User login
COMMENT & CONTROVERSY
Medical library access
During most of my clinical career I had an affiliation with a local medical school as a “Clinical Instructor” and then “Assistant Clinical Professor.” In addition to teaching medical students and residents from that institution that rotated through my hospital, it also gave me certain privileges, the most important of which was access to that institution’s electronic medical library. Using that access, even as an “LMD,” I have been able to contribute to the medical literature on subjects of interest to me and to others in my specialty.
Recently, now as an older clinician, I gave up my hospital privileges, although I continue my office practice. Giving up my hospital privileges meant that I no longer qualified as a faculty member—and therefore lost online access to the medical library. Still wishing to continue my medical writing, I have attempted to attain access to the medical literature by special request to that library, by contacting my state medical society, by contacting my national specialty organization, by contacting the department chair at the institution to which I had been affiliated, and by calling the Dean of the medical school to which my hospital was affiliated. Although meaning well, none was able to get me access to an online medical library. Thus, I am greatly hampered in my attempts to do research and to continue to write further papers on those areas in which I have previously published.
Is there no remedy for this? Should all clinicians who “age out” of institutional affiliations no longer be able to pursue research interests? And what about community physicians who have no academic affiliations? Can they not access the latest information they need to practice evidence-based, up-to-date medicine?
It makes no sense to me that access to the latest and most current aspects of medical care should be withheld from any clinician. For every clinician not to have access to such medical knowledge does a disservice to all those practicing medicine who wish to keep up to date and to all patients of American clinicians whose providers are prevented from practicing the best, evidence-based care.
Henry Lerner, MD
Boston, Massachusetts
Medical library access
During most of my clinical career I had an affiliation with a local medical school as a “Clinical Instructor” and then “Assistant Clinical Professor.” In addition to teaching medical students and residents from that institution that rotated through my hospital, it also gave me certain privileges, the most important of which was access to that institution’s electronic medical library. Using that access, even as an “LMD,” I have been able to contribute to the medical literature on subjects of interest to me and to others in my specialty.
Recently, now as an older clinician, I gave up my hospital privileges, although I continue my office practice. Giving up my hospital privileges meant that I no longer qualified as a faculty member—and therefore lost online access to the medical library. Still wishing to continue my medical writing, I have attempted to attain access to the medical literature by special request to that library, by contacting my state medical society, by contacting my national specialty organization, by contacting the department chair at the institution to which I had been affiliated, and by calling the Dean of the medical school to which my hospital was affiliated. Although meaning well, none was able to get me access to an online medical library. Thus, I am greatly hampered in my attempts to do research and to continue to write further papers on those areas in which I have previously published.
Is there no remedy for this? Should all clinicians who “age out” of institutional affiliations no longer be able to pursue research interests? And what about community physicians who have no academic affiliations? Can they not access the latest information they need to practice evidence-based, up-to-date medicine?
It makes no sense to me that access to the latest and most current aspects of medical care should be withheld from any clinician. For every clinician not to have access to such medical knowledge does a disservice to all those practicing medicine who wish to keep up to date and to all patients of American clinicians whose providers are prevented from practicing the best, evidence-based care.
Henry Lerner, MD
Boston, Massachusetts
Medical library access
During most of my clinical career I had an affiliation with a local medical school as a “Clinical Instructor” and then “Assistant Clinical Professor.” In addition to teaching medical students and residents from that institution that rotated through my hospital, it also gave me certain privileges, the most important of which was access to that institution’s electronic medical library. Using that access, even as an “LMD,” I have been able to contribute to the medical literature on subjects of interest to me and to others in my specialty.
Recently, now as an older clinician, I gave up my hospital privileges, although I continue my office practice. Giving up my hospital privileges meant that I no longer qualified as a faculty member—and therefore lost online access to the medical library. Still wishing to continue my medical writing, I have attempted to attain access to the medical literature by special request to that library, by contacting my state medical society, by contacting my national specialty organization, by contacting the department chair at the institution to which I had been affiliated, and by calling the Dean of the medical school to which my hospital was affiliated. Although meaning well, none was able to get me access to an online medical library. Thus, I am greatly hampered in my attempts to do research and to continue to write further papers on those areas in which I have previously published.
Is there no remedy for this? Should all clinicians who “age out” of institutional affiliations no longer be able to pursue research interests? And what about community physicians who have no academic affiliations? Can they not access the latest information they need to practice evidence-based, up-to-date medicine?
It makes no sense to me that access to the latest and most current aspects of medical care should be withheld from any clinician. For every clinician not to have access to such medical knowledge does a disservice to all those practicing medicine who wish to keep up to date and to all patients of American clinicians whose providers are prevented from practicing the best, evidence-based care.
Henry Lerner, MD
Boston, Massachusetts
Comment & Controversy
Drospirenone vs norethindrone progestin-only pills. Is there a clear winner?
ROBERT L. BARBIERI, MD (FEBRUARY 2022)
Contraception queries
Dr. Barbieri, addressing your editorial on drospirenone and norethindrone pills, can you tell me why there are 4 placebo pills in Slynd? In addition, why did Exeltis choose a 24/4 regimen instead of a continuous regimen? And are there data on bleeding patterns with continuous drospirenone versus 24/4?
Meredith S. Cassidy, MD
Colorado Springs, Colorado
Dr. Barbieri responds
I thank Dr. Cassidy for the excellent question! The purpose of the 4 placebo pills in the Slynd (drospirenone 4 mg) 24/4 progestin-only contraceptive is to induce scheduled bleeding and reduce the number of days of unscheduled uterine bleeding. In a study of 858 patients, compared with a continuous progestin-only desogestrel contraceptive, Slynd with 4 placebo pills, was associated with significantly fewer days of unscheduled bleeding, 22 days versus 35 days (P<.0003) over 8 months of contraceptive use.1
The norethindrone progestin-only pill (POP) , which is available in the United States has very weak anti-ovulatory properties. If there were 4 placebo pills in the norethindrone POP, ovulation rates would increase, leading to reduced contraceptive efficacy. In contrast, Slynd with 4 placebo pills has excellent anti-ovulatory efficacy.
Reference
1. Palacios S, Colli E, Regidor PA. Bleeding profile of women using a drospirenone-ony 4 mg over nine cycles in comparison with desogestrel 0.075 mg. PLoS ONE. 2020;15:e0231856.
Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?
ROBERT L. BARBIERI, MD (NOVEMBER 2022)
ERAS for all cesarean deliveries
In Dr. Barbieri’s editorial “Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?”, he and Dr. Schantz-Dunn outline several reasons why the answer is a resounding, “Yes!”
I would suggest that ERAS principles should be used for all cesarean deliveries (CDs), not only scheduled ones. Many components of CD ERAS pathways are equally applicable to scheduled and unscheduled CDs, specifically those components that apply to intraoperative care (antibiotic prophylaxis, skin preparation, surgical technique, uterotonic administration, normothermia, and multimodal anesthesia) and postoperative care (VTE prophylaxis, gum chewing, early oral intake, early ambulation, early removal of bladder catheter, predischarge patient education, scheduled analgesic prophylaxis with acetaminophen, and NSAIDS). Although scheduled CDs have the additional advantage of the pre-hospital components (breastfeeding education, shortened fasting interval, carbohydrate loading, anemia prevention, and physiologic optimization), most of the benefit of ERAS for CD is likely attributable to the intraoperative and postoperative components.
For example, in our CD ERAS program, the median postoperative opioid consumption was reduced from a baseline of more than 100 morphine mg equivalents (MME) in both scheduled CDs (23 MME, interquartile range [IQR], 0-70) and unscheduled CDs (23 MME, IQR, 0-75).1 Remarkably, 29% of patients in the ERAS pathway used no postoperative opioids at all, a testament to the efficacy of neuraxial morphine and postoperative acetaminophen and NSAIDS. In another program, ERAS was associated with decreased postpartum length of stay and reduced direct costs in both scheduled and unscheduled CDs.2
References
- Combs CA, Robinson T, Mekis C, et al. Enhanced recovery after cesarean: impact on postoperative opioid use and length of stay. Am J Obstet Gynecol. 2021;224:237-239.
- Fay EE, Hitti JE, Delgado CM, et al. An enhanced recovery after surgery pathway for cesarean delivery decreases hospital stay and cost. Am J Obstet Gynecol. 2019;221:349.e1-e9.
C. Andrew Combs, MD, PhD
Sunrise, Florida
Dr. Barbieri responds
I am grateful to Dr. Combs’ advocacy for applying ERAS principles to all CD births, including scheduled and unscheduled operations. Dr. Combs notes that the intraoperative and postoperative components of ERAS can be used for both scheduled and unscheduled CD births. Of particular note is the marked reduction in opioid medication use achieved among Dr. Combs’ patients who were on an ERAS pathway. Hopefully, due to Dr. Combs clinical and research leadership many more patients will benefit from the use of an ERAS pathway.
ObGyns united in a divided post-Dobbs America
ERIN TRACY BRADLEY, MD, MPH, AND MEGAN L. EVANS,MD, MPH (DECEMBER 2022)
ObGyns are not united on this issue
I just finished reading the article by Drs. Bradley and Evans in the December edition of
The unborn seem not to have advocates like Drs. Bradley and Evans. In fact, those who hold pro-life opinions are regularly silenced in publications and on social media. The Facebooks and Twitters of the world tend to hold us in derision when they are not silencing us. There used to be a detente in our field where we each respected the viewpoint of the other, but now it is nonstop advocacy for abortion. Some authors want to accelerate and intensify that advocacy. I suspect that the pro-life views like mine will continue to be silenced. I just want the authors to know that we are not united in this post-Dobbs world. Many of us want appropriate limits on termination. We are not in favor of the unlimited right to abort a fetus up to the moment of delivery.
Steven G. Nelson
Phoenix, Arizona
Drospirenone vs norethindrone progestin-only pills. Is there a clear winner?
ROBERT L. BARBIERI, MD (FEBRUARY 2022)
Contraception queries
Dr. Barbieri, addressing your editorial on drospirenone and norethindrone pills, can you tell me why there are 4 placebo pills in Slynd? In addition, why did Exeltis choose a 24/4 regimen instead of a continuous regimen? And are there data on bleeding patterns with continuous drospirenone versus 24/4?
Meredith S. Cassidy, MD
Colorado Springs, Colorado
Dr. Barbieri responds
I thank Dr. Cassidy for the excellent question! The purpose of the 4 placebo pills in the Slynd (drospirenone 4 mg) 24/4 progestin-only contraceptive is to induce scheduled bleeding and reduce the number of days of unscheduled uterine bleeding. In a study of 858 patients, compared with a continuous progestin-only desogestrel contraceptive, Slynd with 4 placebo pills, was associated with significantly fewer days of unscheduled bleeding, 22 days versus 35 days (P<.0003) over 8 months of contraceptive use.1
The norethindrone progestin-only pill (POP) , which is available in the United States has very weak anti-ovulatory properties. If there were 4 placebo pills in the norethindrone POP, ovulation rates would increase, leading to reduced contraceptive efficacy. In contrast, Slynd with 4 placebo pills has excellent anti-ovulatory efficacy.
Reference
1. Palacios S, Colli E, Regidor PA. Bleeding profile of women using a drospirenone-ony 4 mg over nine cycles in comparison with desogestrel 0.075 mg. PLoS ONE. 2020;15:e0231856.
Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?
ROBERT L. BARBIERI, MD (NOVEMBER 2022)
ERAS for all cesarean deliveries
In Dr. Barbieri’s editorial “Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?”, he and Dr. Schantz-Dunn outline several reasons why the answer is a resounding, “Yes!”
I would suggest that ERAS principles should be used for all cesarean deliveries (CDs), not only scheduled ones. Many components of CD ERAS pathways are equally applicable to scheduled and unscheduled CDs, specifically those components that apply to intraoperative care (antibiotic prophylaxis, skin preparation, surgical technique, uterotonic administration, normothermia, and multimodal anesthesia) and postoperative care (VTE prophylaxis, gum chewing, early oral intake, early ambulation, early removal of bladder catheter, predischarge patient education, scheduled analgesic prophylaxis with acetaminophen, and NSAIDS). Although scheduled CDs have the additional advantage of the pre-hospital components (breastfeeding education, shortened fasting interval, carbohydrate loading, anemia prevention, and physiologic optimization), most of the benefit of ERAS for CD is likely attributable to the intraoperative and postoperative components.
For example, in our CD ERAS program, the median postoperative opioid consumption was reduced from a baseline of more than 100 morphine mg equivalents (MME) in both scheduled CDs (23 MME, interquartile range [IQR], 0-70) and unscheduled CDs (23 MME, IQR, 0-75).1 Remarkably, 29% of patients in the ERAS pathway used no postoperative opioids at all, a testament to the efficacy of neuraxial morphine and postoperative acetaminophen and NSAIDS. In another program, ERAS was associated with decreased postpartum length of stay and reduced direct costs in both scheduled and unscheduled CDs.2
References
- Combs CA, Robinson T, Mekis C, et al. Enhanced recovery after cesarean: impact on postoperative opioid use and length of stay. Am J Obstet Gynecol. 2021;224:237-239.
- Fay EE, Hitti JE, Delgado CM, et al. An enhanced recovery after surgery pathway for cesarean delivery decreases hospital stay and cost. Am J Obstet Gynecol. 2019;221:349.e1-e9.
C. Andrew Combs, MD, PhD
Sunrise, Florida
Dr. Barbieri responds
I am grateful to Dr. Combs’ advocacy for applying ERAS principles to all CD births, including scheduled and unscheduled operations. Dr. Combs notes that the intraoperative and postoperative components of ERAS can be used for both scheduled and unscheduled CD births. Of particular note is the marked reduction in opioid medication use achieved among Dr. Combs’ patients who were on an ERAS pathway. Hopefully, due to Dr. Combs clinical and research leadership many more patients will benefit from the use of an ERAS pathway.
ObGyns united in a divided post-Dobbs America
ERIN TRACY BRADLEY, MD, MPH, AND MEGAN L. EVANS,MD, MPH (DECEMBER 2022)
ObGyns are not united on this issue
I just finished reading the article by Drs. Bradley and Evans in the December edition of
The unborn seem not to have advocates like Drs. Bradley and Evans. In fact, those who hold pro-life opinions are regularly silenced in publications and on social media. The Facebooks and Twitters of the world tend to hold us in derision when they are not silencing us. There used to be a detente in our field where we each respected the viewpoint of the other, but now it is nonstop advocacy for abortion. Some authors want to accelerate and intensify that advocacy. I suspect that the pro-life views like mine will continue to be silenced. I just want the authors to know that we are not united in this post-Dobbs world. Many of us want appropriate limits on termination. We are not in favor of the unlimited right to abort a fetus up to the moment of delivery.
Steven G. Nelson
Phoenix, Arizona
Drospirenone vs norethindrone progestin-only pills. Is there a clear winner?
ROBERT L. BARBIERI, MD (FEBRUARY 2022)
Contraception queries
Dr. Barbieri, addressing your editorial on drospirenone and norethindrone pills, can you tell me why there are 4 placebo pills in Slynd? In addition, why did Exeltis choose a 24/4 regimen instead of a continuous regimen? And are there data on bleeding patterns with continuous drospirenone versus 24/4?
Meredith S. Cassidy, MD
Colorado Springs, Colorado
Dr. Barbieri responds
I thank Dr. Cassidy for the excellent question! The purpose of the 4 placebo pills in the Slynd (drospirenone 4 mg) 24/4 progestin-only contraceptive is to induce scheduled bleeding and reduce the number of days of unscheduled uterine bleeding. In a study of 858 patients, compared with a continuous progestin-only desogestrel contraceptive, Slynd with 4 placebo pills, was associated with significantly fewer days of unscheduled bleeding, 22 days versus 35 days (P<.0003) over 8 months of contraceptive use.1
The norethindrone progestin-only pill (POP) , which is available in the United States has very weak anti-ovulatory properties. If there were 4 placebo pills in the norethindrone POP, ovulation rates would increase, leading to reduced contraceptive efficacy. In contrast, Slynd with 4 placebo pills has excellent anti-ovulatory efficacy.
Reference
1. Palacios S, Colli E, Regidor PA. Bleeding profile of women using a drospirenone-ony 4 mg over nine cycles in comparison with desogestrel 0.075 mg. PLoS ONE. 2020;15:e0231856.
Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?
ROBERT L. BARBIERI, MD (NOVEMBER 2022)
ERAS for all cesarean deliveries
In Dr. Barbieri’s editorial “Should every scheduled cesarean birth use an Enhanced Recovery After Surgery (ERAS) pathway?”, he and Dr. Schantz-Dunn outline several reasons why the answer is a resounding, “Yes!”
