User login
CLINICAL UPDATE A Novel TNF Inhibitor for RA: An Update
A Novel TNF Inhibitor for RA: An Update
Assessing Cardiovascular Risk in the Patient With Lupus |
A supplement to Rheumatology News supported by an unrestricted educational grant from Aspreva Pharmaceuticals. This supplement is based on faculty interviews and is jointly sponsored by The Elsevier Office of Continuing Medical Education (EOCME), an ACCME accredited provider, and Rheumatology News. • Topic/Faculty |

|
Topic/Faculty |
Examining Cardiovascular Risk in Systemic Lupus Erythematosus Managing Cardiovascular Risk in Systemic Lupus Erythematosus |
Target Audience |
The following educational activity is for primary care physicians and rheumatologists who provide care for patients with systemic lupus erythematosus. |
Needs Assessment |
As diagnosis and management of systemic lupus erythematosus (SLE) have improved, patient survival has increased substantially. In the process, the focus of care has shifted toward management of long-term consequences of the disease. In particular, cardiovascular disease (CVD) has emerged as a major source of morbidity and mortality among patients with SLE. Not uncommonly, SLE is associated with multiple CVD risk factors, resulting in a pathologic collaboration that greatly increases the risk of atherosclerosis and myocardial infarction in patients with SLE. The onus is on physicians to monitor CVD risk closely in patients with SLE to improve the chances of early recognition and afford the opportunity for aggressive intervention to keep risk factors at bay. |
Educational Objectives |
After completing this educational activity, participants should be able to: • Understand and appreciate the increased CVD risk faced by patients with SLE. • Identify CVD risk factors that can be minimized by intervention. • Recognize the need for ongoing clinical vigilance, early recognition, and aggressive treatment of CVD risk factors. • Identify therapies that can help reduce the CVD risk in patients with SLE. |
Accreditation Statement |
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the Elsevier Office of Continuing Medical Education (EOCME) and Rheumatology News. The EOCME is accredited by the ACCME to provide continuing medical education (CME) for physicians. The EOCME designates this educational activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should only claim credit commensurate with the extent of their participation in the activity. Term of Approval: May 2007-May 31, 2008. |
Copyright © 2007 Elsevier Inc. |
Assessing Cardiovascular Risk in the Patient With Lupus |
A supplement to Rheumatology News supported by an unrestricted educational grant from Aspreva Pharmaceuticals. This supplement is based on faculty interviews and is jointly sponsored by The Elsevier Office of Continuing Medical Education (EOCME), an ACCME accredited provider, and Rheumatology News. • Topic/Faculty |

|
Topic/Faculty |
Examining Cardiovascular Risk in Systemic Lupus Erythematosus Managing Cardiovascular Risk in Systemic Lupus Erythematosus |
Target Audience |
The following educational activity is for primary care physicians and rheumatologists who provide care for patients with systemic lupus erythematosus. |
Needs Assessment |
As diagnosis and management of systemic lupus erythematosus (SLE) have improved, patient survival has increased substantially. In the process, the focus of care has shifted toward management of long-term consequences of the disease. In particular, cardiovascular disease (CVD) has emerged as a major source of morbidity and mortality among patients with SLE. Not uncommonly, SLE is associated with multiple CVD risk factors, resulting in a pathologic collaboration that greatly increases the risk of atherosclerosis and myocardial infarction in patients with SLE. The onus is on physicians to monitor CVD risk closely in patients with SLE to improve the chances of early recognition and afford the opportunity for aggressive intervention to keep risk factors at bay. |
Educational Objectives |
After completing this educational activity, participants should be able to: • Understand and appreciate the increased CVD risk faced by patients with SLE. • Identify CVD risk factors that can be minimized by intervention. • Recognize the need for ongoing clinical vigilance, early recognition, and aggressive treatment of CVD risk factors. • Identify therapies that can help reduce the CVD risk in patients with SLE. |
Accreditation Statement |
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the Elsevier Office of Continuing Medical Education (EOCME) and Rheumatology News. The EOCME is accredited by the ACCME to provide continuing medical education (CME) for physicians. The EOCME designates this educational activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should only claim credit commensurate with the extent of their participation in the activity. Term of Approval: May 2007-May 31, 2008. |
Copyright © 2007 Elsevier Inc. |
Assessing Cardiovascular Risk in the Patient With Lupus |
A supplement to Rheumatology News supported by an unrestricted educational grant from Aspreva Pharmaceuticals. This supplement is based on faculty interviews and is jointly sponsored by The Elsevier Office of Continuing Medical Education (EOCME), an ACCME accredited provider, and Rheumatology News. • Topic/Faculty |

|
Topic/Faculty |
Examining Cardiovascular Risk in Systemic Lupus Erythematosus Managing Cardiovascular Risk in Systemic Lupus Erythematosus |
Target Audience |
The following educational activity is for primary care physicians and rheumatologists who provide care for patients with systemic lupus erythematosus. |
Needs Assessment |
As diagnosis and management of systemic lupus erythematosus (SLE) have improved, patient survival has increased substantially. In the process, the focus of care has shifted toward management of long-term consequences of the disease. In particular, cardiovascular disease (CVD) has emerged as a major source of morbidity and mortality among patients with SLE. Not uncommonly, SLE is associated with multiple CVD risk factors, resulting in a pathologic collaboration that greatly increases the risk of atherosclerosis and myocardial infarction in patients with SLE. The onus is on physicians to monitor CVD risk closely in patients with SLE to improve the chances of early recognition and afford the opportunity for aggressive intervention to keep risk factors at bay. |
Educational Objectives |
After completing this educational activity, participants should be able to: • Understand and appreciate the increased CVD risk faced by patients with SLE. • Identify CVD risk factors that can be minimized by intervention. • Recognize the need for ongoing clinical vigilance, early recognition, and aggressive treatment of CVD risk factors. • Identify therapies that can help reduce the CVD risk in patients with SLE. |
Accreditation Statement |
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the Elsevier Office of Continuing Medical Education (EOCME) and Rheumatology News. The EOCME is accredited by the ACCME to provide continuing medical education (CME) for physicians. The EOCME designates this educational activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should only claim credit commensurate with the extent of their participation in the activity. Term of Approval: May 2007-May 31, 2008. |
Copyright © 2007 Elsevier Inc. |
A Novel TNF Inhibitor for RA: An Update
A Novel TNF Inhibitor for RA: An Update
BIOLOGIC THERAPIES IN RA: Improving Patient Outcomes
A CME-Certified Supplement to Rheumatology News®, supported by an educational grant from UCB. This activity is jointly sponsored by University of Louisville Continuing Health Sciences Education and Global Academy for Medical Education, an Elsevier business.
