User login
Let’s Dance: A Holistic Approach to Treating Veterans With Posttraumatic Stress Disorder
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
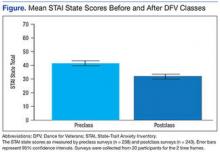
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.
Shared Medical Appointments for Glycemic Management in Rural Veterans
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
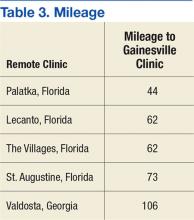
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
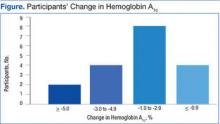
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
In 2005, the VA mandated shared medical appointments (SMAs) to improve clinic efficiency and quality of care. Both local and national Advanced Clinic Access meetings endorsed this method for decreasing wait times, improving patient outcome measures, and minimizing cost. Additionally, SMAs offer an opportunity to use nonphysician providers to their fullest potential. The VA has recognized the important role nonphysicians play in improving care for patients, especially patients with chronic illnesses, such as diabetes mellitus (DM).1
Based on the chronic care model, SMAs are patient medical appointments in which a multidisciplinary/multiexpertise team of providers sees a group of 8 to 20 patients in a 1.5- to 2-hour visit. Chronic illnesses, such as DM, are right for this approach.1
Diabetes mellitus is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults. It also is a major cause of heart disease and stroke, and the seventh leading cause of death in the U.S. The total cost of diagnosed DM in the U.S. in 2012 was $245 billion compared with $174 billion in 2007.2 Direct medical costs accounted for $176 billion, and $69 billion accounted for indirect costs, such as disability, work loss, and premature mortality.2 After adjusting for population age and sex differences, the average medical expenses among people diagnosed with DM were 2.3 times higher than medical expenses for those without DM. This figure does not include the cost of undiagnosed diabetes, prediabetes, or gestational diabetes.2
The purpose of this quality improvement study is to describe the results of SMA for management of DM conducted largely among rural veterans. The effectiveness of DM SMAs has been documented in several previous studies.3-10 However, this study focuses on using SMAs to manage veterans with DM in a rural environment.
Methods
The authors used the Primary Care Almanac (PCA) of the VHA Support Service Center to identify potential study participants at Lake City VAMC in Florida. The PCA is a database of VA primary care patients. The authors identified patients with hemoglobin A1c (HbA1c) level > 9% through the DM Cohort Reports Menu. Veterans with behavioral issues and those with high no-show rates were excluded.
The clinic staff called the eligible participants, educated them about SMA, and asked whether they would be interested in attending a DM SMA. If interested, they were scheduled for the next SMA. If uninterested, they were offered DM home telehealth follow-up, an appointment with the DM pharmacist, an appointment with the dietitian, enrollment into a DM education class, or routine follow-up with their primary care provider (PCP). Using this method, 18 patients were scheduled for the DM SMA between November 2010 and April 2013.
SMA Procedures
A physician or advanced registered nurse practitioner (ARNP) led each appointment, and in most cases other staff attended, including a clinical pharmacist, physical therapist (PT), kinesiotherapist (KT), dietician, social worker, registered nurse (RN), patient educator, and mental health provider. A pharmacist and RN attended all SMA appointments. The basic format consisted of a 90-minute appointment and included an abbreviated, clothed physical exam, which included vital signs; auscultation of heart, lungs, and abdomen; and foot exam. If a veteran had not received an eye exam within the year, an eye clinic consult was ordered. There were 10- to 30-minute blocks of time for the support staff who attended. The physician or ARNP usually led the appointment, and in addition to speaking to the group and discussing a daily topic, also spoke one-on-one with each veteran while support staff spoke to other group members.
During the appointment, the pharmacist answered questions and reviewed and adjusted medications as needed. The RN educator acted as a transcriptionist and answered questions. The PT/KT led interactive exercises. The dietitian answered questions, gave out educational materials, and did cooking demonstrations. The psychologist discussed behavioral health goals and asked each veteran to set a health goal to evaluate at the next meeting. The nursing staff in the primary care clinic checked in the patients. One nurse checked-in 1 to 2 patients and gave the patient a medication list.
