User login
Child of The New Gastroenterologist
Navigating your childcare options in a post-COVID world
When we found out we were expecting our first child, we were ecstatic. Our excitement soon gave way to panic, however, as we realized that we needed a plan for childcare. As full-time physicians early in our careers, neither of us was prepared to drop to part-time or become a stay-at-home caregiver. Not knowing where to start, we turned to our friends and colleagues, and of course, the Internet, for advice on our options.
In our research, we discovered three things. First, with COVID-19, the cost of childcare has skyrocketed, and availability has decreased. Second, there are several options for childcare, each with its own benefits and drawbacks. Third, there is no one-size-fits-all solution.
Family
Using family members to provide childcare is often cost-effective and provides a familiar, supportive environment for children. Proximity does not guarantee a willingness or ability to provide long-term care, however, and it can cause strain on family relationships, lead to intrusions and boundary issues, and create feelings of obligation and guilt. It is important to have very honest, up-front discussions with family members about hopes and expectations if this is your childcare plan.
Daycare, facility-based
Daycare centers are commercial facilities that offer care to multiple children of varying ages, starting from as young as 6 weeks. They have trained professionals and provide structured activities and educational programs for children. Many daycares also provide snacks and lunch, which is included in their tuition. They are a popular choice for families seeking full-time childcare and the social and educational benefits that come with a structured setting.
Daycares also have some downsides. They usually operate during normal workday hours, from 7:00 a.m. to 6:00 p.m., which may not be convenient for physicians who work outside of these hours. Even with feasible hours, getting children dressed, ready, and dropped off each morning could add significant time and stress to your morning routine. Additionally, most daycares have policies that prohibit attendance if a child is sick or febrile, which is a common occurrence, particularly for daycare kids. In case of an illness outbreak, the daycare may even close for several days. Both scenarios require at least one parent to take a day off or have an alternative childcare plan available on short notice.
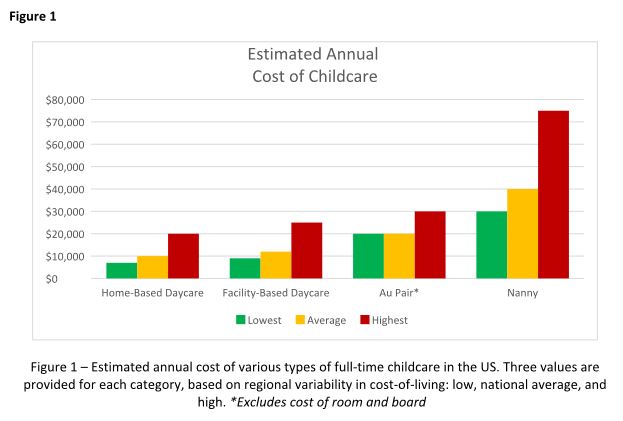
Availability of daycare can be limited, particularly since the COVID pandemic, creating waitlists that can be several months long. Early registration, even during pregnancy, is recommended to secure a spot. It can be helpful to find out if your employer has an agreement with a specific daycare that has “physician-friendly” hours and gives waitlist priority to trainees or even attending physicians. The cost of daycare for one child is typically affordable, around $12,000 per year on average, but can be as high as $25,000 in cities with high cost of living. A sibling discount may be offered, but the cost of daycare for multiple children could still exceed in-home childcare options.1
Daycare, home-based (also known as family care centers)
Family care centers offer a home-like alternative to daycares, with smaller staff-to-child ratios and often more personalized care. They are favored by families seeking a more intimate setting. They might offer more flexible scheduling and are typically less expensive than facility-based daycares, at up to 25% lower cost.1 They may lack the same structure and educational opportunities as facility-based daycares, however, and are not subject to the same health and safety regulations.
Nannies
Nannies are professional caregivers who provide in-home childcare services. Their responsibilities may include feeding, changing, dressing, bathing, and playing with children. In some cases, they may also be expected to do light housekeeping tasks like meal preparation, laundry, and cleaning. It is common for nannies in high-demand markets to refuse to perform these additional tasks, however. Nannies are preferred by families with hectic schedules due to their flexibility. They can work early, late, or even overnight shifts, and provide care in the comfort of your home, avoiding the hassle of drop-off and pick-up times. Nannies also can provide personalized care to meet each child’s specific needs, and they can care for children who are sick or febrile.
When hiring a nanny, it is important to have a written contract outlining their expected hours, wages, benefits, and duties to prevent misunderstandings in the future. Finding a trustworthy and reliable nanny can be a challenge, and families have several options for finding one. They can post jobs on free websites and browse nanny CVs or use a fee-based nanny agency. The cost of using an agency can range from a few hundred to several thousand dollars, so it is important to ask friends and colleagues for recommendations before paying for an agency’s services.
The cost of hiring a nanny is one of its main drawbacks. Nannies typically earn $15 to $30 per hour, and if they work in the family’s home, they are typically considered “household employees” by the IRS. Household employees are entitled to overtime pay for work beyond 40 hours per week, and the employer (you!) is responsible for payroll taxes, withholding, and providing an annual W-2 tax statement.2 There are affordable online nanny payroll services that handle payroll and tax-filing to simplify the process, however. The average annual cost of a full-time nanny is around $40,000 and can be as high as $75,000 in some markets.1 A nanny-share with other families can lower costs, but it may also result in less control over the caregiver and schedule.
It is important to consult a tax professional or the IRS for guidance on nanny wages, taxes, and payroll, as a nanny might rarely be considered an “independent contractor” if they meet certain criteria.
Au pair
An au pair is a live-in childcare provider who travels to a host family’s home from a foreign country on a special J-1 visa. The goal is to provide care for children and participate in cultural exchange activities. Au pairs bring many benefits, such as cost savings compared to traditional childcare options and greater flexibility and customization. They can work up to 10 hours per day and 45 hours a week, performing tasks such as light housekeeping, meal preparation, and transportation for the children. Host families must provide a safe and comfortable living environment, including a private room, meals, and some travel and education expenses.1
The process of hiring an au pair involves working with a designated agency that matches families with applicants and sponsors the J-1 visa. The entire process can take several months, and average program fees cost around $10,000 per placement. Au pairs are hired on a 12-month J-1 visa, which can be extended for up to an additional 12 months, allowing families up to 2 years with the same au pair before needing to find a new placement.
Au pairs earn a minimum weekly stipend of $195.75, set forth by the U.S. State Department.3 Currently, au pairs are not subject to local and state wage requirements, but legal proceedings in various states have recently questioned whether au pairs should be protected under local regulations. Massachusetts has been the most progressive, explicitly protecting au pairs as domestic workers under state labor laws, raising their weekly stipend to roughly $600 to comply with state minimum wage requirements.4 The federal government is expected to provide clarity on this issue, but for the time being, au pairs remain an affordable alternative to a nanny in most states.
Conclusion
Choosing childcare is a complicated process with multiple factors to consider. Figure 1 breaks down the estimated annual cost of each of the options outlined above for a single child in low, average, and high cost-of-living areas. But your decision likely hinges on much more than just cost, and may include family dynamics, scheduling needs, and personal preferences. Gather as much advice and information as possible, but remember to trust your instincts and make the decision that works best for your family. At the end of the day, what matters most is the happiness and well-being of your child.
Dr. Hathorn and Dr. Creighton are married, and both work full-time with a 1-year-old child. Dr. Hathorn is a bariatric and advanced therapeutic endoscopist at the University of North Carolina at Chapel Hill. Dr. Creighton is an anesthesiologist at UNC Chapel Hill. Neither reported any conflicts of interest.
References
1. Care.com. This is how much childcare costs in 2022. 2022 Jun 15.
2. Internal Revenue Service. Publication 926 - Household Employer’s Tax Guide 2023.
3. U.S. Department of State. Au Pair.
4. Commonwealth of Massachusetts. Domestic workers.
Disclaimer
The financial and tax information presented in this article are believed to be true and accurate at the time of writing. However, it’s important to note that tax laws and regulations are subject to change. The authors are not certified financial advisers or tax specialists. It is recommended to seek verification from a local tax expert or the Internal Revenue Service to discuss your specific situation.
When we found out we were expecting our first child, we were ecstatic. Our excitement soon gave way to panic, however, as we realized that we needed a plan for childcare. As full-time physicians early in our careers, neither of us was prepared to drop to part-time or become a stay-at-home caregiver. Not knowing where to start, we turned to our friends and colleagues, and of course, the Internet, for advice on our options.
In our research, we discovered three things. First, with COVID-19, the cost of childcare has skyrocketed, and availability has decreased. Second, there are several options for childcare, each with its own benefits and drawbacks. Third, there is no one-size-fits-all solution.
Family
Using family members to provide childcare is often cost-effective and provides a familiar, supportive environment for children. Proximity does not guarantee a willingness or ability to provide long-term care, however, and it can cause strain on family relationships, lead to intrusions and boundary issues, and create feelings of obligation and guilt. It is important to have very honest, up-front discussions with family members about hopes and expectations if this is your childcare plan.
Daycare, facility-based
Daycare centers are commercial facilities that offer care to multiple children of varying ages, starting from as young as 6 weeks. They have trained professionals and provide structured activities and educational programs for children. Many daycares also provide snacks and lunch, which is included in their tuition. They are a popular choice for families seeking full-time childcare and the social and educational benefits that come with a structured setting.
Daycares also have some downsides. They usually operate during normal workday hours, from 7:00 a.m. to 6:00 p.m., which may not be convenient for physicians who work outside of these hours. Even with feasible hours, getting children dressed, ready, and dropped off each morning could add significant time and stress to your morning routine. Additionally, most daycares have policies that prohibit attendance if a child is sick or febrile, which is a common occurrence, particularly for daycare kids. In case of an illness outbreak, the daycare may even close for several days. Both scenarios require at least one parent to take a day off or have an alternative childcare plan available on short notice.
Availability of daycare can be limited, particularly since the COVID pandemic, creating waitlists that can be several months long. Early registration, even during pregnancy, is recommended to secure a spot. It can be helpful to find out if your employer has an agreement with a specific daycare that has “physician-friendly” hours and gives waitlist priority to trainees or even attending physicians. The cost of daycare for one child is typically affordable, around $12,000 per year on average, but can be as high as $25,000 in cities with high cost of living. A sibling discount may be offered, but the cost of daycare for multiple children could still exceed in-home childcare options.1
Daycare, home-based (also known as family care centers)
Family care centers offer a home-like alternative to daycares, with smaller staff-to-child ratios and often more personalized care. They are favored by families seeking a more intimate setting. They might offer more flexible scheduling and are typically less expensive than facility-based daycares, at up to 25% lower cost.1 They may lack the same structure and educational opportunities as facility-based daycares, however, and are not subject to the same health and safety regulations.
Nannies
Nannies are professional caregivers who provide in-home childcare services. Their responsibilities may include feeding, changing, dressing, bathing, and playing with children. In some cases, they may also be expected to do light housekeeping tasks like meal preparation, laundry, and cleaning. It is common for nannies in high-demand markets to refuse to perform these additional tasks, however. Nannies are preferred by families with hectic schedules due to their flexibility. They can work early, late, or even overnight shifts, and provide care in the comfort of your home, avoiding the hassle of drop-off and pick-up times. Nannies also can provide personalized care to meet each child’s specific needs, and they can care for children who are sick or febrile.
When hiring a nanny, it is important to have a written contract outlining their expected hours, wages, benefits, and duties to prevent misunderstandings in the future. Finding a trustworthy and reliable nanny can be a challenge, and families have several options for finding one. They can post jobs on free websites and browse nanny CVs or use a fee-based nanny agency. The cost of using an agency can range from a few hundred to several thousand dollars, so it is important to ask friends and colleagues for recommendations before paying for an agency’s services.
The cost of hiring a nanny is one of its main drawbacks. Nannies typically earn $15 to $30 per hour, and if they work in the family’s home, they are typically considered “household employees” by the IRS. Household employees are entitled to overtime pay for work beyond 40 hours per week, and the employer (you!) is responsible for payroll taxes, withholding, and providing an annual W-2 tax statement.2 There are affordable online nanny payroll services that handle payroll and tax-filing to simplify the process, however. The average annual cost of a full-time nanny is around $40,000 and can be as high as $75,000 in some markets.1 A nanny-share with other families can lower costs, but it may also result in less control over the caregiver and schedule.
It is important to consult a tax professional or the IRS for guidance on nanny wages, taxes, and payroll, as a nanny might rarely be considered an “independent contractor” if they meet certain criteria.
Au pair
An au pair is a live-in childcare provider who travels to a host family’s home from a foreign country on a special J-1 visa. The goal is to provide care for children and participate in cultural exchange activities. Au pairs bring many benefits, such as cost savings compared to traditional childcare options and greater flexibility and customization. They can work up to 10 hours per day and 45 hours a week, performing tasks such as light housekeeping, meal preparation, and transportation for the children. Host families must provide a safe and comfortable living environment, including a private room, meals, and some travel and education expenses.1
The process of hiring an au pair involves working with a designated agency that matches families with applicants and sponsors the J-1 visa. The entire process can take several months, and average program fees cost around $10,000 per placement. Au pairs are hired on a 12-month J-1 visa, which can be extended for up to an additional 12 months, allowing families up to 2 years with the same au pair before needing to find a new placement.
Au pairs earn a minimum weekly stipend of $195.75, set forth by the U.S. State Department.3 Currently, au pairs are not subject to local and state wage requirements, but legal proceedings in various states have recently questioned whether au pairs should be protected under local regulations. Massachusetts has been the most progressive, explicitly protecting au pairs as domestic workers under state labor laws, raising their weekly stipend to roughly $600 to comply with state minimum wage requirements.4 The federal government is expected to provide clarity on this issue, but for the time being, au pairs remain an affordable alternative to a nanny in most states.
Conclusion
Choosing childcare is a complicated process with multiple factors to consider. Figure 1 breaks down the estimated annual cost of each of the options outlined above for a single child in low, average, and high cost-of-living areas. But your decision likely hinges on much more than just cost, and may include family dynamics, scheduling needs, and personal preferences. Gather as much advice and information as possible, but remember to trust your instincts and make the decision that works best for your family. At the end of the day, what matters most is the happiness and well-being of your child.
Dr. Hathorn and Dr. Creighton are married, and both work full-time with a 1-year-old child. Dr. Hathorn is a bariatric and advanced therapeutic endoscopist at the University of North Carolina at Chapel Hill. Dr. Creighton is an anesthesiologist at UNC Chapel Hill. Neither reported any conflicts of interest.
References
1. Care.com. This is how much childcare costs in 2022. 2022 Jun 15.
2. Internal Revenue Service. Publication 926 - Household Employer’s Tax Guide 2023.
3. U.S. Department of State. Au Pair.
4. Commonwealth of Massachusetts. Domestic workers.
Disclaimer
The financial and tax information presented in this article are believed to be true and accurate at the time of writing. However, it’s important to note that tax laws and regulations are subject to change. The authors are not certified financial advisers or tax specialists. It is recommended to seek verification from a local tax expert or the Internal Revenue Service to discuss your specific situation.
When we found out we were expecting our first child, we were ecstatic. Our excitement soon gave way to panic, however, as we realized that we needed a plan for childcare. As full-time physicians early in our careers, neither of us was prepared to drop to part-time or become a stay-at-home caregiver. Not knowing where to start, we turned to our friends and colleagues, and of course, the Internet, for advice on our options.
In our research, we discovered three things. First, with COVID-19, the cost of childcare has skyrocketed, and availability has decreased. Second, there are several options for childcare, each with its own benefits and drawbacks. Third, there is no one-size-fits-all solution.
Family
Using family members to provide childcare is often cost-effective and provides a familiar, supportive environment for children. Proximity does not guarantee a willingness or ability to provide long-term care, however, and it can cause strain on family relationships, lead to intrusions and boundary issues, and create feelings of obligation and guilt. It is important to have very honest, up-front discussions with family members about hopes and expectations if this is your childcare plan.
Daycare, facility-based
Daycare centers are commercial facilities that offer care to multiple children of varying ages, starting from as young as 6 weeks. They have trained professionals and provide structured activities and educational programs for children. Many daycares also provide snacks and lunch, which is included in their tuition. They are a popular choice for families seeking full-time childcare and the social and educational benefits that come with a structured setting.
Daycares also have some downsides. They usually operate during normal workday hours, from 7:00 a.m. to 6:00 p.m., which may not be convenient for physicians who work outside of these hours. Even with feasible hours, getting children dressed, ready, and dropped off each morning could add significant time and stress to your morning routine. Additionally, most daycares have policies that prohibit attendance if a child is sick or febrile, which is a common occurrence, particularly for daycare kids. In case of an illness outbreak, the daycare may even close for several days. Both scenarios require at least one parent to take a day off or have an alternative childcare plan available on short notice.
Availability of daycare can be limited, particularly since the COVID pandemic, creating waitlists that can be several months long. Early registration, even during pregnancy, is recommended to secure a spot. It can be helpful to find out if your employer has an agreement with a specific daycare that has “physician-friendly” hours and gives waitlist priority to trainees or even attending physicians. The cost of daycare for one child is typically affordable, around $12,000 per year on average, but can be as high as $25,000 in cities with high cost of living. A sibling discount may be offered, but the cost of daycare for multiple children could still exceed in-home childcare options.1
Daycare, home-based (also known as family care centers)
Family care centers offer a home-like alternative to daycares, with smaller staff-to-child ratios and often more personalized care. They are favored by families seeking a more intimate setting. They might offer more flexible scheduling and are typically less expensive than facility-based daycares, at up to 25% lower cost.1 They may lack the same structure and educational opportunities as facility-based daycares, however, and are not subject to the same health and safety regulations.
Nannies
Nannies are professional caregivers who provide in-home childcare services. Their responsibilities may include feeding, changing, dressing, bathing, and playing with children. In some cases, they may also be expected to do light housekeeping tasks like meal preparation, laundry, and cleaning. It is common for nannies in high-demand markets to refuse to perform these additional tasks, however. Nannies are preferred by families with hectic schedules due to their flexibility. They can work early, late, or even overnight shifts, and provide care in the comfort of your home, avoiding the hassle of drop-off and pick-up times. Nannies also can provide personalized care to meet each child’s specific needs, and they can care for children who are sick or febrile.
When hiring a nanny, it is important to have a written contract outlining their expected hours, wages, benefits, and duties to prevent misunderstandings in the future. Finding a trustworthy and reliable nanny can be a challenge, and families have several options for finding one. They can post jobs on free websites and browse nanny CVs or use a fee-based nanny agency. The cost of using an agency can range from a few hundred to several thousand dollars, so it is important to ask friends and colleagues for recommendations before paying for an agency’s services.
The cost of hiring a nanny is one of its main drawbacks. Nannies typically earn $15 to $30 per hour, and if they work in the family’s home, they are typically considered “household employees” by the IRS. Household employees are entitled to overtime pay for work beyond 40 hours per week, and the employer (you!) is responsible for payroll taxes, withholding, and providing an annual W-2 tax statement.2 There are affordable online nanny payroll services that handle payroll and tax-filing to simplify the process, however. The average annual cost of a full-time nanny is around $40,000 and can be as high as $75,000 in some markets.1 A nanny-share with other families can lower costs, but it may also result in less control over the caregiver and schedule.
It is important to consult a tax professional or the IRS for guidance on nanny wages, taxes, and payroll, as a nanny might rarely be considered an “independent contractor” if they meet certain criteria.
Au pair
An au pair is a live-in childcare provider who travels to a host family’s home from a foreign country on a special J-1 visa. The goal is to provide care for children and participate in cultural exchange activities. Au pairs bring many benefits, such as cost savings compared to traditional childcare options and greater flexibility and customization. They can work up to 10 hours per day and 45 hours a week, performing tasks such as light housekeeping, meal preparation, and transportation for the children. Host families must provide a safe and comfortable living environment, including a private room, meals, and some travel and education expenses.1
The process of hiring an au pair involves working with a designated agency that matches families with applicants and sponsors the J-1 visa. The entire process can take several months, and average program fees cost around $10,000 per placement. Au pairs are hired on a 12-month J-1 visa, which can be extended for up to an additional 12 months, allowing families up to 2 years with the same au pair before needing to find a new placement.
Au pairs earn a minimum weekly stipend of $195.75, set forth by the U.S. State Department.3 Currently, au pairs are not subject to local and state wage requirements, but legal proceedings in various states have recently questioned whether au pairs should be protected under local regulations. Massachusetts has been the most progressive, explicitly protecting au pairs as domestic workers under state labor laws, raising their weekly stipend to roughly $600 to comply with state minimum wage requirements.4 The federal government is expected to provide clarity on this issue, but for the time being, au pairs remain an affordable alternative to a nanny in most states.
Conclusion
Choosing childcare is a complicated process with multiple factors to consider. Figure 1 breaks down the estimated annual cost of each of the options outlined above for a single child in low, average, and high cost-of-living areas. But your decision likely hinges on much more than just cost, and may include family dynamics, scheduling needs, and personal preferences. Gather as much advice and information as possible, but remember to trust your instincts and make the decision that works best for your family. At the end of the day, what matters most is the happiness and well-being of your child.
Dr. Hathorn and Dr. Creighton are married, and both work full-time with a 1-year-old child. Dr. Hathorn is a bariatric and advanced therapeutic endoscopist at the University of North Carolina at Chapel Hill. Dr. Creighton is an anesthesiologist at UNC Chapel Hill. Neither reported any conflicts of interest.
References
1. Care.com. This is how much childcare costs in 2022. 2022 Jun 15.
2. Internal Revenue Service. Publication 926 - Household Employer’s Tax Guide 2023.
3. U.S. Department of State. Au Pair.
4. Commonwealth of Massachusetts. Domestic workers.
Disclaimer
The financial and tax information presented in this article are believed to be true and accurate at the time of writing. However, it’s important to note that tax laws and regulations are subject to change. The authors are not certified financial advisers or tax specialists. It is recommended to seek verification from a local tax expert or the Internal Revenue Service to discuss your specific situation.
Telemedicine increases access to care and optimizes practice revenue
The first time I considered telehealth as a viable option for care delivery was in February 2020. I had just heard that one of my patients had been diagnosed with COVID-19 and admitted to Evergreen Health, a hospital our practice covered just outside of Seattle. The news was jarring. Suddenly, it became crystal clear that patient access to care and the economic survival of our business would require another approach. Seemingly overnight, we built a telehealth program and began seeing patients virtually from the comfort and safety of home.
We certainly weren’t alone. From January to March 2020, the Centers for Disease Control and Prevention showed a 154% increase in telehealth visits.1 Even as the postpandemic era settles in, the use of telehealth today is 38 times greater than the pre-COVID baseline, creating a market valued at $250 billion per year.2 What value might gastroenterologists gain from the use of telehealth going forward? 3 For today’s overburdened GI practices, telehealth can improve patient access to care, alleviate the clinician shortage with work-from-home options for practitioners, and present innovative methods of increasing revenue streams – all while improving quality of care.
As GI demand outpaces supply, it’s time to consider alternative channels of care
The prevalence of gastrointestinal illness, the size of the market, and the growing difficulty in gaining access to care makes it natural to consider whether virtual care may benefit patients and GI practices alike. Approximately 70 million Americans, or 1 in 5, live with chronic GI symptoms.4 On an annual basis, more than 50 million primary care visits and 15 million ER visits in the United States have a primary diagnostic code for GI disease.5 Annual expenditures to address GI conditions, valued at $136 billion, outpace those of other high-cost conditions such as heart disease or mental health.6 And with the recent addition of 21 million patients between 45 and 49 years of age who now require colon cancer screening, plus the expected postpandemic increase in GI illness, those numbers are likely to grow.7
Compounding matters is a shortage of clinicians. Between early physician retirements and a limited number of GI fellowships, gastroenterology was recently identified by a Merritt Hawkins survey as the “most in-demand” specialty.8 Patients are already waiting months, and even up to a year in some parts of the country, to see a gastroenterologist. GI physicians, likewise, are running ragged trying to keep up and are burning out in the process.
The case for virtual GI care
Until the pandemic, many of us would not have seriously considered a significant role for virtual care in GI. When necessity demanded it, however, we used this channel effectively with both patients and providers reporting high rates of satisfaction with telehealth for GI clinic visits.9
In a recent published study with a sizable cohort of GI patients across a wide spectrum of conditions, only 17% required a physical exam following a telehealth visit. Over 50% said they were very likely or likely to continue using telehealth in the future. Interestingly, it was not only a young or tech-savvy population that ranked telehealth highly. In fact, Net Promoter Scores (a proven measure of customer experience) were consistently high for employed patients aged 60 or younger.10
Recent research also has demonstrated that telehealth visits meet quality standards and do so efficiently. A Mayo Clinic study demonstrated that telehealth visits in GI were delivered with a similar level of quality based on diagnostic concordance,11 and a recent study by Tang et al. found that 98% of visits for routine GI issues were completed within 20 minutes.12
Finally, establishing a virtual channel allows a clinic to increase its staffing radius by using geographically dispersed GI providers, including appropriately licensed physicians or advanced practice providers who may reside in other states. The use of remote providers opens up the possibility for “time zone arbitrage” to allow for more flexible staffing that’s similar to urgent care with wraparound and weekend hours – all without adding office space or overhead.
Financial implications
Given the long tail of demand in GI, increasing capacity will increase revenue. Telehealth increases capacity by allowing for the efficient use of resources and expanding the reach of practices in engaging potential providers.
The majority of telehealth visits are reimbursable. Since 1995, 40 states and the District of Columbia have enacted mandatory telehealth coverage laws, and 20 states require that telehealth visits be paid on par with in-person visits.13 With the pandemic Medicare waivers, parity was extended through government programs and is expected by many insiders to continue in some form going forward. By an overwhelming bipartisan majority, the House of Representatives recently passed the Advancing Telehealth Beyond COVID-19 Act, which would extend most temporary telemedicine policies through 2024. This legislation would affect only Medicare reimbursement, but changes in Medicare policy often influence the policies of commercial payers.14
While reimbursement for clinic visits is important, the larger financial implication for extending clinics virtually is in the endoscopy suite. Most revenue (70%-80%) in community GI practices is generated from endoscopic services and related ancillary streams. For an endoscopist, spending time in the clinic is effectively a loss leader. Adding capacity with a virtual clinic and geographically dispersed providers can open up GI physicians to spend more time in the endoscopy suite, thereby generating additional revenue.
Given the rapid consolidation of the GI space, income repair post private equity transaction is top of mind for both established physicians and young physicians entering the labor market. Having a virtual ancillary differentiates practices and may prove useful for recruitment. Increasing access by using remote providers during evenings and weekends may “unclog the pipes,” improve the patient and provider experience, and increase revenue.
Overcoming obstacles
Creating a telehealth platform – particularly one that crosses state lines – requires an understanding of a complex and evolving regulatory environment. Licensing is one example. When telehealth is used, it is considered to be rendered at the location of the patient. A provider typically has to be licensed in the state where the patient is located at the time of the clinical encounter. So, if providers cross jurisdictional boundaries to provide care, multiple state licenses may be required.
In addition, medical malpractice and cyber insurance for telemedicine providers are niche products. And as with the use of any technology, risks of a data breach or other unauthorized disclosure of protected health information make it vital to ensure data are fully encrypted, networks are secure, and all safeguards are followed according to the Health Information and Portability and Accountability Act (HIPAA).
Perhaps most challenging are payers, both commercial and governmental. The location of a distant site provider can affect network participation for some but not all payers. Understanding payer reimbursement policies is time-intensive, and building relationships within these organizations is crucial in today’s rapidly changing environment.
The ultimate aim: Better patient outcomes
Of course, the main goal is to take care of patients well and in a timely fashion. Better access will lead to an improved patient experience and a greater emphasis on the important cognitive aspects of GI care. Moreover, efficient use of physician time will also improve clinician satisfaction while increasing revenue and downstream value. Most importantly, increased access via a virtual channel may positively impact patient outcomes. For instance, data show that distance from an endoscopy center is negatively associated with the stage of colon cancer diagnosis.15 Providing a virtual channel to reach these distant patients will likely increase the opportunity for high-impact procedures like colonoscopy.
Change can be hard, but it will come
The old saying is that change comes slowly, then all at once. Access is a chronic pain point for GI practices that has now reached a critical level.
The GI market is enormous and rapidly evolving; it will continue to attract disruptive interest and several early-stage digital first GI companies have entered the ecosystem. There is a risk for disintermediation as well as opportunities for collaboration. The next few years will be interesting.
As we transition to a postpandemic environment, telehealth can continue to improve patient access and present new revenue streams for GI practices – all while improving quality of care. Seeing around the corner likely means expanding the reach of your clinic and offering multiple channels of care. There is likely a significant opportunity for those who choose to adapt.
Dr. Arjal is cofounder, chief medical officer, and president of Telebelly Health and is a board-certified gastroenterologist who previously served as vice president of Puget Sound Gastroenterology and a vice president of clinical affairs for GastroHealth. He currently serves on the American Gastroenterological Association (AGA) Practice Management and Economics Committee. He has no conflicts. He is on LinkedIn and Twitter (@RussArjalMD).
References
1. Koonin LM et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic – United States, January-March 2020. MMWR Morb Mortal Wkly Rep. 2020. Oct 30;69(43):1595-9.
2. “Telehealth: A quarter-trillion-dollar post-COVID-19 reality?” McKinsey & Company, July 9, 2021.
3. The telehealth era is just beginning, Robert Pearl and Brian Wayling, Harvard Business Review, May-June, 2022.
4. Peery et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology. 2019. Jan;156(1):254-72.
5. See id.
6. See id.
7. Sieh, K. Post-COVID-19 functional gastrointestinal disorders: Prepare for a GI aftershock. J Gastroenterol Hepatol. 2022 March;37(3):413-4.
8. Newitt, P. Gastroenterology’s biggest threats. Becker’s, GI & Endoscopy, 2021 Oct 8, and Physician Compensation Report, 2022. Physicians Thrive (projecting a shortage of over 1,600 Gastroenterologists by 2025).
9. Dobrusin et al. Gastroenterologists and patients report high satisfaction rates with Telehealth services during the novel coronavirus 2019 pandemic. Clin Gastroenterol Hepatol. 2020;8(11):2393-7.