- Topic Highlights
- Faculty/Faculty Disclosure Statement
- Target Audience
- Educational Needs
- Learning Objectives
- Accreditation Statement
- Credit Designation
- Link to post-test and evaluation
Topic Highlights
*Optimizing the Use of Anti-TNF Therapy in RA
*Treating to Target and Achieving Remission in RA
Faculty/Faculty Disclosure Statement
Roy M. Fleischmann, MD
Clinical Professor of Medicine
University of Texas Southwestern Medical Center
Co-Medical Director, Metroplex Clinical Research Center (MCRC)
Dallas, FL
Roy M. Fleischmann, MD: Neither Dr Fleischmann nor his immediate family members have a personal financial relationship relevant to the content of this CME journal.
Iain McInnes, MRCP, PhD
Professor of Experimental Medicine and Rheumatology
Glasgow Biomedical Research Centre
University of Glasgow
United Kingdom
Iain McInnes, MRCP, PhD: Research Grant: Hoffman-La Roche Inc and Bristol-Myers Squibb Company. Speakers Bureau: Merck Sharp & Dohme Limited and Bristol-Myers Squibb Company.
Target Audience
This educational activity is designed for rheumatologists and other health care professionals involved in the care of patients with rheumatoid arthritis (RA).
Educational Needs
The emerging understanding of inflammatory pathways provided the basis for development of biologic disease-modifying antirheumatic drugs (DMARDs) that offer more specific therapy for RA. Five of these agents target the tumor necrosis factor (TNF) inflammatory pathway (adalimumab, certolizumab pegol, etanercept, golimumab, and infliximab). During more than a decade of clinical use, inhibitors of TNF have played a major role in treatment advances that have improved disease control, helped preserve functional ability, and improved outcomes for patients with RA. The development of more effective therapy and therapeutic strategies for RA has brought to the field of rheumatology the concept of tight
control or treatment to target. Remission and low-level activity have become appropriate, and achievable, therapeutic goals for most patients with RA. Intuitively, treatment strategies that achieve and maintain a specified low level of disease activity might be expected to improve patient outcomes in RA. Data from well-designed clinical trials remain somewhat limited but have provided reason for optimism that treating to target will improve RA outcomes, similar to the clinical experience in diabetes and hypertension.
Learning Objectives
At the conclusion of the activity, the participants should be able to:
· Describe the principal findings from selected studies on RA recently presented that have implications for patient management
· Identify and understand strategies for treating RA to a specific target of low-level disease activity
· Appreciate the potential benefits and limitations of switching patients with RA from one TNF inhibitor to another in the class
Accreditation Statement
This activity has been planned and implementedin accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the University of Louisville School of Medicine Continuing Health Sciences Education (CHSE) and Global Academy for Medical Education, an Elsevier business. CHSE is accredited by the ACCME to provide continuing education for physicians.
CREDIT DESIGNATION
CHSE designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
<<<<link to post-test and evaluation>>>>
Copyright © 2011 Elsevier Inc.
A CME-Certified Supplement to Rheumatology News®, supported by an educational grant from UCB. This activity is jointly sponsored by University of Louisville Continuing Health Sciences Education and Global Academy for Medical Education, an Elsevier business.
- Topic Highlights
- Faculty/Faculty Disclosure Statement
- Target Audience
- Educational Needs
- Learning Objectives
- Accreditation Statement
- Credit Designation
- Link to post-test and evaluation
Topic Highlights
*Optimizing the Use of Anti-TNF Therapy in RA
*Treating to Target and Achieving Remission in RA
Faculty/Faculty Disclosure Statement
Roy M. Fleischmann, MD
Clinical Professor of Medicine
University of Texas Southwestern Medical Center
Co-Medical Director, Metroplex Clinical Research Center (MCRC)
Dallas, FL
Roy M. Fleischmann, MD: Neither Dr Fleischmann nor his immediate family members have a personal financial relationship relevant to the content of this CME journal.
Iain McInnes, MRCP, PhD
Professor of Experimental Medicine and Rheumatology
Glasgow Biomedical Research Centre
University of Glasgow
United Kingdom
Iain McInnes, MRCP, PhD: Research Grant: Hoffman-La Roche Inc and Bristol-Myers Squibb Company. Speakers Bureau: Merck Sharp & Dohme Limited and Bristol-Myers Squibb Company.
Target Audience
This educational activity is designed for rheumatologists and other health care professionals involved in the care of patients with rheumatoid arthritis (RA).
Educational Needs
The emerging understanding of inflammatory pathways provided the basis for development of biologic disease-modifying antirheumatic drugs (DMARDs) that offer more specific therapy for RA. Five of these agents target the tumor necrosis factor (TNF) inflammatory pathway (adalimumab, certolizumab pegol, etanercept, golimumab, and infliximab). During more than a decade of clinical use, inhibitors of TNF have played a major role in treatment advances that have improved disease control, helped preserve functional ability, and improved outcomes for patients with RA. The development of more effective therapy and therapeutic strategies for RA has brought to the field of rheumatology the concept of tight
control or treatment to target. Remission and low-level activity have become appropriate, and achievable, therapeutic goals for most patients with RA. Intuitively, treatment strategies that achieve and maintain a specified low level of disease activity might be expected to improve patient outcomes in RA. Data from well-designed clinical trials remain somewhat limited but have provided reason for optimism that treating to target will improve RA outcomes, similar to the clinical experience in diabetes and hypertension.
Learning Objectives
At the conclusion of the activity, the participants should be able to:
· Describe the principal findings from selected studies on RA recently presented that have implications for patient management
· Identify and understand strategies for treating RA to a specific target of low-level disease activity
· Appreciate the potential benefits and limitations of switching patients with RA from one TNF inhibitor to another in the class
Accreditation Statement
This activity has been planned and implementedin accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the University of Louisville School of Medicine Continuing Health Sciences Education (CHSE) and Global Academy for Medical Education, an Elsevier business. CHSE is accredited by the ACCME to provide continuing education for physicians.
CREDIT DESIGNATION
CHSE designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
<<<<link to post-test and evaluation>>>>
Copyright © 2011 Elsevier Inc.
A CME-Certified Supplement to Rheumatology News®, supported by an educational grant from UCB. This activity is jointly sponsored by University of Louisville Continuing Health Sciences Education and Global Academy for Medical Education, an Elsevier business.
- Topic Highlights
- Faculty/Faculty Disclosure Statement
- Target Audience
- Educational Needs
- Learning Objectives
- Accreditation Statement
- Credit Designation
- Link to post-test and evaluation
Topic Highlights
*Optimizing the Use of Anti-TNF Therapy in RA
*Treating to Target and Achieving Remission in RA
Faculty/Faculty Disclosure Statement
Roy M. Fleischmann, MD
Clinical Professor of Medicine
University of Texas Southwestern Medical Center
Co-Medical Director, Metroplex Clinical Research Center (MCRC)
Dallas, FL
Roy M. Fleischmann, MD: Neither Dr Fleischmann nor his immediate family members have a personal financial relationship relevant to the content of this CME journal.
