User login
We’re all vaccinated: Can we go back to the office (unmasked) now?
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
The Physician Support Line: One psychiatrist strives to make a difference
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
The brother’s keeper: A psychiatrist writes about his career treating physicians and their families
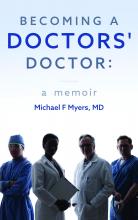
I started reading “Becoming a Doctors’ Doctor: A Memoir” by Michael F. Myers, MD, with high expectations and enthusiasm. Dr. Myers is a Canadian psychiatrist who has devoted his career to caring for physicians in his half-time private practice; he turns all other comers away.
This career path began in 1962 during his first year in medical school when Dr. Myers returned to his apartment after Thanksgiving break to be greeted with tragic news: One of the young men he shared the apartment with had died of suicide. The tragedy marked him – along with the silence about what had transpired – and he would later look back to realize it was the beginning of his journey to becoming a psychiatrist, one who cares for other physicians.
The book is filled with patient vignettes, gentle musings that Dr. Myers recounts with warmth, adding what he has learned from them.
There is, for example, the heart-wrenching account of “DJ,” a lonely medical student who is emergently hospitalized for depression, after the worried author anxiously drove the patient from his office to the hospital. DJ is all alone, and he writes to a friend and offers to pay for her transportation if she will come visit him in the hospital, a fact Dr. Myers knows only because he was later shown a letter DJ had written to his friend.
“He has been diminished and altered by his disease and the requisite hospital treatment, factors that we as mental health caregivers must never forget – or minimize. Visits from friends become visits of the representatives from the outside world, the link to normality, sanity, and anticipated return. These encounters are precious,” Dr. Myers writes.
As the book progressed, I began to wonder more about the author as a person. It is a memoir, so stated on the cover, but very little about his life is revealed. There are résumé-style facts: where he studied, or worked, or went to conferences, what he learned and what he spoke about, but I wanted to know more about how his experiences intertwined with his life. In the foreword, he talks about having an alcoholic mother. He tells the reader that being a husband and father was important to him, and that his conversion to Judaism – his wife’s religion – was meaningful, but there is no backstory, and I was looking for more. A quick reference is made to visiting a therapist, but those few sentences are the total of what I knew about Michael Myers midway through his memoir.
I looked for a photo of the author. I found it at the back of the book with a brief biography beneath it, ending with the fact that he lives with his husband. I had gotten halfway through the memoir, including chapters about how Myers had treated gay physicians, gay couples, and physicians with AIDS, and yet there was no mention of his husband, and how his sexual orientation influenced these encounters. I didn’t quite know what to think.
And then, in a section called “Getting Personal,” suddenly the tone of the book changed. Dr. Myers talked about his own sexual confusion as a young man and about the decision to marry a woman, knowing he was bisexual. He wrote about the shame he felt concerning his sexual desires at a time when homosexuality was still classified as a psychiatric disorder, the fear of judgment, and the sense that this – his ninth book – was his first genuine book.
“And so, I come full circle. It is my otherness that fundamentally – but not with full awareness – attracted me to psychiatry, and ultimately to becoming a doctors’ doctor. I’ve been able to empathize with my doctor patients’ burden with the scourge of mental illness, coping with brokenness, and struggling for acceptance and belonging in a profession of perfection and stature. And I understand what it’s like to feel a bit of a misfit, less than, unclean and tattered. But as a wounded healer, I know the restorative value of listening, acceptance, caring, doggedness, and hope.” And so I found Dr. Myers.
These few pages in the middle of the book pulled everything else into focus. The writing opened and the rest of the book flowed. The author’s insights about physician-patients became even more insightful. It’s almost as though he was anxious about revealing himself, and his writing infused itself with this worry, so that once his secret was revealed, he was free to be genuine in a way that makes this book a gem of a read.
His insights about treating troubled physicians are invaluable. He talks of their struggles with loss, and of their flawed roles as patients.
“At the point that they become a patient these individuals may already be quite ill, and this needs to be recognized and accepted by the treating psychiatrist. Judging the doctor for so many self-defeating behaviors is unacceptable and unprofessional. I have found it best to simply accept the old adage ‘It is what it is.’ And I try my best to be patient and understanding with such difficult and interwoven issues, in that for physicians becoming a patient is a process not an event.”
Written with empathy, warmth, and vulnerability, “Becoming a Doctors’ Doctor” is a worthwhile read for any psychiatrist who treats other physicians.
Dr. Miller is coauthor of “Committed: The Battle over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no conflicts of interest.
I started reading “Becoming a Doctors’ Doctor: A Memoir” by Michael F. Myers, MD, with high expectations and enthusiasm. Dr. Myers is a Canadian psychiatrist who has devoted his career to caring for physicians in his half-time private practice; he turns all other comers away.
This career path began in 1962 during his first year in medical school when Dr. Myers returned to his apartment after Thanksgiving break to be greeted with tragic news: One of the young men he shared the apartment with had died of suicide. The tragedy marked him – along with the silence about what had transpired – and he would later look back to realize it was the beginning of his journey to becoming a psychiatrist, one who cares for other physicians.
The book is filled with patient vignettes, gentle musings that Dr. Myers recounts with warmth, adding what he has learned from them.
There is, for example, the heart-wrenching account of “DJ,” a lonely medical student who is emergently hospitalized for depression, after the worried author anxiously drove the patient from his office to the hospital. DJ is all alone, and he writes to a friend and offers to pay for her transportation if she will come visit him in the hospital, a fact Dr. Myers knows only because he was later shown a letter DJ had written to his friend.
“He has been diminished and altered by his disease and the requisite hospital treatment, factors that we as mental health caregivers must never forget – or minimize. Visits from friends become visits of the representatives from the outside world, the link to normality, sanity, and anticipated return. These encounters are precious,” Dr. Myers writes.
As the book progressed, I began to wonder more about the author as a person. It is a memoir, so stated on the cover, but very little about his life is revealed. There are résumé-style facts: where he studied, or worked, or went to conferences, what he learned and what he spoke about, but I wanted to know more about how his experiences intertwined with his life. In the foreword, he talks about having an alcoholic mother. He tells the reader that being a husband and father was important to him, and that his conversion to Judaism – his wife’s religion – was meaningful, but there is no backstory, and I was looking for more. A quick reference is made to visiting a therapist, but those few sentences are the total of what I knew about Michael Myers midway through his memoir.
I looked for a photo of the author. I found it at the back of the book with a brief biography beneath it, ending with the fact that he lives with his husband. I had gotten halfway through the memoir, including chapters about how Myers had treated gay physicians, gay couples, and physicians with AIDS, and yet there was no mention of his husband, and how his sexual orientation influenced these encounters. I didn’t quite know what to think.
And then, in a section called “Getting Personal,” suddenly the tone of the book changed. Dr. Myers talked about his own sexual confusion as a young man and about the decision to marry a woman, knowing he was bisexual. He wrote about the shame he felt concerning his sexual desires at a time when homosexuality was still classified as a psychiatric disorder, the fear of judgment, and the sense that this – his ninth book – was his first genuine book.
“And so, I come full circle. It is my otherness that fundamentally – but not with full awareness – attracted me to psychiatry, and ultimately to becoming a doctors’ doctor. I’ve been able to empathize with my doctor patients’ burden with the scourge of mental illness, coping with brokenness, and struggling for acceptance and belonging in a profession of perfection and stature. And I understand what it’s like to feel a bit of a misfit, less than, unclean and tattered. But as a wounded healer, I know the restorative value of listening, acceptance, caring, doggedness, and hope.” And so I found Dr. Myers.
These few pages in the middle of the book pulled everything else into focus. The writing opened and the rest of the book flowed. The author’s insights about physician-patients became even more insightful. It’s almost as though he was anxious about revealing himself, and his writing infused itself with this worry, so that once his secret was revealed, he was free to be genuine in a way that makes this book a gem of a read.
His insights about treating troubled physicians are invaluable. He talks of their struggles with loss, and of their flawed roles as patients.