I would suggest that ERAS principles should be used for all cesarean deliveries (CDs), not only scheduled ones. Many components of CD ERAS pathways are equally applicable to scheduled and unscheduled CDs, specifically those components that apply to intraoperative care (antibiotic prophylaxis, skin preparation, surgical technique, uterotonic administration, normothermia, and multimodal anesthesia) and postoperative care (VTE prophylaxis, gum chewing, early oral intake, early ambulation, early removal of bladder catheter, predischarge patient education, scheduled analgesic prophylaxis with acetaminophen, and NSAIDS). Although scheduled CDs have the additional advantage of the pre-hospital components (breastfeeding education, shortened fasting interval, carbohydrate loading, anemia prevention, and physiologic optimization), most of the benefit of ERAS for CD is likely attributable to the intraoperative and postoperative components.
For example, in our CD ERAS program, the median postoperative opioid consumption was reduced from a baseline of more than 100 morphine mg equivalents (MME) in both scheduled CDs (23 MME, interquartile range [IQR], 0-70) and unscheduled CDs (23 MME, IQR, 0-75).1 Remarkably, 29% of patients in the ERAS pathway used no postoperative opioids at all, a testament to the efficacy of neuraxial morphine and postoperative acetaminophen and NSAIDS. In another program, ERAS was associated with decreased postpartum length of stay and reduced direct costs in both scheduled and unscheduled CDs.2
References
- Combs CA, Robinson T, Mekis C, et al. Enhanced recovery after cesarean: impact on postoperative opioid use and length of stay. Am J Obstet Gynecol. 2021;224:237-239.
- Fay EE, Hitti JE, Delgado CM, et al. An enhanced recovery after surgery pathway for cesarean delivery decreases hospital stay and cost. Am J Obstet Gynecol. 2019;221:349.e1-e9.
C. Andrew Combs, MD, PhD
Sunrise, Florida
Dr. Barbieri responds
I am grateful to Dr. Combs’ advocacy for applying ERAS principles to all CD births, including scheduled and unscheduled operations. Dr. Combs notes that the intraoperative and postoperative components of ERAS can be used for both scheduled and unscheduled CD births. Of particular note is the marked reduction in opioid medication use achieved among Dr. Combs’ patients who were on an ERAS pathway. Hopefully, due to Dr. Combs clinical and research leadership many more patients will benefit from the use of an ERAS pathway.
ObGyns united in a divided post-Dobbs America
ERIN TRACY BRADLEY, MD, MPH, AND MEGAN L. EVANS,MD, MPH (DECEMBER 2022)
ObGyns are not united on this issue
I just finished reading the article by Drs. Bradley and Evans in the December edition of
The unborn seem not to have advocates like Drs. Bradley and Evans. In fact, those who hold pro-life opinions are regularly silenced in publications and on social media. The Facebooks and Twitters of the world tend to hold us in derision when they are not silencing us. There used to be a detente in our field where we each respected the viewpoint of the other, but now it is nonstop advocacy for abortion. Some authors want to accelerate and intensify that advocacy. I suspect that the pro-life views like mine will continue to be silenced. I just want the authors to know that we are not united in this post-Dobbs world. Many of us want appropriate limits on termination. We are not in favor of the unlimited right to abort a fetus up to the moment of delivery.
Steven G. Nelson
Phoenix, Arizona
COMMENT & CONTROVERSY
Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes?
JAIMEY M. PAULI, MD (JUNE 2022)
Consider this, when it comes to treating chronic hypertension
I welcome the article by Dr. Jaimey Pauli, which focuses on initiating treatment for mild chronic hypertension in pregnancy to reach a goal blood pressure (BP) of <140/90 mm Hg to prevent adverse maternal and fetal outcomes.1 I would like to offer 3 additional thoughts for your consideration. First, it is known that there is a physiological decrease in BP during the second trimester, which results in a normotensive presentation. Thus, it would be beneficial to see if pregnant women with high-normal BP levels before the third trimester be administered a lower dose of antihypertensives. However, there is also a concern that decreased maternal BP may compromise uteroplacental perfusion and fetal circulation, which also could be evaluated.2
Second, I would like to see how comorbidities affect the initiation of antihypertensives for mild chronic hypertension in pregnancy. Research incorporating pregnant women with borderline hypertension and comorbidities such as obesity, hyperlipidemia, and diabetes mellitus type 2 (DM) is likely to yield informative results. This is especially beneficial since, for example, chronic hypertension and DM are independent risk factors for adverse maternal and fetal outcomes; therefore, a mother with both these conditions may have additive effects on obstetric outcomes.3
Lastly, I would suggest you include a brief conversation about prepregnancy ways to manage women with chronic hypertension. Because many women who enter pregnancy with chronic hypertension have hypertension of unknown origin, it would be beneficial to optimize antihypertensive regimens before conception.4 Also, it should be further evaluated whether initiation of lifestyle modifications, such as weight reduction and the DASH diet before pregnancy, for women with chronic hypertension improves pregnancy outcomes.
Cassandra Maafoh, MD
Macon, Georgia
References
- Pauli JM. Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes? OBG Manag. 2022;34:14-15.
- Brown CM, Garovic VD. Drug treatment of hypertension in pregnancy. Drugs. 2014;74:283-296. https://doi.org/10.1007/s40265-014-0187-7.
- Yanit KE, Snowden JM, Cheng YW, et al. The impact of chronic hypertension and pregestational diabetes on pregnancy outcomes. Am J Obstet Gynecol. 2012;207. https://doi. org/10.1016/j.ajog.2012.06.066.
- Seely EW, Ecker J. Chronic hypertension in pregnancy. Circulation. 2014;129:1254-1261. https:// doi.org/10.1161/circulationaha.113.003904.
BARBARA LEVY, MD (AUGUST 2022)
Are these new and rare syndromes’ pathophysiological mechanisms related?
I read with great interest Dr. Barbara Levy’s UPDATE in the August 2022 issue on testosterone therapy for women with hypoactive sexual desire disorder (HSDD), as well as her comments on persistent genital arousal disorder/genito-pelvic dysesthesia (PGAD/GPD) that was recently so coined by the International Society for the Study of Women’s Sexual Health (ISSWSH) as a 2-component syndrome.1 The new syndrome, explains Dr. Levy, presents with “the perception of genital arousal that is involuntary, unrelated to sexual desire, without any identified cause, not relieved with orgasm, and distressing to the patient (the PGAD component),” combined with “itching, burning, tingling, or pain” (the GPD component).
Although agreeing with ISSWSH that diagnosis and management require a multidisciplinary biopsychosocial approach, in her practical advice, Dr. Levy mentioned: “neuropathic signaling” with “aberrant sensory processing” as the syndrome’s possible main pathophysiology. Interestingly, there are 2 other rare, chronic, and “poorly recognized source(s) of major distress to a small but significant group of patients.” Persistent idiopathic oro-facial pain (PIFP) disorder2 after dental interventions and burning mouth syndrome (BMS),3 defined by the absence of any local or systemic contributing etiology, also present with continuous local burning and pain (as in GPD). Consequently, PGAD/GPD may indeed have the same pathophysiological explanation—as Dr. Levy suggested—of being a (genital) peripheral chronic neuropathic pain condition.
A potentially promising new therapeutic approach for PGAD/GPD would then be to use the same, or similar, antineuropathic medications (Clonazepam, Nortriptyline, Pregabalin, etc.) in the form of topical vaginal swishing solutions similar to the presently recommended antiepileptic and/or antidepressant oral swishing treatment for PIFP and BMS. As the topical approach works well for oral neuropathic pain, vaginal swishing could potentially be the answer for PGAD/GPD peripheral neuropathic pain. Moreover, such a novel topical approach would significantly increase patient motivation for treatment by avoiding the adverse effects of ingested antiepileptic or antidepressant drugs.
This is the first time that anticonvulsant and/or antidepressant vaginal swishing is proposed as topical therapy for GPD peripheral neuropathic pain, still pending scientific/clinical validation. ●
Zwi Hoch, MD
Newton, Massachusetts
- Goldstein I, Komisaruk BR, Pukall CF, et al. International Society for the Study of Women’s Sexual Health (ISSWSH) Review of Epidemiology and Pathophysiology, and a Consensus Nomenclature and Process of Care for the Management of Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia (PGAD/GPD). J Sex Med. 2021;18:665-697.
- Baad-Hansen L, Benoliel R. Neuropathic orofacial pain: facts and fiction. Cephalgia. 2017;37:670-679.
- Kuten-Shorer M, Treister NS, Stock S, et al. Safety and tolerability of topical clonazepam solution for management of oral dysesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124: 146-151.
Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes?
JAIMEY M. PAULI, MD (JUNE 2022)
Consider this, when it comes to treating chronic hypertension
I welcome the article by Dr. Jaimey Pauli, which focuses on initiating treatment for mild chronic hypertension in pregnancy to reach a goal blood pressure (BP) of <140/90 mm Hg to prevent adverse maternal and fetal outcomes.1 I would like to offer 3 additional thoughts for your consideration. First, it is known that there is a physiological decrease in BP during the second trimester, which results in a normotensive presentation. Thus, it would be beneficial to see if pregnant women with high-normal BP levels before the third trimester be administered a lower dose of antihypertensives. However, there is also a concern that decreased maternal BP may compromise uteroplacental perfusion and fetal circulation, which also could be evaluated.2
Second, I would like to see how comorbidities affect the initiation of antihypertensives for mild chronic hypertension in pregnancy. Research incorporating pregnant women with borderline hypertension and comorbidities such as obesity, hyperlipidemia, and diabetes mellitus type 2 (DM) is likely to yield informative results. This is especially beneficial since, for example, chronic hypertension and DM are independent risk factors for adverse maternal and fetal outcomes; therefore, a mother with both these conditions may have additive effects on obstetric outcomes.3
Lastly, I would suggest you include a brief conversation about prepregnancy ways to manage women with chronic hypertension. Because many women who enter pregnancy with chronic hypertension have hypertension of unknown origin, it would be beneficial to optimize antihypertensive regimens before conception.4 Also, it should be further evaluated whether initiation of lifestyle modifications, such as weight reduction and the DASH diet before pregnancy, for women with chronic hypertension improves pregnancy outcomes.
Cassandra Maafoh, MD
Macon, Georgia
References
- Pauli JM. Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes? OBG Manag. 2022;34:14-15.
- Brown CM, Garovic VD. Drug treatment of hypertension in pregnancy. Drugs. 2014;74:283-296. https://doi.org/10.1007/s40265-014-0187-7.
- Yanit KE, Snowden JM, Cheng YW, et al. The impact of chronic hypertension and pregestational diabetes on pregnancy outcomes. Am J Obstet Gynecol. 2012;207. https://doi. org/10.1016/j.ajog.2012.06.066.
- Seely EW, Ecker J. Chronic hypertension in pregnancy. Circulation. 2014;129:1254-1261. https:// doi.org/10.1161/circulationaha.113.003904.
BARBARA LEVY, MD (AUGUST 2022)
Are these new and rare syndromes’ pathophysiological mechanisms related?
I read with great interest Dr. Barbara Levy’s UPDATE in the August 2022 issue on testosterone therapy for women with hypoactive sexual desire disorder (HSDD), as well as her comments on persistent genital arousal disorder/genito-pelvic dysesthesia (PGAD/GPD) that was recently so coined by the International Society for the Study of Women’s Sexual Health (ISSWSH) as a 2-component syndrome.1 The new syndrome, explains Dr. Levy, presents with “the perception of genital arousal that is involuntary, unrelated to sexual desire, without any identified cause, not relieved with orgasm, and distressing to the patient (the PGAD component),” combined with “itching, burning, tingling, or pain” (the GPD component).
Although agreeing with ISSWSH that diagnosis and management require a multidisciplinary biopsychosocial approach, in her practical advice, Dr. Levy mentioned: “neuropathic signaling” with “aberrant sensory processing” as the syndrome’s possible main pathophysiology. Interestingly, there are 2 other rare, chronic, and “poorly recognized source(s) of major distress to a small but significant group of patients.” Persistent idiopathic oro-facial pain (PIFP) disorder2 after dental interventions and burning mouth syndrome (BMS),3 defined by the absence of any local or systemic contributing etiology, also present with continuous local burning and pain (as in GPD). Consequently, PGAD/GPD may indeed have the same pathophysiological explanation—as Dr. Levy suggested—of being a (genital) peripheral chronic neuropathic pain condition.
A potentially promising new therapeutic approach for PGAD/GPD would then be to use the same, or similar, antineuropathic medications (Clonazepam, Nortriptyline, Pregabalin, etc.) in the form of topical vaginal swishing solutions similar to the presently recommended antiepileptic and/or antidepressant oral swishing treatment for PIFP and BMS. As the topical approach works well for oral neuropathic pain, vaginal swishing could potentially be the answer for PGAD/GPD peripheral neuropathic pain. Moreover, such a novel topical approach would significantly increase patient motivation for treatment by avoiding the adverse effects of ingested antiepileptic or antidepressant drugs.
This is the first time that anticonvulsant and/or antidepressant vaginal swishing is proposed as topical therapy for GPD peripheral neuropathic pain, still pending scientific/clinical validation. ●
Zwi Hoch, MD
Newton, Massachusetts
- Goldstein I, Komisaruk BR, Pukall CF, et al. International Society for the Study of Women’s Sexual Health (ISSWSH) Review of Epidemiology and Pathophysiology, and a Consensus Nomenclature and Process of Care for the Management of Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia (PGAD/GPD). J Sex Med. 2021;18:665-697.
- Baad-Hansen L, Benoliel R. Neuropathic orofacial pain: facts and fiction. Cephalgia. 2017;37:670-679.
- Kuten-Shorer M, Treister NS, Stock S, et al. Safety and tolerability of topical clonazepam solution for management of oral dysesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124: 146-151.
Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes?
JAIMEY M. PAULI, MD (JUNE 2022)
Consider this, when it comes to treating chronic hypertension
I welcome the article by Dr. Jaimey Pauli, which focuses on initiating treatment for mild chronic hypertension in pregnancy to reach a goal blood pressure (BP) of <140/90 mm Hg to prevent adverse maternal and fetal outcomes.1 I would like to offer 3 additional thoughts for your consideration. First, it is known that there is a physiological decrease in BP during the second trimester, which results in a normotensive presentation. Thus, it would be beneficial to see if pregnant women with high-normal BP levels before the third trimester be administered a lower dose of antihypertensives. However, there is also a concern that decreased maternal BP may compromise uteroplacental perfusion and fetal circulation, which also could be evaluated.2
Second, I would like to see how comorbidities affect the initiation of antihypertensives for mild chronic hypertension in pregnancy. Research incorporating pregnant women with borderline hypertension and comorbidities such as obesity, hyperlipidemia, and diabetes mellitus type 2 (DM) is likely to yield informative results. This is especially beneficial since, for example, chronic hypertension and DM are independent risk factors for adverse maternal and fetal outcomes; therefore, a mother with both these conditions may have additive effects on obstetric outcomes.3
Lastly, I would suggest you include a brief conversation about prepregnancy ways to manage women with chronic hypertension. Because many women who enter pregnancy with chronic hypertension have hypertension of unknown origin, it would be beneficial to optimize antihypertensive regimens before conception.4 Also, it should be further evaluated whether initiation of lifestyle modifications, such as weight reduction and the DASH diet before pregnancy, for women with chronic hypertension improves pregnancy outcomes.
Cassandra Maafoh, MD
Macon, Georgia
References
- Pauli JM. Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes? OBG Manag. 2022;34:14-15.
- Brown CM, Garovic VD. Drug treatment of hypertension in pregnancy. Drugs. 2014;74:283-296. https://doi.org/10.1007/s40265-014-0187-7.
- Yanit KE, Snowden JM, Cheng YW, et al. The impact of chronic hypertension and pregestational diabetes on pregnancy outcomes. Am J Obstet Gynecol. 2012;207. https://doi. org/10.1016/j.ajog.2012.06.066.
- Seely EW, Ecker J. Chronic hypertension in pregnancy. Circulation. 2014;129:1254-1261. https:// doi.org/10.1161/circulationaha.113.003904.
BARBARA LEVY, MD (AUGUST 2022)
Are these new and rare syndromes’ pathophysiological mechanisms related?
I read with great interest Dr. Barbara Levy’s UPDATE in the August 2022 issue on testosterone therapy for women with hypoactive sexual desire disorder (HSDD), as well as her comments on persistent genital arousal disorder/genito-pelvic dysesthesia (PGAD/GPD) that was recently so coined by the International Society for the Study of Women’s Sexual Health (ISSWSH) as a 2-component syndrome.1 The new syndrome, explains Dr. Levy, presents with “the perception of genital arousal that is involuntary, unrelated to sexual desire, without any identified cause, not relieved with orgasm, and distressing to the patient (the PGAD component),” combined with “itching, burning, tingling, or pain” (the GPD component).
