User login
Enlarging lesion on temple

A shave biopsy revealed acanthosis, papillomatosis, hyperkeratosis, hypergranulosis, parakeratosis, and cytoplasmic viral-like inclusions without atypia, consistent with a diagnosis of a common wart. The biopsy ruled out other possible diagnoses, which included keratoacanthoma, seborrheic keratosis, and squamous cell carcinoma.
Cutaneous warts can manifest as common warts (verruca vulgaris), plantar warts (verruca plantaris), or plane warts (verruca plana). These benign skin lesions are caused by human papillomavirus and can manifest in areas of skin trauma; this is known as the Koebner phenomenon. Most warts can be diagnosed through clinical history and examination. Dermoscopy, if performed, may reveal thrombosed capillaries as dotted structures, but there is an increased risk of cross-contamination.1 That said, some dermatoscopes have disposable covers or can be cleaned with antiviral, antibacterial wipes. If the diagnosis is unclear or the exam is clinically suspicious, a biopsy may be required.
Cases with progressive enlargement and extensive involvement of the skin (as was seen here) are generally associated with certain predisposing conditions, such as atopic dermatitis and immunosuppression.2 Our patient screened negative for HIV infection, and further evaluation did not reveal any concerns for immunosuppression.
Treatment for a common wart depends on patient characteristics, preferences, cost, and possible adverse effects. Standard treatment options are topical salicylic acid and cryotherapy with liquid nitrogen. Depending on the location and type of the wart, multiple treatments may be required, and recurrences are common. Intralesional injection with bleomycin, 5‐fluorouracil, or cidofovir is often used for recurrent and refractory warts.
Patients unable to tolerate cryotherapy or local injections may benefit from thermotherapy by heating the wart with a pulsed dye laser.3 Observation is also a reasonable course of action for new warts, as they may spontaneously resolve within a year.
In this case, the patient opted for over-the-counter salicylic acid 17% to be applied nightly until resolution. Cryosurgery would be a next step for him if the lesion does not resolve after 3 months of treatment.
Image courtesy of Faryal Tahir, MD. Text courtesy of Faryal Tahir, MD, Assistant Professor, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Mun JH, Park SM, Ko HC, et al. Prevention of possible cross-infection among patients by dermoscopy: a brief review of the literature and our suggestion. Dermatol Pract Concept. 2013;3:33-34. doi: 10.5826/dpc.0304a07
2. Leiding JW, Holland SM. Warts and all: human papillomavirus in primary immunodeficiencies. J Allergy Clin Immunol. 2012;130:1030-1048. doi: 10.1016/j.jaci.2012.07.049
3. Zhu P, Qi RQ, Yang Y, et al. Clinical guideline for the diagnosis and treatment of cutaneous warts (2022). J Evid Based Med. 2022;15:284-301. doi: 10.1111/jebm.12494

A shave biopsy revealed acanthosis, papillomatosis, hyperkeratosis, hypergranulosis, parakeratosis, and cytoplasmic viral-like inclusions without atypia, consistent with a diagnosis of a common wart. The biopsy ruled out other possible diagnoses, which included keratoacanthoma, seborrheic keratosis, and squamous cell carcinoma.
Cutaneous warts can manifest as common warts (verruca vulgaris), plantar warts (verruca plantaris), or plane warts (verruca plana). These benign skin lesions are caused by human papillomavirus and can manifest in areas of skin trauma; this is known as the Koebner phenomenon. Most warts can be diagnosed through clinical history and examination. Dermoscopy, if performed, may reveal thrombosed capillaries as dotted structures, but there is an increased risk of cross-contamination.1 That said, some dermatoscopes have disposable covers or can be cleaned with antiviral, antibacterial wipes. If the diagnosis is unclear or the exam is clinically suspicious, a biopsy may be required.
Cases with progressive enlargement and extensive involvement of the skin (as was seen here) are generally associated with certain predisposing conditions, such as atopic dermatitis and immunosuppression.2 Our patient screened negative for HIV infection, and further evaluation did not reveal any concerns for immunosuppression.
Treatment for a common wart depends on patient characteristics, preferences, cost, and possible adverse effects. Standard treatment options are topical salicylic acid and cryotherapy with liquid nitrogen. Depending on the location and type of the wart, multiple treatments may be required, and recurrences are common. Intralesional injection with bleomycin, 5‐fluorouracil, or cidofovir is often used for recurrent and refractory warts.
Patients unable to tolerate cryotherapy or local injections may benefit from thermotherapy by heating the wart with a pulsed dye laser.3 Observation is also a reasonable course of action for new warts, as they may spontaneously resolve within a year.
In this case, the patient opted for over-the-counter salicylic acid 17% to be applied nightly until resolution. Cryosurgery would be a next step for him if the lesion does not resolve after 3 months of treatment.
Image courtesy of Faryal Tahir, MD. Text courtesy of Faryal Tahir, MD, Assistant Professor, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.