“At the point that they become a patient these individuals may already be quite ill, and this needs to be recognized and accepted by the treating psychiatrist. Judging the doctor for so many self-defeating behaviors is unacceptable and unprofessional. I have found it best to simply accept the old adage ‘It is what it is.’ And I try my best to be patient and understanding with such difficult and interwoven issues, in that for physicians becoming a patient is a process not an event.”
Written with empathy, warmth, and vulnerability, “Becoming a Doctors’ Doctor” is a worthwhile read for any psychiatrist who treats other physicians.
Dr. Miller is coauthor of “Committed: The Battle over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no conflicts of interest.
I started reading “Becoming a Doctors’ Doctor: A Memoir” by Michael F. Myers, MD, with high expectations and enthusiasm. Dr. Myers is a Canadian psychiatrist who has devoted his career to caring for physicians in his half-time private practice; he turns all other comers away.
This career path began in 1962 during his first year in medical school when Dr. Myers returned to his apartment after Thanksgiving break to be greeted with tragic news: One of the young men he shared the apartment with had died of suicide. The tragedy marked him – along with the silence about what had transpired – and he would later look back to realize it was the beginning of his journey to becoming a psychiatrist, one who cares for other physicians.
The book is filled with patient vignettes, gentle musings that Dr. Myers recounts with warmth, adding what he has learned from them.
There is, for example, the heart-wrenching account of “DJ,” a lonely medical student who is emergently hospitalized for depression, after the worried author anxiously drove the patient from his office to the hospital. DJ is all alone, and he writes to a friend and offers to pay for her transportation if she will come visit him in the hospital, a fact Dr. Myers knows only because he was later shown a letter DJ had written to his friend.
“He has been diminished and altered by his disease and the requisite hospital treatment, factors that we as mental health caregivers must never forget – or minimize. Visits from friends become visits of the representatives from the outside world, the link to normality, sanity, and anticipated return. These encounters are precious,” Dr. Myers writes.
As the book progressed, I began to wonder more about the author as a person. It is a memoir, so stated on the cover, but very little about his life is revealed. There are résumé-style facts: where he studied, or worked, or went to conferences, what he learned and what he spoke about, but I wanted to know more about how his experiences intertwined with his life. In the foreword, he talks about having an alcoholic mother. He tells the reader that being a husband and father was important to him, and that his conversion to Judaism – his wife’s religion – was meaningful, but there is no backstory, and I was looking for more. A quick reference is made to visiting a therapist, but those few sentences are the total of what I knew about Michael Myers midway through his memoir.
I looked for a photo of the author. I found it at the back of the book with a brief biography beneath it, ending with the fact that he lives with his husband. I had gotten halfway through the memoir, including chapters about how Myers had treated gay physicians, gay couples, and physicians with AIDS, and yet there was no mention of his husband, and how his sexual orientation influenced these encounters. I didn’t quite know what to think.
And then, in a section called “Getting Personal,” suddenly the tone of the book changed. Dr. Myers talked about his own sexual confusion as a young man and about the decision to marry a woman, knowing he was bisexual. He wrote about the shame he felt concerning his sexual desires at a time when homosexuality was still classified as a psychiatric disorder, the fear of judgment, and the sense that this – his ninth book – was his first genuine book.
“And so, I come full circle. It is my otherness that fundamentally – but not with full awareness – attracted me to psychiatry, and ultimately to becoming a doctors’ doctor. I’ve been able to empathize with my doctor patients’ burden with the scourge of mental illness, coping with brokenness, and struggling for acceptance and belonging in a profession of perfection and stature. And I understand what it’s like to feel a bit of a misfit, less than, unclean and tattered. But as a wounded healer, I know the restorative value of listening, acceptance, caring, doggedness, and hope.” And so I found Dr. Myers.
These few pages in the middle of the book pulled everything else into focus. The writing opened and the rest of the book flowed. The author’s insights about physician-patients became even more insightful. It’s almost as though he was anxious about revealing himself, and his writing infused itself with this worry, so that once his secret was revealed, he was free to be genuine in a way that makes this book a gem of a read.
His insights about treating troubled physicians are invaluable. He talks of their struggles with loss, and of their flawed roles as patients.
“At the point that they become a patient these individuals may already be quite ill, and this needs to be recognized and accepted by the treating psychiatrist. Judging the doctor for so many self-defeating behaviors is unacceptable and unprofessional. I have found it best to simply accept the old adage ‘It is what it is.’ And I try my best to be patient and understanding with such difficult and interwoven issues, in that for physicians becoming a patient is a process not an event.”
Written with empathy, warmth, and vulnerability, “Becoming a Doctors’ Doctor” is a worthwhile read for any psychiatrist who treats other physicians.
Dr. Miller is coauthor of “Committed: The Battle over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no conflicts of interest.
The psychiatrist and the vaccine
When the long-awaited news of a Food and Drug Administration–approved vaccine came on Dec. 11, 2020, my first thought was that I would wait. I can manage a few more months of Zooming for work, my household is down to two people, I’m not at high risk of dying from COVID, and my husband is not going to be vaccinated any time soon, so a change in my status wouldn’t “free” me. I would rather have “my” vaccine go to a 70-year-old ICU janitor or a bus driver.
The weeks have gone by. I expected there would be kinks, but it has now been a month – one in which COVID rates have soared, and hospitalizations and deaths have risen to unmanageable numbers in some places. Still, vaccines remain in freezers – people are dying while vials of prevention sit unused. I began to think that, when my “turn” came, the better thing was to be vaccinated. We need to have a large segment of the population vaccinated to squelch this virus, and it’s become much less clear to me that, if I yield my turn, it will go into the arm of a bus driver. The process has not been fair, and there are moments of media outrage when one group gets vaccinated before another, so perhaps we have reached point where the goal should not be to get the vaccine into the exact right person in the exact right order, but to get the vaccine into arms according to the protocol that has already been set. Anyone who does not end up in a hospital bed is doing the system a favor.
Mahmood Jahromi, MD, a psychiatrist in private practice in Towson, Md., described the process of vaccination as being similar to a bottleneck traffic jam. “Yes, one must be courteous to the car trying to but in, but no, don’t jam the glue because you are excessively kind. Let the traffic police do their job. When your name is called, go ahead and take it. The system needs to know people are accepting the vaccine, not by begging the authorities to be called ahead of others, but with respect for what is already designed.”
On Friday, Jan. 8, I received information on how to get vaccinated – it seems my “turn” has arrived. An email from the board of physicians informed me that I am in the “1A” category and included a link to sign up for a vaccine in Baltimore – vaccinations would be given until Jan. 29, Mondays to Thursdays from 10 a.m. to 4 p.m. and Fridays from 10 a.m. to 1 p.m. There are no weekend or evening hours, and one might think there would be enough urgency to call for this. The Maryland Psychiatric Society sent out a notice that Sheppard Pratt would be offering vaccines to all behavioral health providers in the state of Maryland during a 2-day clinic. I heard from others that health care workers can now get vaccinated at the Cow Palace (how great is that?) at the Maryland State Fairgrounds and another link was sent for those in Howard County, between Baltimore and Washington.
As I discussed this with colleagues, a couple of issues came up – the most common was one of not wanting to get the vaccine yet because there are others who need it more. Others voiced concern about a vaccine where the long-term effects remain unknown: Is this vaccine safe, might it spur autoimmune problems in the months or years to come? Is it safe for women who plan to become pregnant? Some have insisted it is safe. They say “follow the science” and have dismissed the skepticism. To my read, it makes perfect sense to be wary, but COVID spreads silently and it kills.
With a vaccine where so many are reluctant to get it, including many health care workers, Sue Kim, MD, a psychiatrist in private practice in Lutherville, Md., noted that she has concerns about the safety of the vaccine. “Getting it now is both altruistic and selfish, but letting others go first is also altruistic and selfish. In the meantime, if I get sick, I was too smart for my own good. How do you weigh this ethically?”
