User login
New-onset AF after aortic valve replacement did not affect long-term survival
New-onset atrial fibrillation after aortic valve replacement was not an independent risk factor for decreased long-term survival, according to the results of a single-center, retrospective study reported by Ben M. Swinkels, MD, of St Antonius Hospital, Nieuwegein, and his colleagues in the Netherlands.
Key to this success, however, is restoring normal sinus rhythm before hospital discharge, they said.
In this retrospective, longitudinal cohort study, 569 consecutive patients with no history of AF who underwent AVR with or without concomitant coronary artery bypass grafting during 1990-1993 were followed for a mean of 17.8 years (J Thorac Cardiovasc Surg. 2017;154:492-8).
Thirty-day and long-term survival rates were determined in the 241 patients (42%) with and the 328 patients (58%) without new-onset postoperative atrial fibrillation (POAF), which was defined as electrocardiographically documented AF lasting for at least several hours, and occurring after AVR while the patient was still admitted. Standard therapy to prevent new onset POAF was the use of sotalol in patients who were not on beta-blocker therapy, and continuation of beta-blocker therapy for those who were already on it.
There were no significant differences between the two groups in demographic characteristics. There were also no significant differences between the two groups in operative characteristics, postoperative in-hospital adverse events, and postoperative hospital lengths of stay until discharge home, except for mechanical ventilation time, which was significantly longer in the patients with new-onset POAF (P = .011).
Thirty-day mortality was 1.2% in the patients with POAF, and 2.7% in those without, a nonsignificant difference. There was no statistically significant difference between the two survival curves and the Kaplan-Meier overall cumulative survival rates at 15 years of follow-up in the patients with new-onset POAF vs. those without were not statistically different (41.5% vs. 41.3%, respectively).
In addition, the 18-year probability of long-term first adverse events, including recurrent AF, transient ischemic attack, ischemic or hemorrhagic stroke, peripheral venous thromboembolism, or major or minor bleeding was not significantly different between the two groups.
“New-onset POAF after AVR does not affect long-term survival when treatment is aimed to restore sinus rhythm before the patient is discharged home. Future studies with a prospective, randomized design should be done to confirm this finding in patients undergoing different kinds of cardiac surgery,” the researchers concluded.
The study was funded by the authors’ home institution; the authors reported they had nothing to disclose.
The incidence of atrial fibrillation after valve surgery has been described to be as high as 50%, Manuel J. Antunes, MD, said in an editorial commentary. “The adverse effect on long-term survival may not be related to the short-lived new-onset AF but rather to the underlying pathology associated to the arrhythmia, especially pathology that affects the myocardium, principally in atherosclerotic coronary artery disease,” he wrote. “It is not survival alone, however, that should be cause for concern; AF, even in episodes of limited duration, may result in transient ischemic attacks, ischemic, or hemorrhagic strokes, and peripheral thromboembolism, which is why affected patients should immediately be anticoagulated.”
This study, however, is at odds with previously published studies, with opposite conclusions, according to Dr. Antunes. Swinkels and his colleagues suggest that one of the reasons for the discrepancy was the homogeneous character of their series, which consisted almost entirely of patients who had isolated AVR. Dr. Antunes also adds that another important aspect to consider is that the antiarrhythmic drugs used prophylactically or therapeutically for this patient cohort (treated during 1990-1993) are no longer used or have been replaced by new and more efficacious pharmacologic agents.
Manuel J. Antunes, MD, of the University Hospital and Faculty of Medicine, Coimbra, Portugal, made these remarks in an invited editorial (J Thorac Cardiovasc Surg. 2017;154:490-1). He reported having nothing to disclose.
The incidence of atrial fibrillation after valve surgery has been described to be as high as 50%, Manuel J. Antunes, MD, said in an editorial commentary. “The adverse effect on long-term survival may not be related to the short-lived new-onset AF but rather to the underlying pathology associated to the arrhythmia, especially pathology that affects the myocardium, principally in atherosclerotic coronary artery disease,” he wrote. “It is not survival alone, however, that should be cause for concern; AF, even in episodes of limited duration, may result in transient ischemic attacks, ischemic, or hemorrhagic strokes, and peripheral thromboembolism, which is why affected patients should immediately be anticoagulated.”
This study, however, is at odds with previously published studies, with opposite conclusions, according to Dr. Antunes. Swinkels and his colleagues suggest that one of the reasons for the discrepancy was the homogeneous character of their series, which consisted almost entirely of patients who had isolated AVR. Dr. Antunes also adds that another important aspect to consider is that the antiarrhythmic drugs used prophylactically or therapeutically for this patient cohort (treated during 1990-1993) are no longer used or have been replaced by new and more efficacious pharmacologic agents.
Manuel J. Antunes, MD, of the University Hospital and Faculty of Medicine, Coimbra, Portugal, made these remarks in an invited editorial (J Thorac Cardiovasc Surg. 2017;154:490-1). He reported having nothing to disclose.
The incidence of atrial fibrillation after valve surgery has been described to be as high as 50%, Manuel J. Antunes, MD, said in an editorial commentary. “The adverse effect on long-term survival may not be related to the short-lived new-onset AF but rather to the underlying pathology associated to the arrhythmia, especially pathology that affects the myocardium, principally in atherosclerotic coronary artery disease,” he wrote. “It is not survival alone, however, that should be cause for concern; AF, even in episodes of limited duration, may result in transient ischemic attacks, ischemic, or hemorrhagic strokes, and peripheral thromboembolism, which is why affected patients should immediately be anticoagulated.”
This study, however, is at odds with previously published studies, with opposite conclusions, according to Dr. Antunes. Swinkels and his colleagues suggest that one of the reasons for the discrepancy was the homogeneous character of their series, which consisted almost entirely of patients who had isolated AVR. Dr. Antunes also adds that another important aspect to consider is that the antiarrhythmic drugs used prophylactically or therapeutically for this patient cohort (treated during 1990-1993) are no longer used or have been replaced by new and more efficacious pharmacologic agents.
Manuel J. Antunes, MD, of the University Hospital and Faculty of Medicine, Coimbra, Portugal, made these remarks in an invited editorial (J Thorac Cardiovasc Surg. 2017;154:490-1). He reported having nothing to disclose.
New-onset atrial fibrillation after aortic valve replacement was not an independent risk factor for decreased long-term survival, according to the results of a single-center, retrospective study reported by Ben M. Swinkels, MD, of St Antonius Hospital, Nieuwegein, and his colleagues in the Netherlands.
Key to this success, however, is restoring normal sinus rhythm before hospital discharge, they said.
In this retrospective, longitudinal cohort study, 569 consecutive patients with no history of AF who underwent AVR with or without concomitant coronary artery bypass grafting during 1990-1993 were followed for a mean of 17.8 years (J Thorac Cardiovasc Surg. 2017;154:492-8).
Thirty-day and long-term survival rates were determined in the 241 patients (42%) with and the 328 patients (58%) without new-onset postoperative atrial fibrillation (POAF), which was defined as electrocardiographically documented AF lasting for at least several hours, and occurring after AVR while the patient was still admitted. Standard therapy to prevent new onset POAF was the use of sotalol in patients who were not on beta-blocker therapy, and continuation of beta-blocker therapy for those who were already on it.
There were no significant differences between the two groups in demographic characteristics. There were also no significant differences between the two groups in operative characteristics, postoperative in-hospital adverse events, and postoperative hospital lengths of stay until discharge home, except for mechanical ventilation time, which was significantly longer in the patients with new-onset POAF (P = .011).
Thirty-day mortality was 1.2% in the patients with POAF, and 2.7% in those without, a nonsignificant difference. There was no statistically significant difference between the two survival curves and the Kaplan-Meier overall cumulative survival rates at 15 years of follow-up in the patients with new-onset POAF vs. those without were not statistically different (41.5% vs. 41.3%, respectively).
In addition, the 18-year probability of long-term first adverse events, including recurrent AF, transient ischemic attack, ischemic or hemorrhagic stroke, peripheral venous thromboembolism, or major or minor bleeding was not significantly different between the two groups.
“New-onset POAF after AVR does not affect long-term survival when treatment is aimed to restore sinus rhythm before the patient is discharged home. Future studies with a prospective, randomized design should be done to confirm this finding in patients undergoing different kinds of cardiac surgery,” the researchers concluded.
The study was funded by the authors’ home institution; the authors reported they had nothing to disclose.
New-onset atrial fibrillation after aortic valve replacement was not an independent risk factor for decreased long-term survival, according to the results of a single-center, retrospective study reported by Ben M. Swinkels, MD, of St Antonius Hospital, Nieuwegein, and his colleagues in the Netherlands.
Key to this success, however, is restoring normal sinus rhythm before hospital discharge, they said.
In this retrospective, longitudinal cohort study, 569 consecutive patients with no history of AF who underwent AVR with or without concomitant coronary artery bypass grafting during 1990-1993 were followed for a mean of 17.8 years (J Thorac Cardiovasc Surg. 2017;154:492-8).
Thirty-day and long-term survival rates were determined in the 241 patients (42%) with and the 328 patients (58%) without new-onset postoperative atrial fibrillation (POAF), which was defined as electrocardiographically documented AF lasting for at least several hours, and occurring after AVR while the patient was still admitted. Standard therapy to prevent new onset POAF was the use of sotalol in patients who were not on beta-blocker therapy, and continuation of beta-blocker therapy for those who were already on it.
There were no significant differences between the two groups in demographic characteristics. There were also no significant differences between the two groups in operative characteristics, postoperative in-hospital adverse events, and postoperative hospital lengths of stay until discharge home, except for mechanical ventilation time, which was significantly longer in the patients with new-onset POAF (P = .011).
Thirty-day mortality was 1.2% in the patients with POAF, and 2.7% in those without, a nonsignificant difference. There was no statistically significant difference between the two survival curves and the Kaplan-Meier overall cumulative survival rates at 15 years of follow-up in the patients with new-onset POAF vs. those without were not statistically different (41.5% vs. 41.3%, respectively).
In addition, the 18-year probability of long-term first adverse events, including recurrent AF, transient ischemic attack, ischemic or hemorrhagic stroke, peripheral venous thromboembolism, or major or minor bleeding was not significantly different between the two groups.
“New-onset POAF after AVR does not affect long-term survival when treatment is aimed to restore sinus rhythm before the patient is discharged home. Future studies with a prospective, randomized design should be done to confirm this finding in patients undergoing different kinds of cardiac surgery,” the researchers concluded.
The study was funded by the authors’ home institution; the authors reported they had nothing to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:
Major finding: Cumulative 15-year survival rates were similar in the patients with new-onset postop AF (41.5%) to those without (41.3%).