A shave biopsy revealed acanthosis, papillomatosis, hyperkeratosis, hypergranulosis, parakeratosis, and cytoplasmic viral-like inclusions without atypia, consistent with a diagnosis of a common wart. The biopsy ruled out other possible diagnoses, which included keratoacanthoma, seborrheic keratosis, and squamous cell carcinoma.
Cutaneous warts can manifest as common warts (verruca vulgaris), plantar warts (verruca plantaris), or plane warts (verruca plana). These benign skin lesions are caused by human papillomavirus and can manifest in areas of skin trauma; this is known as the Koebner phenomenon. Most warts can be diagnosed through clinical history and examination. Dermoscopy, if performed, may reveal thrombosed capillaries as dotted structures, but there is an increased risk of cross-contamination.1 That said, some dermatoscopes have disposable covers or can be cleaned with antiviral, antibacterial wipes. If the diagnosis is unclear or the exam is clinically suspicious, a biopsy may be required.
Cases with progressive enlargement and extensive involvement of the skin (as was seen here) are generally associated with certain predisposing conditions, such as atopic dermatitis and immunosuppression.2 Our patient screened negative for HIV infection, and further evaluation did not reveal any concerns for immunosuppression.
Treatment for a common wart depends on patient characteristics, preferences, cost, and possible adverse effects. Standard treatment options are topical salicylic acid and cryotherapy with liquid nitrogen. Depending on the location and type of the wart, multiple treatments may be required, and recurrences are common. Intralesional injection with bleomycin, 5‐fluorouracil, or cidofovir is often used for recurrent and refractory warts.
Patients unable to tolerate cryotherapy or local injections may benefit from thermotherapy by heating the wart with a pulsed dye laser.3 Observation is also a reasonable course of action for new warts, as they may spontaneously resolve within a year.
In this case, the patient opted for over-the-counter salicylic acid 17% to be applied nightly until resolution. Cryosurgery would be a next step for him if the lesion does not resolve after 3 months of treatment.
Image courtesy of Faryal Tahir, MD. Text courtesy of Faryal Tahir, MD, Assistant Professor, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Mun JH, Park SM, Ko HC, et al. Prevention of possible cross-infection among patients by dermoscopy: a brief review of the literature and our suggestion. Dermatol Pract Concept. 2013;3:33-34. doi: 10.5826/dpc.0304a07
2. Leiding JW, Holland SM. Warts and all: human papillomavirus in primary immunodeficiencies. J Allergy Clin Immunol. 2012;130:1030-1048. doi: 10.1016/j.jaci.2012.07.049
3. Zhu P, Qi RQ, Yang Y, et al. Clinical guideline for the diagnosis and treatment of cutaneous warts (2022). J Evid Based Med. 2022;15:284-301. doi: 10.1111/jebm.12494
1. Mun JH, Park SM, Ko HC, et al. Prevention of possible cross-infection among patients by dermoscopy: a brief review of the literature and our suggestion. Dermatol Pract Concept. 2013;3:33-34. doi: 10.5826/dpc.0304a07
2. Leiding JW, Holland SM. Warts and all: human papillomavirus in primary immunodeficiencies. J Allergy Clin Immunol. 2012;130:1030-1048. doi: 10.1016/j.jaci.2012.07.049
3. Zhu P, Qi RQ, Yang Y, et al. Clinical guideline for the diagnosis and treatment of cutaneous warts (2022). J Evid Based Med. 2022;15:284-301. doi: 10.1111/jebm.12494
Enlarging pink patches after traveling

The patient’s multiple pink, subtly annular patches after recent travel to Lyme-endemic areas of the United States demonstrated a classic manifestation of disseminated Lyme disease. An enzyme-linked immunosorbent assay was positive for Borrelia burgdorferi IgM and IgG antibodies, confirming an acute infection.
While not usually necessary, skin biopsy shows a nonspecific perivascular cellular infiltrate that may be comprised of histiocytes, lymphocytes, and plasma cells. Spirochetes are not typically seen, but they may be identified with antibody-labeled or silver stains.
Lyme disease initially manifests as localized disease with erythema migrans, a targetoid lesion on the skin that appears at the site of the tick bite. This initial stage develops within the first few weeks of the bite and may be accompanied by fatigue and a low-grade fever.
If left untreated, the infection may progress to early disseminated disease, which occurs weeks to months after the initial bite. This second stage of Lyme disease manifests with multiple erythema migrans lesions on additional parts of the body, indicating spirochete dissemination through the bloodstream and lymphatic system. Early disseminated disease may also include borrelial lymphocytoma, Lyme neuroborreliosis, and cardiac conduction abnormalities such as AV block.
The third stage of Lyme disease, late Lyme disease, occurs months to years after an initial infection that has gone untreated. The key feature of this stage is arthritis, which tends to affect the knees and may be migratory in nature. Neurological symptoms such as encephalopathy and polyneuropathies may also develop. A minority of patients with late Lyme disease may develop acrodermatitis chronica atrophicans, a rash that typically occurs on the dorsal hands and feet as blue-red plaques that turn the affected skin atrophic.1
This patient was treated with a 3-week course of oral doxycycline 100 mg twice daily and was referred to an infectious disease specialist for further work-up of systemic symptoms, given the risk for cardiac pathology in disseminated Lyme disease.
Photo courtesy of Le Wen Chiu, MD. Text courtesy of Le Wen Chiu, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Cardenas-de la Garza JA, De la Cruz-Valadez E, Ocampo-Candiani J, et al. Clinical spectrum of Lyme disease. Eur J Clin Microbiol Infect Dis. 2019;38:201-208. doi:10.1007/s10096-018-3417-1