10. Dobrusin et al. Patients with gastrointestinal conditions consider telehealth equivalent to in-person care. Gastroenterology. 2022 Oct 4. doi: 10.1053/j.gastro.2022.09.035.
11. Demaerschalk et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June, 2020. JAMA Netw Open. 2022 Sep;5(9):e2229958.
12. Tang et al. A model for the pandemic and beyond: Telemedicine for all gastroenterology referrals reduces unnecessary clinic visits. J Telemed Telecare. 2022 Sep 28(8):577-82.
13. Dills A. Policy brief: Telehealth payment parity laws at the state level. Mercatus Center, George Mason University.
14. H.R.4040 – Advancing Telehealth Beyond COVID-19 Act of 2021. Congress.gov.
15. Brand et al. Association of distance, region, and insurance with advanced colon cancer at initial diagnosis. JAMA Netw Open. 2022 Sep 1;5(9):e2229954.
The first time I considered telehealth as a viable option for care delivery was in February 2020. I had just heard that one of my patients had been diagnosed with COVID-19 and admitted to Evergreen Health, a hospital our practice covered just outside of Seattle. The news was jarring. Suddenly, it became crystal clear that patient access to care and the economic survival of our business would require another approach. Seemingly overnight, we built a telehealth program and began seeing patients virtually from the comfort and safety of home.
We certainly weren’t alone. From January to March 2020, the Centers for Disease Control and Prevention showed a 154% increase in telehealth visits.1 Even as the postpandemic era settles in, the use of telehealth today is 38 times greater than the pre-COVID baseline, creating a market valued at $250 billion per year.2 What value might gastroenterologists gain from the use of telehealth going forward? 3 For today’s overburdened GI practices, telehealth can improve patient access to care, alleviate the clinician shortage with work-from-home options for practitioners, and present innovative methods of increasing revenue streams – all while improving quality of care.
As GI demand outpaces supply, it’s time to consider alternative channels of care
The prevalence of gastrointestinal illness, the size of the market, and the growing difficulty in gaining access to care makes it natural to consider whether virtual care may benefit patients and GI practices alike. Approximately 70 million Americans, or 1 in 5, live with chronic GI symptoms.4 On an annual basis, more than 50 million primary care visits and 15 million ER visits in the United States have a primary diagnostic code for GI disease.5 Annual expenditures to address GI conditions, valued at $136 billion, outpace those of other high-cost conditions such as heart disease or mental health.6 And with the recent addition of 21 million patients between 45 and 49 years of age who now require colon cancer screening, plus the expected postpandemic increase in GI illness, those numbers are likely to grow.7
Compounding matters is a shortage of clinicians. Between early physician retirements and a limited number of GI fellowships, gastroenterology was recently identified by a Merritt Hawkins survey as the “most in-demand” specialty.8 Patients are already waiting months, and even up to a year in some parts of the country, to see a gastroenterologist. GI physicians, likewise, are running ragged trying to keep up and are burning out in the process.
The case for virtual GI care
Until the pandemic, many of us would not have seriously considered a significant role for virtual care in GI. When necessity demanded it, however, we used this channel effectively with both patients and providers reporting high rates of satisfaction with telehealth for GI clinic visits.9
In a recent published study with a sizable cohort of GI patients across a wide spectrum of conditions, only 17% required a physical exam following a telehealth visit. Over 50% said they were very likely or likely to continue using telehealth in the future. Interestingly, it was not only a young or tech-savvy population that ranked telehealth highly. In fact, Net Promoter Scores (a proven measure of customer experience) were consistently high for employed patients aged 60 or younger.10
Recent research also has demonstrated that telehealth visits meet quality standards and do so efficiently. A Mayo Clinic study demonstrated that telehealth visits in GI were delivered with a similar level of quality based on diagnostic concordance,11 and a recent study by Tang et al. found that 98% of visits for routine GI issues were completed within 20 minutes.12
Finally, establishing a virtual channel allows a clinic to increase its staffing radius by using geographically dispersed GI providers, including appropriately licensed physicians or advanced practice providers who may reside in other states. The use of remote providers opens up the possibility for “time zone arbitrage” to allow for more flexible staffing that’s similar to urgent care with wraparound and weekend hours – all without adding office space or overhead.
Financial implications
Given the long tail of demand in GI, increasing capacity will increase revenue. Telehealth increases capacity by allowing for the efficient use of resources and expanding the reach of practices in engaging potential providers.
The majority of telehealth visits are reimbursable. Since 1995, 40 states and the District of Columbia have enacted mandatory telehealth coverage laws, and 20 states require that telehealth visits be paid on par with in-person visits.13 With the pandemic Medicare waivers, parity was extended through government programs and is expected by many insiders to continue in some form going forward. By an overwhelming bipartisan majority, the House of Representatives recently passed the Advancing Telehealth Beyond COVID-19 Act, which would extend most temporary telemedicine policies through 2024. This legislation would affect only Medicare reimbursement, but changes in Medicare policy often influence the policies of commercial payers.14
While reimbursement for clinic visits is important, the larger financial implication for extending clinics virtually is in the endoscopy suite. Most revenue (70%-80%) in community GI practices is generated from endoscopic services and related ancillary streams. For an endoscopist, spending time in the clinic is effectively a loss leader. Adding capacity with a virtual clinic and geographically dispersed providers can open up GI physicians to spend more time in the endoscopy suite, thereby generating additional revenue.
Given the rapid consolidation of the GI space, income repair post private equity transaction is top of mind for both established physicians and young physicians entering the labor market. Having a virtual ancillary differentiates practices and may prove useful for recruitment. Increasing access by using remote providers during evenings and weekends may “unclog the pipes,” improve the patient and provider experience, and increase revenue.
Overcoming obstacles
Creating a telehealth platform – particularly one that crosses state lines – requires an understanding of a complex and evolving regulatory environment. Licensing is one example. When telehealth is used, it is considered to be rendered at the location of the patient. A provider typically has to be licensed in the state where the patient is located at the time of the clinical encounter. So, if providers cross jurisdictional boundaries to provide care, multiple state licenses may be required.
In addition, medical malpractice and cyber insurance for telemedicine providers are niche products. And as with the use of any technology, risks of a data breach or other unauthorized disclosure of protected health information make it vital to ensure data are fully encrypted, networks are secure, and all safeguards are followed according to the Health Information and Portability and Accountability Act (HIPAA).
Perhaps most challenging are payers, both commercial and governmental. The location of a distant site provider can affect network participation for some but not all payers. Understanding payer reimbursement policies is time-intensive, and building relationships within these organizations is crucial in today’s rapidly changing environment.
The ultimate aim: Better patient outcomes
Of course, the main goal is to take care of patients well and in a timely fashion. Better access will lead to an improved patient experience and a greater emphasis on the important cognitive aspects of GI care. Moreover, efficient use of physician time will also improve clinician satisfaction while increasing revenue and downstream value. Most importantly, increased access via a virtual channel may positively impact patient outcomes. For instance, data show that distance from an endoscopy center is negatively associated with the stage of colon cancer diagnosis.15 Providing a virtual channel to reach these distant patients will likely increase the opportunity for high-impact procedures like colonoscopy.
Change can be hard, but it will come
The old saying is that change comes slowly, then all at once. Access is a chronic pain point for GI practices that has now reached a critical level.
The GI market is enormous and rapidly evolving; it will continue to attract disruptive interest and several early-stage digital first GI companies have entered the ecosystem. There is a risk for disintermediation as well as opportunities for collaboration. The next few years will be interesting.
As we transition to a postpandemic environment, telehealth can continue to improve patient access and present new revenue streams for GI practices – all while improving quality of care. Seeing around the corner likely means expanding the reach of your clinic and offering multiple channels of care. There is likely a significant opportunity for those who choose to adapt.
Dr. Arjal is cofounder, chief medical officer, and president of Telebelly Health and is a board-certified gastroenterologist who previously served as vice president of Puget Sound Gastroenterology and a vice president of clinical affairs for GastroHealth. He currently serves on the American Gastroenterological Association (AGA) Practice Management and Economics Committee. He has no conflicts. He is on LinkedIn and Twitter (@RussArjalMD).
References
1. Koonin LM et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic – United States, January-March 2020. MMWR Morb Mortal Wkly Rep. 2020. Oct 30;69(43):1595-9.
2. “Telehealth: A quarter-trillion-dollar post-COVID-19 reality?” McKinsey & Company, July 9, 2021.
3. The telehealth era is just beginning, Robert Pearl and Brian Wayling, Harvard Business Review, May-June, 2022.
4. Peery et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology. 2019. Jan;156(1):254-72.
5. See id.
6. See id.
7. Sieh, K. Post-COVID-19 functional gastrointestinal disorders: Prepare for a GI aftershock. J Gastroenterol Hepatol. 2022 March;37(3):413-4.
8. Newitt, P. Gastroenterology’s biggest threats. Becker’s, GI & Endoscopy, 2021 Oct 8, and Physician Compensation Report, 2022. Physicians Thrive (projecting a shortage of over 1,600 Gastroenterologists by 2025).
9. Dobrusin et al. Gastroenterologists and patients report high satisfaction rates with Telehealth services during the novel coronavirus 2019 pandemic. Clin Gastroenterol Hepatol. 2020;8(11):2393-7.
10. Dobrusin et al. Patients with gastrointestinal conditions consider telehealth equivalent to in-person care. Gastroenterology. 2022 Oct 4. doi: 10.1053/j.gastro.2022.09.035.
11. Demaerschalk et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June, 2020. JAMA Netw Open. 2022 Sep;5(9):e2229958.
12. Tang et al. A model for the pandemic and beyond: Telemedicine for all gastroenterology referrals reduces unnecessary clinic visits. J Telemed Telecare. 2022 Sep 28(8):577-82.
13. Dills A. Policy brief: Telehealth payment parity laws at the state level. Mercatus Center, George Mason University.
14. H.R.4040 – Advancing Telehealth Beyond COVID-19 Act of 2021. Congress.gov.
15. Brand et al. Association of distance, region, and insurance with advanced colon cancer at initial diagnosis. JAMA Netw Open. 2022 Sep 1;5(9):e2229954.
The first time I considered telehealth as a viable option for care delivery was in February 2020. I had just heard that one of my patients had been diagnosed with COVID-19 and admitted to Evergreen Health, a hospital our practice covered just outside of Seattle. The news was jarring. Suddenly, it became crystal clear that patient access to care and the economic survival of our business would require another approach. Seemingly overnight, we built a telehealth program and began seeing patients virtually from the comfort and safety of home.
We certainly weren’t alone. From January to March 2020, the Centers for Disease Control and Prevention showed a 154% increase in telehealth visits.1 Even as the postpandemic era settles in, the use of telehealth today is 38 times greater than the pre-COVID baseline, creating a market valued at $250 billion per year.2 What value might gastroenterologists gain from the use of telehealth going forward? 3 For today’s overburdened GI practices, telehealth can improve patient access to care, alleviate the clinician shortage with work-from-home options for practitioners, and present innovative methods of increasing revenue streams – all while improving quality of care.
As GI demand outpaces supply, it’s time to consider alternative channels of care
The prevalence of gastrointestinal illness, the size of the market, and the growing difficulty in gaining access to care makes it natural to consider whether virtual care may benefit patients and GI practices alike. Approximately 70 million Americans, or 1 in 5, live with chronic GI symptoms.4 On an annual basis, more than 50 million primary care visits and 15 million ER visits in the United States have a primary diagnostic code for GI disease.5 Annual expenditures to address GI conditions, valued at $136 billion, outpace those of other high-cost conditions such as heart disease or mental health.6 And with the recent addition of 21 million patients between 45 and 49 years of age who now require colon cancer screening, plus the expected postpandemic increase in GI illness, those numbers are likely to grow.7
Compounding matters is a shortage of clinicians. Between early physician retirements and a limited number of GI fellowships, gastroenterology was recently identified by a Merritt Hawkins survey as the “most in-demand” specialty.8 Patients are already waiting months, and even up to a year in some parts of the country, to see a gastroenterologist. GI physicians, likewise, are running ragged trying to keep up and are burning out in the process.
The case for virtual GI care
Until the pandemic, many of us would not have seriously considered a significant role for virtual care in GI. When necessity demanded it, however, we used this channel effectively with both patients and providers reporting high rates of satisfaction with telehealth for GI clinic visits.9
In a recent published study with a sizable cohort of GI patients across a wide spectrum of conditions, only 17% required a physical exam following a telehealth visit. Over 50% said they were very likely or likely to continue using telehealth in the future. Interestingly, it was not only a young or tech-savvy population that ranked telehealth highly. In fact, Net Promoter Scores (a proven measure of customer experience) were consistently high for employed patients aged 60 or younger.10
Recent research also has demonstrated that telehealth visits meet quality standards and do so efficiently. A Mayo Clinic study demonstrated that telehealth visits in GI were delivered with a similar level of quality based on diagnostic concordance,11 and a recent study by Tang et al. found that 98% of visits for routine GI issues were completed within 20 minutes.12
Finally, establishing a virtual channel allows a clinic to increase its staffing radius by using geographically dispersed GI providers, including appropriately licensed physicians or advanced practice providers who may reside in other states. The use of remote providers opens up the possibility for “time zone arbitrage” to allow for more flexible staffing that’s similar to urgent care with wraparound and weekend hours – all without adding office space or overhead.
Financial implications
Given the long tail of demand in GI, increasing capacity will increase revenue. Telehealth increases capacity by allowing for the efficient use of resources and expanding the reach of practices in engaging potential providers.
The majority of telehealth visits are reimbursable. Since 1995, 40 states and the District of Columbia have enacted mandatory telehealth coverage laws, and 20 states require that telehealth visits be paid on par with in-person visits.13 With the pandemic Medicare waivers, parity was extended through government programs and is expected by many insiders to continue in some form going forward. By an overwhelming bipartisan majority, the House of Representatives recently passed the Advancing Telehealth Beyond COVID-19 Act, which would extend most temporary telemedicine policies through 2024. This legislation would affect only Medicare reimbursement, but changes in Medicare policy often influence the policies of commercial payers.14
While reimbursement for clinic visits is important, the larger financial implication for extending clinics virtually is in the endoscopy suite. Most revenue (70%-80%) in community GI practices is generated from endoscopic services and related ancillary streams. For an endoscopist, spending time in the clinic is effectively a loss leader. Adding capacity with a virtual clinic and geographically dispersed providers can open up GI physicians to spend more time in the endoscopy suite, thereby generating additional revenue.
Given the rapid consolidation of the GI space, income repair post private equity transaction is top of mind for both established physicians and young physicians entering the labor market. Having a virtual ancillary differentiates practices and may prove useful for recruitment. Increasing access by using remote providers during evenings and weekends may “unclog the pipes,” improve the patient and provider experience, and increase revenue.
Overcoming obstacles
Creating a telehealth platform – particularly one that crosses state lines – requires an understanding of a complex and evolving regulatory environment. Licensing is one example. When telehealth is used, it is considered to be rendered at the location of the patient. A provider typically has to be licensed in the state where the patient is located at the time of the clinical encounter. So, if providers cross jurisdictional boundaries to provide care, multiple state licenses may be required.
In addition, medical malpractice and cyber insurance for telemedicine providers are niche products. And as with the use of any technology, risks of a data breach or other unauthorized disclosure of protected health information make it vital to ensure data are fully encrypted, networks are secure, and all safeguards are followed according to the Health Information and Portability and Accountability Act (HIPAA).
Perhaps most challenging are payers, both commercial and governmental. The location of a distant site provider can affect network participation for some but not all payers. Understanding payer reimbursement policies is time-intensive, and building relationships within these organizations is crucial in today’s rapidly changing environment.
The ultimate aim: Better patient outcomes
Of course, the main goal is to take care of patients well and in a timely fashion. Better access will lead to an improved patient experience and a greater emphasis on the important cognitive aspects of GI care. Moreover, efficient use of physician time will also improve clinician satisfaction while increasing revenue and downstream value. Most importantly, increased access via a virtual channel may positively impact patient outcomes. For instance, data show that distance from an endoscopy center is negatively associated with the stage of colon cancer diagnosis.15 Providing a virtual channel to reach these distant patients will likely increase the opportunity for high-impact procedures like colonoscopy.
Change can be hard, but it will come
The old saying is that change comes slowly, then all at once. Access is a chronic pain point for GI practices that has now reached a critical level.
The GI market is enormous and rapidly evolving; it will continue to attract disruptive interest and several early-stage digital first GI companies have entered the ecosystem. There is a risk for disintermediation as well as opportunities for collaboration. The next few years will be interesting.
As we transition to a postpandemic environment, telehealth can continue to improve patient access and present new revenue streams for GI practices – all while improving quality of care. Seeing around the corner likely means expanding the reach of your clinic and offering multiple channels of care. There is likely a significant opportunity for those who choose to adapt.
Dr. Arjal is cofounder, chief medical officer, and president of Telebelly Health and is a board-certified gastroenterologist who previously served as vice president of Puget Sound Gastroenterology and a vice president of clinical affairs for GastroHealth. He currently serves on the American Gastroenterological Association (AGA) Practice Management and Economics Committee. He has no conflicts. He is on LinkedIn and Twitter (@RussArjalMD).
References
1. Koonin LM et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic – United States, January-March 2020. MMWR Morb Mortal Wkly Rep. 2020. Oct 30;69(43):1595-9.
2. “Telehealth: A quarter-trillion-dollar post-COVID-19 reality?” McKinsey & Company, July 9, 2021.
3. The telehealth era is just beginning, Robert Pearl and Brian Wayling, Harvard Business Review, May-June, 2022.
4. Peery et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology. 2019. Jan;156(1):254-72.
5. See id.
6. See id.
7. Sieh, K. Post-COVID-19 functional gastrointestinal disorders: Prepare for a GI aftershock. J Gastroenterol Hepatol. 2022 March;37(3):413-4.
8. Newitt, P. Gastroenterology’s biggest threats. Becker’s, GI & Endoscopy, 2021 Oct 8, and Physician Compensation Report, 2022. Physicians Thrive (projecting a shortage of over 1,600 Gastroenterologists by 2025).
9. Dobrusin et al. Gastroenterologists and patients report high satisfaction rates with Telehealth services during the novel coronavirus 2019 pandemic. Clin Gastroenterol Hepatol. 2020;8(11):2393-7.
10. Dobrusin et al. Patients with gastrointestinal conditions consider telehealth equivalent to in-person care. Gastroenterology. 2022 Oct 4. doi: 10.1053/j.gastro.2022.09.035.
11. Demaerschalk et al. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at Mayo Clinic during the beginning of COVID-19 pandemic from March to June, 2020. JAMA Netw Open. 2022 Sep;5(9):e2229958.
12. Tang et al. A model for the pandemic and beyond: Telemedicine for all gastroenterology referrals reduces unnecessary clinic visits. J Telemed Telecare. 2022 Sep 28(8):577-82.
13. Dills A. Policy brief: Telehealth payment parity laws at the state level. Mercatus Center, George Mason University.
14. H.R.4040 – Advancing Telehealth Beyond COVID-19 Act of 2021. Congress.gov.
15. Brand et al. Association of distance, region, and insurance with advanced colon cancer at initial diagnosis. JAMA Netw Open. 2022 Sep 1;5(9):e2229954.
Passive income for the astute gastroenterologist
I don’t think I heard the term “passive income” until I was already an attending gastroenterologist.
That was no surprise. Why would I as a gastroenterologist with a focus in inflammatory bowel diseases be even remotely interested in that term?
Like most physicians, I went into medicine to take care of patients. That was my entire dream. It was a pleasant surprise to hear that gastroenterologists were relatively well paid compared to many other internal medicine specialties.
That was a bonus. I was not practicing medicine for the money. I was here to do good, only. Money was the evil one. It’s no surprise money remained a taboo topic amongst physicians.
This is reflected in the lack of financial education in our training.
I went through all my medical training without getting any financial education. In my last year of training, I wondered how I was going to not end up being a burned out, overworked physician mom. I knew I was going to work in a large hospital-based practice or academic center. I was already aware that employed physicians had a higher burnout rate compared to independent physicians. My desperation to avoid what looked like the natural history of most physicians in medicine was what led me to my financial awakening, as you could call it.
I became curious about where my money was going as it hit my bank account. Where was I investing? How was I going to ensure that I wasn’t putting all my financial eggs in one basket by relying solely on my clinical income? This road led me into a world that I didn’t know existed. It was the world of physician entrepreneurs.
I began thinking more critically of how I was spending my time outside of the hospital. As a busy physician mom, there already were a lot of competing needs and demands on the 24 hours that I was limited to within a day. How could I get things done and increase my earnability without needing to exchange more time for money in a one-to-one ratio?
Passive income!
First of all, what exactly is passive income?
It refers to money earned that does not require you to physically and actively pump in time in order to get money out. For instance, seeing patients clinically is not passive. Performing procedures is not passive.
What are some examples of passive income?
• Dividend paying stocks or funds
• Investing through retirement accounts
• Passive real estate investment through syndications, crowdfunding, REITs
• Book writing
• Business partnership or ownership such as surgery center co-ownership
• Peer-to-peer lending
• Affiliate marketing
• House hacking
• Rent out your car
• Rent out your backyard/ swimming pool
• Invention with royalty payment
• Podcasting
There are some myths about passive income that are worth exploring
1. Passive income is completely passive: This is relative passivity, meaning that for every investment, there is a phase of learning, acquiring knowledge, vetting, and possibly researching that is not passive. After the initial phase of set up, most passive sources of income may require some monitoring or checking in. However, what makes an investment passive is the absence of that one-to-one ratio of input to output that would normally exist in a more active income source.
2. Making passive income is lazy: If you are a physician, you are probably not lazy. Yes, we have a high standard of expectation for ourselves, but anyone that is able to withstand the rigors of medical training, residency, and fellowship is not lazy in my books. Burnout can present in various ways, including apathy. Let’s not confuse that as lazy because, if we do, that would qualify as gaslighting and self-splaining. As someone that teaches physicians how to have money, here is my opinion: In order to make money ethically, there has to be exchange in value. One person gives value, the other gives money as a thank you. Value can be physical as seen in clinical work. Value can also be monetary. For example, I could give $100,000 to a start-up company that needs that money to execute their brilliant idea, and, in return for my investment, they could give me a 15% return per year. Is that lazy? Without this, their brilliant idea may not see daylight. Value exchange is the key. Giving value comes in different ways.
3. Finding ideas for passive income is hard: Many of us are invested in the stock market, most commonly through retirement accounts. This would qualify as passive income. Typically, we have simply elected that the growth in our investment or dividends be reinvested as we are choosing to use this money long term. In other words, if you have a retirement account, you already have passive income. The question now is how you can find additional passive ways to invest.
What are the benefits to passive income as a gastroenterologist?
1. Changing landscape of medicine: Over the last few decades, we have seen a growing shift in the landscape of medicine. There has been an increase in administrations surpassing the increase in physicians. There seem to be more and more growing bodies that are wedging between physicians and patients. This has led to increasing dissatisfaction for patients and physicians alike. In order to respond to these changes and create lasting changes, there is a need for a change in the leadership. It is fair to say that when you have a more diversified source of income, there is less pressure on a single source of income to provide “food and shelter” for your family. Physician leaders that are liberated have to have a sense of financial liberation.
2. Not putting eggs in one basket: At the beginning of the COVID-19 pandemic, there was significant fear of the unknown. Elective procedures were canceled, leading to financial strain for physicians. Gastroenterologists were not spared. When your income source is diverse, it provides more peace of mind.
3. Mental resourcefulness: This is an understated benefit of passive income and diversified income. As physicians, we went through a lot of hard work to get to where we are today. An average incoming medical student has had extensive demonstration of activity, volunteerism, and problem solving. Yet, as attending physicians, because of the burden of everyday clinical responsibilities and endless paperwork, as well as the platform and “warehouse” and “administrative-type involvement” in medicine, the average physician isn’t creating avenues to expend their cognitive abilities in a way that is diverse outside of the clinical setting. Having passive income opportunities creates a gym for mental resourcefulness that increases work satisfaction and may positively impact burnout.
4. Relationship building: As physicians, we tend to stick with our own. After working 60-80 hours per week, it is no surprise that most of your social network may end up being those that you work with. Passive income opportunities expose physicians to networking and social opportunities that may be critical for relationship building. This may improve mental wellness and overall sense of well-being.
5. Longevity in medicine: As more physicians elect to be employed by larger organizations outside of academics, sabbaticals are becoming less and less available. Having passive sources of income may permit a physician who would otherwise not be able to suffer loss of income the opportunity to take a leave of absence in the short term that may provide long-term longevity in medicine, while promoting wellness.
6. Wealth building: Wealth has had a negative reputation in the world. We seem to equate wealth as bad and being the source of evil. We forget that money is simply a tool that takes the shape of the container you place it in. If you are good, money becomes a tool for more good. Having passive income can help accelerate the journey to wealth building. This can be a great resource as physicians can support unique lifesaving, community-building, and environment-protecting initiatives, as well as support political candidates who will have a positive effect on patient care and the future of medicine.
I hope you are convinced that, Gastroenterologists have to do their due diligence to ensure that their finances are future proof to the best of their abilities.
Dr. Alli-Akintade, a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center, is founder of The MoneyFitMD and creator of The MoneyFitMD podcast (www.moneyfitmd.com).
I don’t think I heard the term “passive income” until I was already an attending gastroenterologist.
That was no surprise. Why would I as a gastroenterologist with a focus in inflammatory bowel diseases be even remotely interested in that term?
Like most physicians, I went into medicine to take care of patients. That was my entire dream. It was a pleasant surprise to hear that gastroenterologists were relatively well paid compared to many other internal medicine specialties.
That was a bonus. I was not practicing medicine for the money. I was here to do good, only. Money was the evil one. It’s no surprise money remained a taboo topic amongst physicians.
This is reflected in the lack of financial education in our training.
I went through all my medical training without getting any financial education. In my last year of training, I wondered how I was going to not end up being a burned out, overworked physician mom. I knew I was going to work in a large hospital-based practice or academic center. I was already aware that employed physicians had a higher burnout rate compared to independent physicians. My desperation to avoid what looked like the natural history of most physicians in medicine was what led me to my financial awakening, as you could call it.
I became curious about where my money was going as it hit my bank account. Where was I investing? How was I going to ensure that I wasn’t putting all my financial eggs in one basket by relying solely on my clinical income? This road led me into a world that I didn’t know existed. It was the world of physician entrepreneurs.
I began thinking more critically of how I was spending my time outside of the hospital. As a busy physician mom, there already were a lot of competing needs and demands on the 24 hours that I was limited to within a day. How could I get things done and increase my earnability without needing to exchange more time for money in a one-to-one ratio?
Passive income!
First of all, what exactly is passive income?
It refers to money earned that does not require you to physically and actively pump in time in order to get money out. For instance, seeing patients clinically is not passive. Performing procedures is not passive.
What are some examples of passive income?
• Dividend paying stocks or funds
• Investing through retirement accounts
• Passive real estate investment through syndications, crowdfunding, REITs
• Book writing
• Business partnership or ownership such as surgery center co-ownership
• Peer-to-peer lending
• Affiliate marketing
• House hacking
• Rent out your car
• Rent out your backyard/ swimming pool
• Invention with royalty payment
• Podcasting
There are some myths about passive income that are worth exploring
1. Passive income is completely passive: This is relative passivity, meaning that for every investment, there is a phase of learning, acquiring knowledge, vetting, and possibly researching that is not passive. After the initial phase of set up, most passive sources of income may require some monitoring or checking in. However, what makes an investment passive is the absence of that one-to-one ratio of input to output that would normally exist in a more active income source.
2. Making passive income is lazy: If you are a physician, you are probably not lazy. Yes, we have a high standard of expectation for ourselves, but anyone that is able to withstand the rigors of medical training, residency, and fellowship is not lazy in my books. Burnout can present in various ways, including apathy. Let’s not confuse that as lazy because, if we do, that would qualify as gaslighting and self-splaining. As someone that teaches physicians how to have money, here is my opinion: In order to make money ethically, there has to be exchange in value. One person gives value, the other gives money as a thank you. Value can be physical as seen in clinical work. Value can also be monetary. For example, I could give $100,000 to a start-up company that needs that money to execute their brilliant idea, and, in return for my investment, they could give me a 15% return per year. Is that lazy? Without this, their brilliant idea may not see daylight. Value exchange is the key. Giving value comes in different ways.
3. Finding ideas for passive income is hard: Many of us are invested in the stock market, most commonly through retirement accounts. This would qualify as passive income. Typically, we have simply elected that the growth in our investment or dividends be reinvested as we are choosing to use this money long term. In other words, if you have a retirement account, you already have passive income. The question now is how you can find additional passive ways to invest.
What are the benefits to passive income as a gastroenterologist?
1. Changing landscape of medicine: Over the last few decades, we have seen a growing shift in the landscape of medicine. There has been an increase in administrations surpassing the increase in physicians. There seem to be more and more growing bodies that are wedging between physicians and patients. This has led to increasing dissatisfaction for patients and physicians alike. In order to respond to these changes and create lasting changes, there is a need for a change in the leadership. It is fair to say that when you have a more diversified source of income, there is less pressure on a single source of income to provide “food and shelter” for your family. Physician leaders that are liberated have to have a sense of financial liberation.
2. Not putting eggs in one basket: At the beginning of the COVID-19 pandemic, there was significant fear of the unknown. Elective procedures were canceled, leading to financial strain for physicians. Gastroenterologists were not spared. When your income source is diverse, it provides more peace of mind.
3. Mental resourcefulness: This is an understated benefit of passive income and diversified income. As physicians, we went through a lot of hard work to get to where we are today. An average incoming medical student has had extensive demonstration of activity, volunteerism, and problem solving. Yet, as attending physicians, because of the burden of everyday clinical responsibilities and endless paperwork, as well as the platform and “warehouse” and “administrative-type involvement” in medicine, the average physician isn’t creating avenues to expend their cognitive abilities in a way that is diverse outside of the clinical setting. Having passive income opportunities creates a gym for mental resourcefulness that increases work satisfaction and may positively impact burnout.