Data source: A retrospective longitudinal cohort study of 569 consecutive patients without a history of AF who were followed for a mean of 17.8 years after AVR with or without concomitant CABG.
Disclosures: The study was funded by the authors’ home institution and the authors reported they had nothing to disclose.
Preop atrial fib in CABG patients spells trouble
COLORADO SPRINGS – Preoperative atrial fibrillation is present in more than 10% of patients undergoing isolated coronary artery bypass graft (CABG) surgery, and if not subjected to concomitant surgical ablation it’s associated with increased perioperative and long-term major morbidity and mortality, S. Chris Malaisrie, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
The increased early and late risks posed by preoperative atrial fibrillation (AF) that go unaddressed remain significant even after adjusting for the numerous comorbid conditions more prevalent in CABG patients with preoperative AF than in those without the arrhythmia, added Dr. Malaisrie, a cardiac surgeon at Northwestern University in Chicago.
The unadjusted operative mortality rate was 1.8% in the no-AF group and 4.0% in patients with preoperative AF. Unadjusted in-hospital rates of permanent stroke, prolonged ventilation, reoperation, and new renal failure were also significantly higher in the preoperative AF group.
Not surprisingly, the preoperative AF group was older. They also had significantly higher baseline rates of numerous comorbid conditions, including diabetes, peripheral vascular disease, renal failure, and prior stroke, as well as a lower mean left ventricular ejection fraction. However, after adjustment for the many comorbidities in multivariate regression analysis, the risks of all in-hospital adverse outcomes remained significantly higher in the preoperative AF group. For example, their adjusted risk of operative mortality was 1.5-fold greater than in the no-AF patients.
In the long-term follow-up analysis, the unadjusted risk of mortality in the first 5 years after CABG was 2.5-fold greater in the preoperative AF group. Their 5-year risk of stroke or systemic embolization was 1.5-fold greater, too. Upon adjustment for potentially confounding comorbid conditions, preoperative AF was associated with a 1.5-fold increased 5-year risk of mortality and a 1.2-fold increase in stroke or systemic embolism.
In an effort to identify a particularly high-risk group of CABG patients with preoperative AF, Dr. Malaisrie and his coinvestigators stratified the group’s long-term stroke and mortality risks by their CHA2DS2-VASc score at the time of surgery. The results were revealing: the unadjusted 5-year risk of stroke or systemic embolization was 7.9% in those with a CHA2DS2-VASc score of 1-3, 12.2% with a score of 4-6, and 15.4% with a score of 7-9. The 5-year survival rate was 74.8% with a score of 1-3, 56.5% with a score of 4-6, and 41.2% with a score of 7-9.
“That’s really a striking finding,” Dr. Malaisrie observed. “When you consider a patient who’s, say, 72-75 years old, who is undergoing isolated CABG with preoperative atrial fibrillation and who has a high CHA2DS2-VASc score of 7-9, 5-year survival is only 41%, with a 15% risk of stroke or systemic embolization.”
Discussant William T. Caine, MD, found the study results unsettling.
“I was surprised to see that in this day and age, fully two-thirds of the patients who had preoperative atrial fibrillation had no attempt at any ablation procedure to treat their atrial fibrillation,” declared Dr. Caine of Intermountain Medical Center in Salt Lake City.
In reply, Dr. Malaisrie noted that other, smaller studies have also found that only about 30% of CABG patients with preoperative AF undergo surgical AF ablation through a maze procedure or some other method.
“Probably most of us in this room would go ahead and perform surgical ablation, but the STS database represents all isolated CABG procedures done throughout the United States,” Dr. Malaisrie said. “I think this dataset should help convince the other 70% of surgeons out there that there is a high cost for preoperative AF – in particular, in patients with very high CHA2DS2-VASc scores. If you can identify a group of patients at increased risk for stroke and mortality, you’d certainly want to bend their survival curve.”
The maze procedure has been convincingly shown to be very safe, with no associated increased risk of perioperative morbidity and mortality. The downside is cost. But while it’s true that adding surgical ablation to an isolated CABG procedure boosts OR time and procedural costs, a successful ablation is likely to pay dividends through reduced downstream rates of major morbidity and mortality.
“I look forward to the second part of our analysis, where we’ll look at the comparative data for the patients who did in fact have surgical ablation. That dataset is pending from the Duke Clinical Research Institute,” according to Dr. Malaisrie.
He cited as study limitations the inability to complete linkage to the Medicare database in about 37% of CABG patients in the STS database, or more than 200,000 people. Also, the Medicare database is an administrative dataset reliant upon medical record coding. The mortality data are probably quite accurate, but the stroke and systemic embolization rates cited in this analysis likely underestimate the true rates.
He reported serving as a consultant to Edwards Lifesciences, Abbott Vascular, and Baxter, and serving on speakers’ bureaus for Bolton and Abiomed. However, the STS analysis was funded exclusively by philanthropy.
COLORADO SPRINGS – Preoperative atrial fibrillation is present in more than 10% of patients undergoing isolated coronary artery bypass graft (CABG) surgery, and if not subjected to concomitant surgical ablation it’s associated with increased perioperative and long-term major morbidity and mortality, S. Chris Malaisrie, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
The increased early and late risks posed by preoperative atrial fibrillation (AF) that go unaddressed remain significant even after adjusting for the numerous comorbid conditions more prevalent in CABG patients with preoperative AF than in those without the arrhythmia, added Dr. Malaisrie, a cardiac surgeon at Northwestern University in Chicago.
The unadjusted operative mortality rate was 1.8% in the no-AF group and 4.0% in patients with preoperative AF. Unadjusted in-hospital rates of permanent stroke, prolonged ventilation, reoperation, and new renal failure were also significantly higher in the preoperative AF group.
Not surprisingly, the preoperative AF group was older. They also had significantly higher baseline rates of numerous comorbid conditions, including diabetes, peripheral vascular disease, renal failure, and prior stroke, as well as a lower mean left ventricular ejection fraction. However, after adjustment for the many comorbidities in multivariate regression analysis, the risks of all in-hospital adverse outcomes remained significantly higher in the preoperative AF group. For example, their adjusted risk of operative mortality was 1.5-fold greater than in the no-AF patients.
In the long-term follow-up analysis, the unadjusted risk of mortality in the first 5 years after CABG was 2.5-fold greater in the preoperative AF group. Their 5-year risk of stroke or systemic embolization was 1.5-fold greater, too. Upon adjustment for potentially confounding comorbid conditions, preoperative AF was associated with a 1.5-fold increased 5-year risk of mortality and a 1.2-fold increase in stroke or systemic embolism.
In an effort to identify a particularly high-risk group of CABG patients with preoperative AF, Dr. Malaisrie and his coinvestigators stratified the group’s long-term stroke and mortality risks by their CHA2DS2-VASc score at the time of surgery. The results were revealing: the unadjusted 5-year risk of stroke or systemic embolization was 7.9% in those with a CHA2DS2-VASc score of 1-3, 12.2% with a score of 4-6, and 15.4% with a score of 7-9. The 5-year survival rate was 74.8% with a score of 1-3, 56.5% with a score of 4-6, and 41.2% with a score of 7-9.
“That’s really a striking finding,” Dr. Malaisrie observed. “When you consider a patient who’s, say, 72-75 years old, who is undergoing isolated CABG with preoperative atrial fibrillation and who has a high CHA2DS2-VASc score of 7-9, 5-year survival is only 41%, with a 15% risk of stroke or systemic embolization.”
Discussant William T. Caine, MD, found the study results unsettling.
“I was surprised to see that in this day and age, fully two-thirds of the patients who had preoperative atrial fibrillation had no attempt at any ablation procedure to treat their atrial fibrillation,” declared Dr. Caine of Intermountain Medical Center in Salt Lake City.
In reply, Dr. Malaisrie noted that other, smaller studies have also found that only about 30% of CABG patients with preoperative AF undergo surgical AF ablation through a maze procedure or some other method.
“Probably most of us in this room would go ahead and perform surgical ablation, but the STS database represents all isolated CABG procedures done throughout the United States,” Dr. Malaisrie said. “I think this dataset should help convince the other 70% of surgeons out there that there is a high cost for preoperative AF – in particular, in patients with very high CHA2DS2-VASc scores. If you can identify a group of patients at increased risk for stroke and mortality, you’d certainly want to bend their survival curve.”
The maze procedure has been convincingly shown to be very safe, with no associated increased risk of perioperative morbidity and mortality. The downside is cost. But while it’s true that adding surgical ablation to an isolated CABG procedure boosts OR time and procedural costs, a successful ablation is likely to pay dividends through reduced downstream rates of major morbidity and mortality.
“I look forward to the second part of our analysis, where we’ll look at the comparative data for the patients who did in fact have surgical ablation. That dataset is pending from the Duke Clinical Research Institute,” according to Dr. Malaisrie.
He cited as study limitations the inability to complete linkage to the Medicare database in about 37% of CABG patients in the STS database, or more than 200,000 people. Also, the Medicare database is an administrative dataset reliant upon medical record coding. The mortality data are probably quite accurate, but the stroke and systemic embolization rates cited in this analysis likely underestimate the true rates.
He reported serving as a consultant to Edwards Lifesciences, Abbott Vascular, and Baxter, and serving on speakers’ bureaus for Bolton and Abiomed. However, the STS analysis was funded exclusively by philanthropy.
COLORADO SPRINGS – Preoperative atrial fibrillation is present in more than 10% of patients undergoing isolated coronary artery bypass graft (CABG) surgery, and if not subjected to concomitant surgical ablation it’s associated with increased perioperative and long-term major morbidity and mortality, S. Chris Malaisrie, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
The increased early and late risks posed by preoperative atrial fibrillation (AF) that go unaddressed remain significant even after adjusting for the numerous comorbid conditions more prevalent in CABG patients with preoperative AF than in those without the arrhythmia, added Dr. Malaisrie, a cardiac surgeon at Northwestern University in Chicago.
The unadjusted operative mortality rate was 1.8% in the no-AF group and 4.0% in patients with preoperative AF. Unadjusted in-hospital rates of permanent stroke, prolonged ventilation, reoperation, and new renal failure were also significantly higher in the preoperative AF group.
Not surprisingly, the preoperative AF group was older. They also had significantly higher baseline rates of numerous comorbid conditions, including diabetes, peripheral vascular disease, renal failure, and prior stroke, as well as a lower mean left ventricular ejection fraction. However, after adjustment for the many comorbidities in multivariate regression analysis, the risks of all in-hospital adverse outcomes remained significantly higher in the preoperative AF group. For example, their adjusted risk of operative mortality was 1.5-fold greater than in the no-AF patients.