The patient’s multiple pink, subtly annular patches after recent travel to Lyme-endemic areas of the United States demonstrated a classic manifestation of disseminated Lyme disease. An enzyme-linked immunosorbent assay was positive for Borrelia burgdorferi IgM and IgG antibodies, confirming an acute infection.
While not usually necessary, skin biopsy shows a nonspecific perivascular cellular infiltrate that may be comprised of histiocytes, lymphocytes, and plasma cells. Spirochetes are not typically seen, but they may be identified with antibody-labeled or silver stains.
Lyme disease initially manifests as localized disease with erythema migrans, a targetoid lesion on the skin that appears at the site of the tick bite. This initial stage develops within the first few weeks of the bite and may be accompanied by fatigue and a low-grade fever.
If left untreated, the infection may progress to early disseminated disease, which occurs weeks to months after the initial bite. This second stage of Lyme disease manifests with multiple erythema migrans lesions on additional parts of the body, indicating spirochete dissemination through the bloodstream and lymphatic system. Early disseminated disease may also include borrelial lymphocytoma, Lyme neuroborreliosis, and cardiac conduction abnormalities such as AV block.
The third stage of Lyme disease, late Lyme disease, occurs months to years after an initial infection that has gone untreated. The key feature of this stage is arthritis, which tends to affect the knees and may be migratory in nature. Neurological symptoms such as encephalopathy and polyneuropathies may also develop. A minority of patients with late Lyme disease may develop acrodermatitis chronica atrophicans, a rash that typically occurs on the dorsal hands and feet as blue-red plaques that turn the affected skin atrophic.1
This patient was treated with a 3-week course of oral doxycycline 100 mg twice daily and was referred to an infectious disease specialist for further work-up of systemic symptoms, given the risk for cardiac pathology in disseminated Lyme disease.
Photo courtesy of Le Wen Chiu, MD. Text courtesy of Le Wen Chiu, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.

The patient’s multiple pink, subtly annular patches after recent travel to Lyme-endemic areas of the United States demonstrated a classic manifestation of disseminated Lyme disease. An enzyme-linked immunosorbent assay was positive for Borrelia burgdorferi IgM and IgG antibodies, confirming an acute infection.
While not usually necessary, skin biopsy shows a nonspecific perivascular cellular infiltrate that may be comprised of histiocytes, lymphocytes, and plasma cells. Spirochetes are not typically seen, but they may be identified with antibody-labeled or silver stains.
Lyme disease initially manifests as localized disease with erythema migrans, a targetoid lesion on the skin that appears at the site of the tick bite. This initial stage develops within the first few weeks of the bite and may be accompanied by fatigue and a low-grade fever.
If left untreated, the infection may progress to early disseminated disease, which occurs weeks to months after the initial bite. This second stage of Lyme disease manifests with multiple erythema migrans lesions on additional parts of the body, indicating spirochete dissemination through the bloodstream and lymphatic system. Early disseminated disease may also include borrelial lymphocytoma, Lyme neuroborreliosis, and cardiac conduction abnormalities such as AV block.
The third stage of Lyme disease, late Lyme disease, occurs months to years after an initial infection that has gone untreated. The key feature of this stage is arthritis, which tends to affect the knees and may be migratory in nature. Neurological symptoms such as encephalopathy and polyneuropathies may also develop. A minority of patients with late Lyme disease may develop acrodermatitis chronica atrophicans, a rash that typically occurs on the dorsal hands and feet as blue-red plaques that turn the affected skin atrophic.1
This patient was treated with a 3-week course of oral doxycycline 100 mg twice daily and was referred to an infectious disease specialist for further work-up of systemic symptoms, given the risk for cardiac pathology in disseminated Lyme disease.
Photo courtesy of Le Wen Chiu, MD. Text courtesy of Le Wen Chiu, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque, and Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Cardenas-de la Garza JA, De la Cruz-Valadez E, Ocampo-Candiani J, et al. Clinical spectrum of Lyme disease. Eur J Clin Microbiol Infect Dis. 2019;38:201-208. doi:10.1007/s10096-018-3417-1
1. Cardenas-de la Garza JA, De la Cruz-Valadez E, Ocampo-Candiani J, et al. Clinical spectrum of Lyme disease. Eur J Clin Microbiol Infect Dis. 2019;38:201-208. doi:10.1007/s10096-018-3417-1
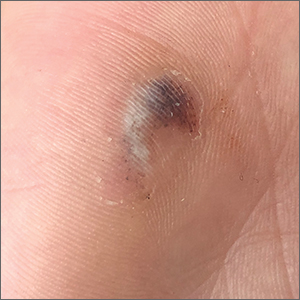
Hyperpigmented lesion on palm

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD

This patient had a posttraumatic tache noir (also known as talon noir on the volar aspect of the feet); it is a subcorneal hematoma. The diagnosis is made clinically. Dermoscopic evaluation of tache/talon noir will reveal “pebbles on a ridge” or “satellite globules.” Confirmation of tache/talon noir can be made by paring the corneum with a #15 blade, which will reveal blood in the shavings and punctate lesions.1
This patient noted that the knob of his baseball bat rubbed the hypothenar eminence of his nondominant hand when he took a swing. The sheer force of the knob led to the subcorneal hematoma. Tache noir was high on the differential due to his physician’s clinical experience with similar cases. Tache noir occurs predominantly in people ages 12 to 24 years, without regard to gender.2 The condition is commonly found in athletes who participate in baseball, cricket, racquet sports, weightlifting, and rock climbing.2-4
Talon noir occurs most commonly in athletes who are frequently jumping, turning, and pivoting, as in football, basketball, tennis, and lacrosse.
Tache noir can be differentiated from other conditions by the presence of preserved architecture of the skin surface and punctate capillaries beneath the stratum corneum. The differential diagnosis includes verruca vulgaris, acral melanoma, and a traumatic tattoo.
Talon/tache noir are benign conditions that do not require treatment and do not affect sports performance. The lesion will usually self-resolve within a matter of weeks from onset or can even be gently scraped with a sterile needle or blade.
This patient was advised that the lesion would resolve on its own. His knee pain was determined to be a simple case of patellofemoral syndrome or “runner’s knee” and he opted to complete a home exercise program to obtain relief.
This case was adapted from: Warden D. Hyperpigmented lesion on left palm. J Fam Pract. 2021;70:459-460. Photos courtesy of Daniel Warden, MD
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.
1. Googe AB, Schulmeier JS, Jackson AR, et al. Talon noir: paring can eliminate the need for biopsy. Postgrad Med J. 2014;90:730-731. doi: 10.1136/postgradmedj-2014-132996
2. Burkhart C, Nguyen N. Talon noire. Dermatology Advisor. Accessed October 19, 2021. www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/talon-noire-black-heel-calcaneal-petechiae-runners-heel-basketball-heel-tennis-heel-hyperkeratosis-hemorrhagica-pseudochromhidrosis-plantaris-chromidrose-plantaire-eccrine-intracorne/
3. Talon noir. Primary Care Dermatology Society. Updated August 1, 2021. Accessed October 19, 2021. www.pcds.org.uk/clinical-guidance/talon-noir
4. Birrer RB, Griesemer BA, Cataletto MB, eds. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; 2002.
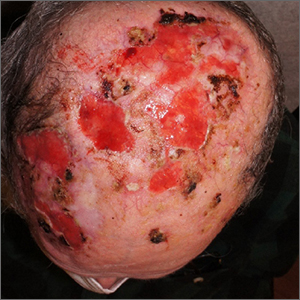
Nonhealing postsurgical scalp ulcers

