User login
The SHM Fellow designation: Class of 2020
Society invites applicants in multiple membership categories
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Society invites applicants in multiple membership categories
Society invites applicants in multiple membership categories
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
In an industry brimming with opportunity and ongoing transformation, it is easy to feel indecisive about your next professional step when ample career paths exist in hospital medicine.
Yingkei Hui, MD, FHM, is an academic hospitalist at St. Vincent Indianapolis, and a Society of Hospital Medicine member since 2015. Seeking to set herself apart as an aspiring patient safety and quality improvement leader while continuing her professional development, she looked to SHM’s Fellow designation as the next piece of her career puzzle.
With more than 14 years of experience in the health care industry, Dr. Hui fell in love with the specialty because of its flexibility and patient-centric focus.
“I have a broad interest in medicine and want to learn everything under the larger umbrella of medicine,” she said. “I also find myself deeply in love with hospital medicine because it provides me with the opportunity to participate in various hospital committees and allows me to enjoy my practice from a macroscopic view of U.S. health care transformation – especially given the popular value-based patient care approach from recent years.”
Dr. Hui’s breadth of experience has allowed her to gain a unique set of perspectives and experiences from international and domestic standpoints. From attending medical school at the Chinese University of Hong Kong to completing her residency on the east coast at Pennsylvania Hospital in Philadelphia – part of the University of Pennsylvania Health System – Dr. Hui has held active medical licenses in New Jersey and currently, Indiana.
“SHM’s Fellow designation allows me to challenge myself in setting my career goal as a patient safety and quality improvement leader in my program,” she said. “It means a lot to me as it is a stand-out recognition of my participation in and contribution to patient care in my institution.”
When asked about the most rewarding aspect of being a part of the hospital medicine community, Dr. Hui identified “satisfaction in the teaching role.” She said she is “motivated by the holistic care for the patients, the integration of medical knowledge and coordination of care, and also the opportunity to conduct quality improvement projects.”
Motivated by her colleagues, Dr. Hui credits SHM with providing her with the inspiration and tools to push herself and advance her career in hospital medicine.
“I enjoy immersing myself in SHM’s patient safety and quality improvement resources; they are perfect for frontline hospitalists and also provide CME [continuing medical education],” she noted. “My previous medical directors were all Senior Fellows; they are my role models and continue to inspire me throughout my career.”
Dr. Hui also said that networking within the SHM community has been encouraging. “I’ve met talented Fellows at a number of hospital medicine annual conferences who have inspired me in the areas of patient care, education, and health promotion,” she explained. “Some of them have extensive publications; they are truly amazing physicians. SHM’s Annual Conference provides great opportunities for networking.”
As Dr. Hui continues to progress her career in hospital medicine, she believes that communication is a key pillar in her success. “Be a true listener and fill your heart with compassion, empathy, and courage,” she said. “Recognize your role as the enabler for the patients to improve their health.”
Completing her Master’s degree in population health management at Johns Hopkins University and expecting to graduate in May 2020, Dr. Hui is the designer of system safety (comprising patient safety, second victim safety, quality improvement, and just culture) in the academic setting of her residency program. She is also chairing a pioneer project for the St. Vincent IM residency program.
Dr. Hui plans to apply for a Senior Fellow designation with SHM in the future.
If you would like to join Dr. Hui and other like-minded hospital medicine leaders in taking your career to the next level, SHM is currently recruiting for the Fellows and Senior Fellows: Class of 2020. Applications are open until Nov. 29 of this year. These designations are available across a variety of membership categories, including physicians, nurse practitioners, physician assistants, and qualified practice administrators. Dedicated to promoting excellence, innovation, and improving the quality of patient care, Fellows designations provide members with a distinguishing credential as established pioneers in the industry.
For more information and to review your eligibility, visit hospitalmedicine.org/fellows.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
The growing NP and PA workforce in hospital medicine
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
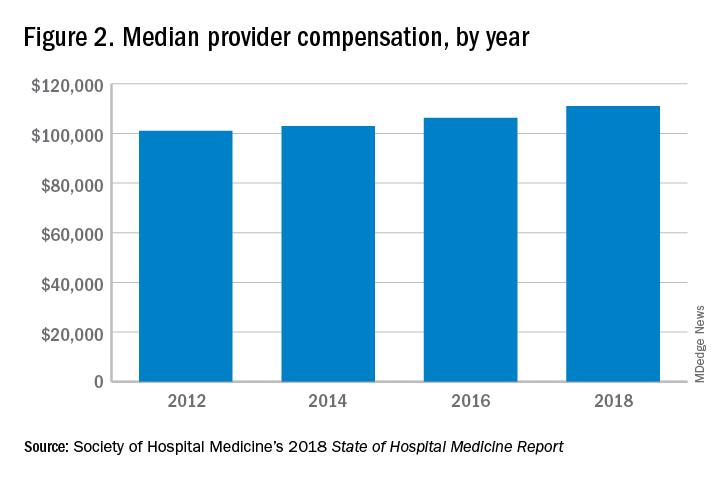
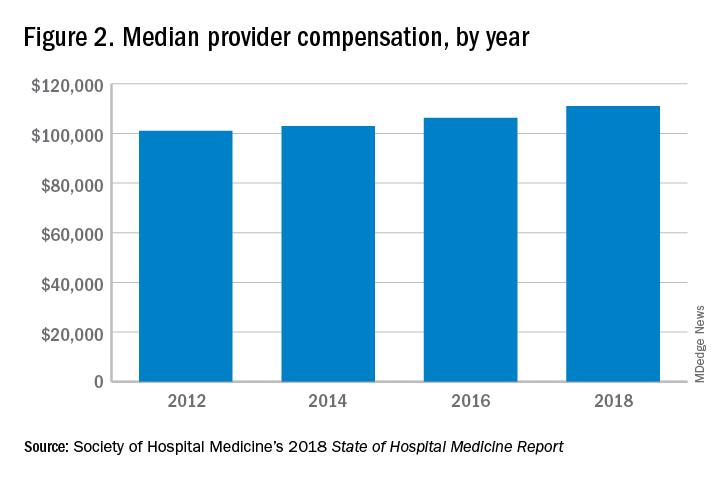
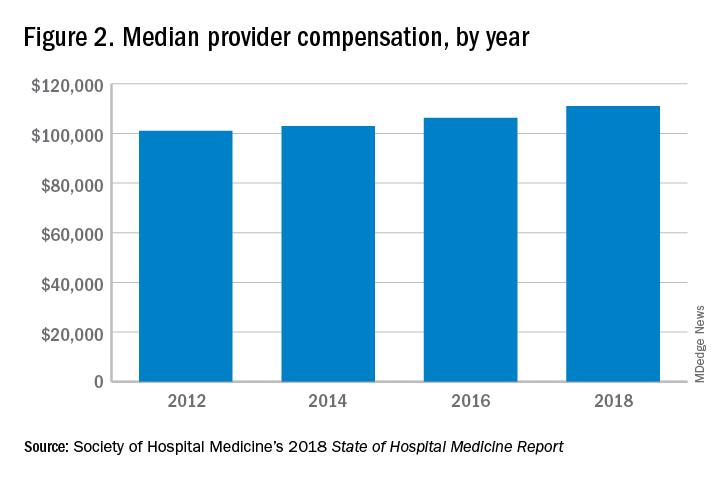
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.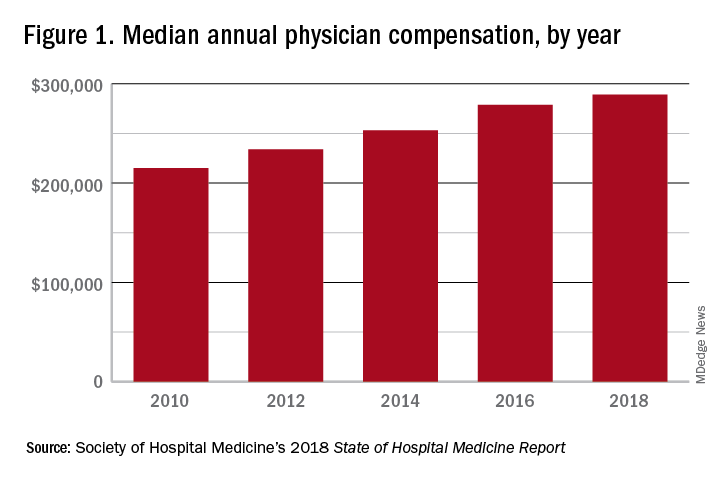
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.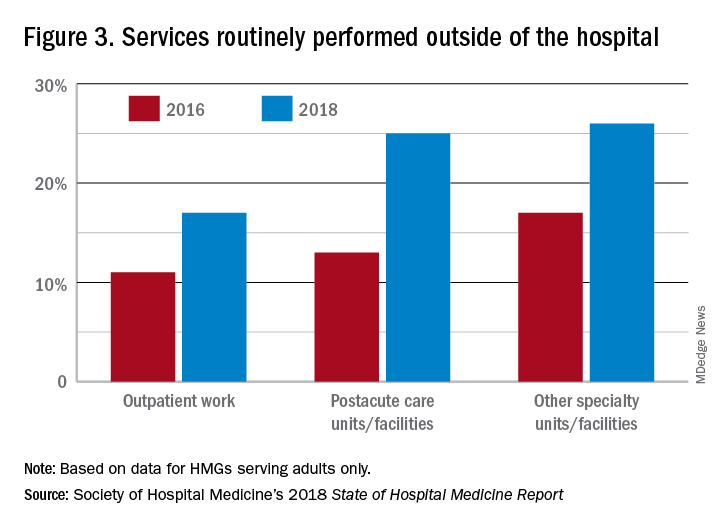
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
High rate of turnover among NPs, PAs
High rate of turnover among NPs, PAs
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.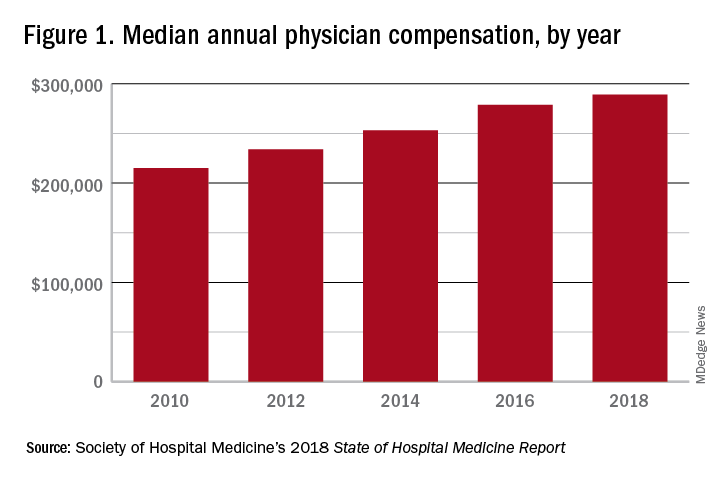
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.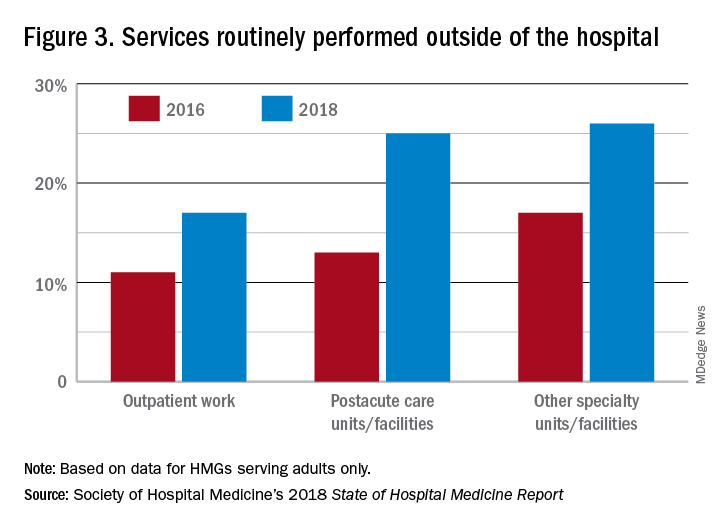
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
If you were a physician hospitalist in a group serving adults in 2017 you probably worked with nurse practitioners (NPs) and/or physician assistants (PAs). Seventy-seven percent of hospital medicine groups (HMGs) employed NPs and PAs that year.
In addition, the larger the group, the more likely the group was to have NPs and PAs as part of their practice model – 89% of hospital medicine groups with more than 30 physician had NPs and/or PAs as partners. In addition, the mean number of physicians for adult hospital medicine groups was 17.9. The same practices employed an average of 3.5 NPs, and 2.6 PAs.
Based on these numbers, there are just under three physicians per NP and PA in the typical HMG serving adults. This is all according to data from the 2018 State of Hospital Medicine (SoHM) report that was published in 2019 by the Society of Hospital Medicine.