In the long-term follow-up analysis, the unadjusted risk of mortality in the first 5 years after CABG was 2.5-fold greater in the preoperative AF group. Their 5-year risk of stroke or systemic embolization was 1.5-fold greater, too. Upon adjustment for potentially confounding comorbid conditions, preoperative AF was associated with a 1.5-fold increased 5-year risk of mortality and a 1.2-fold increase in stroke or systemic embolism.
In an effort to identify a particularly high-risk group of CABG patients with preoperative AF, Dr. Malaisrie and his coinvestigators stratified the group’s long-term stroke and mortality risks by their CHA2DS2-VASc score at the time of surgery. The results were revealing: the unadjusted 5-year risk of stroke or systemic embolization was 7.9% in those with a CHA2DS2-VASc score of 1-3, 12.2% with a score of 4-6, and 15.4% with a score of 7-9. The 5-year survival rate was 74.8% with a score of 1-3, 56.5% with a score of 4-6, and 41.2% with a score of 7-9.
“That’s really a striking finding,” Dr. Malaisrie observed. “When you consider a patient who’s, say, 72-75 years old, who is undergoing isolated CABG with preoperative atrial fibrillation and who has a high CHA2DS2-VASc score of 7-9, 5-year survival is only 41%, with a 15% risk of stroke or systemic embolization.”
Discussant William T. Caine, MD, found the study results unsettling.
“I was surprised to see that in this day and age, fully two-thirds of the patients who had preoperative atrial fibrillation had no attempt at any ablation procedure to treat their atrial fibrillation,” declared Dr. Caine of Intermountain Medical Center in Salt Lake City.
In reply, Dr. Malaisrie noted that other, smaller studies have also found that only about 30% of CABG patients with preoperative AF undergo surgical AF ablation through a maze procedure or some other method.
“Probably most of us in this room would go ahead and perform surgical ablation, but the STS database represents all isolated CABG procedures done throughout the United States,” Dr. Malaisrie said. “I think this dataset should help convince the other 70% of surgeons out there that there is a high cost for preoperative AF – in particular, in patients with very high CHA2DS2-VASc scores. If you can identify a group of patients at increased risk for stroke and mortality, you’d certainly want to bend their survival curve.”
The maze procedure has been convincingly shown to be very safe, with no associated increased risk of perioperative morbidity and mortality. The downside is cost. But while it’s true that adding surgical ablation to an isolated CABG procedure boosts OR time and procedural costs, a successful ablation is likely to pay dividends through reduced downstream rates of major morbidity and mortality.
“I look forward to the second part of our analysis, where we’ll look at the comparative data for the patients who did in fact have surgical ablation. That dataset is pending from the Duke Clinical Research Institute,” according to Dr. Malaisrie.
He cited as study limitations the inability to complete linkage to the Medicare database in about 37% of CABG patients in the STS database, or more than 200,000 people. Also, the Medicare database is an administrative dataset reliant upon medical record coding. The mortality data are probably quite accurate, but the stroke and systemic embolization rates cited in this analysis likely underestimate the true rates.
He reported serving as a consultant to Edwards Lifesciences, Abbott Vascular, and Baxter, and serving on speakers’ bureaus for Bolton and Abiomed. However, the STS analysis was funded exclusively by philanthropy.
AT THE WTSA ANNUAL MEETING
Key clinical point:
Major finding: Preoperative AF in patients undergoing isolated CABG was tied to an adjusted 45% greater 5-year mortality and 25% increase in stroke and systemic embolization risk, compared with CABG patients without the preoperative arrhythmia.
Data source: This retrospective study compared perioperative and long-term morbidity and mortality in nearly 350,000 patients in the Society of Thoracic Surgeons database who underwent isolated CABG, including more than 24,000 who had preoperative atrial fibrillation that wasn’t addressed surgically.
Disclosures: The study presenter reported serving as a consultant to Edwards Lifesciences, Abbott Vascular, and Baxter, and serving on speakers’ bureaus for Bolton and Abiomed. However, the STS analysis was funded exclusively by philanthropy.
First trial of TAVR vs. SAVR in low-risk patients
PARIS – Five-year hemodynamic results of the first randomized trial of transcatheter versus surgical aortic valve replacement in low-surgical-risk patients with severe aortic stenosis showed continued superior valve performance in the TAVR group, Lars Sondergaard, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The durability results are very encouraging. We can’t see that the TAVR patients are doing worse. So I think this is setting the scene to try to move forward in patients at low risk and also in younger patients,” declared Dr. Sondergaard, professor of cardiology at the University of Copenhagen.
He presented an update from the Nordic Aortic Valve Intervention (NOTION) trial, a prospective, multicenter, randomized, all-comers clinical trial in which 280 patients with symptomatic severe aortic stenosis at low surgical risk were assigned to surgical aortic valve replacement (SAVR) or to TAVR with the self-expanding CoreValve. Their mean age was 79 years, with an average Society of Thoracic Surgeons projected risk of mortality score of 3%. Eighty-two percent of participants had an STS score below 4%. Roughly 40% of TAVR patients got the first-generation CoreValve in the 26-mm size, 40% received the 29-mm version, and the rest got the 31-mm CoreValve.
Among patients in the lowest-surgical-risk and youngest subgroup – those aged 70-75 with a Society of Thoracic Surgeons risk score below 4% – the composite primary endpoint rate at 4 years was 15.6% with TAVR compared with 27.2% with SAVR. However, only 62 NOTION participants fell into this category, so the between-group difference, while sizable, didn’t achieve statistical significance, according to Dr. Sondergaard.
There was a trade-off between the two valve replacement strategies with regard to procedural complications. The rate of new-onset atrial fibrillation was far higher in the SAVR group: 59.4% at 1 year and 60.2% at 4 years of follow-up, compared with 21.2% and 24.5% at 1 and 4 years, respectively, in the TAVR group.
On the other hand, 38% of the TAVR patients got a new pacemaker within the first year of follow-up, compared with only 2.4% in the SAVR group. At 4 years, 43.7% of the TAVR group had a pacemaker, versus 9% of the SAVR group.
Turning to the hemodynamic data, the cardiologist noted that the effective orifice area in the TAVR group went from 0.71 cm2 at baseline to 1.66 at 1 year and remained steady thereafter at 1.67 cm2 through 5 years. The TAVR group’s mean gradient improved from 45.4 mm Hg at baseline to 8.6 mm Hg at 1 year and 7.9 mm Hg at 5 years. These outcomes were significantly better than in the SAVR group, where the effective orifice area went from 0.74 cm2 at baseline to 1.32 at 1 year and 1.24 cm2 at 5 years, while the mean gradient fell from 44.9 mm Hg to 12.5 at 1 year and 13.6 mm Hg at 5 years.
Moderate hemodynamic structural valve deterioration was significantly more common in the SAVR group: 20.7% at 5 years, compared with 2.9% in the TAVR patients. The opposite was true with regard to moderate paravalvular leak, which occurred in 20.9% of the TAVI group but only 1.5% of SAVR patients.
Late complications were rare following either procedure. There were no cases of valve thrombosis through 5 years. The incidence of endocarditis at 5 years was 4.3% in the TAVR patients and similar at 5.9% in the SAVR group.
Discussant Samer Mansour, MD, of the University of Montreal, remarked that the rate of new pacemaker implantation following TAVR seemed extraordinarily high.
“This was early days,” Dr. Sondergaard explained. “We had a lower threshold for putting in a pacemaker and we put the valves in a little deeper.”
About half of new pacemaker recipients didn’t use the device after the first year, he added. Also, neither getting a new pacemaker nor moderate paravalvular leak was associated with increased mortality in the TAVR group.
Dr. Mansour observed that subtle but real differences in mortality probably wouldn’t show up in a 280-patient trial. Dr. Sondergaard concurred.
“We designed the NOTION trial in 2008-2009. Knowing what we know now, we should have had a larger study, but at that time TAVR volume wasn’t that big and it wasn’t realistic as a Nordic trial to include 1,000 patients. This was the best we could do,” he said.
Follow-up in the NOTION study will continue out to 10 years.
The study is funded by Medtronic. Dr. Sondergaard reported serving as a consultant to and receiving research grant support from the company.
PARIS – Five-year hemodynamic results of the first randomized trial of transcatheter versus surgical aortic valve replacement in low-surgical-risk patients with severe aortic stenosis showed continued superior valve performance in the TAVR group, Lars Sondergaard, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The durability results are very encouraging. We can’t see that the TAVR patients are doing worse. So I think this is setting the scene to try to move forward in patients at low risk and also in younger patients,” declared Dr. Sondergaard, professor of cardiology at the University of Copenhagen.
He presented an update from the Nordic Aortic Valve Intervention (NOTION) trial, a prospective, multicenter, randomized, all-comers clinical trial in which 280 patients with symptomatic severe aortic stenosis at low surgical risk were assigned to surgical aortic valve replacement (SAVR) or to TAVR with the self-expanding CoreValve. Their mean age was 79 years, with an average Society of Thoracic Surgeons projected risk of mortality score of 3%. Eighty-two percent of participants had an STS score below 4%. Roughly 40% of TAVR patients got the first-generation CoreValve in the 26-mm size, 40% received the 29-mm version, and the rest got the 31-mm CoreValve.
Among patients in the lowest-surgical-risk and youngest subgroup – those aged 70-75 with a Society of Thoracic Surgeons risk score below 4% – the composite primary endpoint rate at 4 years was 15.6% with TAVR compared with 27.2% with SAVR. However, only 62 NOTION participants fell into this category, so the between-group difference, while sizable, didn’t achieve statistical significance, according to Dr. Sondergaard.
There was a trade-off between the two valve replacement strategies with regard to procedural complications. The rate of new-onset atrial fibrillation was far higher in the SAVR group: 59.4% at 1 year and 60.2% at 4 years of follow-up, compared with 21.2% and 24.5% at 1 and 4 years, respectively, in the TAVR group.
On the other hand, 38% of the TAVR patients got a new pacemaker within the first year of follow-up, compared with only 2.4% in the SAVR group. At 4 years, 43.7% of the TAVR group had a pacemaker, versus 9% of the SAVR group.
Turning to the hemodynamic data, the cardiologist noted that the effective orifice area in the TAVR group went from 0.71 cm2 at baseline to 1.66 at 1 year and remained steady thereafter at 1.67 cm2 through 5 years. The TAVR group’s mean gradient improved from 45.4 mm Hg at baseline to 8.6 mm Hg at 1 year and 7.9 mm Hg at 5 years. These outcomes were significantly better than in the SAVR group, where the effective orifice area went from 0.74 cm2 at baseline to 1.32 at 1 year and 1.24 cm2 at 5 years, while the mean gradient fell from 44.9 mm Hg to 12.5 at 1 year and 13.6 mm Hg at 5 years.