Although agreeing with ISSWSH that diagnosis and management require a multidisciplinary biopsychosocial approach, in her practical advice, Dr. Levy mentioned: “neuropathic signaling” with “aberrant sensory processing” as the syndrome’s possible main pathophysiology. Interestingly, there are 2 other rare, chronic, and “poorly recognized source(s) of major distress to a small but significant group of patients.” Persistent idiopathic oro-facial pain (PIFP) disorder2 after dental interventions and burning mouth syndrome (BMS),3 defined by the absence of any local or systemic contributing etiology, also present with continuous local burning and pain (as in GPD). Consequently, PGAD/GPD may indeed have the same pathophysiological explanation—as Dr. Levy suggested—of being a (genital) peripheral chronic neuropathic pain condition.
A potentially promising new therapeutic approach for PGAD/GPD would then be to use the same, or similar, antineuropathic medications (Clonazepam, Nortriptyline, Pregabalin, etc.) in the form of topical vaginal swishing solutions similar to the presently recommended antiepileptic and/or antidepressant oral swishing treatment for PIFP and BMS. As the topical approach works well for oral neuropathic pain, vaginal swishing could potentially be the answer for PGAD/GPD peripheral neuropathic pain. Moreover, such a novel topical approach would significantly increase patient motivation for treatment by avoiding the adverse effects of ingested antiepileptic or antidepressant drugs.
This is the first time that anticonvulsant and/or antidepressant vaginal swishing is proposed as topical therapy for GPD peripheral neuropathic pain, still pending scientific/clinical validation. ●
Zwi Hoch, MD
Newton, Massachusetts
- Goldstein I, Komisaruk BR, Pukall CF, et al. International Society for the Study of Women’s Sexual Health (ISSWSH) Review of Epidemiology and Pathophysiology, and a Consensus Nomenclature and Process of Care for the Management of Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia (PGAD/GPD). J Sex Med. 2021;18:665-697.
- Baad-Hansen L, Benoliel R. Neuropathic orofacial pain: facts and fiction. Cephalgia. 2017;37:670-679.
- Kuten-Shorer M, Treister NS, Stock S, et al. Safety and tolerability of topical clonazepam solution for management of oral dysesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124: 146-151.
COMMENT & CONTROVERSY
How common is IUD perforation, expulsion, and malposition?
ROBERT L. BARBIERI, MD (APRIL 2022)
The seriousness of IUD embedment
I appreciated Dr. Barbieri’s comprehensive review of clinical problems regarding the intrauterine device (IUD). It is interesting that, in spite of your mention of IUD embedment in the myometrium, other publications regarding this phenomenon are seemingly absent (except for ours).1 Whether or not there is associated pain (and sometimes there is not), in our experience its removal can result in IUD fracture. As you stated, it is true that 3D transvaginal sonography perfectly enables this visualization, yet it is surprising that others have not experienced what we have. Nonetheless, it is encouraging to see that IUD embedment is seriously mentioned.
- Fernandez CM, Levine EM, Cabiya M, et al. Intrauterine device embedment resulting in its fracture: a case series. Arch Obstet Gynecol. 2021;2:1-4.
Elliot Levine, MD
Chicago, Illinois
Dr. Barbieri responds
I thank Dr. Levine for highlighting the important issue of IUD fracture and providing a reference to a case series of IUD fractures. Although such fracture is not common, when it does occur it may require a hysteroscopic procedure to remove all pieces of the IUD. In the cited case series, fracture was more commonly observed with the copper IUD than with the LNG-IUD. With regard to IUD malposition, 4 publications reviewed in my recent editorial describe the problem of an IUD arm embedded in the myometrium.1-4
References
- Benacerraf BR, Shipp TD, Bromley B. Three-dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol. 2009;34:110-115.
- Braaten KP, Benson CB, Maurer R, et al. Malpositioned intrauterine contraceptive devices: risk factors, outcomes and future pregnancies. Obstet Gynecol. 2011;118:1014-1020.
- Gerkowicz SA, Fiorentino DG, Kovacs AP, et al. Uterine structural abnormality and intrauterine device malposition: analysis of ultrasonographic and demographic variables of 517 patients. Am J Obstet Gynecol. 2019;220:183.e1-e8.
- Connolly CT, Fox NS. Incidence and risk factors for a malpositioned intrauterine device detected on three-dimensional ultrasound within eight weeks of placement. J Ultrasound Med. September 27, 2021.
Will NAAT replace microscopy for the identification of organisms causing vaginitis?
ROBERT L. BARBIERI, MD (MARCH 2022)
Follow-up questions on NAAT testing
The sensitivity of NAAT testing, as outlined in Dr. Barbieri’s editorial, is undoubtedly better than the clinical methods most clinicians are using. I appreciate the frustration we providers often experience in drawing conclusions for patients based on the Amsel criteria for bacterial vaginitis (BV). I am surprised by the low sensitivity of microscopy for yeast vaginitis. My follow-up questions are:
- Have the NAATs referenced been validated in clinical trials and proven to improve patient outcomes?
- Will the proposal to begin empiric therapy for both yeast vaginitis and BV in combination while waiting for NAAT results lead to an increase of resistant strains?
- What is the cost of NAAT for vaginitis, and is this cost effective in routine practice?
- Can NAATs be utilized to detect resistant strains of yeast or Gardnerella sp?
Alan Paul Gehrich, MD (COL, MC ret.)
Bethesda, Maryland
Dr. Barbieri responds
I thank Dr. Gehrich for raising the important issue of what is the optimal endpoint to assess the clinical utility of NAAT testing for vaginitis. Most studies of the use of NAAT to diagnose the cause of vaginitis focus on comparing NAAT results to standard clinical practice (microscopy and pH), and to a “gold standard.” In most studies the gold standards are Nugent scoring with Amsel criteria to resolve intermediate Nugent scores for bacterial vaginosis, culture for Candida, and culture for Trichomonas vaginalis. It is clear from multiple studies that NAAT provides superior sensitivity and specificity compared with standard clinical practice.1-3 As noted in the editorial, in a study of 466 patients with symptoms of vaginitis, standard office approaches to the diagnosis of vaginitis resulted in the failure to identify the correct infection in a large number of cases.4 For the diagnosis of BV, clinicians missed 42% of the cases identified by NAAT. For the diagnosis of Candida, clinicians missed 46% of the cases identified by NAAT. For the diagnosis of T vaginalis, clinicians missed 72% of the cases identified by NAAT. This resulted in clinicians not appropriately treating many infections detected by NAAT.
NAAT does provide information about the presence of Candida glabrata and Candida krusei, organisms which may be resistant to fluconazole. I agree with Dr. Gehrich that the optimal use of NAAT testing in practice is poorly studied with regard to treatment between sample collection and NAAT results. Cost of testing is a complex issue. Standard microscopy is relatively inexpensive, but performs poorly in clinical practice, resulting in misdiagnosis. NAAT testing is expensive but correctly identifies causes of vaginitis.
References
- Schwebke JR, Gaydos CA, Hyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of vaginal panel assay compared with clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Schwebke JR, Taylor SN, Ackerman N, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginalis assays: results from a prospective multi-center study. J Clin Microbiol. 2020;58:e01643-19. 4
- Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
How common is IUD perforation, expulsion, and malposition?
ROBERT L. BARBIERI, MD (APRIL 2022)
The seriousness of IUD embedment
I appreciated Dr. Barbieri’s comprehensive review of clinical problems regarding the intrauterine device (IUD). It is interesting that, in spite of your mention of IUD embedment in the myometrium, other publications regarding this phenomenon are seemingly absent (except for ours).1 Whether or not there is associated pain (and sometimes there is not), in our experience its removal can result in IUD fracture. As you stated, it is true that 3D transvaginal sonography perfectly enables this visualization, yet it is surprising that others have not experienced what we have. Nonetheless, it is encouraging to see that IUD embedment is seriously mentioned.
- Fernandez CM, Levine EM, Cabiya M, et al. Intrauterine device embedment resulting in its fracture: a case series. Arch Obstet Gynecol. 2021;2:1-4.
Elliot Levine, MD
Chicago, Illinois
Dr. Barbieri responds
I thank Dr. Levine for highlighting the important issue of IUD fracture and providing a reference to a case series of IUD fractures. Although such fracture is not common, when it does occur it may require a hysteroscopic procedure to remove all pieces of the IUD. In the cited case series, fracture was more commonly observed with the copper IUD than with the LNG-IUD. With regard to IUD malposition, 4 publications reviewed in my recent editorial describe the problem of an IUD arm embedded in the myometrium.1-4
References
- Benacerraf BR, Shipp TD, Bromley B. Three-dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol. 2009;34:110-115.
- Braaten KP, Benson CB, Maurer R, et al. Malpositioned intrauterine contraceptive devices: risk factors, outcomes and future pregnancies. Obstet Gynecol. 2011;118:1014-1020.
- Gerkowicz SA, Fiorentino DG, Kovacs AP, et al. Uterine structural abnormality and intrauterine device malposition: analysis of ultrasonographic and demographic variables of 517 patients. Am J Obstet Gynecol. 2019;220:183.e1-e8.
- Connolly CT, Fox NS. Incidence and risk factors for a malpositioned intrauterine device detected on three-dimensional ultrasound within eight weeks of placement. J Ultrasound Med. September 27, 2021.
Will NAAT replace microscopy for the identification of organisms causing vaginitis?
ROBERT L. BARBIERI, MD (MARCH 2022)
Follow-up questions on NAAT testing
The sensitivity of NAAT testing, as outlined in Dr. Barbieri’s editorial, is undoubtedly better than the clinical methods most clinicians are using. I appreciate the frustration we providers often experience in drawing conclusions for patients based on the Amsel criteria for bacterial vaginitis (BV). I am surprised by the low sensitivity of microscopy for yeast vaginitis. My follow-up questions are:
- Have the NAATs referenced been validated in clinical trials and proven to improve patient outcomes?
- Will the proposal to begin empiric therapy for both yeast vaginitis and BV in combination while waiting for NAAT results lead to an increase of resistant strains?
- What is the cost of NAAT for vaginitis, and is this cost effective in routine practice?
- Can NAATs be utilized to detect resistant strains of yeast or Gardnerella sp?
Alan Paul Gehrich, MD (COL, MC ret.)
Bethesda, Maryland
Dr. Barbieri responds
I thank Dr. Gehrich for raising the important issue of what is the optimal endpoint to assess the clinical utility of NAAT testing for vaginitis. Most studies of the use of NAAT to diagnose the cause of vaginitis focus on comparing NAAT results to standard clinical practice (microscopy and pH), and to a “gold standard.” In most studies the gold standards are Nugent scoring with Amsel criteria to resolve intermediate Nugent scores for bacterial vaginosis, culture for Candida, and culture for Trichomonas vaginalis. It is clear from multiple studies that NAAT provides superior sensitivity and specificity compared with standard clinical practice.1-3 As noted in the editorial, in a study of 466 patients with symptoms of vaginitis, standard office approaches to the diagnosis of vaginitis resulted in the failure to identify the correct infection in a large number of cases.4 For the diagnosis of BV, clinicians missed 42% of the cases identified by NAAT. For the diagnosis of Candida, clinicians missed 46% of the cases identified by NAAT. For the diagnosis of T vaginalis, clinicians missed 72% of the cases identified by NAAT. This resulted in clinicians not appropriately treating many infections detected by NAAT.
NAAT does provide information about the presence of Candida glabrata and Candida krusei, organisms which may be resistant to fluconazole. I agree with Dr. Gehrich that the optimal use of NAAT testing in practice is poorly studied with regard to treatment between sample collection and NAAT results. Cost of testing is a complex issue. Standard microscopy is relatively inexpensive, but performs poorly in clinical practice, resulting in misdiagnosis. NAAT testing is expensive but correctly identifies causes of vaginitis.
References
- Schwebke JR, Gaydos CA, Hyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of vaginal panel assay compared with clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Schwebke JR, Taylor SN, Ackerman N, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginalis assays: results from a prospective multi-center study. J Clin Microbiol. 2020;58:e01643-19. 4
- Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
How common is IUD perforation, expulsion, and malposition?
ROBERT L. BARBIERI, MD (APRIL 2022)
The seriousness of IUD embedment
I appreciated Dr. Barbieri’s comprehensive review of clinical problems regarding the intrauterine device (IUD). It is interesting that, in spite of your mention of IUD embedment in the myometrium, other publications regarding this phenomenon are seemingly absent (except for ours).1 Whether or not there is associated pain (and sometimes there is not), in our experience its removal can result in IUD fracture. As you stated, it is true that 3D transvaginal sonography perfectly enables this visualization, yet it is surprising that others have not experienced what we have. Nonetheless, it is encouraging to see that IUD embedment is seriously mentioned.
- Fernandez CM, Levine EM, Cabiya M, et al. Intrauterine device embedment resulting in its fracture: a case series. Arch Obstet Gynecol. 2021;2:1-4.
Elliot Levine, MD
Chicago, Illinois
Dr. Barbieri responds
I thank Dr. Levine for highlighting the important issue of IUD fracture and providing a reference to a case series of IUD fractures. Although such fracture is not common, when it does occur it may require a hysteroscopic procedure to remove all pieces of the IUD. In the cited case series, fracture was more commonly observed with the copper IUD than with the LNG-IUD. With regard to IUD malposition, 4 publications reviewed in my recent editorial describe the problem of an IUD arm embedded in the myometrium.1-4
References
- Benacerraf BR, Shipp TD, Bromley B. Three-dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol. 2009;34:110-115.
- Braaten KP, Benson CB, Maurer R, et al. Malpositioned intrauterine contraceptive devices: risk factors, outcomes and future pregnancies. Obstet Gynecol. 2011;118:1014-1020.
- Gerkowicz SA, Fiorentino DG, Kovacs AP, et al. Uterine structural abnormality and intrauterine device malposition: analysis of ultrasonographic and demographic variables of 517 patients. Am J Obstet Gynecol. 2019;220:183.e1-e8.
- Connolly CT, Fox NS. Incidence and risk factors for a malpositioned intrauterine device detected on three-dimensional ultrasound within eight weeks of placement. J Ultrasound Med. September 27, 2021.
Will NAAT replace microscopy for the identification of organisms causing vaginitis?
ROBERT L. BARBIERI, MD (MARCH 2022)
Follow-up questions on NAAT testing
The sensitivity of NAAT testing, as outlined in Dr. Barbieri’s editorial, is undoubtedly better than the clinical methods most clinicians are using. I appreciate the frustration we providers often experience in drawing conclusions for patients based on the Amsel criteria for bacterial vaginitis (BV). I am surprised by the low sensitivity of microscopy for yeast vaginitis. My follow-up questions are:
- Have the NAATs referenced been validated in clinical trials and proven to improve patient outcomes?
- Will the proposal to begin empiric therapy for both yeast vaginitis and BV in combination while waiting for NAAT results lead to an increase of resistant strains?
- What is the cost of NAAT for vaginitis, and is this cost effective in routine practice?
- Can NAATs be utilized to detect resistant strains of yeast or Gardnerella sp?
Alan Paul Gehrich, MD (COL, MC ret.)
Bethesda, Maryland
Dr. Barbieri responds
I thank Dr. Gehrich for raising the important issue of what is the optimal endpoint to assess the clinical utility of NAAT testing for vaginitis. Most studies of the use of NAAT to diagnose the cause of vaginitis focus on comparing NAAT results to standard clinical practice (microscopy and pH), and to a “gold standard.” In most studies the gold standards are Nugent scoring with Amsel criteria to resolve intermediate Nugent scores for bacterial vaginosis, culture for Candida, and culture for Trichomonas vaginalis. It is clear from multiple studies that NAAT provides superior sensitivity and specificity compared with standard clinical practice.1-3 As noted in the editorial, in a study of 466 patients with symptoms of vaginitis, standard office approaches to the diagnosis of vaginitis resulted in the failure to identify the correct infection in a large number of cases.4 For the diagnosis of BV, clinicians missed 42% of the cases identified by NAAT. For the diagnosis of Candida, clinicians missed 46% of the cases identified by NAAT. For the diagnosis of T vaginalis, clinicians missed 72% of the cases identified by NAAT. This resulted in clinicians not appropriately treating many infections detected by NAAT.
NAAT does provide information about the presence of Candida glabrata and Candida krusei, organisms which may be resistant to fluconazole. I agree with Dr. Gehrich that the optimal use of NAAT testing in practice is poorly studied with regard to treatment between sample collection and NAAT results. Cost of testing is a complex issue. Standard microscopy is relatively inexpensive, but performs poorly in clinical practice, resulting in misdiagnosis. NAAT testing is expensive but correctly identifies causes of vaginitis.