These observations lead to a number of questions. One thing that is not clear from the SoHM is why NPs and PAs are becoming a larger part of the hospital medicine workforce, but there are some insights and conjecture that can be drawn from the data. The first is economics. Over 6 years, the median incomes of NPs and PAs have risen a relatively modest 10%; over the same period physician hospitalists have seen a whopping 23.6% median pay increase.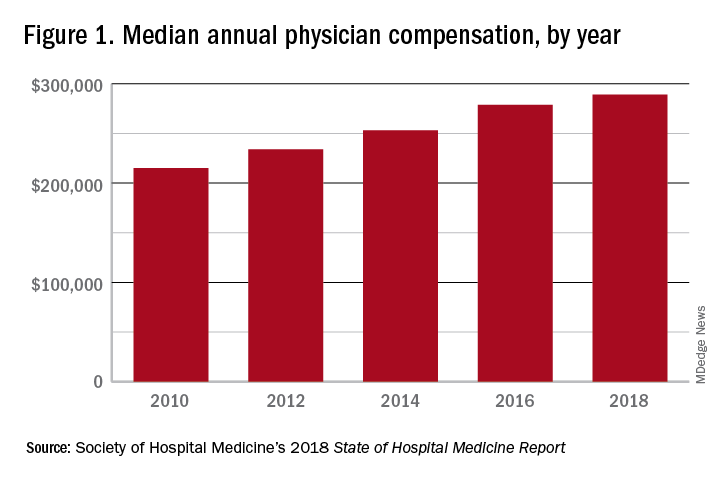
One argument against economics as a driving force behind greater use of NPs and PAs in the hospital medicine workforce is the billing patterns of HMGs that use NPs and PAs. Ten percent of HMGs do not have their NPs and PAs bill at all. The distribution of HMGs that predominantly bill NP and PA services as shared visits, versus having NPs and PAs bill independently, has also not changed much over the years, with 22% of HMGs having NPs and PAs bill independently as a predominant model. This would seem to suggest that some HMGs may not have learned how to deploy NPs and PAs effectively.
While inefficiency can be due to hospital bylaws, the culture of the hospital medicine group, or the skill set of the NPs and PAs working in HMGs – it would seem that if the driving force for the increase in the utilization of NPs and PAs in HMGs was financial, then that would also result in more of these providers billing independently, or alternatively, an increase in hospitalist physician productivity, which the data do not show. However, multistate HMGs may have this figured out better than some of the rest of us – 78% of these HMGs have NPs and PAs billing independently! All other categories of HMGs together are around 13%, with the next highest being hospital or health system integrated delivery systems, where NPs/PAs bill independently about 15% of the time.
In the last 2 years of the survey, there have been marked increases in the number of NPs and PAs at HMGs performing “nontraditional” services. For example, outpatient work has increased from 11% to 17%, and work in the postacute space has increased from 13% to 25%. Work in behavioral health and alcohol and drug rehab facilities has also increased, from 17% to 26%. As HMGs seek to rationalize their workforce while expanding, it is possible that decision makers have felt that it was either more economical to place NPs and PAs in positions where they are seeing these patients, or it was more aligned with the NP/PA skill set, or both. In any event, as the scope of hospital medicine broadens, the use of PAs and NPs has also increased – which is probably not coincidental.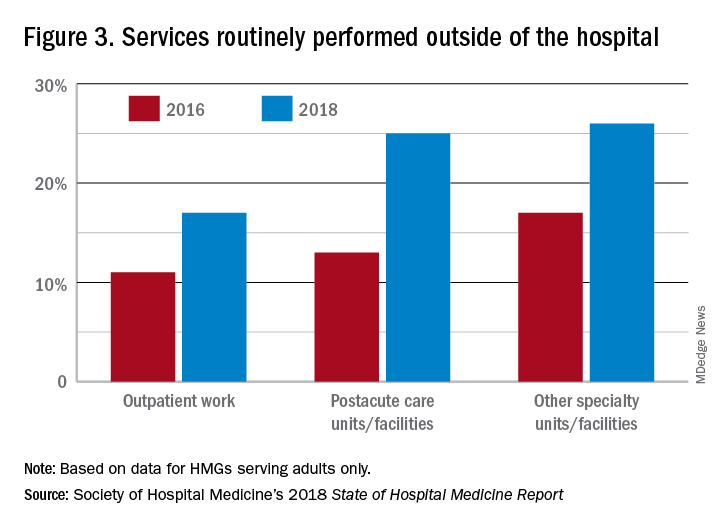
The average hospital medicine group continues to have staff openings. Workforce shortages may be leading to what in the past may have been considered physician openings being filled by NPs and PAs. Only 33% of HMGs reported having all their physician openings filled. Median physician shortage was 12% of total approved staffing. Given concerns in hospital medicine about provider burnout, the number of hospital medicine openings is no doubt a concern to HMG leaders and hospitalists. And necessity being the mother of invention, HMG leadership must be thinking differently than in the past about open positions and the skill mix needed to fill them. I believe this is leading to NPs and PAs being considered more often for a role that would have been open only to a physician in the past.
Just as open positions are a concern, so is turnover. One striking finding in the SoHM is the very high rate of turnover among NPs and PAs – a whopping 19.1% per year. For physicians, the same rate was 7.4% and has been declining every survey for many years. While NPs and PAs may be intended to stabilize the workforce, because of how this is being done in some groups, NPs and PAs may instead be a destabilizing factor. Rapid growth can lead to haphazard onboarding and less than clearly defined roles. NPs and PAs may often be placed into roles for which they are not yet prepared. In addition, the pay disparity between NPs and PAs and physicians has increased. As a new field, and with many HMGs still rapidly growing, increased thoughtfulness and maturity about how NPs and PAs are integrated into hospital medicine practices should lead to less turnover and better HMG stability in the future.
These observations could mark a future that includes higher pay for hospital medicine PAs and NPs (and potentially a slowdown in salary growth for physicians); HMGs taking steps to make the financial model more attractive by having NPs and PAs bill independently more often; and HMGs and their leaders engaging NPs and PAs by more clearly defining roles, shoring up onboarding and mentoring programs, and other measures that decrease turnover. This would help to make hospital medicine a career destination, rather than a stopping off point for NPs and PAs, much as it has become for internists over the past 20 years.
Dr. Frederickson is medical director, hospital medicine and palliative care, at CHI Health, Omaha, Neb., and assistant professor at Creighton University, Omaha.
i-HOPE study engages patients, families to improve quality of hospital stays
Make patients ‘equal members of the team.’
Hospitalization can be a challenging and vulnerable time for patients and their families. While challenges associated with the quality and safety of hospital care are well documented, perspectives of patients, families, caregivers, and other stakeholders are not as easily understood and are important targets of improvement research.
This led to the initiation of the i-HOPE Patient Engagement Study, a collaboration including the Society for Hospital Medicine’s Center for Quality Improvement. The team completed a systematic and broad engagement process with patients, families, and caregivers, followed by an in-person prioritization meeting to generate a priority list of research topics that describe the most important gaps in the care of hospitalized patients.
The Hospitalist recently spoke with Luci Leykum, MD, MSc, MBA, SFHM, principal investigator for the i-HOPE Study, professor of medicine and investigator in the South Texas Veterans Health Care System and incoming associate chair for clinical innovation at the University of Texas at Austin.
Why is it so important to include the perspective of the patient during a hospital stay?
We cannot optimally improve outcomes of hospitalized patients if we don’t have patients’ perspectives on what needs to be improved. Hearing these perspectives also provides insights into how we can address gaps in hospital care.
How were patients and other stakeholders engaged during the i-HOPE program?
Patients, caregivers, and stakeholders were engaged throughout the entire project, from conceptualization to dissemination of results.
We worked with seven patient partners to develop the proposal that we submitted to the Patient-Centered Outcomes Research Institute. They were involved in all phases of the project, from developing the informational webinars and surveys to analyzing our results.
We engaged additional patients, caregivers, and stakeholders to submit their highest priority unanswered research questions for improving hospital care. A total of 117 patients and 127 caregivers submitted questions. Our patient partners and more than 30 stakeholders were involved in prioritizing those research questions to develop our final agenda.
What is unique about the approach in the i-HOPE project, compared with other projects that may have had similar intended objectives?
Our project is unique in several respects. First, it was completely patient partnered. Having patients as equal members of the team changed our approach at every level – from how we communicated with patients and stakeholders to how we analyzed and presented our data. Second, we worked with a larger number of stakeholders representing a broad range of constituencies, from professional societies to health care delivery systems to payers.
How has SHM’s Center for Quality Improvement helped the i-HOPE program to realize its goals?
The Center for Quality Improvement helped considerably with the execution of the project. The researchers involved in i-HOPE were all members of the SHM Research Committee and were familiar with SHM’s capability as a partner in these larger-scale projects. The SHM Meetings team was instrumental in making our in-person patient and stakeholder prioritization meeting happen as well.
How can the findings of the i-HOPE program be applied?
We hope everyone can utilize our findings. Patients, families, and caregivers can use our results to improve their own care. Providers and delivery systems can target their improvement efforts using our findings to ensure that their work has the greatest impact on patients. Policy makers and funders can use our findings to direct work to the priority areas we identified. And finally, we hope the hospital research community uses our results to develop novel interventions to improve care.
For more information on the i-HOPE Patient Engagement Study, visit hospitalmedicine.org/ihope.
Make patients ‘equal members of the team.’
Make patients ‘equal members of the team.’
Hospitalization can be a challenging and vulnerable time for patients and their families. While challenges associated with the quality and safety of hospital care are well documented, perspectives of patients, families, caregivers, and other stakeholders are not as easily understood and are important targets of improvement research.
This led to the initiation of the i-HOPE Patient Engagement Study, a collaboration including the Society for Hospital Medicine’s Center for Quality Improvement. The team completed a systematic and broad engagement process with patients, families, and caregivers, followed by an in-person prioritization meeting to generate a priority list of research topics that describe the most important gaps in the care of hospitalized patients.
The Hospitalist recently spoke with Luci Leykum, MD, MSc, MBA, SFHM, principal investigator for the i-HOPE Study, professor of medicine and investigator in the South Texas Veterans Health Care System and incoming associate chair for clinical innovation at the University of Texas at Austin.
Why is it so important to include the perspective of the patient during a hospital stay?
We cannot optimally improve outcomes of hospitalized patients if we don’t have patients’ perspectives on what needs to be improved. Hearing these perspectives also provides insights into how we can address gaps in hospital care.
How were patients and other stakeholders engaged during the i-HOPE program?
Patients, caregivers, and stakeholders were engaged throughout the entire project, from conceptualization to dissemination of results.
We worked with seven patient partners to develop the proposal that we submitted to the Patient-Centered Outcomes Research Institute. They were involved in all phases of the project, from developing the informational webinars and surveys to analyzing our results.
We engaged additional patients, caregivers, and stakeholders to submit their highest priority unanswered research questions for improving hospital care. A total of 117 patients and 127 caregivers submitted questions. Our patient partners and more than 30 stakeholders were involved in prioritizing those research questions to develop our final agenda.
What is unique about the approach in the i-HOPE project, compared with other projects that may have had similar intended objectives?
Our project is unique in several respects. First, it was completely patient partnered. Having patients as equal members of the team changed our approach at every level – from how we communicated with patients and stakeholders to how we analyzed and presented our data. Second, we worked with a larger number of stakeholders representing a broad range of constituencies, from professional societies to health care delivery systems to payers.
How has SHM’s Center for Quality Improvement helped the i-HOPE program to realize its goals?
The Center for Quality Improvement helped considerably with the execution of the project. The researchers involved in i-HOPE were all members of the SHM Research Committee and were familiar with SHM’s capability as a partner in these larger-scale projects. The SHM Meetings team was instrumental in making our in-person patient and stakeholder prioritization meeting happen as well.
How can the findings of the i-HOPE program be applied?
We hope everyone can utilize our findings. Patients, families, and caregivers can use our results to improve their own care. Providers and delivery systems can target their improvement efforts using our findings to ensure that their work has the greatest impact on patients. Policy makers and funders can use our findings to direct work to the priority areas we identified. And finally, we hope the hospital research community uses our results to develop novel interventions to improve care.
For more information on the i-HOPE Patient Engagement Study, visit hospitalmedicine.org/ihope.
Hospitalization can be a challenging and vulnerable time for patients and their families. While challenges associated with the quality and safety of hospital care are well documented, perspectives of patients, families, caregivers, and other stakeholders are not as easily understood and are important targets of improvement research.
This led to the initiation of the i-HOPE Patient Engagement Study, a collaboration including the Society for Hospital Medicine’s Center for Quality Improvement. The team completed a systematic and broad engagement process with patients, families, and caregivers, followed by an in-person prioritization meeting to generate a priority list of research topics that describe the most important gaps in the care of hospitalized patients.
The Hospitalist recently spoke with Luci Leykum, MD, MSc, MBA, SFHM, principal investigator for the i-HOPE Study, professor of medicine and investigator in the South Texas Veterans Health Care System and incoming associate chair for clinical innovation at the University of Texas at Austin.
Why is it so important to include the perspective of the patient during a hospital stay?
We cannot optimally improve outcomes of hospitalized patients if we don’t have patients’ perspectives on what needs to be improved. Hearing these perspectives also provides insights into how we can address gaps in hospital care.
How were patients and other stakeholders engaged during the i-HOPE program?
Patients, caregivers, and stakeholders were engaged throughout the entire project, from conceptualization to dissemination of results.
We worked with seven patient partners to develop the proposal that we submitted to the Patient-Centered Outcomes Research Institute. They were involved in all phases of the project, from developing the informational webinars and surveys to analyzing our results.
We engaged additional patients, caregivers, and stakeholders to submit their highest priority unanswered research questions for improving hospital care. A total of 117 patients and 127 caregivers submitted questions. Our patient partners and more than 30 stakeholders were involved in prioritizing those research questions to develop our final agenda.
What is unique about the approach in the i-HOPE project, compared with other projects that may have had similar intended objectives?
Our project is unique in several respects. First, it was completely patient partnered. Having patients as equal members of the team changed our approach at every level – from how we communicated with patients and stakeholders to how we analyzed and presented our data. Second, we worked with a larger number of stakeholders representing a broad range of constituencies, from professional societies to health care delivery systems to payers.
How has SHM’s Center for Quality Improvement helped the i-HOPE program to realize its goals?
The Center for Quality Improvement helped considerably with the execution of the project. The researchers involved in i-HOPE were all members of the SHM Research Committee and were familiar with SHM’s capability as a partner in these larger-scale projects. The SHM Meetings team was instrumental in making our in-person patient and stakeholder prioritization meeting happen as well.