Moderate hemodynamic structural valve deterioration was significantly more common in the SAVR group: 20.7% at 5 years, compared with 2.9% in the TAVR patients. The opposite was true with regard to moderate paravalvular leak, which occurred in 20.9% of the TAVI group but only 1.5% of SAVR patients.
Late complications were rare following either procedure. There were no cases of valve thrombosis through 5 years. The incidence of endocarditis at 5 years was 4.3% in the TAVR patients and similar at 5.9% in the SAVR group.
Discussant Samer Mansour, MD, of the University of Montreal, remarked that the rate of new pacemaker implantation following TAVR seemed extraordinarily high.
“This was early days,” Dr. Sondergaard explained. “We had a lower threshold for putting in a pacemaker and we put the valves in a little deeper.”
About half of new pacemaker recipients didn’t use the device after the first year, he added. Also, neither getting a new pacemaker nor moderate paravalvular leak was associated with increased mortality in the TAVR group.
Dr. Mansour observed that subtle but real differences in mortality probably wouldn’t show up in a 280-patient trial. Dr. Sondergaard concurred.
“We designed the NOTION trial in 2008-2009. Knowing what we know now, we should have had a larger study, but at that time TAVR volume wasn’t that big and it wasn’t realistic as a Nordic trial to include 1,000 patients. This was the best we could do,” he said.
Follow-up in the NOTION study will continue out to 10 years.
The study is funded by Medtronic. Dr. Sondergaard reported serving as a consultant to and receiving research grant support from the company.
PARIS – Five-year hemodynamic results of the first randomized trial of transcatheter versus surgical aortic valve replacement in low-surgical-risk patients with severe aortic stenosis showed continued superior valve performance in the TAVR group, Lars Sondergaard, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The durability results are very encouraging. We can’t see that the TAVR patients are doing worse. So I think this is setting the scene to try to move forward in patients at low risk and also in younger patients,” declared Dr. Sondergaard, professor of cardiology at the University of Copenhagen.
He presented an update from the Nordic Aortic Valve Intervention (NOTION) trial, a prospective, multicenter, randomized, all-comers clinical trial in which 280 patients with symptomatic severe aortic stenosis at low surgical risk were assigned to surgical aortic valve replacement (SAVR) or to TAVR with the self-expanding CoreValve. Their mean age was 79 years, with an average Society of Thoracic Surgeons projected risk of mortality score of 3%. Eighty-two percent of participants had an STS score below 4%. Roughly 40% of TAVR patients got the first-generation CoreValve in the 26-mm size, 40% received the 29-mm version, and the rest got the 31-mm CoreValve.
Among patients in the lowest-surgical-risk and youngest subgroup – those aged 70-75 with a Society of Thoracic Surgeons risk score below 4% – the composite primary endpoint rate at 4 years was 15.6% with TAVR compared with 27.2% with SAVR. However, only 62 NOTION participants fell into this category, so the between-group difference, while sizable, didn’t achieve statistical significance, according to Dr. Sondergaard.
There was a trade-off between the two valve replacement strategies with regard to procedural complications. The rate of new-onset atrial fibrillation was far higher in the SAVR group: 59.4% at 1 year and 60.2% at 4 years of follow-up, compared with 21.2% and 24.5% at 1 and 4 years, respectively, in the TAVR group.
On the other hand, 38% of the TAVR patients got a new pacemaker within the first year of follow-up, compared with only 2.4% in the SAVR group. At 4 years, 43.7% of the TAVR group had a pacemaker, versus 9% of the SAVR group.
Turning to the hemodynamic data, the cardiologist noted that the effective orifice area in the TAVR group went from 0.71 cm2 at baseline to 1.66 at 1 year and remained steady thereafter at 1.67 cm2 through 5 years. The TAVR group’s mean gradient improved from 45.4 mm Hg at baseline to 8.6 mm Hg at 1 year and 7.9 mm Hg at 5 years. These outcomes were significantly better than in the SAVR group, where the effective orifice area went from 0.74 cm2 at baseline to 1.32 at 1 year and 1.24 cm2 at 5 years, while the mean gradient fell from 44.9 mm Hg to 12.5 at 1 year and 13.6 mm Hg at 5 years.
Moderate hemodynamic structural valve deterioration was significantly more common in the SAVR group: 20.7% at 5 years, compared with 2.9% in the TAVR patients. The opposite was true with regard to moderate paravalvular leak, which occurred in 20.9% of the TAVI group but only 1.5% of SAVR patients.
Late complications were rare following either procedure. There were no cases of valve thrombosis through 5 years. The incidence of endocarditis at 5 years was 4.3% in the TAVR patients and similar at 5.9% in the SAVR group.
Discussant Samer Mansour, MD, of the University of Montreal, remarked that the rate of new pacemaker implantation following TAVR seemed extraordinarily high.
“This was early days,” Dr. Sondergaard explained. “We had a lower threshold for putting in a pacemaker and we put the valves in a little deeper.”
About half of new pacemaker recipients didn’t use the device after the first year, he added. Also, neither getting a new pacemaker nor moderate paravalvular leak was associated with increased mortality in the TAVR group.
Dr. Mansour observed that subtle but real differences in mortality probably wouldn’t show up in a 280-patient trial. Dr. Sondergaard concurred.
“We designed the NOTION trial in 2008-2009. Knowing what we know now, we should have had a larger study, but at that time TAVR volume wasn’t that big and it wasn’t realistic as a Nordic trial to include 1,000 patients. This was the best we could do,” he said.
Follow-up in the NOTION study will continue out to 10 years.
The study is funded by Medtronic. Dr. Sondergaard reported serving as a consultant to and receiving research grant support from the company.
AT EuroPCR
Key clinical point:
Major finding: At 4 years of follow-up, the composite endpoint of all-cause mortality, MI, or stroke occurred in 29% of low-surgical-risk patients with severe aortic stenosis who were randomized to transcatheter aortic valve replacement (TAVR) and 30% of those who underwent surgical valve replacement.
Data source: NOTION, a prospective multicenter randomized trial in which 280 Nordic patients with symptomatic severe aortic stenosis at low surgical risk were assigned to surgical aortic valve replacement (SAVR) or to TAVR with the self-expanding CoreValve.
Disclosures: The study is funded by Medtronic. The presenter reported serving as a consultant to and receiving research grant support from the company.
Childhood poverty sets stage for adult heart disease
Children from the poorest families show signs of thicker carotid artery walls that may raise their risk for heart attack and stroke as adults, according to data from a longitudinal study of more than 1,000 families in Australia.
“Understanding when associations between SEP [socioeconomic position] and CVD [cardiovascular disease] first appear may help address the increasing social gradients in CVD outcomes and risk factors,” wrote Richard S. Liu, MD, of the Murdoch Children’s Research Institute, Parkville, Australia, and colleagues.
The researchers reviewed data from 1,477 families in Australia. Socioeconomic position of the children’s families was measured biennially at age 0-1 year and onward, and the researchers used imaging to measure the right carotid arteries of children between age 11 and 12 years. Overall, children in the lowest socioeconomic quartile at age 11-12 years were 46% more likely than those in the highest quartile to have thicker carotid arteries (defined as greater than the 75th percentile).
“In univariable analyses, each quartile increment higher of family SEP was associated with a 3.7-micrometer thicker carotid intima-media thickness [IMT],” and the association remained significant in a multivariate analysis controlling for cardiovascular risk factors including secondhand smoke, body weight, and blood pressure, the researchers wrote.
The socioeconomic status of the family had a greater impact than that of the neighborhood, they noted.
In addition, low socioeconomic status of a child’s family at age 2-3 years was associated with thickness in carotid artery measurements at age 11-12 years.
The study findings were limited by several factors, including a lack of data on the clinical consequences of increased carotid thickness in children, as well as the need for investigation of other signs of subclinical atherosclerosis, the researchers said. However, “consistent evidence showed an association between SEP from early life and midchildhood carotid IMT,” and additional research is needed to explore the impact of household factors on childhood health, they emphasized.
The findings were published online Aug. 9 in the Journal of the American Heart Association (J Am Heart Assoc. 2017;6:e0059255).
The study was funded by the National Health and Medical Research Council of Australia and several research institutions. The researchers had no financial conflicts to disclose.
Children from the poorest families show signs of thicker carotid artery walls that may raise their risk for heart attack and stroke as adults, according to data from a longitudinal study of more than 1,000 families in Australia.
“Understanding when associations between SEP [socioeconomic position] and CVD [cardiovascular disease] first appear may help address the increasing social gradients in CVD outcomes and risk factors,” wrote Richard S. Liu, MD, of the Murdoch Children’s Research Institute, Parkville, Australia, and colleagues.
The researchers reviewed data from 1,477 families in Australia. Socioeconomic position of the children’s families was measured biennially at age 0-1 year and onward, and the researchers used imaging to measure the right carotid arteries of children between age 11 and 12 years. Overall, children in the lowest socioeconomic quartile at age 11-12 years were 46% more likely than those in the highest quartile to have thicker carotid arteries (defined as greater than the 75th percentile).
“In univariable analyses, each quartile increment higher of family SEP was associated with a 3.7-micrometer thicker carotid intima-media thickness [IMT],” and the association remained significant in a multivariate analysis controlling for cardiovascular risk factors including secondhand smoke, body weight, and blood pressure, the researchers wrote.
The socioeconomic status of the family had a greater impact than that of the neighborhood, they noted.
In addition, low socioeconomic status of a child’s family at age 2-3 years was associated with thickness in carotid artery measurements at age 11-12 years.
The study findings were limited by several factors, including a lack of data on the clinical consequences of increased carotid thickness in children, as well as the need for investigation of other signs of subclinical atherosclerosis, the researchers said. However, “consistent evidence showed an association between SEP from early life and midchildhood carotid IMT,” and additional research is needed to explore the impact of household factors on childhood health, they emphasized.
The findings were published online Aug. 9 in the Journal of the American Heart Association (J Am Heart Assoc. 2017;6:e0059255).
The study was funded by the National Health and Medical Research Council of Australia and several research institutions. The researchers had no financial conflicts to disclose.
Children from the poorest families show signs of thicker carotid artery walls that may raise their risk for heart attack and stroke as adults, according to data from a longitudinal study of more than 1,000 families in Australia.
“Understanding when associations between SEP [socioeconomic position] and CVD [cardiovascular disease] first appear may help address the increasing social gradients in CVD outcomes and risk factors,” wrote Richard S. Liu, MD, of the Murdoch Children’s Research Institute, Parkville, Australia, and colleagues.