4. Relationship building: As physicians, we tend to stick with our own. After working 60-80 hours per week, it is no surprise that most of your social network may end up being those that you work with. Passive income opportunities expose physicians to networking and social opportunities that may be critical for relationship building. This may improve mental wellness and overall sense of well-being.
5. Longevity in medicine: As more physicians elect to be employed by larger organizations outside of academics, sabbaticals are becoming less and less available. Having passive sources of income may permit a physician who would otherwise not be able to suffer loss of income the opportunity to take a leave of absence in the short term that may provide long-term longevity in medicine, while promoting wellness.
6. Wealth building: Wealth has had a negative reputation in the world. We seem to equate wealth as bad and being the source of evil. We forget that money is simply a tool that takes the shape of the container you place it in. If you are good, money becomes a tool for more good. Having passive income can help accelerate the journey to wealth building. This can be a great resource as physicians can support unique lifesaving, community-building, and environment-protecting initiatives, as well as support political candidates who will have a positive effect on patient care and the future of medicine.
I hope you are convinced that, Gastroenterologists have to do their due diligence to ensure that their finances are future proof to the best of their abilities.
Dr. Alli-Akintade, a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center, is founder of The MoneyFitMD and creator of The MoneyFitMD podcast (www.moneyfitmd.com).
I don’t think I heard the term “passive income” until I was already an attending gastroenterologist.
That was no surprise. Why would I as a gastroenterologist with a focus in inflammatory bowel diseases be even remotely interested in that term?
Like most physicians, I went into medicine to take care of patients. That was my entire dream. It was a pleasant surprise to hear that gastroenterologists were relatively well paid compared to many other internal medicine specialties.
That was a bonus. I was not practicing medicine for the money. I was here to do good, only. Money was the evil one. It’s no surprise money remained a taboo topic amongst physicians.
This is reflected in the lack of financial education in our training.
I went through all my medical training without getting any financial education. In my last year of training, I wondered how I was going to not end up being a burned out, overworked physician mom. I knew I was going to work in a large hospital-based practice or academic center. I was already aware that employed physicians had a higher burnout rate compared to independent physicians. My desperation to avoid what looked like the natural history of most physicians in medicine was what led me to my financial awakening, as you could call it.
I became curious about where my money was going as it hit my bank account. Where was I investing? How was I going to ensure that I wasn’t putting all my financial eggs in one basket by relying solely on my clinical income? This road led me into a world that I didn’t know existed. It was the world of physician entrepreneurs.
I began thinking more critically of how I was spending my time outside of the hospital. As a busy physician mom, there already were a lot of competing needs and demands on the 24 hours that I was limited to within a day. How could I get things done and increase my earnability without needing to exchange more time for money in a one-to-one ratio?
Passive income!
First of all, what exactly is passive income?
It refers to money earned that does not require you to physically and actively pump in time in order to get money out. For instance, seeing patients clinically is not passive. Performing procedures is not passive.
What are some examples of passive income?
• Dividend paying stocks or funds
• Investing through retirement accounts
• Passive real estate investment through syndications, crowdfunding, REITs
• Book writing
• Business partnership or ownership such as surgery center co-ownership
• Peer-to-peer lending
• Affiliate marketing
• House hacking
• Rent out your car
• Rent out your backyard/ swimming pool
• Invention with royalty payment
• Podcasting
There are some myths about passive income that are worth exploring
1. Passive income is completely passive: This is relative passivity, meaning that for every investment, there is a phase of learning, acquiring knowledge, vetting, and possibly researching that is not passive. After the initial phase of set up, most passive sources of income may require some monitoring or checking in. However, what makes an investment passive is the absence of that one-to-one ratio of input to output that would normally exist in a more active income source.
2. Making passive income is lazy: If you are a physician, you are probably not lazy. Yes, we have a high standard of expectation for ourselves, but anyone that is able to withstand the rigors of medical training, residency, and fellowship is not lazy in my books. Burnout can present in various ways, including apathy. Let’s not confuse that as lazy because, if we do, that would qualify as gaslighting and self-splaining. As someone that teaches physicians how to have money, here is my opinion: In order to make money ethically, there has to be exchange in value. One person gives value, the other gives money as a thank you. Value can be physical as seen in clinical work. Value can also be monetary. For example, I could give $100,000 to a start-up company that needs that money to execute their brilliant idea, and, in return for my investment, they could give me a 15% return per year. Is that lazy? Without this, their brilliant idea may not see daylight. Value exchange is the key. Giving value comes in different ways.
3. Finding ideas for passive income is hard: Many of us are invested in the stock market, most commonly through retirement accounts. This would qualify as passive income. Typically, we have simply elected that the growth in our investment or dividends be reinvested as we are choosing to use this money long term. In other words, if you have a retirement account, you already have passive income. The question now is how you can find additional passive ways to invest.
What are the benefits to passive income as a gastroenterologist?
1. Changing landscape of medicine: Over the last few decades, we have seen a growing shift in the landscape of medicine. There has been an increase in administrations surpassing the increase in physicians. There seem to be more and more growing bodies that are wedging between physicians and patients. This has led to increasing dissatisfaction for patients and physicians alike. In order to respond to these changes and create lasting changes, there is a need for a change in the leadership. It is fair to say that when you have a more diversified source of income, there is less pressure on a single source of income to provide “food and shelter” for your family. Physician leaders that are liberated have to have a sense of financial liberation.
2. Not putting eggs in one basket: At the beginning of the COVID-19 pandemic, there was significant fear of the unknown. Elective procedures were canceled, leading to financial strain for physicians. Gastroenterologists were not spared. When your income source is diverse, it provides more peace of mind.
3. Mental resourcefulness: This is an understated benefit of passive income and diversified income. As physicians, we went through a lot of hard work to get to where we are today. An average incoming medical student has had extensive demonstration of activity, volunteerism, and problem solving. Yet, as attending physicians, because of the burden of everyday clinical responsibilities and endless paperwork, as well as the platform and “warehouse” and “administrative-type involvement” in medicine, the average physician isn’t creating avenues to expend their cognitive abilities in a way that is diverse outside of the clinical setting. Having passive income opportunities creates a gym for mental resourcefulness that increases work satisfaction and may positively impact burnout.
4. Relationship building: As physicians, we tend to stick with our own. After working 60-80 hours per week, it is no surprise that most of your social network may end up being those that you work with. Passive income opportunities expose physicians to networking and social opportunities that may be critical for relationship building. This may improve mental wellness and overall sense of well-being.
5. Longevity in medicine: As more physicians elect to be employed by larger organizations outside of academics, sabbaticals are becoming less and less available. Having passive sources of income may permit a physician who would otherwise not be able to suffer loss of income the opportunity to take a leave of absence in the short term that may provide long-term longevity in medicine, while promoting wellness.
6. Wealth building: Wealth has had a negative reputation in the world. We seem to equate wealth as bad and being the source of evil. We forget that money is simply a tool that takes the shape of the container you place it in. If you are good, money becomes a tool for more good. Having passive income can help accelerate the journey to wealth building. This can be a great resource as physicians can support unique lifesaving, community-building, and environment-protecting initiatives, as well as support political candidates who will have a positive effect on patient care and the future of medicine.
I hope you are convinced that, Gastroenterologists have to do their due diligence to ensure that their finances are future proof to the best of their abilities.
Dr. Alli-Akintade, a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center, is founder of The MoneyFitMD and creator of The MoneyFitMD podcast (www.moneyfitmd.com).
This insurance agent thinks disability insurance deserves a rebrand, and he's a doctor
If you already have disability insurance, keep reading as well. I have a great tip for you from personal experience that made a difference in the job I selected.
Let’s start with an important rebrand for “disability insurance.” What does it protect? Income! Car insurance is not called crash insurance. House insurance is not called burnt house insurance. And unlike a car or a house, it protects an asset with 10-20 times as much value as a million-dollar house.
So, let’s call it what it is: “income protection insurance.”
It’s always a bit nerdy when I talk about how much I appreciate insurance that protects lifelong income. I often make an argument that it is simply one of the best products that exists, especially for high-income earners with lots of debt. Many of us doctors are in that category and are not even slightly jealous of our friends whose parents paid for school (I’m looking at you not-her-real-name-Mary).
Disability is not the catchiest name for a product, but it is more pronounceable than “ophthalmology” and way easier to spell. This is my specialty, and I can’t believe we still haven’t gone with “eye surgeon,” but I digress.
So, let’s rebrand “disability insurance” for the sake of clarity:
I personally like to think of it as a monthly subscription for a soft landing in a worst-case scenario. Call me a millennial, but it just goes down smoother in my mind as a subscription a la Netflix ... and the four other streaming services that someone gave me a password to – if you’re a 55-year-old GI specialist, I know you’re on the Spotify family plan, too. No judgment from me.
So, for $15, you get a bunch of movies with Netflix, and, for $150-$300, you cover a lifetime of income. That’s a pretty decent service even without “The Office.”
Disability insurance often covers at least $15-$20 million dollars over a lifetime of earnings for only 1%-2% of your salary per year.
But I’ll pause here. The numbers are irrelevant if you never get the insurance.
I have one goal for this article, and it is simply to try to help you break down that procrastination habit we all have. I will have added immense value to at least one family’s life if you go and get a policy this week that saves your family from substantial loss of income. This is why I love insurance.
Doctors sacrifice essential life steps to get through training. But we are not alone in that.
Tim Kasser, PhD, puts it well when he said: “We live in a machine that is designed to get us to neglect what is important about life.” Here he is talking about relationships, but securing financial protection is loving to those closest to us.
So, what holds us back from taking a seemingly easy step like locking in disability insurance early in training?
Is it the stress of residency? Studying for Step 1? Moving cities and finding a home during a housing crisis? Job change during COVID? Is it because we have already put it off so long that we don’t want to think about it?
Totally fair.
For all of us busy doctors, the necessity and obviousness of buying disability insurance, *ehem*, income protection insurance makes you feel like you can get to it when you get to it because you know you will, so ... what’s the rush?
Or, is it our desire to bet on ourselves, and every month that goes by without insurance is one less payment? Roll the dice! Woo!
The reason to not put off the important things in life
I will give you a few reasons of “the why of” how we can all benefit from disability insurance and the reason there is no benefit in waiting to get a policy.
But, most importantly, I want to talk to you about your life and why you are putting off a lot of important things.
That diet you’ve been wanting to start? Yep.
That ring you haven’t purchased? Maybe that!
That article you’ve been meaning to write for the GI journal? Yes, especially that.
Remember: Take a deep breath in and exhaaaaale.
So, why do we put off the important?
First, even though the “why” of purchasing income protection is a bit basic, I do find it helpful to have discrete reasons for accomplishing an important task.
Why get disability insurance at all?
Let’s look at the value we get out of covering our income.
Reason No. 1. It softens the landing in the event you have an illness. The stats on disability claims are heavily on the side of illness over accidents or trauma. As you know, many autoimmune conditions show up in the 20’s and 30’s, so those are the things your friends will have first.
Unfortunately, if you have a medical issue before you have a disability policy, you will either not have coverage for that specific condition or you will not be approved for insurance. Unlike health insurance, the company can afford to pay out policies because it is picky on who it is willing to cover. It tries to select healthy people, so apply when you are most healthy, if possible.
Reason No. 2. It’s cheap. When you compare with a $2 million policy for life insurance, it might cost $1,000-$2,000 or so per year for a term policy covering about 25 years. With disability insurance, you can cover about 10x as much for the same annual payment. One could easily make a case that if you do not have dependents, disability insurance should be your first stop even before life insurance. You are more likely to be disabled than to die when you’re in your thirties. Act accordingly.
(Please note for obvious reasons they don’t call life insurance “death insurance.” Disability insurance needs that same rebrand – I’m telling you!)
Reason No. 3. Unless you are independently wealthy, it will be nearly impossible to replace your income and live a similar lifestyle. Lock in the benefits of the work you have already accomplished, and lock in the coverage of ALL of your health while you are healthy.
Time to take action
As Elvis famously sang: “A little less conversation, a little more action please.”
Alright, so how do we get ourselves to ACT and get a policy to protect our income?
Tip No. 1. As doctors we often shoot for perfection. It’s no surprise, therefore, that we have an illusion that we need to find the “perfect policy.”
One of my friends is a great financial adviser, and he often tells me about first meetings with clients to create a long-lasting plan. Often, somewhere along the way when discussing risks of stocks going down and up, someone will ask, “Why don’t we pick one that is low risk but tends to go up in value?” Of course, the reality is that if it were that easy ... everyone would do it!
Fortunately, with disability insurance, the policies are fairly straight forward. You can skip the analysis paralysis with disability insurance by talking with an agent who consistently works with physicians. I enjoy talking policies and helping doctors protect their financial health, so I started selling policies shortly after residency because so many of my co-residents were making me nervous putting it off. Some I helped, and some put it off and are unable to get policies after health issues even just 3 years after residency.
Tip No. 2. Having a policy is better than not having one, and if you’re worried about getting the wrong one, just get two! Seriously, some companies let you split coverage between two and this can even increase the maximum coverage you can get later in life, too. Does it add cost? Surprisingly, it typically does not, and it does not make the agent more money either. In most cases it’s actually more work for them for the same amount of commission. Don’t be afraid to ask about this.
Tip No. 3. This is my hot tip for current policy owners: ask for the full version of your policy, and read the entire policy. I recently asked for my policy because I was doing some international work abroad and wanted to know if I could reside abroad if I made a disability claim. My policy stated that I would need to reside in the United States within 12 months of disability. I likely would do this in the event of disability, but it is quite important to know these aspects.
While reading the fine print, I found that a minimum number of work-hours per week (35 for my policy) was required to qualify for my physician-specific coverage. This was an important part of my job criteria when looking for a new position and is worth investigating for anyone considering part-time employment.
Tip No. 4. The obvious tip: The fear of failure gets a lot of perfectionists from even starting a task unless they know everything about it.
Just start.
That’s my go-to for overcoming fear of failure. You won’t fail. You just won’t. You will learn!
Pretend you are curious about it and try with any of these actionable steps:
- Google disability insurance.
- Email me at [email protected].
- Read an article on a doctor-based blog.
I personally geeked out on insurance so much in residency that I became an insurance agent. I am an independent broker, so I have no bias toward any particular policies (email me anytime even if just with questions). Personally, I believe in this product and the value of this type of insurance, and I would hate for anyone to not have coverage of their most valuable asset: lifelong income!
The steps of applying for disability insurance
Now you know all the great reasons to get going! What are the next steps?
No matter where you get your policy, you can expect the process to be fairly simple. If it’s not then shoot me an email and I’m happy to help chat and discuss further.
The general process is:
Step 1. Initial phone call or email: Chat with an agent to discuss your needs and situation. Immediately after, you can sign initial application documents with DocuSign. (20 minutes).
Step 2. Complete health questionnaire on the phone with the insurance company. (20-40 minutes).
Step 3. Sign the final documents and confirm physician-specific language in their policies. (20 minutes).
The whole application period typically lasts only 2-4 weeks from start to finish and, if you pay up front, you are covered from the moment you send in the check. If you don’t accept the policy, you even get the money back.
I genuinely enjoy talking with my colleagues from all over the world and learning about their lives and plans, so, if you have any questions, please do not hesitate to email me at [email protected]. Also, feel free to check out my mini-blog at curiousmd.com or listen to me chat with Jon Solitro, CFP, on his FinancialMD.com podcast. Similar to this article, it is fairly informal and covers real life, tough career decisions, and actionable financial planning tips.
If you made it to the end of this article, you are a perfectionist and should go back and read Tip No. 1.
Reference
The Context of Things. “We live in a machine that is designed to get us to neglect what’s important about life,” 2021 Aug 24.
Dr. Smith is an ophthalmologist and consultant with Advanced Eyecare Professionals, Grand Rapids, Mich., and founder of DigitalGlaucoma.com. He is cohost of The FinancialMD Show podcast. He is an insurance producer and assists clients with advising and decision-making related to disability insurance at FinancialMD.
If you already have disability insurance, keep reading as well. I have a great tip for you from personal experience that made a difference in the job I selected.
Let’s start with an important rebrand for “disability insurance.” What does it protect? Income! Car insurance is not called crash insurance. House insurance is not called burnt house insurance. And unlike a car or a house, it protects an asset with 10-20 times as much value as a million-dollar house.
So, let’s call it what it is: “income protection insurance.”
It’s always a bit nerdy when I talk about how much I appreciate insurance that protects lifelong income. I often make an argument that it is simply one of the best products that exists, especially for high-income earners with lots of debt. Many of us doctors are in that category and are not even slightly jealous of our friends whose parents paid for school (I’m looking at you not-her-real-name-Mary).
Disability is not the catchiest name for a product, but it is more pronounceable than “ophthalmology” and way easier to spell. This is my specialty, and I can’t believe we still haven’t gone with “eye surgeon,” but I digress.
So, let’s rebrand “disability insurance” for the sake of clarity:
I personally like to think of it as a monthly subscription for a soft landing in a worst-case scenario. Call me a millennial, but it just goes down smoother in my mind as a subscription a la Netflix ... and the four other streaming services that someone gave me a password to – if you’re a 55-year-old GI specialist, I know you’re on the Spotify family plan, too. No judgment from me.
So, for $15, you get a bunch of movies with Netflix, and, for $150-$300, you cover a lifetime of income. That’s a pretty decent service even without “The Office.”
Disability insurance often covers at least $15-$20 million dollars over a lifetime of earnings for only 1%-2% of your salary per year.
But I’ll pause here. The numbers are irrelevant if you never get the insurance.
I have one goal for this article, and it is simply to try to help you break down that procrastination habit we all have. I will have added immense value to at least one family’s life if you go and get a policy this week that saves your family from substantial loss of income. This is why I love insurance.
Doctors sacrifice essential life steps to get through training. But we are not alone in that.
Tim Kasser, PhD, puts it well when he said: “We live in a machine that is designed to get us to neglect what is important about life.” Here he is talking about relationships, but securing financial protection is loving to those closest to us.
So, what holds us back from taking a seemingly easy step like locking in disability insurance early in training?
Is it the stress of residency? Studying for Step 1? Moving cities and finding a home during a housing crisis? Job change during COVID? Is it because we have already put it off so long that we don’t want to think about it?
Totally fair.
For all of us busy doctors, the necessity and obviousness of buying disability insurance, *ehem*, income protection insurance makes you feel like you can get to it when you get to it because you know you will, so ... what’s the rush?
Or, is it our desire to bet on ourselves, and every month that goes by without insurance is one less payment? Roll the dice! Woo!
The reason to not put off the important things in life
I will give you a few reasons of “the why of” how we can all benefit from disability insurance and the reason there is no benefit in waiting to get a policy.
But, most importantly, I want to talk to you about your life and why you are putting off a lot of important things.
That diet you’ve been wanting to start? Yep.
That ring you haven’t purchased? Maybe that!
That article you’ve been meaning to write for the GI journal? Yes, especially that.
Remember: Take a deep breath in and exhaaaaale.
So, why do we put off the important?
First, even though the “why” of purchasing income protection is a bit basic, I do find it helpful to have discrete reasons for accomplishing an important task.
Why get disability insurance at all?
Let’s look at the value we get out of covering our income.
Reason No. 1. It softens the landing in the event you have an illness. The stats on disability claims are heavily on the side of illness over accidents or trauma. As you know, many autoimmune conditions show up in the 20’s and 30’s, so those are the things your friends will have first.
Unfortunately, if you have a medical issue before you have a disability policy, you will either not have coverage for that specific condition or you will not be approved for insurance. Unlike health insurance, the company can afford to pay out policies because it is picky on who it is willing to cover. It tries to select healthy people, so apply when you are most healthy, if possible.
Reason No. 2. It’s cheap. When you compare with a $2 million policy for life insurance, it might cost $1,000-$2,000 or so per year for a term policy covering about 25 years. With disability insurance, you can cover about 10x as much for the same annual payment. One could easily make a case that if you do not have dependents, disability insurance should be your first stop even before life insurance. You are more likely to be disabled than to die when you’re in your thirties. Act accordingly.
(Please note for obvious reasons they don’t call life insurance “death insurance.” Disability insurance needs that same rebrand – I’m telling you!)
Reason No. 3. Unless you are independently wealthy, it will be nearly impossible to replace your income and live a similar lifestyle. Lock in the benefits of the work you have already accomplished, and lock in the coverage of ALL of your health while you are healthy.
Time to take action
As Elvis famously sang: “A little less conversation, a little more action please.”
Alright, so how do we get ourselves to ACT and get a policy to protect our income?
Tip No. 1. As doctors we often shoot for perfection. It’s no surprise, therefore, that we have an illusion that we need to find the “perfect policy.”
One of my friends is a great financial adviser, and he often tells me about first meetings with clients to create a long-lasting plan. Often, somewhere along the way when discussing risks of stocks going down and up, someone will ask, “Why don’t we pick one that is low risk but tends to go up in value?” Of course, the reality is that if it were that easy ... everyone would do it!
Fortunately, with disability insurance, the policies are fairly straight forward. You can skip the analysis paralysis with disability insurance by talking with an agent who consistently works with physicians. I enjoy talking policies and helping doctors protect their financial health, so I started selling policies shortly after residency because so many of my co-residents were making me nervous putting it off. Some I helped, and some put it off and are unable to get policies after health issues even just 3 years after residency.
Tip No. 2. Having a policy is better than not having one, and if you’re worried about getting the wrong one, just get two! Seriously, some companies let you split coverage between two and this can even increase the maximum coverage you can get later in life, too. Does it add cost? Surprisingly, it typically does not, and it does not make the agent more money either. In most cases it’s actually more work for them for the same amount of commission. Don’t be afraid to ask about this.
Tip No. 3. This is my hot tip for current policy owners: ask for the full version of your policy, and read the entire policy. I recently asked for my policy because I was doing some international work abroad and wanted to know if I could reside abroad if I made a disability claim. My policy stated that I would need to reside in the United States within 12 months of disability. I likely would do this in the event of disability, but it is quite important to know these aspects.
While reading the fine print, I found that a minimum number of work-hours per week (35 for my policy) was required to qualify for my physician-specific coverage. This was an important part of my job criteria when looking for a new position and is worth investigating for anyone considering part-time employment.
Tip No. 4. The obvious tip: The fear of failure gets a lot of perfectionists from even starting a task unless they know everything about it.
Just start.
That’s my go-to for overcoming fear of failure. You won’t fail. You just won’t. You will learn!
Pretend you are curious about it and try with any of these actionable steps:
- Google disability insurance.
- Email me at [email protected].
- Read an article on a doctor-based blog.
I personally geeked out on insurance so much in residency that I became an insurance agent. I am an independent broker, so I have no bias toward any particular policies (email me anytime even if just with questions). Personally, I believe in this product and the value of this type of insurance, and I would hate for anyone to not have coverage of their most valuable asset: lifelong income!
The steps of applying for disability insurance
Now you know all the great reasons to get going! What are the next steps?
No matter where you get your policy, you can expect the process to be fairly simple. If it’s not then shoot me an email and I’m happy to help chat and discuss further.
The general process is:
Step 1. Initial phone call or email: Chat with an agent to discuss your needs and situation. Immediately after, you can sign initial application documents with DocuSign. (20 minutes).
Step 2. Complete health questionnaire on the phone with the insurance company. (20-40 minutes).
Step 3. Sign the final documents and confirm physician-specific language in their policies. (20 minutes).
The whole application period typically lasts only 2-4 weeks from start to finish and, if you pay up front, you are covered from the moment you send in the check. If you don’t accept the policy, you even get the money back.
I genuinely enjoy talking with my colleagues from all over the world and learning about their lives and plans, so, if you have any questions, please do not hesitate to email me at [email protected]. Also, feel free to check out my mini-blog at curiousmd.com or listen to me chat with Jon Solitro, CFP, on his FinancialMD.com podcast. Similar to this article, it is fairly informal and covers real life, tough career decisions, and actionable financial planning tips.
If you made it to the end of this article, you are a perfectionist and should go back and read Tip No. 1.
Reference
The Context of Things. “We live in a machine that is designed to get us to neglect what’s important about life,” 2021 Aug 24.
Dr. Smith is an ophthalmologist and consultant with Advanced Eyecare Professionals, Grand Rapids, Mich., and founder of DigitalGlaucoma.com. He is cohost of The FinancialMD Show podcast. He is an insurance producer and assists clients with advising and decision-making related to disability insurance at FinancialMD.
If you already have disability insurance, keep reading as well. I have a great tip for you from personal experience that made a difference in the job I selected.
Let’s start with an important rebrand for “disability insurance.” What does it protect? Income! Car insurance is not called crash insurance. House insurance is not called burnt house insurance. And unlike a car or a house, it protects an asset with 10-20 times as much value as a million-dollar house.
So, let’s call it what it is: “income protection insurance.”
It’s always a bit nerdy when I talk about how much I appreciate insurance that protects lifelong income. I often make an argument that it is simply one of the best products that exists, especially for high-income earners with lots of debt. Many of us doctors are in that category and are not even slightly jealous of our friends whose parents paid for school (I’m looking at you not-her-real-name-Mary).
Disability is not the catchiest name for a product, but it is more pronounceable than “ophthalmology” and way easier to spell. This is my specialty, and I can’t believe we still haven’t gone with “eye surgeon,” but I digress.
So, let’s rebrand “disability insurance” for the sake of clarity:
I personally like to think of it as a monthly subscription for a soft landing in a worst-case scenario. Call me a millennial, but it just goes down smoother in my mind as a subscription a la Netflix ... and the four other streaming services that someone gave me a password to – if you’re a 55-year-old GI specialist, I know you’re on the Spotify family plan, too. No judgment from me.
So, for $15, you get a bunch of movies with Netflix, and, for $150-$300, you cover a lifetime of income. That’s a pretty decent service even without “The Office.”
Disability insurance often covers at least $15-$20 million dollars over a lifetime of earnings for only 1%-2% of your salary per year.
But I’ll pause here. The numbers are irrelevant if you never get the insurance.
I have one goal for this article, and it is simply to try to help you break down that procrastination habit we all have. I will have added immense value to at least one family’s life if you go and get a policy this week that saves your family from substantial loss of income. This is why I love insurance.
Doctors sacrifice essential life steps to get through training. But we are not alone in that.
Tim Kasser, PhD, puts it well when he said: “We live in a machine that is designed to get us to neglect what is important about life.” Here he is talking about relationships, but securing financial protection is loving to those closest to us.
So, what holds us back from taking a seemingly easy step like locking in disability insurance early in training?
Is it the stress of residency? Studying for Step 1? Moving cities and finding a home during a housing crisis? Job change during COVID? Is it because we have already put it off so long that we don’t want to think about it?
Totally fair.
For all of us busy doctors, the necessity and obviousness of buying disability insurance, *ehem*, income protection insurance makes you feel like you can get to it when you get to it because you know you will, so ... what’s the rush?
Or, is it our desire to bet on ourselves, and every month that goes by without insurance is one less payment? Roll the dice! Woo!
The reason to not put off the important things in life
I will give you a few reasons of “the why of” how we can all benefit from disability insurance and the reason there is no benefit in waiting to get a policy.
But, most importantly, I want to talk to you about your life and why you are putting off a lot of important things.
That diet you’ve been wanting to start? Yep.
That ring you haven’t purchased? Maybe that!
That article you’ve been meaning to write for the GI journal? Yes, especially that.
Remember: Take a deep breath in and exhaaaaale.
So, why do we put off the important?
First, even though the “why” of purchasing income protection is a bit basic, I do find it helpful to have discrete reasons for accomplishing an important task.
Why get disability insurance at all?
Let’s look at the value we get out of covering our income.
Reason No. 1. It softens the landing in the event you have an illness. The stats on disability claims are heavily on the side of illness over accidents or trauma. As you know, many autoimmune conditions show up in the 20’s and 30’s, so those are the things your friends will have first.
Unfortunately, if you have a medical issue before you have a disability policy, you will either not have coverage for that specific condition or you will not be approved for insurance. Unlike health insurance, the company can afford to pay out policies because it is picky on who it is willing to cover. It tries to select healthy people, so apply when you are most healthy, if possible.
Reason No. 2. It’s cheap. When you compare with a $2 million policy for life insurance, it might cost $1,000-$2,000 or so per year for a term policy covering about 25 years. With disability insurance, you can cover about 10x as much for the same annual payment. One could easily make a case that if you do not have dependents, disability insurance should be your first stop even before life insurance. You are more likely to be disabled than to die when you’re in your thirties. Act accordingly.
(Please note for obvious reasons they don’t call life insurance “death insurance.” Disability insurance needs that same rebrand – I’m telling you!)
Reason No. 3. Unless you are independently wealthy, it will be nearly impossible to replace your income and live a similar lifestyle. Lock in the benefits of the work you have already accomplished, and lock in the coverage of ALL of your health while you are healthy.
Time to take action
As Elvis famously sang: “A little less conversation, a little more action please.”
Alright, so how do we get ourselves to ACT and get a policy to protect our income?
Tip No. 1. As doctors we often shoot for perfection. It’s no surprise, therefore, that we have an illusion that we need to find the “perfect policy.”
One of my friends is a great financial adviser, and he often tells me about first meetings with clients to create a long-lasting plan. Often, somewhere along the way when discussing risks of stocks going down and up, someone will ask, “Why don’t we pick one that is low risk but tends to go up in value?” Of course, the reality is that if it were that easy ... everyone would do it!
Fortunately, with disability insurance, the policies are fairly straight forward. You can skip the analysis paralysis with disability insurance by talking with an agent who consistently works with physicians. I enjoy talking policies and helping doctors protect their financial health, so I started selling policies shortly after residency because so many of my co-residents were making me nervous putting it off. Some I helped, and some put it off and are unable to get policies after health issues even just 3 years after residency.
Tip No. 2. Having a policy is better than not having one, and if you’re worried about getting the wrong one, just get two! Seriously, some companies let you split coverage between two and this can even increase the maximum coverage you can get later in life, too. Does it add cost? Surprisingly, it typically does not, and it does not make the agent more money either. In most cases it’s actually more work for them for the same amount of commission. Don’t be afraid to ask about this.
