User login
A Practice Resolution
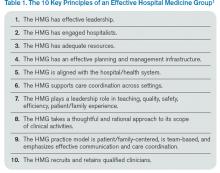
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
Cut Costs, Improve Quality and Patient Experience
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
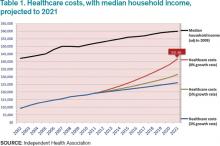
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
Early Warning System Boosts Sepsis Detection, Care
A recent study published in the Journal of Hospital Medicine reports on an early warning and response system (EWRS) for sepsis used in all three hospitals within the Philadelphia-based University of Pennsylvania Health System (UPHS) for three-month spans in 2012 and 2013. The system integrates laboratory values and vital signs into patients EHRs and establishes a threshold for triggering the alert.
After implementing the EWRS, at-risk patients received faster care for sepsis and/or were transferred to the ICU more quickly, says lead author Craig A. Umscheid, MD, MSCE, director of the Center for Evidence-Based Practice at the University of Pennsylvania in Philadelphia. Study authors also note that quicker care suggested reduced mortality from sepsis as well.
"Whenever a patient triggered the alert, their probability of mortality was much higher than patients who didn't trigger the alert," Dr. Umscheid says. "I think what makes our study unique compared to other studies that have tried to predict sepsis is that beyond just creating a prediction rule for sepsis, we actually implemented it into a clinical care setting, alerted providers in real time, and then those providers changed their care based on the prediction."
More than 90% of care teams arrived at the bedside when they received an alert. "Meaning that they saw some value in the alert, and the infrastructure that we put in place was able to mobilize the team and get them to the bedside within 30 minutes," Dr. Umscheid adds. "We saw an increase in sepsis antibiotics used, and we saw an increase in fluid boluses within six hours.”
As many as 3 million cases of severe sepsis occur in the U.S. annually, and 750,000 result in deaths, according to the study. The high number of cases has led to several efforts to create better clinical practices for sepsis patients.
"Sepsis is arguably one of the most, if not the most important, causes of preventable mortality in the inpatient setting," Dr. Umscheid says. "One thing that we thought we could do better was identify sepsis cases earlier so that we could provide early antibiotics and fluids."
Visit our website for more information on identifying and treating sepsis.
A recent study published in the Journal of Hospital Medicine reports on an early warning and response system (EWRS) for sepsis used in all three hospitals within the Philadelphia-based University of Pennsylvania Health System (UPHS) for three-month spans in 2012 and 2013. The system integrates laboratory values and vital signs into patients EHRs and establishes a threshold for triggering the alert.
After implementing the EWRS, at-risk patients received faster care for sepsis and/or were transferred to the ICU more quickly, says lead author Craig A. Umscheid, MD, MSCE, director of the Center for Evidence-Based Practice at the University of Pennsylvania in Philadelphia. Study authors also note that quicker care suggested reduced mortality from sepsis as well.
"Whenever a patient triggered the alert, their probability of mortality was much higher than patients who didn't trigger the alert," Dr. Umscheid says. "I think what makes our study unique compared to other studies that have tried to predict sepsis is that beyond just creating a prediction rule for sepsis, we actually implemented it into a clinical care setting, alerted providers in real time, and then those providers changed their care based on the prediction."
More than 90% of care teams arrived at the bedside when they received an alert. "Meaning that they saw some value in the alert, and the infrastructure that we put in place was able to mobilize the team and get them to the bedside within 30 minutes," Dr. Umscheid adds. "We saw an increase in sepsis antibiotics used, and we saw an increase in fluid boluses within six hours.”
As many as 3 million cases of severe sepsis occur in the U.S. annually, and 750,000 result in deaths, according to the study. The high number of cases has led to several efforts to create better clinical practices for sepsis patients.
"Sepsis is arguably one of the most, if not the most important, causes of preventable mortality in the inpatient setting," Dr. Umscheid says. "One thing that we thought we could do better was identify sepsis cases earlier so that we could provide early antibiotics and fluids."
Visit our website for more information on identifying and treating sepsis.