How can the findings of the i-HOPE program be applied?
We hope everyone can utilize our findings. Patients, families, and caregivers can use our results to improve their own care. Providers and delivery systems can target their improvement efforts using our findings to ensure that their work has the greatest impact on patients. Policy makers and funders can use our findings to direct work to the priority areas we identified. And finally, we hope the hospital research community uses our results to develop novel interventions to improve care.
For more information on the i-HOPE Patient Engagement Study, visit hospitalmedicine.org/ihope.
Flying toward equity and inclusion
Diversity is a ‘team sport’
These are challenging, and sometimes tragic, times in the history of the United States. The image of a father and child face down in the Rio Grande River, drowning as they tried to cross from Mexico into Texas, is heart breaking. Irrespective of your political affiliation, we can agree that the immigration process is far from ideal and that no one should die in pursuit of a better life.
The United States has a complicated history with equity and inclusion, for all persons, and we are now living in times when the scab is being ripped off and these wounds are raw. What role can the Society of Hospital Medicine play to help heal these wounds?
I am a first-generation immigrant to the United States. I remember walking down the streets of my neighborhood in Uganda when my attention was drawn to a plane flying overhead. I thought to myself, “Some lucky duck is going to the U.S.” The United States was the land of opportunity and I was determined to come here. Through hard work and some luck, I arrived in the United States on June 15, 1991, with a single suitcase packed full of hope, dreams, and $3,000.
Fast-forward 28 years. I am now a hospitalist and faculty at the Johns Hopkins University, Baltimore, the associate director of the division of hospital medicine, and the vice chair for clinical operations at Johns Hopkins Bayview Medical Center. I learned about hospital medicine during my third year of medical school at the University of Minnesota, Minneapolis. While I loved general medicine, I could not see myself practicing anywhere outside of the hospital.
Following residency at Johns Hopkins Bayview, I still felt that a hospital-based practice was tailor-made for me. As I matured professionally, I worked to improve the provision of care within my hospital, and then started developing educational and practice programs in hospital medicine, both locally and internationally. My passion for hospital medicine led me to serve on committees for SHM, and this year, I was honored to join the SHM Board of Directors.
It is hard to answer the question of why, or how, one person immigrates to the United States and finds success while another loses their life. A quote attributed to Edmund Burke says, “the only thing necessary for the triumph of evil is for good [wo]men to do nothing.” One of SHM’s core values is to promote diversity and inclusion. A major step taken by the society to promote work in this area was to establish the diversity and inclusion Special Interest Group in 2018. I am the board liaison for the diversity and inclusion SIG and will work alongside this group, which aims to:
- Foster diversity, equity, and inclusion in SHM.
- Increase visibility of diversity, equity, and inclusion to the broader hospital medicine community.
- Support hospital medicine groups in matching their work forces to their diverse patient populations.
- Develop tool kits to improve the provision of care for our diverse patient population.
- Engender diversity among hospitalists.
- Develop opportunities for expanding the fund of knowledge on diversity in hospital medicine through research and discovery.
- Participate in SHM’s advocacy efforts related to diversity and inclusion.
- Develop partnerships with other key organizations to advance diversity, equity, and inclusion platforms so as to increase the scalability of SHM’s efforts.
We have been successful at Hopkins with diversity and inclusion, but that did not occur by chance. I believe that diversity and inclusion is a team sport and that everyone can be an important part of that team. In my hospitalist group, we actively engage women, men, doctors, NPs, PAs, administrators, minorities, and nonminorities. We recruit to – and cherish members of – our group irrespective of religious beliefs or sexual orientation. We believe that a heterogeneous group of people leads to an engaged and high-performing culture.
I have traveled a convoluted path since my arrival in 1991. Along the way, I was blessed with a husband and son who anchor me. Every day they remind me that the hard work I do is to build on the past to improve the future. My husband, an immigrant from Uganda like me, reminds me that we are lucky to have made it to the United States and that the ability and freedom to work hard and be rewarded for that hard work is a great privilege. My son reminds me of the many other children who look at me and know that they too can dare to dream. Occasionally, I still look up and see a plane, and I am reminded of that day many years ago. Hospital medicine is my suitcase packed with hopes and dreams for me, for this specialty, and for this country.
Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview and assistant professor at Johns Hopkins University, both in Baltimore, and a member of the SHM Board of Directors.
Diversity is a ‘team sport’
Diversity is a ‘team sport’
These are challenging, and sometimes tragic, times in the history of the United States. The image of a father and child face down in the Rio Grande River, drowning as they tried to cross from Mexico into Texas, is heart breaking. Irrespective of your political affiliation, we can agree that the immigration process is far from ideal and that no one should die in pursuit of a better life.
The United States has a complicated history with equity and inclusion, for all persons, and we are now living in times when the scab is being ripped off and these wounds are raw. What role can the Society of Hospital Medicine play to help heal these wounds?
I am a first-generation immigrant to the United States. I remember walking down the streets of my neighborhood in Uganda when my attention was drawn to a plane flying overhead. I thought to myself, “Some lucky duck is going to the U.S.” The United States was the land of opportunity and I was determined to come here. Through hard work and some luck, I arrived in the United States on June 15, 1991, with a single suitcase packed full of hope, dreams, and $3,000.
Fast-forward 28 years. I am now a hospitalist and faculty at the Johns Hopkins University, Baltimore, the associate director of the division of hospital medicine, and the vice chair for clinical operations at Johns Hopkins Bayview Medical Center. I learned about hospital medicine during my third year of medical school at the University of Minnesota, Minneapolis. While I loved general medicine, I could not see myself practicing anywhere outside of the hospital.
Following residency at Johns Hopkins Bayview, I still felt that a hospital-based practice was tailor-made for me. As I matured professionally, I worked to improve the provision of care within my hospital, and then started developing educational and practice programs in hospital medicine, both locally and internationally. My passion for hospital medicine led me to serve on committees for SHM, and this year, I was honored to join the SHM Board of Directors.
It is hard to answer the question of why, or how, one person immigrates to the United States and finds success while another loses their life. A quote attributed to Edmund Burke says, “the only thing necessary for the triumph of evil is for good [wo]men to do nothing.” One of SHM’s core values is to promote diversity and inclusion. A major step taken by the society to promote work in this area was to establish the diversity and inclusion Special Interest Group in 2018. I am the board liaison for the diversity and inclusion SIG and will work alongside this group, which aims to:
- Foster diversity, equity, and inclusion in SHM.
- Increase visibility of diversity, equity, and inclusion to the broader hospital medicine community.
- Support hospital medicine groups in matching their work forces to their diverse patient populations.
- Develop tool kits to improve the provision of care for our diverse patient population.
- Engender diversity among hospitalists.
- Develop opportunities for expanding the fund of knowledge on diversity in hospital medicine through research and discovery.
- Participate in SHM’s advocacy efforts related to diversity and inclusion.
- Develop partnerships with other key organizations to advance diversity, equity, and inclusion platforms so as to increase the scalability of SHM’s efforts.
We have been successful at Hopkins with diversity and inclusion, but that did not occur by chance. I believe that diversity and inclusion is a team sport and that everyone can be an important part of that team. In my hospitalist group, we actively engage women, men, doctors, NPs, PAs, administrators, minorities, and nonminorities. We recruit to – and cherish members of – our group irrespective of religious beliefs or sexual orientation. We believe that a heterogeneous group of people leads to an engaged and high-performing culture.
I have traveled a convoluted path since my arrival in 1991. Along the way, I was blessed with a husband and son who anchor me. Every day they remind me that the hard work I do is to build on the past to improve the future. My husband, an immigrant from Uganda like me, reminds me that we are lucky to have made it to the United States and that the ability and freedom to work hard and be rewarded for that hard work is a great privilege. My son reminds me of the many other children who look at me and know that they too can dare to dream. Occasionally, I still look up and see a plane, and I am reminded of that day many years ago. Hospital medicine is my suitcase packed with hopes and dreams for me, for this specialty, and for this country.
Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview and assistant professor at Johns Hopkins University, both in Baltimore, and a member of the SHM Board of Directors.
These are challenging, and sometimes tragic, times in the history of the United States. The image of a father and child face down in the Rio Grande River, drowning as they tried to cross from Mexico into Texas, is heart breaking. Irrespective of your political affiliation, we can agree that the immigration process is far from ideal and that no one should die in pursuit of a better life.
The United States has a complicated history with equity and inclusion, for all persons, and we are now living in times when the scab is being ripped off and these wounds are raw. What role can the Society of Hospital Medicine play to help heal these wounds?
I am a first-generation immigrant to the United States. I remember walking down the streets of my neighborhood in Uganda when my attention was drawn to a plane flying overhead. I thought to myself, “Some lucky duck is going to the U.S.” The United States was the land of opportunity and I was determined to come here. Through hard work and some luck, I arrived in the United States on June 15, 1991, with a single suitcase packed full of hope, dreams, and $3,000.
Fast-forward 28 years. I am now a hospitalist and faculty at the Johns Hopkins University, Baltimore, the associate director of the division of hospital medicine, and the vice chair for clinical operations at Johns Hopkins Bayview Medical Center. I learned about hospital medicine during my third year of medical school at the University of Minnesota, Minneapolis. While I loved general medicine, I could not see myself practicing anywhere outside of the hospital.
Following residency at Johns Hopkins Bayview, I still felt that a hospital-based practice was tailor-made for me. As I matured professionally, I worked to improve the provision of care within my hospital, and then started developing educational and practice programs in hospital medicine, both locally and internationally. My passion for hospital medicine led me to serve on committees for SHM, and this year, I was honored to join the SHM Board of Directors.
It is hard to answer the question of why, or how, one person immigrates to the United States and finds success while another loses their life. A quote attributed to Edmund Burke says, “the only thing necessary for the triumph of evil is for good [wo]men to do nothing.” One of SHM’s core values is to promote diversity and inclusion. A major step taken by the society to promote work in this area was to establish the diversity and inclusion Special Interest Group in 2018. I am the board liaison for the diversity and inclusion SIG and will work alongside this group, which aims to:
- Foster diversity, equity, and inclusion in SHM.
- Increase visibility of diversity, equity, and inclusion to the broader hospital medicine community.
- Support hospital medicine groups in matching their work forces to their diverse patient populations.
- Develop tool kits to improve the provision of care for our diverse patient population.
- Engender diversity among hospitalists.
- Develop opportunities for expanding the fund of knowledge on diversity in hospital medicine through research and discovery.
- Participate in SHM’s advocacy efforts related to diversity and inclusion.
- Develop partnerships with other key organizations to advance diversity, equity, and inclusion platforms so as to increase the scalability of SHM’s efforts.
We have been successful at Hopkins with diversity and inclusion, but that did not occur by chance. I believe that diversity and inclusion is a team sport and that everyone can be an important part of that team. In my hospitalist group, we actively engage women, men, doctors, NPs, PAs, administrators, minorities, and nonminorities. We recruit to – and cherish members of – our group irrespective of religious beliefs or sexual orientation. We believe that a heterogeneous group of people leads to an engaged and high-performing culture.
I have traveled a convoluted path since my arrival in 1991. Along the way, I was blessed with a husband and son who anchor me. Every day they remind me that the hard work I do is to build on the past to improve the future. My husband, an immigrant from Uganda like me, reminds me that we are lucky to have made it to the United States and that the ability and freedom to work hard and be rewarded for that hard work is a great privilege. My son reminds me of the many other children who look at me and know that they too can dare to dream. Occasionally, I still look up and see a plane, and I am reminded of that day many years ago. Hospital medicine is my suitcase packed with hopes and dreams for me, for this specialty, and for this country.
Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview and assistant professor at Johns Hopkins University, both in Baltimore, and a member of the SHM Board of Directors.
SHM and Jefferson College of Population Health partner to provide vital education for hospitalists
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.
Both the Society of Hospital Medicine and Jefferson College of Population Health, of Thomas Jefferson University in Philadelphia, share a goal to educate physicians to be effective leaders and managers in the pursuit of health care quality, safety, and population health, and they have entered into a partnership with this in mind.
Alexis Skoufalos, EdD, associate dean, strategic development, for Jefferson College of Population Health, recently spoke with The Hospitalist to discuss the importance of population health to hospital medicine professionals, the health care landscape as a whole, and the benefits of this new partnership with SHM.
Can you explain the importance of population health in the current health care landscape?
Many people confuse population health with public health. While they are related, they are different disciplines. Public health focuses on prevention and health promotion (clean water, vaccines, exercise, using seat belts, and so on), but it stops there.
Population health builds on the foundation of public health and goes a step further, working to connect health and health care delivery. It takes a more holistic approach, looking at what we need to do inside and outside the delivery system to help people to get and stay healthy, as well as take better care of them when they do get sick.
We work to identify and understand the health impact of social and environmental factors, while also looking for ways to make health care delivery safer, better, and more affordable and accessible.
This can get complicated. It involves sorting through lots of information to uncover the best way to meet the needs of a specific group, whether that is a community, a neighborhood, or a patient with a particular condition.
It’s about taking the time to really look at things from different vantage points. You won’t see the same view if you are looking at something through a telescope as you would looking through a microscope. That information can help you to adjust your perspective to identify the best course of action.
In order to be successful in improving population health, providers need to understand how to work with the other stakeholders in the health care ecosystem. Collaboration and coordination are the best ways to optimize the resources available.
It is important for delivery systems to establish good working relationships with community nonprofit and service organizations, faith-based organizations, social service providers, school systems, and federal, state, and local government.
At Jefferson, we thought it was important to create a college and programs that would prepare professionals across the workforce for this new challenge.
How did this partnership between SHM and Jefferson College of Population Health come to fruition?