Tip No. 3. This is my hot tip for current policy owners: ask for the full version of your policy, and read the entire policy. I recently asked for my policy because I was doing some international work abroad and wanted to know if I could reside abroad if I made a disability claim. My policy stated that I would need to reside in the United States within 12 months of disability. I likely would do this in the event of disability, but it is quite important to know these aspects.
While reading the fine print, I found that a minimum number of work-hours per week (35 for my policy) was required to qualify for my physician-specific coverage. This was an important part of my job criteria when looking for a new position and is worth investigating for anyone considering part-time employment.
Tip No. 4. The obvious tip: The fear of failure gets a lot of perfectionists from even starting a task unless they know everything about it.
Just start.
That’s my go-to for overcoming fear of failure. You won’t fail. You just won’t. You will learn!
Pretend you are curious about it and try with any of these actionable steps:
- Google disability insurance.
- Email me at [email protected].
- Read an article on a doctor-based blog.
I personally geeked out on insurance so much in residency that I became an insurance agent. I am an independent broker, so I have no bias toward any particular policies (email me anytime even if just with questions). Personally, I believe in this product and the value of this type of insurance, and I would hate for anyone to not have coverage of their most valuable asset: lifelong income!
The steps of applying for disability insurance
Now you know all the great reasons to get going! What are the next steps?
No matter where you get your policy, you can expect the process to be fairly simple. If it’s not then shoot me an email and I’m happy to help chat and discuss further.
The general process is:
Step 1. Initial phone call or email: Chat with an agent to discuss your needs and situation. Immediately after, you can sign initial application documents with DocuSign. (20 minutes).
Step 2. Complete health questionnaire on the phone with the insurance company. (20-40 minutes).
Step 3. Sign the final documents and confirm physician-specific language in their policies. (20 minutes).
The whole application period typically lasts only 2-4 weeks from start to finish and, if you pay up front, you are covered from the moment you send in the check. If you don’t accept the policy, you even get the money back.
I genuinely enjoy talking with my colleagues from all over the world and learning about their lives and plans, so, if you have any questions, please do not hesitate to email me at [email protected]. Also, feel free to check out my mini-blog at curiousmd.com or listen to me chat with Jon Solitro, CFP, on his FinancialMD.com podcast. Similar to this article, it is fairly informal and covers real life, tough career decisions, and actionable financial planning tips.
If you made it to the end of this article, you are a perfectionist and should go back and read Tip No. 1.
Reference
The Context of Things. “We live in a machine that is designed to get us to neglect what’s important about life,” 2021 Aug 24.
Dr. Smith is an ophthalmologist and consultant with Advanced Eyecare Professionals, Grand Rapids, Mich., and founder of DigitalGlaucoma.com. He is cohost of The FinancialMD Show podcast. He is an insurance producer and assists clients with advising and decision-making related to disability insurance at FinancialMD.
Your money. Your voice. Your wellness.
I was a third-year gastroenterology fellow when I realized that something had to change. I was on a one-way trip to burnout.
I went through medical school with the sole goal of becoming an excellent physician. Like many physicians, I was six figures deep in student loan debt by the end of training. I remember clearly being told, “You are going to be physicians. Money won’t be a problem.” In fact, in 2021, money remains a taboo topic in medicine, and most of medical education remains void of the fundamentals of money management.
Although I was surrounded by some of the most brilliant minds in medicine, burnout was spreading like a wave. Physicians are becoming increasingly broken, burned out by a system through which we have vowed to care for our patients: For better or for worse. We are required to attend lectures about burnout, yet nothing about money or finances. We can all agree that talking about resilience and burnout during odd hours of the morning are ironic measures that by themselves have done nothing to help us through the crisis that exists.
I noticed that there seemed to be a difference between physicians who had their finances in order and those who didn’t. This eventually made sense as I became more aware of the data that now exists. Healthy financial practices can lead to financial independence, which may in turn decrease burnout-associated stressors.1 This is what we need.
My observation about the difference in satisfaction between physicians led me to decide to explore that path for myself. My hypothesis? Empowering myself financially is an anti-burnout tool that will improve my satisfaction, longevity in medicine, and my well-being. I traded my financial illiteracy for empowerment and I am now on a mission to help physicians become financially empowered. This is an important step toward preventing and recovering from burnout. The surprising part is that it is not difficult. You need to be committed. Our math literacy is already higher than needed. When we physicians are financially independent, we will have the ability to practice medicine in a way that is healthy. In a world where physician suicide, burnout, and dissatisfaction continue to rise, there is an urgent call to financial action. This is a critical key that will help us change the future of medicine.
In this article, I am going to share four myths that are preventing physicians from truly managing their finances.
1. I love medicine. I have no plans of leaving: I love gastroenterology. The ability to use our critical internal medicine skills as well as intervene procedurally is truly a privilege. As a gastroenterologist with a focus on inflammatory bowel diseases, I have the honor of walking patients through seasons of life and making decisions that truly impact their lives. It is an honor. I also believe that good money management allows physicians to become even better physicians. The platforms of medicine continue to change. According to Physician Advocacy Institute, about 70% of physicians report being employed.2 As physicians graduate from training, joining large hospitals, physician autonomy in the practice of medicine is affected. To ensure that we continue to practice medicine at the fullest extent of our oath, it is essential that our finances allow us the ability and capacity to fulfill that oath. Furthermore, the pandemic has shown that physician income is not pandemic-proof. Having a healthy emergency fund and diversifying our income sources is critical as we move forward.
2. I have a financial adviser or planner. They will figure it out for me: Financial advisers and planners are hired professionals with varied levels of training and expertise. A great financial adviser can be an important part of your team. A team that is led by you, the CEO, because no one will care about your finances as much as you do. Investing the time to learn the basics can pay dividends. When I started my financial education journey, I was completely illiterate. I knew I wanted to have money but didn’t know how. One of the first things in my financial competency journey was to hire a financial adviser. Unfortunately, as I learned more about money, I realized that my investments favored him more than they did me. Coincidentally, we had similar starting balances in a different self-management investment account. At the end of our time together, our self-managed funds fared better than his actively picked funds. As humans, we assume that actively picking investments and stocks would be better than passive investments. Based on experience and data, investing in boring, diverse funds such as index funds averagely do better than actively managed funds. Is it wrong then to hire an adviser? No, but you are still the CEO of you-incorporated. Choosing to completely delegate to someone else, avoiding the basic education that would allow you to better screen for effectiveness and competence, may in fact be negligence. After empowering themselves financially, some physicians who have gone through my money curriculum have chosen to keep their advisers; others chose to self-manage. The key is giving yourself the gift of choice: Choosing to have an adviser because you want to rather than because you thought you had no choice.
3. Money management looks complicated. This is one of the most common statements I get for why physicians avoid their own money management. I remember the complex biochemical pathways we learned in medical school. Those were hard and complicated. We chose to stay the course because we believed that, with repetition and simplifying, it would eventually become less difficult. Why then is it any different with money? A physician shared a discussion she once had with a banker. She was told, “Doctors are bad with money.” When did we become the stereotype for being bad with money? If we can learn channelopathies and memorize mechanisms and save lives, we can do money. We have to start somewhere. We may not get it the first time. However, as physicians, we are the more persistent people and are excellent examples of what happens when you commit to learning something new. After coaching hundreds of physicians regarding money management, I have concluded that physicians are not bad with money. We simply may not be committed to learning it. Once we commit, the rest becomes history.
4. I don’t have time. For practicing gastroenterologists dealing with post-lockdown influx of patients, the days can be long. As a gastroenterologist who is also a parent, I know firsthand how time can be tight. When we had two children, we were busy. We thought we were at our capacity on time with two children. Then we had a third. Suddenly, life with two children looked easier than with three. As humans, we have the capacity to create. Things take exactly how much time we commit to them. If I give myself a month to write an article, I will write it in a month. If I give myself 2 weeks, I will be done in 2 weeks. The key is to remember that we all have 24 hours. David Frankel is the author of “The Freedom Formula: How to Succeed in Business Without Sacrificing Your Family, Health, or Life.”3 He analyzed a poll of business owners. He showed that they were wasting an average of 21.8 hours per week. Many times, we talk about our to-do list. We don’t talk enough about our “to don’t list.” This refers to the list of things we need to stop doing so that we can spend time on things that give or add value to our lives. Starting with as little as 30 minutes per day or per week dedicated to learning and/or managing our finances, the result will compound.
As the platform of medicine continues to evolve, it is important for astute gastroenterologists to be part of these conversations. When we are confident in our finances, they become a vehicle that gives strength to the power of our voice. We are less likely to overwork and more likely to find joy and meaning within and outside medicine.
If we want to care for our patients at a high level and keep our oath to do no harm, we have to remember that includes doing no harm to self as well.
Money management tools and empowering ourselves financially should be an essential component of our training; until then, the onus is on you to learn, so that you can be well.
Your voice matters. Your wellness matters. Your time matters. Your money matters.
Dr. Alli-Akintade is a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center. She is the CEO of MoneyFitMD, a financial empowerment coaching platform for female physicians. She is also the host of The MoneyFitMD podcast.
References
1. Royce TJ et al. Pract Radiat Oncol. Jul-Aug 2019;9(4):231-8.
2. Physician Advocacy Institute. “COVID-19’s Impact on Acquisitions of Physician Practices and Physician Employment 2019-2020.” 2021 Jun.
3. Finkel D. “New Study Shows You’re Wasting 21.8 hours a Week.” Inc.com. 2018 Mar 1.
I was a third-year gastroenterology fellow when I realized that something had to change. I was on a one-way trip to burnout.
I went through medical school with the sole goal of becoming an excellent physician. Like many physicians, I was six figures deep in student loan debt by the end of training. I remember clearly being told, “You are going to be physicians. Money won’t be a problem.” In fact, in 2021, money remains a taboo topic in medicine, and most of medical education remains void of the fundamentals of money management.
Although I was surrounded by some of the most brilliant minds in medicine, burnout was spreading like a wave. Physicians are becoming increasingly broken, burned out by a system through which we have vowed to care for our patients: For better or for worse. We are required to attend lectures about burnout, yet nothing about money or finances. We can all agree that talking about resilience and burnout during odd hours of the morning are ironic measures that by themselves have done nothing to help us through the crisis that exists.
I noticed that there seemed to be a difference between physicians who had their finances in order and those who didn’t. This eventually made sense as I became more aware of the data that now exists. Healthy financial practices can lead to financial independence, which may in turn decrease burnout-associated stressors.1 This is what we need.
My observation about the difference in satisfaction between physicians led me to decide to explore that path for myself. My hypothesis? Empowering myself financially is an anti-burnout tool that will improve my satisfaction, longevity in medicine, and my well-being. I traded my financial illiteracy for empowerment and I am now on a mission to help physicians become financially empowered. This is an important step toward preventing and recovering from burnout. The surprising part is that it is not difficult. You need to be committed. Our math literacy is already higher than needed. When we physicians are financially independent, we will have the ability to practice medicine in a way that is healthy. In a world where physician suicide, burnout, and dissatisfaction continue to rise, there is an urgent call to financial action. This is a critical key that will help us change the future of medicine.
In this article, I am going to share four myths that are preventing physicians from truly managing their finances.
1. I love medicine. I have no plans of leaving: I love gastroenterology. The ability to use our critical internal medicine skills as well as intervene procedurally is truly a privilege. As a gastroenterologist with a focus on inflammatory bowel diseases, I have the honor of walking patients through seasons of life and making decisions that truly impact their lives. It is an honor. I also believe that good money management allows physicians to become even better physicians. The platforms of medicine continue to change. According to Physician Advocacy Institute, about 70% of physicians report being employed.2 As physicians graduate from training, joining large hospitals, physician autonomy in the practice of medicine is affected. To ensure that we continue to practice medicine at the fullest extent of our oath, it is essential that our finances allow us the ability and capacity to fulfill that oath. Furthermore, the pandemic has shown that physician income is not pandemic-proof. Having a healthy emergency fund and diversifying our income sources is critical as we move forward.
2. I have a financial adviser or planner. They will figure it out for me: Financial advisers and planners are hired professionals with varied levels of training and expertise. A great financial adviser can be an important part of your team. A team that is led by you, the CEO, because no one will care about your finances as much as you do. Investing the time to learn the basics can pay dividends. When I started my financial education journey, I was completely illiterate. I knew I wanted to have money but didn’t know how. One of the first things in my financial competency journey was to hire a financial adviser. Unfortunately, as I learned more about money, I realized that my investments favored him more than they did me. Coincidentally, we had similar starting balances in a different self-management investment account. At the end of our time together, our self-managed funds fared better than his actively picked funds. As humans, we assume that actively picking investments and stocks would be better than passive investments. Based on experience and data, investing in boring, diverse funds such as index funds averagely do better than actively managed funds. Is it wrong then to hire an adviser? No, but you are still the CEO of you-incorporated. Choosing to completely delegate to someone else, avoiding the basic education that would allow you to better screen for effectiveness and competence, may in fact be negligence. After empowering themselves financially, some physicians who have gone through my money curriculum have chosen to keep their advisers; others chose to self-manage. The key is giving yourself the gift of choice: Choosing to have an adviser because you want to rather than because you thought you had no choice.
3. Money management looks complicated. This is one of the most common statements I get for why physicians avoid their own money management. I remember the complex biochemical pathways we learned in medical school. Those were hard and complicated. We chose to stay the course because we believed that, with repetition and simplifying, it would eventually become less difficult. Why then is it any different with money? A physician shared a discussion she once had with a banker. She was told, “Doctors are bad with money.” When did we become the stereotype for being bad with money? If we can learn channelopathies and memorize mechanisms and save lives, we can do money. We have to start somewhere. We may not get it the first time. However, as physicians, we are the more persistent people and are excellent examples of what happens when you commit to learning something new. After coaching hundreds of physicians regarding money management, I have concluded that physicians are not bad with money. We simply may not be committed to learning it. Once we commit, the rest becomes history.
4. I don’t have time. For practicing gastroenterologists dealing with post-lockdown influx of patients, the days can be long. As a gastroenterologist who is also a parent, I know firsthand how time can be tight. When we had two children, we were busy. We thought we were at our capacity on time with two children. Then we had a third. Suddenly, life with two children looked easier than with three. As humans, we have the capacity to create. Things take exactly how much time we commit to them. If I give myself a month to write an article, I will write it in a month. If I give myself 2 weeks, I will be done in 2 weeks. The key is to remember that we all have 24 hours. David Frankel is the author of “The Freedom Formula: How to Succeed in Business Without Sacrificing Your Family, Health, or Life.”3 He analyzed a poll of business owners. He showed that they were wasting an average of 21.8 hours per week. Many times, we talk about our to-do list. We don’t talk enough about our “to don’t list.” This refers to the list of things we need to stop doing so that we can spend time on things that give or add value to our lives. Starting with as little as 30 minutes per day or per week dedicated to learning and/or managing our finances, the result will compound.
As the platform of medicine continues to evolve, it is important for astute gastroenterologists to be part of these conversations. When we are confident in our finances, they become a vehicle that gives strength to the power of our voice. We are less likely to overwork and more likely to find joy and meaning within and outside medicine.
If we want to care for our patients at a high level and keep our oath to do no harm, we have to remember that includes doing no harm to self as well.
Money management tools and empowering ourselves financially should be an essential component of our training; until then, the onus is on you to learn, so that you can be well.
Your voice matters. Your wellness matters. Your time matters. Your money matters.
Dr. Alli-Akintade is a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center. She is the CEO of MoneyFitMD, a financial empowerment coaching platform for female physicians. She is also the host of The MoneyFitMD podcast.
References
1. Royce TJ et al. Pract Radiat Oncol. Jul-Aug 2019;9(4):231-8.
2. Physician Advocacy Institute. “COVID-19’s Impact on Acquisitions of Physician Practices and Physician Employment 2019-2020.” 2021 Jun.
3. Finkel D. “New Study Shows You’re Wasting 21.8 hours a Week.” Inc.com. 2018 Mar 1.
I was a third-year gastroenterology fellow when I realized that something had to change. I was on a one-way trip to burnout.
I went through medical school with the sole goal of becoming an excellent physician. Like many physicians, I was six figures deep in student loan debt by the end of training. I remember clearly being told, “You are going to be physicians. Money won’t be a problem.” In fact, in 2021, money remains a taboo topic in medicine, and most of medical education remains void of the fundamentals of money management.
Although I was surrounded by some of the most brilliant minds in medicine, burnout was spreading like a wave. Physicians are becoming increasingly broken, burned out by a system through which we have vowed to care for our patients: For better or for worse. We are required to attend lectures about burnout, yet nothing about money or finances. We can all agree that talking about resilience and burnout during odd hours of the morning are ironic measures that by themselves have done nothing to help us through the crisis that exists.
I noticed that there seemed to be a difference between physicians who had their finances in order and those who didn’t. This eventually made sense as I became more aware of the data that now exists. Healthy financial practices can lead to financial independence, which may in turn decrease burnout-associated stressors.1 This is what we need.
My observation about the difference in satisfaction between physicians led me to decide to explore that path for myself. My hypothesis? Empowering myself financially is an anti-burnout tool that will improve my satisfaction, longevity in medicine, and my well-being. I traded my financial illiteracy for empowerment and I am now on a mission to help physicians become financially empowered. This is an important step toward preventing and recovering from burnout. The surprising part is that it is not difficult. You need to be committed. Our math literacy is already higher than needed. When we physicians are financially independent, we will have the ability to practice medicine in a way that is healthy. In a world where physician suicide, burnout, and dissatisfaction continue to rise, there is an urgent call to financial action. This is a critical key that will help us change the future of medicine.
In this article, I am going to share four myths that are preventing physicians from truly managing their finances.
1. I love medicine. I have no plans of leaving: I love gastroenterology. The ability to use our critical internal medicine skills as well as intervene procedurally is truly a privilege. As a gastroenterologist with a focus on inflammatory bowel diseases, I have the honor of walking patients through seasons of life and making decisions that truly impact their lives. It is an honor. I also believe that good money management allows physicians to become even better physicians. The platforms of medicine continue to change. According to Physician Advocacy Institute, about 70% of physicians report being employed.2 As physicians graduate from training, joining large hospitals, physician autonomy in the practice of medicine is affected. To ensure that we continue to practice medicine at the fullest extent of our oath, it is essential that our finances allow us the ability and capacity to fulfill that oath. Furthermore, the pandemic has shown that physician income is not pandemic-proof. Having a healthy emergency fund and diversifying our income sources is critical as we move forward.
2. I have a financial adviser or planner. They will figure it out for me: Financial advisers and planners are hired professionals with varied levels of training and expertise. A great financial adviser can be an important part of your team. A team that is led by you, the CEO, because no one will care about your finances as much as you do. Investing the time to learn the basics can pay dividends. When I started my financial education journey, I was completely illiterate. I knew I wanted to have money but didn’t know how. One of the first things in my financial competency journey was to hire a financial adviser. Unfortunately, as I learned more about money, I realized that my investments favored him more than they did me. Coincidentally, we had similar starting balances in a different self-management investment account. At the end of our time together, our self-managed funds fared better than his actively picked funds. As humans, we assume that actively picking investments and stocks would be better than passive investments. Based on experience and data, investing in boring, diverse funds such as index funds averagely do better than actively managed funds. Is it wrong then to hire an adviser? No, but you are still the CEO of you-incorporated. Choosing to completely delegate to someone else, avoiding the basic education that would allow you to better screen for effectiveness and competence, may in fact be negligence. After empowering themselves financially, some physicians who have gone through my money curriculum have chosen to keep their advisers; others chose to self-manage. The key is giving yourself the gift of choice: Choosing to have an adviser because you want to rather than because you thought you had no choice.
3. Money management looks complicated. This is one of the most common statements I get for why physicians avoid their own money management. I remember the complex biochemical pathways we learned in medical school. Those were hard and complicated. We chose to stay the course because we believed that, with repetition and simplifying, it would eventually become less difficult. Why then is it any different with money? A physician shared a discussion she once had with a banker. She was told, “Doctors are bad with money.” When did we become the stereotype for being bad with money? If we can learn channelopathies and memorize mechanisms and save lives, we can do money. We have to start somewhere. We may not get it the first time. However, as physicians, we are the more persistent people and are excellent examples of what happens when you commit to learning something new. After coaching hundreds of physicians regarding money management, I have concluded that physicians are not bad with money. We simply may not be committed to learning it. Once we commit, the rest becomes history.
4. I don’t have time. For practicing gastroenterologists dealing with post-lockdown influx of patients, the days can be long. As a gastroenterologist who is also a parent, I know firsthand how time can be tight. When we had two children, we were busy. We thought we were at our capacity on time with two children. Then we had a third. Suddenly, life with two children looked easier than with three. As humans, we have the capacity to create. Things take exactly how much time we commit to them. If I give myself a month to write an article, I will write it in a month. If I give myself 2 weeks, I will be done in 2 weeks. The key is to remember that we all have 24 hours. David Frankel is the author of “The Freedom Formula: How to Succeed in Business Without Sacrificing Your Family, Health, or Life.”3 He analyzed a poll of business owners. He showed that they were wasting an average of 21.8 hours per week. Many times, we talk about our to-do list. We don’t talk enough about our “to don’t list.” This refers to the list of things we need to stop doing so that we can spend time on things that give or add value to our lives. Starting with as little as 30 minutes per day or per week dedicated to learning and/or managing our finances, the result will compound.
As the platform of medicine continues to evolve, it is important for astute gastroenterologists to be part of these conversations. When we are confident in our finances, they become a vehicle that gives strength to the power of our voice. We are less likely to overwork and more likely to find joy and meaning within and outside medicine.
If we want to care for our patients at a high level and keep our oath to do no harm, we have to remember that includes doing no harm to self as well.
Money management tools and empowering ourselves financially should be an essential component of our training; until then, the onus is on you to learn, so that you can be well.
Your voice matters. Your wellness matters. Your time matters. Your money matters.
Dr. Alli-Akintade is a gastroenterologist with Kaiser Permanente South Sacramento (Calif.) Medical Center. She is the CEO of MoneyFitMD, a financial empowerment coaching platform for female physicians. She is also the host of The MoneyFitMD podcast.
References
1. Royce TJ et al. Pract Radiat Oncol. Jul-Aug 2019;9(4):231-8.
2. Physician Advocacy Institute. “COVID-19’s Impact on Acquisitions of Physician Practices and Physician Employment 2019-2020.” 2021 Jun.
3. Finkel D. “New Study Shows You’re Wasting 21.8 hours a Week.” Inc.com. 2018 Mar 1.
Open notes: Legal issues
In July, I had my annual physical with my primary care physician, whose practice is based out of a large urban academic medical center. As she concluded my visit and directed me to the lab to have my blood work done, she said, “You’ll be receiving an automatic notice from MyChart by 9 am tomorrow that your medical records from today’s visit are available. I apologize if I have not yet had the opportunity to review them and enter my note, but you’ll get access to all of that, as well, as soon as it is in the system.”
This sort of interaction is increasingly common across the United States as health care institutions implement policies and procedures to comply with new regulations promulgated by the Office of the National Coordinator for Health Information Technology (ONC), which went into effect on April 5, 2021. These rules were promulgated in accordance with the 21st Century Cures Act of 2016 (Cures Act).1 The regulations, known as the Interoperability, Information Blocking, and the ONC Health IT Certification Program, implement provisions of the Cures Act intended to “support the access, exchange, and use of electronic health information.” The rule is considered a significant step in the “open notes” movement, which is intended to make health care more transparent by enabling patients to access their medical records. The drafters of the ONC regulations have carved out certain exceptions to the information blocking rule. For example, one exception allows some patient information to be withheld where making that information available might cause physical harm to the patient or another person.
Thus far, few patients have been informed about the new regulation.2 By forbidding “information blocking,” the rule enables patients to more easily access and control their health information. Records must be provided “without delay,” or at least as soon as the physician’s office receives an electronic copy. In 2022, it will be required that access to even more of a patient’s personal electronic health record be provided in real-time through a patient portal and that electronic health information be shareable across third-party apps.
The Cures Act and the regulations governing its implementation highlight the inherent tension between two core principles of bioethical inquiry: autonomy and beneficence. The first principle, autonomy, champions allowing patient access and control over their own personal information. Beneficence, which is often expressed as paternalism, ensures that the experts are able to analyze and interpret data so that patients are in the best position to then make informed decisions.
With these principles in mind, arguments against open notes have generally fallen into three related categories. First, critics worry that immediate access to one’s medical record will increase patient anxiety caused by feelings of being inundated with complex medical information that patients may be ill-equipped to analyze and understand. This is a common refrain any time policies are implemented to improve medical information sharing. For example, critics of direct-to-consumer genetic testing caution that permitting unfettered access to complex information, particularly without an intermediary to interpret the data, could lead to confusion and poor medical choices.
There may be validity to this claim. One study found that 3% of patients reported feeling very confused when granted access to their medical notes.3 Another study concluded that direct release of medical test results “sometimes leads to unnecessary anxiety.”4 While the drafters of the ONC regulations have carved out certain exceptions to the information blocking rule, those exceptions do not allow for withholding of information because of concerns about patient anxiety or psychological harms.
The second common critique of open notes is that requiring release of all clinical notes will lead to clinician self-censorship, effectively muzzling or silencing the experts whose responsibility it is to objectively interpret results in order to provide the best care for their patients. Some have expressed concern that clinicians will be forced to “code” their records to avoid addressing “sensitive” subjects that might make patients feel offended or judged. This, in turn, might lead to less complete, reliable, or useful clinician communication.3
In fact, open notes has led to changes in the documentation process for some clinicians. They have reported modifying the way they document patient visits by changing their use of critical language and sensitive information.5 One study found that open notes led physicians to adjust “their language to avoid being perceived as critical of patients; omitting certain terms, such as ‘noncompliant’ and ‘patient denies’; and modifying how they document sensitive information.”3
In response, experts recommend focusing on precise and empathetic patient notes; in other words, the clinician should not write something in the note that they would not say directly to the patient. For example, they recommend that clinicians use precise language (for example, identifying the patient’s BMI) rather than using terms that could be offensive (for example, labeling the patient as “obese”).6 The shift to more empathetic note-taking could be seen less as a burden and more as a valuable tool in the shared decision-making endeavor: It could allow physicians to document both their clinical judgments and the patient’s values and preferences, which could lead to better medical decision-making.
Third, critics of open notes point to concerns about the burden it places on clinicians’ already limited time. The ONC rule requires automatic release of test results regardless of whether the clinician has had the opportunity to review them and offer their interpretation and insight. Because physician interpretation of results has known benefits,4 this puts additional pressure on clinicians to review results and enter notes in a timely manner. But physicians have reported that often open notes necessitates that they spend more time on documentation than they would otherwise.5
Despite critiques of open notes, the benefits of allowing patients access to their medical records have been repeatedly demonstrated. And research has shown that patients benefit from accessing open notes by allowing them to access and control their own personal medical information.5 Patients report that they understand and value the information provided to them in their medical records,7 and they feel empowered to participate in their medical decision-making. In surveys, patients report that reading their doctors’ notes is useful for taking care of their health and for remembering their care plans, understanding why a medication was prescribed, and reinforcing the need to take their medications and adhere to treatment plans.8
Importantly, open notes can increase patient engagement and patients’ trust in their physicians,9 thereby improving the doctor-patient relationship.3 And allowing patients to share their medical records with care partners enables supported decision-making, particularly for older and chronically ill individuals.3 Additionally, it is predicted that open notes may, in fact, decrease legal liability.9 By improving both trust in the doctor-patient relationship and safety, some experts expect that legal claims against clinicians will, in turn, decrease.10
The modern practice of medicine necessitates a more empathetic approach to clinical note-taking, even in the absence of regulation requiring it. As the regulations implementing the Cures Act roll out, patients will have easier, and more immediate, access to their medical records. Despite earlier hesitancy, clinicians are steadily beginning to support sharing access to notes with patients.5 Change can be hard. But the change expected of clinicians because of these new regulations appears to be less onerous than originally anticipated.
Prof. Koch is codirector of Health Law & Policy Institute and assistant professor at the University of Houston Law Center, as well as director of law and ethics at the MacLean Center for Clinical Medical Ethics at the University of Chicago. She has no disclosures.
This article was updated Sept. 9, 2021.
References
1. Fed Regist. 2020 May;85(85):25642-961.
2. The Petrie-Flom Center Staff. “New Rule Puts Medical Data in Patients’ Hands.” Bill of Health. July 12, 2021. Accessed August 30, 2021. https://blog.petrieflom.law.harvard.edu/2021/07/12/new-rule-puts-medical-data-in-patients-hands/.
3. Blease C et al. Ann Intern Med. 2021 Jan;174(1):101-2.
4. Pillemer F et al. PLoS One. 2016 Jun. doi: 10.1371/journal.pone.0154743.
5. DesRoches CM et al. JAMA Netw Open. 2020 Mar. doi: 10.1001/jamanetworkopen.2020.1753.
6. Heath S. “Most Patients Understand Clinical Notes, Patient Data Access.” Patient Engagement HIT. July 29, 2020. Accessed August 30, 2021. https://patientengagementhit.com/news/most-patients-understand-clinical-notes-patient-data-access
7. Leveille SG et al. J Gen Intern Med. 2020 Dec;35(12):3510-6.
8. Walker J et al. J Med Internet Res. 2019 May. doi: 10.2196/13876.
9. Bell SK et al. BMJ Qual Saf. 2017 Apr;26(4):262-70.
10. Kachalia A, Mello MM. N Engl J Med. 2011 Apr;364(16):1564-72.
In July, I had my annual physical with my primary care physician, whose practice is based out of a large urban academic medical center. As she concluded my visit and directed me to the lab to have my blood work done, she said, “You’ll be receiving an automatic notice from MyChart by 9 am tomorrow that your medical records from today’s visit are available. I apologize if I have not yet had the opportunity to review them and enter my note, but you’ll get access to all of that, as well, as soon as it is in the system.”