Iain McInnes, MRCP, PhD
Professor of Experimental Medicine and Rheumatology
Glasgow Biomedical Research Centre
University of Glasgow
United Kingdom
Iain McInnes, MRCP, PhD: Research Grant: Hoffman-La Roche Inc and Bristol-Myers Squibb Company. Speakers Bureau: Merck Sharp & Dohme Limited and Bristol-Myers Squibb Company.
Target Audience
This educational activity is designed for rheumatologists and other health care professionals involved in the care of patients with rheumatoid arthritis (RA).
Educational Needs
The emerging understanding of inflammatory pathways provided the basis for development of biologic disease-modifying antirheumatic drugs (DMARDs) that offer more specific therapy for RA. Five of these agents target the tumor necrosis factor (TNF) inflammatory pathway (adalimumab, certolizumab pegol, etanercept, golimumab, and infliximab). During more than a decade of clinical use, inhibitors of TNF have played a major role in treatment advances that have improved disease control, helped preserve functional ability, and improved outcomes for patients with RA. The development of more effective therapy and therapeutic strategies for RA has brought to the field of rheumatology the concept of tight
control or treatment to target. Remission and low-level activity have become appropriate, and achievable, therapeutic goals for most patients with RA. Intuitively, treatment strategies that achieve and maintain a specified low level of disease activity might be expected to improve patient outcomes in RA. Data from well-designed clinical trials remain somewhat limited but have provided reason for optimism that treating to target will improve RA outcomes, similar to the clinical experience in diabetes and hypertension.
Learning Objectives
At the conclusion of the activity, the participants should be able to:
· Describe the principal findings from selected studies on RA recently presented that have implications for patient management
· Identify and understand strategies for treating RA to a specific target of low-level disease activity
· Appreciate the potential benefits and limitations of switching patients with RA from one TNF inhibitor to another in the class
Accreditation Statement
This activity has been planned and implementedin accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the University of Louisville School of Medicine Continuing Health Sciences Education (CHSE) and Global Academy for Medical Education, an Elsevier business. CHSE is accredited by the ACCME to provide continuing education for physicians.
CREDIT DESIGNATION
CHSE designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
<<<<link to post-test and evaluation>>>>
Copyright © 2011 Elsevier Inc.
10 practical, evidence-based recommendations to improve outcomes in women who have eclampsia
Because eclampsia occurs but rarely during pregnancy and the postpartum period, most health-care providers have little to no personal experience with management of this life-threatening obstetric emergency. Knowledge about maternal resuscitation during and after an eclamptic seizure is critical for improving maternal and perinatal outcomes.
In this round-up, I present 10 practical recommendations for prompt diagnosis and management of women who have eclampsia. Immediate implementation of these recommendations can lead to improved maternal and perinatal outcomes (both acute and long-term).
1. Practice. Practice again.
Implement regular monthly simulation training sessions
Fisher N, Bernstein PS, Satin A, et al. Resident training for eclampsia and magnesium toxicity management: simulation or traditional lecture? Am J Obstet Gynecol. 2010;203(4):379.e1–5.
Eclampsia is unpredictable and can develop rapidly at home, in labor and delivery, on the antepartum/postpartum ward, and in the emergency room. Therefore, it is prudent that all health-care providers who treat pregnant or postpartum women on a daily basis be trained and knowledgeable about early detection and management of eclampsia. This goal can be achieved by developing drills for rehearsal and by testing the response and skills of all providers.
2. Preventive: Magnesium sulfate
Do not attempt to arrest the seizure. Use MgSO4 to prevent recurrent convulsions.
Duley L, Henderson-Smart DJ, Walker GJ, Chou D. Magnesium sulfate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2010;(12):CD000127.
Most eclamptic seizures are self-limiting. Therefore, there is no need to administer bolus drugs such as diazepam or midazolam. These drugs are usually used in the emergency room, but they inhibit maternal laryngeal reflexes and may lead to aspiration. They also suppress the central nervous system respiratory centers and can cause apnea, requiring intubation.
When used in the management of eclampsia, magnesium sulfate is associated with a lower rate of recurrent seizures and maternal death than is diazepam.
3. FHR changes? Be patient.
Do not rush the patient to emergent cesarean section because of an abnormal FHR tracing
Sibai BM. Diagnosis, prevention, and management of eclampsia. Obstet Gynecol. 2005;105(2):402–410.
During an eclamptic convulsion, there is usually prolonged fetal heart rate (FHR) deceleration or even bradycardia—with or without an increase in both frequency and uterine tone. After the convulsion, as a result of maternal hypoxia and hypercarbia, the FHR tracing can show tachycardia, reduced beat-to-beat variability, and transient recurrent decelerations. When this happens, concern about fetal status can distract the obstetric provider from resuscitation of the mother. However, these FHR changes usually return to normal after maternal resuscitation. If the FHR changes persist for longer than 15 minutes, consider abruptio placentae and move to delivery.
4. Target: Lower BP
Reduce maternal blood pressure to a safe level to prevent stroke, but without compromising uteroplacental perfusion
Zwart JJ, Richters A, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Eclampsia in the Netherlands. Obstet Gynecol. 2008;112(4):820–827.
In this nationwide review of complications from eclampsia in the Netherlands, the authors found that failure to treat persistent severe hypertension was associated with hypertensive encephalopathy, cerebral infarction, bleeding, or congestive heart failure. They also found that 35.2% of women had systolic or diastolic blood pressure at or above 170/110 mm Hg at admission, but fewer than half were given antihypertensive drugs at that time. Among the cases deemed to have received substandard care, one third involved inadequate treatment of hypertension.
5. Know your antihypertensives
Learn which agents are best to control severe hypertension in eclampsia
Sibai BM. Hypertensive Emergencies. In: Foley MR, Strong TH, Garite TJ, eds. Obstetric Intensive Care Manual. 3rd ed. New York, NY: The McGraw-Hill Companies; 2010.
It is critical to familiarize oneself with the mechanism of action, dose, and potential side effects of agents used to control hypertension. For example, neither hydralazine nor nifedipine should be used in patients who have severe headache and persistent tachycardia (pulse, >100 bpm). Labetalol should be avoided in women who have persistent bradycardia (pulse, <60 bpm), asthma, or congestive heart failure.
For women who have persistent headache and tachycardia, I suggest intravenous (IV) labetalol, starting at a dose of 20 mg, 40 mg, or 80 mg every 10 minutes as needed to keep systolic blood pressure below 160 mm Hg and diastolic blood pressure below 105 mm Hg. The maximum dose of labetalol should not exceed 300 mg in 1 hour.