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425
Painful fingertip tumor in pregnancy

This friable vascular papule was most consistent with a lobular capillary hemangioma (LCH), also called a pyogenic granuloma. A shave biopsy was performed at the base of the tumor to confirm the diagnosis and rule out malignant pedunculated tumors, including nodular melanoma, angiosarcoma, and metastatic carcinoma.
LCHs are benign vascular growths that occur on the skin and mucosa, most often in children and young adults. Growth may occur rapidly over days to weeks and tumors may grow to several centimeters in size. Although LCHs are often painless, they do tend to bleed easily with minor trauma.
While the triggering mechanism is unknown, LCHs have been associated with infection, trauma, hormonal factors (especially in the second and third trimesters of pregnancy), and therapy with retinoids. About 5% of pregnancies are associated with the development of an LCH on the oral mucosa, usually in the second or third trimester.1
Treatment of LCHs is based on small case series and case reports. Individual tumors have a high likelihood of recurrence after a single treatment, so multiple visits for treatment are often recommended. Electrocautery is safe and effective with complete cure occurring after 2 sessions. Similarly, cryotherapy is safe and effective with excellent results after 3 treatment sessions. Cryotherapy may cause depigmentation in patients with darker skin types, so this should be discussed with patients with skin of color. Excision of small lesions is also safe and effective in a single session.2
This patient was treated with light electrodessication and curettage in 2 sessions with complete clearance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Demir Y, Demir S, Aktepe F. Cutaneous lobular capillary hemangioma induced by pregnancy. J Cutan Pathol. 2004;31:77-80. doi: 10.1046/j.0303-6987.2004.0137.x
2. Lee J, Sinno H, Tahiri Y, et al. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011;64:1216-1220. doi: 10.1016/j.bjps.2010.12.021

This friable vascular papule was most consistent with a lobular capillary hemangioma (LCH), also called a pyogenic granuloma. A shave biopsy was performed at the base of the tumor to confirm the diagnosis and rule out malignant pedunculated tumors, including nodular melanoma, angiosarcoma, and metastatic carcinoma.
LCHs are benign vascular growths that occur on the skin and mucosa, most often in children and young adults. Growth may occur rapidly over days to weeks and tumors may grow to several centimeters in size. Although LCHs are often painless, they do tend to bleed easily with minor trauma.
While the triggering mechanism is unknown, LCHs have been associated with infection, trauma, hormonal factors (especially in the second and third trimesters of pregnancy), and therapy with retinoids. About 5% of pregnancies are associated with the development of an LCH on the oral mucosa, usually in the second or third trimester.1
Treatment of LCHs is based on small case series and case reports. Individual tumors have a high likelihood of recurrence after a single treatment, so multiple visits for treatment are often recommended. Electrocautery is safe and effective with complete cure occurring after 2 sessions. Similarly, cryotherapy is safe and effective with excellent results after 3 treatment sessions. Cryotherapy may cause depigmentation in patients with darker skin types, so this should be discussed with patients with skin of color. Excision of small lesions is also safe and effective in a single session.2
This patient was treated with light electrodessication and curettage in 2 sessions with complete clearance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