Appointments were held every 2 to 3 months. All veterans attending were invited to come to the next appointment, and new patients were enrolled throughout the study. The new veterans were invited based on HbA1c readings pulled from the PCA database.
Hemoglobin A1c, blood pressure (BP), weight, and lipid level data were collected. Participation ended when HbA1c improved to < 8%, a patient was no longer interested, or after the patient did not show up for an appointment and did not call to cancel.
Results
Eighteen patients met the inclusion criteria (Table). Participants mean age was 62 years with most aged 50 to 70 years. Most participants were male (94%) and white (61%). Thirty-nine percent of the participants were African American. Twelve group appointments were held from November 2010 through April 2013. The mean enrollment per session was 5.8 patients (range 3-9). The median number of sessions each patient participated in was 3 (range 1 to 10).
SMA Outcomes
Among the 18 participants, the absolute change in HbA1c was -2.2% ± 2.0, representing a relative decrease in HbA1c of 18.2%. The study criterion for success was either a relative decrease of HbA1c by 13.5% or an absolute decrease in HbA1c of 1.5%. Of 18 patients participating in SMA, 14 (78%) patients achieved this goal. Of the 4 patients that were not successful, 2 patients had a relative HbA1c increase of 13% and 14%, respectively, 1 patient had no change at all, and 1 patient had a 9% relative decrease (Figure). Fourteen patients had improvement in their HbA1c after the first appointment, 2 patients had improvement after the second appointment, 1 patient had improvement after the fourth appointment, and 1 patient had no improvement.
In this population of rural veterans with poorly controlled diabetes, participation in SMAs was associated with marked improvement in measures of glucose control. Fourteen of the 18 (78%) veterans who participated in the DM SMA exhibited clinically significant decreases in HbA1c and achieved the defined goal.
Discussion
The effectiveness of DM SMAs has been documented in several previous studies. Sadur and colleagues found that a 6-month cluster visit group model of care for adults with DM improved glycemic control by 1.3% in the intervention subjects vs 0.2% in the control subjects in a randomized, controlled trial (RCT) with 185 participants.3 The intervention group received multidisciplinary outpatient diabetes management delivered by a diabetes nurse educator, a psychologist, a nutritionist, and a pharmacist in cluster visit settings of 10 to 18 patients per month for 6 months.
Metabolic Control
In another RCT trial of 112 patients, Trento and colleagues found that physician-led group consultations may improve metabolic control in the medium term by inducing more appropriate health behaviors.4 The consultations are feasible in everyday clinical practice without increasing working hours. After 2 years, HbA1c levels remained stable in patients seen in groups but had worsened in control subjects.
In a quasi-experiment with concurrent but nonrandomized controls, Kirsh and colleagues concluded that SMAs for DM constitute a practical system redesign that may help improve quality of care.5 Participants included 44 veterans from a VA primary care clinic who attended at least 1 physician-led SMA from April 2005 to September 2005 and from May 2006 to August 2006. Results showed levels of HbA1c, low-density lipoprotein cholesterol (LDL-C), and systolic BP (SBP) fell significantly postintervention with a mean decrease of HbA1c 1.4%, LDL-C 14.8 mg/dL, and SBP 16.0 mm Hg. The reductions in HbA1c and SBP were greater in the intervention group relative to the control group. The LDL-C reduction also was greater in the intervention group; however, the difference was not statistically significant.
Similarly, Sanchez concluded that patients who participated in a physician and nurse practitioner-led SMA using the diabetes self-management education (DSME) process had improvements in their HbA1c, self-management skills, and satisfaction.6 The study was considered a quality improvement project. Data were collected on 70 patients who were 96% Mexican American and received DSME via SMA during a 3-month span. The average HbA1c on visit 1 was 7.95%, 7.48% on visit 2, and 7.51% on visit 3. There were 34 patients with a decrease in HbA1c on visit 2 and 12 patients with a decrease in HbA1c on visit 3. Also, in a study on the effectiveness of SMAs in DM care, Guirguis and colleagues found that veterans showed an average decline in HbA1c whether they attended 1, 2, 3, or 4 SMAs.7 However, the decline was only statistically significant (P = .02) for those who had a baseline HbA1c > 9% prior to the study.