References
- Schwebke JR, Gaydos CA, Hyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of vaginal panel assay compared with clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Schwebke JR, Taylor SN, Ackerman N, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginalis assays: results from a prospective multi-center study. J Clin Microbiol. 2020;58:e01643-19. 4
- Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
COMMENT & CONTROVERSY
UTIs IN PREGNANCY: MANAGING URETHRITIS, ASYMPTOMATIC BACTERIURIA, CYSTITIS, AND PYELONEPHRITIS
PATRICK DUFF, MD (JANUARY 2022)
Clarification on UTI issues
Regarding the article on urinary tract infections (UTIs) in pregnancy, I have 3 points of clarification. First, in 27 years of practice in which I universally performed screening urine cultures on prenatal patients plus all of those with symptoms, I have seen a total of 2 cultures with Staphylococcus saprophyticus. I see this organism listed in references as a major UTI causative, but is that the case? Second, the clinical case and symptoms discussed are accurate, but costovertebral angle tenderness or fever of 101 °F or higher indicate pyelonephritis and should be treated aggressively. Many of these patients will have nausea and vomiting and will be dehydrated. This decreases urine flow, allowing progressive bacterial growth in renal parenchyma. An initial bolus of intravenous fluids, at least 2 L wide open through a large-bore catheter, rapidly decreases fever, flushes the urinary tract, and improves nausea, headaches, and malaise. Finally, nitrofurantoin is excreted in the urine so rapidly that it does not achieve adequate tissue levels, and it should never be used to treat pyelonephritis or, for that matter, any infection other than uncomplicated cystitis/urethritis.
David Janowitz, MD
Houston, Texas
Dr. Duff responds
I appreciate Dr. Janowitz’s interest and thoughtful comments. The patient presented in the case study has acute cystitis, characterized by a low-grade fever, suprapubic pain, dysuria, frequency, and hesitancy. Patients with pyelonephritis typically have a higher fever and significant costovertebral angle pain and tenderness. I agree completely with Dr. Janowitz’s observations about the seriousness of pyelonephritis in pregnancy. Pyelonephritis is an important cause of preterm labor, bacteremia, and even septic shock. As I point out in the article, women with moderate to severe kidney infections should be hospitalized and treated with intravenous fluids, antipyretics, antiemetics, and intravenous antibiotics. My usual recommendation is ceftriaxone. Intravenous antibiotics should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. Once patients improve, they can be transitioned to oral antibiotics to complete a 10-day course of therapy. Again, I agree with Dr. Janowitz’s statement that nitrofurantoin is not an appropriate drug for treatment of pyelonephritis because it does not reach acceptable concentrations in either the blood or the renal parenchyma. Rather, amoxicillin-clavulanate and trimethoprim-sulfamethoxazole are much better choices for oral therapy. However, once the infection is cleared, nitrofurantoin is an excellent agent for suppression of recurrent infection.
Finally, there is no doubt that the principal pathogens that cause UTIs in pregnant women are Escherichia coli, Klebsiella pneumoniae, and Proteus species. However, 3 aerobic Gram-positive cocci do, in fact, cause a small percentage of infections: group B streptococci, enterococci, and Staphylococcus saprophyticus. When the latter bacterium is identified as a single organism in high colony count, particularly in a catheterized urine specimen, it should be considered a true pathogen and not simply a contaminant.
CAN WE RETURN TO THE ABCs OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Another suggestion for reducing note bloat in the EMR
Thank you for picking up a topic that is important for all physicians and one that has been annoying me since the introduction of electronic medical records (EMRs). I like the APSO approach, that works well. My idea for reducing “note bloat” is to eliminate all normal and routine findings and to hide them behind a hyperlink or behind a QR code. This would give you a truly short note and, should you need or want more details, you could always scan the QR code for access to the complete (and bloated) note. I would also recommend hiding all details that do not contribute to the immediate pressing issue at hand (for example, routine depression screening) behind a hyperlink or QR code. The same principle should apply to sending faxes to other physicians’ offices. I “love” receiving a chart an inch thick, only to discover that the whole pile of paper could be reduced to a single page of true information. Too few people speak up about this major time and productivity thief. Thank you!
Matthias Muenzer, MD
Rochester, New Hampshire
Dr. Barbieri responds
I thank Dr. Muenzer for his innovative suggestions for improving medical record notes. We spend many hours per week crafting notes in the medical record. Yet, very little attention is given to the development of best practices for improving the value and effectiveness of our notes for our patients and colleagues.
UTIs IN PREGNANCY: MANAGING URETHRITIS, ASYMPTOMATIC BACTERIURIA, CYSTITIS, AND PYELONEPHRITIS
PATRICK DUFF, MD (JANUARY 2022)
Clarification on UTI issues
Regarding the article on urinary tract infections (UTIs) in pregnancy, I have 3 points of clarification. First, in 27 years of practice in which I universally performed screening urine cultures on prenatal patients plus all of those with symptoms, I have seen a total of 2 cultures with Staphylococcus saprophyticus. I see this organism listed in references as a major UTI causative, but is that the case? Second, the clinical case and symptoms discussed are accurate, but costovertebral angle tenderness or fever of 101 °F or higher indicate pyelonephritis and should be treated aggressively. Many of these patients will have nausea and vomiting and will be dehydrated. This decreases urine flow, allowing progressive bacterial growth in renal parenchyma. An initial bolus of intravenous fluids, at least 2 L wide open through a large-bore catheter, rapidly decreases fever, flushes the urinary tract, and improves nausea, headaches, and malaise. Finally, nitrofurantoin is excreted in the urine so rapidly that it does not achieve adequate tissue levels, and it should never be used to treat pyelonephritis or, for that matter, any infection other than uncomplicated cystitis/urethritis.
David Janowitz, MD
Houston, Texas
Dr. Duff responds
I appreciate Dr. Janowitz’s interest and thoughtful comments. The patient presented in the case study has acute cystitis, characterized by a low-grade fever, suprapubic pain, dysuria, frequency, and hesitancy. Patients with pyelonephritis typically have a higher fever and significant costovertebral angle pain and tenderness. I agree completely with Dr. Janowitz’s observations about the seriousness of pyelonephritis in pregnancy. Pyelonephritis is an important cause of preterm labor, bacteremia, and even septic shock. As I point out in the article, women with moderate to severe kidney infections should be hospitalized and treated with intravenous fluids, antipyretics, antiemetics, and intravenous antibiotics. My usual recommendation is ceftriaxone. Intravenous antibiotics should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. Once patients improve, they can be transitioned to oral antibiotics to complete a 10-day course of therapy. Again, I agree with Dr. Janowitz’s statement that nitrofurantoin is not an appropriate drug for treatment of pyelonephritis because it does not reach acceptable concentrations in either the blood or the renal parenchyma. Rather, amoxicillin-clavulanate and trimethoprim-sulfamethoxazole are much better choices for oral therapy. However, once the infection is cleared, nitrofurantoin is an excellent agent for suppression of recurrent infection.
Finally, there is no doubt that the principal pathogens that cause UTIs in pregnant women are Escherichia coli, Klebsiella pneumoniae, and Proteus species. However, 3 aerobic Gram-positive cocci do, in fact, cause a small percentage of infections: group B streptococci, enterococci, and Staphylococcus saprophyticus. When the latter bacterium is identified as a single organism in high colony count, particularly in a catheterized urine specimen, it should be considered a true pathogen and not simply a contaminant.
CAN WE RETURN TO THE ABCs OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Another suggestion for reducing note bloat in the EMR
Thank you for picking up a topic that is important for all physicians and one that has been annoying me since the introduction of electronic medical records (EMRs). I like the APSO approach, that works well. My idea for reducing “note bloat” is to eliminate all normal and routine findings and to hide them behind a hyperlink or behind a QR code. This would give you a truly short note and, should you need or want more details, you could always scan the QR code for access to the complete (and bloated) note. I would also recommend hiding all details that do not contribute to the immediate pressing issue at hand (for example, routine depression screening) behind a hyperlink or QR code. The same principle should apply to sending faxes to other physicians’ offices. I “love” receiving a chart an inch thick, only to discover that the whole pile of paper could be reduced to a single page of true information. Too few people speak up about this major time and productivity thief. Thank you!
Matthias Muenzer, MD
Rochester, New Hampshire
Dr. Barbieri responds
I thank Dr. Muenzer for his innovative suggestions for improving medical record notes. We spend many hours per week crafting notes in the medical record. Yet, very little attention is given to the development of best practices for improving the value and effectiveness of our notes for our patients and colleagues.
UTIs IN PREGNANCY: MANAGING URETHRITIS, ASYMPTOMATIC BACTERIURIA, CYSTITIS, AND PYELONEPHRITIS
PATRICK DUFF, MD (JANUARY 2022)
Clarification on UTI issues
Regarding the article on urinary tract infections (UTIs) in pregnancy, I have 3 points of clarification. First, in 27 years of practice in which I universally performed screening urine cultures on prenatal patients plus all of those with symptoms, I have seen a total of 2 cultures with Staphylococcus saprophyticus. I see this organism listed in references as a major UTI causative, but is that the case? Second, the clinical case and symptoms discussed are accurate, but costovertebral angle tenderness or fever of 101 °F or higher indicate pyelonephritis and should be treated aggressively. Many of these patients will have nausea and vomiting and will be dehydrated. This decreases urine flow, allowing progressive bacterial growth in renal parenchyma. An initial bolus of intravenous fluids, at least 2 L wide open through a large-bore catheter, rapidly decreases fever, flushes the urinary tract, and improves nausea, headaches, and malaise. Finally, nitrofurantoin is excreted in the urine so rapidly that it does not achieve adequate tissue levels, and it should never be used to treat pyelonephritis or, for that matter, any infection other than uncomplicated cystitis/urethritis.
David Janowitz, MD
Houston, Texas
Dr. Duff responds
I appreciate Dr. Janowitz’s interest and thoughtful comments. The patient presented in the case study has acute cystitis, characterized by a low-grade fever, suprapubic pain, dysuria, frequency, and hesitancy. Patients with pyelonephritis typically have a higher fever and significant costovertebral angle pain and tenderness. I agree completely with Dr. Janowitz’s observations about the seriousness of pyelonephritis in pregnancy. Pyelonephritis is an important cause of preterm labor, bacteremia, and even septic shock. As I point out in the article, women with moderate to severe kidney infections should be hospitalized and treated with intravenous fluids, antipyretics, antiemetics, and intravenous antibiotics. My usual recommendation is ceftriaxone. Intravenous antibiotics should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. Once patients improve, they can be transitioned to oral antibiotics to complete a 10-day course of therapy. Again, I agree with Dr. Janowitz’s statement that nitrofurantoin is not an appropriate drug for treatment of pyelonephritis because it does not reach acceptable concentrations in either the blood or the renal parenchyma. Rather, amoxicillin-clavulanate and trimethoprim-sulfamethoxazole are much better choices for oral therapy. However, once the infection is cleared, nitrofurantoin is an excellent agent for suppression of recurrent infection.
Finally, there is no doubt that the principal pathogens that cause UTIs in pregnant women are Escherichia coli, Klebsiella pneumoniae, and Proteus species. However, 3 aerobic Gram-positive cocci do, in fact, cause a small percentage of infections: group B streptococci, enterococci, and Staphylococcus saprophyticus. When the latter bacterium is identified as a single organism in high colony count, particularly in a catheterized urine specimen, it should be considered a true pathogen and not simply a contaminant.
CAN WE RETURN TO THE ABCs OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Another suggestion for reducing note bloat in the EMR
Thank you for picking up a topic that is important for all physicians and one that has been annoying me since the introduction of electronic medical records (EMRs). I like the APSO approach, that works well. My idea for reducing “note bloat” is to eliminate all normal and routine findings and to hide them behind a hyperlink or behind a QR code. This would give you a truly short note and, should you need or want more details, you could always scan the QR code for access to the complete (and bloated) note. I would also recommend hiding all details that do not contribute to the immediate pressing issue at hand (for example, routine depression screening) behind a hyperlink or QR code. The same principle should apply to sending faxes to other physicians’ offices. I “love” receiving a chart an inch thick, only to discover that the whole pile of paper could be reduced to a single page of true information. Too few people speak up about this major time and productivity thief. Thank you!
Matthias Muenzer, MD
Rochester, New Hampshire
Dr. Barbieri responds
I thank Dr. Muenzer for his innovative suggestions for improving medical record notes. We spend many hours per week crafting notes in the medical record. Yet, very little attention is given to the development of best practices for improving the value and effectiveness of our notes for our patients and colleagues.
COMMENT & CONTROVERSY
HOW TO CHOOSE THE RIGHT VAGINAL MOISTURIZER OR LUBRICANT FOR YOUR PATIENT
JOHN PENNYCUFF, MD, MSPH, AND CHERYL IGLESIA, MD (JUNE 2021)
Which vaginal products to recommend
We applaud Drs. Pennycuff and Iglesia for providing education on lubricants and vaginal moisturizers in their recent article, and agree that ObGyns, urogynecologists, and primary care providers should be aware of the types of products available. However, the authors underplayed the health risks associated with the use of poor-quality lubricants and moisturizers.
Women often turn to lubricants or vaginal moisturizers because they experience vaginal dryness during intercourse, related to menopause, and from certain medications. Vaginal fluid is primarily composed of exudate from capillaries in the vaginal wall. During sexual arousal, blood flow to the vaginal wall increases, and in turn, this should increase exudate. But chronic inflammation can suppress these increases in vaginal blood flow, preventing adequate vaginal fluid production. One such cause of chronic inflammation is using hyperosmolar lubricants, as this has been shown to negatively affect the vaginal epithelium.1,2 In this way, use of hyperosmolar lubricants can actually worsen symptoms, creating a vicious circle of dryness, lubricant use, and worsening dryness.
In addition, hyperosmolar lubricants have been shown to reduce the epithelial barrier properties of the vaginal epithelium, increasing susceptibility to microbes associated with bacterial vaginosis and to true pathogens, including herpes simplex virus type 2.3 In fact, hyperosmolar lubricants are a serious enough problem that the World Health Organization has weighed in, recommending osmolality of personal lubricants be under 380 mOsm/kg to prevent damage to the vaginal epithelium.4
Appropriately acidic pH is just as critical as osmolality. Using products with a pH higher than 4.5 will reduce amounts of protective lactobacilli and other commensal vaginal bacteria, encouraging growth of opportunistic bacteria and yeast already present. This can lead to bacterial vaginosis, aerobic vaginitis, and candidiasis. Bacterial vaginosis can lead to other serious sequelae such as increased risk in acquisition of HIV infection and preterm birth in pregnancy. Unfortunately, much of the data cited in Drs. Pennycuff and Iglesia’s article were sourced from another study (by Edwards and Panay published in Climacteric in 2016), which measured product pH values with an inappropriately calibrated device; the study’s supplemental information stated that calibration was between 5 and 9, and so any measurement below 5 was invalid and subject to error. For example, the Good Clean Love lubricant is listed as having a pH of 4.7, but its pH is never higher than 4.4.
The products on the market that meet the dual criteria of appropriate pH and isotonicity to vaginal epithelial cells may be less well known to consumers. But this should not be a reason to encourage use of hyperosmolar products whose main selling point is that they are the “leading brand.” Educating women on their choices in personal lubricants should include a full discussion of product ingredients and properties, based upon the available literature to help them select a product that supports the health of their intimate tissues.
Members of the Scientific Advisory Board for the Sexual Health and Wellness Institute: Jill Krapf, MD, MEd, IF; Cathy Chung Hwa Yi, MD; Christine Enzmann, MD, PhD, NMCP; Susan Kellogg-Spadt, PhD, CRNP, IF, CSC, FCST; Betsy Greenleaf, DO, MBA; Elizabeth DuPriest, PhD
References
- Dezzutti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV-1 activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal .pone.0048328.
- Ayehunie S, Wang YY, Landry T, et al. Hyperosmolal vaginal lubricants markedly reduce epithelial barrier properties in a threedimensional vaginal epithelium model. Toxicol Rep. 2017;5:134-140. doi: 10.1016 /j.toxrep.2017.12.011.
- Moench TR, Mumper RJ, Hoen TE, et al. Microbicide excipients can greatly increase susceptibility to genital herpes transmission in the mouse. BMC Infect Dis. 2010;10:331. doi: 10.1186/1471 -2334-10-331.
- Use and procurement of additional lubricants for male and female condoms: WHO/UNFPA /FHI360 Advisory note. World Health Organization, 2012. http://apps.who.int/iris/bitstream /handle/10665/76580/WHO_RHR_12.33_eng .pdf?sequence=1. Accessed December 27, 2021.