This friable vascular papule was most consistent with a lobular capillary hemangioma (LCH), also called a pyogenic granuloma. A shave biopsy was performed at the base of the tumor to confirm the diagnosis and rule out malignant pedunculated tumors, including nodular melanoma, angiosarcoma, and metastatic carcinoma.
LCHs are benign vascular growths that occur on the skin and mucosa, most often in children and young adults. Growth may occur rapidly over days to weeks and tumors may grow to several centimeters in size. Although LCHs are often painless, they do tend to bleed easily with minor trauma.
While the triggering mechanism is unknown, LCHs have been associated with infection, trauma, hormonal factors (especially in the second and third trimesters of pregnancy), and therapy with retinoids. About 5% of pregnancies are associated with the development of an LCH on the oral mucosa, usually in the second or third trimester.1
Treatment of LCHs is based on small case series and case reports. Individual tumors have a high likelihood of recurrence after a single treatment, so multiple visits for treatment are often recommended. Electrocautery is safe and effective with complete cure occurring after 2 sessions. Similarly, cryotherapy is safe and effective with excellent results after 3 treatment sessions. Cryotherapy may cause depigmentation in patients with darker skin types, so this should be discussed with patients with skin of color. Excision of small lesions is also safe and effective in a single session.2
This patient was treated with light electrodessication and curettage in 2 sessions with complete clearance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Demir Y, Demir S, Aktepe F. Cutaneous lobular capillary hemangioma induced by pregnancy. J Cutan Pathol. 2004;31:77-80. doi: 10.1046/j.0303-6987.2004.0137.x
2. Lee J, Sinno H, Tahiri Y, et al. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011;64:1216-1220. doi: 10.1016/j.bjps.2010.12.021
1. Demir Y, Demir S, Aktepe F. Cutaneous lobular capillary hemangioma induced by pregnancy. J Cutan Pathol. 2004;31:77-80. doi: 10.1046/j.0303-6987.2004.0137.x
2. Lee J, Sinno H, Tahiri Y, et al. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011;64:1216-1220. doi: 10.1016/j.bjps.2010.12.021
Persistent ‘postherpetic neuralgia’ and well-demarcated plaque
A 75-YEAR-OLD MAN presented to the dermatology clinic for evaluation of localized, persistent burning pain and discomfort attributed to shingles and postherpetic neuralgia. He had received a diagnosis of shingles on his left upper back about 3 years prior to this presentation.
In the ensuing years, the patient had been evaluated and treated by his primary care physician, a pain management team, and a neurologist. These clinicians treated the symptoms as postherpetic neuralgia, with no consensus explanation for the skin findings. The patient reported that his symptoms were unresponsive to trials of gabapentin 800 mg tid, duloxetine 60 mg PO qd, and acetaminophen 1 to 3 g/d PO. He also had undergone several rounds of acupuncture, thoracic and cervical spine steroid injections, and epidurals, without resolution of symptoms. The patient believed the only treatment that helped was a lidocaine 4% patch, which he had used nearly every day for the previous 3 years.
Physical exam by the dermatologist revealed a lidocaine patch applied to the patient’s left upper back. Upon its removal, skin examination showed a well-demarcated, erythematous, hyperpigmented, lichenified plaque with excoriations and erosions where the patch had been (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Contact dermatitis
The patient’s history and skin exam provided enough information to diagnose contact dermatitis. The pruritus, burning, and pain the patient had experienced were due to continuous application of the lidocaine patch to the area rather than postherpetic neuralgia.
There are 2 types of contact dermatitis: irritant and allergic. Irritant contact dermatitis is an inflammatory reaction caused directly by a substance, while allergic contact dermatitis is a delayed hypersensitivity reaction to specific allergens.1 While data to elucidate the incidence and prevalence of allergic contact dermatitis are unknown, common causes include latex, dyes, oils, resins, and compounds in textiles, rubber, cosmetics, and other products used in daily life.1
Allergic contact dermatitis due to lidocaine is becoming more prevalent with increased use and availability of over-the-counter products.2 A retrospective chart review of 1819 patch-tested patients from the University of British Columbia Contact Dermatitis Clinic showed a significant proportion of patients (2.4%) were found to have
The differential varies by area affected
The differential diagnosis for contact dermatitis varies by area affected and the distribution of rash. Atopic dermatitis, lichen planus, and psoriasis are a few dermatologic conditions to consider in the differential diagnosis. They can look similar to contact dermatitis, but the patient’s history can help to discern the most likely diagnosis.1
Atopic dermatitis is a complex dysfunction of the skin barrier and immune factors that often begins in childhood and persists in some patients throughout their lifetime. Atopic dermatitis is associated with other forms of atopy including asthma, allergic rhinitis, and food and contact allergies. Atopic dermatitis in the absence of contact allergies may manifest with chronic, diffuse, scaly patches with poorly defined borders. The patches appear in a symmetrical distribution and favor the flexural surfaces, such as the antecubital fossa, wrists, and neck.
Continue to: Lichen planus
Lichen planus most often manifests in the fourth through sixth decade of life as flat-topped itchy pink-to-purple polygonal papules to plaques. Lesions range from 2 to 10 mm and favor the volar wrists, shins, and lower back, although they may be widespread. Oral lesions manifesting as ulcers or white lacy patches in the buccal mucosa are common and may be a clue to the diagnosis. Unlike more generalized contact dermatitis, lichen planus lesions are discrete.
Psoriasis manifests as well-demarcated scaly plaques distributed symmetrically over extensor surfaces. The plaques commonly are found on the elbows, knees, and scalp. When psoriasis manifests in a very limited form (as just a single plaque or limited number of plaques), it can be hard to confidently exclude other etiologies. In these circumstances, look for psoriasis signs in more unique locations (eg, pitting in the nails or plaques on the scalp or in the gluteal cleft). Adding those findings to an otherwise solitary plaque significantly adds to diagnostic certainty.
Diagnosis entails getting the shape of things
Diagnosis is based on history of exposure to irritating or allergic substances, as well as a clinical exam. Skin examination of contact dermatitis can vary based on how long it has been present: Acute manifestations include erythema, oozing, scale, vesicles, and bullae, while chronic contact dermatitis tends to demonstrate lichenification and scale.1
Distinctive findings. The most distinctive physical exam findings in patients with contact dermatitis are often shape and distribution of the rash, which reflect points of contact with the offending agent. This clue helped to elucidate the diagnosis in our patient: his rash was perfectly demarcated within the precise area where the patch was applied daily.
Irritant vs allergic. Patch testing can be performed to differentiate irritant vs allergic contact dermatitis.1 Irritant contact dermatitis usually is apparent when removing a patch and will resolve over a day, whereas allergic contact dermatitis forms over time and the skin rash is most prominent several days after the patch has been removed.1
Continue to: Treatment
Treatment: First, stop the offense
