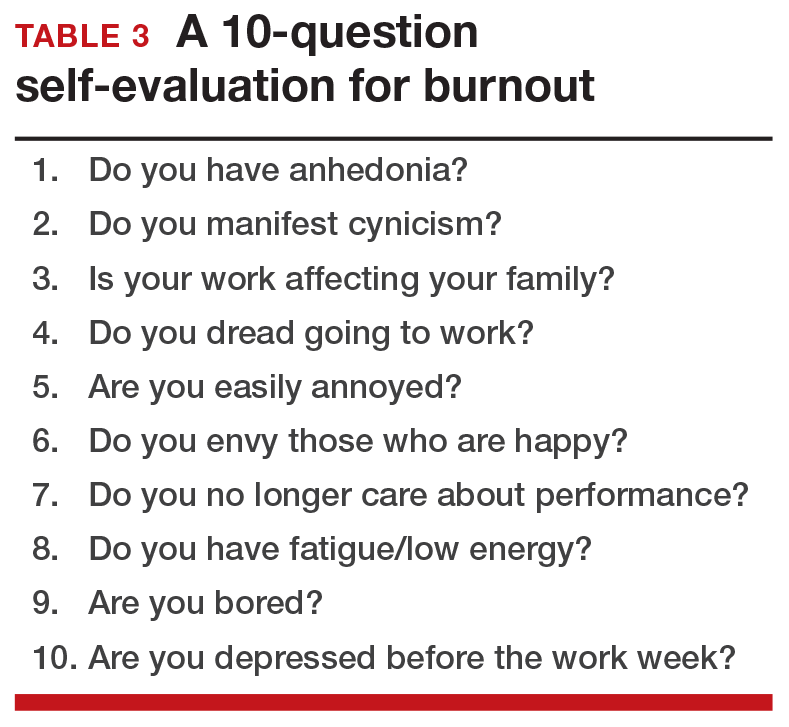
12 stages of burnout. Psychologists Herbert Freudenberger and Gail North have theorized that the burnout process can be divided into 12 phases (TABLE 4).13 These stages are not necessarily sequential—some may be absent and others may present simultaneously. It is easy to see how these can represent stages in a potentially spiraling series of behaviors and changes that result in complete dysfunction. It is also easy to understand that the characteristics that are associated with success in medical school, clinical training, and practice, such as high expectations, placing the needs of others above our own, and a desire to prove oneself, virtually define the first 3 stages.
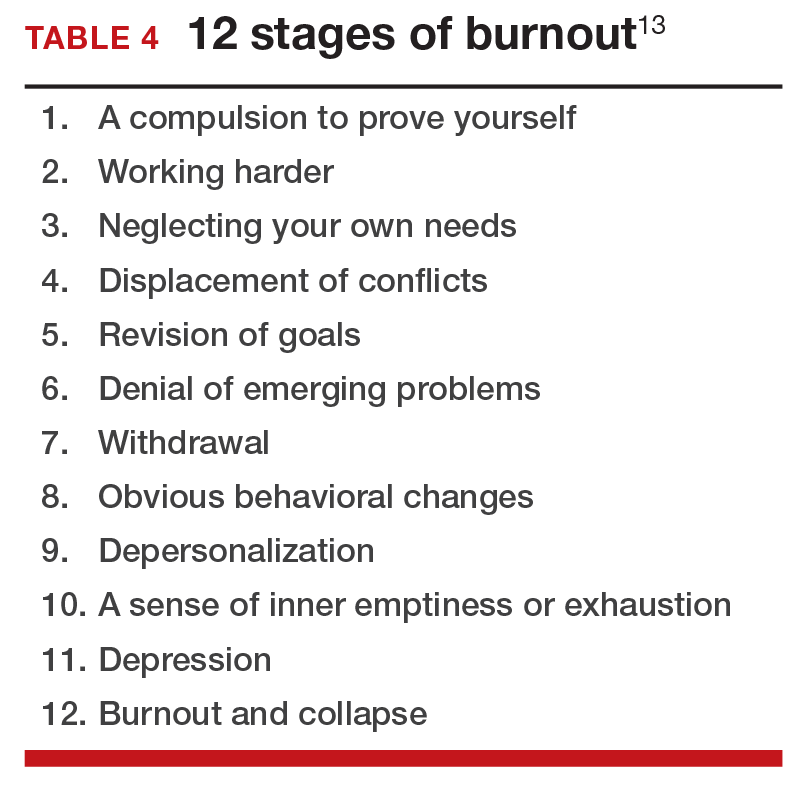
Approaches for burnout control and prevention
There are some simple steps we can take to reduce the risk of burnout or to reverse its effects. Because fatigue and stress are 2 of the greatest risk factors, reducing these is a good place to start.
Prioritize sleep. When it comes to fatigue, that one is easy: get some sleep. Physicians tend to sleep fewer hours than the general population and what we get is often not the type that is restful and restorative.14 Just reducing the number of hours worked is not enough, as a number of studies have found.15 The rest must result in relaxation.
e Stress reduction may seem a more difficult goal than getting more sleep. In reality, there are several simple approaches to use to reduce stress:
- Even though we all have busy clinical schedules, take short breaks to rest, sing, laugh, and exercise. Even breaks as short as 10 minutes can be effective.16
- Separate work from private life by taking a short break to resolve issues before heading home. Avoiding “baggage” or homework will go a long way to giving you the perspective you need from your time off. This may also mean that you have to delegate tasks, share chores, or get carry-out for dinner.
- Set meaningful and realistic goals for yourself professionally and personally. Do not expect or demand more than is possible. This will mean setting priorities and recognizing that some tasks may have to wait.
- Finally, do not forget to pay yourself with hobbies and activities that you enjoy.
Take action
If you feel the effects of burnout tugging at your coattails, you can reduce the effects, deal with the sources, and improve your attitude (TABLE 5). Rest and relaxation will go a long way to helping, but do not forget to take care of your physical well-being with a healthy diet, exercise, and health checkups. Deal with the sources of burnout by identifying the stressors, setting realistic priorities, and practicing good time management.