For patients who have bradycardia and severe asthma, I suggest oral, rapid-acting nifedipine, starting at 10 mg to 20 mg, to be repeated in 20 to 30 minutes as needed, up to a maximum of 50 mg to 60 mg in 1 hour. Oral nifedipine can be used with magnesium sulfate. An alternative is an IV bolus injection of hydralazine, starting at a dose of 5 mg to 10 mg, to be repeated every 15 minutes, up to a maximum dose of 25 mg.
6. Avoid general anesthesia
Use neuraxial anesthesia for labor and delivery in eclampsia
Turner JA. Severe preeclampsia: anesthetic implications of the disease and its management. Am J Ther. 2009;16(4):284–248.
Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Cesarean delivery: a population-based study. Br J Anaesth. 2010;105(6):818–826.
Epidural, spinal, or combined anesthesia is safe in the absence of coagulopathy or severe thrombocytopenia. General anesthesia increases the risk of aspiration, failed intubation due to pharyngolaryngeal edema, and stroke secondary to the increase in systemic and intracerebral pressures during intubation and extubation.
Eclampsia is not an indication for cesarean delivery
Repke JT, Sibai BM. Preeclampsia and eclampsia. OBG Manage. 2009;21(4):44–55.
Once the mother has been resuscitated and stabilized, the provider should choose a mode of delivery that is based on fetal condition, gestational age, presence or absence of labor, and the cervical Bishop score. Vaginal delivery can be achieved in most patients who have a gestational age of 34 weeks or greater.
8. Late presentation happens
Be aware that eclampsia can develop for the first time as long as 28 days postpartum
Sibai BM, Stella CL. Diagnosis and management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol. 2009;200(5):481.e31–37.
Atypical eclampsia is any eclampsia that develops beyond 48 hours postpartum. A history of diagnosed predelivery preeclampsia is not necessary for development of late postpartum eclampsia. In general, more than 50% of patients who develop late postpartum eclampsia have no evidence of preeclampsia prior to delivery.
Be aware that the clinical and neuro-imaging features of eclampsia overlap with those of reversible cerebral vasoconstriction syndrome (angiopathy)
Fletcher JJ, Kramer AH, Bleck TP, Solenski NJ. Overlapping features of eclampsia and postpartum angiopathy. Neurocrit Care. 2009;11(2):199–209.
Women who have reversible cerebral vasoconstriction syndrome have clinical findings (acute onset of recurrent headaches, visual changes, seizures, and hypertension) and cerebral magnetic resonance imaging (MRI) findings (posterior reversible encephalopathy syndrome) that are similar to those of women who have late postpartum eclampsia (FIGURE). However, in women who have postpartum cerebral angiopathy, cerebral angiography will show the presence of bead-like vasoconstriction—which is usually absent in eclampsia.
Posterior reversible encephalopathy syndrome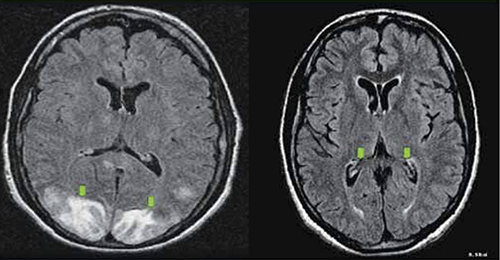
Green arrows point to vasogenic edema in the occipital lobes and, partially, the parietal lobes. The edema is gone on repeat magnetic resonance imaging (see Recommendation #9).
10. Act today, see a better outcome tomorrow
Avoid long-term maternal neurologic injury by managing eclampsia properly
Zeeman GG. Neurologic complications of preeclampsia. Semin Perinatol. 2009;33(3):166–172.
Residual neurologic damage is rare in the majority of women who have eclampsia. However, long-term cerebral white-matter injury (cytotoxic edema, infarction) on MRI imaging and impaired memory and cognitive function may develop in some women who have multiple seizures and who have inadequately controlled persistent severe hypertension.
We want to hear from you! Tell us what you think.
Because eclampsia occurs but rarely during pregnancy and the postpartum period, most health-care providers have little to no personal experience with management of this life-threatening obstetric emergency. Knowledge about maternal resuscitation during and after an eclamptic seizure is critical for improving maternal and perinatal outcomes.
In this round-up, I present 10 practical recommendations for prompt diagnosis and management of women who have eclampsia. Immediate implementation of these recommendations can lead to improved maternal and perinatal outcomes (both acute and long-term).
1. Practice. Practice again.
Implement regular monthly simulation training sessions
Fisher N, Bernstein PS, Satin A, et al. Resident training for eclampsia and magnesium toxicity management: simulation or traditional lecture? Am J Obstet Gynecol. 2010;203(4):379.e1–5.
Eclampsia is unpredictable and can develop rapidly at home, in labor and delivery, on the antepartum/postpartum ward, and in the emergency room. Therefore, it is prudent that all health-care providers who treat pregnant or postpartum women on a daily basis be trained and knowledgeable about early detection and management of eclampsia. This goal can be achieved by developing drills for rehearsal and by testing the response and skills of all providers.
2. Preventive: Magnesium sulfate
Do not attempt to arrest the seizure. Use MgSO4 to prevent recurrent convulsions.
Duley L, Henderson-Smart DJ, Walker GJ, Chou D. Magnesium sulfate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2010;(12):CD000127.
Most eclamptic seizures are self-limiting. Therefore, there is no need to administer bolus drugs such as diazepam or midazolam. These drugs are usually used in the emergency room, but they inhibit maternal laryngeal reflexes and may lead to aspiration. They also suppress the central nervous system respiratory centers and can cause apnea, requiring intubation.
When used in the management of eclampsia, magnesium sulfate is associated with a lower rate of recurrent seizures and maternal death than is diazepam.
3. FHR changes? Be patient.
Do not rush the patient to emergent cesarean section because of an abnormal FHR tracing
Sibai BM. Diagnosis, prevention, and management of eclampsia. Obstet Gynecol. 2005;105(2):402–410.
During an eclamptic convulsion, there is usually prolonged fetal heart rate (FHR) deceleration or even bradycardia—with or without an increase in both frequency and uterine tone. After the convulsion, as a result of maternal hypoxia and hypercarbia, the FHR tracing can show tachycardia, reduced beat-to-beat variability, and transient recurrent decelerations. When this happens, concern about fetal status can distract the obstetric provider from resuscitation of the mother. However, these FHR changes usually return to normal after maternal resuscitation. If the FHR changes persist for longer than 15 minutes, consider abruptio placentae and move to delivery.