A recent study published in the Journal of Hospital Medicine reports on an early warning and response system (EWRS) for sepsis used in all three hospitals within the Philadelphia-based University of Pennsylvania Health System (UPHS) for three-month spans in 2012 and 2013. The system integrates laboratory values and vital signs into patients EHRs and establishes a threshold for triggering the alert.
After implementing the EWRS, at-risk patients received faster care for sepsis and/or were transferred to the ICU more quickly, says lead author Craig A. Umscheid, MD, MSCE, director of the Center for Evidence-Based Practice at the University of Pennsylvania in Philadelphia. Study authors also note that quicker care suggested reduced mortality from sepsis as well.
"Whenever a patient triggered the alert, their probability of mortality was much higher than patients who didn't trigger the alert," Dr. Umscheid says. "I think what makes our study unique compared to other studies that have tried to predict sepsis is that beyond just creating a prediction rule for sepsis, we actually implemented it into a clinical care setting, alerted providers in real time, and then those providers changed their care based on the prediction."
More than 90% of care teams arrived at the bedside when they received an alert. "Meaning that they saw some value in the alert, and the infrastructure that we put in place was able to mobilize the team and get them to the bedside within 30 minutes," Dr. Umscheid adds. "We saw an increase in sepsis antibiotics used, and we saw an increase in fluid boluses within six hours.”
As many as 3 million cases of severe sepsis occur in the U.S. annually, and 750,000 result in deaths, according to the study. The high number of cases has led to several efforts to create better clinical practices for sepsis patients.
"Sepsis is arguably one of the most, if not the most important, causes of preventable mortality in the inpatient setting," Dr. Umscheid says. "One thing that we thought we could do better was identify sepsis cases earlier so that we could provide early antibiotics and fluids."
Visit our website for more information on identifying and treating sepsis.
LISTEN NOW: Dr. Kendall Rogers, MD, SFHM, Encourages Hospitalists to Work as Part of Quality Teams to Achieve Glycemic Control
As SHM's glycemic control lead mentor and a hospitalist at the University of New Mexico in Albuquerque, Kendall Rogers, MD, CPE, FACP, SFHM, offers advice to hospitalists when working as part of a quality team in achieving glycemic control.
As SHM's glycemic control lead mentor and a hospitalist at the University of New Mexico in Albuquerque, Kendall Rogers, MD, CPE, FACP, SFHM, offers advice to hospitalists when working as part of a quality team in achieving glycemic control.
As SHM's glycemic control lead mentor and a hospitalist at the University of New Mexico in Albuquerque, Kendall Rogers, MD, CPE, FACP, SFHM, offers advice to hospitalists when working as part of a quality team in achieving glycemic control.
LISTEN NOW: Kristen Kulasa, MD, Explains How Hospitalists Can Work with Nutritionists and Dieticians
Kristen Kulasa, MD, assistant clinical professor of medicine and director of Inpatient Glycemic Control, Division of Endocrinology, Diabetes, and Metabolism at the University of California in San Diego, provides tips on how hospitalists can work with nutritionists and dieticians for the betterment of diabetic patients. As a mentor for SHM's care coordination program on inpatient diabetes, Dr. Kulasa offers hospitalists advice in treating diabetic patients. She points to SHM’s website, which has a lot of resources to help hospitalists feel comfortable with insulin dosing.
Kristen Kulasa, MD, assistant clinical professor of medicine and director of Inpatient Glycemic Control, Division of Endocrinology, Diabetes, and Metabolism at the University of California in San Diego, provides tips on how hospitalists can work with nutritionists and dieticians for the betterment of diabetic patients. As a mentor for SHM's care coordination program on inpatient diabetes, Dr. Kulasa offers hospitalists advice in treating diabetic patients. She points to SHM’s website, which has a lot of resources to help hospitalists feel comfortable with insulin dosing.
Kristen Kulasa, MD, assistant clinical professor of medicine and director of Inpatient Glycemic Control, Division of Endocrinology, Diabetes, and Metabolism at the University of California in San Diego, provides tips on how hospitalists can work with nutritionists and dieticians for the betterment of diabetic patients. As a mentor for SHM's care coordination program on inpatient diabetes, Dr. Kulasa offers hospitalists advice in treating diabetic patients. She points to SHM’s website, which has a lot of resources to help hospitalists feel comfortable with insulin dosing.