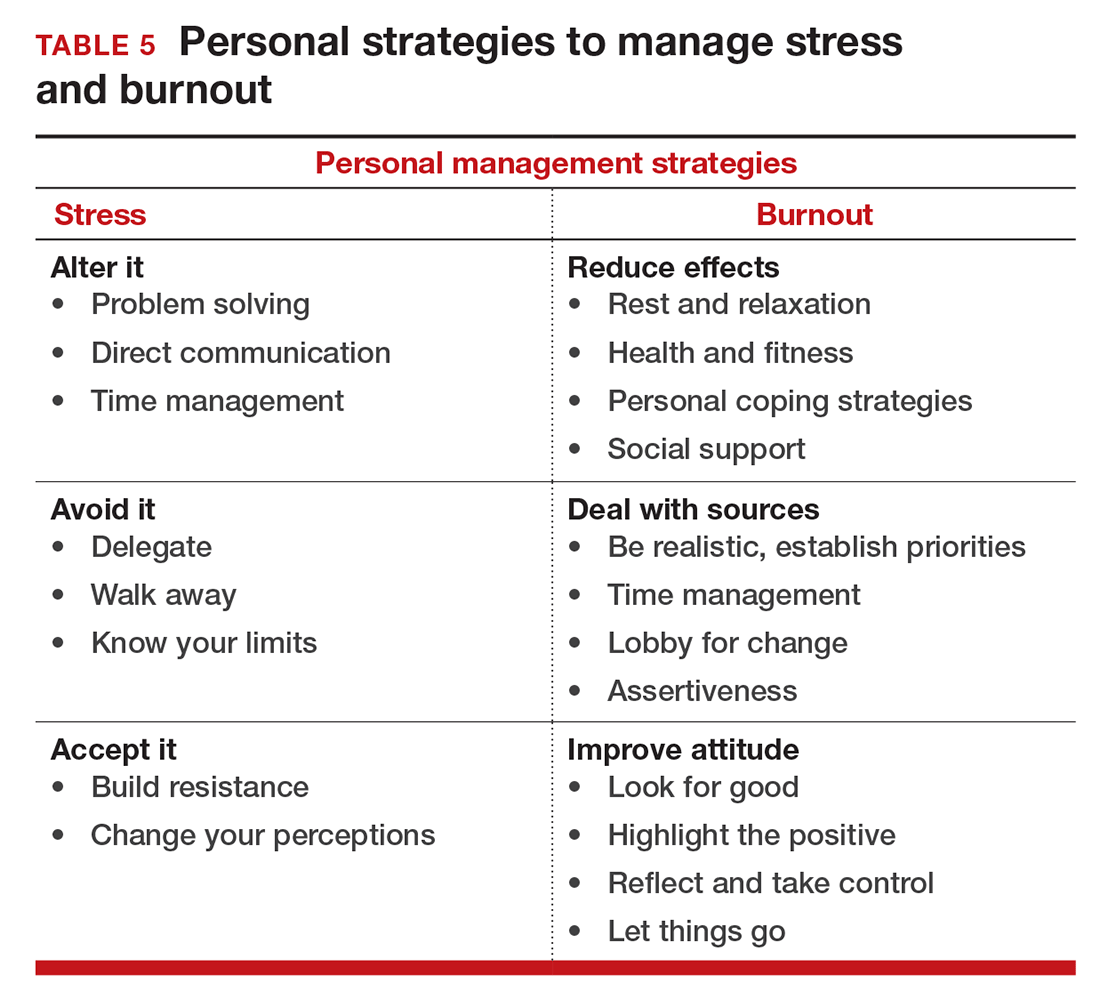
You also should lobby for changes that will increase your control and reduce unnecessary obstacles to completing your goals. Be your own best advocate. Look for the good and try to identify at least one instance during the day where your presence or acts made a difference. In the end, it is like Smokey the Bear says, “Only you can prevent burnout.”
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007;109(4):949-955.
- Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848.
- Gabbe SG, Melville J, Mandel L, Walker E. Burnout in chairs of obstetrics and gynecology: diagnosis, treatment, and prevention. Am J Obstet Gynecol. 2002;186(4):601-612.
- Kok BC, Herrell RK, Grossman SH, West JC, Wilk JE. Prevalence of professional burnout among military mental health service providers. Psychiatr Serv. 2016;67(1):137-140.
- Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, McGee H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293-307.
- Streu R, Hansen J, Abrahamse P, Alderman AK. Professional burnout among US plastic surgeons: results of a national survey. Ann Plast Surg. 2014;72(3):346-350.
- Honkonen T, Ahola K, Pertovaara M, et al. The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61(1):59-66.
- Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014;14:254.
- Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory Manual. Palo Alto, California: Consulting Psychologists Press, 1996.
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress. 2005;19(3):192-207.
- Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E. Comparative symptomatology of burnout and depression. J Health Psychol. 2013;18(6):782-787.
- Bianchi R, Schonfeld I S, Laurent E. Is burnout a depressive disorder? A re-examination with special focus on atypical depression. Intl J Stress Manag. 2014;21(4):307-324.
- Freudenberger HJ, North G. Women's burnout: How to spot it, how to reverse it, and how to prevent it. New York, New York: Doubleday, 1985.
- Abrams RM. Sleep deprivation. Obstet Gynecol Clin North Am. 2015;42(3):493-506.
- Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47-54.
- Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: The personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255(4):625-633.
- Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007;109(4):949-955.
- Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848.
- Gabbe SG, Melville J, Mandel L, Walker E. Burnout in chairs of obstetrics and gynecology: diagnosis, treatment, and prevention. Am J Obstet Gynecol. 2002;186(4):601-612.
- Kok BC, Herrell RK, Grossman SH, West JC, Wilk JE. Prevalence of professional burnout among military mental health service providers. Psychiatr Serv. 2016;67(1):137-140.
- Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, McGee H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293-307.
- Streu R, Hansen J, Abrahamse P, Alderman AK. Professional burnout among US plastic surgeons: results of a national survey. Ann Plast Surg. 2014;72(3):346-350.
- Honkonen T, Ahola K, Pertovaara M, et al. The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61(1):59-66.
- Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014;14:254.
- Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory Manual. Palo Alto, California: Consulting Psychologists Press, 1996.
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress. 2005;19(3):192-207.
- Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E. Comparative symptomatology of burnout and depression. J Health Psychol. 2013;18(6):782-787.
- Bianchi R, Schonfeld I S, Laurent E. Is burnout a depressive disorder? A re-examination with special focus on atypical depression. Intl J Stress Manag. 2014;21(4):307-324.
- Freudenberger HJ, North G. Women's burnout: How to spot it, how to reverse it, and how to prevent it. New York, New York: Doubleday, 1985.
- Abrams RM. Sleep deprivation. Obstet Gynecol Clin North Am. 2015;42(3):493-506.
- Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47-54.
- Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: The personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255(4):625-633.
In this Article
- Symptoms by stage of burnout
- Tips to reduce stress and burnout
- Who is most at risk for burnout?
What is the ideal gestational age for twin delivery to minimize perinatal deaths?
EXPERT COMMENTARY
Cheong-See and colleagues conducted a comprehensive review and analysis of 32 studies of uncomplicated dichorionic and monochorionic twin pregnancies to determine the risks of stillbirth and neonatal complications by gestational age.
Details of the study
The authors searched major databases for studies on twin pregnancies that reported rates of stillbirth as well as neonatal outcomes (neonatal mortality was defined as death up to 28 days after delivery). A total of 32 studies were included in the analysis, with 29,685 dichorionic and 5,486 monochorionic pregnancies in 35,171 women. The authors estimated the gestational-age specific differences in risk for stillbirths and neonatal deaths after 34 weeks’ gestation.