Hospitalists are an important link with a person’s primary care team. The work they do to prepare a person and their family for successful discharge to the community after a hospital stay can make all the difference in a person’s recovery, condition management, and preventing readmission to the hospital.
Because both of our organizations are based in Philadelphia, we have had longstanding connections with SHM leadership. It was only natural for us to talk with SHM about how we can build upon the society’s excellent continuing education offerings and work together to provide members with additional content that can equip them to advance their careers.
How did SHM and Jefferson College of Population Health identify the mutually beneficial educational offerings in each institution that are included in this partnership?
Members of our respective leadership teams got together to complete a detailed review of the offerings from each organization. SHM’s Leadership Academy and JCPH’s Population Health Academy are rigorous continuing education programs that can provide physicians with excellent just-in-time information they can put to use right away.
After a careful examination of the curriculum, JCPH determined that SHM members can apply the credits they earn from completing two qualified sessions from the Leadership Academy to satisfy the elective course requirement for a Master’s degree. (Note: This does not apply to the Population Health Intelligence Program, which does not include an elective course.)
How will this partnership benefit Jefferson College of Population Health?
Our mission is to prepare health care leaders with the skills and tools they need to be effective in improving population health. Clinicians who work in a hospital setting have a key role to play.
We are also dedicated to making a difference right here in Philadelphia. The more students we have in our programs, the more of an impact we (and they) will have in improving outcomes in our own community.
We need to move the needle and get Philadelphia County out of the basement in terms of health rankings. We have a responsibility to do what we can to make a difference, and we appreciate the partnership with SHM to make it happen.
What other components of the partnership are especially noteworthy to highlight?
In addition to what I’ve already discussed, the following are some of the significant benefits that SHM members are entitled to as a result of the partnership with JCPH:
- 15% discount on tuition for any JCPH online graduate degree program.
- Registration discount for JCPH’s Population Health Academy in Philadelphia.
- Special registration rate for Annual Population Health Colloquium.
For more information about this partnership, visit hospitalmedicine.org/jefferson.
Hospitalist movers and shakers – September 2019
Mark Williams, MD, MHM, FACP, recently was appointed chief quality and transformation officer for the University of Kentucky’s UK HealthCare (Lexington). Dr. Williams, a tenured professor in the division of hospital medicine at the UK College of Medicine, will serve as chair of UK HealthCare’s Executive Quality Committee. Dr. Williams will lead integration of quality improvement, safety, and quality reporting with data analytics.
Dr. Williams established the first hospitalist program at a public hospital (Grady Memorial Hospital) and academic hospitalist programs at Emory University, Northwestern University, and UK HealthCare. An inaugural member of SHM, he is a past president, was the founding editor-in-chief of the Journal of Hospital Medicine and led SHM’s Project BOOST.
Also at UK HealthCare, Romil Chadha, MD, MPH, SFHM, FACP, has been named interim chief of the division of hospital medicine and medical director of Physician Information Technology Services. Previously, he was associate chief of the division of hospital medicine, and he also serves as medical director of telemetry.
Dr. Chadha is the founder of the Kentucky chapter of SHM, where he is the immediate past president. He is also the codirector of the Heartland Hospital Medicine Conference.
Amit Vashist, MD, MBA, CPE, FHM, FACP, FAPA, has been named chief clinical officer at Ballad Health, a 21-hospital health system in Northeast Tennessee, Southwest Virginia, Northwest North Carolina, and Southeast Kentucky.
In his new role, he will focus on clinical quality, value-based initiatives to improve quality while reducing cost of care, performance improvement, oversight of the clinical delivery of care and will be the liaison to the Ballad Health Clinical Council. Dr. Vashist is a member of The Hospitalist’s editorial advisory board.
Nagendra Gupta, MD, FACP, CPE, has been appointed to the American Board of Internal Medicine’s Internal Medicine Specialty Board. ABIM Specialty Boards are responsible for the broad definition of the discipline across Certification and Maintenance of Certification (MOC). Specialty Board members work with physicians and medical societies to develop Certification and MOC credentials to recognize physicians for their specialized knowledge and commitment to staying current in their field.
Dr. Gupta is a full-time practicing hospitalist with Apogee Physicians and currently serves as the director of the hospitalist program at Texas Health Arlington (Tex.) Memorial Hospital. He also serves as vice president for SHM’s North Central Texas Chapter.
T. Steen Trawick Jr., MD, was named the CEO of Christus Shreveport-Bossier Health System in Shreveport, La., in August 2019.
Dr. Trawick has worked for Christus as a pediatric hospitalist since 2005 and most recently has served concurrently as associate chief medical officer for Sound Physicians. Through Sound Physicians, Dr. Trawick oversees the hospitalist and emergency medical programs for Christus and other hospitals – 14 in total – in Texas and Louisiana. He has worked in that role for the past 6 years.
Scott Shepherd, DO, FACP, has been selected chief medical officer of the health data enrichment and integration technology company Verinovum in Tulsa, Okla. Dr. Shepherd is the medical director for hospitalist medicine and a practicing hospitalist with St. John Health System in Tulsa, and also medical director of the Center for Health Systems Innovation at his alma mater, Oklahoma State University in Stillwater.
Amanda Logue, MD, has been elevated to chief medical officer at Lafayette (La.) General Hospital. Dr. Logue assumed her role in May 2019, which includes the title of senior vice president.
Dr. Logue has worked at Lafayette General since 2009. A hospitalist/internist, her duties at the facility have included department chair of medicine, physician champion for electronic medical record implementation, medical director of the hospitalist program, and most recently chief medical information officer.
Rina Bansal, MD, MBA, recently was appointed full-time president of Inova Alexandria (Va.) Hospital, taking the reins officially after serving as acting president since November 2018. Dr. Bansal has been at Inova since 2008, when she started as a hospitalist at Inova Fairfax (Va.).
Dr. Bansal created and led Inova’s Clinical Nurse Services Hospitalist program through its department of neurosciences and has done stints as Inova Fairfax’s associate chief medical officer, medical director of Inova Telemedicine, and chief medical officer at Inova Alexandria.
James Napoli, MD, has been named chief medical officer for Blue Cross and Blue Shield of Arizona (BCBSAZ). He has manned the CMO position in an interim role since March, taking those duties on top of his role as BCBSAZ’s enterprise medical director for health care ventures and innovation.
Dr. Napoli came to BCBSAZ in 2013 after more than a decade at Abrazo Arrowhead Campus (Glendale, Ariz.) At Abrazo, he was director of hospitalist services and vice-chief of staff, on top of his efforts as a practicing hospital medicine clinician.
Dr. Napoli was previously medical director at OptumHealth, working specifically in the medical management and quality improvement areas for the health management solutions organization’s Medicare Advantage clients.
Mercy Hospital Fort Smith (Ark.) has partnered with the Ob Hospitalist Group (Greenville, S.C.) to launch an obstetric hospitalist program. OB hospitalists deliver babies when a patient’s physician cannot be present, provide emergency care, and provide support to high-risk pregnancy patients, among other duties within the hospital.
The partnership has allowed Mercy Fort Smith to create a dedicated, four-room obstetric emergency department in its Mercy Childbirth Center. Eight OB hospitalists have been hired and will provide care 24 hours a day, 7 days a week.
Mark Williams, MD, MHM, FACP, recently was appointed chief quality and transformation officer for the University of Kentucky’s UK HealthCare (Lexington). Dr. Williams, a tenured professor in the division of hospital medicine at the UK College of Medicine, will serve as chair of UK HealthCare’s Executive Quality Committee. Dr. Williams will lead integration of quality improvement, safety, and quality reporting with data analytics.
Dr. Williams established the first hospitalist program at a public hospital (Grady Memorial Hospital) and academic hospitalist programs at Emory University, Northwestern University, and UK HealthCare. An inaugural member of SHM, he is a past president, was the founding editor-in-chief of the Journal of Hospital Medicine and led SHM’s Project BOOST.
Also at UK HealthCare, Romil Chadha, MD, MPH, SFHM, FACP, has been named interim chief of the division of hospital medicine and medical director of Physician Information Technology Services. Previously, he was associate chief of the division of hospital medicine, and he also serves as medical director of telemetry.
Dr. Chadha is the founder of the Kentucky chapter of SHM, where he is the immediate past president. He is also the codirector of the Heartland Hospital Medicine Conference.
Amit Vashist, MD, MBA, CPE, FHM, FACP, FAPA, has been named chief clinical officer at Ballad Health, a 21-hospital health system in Northeast Tennessee, Southwest Virginia, Northwest North Carolina, and Southeast Kentucky.
In his new role, he will focus on clinical quality, value-based initiatives to improve quality while reducing cost of care, performance improvement, oversight of the clinical delivery of care and will be the liaison to the Ballad Health Clinical Council. Dr. Vashist is a member of The Hospitalist’s editorial advisory board.
Nagendra Gupta, MD, FACP, CPE, has been appointed to the American Board of Internal Medicine’s Internal Medicine Specialty Board. ABIM Specialty Boards are responsible for the broad definition of the discipline across Certification and Maintenance of Certification (MOC). Specialty Board members work with physicians and medical societies to develop Certification and MOC credentials to recognize physicians for their specialized knowledge and commitment to staying current in their field.
Dr. Gupta is a full-time practicing hospitalist with Apogee Physicians and currently serves as the director of the hospitalist program at Texas Health Arlington (Tex.) Memorial Hospital. He also serves as vice president for SHM’s North Central Texas Chapter.
T. Steen Trawick Jr., MD, was named the CEO of Christus Shreveport-Bossier Health System in Shreveport, La., in August 2019.
Dr. Trawick has worked for Christus as a pediatric hospitalist since 2005 and most recently has served concurrently as associate chief medical officer for Sound Physicians. Through Sound Physicians, Dr. Trawick oversees the hospitalist and emergency medical programs for Christus and other hospitals – 14 in total – in Texas and Louisiana. He has worked in that role for the past 6 years.
Scott Shepherd, DO, FACP, has been selected chief medical officer of the health data enrichment and integration technology company Verinovum in Tulsa, Okla. Dr. Shepherd is the medical director for hospitalist medicine and a practicing hospitalist with St. John Health System in Tulsa, and also medical director of the Center for Health Systems Innovation at his alma mater, Oklahoma State University in Stillwater.
Amanda Logue, MD, has been elevated to chief medical officer at Lafayette (La.) General Hospital. Dr. Logue assumed her role in May 2019, which includes the title of senior vice president.
Dr. Logue has worked at Lafayette General since 2009. A hospitalist/internist, her duties at the facility have included department chair of medicine, physician champion for electronic medical record implementation, medical director of the hospitalist program, and most recently chief medical information officer.
Rina Bansal, MD, MBA, recently was appointed full-time president of Inova Alexandria (Va.) Hospital, taking the reins officially after serving as acting president since November 2018. Dr. Bansal has been at Inova since 2008, when she started as a hospitalist at Inova Fairfax (Va.).
Dr. Bansal created and led Inova’s Clinical Nurse Services Hospitalist program through its department of neurosciences and has done stints as Inova Fairfax’s associate chief medical officer, medical director of Inova Telemedicine, and chief medical officer at Inova Alexandria.
James Napoli, MD, has been named chief medical officer for Blue Cross and Blue Shield of Arizona (BCBSAZ). He has manned the CMO position in an interim role since March, taking those duties on top of his role as BCBSAZ’s enterprise medical director for health care ventures and innovation.
Dr. Napoli came to BCBSAZ in 2013 after more than a decade at Abrazo Arrowhead Campus (Glendale, Ariz.) At Abrazo, he was director of hospitalist services and vice-chief of staff, on top of his efforts as a practicing hospital medicine clinician.
Dr. Napoli was previously medical director at OptumHealth, working specifically in the medical management and quality improvement areas for the health management solutions organization’s Medicare Advantage clients.
Mercy Hospital Fort Smith (Ark.) has partnered with the Ob Hospitalist Group (Greenville, S.C.) to launch an obstetric hospitalist program. OB hospitalists deliver babies when a patient’s physician cannot be present, provide emergency care, and provide support to high-risk pregnancy patients, among other duties within the hospital.
The partnership has allowed Mercy Fort Smith to create a dedicated, four-room obstetric emergency department in its Mercy Childbirth Center. Eight OB hospitalists have been hired and will provide care 24 hours a day, 7 days a week.
Mark Williams, MD, MHM, FACP, recently was appointed chief quality and transformation officer for the University of Kentucky’s UK HealthCare (Lexington). Dr. Williams, a tenured professor in the division of hospital medicine at the UK College of Medicine, will serve as chair of UK HealthCare’s Executive Quality Committee. Dr. Williams will lead integration of quality improvement, safety, and quality reporting with data analytics.
Dr. Williams established the first hospitalist program at a public hospital (Grady Memorial Hospital) and academic hospitalist programs at Emory University, Northwestern University, and UK HealthCare. An inaugural member of SHM, he is a past president, was the founding editor-in-chief of the Journal of Hospital Medicine and led SHM’s Project BOOST.
Also at UK HealthCare, Romil Chadha, MD, MPH, SFHM, FACP, has been named interim chief of the division of hospital medicine and medical director of Physician Information Technology Services. Previously, he was associate chief of the division of hospital medicine, and he also serves as medical director of telemetry.
Dr. Chadha is the founder of the Kentucky chapter of SHM, where he is the immediate past president. He is also the codirector of the Heartland Hospital Medicine Conference.
Amit Vashist, MD, MBA, CPE, FHM, FACP, FAPA, has been named chief clinical officer at Ballad Health, a 21-hospital health system in Northeast Tennessee, Southwest Virginia, Northwest North Carolina, and Southeast Kentucky.
In his new role, he will focus on clinical quality, value-based initiatives to improve quality while reducing cost of care, performance improvement, oversight of the clinical delivery of care and will be the liaison to the Ballad Health Clinical Council. Dr. Vashist is a member of The Hospitalist’s editorial advisory board.