My personal feelings have been influenced by a few things. An article in the New York Times highlighted how New York City vaccinated 5 million people for smallpox in just 2 weeks in 1947. I am frustrated knowing that, a month after approval of the first vaccine, only 7 million people have received it in the entire United States. In that time period, millions have contracted COVID and thousands have died. Closer to home, a 45-year-old psychiatrist in Maryland died of COVID, and I have heard more stories about younger people with long-haul neurologic and vascular symptoms. The risk of COVID is feeling higher than it did, and the fact that the first vaccine was authorized after the election somehow makes me feel that it might be safer. Had it been approved right before, I would have worried – perhaps wrongly – that the authorization was a political maneuver, not one based on science.
As we think about what is best for ourselves, our families, our patients, and society as a whole, I believe that those who want the vaccine but don’t feel they should take their place in line before others who are higher risk must ask if it makes sense to wait. Each state is different. While Houston Methodist Hospital is reportedly giving its health care workers a $500 bonus to get the vaccine, Gov. Andrew Cuomo of New York announced that hospitals would be fined $100,000 if they don’t use all of their vaccines within 7 days of receipt and $1 million if they vaccinate anyone out of order. Gov. Cuomo later broadened who could be vaccinated to prevent wasting the vaccine, but there remains an element of being damned if you do and damned if you don’t.
Paul Nestadt, MD, a psychiatrist at Johns Hopkins University, Baltimore, noted that one distribution site initially had to waste unused vaccine when people did not come for their appointments. A waiting list was created for people who could come right away if called to prevent this waste. “To me, this only highlighted that the tier system, while a good idea, does not need to be written in stone. The goal needs to be getting shots in arms, building herd immunity. If there are two arms in front of you, shoot the health care worker or those who are vulnerable. But if there is a healthy arm in reach, it should get any shot made available.”
I registered to be vaccinated. – senior citizens and essential workers are not yet eligible. In Baltimore, vaccinations are available Mondays to Thursdays from 10 a.m. to 4 p.m. and on Fridays from 10 a.m. to 1 p.m. There are no options for early morning or weekend times, but there are slots still available for the coming week. As of this writing, there are 6,100 Marylanders dead, and more than 1,800 COVID patients in hospital beds, and our governor, Larry Hogan, has commercials to “Mask On Maryland” and “Wear the Damn Mask.” I’ll offer some changes: “Wake Up, World” and “Offer the Damn Shot.”
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller has no disclosures.
When the long-awaited news of a Food and Drug Administration–approved vaccine came on Dec. 11, 2020, my first thought was that I would wait. I can manage a few more months of Zooming for work, my household is down to two people, I’m not at high risk of dying from COVID, and my husband is not going to be vaccinated any time soon, so a change in my status wouldn’t “free” me. I would rather have “my” vaccine go to a 70-year-old ICU janitor or a bus driver.
The weeks have gone by. I expected there would be kinks, but it has now been a month – one in which COVID rates have soared, and hospitalizations and deaths have risen to unmanageable numbers in some places. Still, vaccines remain in freezers – people are dying while vials of prevention sit unused. I began to think that, when my “turn” came, the better thing was to be vaccinated. We need to have a large segment of the population vaccinated to squelch this virus, and it’s become much less clear to me that, if I yield my turn, it will go into the arm of a bus driver. The process has not been fair, and there are moments of media outrage when one group gets vaccinated before another, so perhaps we have reached point where the goal should not be to get the vaccine into the exact right person in the exact right order, but to get the vaccine into arms according to the protocol that has already been set. Anyone who does not end up in a hospital bed is doing the system a favor.
Mahmood Jahromi, MD, a psychiatrist in private practice in Towson, Md., described the process of vaccination as being similar to a bottleneck traffic jam. “Yes, one must be courteous to the car trying to but in, but no, don’t jam the glue because you are excessively kind. Let the traffic police do their job. When your name is called, go ahead and take it. The system needs to know people are accepting the vaccine, not by begging the authorities to be called ahead of others, but with respect for what is already designed.”
On Friday, Jan. 8, I received information on how to get vaccinated – it seems my “turn” has arrived. An email from the board of physicians informed me that I am in the “1A” category and included a link to sign up for a vaccine in Baltimore – vaccinations would be given until Jan. 29, Mondays to Thursdays from 10 a.m. to 4 p.m. and Fridays from 10 a.m. to 1 p.m. There are no weekend or evening hours, and one might think there would be enough urgency to call for this. The Maryland Psychiatric Society sent out a notice that Sheppard Pratt would be offering vaccines to all behavioral health providers in the state of Maryland during a 2-day clinic. I heard from others that health care workers can now get vaccinated at the Cow Palace (how great is that?) at the Maryland State Fairgrounds and another link was sent for those in Howard County, between Baltimore and Washington.
As I discussed this with colleagues, a couple of issues came up – the most common was one of not wanting to get the vaccine yet because there are others who need it more. Others voiced concern about a vaccine where the long-term effects remain unknown: Is this vaccine safe, might it spur autoimmune problems in the months or years to come? Is it safe for women who plan to become pregnant? Some have insisted it is safe. They say “follow the science” and have dismissed the skepticism. To my read, it makes perfect sense to be wary, but COVID spreads silently and it kills.
With a vaccine where so many are reluctant to get it, including many health care workers, Sue Kim, MD, a psychiatrist in private practice in Lutherville, Md., noted that she has concerns about the safety of the vaccine. “Getting it now is both altruistic and selfish, but letting others go first is also altruistic and selfish. In the meantime, if I get sick, I was too smart for my own good. How do you weigh this ethically?”
My personal feelings have been influenced by a few things. An article in the New York Times highlighted how New York City vaccinated 5 million people for smallpox in just 2 weeks in 1947. I am frustrated knowing that, a month after approval of the first vaccine, only 7 million people have received it in the entire United States. In that time period, millions have contracted COVID and thousands have died. Closer to home, a 45-year-old psychiatrist in Maryland died of COVID, and I have heard more stories about younger people with long-haul neurologic and vascular symptoms. The risk of COVID is feeling higher than it did, and the fact that the first vaccine was authorized after the election somehow makes me feel that it might be safer. Had it been approved right before, I would have worried – perhaps wrongly – that the authorization was a political maneuver, not one based on science.
As we think about what is best for ourselves, our families, our patients, and society as a whole, I believe that those who want the vaccine but don’t feel they should take their place in line before others who are higher risk must ask if it makes sense to wait. Each state is different. While Houston Methodist Hospital is reportedly giving its health care workers a $500 bonus to get the vaccine, Gov. Andrew Cuomo of New York announced that hospitals would be fined $100,000 if they don’t use all of their vaccines within 7 days of receipt and $1 million if they vaccinate anyone out of order. Gov. Cuomo later broadened who could be vaccinated to prevent wasting the vaccine, but there remains an element of being damned if you do and damned if you don’t.
Paul Nestadt, MD, a psychiatrist at Johns Hopkins University, Baltimore, noted that one distribution site initially had to waste unused vaccine when people did not come for their appointments. A waiting list was created for people who could come right away if called to prevent this waste. “To me, this only highlighted that the tier system, while a good idea, does not need to be written in stone. The goal needs to be getting shots in arms, building herd immunity. If there are two arms in front of you, shoot the health care worker or those who are vulnerable. But if there is a healthy arm in reach, it should get any shot made available.”
I registered to be vaccinated. – senior citizens and essential workers are not yet eligible. In Baltimore, vaccinations are available Mondays to Thursdays from 10 a.m. to 4 p.m. and on Fridays from 10 a.m. to 1 p.m. There are no options for early morning or weekend times, but there are slots still available for the coming week. As of this writing, there are 6,100 Marylanders dead, and more than 1,800 COVID patients in hospital beds, and our governor, Larry Hogan, has commercials to “Mask On Maryland” and “Wear the Damn Mask.” I’ll offer some changes: “Wake Up, World” and “Offer the Damn Shot.”
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller has no disclosures.