In dichorionic pregnancies, the prospective weekly pooled risk of stillbirths from expectant management and the risk of neonatal mortality from delivery were balanced at 37 weeks of gestation (risk difference, 1.2/1,000, 95% CI, −1.3 to 3.6; I2 = 0%). In monochorionic pregnancies, after 36 weeks there was a trend toward an increase in stillbirths compared with neonatal deaths, with a pooled risk difference of 2.5/1,000 (95% CI, −12.4 to 17.4; I2 = 0%). Neonatal morbidity rates were consistently reduced with increasing gestational age in both monochorionic and dichorionic pregnancies.
The researchers’ recommendations
The authors recommended that dichorionic pregnancies be delivered at 37 weeks and that the evidence for delivery of monochorionic twins prior to 36 weeks is lacking. While the analysis is comprehensive and well done, it cannot escape the limitations that afflict all systematic reviews and meta-analyses, and these limitations are well addressed by the authors. Several factors, however, warrant caution regarding the adoption of the authors’ recommendations.
Cautions. First, determination of chorionicity may not have been accurate in all of the studies reviewed. Additionally, we have no data on how these pregnancies were managed with respect to antepartum fetal surveillance, ultrasound surveillance for growth and discordancy, and management of labor and delivery. There are no data on the quality of the ultrasound examinations being performed at each of the centers.
Also, the factors that may increase the risk of stillbirth are not necessarily the same factors that may influence the neonatal death rate, and this review moves between the use of these terms (stillbirth rate, neonatal mortality rate, and perinatal mortality rate) fairly frequently. For example, an improperly managed labor, an unanticipated difficult breech extraction, or the need for emergent cesarean delivery of the second twin might contribute to the neonatal death rate irrespective of gestational age at delivery. The authors acknowledge that outcomes may have been influenced by differences in obstetric and neonatal management of twin pregnancies that were observed between centers. Another concern is the authors’ use of unpublished aggregate and individual patient data.
While this comprehensive and very well conducted review and meta-analysis highlights the complexity of balancing stillbirth risk against neonatal mortality risk, the limitations of the study are too substantial to allow for any change in current practice. My recommendation for the timing of twin delivery is to adhere to the guidelines that are currently supported by both the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists.1 These guidelines recommend that, for dichorionic-diamniotic twin pregnancy, the general timing of delivery be at early term, with suggested specific timing at 38 0/7 to 38 6/7 weeks of gestation. For monochorionic-diamniotic twin pregnancy, the general timing of delivery may be at late preterm/early term, with suggested specific timing at 34 0/7 to 37 6/7 weeks of gestation. Delivery decisions made within these date ranges depend on numerous factors discussed in the guidelines, and timing of delivery should be individualized.1
-- JOHN T. REPKE, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice, Society for Maternal-Fetal Medicine. ACOG Committee Opinion No. 560. Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910. Reaffirmed 2015.
EXPERT COMMENTARY
Cheong-See and colleagues conducted a comprehensive review and analysis of 32 studies of uncomplicated dichorionic and monochorionic twin pregnancies to determine the risks of stillbirth and neonatal complications by gestational age.
Details of the study
The authors searched major databases for studies on twin pregnancies that reported rates of stillbirth as well as neonatal outcomes (neonatal mortality was defined as death up to 28 days after delivery). A total of 32 studies were included in the analysis, with 29,685 dichorionic and 5,486 monochorionic pregnancies in 35,171 women. The authors estimated the gestational-age specific differences in risk for stillbirths and neonatal deaths after 34 weeks’ gestation.
In dichorionic pregnancies, the prospective weekly pooled risk of stillbirths from expectant management and the risk of neonatal mortality from delivery were balanced at 37 weeks of gestation (risk difference, 1.2/1,000, 95% CI, −1.3 to 3.6; I2 = 0%). In monochorionic pregnancies, after 36 weeks there was a trend toward an increase in stillbirths compared with neonatal deaths, with a pooled risk difference of 2.5/1,000 (95% CI, −12.4 to 17.4; I2 = 0%). Neonatal morbidity rates were consistently reduced with increasing gestational age in both monochorionic and dichorionic pregnancies.
The researchers’ recommendations
The authors recommended that dichorionic pregnancies be delivered at 37 weeks and that the evidence for delivery of monochorionic twins prior to 36 weeks is lacking. While the analysis is comprehensive and well done, it cannot escape the limitations that afflict all systematic reviews and meta-analyses, and these limitations are well addressed by the authors. Several factors, however, warrant caution regarding the adoption of the authors’ recommendations.
Cautions. First, determination of chorionicity may not have been accurate in all of the studies reviewed. Additionally, we have no data on how these pregnancies were managed with respect to antepartum fetal surveillance, ultrasound surveillance for growth and discordancy, and management of labor and delivery. There are no data on the quality of the ultrasound examinations being performed at each of the centers.
Also, the factors that may increase the risk of stillbirth are not necessarily the same factors that may influence the neonatal death rate, and this review moves between the use of these terms (stillbirth rate, neonatal mortality rate, and perinatal mortality rate) fairly frequently. For example, an improperly managed labor, an unanticipated difficult breech extraction, or the need for emergent cesarean delivery of the second twin might contribute to the neonatal death rate irrespective of gestational age at delivery. The authors acknowledge that outcomes may have been influenced by differences in obstetric and neonatal management of twin pregnancies that were observed between centers. Another concern is the authors’ use of unpublished aggregate and individual patient data.
While this comprehensive and very well conducted review and meta-analysis highlights the complexity of balancing stillbirth risk against neonatal mortality risk, the limitations of the study are too substantial to allow for any change in current practice. My recommendation for the timing of twin delivery is to adhere to the guidelines that are currently supported by both the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists.1 These guidelines recommend that, for dichorionic-diamniotic twin pregnancy, the general timing of delivery be at early term, with suggested specific timing at 38 0/7 to 38 6/7 weeks of gestation. For monochorionic-diamniotic twin pregnancy, the general timing of delivery may be at late preterm/early term, with suggested specific timing at 34 0/7 to 37 6/7 weeks of gestation. Delivery decisions made within these date ranges depend on numerous factors discussed in the guidelines, and timing of delivery should be individualized.1
-- JOHN T. REPKE, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Cheong-See and colleagues conducted a comprehensive review and analysis of 32 studies of uncomplicated dichorionic and monochorionic twin pregnancies to determine the risks of stillbirth and neonatal complications by gestational age.
Details of the study
The authors searched major databases for studies on twin pregnancies that reported rates of stillbirth as well as neonatal outcomes (neonatal mortality was defined as death up to 28 days after delivery). A total of 32 studies were included in the analysis, with 29,685 dichorionic and 5,486 monochorionic pregnancies in 35,171 women. The authors estimated the gestational-age specific differences in risk for stillbirths and neonatal deaths after 34 weeks’ gestation.
In dichorionic pregnancies, the prospective weekly pooled risk of stillbirths from expectant management and the risk of neonatal mortality from delivery were balanced at 37 weeks of gestation (risk difference, 1.2/1,000, 95% CI, −1.3 to 3.6; I2 = 0%). In monochorionic pregnancies, after 36 weeks there was a trend toward an increase in stillbirths compared with neonatal deaths, with a pooled risk difference of 2.5/1,000 (95% CI, −12.4 to 17.4; I2 = 0%). Neonatal morbidity rates were consistently reduced with increasing gestational age in both monochorionic and dichorionic pregnancies.