Insulin Rules in the Hospital
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Room for Improvement in Identifying, Treating Sepsis
Despite huge strides in the treatment of heart failure, pneumonia and myocardial infarction, hospitals have a long way to go in improving care for patients with sepsis, say the authors of a recent commentary published online in JAMA.
In a related study published in July in JAMA, sepsis was found to contribute to one in every two to three hospital deaths based on mortality results from two independent patient cohorts measured between 2010 and 2012. Additionally, most instances of sepsis were present upon admission, the report notes.
For their part, hospitalists should focus on identifying the signs and symptoms of sepsis early, according to study authors Colin R. Cooke, MD, MSc, MS, and Theodore J. Iwashyna, MD, PhD, of the division of pulmonary and critical care medicine at the University of Michigan in Ann Arbor.
"When patients are admitted for an illness such as pneumonia, we put them in a bin where we know how to treat patients with pneumonia, but we may fail to recognize when they meet the criteria for sepsis," Dr. Cooke says. "If we can recognize a patient has sepsis, then we can get on top of the illness faster by delivering antibiotics and also ensuring the patient gets fluid resuscitation early in the course of the disease."
In their JAMA article, Dr. Cooke and Dr. Iwashyna call on the Centers for Medicare & Medicaid Services to develop quality mandates that would encourage hospitals to share best practices in treating sepsis. The mandates, however, shouldn't include financial penalties, which the authors say "would create perverse incentives to not report delayed diagnosis of sepsis rather than address the problem."
Visit our website for more information on identifying sepsis in hospitalized patients.
Despite huge strides in the treatment of heart failure, pneumonia and myocardial infarction, hospitals have a long way to go in improving care for patients with sepsis, say the authors of a recent commentary published online in JAMA.
In a related study published in July in JAMA, sepsis was found to contribute to one in every two to three hospital deaths based on mortality results from two independent patient cohorts measured between 2010 and 2012. Additionally, most instances of sepsis were present upon admission, the report notes.
For their part, hospitalists should focus on identifying the signs and symptoms of sepsis early, according to study authors Colin R. Cooke, MD, MSc, MS, and Theodore J. Iwashyna, MD, PhD, of the division of pulmonary and critical care medicine at the University of Michigan in Ann Arbor.
"When patients are admitted for an illness such as pneumonia, we put them in a bin where we know how to treat patients with pneumonia, but we may fail to recognize when they meet the criteria for sepsis," Dr. Cooke says. "If we can recognize a patient has sepsis, then we can get on top of the illness faster by delivering antibiotics and also ensuring the patient gets fluid resuscitation early in the course of the disease."
In their JAMA article, Dr. Cooke and Dr. Iwashyna call on the Centers for Medicare & Medicaid Services to develop quality mandates that would encourage hospitals to share best practices in treating sepsis. The mandates, however, shouldn't include financial penalties, which the authors say "would create perverse incentives to not report delayed diagnosis of sepsis rather than address the problem."
Visit our website for more information on identifying sepsis in hospitalized patients.
Despite huge strides in the treatment of heart failure, pneumonia and myocardial infarction, hospitals have a long way to go in improving care for patients with sepsis, say the authors of a recent commentary published online in JAMA.
In a related study published in July in JAMA, sepsis was found to contribute to one in every two to three hospital deaths based on mortality results from two independent patient cohorts measured between 2010 and 2012. Additionally, most instances of sepsis were present upon admission, the report notes.
For their part, hospitalists should focus on identifying the signs and symptoms of sepsis early, according to study authors Colin R. Cooke, MD, MSc, MS, and Theodore J. Iwashyna, MD, PhD, of the division of pulmonary and critical care medicine at the University of Michigan in Ann Arbor.
"When patients are admitted for an illness such as pneumonia, we put them in a bin where we know how to treat patients with pneumonia, but we may fail to recognize when they meet the criteria for sepsis," Dr. Cooke says. "If we can recognize a patient has sepsis, then we can get on top of the illness faster by delivering antibiotics and also ensuring the patient gets fluid resuscitation early in the course of the disease."