In contrast, other studies found no significant difference in improvement of DM patients in a SMA vs DM patients not in a SMA. Wagner and colleagues found periodic primary care sessions organized to meet the complex needs of diabetic patients improved the process of diabetes care and were associated with better outcomes.11 Primary care practices with a total of 700 patients were randomized within clinics to either a chronic care clinic (intervention) group or a usual care (control) group. Each chronic care clinic consisted of an assessment; individual visits with the primary care physician, nurse, and clinical pharmacist; and a group educational/peer support session. Although they found that the primary care group sessions improved the process of DM care and were associated with better outcomes, the mean HbA1c levels and cholesterol levels were comparable between the 2 groups.
In a 12-month RCT of 186 diabetic patients, Clancy and colleagues concluded physician and RN co-led group visits can improve the quality of care for diabetic patients, but modifications to the content and style of group visits may be necessary to achieve improved clinical outcomes.12 Results showed at both measurement points, HbA1c, BP, and lipid levels did not differ significantly for patients attending group visits vs those in usual care. Similarly, Edelman and colleaguesfound that provider-run group medical appointments are a potent strategy for improving BP but not HbA1c levels in DM patients in a RCT that compared a group medical appointment intervention with usual care among 239 primary care diabetic patients at the Durham VAMC in North Carolina and Hunter Holmes McGuire VAMC in Richmond, Virginia.10 Of note, the HbA1c levels in the group medical clinics did improve from 9.2% at baseline to a final of 8.3%, whereas the HbA1c level in the usual care group only improved from 9.2 to 8.6%.
Pharmacist-Led SMAs
In comparison to physician or nurse practitioner-led SMA, there also have been studies regarding pharmacist-led group medical appointments that have shown to be beneficial. Taveira and colleagues found that pharmacist-led group medical visits were feasible and efficacious for improving cardiac risk factors in patients with DM.8 This RCT with 118 VA patient participants showed a greater proportion of the intervention group vs the usual care alone group achieved a HbA1c of < 7%, and a SBP < 130 mm Hg.
In a separate study, Taveira and colleagues found that pharmacist-led group SMA visits are effective for glycemic control in patients with DM and depression without a change in depression symptoms.9 This RCT compared standard care and VA Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction in Depression vs standard care alone in 88 depressed patients with DM with HbA1c > 6.5%. Also, Cohen and colleagues concluded that pharmacist-led group intervention program was an effective and sustainable collaborative care approach to managing DM and reducing associated cardiovascular risks.10 This study was a RCT that compared standard primary care alone to a 6-month pharmacist-led SMA program added to standard primary care. A total of 99 VA patients were included in the final analysis.
Other studies have looked at patient experiences involving SMAs. In a separate study, Cohen and colleagues explored the experiences of veterans who participated in SMAs.14 Veterans reported improvement in their overall health and well-being, improved self-management skills, and satisfaction with the SMA format.
Benefits to Veteran Patients
The SMA revealed the need for improved glycemic control in the participating patients. All the rural veteran patients included in the SMA had uncontrolled DM, which placed them at risk for many other health problems, such as renal failure, lower-limb amputations, blindness, cardiac disease, and stroke. In addition patients were given individual attention from several health care disciplines. Patients received one-on-one care from the physician or ARNP, nurse, pharmacist, dietitian, and psychologist in the same appointment. This arrangement benefited the patients in regard to their health, well-being, time, and money.
Limitations
Limitations of this study included its small sample size (18 patients), age of the patients, and the gender of patients. Patients average age was about 62 years, and most were aged in their 50s to 70s. Only 1 patient was in her 30s. Patients were predominantly male (17 men, 1 woman).
A second limitation was managing other PCP’s patients. It would be beneficial to see the outcomes of this same study if it were led by the patient’s PCP to find out whether the outcomes would be different regarding participation, no-show rates, and decrease in HbA1c.
A third limitation was the absence of information on time and resource use. Clinical staff members took time to prepare and participate in the SMA, and follow-up afterward. However, comparing the SMA with a regular PCP appointment in which an uncontrolled diabetic patient may be referred to diabetic education classes led by nurse educators and/or dietitians, to an individual nutritionist, to an individual clinical pharmacist, and to a behavioral therapist, the SMA may be a time and resource saver.