The researchers’ recommendations
The authors recommended that dichorionic pregnancies be delivered at 37 weeks and that the evidence for delivery of monochorionic twins prior to 36 weeks is lacking. While the analysis is comprehensive and well done, it cannot escape the limitations that afflict all systematic reviews and meta-analyses, and these limitations are well addressed by the authors. Several factors, however, warrant caution regarding the adoption of the authors’ recommendations.
Cautions. First, determination of chorionicity may not have been accurate in all of the studies reviewed. Additionally, we have no data on how these pregnancies were managed with respect to antepartum fetal surveillance, ultrasound surveillance for growth and discordancy, and management of labor and delivery. There are no data on the quality of the ultrasound examinations being performed at each of the centers.
Also, the factors that may increase the risk of stillbirth are not necessarily the same factors that may influence the neonatal death rate, and this review moves between the use of these terms (stillbirth rate, neonatal mortality rate, and perinatal mortality rate) fairly frequently. For example, an improperly managed labor, an unanticipated difficult breech extraction, or the need for emergent cesarean delivery of the second twin might contribute to the neonatal death rate irrespective of gestational age at delivery. The authors acknowledge that outcomes may have been influenced by differences in obstetric and neonatal management of twin pregnancies that were observed between centers. Another concern is the authors’ use of unpublished aggregate and individual patient data.
While this comprehensive and very well conducted review and meta-analysis highlights the complexity of balancing stillbirth risk against neonatal mortality risk, the limitations of the study are too substantial to allow for any change in current practice. My recommendation for the timing of twin delivery is to adhere to the guidelines that are currently supported by both the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists.1 These guidelines recommend that, for dichorionic-diamniotic twin pregnancy, the general timing of delivery be at early term, with suggested specific timing at 38 0/7 to 38 6/7 weeks of gestation. For monochorionic-diamniotic twin pregnancy, the general timing of delivery may be at late preterm/early term, with suggested specific timing at 34 0/7 to 37 6/7 weeks of gestation. Delivery decisions made within these date ranges depend on numerous factors discussed in the guidelines, and timing of delivery should be individualized.1
-- JOHN T. REPKE, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice, Society for Maternal-Fetal Medicine. ACOG Committee Opinion No. 560. Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910. Reaffirmed 2015.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice, Society for Maternal-Fetal Medicine. ACOG Committee Opinion No. 560. Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910. Reaffirmed 2015.
ObGyn burnout: ACOG takes aim
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
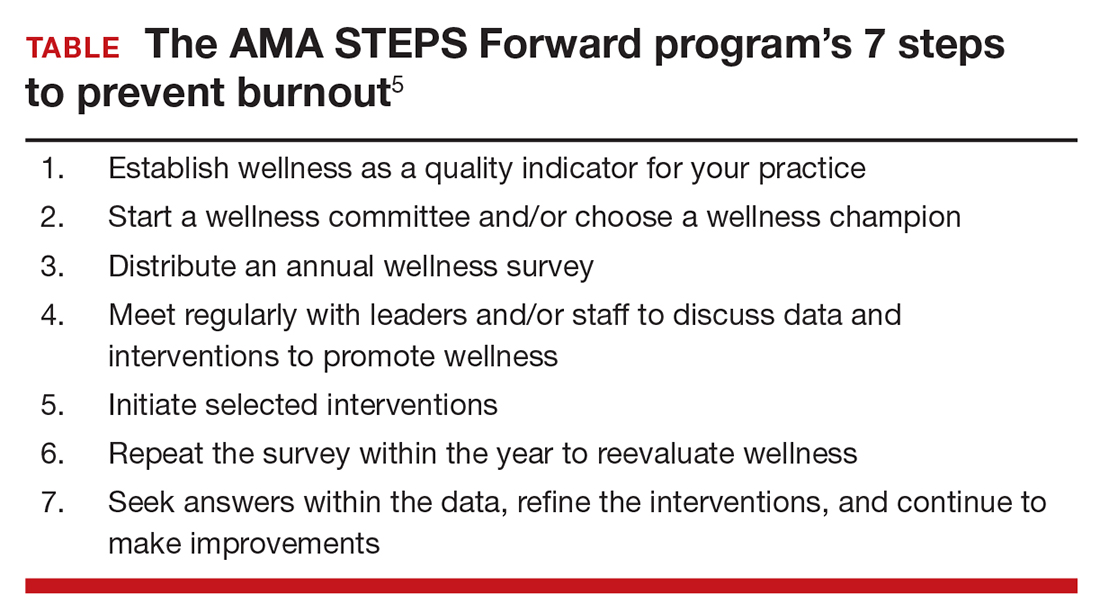
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
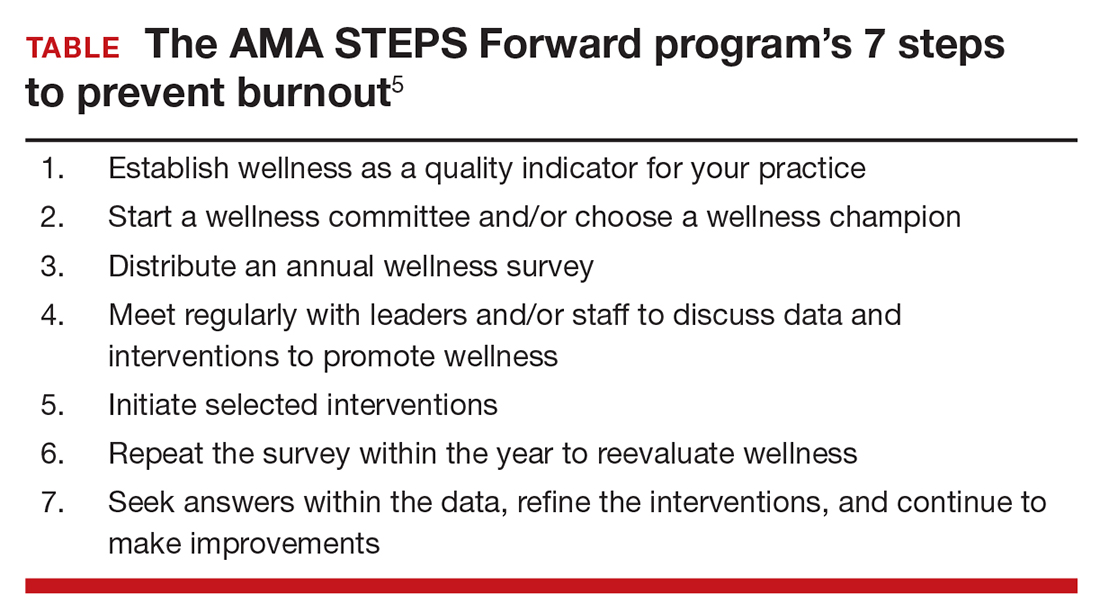
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
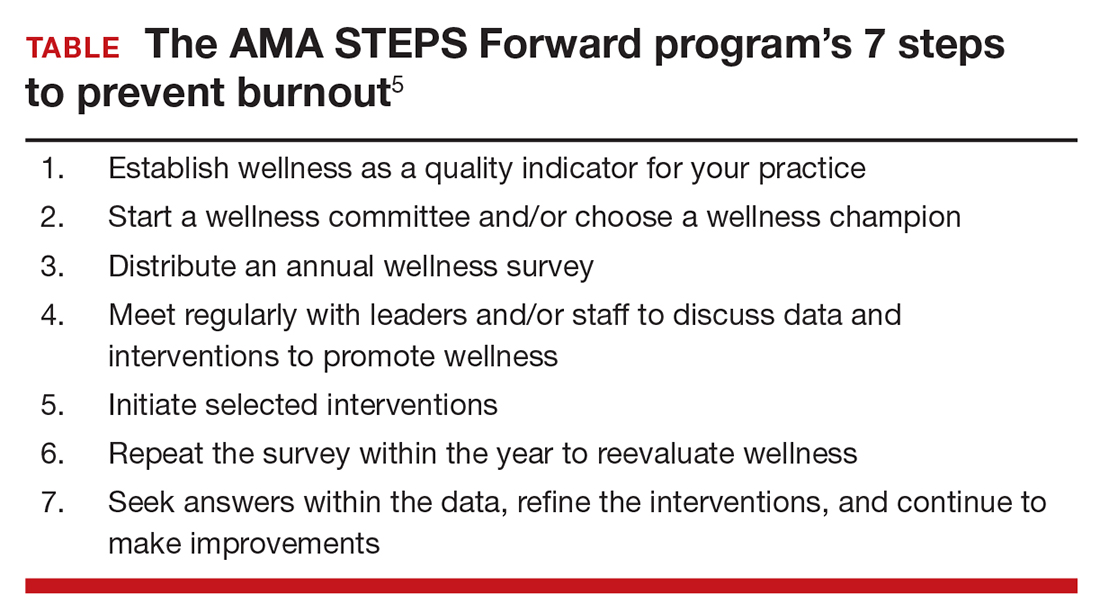
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
In this Article
- Developing outside passions
- Thomas Gellhaus, MD, encourages mentorship
- 7 steps to prevent burnout
Should lower uterine segment thickness measurement be included in the TOLAC decision-making process?
EXPERT COMMENTARY
After having a previous cesarean delivery (CD), women who subsequently become pregnant inevitably face the decision to undergo a repeat CD or attempt a trial of labor after cesarean (TOLAC). Currently in the United States, 83% of women with a prior uterine scar are delivered by repeat CD.1 According to the Consortium on Safe Labor, more than half of all CD indications are attributed to having a prior uterine scar.1 Furthermore, only 28% of women attempt a TOLAC, with a successful vaginal birth after cesarean (VBAC) rate of approximately 57%.1