When the long-awaited news of a Food and Drug Administration–approved vaccine came on Dec. 11, 2020, my first thought was that I would wait. I can manage a few more months of Zooming for work, my household is down to two people, I’m not at high risk of dying from COVID, and my husband is not going to be vaccinated any time soon, so a change in my status wouldn’t “free” me. I would rather have “my” vaccine go to a 70-year-old ICU janitor or a bus driver.
The weeks have gone by. I expected there would be kinks, but it has now been a month – one in which COVID rates have soared, and hospitalizations and deaths have risen to unmanageable numbers in some places. Still, vaccines remain in freezers – people are dying while vials of prevention sit unused. I began to think that, when my “turn” came, the better thing was to be vaccinated. We need to have a large segment of the population vaccinated to squelch this virus, and it’s become much less clear to me that, if I yield my turn, it will go into the arm of a bus driver. The process has not been fair, and there are moments of media outrage when one group gets vaccinated before another, so perhaps we have reached point where the goal should not be to get the vaccine into the exact right person in the exact right order, but to get the vaccine into arms according to the protocol that has already been set. Anyone who does not end up in a hospital bed is doing the system a favor.
Mahmood Jahromi, MD, a psychiatrist in private practice in Towson, Md., described the process of vaccination as being similar to a bottleneck traffic jam. “Yes, one must be courteous to the car trying to but in, but no, don’t jam the glue because you are excessively kind. Let the traffic police do their job. When your name is called, go ahead and take it. The system needs to know people are accepting the vaccine, not by begging the authorities to be called ahead of others, but with respect for what is already designed.”
On Friday, Jan. 8, I received information on how to get vaccinated – it seems my “turn” has arrived. An email from the board of physicians informed me that I am in the “1A” category and included a link to sign up for a vaccine in Baltimore – vaccinations would be given until Jan. 29, Mondays to Thursdays from 10 a.m. to 4 p.m. and Fridays from 10 a.m. to 1 p.m. There are no weekend or evening hours, and one might think there would be enough urgency to call for this. The Maryland Psychiatric Society sent out a notice that Sheppard Pratt would be offering vaccines to all behavioral health providers in the state of Maryland during a 2-day clinic. I heard from others that health care workers can now get vaccinated at the Cow Palace (how great is that?) at the Maryland State Fairgrounds and another link was sent for those in Howard County, between Baltimore and Washington.
As I discussed this with colleagues, a couple of issues came up – the most common was one of not wanting to get the vaccine yet because there are others who need it more. Others voiced concern about a vaccine where the long-term effects remain unknown: Is this vaccine safe, might it spur autoimmune problems in the months or years to come? Is it safe for women who plan to become pregnant? Some have insisted it is safe. They say “follow the science” and have dismissed the skepticism. To my read, it makes perfect sense to be wary, but COVID spreads silently and it kills.
With a vaccine where so many are reluctant to get it, including many health care workers, Sue Kim, MD, a psychiatrist in private practice in Lutherville, Md., noted that she has concerns about the safety of the vaccine. “Getting it now is both altruistic and selfish, but letting others go first is also altruistic and selfish. In the meantime, if I get sick, I was too smart for my own good. How do you weigh this ethically?”
My personal feelings have been influenced by a few things. An article in the New York Times highlighted how New York City vaccinated 5 million people for smallpox in just 2 weeks in 1947. I am frustrated knowing that, a month after approval of the first vaccine, only 7 million people have received it in the entire United States. In that time period, millions have contracted COVID and thousands have died. Closer to home, a 45-year-old psychiatrist in Maryland died of COVID, and I have heard more stories about younger people with long-haul neurologic and vascular symptoms. The risk of COVID is feeling higher than it did, and the fact that the first vaccine was authorized after the election somehow makes me feel that it might be safer. Had it been approved right before, I would have worried – perhaps wrongly – that the authorization was a political maneuver, not one based on science.
As we think about what is best for ourselves, our families, our patients, and society as a whole, I believe that those who want the vaccine but don’t feel they should take their place in line before others who are higher risk must ask if it makes sense to wait. Each state is different. While Houston Methodist Hospital is reportedly giving its health care workers a $500 bonus to get the vaccine, Gov. Andrew Cuomo of New York announced that hospitals would be fined $100,000 if they don’t use all of their vaccines within 7 days of receipt and $1 million if they vaccinate anyone out of order. Gov. Cuomo later broadened who could be vaccinated to prevent wasting the vaccine, but there remains an element of being damned if you do and damned if you don’t.
Paul Nestadt, MD, a psychiatrist at Johns Hopkins University, Baltimore, noted that one distribution site initially had to waste unused vaccine when people did not come for their appointments. A waiting list was created for people who could come right away if called to prevent this waste. “To me, this only highlighted that the tier system, while a good idea, does not need to be written in stone. The goal needs to be getting shots in arms, building herd immunity. If there are two arms in front of you, shoot the health care worker or those who are vulnerable. But if there is a healthy arm in reach, it should get any shot made available.”
I registered to be vaccinated. – senior citizens and essential workers are not yet eligible. In Baltimore, vaccinations are available Mondays to Thursdays from 10 a.m. to 4 p.m. and on Fridays from 10 a.m. to 1 p.m. There are no options for early morning or weekend times, but there are slots still available for the coming week. As of this writing, there are 6,100 Marylanders dead, and more than 1,800 COVID patients in hospital beds, and our governor, Larry Hogan, has commercials to “Mask On Maryland” and “Wear the Damn Mask.” I’ll offer some changes: “Wake Up, World” and “Offer the Damn Shot.”
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. Dr. Miller has no disclosures.
Zoom Zoom Zoom: An end-of-year update from a virtual psychiatrist
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Can mental health teams de-escalate crises in NYC?
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
Conquering the stigma of getting mental health care
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.
Last summer, back when people traveled, I had the pleasure of being in Amsterdam for Pride Week. With a half-million tourists, it was a colorful and costumed display of LGBTQ pride, and both the streets and canals had celebrations with food, drinks, music, and displays beyond anything I could describe.
It was all not that long ago that the American Psychiatric Association classified homosexuality as a psychiatric disorder. Now we have Pride celebrations, and I don’t think twice about mentioning my brother-in-law’s husband, or a female colleague’s wife, nor am I shocked when I hear that the children of my friends are in the process of gender transition. Obviously, the idea that people express both their gender and their sexuality in diverse ways is not accepted by everyone, but we’ve come a long way toward acceptance of people who were once stigmatized and pathologized. I’ll also point out that this shift occurred despite the fact that the gay community was affected by AIDS.
There are many other differences – and illnesses – that our society has come to either accept or sympathize with more graciously over time, and yet both mental illness and substance abuse disorders remain stigmatized and punished. To put it bluntly, we have done a terrible job of making these conditions acceptable illnesses to have, even though we have done a reasonably good job of offering effective treatments. Cancer no longer carries the stigma it once did, even though cancer is a leading cause of death, and the treatments are painful, toxic, and may include the loss of body parts and hair. But if you become ill with cancer, your friends bring casseroles (or perhaps rotisserie chickens), and if you’re hospitalized with bipolar disorder or check into a drug treatment center, you’re more likely to be the recipient of judgment and even scorn.
We have to fix this. We talk about the need to destigmatize mental illness and substance use disorders, and to make these illnesses more on par with other diseases. Maybe that is the wrong call: These disorders sometimes cause people to behave in disruptive, dangerous, and illegal ways that we don’t often see with other illnesses. Frankly psychotic people may be seen as “other,” they may smell bad, they may behave in bizarre ways, and they may be frightening. Their rare acts of violence have been publicized so much that “He’s mentally ill” is accepted by the public as a full explanation for why someone would commit a mass shooting. Depression can cause people to be irritable and unpleasant, and our society equates a lack of motivation with laziness. While people may have sympathy for the suicidal thoughts and feelings of others, completed suicide leaves behind devastated survivors. People with substance use problems may become belligerent or commit crimes to support their addictions. In 2018, over 10,500 people were killed by drivers who were impaired by alcohol. I’m not sure how we destigmatize these conditions, but commercials, billboards, and educational programs aren’t doing it.