Conclusion
The study shows the practicality of implementing an effective SMA using a group interdisciplinary team approach to care for rural veterans with DM. The DM SMA may assist in improving quality of care and improve diabetic patients’ blood glucose. The SMA also may benefit patients who are nonadherent by educating them more thoroughly and letting them express themselves or share life experiences with fellow veterans who have the same diagnoses. Future studies are needed to determine the efficacy of DM SMAs especially with patients’ own PCPs.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.
1. Kirsh S, Watts S, Schaub K, et al. VA shared medical appointments for patients with diabetes: maximizing patient & provider expertise to strengthen care management. U.S. Department of Veterans Affairs website. http://www.queri.research.va.gov/tools/diabetes/shared-med-appt.pdf. Published December 2008. Accessed May 10, 2016.
2. American Diabetes Association. Statistics about diabetes. American Diabetes Association website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Updated April 1, 2016. Accessed May 14, 2016.
3. Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011-2017.
4. Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24(6):995-1000.
5. Kirsh S, Watts S, Pascuzzi K, et al. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349-353.
6. Sanchez I. Implementation of a diabetes self-management education program in primary care for adults using shared medical appointments. Diabetes Educ. 2011;37(3):381-391.
7. Guirguis AB, Lugovich J, Jay J, et al. Improving diabetes control using shared medical appointments. Am J Med. 2013;126(12):1043-1044.
8. Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ. 2010;36(1):109-117.
9. Taveira TH, Dooley AG, Cohen LB, Khatana SA, Wu WC. Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Ann Pharmacother. 2011;45(11):1346-1355.
10. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801-812.
11. Wagner EH, Grothaus LC, Sandhu N, et al. Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care. 2001;24(4):695-700.
12. Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM. Group visits: promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620-624.
13. Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med. 2010;152(11):689-696.
14. Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11):1287-1292.
Clinical Video Telehealth for Gait and Balance
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
Supporting Caregivers of Veterans Online: A Partnership of the National Council on Aging and VA
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
Family caregivers fill a critical need in our nation’s health care system by providing essential services and support for chronically ill and disabled persons. Yet their physical, mental, and emotional well-being are often compromised due to their caregiving roles and responsibilities. Several nationally representative surveys of military caregivers have highlighted differences that are unique to caregivers of veterans.1,2 According to a RAND Corporation report, caregivers of veterans differ from other family caregivers in that they are younger with dependent children, often live with the person they are caring for, and provide care for up to a decade longer than do other caregivers.3 While most caregivers experience similar stressors, caregivers of veterans face distinct challenges, partly because veterans’ illnesses can be markedly different from the general population of disabled and/or chronically ill individuals.
Veterans and their caregivers also must navigate within large and complex health care, legal, and financial systems.3 Recently, the VA has begun to institute a number of programs and services to support veterans. One of these is the Building Better Caregivers (BBC) program. Building Better Caregivers is an online 6-week workshop aimed to equip caregivers of persons with physical and cognitive impairment with the knowledge, skills, and support to boost self-confidence in their ability to maintain and lead active and fulfilling lives. Developed at Stanford University and tested in partnership with the VA, BBC has shown significant improvements in caregivers’ health and health-related behaviors. Moreover, its online format allows for caregivers to access support and information when it is most convenient to them.4
The National Council on Aging (NCOA) has more than a decade of experience disseminating evidence-based solutions in partnership with a variety of organizations. Previously NCOA held an exclusive license to disseminate the BBC program (Canary Health now holds the license). Following a pilot study of the program, the VA partnered with NCOA to implement and sustain BBC. By integrating the program into clinical practice, NCOA and VA have positioned this program under the VA’s Caregiver Support Program (CSP). Caregiver support coordinators have referred > 5,000 caregivers to date, and > 2,654 of those caregivers expressed interest and were assigned to a workshop. Seventy percent of participants attended 4 out of 6 sessions, which is considered completing the workshop.