Treatment of both variants of contact dermatitis includes avoidance of the causative substance and symptomatic treatment with topical steroids, antihistamines, and possibly oral steroids depending on the severity.1
For our patient, a viral swab was taken and submitted for varicella zoster virus polymerase chain reaction testing to rule out persistent herpes zoster infection; the result was negative. The patient was counseled to discontinue use of the lidocaine patch.
Given the severity and protracted duration of the patient’s symptoms, he also was started on high-potency topical steroids (clobetasol 0.05% ointment to be applied twice daily under occlusion for 2 months), a 4-week prednisone taper (60 mg × 1 week, 40 mg × 1 week, 20 mg × 1 week, 10 mg × 1 week, then stop), and hydroxyzine (25 mg nightly as needed for pruritus). The patient’s rash and symptoms improved dramatically within the first few doses of prednisone and completely cleared by Week 4 of the prednisone taper. At his follow-up appointment 1 month after completing the prednisone taper, he stated that the pain on his back had resolved
1. Li Y, Li L. Contact dermatitis: classifications and management. Clin Rev Allergy Immunol. 2021;61:245-281. doi: 10.1007/s12016-021-08875-0
2. Cline AE, Turrentine JE. Compounded topical analgesics for chronic pain. Dermatitis. 2016;27:263-271. doi: 10.1097/DER.0000000000000216
3. To D, Kossintseva I, de Gannes G. Lidocaine contact allergy is becoming more prevalent. Dermatol Surg. 2014;40:1367-1372. doi: 10.1097/DSS.0000000000000190
A 75-YEAR-OLD MAN presented to the dermatology clinic for evaluation of localized, persistent burning pain and discomfort attributed to shingles and postherpetic neuralgia. He had received a diagnosis of shingles on his left upper back about 3 years prior to this presentation.
In the ensuing years, the patient had been evaluated and treated by his primary care physician, a pain management team, and a neurologist. These clinicians treated the symptoms as postherpetic neuralgia, with no consensus explanation for the skin findings. The patient reported that his symptoms were unresponsive to trials of gabapentin 800 mg tid, duloxetine 60 mg PO qd, and acetaminophen 1 to 3 g/d PO. He also had undergone several rounds of acupuncture, thoracic and cervical spine steroid injections, and epidurals, without resolution of symptoms. The patient believed the only treatment that helped was a lidocaine 4% patch, which he had used nearly every day for the previous 3 years.
Physical exam by the dermatologist revealed a lidocaine patch applied to the patient’s left upper back. Upon its removal, skin examination showed a well-demarcated, erythematous, hyperpigmented, lichenified plaque with excoriations and erosions where the patch had been (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Contact dermatitis
The patient’s history and skin exam provided enough information to diagnose contact dermatitis. The pruritus, burning, and pain the patient had experienced were due to continuous application of the lidocaine patch to the area rather than postherpetic neuralgia.
There are 2 types of contact dermatitis: irritant and allergic. Irritant contact dermatitis is an inflammatory reaction caused directly by a substance, while allergic contact dermatitis is a delayed hypersensitivity reaction to specific allergens.1 While data to elucidate the incidence and prevalence of allergic contact dermatitis are unknown, common causes include latex, dyes, oils, resins, and compounds in textiles, rubber, cosmetics, and other products used in daily life.1
Allergic contact dermatitis due to lidocaine is becoming more prevalent with increased use and availability of over-the-counter products.2 A retrospective chart review of 1819 patch-tested patients from the University of British Columbia Contact Dermatitis Clinic showed a significant proportion of patients (2.4%) were found to have
The differential varies by area affected
The differential diagnosis for contact dermatitis varies by area affected and the distribution of rash. Atopic dermatitis, lichen planus, and psoriasis are a few dermatologic conditions to consider in the differential diagnosis. They can look similar to contact dermatitis, but the patient’s history can help to discern the most likely diagnosis.1
Atopic dermatitis is a complex dysfunction of the skin barrier and immune factors that often begins in childhood and persists in some patients throughout their lifetime. Atopic dermatitis is associated with other forms of atopy including asthma, allergic rhinitis, and food and contact allergies. Atopic dermatitis in the absence of contact allergies may manifest with chronic, diffuse, scaly patches with poorly defined borders. The patches appear in a symmetrical distribution and favor the flexural surfaces, such as the antecubital fossa, wrists, and neck.
Continue to: Lichen planus
Lichen planus most often manifests in the fourth through sixth decade of life as flat-topped itchy pink-to-purple polygonal papules to plaques. Lesions range from 2 to 10 mm and favor the volar wrists, shins, and lower back, although they may be widespread. Oral lesions manifesting as ulcers or white lacy patches in the buccal mucosa are common and may be a clue to the diagnosis. Unlike more generalized contact dermatitis, lichen planus lesions are discrete.
Psoriasis manifests as well-demarcated scaly plaques distributed symmetrically over extensor surfaces. The plaques commonly are found on the elbows, knees, and scalp. When psoriasis manifests in a very limited form (as just a single plaque or limited number of plaques), it can be hard to confidently exclude other etiologies. In these circumstances, look for psoriasis signs in more unique locations (eg, pitting in the nails or plaques on the scalp or in the gluteal cleft). Adding those findings to an otherwise solitary plaque significantly adds to diagnostic certainty.
Diagnosis entails getting the shape of things
Diagnosis is based on history of exposure to irritating or allergic substances, as well as a clinical exam. Skin examination of contact dermatitis can vary based on how long it has been present: Acute manifestations include erythema, oozing, scale, vesicles, and bullae, while chronic contact dermatitis tends to demonstrate lichenification and scale.1
Distinctive findings. The most distinctive physical exam findings in patients with contact dermatitis are often shape and distribution of the rash, which reflect points of contact with the offending agent. This clue helped to elucidate the diagnosis in our patient: his rash was perfectly demarcated within the precise area where the patch was applied daily.
Irritant vs allergic. Patch testing can be performed to differentiate irritant vs allergic contact dermatitis.1 Irritant contact dermatitis usually is apparent when removing a patch and will resolve over a day, whereas allergic contact dermatitis forms over time and the skin rash is most prominent several days after the patch has been removed.1
Continue to: Treatment
Treatment: First, stop the offense
Treatment of both variants of contact dermatitis includes avoidance of the causative substance and symptomatic treatment with topical steroids, antihistamines, and possibly oral steroids depending on the severity.1
For our patient, a viral swab was taken and submitted for varicella zoster virus polymerase chain reaction testing to rule out persistent herpes zoster infection; the result was negative. The patient was counseled to discontinue use of the lidocaine patch.
Given the severity and protracted duration of the patient’s symptoms, he also was started on high-potency topical steroids (clobetasol 0.05% ointment to be applied twice daily under occlusion for 2 months), a 4-week prednisone taper (60 mg × 1 week, 40 mg × 1 week, 20 mg × 1 week, 10 mg × 1 week, then stop), and hydroxyzine (25 mg nightly as needed for pruritus). The patient’s rash and symptoms improved dramatically within the first few doses of prednisone and completely cleared by Week 4 of the prednisone taper. At his follow-up appointment 1 month after completing the prednisone taper, he stated that the pain on his back had resolved