Drs. Pennycuff And Iglesia Respond
We thank the members of the scientific advisory board for the Sexual Health and Wellness Institute for their thoughtful and insightful comments to our article. We agree with their comments on the importance of both pH and osmolality for vaginal moisturizers and lubricants. We also agree that selection of an incorrectly formulated product may lead to worsening of vulvovaginal symptoms as well as dysbiosis and all of its sequelae as the letter writers mentioned.
In writing the review article, we attempted to address the role that pH and osmolality play in vaginal moisturizers and lubricants and make clinicians more aware of the importance of these factors in product formulation. Our goal was to help to improve patient counseling. We tried to amass as much of the available literature as we could to act as a resource for practitioners, such as the table included in the article as well as the supplemental table included online. We hoped that by writing this article we would heighten awareness among female health practitioners about vaginal health products and encourage them to consider those products that may be better suited for their patients based on pH and osmolality.
While there remains a paucity of research on vaginal moisturizers and lubricants, there is even less consumer knowledge regarding ingredients and formulations of these products. We wholeheartedly agree with the scientific advisory board that we as health providers need to help educate women on the full spectrum of products available beyond the “leading brands.” Furthermore, we advocate that there be continued research on these products as well as more manufacturer transparency regarding not only the ingredients contained within these products but also the pH and osmolality. Simple steps such as these would ensure that providers could help counsel patients to make informed decisions regarding products for their pelvic health.
Continue to: DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES...
DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES
CASSANDRA CARBERRY, MD, MS; ANNETTA MADSEN, MD; OLIVIA CARDENAS-TROWERS, MD; OLUWATENIOLA BROWN, MD; MOIURI SIDDIQUE, MD; AND BLAIR WASHINGTON, MD, MHA (AUGUST 2021)
Dissenting opinion
“Race is real but it’s not biologic.” “Race is not based on genetic or biologic inheritance.” Am I the only one with a dissenting voice of opinion when it comes to these types of statements?
Scott Peters, MD
Oak Ridge, Tennessee
The Authors Respond
Thank you for your opinion, Dr. Peters. Although it is not completely clear what your question is, it seems that it concerns the validity of the idea that race is a social construct. We will address this question with the assumption that this letter was an effort to invite discussion and increase understanding.
The National Human Genome Research Institute describes race in this way: “Race is a fluid concept used to group people according to various factors, including ancestral background and social identity. Race is also used to group people that share a set of visible characteristics, such as skin color and facial features. Though these visible traits are influenced by genes, the vast majority of genetic variation exists within racial groups and not between them.”1
The understanding that race is a social construct has been upheld by numerous medical organizations. In August 2020, a Joint Statement was published by the American College of Obstetricians and Gynecologists, the American Board of Obstetricians and Gynecologists, and 22 other organizations representing our specialty. This document states: “Recognizing that race is a social construct, not biologically based, is important to understanding that racism, not race, impacts health care, health, and health outcomes.”2
This idea is also endorsed by the AMA, who in November 2020 adopted the following policies3:
- “Recognize that race is a social construct and is distinct from ethnicity, genetic ancestry, or biology
- Support ending the practice of using race as a proxy for biology or genetics in medical education, research, and clinical practice.”
There are numerous sources that further illuminate why race is a social construct. Here are a few:
- https://www.racepowerofanillusion .org/resources/
- https ://www.pewresearch.org /fact-tank/2020/02/25/the-changing -categories-the-u-s-has-used-to -measure-race/
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press. 2011.
- Yudell M, Roberts D, DeSalle R, et al. Science and society. Taking race out of human genetics. Science. 2016;351(6273):564-5. doi: 10.1126/science.aac4951.
References
- National Human Genome Research Institute. Race. https://www.genome.gov/genetic-glossary /Race. Accessed December 27, 2021.
- The American College of Obstetricians and Gynecologists. Joint Statement: Collective Action Addressing Racism. https://www.acog.org /news/news-articles/2020/08/joint-statementobstetrics-and-gynecology-collective-actionaddressing-racism.
- O’Reilly KB. AMA: Racism is a threat to public health. November 16, 2020. https://www.ama -assn.org/delivering-care/health-equity/ama -racism-threat-public-health. Accessed December 27, 2021.
HOW TO CHOOSE THE RIGHT VAGINAL MOISTURIZER OR LUBRICANT FOR YOUR PATIENT
JOHN PENNYCUFF, MD, MSPH, AND CHERYL IGLESIA, MD (JUNE 2021)
Which vaginal products to recommend
We applaud Drs. Pennycuff and Iglesia for providing education on lubricants and vaginal moisturizers in their recent article, and agree that ObGyns, urogynecologists, and primary care providers should be aware of the types of products available. However, the authors underplayed the health risks associated with the use of poor-quality lubricants and moisturizers.
Women often turn to lubricants or vaginal moisturizers because they experience vaginal dryness during intercourse, related to menopause, and from certain medications. Vaginal fluid is primarily composed of exudate from capillaries in the vaginal wall. During sexual arousal, blood flow to the vaginal wall increases, and in turn, this should increase exudate. But chronic inflammation can suppress these increases in vaginal blood flow, preventing adequate vaginal fluid production. One such cause of chronic inflammation is using hyperosmolar lubricants, as this has been shown to negatively affect the vaginal epithelium.1,2 In this way, use of hyperosmolar lubricants can actually worsen symptoms, creating a vicious circle of dryness, lubricant use, and worsening dryness.
In addition, hyperosmolar lubricants have been shown to reduce the epithelial barrier properties of the vaginal epithelium, increasing susceptibility to microbes associated with bacterial vaginosis and to true pathogens, including herpes simplex virus type 2.3 In fact, hyperosmolar lubricants are a serious enough problem that the World Health Organization has weighed in, recommending osmolality of personal lubricants be under 380 mOsm/kg to prevent damage to the vaginal epithelium.4
Appropriately acidic pH is just as critical as osmolality. Using products with a pH higher than 4.5 will reduce amounts of protective lactobacilli and other commensal vaginal bacteria, encouraging growth of opportunistic bacteria and yeast already present. This can lead to bacterial vaginosis, aerobic vaginitis, and candidiasis. Bacterial vaginosis can lead to other serious sequelae such as increased risk in acquisition of HIV infection and preterm birth in pregnancy. Unfortunately, much of the data cited in Drs. Pennycuff and Iglesia’s article were sourced from another study (by Edwards and Panay published in Climacteric in 2016), which measured product pH values with an inappropriately calibrated device; the study’s supplemental information stated that calibration was between 5 and 9, and so any measurement below 5 was invalid and subject to error. For example, the Good Clean Love lubricant is listed as having a pH of 4.7, but its pH is never higher than 4.4.
The products on the market that meet the dual criteria of appropriate pH and isotonicity to vaginal epithelial cells may be less well known to consumers. But this should not be a reason to encourage use of hyperosmolar products whose main selling point is that they are the “leading brand.” Educating women on their choices in personal lubricants should include a full discussion of product ingredients and properties, based upon the available literature to help them select a product that supports the health of their intimate tissues.
Members of the Scientific Advisory Board for the Sexual Health and Wellness Institute: Jill Krapf, MD, MEd, IF; Cathy Chung Hwa Yi, MD; Christine Enzmann, MD, PhD, NMCP; Susan Kellogg-Spadt, PhD, CRNP, IF, CSC, FCST; Betsy Greenleaf, DO, MBA; Elizabeth DuPriest, PhD
References
- Dezzutti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV-1 activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal .pone.0048328.
- Ayehunie S, Wang YY, Landry T, et al. Hyperosmolal vaginal lubricants markedly reduce epithelial barrier properties in a threedimensional vaginal epithelium model. Toxicol Rep. 2017;5:134-140. doi: 10.1016 /j.toxrep.2017.12.011.
- Moench TR, Mumper RJ, Hoen TE, et al. Microbicide excipients can greatly increase susceptibility to genital herpes transmission in the mouse. BMC Infect Dis. 2010;10:331. doi: 10.1186/1471 -2334-10-331.
- Use and procurement of additional lubricants for male and female condoms: WHO/UNFPA /FHI360 Advisory note. World Health Organization, 2012. http://apps.who.int/iris/bitstream /handle/10665/76580/WHO_RHR_12.33_eng .pdf?sequence=1. Accessed December 27, 2021.
Drs. Pennycuff And Iglesia Respond
We thank the members of the scientific advisory board for the Sexual Health and Wellness Institute for their thoughtful and insightful comments to our article. We agree with their comments on the importance of both pH and osmolality for vaginal moisturizers and lubricants. We also agree that selection of an incorrectly formulated product may lead to worsening of vulvovaginal symptoms as well as dysbiosis and all of its sequelae as the letter writers mentioned.
In writing the review article, we attempted to address the role that pH and osmolality play in vaginal moisturizers and lubricants and make clinicians more aware of the importance of these factors in product formulation. Our goal was to help to improve patient counseling. We tried to amass as much of the available literature as we could to act as a resource for practitioners, such as the table included in the article as well as the supplemental table included online. We hoped that by writing this article we would heighten awareness among female health practitioners about vaginal health products and encourage them to consider those products that may be better suited for their patients based on pH and osmolality.
While there remains a paucity of research on vaginal moisturizers and lubricants, there is even less consumer knowledge regarding ingredients and formulations of these products. We wholeheartedly agree with the scientific advisory board that we as health providers need to help educate women on the full spectrum of products available beyond the “leading brands.” Furthermore, we advocate that there be continued research on these products as well as more manufacturer transparency regarding not only the ingredients contained within these products but also the pH and osmolality. Simple steps such as these would ensure that providers could help counsel patients to make informed decisions regarding products for their pelvic health.
Continue to: DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES...
DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES
CASSANDRA CARBERRY, MD, MS; ANNETTA MADSEN, MD; OLIVIA CARDENAS-TROWERS, MD; OLUWATENIOLA BROWN, MD; MOIURI SIDDIQUE, MD; AND BLAIR WASHINGTON, MD, MHA (AUGUST 2021)
Dissenting opinion
“Race is real but it’s not biologic.” “Race is not based on genetic or biologic inheritance.” Am I the only one with a dissenting voice of opinion when it comes to these types of statements?
Scott Peters, MD
Oak Ridge, Tennessee
The Authors Respond
Thank you for your opinion, Dr. Peters. Although it is not completely clear what your question is, it seems that it concerns the validity of the idea that race is a social construct. We will address this question with the assumption that this letter was an effort to invite discussion and increase understanding.
The National Human Genome Research Institute describes race in this way: “Race is a fluid concept used to group people according to various factors, including ancestral background and social identity. Race is also used to group people that share a set of visible characteristics, such as skin color and facial features. Though these visible traits are influenced by genes, the vast majority of genetic variation exists within racial groups and not between them.”1
The understanding that race is a social construct has been upheld by numerous medical organizations. In August 2020, a Joint Statement was published by the American College of Obstetricians and Gynecologists, the American Board of Obstetricians and Gynecologists, and 22 other organizations representing our specialty. This document states: “Recognizing that race is a social construct, not biologically based, is important to understanding that racism, not race, impacts health care, health, and health outcomes.”2
This idea is also endorsed by the AMA, who in November 2020 adopted the following policies3:
- “Recognize that race is a social construct and is distinct from ethnicity, genetic ancestry, or biology
- Support ending the practice of using race as a proxy for biology or genetics in medical education, research, and clinical practice.”
There are numerous sources that further illuminate why race is a social construct. Here are a few:
- https://www.racepowerofanillusion .org/resources/
- https ://www.pewresearch.org /fact-tank/2020/02/25/the-changing -categories-the-u-s-has-used-to -measure-race/
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press. 2011.
- Yudell M, Roberts D, DeSalle R, et al. Science and society. Taking race out of human genetics. Science. 2016;351(6273):564-5. doi: 10.1126/science.aac4951.
References
- National Human Genome Research Institute. Race. https://www.genome.gov/genetic-glossary /Race. Accessed December 27, 2021.
- The American College of Obstetricians and Gynecologists. Joint Statement: Collective Action Addressing Racism. https://www.acog.org /news/news-articles/2020/08/joint-statementobstetrics-and-gynecology-collective-actionaddressing-racism.
- O’Reilly KB. AMA: Racism is a threat to public health. November 16, 2020. https://www.ama -assn.org/delivering-care/health-equity/ama -racism-threat-public-health. Accessed December 27, 2021.
HOW TO CHOOSE THE RIGHT VAGINAL MOISTURIZER OR LUBRICANT FOR YOUR PATIENT
JOHN PENNYCUFF, MD, MSPH, AND CHERYL IGLESIA, MD (JUNE 2021)
Which vaginal products to recommend
We applaud Drs. Pennycuff and Iglesia for providing education on lubricants and vaginal moisturizers in their recent article, and agree that ObGyns, urogynecologists, and primary care providers should be aware of the types of products available. However, the authors underplayed the health risks associated with the use of poor-quality lubricants and moisturizers.
Women often turn to lubricants or vaginal moisturizers because they experience vaginal dryness during intercourse, related to menopause, and from certain medications. Vaginal fluid is primarily composed of exudate from capillaries in the vaginal wall. During sexual arousal, blood flow to the vaginal wall increases, and in turn, this should increase exudate. But chronic inflammation can suppress these increases in vaginal blood flow, preventing adequate vaginal fluid production. One such cause of chronic inflammation is using hyperosmolar lubricants, as this has been shown to negatively affect the vaginal epithelium.1,2 In this way, use of hyperosmolar lubricants can actually worsen symptoms, creating a vicious circle of dryness, lubricant use, and worsening dryness.
In addition, hyperosmolar lubricants have been shown to reduce the epithelial barrier properties of the vaginal epithelium, increasing susceptibility to microbes associated with bacterial vaginosis and to true pathogens, including herpes simplex virus type 2.3 In fact, hyperosmolar lubricants are a serious enough problem that the World Health Organization has weighed in, recommending osmolality of personal lubricants be under 380 mOsm/kg to prevent damage to the vaginal epithelium.4
Appropriately acidic pH is just as critical as osmolality. Using products with a pH higher than 4.5 will reduce amounts of protective lactobacilli and other commensal vaginal bacteria, encouraging growth of opportunistic bacteria and yeast already present. This can lead to bacterial vaginosis, aerobic vaginitis, and candidiasis. Bacterial vaginosis can lead to other serious sequelae such as increased risk in acquisition of HIV infection and preterm birth in pregnancy. Unfortunately, much of the data cited in Drs. Pennycuff and Iglesia’s article were sourced from another study (by Edwards and Panay published in Climacteric in 2016), which measured product pH values with an inappropriately calibrated device; the study’s supplemental information stated that calibration was between 5 and 9, and so any measurement below 5 was invalid and subject to error. For example, the Good Clean Love lubricant is listed as having a pH of 4.7, but its pH is never higher than 4.4.
The products on the market that meet the dual criteria of appropriate pH and isotonicity to vaginal epithelial cells may be less well known to consumers. But this should not be a reason to encourage use of hyperosmolar products whose main selling point is that they are the “leading brand.” Educating women on their choices in personal lubricants should include a full discussion of product ingredients and properties, based upon the available literature to help them select a product that supports the health of their intimate tissues.
Members of the Scientific Advisory Board for the Sexual Health and Wellness Institute: Jill Krapf, MD, MEd, IF; Cathy Chung Hwa Yi, MD; Christine Enzmann, MD, PhD, NMCP; Susan Kellogg-Spadt, PhD, CRNP, IF, CSC, FCST; Betsy Greenleaf, DO, MBA; Elizabeth DuPriest, PhD
References
- Dezzutti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV-1 activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal .pone.0048328.
- Ayehunie S, Wang YY, Landry T, et al. Hyperosmolal vaginal lubricants markedly reduce epithelial barrier properties in a threedimensional vaginal epithelium model. Toxicol Rep. 2017;5:134-140. doi: 10.1016 /j.toxrep.2017.12.011.
- Moench TR, Mumper RJ, Hoen TE, et al. Microbicide excipients can greatly increase susceptibility to genital herpes transmission in the mouse. BMC Infect Dis. 2010;10:331. doi: 10.1186/1471 -2334-10-331.
- Use and procurement of additional lubricants for male and female condoms: WHO/UNFPA /FHI360 Advisory note. World Health Organization, 2012. http://apps.who.int/iris/bitstream /handle/10665/76580/WHO_RHR_12.33_eng .pdf?sequence=1. Accessed December 27, 2021.
Drs. Pennycuff And Iglesia Respond
We thank the members of the scientific advisory board for the Sexual Health and Wellness Institute for their thoughtful and insightful comments to our article. We agree with their comments on the importance of both pH and osmolality for vaginal moisturizers and lubricants. We also agree that selection of an incorrectly formulated product may lead to worsening of vulvovaginal symptoms as well as dysbiosis and all of its sequelae as the letter writers mentioned.