In their JAMA article, Dr. Cooke and Dr. Iwashyna call on the Centers for Medicare & Medicaid Services to develop quality mandates that would encourage hospitals to share best practices in treating sepsis. The mandates, however, shouldn't include financial penalties, which the authors say "would create perverse incentives to not report delayed diagnosis of sepsis rather than address the problem."
Visit our website for more information on identifying sepsis in hospitalized patients.
Primary-Care Physicians Weigh in on Quality of Care Transitions
A new study on transitions of care gives hospitalists a view from the other side.
Published recently online in the Journal of Hospital Medicine, the authors surveyed 22 primary-care physician leaders in California-based post-discharge clinics and asked them about ways to improve care transitions.
Physicians' responses focused on several areas that need work, most notably aligned financial incentives, regulations to standardize interoperability among electronic health records (EHR) and data sharing, and more opportunities for professional networking, the authors note.
Although the qualitative study takes a broad view of the healthcare system, its lead author says hospitalists should view "systems change" as a long-term goal achievable via incremental improvements that can start now.
"National policy change is needed to move the needle for the whole health system," says hospitalist Oanh Kieu Nguyen, MD, MAS, of the University of Texas Southwestern Medical Center in Dallas. "But locally, you can innovate within these domains and start to make changes to improve practice settings more immediately. National policy to align financial incentives and improve EHR interoperability will be key to helping local changes take hold and spread across systems. Otherwise, there will continue to be a lot of variability and fragmentation around care transitions on a national level."
Dr. Nguyen, who has practiced as both a hospitalist and PCP, says that because policies and studies on post-discharge care transitions primarily have focused on the hospital perspective, it is important to gain an understanding of the primary-care point of view.
"As a hospitalist, it's really easy to get caught up in just wanting to get patients teed up and sent home. Once they're out, we think they're no longer really our problem," Dr. Nguyen adds. "It's easy to forget that primary care is an important part of the other side of the equation. The way our healthcare system is designed doesn't really give physicians an incentive to look at the whole picture of a patient across all the environments they're in."
Many hospitalists are sharing their challenges and successes in care transitions through HMX. Join the conversation now.
Visit our website for more information on transitions of care.
A new study on transitions of care gives hospitalists a view from the other side.
Published recently online in the Journal of Hospital Medicine, the authors surveyed 22 primary-care physician leaders in California-based post-discharge clinics and asked them about ways to improve care transitions.
Physicians' responses focused on several areas that need work, most notably aligned financial incentives, regulations to standardize interoperability among electronic health records (EHR) and data sharing, and more opportunities for professional networking, the authors note.
Although the qualitative study takes a broad view of the healthcare system, its lead author says hospitalists should view "systems change" as a long-term goal achievable via incremental improvements that can start now.
"National policy change is needed to move the needle for the whole health system," says hospitalist Oanh Kieu Nguyen, MD, MAS, of the University of Texas Southwestern Medical Center in Dallas. "But locally, you can innovate within these domains and start to make changes to improve practice settings more immediately. National policy to align financial incentives and improve EHR interoperability will be key to helping local changes take hold and spread across systems. Otherwise, there will continue to be a lot of variability and fragmentation around care transitions on a national level."
Dr. Nguyen, who has practiced as both a hospitalist and PCP, says that because policies and studies on post-discharge care transitions primarily have focused on the hospital perspective, it is important to gain an understanding of the primary-care point of view.
"As a hospitalist, it's really easy to get caught up in just wanting to get patients teed up and sent home. Once they're out, we think they're no longer really our problem," Dr. Nguyen adds. "It's easy to forget that primary care is an important part of the other side of the equation. The way our healthcare system is designed doesn't really give physicians an incentive to look at the whole picture of a patient across all the environments they're in."
Many hospitalists are sharing their challenges and successes in care transitions through HMX. Join the conversation now.
Visit our website for more information on transitions of care.
A new study on transitions of care gives hospitalists a view from the other side.
Published recently online in the Journal of Hospital Medicine, the authors surveyed 22 primary-care physician leaders in California-based post-discharge clinics and asked them about ways to improve care transitions.
Physicians' responses focused on several areas that need work, most notably aligned financial incentives, regulations to standardize interoperability among electronic health records (EHR) and data sharing, and more opportunities for professional networking, the authors note.
