User login
FDA clears portable hematology analyzer
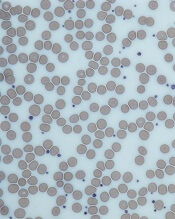
The U.S. Food and Drug Administration (FDA) has granted 510(k) clearance for PixCell Medical’s HemoScreen™.
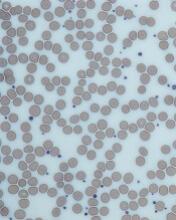
This portable hematology analyzer is used to perform a complete blood count at the point of care.
HemoScreen requires a single drop of blood and uses disposable cartridges that provide automatic sample preparation.
HemoScreen can analyze 20 standard complete blood count parameters and produces results within 5 minutes.
Study results suggested that HemoScreen provides results comparable to those of another hematology analyzer, Sysmex XE-2100. This study was published in the Journal of Clinical Pathology in 2016.
“The HemoScreen delivers lab-accurate results,” said Avishay Bransky, PhD, chief executive officer of PixCell Medical.
He added that HemoScreen “would be especially useful” in physicians’ offices, emergency rooms, intensive care units, oncology clinics, and remote locations.
HemoScreen makes use of a technology called viscoelastic focusing, which employs microfluidics and machine vision algorithms to analyze cells.
The U.S. Food and Drug Administration (FDA) has granted 510(k) clearance for PixCell Medical’s HemoScreen™.
This portable hematology analyzer is used to perform a complete blood count at the point of care.
HemoScreen requires a single drop of blood and uses disposable cartridges that provide automatic sample preparation.
HemoScreen can analyze 20 standard complete blood count parameters and produces results within 5 minutes.
Study results suggested that HemoScreen provides results comparable to those of another hematology analyzer, Sysmex XE-2100. This study was published in the Journal of Clinical Pathology in 2016.
“The HemoScreen delivers lab-accurate results,” said Avishay Bransky, PhD, chief executive officer of PixCell Medical.
He added that HemoScreen “would be especially useful” in physicians’ offices, emergency rooms, intensive care units, oncology clinics, and remote locations.
HemoScreen makes use of a technology called viscoelastic focusing, which employs microfluidics and machine vision algorithms to analyze cells.
The U.S. Food and Drug Administration (FDA) has granted 510(k) clearance for PixCell Medical’s HemoScreen™.
This portable hematology analyzer is used to perform a complete blood count at the point of care.
HemoScreen requires a single drop of blood and uses disposable cartridges that provide automatic sample preparation.
HemoScreen can analyze 20 standard complete blood count parameters and produces results within 5 minutes.
Study results suggested that HemoScreen provides results comparable to those of another hematology analyzer, Sysmex XE-2100. This study was published in the Journal of Clinical Pathology in 2016.
“The HemoScreen delivers lab-accurate results,” said Avishay Bransky, PhD, chief executive officer of PixCell Medical.
He added that HemoScreen “would be especially useful” in physicians’ offices, emergency rooms, intensive care units, oncology clinics, and remote locations.
HemoScreen makes use of a technology called viscoelastic focusing, which employs microfluidics and machine vision algorithms to analyze cells.
Denosumab fights osteoporosis in TDT patients
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to research published in Blood Advances.
Researchers found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” said study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens in Greece.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis.
They were randomized (in a double-blinded fashion) to receive 60 mg of denosumab (n=32) or placebo (n=31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms.
However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm—68.48 IU/L and 85.45 IU/L, respectively (P=0.013).
And the mean value of the tartrate-resistant acid phosphatase isoform-5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm—0.42 IU/L and 0.16 IU/L, respectively (P=0.026).
Results
The researchers measured bone mineral density in the L1-L4 lumbar spine, the wrist, and the femoral neck.
At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P=0.043).
The mean decrease in wrist bone mineral density was -0.26% and -3.92%, respectively (P=0.035).
And the mean increase in femoral neck bone mineral density was 4.08% and 1.96%, respectively (P=0.870).
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and Huskisson’s visual analog scale (P<0.001 for both).