A 75-YEAR-OLD MAN presented to the dermatology clinic for evaluation of localized, persistent burning pain and discomfort attributed to shingles and postherpetic neuralgia. He had received a diagnosis of shingles on his left upper back about 3 years prior to this presentation.
In the ensuing years, the patient had been evaluated and treated by his primary care physician, a pain management team, and a neurologist. These clinicians treated the symptoms as postherpetic neuralgia, with no consensus explanation for the skin findings. The patient reported that his symptoms were unresponsive to trials of gabapentin 800 mg tid, duloxetine 60 mg PO qd, and acetaminophen 1 to 3 g/d PO. He also had undergone several rounds of acupuncture, thoracic and cervical spine steroid injections, and epidurals, without resolution of symptoms. The patient believed the only treatment that helped was a lidocaine 4% patch, which he had used nearly every day for the previous 3 years.
Physical exam by the dermatologist revealed a lidocaine patch applied to the patient’s left upper back. Upon its removal, skin examination showed a well-demarcated, erythematous, hyperpigmented, lichenified plaque with excoriations and erosions where the patch had been (FIGURE).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Contact dermatitis
The patient’s history and skin exam provided enough information to diagnose contact dermatitis. The pruritus, burning, and pain the patient had experienced were due to continuous application of the lidocaine patch to the area rather than postherpetic neuralgia.
There are 2 types of contact dermatitis: irritant and allergic. Irritant contact dermatitis is an inflammatory reaction caused directly by a substance, while allergic contact dermatitis is a delayed hypersensitivity reaction to specific allergens.1 While data to elucidate the incidence and prevalence of allergic contact dermatitis are unknown, common causes include latex, dyes, oils, resins, and compounds in textiles, rubber, cosmetics, and other products used in daily life.1
Allergic contact dermatitis due to lidocaine is becoming more prevalent with increased use and availability of over-the-counter products.2 A retrospective chart review of 1819 patch-tested patients from the University of British Columbia Contact Dermatitis Clinic showed a significant proportion of patients (2.4%) were found to have
The differential varies by area affected
The differential diagnosis for contact dermatitis varies by area affected and the distribution of rash. Atopic dermatitis, lichen planus, and psoriasis are a few dermatologic conditions to consider in the differential diagnosis. They can look similar to contact dermatitis, but the patient’s history can help to discern the most likely diagnosis.1
Atopic dermatitis is a complex dysfunction of the skin barrier and immune factors that often begins in childhood and persists in some patients throughout their lifetime. Atopic dermatitis is associated with other forms of atopy including asthma, allergic rhinitis, and food and contact allergies. Atopic dermatitis in the absence of contact allergies may manifest with chronic, diffuse, scaly patches with poorly defined borders. The patches appear in a symmetrical distribution and favor the flexural surfaces, such as the antecubital fossa, wrists, and neck.
Continue to: Lichen planus
Lichen planus most often manifests in the fourth through sixth decade of life as flat-topped itchy pink-to-purple polygonal papules to plaques. Lesions range from 2 to 10 mm and favor the volar wrists, shins, and lower back, although they may be widespread. Oral lesions manifesting as ulcers or white lacy patches in the buccal mucosa are common and may be a clue to the diagnosis. Unlike more generalized contact dermatitis, lichen planus lesions are discrete.
Psoriasis manifests as well-demarcated scaly plaques distributed symmetrically over extensor surfaces. The plaques commonly are found on the elbows, knees, and scalp. When psoriasis manifests in a very limited form (as just a single plaque or limited number of plaques), it can be hard to confidently exclude other etiologies. In these circumstances, look for psoriasis signs in more unique locations (eg, pitting in the nails or plaques on the scalp or in the gluteal cleft). Adding those findings to an otherwise solitary plaque significantly adds to diagnostic certainty.
Diagnosis entails getting the shape of things
Diagnosis is based on history of exposure to irritating or allergic substances, as well as a clinical exam. Skin examination of contact dermatitis can vary based on how long it has been present: Acute manifestations include erythema, oozing, scale, vesicles, and bullae, while chronic contact dermatitis tends to demonstrate lichenification and scale.1
Distinctive findings. The most distinctive physical exam findings in patients with contact dermatitis are often shape and distribution of the rash, which reflect points of contact with the offending agent. This clue helped to elucidate the diagnosis in our patient: his rash was perfectly demarcated within the precise area where the patch was applied daily.
Irritant vs allergic. Patch testing can be performed to differentiate irritant vs allergic contact dermatitis.1 Irritant contact dermatitis usually is apparent when removing a patch and will resolve over a day, whereas allergic contact dermatitis forms over time and the skin rash is most prominent several days after the patch has been removed.1
Continue to: Treatment
Treatment: First, stop the offense
Treatment of both variants of contact dermatitis includes avoidance of the causative substance and symptomatic treatment with topical steroids, antihistamines, and possibly oral steroids depending on the severity.1
For our patient, a viral swab was taken and submitted for varicella zoster virus polymerase chain reaction testing to rule out persistent herpes zoster infection; the result was negative. The patient was counseled to discontinue use of the lidocaine patch.
Given the severity and protracted duration of the patient’s symptoms, he also was started on high-potency topical steroids (clobetasol 0.05% ointment to be applied twice daily under occlusion for 2 months), a 4-week prednisone taper (60 mg × 1 week, 40 mg × 1 week, 20 mg × 1 week, 10 mg × 1 week, then stop), and hydroxyzine (25 mg nightly as needed for pruritus). The patient’s rash and symptoms improved dramatically within the first few doses of prednisone and completely cleared by Week 4 of the prednisone taper. At his follow-up appointment 1 month after completing the prednisone taper, he stated that the pain on his back had resolved
1. Li Y, Li L. Contact dermatitis: classifications and management. Clin Rev Allergy Immunol. 2021;61:245-281. doi: 10.1007/s12016-021-08875-0
2. Cline AE, Turrentine JE. Compounded topical analgesics for chronic pain. Dermatitis. 2016;27:263-271. doi: 10.1097/DER.0000000000000216
3. To D, Kossintseva I, de Gannes G. Lidocaine contact allergy is becoming more prevalent. Dermatol Surg. 2014;40:1367-1372. doi: 10.1097/DSS.0000000000000190
1. Li Y, Li L. Contact dermatitis: classifications and management. Clin Rev Allergy Immunol. 2021;61:245-281. doi: 10.1007/s12016-021-08875-0
2. Cline AE, Turrentine JE. Compounded topical analgesics for chronic pain. Dermatitis. 2016;27:263-271. doi: 10.1097/DER.0000000000000216
3. To D, Kossintseva I, de Gannes G. Lidocaine contact allergy is becoming more prevalent. Dermatol Surg. 2014;40:1367-1372. doi: 10.1097/DSS.0000000000000190
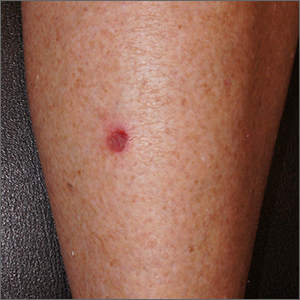
Small persistent leg wound