Fears around treatment
Perhaps our efforts need to go toward destigmatizing treatment. It is shocking to me how resistant people are to getting help, or having others know they are getting help, when treatment often renders them free from the psychological agony or misbehaviors caused by their condition.
Since I work in an outpatient setting, I see people who have made it beyond the barrier of seeking help. Almost all of my patients are willing to try medications – there is self-selection among those who chose to see a psychiatrist as opposed to another type of psychotherapist. I also believe that direct-to-consumer advertising has helped normalize the use of psychotropic medications.
When it comes to getting a higher level of care, however, the conversations are so much harder. Many of my patients insist they will never be admitted to a psychiatric unit, and when I ask depressed people if they are having suicidal thoughts, some tell me they are afraid to let me know they are for fear I might hospitalize them. This fear of hospitalization is present in people who have never been in a hospital and have only media depictions or their imaginations to go by, but I also see this with patients who have previously been hospitalized and have emerged from their inpatient stays feeling much better. While we know that any type of hospitalization involves a loss of control, unpleasant moments, and sometimes painful procedures, I have never heard anyone say that, if they were to have a second heart attack, they would refuse an admission to the cardiac care unit.
Discussions about treatment for substance use are even more difficult. People with addictions often don’t want to abstain from the substance they are using, and this is an enormous hurdle. Beyond that, they don’t like the labels that come with acknowledging a problem – words like “junkie,” “addict,” “drunk,” and “alcoholic” are hard to escape.
People fear hospitalization for many reasons: They fear losing control, they don’t recognize that they have a problem, or they rationalize their psychosis or substance use as normal. Most of all, they fear what others will think of them and what repercussions this will have for their futures. Patients would rather continue in a state of agony and dysfunction when inpatient treatment would make them better faster. This is nothing short of tragic.
What can we do? The answer is “a lot.” We need to work harder to make the hospital experience a pleasant one for patients. Inpatient units need to be clean, safe places where patients are treated with kindness, dignity, and respect and activities are appropriate, interesting, and promote healing.
Maria, a Maryland attorney, told me about her experience with inpatient treatment. “I experienced my hospitalization as jailing and acutely felt the loss of liberty, especially in the ER, where I was confined to something I recognized from my time visiting incarcerated and detained people as a holding cell, complete with a uniformed guard. I was scared to engage in any kind of meaningful self-advocacy around leaving out of fear for my license to practice law and of lengthening my time as an inpatient. As a result, I found myself concentrating on getting out, and not on getting well. With the benefit of hindsight, I can say now that my hospitalization was a lost opportunity, and the coercive elements were barriers to accessing the treatment that I needed, both at the time and in the years following the hospitalization.”
We have too many policies in place where infractions are met with force, seclusion, and sometimes restraint, and we need to be more flexible with these policies. If a psychiatric unit requires lab work prior to admission and the patient refuses, should force be used in the emergency department if there is nothing to indicate that the patient’s health is in imminent danger? And if the hospital has a policy that all psychiatric patients must disrobe to be examined for preexisting scars or contraband – this is an admission standard for some hospitals, but not others – and the patient refuses, what then? Typically, inpatients are not allowed access to their cell phones or the Internet (for many good reasons), but patients find this very upsetting; might it make sense to allow periods where they can use devices with supervision? Hospitals often forbid smoking, and people with psychiatric disorders may smoke – while it is a wonderful health ideal, is it reasonable to forbid smoking for the course of a hospitalization?
We must work to get questions about psychiatric and substance use disorders removed from any job- or licensure-related forms. There is no reason to believe that people answer these forms truthfully or that including these questions protects the public in any way. What we do know is that people don’t seek help because they, like Maria, are afraid of the consequences of getting care. It doesn’t matter if a surgeon’s abilities are limited because he has episodes of hypoglycemia or past episodes of mania, and the only question on licensing forms should be about current conditions that impair the ability to work. Every district branch of the American Psychiatric Association should be actively speaking with their state professional licensing boards about the harm these questions do.
We need better treatments that have fewer side effects, and we need to acknowledge that, while getting help is the right thing to do, not everyone finds the right treatment with the first attempt and not everyone gets better. Our party line to those who feel suicidal has been “Get Help,” often with a phone number for the National Suicide Prevention Lifeline. While this is an important resource to have readily available, many of the people who die of suicide are already in active treatment. Our party line needs to change to “Get Help, and if it isn’t working, Get Different Help.” We want to be careful that our messaging does not foster a sense of hopelessness in those who have sought care and still suffer.
It’s good to talk about the potential benefits of treatment, but we don’t have enough beds and we don’t have enough mental health clinicians. There are states where psychiatric patients who have committed no crime are held in jail cells while they wait for beds to open – that we allow this is nothing short of a disgrace. The sickest patients with treatment-resistant conditions need access to the best care, and that access should not be limited by finances or networks. And while I’m here: We need our mental health professionals to spend their time working with patients, not computer screens, check boxes, and prior authorization protocols.
Finally, we need to work with the media to show positive and accurate depictions of psychiatric treatment as something that helps. We are still undoing the harm of Nurse Ratched and the depiction of electroconvulsive therapy in the 1975 film “One Flew Over the Cuckoo’s Nest,” and the current focus on mental illness and violence does nothing to help people feel comfortable seeking care.
I’ll end with one more thought from Maria: “Mental health professionals need to talk about hospitalization up front, no matter how uncomfortable, and encourage patients to think about hospitalization as a treatment option on a continuum before it is needed, so they are not approaching hospitalization as an abstract concept, often with a lot of fear and stigma attached to it, but rather as an option that they might explore in a fact-based way.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore. She reported having nothing to disclose.
Listening to Tim Ferriss
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Let me tell you about Tim Ferriss. A few years ago, I started reading his best-selling book, The 4-Hour Body. Ferris detailed how he made himself into a one-man experiment – he’d make changes to his diet, checked his weight and his labs, maybe he even had metabolic studies done.
He’d take these measures after soaking in hot baths, then ice baths, and while I admired his discipline, he did lose me during the chapter where he was using steroids. In the end, he advised a dairy-free, low-carbohydrate diet of green vegetables, beans or lentils, and protein for four meals a day, 6 days a week, with free-for-all eating on the 7th day. Then, there was a weight-lifting routine with kettle bells and ice packs to be placed on your shoulders for a set amount of time each day.
I may not remember the program’s details, but something about Ferris fascinated me. He brands himself as being a “human guinea pig,” about “lifestyle design,” and whatever that is, I like it. Perhaps I am attracted to the idea that we might control the trajectories of our generally uncontrollable lives.
Tim Ferriss graduated from Princeton, he’s written five best-selling books and has a popular podcast, he’s been a TED speaker, and he’s been on Fortune’s “40 under 40” list – and there’s so much more. Ferriss is brilliant, innovative, handsome, charismatic, prolific, extraordinarily athletic. I may have forgotten to mention that he was the National Chinese Kickboxing Champion and was a semifinalist in the World Champion Tango competition in Buenos Aires. He’s adventuresome and fearless, and if that isn’t enough, he speaks five languages. In the genetic dice roll, Mr. Ferriss did well, and he’s a driven and energetic hard worker who is open to new experiences.
I subscribe to the Tim Ferriss podcast – as of this writing, there are 466 episodes, with an incredible lineup of interviews with famous and successful guests. I also subscribe to his “5-Bullet Friday” email list where he mentions the interesting things he is reading, watching, learning about, or eating, and the products he is trying – single-ply toilet paper gets a thumbs down – then ends with a thought-provoking quote. This gentleman spends a tremendous amount of time searching and striving, working on himself and his own emotional growth and self-improvement, and yet he still has time for incredible explorations and experiences.