Nagendra Gupta, MD, FACP, CPE, has been appointed to the American Board of Internal Medicine’s Internal Medicine Specialty Board. ABIM Specialty Boards are responsible for the broad definition of the discipline across Certification and Maintenance of Certification (MOC). Specialty Board members work with physicians and medical societies to develop Certification and MOC credentials to recognize physicians for their specialized knowledge and commitment to staying current in their field.
Dr. Gupta is a full-time practicing hospitalist with Apogee Physicians and currently serves as the director of the hospitalist program at Texas Health Arlington (Tex.) Memorial Hospital. He also serves as vice president for SHM’s North Central Texas Chapter.
T. Steen Trawick Jr., MD, was named the CEO of Christus Shreveport-Bossier Health System in Shreveport, La., in August 2019.
Dr. Trawick has worked for Christus as a pediatric hospitalist since 2005 and most recently has served concurrently as associate chief medical officer for Sound Physicians. Through Sound Physicians, Dr. Trawick oversees the hospitalist and emergency medical programs for Christus and other hospitals – 14 in total – in Texas and Louisiana. He has worked in that role for the past 6 years.
Scott Shepherd, DO, FACP, has been selected chief medical officer of the health data enrichment and integration technology company Verinovum in Tulsa, Okla. Dr. Shepherd is the medical director for hospitalist medicine and a practicing hospitalist with St. John Health System in Tulsa, and also medical director of the Center for Health Systems Innovation at his alma mater, Oklahoma State University in Stillwater.
Amanda Logue, MD, has been elevated to chief medical officer at Lafayette (La.) General Hospital. Dr. Logue assumed her role in May 2019, which includes the title of senior vice president.
Dr. Logue has worked at Lafayette General since 2009. A hospitalist/internist, her duties at the facility have included department chair of medicine, physician champion for electronic medical record implementation, medical director of the hospitalist program, and most recently chief medical information officer.
Rina Bansal, MD, MBA, recently was appointed full-time president of Inova Alexandria (Va.) Hospital, taking the reins officially after serving as acting president since November 2018. Dr. Bansal has been at Inova since 2008, when she started as a hospitalist at Inova Fairfax (Va.).
Dr. Bansal created and led Inova’s Clinical Nurse Services Hospitalist program through its department of neurosciences and has done stints as Inova Fairfax’s associate chief medical officer, medical director of Inova Telemedicine, and chief medical officer at Inova Alexandria.
James Napoli, MD, has been named chief medical officer for Blue Cross and Blue Shield of Arizona (BCBSAZ). He has manned the CMO position in an interim role since March, taking those duties on top of his role as BCBSAZ’s enterprise medical director for health care ventures and innovation.
Dr. Napoli came to BCBSAZ in 2013 after more than a decade at Abrazo Arrowhead Campus (Glendale, Ariz.) At Abrazo, he was director of hospitalist services and vice-chief of staff, on top of his efforts as a practicing hospital medicine clinician.
Dr. Napoli was previously medical director at OptumHealth, working specifically in the medical management and quality improvement areas for the health management solutions organization’s Medicare Advantage clients.
Mercy Hospital Fort Smith (Ark.) has partnered with the Ob Hospitalist Group (Greenville, S.C.) to launch an obstetric hospitalist program. OB hospitalists deliver babies when a patient’s physician cannot be present, provide emergency care, and provide support to high-risk pregnancy patients, among other duties within the hospital.
The partnership has allowed Mercy Fort Smith to create a dedicated, four-room obstetric emergency department in its Mercy Childbirth Center. Eight OB hospitalists have been hired and will provide care 24 hours a day, 7 days a week.
Managing alcohol withdrawal in the hospitalized patient
Symptom-triggered therapy has multiple benefits
Case
A 57-year-old man with a history of alcohol abuse (no history of seizures) presents to the ED “feeling awful.” He claims his last drink was 1 day prior. Initial vital signs are: T = 99.1°F, HR 102 bpm, BP 162/85 mm Hg, respirations 18/minute, and 99% oxygen saturation. He is tremulous, diaphoretic, and has an unsteady gait. What is the best way to manage his symptoms while hospitalized?
Brief overview of the issue
With over 15 million people with alcohol use disorder (AUD) in the United States alone, alcohol dependence and misuse remain significant issues among hospitalized patients.1 It is estimated that over 20% of admitted patients meet DSM-5 criteria for AUD and that over 2 million will withdraw each year.2,3 Acute withdrawal includes a spectrum of symptoms ranging from mild anxiety and diaphoresis to hallucinations, seizures, and delirium tremens. Onset of these symptoms ranges from 24 hours up to 5 days.
Severe alcohol withdrawal syndrome (SAWS) attributable to abrupt discontinuation of alcohol leads to increased morbidity and mortality; therefore, early detection and prevention in the acute care setting is critical. Several factors can help predict who may withdraw, and once detected, pharmacological treatment is necessary.4 Thorough evaluation and treatment can help reduce mortality from the most severe forms of alcohol withdrawal including delirium tremens, which has up to 40% mortality if left untreated.5
Overview of the data
How do we use benzodiazepines to treat alcohol withdrawal?
Benzodiazepines are the mainstay of alcohol withdrawal treatment. Benzodiazepines work by stimulating the gamma-aminobutyric acid (GABA) receptor resulting in a reduction of neuronal activity. This leads to a sedative effect and thus slows the progression of withdrawal symptoms.
Long-acting benzodiazepines, such as chlordiazepoxide and diazepam, are the preferred choices for most patients. Their active metabolites have a rapid onset of action and their long half-lives allow for a lower incidence of breakthrough symptoms and rebound phenomena such as seizures.6 Benzodiazepines with shorter half-lives, such as lorazepam and oxazepam, are preferred in patients with liver dysfunction and those prone to respiratory depression.
Intravenous administration has a rapid onset of action and is the standard administration route of choice in patients with acute severe withdrawal, delirium tremens, and seizure activity. In patients with mild withdrawal symptoms or those in the outpatient setting, oral administration is generally effective.6
The Clinical Institute Withdrawal Assessment (CIWA) is one commonly used titration model that requires calculation of a symptom-based withdrawal score. Data have consistently demonstrated that a symptom-triggered method results in administration of less total benzodiazepines over a significantly shorter duration, thereby reducing cost and duration of treatment and minimizing side effects. This regimen may also reduce the risk of undermedicating or overmedicating a patient since the dosing is based upon an individual’s symptoms.7,8
The efficacy of symptom-triggered regimens however, depends on the reliability and accuracy of the patient assessment. A fixed-interval benzodiazepine-dosing approach where benzodiazepines are administered regardless of symptoms is useful when frequent monitoring and reassessment are not feasible or are unreliable.
What about phenobarbital?
Phenobarbital has similar pharmacokinetics to the benzodiazepines frequently used for alcohol withdrawal, including simultaneous effects on gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) receptors, and has been proposed as a treatment option for delirium tremens.
In 2019, as reported in the American Journal of Emergency Medicine, Nelson et al. found that incorporating phenobarbital into a benzodiazepine-based protocol or as sole agent led to similar rates of ICU admission, length of stay, and need for mechanical ventilation in patients treated for alcohol withdrawal in the emergency department.9 The authors concluded that “phenobarbital (was) a safe and effective treatment alternative for alcohol withdrawal.” The systematic review by Hammond et al. in 2017 found that phenobarbital, either as monotherapy or in conjunction with benzodiazepines, could have comparable or superior results in comparison to other treatments, including benzodiazepines monotherapy.10 Further studies are needed to determine dosing and the most effective way to incorporate the use of phenobarbital in treatment of Alcohol Withdrawal Syndrome (AWS).
Should gabapentin or any other medications be added to his treatment regimen?
Chronic alcohol use induces a reduction in GABA activity (the major inhibitory neurotransmitter in the brain) and alcohol cessation results in decreased inhibitory tone. This physiologic imbalance contributes to the syndrome of alcohol withdrawal. As such, gabapentin has emerged as a promising treatment option in AWS and may help reduce the need for benzodiazepines.
Gabapentin has few drug-drug interactions and is safe for use in patients with impaired liver function; however, dosage adjustment is required for renal dysfunction (CrCl less than 60 mL/min). Gabapentin’s neuroprotective effects may also help decrease the neurotoxic effects associated with AWS. Common side effects of gabapentin include dizziness, drowsiness, ataxia, diarrhea, nausea, and vomiting. The potential for misuse has been reported.
In several small studies, gabapentin monotherapy was found to be comparable to benzodiazepines in the treatment of mild to moderate AWS. Gabapentin is efficacious in reducing cravings as well as improving mood, anxiety, and sleep, and showed an advantage over benzodiazepines in preventing relapse with no difference in length of hospital stay.6,11 Given the small sample sizes of these studies and the differing methods, settings, and inclusion/ exclusion criteria used, the generalizability of these findings to patients with significant medical and/or psychiatric comorbidities remains limited. Additional studies are needed to standardize dosing protocols and treatment strategies for both inpatients and outpatients.
Alternative agents such as antipsychotics (e.g., haloperidol), centrally acting alpha-2 agonists (e.g., clonidine), beta-blockers, and an agonist of the GABA-B receptor (e.g., baclofen) may also attenuate the symptoms of withdrawal. Since these all have limited evidence of their efficacy and have potential for harm, such as masking symptoms of progressive withdrawal and lowering seizure threshold, these agents are not routinely recommended for use. Valproic acid/divalproex, levetiracetam, topiramate, and zonisamide have also showed some efficacy in reducing symptoms of alcohol withdrawal in limited studies. The data on prevention of withdrawal seizures or delirium tremens when used as monotherapy is less robust.12
A daily multivitamin and folate are ordered. What about thiamine? Does the route matter?
Alarmingly, 80% of people who chronically abuse alcohol are thiamine deficient.13 This deficiency is attributable to several factors including inadequate oral intake, malabsorption, and decreased cellular utilization. Thiamine is a crucial factor in multiple enzymatic and metabolic pathways. Its deficiency can lead to free radical production, neurotoxicity, impaired glucose metabolism, and ultimately, cell death.14 A clinical concern stemming from thiamine deficiency is the development of Wernicke’s encephalopathy (WE), which is potentially reversible with prompt recognition and treatment, in comparison to its irreversible amnestic sequela, Korsakoff’s syndrome.
Wernicke’s encephalopathy had been defined as a triad of ataxia, ophthalmoplegia, and global confusion. However, Harper et al. discovered that only 16% of patients presented with the classic triad and 19% had none of these signs.15 Diagnosis is clinical since thiamine serology results do not accurately represent brain storage.
Currently, there are no consistent guidelines regarding repletion of thiamine administration in the treatment or prevention of WE attributable to alcohol overuse. Thiamine has a safe toxicity profile as excess thiamine is excreted in the urine. Outside of rare reports of anaphylactoid reactions involving large parenteral doses, there is no concern for overtreatment. As Wernicke-Korsakoff syndrome is associated with significant morbidity and mortality, high doses such as 200 to 500 mg are recommended to ensure blood-brain barrier passage. The intravenous route is optimal over oral administration to bypass concerns of gastrointestinal malabsorption. Thiamine 100 mg by mouth daily for ongoing supplementation can be considered for patients who are at risk for WE. It is also important to recognize that magnesium and thiamine are intertwined in several key enzymatic pathways. To optimize the responsiveness of thiamine repletion, magnesium levels should be tested and repleted if low.
Application of the data to our patient
Nurses are able to frequently monitor the patient so he is started on symptom-triggered treatment with chlordiazepoxide using the CIWA protocol. This strategy will help limit the amount of benzodiazepines he receives and shorten his treatment duration. Given the ataxia, the patient is also started on high-dose IV thiamine three times a day to treat possible Wernicke’s encephalopathy. Gabapentin is added to his regimen to help manage his moderate alcohol withdrawal syndrome.
Bottom line
Long-acting benzodiazepines using symptom-triggered administration when feasible are the mainstay of treating alcohol withdrawal. Other medications such as gabapentin, carbamazepine, and phenobarbital can be considered as adjunctive agents. Given the high rate of thiamine deficiency and the low risk of overreplacement, intravenous thiamine can be considered for inpatients with AWS.
Dr. Agrawal, Dr. Chernyavsky, Dr. Dharapak, Dr. Grabscheid, Dr. Merrill, Dr. Pillay, and Dr. Rizk are hospitalists at Mount Sinai Beth Israel in New York.
References
1. CDC - Fact Sheets: “Alcohol Use And Health – Alcohol.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 3 Jan. 2018.
2. Rawlani V et al. Treatment of the hospitalized alcohol-dependent patient with alcohol withdrawal syndrome. Internet J Intern Med. 2008;8(1).
3. Grant BF et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757.
4. Wood E et al. Will this hospitalized patient develop severe alcohol withdrawal syndrome?: The Rational Clinical Examination Systematic Review. JAMA. 2018;320:825.
5. Sarkar S et al. Risk factors for the development of delirium in alcohol dependence syndrome: Clinical and neurobiological implications. Indian J Psychiatry. 2017 Jul-Sep;59(3):300-5.
6. Sachdeva A et al. Alcohol withdrawal syndrome: Benzodiazepines and beyond. J Clinical Diagn Res. 2015 Sep 9(9).
7. Sullivan JT et al. Benzodiazepine requirements during alcohol withdrawal syndrome: Clinical implications of using a standardized withdrawal scale. J Clin Psychopharmacol. 1991;11:291-5.
8. Saitz R et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519.
9. Nelson AC et al. Benzodiazepines vs. barbiturates for alcohol withdrawal: Analysis of 3 different treatment protocols. Am J Emerg Med. 2019 Jan 3.