The reason for the low TOLAC rate is multifactorial, but a primary concern may be the safety risk of a TOLAC as it relates to uterine rupture, a rare but potentially catastrophic complication. In a large, multicenter prospective observational trial of more than 17,800 women attempting a TOLAC, the symptomatic uterine rupture rate was 0.7%.2 As such, efforts to identify women at highest risk for uterine rupture and those with characteristics predictive of a successful VBAC have remained ongoing. Jastrow and colleagues have expanded this body of knowledge with their prospective cohort study.
Details of the study
The researchers assessed lower uterine segment thickness via vaginal and abdominal ultrasound at 34 to 38 weeks’ gestation in more than 1,850 women with a previous CD. Women enrolled in the trial were classified into 3 risk categories based on lower uterine segment thickness: high risk (<2.0 mm), intermediate risk (2.0 to 2.4 mm), and low risk (≥2.5 mm). The investigators’ objective was to estimate the occurrence of uterine rupture when this measurement was included in the decision-making process on mode of delivery.
An important aspect of this study involved how the provider discussed the mode of delivery with the patient after the lower uterine segment measurement was obtained. Both the provider and the patient were informed of the risk category, and further counseling included the following:
- average overall uterine rupture risk, 0.5% to 1%
- if <2.0 mm, uterine rupture risk likely >1%
- if ≥2.5 mm, uterine rupture risk likely <0.5%
- uterine rupture risks (including perinatal asphyxia and death)
- maternal and neonatal complications of cesarean
- estimation of likelihood for successful VBAC.
How did risk-stratified women fare?
In approximately 1,000 cases, the authors reported no symptomatic uterine ruptures. Of particular interest, however, is the rate of women attempting a TOLAC in each category:
- 194 women with high risk
- 9% underwent a TOLAC
- 82% had a successful vaginal birth
- 217 women with intermediate risk
- 42% underwent a TOLAC
- 78% had a successful vaginal birth
- 1,438 women with low risk
- 61% underwent a TOLAC
- 66% had a successful vaginal birth.
Considering cesarean scar defect
Finally, uterine scar defects at CD in those who underwent a TOLAC were 0/3 (0%), 5/21 (25%), and 20/276 (7%) in the high-, intermediate-, and low-risk groups, respectively. Given the observational nature of the study, the authors suggest that uterine scar dehiscence may be predictive of labor dystocia, but it remains unclear if it predicts or is a prerequisite for subsequent uterine rupture if labor occurs.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Zhang J, Troendle J, Reddy UM, et al; Consortium on Safe Labor. Am J Obstet Gynecol. 2010;203(4):326.e1–326.e10.
- Landon MB, Hauth JC, Leveno KJ, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;16;351(25):2581–2589.
EXPERT COMMENTARY
After having a previous cesarean delivery (CD), women who subsequently become pregnant inevitably face the decision to undergo a repeat CD or attempt a trial of labor after cesarean (TOLAC). Currently in the United States, 83% of women with a prior uterine scar are delivered by repeat CD.1 According to the Consortium on Safe Labor, more than half of all CD indications are attributed to having a prior uterine scar.1 Furthermore, only 28% of women attempt a TOLAC, with a successful vaginal birth after cesarean (VBAC) rate of approximately 57%.1
The reason for the low TOLAC rate is multifactorial, but a primary concern may be the safety risk of a TOLAC as it relates to uterine rupture, a rare but potentially catastrophic complication. In a large, multicenter prospective observational trial of more than 17,800 women attempting a TOLAC, the symptomatic uterine rupture rate was 0.7%.2 As such, efforts to identify women at highest risk for uterine rupture and those with characteristics predictive of a successful VBAC have remained ongoing. Jastrow and colleagues have expanded this body of knowledge with their prospective cohort study.
Details of the study
The researchers assessed lower uterine segment thickness via vaginal and abdominal ultrasound at 34 to 38 weeks’ gestation in more than 1,850 women with a previous CD. Women enrolled in the trial were classified into 3 risk categories based on lower uterine segment thickness: high risk (<2.0 mm), intermediate risk (2.0 to 2.4 mm), and low risk (≥2.5 mm). The investigators’ objective was to estimate the occurrence of uterine rupture when this measurement was included in the decision-making process on mode of delivery.