A search for psychic peace
Honestly, were it not for a few little details, I would like to be Tim Ferriss. Who wouldn’t? But what stops me from actually wanting to be Ferriss is that early on while listening to him, I realized that his drive has been fueled by intense psychic pain. He talks openly about being very close to suicide in college, about a tormenting mood disorder, demons to tame, and productivity as an antidote to a fear of failure, not always as a joy for life. There are moments that I have felt so sad for this remarkable stranger. Tim Ferriss is a searcher and what I believe he searches for most is his own psychic peace.
In a forum for psychiatrists, I wish I could write that Ferriss has found solace with our Food and Drug Administration–approved pharmaceuticals and with psychotherapy, but that’s not what he says. What Ferriss has found helpful, however, is psychedelics, and a wide variety of psychological and philosophical teachings ranging from meditation to Stoicism. And most notably, Ferriss has been an advocate for using hallucinogens as a legal medical intervention. Ferriss was one of four philanthropists who donated a total of $17 million to fund the Johns Hopkins Center for Psychedelic & Consciousness Research. He’s helped to move this field forward and to improve its credibility.
On Sept. 14, 2020, Tim Ferriss released a podcast he recorded with his dance partner and close friend, Debbie Millman, and when he recorded it, he was not certain he would release it. None of his usual sponsors endorsed during the podcast. He starts Episode #464 with, “For me, this is the most important podcast episode I’ve ever published. In it, I describe the most life-shaping, certainly the most difficult, and certainly the most transformative journey of my 43 years on this planet. I’ve never shared it before.”
by a babysitter’s son. He worried about how this would affect his family, if they would be left feeling guilty or devastated. He says, “Please note that I expect to be completely overwhelmed emotionally and otherwise when this is published and please understand if I’m not able to reply to any outreach.”
Ferriss and Millman had a long discussion about their sexual abuse as children. Millman was abused by her stepfather at the age of 9, and she talks about confronting him many years later. Ferriss has not confronted his perpetrator, though he has contemplated doing so.
Sexual violence and violation at any age leaves people scarred. In a recent letter to the New York Times in response to President Trump’s words of support to Ghislaine Maxwell, the woman who helped Jeffrey Epstein find his victims, Baltimore psychiatrist Robin Weiss wrote, “Thirty-eight years ago, when I was 32, I was raped. I was married, I was a doctor – you might say I was in pretty stable shape. Yet the shame and guilt I felt were overwhelming. Why didn’t I fight harder? How did I let this happen? I knew better, yet it took me years to overcome those irrational feelings.” These feelings of shame, guilt, self-doubt, and self-blame are nearly universal in survivors of sexual trauma. In children, they can be even worse, as children often don’t have an understanding that what is being done to them is wrong. They lack the language and the maturity to process the events, and ongoing abuse may be accompanied by threats to life of the child or their family members if they tell others, as was the case with Millman. She chose to process her abuse and the consequent difficulties she had by seeking psychiatric care. She took antidepressants and has been in psychoanalysis, both of which she has found to be helpful. Her treatment has tamed her demons, it is ongoing decades later and those demons have not vanished.
Abuse comes back in ‘a tidal wave’
Not surprisingly, Ferriss struggled with whether to make these events public. While so much of his story feels familiar to those of us who help patients process their trauma, it’s not completely typical. Ferriss remembered these episodes of sexual abuse “in high resolution,” while using ayahuasca, a hallucinogen, about 5 years ago. He describes suppressing and discounting these memories until he attended a 10-day silent retreat where he used psilocybin. I found it interesting that Ferriss fasted for 5 days before attending the retreat “to increase the depth of the experience.” He goes on to say, “Around day 6 of this silent retreat, all of this abuse came back to me like a tidal wave and it was replaying as if I was wearing a virtual reality headset. I was immersed, I wasn’t an observer, it was as though I was being traumatized and retraumatized 24/7.” He describes an excruciating and horrifying experience and he referred to it as a “psychotic break.”
Ferriss goes on to talk about how bringing these memories to light has affected him, how it’s explained many of his behaviors and ways of relating in a way that has helped him organize and understand his life.
“It was at the tail end of the retreat that I realized that these 17 seemingly inexplicable behaviors of mine – these vicious cycles or triggers that I had been treating like separate problems to be solved, were all downstream of this trauma. Oh, now that you click that puzzle piece into place, these really strange behaviors – this self-loathing, this rage that was seemingly so exaggerated and disproportionate – leading to the near-suicide I had in college – all these things fell into places making sense.” It gave him a sense of relief but was simultaneously overwhelming.
Both Ferriss and Millman talk about books and treatments that have been helpful to them. Their knowledge of trauma treatments and resources is impressive and can be found at: Tim Ferriss – My Healing Journey After Childhood Abuse (Includes Extensive Resource List). Their wish is to share their suffering as a way to help others, impart hope, and better connect.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
A doctor conquers his demons
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
I am part of the problem
Race is not something I’ve spent that much time contemplating. I grew up in Elizabeth, N.J., a city of just over 100,000, in the 1970s and attended public schools where people came in all shapes and colors; diversity came with the turf, it wasn’t something anyone needed to strive for.
My high school had more than 4,000 students with roughly even numbers of white, black, and Hispanic students. Armed police patrolled the halls, the thick aroma of weed settled in the stairwells and restrooms, girls brought their babies to school to show them off on half-days, and the “preppies” wore Fair Isle sweaters and played on the tennis team. The school’s campus was brand new and every lab, studio, and athletic amenity was state of the art; at the time, it was the most expensive public high school ever built in America. There were black teachers, librarians, and administrators, and segregation was something we read about in history books. I lived in a world of Technicolor and the Civil Rights movement of the 1960s, while still fresh in the minds of the adults, was something that showed up on black-and-white footage from another time.
My world became both wealthier and whiter when I went to college. There were minority students, but many of the black students at the University of Pennsylvania chose to live in the W.E.B. Du Bois College House.
People are often more comfortable being with others who share their backgrounds and this makes for an interesting conundrum: We all agree that desegregation is a good thing, but not everyone wishes to be told either where to go or not go, and there is an odd unbalance to creating a safe place for black students to be, one that both integrates and separates them from the larger community. Perhaps all our lines get fuzzy – I recall when I was on the Maryland Psychiatric Society Women’s Committee and a male psychiatrist signed up to join us – he was politely told that he could not join, but 20 years later, I’m wondering if it was okay to exclude a man who expressed interest in women’s issues.
In medical school, we were taught to note a patient’s age, race, and marital status, and we might learn that certain illnesses were more prevalent in certain populations, but there was no discussion of racial inequities in health care or anywhere else.
What was really different about the world back then, however, was what we didn’t see and what we didn’t talk about. Social media has opened a world where we can share our pain in the moment and we can band together to speak out against crimes and injustices in every realm. From the MeToo moments, to racially motivated police brutality. Cell phone cameras let us record and publicize these moments so the world can be the judge. George Floyd’s sadistic murder by a police officer, as other officers stood by and watched 8 minutes and 46 seconds of torture, left us all triggered, distressed, angry, sad, and activated. Maybe now we can make real progress on a discussion that began in 1992 with the videotape of Rodney King’s assault, a discussion we’ve had over and over to no avail.
Obviously, I have also been provoked by the events of the past weeks – like many Americans, I’ve paused to wonder how I can help the cause, both personally and as a psychiatrist. I would not normally write about racial topics – as a white woman I can listen, but I don’t feel this pain in the same way as someone who has lived with a lifetime of discrimination and oppression. Dr. Lorenzo Norris and Dr. Brandon Newsome,two black psychiatrists, put out a special edition of the MDEdge Psychcast, “The fallout from George Floyd’s death,” and Dr. Norris noted that two of his white colleagues told him they thought of checking on him, but they didn’t know what to say. Yes, I thought, that’s exactly it, I don’t know what to say and I worry that I might unintentionally say something that would worsen someone else’s pain. Staying silent has always seemed to be the safest option. With this article, I’m moving from a place of comfort.