This sort of interaction is increasingly common across the United States as health care institutions implement policies and procedures to comply with new regulations promulgated by the Office of the National Coordinator for Health Information Technology (ONC), which went into effect on April 5, 2021. These rules were promulgated in accordance with the 21st Century Cures Act of 2016 (Cures Act).1 The regulations, known as the Interoperability, Information Blocking, and the ONC Health IT Certification Program, implement provisions of the Cures Act intended to “support the access, exchange, and use of electronic health information.” The rule is considered a significant step in the “open notes” movement, which is intended to make health care more transparent by enabling patients to access their medical records. The drafters of the ONC regulations have carved out certain exceptions to the information blocking rule. For example, one exception allows some patient information to be withheld where making that information available might cause physical harm to the patient or another person.
Thus far, few patients have been informed about the new regulation.2 By forbidding “information blocking,” the rule enables patients to more easily access and control their health information. Records must be provided “without delay,” or at least as soon as the physician’s office receives an electronic copy. In 2022, it will be required that access to even more of a patient’s personal electronic health record be provided in real-time through a patient portal and that electronic health information be shareable across third-party apps.
The Cures Act and the regulations governing its implementation highlight the inherent tension between two core principles of bioethical inquiry: autonomy and beneficence. The first principle, autonomy, champions allowing patient access and control over their own personal information. Beneficence, which is often expressed as paternalism, ensures that the experts are able to analyze and interpret data so that patients are in the best position to then make informed decisions.
With these principles in mind, arguments against open notes have generally fallen into three related categories. First, critics worry that immediate access to one’s medical record will increase patient anxiety caused by feelings of being inundated with complex medical information that patients may be ill-equipped to analyze and understand. This is a common refrain any time policies are implemented to improve medical information sharing. For example, critics of direct-to-consumer genetic testing caution that permitting unfettered access to complex information, particularly without an intermediary to interpret the data, could lead to confusion and poor medical choices.
There may be validity to this claim. One study found that 3% of patients reported feeling very confused when granted access to their medical notes.3 Another study concluded that direct release of medical test results “sometimes leads to unnecessary anxiety.”4 While the drafters of the ONC regulations have carved out certain exceptions to the information blocking rule, those exceptions do not allow for withholding of information because of concerns about patient anxiety or psychological harms.
The second common critique of open notes is that requiring release of all clinical notes will lead to clinician self-censorship, effectively muzzling or silencing the experts whose responsibility it is to objectively interpret results in order to provide the best care for their patients. Some have expressed concern that clinicians will be forced to “code” their records to avoid addressing “sensitive” subjects that might make patients feel offended or judged. This, in turn, might lead to less complete, reliable, or useful clinician communication.3
In fact, open notes has led to changes in the documentation process for some clinicians. They have reported modifying the way they document patient visits by changing their use of critical language and sensitive information.5 One study found that open notes led physicians to adjust “their language to avoid being perceived as critical of patients; omitting certain terms, such as ‘noncompliant’ and ‘patient denies’; and modifying how they document sensitive information.”3
In response, experts recommend focusing on precise and empathetic patient notes; in other words, the clinician should not write something in the note that they would not say directly to the patient. For example, they recommend that clinicians use precise language (for example, identifying the patient’s BMI) rather than using terms that could be offensive (for example, labeling the patient as “obese”).6 The shift to more empathetic note-taking could be seen less as a burden and more as a valuable tool in the shared decision-making endeavor: It could allow physicians to document both their clinical judgments and the patient’s values and preferences, which could lead to better medical decision-making.
Third, critics of open notes point to concerns about the burden it places on clinicians’ already limited time. The ONC rule requires automatic release of test results regardless of whether the clinician has had the opportunity to review them and offer their interpretation and insight. Because physician interpretation of results has known benefits,4 this puts additional pressure on clinicians to review results and enter notes in a timely manner. But physicians have reported that often open notes necessitates that they spend more time on documentation than they would otherwise.5
Despite critiques of open notes, the benefits of allowing patients access to their medical records have been repeatedly demonstrated. And research has shown that patients benefit from accessing open notes by allowing them to access and control their own personal medical information.5 Patients report that they understand and value the information provided to them in their medical records,7 and they feel empowered to participate in their medical decision-making. In surveys, patients report that reading their doctors’ notes is useful for taking care of their health and for remembering their care plans, understanding why a medication was prescribed, and reinforcing the need to take their medications and adhere to treatment plans.8
Importantly, open notes can increase patient engagement and patients’ trust in their physicians,9 thereby improving the doctor-patient relationship.3 And allowing patients to share their medical records with care partners enables supported decision-making, particularly for older and chronically ill individuals.3 Additionally, it is predicted that open notes may, in fact, decrease legal liability.9 By improving both trust in the doctor-patient relationship and safety, some experts expect that legal claims against clinicians will, in turn, decrease.10
The modern practice of medicine necessitates a more empathetic approach to clinical note-taking, even in the absence of regulation requiring it. As the regulations implementing the Cures Act roll out, patients will have easier, and more immediate, access to their medical records. Despite earlier hesitancy, clinicians are steadily beginning to support sharing access to notes with patients.5 Change can be hard. But the change expected of clinicians because of these new regulations appears to be less onerous than originally anticipated.
Prof. Koch is codirector of Health Law & Policy Institute and assistant professor at the University of Houston Law Center, as well as director of law and ethics at the MacLean Center for Clinical Medical Ethics at the University of Chicago. She has no disclosures.
This article was updated Sept. 9, 2021.
References
1. Fed Regist. 2020 May;85(85):25642-961.
2. The Petrie-Flom Center Staff. “New Rule Puts Medical Data in Patients’ Hands.” Bill of Health. July 12, 2021. Accessed August 30, 2021. https://blog.petrieflom.law.harvard.edu/2021/07/12/new-rule-puts-medical-data-in-patients-hands/.
3. Blease C et al. Ann Intern Med. 2021 Jan;174(1):101-2.
4. Pillemer F et al. PLoS One. 2016 Jun. doi: 10.1371/journal.pone.0154743.
5. DesRoches CM et al. JAMA Netw Open. 2020 Mar. doi: 10.1001/jamanetworkopen.2020.1753.
6. Heath S. “Most Patients Understand Clinical Notes, Patient Data Access.” Patient Engagement HIT. July 29, 2020. Accessed August 30, 2021. https://patientengagementhit.com/news/most-patients-understand-clinical-notes-patient-data-access
7. Leveille SG et al. J Gen Intern Med. 2020 Dec;35(12):3510-6.
8. Walker J et al. J Med Internet Res. 2019 May. doi: 10.2196/13876.
9. Bell SK et al. BMJ Qual Saf. 2017 Apr;26(4):262-70.
10. Kachalia A, Mello MM. N Engl J Med. 2011 Apr;364(16):1564-72.
In July, I had my annual physical with my primary care physician, whose practice is based out of a large urban academic medical center. As she concluded my visit and directed me to the lab to have my blood work done, she said, “You’ll be receiving an automatic notice from MyChart by 9 am tomorrow that your medical records from today’s visit are available. I apologize if I have not yet had the opportunity to review them and enter my note, but you’ll get access to all of that, as well, as soon as it is in the system.”
This sort of interaction is increasingly common across the United States as health care institutions implement policies and procedures to comply with new regulations promulgated by the Office of the National Coordinator for Health Information Technology (ONC), which went into effect on April 5, 2021. These rules were promulgated in accordance with the 21st Century Cures Act of 2016 (Cures Act).1 The regulations, known as the Interoperability, Information Blocking, and the ONC Health IT Certification Program, implement provisions of the Cures Act intended to “support the access, exchange, and use of electronic health information.” The rule is considered a significant step in the “open notes” movement, which is intended to make health care more transparent by enabling patients to access their medical records. The drafters of the ONC regulations have carved out certain exceptions to the information blocking rule. For example, one exception allows some patient information to be withheld where making that information available might cause physical harm to the patient or another person.
Thus far, few patients have been informed about the new regulation.2 By forbidding “information blocking,” the rule enables patients to more easily access and control their health information. Records must be provided “without delay,” or at least as soon as the physician’s office receives an electronic copy. In 2022, it will be required that access to even more of a patient’s personal electronic health record be provided in real-time through a patient portal and that electronic health information be shareable across third-party apps.
The Cures Act and the regulations governing its implementation highlight the inherent tension between two core principles of bioethical inquiry: autonomy and beneficence. The first principle, autonomy, champions allowing patient access and control over their own personal information. Beneficence, which is often expressed as paternalism, ensures that the experts are able to analyze and interpret data so that patients are in the best position to then make informed decisions.
With these principles in mind, arguments against open notes have generally fallen into three related categories. First, critics worry that immediate access to one’s medical record will increase patient anxiety caused by feelings of being inundated with complex medical information that patients may be ill-equipped to analyze and understand. This is a common refrain any time policies are implemented to improve medical information sharing. For example, critics of direct-to-consumer genetic testing caution that permitting unfettered access to complex information, particularly without an intermediary to interpret the data, could lead to confusion and poor medical choices.
There may be validity to this claim. One study found that 3% of patients reported feeling very confused when granted access to their medical notes.3 Another study concluded that direct release of medical test results “sometimes leads to unnecessary anxiety.”4 While the drafters of the ONC regulations have carved out certain exceptions to the information blocking rule, those exceptions do not allow for withholding of information because of concerns about patient anxiety or psychological harms.
The second common critique of open notes is that requiring release of all clinical notes will lead to clinician self-censorship, effectively muzzling or silencing the experts whose responsibility it is to objectively interpret results in order to provide the best care for their patients. Some have expressed concern that clinicians will be forced to “code” their records to avoid addressing “sensitive” subjects that might make patients feel offended or judged. This, in turn, might lead to less complete, reliable, or useful clinician communication.3
In fact, open notes has led to changes in the documentation process for some clinicians. They have reported modifying the way they document patient visits by changing their use of critical language and sensitive information.5 One study found that open notes led physicians to adjust “their language to avoid being perceived as critical of patients; omitting certain terms, such as ‘noncompliant’ and ‘patient denies’; and modifying how they document sensitive information.”3
In response, experts recommend focusing on precise and empathetic patient notes; in other words, the clinician should not write something in the note that they would not say directly to the patient. For example, they recommend that clinicians use precise language (for example, identifying the patient’s BMI) rather than using terms that could be offensive (for example, labeling the patient as “obese”).6 The shift to more empathetic note-taking could be seen less as a burden and more as a valuable tool in the shared decision-making endeavor: It could allow physicians to document both their clinical judgments and the patient’s values and preferences, which could lead to better medical decision-making.
Third, critics of open notes point to concerns about the burden it places on clinicians’ already limited time. The ONC rule requires automatic release of test results regardless of whether the clinician has had the opportunity to review them and offer their interpretation and insight. Because physician interpretation of results has known benefits,4 this puts additional pressure on clinicians to review results and enter notes in a timely manner. But physicians have reported that often open notes necessitates that they spend more time on documentation than they would otherwise.5
Despite critiques of open notes, the benefits of allowing patients access to their medical records have been repeatedly demonstrated. And research has shown that patients benefit from accessing open notes by allowing them to access and control their own personal medical information.5 Patients report that they understand and value the information provided to them in their medical records,7 and they feel empowered to participate in their medical decision-making. In surveys, patients report that reading their doctors’ notes is useful for taking care of their health and for remembering their care plans, understanding why a medication was prescribed, and reinforcing the need to take their medications and adhere to treatment plans.8
Importantly, open notes can increase patient engagement and patients’ trust in their physicians,9 thereby improving the doctor-patient relationship.3 And allowing patients to share their medical records with care partners enables supported decision-making, particularly for older and chronically ill individuals.3 Additionally, it is predicted that open notes may, in fact, decrease legal liability.9 By improving both trust in the doctor-patient relationship and safety, some experts expect that legal claims against clinicians will, in turn, decrease.10
The modern practice of medicine necessitates a more empathetic approach to clinical note-taking, even in the absence of regulation requiring it. As the regulations implementing the Cures Act roll out, patients will have easier, and more immediate, access to their medical records. Despite earlier hesitancy, clinicians are steadily beginning to support sharing access to notes with patients.5 Change can be hard. But the change expected of clinicians because of these new regulations appears to be less onerous than originally anticipated.
Prof. Koch is codirector of Health Law & Policy Institute and assistant professor at the University of Houston Law Center, as well as director of law and ethics at the MacLean Center for Clinical Medical Ethics at the University of Chicago. She has no disclosures.
This article was updated Sept. 9, 2021.
References
1. Fed Regist. 2020 May;85(85):25642-961.
2. The Petrie-Flom Center Staff. “New Rule Puts Medical Data in Patients’ Hands.” Bill of Health. July 12, 2021. Accessed August 30, 2021. https://blog.petrieflom.law.harvard.edu/2021/07/12/new-rule-puts-medical-data-in-patients-hands/.
3. Blease C et al. Ann Intern Med. 2021 Jan;174(1):101-2.
4. Pillemer F et al. PLoS One. 2016 Jun. doi: 10.1371/journal.pone.0154743.
5. DesRoches CM et al. JAMA Netw Open. 2020 Mar. doi: 10.1001/jamanetworkopen.2020.1753.
6. Heath S. “Most Patients Understand Clinical Notes, Patient Data Access.” Patient Engagement HIT. July 29, 2020. Accessed August 30, 2021. https://patientengagementhit.com/news/most-patients-understand-clinical-notes-patient-data-access
7. Leveille SG et al. J Gen Intern Med. 2020 Dec;35(12):3510-6.
8. Walker J et al. J Med Internet Res. 2019 May. doi: 10.2196/13876.
9. Bell SK et al. BMJ Qual Saf. 2017 Apr;26(4):262-70.
10. Kachalia A, Mello MM. N Engl J Med. 2011 Apr;364(16):1564-72.
The doctor house: What to know in 2021
The concept of home ownership has changed for this generation, not only in the logistics of the best way to do it, but also in the desire and demand for owning versus renting. According to the Penn Institute for Urban Research, the U.S. homeownership rate is now at 63.7%, the lowest in 48 years. “Homeownership rates have declined for all demographic age groups. Since 2006, the number of households who own their home in the United States has decreased by 674,000 while the number of renters has increased by over 8 million.”1
But isn’t owning your own home the American dream? Isn’t it a great investment? If we’re looking strictly at the monthly payment numbers, traditionally paying a mortgage is cheaper than paying rent for the same-size home. That became even more true as home prices dropped in 2007-2008 and as interest rates also dropped over the last several years. Then there’s the age-old concept of “building equity” or “throwing away money on rent.” As a financial planner, I get asked all the time about a home as an investment. It certainly can be, like any investment, if you buy and sell at the right time. But something is only an investment if it grows, and you can’t predict if you’re going to buy and sell your house at the right time. The median price of an existing home sold in March 2021 was $329,100. That’s a 17.2% increase from March 2020. Times are certainly crazy right now in the real estate market.
What many people don’t think about are the other costs, and not just financial costs. Today’s generation is more aware of the added stress and burden of maintaining a home and the money you can sink into it for maintenance, let alone remodeling. Then of course there’s the mortgage interest, property taxes, and insurance that you won’t have with a rental. Lastly, the biggest reason today’s generation is choosing to rent more and more is the flexibility. They want to be more mobile, able to get up and move without having to worry about listing, selling, and possibly owing more than the house is worth, and being stuck. We saw this with many residents that bought a home during residency and then tried to sell when they landed their first job, only to find out they owed more than it was worth because of the real estate market collapse of 2008. Approximately 50% of physicians will leave their first job within 1-3 years, so it’s a gamble that you’ll be able to sell your house when you want to for the price you need.
But what are the benefits of buying? First, there is the age-old argument of building equity. If you stay in your house long enough, and plan to sell it when you retire and downsize, it can definitely be an investment. If you keep a mortgage long enough, eventually you’ll pay it off, and have no payment. Mortgage interest is also tax-deductible. Lastly, there are the intangibles – like being able to put down roots, build a community, and have the ability to remodel and customize your home, a feature not usually available when renting.
Now that I’ve effectively talked you out and back in again, what’s the best way to go about buying a house in today’s crazy market? We’ve seen houses list and sell within a day and get multiple offers well over asking price. It’s a very difficult time to buy, but there are ways to make it easier. First, be clear on what you want in a house, especially location. There’s nothing worse than buyer’s remorse in your primary residence, and that happens more these days when people have to quickly make a decision. Find a good, fee-based financial planner to help you decide how much house fits in your budget and your long-term goals. You’d be surprised how easily we can talk ourselves into paying much more than we had originally decided. Use your financial planner to help avoid emotions getting involved and creeping up your price (especially when multiple offers are involved). A good rule of thumb is for a housing payment to be no more than 33% of your take-home income. This includes principal, interest, and taxes. Or, many planners will use the “2x income” rule of thumb. So if you make $300,000, don’t go over $600,000. Although with today’s low interest rates, there is some more wiggle room on that. Next, get a good referral from someone you trust in looking for a realtor. Real estate is a commission-based job and can have some potential conflicts of interest, so getting a recommendation can help. Or, there are realtors who will work for a flat fee, regardless of how much you pay for a house. That can help reduce the conflict.
You made the offer, you beat out the other bids, and you’re getting a house! How are you paying for it? Hopefully, you already got preapproved. This means finding a good, reputable mortgage professional. Get referrals, shop around, and take your time. Get multiple quotes before you start the underwriting process. They shouldn’t have to pull your credit to give you a fairly accurate estimate of what interest rate you’ll qualify for. Usually, they will give you fixed and variable interest quotes. I normally recommend fixed interest. Because interest rates are so low right now, they’re only going to go up in the future, and if you have a variable rate loan, your payment will go up as interest rates rise.
Is a physician loan a good idea? Depending on your circumstance, it can often be a good deal. Most new attendings don’t have cash saved up for a down payment, and these often don’t require one. And the other big benefit is that they won’t consider your student loan payments when calculating your debt-to-income ratio. Mortgage lenders will look at how much other debt you have when determining an approval. And a conventional mortgage will take your student loan payments into consideration, which means you’ll qualify for a much lower payment and purchase price. In my experience, you want a credit score of around 700 or higher to qualify for these types of loans. The only downside of a physician mortgage is the rates are slightly higher. I encourage you to start the application process early; they’re taking upward of 90 days lately.
As the mortgage is being processed, you’ll have an inspection and appraisal, and as long as those are all favorable, you’re in! Now, should you take any surplus income each month and pay extra on your mortgage to pay it down sooner, or invest it? Everyone’s situation is different, but a good rule of thumb is to look at interest rates on the debt you want to pay off versus expected rate of return on the potential investment. For example, if you have extra money, should you invest it in an SP500 index fund that historically gets 8%-12% per year, or put it on the principal of your mortgage that has an interest rate of 3%? Assuming no other factors or goals, and you just want the best bang for your buck, my money would go toward the investment getting 8%-12% over saving 3% on my mortgage.
Take your time, do your research, and find good professionals. There’s no right answer for everyone, but there are certainly some good practices when walking through the first home decision. Here at FinancialMD, we only work with physicians, and we’re happy to chat if you want some guidance on this. Send me an email and subscribe to our weekly Didactic Minute videos on YouTube for more financial tips for young physicians. Good luck!
Mr. Solitro is a financial planner and CEO of FinancialMD. He has no other conflicts of interest.
Investment advisory services offered through FinancialMD, a registered investment adviser. Registration as an investment adviser does not imply a certain level of skill or training. This article is provided for informational purposes only and nothing contained herein should be construed as a solicitation to buy or sell any products. Advisory services are offered only to clients and prospective clients in places where FinancialMD and its investment adviser representatives are registered or exempt from registration. Investing involves the risk of loss of principal. Past performance is no guarantee of future performance and no investment strategy can guarantee a profit or protect against loss.
This article was updated June 8, 2021.
Reference
1. Wachter S and Acolin A. Owning or Renting in the US: Shifting Dynamics of the Housing Market. Penn Institute for Urban Research. 2016 May.
The concept of home ownership has changed for this generation, not only in the logistics of the best way to do it, but also in the desire and demand for owning versus renting. According to the Penn Institute for Urban Research, the U.S. homeownership rate is now at 63.7%, the lowest in 48 years. “Homeownership rates have declined for all demographic age groups. Since 2006, the number of households who own their home in the United States has decreased by 674,000 while the number of renters has increased by over 8 million.”1
But isn’t owning your own home the American dream? Isn’t it a great investment? If we’re looking strictly at the monthly payment numbers, traditionally paying a mortgage is cheaper than paying rent for the same-size home. That became even more true as home prices dropped in 2007-2008 and as interest rates also dropped over the last several years. Then there’s the age-old concept of “building equity” or “throwing away money on rent.” As a financial planner, I get asked all the time about a home as an investment. It certainly can be, like any investment, if you buy and sell at the right time. But something is only an investment if it grows, and you can’t predict if you’re going to buy and sell your house at the right time. The median price of an existing home sold in March 2021 was $329,100. That’s a 17.2% increase from March 2020. Times are certainly crazy right now in the real estate market.
What many people don’t think about are the other costs, and not just financial costs. Today’s generation is more aware of the added stress and burden of maintaining a home and the money you can sink into it for maintenance, let alone remodeling. Then of course there’s the mortgage interest, property taxes, and insurance that you won’t have with a rental. Lastly, the biggest reason today’s generation is choosing to rent more and more is the flexibility. They want to be more mobile, able to get up and move without having to worry about listing, selling, and possibly owing more than the house is worth, and being stuck. We saw this with many residents that bought a home during residency and then tried to sell when they landed their first job, only to find out they owed more than it was worth because of the real estate market collapse of 2008. Approximately 50% of physicians will leave their first job within 1-3 years, so it’s a gamble that you’ll be able to sell your house when you want to for the price you need.
But what are the benefits of buying? First, there is the age-old argument of building equity. If you stay in your house long enough, and plan to sell it when you retire and downsize, it can definitely be an investment. If you keep a mortgage long enough, eventually you’ll pay it off, and have no payment. Mortgage interest is also tax-deductible. Lastly, there are the intangibles – like being able to put down roots, build a community, and have the ability to remodel and customize your home, a feature not usually available when renting.
Now that I’ve effectively talked you out and back in again, what’s the best way to go about buying a house in today’s crazy market? We’ve seen houses list and sell within a day and get multiple offers well over asking price. It’s a very difficult time to buy, but there are ways to make it easier. First, be clear on what you want in a house, especially location. There’s nothing worse than buyer’s remorse in your primary residence, and that happens more these days when people have to quickly make a decision. Find a good, fee-based financial planner to help you decide how much house fits in your budget and your long-term goals. You’d be surprised how easily we can talk ourselves into paying much more than we had originally decided. Use your financial planner to help avoid emotions getting involved and creeping up your price (especially when multiple offers are involved). A good rule of thumb is for a housing payment to be no more than 33% of your take-home income. This includes principal, interest, and taxes. Or, many planners will use the “2x income” rule of thumb. So if you make $300,000, don’t go over $600,000. Although with today’s low interest rates, there is some more wiggle room on that. Next, get a good referral from someone you trust in looking for a realtor. Real estate is a commission-based job and can have some potential conflicts of interest, so getting a recommendation can help. Or, there are realtors who will work for a flat fee, regardless of how much you pay for a house. That can help reduce the conflict.
You made the offer, you beat out the other bids, and you’re getting a house! How are you paying for it? Hopefully, you already got preapproved. This means finding a good, reputable mortgage professional. Get referrals, shop around, and take your time. Get multiple quotes before you start the underwriting process. They shouldn’t have to pull your credit to give you a fairly accurate estimate of what interest rate you’ll qualify for. Usually, they will give you fixed and variable interest quotes. I normally recommend fixed interest. Because interest rates are so low right now, they’re only going to go up in the future, and if you have a variable rate loan, your payment will go up as interest rates rise.
Is a physician loan a good idea? Depending on your circumstance, it can often be a good deal. Most new attendings don’t have cash saved up for a down payment, and these often don’t require one. And the other big benefit is that they won’t consider your student loan payments when calculating your debt-to-income ratio. Mortgage lenders will look at how much other debt you have when determining an approval. And a conventional mortgage will take your student loan payments into consideration, which means you’ll qualify for a much lower payment and purchase price. In my experience, you want a credit score of around 700 or higher to qualify for these types of loans. The only downside of a physician mortgage is the rates are slightly higher. I encourage you to start the application process early; they’re taking upward of 90 days lately.
As the mortgage is being processed, you’ll have an inspection and appraisal, and as long as those are all favorable, you’re in! Now, should you take any surplus income each month and pay extra on your mortgage to pay it down sooner, or invest it? Everyone’s situation is different, but a good rule of thumb is to look at interest rates on the debt you want to pay off versus expected rate of return on the potential investment. For example, if you have extra money, should you invest it in an SP500 index fund that historically gets 8%-12% per year, or put it on the principal of your mortgage that has an interest rate of 3%? Assuming no other factors or goals, and you just want the best bang for your buck, my money would go toward the investment getting 8%-12% over saving 3% on my mortgage.
Take your time, do your research, and find good professionals. There’s no right answer for everyone, but there are certainly some good practices when walking through the first home decision. Here at FinancialMD, we only work with physicians, and we’re happy to chat if you want some guidance on this. Send me an email and subscribe to our weekly Didactic Minute videos on YouTube for more financial tips for young physicians. Good luck!
Mr. Solitro is a financial planner and CEO of FinancialMD. He has no other conflicts of interest.
Investment advisory services offered through FinancialMD, a registered investment adviser. Registration as an investment adviser does not imply a certain level of skill or training. This article is provided for informational purposes only and nothing contained herein should be construed as a solicitation to buy or sell any products. Advisory services are offered only to clients and prospective clients in places where FinancialMD and its investment adviser representatives are registered or exempt from registration. Investing involves the risk of loss of principal. Past performance is no guarantee of future performance and no investment strategy can guarantee a profit or protect against loss.
This article was updated June 8, 2021.
Reference
1. Wachter S and Acolin A. Owning or Renting in the US: Shifting Dynamics of the Housing Market. Penn Institute for Urban Research. 2016 May.
The concept of home ownership has changed for this generation, not only in the logistics of the best way to do it, but also in the desire and demand for owning versus renting. According to the Penn Institute for Urban Research, the U.S. homeownership rate is now at 63.7%, the lowest in 48 years. “Homeownership rates have declined for all demographic age groups. Since 2006, the number of households who own their home in the United States has decreased by 674,000 while the number of renters has increased by over 8 million.”1
But isn’t owning your own home the American dream? Isn’t it a great investment? If we’re looking strictly at the monthly payment numbers, traditionally paying a mortgage is cheaper than paying rent for the same-size home. That became even more true as home prices dropped in 2007-2008 and as interest rates also dropped over the last several years. Then there’s the age-old concept of “building equity” or “throwing away money on rent.” As a financial planner, I get asked all the time about a home as an investment. It certainly can be, like any investment, if you buy and sell at the right time. But something is only an investment if it grows, and you can’t predict if you’re going to buy and sell your house at the right time. The median price of an existing home sold in March 2021 was $329,100. That’s a 17.2% increase from March 2020. Times are certainly crazy right now in the real estate market.
What many people don’t think about are the other costs, and not just financial costs. Today’s generation is more aware of the added stress and burden of maintaining a home and the money you can sink into it for maintenance, let alone remodeling. Then of course there’s the mortgage interest, property taxes, and insurance that you won’t have with a rental. Lastly, the biggest reason today’s generation is choosing to rent more and more is the flexibility. They want to be more mobile, able to get up and move without having to worry about listing, selling, and possibly owing more than the house is worth, and being stuck. We saw this with many residents that bought a home during residency and then tried to sell when they landed their first job, only to find out they owed more than it was worth because of the real estate market collapse of 2008. Approximately 50% of physicians will leave their first job within 1-3 years, so it’s a gamble that you’ll be able to sell your house when you want to for the price you need.
But what are the benefits of buying? First, there is the age-old argument of building equity. If you stay in your house long enough, and plan to sell it when you retire and downsize, it can definitely be an investment. If you keep a mortgage long enough, eventually you’ll pay it off, and have no payment. Mortgage interest is also tax-deductible. Lastly, there are the intangibles – like being able to put down roots, build a community, and have the ability to remodel and customize your home, a feature not usually available when renting.
Now that I’ve effectively talked you out and back in again, what’s the best way to go about buying a house in today’s crazy market? We’ve seen houses list and sell within a day and get multiple offers well over asking price. It’s a very difficult time to buy, but there are ways to make it easier. First, be clear on what you want in a house, especially location. There’s nothing worse than buyer’s remorse in your primary residence, and that happens more these days when people have to quickly make a decision. Find a good, fee-based financial planner to help you decide how much house fits in your budget and your long-term goals. You’d be surprised how easily we can talk ourselves into paying much more than we had originally decided. Use your financial planner to help avoid emotions getting involved and creeping up your price (especially when multiple offers are involved). A good rule of thumb is for a housing payment to be no more than 33% of your take-home income. This includes principal, interest, and taxes. Or, many planners will use the “2x income” rule of thumb. So if you make $300,000, don’t go over $600,000. Although with today’s low interest rates, there is some more wiggle room on that. Next, get a good referral from someone you trust in looking for a realtor. Real estate is a commission-based job and can have some potential conflicts of interest, so getting a recommendation can help. Or, there are realtors who will work for a flat fee, regardless of how much you pay for a house. That can help reduce the conflict.
You made the offer, you beat out the other bids, and you’re getting a house! How are you paying for it? Hopefully, you already got preapproved. This means finding a good, reputable mortgage professional. Get referrals, shop around, and take your time. Get multiple quotes before you start the underwriting process. They shouldn’t have to pull your credit to give you a fairly accurate estimate of what interest rate you’ll qualify for. Usually, they will give you fixed and variable interest quotes. I normally recommend fixed interest. Because interest rates are so low right now, they’re only going to go up in the future, and if you have a variable rate loan, your payment will go up as interest rates rise.