4. Target: Lower BP
Reduce maternal blood pressure to a safe level to prevent stroke, but without compromising uteroplacental perfusion
Zwart JJ, Richters A, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Eclampsia in the Netherlands. Obstet Gynecol. 2008;112(4):820–827.
In this nationwide review of complications from eclampsia in the Netherlands, the authors found that failure to treat persistent severe hypertension was associated with hypertensive encephalopathy, cerebral infarction, bleeding, or congestive heart failure. They also found that 35.2% of women had systolic or diastolic blood pressure at or above 170/110 mm Hg at admission, but fewer than half were given antihypertensive drugs at that time. Among the cases deemed to have received substandard care, one third involved inadequate treatment of hypertension.
5. Know your antihypertensives
Learn which agents are best to control severe hypertension in eclampsia
Sibai BM. Hypertensive Emergencies. In: Foley MR, Strong TH, Garite TJ, eds. Obstetric Intensive Care Manual. 3rd ed. New York, NY: The McGraw-Hill Companies; 2010.
It is critical to familiarize oneself with the mechanism of action, dose, and potential side effects of agents used to control hypertension. For example, neither hydralazine nor nifedipine should be used in patients who have severe headache and persistent tachycardia (pulse, >100 bpm). Labetalol should be avoided in women who have persistent bradycardia (pulse, <60 bpm), asthma, or congestive heart failure.
For women who have persistent headache and tachycardia, I suggest intravenous (IV) labetalol, starting at a dose of 20 mg, 40 mg, or 80 mg every 10 minutes as needed to keep systolic blood pressure below 160 mm Hg and diastolic blood pressure below 105 mm Hg. The maximum dose of labetalol should not exceed 300 mg in 1 hour.
For patients who have bradycardia and severe asthma, I suggest oral, rapid-acting nifedipine, starting at 10 mg to 20 mg, to be repeated in 20 to 30 minutes as needed, up to a maximum of 50 mg to 60 mg in 1 hour. Oral nifedipine can be used with magnesium sulfate. An alternative is an IV bolus injection of hydralazine, starting at a dose of 5 mg to 10 mg, to be repeated every 15 minutes, up to a maximum dose of 25 mg.
6. Avoid general anesthesia
Use neuraxial anesthesia for labor and delivery in eclampsia
Turner JA. Severe preeclampsia: anesthetic implications of the disease and its management. Am J Ther. 2009;16(4):284–248.
Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Cesarean delivery: a population-based study. Br J Anaesth. 2010;105(6):818–826.
Epidural, spinal, or combined anesthesia is safe in the absence of coagulopathy or severe thrombocytopenia. General anesthesia increases the risk of aspiration, failed intubation due to pharyngolaryngeal edema, and stroke secondary to the increase in systemic and intracerebral pressures during intubation and extubation.
Eclampsia is not an indication for cesarean delivery
Repke JT, Sibai BM. Preeclampsia and eclampsia. OBG Manage. 2009;21(4):44–55.
Once the mother has been resuscitated and stabilized, the provider should choose a mode of delivery that is based on fetal condition, gestational age, presence or absence of labor, and the cervical Bishop score. Vaginal delivery can be achieved in most patients who have a gestational age of 34 weeks or greater.
8. Late presentation happens
Be aware that eclampsia can develop for the first time as long as 28 days postpartum
Sibai BM, Stella CL. Diagnosis and management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol. 2009;200(5):481.e31–37.
Atypical eclampsia is any eclampsia that develops beyond 48 hours postpartum. A history of diagnosed predelivery preeclampsia is not necessary for development of late postpartum eclampsia. In general, more than 50% of patients who develop late postpartum eclampsia have no evidence of preeclampsia prior to delivery.
Be aware that the clinical and neuro-imaging features of eclampsia overlap with those of reversible cerebral vasoconstriction syndrome (angiopathy)
Fletcher JJ, Kramer AH, Bleck TP, Solenski NJ. Overlapping features of eclampsia and postpartum angiopathy. Neurocrit Care. 2009;11(2):199–209.
Women who have reversible cerebral vasoconstriction syndrome have clinical findings (acute onset of recurrent headaches, visual changes, seizures, and hypertension) and cerebral magnetic resonance imaging (MRI) findings (posterior reversible encephalopathy syndrome) that are similar to those of women who have late postpartum eclampsia (FIGURE). However, in women who have postpartum cerebral angiopathy, cerebral angiography will show the presence of bead-like vasoconstriction—which is usually absent in eclampsia.
Posterior reversible encephalopathy syndrome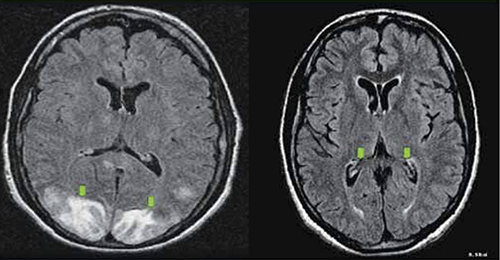
Green arrows point to vasogenic edema in the occipital lobes and, partially, the parietal lobes. The edema is gone on repeat magnetic resonance imaging (see Recommendation #9).
10. Act today, see a better outcome tomorrow
Avoid long-term maternal neurologic injury by managing eclampsia properly
Zeeman GG. Neurologic complications of preeclampsia. Semin Perinatol. 2009;33(3):166–172.
Residual neurologic damage is rare in the majority of women who have eclampsia. However, long-term cerebral white-matter injury (cytotoxic edema, infarction) on MRI imaging and impaired memory and cognitive function may develop in some women who have multiple seizures and who have inadequately controlled persistent severe hypertension.
We want to hear from you! Tell us what you think.
Because eclampsia occurs but rarely during pregnancy and the postpartum period, most health-care providers have little to no personal experience with management of this life-threatening obstetric emergency. Knowledge about maternal resuscitation during and after an eclamptic seizure is critical for improving maternal and perinatal outcomes.
In this round-up, I present 10 practical recommendations for prompt diagnosis and management of women who have eclampsia. Immediate implementation of these recommendations can lead to improved maternal and perinatal outcomes (both acute and long-term).
1. Practice. Practice again.
Implement regular monthly simulation training sessions
Fisher N, Bernstein PS, Satin A, et al. Resident training for eclampsia and magnesium toxicity management: simulation or traditional lecture? Am J Obstet Gynecol. 2010;203(4):379.e1–5.
Eclampsia is unpredictable and can develop rapidly at home, in labor and delivery, on the antepartum/postpartum ward, and in the emergency room. Therefore, it is prudent that all health-care providers who treat pregnant or postpartum women on a daily basis be trained and knowledgeable about early detection and management of eclampsia. This goal can be achieved by developing drills for rehearsal and by testing the response and skills of all providers.
2. Preventive: Magnesium sulfate
Do not attempt to arrest the seizure. Use MgSO4 to prevent recurrent convulsions.