Although the qualitative study takes a broad view of the healthcare system, its lead author says hospitalists should view "systems change" as a long-term goal achievable via incremental improvements that can start now.
"National policy change is needed to move the needle for the whole health system," says hospitalist Oanh Kieu Nguyen, MD, MAS, of the University of Texas Southwestern Medical Center in Dallas. "But locally, you can innovate within these domains and start to make changes to improve practice settings more immediately. National policy to align financial incentives and improve EHR interoperability will be key to helping local changes take hold and spread across systems. Otherwise, there will continue to be a lot of variability and fragmentation around care transitions on a national level."
Dr. Nguyen, who has practiced as both a hospitalist and PCP, says that because policies and studies on post-discharge care transitions primarily have focused on the hospital perspective, it is important to gain an understanding of the primary-care point of view.
"As a hospitalist, it's really easy to get caught up in just wanting to get patients teed up and sent home. Once they're out, we think they're no longer really our problem," Dr. Nguyen adds. "It's easy to forget that primary care is an important part of the other side of the equation. The way our healthcare system is designed doesn't really give physicians an incentive to look at the whole picture of a patient across all the environments they're in."
Many hospitalists are sharing their challenges and successes in care transitions through HMX. Join the conversation now.
Visit our website for more information on transitions of care.
Medication Reconciliation Toolkit Updated, Available to Hospitalists
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Post-Acute Care Transitions Toolkit Available to Hospitalists
Hospitalists know that many hospitalizations aren’t like those on TV. Instead of being discharged to their homes, many patients are discharged to post-acute care facilities for further care. And those transitions from hospital to post-acute care can be just as challenging as—if not more than—discharges to home care.
Making those transitions safer, smoother, and more effective can not only help an individual patient, but it can have a broader impact, according to the lead author of SHM’s new Post-Acute Care Transitions Toolkit, now available at www.hospitalmedicine.org/pact.
“Post-acute care transitions is an important area where hospitalists can contribute to improving the population health of their community,” says hospitalist Robert Young, MD, of Northwestern University in Chicago.
Both Dr. Young and the new toolkit recommend that hospitalists partner with the post-acute providers to make sure that communication between settings is complete during transitioning and open for ongoing questions as they arise. “Developing a relationship with your post-acute providers to work on these transitions issues provides the opportunity for ongoing quality and process improvement vital to our patients’ care,” Dr. Young says.
Hospitalists know that many hospitalizations aren’t like those on TV. Instead of being discharged to their homes, many patients are discharged to post-acute care facilities for further care. And those transitions from hospital to post-acute care can be just as challenging as—if not more than—discharges to home care.
Making those transitions safer, smoother, and more effective can not only help an individual patient, but it can have a broader impact, according to the lead author of SHM’s new Post-Acute Care Transitions Toolkit, now available at www.hospitalmedicine.org/pact.
“Post-acute care transitions is an important area where hospitalists can contribute to improving the population health of their community,” says hospitalist Robert Young, MD, of Northwestern University in Chicago.
Both Dr. Young and the new toolkit recommend that hospitalists partner with the post-acute providers to make sure that communication between settings is complete during transitioning and open for ongoing questions as they arise. “Developing a relationship with your post-acute providers to work on these transitions issues provides the opportunity for ongoing quality and process improvement vital to our patients’ care,” Dr. Young says.
Hospitalists know that many hospitalizations aren’t like those on TV. Instead of being discharged to their homes, many patients are discharged to post-acute care facilities for further care. And those transitions from hospital to post-acute care can be just as challenging as—if not more than—discharges to home care.
Making those transitions safer, smoother, and more effective can not only help an individual patient, but it can have a broader impact, according to the lead author of SHM’s new Post-Acute Care Transitions Toolkit, now available at www.hospitalmedicine.org/pact.
“Post-acute care transitions is an important area where hospitalists can contribute to improving the population health of their community,” says hospitalist Robert Young, MD, of Northwestern University in Chicago.
Both Dr. Young and the new toolkit recommend that hospitalists partner with the post-acute providers to make sure that communication between settings is complete during transitioning and open for ongoing questions as they arise. “Developing a relationship with your post-acute providers to work on these transitions issues provides the opportunity for ongoing quality and process improvement vital to our patients’ care,” Dr. Young says.