10. Hammond DA et al. Patient outcomes associated with phenobarbital use with or without benzodiazepines for alcohol withdrawal syndrome: A systematic review. Hosp Pharm. 2017 Oct;52(9):607-16.
11. Mo Y et al. Current practice patterns in the management of alcohol withdrawal syndrome. P T. 2018 Mar;43(3):158-62.
12. Leung JG et al. The role of gabapentin in the management of alcohol withdrawal and dependence. Ann Pharmacother. 2015 Aug;49(8):897-906.
13. Martin P et al. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003:27(2):134-42.
14. Flannery A et al. Unpeeling the evidence for the banana bag: Evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016 Aug:44(8):1545-52.
15. Harper CG et al. Clinical signs in Wernicke Korsakoff complex: A retrospective analysis of 131 cases diagnosed at autopsy. J Neurol Neurosurg Psychiatry. 1986;49(4):341-5.
Key points
- Alcohol use disorder and alcohol withdrawal are significant problems in hospitalized patients; early detection and treatment are crucial in preventing high morbidity and mortality.
- Long acting benzodiazepines with active metabolites such as chlordiazepoxide and diazepam are the preferred treatment for alcohol withdrawal except for patients with advanced liver disease or those prone to respiratory depression.
- Symptom-triggered therapy decreases the amount of medication, shortens treatment duration, and decreases inpatient length of stay, compared with fixed schedule dosing.
- Gabapentin may be effective in the treatment of mild to moderate AWS but cannot yet be routinely recommended as monotherapy in severe withdrawal, in patients with seizure history, or in patients who are at high risk for progression to delirium tremens.
- Thiamine deficiency is common in chronic alcohol use disorders; thiamine repletion should be considered for patients at risk or when Wernicke’s encephalopathy and Korsakoff’s syndrome are suspected.
Additional reading
1. Perry EC. Inpatient management of acute alcohol withdrawal syndrome. CNS Drugs. 2014;28(5):401-10.
2. Mayo-Smith MF. Pharmacological management of alcohol withdrawal: A meta-analysis and evidence-based practice guideline. JAMA. 1997;278(2):144-51.
3. Michael F. Mayo-Smith, MD, MPH et al. for the Working Group on the Management of Alcohol Withdrawal Delirium, Practice Guidelines Committee, American Society of Addiction Medicine. Management of alcohol withdrawal delirium: An evidence-based practice guideline. Arch Intern Med. 2004;164(13):1405-12.
Quiz
A 51-year-old female with a history of hypertension and continuous alcohol abuse presents to the hospital with fever and cough. She is found to have community-acquired pneumonia and is admitted for treatment. How else would you manage this patient?
A. Start scheduled benzodiazepines and oral thiamine.
B. Start CIWA protocol using a long-acting benzodiazepine and oral thiamine.
C. Start scheduled benzodiazepines and IV thiamine.
D. Start CIWA protocol using a long-acting benzodiazepine and consider IV or oral thiamine.
Answer: D. Symptom-triggered benzodiazepine therapy is favored as is consideration for thiamine repletion in the treatment of AWS.
Symptom-triggered therapy has multiple benefits
Symptom-triggered therapy has multiple benefits
Case
A 57-year-old man with a history of alcohol abuse (no history of seizures) presents to the ED “feeling awful.” He claims his last drink was 1 day prior. Initial vital signs are: T = 99.1°F, HR 102 bpm, BP 162/85 mm Hg, respirations 18/minute, and 99% oxygen saturation. He is tremulous, diaphoretic, and has an unsteady gait. What is the best way to manage his symptoms while hospitalized?
Brief overview of the issue
With over 15 million people with alcohol use disorder (AUD) in the United States alone, alcohol dependence and misuse remain significant issues among hospitalized patients.1 It is estimated that over 20% of admitted patients meet DSM-5 criteria for AUD and that over 2 million will withdraw each year.2,3 Acute withdrawal includes a spectrum of symptoms ranging from mild anxiety and diaphoresis to hallucinations, seizures, and delirium tremens. Onset of these symptoms ranges from 24 hours up to 5 days.
Severe alcohol withdrawal syndrome (SAWS) attributable to abrupt discontinuation of alcohol leads to increased morbidity and mortality; therefore, early detection and prevention in the acute care setting is critical. Several factors can help predict who may withdraw, and once detected, pharmacological treatment is necessary.4 Thorough evaluation and treatment can help reduce mortality from the most severe forms of alcohol withdrawal including delirium tremens, which has up to 40% mortality if left untreated.5
Overview of the data
How do we use benzodiazepines to treat alcohol withdrawal?
Benzodiazepines are the mainstay of alcohol withdrawal treatment. Benzodiazepines work by stimulating the gamma-aminobutyric acid (GABA) receptor resulting in a reduction of neuronal activity. This leads to a sedative effect and thus slows the progression of withdrawal symptoms.
Long-acting benzodiazepines, such as chlordiazepoxide and diazepam, are the preferred choices for most patients. Their active metabolites have a rapid onset of action and their long half-lives allow for a lower incidence of breakthrough symptoms and rebound phenomena such as seizures.6 Benzodiazepines with shorter half-lives, such as lorazepam and oxazepam, are preferred in patients with liver dysfunction and those prone to respiratory depression.
Intravenous administration has a rapid onset of action and is the standard administration route of choice in patients with acute severe withdrawal, delirium tremens, and seizure activity. In patients with mild withdrawal symptoms or those in the outpatient setting, oral administration is generally effective.6
The Clinical Institute Withdrawal Assessment (CIWA) is one commonly used titration model that requires calculation of a symptom-based withdrawal score. Data have consistently demonstrated that a symptom-triggered method results in administration of less total benzodiazepines over a significantly shorter duration, thereby reducing cost and duration of treatment and minimizing side effects. This regimen may also reduce the risk of undermedicating or overmedicating a patient since the dosing is based upon an individual’s symptoms.7,8
The efficacy of symptom-triggered regimens however, depends on the reliability and accuracy of the patient assessment. A fixed-interval benzodiazepine-dosing approach where benzodiazepines are administered regardless of symptoms is useful when frequent monitoring and reassessment are not feasible or are unreliable.
What about phenobarbital?
Phenobarbital has similar pharmacokinetics to the benzodiazepines frequently used for alcohol withdrawal, including simultaneous effects on gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) receptors, and has been proposed as a treatment option for delirium tremens.
In 2019, as reported in the American Journal of Emergency Medicine, Nelson et al. found that incorporating phenobarbital into a benzodiazepine-based protocol or as sole agent led to similar rates of ICU admission, length of stay, and need for mechanical ventilation in patients treated for alcohol withdrawal in the emergency department.9 The authors concluded that “phenobarbital (was) a safe and effective treatment alternative for alcohol withdrawal.” The systematic review by Hammond et al. in 2017 found that phenobarbital, either as monotherapy or in conjunction with benzodiazepines, could have comparable or superior results in comparison to other treatments, including benzodiazepines monotherapy.10 Further studies are needed to determine dosing and the most effective way to incorporate the use of phenobarbital in treatment of Alcohol Withdrawal Syndrome (AWS).
Should gabapentin or any other medications be added to his treatment regimen?
Chronic alcohol use induces a reduction in GABA activity (the major inhibitory neurotransmitter in the brain) and alcohol cessation results in decreased inhibitory tone. This physiologic imbalance contributes to the syndrome of alcohol withdrawal. As such, gabapentin has emerged as a promising treatment option in AWS and may help reduce the need for benzodiazepines.
Gabapentin has few drug-drug interactions and is safe for use in patients with impaired liver function; however, dosage adjustment is required for renal dysfunction (CrCl less than 60 mL/min). Gabapentin’s neuroprotective effects may also help decrease the neurotoxic effects associated with AWS. Common side effects of gabapentin include dizziness, drowsiness, ataxia, diarrhea, nausea, and vomiting. The potential for misuse has been reported.
In several small studies, gabapentin monotherapy was found to be comparable to benzodiazepines in the treatment of mild to moderate AWS. Gabapentin is efficacious in reducing cravings as well as improving mood, anxiety, and sleep, and showed an advantage over benzodiazepines in preventing relapse with no difference in length of hospital stay.6,11 Given the small sample sizes of these studies and the differing methods, settings, and inclusion/ exclusion criteria used, the generalizability of these findings to patients with significant medical and/or psychiatric comorbidities remains limited. Additional studies are needed to standardize dosing protocols and treatment strategies for both inpatients and outpatients.
Alternative agents such as antipsychotics (e.g., haloperidol), centrally acting alpha-2 agonists (e.g., clonidine), beta-blockers, and an agonist of the GABA-B receptor (e.g., baclofen) may also attenuate the symptoms of withdrawal. Since these all have limited evidence of their efficacy and have potential for harm, such as masking symptoms of progressive withdrawal and lowering seizure threshold, these agents are not routinely recommended for use. Valproic acid/divalproex, levetiracetam, topiramate, and zonisamide have also showed some efficacy in reducing symptoms of alcohol withdrawal in limited studies. The data on prevention of withdrawal seizures or delirium tremens when used as monotherapy is less robust.12
A daily multivitamin and folate are ordered. What about thiamine? Does the route matter?
Alarmingly, 80% of people who chronically abuse alcohol are thiamine deficient.13 This deficiency is attributable to several factors including inadequate oral intake, malabsorption, and decreased cellular utilization. Thiamine is a crucial factor in multiple enzymatic and metabolic pathways. Its deficiency can lead to free radical production, neurotoxicity, impaired glucose metabolism, and ultimately, cell death.14 A clinical concern stemming from thiamine deficiency is the development of Wernicke’s encephalopathy (WE), which is potentially reversible with prompt recognition and treatment, in comparison to its irreversible amnestic sequela, Korsakoff’s syndrome.
Wernicke’s encephalopathy had been defined as a triad of ataxia, ophthalmoplegia, and global confusion. However, Harper et al. discovered that only 16% of patients presented with the classic triad and 19% had none of these signs.15 Diagnosis is clinical since thiamine serology results do not accurately represent brain storage.
Currently, there are no consistent guidelines regarding repletion of thiamine administration in the treatment or prevention of WE attributable to alcohol overuse. Thiamine has a safe toxicity profile as excess thiamine is excreted in the urine. Outside of rare reports of anaphylactoid reactions involving large parenteral doses, there is no concern for overtreatment. As Wernicke-Korsakoff syndrome is associated with significant morbidity and mortality, high doses such as 200 to 500 mg are recommended to ensure blood-brain barrier passage. The intravenous route is optimal over oral administration to bypass concerns of gastrointestinal malabsorption. Thiamine 100 mg by mouth daily for ongoing supplementation can be considered for patients who are at risk for WE. It is also important to recognize that magnesium and thiamine are intertwined in several key enzymatic pathways. To optimize the responsiveness of thiamine repletion, magnesium levels should be tested and repleted if low.
Application of the data to our patient
Nurses are able to frequently monitor the patient so he is started on symptom-triggered treatment with chlordiazepoxide using the CIWA protocol. This strategy will help limit the amount of benzodiazepines he receives and shorten his treatment duration. Given the ataxia, the patient is also started on high-dose IV thiamine three times a day to treat possible Wernicke’s encephalopathy. Gabapentin is added to his regimen to help manage his moderate alcohol withdrawal syndrome.
Bottom line
Long-acting benzodiazepines using symptom-triggered administration when feasible are the mainstay of treating alcohol withdrawal. Other medications such as gabapentin, carbamazepine, and phenobarbital can be considered as adjunctive agents. Given the high rate of thiamine deficiency and the low risk of overreplacement, intravenous thiamine can be considered for inpatients with AWS.
Dr. Agrawal, Dr. Chernyavsky, Dr. Dharapak, Dr. Grabscheid, Dr. Merrill, Dr. Pillay, and Dr. Rizk are hospitalists at Mount Sinai Beth Israel in New York.
References
1. CDC - Fact Sheets: “Alcohol Use And Health – Alcohol.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 3 Jan. 2018.
2. Rawlani V et al. Treatment of the hospitalized alcohol-dependent patient with alcohol withdrawal syndrome. Internet J Intern Med. 2008;8(1).
3. Grant BF et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757.
4. Wood E et al. Will this hospitalized patient develop severe alcohol withdrawal syndrome?: The Rational Clinical Examination Systematic Review. JAMA. 2018;320:825.
5. Sarkar S et al. Risk factors for the development of delirium in alcohol dependence syndrome: Clinical and neurobiological implications. Indian J Psychiatry. 2017 Jul-Sep;59(3):300-5.
6. Sachdeva A et al. Alcohol withdrawal syndrome: Benzodiazepines and beyond. J Clinical Diagn Res. 2015 Sep 9(9).
7. Sullivan JT et al. Benzodiazepine requirements during alcohol withdrawal syndrome: Clinical implications of using a standardized withdrawal scale. J Clin Psychopharmacol. 1991;11:291-5.
8. Saitz R et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519.
9. Nelson AC et al. Benzodiazepines vs. barbiturates for alcohol withdrawal: Analysis of 3 different treatment protocols. Am J Emerg Med. 2019 Jan 3.
10. Hammond DA et al. Patient outcomes associated with phenobarbital use with or without benzodiazepines for alcohol withdrawal syndrome: A systematic review. Hosp Pharm. 2017 Oct;52(9):607-16.
11. Mo Y et al. Current practice patterns in the management of alcohol withdrawal syndrome. P T. 2018 Mar;43(3):158-62.
12. Leung JG et al. The role of gabapentin in the management of alcohol withdrawal and dependence. Ann Pharmacother. 2015 Aug;49(8):897-906.
13. Martin P et al. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003:27(2):134-42.
14. Flannery A et al. Unpeeling the evidence for the banana bag: Evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016 Aug:44(8):1545-52.