The researchers reviewed data from 1,477 families in Australia. Socioeconomic position of the children’s families was measured biennially at age 0-1 year and onward, and the researchers used imaging to measure the right carotid arteries of children between age 11 and 12 years. Overall, children in the lowest socioeconomic quartile at age 11-12 years were 46% more likely than those in the highest quartile to have thicker carotid arteries (defined as greater than the 75th percentile).
“In univariable analyses, each quartile increment higher of family SEP was associated with a 3.7-micrometer thicker carotid intima-media thickness [IMT],” and the association remained significant in a multivariate analysis controlling for cardiovascular risk factors including secondhand smoke, body weight, and blood pressure, the researchers wrote.
The socioeconomic status of the family had a greater impact than that of the neighborhood, they noted.
In addition, low socioeconomic status of a child’s family at age 2-3 years was associated with thickness in carotid artery measurements at age 11-12 years.
The study findings were limited by several factors, including a lack of data on the clinical consequences of increased carotid thickness in children, as well as the need for investigation of other signs of subclinical atherosclerosis, the researchers said. However, “consistent evidence showed an association between SEP from early life and midchildhood carotid IMT,” and additional research is needed to explore the impact of household factors on childhood health, they emphasized.
The findings were published online Aug. 9 in the Journal of the American Heart Association (J Am Heart Assoc. 2017;6:e0059255).
The study was funded by the National Health and Medical Research Council of Australia and several research institutions. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Key clinical point: Low socioeconomic status of families was significantly linked with thicker carotid arteries in children at age 11-12 years, which could increase the risk of stroke in adulthood.
Major finding: Children in the lowest socioeconomic group at age 11-12 years were 46% more likely to have carotid intima-media thickness at a level above the 75th percentile.
Data source: A longitudinal study of children from 1,477 families in Australia.
Disclosures: The study was funded by the National Health and Medical Research Council of Australia and several research institutions. The researchers had no financial conflicts to disclose.
TAVR for failed surgical valves: the VIVA study
PARIS – Transcatheter aortic valve replacement using the self-expanding Evolut R device in high-surgical-risk patients with failing surgical aortic bioprostheses showed promising 30-day safety and effectiveness results in the ongoing VIVA study, Ran Kornowski, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We had a lot of patients with small, failing valves in this study. Despite this, our valve gradients postprocedure were very, very low. This means to me that this platform is very well suited to deal with valve-in-valve procedures in general and with small bioprosthetic valves in particular,” observed Dr. Kornowski, chairman of the department of cardiology at Rabin Medical Center in Petah Tikva, Israel, and president of the Israel Heart Society.
The participants’ last surgical aortic valve replacement had been a mean of 9.3 years earlier. Seventy-one percent of subjects were New York Heart Association class III or IV. The mode of bioprosthetic failure was stenosis in 56% of cases, regurgitation in 23%, and both in the remainder. Ninety-three percent of their failing biosprothetic valves were stented devices. Forty-one percent of the devices were up to 21 mm and another 33% were more than 21 but less than 25 mm.
TAVR procedural access was by the iliofemoral route in 97% of cases. Local anesthesia was used in 42% of cases and conscious sedation in 35%. Fourteen percent of patients underwent preimplantation valvuloplasty; 21% postimplantation valvuloplasty. The procedural success rate was 98.5%.
The primary safety endpoint was 30-day cardiovascular mortality. The 2.0% rate was far lower than the prespecified cutoff which defined a positive outcome as less than a 10% rate in this high-surgical-risk population.
Other key 30-day outcomes:
• All-cause mortality occurred in 2.5% of patients.
• The 30-day stroke rate was 3%, with no disabling strokes.
• Major vascular complications occurred in 6.5% of the VIVA patients.
• Major bleeding occurred in 7%, minor bleeding in 7.9%. There were no cases of life-threatening bleeding.
• The incidence of Stage I acute kidney injury was rare, at 0.5%.
• Seven percent of patients received a permanent pacemaker.
• Eighty-seven percent of patients had no postprocedure paravalvular regurgitation (PVR), 11.4 had mild PVR, and 1.5% had moderate PVR.
• NYHA classification improved from baseline to 30 days in 81% of patients. At 30 days, 93% of participants were NYHA class I or II.
Turning to echocardiographic findings, the mean gradient improved from a mean baseline of 31.8 mm Hg to 12.6 mm Hg, while the effective orifice area rose from 1.0 to 1.5 cm2. The magnitude of both improvements was greater for patients with stenosis as their mode of valve failure.
“With the Evolut R, we aim for higher implantations – not more than about 4 mm below the ring – because going deeper could bring about higher gradients and functional deterioration later on,” the cardiologist explained.
The 1-year primary efficacy endpoint – lack of significant aortic stenosis as defined by a mean gradient less than 40 mm Hg – will be reported soon. The VIVA study is sponsored by Medtronic. Dr. Kornowski reported serving as a consultant to the company.
PARIS – Transcatheter aortic valve replacement using the self-expanding Evolut R device in high-surgical-risk patients with failing surgical aortic bioprostheses showed promising 30-day safety and effectiveness results in the ongoing VIVA study, Ran Kornowski, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We had a lot of patients with small, failing valves in this study. Despite this, our valve gradients postprocedure were very, very low. This means to me that this platform is very well suited to deal with valve-in-valve procedures in general and with small bioprosthetic valves in particular,” observed Dr. Kornowski, chairman of the department of cardiology at Rabin Medical Center in Petah Tikva, Israel, and president of the Israel Heart Society.
The participants’ last surgical aortic valve replacement had been a mean of 9.3 years earlier. Seventy-one percent of subjects were New York Heart Association class III or IV. The mode of bioprosthetic failure was stenosis in 56% of cases, regurgitation in 23%, and both in the remainder. Ninety-three percent of their failing biosprothetic valves were stented devices. Forty-one percent of the devices were up to 21 mm and another 33% were more than 21 but less than 25 mm.
TAVR procedural access was by the iliofemoral route in 97% of cases. Local anesthesia was used in 42% of cases and conscious sedation in 35%. Fourteen percent of patients underwent preimplantation valvuloplasty; 21% postimplantation valvuloplasty. The procedural success rate was 98.5%.
The primary safety endpoint was 30-day cardiovascular mortality. The 2.0% rate was far lower than the prespecified cutoff which defined a positive outcome as less than a 10% rate in this high-surgical-risk population.
Other key 30-day outcomes:
• All-cause mortality occurred in 2.5% of patients.
• The 30-day stroke rate was 3%, with no disabling strokes.
• Major vascular complications occurred in 6.5% of the VIVA patients.
• Major bleeding occurred in 7%, minor bleeding in 7.9%. There were no cases of life-threatening bleeding.
• The incidence of Stage I acute kidney injury was rare, at 0.5%.
• Seven percent of patients received a permanent pacemaker.
• Eighty-seven percent of patients had no postprocedure paravalvular regurgitation (PVR), 11.4 had mild PVR, and 1.5% had moderate PVR.
• NYHA classification improved from baseline to 30 days in 81% of patients. At 30 days, 93% of participants were NYHA class I or II.
Turning to echocardiographic findings, the mean gradient improved from a mean baseline of 31.8 mm Hg to 12.6 mm Hg, while the effective orifice area rose from 1.0 to 1.5 cm2. The magnitude of both improvements was greater for patients with stenosis as their mode of valve failure.
“With the Evolut R, we aim for higher implantations – not more than about 4 mm below the ring – because going deeper could bring about higher gradients and functional deterioration later on,” the cardiologist explained.
The 1-year primary efficacy endpoint – lack of significant aortic stenosis as defined by a mean gradient less than 40 mm Hg – will be reported soon. The VIVA study is sponsored by Medtronic. Dr. Kornowski reported serving as a consultant to the company.
PARIS – Transcatheter aortic valve replacement using the self-expanding Evolut R device in high-surgical-risk patients with failing surgical aortic bioprostheses showed promising 30-day safety and effectiveness results in the ongoing VIVA study, Ran Kornowski, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We had a lot of patients with small, failing valves in this study. Despite this, our valve gradients postprocedure were very, very low. This means to me that this platform is very well suited to deal with valve-in-valve procedures in general and with small bioprosthetic valves in particular,” observed Dr. Kornowski, chairman of the department of cardiology at Rabin Medical Center in Petah Tikva, Israel, and president of the Israel Heart Society.
The participants’ last surgical aortic valve replacement had been a mean of 9.3 years earlier. Seventy-one percent of subjects were New York Heart Association class III or IV. The mode of bioprosthetic failure was stenosis in 56% of cases, regurgitation in 23%, and both in the remainder. Ninety-three percent of their failing biosprothetic valves were stented devices. Forty-one percent of the devices were up to 21 mm and another 33% were more than 21 but less than 25 mm.
TAVR procedural access was by the iliofemoral route in 97% of cases. Local anesthesia was used in 42% of cases and conscious sedation in 35%. Fourteen percent of patients underwent preimplantation valvuloplasty; 21% postimplantation valvuloplasty. The procedural success rate was 98.5%.
The primary safety endpoint was 30-day cardiovascular mortality. The 2.0% rate was far lower than the prespecified cutoff which defined a positive outcome as less than a 10% rate in this high-surgical-risk population.
Other key 30-day outcomes:
• All-cause mortality occurred in 2.5% of patients.
• The 30-day stroke rate was 3%, with no disabling strokes.
• Major vascular complications occurred in 6.5% of the VIVA patients.
• Major bleeding occurred in 7%, minor bleeding in 7.9%. There were no cases of life-threatening bleeding.
• The incidence of Stage I acute kidney injury was rare, at 0.5%.
• Seven percent of patients received a permanent pacemaker.
• Eighty-seven percent of patients had no postprocedure paravalvular regurgitation (PVR), 11.4 had mild PVR, and 1.5% had moderate PVR.
• NYHA classification improved from baseline to 30 days in 81% of patients. At 30 days, 93% of participants were NYHA class I or II.
Turning to echocardiographic findings, the mean gradient improved from a mean baseline of 31.8 mm Hg to 12.6 mm Hg, while the effective orifice area rose from 1.0 to 1.5 cm2. The magnitude of both improvements was greater for patients with stenosis as their mode of valve failure.
“With the Evolut R, we aim for higher implantations – not more than about 4 mm below the ring – because going deeper could bring about higher gradients and functional deterioration later on,” the cardiologist explained.
The 1-year primary efficacy endpoint – lack of significant aortic stenosis as defined by a mean gradient less than 40 mm Hg – will be reported soon. The VIVA study is sponsored by Medtronic. Dr. Kornowski reported serving as a consultant to the company.
AT EuroPCR
Key clinical point:
Major finding: The 30-day cardiovascular mortality rate after transcatheter aortic valve replacement via a valve-in-valve procedure in patients with a failing surgically implanted bioprosthesis was 2%, compared with a projected rate of at least 10% with redo surgery.