However, there was no significant change in pain for patients in the placebo arm (P=0.356 with Huskisson’s and P=0.768 with McGill-Melzack).
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline (P<0.001 for all) in several markers of bone remodeling, including:
- Soluble receptor activator of nuclear factor kappa-B ligand (sRANKL)
- Osteoprotegerin (OPG)
- sRANKL/OPG ratio
- C-terminal crosslinking telopeptide of type I collagen (CTX)
- TRACP-5b
- bALP.
There were no significant changes in dickkopf-1 (Dkk-1), sclerostin, or osteocalcin (OC) in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, Dkk-1, sclerostin, CTX, TRACP-5b, and bALP (P<0.001 for all). There was no significant change from baseline in the sRANKL/OPG ratio or OC.
In all, there were 17 adverse events (AEs) in 14 patients.
There were three grade 1 AEs in the placebo arm and 11 in the denosumab arm. Most grade 1 AEs in the denosumab arm were test abnormalities, although three were not—headache, diarrhea, and fever.
There were three serious AEs in the denosumab arm as well—pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these AEs were considered unrelated to denosumab.
This study was funded by Amgen, which markets denosumab as Xgeva. The authors said they had no competing financial interests.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to research published in Blood Advances.
Researchers found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” said study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens in Greece.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis.
They were randomized (in a double-blinded fashion) to receive 60 mg of denosumab (n=32) or placebo (n=31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms.
However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm—68.48 IU/L and 85.45 IU/L, respectively (P=0.013).
And the mean value of the tartrate-resistant acid phosphatase isoform-5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm—0.42 IU/L and 0.16 IU/L, respectively (P=0.026).
Results
The researchers measured bone mineral density in the L1-L4 lumbar spine, the wrist, and the femoral neck.
At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P=0.043).
The mean decrease in wrist bone mineral density was -0.26% and -3.92%, respectively (P=0.035).
And the mean increase in femoral neck bone mineral density was 4.08% and 1.96%, respectively (P=0.870).
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and Huskisson’s visual analog scale (P<0.001 for both).
However, there was no significant change in pain for patients in the placebo arm (P=0.356 with Huskisson’s and P=0.768 with McGill-Melzack).
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline (P<0.001 for all) in several markers of bone remodeling, including:
- Soluble receptor activator of nuclear factor kappa-B ligand (sRANKL)
- Osteoprotegerin (OPG)
- sRANKL/OPG ratio
- C-terminal crosslinking telopeptide of type I collagen (CTX)
- TRACP-5b
- bALP.
There were no significant changes in dickkopf-1 (Dkk-1), sclerostin, or osteocalcin (OC) in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, Dkk-1, sclerostin, CTX, TRACP-5b, and bALP (P<0.001 for all). There was no significant change from baseline in the sRANKL/OPG ratio or OC.
In all, there were 17 adverse events (AEs) in 14 patients.
There were three grade 1 AEs in the placebo arm and 11 in the denosumab arm. Most grade 1 AEs in the denosumab arm were test abnormalities, although three were not—headache, diarrhea, and fever.
There were three serious AEs in the denosumab arm as well—pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these AEs were considered unrelated to denosumab.
This study was funded by Amgen, which markets denosumab as Xgeva. The authors said they had no competing financial interests.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to research published in Blood Advances.
Researchers found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” said study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens in Greece.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis.
They were randomized (in a double-blinded fashion) to receive 60 mg of denosumab (n=32) or placebo (n=31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms.
However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm—68.48 IU/L and 85.45 IU/L, respectively (P=0.013).
And the mean value of the tartrate-resistant acid phosphatase isoform-5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm—0.42 IU/L and 0.16 IU/L, respectively (P=0.026).
Results
The researchers measured bone mineral density in the L1-L4 lumbar spine, the wrist, and the femoral neck.
At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P=0.043).
The mean decrease in wrist bone mineral density was -0.26% and -3.92%, respectively (P=0.035).
And the mean increase in femoral neck bone mineral density was 4.08% and 1.96%, respectively (P=0.870).
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and Huskisson’s visual analog scale (P<0.001 for both).