In writing the review article, we attempted to address the role that pH and osmolality play in vaginal moisturizers and lubricants and make clinicians more aware of the importance of these factors in product formulation. Our goal was to help to improve patient counseling. We tried to amass as much of the available literature as we could to act as a resource for practitioners, such as the table included in the article as well as the supplemental table included online. We hoped that by writing this article we would heighten awareness among female health practitioners about vaginal health products and encourage them to consider those products that may be better suited for their patients based on pH and osmolality.
While there remains a paucity of research on vaginal moisturizers and lubricants, there is even less consumer knowledge regarding ingredients and formulations of these products. We wholeheartedly agree with the scientific advisory board that we as health providers need to help educate women on the full spectrum of products available beyond the “leading brands.” Furthermore, we advocate that there be continued research on these products as well as more manufacturer transparency regarding not only the ingredients contained within these products but also the pH and osmolality. Simple steps such as these would ensure that providers could help counsel patients to make informed decisions regarding products for their pelvic health.
Continue to: DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES...
DISMANTLING RACISM IN YOUR PERSONAL AND PROFESSIONAL SPHERES
CASSANDRA CARBERRY, MD, MS; ANNETTA MADSEN, MD; OLIVIA CARDENAS-TROWERS, MD; OLUWATENIOLA BROWN, MD; MOIURI SIDDIQUE, MD; AND BLAIR WASHINGTON, MD, MHA (AUGUST 2021)
Dissenting opinion
“Race is real but it’s not biologic.” “Race is not based on genetic or biologic inheritance.” Am I the only one with a dissenting voice of opinion when it comes to these types of statements?
Scott Peters, MD
Oak Ridge, Tennessee
The Authors Respond
Thank you for your opinion, Dr. Peters. Although it is not completely clear what your question is, it seems that it concerns the validity of the idea that race is a social construct. We will address this question with the assumption that this letter was an effort to invite discussion and increase understanding.
The National Human Genome Research Institute describes race in this way: “Race is a fluid concept used to group people according to various factors, including ancestral background and social identity. Race is also used to group people that share a set of visible characteristics, such as skin color and facial features. Though these visible traits are influenced by genes, the vast majority of genetic variation exists within racial groups and not between them.”1
The understanding that race is a social construct has been upheld by numerous medical organizations. In August 2020, a Joint Statement was published by the American College of Obstetricians and Gynecologists, the American Board of Obstetricians and Gynecologists, and 22 other organizations representing our specialty. This document states: “Recognizing that race is a social construct, not biologically based, is important to understanding that racism, not race, impacts health care, health, and health outcomes.”2
This idea is also endorsed by the AMA, who in November 2020 adopted the following policies3:
- “Recognize that race is a social construct and is distinct from ethnicity, genetic ancestry, or biology
- Support ending the practice of using race as a proxy for biology or genetics in medical education, research, and clinical practice.”
There are numerous sources that further illuminate why race is a social construct. Here are a few:
- https://www.racepowerofanillusion .org/resources/
- https ://www.pewresearch.org /fact-tank/2020/02/25/the-changing -categories-the-u-s-has-used-to -measure-race/
- Roberts D. Fatal Invention: How Science, Politics and Big Business Re-create Race in the Twenty-First Century. The New Press. 2011.
- Yudell M, Roberts D, DeSalle R, et al. Science and society. Taking race out of human genetics. Science. 2016;351(6273):564-5. doi: 10.1126/science.aac4951.
References
- National Human Genome Research Institute. Race. https://www.genome.gov/genetic-glossary /Race. Accessed December 27, 2021.
- The American College of Obstetricians and Gynecologists. Joint Statement: Collective Action Addressing Racism. https://www.acog.org /news/news-articles/2020/08/joint-statementobstetrics-and-gynecology-collective-actionaddressing-racism.
- O’Reilly KB. AMA: Racism is a threat to public health. November 16, 2020. https://www.ama -assn.org/delivering-care/health-equity/ama -racism-threat-public-health. Accessed December 27, 2021.
Pooled Testing for SARS-CoV-2 for Resource Conservation in the Hospital: A Dynamic Process
Pooled testing for SARS-CoV-2 has been proposed as a strategy to facilitate testing and conserve scarce laboratory resources in a variety of settings. Previously in the Journal of Hospital Medicine, we reported our initial experience with pooled testing in low-risk admitted patients from April 17, 2020, to May 11, 2020, at Saratoga Hospital, Saratoga Springs, New York.1 Early in the pandemic, when testing resources were critically short, pooling allowed us to meet our clinical goal of testing all admitted inpatients. We now present our subsequent experience to emphasize the dynamic nature of this strategy when used to offer testing while conserving resources within a hospital system.
From April 17, 2020, to December 10, 2020, pooled testing using the GeneXpert system (Cepheid) was performed as previously described on all patients admitted from the emergency department (ED) of Saratoga Hospital who met criteria for being at low risk for SARS-CoV-2 infection.1 During this period, we had a low community prevalence (<1%-2%). In our low-risk admitted patients, an overall positive rate of 0.5% allowed us to expand the pool size from our initial reported size of three samples to a maximum of five samples. As ED volumes changed, pool sizes could be adjusted by clinical leaders as supplies allowed the demands of throughput to be met. These adjustments were facilitated by regular discussion of aggregate testing results, pool size, patient-flow issues, and supply levels among our staff. In December 2020, we experienced a marked increase in community prevalence and hospital admissions. This surge ended our use of pooling and required us to test each admitted patient with a single cartridge, which fortunately had become available.
During our period of pooling, we tested 7755 low-risk patients using 1738 cartridges (1177 pools of five samples; 211 pools of four samples; 326 pools of three samples; and 24 pools of two samples). We had 39 positive pooled cartridges, which required the use of 174 additional single cartridges. The instructions for use of this system with single cartridges report a negative percent agreement (sensitivity) of 95.6% and a positive percent agreement (specificity) of 97.8% in the lab.2 We did not have any patients who tested negative in a pool subsequently turn positive during admission unless they had a known in-hospital exposure; however, our public health service alerted us to several patients with high-risk exposures who were excluded from pooling. Our pooling strategy resulted in use of 5843 fewer cartridges than if each test had been performed on a single patient. The total savings on cartridges was $225,000. Pooling did not directly increase staff costs, but required significant individual and organizational energy and commitment. At times, pooling could delay throughput of admitted patients from the ED to inpatient beds. The testing process often added 60 to 90 minutes to throughput time. During the night, waiting for admissions to create a pool could also cause delay. Close and ongoing communication among our ED, inpatient teams, nursing, and laboratory was required to minimize these negative effects.
Pooling can be an effective method of resource conservation in low-risk populations. The theoretical benefits of pooling have been calculated in various scenarios3 and recently comprehensively reviewed with emphasis on selecting the pooling method.4 Practically, pooling has been aptly described as a complex undertaking that should be one part of a broad approach to achieving various COVID-19 control goals.5 Our experience is that, in the hospital setting, it is a dynamic process that requires repeatedly balancing clinical goals, organizational realities, laboratory and mathematical parameters, and competing staff duties. The potential costs and benefits may change over time. We found success was highly dependent on our staff, who were highly motivated by strongly agreeing with our commitment to test all inpatients and our desire to maintain adequate supplies to accomplish this goal.
1. Mastrianni D, Falivena R, Brooks T, et al. Pooled testing for SARS-CoV-2 in hospitalized patients. J Hosp Med. 2020;15:538-539. https://doi.org/10.12788/jhm.3501
2. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid; 2020. Accessed October 7, 2021. https://www.cepheid.com/Package%20Insert%20Files/Xpert%20Xpress%20SARS-CoV-2%20Assay%20ENGLISH%20Package%20Insert%20302-3787%20Rev.%20B.pdf
3. Abdalhamid B, Bilder CR, McCutchen EL, Hinrichs SH, Koepsell SA, Iwen PC. Assessment of specimen pooling to conserve SARS CoV-2 testing resources. Am J Clin Pathol. 2020;153(6):715-718. https://doi.org/10.1093/ajcp/aqaa064
4. Daniel EA, Esakialraj L BH, Anbalagan S, et al. Pooled testing strategies for SARS-CoV-2 diagnosis: a comprehensive review. Diagn Microbiol Infect Dis. 2021;101(2):115432. https://doi.org/10.1016/j.diagmicrobio.2021.115432
5. Schulte PA, Weissman DN, Luckhaupt SE, et al. Considerations for pooled testing of employees for SARS-CoV-2. J Occup Environ Med. 2021;63(1):1-9. https://doi.org/10.1097/JOM.0000000000002049
Pooled testing for SARS-CoV-2 has been proposed as a strategy to facilitate testing and conserve scarce laboratory resources in a variety of settings. Previously in the Journal of Hospital Medicine, we reported our initial experience with pooled testing in low-risk admitted patients from April 17, 2020, to May 11, 2020, at Saratoga Hospital, Saratoga Springs, New York.1 Early in the pandemic, when testing resources were critically short, pooling allowed us to meet our clinical goal of testing all admitted inpatients. We now present our subsequent experience to emphasize the dynamic nature of this strategy when used to offer testing while conserving resources within a hospital system.
From April 17, 2020, to December 10, 2020, pooled testing using the GeneXpert system (Cepheid) was performed as previously described on all patients admitted from the emergency department (ED) of Saratoga Hospital who met criteria for being at low risk for SARS-CoV-2 infection.1 During this period, we had a low community prevalence (<1%-2%). In our low-risk admitted patients, an overall positive rate of 0.5% allowed us to expand the pool size from our initial reported size of three samples to a maximum of five samples. As ED volumes changed, pool sizes could be adjusted by clinical leaders as supplies allowed the demands of throughput to be met. These adjustments were facilitated by regular discussion of aggregate testing results, pool size, patient-flow issues, and supply levels among our staff. In December 2020, we experienced a marked increase in community prevalence and hospital admissions. This surge ended our use of pooling and required us to test each admitted patient with a single cartridge, which fortunately had become available.
During our period of pooling, we tested 7755 low-risk patients using 1738 cartridges (1177 pools of five samples; 211 pools of four samples; 326 pools of three samples; and 24 pools of two samples). We had 39 positive pooled cartridges, which required the use of 174 additional single cartridges. The instructions for use of this system with single cartridges report a negative percent agreement (sensitivity) of 95.6% and a positive percent agreement (specificity) of 97.8% in the lab.2 We did not have any patients who tested negative in a pool subsequently turn positive during admission unless they had a known in-hospital exposure; however, our public health service alerted us to several patients with high-risk exposures who were excluded from pooling. Our pooling strategy resulted in use of 5843 fewer cartridges than if each test had been performed on a single patient. The total savings on cartridges was $225,000. Pooling did not directly increase staff costs, but required significant individual and organizational energy and commitment. At times, pooling could delay throughput of admitted patients from the ED to inpatient beds. The testing process often added 60 to 90 minutes to throughput time. During the night, waiting for admissions to create a pool could also cause delay. Close and ongoing communication among our ED, inpatient teams, nursing, and laboratory was required to minimize these negative effects.
Pooling can be an effective method of resource conservation in low-risk populations. The theoretical benefits of pooling have been calculated in various scenarios3 and recently comprehensively reviewed with emphasis on selecting the pooling method.4 Practically, pooling has been aptly described as a complex undertaking that should be one part of a broad approach to achieving various COVID-19 control goals.5 Our experience is that, in the hospital setting, it is a dynamic process that requires repeatedly balancing clinical goals, organizational realities, laboratory and mathematical parameters, and competing staff duties. The potential costs and benefits may change over time. We found success was highly dependent on our staff, who were highly motivated by strongly agreeing with our commitment to test all inpatients and our desire to maintain adequate supplies to accomplish this goal.
Pooled testing for SARS-CoV-2 has been proposed as a strategy to facilitate testing and conserve scarce laboratory resources in a variety of settings. Previously in the Journal of Hospital Medicine, we reported our initial experience with pooled testing in low-risk admitted patients from April 17, 2020, to May 11, 2020, at Saratoga Hospital, Saratoga Springs, New York.1 Early in the pandemic, when testing resources were critically short, pooling allowed us to meet our clinical goal of testing all admitted inpatients. We now present our subsequent experience to emphasize the dynamic nature of this strategy when used to offer testing while conserving resources within a hospital system.
From April 17, 2020, to December 10, 2020, pooled testing using the GeneXpert system (Cepheid) was performed as previously described on all patients admitted from the emergency department (ED) of Saratoga Hospital who met criteria for being at low risk for SARS-CoV-2 infection.1 During this period, we had a low community prevalence (<1%-2%). In our low-risk admitted patients, an overall positive rate of 0.5% allowed us to expand the pool size from our initial reported size of three samples to a maximum of five samples. As ED volumes changed, pool sizes could be adjusted by clinical leaders as supplies allowed the demands of throughput to be met. These adjustments were facilitated by regular discussion of aggregate testing results, pool size, patient-flow issues, and supply levels among our staff. In December 2020, we experienced a marked increase in community prevalence and hospital admissions. This surge ended our use of pooling and required us to test each admitted patient with a single cartridge, which fortunately had become available.
During our period of pooling, we tested 7755 low-risk patients using 1738 cartridges (1177 pools of five samples; 211 pools of four samples; 326 pools of three samples; and 24 pools of two samples). We had 39 positive pooled cartridges, which required the use of 174 additional single cartridges. The instructions for use of this system with single cartridges report a negative percent agreement (sensitivity) of 95.6% and a positive percent agreement (specificity) of 97.8% in the lab.2 We did not have any patients who tested negative in a pool subsequently turn positive during admission unless they had a known in-hospital exposure; however, our public health service alerted us to several patients with high-risk exposures who were excluded from pooling. Our pooling strategy resulted in use of 5843 fewer cartridges than if each test had been performed on a single patient. The total savings on cartridges was $225,000. Pooling did not directly increase staff costs, but required significant individual and organizational energy and commitment. At times, pooling could delay throughput of admitted patients from the ED to inpatient beds. The testing process often added 60 to 90 minutes to throughput time. During the night, waiting for admissions to create a pool could also cause delay. Close and ongoing communication among our ED, inpatient teams, nursing, and laboratory was required to minimize these negative effects.
Pooling can be an effective method of resource conservation in low-risk populations. The theoretical benefits of pooling have been calculated in various scenarios3 and recently comprehensively reviewed with emphasis on selecting the pooling method.4 Practically, pooling has been aptly described as a complex undertaking that should be one part of a broad approach to achieving various COVID-19 control goals.5 Our experience is that, in the hospital setting, it is a dynamic process that requires repeatedly balancing clinical goals, organizational realities, laboratory and mathematical parameters, and competing staff duties. The potential costs and benefits may change over time. We found success was highly dependent on our staff, who were highly motivated by strongly agreeing with our commitment to test all inpatients and our desire to maintain adequate supplies to accomplish this goal.