Data source: VIVA, a prospective observational registry of 202 high-surgical-risk patients at 23 centers in four countries who underwent valve-in-valve transcatheter aortic valve replacement because of a failing surgically implanted aortic bioprosthesis.
Disclosures: VIVA is sponsored by Medtronic. The presenter reported serving as a consultant to the company.
Bailout stenting for coronary bifurcations brings ‘unacceptable’ hazards
PARIS – Bailout stenting during percutaneous coronary intervention for coronary bifurcations doubled the risk of major adverse cardiovascular events in the world’s largest registry of patients with these often-challenging lesions treated using bioactive stents, Marco Zimarino, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Indeed, resort to bailout stenting stood out as the major potentially modifiable risk factor for adverse outcomes among the 4,306 participants in the P2BiTO registry, an international collaboration supported by members of the EuroBifurcation Club. Most of the other independent risk factors identified in a multivariate regression analysis of the P2BiTO database were beyond operator control, including diabetes, advanced age, and presentation with an acute coronary syndrome, according to Dr. Zimarino of the University of Chieti (Italy).
Bailout stenting is largely avoidable through meticulous procedural planning, the interventional cardiologist added.
“Careful planning is always mandatory because bailout stenting is associated with an unacceptably higher risk of both in-hospital and 1-year adverse outcomes,” Dr. Zimarino emphasized. “It’s much better to leave a degraded side branch instead of using bailout stenting to get an excellent angiographic outcome that’s a predictor of a worse clinical outcome.”
Conventional wisdom holds that single stenting of either the main artery or a side branch in a patient with coronary bifurcation is safer than double stenting of both. However, that wasn’t really borne out in the P2BiTO registry provided the operator’s plan was for double stenting. The difference in 1-year major adverse cardiovascular events (MACE) between patients treated using a single- or double-stenting strategy wasn’t statistically significant, provided bailout stenting wasn’t utilized. If bailout stenting was employed, though, the risk of MACE was 2.2-fold greater than if the cardiologist stuck with the plan.
Ninety-eight percent of patients in the P2BiTO registry received drug-eluting stents. The other 2% got the Absorb bioabsorbable vascular scaffold. The percutaneous coronary intervention access site, treatment strategy, choice of stent, and duration of dual-antiplatelet therapy were left up to the operator’s discretion.
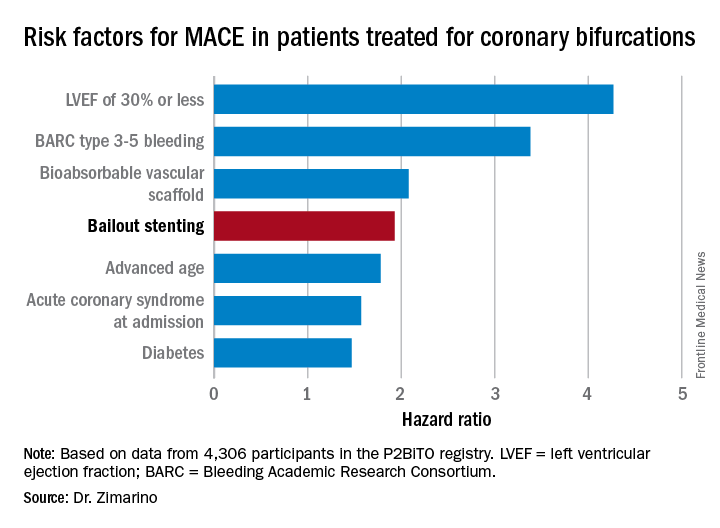
The risk of MACE was reduced by 39% in patients on dual-antiplatelet therapy for 6-12 months, compared with less than 6 months.
Discussant Graham Cassel, MD, director of the heart transplant unit at Milpark Hospital in Johannesburg, commented, “The message comes through very clearly that, if you plan your procedure well, the chance of bailout is far less – and if you do have to bail out, the results are uniformly bad. If you can avoid putting in two or three stents, that’s beneficial.”
Dr. Zimarino reported having no financial conflicts of interest regarding his presentation.
PARIS – Bailout stenting during percutaneous coronary intervention for coronary bifurcations doubled the risk of major adverse cardiovascular events in the world’s largest registry of patients with these often-challenging lesions treated using bioactive stents, Marco Zimarino, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Indeed, resort to bailout stenting stood out as the major potentially modifiable risk factor for adverse outcomes among the 4,306 participants in the P2BiTO registry, an international collaboration supported by members of the EuroBifurcation Club. Most of the other independent risk factors identified in a multivariate regression analysis of the P2BiTO database were beyond operator control, including diabetes, advanced age, and presentation with an acute coronary syndrome, according to Dr. Zimarino of the University of Chieti (Italy).
Bailout stenting is largely avoidable through meticulous procedural planning, the interventional cardiologist added.
“Careful planning is always mandatory because bailout stenting is associated with an unacceptably higher risk of both in-hospital and 1-year adverse outcomes,” Dr. Zimarino emphasized. “It’s much better to leave a degraded side branch instead of using bailout stenting to get an excellent angiographic outcome that’s a predictor of a worse clinical outcome.”
Conventional wisdom holds that single stenting of either the main artery or a side branch in a patient with coronary bifurcation is safer than double stenting of both. However, that wasn’t really borne out in the P2BiTO registry provided the operator’s plan was for double stenting. The difference in 1-year major adverse cardiovascular events (MACE) between patients treated using a single- or double-stenting strategy wasn’t statistically significant, provided bailout stenting wasn’t utilized. If bailout stenting was employed, though, the risk of MACE was 2.2-fold greater than if the cardiologist stuck with the plan.
Ninety-eight percent of patients in the P2BiTO registry received drug-eluting stents. The other 2% got the Absorb bioabsorbable vascular scaffold. The percutaneous coronary intervention access site, treatment strategy, choice of stent, and duration of dual-antiplatelet therapy were left up to the operator’s discretion.
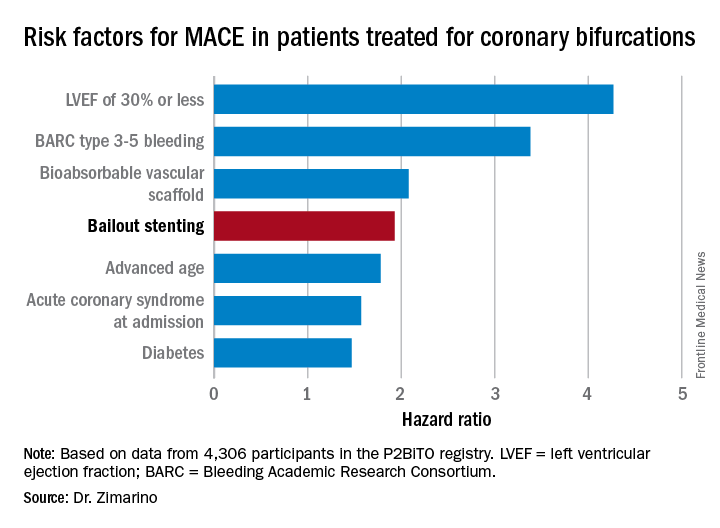
The risk of MACE was reduced by 39% in patients on dual-antiplatelet therapy for 6-12 months, compared with less than 6 months.
Discussant Graham Cassel, MD, director of the heart transplant unit at Milpark Hospital in Johannesburg, commented, “The message comes through very clearly that, if you plan your procedure well, the chance of bailout is far less – and if you do have to bail out, the results are uniformly bad. If you can avoid putting in two or three stents, that’s beneficial.”
Dr. Zimarino reported having no financial conflicts of interest regarding his presentation.
PARIS – Bailout stenting during percutaneous coronary intervention for coronary bifurcations doubled the risk of major adverse cardiovascular events in the world’s largest registry of patients with these often-challenging lesions treated using bioactive stents, Marco Zimarino, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Indeed, resort to bailout stenting stood out as the major potentially modifiable risk factor for adverse outcomes among the 4,306 participants in the P2BiTO registry, an international collaboration supported by members of the EuroBifurcation Club. Most of the other independent risk factors identified in a multivariate regression analysis of the P2BiTO database were beyond operator control, including diabetes, advanced age, and presentation with an acute coronary syndrome, according to Dr. Zimarino of the University of Chieti (Italy).
Bailout stenting is largely avoidable through meticulous procedural planning, the interventional cardiologist added.
“Careful planning is always mandatory because bailout stenting is associated with an unacceptably higher risk of both in-hospital and 1-year adverse outcomes,” Dr. Zimarino emphasized. “It’s much better to leave a degraded side branch instead of using bailout stenting to get an excellent angiographic outcome that’s a predictor of a worse clinical outcome.”
Conventional wisdom holds that single stenting of either the main artery or a side branch in a patient with coronary bifurcation is safer than double stenting of both. However, that wasn’t really borne out in the P2BiTO registry provided the operator’s plan was for double stenting. The difference in 1-year major adverse cardiovascular events (MACE) between patients treated using a single- or double-stenting strategy wasn’t statistically significant, provided bailout stenting wasn’t utilized. If bailout stenting was employed, though, the risk of MACE was 2.2-fold greater than if the cardiologist stuck with the plan.
Ninety-eight percent of patients in the P2BiTO registry received drug-eluting stents. The other 2% got the Absorb bioabsorbable vascular scaffold. The percutaneous coronary intervention access site, treatment strategy, choice of stent, and duration of dual-antiplatelet therapy were left up to the operator’s discretion.
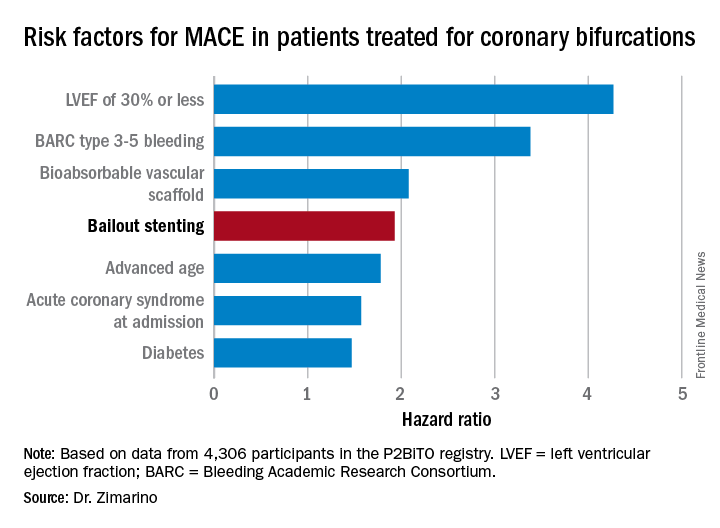
The risk of MACE was reduced by 39% in patients on dual-antiplatelet therapy for 6-12 months, compared with less than 6 months.