15. Harper CG et al. Clinical signs in Wernicke Korsakoff complex: A retrospective analysis of 131 cases diagnosed at autopsy. J Neurol Neurosurg Psychiatry. 1986;49(4):341-5.
Key points
- Alcohol use disorder and alcohol withdrawal are significant problems in hospitalized patients; early detection and treatment are crucial in preventing high morbidity and mortality.
- Long acting benzodiazepines with active metabolites such as chlordiazepoxide and diazepam are the preferred treatment for alcohol withdrawal except for patients with advanced liver disease or those prone to respiratory depression.
- Symptom-triggered therapy decreases the amount of medication, shortens treatment duration, and decreases inpatient length of stay, compared with fixed schedule dosing.
- Gabapentin may be effective in the treatment of mild to moderate AWS but cannot yet be routinely recommended as monotherapy in severe withdrawal, in patients with seizure history, or in patients who are at high risk for progression to delirium tremens.
- Thiamine deficiency is common in chronic alcohol use disorders; thiamine repletion should be considered for patients at risk or when Wernicke’s encephalopathy and Korsakoff’s syndrome are suspected.
Additional reading
1. Perry EC. Inpatient management of acute alcohol withdrawal syndrome. CNS Drugs. 2014;28(5):401-10.
2. Mayo-Smith MF. Pharmacological management of alcohol withdrawal: A meta-analysis and evidence-based practice guideline. JAMA. 1997;278(2):144-51.
3. Michael F. Mayo-Smith, MD, MPH et al. for the Working Group on the Management of Alcohol Withdrawal Delirium, Practice Guidelines Committee, American Society of Addiction Medicine. Management of alcohol withdrawal delirium: An evidence-based practice guideline. Arch Intern Med. 2004;164(13):1405-12.
Quiz
A 51-year-old female with a history of hypertension and continuous alcohol abuse presents to the hospital with fever and cough. She is found to have community-acquired pneumonia and is admitted for treatment. How else would you manage this patient?
A. Start scheduled benzodiazepines and oral thiamine.
B. Start CIWA protocol using a long-acting benzodiazepine and oral thiamine.
C. Start scheduled benzodiazepines and IV thiamine.
D. Start CIWA protocol using a long-acting benzodiazepine and consider IV or oral thiamine.
Answer: D. Symptom-triggered benzodiazepine therapy is favored as is consideration for thiamine repletion in the treatment of AWS.
Case
A 57-year-old man with a history of alcohol abuse (no history of seizures) presents to the ED “feeling awful.” He claims his last drink was 1 day prior. Initial vital signs are: T = 99.1°F, HR 102 bpm, BP 162/85 mm Hg, respirations 18/minute, and 99% oxygen saturation. He is tremulous, diaphoretic, and has an unsteady gait. What is the best way to manage his symptoms while hospitalized?
Brief overview of the issue
With over 15 million people with alcohol use disorder (AUD) in the United States alone, alcohol dependence and misuse remain significant issues among hospitalized patients.1 It is estimated that over 20% of admitted patients meet DSM-5 criteria for AUD and that over 2 million will withdraw each year.2,3 Acute withdrawal includes a spectrum of symptoms ranging from mild anxiety and diaphoresis to hallucinations, seizures, and delirium tremens. Onset of these symptoms ranges from 24 hours up to 5 days.
Severe alcohol withdrawal syndrome (SAWS) attributable to abrupt discontinuation of alcohol leads to increased morbidity and mortality; therefore, early detection and prevention in the acute care setting is critical. Several factors can help predict who may withdraw, and once detected, pharmacological treatment is necessary.4 Thorough evaluation and treatment can help reduce mortality from the most severe forms of alcohol withdrawal including delirium tremens, which has up to 40% mortality if left untreated.5
Overview of the data
How do we use benzodiazepines to treat alcohol withdrawal?
Benzodiazepines are the mainstay of alcohol withdrawal treatment. Benzodiazepines work by stimulating the gamma-aminobutyric acid (GABA) receptor resulting in a reduction of neuronal activity. This leads to a sedative effect and thus slows the progression of withdrawal symptoms.
Long-acting benzodiazepines, such as chlordiazepoxide and diazepam, are the preferred choices for most patients. Their active metabolites have a rapid onset of action and their long half-lives allow for a lower incidence of breakthrough symptoms and rebound phenomena such as seizures.6 Benzodiazepines with shorter half-lives, such as lorazepam and oxazepam, are preferred in patients with liver dysfunction and those prone to respiratory depression.
Intravenous administration has a rapid onset of action and is the standard administration route of choice in patients with acute severe withdrawal, delirium tremens, and seizure activity. In patients with mild withdrawal symptoms or those in the outpatient setting, oral administration is generally effective.6
The Clinical Institute Withdrawal Assessment (CIWA) is one commonly used titration model that requires calculation of a symptom-based withdrawal score. Data have consistently demonstrated that a symptom-triggered method results in administration of less total benzodiazepines over a significantly shorter duration, thereby reducing cost and duration of treatment and minimizing side effects. This regimen may also reduce the risk of undermedicating or overmedicating a patient since the dosing is based upon an individual’s symptoms.7,8
The efficacy of symptom-triggered regimens however, depends on the reliability and accuracy of the patient assessment. A fixed-interval benzodiazepine-dosing approach where benzodiazepines are administered regardless of symptoms is useful when frequent monitoring and reassessment are not feasible or are unreliable.
What about phenobarbital?
Phenobarbital has similar pharmacokinetics to the benzodiazepines frequently used for alcohol withdrawal, including simultaneous effects on gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) receptors, and has been proposed as a treatment option for delirium tremens.
In 2019, as reported in the American Journal of Emergency Medicine, Nelson et al. found that incorporating phenobarbital into a benzodiazepine-based protocol or as sole agent led to similar rates of ICU admission, length of stay, and need for mechanical ventilation in patients treated for alcohol withdrawal in the emergency department.9 The authors concluded that “phenobarbital (was) a safe and effective treatment alternative for alcohol withdrawal.” The systematic review by Hammond et al. in 2017 found that phenobarbital, either as monotherapy or in conjunction with benzodiazepines, could have comparable or superior results in comparison to other treatments, including benzodiazepines monotherapy.10 Further studies are needed to determine dosing and the most effective way to incorporate the use of phenobarbital in treatment of Alcohol Withdrawal Syndrome (AWS).
Should gabapentin or any other medications be added to his treatment regimen?
Chronic alcohol use induces a reduction in GABA activity (the major inhibitory neurotransmitter in the brain) and alcohol cessation results in decreased inhibitory tone. This physiologic imbalance contributes to the syndrome of alcohol withdrawal. As such, gabapentin has emerged as a promising treatment option in AWS and may help reduce the need for benzodiazepines.
Gabapentin has few drug-drug interactions and is safe for use in patients with impaired liver function; however, dosage adjustment is required for renal dysfunction (CrCl less than 60 mL/min). Gabapentin’s neuroprotective effects may also help decrease the neurotoxic effects associated with AWS. Common side effects of gabapentin include dizziness, drowsiness, ataxia, diarrhea, nausea, and vomiting. The potential for misuse has been reported.
In several small studies, gabapentin monotherapy was found to be comparable to benzodiazepines in the treatment of mild to moderate AWS. Gabapentin is efficacious in reducing cravings as well as improving mood, anxiety, and sleep, and showed an advantage over benzodiazepines in preventing relapse with no difference in length of hospital stay.6,11 Given the small sample sizes of these studies and the differing methods, settings, and inclusion/ exclusion criteria used, the generalizability of these findings to patients with significant medical and/or psychiatric comorbidities remains limited. Additional studies are needed to standardize dosing protocols and treatment strategies for both inpatients and outpatients.
Alternative agents such as antipsychotics (e.g., haloperidol), centrally acting alpha-2 agonists (e.g., clonidine), beta-blockers, and an agonist of the GABA-B receptor (e.g., baclofen) may also attenuate the symptoms of withdrawal. Since these all have limited evidence of their efficacy and have potential for harm, such as masking symptoms of progressive withdrawal and lowering seizure threshold, these agents are not routinely recommended for use. Valproic acid/divalproex, levetiracetam, topiramate, and zonisamide have also showed some efficacy in reducing symptoms of alcohol withdrawal in limited studies. The data on prevention of withdrawal seizures or delirium tremens when used as monotherapy is less robust.12
A daily multivitamin and folate are ordered. What about thiamine? Does the route matter?
Alarmingly, 80% of people who chronically abuse alcohol are thiamine deficient.13 This deficiency is attributable to several factors including inadequate oral intake, malabsorption, and decreased cellular utilization. Thiamine is a crucial factor in multiple enzymatic and metabolic pathways. Its deficiency can lead to free radical production, neurotoxicity, impaired glucose metabolism, and ultimately, cell death.14 A clinical concern stemming from thiamine deficiency is the development of Wernicke’s encephalopathy (WE), which is potentially reversible with prompt recognition and treatment, in comparison to its irreversible amnestic sequela, Korsakoff’s syndrome.
Wernicke’s encephalopathy had been defined as a triad of ataxia, ophthalmoplegia, and global confusion. However, Harper et al. discovered that only 16% of patients presented with the classic triad and 19% had none of these signs.15 Diagnosis is clinical since thiamine serology results do not accurately represent brain storage.
Currently, there are no consistent guidelines regarding repletion of thiamine administration in the treatment or prevention of WE attributable to alcohol overuse. Thiamine has a safe toxicity profile as excess thiamine is excreted in the urine. Outside of rare reports of anaphylactoid reactions involving large parenteral doses, there is no concern for overtreatment. As Wernicke-Korsakoff syndrome is associated with significant morbidity and mortality, high doses such as 200 to 500 mg are recommended to ensure blood-brain barrier passage. The intravenous route is optimal over oral administration to bypass concerns of gastrointestinal malabsorption. Thiamine 100 mg by mouth daily for ongoing supplementation can be considered for patients who are at risk for WE. It is also important to recognize that magnesium and thiamine are intertwined in several key enzymatic pathways. To optimize the responsiveness of thiamine repletion, magnesium levels should be tested and repleted if low.
Application of the data to our patient
Nurses are able to frequently monitor the patient so he is started on symptom-triggered treatment with chlordiazepoxide using the CIWA protocol. This strategy will help limit the amount of benzodiazepines he receives and shorten his treatment duration. Given the ataxia, the patient is also started on high-dose IV thiamine three times a day to treat possible Wernicke’s encephalopathy. Gabapentin is added to his regimen to help manage his moderate alcohol withdrawal syndrome.
Bottom line
Long-acting benzodiazepines using symptom-triggered administration when feasible are the mainstay of treating alcohol withdrawal. Other medications such as gabapentin, carbamazepine, and phenobarbital can be considered as adjunctive agents. Given the high rate of thiamine deficiency and the low risk of overreplacement, intravenous thiamine can be considered for inpatients with AWS.
Dr. Agrawal, Dr. Chernyavsky, Dr. Dharapak, Dr. Grabscheid, Dr. Merrill, Dr. Pillay, and Dr. Rizk are hospitalists at Mount Sinai Beth Israel in New York.
References
1. CDC - Fact Sheets: “Alcohol Use And Health – Alcohol.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 3 Jan. 2018.
2. Rawlani V et al. Treatment of the hospitalized alcohol-dependent patient with alcohol withdrawal syndrome. Internet J Intern Med. 2008;8(1).
3. Grant BF et al. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757.
4. Wood E et al. Will this hospitalized patient develop severe alcohol withdrawal syndrome?: The Rational Clinical Examination Systematic Review. JAMA. 2018;320:825.
5. Sarkar S et al. Risk factors for the development of delirium in alcohol dependence syndrome: Clinical and neurobiological implications. Indian J Psychiatry. 2017 Jul-Sep;59(3):300-5.
6. Sachdeva A et al. Alcohol withdrawal syndrome: Benzodiazepines and beyond. J Clinical Diagn Res. 2015 Sep 9(9).
7. Sullivan JT et al. Benzodiazepine requirements during alcohol withdrawal syndrome: Clinical implications of using a standardized withdrawal scale. J Clin Psychopharmacol. 1991;11:291-5.
8. Saitz R et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519.
9. Nelson AC et al. Benzodiazepines vs. barbiturates for alcohol withdrawal: Analysis of 3 different treatment protocols. Am J Emerg Med. 2019 Jan 3.
10. Hammond DA et al. Patient outcomes associated with phenobarbital use with or without benzodiazepines for alcohol withdrawal syndrome: A systematic review. Hosp Pharm. 2017 Oct;52(9):607-16.
11. Mo Y et al. Current practice patterns in the management of alcohol withdrawal syndrome. P T. 2018 Mar;43(3):158-62.
12. Leung JG et al. The role of gabapentin in the management of alcohol withdrawal and dependence. Ann Pharmacother. 2015 Aug;49(8):897-906.
13. Martin P et al. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003:27(2):134-42.
14. Flannery A et al. Unpeeling the evidence for the banana bag: Evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016 Aug:44(8):1545-52.
15. Harper CG et al. Clinical signs in Wernicke Korsakoff complex: A retrospective analysis of 131 cases diagnosed at autopsy. J Neurol Neurosurg Psychiatry. 1986;49(4):341-5.
Key points
- Alcohol use disorder and alcohol withdrawal are significant problems in hospitalized patients; early detection and treatment are crucial in preventing high morbidity and mortality.
- Long acting benzodiazepines with active metabolites such as chlordiazepoxide and diazepam are the preferred treatment for alcohol withdrawal except for patients with advanced liver disease or those prone to respiratory depression.
- Symptom-triggered therapy decreases the amount of medication, shortens treatment duration, and decreases inpatient length of stay, compared with fixed schedule dosing.