Duley L, Henderson-Smart DJ, Walker GJ, Chou D. Magnesium sulfate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2010;(12):CD000127.
Most eclamptic seizures are self-limiting. Therefore, there is no need to administer bolus drugs such as diazepam or midazolam. These drugs are usually used in the emergency room, but they inhibit maternal laryngeal reflexes and may lead to aspiration. They also suppress the central nervous system respiratory centers and can cause apnea, requiring intubation.
When used in the management of eclampsia, magnesium sulfate is associated with a lower rate of recurrent seizures and maternal death than is diazepam.
3. FHR changes? Be patient.
Do not rush the patient to emergent cesarean section because of an abnormal FHR tracing
Sibai BM. Diagnosis, prevention, and management of eclampsia. Obstet Gynecol. 2005;105(2):402–410.
During an eclamptic convulsion, there is usually prolonged fetal heart rate (FHR) deceleration or even bradycardia—with or without an increase in both frequency and uterine tone. After the convulsion, as a result of maternal hypoxia and hypercarbia, the FHR tracing can show tachycardia, reduced beat-to-beat variability, and transient recurrent decelerations. When this happens, concern about fetal status can distract the obstetric provider from resuscitation of the mother. However, these FHR changes usually return to normal after maternal resuscitation. If the FHR changes persist for longer than 15 minutes, consider abruptio placentae and move to delivery.
4. Target: Lower BP
Reduce maternal blood pressure to a safe level to prevent stroke, but without compromising uteroplacental perfusion
Zwart JJ, Richters A, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Eclampsia in the Netherlands. Obstet Gynecol. 2008;112(4):820–827.
In this nationwide review of complications from eclampsia in the Netherlands, the authors found that failure to treat persistent severe hypertension was associated with hypertensive encephalopathy, cerebral infarction, bleeding, or congestive heart failure. They also found that 35.2% of women had systolic or diastolic blood pressure at or above 170/110 mm Hg at admission, but fewer than half were given antihypertensive drugs at that time. Among the cases deemed to have received substandard care, one third involved inadequate treatment of hypertension.
5. Know your antihypertensives
Learn which agents are best to control severe hypertension in eclampsia
Sibai BM. Hypertensive Emergencies. In: Foley MR, Strong TH, Garite TJ, eds. Obstetric Intensive Care Manual. 3rd ed. New York, NY: The McGraw-Hill Companies; 2010.
It is critical to familiarize oneself with the mechanism of action, dose, and potential side effects of agents used to control hypertension. For example, neither hydralazine nor nifedipine should be used in patients who have severe headache and persistent tachycardia (pulse, >100 bpm). Labetalol should be avoided in women who have persistent bradycardia (pulse, <60 bpm), asthma, or congestive heart failure.
For women who have persistent headache and tachycardia, I suggest intravenous (IV) labetalol, starting at a dose of 20 mg, 40 mg, or 80 mg every 10 minutes as needed to keep systolic blood pressure below 160 mm Hg and diastolic blood pressure below 105 mm Hg. The maximum dose of labetalol should not exceed 300 mg in 1 hour.
For patients who have bradycardia and severe asthma, I suggest oral, rapid-acting nifedipine, starting at 10 mg to 20 mg, to be repeated in 20 to 30 minutes as needed, up to a maximum of 50 mg to 60 mg in 1 hour. Oral nifedipine can be used with magnesium sulfate. An alternative is an IV bolus injection of hydralazine, starting at a dose of 5 mg to 10 mg, to be repeated every 15 minutes, up to a maximum dose of 25 mg.
6. Avoid general anesthesia
Use neuraxial anesthesia for labor and delivery in eclampsia
Turner JA. Severe preeclampsia: anesthetic implications of the disease and its management. Am J Ther. 2009;16(4):284–248.
Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Cesarean delivery: a population-based study. Br J Anaesth. 2010;105(6):818–826.
Epidural, spinal, or combined anesthesia is safe in the absence of coagulopathy or severe thrombocytopenia. General anesthesia increases the risk of aspiration, failed intubation due to pharyngolaryngeal edema, and stroke secondary to the increase in systemic and intracerebral pressures during intubation and extubation.
Eclampsia is not an indication for cesarean delivery
Repke JT, Sibai BM. Preeclampsia and eclampsia. OBG Manage. 2009;21(4):44–55.
Once the mother has been resuscitated and stabilized, the provider should choose a mode of delivery that is based on fetal condition, gestational age, presence or absence of labor, and the cervical Bishop score. Vaginal delivery can be achieved in most patients who have a gestational age of 34 weeks or greater.
8. Late presentation happens
Be aware that eclampsia can develop for the first time as long as 28 days postpartum
Sibai BM, Stella CL. Diagnosis and management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol. 2009;200(5):481.e31–37.
Atypical eclampsia is any eclampsia that develops beyond 48 hours postpartum. A history of diagnosed predelivery preeclampsia is not necessary for development of late postpartum eclampsia. In general, more than 50% of patients who develop late postpartum eclampsia have no evidence of preeclampsia prior to delivery.
Be aware that the clinical and neuro-imaging features of eclampsia overlap with those of reversible cerebral vasoconstriction syndrome (angiopathy)
Fletcher JJ, Kramer AH, Bleck TP, Solenski NJ. Overlapping features of eclampsia and postpartum angiopathy. Neurocrit Care. 2009;11(2):199–209.
Women who have reversible cerebral vasoconstriction syndrome have clinical findings (acute onset of recurrent headaches, visual changes, seizures, and hypertension) and cerebral magnetic resonance imaging (MRI) findings (posterior reversible encephalopathy syndrome) that are similar to those of women who have late postpartum eclampsia (FIGURE). However, in women who have postpartum cerebral angiopathy, cerebral angiography will show the presence of bead-like vasoconstriction—which is usually absent in eclampsia.
Posterior reversible encephalopathy syndrome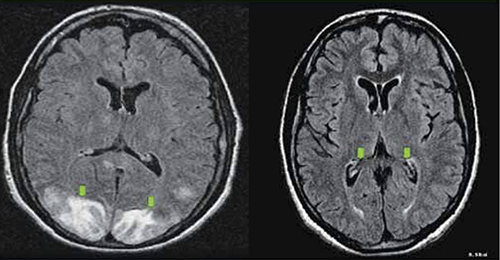
Green arrows point to vasogenic edema in the occipital lobes and, partially, the parietal lobes. The edema is gone on repeat magnetic resonance imaging (see Recommendation #9).
10. Act today, see a better outcome tomorrow
Avoid long-term maternal neurologic injury by managing eclampsia properly
Zeeman GG. Neurologic complications of preeclampsia. Semin Perinatol. 2009;33(3):166–172.