Discussant Graham Cassel, MD, director of the heart transplant unit at Milpark Hospital in Johannesburg, commented, “The message comes through very clearly that, if you plan your procedure well, the chance of bailout is far less – and if you do have to bail out, the results are uniformly bad. If you can avoid putting in two or three stents, that’s beneficial.”
Dr. Zimarino reported having no financial conflicts of interest regarding his presentation.
AT EUROPCR
Key clinical point:
Major finding: Bailout stenting during PCI for coronary bifurcations doubles the risk of major adverse cardiovascular events.
Data source: The P2BiTO registry includes 4,306 patients who received one or more drug-eluting stents or bioabsorbable vascular scaffolds for treatment of coronary bifurcations.
Disclosures: The study presenter reported having no financial conflicts of interest.
Revascularization of CTOs improves health status more than medical therapy
PARIS – The first randomized clinical trial to evaluate quality of life and clinical symptoms as the primary efficacy outcome in patients with coronary chronic total occlusion (CTO) showed a clear advantage for percutaneous revascularization over optimal medical therapy.
At 12 months’ follow-up in the 26-site, 396-patient EuroCTO trial, patients randomized to PCI with drug-eluting stents had significantly less angina and physical limitations coupled with greater improvement in quality of life than the optimal medical therapy (OMT) group on subscales of the Seattle Angina Questionnaire. On the angina frequency subscale, for example, the PCI group improved from a mean baseline score of 77.2 to 91.4 at 12 months, a significantly better result than the OMT group improvement from 80.6 to 87.5.
The PCI group also experienced greater mobility, better activity status, and less pain and discomfort as assessed by the EuroQOL five dimensions questionnaire (EQ-5D), Gerald S. Werner, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“PCI of a CTO should be considered as a primary option in symptomatic patients. It is a safe and effective treatment option in expert hands,” said Dr. Werner, director of cardiology and nonsurgical intensive care at the Darmstadt (Ger.) Clinic.
He emphasized the point about “expert hands,” drawing attention to the stellar 86.3% successful revascularization rate in the EuroCTO trial, even though these were often complex procedures. Indeed, in 36% of the CTO PCIs, a retrograde approach was used.
“CTO is a special field. Just like not everybody in every hospital will do a transcatheter aortic valve replacement, not everybody should do a CTO. It can be done safely and to the benefit of the patient, but it needs to be done by someone with expertise,” the cardiologist said.
Study participants were evenly split between those with single- and multivessel disease. Patients with additional nonocclusive disease had those lesions treated by PCI before the 2:1 randomization to CTO PCI or OMT.
The periprocedural complication rate was low at 2.9%, a figure that included a 1.5% incidence of pericardial tamponade as well as vascular repairs. There were no periprocedural MIs or deaths. The 1-year major adverse cardiac event rate was roughly 6% in both study arms.
The PCI group received 6-12 months of dual-antiplatelet therapy with clopidogrel and aspirin. So did roughly 40% of the OMT group because of prior PCI.
Both study arms had comparably high rates of guideline-directed medical therapy, including statins, beta-blockers, and ACE inhibitors. However, the PCI group made significantly less use of nitrates than the OMT group during follow-up, reflecting their greater reduction in angina frequency. The crossover rate from OMT to PCI because of ongoing angina was 7.3%.
The long-term safety and durability of the two treatment strategies will be assessed at 3 years of follow-up.
The EuroCTO trial was originally planned for 600 patients. The investigators eventually settled for less because of slow enrollment. Many interventionalists who are skilled in treating CTOs proved reluctant to randomize the patients.
Dr. Werner contrasted the positive EuroCTO findings regarding clinical symptoms and quality of life to the negative results of the Korean DECISION CTO trial presented at the 2017 meeting of the American College of Cardiology. DECISION CTO found that PCI plus OMT wasn’t superior to OMT alone in reducing MI and other major adverse cardiac events in patients with at least one CTO. In Dr. Werner’s view, the Korean investigators chose the wrong endpoint.
“The quality of life improvement we’ve shown after PCI in EuroCTO is a valid clinical goal in treating stable coronary artery disease. I don’t think we can aim at improving prognosis,” according to Dr. Werner.
The impetus for EuroCTO was a recognition that CTOs are common and seriously undertreated. CTOs account for 16%-18% of all coronary lesions in patients with stable coronary artery disease, yet U.S. national data indicate only 5% of PCIs are performed to treat CTOs.
The EuroCTO trial was sponsored by the Euro CTO Club and supported by research grants from Biosensors and Asahi.
PARIS – The first randomized clinical trial to evaluate quality of life and clinical symptoms as the primary efficacy outcome in patients with coronary chronic total occlusion (CTO) showed a clear advantage for percutaneous revascularization over optimal medical therapy.
At 12 months’ follow-up in the 26-site, 396-patient EuroCTO trial, patients randomized to PCI with drug-eluting stents had significantly less angina and physical limitations coupled with greater improvement in quality of life than the optimal medical therapy (OMT) group on subscales of the Seattle Angina Questionnaire. On the angina frequency subscale, for example, the PCI group improved from a mean baseline score of 77.2 to 91.4 at 12 months, a significantly better result than the OMT group improvement from 80.6 to 87.5.
The PCI group also experienced greater mobility, better activity status, and less pain and discomfort as assessed by the EuroQOL five dimensions questionnaire (EQ-5D), Gerald S. Werner, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“PCI of a CTO should be considered as a primary option in symptomatic patients. It is a safe and effective treatment option in expert hands,” said Dr. Werner, director of cardiology and nonsurgical intensive care at the Darmstadt (Ger.) Clinic.
He emphasized the point about “expert hands,” drawing attention to the stellar 86.3% successful revascularization rate in the EuroCTO trial, even though these were often complex procedures. Indeed, in 36% of the CTO PCIs, a retrograde approach was used.
“CTO is a special field. Just like not everybody in every hospital will do a transcatheter aortic valve replacement, not everybody should do a CTO. It can be done safely and to the benefit of the patient, but it needs to be done by someone with expertise,” the cardiologist said.
Study participants were evenly split between those with single- and multivessel disease. Patients with additional nonocclusive disease had those lesions treated by PCI before the 2:1 randomization to CTO PCI or OMT.
The periprocedural complication rate was low at 2.9%, a figure that included a 1.5% incidence of pericardial tamponade as well as vascular repairs. There were no periprocedural MIs or deaths. The 1-year major adverse cardiac event rate was roughly 6% in both study arms.
The PCI group received 6-12 months of dual-antiplatelet therapy with clopidogrel and aspirin. So did roughly 40% of the OMT group because of prior PCI.
Both study arms had comparably high rates of guideline-directed medical therapy, including statins, beta-blockers, and ACE inhibitors. However, the PCI group made significantly less use of nitrates than the OMT group during follow-up, reflecting their greater reduction in angina frequency. The crossover rate from OMT to PCI because of ongoing angina was 7.3%.
The long-term safety and durability of the two treatment strategies will be assessed at 3 years of follow-up.
The EuroCTO trial was originally planned for 600 patients. The investigators eventually settled for less because of slow enrollment. Many interventionalists who are skilled in treating CTOs proved reluctant to randomize the patients.
Dr. Werner contrasted the positive EuroCTO findings regarding clinical symptoms and quality of life to the negative results of the Korean DECISION CTO trial presented at the 2017 meeting of the American College of Cardiology. DECISION CTO found that PCI plus OMT wasn’t superior to OMT alone in reducing MI and other major adverse cardiac events in patients with at least one CTO. In Dr. Werner’s view, the Korean investigators chose the wrong endpoint.
“The quality of life improvement we’ve shown after PCI in EuroCTO is a valid clinical goal in treating stable coronary artery disease. I don’t think we can aim at improving prognosis,” according to Dr. Werner.
The impetus for EuroCTO was a recognition that CTOs are common and seriously undertreated. CTOs account for 16%-18% of all coronary lesions in patients with stable coronary artery disease, yet U.S. national data indicate only 5% of PCIs are performed to treat CTOs.
The EuroCTO trial was sponsored by the Euro CTO Club and supported by research grants from Biosensors and Asahi.
PARIS – The first randomized clinical trial to evaluate quality of life and clinical symptoms as the primary efficacy outcome in patients with coronary chronic total occlusion (CTO) showed a clear advantage for percutaneous revascularization over optimal medical therapy.
At 12 months’ follow-up in the 26-site, 396-patient EuroCTO trial, patients randomized to PCI with drug-eluting stents had significantly less angina and physical limitations coupled with greater improvement in quality of life than the optimal medical therapy (OMT) group on subscales of the Seattle Angina Questionnaire. On the angina frequency subscale, for example, the PCI group improved from a mean baseline score of 77.2 to 91.4 at 12 months, a significantly better result than the OMT group improvement from 80.6 to 87.5.
The PCI group also experienced greater mobility, better activity status, and less pain and discomfort as assessed by the EuroQOL five dimensions questionnaire (EQ-5D), Gerald S. Werner, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“PCI of a CTO should be considered as a primary option in symptomatic patients. It is a safe and effective treatment option in expert hands,” said Dr. Werner, director of cardiology and nonsurgical intensive care at the Darmstadt (Ger.) Clinic.
He emphasized the point about “expert hands,” drawing attention to the stellar 86.3% successful revascularization rate in the EuroCTO trial, even though these were often complex procedures. Indeed, in 36% of the CTO PCIs, a retrograde approach was used.
“CTO is a special field. Just like not everybody in every hospital will do a transcatheter aortic valve replacement, not everybody should do a CTO. It can be done safely and to the benefit of the patient, but it needs to be done by someone with expertise,” the cardiologist said.
Study participants were evenly split between those with single- and multivessel disease. Patients with additional nonocclusive disease had those lesions treated by PCI before the 2:1 randomization to CTO PCI or OMT.
The periprocedural complication rate was low at 2.9%, a figure that included a 1.5% incidence of pericardial tamponade as well as vascular repairs. There were no periprocedural MIs or deaths. The 1-year major adverse cardiac event rate was roughly 6% in both study arms.
The PCI group received 6-12 months of dual-antiplatelet therapy with clopidogrel and aspirin. So did roughly 40% of the OMT group because of prior PCI.
Both study arms had comparably high rates of guideline-directed medical therapy, including statins, beta-blockers, and ACE inhibitors. However, the PCI group made significantly less use of nitrates than the OMT group during follow-up, reflecting their greater reduction in angina frequency. The crossover rate from OMT to PCI because of ongoing angina was 7.3%.
The long-term safety and durability of the two treatment strategies will be assessed at 3 years of follow-up.