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x
Inner lip erosions

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.

The patient was having a flare of pemphigus vulgaris (PV), a rare and sometimes life-threatening acquired autoimmune blistering disease that affects the skin and/or mucosa. Ashkenazi Jewish patients and patients from Mediterranean and Middle Eastern countries are more likely to be affected.
In PV, acquired autoantibodies target the desmosomes that connect epithelial cells together, weakening the intercellular adhesion. It can affect skin, mucosa, or both. Patients present with fragile bullae or ulcers. The connections between the cells are often so damaged that rubbing on the skin creates a new blister called “Nikolsky sign.” In the mouth, bullae erode rapidly. Look for disease affecting the ocular conjunctiva or sclera, as well. PV can also occasionally affect the nasopharynx and esophagus, usually manifesting as hemoptysis, dysphagia, and nosebleeds with ulcer seen on endoscopy or otolaryngoscopy.
Although PV is often severe (and can warrant hospitalization when significant body surface area is involved), some patients may have few active lesions and can be managed safely as outpatients.
The diagnosis requires 2 biopsies and serum for indirect immunofluorescence. One biopsy (either by punch or shave to the upper dermis) is taken from the edge of a bulla or ulcer. Another biopsy (by punch or shave) is taken from nearby normal-looking skin or mucosa for testing the direct immunofluorescence pattern. In the mucosa, a punch biopsy may be left open or closed with absorbable sutures. A serum sample is taken for indirect immunofluorescence to differentiate pemphigus vulgaris from other forms of pemphigus.1
PV is treated by suppressing the immune system. Focal disease may be treated with super-potent topical steroids, including clobetasol 0.05% ointment. Even in the mouth, topical clobetasol 0.05% may be used off-label twice daily until control is achieved. When topical treatment is used in the mouth, advise patients to apply the clobetasol ointment to a piece of gauze and place the gauze (ointment side down) over affected areas for 20 to 30 minutes twice daily.
Patients with widespread or severe disease should be hospitalized. In severe cases, supportive wound care is provided, and treatment is aimed at immunosuppression. Systemic options include high-dose prednisone 0.5 to 1 mg/kg daily until clear, a steroid-sparing immunosuppressant such as mycophenolate mofetil up to 1000 mg bid, or rituximab in 1 of several regimens.
Three years prior to this patient’s visit, she had been successfully treated for PV with a course of rituximab. To treat the current flare, she was started on prednisone 60 mg/d. In addition, the plan was for her to complete 2 infusions of 1000 mg rituximab 2 weeks apart.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174
1. Didona, D, Schmidt, MF, Maglie, R, et al. Pemphigus and pemphigoids: clinical presentation, diagnosis and therapy. J Dtsch Dermatol Ges. 2023;1-20. doi: 10.1111/ddg.15174