However, there was no significant change in pain for patients in the placebo arm (P=0.356 with Huskisson’s and P=0.768 with McGill-Melzack).
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline (P<0.001 for all) in several markers of bone remodeling, including:
- Soluble receptor activator of nuclear factor kappa-B ligand (sRANKL)
- Osteoprotegerin (OPG)
- sRANKL/OPG ratio
- C-terminal crosslinking telopeptide of type I collagen (CTX)
- TRACP-5b
- bALP.
There were no significant changes in dickkopf-1 (Dkk-1), sclerostin, or osteocalcin (OC) in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, Dkk-1, sclerostin, CTX, TRACP-5b, and bALP (P<0.001 for all). There was no significant change from baseline in the sRANKL/OPG ratio or OC.
In all, there were 17 adverse events (AEs) in 14 patients.
There were three grade 1 AEs in the placebo arm and 11 in the denosumab arm. Most grade 1 AEs in the denosumab arm were test abnormalities, although three were not—headache, diarrhea, and fever.
There were three serious AEs in the denosumab arm as well—pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these AEs were considered unrelated to denosumab.
This study was funded by Amgen, which markets denosumab as Xgeva. The authors said they had no competing financial interests.
Primary care needs pile up for sickle cell patients
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
EXPERT ANALYSIS FROM SICKLE CELL IN FOCUS
Sickle cell disease gene therapy seen advancing
BETHESDA, MD. – Experimental gene therapies for sickle cell disease and thalassemia appear to be advancing, with BCL11A among the most promising targets in this field, researchers said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
Several highly anticipated presentations on the topic are expected for December meeting of the American Society of Hematology.
Alexis A. Thompson, MD, of Northwestern University, Chicago, reviewed highlights from a study in which the majority of patients given a gene therapy for transfusion dependent beta-thalassemia didn’t need subsequent blood transfusions. The New England Journal of Medicine in April published the results of this work done with Bluebird Bio’s LentiGlobin gene therapy (N Engl J Med. 2018; 378:1479-93).
Of the 22 patients in this trial, 15 have become transfusion independent, Dr. Thompson said in her presentation. Those patients that did not have this positive outcome still appear to have been helped by the gene therapy, she said. They had a median of 60% reduction in their transfusion volumes and nearly 60% in their number of transfusions.
“Whether it was transfusion independence or reduction in their transfusion volume or number, the vast majority of individuals in this first large-scale study had clinical benefit” from the therapy, said Dr. Thompson, who was the lead author of the study.
Dr. Thompson, the current president of the American Society of Hematology (ASH), said she’s looking forward to presentations on some of the most advanced gene therapies for sickle cell disease and thalassemia at the group’s annual meeting in December. The ASH presentations include those of John F. Tisdale, MD, who will report the latest data on LentiGlobin gene therapy in sickle cell disease, and Punam Malik, MD, of Cincinnati Children’s Hospital, who has developed a gamma globin lentivirus vector. There also will be a first readout on a particularly novel approach taken by researchers at Boston Children’s Hospital, led by David Williams, MD.
The development of CRISPR-Cas9 “has really opened up the field” of gene therapy, aiding researchers at Boston Children’s in their efforts to develop a treatment to maintain fetal hemoglobin production, Daniel E. Bauer, MD, PhD, of Boston Children’s Hospital, said during his presentation at the NIH conference.
Dr. Bauer provided an update on the BCL11A research that seeks to block what amounts to a genetic “off switch” for production of fetal hemoglobin. It’s long been known that erythrocytes of newborns with sickle cell disease are protected from sickling by high levels of fetal hemoglobin. Clinical manifestations of sickle cell disease then emerge in the first year of life as fetal hemoglobin levels decline.
“A main goal in hematology has been to understand how is it that these alternative fetal hemoglobin genes get silenced and how can we turn them back on,” said Dr. Bauer, a staff physician in pediatric hematology/oncology.
The gene BCL11A also plays key roles in the development of the central nervous system, B lymphatic lymphocyte maturation, and hematopoietic stem cell self-renewal. That led the researchers to hone in on targeting sequences around the BCL11A gene that act as erythroid enhancers, intending to limit potential complications by creating a very specific therapy for sickle cell disease.