An important aspect of this study involved how the provider discussed the mode of delivery with the patient after the lower uterine segment measurement was obtained. Both the provider and the patient were informed of the risk category, and further counseling included the following:
- average overall uterine rupture risk, 0.5% to 1%
- if <2.0 mm, uterine rupture risk likely >1%
- if ≥2.5 mm, uterine rupture risk likely <0.5%
- uterine rupture risks (including perinatal asphyxia and death)
- maternal and neonatal complications of cesarean
- estimation of likelihood for successful VBAC.
How did risk-stratified women fare?
In approximately 1,000 cases, the authors reported no symptomatic uterine ruptures. Of particular interest, however, is the rate of women attempting a TOLAC in each category:
- 194 women with high risk
- 9% underwent a TOLAC
- 82% had a successful vaginal birth
- 217 women with intermediate risk
- 42% underwent a TOLAC
- 78% had a successful vaginal birth
- 1,438 women with low risk
- 61% underwent a TOLAC
- 66% had a successful vaginal birth.
Considering cesarean scar defect
Finally, uterine scar defects at CD in those who underwent a TOLAC were 0/3 (0%), 5/21 (25%), and 20/276 (7%) in the high-, intermediate-, and low-risk groups, respectively. Given the observational nature of the study, the authors suggest that uterine scar dehiscence may be predictive of labor dystocia, but it remains unclear if it predicts or is a prerequisite for subsequent uterine rupture if labor occurs.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
After having a previous cesarean delivery (CD), women who subsequently become pregnant inevitably face the decision to undergo a repeat CD or attempt a trial of labor after cesarean (TOLAC). Currently in the United States, 83% of women with a prior uterine scar are delivered by repeat CD.1 According to the Consortium on Safe Labor, more than half of all CD indications are attributed to having a prior uterine scar.1 Furthermore, only 28% of women attempt a TOLAC, with a successful vaginal birth after cesarean (VBAC) rate of approximately 57%.1
The reason for the low TOLAC rate is multifactorial, but a primary concern may be the safety risk of a TOLAC as it relates to uterine rupture, a rare but potentially catastrophic complication. In a large, multicenter prospective observational trial of more than 17,800 women attempting a TOLAC, the symptomatic uterine rupture rate was 0.7%.2 As such, efforts to identify women at highest risk for uterine rupture and those with characteristics predictive of a successful VBAC have remained ongoing. Jastrow and colleagues have expanded this body of knowledge with their prospective cohort study.
Details of the study
The researchers assessed lower uterine segment thickness via vaginal and abdominal ultrasound at 34 to 38 weeks’ gestation in more than 1,850 women with a previous CD. Women enrolled in the trial were classified into 3 risk categories based on lower uterine segment thickness: high risk (<2.0 mm), intermediate risk (2.0 to 2.4 mm), and low risk (≥2.5 mm). The investigators’ objective was to estimate the occurrence of uterine rupture when this measurement was included in the decision-making process on mode of delivery.
An important aspect of this study involved how the provider discussed the mode of delivery with the patient after the lower uterine segment measurement was obtained. Both the provider and the patient were informed of the risk category, and further counseling included the following:
- average overall uterine rupture risk, 0.5% to 1%
- if <2.0 mm, uterine rupture risk likely >1%
- if ≥2.5 mm, uterine rupture risk likely <0.5%
- uterine rupture risks (including perinatal asphyxia and death)
- maternal and neonatal complications of cesarean
- estimation of likelihood for successful VBAC.
How did risk-stratified women fare?
In approximately 1,000 cases, the authors reported no symptomatic uterine ruptures. Of particular interest, however, is the rate of women attempting a TOLAC in each category:
- 194 women with high risk
- 9% underwent a TOLAC
- 82% had a successful vaginal birth
- 217 women with intermediate risk
- 42% underwent a TOLAC
- 78% had a successful vaginal birth
- 1,438 women with low risk
- 61% underwent a TOLAC
- 66% had a successful vaginal birth.
Considering cesarean scar defect
Finally, uterine scar defects at CD in those who underwent a TOLAC were 0/3 (0%), 5/21 (25%), and 20/276 (7%) in the high-, intermediate-, and low-risk groups, respectively. Given the observational nature of the study, the authors suggest that uterine scar dehiscence may be predictive of labor dystocia, but it remains unclear if it predicts or is a prerequisite for subsequent uterine rupture if labor occurs.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Zhang J, Troendle J, Reddy UM, et al; Consortium on Safe Labor. Am J Obstet Gynecol. 2010;203(4):326.e1–326.e10.
- Landon MB, Hauth JC, Leveno KJ, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;16;351(25):2581–2589.
- Zhang J, Troendle J, Reddy UM, et al; Consortium on Safe Labor. Am J Obstet Gynecol. 2010;203(4):326.e1–326.e10.
- Landon MB, Hauth JC, Leveno KJ, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;16;351(25):2581–2589.
Thinking through the State of Hospital Medicine Report
sSHM’s 2016 State of Hospital Medicine Report (SoHM) is now available, and it’s unquestionably the best source of detail regarding how hospital medicine groups are configured and operated.1
The SoHM is published in even years and combines data from two sources:
- Hospitalist data from Medical Group Management Association’s Physician Compensation and Productivity Survey. Within the SoHM, you will find the same figures for hospitalist compensation, production, and a few related metrics that are from the MGMA survey report.
- SHM’s survey of hospital medicine groups. This survey drills into significant detail on things like scope of clinical practice, staffing levels, work schedules, bonus metrics, CPT code distribution, roles for NPs and PAs, and the amount of financial support provided to the group.
There are several new topics in this year’s SoHM, including CME allowances, utilization of prolonged service codes, and charge capture methodologies being used by hospital medicine groups. My colleague, Leslie Flores, has been very involved in the survey for 10 years and has written a blog with more details.
One Caveat …
The mix of survey respondents varies and includes a much larger portion of hospital medicine groups employed by multi-state management companies than prior surveys. Even if a parameter hasn’t changed for any hospitalist group, the fact that responses come from different contingents of the hospitalist workforce can result in a different result from one survey to the next. It is difficult to be certain if variations across successive surveys reflect a real change in the marketplace or are a function of variation in the respondent population.
Now let’s review and analyze some of this year’s survey findings for hospital medicine groups caring for adults:
Financial Support Stayed Flat
The amount of financial support provided to a hospital medicine group per FTE has increased significantly in every prior survey. This money typically comes from the hospital that the hospital medicine group serves and is sometimes referred to as the “subsidy.” For hospital medicine groups serving adults, it was $139,000 in 2012 and $156,000 in 2014.