I started my career with a mix of private practice and community psychiatry. There were things I loved about working in a community clinic: the social aspects of being part of a team, seeing a full range of psychopathology, and treating patients in which the racial and ethnic demographics mirrored that of the community. There were things I didn’t like, however. The pay was low, there were constant institutional requirements that were not relevant to the practice of psychiatry, and my relationship with the patients as their prescriber was much less fulfilling than the relationship I have with those I see for both psychotherapy and medication. Ultimately, the hospital shift to electronic medical records was the final distraction that caused me to leave community work.
Like roughly half of psychiatrists in private practice, I don’t participate with commercial or public insurance plans. Early in my career, I worked in a group setting with billing secretaries, and I did participate with Blue Cross, but even with administrative help, nothing about this was easy, and when I left to do solo practice, I left insurance participation behind. I love the autonomy of my career, I’m proud of the care I am able to give in this setting, and I don’t miss the hassles. But – the out-of-pocket cost of care is higher and the effort of trying to get reimbursed falls to the patient. It means that most of the patients I see have the means to pay for care, none are impoverished or homeless, and while I work in a city that is 62% black, black patients make up a small percentage of my caseload. I don’t think I am unique in this; I would be shocked if any white private practice psychiatrist who specializes in psychotherapy is serving a racially proportionate population. As we start to embrace the idea that people don’t neatly divide into being racist or not, and that bias affects us all, we must acknowledge that medical practices that don’t support racially balanced access to care are part of the problem.
Amy R. Greensfelder, LMSW, is the executive director of Maryland’s Pro Bono Counseling Project (PBCP), an organization that coordinates mental health professionals in private practice in Maryland to volunteer their services to those with limited resources. PBCP has found that 50% of those seeking services share that they are black or African American, and an additional 5% identify as multiracial. Of all of those seeking care approximately 65% are black, Indigenous, or People of Color (BIPOC), and and 14% are Latino/a/x/Hispanic. She says: “We see the racial composition of our clients as a direct demonstration of who is being left behind in the mental health system as it’s currently set up, as BIPOC individuals are represented to a greater degree in our clients than they are in the general population of Maryland. During our intake interview, we provide an opportunity for clients to share if there are certain characteristics they are looking for in a therapist – often black clients share that they would prefer to be matched with a black therapist or a therapist who has received specific training on working with black clients.”
While 13% of the American population is black, only 4% of physicians, 2% of psychiatrists, and 4% of psychologists are black. In her Psychology Today blog post, “Why African Americans Avoid Psychotherapy,” Monnica T. Williams, PhD, notes: “Apprehension about clashing with the values or worldview of the clinician can cause ambivalence about seeking help, and this may be especially true for the many who believe that mental health treatment was designed by white people for white people.” Dr. Williams notes that black Americans also are less likely to seek care because of increased stigma and fear of judgment, concerns about the treatment process, and fears of being involuntarily hospitalized, cost and lack of insurance, and finally logistical issues with work, transportation, and family responsibilities.
George Floyd’s tragic death has led us to a moment of crisis. It’s my hope that the dialogue is now galvanized to make meaningful changes toward fixing racial inequities. I am part of the problem and these conversations need to include more equitable access to psychiatric care.
My thanks to Rachel Donabedian and Gina Henderson for their help with this article.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Race is not something I’ve spent that much time contemplating. I grew up in Elizabeth, N.J., a city of just over 100,000, in the 1970s and attended public schools where people came in all shapes and colors; diversity came with the turf, it wasn’t something anyone needed to strive for.
My high school had more than 4,000 students with roughly even numbers of white, black, and Hispanic students. Armed police patrolled the halls, the thick aroma of weed settled in the stairwells and restrooms, girls brought their babies to school to show them off on half-days, and the “preppies” wore Fair Isle sweaters and played on the tennis team. The school’s campus was brand new and every lab, studio, and athletic amenity was state of the art; at the time, it was the most expensive public high school ever built in America. There were black teachers, librarians, and administrators, and segregation was something we read about in history books. I lived in a world of Technicolor and the Civil Rights movement of the 1960s, while still fresh in the minds of the adults, was something that showed up on black-and-white footage from another time.
My world became both wealthier and whiter when I went to college. There were minority students, but many of the black students at the University of Pennsylvania chose to live in the W.E.B. Du Bois College House.
People are often more comfortable being with others who share their backgrounds and this makes for an interesting conundrum: We all agree that desegregation is a good thing, but not everyone wishes to be told either where to go or not go, and there is an odd unbalance to creating a safe place for black students to be, one that both integrates and separates them from the larger community. Perhaps all our lines get fuzzy – I recall when I was on the Maryland Psychiatric Society Women’s Committee and a male psychiatrist signed up to join us – he was politely told that he could not join, but 20 years later, I’m wondering if it was okay to exclude a man who expressed interest in women’s issues.
In medical school, we were taught to note a patient’s age, race, and marital status, and we might learn that certain illnesses were more prevalent in certain populations, but there was no discussion of racial inequities in health care or anywhere else.
What was really different about the world back then, however, was what we didn’t see and what we didn’t talk about. Social media has opened a world where we can share our pain in the moment and we can band together to speak out against crimes and injustices in every realm. From the MeToo moments, to racially motivated police brutality. Cell phone cameras let us record and publicize these moments so the world can be the judge. George Floyd’s sadistic murder by a police officer, as other officers stood by and watched 8 minutes and 46 seconds of torture, left us all triggered, distressed, angry, sad, and activated. Maybe now we can make real progress on a discussion that began in 1992 with the videotape of Rodney King’s assault, a discussion we’ve had over and over to no avail.
Obviously, I have also been provoked by the events of the past weeks – like many Americans, I’ve paused to wonder how I can help the cause, both personally and as a psychiatrist. I would not normally write about racial topics – as a white woman I can listen, but I don’t feel this pain in the same way as someone who has lived with a lifetime of discrimination and oppression. Dr. Lorenzo Norris and Dr. Brandon Newsome,two black psychiatrists, put out a special edition of the MDEdge Psychcast, “The fallout from George Floyd’s death,” and Dr. Norris noted that two of his white colleagues told him they thought of checking on him, but they didn’t know what to say. Yes, I thought, that’s exactly it, I don’t know what to say and I worry that I might unintentionally say something that would worsen someone else’s pain. Staying silent has always seemed to be the safest option. With this article, I’m moving from a place of comfort.
I started my career with a mix of private practice and community psychiatry. There were things I loved about working in a community clinic: the social aspects of being part of a team, seeing a full range of psychopathology, and treating patients in which the racial and ethnic demographics mirrored that of the community. There were things I didn’t like, however. The pay was low, there were constant institutional requirements that were not relevant to the practice of psychiatry, and my relationship with the patients as their prescriber was much less fulfilling than the relationship I have with those I see for both psychotherapy and medication. Ultimately, the hospital shift to electronic medical records was the final distraction that caused me to leave community work.
Like roughly half of psychiatrists in private practice, I don’t participate with commercial or public insurance plans. Early in my career, I worked in a group setting with billing secretaries, and I did participate with Blue Cross, but even with administrative help, nothing about this was easy, and when I left to do solo practice, I left insurance participation behind. I love the autonomy of my career, I’m proud of the care I am able to give in this setting, and I don’t miss the hassles. But – the out-of-pocket cost of care is higher and the effort of trying to get reimbursed falls to the patient. It means that most of the patients I see have the means to pay for care, none are impoverished or homeless, and while I work in a city that is 62% black, black patients make up a small percentage of my caseload. I don’t think I am unique in this; I would be shocked if any white private practice psychiatrist who specializes in psychotherapy is serving a racially proportionate population. As we start to embrace the idea that people don’t neatly divide into being racist or not, and that bias affects us all, we must acknowledge that medical practices that don’t support racially balanced access to care are part of the problem.