1. Mastrianni D, Falivena R, Brooks T, et al. Pooled testing for SARS-CoV-2 in hospitalized patients. J Hosp Med. 2020;15:538-539. https://doi.org/10.12788/jhm.3501
2. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid; 2020. Accessed October 7, 2021. https://www.cepheid.com/Package%20Insert%20Files/Xpert%20Xpress%20SARS-CoV-2%20Assay%20ENGLISH%20Package%20Insert%20302-3787%20Rev.%20B.pdf
3. Abdalhamid B, Bilder CR, McCutchen EL, Hinrichs SH, Koepsell SA, Iwen PC. Assessment of specimen pooling to conserve SARS CoV-2 testing resources. Am J Clin Pathol. 2020;153(6):715-718. https://doi.org/10.1093/ajcp/aqaa064
4. Daniel EA, Esakialraj L BH, Anbalagan S, et al. Pooled testing strategies for SARS-CoV-2 diagnosis: a comprehensive review. Diagn Microbiol Infect Dis. 2021;101(2):115432. https://doi.org/10.1016/j.diagmicrobio.2021.115432
5. Schulte PA, Weissman DN, Luckhaupt SE, et al. Considerations for pooled testing of employees for SARS-CoV-2. J Occup Environ Med. 2021;63(1):1-9. https://doi.org/10.1097/JOM.0000000000002049
1. Mastrianni D, Falivena R, Brooks T, et al. Pooled testing for SARS-CoV-2 in hospitalized patients. J Hosp Med. 2020;15:538-539. https://doi.org/10.12788/jhm.3501
2. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid; 2020. Accessed October 7, 2021. https://www.cepheid.com/Package%20Insert%20Files/Xpert%20Xpress%20SARS-CoV-2%20Assay%20ENGLISH%20Package%20Insert%20302-3787%20Rev.%20B.pdf
3. Abdalhamid B, Bilder CR, McCutchen EL, Hinrichs SH, Koepsell SA, Iwen PC. Assessment of specimen pooling to conserve SARS CoV-2 testing resources. Am J Clin Pathol. 2020;153(6):715-718. https://doi.org/10.1093/ajcp/aqaa064
4. Daniel EA, Esakialraj L BH, Anbalagan S, et al. Pooled testing strategies for SARS-CoV-2 diagnosis: a comprehensive review. Diagn Microbiol Infect Dis. 2021;101(2):115432. https://doi.org/10.1016/j.diagmicrobio.2021.115432
5. Schulte PA, Weissman DN, Luckhaupt SE, et al. Considerations for pooled testing of employees for SARS-CoV-2. J Occup Environ Med. 2021;63(1):1-9. https://doi.org/10.1097/JOM.0000000000002049
© 2021 Society of Hospital Medicine
Morning Discharges Are Also Not Associated With Emergency Department Boarding Times
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
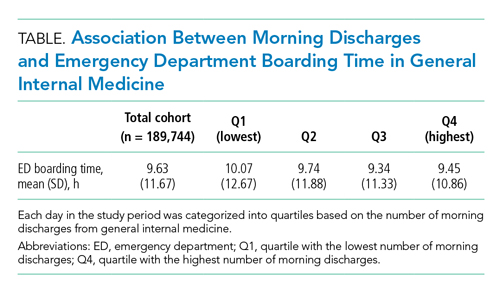
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
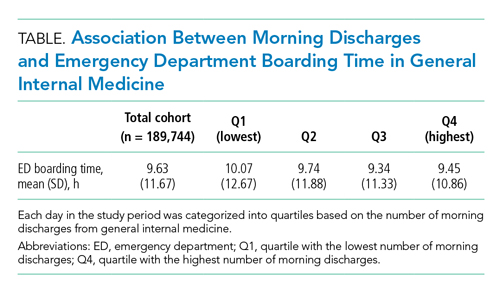
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
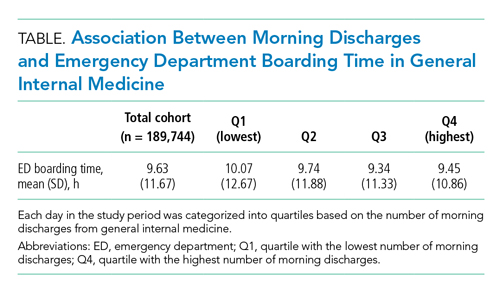
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
© 2021 Society of Hospital Medicine
COMMENT & CONTROVERSY
OBSTETRIC ANAL SPHINCTER INJURY: PREVENTION AND REPAIR
ROBERT L. BARBIERI, MD (EDITORIAL; MAY 2021)
Experience with warm perineal compresses and massage
I have been a midwife for 45 years. I have used warm compresses on the perineum my whole career. I don't need data to tell me it provides comfort. My patients do.
I don't do much massage of the perineum, only slightly while applying K-Y or another water-soluble gel.
A slow, controlled extension of the vertex and healthy tissue is the best way to prevent tears.
Karen Parker, MN, CNM
Ashland, Oregon
Dr. Barbieri responds
I thank Ms. Parker for her clinical recommendation: "Yes to warm compresses" and "Massage of the perineum?" Not so much.
Continue to: CESAREAN MYOMECTOMY...
CESAREAN MYOMECTOMY: SAFE OPERATION OR SURGICAL FOLLY?
ROBERT L. BARBIERI, MD (EDITORIAL; FEBRUARY 2021)
Timely comments on cesarean myomectomy
Dr. Barbieri's editorial on cesarean myomectomy is very timely, especially the quote from Dr. K.S.J. Olah: "The berating I received was severe and disproportionate to the crime. The rule was that myomectomy performed at cesarean section was not just frowned upon but expressly forbidden."
I had a very similar experience with panniculectomy and "tummy tuck" as a part of cesarean delivery (CD). Traditionally, a combination of a CD with any other surgical procedures (myomectomy, abdominoplasty, and so on) has not been accepted in the obstetric community. The main reason for such an opinion has been the unfounded fear of complications of combined procedures, including but not limited to infection, hematomas, and poor wound healing. None of these concerns have been supported by studies. Obvious advantages of combining a CD with other surgical procedures, including abdominoplasty, are obvious: the elimination of a second anesthesia, increased patient satisfaction, and no need for a second surgery.
We reviewed the outcomes in 52 patients who underwent a combination of CD with other procedures (such as panniculectomy, abdominoplasty, hernia repairs, myomectomies, and ovarian biopsies). The postsurgical outcomes included in the analysis were postsurgical fever and the presence of seromas, hematomas, and wound dehiscence.1 Twelve of our own patients had a panniculectomy during CD performed by a plastic surgeon. While the preoperative complications of panniculectomy may have been well described, there is a paucity of data in women who underwent the cosmetic procedure at the time of CD. We concluded that the performance of a panniculectomy and tummy tuck as part of a CD does not appear to increase surgical complications in patients with a high body mass index. Our preliminary results and call for further studies were received at the American College of Surgeons 2017 meeting in San Diego.2
Boris Petrikovsky, MD, PhD
Sunny Island Beach, Florida
References
1. Petrikovsky BM, Swancoat S, Zharov EV. Safety of panniculectomy during cesarean section: a prospective, non-randomized study. J Reprod Med. 2019;64:197-200.
2. Petrikovsky BM. Is the combination of panniculectomy and cesarean section safe? Scientific Poster Presentation-Obstetrics and Gynecology. J Am Coll Surg. 2017;225(4 suppl 2):E130.
Dr. Barbieri responds
I agree with Dr. Petrikovsky that advances in the field of obstetrical surgery have been inhibited by a tendency to criticize innovation. Less than 40 years ago, leaders in gynecology did not initially accept the application of minimally invasive gynecology surgical techniques to common gyn procedures including hysterectomy. Every surgical field is rapidly innovating. Obstetrical surgeons should be encouraged to pursue new approaches, as you are doing. We wish you success in your pioneering work.
Continue to: A CASE OF BV...
A CASE OF BV DURING PREGNANCY: BEST MANAGEMENT APPROACH
CALLIE FOX REEDER, MD, AND PATRICK DUFF, MD (ID CONSULT; FEBRUARY 2021)
Secnidazole for treatment of BV
The article by Drs. Reeder and Duff incorrectly states that there are no single-dose therapeutic options for bacterial vaginosis (BV) in the United States. Secnidazole 2 g single oral dose was approved by the US Food and Drug Administration (FDA) in 2017, and it is now included in the American College of Obstetricians and Gynecologists' (ACOG) clinical management guidelines for the treatment of BV in nonpregnant patients.
Secnidazole is not contraindicated in pregnancy. In a poster presented at the 2020 ACOG annual clinical meeting, we summarized results of the preclinical studies that were part of the FDA submission.1 There was no evidence of secnidazole toxicity in fertility and pre- and postnatal reproductive toxicology studies. In addition, there were no adverse developmental outcomes when secnidazole was administered orally to pregnant rats and rabbits during organogenesis at doses up to 4 times the clinical dose. These findings are consistent with the observation that no other preclinical studies, or experience from postmarketing use of secnidazole for approved indications, have suggested a risk of adverse effects when using secnidazole in pregnancy.
Steven E. Chavoustie, MD
North Miami, Florida
Reference
1. Pentikis H, Eder S, Kaufman G, Chavoustie S. Secnidazole, an approved single dose drug for bacterial vaginosis, does not cause reproductive toxicity in animals [16A]. Obstet Gynecol. 2020;135:12S.
Drs. Reeder and Duff respond
We are very appreciative of Dr. Chavoustie's interest in our article and for his thoughtful assessment of the role of single-dose secnidazole for the treatment of BV. As we noted in our article, this drug has been used extensively in Europe and Asia, but there is much less published experience with the drug in the United States. We pointed out the excellent results reported by Hillier and colleagues with 1-g and 2-g doses of this medication.1 Dr. Chavoustie is correct in stating that there is no risk of fetal harm based on animal data at up to 4 times the recommended human dose, although the manufacturer recommends discontinuing breastfeeding during, and for 96 hours after, treatment. According to www.goodrx.com, the cost of a single 2-g dose of secnidazole is $325; the cost of a 7-day course of metronidazole is approximately $16.
Reference
1. Hillier SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
Continue to: OPTIMIZING THE USE OF...
OPTIMIZING THE USE OF OXYTOCIN ON LABOR AND DELIVERY
ROBERT L. BARBIERI, MD (EDITORIAL; JANUARY 2021)
Vigilant labor progress aids in oxytocin optimization
I read with particular interest Dr. Barbieri's editorial on optimizing oxytocin infusion. This topic is relevant for my practice as I am the kind of physician described and I usually get upset when the oxytocin is not managed as I ordered.
In my opinion, several things need clarification. On our unit, the most significant point of controversy is the definition of tachysystole, mainly when we are using a tocodynamometer and not an internal transducer.
I contend that it is quite challenging to ascertain the effectiveness of any given labor pattern based only on the number of contractions. Although we joke about "pit to distress," the truth is that contractions need to be "effective," which to me means strong enough to induce cervical changes.
In my clinical practice, with a tocodynamometer, having 5 contractions that do not produce cervical changes (unless associated with abnormalities of the fetal heart rate tracing) is not a clinically relevant finding as we do not have a way to gauge the strength of such contractions.
I usually employ a mid-range oxytocin protocol, starting at 4 mU per minute and increasing by 4 mU every 20 minutes. Through 30 years of practicing obstetrics, I have found that this protocol renders excellent results in achieving an efficient labor pattern without jeopardizing fetal well-being.
On learning about oxytocin's pharmacokinetics, I still support Dr. Rhonda L. Perry and her colleagues' conclusion that, until we learn better about this aspect of oxytocin pharmacology, each woman is her own bioassay.1 Furthermore, we see this in our daily practice: some patients go into full efficient labor with oxytocin at 4 mU per minute while others at 30 mU per minute do zilch.
Based on the above, I think that optimization requires close vigilance of the labor and the fetal status at any given time, not determining an oxytocin rate of infusion or dosage.
We should be observant on evaluating labor progress, and we should not hesitate to use internal pressure catheters when needed to obtain a more accurate evaluation of the labor pattern.
By examining the patient's labor progress at regular intervals, we also optimize the oxytocin infusion by determining if the infusion is producing the expected cervical changes.
Tomas Hernandez-Mejia, MD
Pasco, Washington
Reference
1. Perry RL, Satin AJ, Barth WH, et al. The pharmacokinetics of oxytocin as they apply to labor induction. Am J Obstet Gynecol. 1996;174:1590-1593.
Dr. Barbieri responds
I thank Dr. Tomas Hernandez-Mejia for sharing his expertise in utilizing a higher dose of oxytocin to optimize labor and birth. Dr. Hernandez-Mejia's view is supported by the recent publication of a high-quality clinical trial showing that a high-dose oxytocin protocol (initial and incremental rate of 6 mIU/min) did not cause an increase in adverse perinatal outcomes compared with a standard-dose protocol (initial and incremental rate of 2 mIU/min) but slightly shortened the duration of labor.1 Based on this clinical trial, my conclusion is that the high-dose protocol, if appropriately monitored for excess uterine contractions and fetal heart rate pattern, is safe.
Reference
1. Son M, Roy A, Stetson BT, et al. High-dose compared with standard-dose oxytocin regimens to augment labor in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2021;137:991-998.
Continue to: PREGNANCY OF UNKNOWN...
PREGNANCY OF UNKNOWN LOCATION: EVIDENCE-BASED EVALUATION AND MANAGEMENT
IRIS G. INSOGNA, MD, AND PAULA C. BRADY, MD (AUGUST 2020)
I would like to thank Dr. Iris Insogna and Dr. Paula Brady for their very informative article on pregnancy of unknown location. However, please allow me to make a suggestion that will clarify terminology for all practicing ObGyns.
The medical literature uses the terms cornual pregnancy and interstitial pregnancy interchangeably, although they are actually very different conditions and have significant different implications. Clinicians are often confused about which is an intrauterine pregnancy and which is a true ectopic pregnancy. This confusion was addressed in a 2006 article in Fertility and Sterility, which explains that a cornual pregnancy refers to the implantation and development of a gestation in one of the upper and lateral portions of the uterus.1 This may occur in a rudimentary horn or in one horn of a septate or bicornuate uterus. Conversely, an interstitial pregnancy is a gestation that implants within the proximal, intramural portion of the fallopian tube that is enveloped by myometrium. Therefore, a cornual pregnancy is actually an intrauterine pregnancy, whereas an interstitial pregnancy is a true ectopic pregnancy.
I hope that all clinicians will read the article in Fertility and Sterility and adopt this terminology to avoid future confusion and misunderstandings.
Alan D. Rosen, MD
Houston, Texas
Reference
1. Malinowski A, Bates SK. Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril. 2006;86:1764.e11-1764.e14.
OBSTETRIC ANAL SPHINCTER INJURY: PREVENTION AND REPAIR
ROBERT L. BARBIERI, MD (EDITORIAL; MAY 2021)
Experience with warm perineal compresses and massage
I have been a midwife for 45 years. I have used warm compresses on the perineum my whole career. I don't need data to tell me it provides comfort. My patients do.
I don't do much massage of the perineum, only slightly while applying K-Y or another water-soluble gel.
A slow, controlled extension of the vertex and healthy tissue is the best way to prevent tears.
Karen Parker, MN, CNM
Ashland, Oregon
Dr. Barbieri responds
I thank Ms. Parker for her clinical recommendation: "Yes to warm compresses" and "Massage of the perineum?" Not so much.
Continue to: CESAREAN MYOMECTOMY...
CESAREAN MYOMECTOMY: SAFE OPERATION OR SURGICAL FOLLY?
ROBERT L. BARBIERI, MD (EDITORIAL; FEBRUARY 2021)
Timely comments on cesarean myomectomy
Dr. Barbieri's editorial on cesarean myomectomy is very timely, especially the quote from Dr. K.S.J. Olah: "The berating I received was severe and disproportionate to the crime. The rule was that myomectomy performed at cesarean section was not just frowned upon but expressly forbidden."
I had a very similar experience with panniculectomy and "tummy tuck" as a part of cesarean delivery (CD). Traditionally, a combination of a CD with any other surgical procedures (myomectomy, abdominoplasty, and so on) has not been accepted in the obstetric community. The main reason for such an opinion has been the unfounded fear of complications of combined procedures, including but not limited to infection, hematomas, and poor wound healing. None of these concerns have been supported by studies. Obvious advantages of combining a CD with other surgical procedures, including abdominoplasty, are obvious: the elimination of a second anesthesia, increased patient satisfaction, and no need for a second surgery.
We reviewed the outcomes in 52 patients who underwent a combination of CD with other procedures (such as panniculectomy, abdominoplasty, hernia repairs, myomectomies, and ovarian biopsies). The postsurgical outcomes included in the analysis were postsurgical fever and the presence of seromas, hematomas, and wound dehiscence.1 Twelve of our own patients had a panniculectomy during CD performed by a plastic surgeon. While the preoperative complications of panniculectomy may have been well described, there is a paucity of data in women who underwent the cosmetic procedure at the time of CD. We concluded that the performance of a panniculectomy and tummy tuck as part of a CD does not appear to increase surgical complications in patients with a high body mass index. Our preliminary results and call for further studies were received at the American College of Surgeons 2017 meeting in San Diego.2
Boris Petrikovsky, MD, PhD
Sunny Island Beach, Florida
References
1. Petrikovsky BM, Swancoat S, Zharov EV. Safety of panniculectomy during cesarean section: a prospective, non-randomized study. J Reprod Med. 2019;64:197-200.
2. Petrikovsky BM. Is the combination of panniculectomy and cesarean section safe? Scientific Poster Presentation-Obstetrics and Gynecology. J Am Coll Surg. 2017;225(4 suppl 2):E130.
Dr. Barbieri responds
I agree with Dr. Petrikovsky that advances in the field of obstetrical surgery have been inhibited by a tendency to criticize innovation. Less than 40 years ago, leaders in gynecology did not initially accept the application of minimally invasive gynecology surgical techniques to common gyn procedures including hysterectomy. Every surgical field is rapidly innovating. Obstetrical surgeons should be encouraged to pursue new approaches, as you are doing. We wish you success in your pioneering work.
Continue to: A CASE OF BV...
A CASE OF BV DURING PREGNANCY: BEST MANAGEMENT APPROACH
CALLIE FOX REEDER, MD, AND PATRICK DUFF, MD (ID CONSULT; FEBRUARY 2021)
Secnidazole for treatment of BV
The article by Drs. Reeder and Duff incorrectly states that there are no single-dose therapeutic options for bacterial vaginosis (BV) in the United States. Secnidazole 2 g single oral dose was approved by the US Food and Drug Administration (FDA) in 2017, and it is now included in the American College of Obstetricians and Gynecologists' (ACOG) clinical management guidelines for the treatment of BV in nonpregnant patients.