Residual neurologic damage is rare in the majority of women who have eclampsia. However, long-term cerebral white-matter injury (cytotoxic edema, infarction) on MRI imaging and impaired memory and cognitive function may develop in some women who have multiple seizures and who have inadequately controlled persistent severe hypertension.
We want to hear from you! Tell us what you think.
Health care models for treatment and management of diabetes
Type 2 diabetes is a complex, chronic illness that requires continuity of care as well as collaboration between healthcare practitioners and patients. The increasing incidence of type 2 diabetes, along with the fact that only about 12% of treated patients are able to achieve combined targets for glycated hemoglobin, blood pressure, and cholesterol, shows that it may be unrealistic to expect a chronic disease such as type 2 diabetes to be managed in a system designed for acute conditions. This supplement compares some of the existing health care models in the US for the treatment and management of diabetes patients. Although there is no single model of care that is able to fully overcome the obstacles facing diabetes patients and healthcare practitioners, the authors provide a candid view of the advantages and disadvantages of some traditional and nontraditional models of diabetes care.
Type 2 diabetes is a complex, chronic illness that requires continuity of care as well as collaboration between healthcare practitioners and patients. The increasing incidence of type 2 diabetes, along with the fact that only about 12% of treated patients are able to achieve combined targets for glycated hemoglobin, blood pressure, and cholesterol, shows that it may be unrealistic to expect a chronic disease such as type 2 diabetes to be managed in a system designed for acute conditions. This supplement compares some of the existing health care models in the US for the treatment and management of diabetes patients. Although there is no single model of care that is able to fully overcome the obstacles facing diabetes patients and healthcare practitioners, the authors provide a candid view of the advantages and disadvantages of some traditional and nontraditional models of diabetes care.
Type 2 diabetes is a complex, chronic illness that requires continuity of care as well as collaboration between healthcare practitioners and patients. The increasing incidence of type 2 diabetes, along with the fact that only about 12% of treated patients are able to achieve combined targets for glycated hemoglobin, blood pressure, and cholesterol, shows that it may be unrealistic to expect a chronic disease such as type 2 diabetes to be managed in a system designed for acute conditions. This supplement compares some of the existing health care models in the US for the treatment and management of diabetes patients. Although there is no single model of care that is able to fully overcome the obstacles facing diabetes patients and healthcare practitioners, the authors provide a candid view of the advantages and disadvantages of some traditional and nontraditional models of diabetes care.
Managing High-Risk Patients With Acute Coronary Syndrome
A supplement to Cardiology News. This supplement was sponsored by Merck.
Written by Paul Cerrato, Medical Writer
• Acute coronary syndrome
• Acute myocardial infarction
• GP IIb/IIIa inhibitors
• Eptifibatide
• Cardiology
• percutaneous coronary intervention
Faculty/Faculty Disclosures
Marc Cohen, MD, FACC
Director
Division of Cardiology
Newark Beth Israel
Medical Center
Newark, New Jersey
Professor of Medicine
Mount Sinai School
of Medicine
New York, New York
Dr Cohen has disclosed that he has served as an advisor or consultant for Bristol-Myers Squibb, Datascope, and sanofi-aventis; has received grant/research support from Bristol-Myers Squibb, Cordis, and Datascope; and has served as a speaker or a member of a speakers bureau for Bristol-Myers Squibb, Merck, and sanofi-aventis.
A supplement to Cardiology News. This supplement was sponsored by Merck.
Written by Paul Cerrato, Medical Writer
• Acute coronary syndrome
• Acute myocardial infarction
• GP IIb/IIIa inhibitors
• Eptifibatide
• Cardiology
• percutaneous coronary intervention
Faculty/Faculty Disclosures
Marc Cohen, MD, FACC
Director
Division of Cardiology
Newark Beth Israel
Medical Center
Newark, New Jersey
Professor of Medicine
Mount Sinai School
of Medicine
New York, New York
Dr Cohen has disclosed that he has served as an advisor or consultant for Bristol-Myers Squibb, Datascope, and sanofi-aventis; has received grant/research support from Bristol-Myers Squibb, Cordis, and Datascope; and has served as a speaker or a member of a speakers bureau for Bristol-Myers Squibb, Merck, and sanofi-aventis.
A supplement to Cardiology News. This supplement was sponsored by Merck.
Written by Paul Cerrato, Medical Writer
• Acute coronary syndrome
• Acute myocardial infarction
• GP IIb/IIIa inhibitors
• Eptifibatide
• Cardiology
• percutaneous coronary intervention
Faculty/Faculty Disclosures
Marc Cohen, MD, FACC
Director
Division of Cardiology
Newark Beth Israel
Medical Center
Newark, New Jersey
Professor of Medicine
Mount Sinai School
of Medicine
New York, New York
Dr Cohen has disclosed that he has served as an advisor or consultant for Bristol-Myers Squibb, Datascope, and sanofi-aventis; has received grant/research support from Bristol-Myers Squibb, Cordis, and Datascope; and has served as a speaker or a member of a speakers bureau for Bristol-Myers Squibb, Merck, and sanofi-aventis.
Clinical Perspectives in Pulmonary Arterial Hypertension
A Journal Scan supplement to Cardiology News. This promotional supplement was sponsored by Actelion Pharmaceuticals Ltd.
• Introduction
• Managing PAH - A Cardiologist's Perspective and A Pulmonologist's Perspective
• Clinical Classification of Pulmonary Arterial Hypertension
• Targeting Endothelin-1 in PAH With Bosentan
• Bosentan Therapy For Pulmonary Arterial Hypertension
• Treatment of Functional Class II PAH With Bosentan
• Treatment of Eisenmenger Syndrome with Bosentan
• Safety Profile Information
Faculty/Faculty Disclosures
Vallerie McLaughlin, MD
Professor of Medicine
University of Michigan
Ann Arbor, MI
Dr McLaughlin is a consultant to Actelion Pharmaceuticals Ltd., and Gilead, and has received funding for clinical grants from Actelion and United Therapeutics Corporation.
Richard Channick, MD
Director, Pulmonary Hypertension
Program, Massachusetts General
Hospital, Harvard Medical School
Boston, MA
Dr Channick is a consultant to, and has received funding for clinical grants from Actelion Pharmaceuticals Ltd., Gilead, and United Therapeutics Corporation.
A Journal Scan supplement to Cardiology News. This promotional supplement was sponsored by Actelion Pharmaceuticals Ltd.