- Gabapentin may be effective in the treatment of mild to moderate AWS but cannot yet be routinely recommended as monotherapy in severe withdrawal, in patients with seizure history, or in patients who are at high risk for progression to delirium tremens.
- Thiamine deficiency is common in chronic alcohol use disorders; thiamine repletion should be considered for patients at risk or when Wernicke’s encephalopathy and Korsakoff’s syndrome are suspected.
Additional reading
1. Perry EC. Inpatient management of acute alcohol withdrawal syndrome. CNS Drugs. 2014;28(5):401-10.
2. Mayo-Smith MF. Pharmacological management of alcohol withdrawal: A meta-analysis and evidence-based practice guideline. JAMA. 1997;278(2):144-51.
3. Michael F. Mayo-Smith, MD, MPH et al. for the Working Group on the Management of Alcohol Withdrawal Delirium, Practice Guidelines Committee, American Society of Addiction Medicine. Management of alcohol withdrawal delirium: An evidence-based practice guideline. Arch Intern Med. 2004;164(13):1405-12.
Quiz
A 51-year-old female with a history of hypertension and continuous alcohol abuse presents to the hospital with fever and cough. She is found to have community-acquired pneumonia and is admitted for treatment. How else would you manage this patient?
A. Start scheduled benzodiazepines and oral thiamine.
B. Start CIWA protocol using a long-acting benzodiazepine and oral thiamine.
C. Start scheduled benzodiazepines and IV thiamine.
D. Start CIWA protocol using a long-acting benzodiazepine and consider IV or oral thiamine.
Answer: D. Symptom-triggered benzodiazepine therapy is favored as is consideration for thiamine repletion in the treatment of AWS.
Introducing SHM’s president-elect
Hoping to expand membership beyond the traditional ‘core’
It is with great pleasure that I enter my president-elect year for the Society of Hospital Medicine! I am hopeful that this year will allow me time to get to know the organization even better than I already do, and truly understand the needs of our members so I can focus on meeting and exceeding your expectations!
I have been a hospitalist now for 17 years and have practiced in both academic tertiary care and community hospital settings. As a chief quality officer, I also work with improving quality and safety in all health care settings, including ambulatory, nursing homes, home health, and surgical centers. As such, I hope I can bring a broad lens of the medical industry to this position, improving the lives and careers of hospitalists and the patients and families they serve.
As we all know, the demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, as we now occupy almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole. That is where our board and SHM come into play – to provide the resources you need to improve health care.
These resources come in the form of education and training (live or on demand); leadership and professional development; practice management assistance; advocacy work; mentored quality improvement; networking and project work (through special interest groups, local chapter meetings, and committee work); stimulation of research, new knowledge, and innovation; and promotion of evidence-based practice through our educational resources, publications, and other communications. The purpose of our existence is to provide you what you need to improve your work lives and your patients’ health.
SHM has always fostered a “big-tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics, and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members, with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
My humble hope, as it is with any of my leadership positions, is to leave SHM better than I found it. As such, please contact me at any time if you have ideas or suggestions on how we can better help you be successful in improving the care for your patients, your systems, and health care as a whole. I look forward to serving you in this incredible journey and mission.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the medical editor of the Hospitalist, and president-elect of SHM.
Hoping to expand membership beyond the traditional ‘core’
Hoping to expand membership beyond the traditional ‘core’
It is with great pleasure that I enter my president-elect year for the Society of Hospital Medicine! I am hopeful that this year will allow me time to get to know the organization even better than I already do, and truly understand the needs of our members so I can focus on meeting and exceeding your expectations!
I have been a hospitalist now for 17 years and have practiced in both academic tertiary care and community hospital settings. As a chief quality officer, I also work with improving quality and safety in all health care settings, including ambulatory, nursing homes, home health, and surgical centers. As such, I hope I can bring a broad lens of the medical industry to this position, improving the lives and careers of hospitalists and the patients and families they serve.
As we all know, the demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, as we now occupy almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole. That is where our board and SHM come into play – to provide the resources you need to improve health care.
These resources come in the form of education and training (live or on demand); leadership and professional development; practice management assistance; advocacy work; mentored quality improvement; networking and project work (through special interest groups, local chapter meetings, and committee work); stimulation of research, new knowledge, and innovation; and promotion of evidence-based practice through our educational resources, publications, and other communications. The purpose of our existence is to provide you what you need to improve your work lives and your patients’ health.
SHM has always fostered a “big-tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics, and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members, with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
My humble hope, as it is with any of my leadership positions, is to leave SHM better than I found it. As such, please contact me at any time if you have ideas or suggestions on how we can better help you be successful in improving the care for your patients, your systems, and health care as a whole. I look forward to serving you in this incredible journey and mission.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the medical editor of the Hospitalist, and president-elect of SHM.
It is with great pleasure that I enter my president-elect year for the Society of Hospital Medicine! I am hopeful that this year will allow me time to get to know the organization even better than I already do, and truly understand the needs of our members so I can focus on meeting and exceeding your expectations!
I have been a hospitalist now for 17 years and have practiced in both academic tertiary care and community hospital settings. As a chief quality officer, I also work with improving quality and safety in all health care settings, including ambulatory, nursing homes, home health, and surgical centers. As such, I hope I can bring a broad lens of the medical industry to this position, improving the lives and careers of hospitalists and the patients and families they serve.
As we all know, the demands placed on hospitalists are greater than ever. With shortening length of stay, rising acuity and complexity, increasing administrative burdens, and high emphasis on care transitions, our skills (and our patience) need to rise to these increasing demands. As a member-based society, SHM (and the board of directors) seeks to ensure we are helping hospitalists be the very best they can be, regardless of hospitalist type or practice setting.
The good news is that we are still in high demand. Within the medical industry, there has been an explosive growth in the need for hospitalists, as we now occupy almost every hospital setting in the United States. But as a current commodity, it is imperative that we continue to prove the value we are adding to our patients and their families, the systems in which we work, and the industry as a whole. That is where our board and SHM come into play – to provide the resources you need to improve health care.
These resources come in the form of education and training (live or on demand); leadership and professional development; practice management assistance; advocacy work; mentored quality improvement; networking and project work (through special interest groups, local chapter meetings, and committee work); stimulation of research, new knowledge, and innovation; and promotion of evidence-based practice through our educational resources, publications, and other communications. The purpose of our existence is to provide you what you need to improve your work lives and your patients’ health.
SHM has always fostered a “big-tent” philosophy, so we will continue to explore ways to expand membership beyond “the core” of internal medicine, family medicine, and pediatrics, and reach a better understanding of what our constituents need and how we can add value to their work lives and careers. In addition to expanding membership within our borders, other expansions already include working with international chapters and members, with an “all teach, all learn” attitude to better understand mutually beneficial partnerships with international members. Through all these expansions, we will come closer to truly realizing our mission at SHM, which is to “promote exceptional care for hospitalized patients.”
My humble hope, as it is with any of my leadership positions, is to leave SHM better than I found it. As such, please contact me at any time if you have ideas or suggestions on how we can better help you be successful in improving the care for your patients, your systems, and health care as a whole. I look forward to serving you in this incredible journey and mission.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the medical editor of the Hospitalist, and president-elect of SHM.
Obtain proper reimbursements with more effective documentation and coding
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
SHM webinar series provides hospitalists with best practices to improve accuracy and compliance
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Hospitalists cannot bill for everything they do, but they can document and code to obtain appropriate reimbursements. It is important for hospitalists to know the factors that influence coding to ensure accuracy and compliance.
The Society of Hospital Medicine developed the Clinical Documentation & Coding for Hospitalists webinar series (formerly known as CODE-H) to provide hospitalists with the latest information on best practices in coding, documentation, and compliance from nationally recognized experts, along with the opportunity to claim CME.
The Hospitalist recently spoke with Carol Pohlig, BSN, RN, CPC, ACS, course director of the webinar series and a coding and documentation expert at the University of Pennsylvania Medical Center in Philadelphia. She was instrumental in developing the content in the series to ensure it was specifically designed to address challenges regularly faced by hospitalists.
What inspired the creation of Clinical Documentation & Coding for Hospitalists?
Providers are so busy trying to keep up with regulations for their institution, such as malpractice and quality issues, that the focus isn’t always on the documentation required for reimbursement. The creation of the series rose out of a need for providers to understand key issues related to documentation and billing and some of the hurdles that they need to overcome – or need to be aware of in the first place.
This series brings awareness and solutions to some of these problems. It is available on an ongoing basis, so viewers can move at their own pace. Given the wealth of information in the series, it made sense to create it in this format.
What are some common challenges that hospitalists encounter when coding, and how does this webinar series help to address these challenges?
Some common challenges relate to concurrent care or comanagement. Hospitalists are hired to be the gatekeepers – the ones overseeing patient care. When other consultants are on board, they wind up sharing responsibilities, which can muddy the waters at times, especially with billing and coding. It is important for hospitalists to understand their role in comanagement and, in turn, how the payers view their role.
We highlight everything – including requirements for history, exam, and medical decision making – and review each component in depth. We also discuss billing based on these key components or, when it is appropriate, billing based on time. However, when billing time-based services, you have to meet certain qualifications because it is different from the standard way of reporting, which is something we break down in the series.
Related to mitigating risk, EMRs and their copy and paste function is another topic we delve into. It’s easy to copy and paste and pull forward information from a previous note to help save time. However, it is important to understand what the ramifications are. Each of these copied and pasted encounters must be modified to make it applicable to the current day’s patient and ensure care is not being misrepresented.
Those are just a few of the items covered, but we believe that each of the eight modules in the series offers something unique that will help improve documentation and coding practices.
How can this webinar series go beyond the hospital medicine care team and more broadly affect the institution as a whole?
Hospitalists are often involved in a number of different categories of services, including observation and same-day admission/discharge. The series reviews rules and challenges specific to those sites of service, which on a broader scale, impact not only providers in other service lines but also those who work in the revenue cycle at the parent institution. How each of these parties understands the nuances explained in the series can directly affect the successful processing of the submitted claims.
In addition, interpretation of rules when it comes to coding and documentation can vary at a local level. We raise awareness of local interpretations to ensure everyone involved in the documentation and coding process knows things to look out for when reading rules. You might think it means one thing when, in reality, it could mean another. With this series, everyone involved with billing and coding can reflect on the implications that incorrect or inaccurate coding may have on their hospital.
Who would benefit from viewing this webinar series?
Although we primarily had hospitalists of all types – including physicians, nurse practitioners, and physician assistants – in mind during the development of course content, anyone who works as a practice manager, biller, coder, or internal auditor has the potential to benefit from the series. If they understand broader challenges in coding, it could help them proactively prevent issues throughout the process with more accurate documentation that could reduce claims denials.
Let SHM’s Clinical Documentation & Coding for Hospitalists webinar series bolster your and your team’s accuracy and compliance. Individual and group subscriptions are available. For more information, visit hospitalmedicine.org/coding.
Am I still a hospitalist?
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
HM as a force for change
HM as a force for change
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.
I wear a suit every day to work. I count the time between shifts in months, not days. Rather than looking for subtle diagnostic clues hidden in clinical information, I find myself up to my elbows in performance and financial data. Instead of meetings complicated by challenging family dynamics, I spend my time calming the waters between clinical departments that each feel slighted.
And yet, when people ask me what I do, I do not say I am a health system CEO. Rather, I am a hospitalist. I say it, not out of habit, but with pride and clear intention. Almost 20 years ago, I had to explain to my parents what a hospitalist was as I made the transition from primary care doctor to hospitalist. I told them that hospitalists take care of sick people who are in the hospital, but also are charged with making the hospital a better place to take care of people. I hope that in some small way, in every role I have had over the past 20 years as a hospitalist, I have been able to do that.
While the small changes we can all make every day are important, massive changes to health care, hospitals, and providers are coming. The forces driving these changes are manifold, complex, and powerful. Individual hospitalists, hospital groups, and hospitals will be challenged to keep up with responding to these changes. I hope, though, that our field, hospital medicine, will not be sitting there, waiting for the changes to come, but will instead be one of the forces for change.
I also believe that hospital medicine and health care delivery systems should drive the change in a coordinated and collaborative partnership. A partnership not built on self-advocacy but one in which we remember why we exist – to take care of people. A force for change that preserves the essential, evolves what needs improvement, and revolutionizes the archaic.
Partnerships between hospitalist groups and health care administration will always face the day-to-day challenges of balancing the need for resources with the ability to provide them, agreeing on how to measure and assess quality, and aligning rewards with priorities. However, by working together in venues that allow us to think beyond the day-to-day issues, we in hospital medicine will be leaders in the change that is coming. I believe that today, the Society of Hospital Medicine must be one of those venues. Through its committees, meetings, advocacy, publications, and most importantly, members, SHM will continue to shape the future of care delivery in this country and beyond.
SHM has been my professional home for almost 20 years, helping me think about how to make the hospital a better place to take care of people. Recent examples of SHM and its members partnering in this area include advocacy work to improve alternative payment models, such as Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), as well as educational efforts for its members on how to navigate the current rules around MACRA.
For many years, SHM has been the leader in professional organizations for leading the way on quality improvement. Through the Center for Quality Improvement, SHM not only offers robust educational tools to better enable members to lead efforts at their home institutions but also has led multi-institutional efforts to reduce harm that have been recognized nationally for their impact.
As we move further down the path from volume to value toward population health, the SHM Board will be sure that the society continues to be a leader for both its members and the health system at large as we face these changes. We have the opportunity in front of us to collectively embrace and create the changes coming toward us with that shared purpose of making wherever it is that we care for people better places to provide that care. How could one not be proud to say, with intent, “I am a hospitalist,” regardless of what it is that brings each of us to SHM.
Dr. Whelan is CEO of Banner–University Medical Center Tucson (Ariz.) and a member of the SHM Board of Directors.