Secnidazole is not contraindicated in pregnancy. In a poster presented at the 2020 ACOG annual clinical meeting, we summarized results of the preclinical studies that were part of the FDA submission.1 There was no evidence of secnidazole toxicity in fertility and pre- and postnatal reproductive toxicology studies. In addition, there were no adverse developmental outcomes when secnidazole was administered orally to pregnant rats and rabbits during organogenesis at doses up to 4 times the clinical dose. These findings are consistent with the observation that no other preclinical studies, or experience from postmarketing use of secnidazole for approved indications, have suggested a risk of adverse effects when using secnidazole in pregnancy.
Steven E. Chavoustie, MD
North Miami, Florida
Reference
1. Pentikis H, Eder S, Kaufman G, Chavoustie S. Secnidazole, an approved single dose drug for bacterial vaginosis, does not cause reproductive toxicity in animals [16A]. Obstet Gynecol. 2020;135:12S.
Drs. Reeder and Duff respond
We are very appreciative of Dr. Chavoustie's interest in our article and for his thoughtful assessment of the role of single-dose secnidazole for the treatment of BV. As we noted in our article, this drug has been used extensively in Europe and Asia, but there is much less published experience with the drug in the United States. We pointed out the excellent results reported by Hillier and colleagues with 1-g and 2-g doses of this medication.1 Dr. Chavoustie is correct in stating that there is no risk of fetal harm based on animal data at up to 4 times the recommended human dose, although the manufacturer recommends discontinuing breastfeeding during, and for 96 hours after, treatment. According to www.goodrx.com, the cost of a single 2-g dose of secnidazole is $325; the cost of a 7-day course of metronidazole is approximately $16.
Reference
1. Hillier SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
Continue to: OPTIMIZING THE USE OF...
OPTIMIZING THE USE OF OXYTOCIN ON LABOR AND DELIVERY
ROBERT L. BARBIERI, MD (EDITORIAL; JANUARY 2021)
Vigilant labor progress aids in oxytocin optimization
I read with particular interest Dr. Barbieri's editorial on optimizing oxytocin infusion. This topic is relevant for my practice as I am the kind of physician described and I usually get upset when the oxytocin is not managed as I ordered.
In my opinion, several things need clarification. On our unit, the most significant point of controversy is the definition of tachysystole, mainly when we are using a tocodynamometer and not an internal transducer.
I contend that it is quite challenging to ascertain the effectiveness of any given labor pattern based only on the number of contractions. Although we joke about "pit to distress," the truth is that contractions need to be "effective," which to me means strong enough to induce cervical changes.
In my clinical practice, with a tocodynamometer, having 5 contractions that do not produce cervical changes (unless associated with abnormalities of the fetal heart rate tracing) is not a clinically relevant finding as we do not have a way to gauge the strength of such contractions.
I usually employ a mid-range oxytocin protocol, starting at 4 mU per minute and increasing by 4 mU every 20 minutes. Through 30 years of practicing obstetrics, I have found that this protocol renders excellent results in achieving an efficient labor pattern without jeopardizing fetal well-being.
On learning about oxytocin's pharmacokinetics, I still support Dr. Rhonda L. Perry and her colleagues' conclusion that, until we learn better about this aspect of oxytocin pharmacology, each woman is her own bioassay.1 Furthermore, we see this in our daily practice: some patients go into full efficient labor with oxytocin at 4 mU per minute while others at 30 mU per minute do zilch.
Based on the above, I think that optimization requires close vigilance of the labor and the fetal status at any given time, not determining an oxytocin rate of infusion or dosage.
We should be observant on evaluating labor progress, and we should not hesitate to use internal pressure catheters when needed to obtain a more accurate evaluation of the labor pattern.
By examining the patient's labor progress at regular intervals, we also optimize the oxytocin infusion by determining if the infusion is producing the expected cervical changes.
Tomas Hernandez-Mejia, MD
Pasco, Washington
Reference
1. Perry RL, Satin AJ, Barth WH, et al. The pharmacokinetics of oxytocin as they apply to labor induction. Am J Obstet Gynecol. 1996;174:1590-1593.
Dr. Barbieri responds
I thank Dr. Tomas Hernandez-Mejia for sharing his expertise in utilizing a higher dose of oxytocin to optimize labor and birth. Dr. Hernandez-Mejia's view is supported by the recent publication of a high-quality clinical trial showing that a high-dose oxytocin protocol (initial and incremental rate of 6 mIU/min) did not cause an increase in adverse perinatal outcomes compared with a standard-dose protocol (initial and incremental rate of 2 mIU/min) but slightly shortened the duration of labor.1 Based on this clinical trial, my conclusion is that the high-dose protocol, if appropriately monitored for excess uterine contractions and fetal heart rate pattern, is safe.
Reference
1. Son M, Roy A, Stetson BT, et al. High-dose compared with standard-dose oxytocin regimens to augment labor in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2021;137:991-998.
Continue to: PREGNANCY OF UNKNOWN...
PREGNANCY OF UNKNOWN LOCATION: EVIDENCE-BASED EVALUATION AND MANAGEMENT
IRIS G. INSOGNA, MD, AND PAULA C. BRADY, MD (AUGUST 2020)
I would like to thank Dr. Iris Insogna and Dr. Paula Brady for their very informative article on pregnancy of unknown location. However, please allow me to make a suggestion that will clarify terminology for all practicing ObGyns.
The medical literature uses the terms cornual pregnancy and interstitial pregnancy interchangeably, although they are actually very different conditions and have significant different implications. Clinicians are often confused about which is an intrauterine pregnancy and which is a true ectopic pregnancy. This confusion was addressed in a 2006 article in Fertility and Sterility, which explains that a cornual pregnancy refers to the implantation and development of a gestation in one of the upper and lateral portions of the uterus.1 This may occur in a rudimentary horn or in one horn of a septate or bicornuate uterus. Conversely, an interstitial pregnancy is a gestation that implants within the proximal, intramural portion of the fallopian tube that is enveloped by myometrium. Therefore, a cornual pregnancy is actually an intrauterine pregnancy, whereas an interstitial pregnancy is a true ectopic pregnancy.
I hope that all clinicians will read the article in Fertility and Sterility and adopt this terminology to avoid future confusion and misunderstandings.
Alan D. Rosen, MD
Houston, Texas
Reference
1. Malinowski A, Bates SK. Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril. 2006;86:1764.e11-1764.e14.
OBSTETRIC ANAL SPHINCTER INJURY: PREVENTION AND REPAIR
ROBERT L. BARBIERI, MD (EDITORIAL; MAY 2021)
Experience with warm perineal compresses and massage
I have been a midwife for 45 years. I have used warm compresses on the perineum my whole career. I don't need data to tell me it provides comfort. My patients do.
I don't do much massage of the perineum, only slightly while applying K-Y or another water-soluble gel.
A slow, controlled extension of the vertex and healthy tissue is the best way to prevent tears.
Karen Parker, MN, CNM
Ashland, Oregon
Dr. Barbieri responds
I thank Ms. Parker for her clinical recommendation: "Yes to warm compresses" and "Massage of the perineum?" Not so much.
Continue to: CESAREAN MYOMECTOMY...
CESAREAN MYOMECTOMY: SAFE OPERATION OR SURGICAL FOLLY?
ROBERT L. BARBIERI, MD (EDITORIAL; FEBRUARY 2021)
Timely comments on cesarean myomectomy
Dr. Barbieri's editorial on cesarean myomectomy is very timely, especially the quote from Dr. K.S.J. Olah: "The berating I received was severe and disproportionate to the crime. The rule was that myomectomy performed at cesarean section was not just frowned upon but expressly forbidden."
I had a very similar experience with panniculectomy and "tummy tuck" as a part of cesarean delivery (CD). Traditionally, a combination of a CD with any other surgical procedures (myomectomy, abdominoplasty, and so on) has not been accepted in the obstetric community. The main reason for such an opinion has been the unfounded fear of complications of combined procedures, including but not limited to infection, hematomas, and poor wound healing. None of these concerns have been supported by studies. Obvious advantages of combining a CD with other surgical procedures, including abdominoplasty, are obvious: the elimination of a second anesthesia, increased patient satisfaction, and no need for a second surgery.
We reviewed the outcomes in 52 patients who underwent a combination of CD with other procedures (such as panniculectomy, abdominoplasty, hernia repairs, myomectomies, and ovarian biopsies). The postsurgical outcomes included in the analysis were postsurgical fever and the presence of seromas, hematomas, and wound dehiscence.1 Twelve of our own patients had a panniculectomy during CD performed by a plastic surgeon. While the preoperative complications of panniculectomy may have been well described, there is a paucity of data in women who underwent the cosmetic procedure at the time of CD. We concluded that the performance of a panniculectomy and tummy tuck as part of a CD does not appear to increase surgical complications in patients with a high body mass index. Our preliminary results and call for further studies were received at the American College of Surgeons 2017 meeting in San Diego.2
Boris Petrikovsky, MD, PhD
Sunny Island Beach, Florida
References
1. Petrikovsky BM, Swancoat S, Zharov EV. Safety of panniculectomy during cesarean section: a prospective, non-randomized study. J Reprod Med. 2019;64:197-200.
2. Petrikovsky BM. Is the combination of panniculectomy and cesarean section safe? Scientific Poster Presentation-Obstetrics and Gynecology. J Am Coll Surg. 2017;225(4 suppl 2):E130.
Dr. Barbieri responds
I agree with Dr. Petrikovsky that advances in the field of obstetrical surgery have been inhibited by a tendency to criticize innovation. Less than 40 years ago, leaders in gynecology did not initially accept the application of minimally invasive gynecology surgical techniques to common gyn procedures including hysterectomy. Every surgical field is rapidly innovating. Obstetrical surgeons should be encouraged to pursue new approaches, as you are doing. We wish you success in your pioneering work.
Continue to: A CASE OF BV...
A CASE OF BV DURING PREGNANCY: BEST MANAGEMENT APPROACH
CALLIE FOX REEDER, MD, AND PATRICK DUFF, MD (ID CONSULT; FEBRUARY 2021)
Secnidazole for treatment of BV
The article by Drs. Reeder and Duff incorrectly states that there are no single-dose therapeutic options for bacterial vaginosis (BV) in the United States. Secnidazole 2 g single oral dose was approved by the US Food and Drug Administration (FDA) in 2017, and it is now included in the American College of Obstetricians and Gynecologists' (ACOG) clinical management guidelines for the treatment of BV in nonpregnant patients.
Secnidazole is not contraindicated in pregnancy. In a poster presented at the 2020 ACOG annual clinical meeting, we summarized results of the preclinical studies that were part of the FDA submission.1 There was no evidence of secnidazole toxicity in fertility and pre- and postnatal reproductive toxicology studies. In addition, there were no adverse developmental outcomes when secnidazole was administered orally to pregnant rats and rabbits during organogenesis at doses up to 4 times the clinical dose. These findings are consistent with the observation that no other preclinical studies, or experience from postmarketing use of secnidazole for approved indications, have suggested a risk of adverse effects when using secnidazole in pregnancy.
Steven E. Chavoustie, MD
North Miami, Florida
Reference
1. Pentikis H, Eder S, Kaufman G, Chavoustie S. Secnidazole, an approved single dose drug for bacterial vaginosis, does not cause reproductive toxicity in animals [16A]. Obstet Gynecol. 2020;135:12S.
Drs. Reeder and Duff respond
We are very appreciative of Dr. Chavoustie's interest in our article and for his thoughtful assessment of the role of single-dose secnidazole for the treatment of BV. As we noted in our article, this drug has been used extensively in Europe and Asia, but there is much less published experience with the drug in the United States. We pointed out the excellent results reported by Hillier and colleagues with 1-g and 2-g doses of this medication.1 Dr. Chavoustie is correct in stating that there is no risk of fetal harm based on animal data at up to 4 times the recommended human dose, although the manufacturer recommends discontinuing breastfeeding during, and for 96 hours after, treatment. According to www.goodrx.com, the cost of a single 2-g dose of secnidazole is $325; the cost of a 7-day course of metronidazole is approximately $16.
Reference
1. Hillier SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
Continue to: OPTIMIZING THE USE OF...
OPTIMIZING THE USE OF OXYTOCIN ON LABOR AND DELIVERY
ROBERT L. BARBIERI, MD (EDITORIAL; JANUARY 2021)
Vigilant labor progress aids in oxytocin optimization
I read with particular interest Dr. Barbieri's editorial on optimizing oxytocin infusion. This topic is relevant for my practice as I am the kind of physician described and I usually get upset when the oxytocin is not managed as I ordered.
In my opinion, several things need clarification. On our unit, the most significant point of controversy is the definition of tachysystole, mainly when we are using a tocodynamometer and not an internal transducer.
I contend that it is quite challenging to ascertain the effectiveness of any given labor pattern based only on the number of contractions. Although we joke about "pit to distress," the truth is that contractions need to be "effective," which to me means strong enough to induce cervical changes.
In my clinical practice, with a tocodynamometer, having 5 contractions that do not produce cervical changes (unless associated with abnormalities of the fetal heart rate tracing) is not a clinically relevant finding as we do not have a way to gauge the strength of such contractions.
I usually employ a mid-range oxytocin protocol, starting at 4 mU per minute and increasing by 4 mU every 20 minutes. Through 30 years of practicing obstetrics, I have found that this protocol renders excellent results in achieving an efficient labor pattern without jeopardizing fetal well-being.
On learning about oxytocin's pharmacokinetics, I still support Dr. Rhonda L. Perry and her colleagues' conclusion that, until we learn better about this aspect of oxytocin pharmacology, each woman is her own bioassay.1 Furthermore, we see this in our daily practice: some patients go into full efficient labor with oxytocin at 4 mU per minute while others at 30 mU per minute do zilch.
Based on the above, I think that optimization requires close vigilance of the labor and the fetal status at any given time, not determining an oxytocin rate of infusion or dosage.
We should be observant on evaluating labor progress, and we should not hesitate to use internal pressure catheters when needed to obtain a more accurate evaluation of the labor pattern.
By examining the patient's labor progress at regular intervals, we also optimize the oxytocin infusion by determining if the infusion is producing the expected cervical changes.
Tomas Hernandez-Mejia, MD
Pasco, Washington
Reference
1. Perry RL, Satin AJ, Barth WH, et al. The pharmacokinetics of oxytocin as they apply to labor induction. Am J Obstet Gynecol. 1996;174:1590-1593.
Dr. Barbieri responds
I thank Dr. Tomas Hernandez-Mejia for sharing his expertise in utilizing a higher dose of oxytocin to optimize labor and birth. Dr. Hernandez-Mejia's view is supported by the recent publication of a high-quality clinical trial showing that a high-dose oxytocin protocol (initial and incremental rate of 6 mIU/min) did not cause an increase in adverse perinatal outcomes compared with a standard-dose protocol (initial and incremental rate of 2 mIU/min) but slightly shortened the duration of labor.1 Based on this clinical trial, my conclusion is that the high-dose protocol, if appropriately monitored for excess uterine contractions and fetal heart rate pattern, is safe.
Reference
1. Son M, Roy A, Stetson BT, et al. High-dose compared with standard-dose oxytocin regimens to augment labor in nulliparous women: a randomized controlled trial. Obstet Gynecol. 2021;137:991-998.
Continue to: PREGNANCY OF UNKNOWN...
PREGNANCY OF UNKNOWN LOCATION: EVIDENCE-BASED EVALUATION AND MANAGEMENT
IRIS G. INSOGNA, MD, AND PAULA C. BRADY, MD (AUGUST 2020)
I would like to thank Dr. Iris Insogna and Dr. Paula Brady for their very informative article on pregnancy of unknown location. However, please allow me to make a suggestion that will clarify terminology for all practicing ObGyns.
The medical literature uses the terms cornual pregnancy and interstitial pregnancy interchangeably, although they are actually very different conditions and have significant different implications. Clinicians are often confused about which is an intrauterine pregnancy and which is a true ectopic pregnancy. This confusion was addressed in a 2006 article in Fertility and Sterility, which explains that a cornual pregnancy refers to the implantation and development of a gestation in one of the upper and lateral portions of the uterus.1 This may occur in a rudimentary horn or in one horn of a septate or bicornuate uterus. Conversely, an interstitial pregnancy is a gestation that implants within the proximal, intramural portion of the fallopian tube that is enveloped by myometrium. Therefore, a cornual pregnancy is actually an intrauterine pregnancy, whereas an interstitial pregnancy is a true ectopic pregnancy.
I hope that all clinicians will read the article in Fertility and Sterility and adopt this terminology to avoid future confusion and misunderstandings.
Alan D. Rosen, MD
Houston, Texas
Reference
1. Malinowski A, Bates SK. Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril. 2006;86:1764.e11-1764.e14.