Is a physician loan a good idea? Depending on your circumstance, it can often be a good deal. Most new attendings don’t have cash saved up for a down payment, and these often don’t require one. And the other big benefit is that they won’t consider your student loan payments when calculating your debt-to-income ratio. Mortgage lenders will look at how much other debt you have when determining an approval. And a conventional mortgage will take your student loan payments into consideration, which means you’ll qualify for a much lower payment and purchase price. In my experience, you want a credit score of around 700 or higher to qualify for these types of loans. The only downside of a physician mortgage is the rates are slightly higher. I encourage you to start the application process early; they’re taking upward of 90 days lately.
As the mortgage is being processed, you’ll have an inspection and appraisal, and as long as those are all favorable, you’re in! Now, should you take any surplus income each month and pay extra on your mortgage to pay it down sooner, or invest it? Everyone’s situation is different, but a good rule of thumb is to look at interest rates on the debt you want to pay off versus expected rate of return on the potential investment. For example, if you have extra money, should you invest it in an SP500 index fund that historically gets 8%-12% per year, or put it on the principal of your mortgage that has an interest rate of 3%? Assuming no other factors or goals, and you just want the best bang for your buck, my money would go toward the investment getting 8%-12% over saving 3% on my mortgage.
Take your time, do your research, and find good professionals. There’s no right answer for everyone, but there are certainly some good practices when walking through the first home decision. Here at FinancialMD, we only work with physicians, and we’re happy to chat if you want some guidance on this. Send me an email and subscribe to our weekly Didactic Minute videos on YouTube for more financial tips for young physicians. Good luck!
Mr. Solitro is a financial planner and CEO of FinancialMD. He has no other conflicts of interest.
Investment advisory services offered through FinancialMD, a registered investment adviser. Registration as an investment adviser does not imply a certain level of skill or training. This article is provided for informational purposes only and nothing contained herein should be construed as a solicitation to buy or sell any products. Advisory services are offered only to clients and prospective clients in places where FinancialMD and its investment adviser representatives are registered or exempt from registration. Investing involves the risk of loss of principal. Past performance is no guarantee of future performance and no investment strategy can guarantee a profit or protect against loss.
This article was updated June 8, 2021.
Reference
1. Wachter S and Acolin A. Owning or Renting in the US: Shifting Dynamics of the Housing Market. Penn Institute for Urban Research. 2016 May.
Medical professional liability risk and mitigation: An overview for early-career gastroenterologists
Disclaimer: This article is for educational purposes only. All examples are hypothetical and aim to illustrate common clinical scenarios and challenges gastroenterologists may encounter within their scope of practice. The content herein should not be interpreted as legal advice for individual cases nor a substitute for seeking the advice of an attorney.
There are unique potential stressors faced by the gastroenterologist at each career stage, some more so early on. One such stressor, and one particularly important in a procedure-intensive specialty like GI, is medical professional liability (MPL), historically termed “medical malpractice.” Between 2009 and 2018, GI was the second-highest internal medicine subspecialty in both MPL claims made and claims paid,1 yet instruction on MPL risk and mitigation is scarce in fellowship, as is the available GI-related literature on the topic. This scarcity may generate untoward stress and unnecessarily expose gastroenterologists to avoidable MPL pitfalls. Therefore, it is vital for GI trainees, early-career gastroenterologists, and even seasoned gastroenterologists to have a working and updated knowledge of the general principles of MPL and GI-specific considerations. Such understanding can help preserve physician well-being, increase professional satisfaction, strengthen the doctor-patient relationship, and improve health care outcomes.2
To this end, we herein provide a focused review of the following: key MPL concepts, trends in MPL claims, GI-related MPL risk scenarios and considerations, adverse provider defensive mechanisms, documentation tenets, challenges posed by telemedicine, and the concept of “vicarious liability.”
Key MPL concepts
MPL falls under the umbrella of tort law, which itself falls under the umbrella of civil law; that is, civil (as opposed to criminal) justice governs torts – including but not limited to MPL claims – as well as other areas of law concerning noncriminal injury.3 A “tort” is a “civil wrong that unfairly causes another to experience loss or harm resulting in legal liability.”3 MPL claims assert the tort of negligence (similar to the concept of “incompetence”) and endeavor to compensate the harmed patient/individual while simultaneously dissuading suboptimal medical care by the provider in the future.4,5 A successful MPL claim must prove four overlapping elements: that the tortfeasor (here, the gastroenterologist) owed a duty of care to the injured party and breached that duty, which caused damages.6 Given that MPL cases exist within tort law rather than criminal law, the burden of proof for these cases is not “beyond a reasonable doubt”; instead, it’s “to a reasonable medical probability.”7
Trends in MPL claims
According to data compiled by the MPL Association, 278,220 MPL claims were made in the United States from 1985 to 2012.3,8-10 Among these, 1.8% involved gastroenterologists, which puts it at 17th place out of the 20 specialties surveyed.9 While the number of paid claims over this time frame decreased in GI by 34.6% (from 18.5 to 12.1 cases per 1,000 physician-years), there was a concurrent 23.3% increase in average claim compensation; essentially, there were fewer paid GI-related claims but there were higher payouts per paid claim.11,12 From 2009 to 2018, average legal defense costs for paid GI-related claims were $97,392, and average paid amount was $330,876.1
GI-related MPL risk scenarios and considerations
Many MPL claims relate to situations involving medical errors or adverse events (AEs), be they procedural or nonprocedural. However other aspects of GI also carry MPL risk.
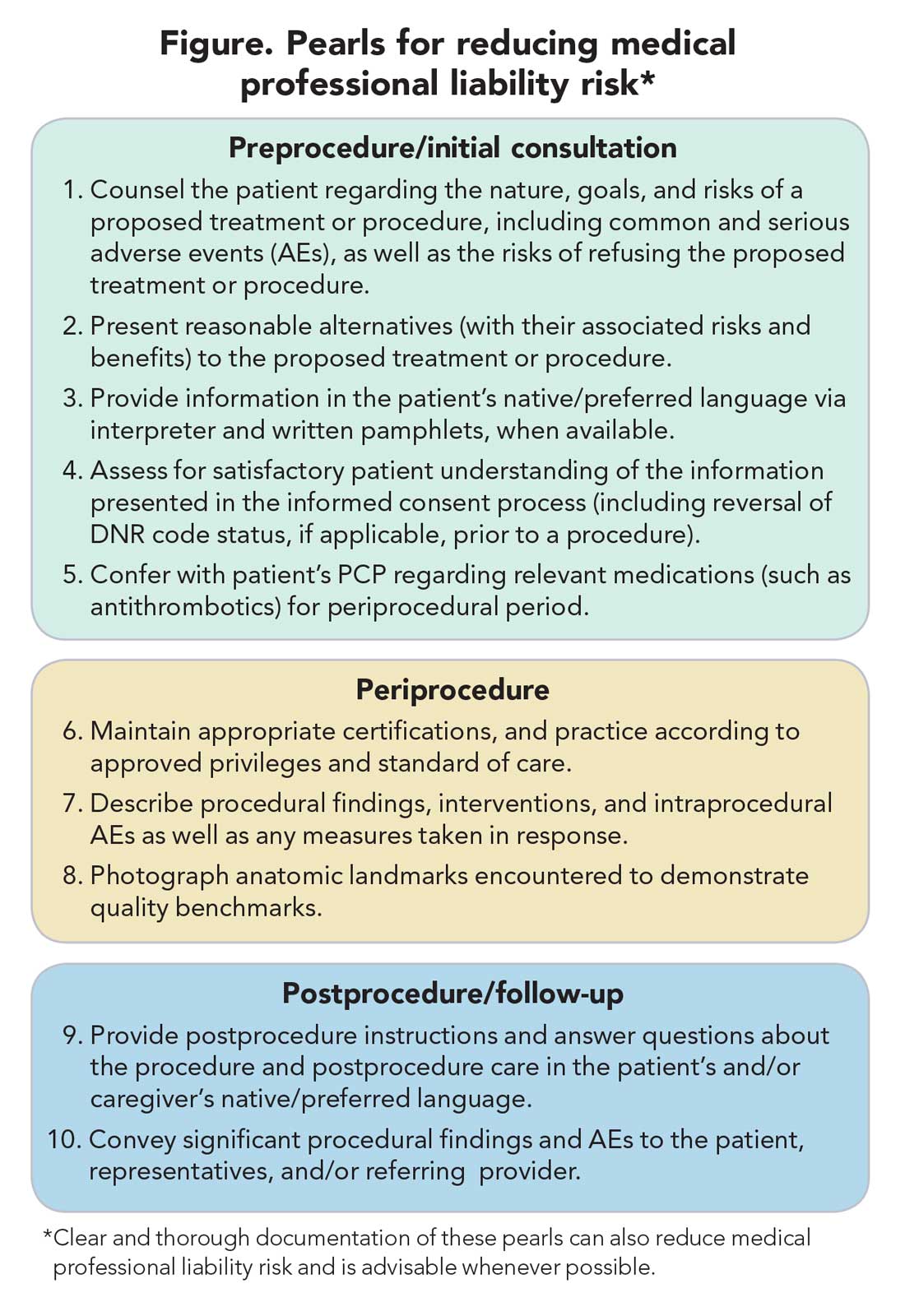
Informed consent
MPL claims may be made not only on the grounds of inadequately informed consent but also inadequately informed refusal.5,13,14 While standards for adequate informed consent vary by state, most states apply the “reasonable patient standard,” i.e., assuming an average patient with enough information to be an active participant in the medical decision-making process. Generally, informed consent should ensure that the patient understands the nature of the procedure/treatment being proposed, there is a discussion of the risks and benefits of undergoing and not undergoing the procedure/treatment, reasonable alternatives are presented, the risks and benefits associated with these alternatives are discussed, and the patient’s comprehension of these things is assessed (Figure).15 Additionally, informed consent should be tailored to each patient and GI procedure/treatment on a case-by-case basis rather than using a one-size-fits-all approach. Moreover, documentation of the patient’s understanding of the (tailored) information provided can concurrently improve quality of the consent and potentially decrease MPL risk (Figure).16
Endoscopic procedures
Procedure-related MPL claims represent approximately 25% of all GI-related claims (8,17). Among these, 52% involve colonoscopy, 16% involve endoscopic retrograde cholangiopancreatography (ERCP), and 11% involve esophagogastroduodenoscopy.8 Albeit generally safe, colonoscopy, as with esophagogastroduodenoscopy, is subject to rare but serious AEs.18,19 Risk of these AEs may be accentuated in certain scenarios (such as severe colonic inflammation or coagulopathy) and, as discussed earlier, may merit tailored informed consent. Regardless of the procedure, in the event of postprocedural development of signs/symptoms (such as tachycardia, fever, chest or abdominal discomfort, or hypotension) indicating a potential AE, stabilizing measures and evaluation (such as blood work and imaging) should be undertaken, and hospital admission (if not already hospitalized) should be considered until discharge is deemed safe.19
ERCP-related MPL claims, for many years, have had the highest average compensation of any GI procedure.11 Though discussion of advanced procedures is beyond the scope of this article, it is worth mentioning the observation that most of such claims involve an allegation that the procedure was not indicated (for example, that it was performed based on inadequate evidence of pancreatobiliary pathology), or was for diagnostic purposes (for example, being done instead of noninvasive imaging) rather than therapeutic.20-23 This emphasizes the importance of appropriate procedure indications.
Percutaneous endoscopic gastrostomy (PEG) placement merits special mention given it can be complicated by ethical challenges (for example, needing a surrogate decision-maker’s consent or representing medical futility) and has a relatively high potential for MPL claims. PEG placement carries a low AE rate (0.1%-1%), but these AEs may result in high morbidity/mortality, in part because of the underlying comorbidities of patients needing PEG placement.24,25 Also, timing of a patient’s demise may coincide with PEG placement, thereby prompting (possibly unfounded) perceptions of causality.24-27 Therefore, such scenarios merit unique additional preprocedure safeguards. For instance, for patients lacking capacity to provide informed consent, especially when family members may differ on whether PEG should be placed, it is advisable to ask the family to select one surrogate decision-maker (if there’s no advance directive) to whom the gastroenterologist should discuss both the risks, benefits, and goals of PEG placement in the context of the patient’s overall clinical trajectory/life expectancy and the need for consent (or refusal) based on what the patient would have wished. In addition, having a medical professional witness this discussion may be useful.27
Antithrombotic agents
Periprocedural management of antithrombotics, including anticoagulants and antiplatelets, can pose challenges for the gastroenterologist. While clinical practice guidelines exist to guide decision-making in this regard, the variables involved may extend beyond the expertise of the gastroenterologist.28 For instance, in addition to the procedural risk for bleeding, the indication for antithrombotic therapy, risk of a thrombotic event, duration of action of the antithrombotic, and available bridging options should all be considered according to recommendations.28,29 While requiring more time on the part of the gastroenterologist, the optimal periprocedural management of antithrombotic agents would usually involve discussion with the provider managing antithrombotic therapy to best conduct a risk-benefit assessment regarding if (and how long) the antithrombotic therapy should be held (Figure). This shared decision-making, which should also include the patient, may help decrease MPL risk and improve outcomes.
Provider defense mechanisms
Physicians may engage in various defensive behaviors in an attempt to mitigate MPL risk; however, these behaviors may, paradoxically, increase risk.30,31
Assurance behaviors
Assurance behaviors refer to the practice of recommending or performing additional services (such as medications, imaging, procedures, and referrals) that are not clearly indicated.2,30,31 Assurance behaviors are driven by fear of MPL risk and/or missing a potential diagnosis. Recent studies have estimated that more than 50% of gastroenterologists worldwide have performed additional invasive procedures without clear indications, and that nearly one-third of endoscopic procedures annually have questionable indications.30,32 While assurance behaviors may seem likely to decrease MPL risk, overall, they may inadvertently increase AE and MPL risk, as well as health care expenditures.3,30,32
Avoidance behaviors
Avoidance behaviors refer to providers avoiding participation in potentially high-risk clinical interventions (for example, the actual procedures), including those for which they are credentialed/certified proficient.30,31 Two clinical scenarios that illustrate this behavior include the following: An advanced endoscopist credentialed to perform ERCP might refer a “high-risk” elderly patient with cholangitis to another provider to perform said ERCP or for percutaneous transhepatic drainage (in the absence of a clear benefit to such), or a gastroenterologist might refer a patient to interventional gastroenterology for resection of a large polyp even though gastroenterologists are usually proficient in this skill and may feel comfortable performing the resection themselves. Avoidance behaviors are driven by a fear of MPL risk and can have several negative consequences.33 For example, patients may not receive indicated interventions. Additionally, patients may have to wait longer for an intervention because they are referred to another provider, which also increases potential for loss to follow-up.2,30,31 This may be viewed as noncompliance with the standard of care, among other hazards, thereby increasing MPL risk.
Documentation tenets
Thorough documentation can decrease MPL risk, especially since it is often used as legal evidence.16 Documenting, for instance, preprocedure discussion of potential risk of AEs (such as bleeding or perforation) or procedural failure (for example, missed lesions)can protect gastroenterologists (Figure).16 While, as discussed previously, these should be covered in the informed consent process (which itself reduces MPL risk), proof of compliance in providing adequate informed consent must come in the form of documentation that indicates that the process took place and specifically what topics were discussed therein. MPL risk may be further decreased by documenting steps taken during a procedure and anatomic landmarks encountered to offer proof of technical competency and compliance with standards of care (Figure).16,34 In this context, it is worth recalling the adage: “If it’s not documented, it did not occur.”
Curbside consults versus consultation
Also germane here is the topic of whether documentation is needed for “curbside consults.” The uncertainty is, in part, semantic; that is, at what point does a “curbside” become a consultation? A curbside is a general question or query (such as anything that could also be answered by searching the Internet or reference materials) in response to which information is provided; once it involves provision of medical advice for a specific patient (for example, when patient identifiers have been shared or their EHR has been accessed), it constitutes a consultation. Based on these definitions, a curbside need not be documented, whereas a consultation – even if seemingly trivial – should be.
Consideration of language and cultural factors
Language barriers should be considered when the gastroenterologist is communicating with the patient, and such efforts, whenever made, should be documented to best protect against MPL.16,35 These considerations arise not only during the consent process but when obtaining a history, providing postprocedure instructions, and during follow-ups. To this end, 24/7 telephone interpreter services may assist the gastroenterologist (when one is communicating with non–English speakers and is not medically certified in the patient’s native/preferred language) and strengthen trust in the provider-patient relationship.36 Additionally, written materials (such as consent forms, procedural information) in patients’ native/preferred languages should be provided, when available, to enhance patient understanding and participation in care (Figure).35
Challenges posed by telemedicine
The COVID-19 pandemic has rapidly led to more virtual encounters. While increased utilization of telemedicine platforms may make health care more accessible, it does not lessen the clinicians’ duty to patients and may actually expose them to greater MPL risk.18,37,38 Therefore, the provider must be cognizant of two key principles to mitigate MPL risk in the context of telemedicine encounters. First, the same standard of care applies to virtual and in-person encounters.18,37,38 Second, patient privacy and HIPAA regulations are not waived during telemedicine encounters, and breaches of such may result in an MPL claim.18,37,38
With regard to the first principle, for patients who have not been physically examined (such as when a telemedicine visit was substituted for an in-person clinic encounter), gastroenterologists should not overlook requesting timely preprocedure anesthesia consultation or obtaining additional laboratory studies as needed to ensure safety and the same standard of care. Moreover, particularly in the context of pandemic-related decreased procedural capacity, triaging procedures can be especially challenging. Standardized institutional criteria which prioritize certain diagnoses/conditions over others, leaving room for justifiable exceptions, are advisable.
Vicarious liability
“Vicarious liability” is defined as that extending to persons who have not committed a wrong but on whose behalf wrongdoers acted.39 Therefore, gastroenterologists may be liable not only for their own actions but also for those of personnel they supervise (such as fellow trainees and non–physician practitioners).39 Vicarious liability aims to ensure that systemic checks and balances are in place so that, if failure occurs, harm can still be mitigated and/or avoided, as illustrated by Reason’s “Swiss Cheese Model.”40
Conclusion
Any gastroenterologist can experience an MPL claim. Such an experience can be especially stressful and confusing to early-career clinicians, especially if they’re unfamiliar with legal proceedings. Although MPL principles are not often taught in medical school or residency, it is important for gastroenterologists to be informed regarding tenets of MPL and cognizant of clinical situations which have relatively higher MPL risk. This can assuage untoward angst regarding MPL and highlight proactive risk-mitigation strategies. In general, gastroenterologist practices that can mitigate MPL risk include effective communication; adequate informed consent/refusal; documentation of preprocedure counseling, periprocedure events, and postprocedure recommendations; and maintenance of proper certification and privileging.
Dr. Azizian and Dr. Dalai are with the University of California, Los Angeles and the department of medicine at Olive View–UCLA Medical Center, Sylmar, Calif. They are co–first authors of this paper. Dr. Dalai is also with the division of gastroenterology at the University of New Mexico, Albuquerque. Dr. Adams is with the Center for Clinical Management Research in Veterans Affairs Ann Arbor Healthcare System, the division of gastroenterology at the University of Michigan Health System, and the Institute for Healthcare Policy and Innovation, all in Ann Arbor, Mich. Dr. Tabibian is with UCLA and the division of gastroenterology at Olive View–UCLA Medical Center. The authors have no conflicts of interest.
References
1. 2020 Data Sharing Project Gastroenterology 2009-2018. Inside Medical Liability: Second Quarter. Accessed 2020 Dec 6.
2. Mello MM et al. Health Aff (Millwood). 2004 Jul-Aug;23(4):42-53.
3. Adams MA et al. JAMA. 2014 Oct;312(13):1348-9.
4. Pegalis SE. American Law of Medical Malpractice 3d, Vol. 2. St. Paul, Minn.: Thomson Reuters, 2005.
5. Feld LD et al. Am J Gastroenterol. 2018 Nov;113(11):1577-9.
6. Sawyer v. Wight, 196 F. Supp. 2d 220, 226 (E.D.N.Y. 2002).
7. Michael A. Sita v. Long Island Jewish-Hillside Medical Center, 22 A.D.3d 743 (N.Y. App. Div. 2005).
8. Conklin LS et al. Clin Gastroenterol Hepatol. 2008 Jun;6(6):677-81.
9. Jena AB et al. N Engl J Med. 2011 Aug 18;365(7):629-36.
10. Kane CK. “Policy Research Perspectives Medical Liability Claim Frequency: A 2007-2008 Snapshot of Physicians.” Chicago: American Medical Association, 2010.
11. Hernandez LV et al. World J Gastrointest Endosc. 2013 Apr 16;5(4):169-73.
12. Schaffer AC et al. JAMA Intern Med. 2017 May 1;177(5):710-8.
13. Natanson v. Kline, 186 Kan. 393, 409, 350 P.2d 1093, 1106, decision clarified on denial of reh’g, 187 Kan. 186, 354 P.2d 670 (1960).
14. Truman v. Thomas, 27 Cal. 3d 285, 292, 611 P.2d 902, 906 (1980).
15. Shah P et al. Informed Consent, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Aug 22.
16. Rex DK. Clin Gastroenterol Hepatol. 2013 Jul;11(7):768-73.
17. Gerstenberger PD, Plumeri PA. Gastrointest Endosc. Mar-Apr 1993;39(2):132-8.
18. Adams MA and Allen JI. Clin Gastroenterol Hepatol. 2019 Nov;17(12):2392-6.e1.
19. Ahlawat R et al. Esophagogastroduodenoscopy, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Dec 9.
20. Cotton PB. Gastrointest Endosc. 2006 Mar;63(3):378-82.
21. Cotton PB. Gastrointest Endosc. 2010 Oct;72(4):904.
22. Adamson TE et al. West J Med. 1989 Mar;150(3):356-60.
23. Trap R et al. Endoscopy. 1999 Feb;31(2):125-30.
24. Funaki B. Semin Intervent Radiol. 2015 Mar;32(1):61-4.
25. Feeding Tube Nursing Home and Hospital Malpractice. Miller & Zois, Attorneys at Law. Accessed 2020 Jun 20.
26. Medical Malpractice Lawsuit Brings $750,000 Settlement: Death of 82-year-old woman from sepsis due to improper placement of feeding tube. Lubin & Meyers PC. Accessed 2020 Jun 20.
27. Brendel RW et al. Med Clin North Am. 2010 Nov;94(6):1229-40, xi-ii.
28. ASGE Standards of Practice Committee; Acosta RD et al. Gastrointest Endosc. 2016 Jan;83(1):3-16.
29. Saleem S and Thomas AL. Cureus. 2018 Jun 25;10(6):e2878.
30. Hiyama T et al. World J Gastroenterol. 2006 Dec 21;12(47):7671-5.
31. Studdert DM et al. JAMA. 2005 Jun 1;293(21):2609-17.
32. Shaheen NJ et al. Gastroenterology. 2018 May;154(7):1993-2003.
33. Oza VM et al. Clin Gastroenterol Hepatol. 2016 Feb;14(2):172-4.
34. Feld AD. Gastrointest Endosc Clin N Am. 2002 Jan;12(1):171-9, viii-ix.
35. Lee JS et al. J Gen Intern Med. 2017 Aug;32(8):863-70.
36. Forrow L and Kontrimas JC. J Gen Intern Med. 2017 Aug;32(8):855-7.
37. Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
38. Tabibian JH. “The Evolution of Telehealth.” Guidepoint: Legal Solutions Blog. Accessed 2020 Aug 12.
39. Feld AD. Am J Gastroenterol. 2004 Sep;99(9):1641-4.
40. Reason J. BMJ. 2000;320(7237):768‐70.
Disclaimer: This article is for educational purposes only. All examples are hypothetical and aim to illustrate common clinical scenarios and challenges gastroenterologists may encounter within their scope of practice. The content herein should not be interpreted as legal advice for individual cases nor a substitute for seeking the advice of an attorney.
There are unique potential stressors faced by the gastroenterologist at each career stage, some more so early on. One such stressor, and one particularly important in a procedure-intensive specialty like GI, is medical professional liability (MPL), historically termed “medical malpractice.” Between 2009 and 2018, GI was the second-highest internal medicine subspecialty in both MPL claims made and claims paid,1 yet instruction on MPL risk and mitigation is scarce in fellowship, as is the available GI-related literature on the topic. This scarcity may generate untoward stress and unnecessarily expose gastroenterologists to avoidable MPL pitfalls. Therefore, it is vital for GI trainees, early-career gastroenterologists, and even seasoned gastroenterologists to have a working and updated knowledge of the general principles of MPL and GI-specific considerations. Such understanding can help preserve physician well-being, increase professional satisfaction, strengthen the doctor-patient relationship, and improve health care outcomes.2
To this end, we herein provide a focused review of the following: key MPL concepts, trends in MPL claims, GI-related MPL risk scenarios and considerations, adverse provider defensive mechanisms, documentation tenets, challenges posed by telemedicine, and the concept of “vicarious liability.”
Key MPL concepts
MPL falls under the umbrella of tort law, which itself falls under the umbrella of civil law; that is, civil (as opposed to criminal) justice governs torts – including but not limited to MPL claims – as well as other areas of law concerning noncriminal injury.3 A “tort” is a “civil wrong that unfairly causes another to experience loss or harm resulting in legal liability.”3 MPL claims assert the tort of negligence (similar to the concept of “incompetence”) and endeavor to compensate the harmed patient/individual while simultaneously dissuading suboptimal medical care by the provider in the future.4,5 A successful MPL claim must prove four overlapping elements: that the tortfeasor (here, the gastroenterologist) owed a duty of care to the injured party and breached that duty, which caused damages.6 Given that MPL cases exist within tort law rather than criminal law, the burden of proof for these cases is not “beyond a reasonable doubt”; instead, it’s “to a reasonable medical probability.”7
Trends in MPL claims
According to data compiled by the MPL Association, 278,220 MPL claims were made in the United States from 1985 to 2012.3,8-10 Among these, 1.8% involved gastroenterologists, which puts it at 17th place out of the 20 specialties surveyed.9 While the number of paid claims over this time frame decreased in GI by 34.6% (from 18.5 to 12.1 cases per 1,000 physician-years), there was a concurrent 23.3% increase in average claim compensation; essentially, there were fewer paid GI-related claims but there were higher payouts per paid claim.11,12 From 2009 to 2018, average legal defense costs for paid GI-related claims were $97,392, and average paid amount was $330,876.1
GI-related MPL risk scenarios and considerations
Many MPL claims relate to situations involving medical errors or adverse events (AEs), be they procedural or nonprocedural. However other aspects of GI also carry MPL risk.
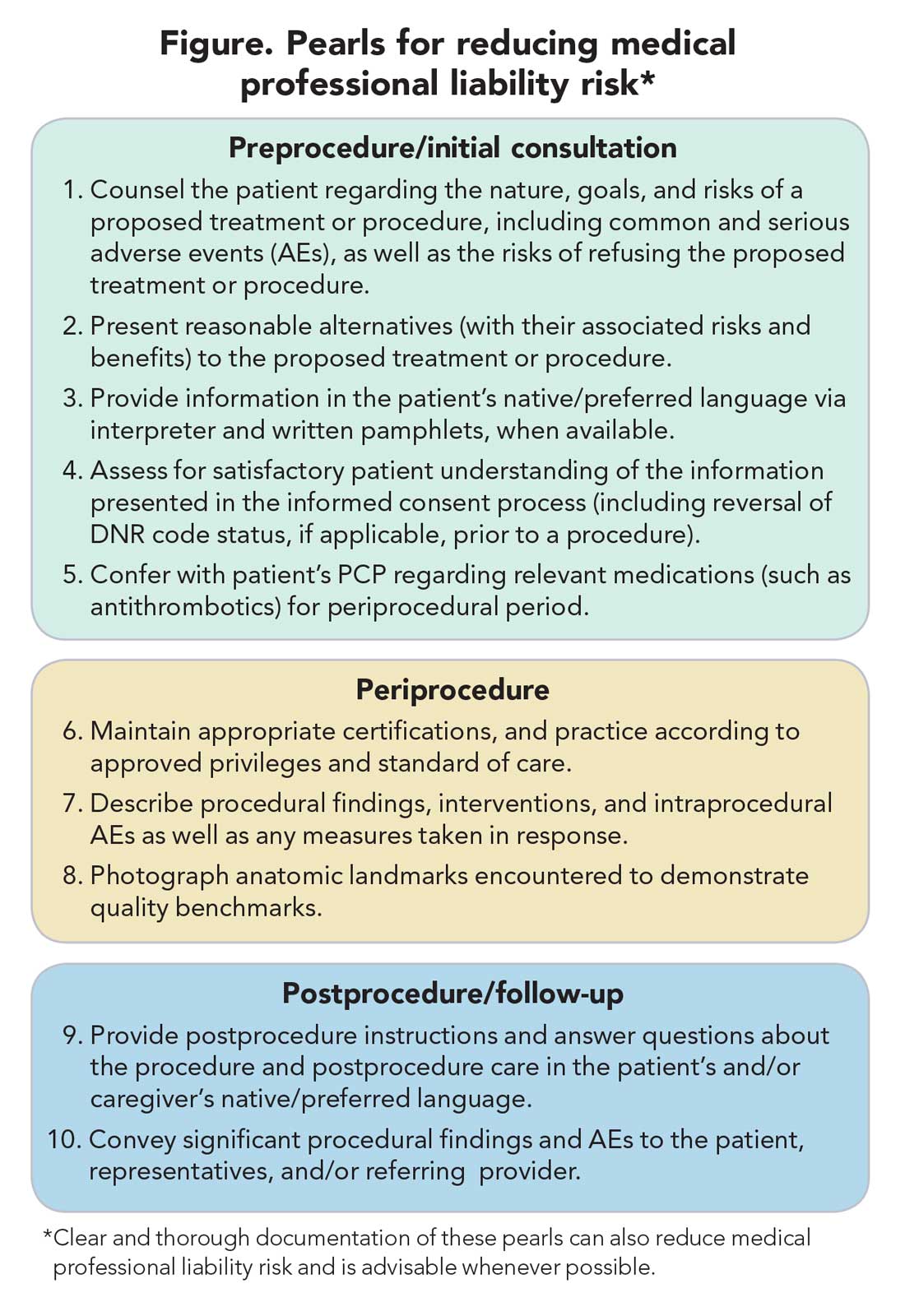
Informed consent
MPL claims may be made not only on the grounds of inadequately informed consent but also inadequately informed refusal.5,13,14 While standards for adequate informed consent vary by state, most states apply the “reasonable patient standard,” i.e., assuming an average patient with enough information to be an active participant in the medical decision-making process. Generally, informed consent should ensure that the patient understands the nature of the procedure/treatment being proposed, there is a discussion of the risks and benefits of undergoing and not undergoing the procedure/treatment, reasonable alternatives are presented, the risks and benefits associated with these alternatives are discussed, and the patient’s comprehension of these things is assessed (Figure).15 Additionally, informed consent should be tailored to each patient and GI procedure/treatment on a case-by-case basis rather than using a one-size-fits-all approach. Moreover, documentation of the patient’s understanding of the (tailored) information provided can concurrently improve quality of the consent and potentially decrease MPL risk (Figure).16
Endoscopic procedures
Procedure-related MPL claims represent approximately 25% of all GI-related claims (8,17). Among these, 52% involve colonoscopy, 16% involve endoscopic retrograde cholangiopancreatography (ERCP), and 11% involve esophagogastroduodenoscopy.8 Albeit generally safe, colonoscopy, as with esophagogastroduodenoscopy, is subject to rare but serious AEs.18,19 Risk of these AEs may be accentuated in certain scenarios (such as severe colonic inflammation or coagulopathy) and, as discussed earlier, may merit tailored informed consent. Regardless of the procedure, in the event of postprocedural development of signs/symptoms (such as tachycardia, fever, chest or abdominal discomfort, or hypotension) indicating a potential AE, stabilizing measures and evaluation (such as blood work and imaging) should be undertaken, and hospital admission (if not already hospitalized) should be considered until discharge is deemed safe.19
ERCP-related MPL claims, for many years, have had the highest average compensation of any GI procedure.11 Though discussion of advanced procedures is beyond the scope of this article, it is worth mentioning the observation that most of such claims involve an allegation that the procedure was not indicated (for example, that it was performed based on inadequate evidence of pancreatobiliary pathology), or was for diagnostic purposes (for example, being done instead of noninvasive imaging) rather than therapeutic.20-23 This emphasizes the importance of appropriate procedure indications.