The EuroCTO trial was originally planned for 600 patients. The investigators eventually settled for less because of slow enrollment. Many interventionalists who are skilled in treating CTOs proved reluctant to randomize the patients.
Dr. Werner contrasted the positive EuroCTO findings regarding clinical symptoms and quality of life to the negative results of the Korean DECISION CTO trial presented at the 2017 meeting of the American College of Cardiology. DECISION CTO found that PCI plus OMT wasn’t superior to OMT alone in reducing MI and other major adverse cardiac events in patients with at least one CTO. In Dr. Werner’s view, the Korean investigators chose the wrong endpoint.
“The quality of life improvement we’ve shown after PCI in EuroCTO is a valid clinical goal in treating stable coronary artery disease. I don’t think we can aim at improving prognosis,” according to Dr. Werner.
The impetus for EuroCTO was a recognition that CTOs are common and seriously undertreated. CTOs account for 16%-18% of all coronary lesions in patients with stable coronary artery disease, yet U.S. national data indicate only 5% of PCIs are performed to treat CTOs.
The EuroCTO trial was sponsored by the Euro CTO Club and supported by research grants from Biosensors and Asahi.
AT EUROPCR
Key clinical point:
Major finding: Patients whose chronic total occlusions were treated by PCI rather than optimal medical therapy experienced significantly less angina and greater improvement in quality of life during 12 months of follow-up.
Data source: EuroCTO, a prospective, 26-site study in which 396 patients with coronary chronic total occlusions were randomized 2:1 to PCI or optimal medical therapy.
Disclosures: EuroCTO was sponsored by the Euro CTO Club and supported by research grants from Biosensors and Asahi.
Hidden CABG costs will disrupt bundled payment systems
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
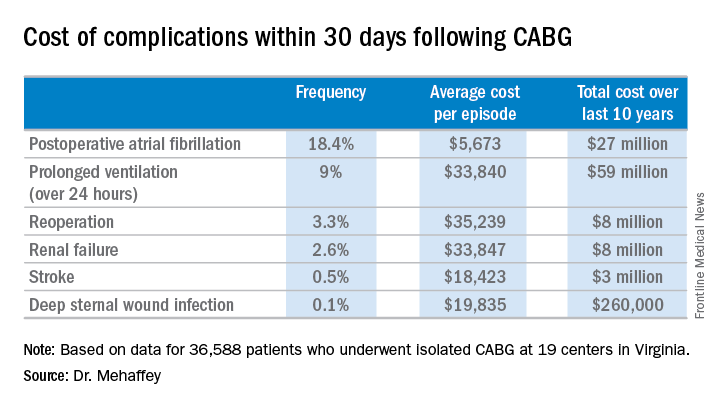
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
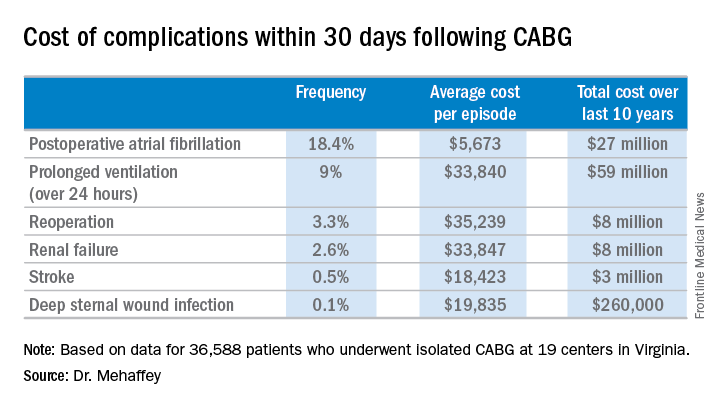
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
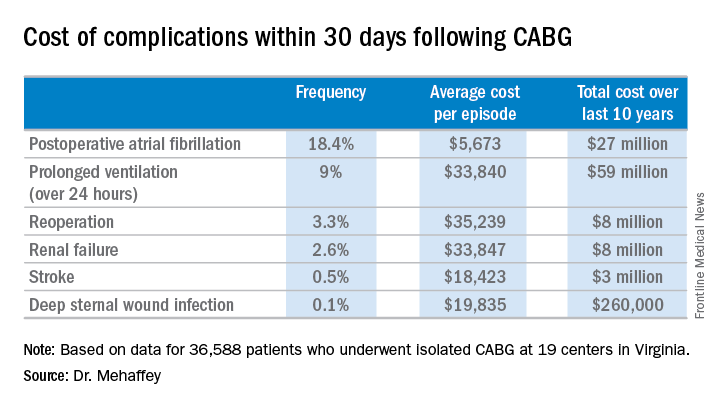
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
AT THE WTSA ANNUAL MEETING
Key clinical point:
Major finding: The average 30-day total hospital cost of an isolated CABG procedure during 2006-2015 in Virginia was $36,580 if there were no postoperative complications, jumping to $64,542 with one major complication and $111,239 with two.
Data source: A retrospective study of the 30-day total hospital costs for all isolated CABG procedures performed in Virginia during 2006-2015.
Disclosures: The study presenter reported having no financial conflicts.
Malperfusion key in aortic dissection repair outcomes
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Malperfusion is a main determinant of outcomes for patients having surgical repair for acute type A aortic dissection.
Major finding: Patients in the early surgery group (surgery within 12 hours of onset) were more likely to have malperfusion than those who had surgery later, 47% vs. 31%.
Data source: Single-center analysis of 152 operations for repair of acute type A aortic dissections over a 17-year period.
Disclosures: Dr. Narayan and his coauthors had no financial relationships to disclose.
Novel drug-eluting coronary stent looks good in DESSOLVE III
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
PARIS – A unique drug-eluting coronary stent showed positive interim results in the DESSOLVE III trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
In DESSOLVE III, 1,398 patients undergoing percutaneous coronary intervention were randomized to the widely used Xience everolimus-eluting stent or to MiStent, a novel thin-strut stent with a polymer coating that is quickly absorbed after delivering microcrystalline sirolimus into the vessel wall for prolonged release at a near-linear rate.
At an interim analysis at 12 months of follow-up, the primary endpoint – a composite of cardiac death, target vessel MI, and clinically indicated target lesion revascularization – had occurred in 5.8% of the MiStent group and 6.5% of Xience recipients in the study, which was designed as a noninferiority trial, reported Robbert J. de Winter, MD, professor of clinical cardiology at the Academic Medical Center in Amsterdam.
“The data support the hypothesis that long-term cytostatic inhibition of early neointima could prevent the late neointimal growth seen at medium and long term with conventional drug-eluting stents,” he said.
MiStent is designed to overcome a shortcoming of conventional drug-eluting stents: namely, their durable polymer coating sticks around after the cytostatic drug is finished being released. It is believed that this residual polymer, which may not disappear for 6-9 months, induces inflammation in the vessel wall, eventually leading to intimal growth, restenosis, and new atherosclerosis.
“The unique feature of the MiStent is that the polymer is bioabsorbable and is fully absorbed at 3 months, whereas the drug is present in the vessel wall out to 9 months, well after the coating has disappeared. So in theory you would expect that any inflammatory response caused by the polymer coating will be counteracted by the drug. This was seen in animal models. And in the DESSOLVE I and II studies, angiographic follow-up showed that late luminal loss was flat after 6 months, in contrast to other drug-eluting stents, which show accrual of late neointimal growth after 6 months to a year,” according to the cardiologist.
DESSOLVE III is planned as a 3-year study. Already by 6 months the curves for target lesion revascularization started to separate, with a 12-month rate of 2.6% in the MiStent group versus 3.8% for Xience. And while this difference is not yet statistically significant, Dr. de Winter and his coinvestigators expect that by 3 years the separation will have grown to the point that the difference becomes statistically significant and clinically meaningful.
The MiStent platform is composed of a cobalt/chromium alloy. The stent strut thickness is only 64 microns, in contrast to 81 microns for the Xience stent. Thinner stent struts have previously been shown to be less injurious to the vessel wall.
DESSOLVE III is an all-comers trial conducted at 20 sites in four European countries. Participants had to have a reference vessel diameter of 2.5-3.5 mm. Roughly 60% of patients had an acute coronary syndrome as their indication for PCI. The study population included, among others, patients with left main coronary artery lesions, restenotic lesions, and failed saphenous vein grafts. Dual-antiplatelet therapy was given for 6 months in patients with stable angina and 12 months for those with ACS, in accordance with European Society of Cardiology guidelines.
Discussant Robert A. Byrne, MD, of the German Heart Center in Munich, declared: “For me, this is a potentially interesting device. It’s the only device where we have a drug elution that’s more prolonged than the polymer, and this does offer the potential for later benefit.”
Dr. Byrne was a member of a European Commission–backed task force that developed European regulatory guidance for the evaluation of new coronary stents. “This MiStent trial program ticks off a lot of boxes: We had a successful first human use study, then we had a modest-size angiographic endpoint study where the late lumen loss looked good, and now we have a clinical endpoint study. This is what we want to see in the regulatory space.”
Another discussant, Chaim Lotan, MD, pronounced the MiStent “definitely another good stent on the shelf.”
It’s impossible to say whether the excellent 1-year outcomes seen with MiStent in DESSOLVE III were due to the prolonged-release microcrystalline sirolimus, the ultrathin stent struts, or both. In any case, the major adverse cardiovascular event rates seen in DESSOLVE III are so low by historical standards that it will become extremely difficult to show superiority for one contemporary drug-eluting stent over another, predicted Dr. Lotan of Hadassah Medical Center in Jerusalem.
Dr. de Winter concurred.
“I think we can now say that the benchmark for present day drug-eluting stents is a target lesion failure rate of about 6% at 12 months and a stent thrombosis rate below 1% at 12 months. It’s going to be increasingly more difficult to improve on that,” he said.
The MiStent, manufactured by Micell Technologies, is commercially available in Europe but investigational in the United States.
DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys.
Dr. de Winter reported receiving research grants from OrbusNeich, Abbott Vascular, AstraZeneca, Stentys, and Tryton.
AT EUROPCR
Key clinical point:
Major finding: At an interim 12-month analysis, the composite rate of cardiac death, target vessel MI, and clinically indicated target lesion revascularization was 6.5% in recipients of a Xience everolimus-eluting coronary stent and 5.8% in those randomized to the novel MiStent.
Data source: DESSOLVE III, a prospective, randomized, international trial that randomized 1,398 real-world-type all-comers undergoing PCI to the Xience device or the MiStent.
Disclosures: DESSOLVE III was sponsored by the European Cardiovascular Research Institute and supported by grants from Micell Technologies and Stentys. The presenter reported receiving research grants from both companies.