The current survey showed a median of $157,500, essentially unchanged from two years prior. This is either an aberration in the survey (e.g., a result of a different survey population) or an indicator that this amount has begun to level off. Clearly, there is an upper limit to the amount of financial support the marketplace can support, but from my experience working with hospitalist groups around the country, I haven’t seen evidence that we’ve reached that point. I suspect it is an aberration and future surveys will show a continued rising trend, though perhaps not as rapidly as in years past.
Compensation Method Is Evolving
A mean of 14.7% of compensation was tied to production, up from around 10% in prior surveys. And the portion tied to performance (e.g., patient satisfaction, quality metrics) was unchanged at 6%. It’s interesting that despite proliferation of pay-for-performance programs and increasing emphasis on quality and value, it is the productivity portion of compensation that increased. It’s hard to know if that is a meaningful trend.
Compensation Amount Continues to Increase
For hospitalists caring for adults, the median amount of compensation rose to $278,746, up from $253,000 in 2014, $234,000 in 2013, and $221,000 in 2011. These figures come from the MGMA survey, and the financial support figures above come from the separate SHM survey. That means it’s impossible to make firm conclusions about how the numbers do or don’t interrelate.
Don’t forget that surveys report all forms of compensation, including base, production, bonus, extra shifts, and other elements. This year’s $278,746 includes all the bonus dollars earned by each hospitalist in the survey. We can make a very rough guess at the bonus by multiplying the portion of total compensation tied to performance in the SHM survey (6%) by the total compensation ($278,746) from the MGMA survey, which comes to $13,397. But we still don’t know the portion of the total bonus dollars available that represents. My experience is that the total bonus dollars available is around $20,000 or more at most hospital medicine groups. Therefore, a doctor who earned $13,397 presumably didn’t meet all performance goals.
A Deeper Dive into Hospital Medicine Group Finances
It is really interesting to ponder where the dollars come from to fund higher hospitalist compensation if the financial support provided per FTE hasn’t increased. Perhaps hospitalists are generating more encounters, work relative value units (wRVUs), or professional fee collections?
Median professional fee collections were $213,000 this year, up from $151,000 in the prior survey two years ago. This increase could, in theory, fully fund the higher hospitalist compensation without the need for an increase in other sources of revenue.
So why are collections up? It could be because hospitalists are coding the average visit at a higher level: 2.02 wRVUs per encounter this year compared to 1.97 in 2014 and 1.91 in 2012. The survey can’t help distinguish whether this increase is because we’re seeing more complex patients or whether we’re improving our documentation to catch up with the complexity of the patients we’ve been seeing all along. I suspect it is both.
The increase in wRVUs per encounter, however, is offset by a continued downward trend in numbers of encounters: 1,684 this year compared to 1,850 in 2014 and 2,078 in 2012. The total wRVUs generated per hospitalist in a year stayed about the same at 4,247 compared to 4,298 in 2014.
The best explanation for why total collections are up would be that payor rates have increased. But Medicare, which accounts for about 60%–65% of the payor mix for most hospital medicine groups, hasn’t increased rates enough to explain this, and I’m not aware of other payor classes that have increased significantly. Another explanation could be that hospital medicine groups are simply doing a better job with billing and collections and other revenue-cycle management activities, resulting in increased revenue.
I guess it shouldn’t be surprising that some of the survey results don’t seem internally consistent. The data come from two different surveys, the response rate for each question varies, and other issues mean the survey just can’t provide that level of precision. We also need to keep in mind that analyses like I’ve provided here are only very rough explanations. But I think they’re still valuable to think about even if they don’t provide definitive answers. TH
Reference
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed August 9, 2016.

sSHM’s 2016 State of Hospital Medicine Report (SoHM) is now available, and it’s unquestionably the best source of detail regarding how hospital medicine groups are configured and operated.1
The SoHM is published in even years and combines data from two sources:
- Hospitalist data from Medical Group Management Association’s Physician Compensation and Productivity Survey. Within the SoHM, you will find the same figures for hospitalist compensation, production, and a few related metrics that are from the MGMA survey report.
- SHM’s survey of hospital medicine groups. This survey drills into significant detail on things like scope of clinical practice, staffing levels, work schedules, bonus metrics, CPT code distribution, roles for NPs and PAs, and the amount of financial support provided to the group.
There are several new topics in this year’s SoHM, including CME allowances, utilization of prolonged service codes, and charge capture methodologies being used by hospital medicine groups. My colleague, Leslie Flores, has been very involved in the survey for 10 years and has written a blog with more details.
One Caveat …
The mix of survey respondents varies and includes a much larger portion of hospital medicine groups employed by multi-state management companies than prior surveys. Even if a parameter hasn’t changed for any hospitalist group, the fact that responses come from different contingents of the hospitalist workforce can result in a different result from one survey to the next. It is difficult to be certain if variations across successive surveys reflect a real change in the marketplace or are a function of variation in the respondent population.
Now let’s review and analyze some of this year’s survey findings for hospital medicine groups caring for adults:
Financial Support Stayed Flat
The amount of financial support provided to a hospital medicine group per FTE has increased significantly in every prior survey. This money typically comes from the hospital that the hospital medicine group serves and is sometimes referred to as the “subsidy.” For hospital medicine groups serving adults, it was $139,000 in 2012 and $156,000 in 2014.
The current survey showed a median of $157,500, essentially unchanged from two years prior. This is either an aberration in the survey (e.g., a result of a different survey population) or an indicator that this amount has begun to level off. Clearly, there is an upper limit to the amount of financial support the marketplace can support, but from my experience working with hospitalist groups around the country, I haven’t seen evidence that we’ve reached that point. I suspect it is an aberration and future surveys will show a continued rising trend, though perhaps not as rapidly as in years past.
Compensation Method Is Evolving
A mean of 14.7% of compensation was tied to production, up from around 10% in prior surveys. And the portion tied to performance (e.g., patient satisfaction, quality metrics) was unchanged at 6%. It’s interesting that despite proliferation of pay-for-performance programs and increasing emphasis on quality and value, it is the productivity portion of compensation that increased. It’s hard to know if that is a meaningful trend.
Compensation Amount Continues to Increase
For hospitalists caring for adults, the median amount of compensation rose to $278,746, up from $253,000 in 2014, $234,000 in 2013, and $221,000 in 2011. These figures come from the MGMA survey, and the financial support figures above come from the separate SHM survey. That means it’s impossible to make firm conclusions about how the numbers do or don’t interrelate.
Don’t forget that surveys report all forms of compensation, including base, production, bonus, extra shifts, and other elements. This year’s $278,746 includes all the bonus dollars earned by each hospitalist in the survey. We can make a very rough guess at the bonus by multiplying the portion of total compensation tied to performance in the SHM survey (6%) by the total compensation ($278,746) from the MGMA survey, which comes to $13,397. But we still don’t know the portion of the total bonus dollars available that represents. My experience is that the total bonus dollars available is around $20,000 or more at most hospital medicine groups. Therefore, a doctor who earned $13,397 presumably didn’t meet all performance goals.