Percutaneous endoscopic gastrostomy (PEG) placement merits special mention given it can be complicated by ethical challenges (for example, needing a surrogate decision-maker’s consent or representing medical futility) and has a relatively high potential for MPL claims. PEG placement carries a low AE rate (0.1%-1%), but these AEs may result in high morbidity/mortality, in part because of the underlying comorbidities of patients needing PEG placement.24,25 Also, timing of a patient’s demise may coincide with PEG placement, thereby prompting (possibly unfounded) perceptions of causality.24-27 Therefore, such scenarios merit unique additional preprocedure safeguards. For instance, for patients lacking capacity to provide informed consent, especially when family members may differ on whether PEG should be placed, it is advisable to ask the family to select one surrogate decision-maker (if there’s no advance directive) to whom the gastroenterologist should discuss both the risks, benefits, and goals of PEG placement in the context of the patient’s overall clinical trajectory/life expectancy and the need for consent (or refusal) based on what the patient would have wished. In addition, having a medical professional witness this discussion may be useful.27
Antithrombotic agents
Periprocedural management of antithrombotics, including anticoagulants and antiplatelets, can pose challenges for the gastroenterologist. While clinical practice guidelines exist to guide decision-making in this regard, the variables involved may extend beyond the expertise of the gastroenterologist.28 For instance, in addition to the procedural risk for bleeding, the indication for antithrombotic therapy, risk of a thrombotic event, duration of action of the antithrombotic, and available bridging options should all be considered according to recommendations.28,29 While requiring more time on the part of the gastroenterologist, the optimal periprocedural management of antithrombotic agents would usually involve discussion with the provider managing antithrombotic therapy to best conduct a risk-benefit assessment regarding if (and how long) the antithrombotic therapy should be held (Figure). This shared decision-making, which should also include the patient, may help decrease MPL risk and improve outcomes.
Provider defense mechanisms
Physicians may engage in various defensive behaviors in an attempt to mitigate MPL risk; however, these behaviors may, paradoxically, increase risk.30,31
Assurance behaviors
Assurance behaviors refer to the practice of recommending or performing additional services (such as medications, imaging, procedures, and referrals) that are not clearly indicated.2,30,31 Assurance behaviors are driven by fear of MPL risk and/or missing a potential diagnosis. Recent studies have estimated that more than 50% of gastroenterologists worldwide have performed additional invasive procedures without clear indications, and that nearly one-third of endoscopic procedures annually have questionable indications.30,32 While assurance behaviors may seem likely to decrease MPL risk, overall, they may inadvertently increase AE and MPL risk, as well as health care expenditures.3,30,32
Avoidance behaviors
Avoidance behaviors refer to providers avoiding participation in potentially high-risk clinical interventions (for example, the actual procedures), including those for which they are credentialed/certified proficient.30,31 Two clinical scenarios that illustrate this behavior include the following: An advanced endoscopist credentialed to perform ERCP might refer a “high-risk” elderly patient with cholangitis to another provider to perform said ERCP or for percutaneous transhepatic drainage (in the absence of a clear benefit to such), or a gastroenterologist might refer a patient to interventional gastroenterology for resection of a large polyp even though gastroenterologists are usually proficient in this skill and may feel comfortable performing the resection themselves. Avoidance behaviors are driven by a fear of MPL risk and can have several negative consequences.33 For example, patients may not receive indicated interventions. Additionally, patients may have to wait longer for an intervention because they are referred to another provider, which also increases potential for loss to follow-up.2,30,31 This may be viewed as noncompliance with the standard of care, among other hazards, thereby increasing MPL risk.
Documentation tenets
Thorough documentation can decrease MPL risk, especially since it is often used as legal evidence.16 Documenting, for instance, preprocedure discussion of potential risk of AEs (such as bleeding or perforation) or procedural failure (for example, missed lesions)can protect gastroenterologists (Figure).16 While, as discussed previously, these should be covered in the informed consent process (which itself reduces MPL risk), proof of compliance in providing adequate informed consent must come in the form of documentation that indicates that the process took place and specifically what topics were discussed therein. MPL risk may be further decreased by documenting steps taken during a procedure and anatomic landmarks encountered to offer proof of technical competency and compliance with standards of care (Figure).16,34 In this context, it is worth recalling the adage: “If it’s not documented, it did not occur.”
Curbside consults versus consultation
Also germane here is the topic of whether documentation is needed for “curbside consults.” The uncertainty is, in part, semantic; that is, at what point does a “curbside” become a consultation? A curbside is a general question or query (such as anything that could also be answered by searching the Internet or reference materials) in response to which information is provided; once it involves provision of medical advice for a specific patient (for example, when patient identifiers have been shared or their EHR has been accessed), it constitutes a consultation. Based on these definitions, a curbside need not be documented, whereas a consultation – even if seemingly trivial – should be.
Consideration of language and cultural factors
Language barriers should be considered when the gastroenterologist is communicating with the patient, and such efforts, whenever made, should be documented to best protect against MPL.16,35 These considerations arise not only during the consent process but when obtaining a history, providing postprocedure instructions, and during follow-ups. To this end, 24/7 telephone interpreter services may assist the gastroenterologist (when one is communicating with non–English speakers and is not medically certified in the patient’s native/preferred language) and strengthen trust in the provider-patient relationship.36 Additionally, written materials (such as consent forms, procedural information) in patients’ native/preferred languages should be provided, when available, to enhance patient understanding and participation in care (Figure).35
Challenges posed by telemedicine
The COVID-19 pandemic has rapidly led to more virtual encounters. While increased utilization of telemedicine platforms may make health care more accessible, it does not lessen the clinicians’ duty to patients and may actually expose them to greater MPL risk.18,37,38 Therefore, the provider must be cognizant of two key principles to mitigate MPL risk in the context of telemedicine encounters. First, the same standard of care applies to virtual and in-person encounters.18,37,38 Second, patient privacy and HIPAA regulations are not waived during telemedicine encounters, and breaches of such may result in an MPL claim.18,37,38
With regard to the first principle, for patients who have not been physically examined (such as when a telemedicine visit was substituted for an in-person clinic encounter), gastroenterologists should not overlook requesting timely preprocedure anesthesia consultation or obtaining additional laboratory studies as needed to ensure safety and the same standard of care. Moreover, particularly in the context of pandemic-related decreased procedural capacity, triaging procedures can be especially challenging. Standardized institutional criteria which prioritize certain diagnoses/conditions over others, leaving room for justifiable exceptions, are advisable.
Vicarious liability
“Vicarious liability” is defined as that extending to persons who have not committed a wrong but on whose behalf wrongdoers acted.39 Therefore, gastroenterologists may be liable not only for their own actions but also for those of personnel they supervise (such as fellow trainees and non–physician practitioners).39 Vicarious liability aims to ensure that systemic checks and balances are in place so that, if failure occurs, harm can still be mitigated and/or avoided, as illustrated by Reason’s “Swiss Cheese Model.”40
Conclusion
Any gastroenterologist can experience an MPL claim. Such an experience can be especially stressful and confusing to early-career clinicians, especially if they’re unfamiliar with legal proceedings. Although MPL principles are not often taught in medical school or residency, it is important for gastroenterologists to be informed regarding tenets of MPL and cognizant of clinical situations which have relatively higher MPL risk. This can assuage untoward angst regarding MPL and highlight proactive risk-mitigation strategies. In general, gastroenterologist practices that can mitigate MPL risk include effective communication; adequate informed consent/refusal; documentation of preprocedure counseling, periprocedure events, and postprocedure recommendations; and maintenance of proper certification and privileging.
Dr. Azizian and Dr. Dalai are with the University of California, Los Angeles and the department of medicine at Olive View–UCLA Medical Center, Sylmar, Calif. They are co–first authors of this paper. Dr. Dalai is also with the division of gastroenterology at the University of New Mexico, Albuquerque. Dr. Adams is with the Center for Clinical Management Research in Veterans Affairs Ann Arbor Healthcare System, the division of gastroenterology at the University of Michigan Health System, and the Institute for Healthcare Policy and Innovation, all in Ann Arbor, Mich. Dr. Tabibian is with UCLA and the division of gastroenterology at Olive View–UCLA Medical Center. The authors have no conflicts of interest.
References
1. 2020 Data Sharing Project Gastroenterology 2009-2018. Inside Medical Liability: Second Quarter. Accessed 2020 Dec 6.
2. Mello MM et al. Health Aff (Millwood). 2004 Jul-Aug;23(4):42-53.
3. Adams MA et al. JAMA. 2014 Oct;312(13):1348-9.
4. Pegalis SE. American Law of Medical Malpractice 3d, Vol. 2. St. Paul, Minn.: Thomson Reuters, 2005.
5. Feld LD et al. Am J Gastroenterol. 2018 Nov;113(11):1577-9.
6. Sawyer v. Wight, 196 F. Supp. 2d 220, 226 (E.D.N.Y. 2002).
7. Michael A. Sita v. Long Island Jewish-Hillside Medical Center, 22 A.D.3d 743 (N.Y. App. Div. 2005).
8. Conklin LS et al. Clin Gastroenterol Hepatol. 2008 Jun;6(6):677-81.
9. Jena AB et al. N Engl J Med. 2011 Aug 18;365(7):629-36.
10. Kane CK. “Policy Research Perspectives Medical Liability Claim Frequency: A 2007-2008 Snapshot of Physicians.” Chicago: American Medical Association, 2010.
11. Hernandez LV et al. World J Gastrointest Endosc. 2013 Apr 16;5(4):169-73.
12. Schaffer AC et al. JAMA Intern Med. 2017 May 1;177(5):710-8.
13. Natanson v. Kline, 186 Kan. 393, 409, 350 P.2d 1093, 1106, decision clarified on denial of reh’g, 187 Kan. 186, 354 P.2d 670 (1960).
14. Truman v. Thomas, 27 Cal. 3d 285, 292, 611 P.2d 902, 906 (1980).
15. Shah P et al. Informed Consent, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Aug 22.
16. Rex DK. Clin Gastroenterol Hepatol. 2013 Jul;11(7):768-73.
17. Gerstenberger PD, Plumeri PA. Gastrointest Endosc. Mar-Apr 1993;39(2):132-8.
18. Adams MA and Allen JI. Clin Gastroenterol Hepatol. 2019 Nov;17(12):2392-6.e1.
19. Ahlawat R et al. Esophagogastroduodenoscopy, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Dec 9.
20. Cotton PB. Gastrointest Endosc. 2006 Mar;63(3):378-82.
21. Cotton PB. Gastrointest Endosc. 2010 Oct;72(4):904.
22. Adamson TE et al. West J Med. 1989 Mar;150(3):356-60.
23. Trap R et al. Endoscopy. 1999 Feb;31(2):125-30.
24. Funaki B. Semin Intervent Radiol. 2015 Mar;32(1):61-4.
25. Feeding Tube Nursing Home and Hospital Malpractice. Miller & Zois, Attorneys at Law. Accessed 2020 Jun 20.
26. Medical Malpractice Lawsuit Brings $750,000 Settlement: Death of 82-year-old woman from sepsis due to improper placement of feeding tube. Lubin & Meyers PC. Accessed 2020 Jun 20.
27. Brendel RW et al. Med Clin North Am. 2010 Nov;94(6):1229-40, xi-ii.
28. ASGE Standards of Practice Committee; Acosta RD et al. Gastrointest Endosc. 2016 Jan;83(1):3-16.
29. Saleem S and Thomas AL. Cureus. 2018 Jun 25;10(6):e2878.
30. Hiyama T et al. World J Gastroenterol. 2006 Dec 21;12(47):7671-5.
31. Studdert DM et al. JAMA. 2005 Jun 1;293(21):2609-17.
32. Shaheen NJ et al. Gastroenterology. 2018 May;154(7):1993-2003.
33. Oza VM et al. Clin Gastroenterol Hepatol. 2016 Feb;14(2):172-4.
34. Feld AD. Gastrointest Endosc Clin N Am. 2002 Jan;12(1):171-9, viii-ix.
35. Lee JS et al. J Gen Intern Med. 2017 Aug;32(8):863-70.
36. Forrow L and Kontrimas JC. J Gen Intern Med. 2017 Aug;32(8):855-7.
37. Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
38. Tabibian JH. “The Evolution of Telehealth.” Guidepoint: Legal Solutions Blog. Accessed 2020 Aug 12.
39. Feld AD. Am J Gastroenterol. 2004 Sep;99(9):1641-4.
40. Reason J. BMJ. 2000;320(7237):768‐70.
Disclaimer: This article is for educational purposes only. All examples are hypothetical and aim to illustrate common clinical scenarios and challenges gastroenterologists may encounter within their scope of practice. The content herein should not be interpreted as legal advice for individual cases nor a substitute for seeking the advice of an attorney.
There are unique potential stressors faced by the gastroenterologist at each career stage, some more so early on. One such stressor, and one particularly important in a procedure-intensive specialty like GI, is medical professional liability (MPL), historically termed “medical malpractice.” Between 2009 and 2018, GI was the second-highest internal medicine subspecialty in both MPL claims made and claims paid,1 yet instruction on MPL risk and mitigation is scarce in fellowship, as is the available GI-related literature on the topic. This scarcity may generate untoward stress and unnecessarily expose gastroenterologists to avoidable MPL pitfalls. Therefore, it is vital for GI trainees, early-career gastroenterologists, and even seasoned gastroenterologists to have a working and updated knowledge of the general principles of MPL and GI-specific considerations. Such understanding can help preserve physician well-being, increase professional satisfaction, strengthen the doctor-patient relationship, and improve health care outcomes.2
To this end, we herein provide a focused review of the following: key MPL concepts, trends in MPL claims, GI-related MPL risk scenarios and considerations, adverse provider defensive mechanisms, documentation tenets, challenges posed by telemedicine, and the concept of “vicarious liability.”
Key MPL concepts
MPL falls under the umbrella of tort law, which itself falls under the umbrella of civil law; that is, civil (as opposed to criminal) justice governs torts – including but not limited to MPL claims – as well as other areas of law concerning noncriminal injury.3 A “tort” is a “civil wrong that unfairly causes another to experience loss or harm resulting in legal liability.”3 MPL claims assert the tort of negligence (similar to the concept of “incompetence”) and endeavor to compensate the harmed patient/individual while simultaneously dissuading suboptimal medical care by the provider in the future.4,5 A successful MPL claim must prove four overlapping elements: that the tortfeasor (here, the gastroenterologist) owed a duty of care to the injured party and breached that duty, which caused damages.6 Given that MPL cases exist within tort law rather than criminal law, the burden of proof for these cases is not “beyond a reasonable doubt”; instead, it’s “to a reasonable medical probability.”7
Trends in MPL claims
According to data compiled by the MPL Association, 278,220 MPL claims were made in the United States from 1985 to 2012.3,8-10 Among these, 1.8% involved gastroenterologists, which puts it at 17th place out of the 20 specialties surveyed.9 While the number of paid claims over this time frame decreased in GI by 34.6% (from 18.5 to 12.1 cases per 1,000 physician-years), there was a concurrent 23.3% increase in average claim compensation; essentially, there were fewer paid GI-related claims but there were higher payouts per paid claim.11,12 From 2009 to 2018, average legal defense costs for paid GI-related claims were $97,392, and average paid amount was $330,876.1
GI-related MPL risk scenarios and considerations
Many MPL claims relate to situations involving medical errors or adverse events (AEs), be they procedural or nonprocedural. However other aspects of GI also carry MPL risk.
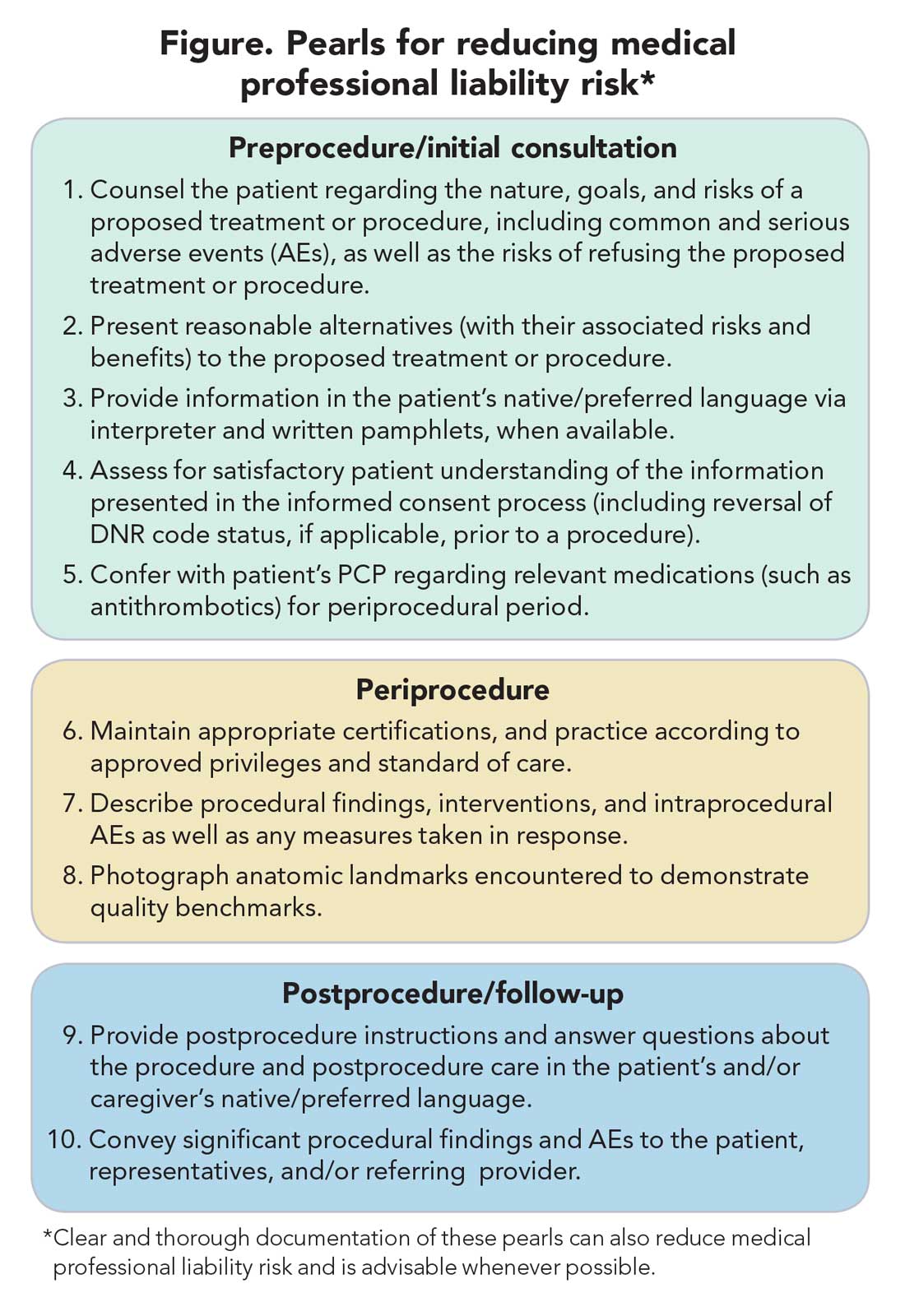
Informed consent
MPL claims may be made not only on the grounds of inadequately informed consent but also inadequately informed refusal.5,13,14 While standards for adequate informed consent vary by state, most states apply the “reasonable patient standard,” i.e., assuming an average patient with enough information to be an active participant in the medical decision-making process. Generally, informed consent should ensure that the patient understands the nature of the procedure/treatment being proposed, there is a discussion of the risks and benefits of undergoing and not undergoing the procedure/treatment, reasonable alternatives are presented, the risks and benefits associated with these alternatives are discussed, and the patient’s comprehension of these things is assessed (Figure).15 Additionally, informed consent should be tailored to each patient and GI procedure/treatment on a case-by-case basis rather than using a one-size-fits-all approach. Moreover, documentation of the patient’s understanding of the (tailored) information provided can concurrently improve quality of the consent and potentially decrease MPL risk (Figure).16
Endoscopic procedures
Procedure-related MPL claims represent approximately 25% of all GI-related claims (8,17). Among these, 52% involve colonoscopy, 16% involve endoscopic retrograde cholangiopancreatography (ERCP), and 11% involve esophagogastroduodenoscopy.8 Albeit generally safe, colonoscopy, as with esophagogastroduodenoscopy, is subject to rare but serious AEs.18,19 Risk of these AEs may be accentuated in certain scenarios (such as severe colonic inflammation or coagulopathy) and, as discussed earlier, may merit tailored informed consent. Regardless of the procedure, in the event of postprocedural development of signs/symptoms (such as tachycardia, fever, chest or abdominal discomfort, or hypotension) indicating a potential AE, stabilizing measures and evaluation (such as blood work and imaging) should be undertaken, and hospital admission (if not already hospitalized) should be considered until discharge is deemed safe.19
ERCP-related MPL claims, for many years, have had the highest average compensation of any GI procedure.11 Though discussion of advanced procedures is beyond the scope of this article, it is worth mentioning the observation that most of such claims involve an allegation that the procedure was not indicated (for example, that it was performed based on inadequate evidence of pancreatobiliary pathology), or was for diagnostic purposes (for example, being done instead of noninvasive imaging) rather than therapeutic.20-23 This emphasizes the importance of appropriate procedure indications.
Percutaneous endoscopic gastrostomy (PEG) placement merits special mention given it can be complicated by ethical challenges (for example, needing a surrogate decision-maker’s consent or representing medical futility) and has a relatively high potential for MPL claims. PEG placement carries a low AE rate (0.1%-1%), but these AEs may result in high morbidity/mortality, in part because of the underlying comorbidities of patients needing PEG placement.24,25 Also, timing of a patient’s demise may coincide with PEG placement, thereby prompting (possibly unfounded) perceptions of causality.24-27 Therefore, such scenarios merit unique additional preprocedure safeguards. For instance, for patients lacking capacity to provide informed consent, especially when family members may differ on whether PEG should be placed, it is advisable to ask the family to select one surrogate decision-maker (if there’s no advance directive) to whom the gastroenterologist should discuss both the risks, benefits, and goals of PEG placement in the context of the patient’s overall clinical trajectory/life expectancy and the need for consent (or refusal) based on what the patient would have wished. In addition, having a medical professional witness this discussion may be useful.27
Antithrombotic agents
Periprocedural management of antithrombotics, including anticoagulants and antiplatelets, can pose challenges for the gastroenterologist. While clinical practice guidelines exist to guide decision-making in this regard, the variables involved may extend beyond the expertise of the gastroenterologist.28 For instance, in addition to the procedural risk for bleeding, the indication for antithrombotic therapy, risk of a thrombotic event, duration of action of the antithrombotic, and available bridging options should all be considered according to recommendations.28,29 While requiring more time on the part of the gastroenterologist, the optimal periprocedural management of antithrombotic agents would usually involve discussion with the provider managing antithrombotic therapy to best conduct a risk-benefit assessment regarding if (and how long) the antithrombotic therapy should be held (Figure). This shared decision-making, which should also include the patient, may help decrease MPL risk and improve outcomes.
Provider defense mechanisms
Physicians may engage in various defensive behaviors in an attempt to mitigate MPL risk; however, these behaviors may, paradoxically, increase risk.30,31
Assurance behaviors
Assurance behaviors refer to the practice of recommending or performing additional services (such as medications, imaging, procedures, and referrals) that are not clearly indicated.2,30,31 Assurance behaviors are driven by fear of MPL risk and/or missing a potential diagnosis. Recent studies have estimated that more than 50% of gastroenterologists worldwide have performed additional invasive procedures without clear indications, and that nearly one-third of endoscopic procedures annually have questionable indications.30,32 While assurance behaviors may seem likely to decrease MPL risk, overall, they may inadvertently increase AE and MPL risk, as well as health care expenditures.3,30,32
Avoidance behaviors
Avoidance behaviors refer to providers avoiding participation in potentially high-risk clinical interventions (for example, the actual procedures), including those for which they are credentialed/certified proficient.30,31 Two clinical scenarios that illustrate this behavior include the following: An advanced endoscopist credentialed to perform ERCP might refer a “high-risk” elderly patient with cholangitis to another provider to perform said ERCP or for percutaneous transhepatic drainage (in the absence of a clear benefit to such), or a gastroenterologist might refer a patient to interventional gastroenterology for resection of a large polyp even though gastroenterologists are usually proficient in this skill and may feel comfortable performing the resection themselves. Avoidance behaviors are driven by a fear of MPL risk and can have several negative consequences.33 For example, patients may not receive indicated interventions. Additionally, patients may have to wait longer for an intervention because they are referred to another provider, which also increases potential for loss to follow-up.2,30,31 This may be viewed as noncompliance with the standard of care, among other hazards, thereby increasing MPL risk.
Documentation tenets
Thorough documentation can decrease MPL risk, especially since it is often used as legal evidence.16 Documenting, for instance, preprocedure discussion of potential risk of AEs (such as bleeding or perforation) or procedural failure (for example, missed lesions)can protect gastroenterologists (Figure).16 While, as discussed previously, these should be covered in the informed consent process (which itself reduces MPL risk), proof of compliance in providing adequate informed consent must come in the form of documentation that indicates that the process took place and specifically what topics were discussed therein. MPL risk may be further decreased by documenting steps taken during a procedure and anatomic landmarks encountered to offer proof of technical competency and compliance with standards of care (Figure).16,34 In this context, it is worth recalling the adage: “If it’s not documented, it did not occur.”
Curbside consults versus consultation
Also germane here is the topic of whether documentation is needed for “curbside consults.” The uncertainty is, in part, semantic; that is, at what point does a “curbside” become a consultation? A curbside is a general question or query (such as anything that could also be answered by searching the Internet or reference materials) in response to which information is provided; once it involves provision of medical advice for a specific patient (for example, when patient identifiers have been shared or their EHR has been accessed), it constitutes a consultation. Based on these definitions, a curbside need not be documented, whereas a consultation – even if seemingly trivial – should be.
Consideration of language and cultural factors
Language barriers should be considered when the gastroenterologist is communicating with the patient, and such efforts, whenever made, should be documented to best protect against MPL.16,35 These considerations arise not only during the consent process but when obtaining a history, providing postprocedure instructions, and during follow-ups. To this end, 24/7 telephone interpreter services may assist the gastroenterologist (when one is communicating with non–English speakers and is not medically certified in the patient’s native/preferred language) and strengthen trust in the provider-patient relationship.36 Additionally, written materials (such as consent forms, procedural information) in patients’ native/preferred languages should be provided, when available, to enhance patient understanding and participation in care (Figure).35
Challenges posed by telemedicine
The COVID-19 pandemic has rapidly led to more virtual encounters. While increased utilization of telemedicine platforms may make health care more accessible, it does not lessen the clinicians’ duty to patients and may actually expose them to greater MPL risk.18,37,38 Therefore, the provider must be cognizant of two key principles to mitigate MPL risk in the context of telemedicine encounters. First, the same standard of care applies to virtual and in-person encounters.18,37,38 Second, patient privacy and HIPAA regulations are not waived during telemedicine encounters, and breaches of such may result in an MPL claim.18,37,38
With regard to the first principle, for patients who have not been physically examined (such as when a telemedicine visit was substituted for an in-person clinic encounter), gastroenterologists should not overlook requesting timely preprocedure anesthesia consultation or obtaining additional laboratory studies as needed to ensure safety and the same standard of care. Moreover, particularly in the context of pandemic-related decreased procedural capacity, triaging procedures can be especially challenging. Standardized institutional criteria which prioritize certain diagnoses/conditions over others, leaving room for justifiable exceptions, are advisable.