In the original pilot study with Stanford University, caregivers taking BBC showed significant improvements in depression, pain, stress, caregiver burden, and 63% completed at least 4 of the 6 sessions.4 Current BBC outcomes continue to show reductions in stress. In addition, participant completer rates are even greater than the original study outcomes with 75% of caregivers completing 4 out of 6 sessions. Additionally, > 50% of workshop graduates elect to participate in a BBC online community that continues to support them in their role as caregiver. Nearly half of all U.S. adults and 80% of adults aged > 55 years have more than 1 chronic condition and/or disability.3 Unlike acute care, the majority of care for chronically ill individuals is provided outside of the medical system and in homes by family caregivers. Family caregivers provide assistance with routine, daily activities, such as bathing and meal preparation, as well as more specialized tasks, such as meeting with health care providers and administering medications.
The amount of weekly care provided averages 21 hours per week for persons with physical impairment, and 22 to 47 hours per week for persons with cognitive impairment.5,6 According to the National Alliance of Caregivers, there are > 65 million individuals in the U.S. who provide care to a family member or friend who is chronically ill and/or disabled.1 As the U.S. population continues to age, so will the proportion of individuals with chronic conditions. That means a growing need for caregivers. And due to advancements in health care, more individuals are aging with disabilities, resulting in a prolonged need for caregivers.
Caregiver Challenges
Family caregivers represent a very diverse segment of the U.S. population, cutting across most demographic groups. While research indicates that living arrangements, hours of care provided, and money spent may vary by race/ethnicity, socioeconomic status, and gender, most caregivers provide similar types of care and experience similar stresses.7 However, many caregivers of veterans face a unique set of challenges and subsequently experience disproportionately poor mental and emotional health than do caregivers in the general population.3 These findings are also supported by nationally representative surveys of caregivers, one of family caregivers in general and other of caregivers of veterans.
In addition to providing assistance with daily activities and specialized tasks, caregivers of veterans usually have added roles and responsibilities that are markedly different from the general caregiver population due to the severity of veterans’ illnesses and disabilities. Many veterans experience mental illness, with > 70% of those who require caregivers having reported anxiety and/or depression, and 60% having been diagnosed with posttraumatic stress disorder (PTSD). In addition, almost half of all veterans have cognitive impairment, and nearly one-third experiencing traumatic brain injuries (TBI).8 These “invisible wounds” often require caregivers to spend a significant amount of time providing behavioral care (ie, avoiding certain triggers and providing cues), as well as emotional support, along with standard physical care.1 Behavioral care and emotional support are ongoing and more challenging than physical care, and thus more taxing on the caregiver.
Profile of Caregivers of Veterans
Caregivers of veterans also face the additional challenge of navigating large and complex systems across multiple government organizations. There are a myriad of services and benefits available to veterans, and their caregivers typically serve as care coordinators—facilitating care, services, and benefits for their loved ones. Caregivers of veterans may also handle all financial and legal matters, such as drafting wills and advance directives.3 Coordinating care and handling financial and legal matters can prove to be extremely difficult and time consuming.
It is, therefore, not surprising that caregivers of veterans experience higher levels of physical strain as well as poorer mental and emotional health. Six out of 10 caregivers of veterans report their health has declined due to their caregiving role, and the majority find themselves socially isolated and depressed (Figure 1).1,2,8
VA Support for Caregivers
The VA has long supported family caregivers of veterans through services such as home health care and programming, such as home-based primary care, teaching, and support. Following the passage of Public Law 111-163, the Caregivers and Veterans Omnibus Health Act of 2010, the VA has been able to increase its support to family caregivers to an unprecedented level. The programs and services established under this act include a national CSP and caregiver support line, as well as placement of caregiver support coordinators at each VA medical center. The VA has also developed a VA caregiver website (http://www.caregiver.va.gov), rolled out a national Peer Support Mentoring program and a number of self-care courses. Other additional supports for caregivers of veterans injured in the line of duty on or after September 11, 2001, include monthly stipends, mental health services, insurance coverage, and enhanced respite care. These caregiver programs and services utilize a variety of models to assist in the engagement of the diverse caregiver population across the military service eras.
Why Building Better Caregivers?