A Deeper Dive into Hospital Medicine Group Finances
It is really interesting to ponder where the dollars come from to fund higher hospitalist compensation if the financial support provided per FTE hasn’t increased. Perhaps hospitalists are generating more encounters, work relative value units (wRVUs), or professional fee collections?
Median professional fee collections were $213,000 this year, up from $151,000 in the prior survey two years ago. This increase could, in theory, fully fund the higher hospitalist compensation without the need for an increase in other sources of revenue.
So why are collections up? It could be because hospitalists are coding the average visit at a higher level: 2.02 wRVUs per encounter this year compared to 1.97 in 2014 and 1.91 in 2012. The survey can’t help distinguish whether this increase is because we’re seeing more complex patients or whether we’re improving our documentation to catch up with the complexity of the patients we’ve been seeing all along. I suspect it is both.
The increase in wRVUs per encounter, however, is offset by a continued downward trend in numbers of encounters: 1,684 this year compared to 1,850 in 2014 and 2,078 in 2012. The total wRVUs generated per hospitalist in a year stayed about the same at 4,247 compared to 4,298 in 2014.
The best explanation for why total collections are up would be that payor rates have increased. But Medicare, which accounts for about 60%–65% of the payor mix for most hospital medicine groups, hasn’t increased rates enough to explain this, and I’m not aware of other payor classes that have increased significantly. Another explanation could be that hospital medicine groups are simply doing a better job with billing and collections and other revenue-cycle management activities, resulting in increased revenue.
I guess it shouldn’t be surprising that some of the survey results don’t seem internally consistent. The data come from two different surveys, the response rate for each question varies, and other issues mean the survey just can’t provide that level of precision. We also need to keep in mind that analyses like I’ve provided here are only very rough explanations. But I think they’re still valuable to think about even if they don’t provide definitive answers. TH
Reference
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed August 9, 2016.

sSHM’s 2016 State of Hospital Medicine Report (SoHM) is now available, and it’s unquestionably the best source of detail regarding how hospital medicine groups are configured and operated.1
The SoHM is published in even years and combines data from two sources:
- Hospitalist data from Medical Group Management Association’s Physician Compensation and Productivity Survey. Within the SoHM, you will find the same figures for hospitalist compensation, production, and a few related metrics that are from the MGMA survey report.
- SHM’s survey of hospital medicine groups. This survey drills into significant detail on things like scope of clinical practice, staffing levels, work schedules, bonus metrics, CPT code distribution, roles for NPs and PAs, and the amount of financial support provided to the group.
There are several new topics in this year’s SoHM, including CME allowances, utilization of prolonged service codes, and charge capture methodologies being used by hospital medicine groups. My colleague, Leslie Flores, has been very involved in the survey for 10 years and has written a blog with more details.
One Caveat …
The mix of survey respondents varies and includes a much larger portion of hospital medicine groups employed by multi-state management companies than prior surveys. Even if a parameter hasn’t changed for any hospitalist group, the fact that responses come from different contingents of the hospitalist workforce can result in a different result from one survey to the next. It is difficult to be certain if variations across successive surveys reflect a real change in the marketplace or are a function of variation in the respondent population.
Now let’s review and analyze some of this year’s survey findings for hospital medicine groups caring for adults:
Financial Support Stayed Flat
The amount of financial support provided to a hospital medicine group per FTE has increased significantly in every prior survey. This money typically comes from the hospital that the hospital medicine group serves and is sometimes referred to as the “subsidy.” For hospital medicine groups serving adults, it was $139,000 in 2012 and $156,000 in 2014.
The current survey showed a median of $157,500, essentially unchanged from two years prior. This is either an aberration in the survey (e.g., a result of a different survey population) or an indicator that this amount has begun to level off. Clearly, there is an upper limit to the amount of financial support the marketplace can support, but from my experience working with hospitalist groups around the country, I haven’t seen evidence that we’ve reached that point. I suspect it is an aberration and future surveys will show a continued rising trend, though perhaps not as rapidly as in years past.
Compensation Method Is Evolving
A mean of 14.7% of compensation was tied to production, up from around 10% in prior surveys. And the portion tied to performance (e.g., patient satisfaction, quality metrics) was unchanged at 6%. It’s interesting that despite proliferation of pay-for-performance programs and increasing emphasis on quality and value, it is the productivity portion of compensation that increased. It’s hard to know if that is a meaningful trend.
Compensation Amount Continues to Increase
For hospitalists caring for adults, the median amount of compensation rose to $278,746, up from $253,000 in 2014, $234,000 in 2013, and $221,000 in 2011. These figures come from the MGMA survey, and the financial support figures above come from the separate SHM survey. That means it’s impossible to make firm conclusions about how the numbers do or don’t interrelate.
Don’t forget that surveys report all forms of compensation, including base, production, bonus, extra shifts, and other elements. This year’s $278,746 includes all the bonus dollars earned by each hospitalist in the survey. We can make a very rough guess at the bonus by multiplying the portion of total compensation tied to performance in the SHM survey (6%) by the total compensation ($278,746) from the MGMA survey, which comes to $13,397. But we still don’t know the portion of the total bonus dollars available that represents. My experience is that the total bonus dollars available is around $20,000 or more at most hospital medicine groups. Therefore, a doctor who earned $13,397 presumably didn’t meet all performance goals.
A Deeper Dive into Hospital Medicine Group Finances
It is really interesting to ponder where the dollars come from to fund higher hospitalist compensation if the financial support provided per FTE hasn’t increased. Perhaps hospitalists are generating more encounters, work relative value units (wRVUs), or professional fee collections?
Median professional fee collections were $213,000 this year, up from $151,000 in the prior survey two years ago. This increase could, in theory, fully fund the higher hospitalist compensation without the need for an increase in other sources of revenue.
So why are collections up? It could be because hospitalists are coding the average visit at a higher level: 2.02 wRVUs per encounter this year compared to 1.97 in 2014 and 1.91 in 2012. The survey can’t help distinguish whether this increase is because we’re seeing more complex patients or whether we’re improving our documentation to catch up with the complexity of the patients we’ve been seeing all along. I suspect it is both.
The increase in wRVUs per encounter, however, is offset by a continued downward trend in numbers of encounters: 1,684 this year compared to 1,850 in 2014 and 2,078 in 2012. The total wRVUs generated per hospitalist in a year stayed about the same at 4,247 compared to 4,298 in 2014.
The best explanation for why total collections are up would be that payor rates have increased. But Medicare, which accounts for about 60%–65% of the payor mix for most hospital medicine groups, hasn’t increased rates enough to explain this, and I’m not aware of other payor classes that have increased significantly. Another explanation could be that hospital medicine groups are simply doing a better job with billing and collections and other revenue-cycle management activities, resulting in increased revenue.
I guess it shouldn’t be surprising that some of the survey results don’t seem internally consistent. The data come from two different surveys, the response rate for each question varies, and other issues mean the survey just can’t provide that level of precision. We also need to keep in mind that analyses like I’ve provided here are only very rough explanations. But I think they’re still valuable to think about even if they don’t provide definitive answers. TH
Reference
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed August 9, 2016.