Vicarious liability
“Vicarious liability” is defined as that extending to persons who have not committed a wrong but on whose behalf wrongdoers acted.39 Therefore, gastroenterologists may be liable not only for their own actions but also for those of personnel they supervise (such as fellow trainees and non–physician practitioners).39 Vicarious liability aims to ensure that systemic checks and balances are in place so that, if failure occurs, harm can still be mitigated and/or avoided, as illustrated by Reason’s “Swiss Cheese Model.”40
Conclusion
Any gastroenterologist can experience an MPL claim. Such an experience can be especially stressful and confusing to early-career clinicians, especially if they’re unfamiliar with legal proceedings. Although MPL principles are not often taught in medical school or residency, it is important for gastroenterologists to be informed regarding tenets of MPL and cognizant of clinical situations which have relatively higher MPL risk. This can assuage untoward angst regarding MPL and highlight proactive risk-mitigation strategies. In general, gastroenterologist practices that can mitigate MPL risk include effective communication; adequate informed consent/refusal; documentation of preprocedure counseling, periprocedure events, and postprocedure recommendations; and maintenance of proper certification and privileging.
Dr. Azizian and Dr. Dalai are with the University of California, Los Angeles and the department of medicine at Olive View–UCLA Medical Center, Sylmar, Calif. They are co–first authors of this paper. Dr. Dalai is also with the division of gastroenterology at the University of New Mexico, Albuquerque. Dr. Adams is with the Center for Clinical Management Research in Veterans Affairs Ann Arbor Healthcare System, the division of gastroenterology at the University of Michigan Health System, and the Institute for Healthcare Policy and Innovation, all in Ann Arbor, Mich. Dr. Tabibian is with UCLA and the division of gastroenterology at Olive View–UCLA Medical Center. The authors have no conflicts of interest.
References
1. 2020 Data Sharing Project Gastroenterology 2009-2018. Inside Medical Liability: Second Quarter. Accessed 2020 Dec 6.
2. Mello MM et al. Health Aff (Millwood). 2004 Jul-Aug;23(4):42-53.
3. Adams MA et al. JAMA. 2014 Oct;312(13):1348-9.
4. Pegalis SE. American Law of Medical Malpractice 3d, Vol. 2. St. Paul, Minn.: Thomson Reuters, 2005.
5. Feld LD et al. Am J Gastroenterol. 2018 Nov;113(11):1577-9.
6. Sawyer v. Wight, 196 F. Supp. 2d 220, 226 (E.D.N.Y. 2002).
7. Michael A. Sita v. Long Island Jewish-Hillside Medical Center, 22 A.D.3d 743 (N.Y. App. Div. 2005).
8. Conklin LS et al. Clin Gastroenterol Hepatol. 2008 Jun;6(6):677-81.
9. Jena AB et al. N Engl J Med. 2011 Aug 18;365(7):629-36.
10. Kane CK. “Policy Research Perspectives Medical Liability Claim Frequency: A 2007-2008 Snapshot of Physicians.” Chicago: American Medical Association, 2010.
11. Hernandez LV et al. World J Gastrointest Endosc. 2013 Apr 16;5(4):169-73.
12. Schaffer AC et al. JAMA Intern Med. 2017 May 1;177(5):710-8.
13. Natanson v. Kline, 186 Kan. 393, 409, 350 P.2d 1093, 1106, decision clarified on denial of reh’g, 187 Kan. 186, 354 P.2d 670 (1960).
14. Truman v. Thomas, 27 Cal. 3d 285, 292, 611 P.2d 902, 906 (1980).
15. Shah P et al. Informed Consent, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Aug 22.
16. Rex DK. Clin Gastroenterol Hepatol. 2013 Jul;11(7):768-73.
17. Gerstenberger PD, Plumeri PA. Gastrointest Endosc. Mar-Apr 1993;39(2):132-8.
18. Adams MA and Allen JI. Clin Gastroenterol Hepatol. 2019 Nov;17(12):2392-6.e1.
19. Ahlawat R et al. Esophagogastroduodenoscopy, in “StatPearls.” Treasure Island, Fla.: StatPearls Publishing, 2020 Jan. Updated 2020 Dec 9.
20. Cotton PB. Gastrointest Endosc. 2006 Mar;63(3):378-82.
21. Cotton PB. Gastrointest Endosc. 2010 Oct;72(4):904.
22. Adamson TE et al. West J Med. 1989 Mar;150(3):356-60.
23. Trap R et al. Endoscopy. 1999 Feb;31(2):125-30.
24. Funaki B. Semin Intervent Radiol. 2015 Mar;32(1):61-4.
25. Feeding Tube Nursing Home and Hospital Malpractice. Miller & Zois, Attorneys at Law. Accessed 2020 Jun 20.
26. Medical Malpractice Lawsuit Brings $750,000 Settlement: Death of 82-year-old woman from sepsis due to improper placement of feeding tube. Lubin & Meyers PC. Accessed 2020 Jun 20.
27. Brendel RW et al. Med Clin North Am. 2010 Nov;94(6):1229-40, xi-ii.
28. ASGE Standards of Practice Committee; Acosta RD et al. Gastrointest Endosc. 2016 Jan;83(1):3-16.
29. Saleem S and Thomas AL. Cureus. 2018 Jun 25;10(6):e2878.
30. Hiyama T et al. World J Gastroenterol. 2006 Dec 21;12(47):7671-5.
31. Studdert DM et al. JAMA. 2005 Jun 1;293(21):2609-17.
32. Shaheen NJ et al. Gastroenterology. 2018 May;154(7):1993-2003.
33. Oza VM et al. Clin Gastroenterol Hepatol. 2016 Feb;14(2):172-4.
34. Feld AD. Gastrointest Endosc Clin N Am. 2002 Jan;12(1):171-9, viii-ix.
35. Lee JS et al. J Gen Intern Med. 2017 Aug;32(8):863-70.
36. Forrow L and Kontrimas JC. J Gen Intern Med. 2017 Aug;32(8):855-7.
37. Moses RE et al. Am J Gastroenterol. 2014 Aug;109(8):1128-32.
38. Tabibian JH. “The Evolution of Telehealth.” Guidepoint: Legal Solutions Blog. Accessed 2020 Aug 12.
39. Feld AD. Am J Gastroenterol. 2004 Sep;99(9):1641-4.
40. Reason J. BMJ. 2000;320(7237):768‐70.
Understand the legal implications of telehealth medicine
Telehealth has been steadily gaining mainstream use throughout the last decade, but the practice was recently shoved, almost overnight, into the forefront of the health care profession. Telehealth is now used more frequently by medical groups and physicians than ever before. General reports before the COVID-19 pandemic approximated 90% of health care organizations used or planned to use telehealth in the future. This future may already be a reality, with a McKinsey & Company report estimating that physicians saw 50-175 times more patients over telehealth platforms since the pandemic’s start.1
In general, telehealth includes use of electronic communication and information technologies to deliver long-distance or remote health care. A physician’s use of telemedicine (clinical services) is one of the most common uses, but the industry also includes other professionals, such as pharmacists and nurses.
Telehealth platforms can be used to monitor, diagnose, treat, and counsel patients successfully. It works best for reading images, follow-up care, outpatient care, and long-term care. However, telemedicine is inappropriate for urgent issues, diagnosing underlying health conditions, or any practice where the standard of care would require a physical exam. There is potential liability for decision making without a proper physical exam.
There are many advantages to telehealth over more traditional health care options. Some of these advantages include:
- Increased access to health care.
- Increased access to medical specialists in small and rural communities.
- Improved long-term care from the comfort of patients’ homes.
- Improved platforms to document patient care outside regular business hours.
But along with these benefits, telehealth carries the disadvantage of potential increased liability. This increased liability could stem from:
- Breached standards of care.
- Inadequate or improper licensing.
- Limited care options.
- Decision making without a proper physical exam.
- Increased informed consent requirements.
- Restricted prescription access.
Before expanding any practice into telemedicine, awareness of potential legal issues is crucial.
Standard of care
Currently, telehealth laws and regulations vary significantly from state to state. But one rule is consistent across the board – that the standard of care for practicing medicine through telemedicine is identical to the standard of care required for practicing medicine during physical practice. It still requires the appropriate examination, testing, labs, imaging, and consultations that any in-person diagnosis needs. For physicians, it also includes supervising nonphysician clinicians, where state law requires supervision.
The American Telemedicine Association currently determines the primary governing standards and guidelines for telemedicine. These can help physicians understand best practices in meeting the standard of care through telemedicine. The American Gastroenterological Association provides coding guidelines and other resources to help physicians with telehealth and e-visits. Other professional societies, such as the American College of Radiology and the American Academy of Dermatology, offer guidelines specific to their medical specialties’ standards of care. These standards still vary from state to state, so medical professionals must be aware of any differences before treating patients in multiple states.
Licensing
Licensing is one of telemedicine’s most confusing legal issues. All states require a license to practice medicine (traditional or telehealth) within their borders. Without that license, practicing medicine in the state is a crime. On top of being criminal, unlicensed practice can affect insurance, liability, billing, and malpractice coverage. When in a brick-and-mortar clinic, a physician’s confidence in practicing within the licensed jurisdiction is easy. Now, the distinction is not so clear. Patients and physicians no longer have to be in the same room, city, or even state, meaning there could be unknown conflicting laws between the two locations. With rare exceptions, standards of care are based on the patient’s location, not the physician’s location. This increases the risk of practicing without being correctly licensed to higher than ever.
Because licensing is a significant roadblock in providing telemedicine, efforts are underway to make the process simpler and more streamlined. The Federation of State Medical Boards developed the Interstate Medical Licensure Compact (IMLC).2 This can qualify physicians to practice medicine across state lines within the compact so long as they meet specific eligibility requirements. The IMLC creates a fast-track option for physicians to fill out one application and receive licenses from multiple states at once. Currently, the compact includes 32 states, the District of Columbia, and Guam.3
Informed consent
Telemedicine health care still requires informed consent from patients. In fact, in some states, the requirements for care provided through telehealth are actually stricter than requirements for informed consent obtained in person.
Most informed consent laws require physicians to cover the risks and benefits of a recommended course of treatment and all feasible and reasonable material alternatives. On top of this traditional informed consent, physicians must get additional consent to receive care over a telehealth platform. This unique requirement explains what telehealth is, possible risks and expected benefits, and security measures used to protect patient information. States vary regarding when verbal consent is sufficient, and when written consent is required.
Prescriptions
Telemedicine is still a relatively new industry, and few legal opinions specifically address telemedicine malpractice. However, prescribing medication based on telemedicine information is among the few issues the courts have addressed. A 2008 decision found that a physician review of patient questionnaires submitted over the Internet was insufficient to prescribe medication without a physical examination determining patient health.4 This cautious approach stemmed from telehealth’s early concern about the absence of patient-physician relationships and potential online pharmacy abuse. Since this decision, many states require an “in-person” visit with a patient before prescribing medication. The definition of what qualifies as an in-person visit varies from state to state – some still consider the use of real-time, audiovisual conferencing sufficient.
The law is still evolving for prescriptions. Some states don’t allow any prescriptions, while others allow physicians to prescribe their patients’ medications as part of an appropriate treatment plan according to their professional discretion. Almost every state prohibits the prescription of controlled substances based on telemedicine.
Conclusion
Telemedicine is becoming an increasingly significant part of both physician-patient relationships and the broader health care industry. Used appropriately, it can be an incredibly effective method of care for physicians and patients. Physicians should learn the laws governing telemedicine in every state they want to practice and continue to stay current on any changes. The Center for Connected Health Policy offers a report, updated semiannually, to help physicians stay up to date on their state laws. These efforts will help prevent physicians from exposure to liability and medical malpractice claims.
Mr. Hyde is a partner at Younker Hyde Macfarlane, a law firm that focuses on prosecuting medical malpractice claims on behalf of injured patients. Ms. Johnson is an associate attorney with the firm. You can find them at YHMLaw.com.
References
1. Bestsennyy O, Harris A, Rost J. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? Mckinsey & Company, May 29, 2020.
2. FSMB: Draft Interstate Compact for Physician Licensure Nears Completion, 2014.
3. Interstate Medical Licensure Compact: U.S. State Participation in the Compact.
4. See, Low Cost Pharm., Inc. v. Ariz. State Bd. Of Pharm, 2008 Ariz. App. Unpub. LEXIS 790, referencing conclusion of Arizona Medical Board.
Telehealth has been steadily gaining mainstream use throughout the last decade, but the practice was recently shoved, almost overnight, into the forefront of the health care profession. Telehealth is now used more frequently by medical groups and physicians than ever before. General reports before the COVID-19 pandemic approximated 90% of health care organizations used or planned to use telehealth in the future. This future may already be a reality, with a McKinsey & Company report estimating that physicians saw 50-175 times more patients over telehealth platforms since the pandemic’s start.1
In general, telehealth includes use of electronic communication and information technologies to deliver long-distance or remote health care. A physician’s use of telemedicine (clinical services) is one of the most common uses, but the industry also includes other professionals, such as pharmacists and nurses.
Telehealth platforms can be used to monitor, diagnose, treat, and counsel patients successfully. It works best for reading images, follow-up care, outpatient care, and long-term care. However, telemedicine is inappropriate for urgent issues, diagnosing underlying health conditions, or any practice where the standard of care would require a physical exam. There is potential liability for decision making without a proper physical exam.
There are many advantages to telehealth over more traditional health care options. Some of these advantages include:
- Increased access to health care.
- Increased access to medical specialists in small and rural communities.
- Improved long-term care from the comfort of patients’ homes.
- Improved platforms to document patient care outside regular business hours.
But along with these benefits, telehealth carries the disadvantage of potential increased liability. This increased liability could stem from:
- Breached standards of care.
- Inadequate or improper licensing.
- Limited care options.
- Decision making without a proper physical exam.
- Increased informed consent requirements.
- Restricted prescription access.
Before expanding any practice into telemedicine, awareness of potential legal issues is crucial.
Standard of care
Currently, telehealth laws and regulations vary significantly from state to state. But one rule is consistent across the board – that the standard of care for practicing medicine through telemedicine is identical to the standard of care required for practicing medicine during physical practice. It still requires the appropriate examination, testing, labs, imaging, and consultations that any in-person diagnosis needs. For physicians, it also includes supervising nonphysician clinicians, where state law requires supervision.
The American Telemedicine Association currently determines the primary governing standards and guidelines for telemedicine. These can help physicians understand best practices in meeting the standard of care through telemedicine. The American Gastroenterological Association provides coding guidelines and other resources to help physicians with telehealth and e-visits. Other professional societies, such as the American College of Radiology and the American Academy of Dermatology, offer guidelines specific to their medical specialties’ standards of care. These standards still vary from state to state, so medical professionals must be aware of any differences before treating patients in multiple states.
Licensing
Licensing is one of telemedicine’s most confusing legal issues. All states require a license to practice medicine (traditional or telehealth) within their borders. Without that license, practicing medicine in the state is a crime. On top of being criminal, unlicensed practice can affect insurance, liability, billing, and malpractice coverage. When in a brick-and-mortar clinic, a physician’s confidence in practicing within the licensed jurisdiction is easy. Now, the distinction is not so clear. Patients and physicians no longer have to be in the same room, city, or even state, meaning there could be unknown conflicting laws between the two locations. With rare exceptions, standards of care are based on the patient’s location, not the physician’s location. This increases the risk of practicing without being correctly licensed to higher than ever.
Because licensing is a significant roadblock in providing telemedicine, efforts are underway to make the process simpler and more streamlined. The Federation of State Medical Boards developed the Interstate Medical Licensure Compact (IMLC).2 This can qualify physicians to practice medicine across state lines within the compact so long as they meet specific eligibility requirements. The IMLC creates a fast-track option for physicians to fill out one application and receive licenses from multiple states at once. Currently, the compact includes 32 states, the District of Columbia, and Guam.3
Informed consent
Telemedicine health care still requires informed consent from patients. In fact, in some states, the requirements for care provided through telehealth are actually stricter than requirements for informed consent obtained in person.
Most informed consent laws require physicians to cover the risks and benefits of a recommended course of treatment and all feasible and reasonable material alternatives. On top of this traditional informed consent, physicians must get additional consent to receive care over a telehealth platform. This unique requirement explains what telehealth is, possible risks and expected benefits, and security measures used to protect patient information. States vary regarding when verbal consent is sufficient, and when written consent is required.
Prescriptions
Telemedicine is still a relatively new industry, and few legal opinions specifically address telemedicine malpractice. However, prescribing medication based on telemedicine information is among the few issues the courts have addressed. A 2008 decision found that a physician review of patient questionnaires submitted over the Internet was insufficient to prescribe medication without a physical examination determining patient health.4 This cautious approach stemmed from telehealth’s early concern about the absence of patient-physician relationships and potential online pharmacy abuse. Since this decision, many states require an “in-person” visit with a patient before prescribing medication. The definition of what qualifies as an in-person visit varies from state to state – some still consider the use of real-time, audiovisual conferencing sufficient.
The law is still evolving for prescriptions. Some states don’t allow any prescriptions, while others allow physicians to prescribe their patients’ medications as part of an appropriate treatment plan according to their professional discretion. Almost every state prohibits the prescription of controlled substances based on telemedicine.
Conclusion
Telemedicine is becoming an increasingly significant part of both physician-patient relationships and the broader health care industry. Used appropriately, it can be an incredibly effective method of care for physicians and patients. Physicians should learn the laws governing telemedicine in every state they want to practice and continue to stay current on any changes. The Center for Connected Health Policy offers a report, updated semiannually, to help physicians stay up to date on their state laws. These efforts will help prevent physicians from exposure to liability and medical malpractice claims.
Mr. Hyde is a partner at Younker Hyde Macfarlane, a law firm that focuses on prosecuting medical malpractice claims on behalf of injured patients. Ms. Johnson is an associate attorney with the firm. You can find them at YHMLaw.com.
References
1. Bestsennyy O, Harris A, Rost J. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? Mckinsey & Company, May 29, 2020.
2. FSMB: Draft Interstate Compact for Physician Licensure Nears Completion, 2014.
3. Interstate Medical Licensure Compact: U.S. State Participation in the Compact.
4. See, Low Cost Pharm., Inc. v. Ariz. State Bd. Of Pharm, 2008 Ariz. App. Unpub. LEXIS 790, referencing conclusion of Arizona Medical Board.
Telehealth has been steadily gaining mainstream use throughout the last decade, but the practice was recently shoved, almost overnight, into the forefront of the health care profession. Telehealth is now used more frequently by medical groups and physicians than ever before. General reports before the COVID-19 pandemic approximated 90% of health care organizations used or planned to use telehealth in the future. This future may already be a reality, with a McKinsey & Company report estimating that physicians saw 50-175 times more patients over telehealth platforms since the pandemic’s start.1
In general, telehealth includes use of electronic communication and information technologies to deliver long-distance or remote health care. A physician’s use of telemedicine (clinical services) is one of the most common uses, but the industry also includes other professionals, such as pharmacists and nurses.
Telehealth platforms can be used to monitor, diagnose, treat, and counsel patients successfully. It works best for reading images, follow-up care, outpatient care, and long-term care. However, telemedicine is inappropriate for urgent issues, diagnosing underlying health conditions, or any practice where the standard of care would require a physical exam. There is potential liability for decision making without a proper physical exam.
There are many advantages to telehealth over more traditional health care options. Some of these advantages include:
- Increased access to health care.
- Increased access to medical specialists in small and rural communities.
- Improved long-term care from the comfort of patients’ homes.
- Improved platforms to document patient care outside regular business hours.
But along with these benefits, telehealth carries the disadvantage of potential increased liability. This increased liability could stem from:
- Breached standards of care.
- Inadequate or improper licensing.
- Limited care options.
- Decision making without a proper physical exam.
- Increased informed consent requirements.
- Restricted prescription access.
Before expanding any practice into telemedicine, awareness of potential legal issues is crucial.
Standard of care
Currently, telehealth laws and regulations vary significantly from state to state. But one rule is consistent across the board – that the standard of care for practicing medicine through telemedicine is identical to the standard of care required for practicing medicine during physical practice. It still requires the appropriate examination, testing, labs, imaging, and consultations that any in-person diagnosis needs. For physicians, it also includes supervising nonphysician clinicians, where state law requires supervision.
The American Telemedicine Association currently determines the primary governing standards and guidelines for telemedicine. These can help physicians understand best practices in meeting the standard of care through telemedicine. The American Gastroenterological Association provides coding guidelines and other resources to help physicians with telehealth and e-visits. Other professional societies, such as the American College of Radiology and the American Academy of Dermatology, offer guidelines specific to their medical specialties’ standards of care. These standards still vary from state to state, so medical professionals must be aware of any differences before treating patients in multiple states.
Licensing
Licensing is one of telemedicine’s most confusing legal issues. All states require a license to practice medicine (traditional or telehealth) within their borders. Without that license, practicing medicine in the state is a crime. On top of being criminal, unlicensed practice can affect insurance, liability, billing, and malpractice coverage. When in a brick-and-mortar clinic, a physician’s confidence in practicing within the licensed jurisdiction is easy. Now, the distinction is not so clear. Patients and physicians no longer have to be in the same room, city, or even state, meaning there could be unknown conflicting laws between the two locations. With rare exceptions, standards of care are based on the patient’s location, not the physician’s location. This increases the risk of practicing without being correctly licensed to higher than ever.
Because licensing is a significant roadblock in providing telemedicine, efforts are underway to make the process simpler and more streamlined. The Federation of State Medical Boards developed the Interstate Medical Licensure Compact (IMLC).2 This can qualify physicians to practice medicine across state lines within the compact so long as they meet specific eligibility requirements. The IMLC creates a fast-track option for physicians to fill out one application and receive licenses from multiple states at once. Currently, the compact includes 32 states, the District of Columbia, and Guam.3
Informed consent
Telemedicine health care still requires informed consent from patients. In fact, in some states, the requirements for care provided through telehealth are actually stricter than requirements for informed consent obtained in person.
Most informed consent laws require physicians to cover the risks and benefits of a recommended course of treatment and all feasible and reasonable material alternatives. On top of this traditional informed consent, physicians must get additional consent to receive care over a telehealth platform. This unique requirement explains what telehealth is, possible risks and expected benefits, and security measures used to protect patient information. States vary regarding when verbal consent is sufficient, and when written consent is required.
Prescriptions
Telemedicine is still a relatively new industry, and few legal opinions specifically address telemedicine malpractice. However, prescribing medication based on telemedicine information is among the few issues the courts have addressed. A 2008 decision found that a physician review of patient questionnaires submitted over the Internet was insufficient to prescribe medication without a physical examination determining patient health.4 This cautious approach stemmed from telehealth’s early concern about the absence of patient-physician relationships and potential online pharmacy abuse. Since this decision, many states require an “in-person” visit with a patient before prescribing medication. The definition of what qualifies as an in-person visit varies from state to state – some still consider the use of real-time, audiovisual conferencing sufficient.
The law is still evolving for prescriptions. Some states don’t allow any prescriptions, while others allow physicians to prescribe their patients’ medications as part of an appropriate treatment plan according to their professional discretion. Almost every state prohibits the prescription of controlled substances based on telemedicine.
Conclusion
Telemedicine is becoming an increasingly significant part of both physician-patient relationships and the broader health care industry. Used appropriately, it can be an incredibly effective method of care for physicians and patients. Physicians should learn the laws governing telemedicine in every state they want to practice and continue to stay current on any changes. The Center for Connected Health Policy offers a report, updated semiannually, to help physicians stay up to date on their state laws. These efforts will help prevent physicians from exposure to liability and medical malpractice claims.
Mr. Hyde is a partner at Younker Hyde Macfarlane, a law firm that focuses on prosecuting medical malpractice claims on behalf of injured patients. Ms. Johnson is an associate attorney with the firm. You can find them at YHMLaw.com.
References
1. Bestsennyy O, Harris A, Rost J. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? Mckinsey & Company, May 29, 2020.
2. FSMB: Draft Interstate Compact for Physician Licensure Nears Completion, 2014.
3. Interstate Medical Licensure Compact: U.S. State Participation in the Compact.
4. See, Low Cost Pharm., Inc. v. Ariz. State Bd. Of Pharm, 2008 Ariz. App. Unpub. LEXIS 790, referencing conclusion of Arizona Medical Board.
Staying financially well in the time of COVID-19
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.
As COVID-19 continues to threaten the United States and the world, individuals in every profession have been challenged to examine their financial situation. At Fidelity Investments, we recently conducted a national survey asking people how current events have affected their opinions and behaviors when it comes to their money. The results showed that six in 10 Americans are concerned about household finances over the next 6 months. Unfortunately, we’ve seen that even health care professionals have not been financially spared, with salaries or benefits cut or, worse, furloughs and layoffs as hospital systems struggle. I work with many physicians, including gastroenterologists, in my role as a wealth planner for Fidelity Investments and have received quite a few questions related to shoring up family finances during these difficult times.
Luckily, the financial best practices that I share in “good” times ring true even in today’s world, with a few additions given the health and economic risks created by COVID-19.
1. Review your budget. It’s one thing to know that your budget is generally balanced (the dollars you spend are less than the dollars you earn). But it’s worth taking a closer look to see just where those dollars are going. In times of uncertainty, cutting back on expenses that aren’t necessary or don’t provide meaningful value to your life can be worthwhile. If you or your family have lost income because of the pandemic, you might consider these seven simple tips to help boost your cash flow.
2. Tackle (or find relief from) student loan debt. Doctors today graduate medical school with a median debt of just under $195,000.1 Repaying these loans is daunting, particularly during the COVID-19 crisis. The recent passing of the CARES Act recognizes these difficult times: in fact, it automatically suspended required minimum loan payments and interest accrual on federal student loans until Sept. 30, 2020. This only applies to federal student loans, not private student loans. Beyond this period, if you are still struggling with payments, you may explore the possibility of refinancing, by taking out a lower-interest private loan and using that to pay off student loans (although this may extend the life of your loan). Borrowers could also consider other programs, such as REPAYE (Revised Pay As You Earn) through which your monthly payment tops out at 10% of your monthly income, or Public Service Loan Forgiveness (PSLF) if you work for a not-for-profit hospital or other qualifying employer. This program forgives the remaining balance on your direct loans after you have made 120 qualifying monthly payments while working full-time for a qualifying employer.
Additionally, borrowers could look for opportunities to reduce accrued interest, either by refinancing to a lower rate or making payments every 2 weeks rather than once each month.
3. Evaluate your emergency fund. It’s a good idea to keep 3-6 months’ of essential expenses in cash or cash-like investments. If you don’t yet have this 3- to 6-month cushion saved, now is a good time to work to reduce your expenses and stash away any extra cash.
4. Save early and often for retirement. You can borrow money to support many of life’s needs, from housing, to cars, to college. But you can’t borrow for retirement. That is why I encourage clients to put retirement savings at the top of the list, after accounting for day-to-day needs of their families. People often ask me whether it makes sense to continue saving for retirement, often a far-off goal for younger doctors, especially in these uncertain times. My answer? Yes. If you are able to save, continue to save: the earlier you begin to make contributions to your retirement account, and the longer you continue to do so, the more your retirement account(s) have the potential to grow over time.
Another question I receive is whether to take distributions from a retirement account early if you find yourself in a precarious financial situation because of the COVID-19 crisis. The CARES Act provides options allowing Americans to take a withdrawal or loan from a participating retirement plan if you, your spouse, or your dependent have a COVID-19 related illness or you’re experiencing a loss of income related to the COVID-19 pandemic. Try to look at alternative sources of income before tapping your hard-earned retirement savings. If you can find a way to continue saving and avoid drawing down your retirement accounts, your future self will thank you.
5. If you have a high-deductible health plan that offers it, explore a Health Savings Account (HSA). One of the most important factors in a solid financial plan is knowing how to pay for health care expenses, both now and as we age. HSAs are a tax-advantaged account that can be used to save money for qualified medical expenses. They are considered to provide a “triple-tax advantage” since contributions, qualified withdrawals, and investment growth are all tax-free.2 The dollars in these accounts can stay there over time, so in years with low expenses you could use these to save for health care in retirement, while in other years they can be used to pay necessary medical bills. HSAs require the participant to be enrolled in a high-deductible health plan, so you would first need to verify that your employer provides this option.
6. Be prepared to protect yourself, your practice, and your family. Typically, I encourage the medical professionals I work with to review their current insurance plans (such as disability, life, and malpractice) to determine whether they have the right levels of coverage for their situation. With COVID-19 layered on top of the usual level of risk, it’s important to consider reviewing or updating other key elements of your family’s plan, like your health care proxies and a living will.
7. Put your income to work. When your disposable income grows, and you’ve covered all of the foundational elements of a financial plan (a rainy-day fund, contingency planning for health care costs, and so on), it might be the right time to consider investing for something other than retirement. As you do that, be sure you are invested in a diversified strategy with a balance of risk and return that is comfortable for you.
Recent market volatility can bring nerves that make it difficult to stay invested. However, as long as your risk tolerance and time horizon reflect your asset allocation – the mix of stock, bonds, and cash (which a financial planner can help with) – you can take comfort in knowing that historically every severe downturn has eventually given way to further growth.
During uncertain times like these, I think the best guidance is to focus on what you can control. The considerations above are a great place to start building a financial plan to solidify you and your family’s future. A Fidelity survey found that 44% of Americans are now working to build up their emergency savings, and one-third (34%) are rethinking how they manage their money because of the COVID-19 crisis.3 Despite the stresses we all face, there is no time like the present to start or revisit your financial plan.
Footnotes
1. Barron D. Why Doctors Are Drowning in Medical School Debt. Scientific American. July 15, 2019.
2. With respect to federal taxation only. Contributions, investment earnings, and distributions may or may not be subject to state taxation. The triple tax advantages are only applicable if the money is used to pay for qualified medical expenses as described in IRS Publication 969.
3. Fidelity Market Sentiment Study presents the findings of a nationwide online survey consisting of 3,012 adults, at least 18 years of age, from which 1,591 respondents qualified as having at least one investment account. The study was fielded April 1-8, 2020, by ENGINE INSIGHTS, an independent research firm not affiliated with Fidelity Investments. The results of this survey may not be representative of all adults meeting the same criteria as those surveyed for this study. For the purposes of this study, the generations are defined as follows: Millennials (aged 24-39 years); Generation X (aged 40-55 years); Baby Boomers (aged 56-74 years).
Mr. Tudor is Vice President, Wealth Planning Consultant at Fidelity Investments.