The VHA piloted a number of programs for caregivers prior to the implementation of the CSP. In 2009, VHA partnered with Stanford University to pilot the BBC self-management workshop for caregivers of veterans. The online pilot addressed the needs of those looking after their family members or friends with cognitive difficulties, such as dementia, TBI, PTSD, memory problems, and other care needs. The online format provided an additional option for caregivers to access support in a nontraditional format outside of their local VAMC. This format also allowed caregivers the flexibility to access support and information in the convenience of their home, based on their availability and schedule. This feature was especially important due to the challenges some caregivers experience, whether it is their rural residence, limited ability to travel to a medical center, or lack of support to leave their loved one to attend a support group.
How It Works
The BBC program, developed at Stanford University, is a 6-week workshop offered on a dedicated website. Each workshop is composed of 20 to 25 caregivers. The workshop is moderated by 2 trained facilitators—at least 1 of whom is a caregiver. Facilitators and participants together address a number of topics, including managing difficult care partner behaviors and emotions, reducing stress for the caregiver, self-care methods to improve the caregiver’s health, making decisions, finding additional help and resources, and planning for the future. Weekly activities include reading and applying new knowledge through a rich content learning center; making and posting a weekly action plan, brainstorming, problem solving, and celebrating milestones with fellow participants via 4 directed bulletin boards; and participating in any appropriate self-tests and activities.
There is no real-time attendance, so caregivers can choose the time of day and days of the week that are convenient to them to log in and participate.
VA/NCOA Partnership
An exclusive license to disseminate this program and other online programs developed and tested at Stanford is held by NCOA. In licensing the program, NCOA also offers technical assistance, training, and technologic support needed to implement and sustain the program. Following the success of the BBC pilot, VA worked with NCOA to implement the program under its CSP.
The NCOA has over a decade of experience in disseminating evidence-based programs and working with organizations at the federal, state, and local level to embed these programs into organizations so that they become standard practice and are sustainable. It also has several years of experience in disseminating programs online. The VA is a leading organization in caregiver support services and has built a national CSP that reaches tens of thousands of caregivers.
In addition to maximizing the resource potential of each organization, both organizations see the importance of clear and frequent communication in program dissemination. Each organization took the time to learn the other’s culture and have an appreciation for how each organization operates. The VA and NCOA meet weekly and work together on every aspect of the project.
Implementation
A rigorous implementation time line was developed by NCOA and VA and achieved the goal of launching the program within 90 days of the kick-off meeting. Key indicators for the success of this program are detailed in the Table.
Both NCOA and VA saw the importance of creating a program that fits well within the overarching CSP and complements its services and resources (Figure 3).
Training and Support
Adequate training and support are essential to maintaining the integrity of this program. A total of 30 facilitators and 5 mentors to support workshops were trained by NCOA, and NCOA screened all facilitator candidates and provided training with ongoing support to all certified and accredited facilitators.
In addition, an online community offers continued support for workshop participants once they have completed the workshop. Graduates can access tools and resources, as well as problem solve, brainstorm, celebrate, and set goals along with other peer graduates via moderated discussion boards.
Preliminary Findings
More than 50% of workshop participants were aged 31 to 50 years, 85% lived with the veteran they were caring for, and 78% were spouses of the care recipient. Seventy-two percent of the veterans being cared for were white, and 93% were male. Nearly 80% of the veterans had PTSD, and more than half had TBI and/or a mental health disorder.
Clinical Indicators
Caregivers in the general population and those caring for veterans consider their caregiving situation stressful. In this implementation, participants are showing a statistically significant reduction in stress when measured at week 1 and week 6 with an average change score of 1.3 on a 10-point scale. Similar reductions in stress were seen in the original Stanford University study 3 months after the workshop had ended.2
Satisfaction
Participant satisfaction was high, averaging 4.5 on a 5-point Likert scale. Caregiver participants reported that what they liked best about the workshop was the shared experience with other caregivers, timing/convenience, giving and receiving help, and goal setting.
One recent caregiver who was caring for her husband remarked “I really enjoyed the workshop. Interacting with others, heartfelt stories of celebration, and frustration. The concern for the whole woman/man; physically and emotionally. I enjoyed the helpful suggestions/encouraging words of the leaders as well. I hope more people take advantage of this program.”
“I like the informal nature and self-paced aspect. We all have crazy lives but I think this was easy to do,” said another caregiver.
“This was a place where you can put out your problem and no one will judge you,” a caregiver explained. “There was respect for each other’s situations. Learning from others’ problem and how others share the solution. I saw how important the caregivers are, taking care of our self first so we can take care of the rest.”