Amy R. Greensfelder, LMSW, is the executive director of Maryland’s Pro Bono Counseling Project (PBCP), an organization that coordinates mental health professionals in private practice in Maryland to volunteer their services to those with limited resources. PBCP has found that 50% of those seeking services share that they are black or African American, and an additional 5% identify as multiracial. Of all of those seeking care approximately 65% are black, Indigenous, or People of Color (BIPOC), and and 14% are Latino/a/x/Hispanic. She says: “We see the racial composition of our clients as a direct demonstration of who is being left behind in the mental health system as it’s currently set up, as BIPOC individuals are represented to a greater degree in our clients than they are in the general population of Maryland. During our intake interview, we provide an opportunity for clients to share if there are certain characteristics they are looking for in a therapist – often black clients share that they would prefer to be matched with a black therapist or a therapist who has received specific training on working with black clients.”
While 13% of the American population is black, only 4% of physicians, 2% of psychiatrists, and 4% of psychologists are black. In her Psychology Today blog post, “Why African Americans Avoid Psychotherapy,” Monnica T. Williams, PhD, notes: “Apprehension about clashing with the values or worldview of the clinician can cause ambivalence about seeking help, and this may be especially true for the many who believe that mental health treatment was designed by white people for white people.” Dr. Williams notes that black Americans also are less likely to seek care because of increased stigma and fear of judgment, concerns about the treatment process, and fears of being involuntarily hospitalized, cost and lack of insurance, and finally logistical issues with work, transportation, and family responsibilities.
George Floyd’s tragic death has led us to a moment of crisis. It’s my hope that the dialogue is now galvanized to make meaningful changes toward fixing racial inequities. I am part of the problem and these conversations need to include more equitable access to psychiatric care.
My thanks to Rachel Donabedian and Gina Henderson for their help with this article.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Race is not something I’ve spent that much time contemplating. I grew up in Elizabeth, N.J., a city of just over 100,000, in the 1970s and attended public schools where people came in all shapes and colors; diversity came with the turf, it wasn’t something anyone needed to strive for.
My high school had more than 4,000 students with roughly even numbers of white, black, and Hispanic students. Armed police patrolled the halls, the thick aroma of weed settled in the stairwells and restrooms, girls brought their babies to school to show them off on half-days, and the “preppies” wore Fair Isle sweaters and played on the tennis team. The school’s campus was brand new and every lab, studio, and athletic amenity was state of the art; at the time, it was the most expensive public high school ever built in America. There were black teachers, librarians, and administrators, and segregation was something we read about in history books. I lived in a world of Technicolor and the Civil Rights movement of the 1960s, while still fresh in the minds of the adults, was something that showed up on black-and-white footage from another time.
My world became both wealthier and whiter when I went to college. There were minority students, but many of the black students at the University of Pennsylvania chose to live in the W.E.B. Du Bois College House.
People are often more comfortable being with others who share their backgrounds and this makes for an interesting conundrum: We all agree that desegregation is a good thing, but not everyone wishes to be told either where to go or not go, and there is an odd unbalance to creating a safe place for black students to be, one that both integrates and separates them from the larger community. Perhaps all our lines get fuzzy – I recall when I was on the Maryland Psychiatric Society Women’s Committee and a male psychiatrist signed up to join us – he was politely told that he could not join, but 20 years later, I’m wondering if it was okay to exclude a man who expressed interest in women’s issues.
In medical school, we were taught to note a patient’s age, race, and marital status, and we might learn that certain illnesses were more prevalent in certain populations, but there was no discussion of racial inequities in health care or anywhere else.
What was really different about the world back then, however, was what we didn’t see and what we didn’t talk about. Social media has opened a world where we can share our pain in the moment and we can band together to speak out against crimes and injustices in every realm. From the MeToo moments, to racially motivated police brutality. Cell phone cameras let us record and publicize these moments so the world can be the judge. George Floyd’s sadistic murder by a police officer, as other officers stood by and watched 8 minutes and 46 seconds of torture, left us all triggered, distressed, angry, sad, and activated. Maybe now we can make real progress on a discussion that began in 1992 with the videotape of Rodney King’s assault, a discussion we’ve had over and over to no avail.
Obviously, I have also been provoked by the events of the past weeks – like many Americans, I’ve paused to wonder how I can help the cause, both personally and as a psychiatrist. I would not normally write about racial topics – as a white woman I can listen, but I don’t feel this pain in the same way as someone who has lived with a lifetime of discrimination and oppression. Dr. Lorenzo Norris and Dr. Brandon Newsome,two black psychiatrists, put out a special edition of the MDEdge Psychcast, “The fallout from George Floyd’s death,” and Dr. Norris noted that two of his white colleagues told him they thought of checking on him, but they didn’t know what to say. Yes, I thought, that’s exactly it, I don’t know what to say and I worry that I might unintentionally say something that would worsen someone else’s pain. Staying silent has always seemed to be the safest option. With this article, I’m moving from a place of comfort.
I started my career with a mix of private practice and community psychiatry. There were things I loved about working in a community clinic: the social aspects of being part of a team, seeing a full range of psychopathology, and treating patients in which the racial and ethnic demographics mirrored that of the community. There were things I didn’t like, however. The pay was low, there were constant institutional requirements that were not relevant to the practice of psychiatry, and my relationship with the patients as their prescriber was much less fulfilling than the relationship I have with those I see for both psychotherapy and medication. Ultimately, the hospital shift to electronic medical records was the final distraction that caused me to leave community work.
Like roughly half of psychiatrists in private practice, I don’t participate with commercial or public insurance plans. Early in my career, I worked in a group setting with billing secretaries, and I did participate with Blue Cross, but even with administrative help, nothing about this was easy, and when I left to do solo practice, I left insurance participation behind. I love the autonomy of my career, I’m proud of the care I am able to give in this setting, and I don’t miss the hassles. But – the out-of-pocket cost of care is higher and the effort of trying to get reimbursed falls to the patient. It means that most of the patients I see have the means to pay for care, none are impoverished or homeless, and while I work in a city that is 62% black, black patients make up a small percentage of my caseload. I don’t think I am unique in this; I would be shocked if any white private practice psychiatrist who specializes in psychotherapy is serving a racially proportionate population. As we start to embrace the idea that people don’t neatly divide into being racist or not, and that bias affects us all, we must acknowledge that medical practices that don’t support racially balanced access to care are part of the problem.
Amy R. Greensfelder, LMSW, is the executive director of Maryland’s Pro Bono Counseling Project (PBCP), an organization that coordinates mental health professionals in private practice in Maryland to volunteer their services to those with limited resources. PBCP has found that 50% of those seeking services share that they are black or African American, and an additional 5% identify as multiracial. Of all of those seeking care approximately 65% are black, Indigenous, or People of Color (BIPOC), and and 14% are Latino/a/x/Hispanic. She says: “We see the racial composition of our clients as a direct demonstration of who is being left behind in the mental health system as it’s currently set up, as BIPOC individuals are represented to a greater degree in our clients than they are in the general population of Maryland. During our intake interview, we provide an opportunity for clients to share if there are certain characteristics they are looking for in a therapist – often black clients share that they would prefer to be matched with a black therapist or a therapist who has received specific training on working with black clients.”
While 13% of the American population is black, only 4% of physicians, 2% of psychiatrists, and 4% of psychologists are black. In her Psychology Today blog post, “Why African Americans Avoid Psychotherapy,” Monnica T. Williams, PhD, notes: “Apprehension about clashing with the values or worldview of the clinician can cause ambivalence about seeking help, and this may be especially true for the many who believe that mental health treatment was designed by white people for white people.” Dr. Williams notes that black Americans also are less likely to seek care because of increased stigma and fear of judgment, concerns about the treatment process, and fears of being involuntarily hospitalized, cost and lack of insurance, and finally logistical issues with work, transportation, and family responsibilities.
George Floyd’s tragic death has led us to a moment of crisis. It’s my hope that the dialogue is now galvanized to make meaningful changes toward fixing racial inequities. I am part of the problem and these conversations need to include more equitable access to psychiatric care.
My thanks to Rachel Donabedian and Gina Henderson for their help with this article.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.