• Introduction
• Managing PAH - A Cardiologist's Perspective and A Pulmonologist's Perspective
• Clinical Classification of Pulmonary Arterial Hypertension
• Targeting Endothelin-1 in PAH With Bosentan
• Bosentan Therapy For Pulmonary Arterial Hypertension
• Treatment of Functional Class II PAH With Bosentan
• Treatment of Eisenmenger Syndrome with Bosentan
• Safety Profile Information
Faculty/Faculty Disclosures
Vallerie McLaughlin, MD
Professor of Medicine
University of Michigan
Ann Arbor, MI
Dr McLaughlin is a consultant to Actelion Pharmaceuticals Ltd., and Gilead, and has received funding for clinical grants from Actelion and United Therapeutics Corporation.
Richard Channick, MD
Director, Pulmonary Hypertension
Program, Massachusetts General
Hospital, Harvard Medical School
Boston, MA
Dr Channick is a consultant to, and has received funding for clinical grants from Actelion Pharmaceuticals Ltd., Gilead, and United Therapeutics Corporation.
A Journal Scan supplement to Cardiology News. This promotional supplement was sponsored by Actelion Pharmaceuticals Ltd.
• Introduction
• Managing PAH - A Cardiologist's Perspective and A Pulmonologist's Perspective
• Clinical Classification of Pulmonary Arterial Hypertension
• Targeting Endothelin-1 in PAH With Bosentan
• Bosentan Therapy For Pulmonary Arterial Hypertension
• Treatment of Functional Class II PAH With Bosentan
• Treatment of Eisenmenger Syndrome with Bosentan
• Safety Profile Information
Faculty/Faculty Disclosures
Vallerie McLaughlin, MD
Professor of Medicine
University of Michigan
Ann Arbor, MI
Dr McLaughlin is a consultant to Actelion Pharmaceuticals Ltd., and Gilead, and has received funding for clinical grants from Actelion and United Therapeutics Corporation.
Richard Channick, MD
Director, Pulmonary Hypertension
Program, Massachusetts General
Hospital, Harvard Medical School
Boston, MA
Dr Channick is a consultant to, and has received funding for clinical grants from Actelion Pharmaceuticals Ltd., Gilead, and United Therapeutics Corporation.
Antiplatelet Therapy: Role of Effient (prasugrel)
A Best Practices supplement to Cardiology News. This promotional supplement was supported by Daiichi-Sankyo, Inc. and Eli Lilly and Company.
• Introduction
• Clinical Pharmacology
• TRITON-TIMI 38
• Bleeding
• Application of TRITON-TIMI 38 to Clinical Practice
• Conclusion
• Effient Important Safety Information
Faculty/Faculty Disclosures
Roxana Mehran, MD
Director of Interventional Cardiovascular Research and Clinical Trials
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Chief Scientific Officer
Clinical Trials Center
Cardiovascular Research Foundation
New York, NY
Dr Mehran receives grant support from sanofi-aventis/Bristol-Myers Squibb and is a consultant for Abbott Vascular, Accumetrics, Cardiva, and The Medicines Company and is a paid consultant to Daiichi Sankyo, Inc. and Lilly USA, LLC.
Benjamin Z. Galper, MD, MPH
Medical Resident
Department of Medicine
New York Presbyterian Hospital/Columbia University Medical Center
New York, NY
Dr Galper is a paid consultant of Daiichi Sankyo, Inc. and Lilly USA, LLC.
George D. Dangas, MD, PhD
Director of Cardiovascular Innovation
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Director, Academic Affairs
Cardiovascular Research Foundation
New York, NY
Dr Dangas is a consultant for AstraZeneca and Cordis Corp. (a Johnson & Johnson Company) and a paid consultant to
Daiichi Sankyo, Inc. and Lilly USA, LLC.
A Best Practices supplement to Cardiology News. This promotional supplement was supported by Daiichi-Sankyo, Inc. and Eli Lilly and Company.
• Introduction
• Clinical Pharmacology
• TRITON-TIMI 38
• Bleeding
• Application of TRITON-TIMI 38 to Clinical Practice
• Conclusion
• Effient Important Safety Information
Faculty/Faculty Disclosures
Roxana Mehran, MD
Director of Interventional Cardiovascular Research and Clinical Trials
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Chief Scientific Officer
Clinical Trials Center
Cardiovascular Research Foundation
New York, NY
Dr Mehran receives grant support from sanofi-aventis/Bristol-Myers Squibb and is a consultant for Abbott Vascular, Accumetrics, Cardiva, and The Medicines Company and is a paid consultant to Daiichi Sankyo, Inc. and Lilly USA, LLC.
Benjamin Z. Galper, MD, MPH
Medical Resident
Department of Medicine
New York Presbyterian Hospital/Columbia University Medical Center
New York, NY
Dr Galper is a paid consultant of Daiichi Sankyo, Inc. and Lilly USA, LLC.
George D. Dangas, MD, PhD
Director of Cardiovascular Innovation
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Director, Academic Affairs
Cardiovascular Research Foundation
New York, NY
Dr Dangas is a consultant for AstraZeneca and Cordis Corp. (a Johnson & Johnson Company) and a paid consultant to
Daiichi Sankyo, Inc. and Lilly USA, LLC.
A Best Practices supplement to Cardiology News. This promotional supplement was supported by Daiichi-Sankyo, Inc. and Eli Lilly and Company.
• Introduction
• Clinical Pharmacology
• TRITON-TIMI 38
• Bleeding
• Application of TRITON-TIMI 38 to Clinical Practice
• Conclusion
• Effient Important Safety Information
Faculty/Faculty Disclosures
Roxana Mehran, MD
Director of Interventional Cardiovascular Research and Clinical Trials
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Chief Scientific Officer
Clinical Trials Center
Cardiovascular Research Foundation
New York, NY
Dr Mehran receives grant support from sanofi-aventis/Bristol-Myers Squibb and is a consultant for Abbott Vascular, Accumetrics, Cardiva, and The Medicines Company and is a paid consultant to Daiichi Sankyo, Inc. and Lilly USA, LLC.
Benjamin Z. Galper, MD, MPH
Medical Resident
Department of Medicine
New York Presbyterian Hospital/Columbia University Medical Center
New York, NY
Dr Galper is a paid consultant of Daiichi Sankyo, Inc. and Lilly USA, LLC.
George D. Dangas, MD, PhD
Director of Cardiovascular Innovation
Zena and Michael A. Wiener Cardiovascular Institute
Mount Sinai School of Medicine
Professor of Medicine
Mount Sinai School of Medicine
Director, Academic Affairs
Cardiovascular Research Foundation
New York, NY
Dr Dangas is a consultant for AstraZeneca and Cordis Corp. (a Johnson & Johnson Company) and a paid consultant to
Daiichi Sankyo, Inc. and Lilly USA, LLC.
An Approach to the Management of Type 2 Diabetes Mellitus in Patients Receiving Add-On Therapy With Colesevelam HCl
A supplement to Cardiology News and sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.
A supplement to Cardiology News and sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.
A supplement to Cardiology News and sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.