Recruitment
In the 36 months since implementation, > 5,000 referrals were made for BBC, resulting in 2,654 caregivers being assigned to workshops; 75% of caregivers completed a workshop. Nearly half of all workshop graduates elected to join a moderated online community.
Discussion
Internal BBC recruitment data are captured monthly and reported to the Caregiver Support Program for each of the local VAMCs. Although recruitment goals are being met, a consistent referral pattern is not occurring at local VA sites. Not all VA sites are referring participants, and the referrals to BBC at some VA sites have been low in comparison with other higher performing VA sites. The percentage of sites with no referrals is 2%; lower performing sites with less than 20 caregivers referred represent 50% of sites.
A variety of factors contribute to disparities in referrals at different sites. A primary challenge is the increased demands on caregiver support coordinators nationally as they continue to prioritize the enrollment of caregivers into a variety of other programs available within CSP. The CSP office has developed other caregiver resources and tools that may compete with referral to BBC due to the preference of the staff and caregivers. Additional factors may also include no prescribed referral metrics for local sites and variances in local marketing and promotion of BBC. As the partnership between NCOA and the VA continues, additional caregiver referral methods are being explored to facilitate local promotion and marketing to engage caregivers of all eras.
Lessons and Next Steps
This partnership and program implementation have yielded a number of lessons learned and indications for next steps. The most significant lesson also proved to be the biggest success: the program can be embedded into clinical practice. Integrating the referral process into VA staff’s daily operations and depending on them to bring forward viable participants proved highly successful, with the majority of caregiver support coordinators making ≥ 1 referral and 50% of referred caregivers electing to take the workshop.
The VA and NCOA subsequently learned through focus groups that the relationship between the CSC and caregiver is strong, but there is also a need for continual follow-up and—more often than not—these referred caregivers need reminder e-mails to complete the sign-up process. The NCOA and VA also saw a larger proportion of post 9/11 caregivers (70%) recruited to the program compared with other eras (30%). Future recruitment will focus on ways to get caregivers of older era veterans involved with BBC.
Last, the VA and NCOA learned that participants really enjoyed the program. In the future more participant testimonials and stories will be used to spread the word to other caregivers about the program.
Conclusion
Caregivers of veterans face a unique set of challenges. Throughout both the VA pilot and the current partnership with NCOA, BBC is a promising solution for improving the well-being of caregivers of veterans. The success of its integration into clinical practice and participant satisfaction speak to both the quality of the program, as well as the partnership between NCOA and VA. Both NCOA and VA are working to expand its reach and make BBC readily available to as many caregivers of veterans as possible.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.
1. National Alliance for Caregiving, AARP. Caregiving in the U.S. National Alliance for Caregiving Website. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Published November 2009. Accessed December 17, 2015.
2. National Alliance for Caregiving, United Health Foundation, Caregivers of Veterans: Serving on the home front. National Alliance for Caregiving Website. http://www.caregiving.org/data/2010_Caregivers_of_Veterans_FULLREPORT_WEB_FINAL.pdf. Published November 2010. Accessed December 17, 2015.
3. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. Santa Monica, CA: RAND Corporation; 2013.
4. Lorig K, Thompson-Gallagher D, Traylor L, et al. Building Better Caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J Appl Gerontol. 2012;31(3):423-437.
5. Hendrie HC, Albert MS, Butters MA, et al. The NIH Cognitive and Emotional Health Project. Report of the Critical Evaluation Study Committee.” Alzheimer’s Dement. 2006;2(1):12-32.
6. MetLife Mature Market Institute, LifePlans. The MetLife study of alzheimer’s disease: the caregiving experience. MetLife Website. https://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf. Published August 2006. Accessed December 17, 2015.
7. Pandya S. Racial and ethnic differences among older adults in long-term care service use. http://www.aarp.org/home-garden/livable-communities/info-2005/fs119_ltc.html. Published June 2005. Accessed December 17, 2015.
8. Resnik LJ, Allen SM. Using international classification of functioning, disability and health to understand challenges in community reintegration of injured veterans. J Rehab Res Dev. 2007;44(7):991-1006.