In a related clinical trial, using lentiviral gene therapy rather than gene editing, researchers at Boston Children’s began an open-label, nonrandomized, single-center pilot study that involves a single infusion of autologous bone marrow derived CD34+ HSC cells transduced by a vector containing a short-hairpin segment of RNA targeting the gene BCL11A.
The study has a maximum accrual of seven evaluable patients, according to the NIH’s clinical trials website. The protocol is similar to bone marrow transplant, in that native blood stem cells are eliminated by myeloablative conditioning therapy. In this gene therapy, the patient’s own blood stem cells are then infused after the new genetic material has been added to counter the normal BCL11A off switch.
Swee Lay Thein, MBBS, an organizer of the NIH’s sickle cell conference, said in an interview that the “gene therapy side is really looking very optimistic.”
Dr. Thein, a senior investigator for sickle-cell genetics at the National Heart, Lung, and Blood Institute, earlier in her career discovered segments of DNA, including the BCL11A gene. She said that gaining greater understanding about genomic variation might someday aid in determining which people need more intense intervention for their sickle cell disease.
“You would be able to predict who will have more severe disease; we could monitor them more closely and perhaps even advocate for gene therapy or bone marrow transplant before complications have occurred rather than waiting for them to occur,” Dr. Thein said.
She referred to this as her “dream” for care of people with sickle cell disease. “This is still far off in the horizon.”
The NHLBI in September 2018 launched its Cure Sickle Cell Initiative. The agency estimates that it spends about $100 million on sickle cell disease research each year. The inherited blood disorder affects about 100,000 people in the United States and 20 million individuals worldwide. In sickle cell disease, a single genetic mutation causes red blood cells to form abnormal, sickle shapes that can clog the blood vessels and deprive cells of oxygen.
Dr. Thompson reported research funding and consulting agreements with Biomarin, Bluebird Bio, Celgene, Novartis, and Shire. Dr. Bauer reported patents related to BCL11A enhancer editing, consulting agreements with Merck and Pfizer, and research support from Bioverativ.
BETHESDA, MD. – Experimental gene therapies for sickle cell disease and thalassemia appear to be advancing, with BCL11A among the most promising targets in this field, researchers said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
Several highly anticipated presentations on the topic are expected for December meeting of the American Society of Hematology.
Alexis A. Thompson, MD, of Northwestern University, Chicago, reviewed highlights from a study in which the majority of patients given a gene therapy for transfusion dependent beta-thalassemia didn’t need subsequent blood transfusions. The New England Journal of Medicine in April published the results of this work done with Bluebird Bio’s LentiGlobin gene therapy (N Engl J Med. 2018; 378:1479-93).
Of the 22 patients in this trial, 15 have become transfusion independent, Dr. Thompson said in her presentation. Those patients that did not have this positive outcome still appear to have been helped by the gene therapy, she said. They had a median of 60% reduction in their transfusion volumes and nearly 60% in their number of transfusions.
“Whether it was transfusion independence or reduction in their transfusion volume or number, the vast majority of individuals in this first large-scale study had clinical benefit” from the therapy, said Dr. Thompson, who was the lead author of the study.
Dr. Thompson, the current president of the American Society of Hematology (ASH), said she’s looking forward to presentations on some of the most advanced gene therapies for sickle cell disease and thalassemia at the group’s annual meeting in December. The ASH presentations include those of John F. Tisdale, MD, who will report the latest data on LentiGlobin gene therapy in sickle cell disease, and Punam Malik, MD, of Cincinnati Children’s Hospital, who has developed a gamma globin lentivirus vector. There also will be a first readout on a particularly novel approach taken by researchers at Boston Children’s Hospital, led by David Williams, MD.
The development of CRISPR-Cas9 “has really opened up the field” of gene therapy, aiding researchers at Boston Children’s in their efforts to develop a treatment to maintain fetal hemoglobin production, Daniel E. Bauer, MD, PhD, of Boston Children’s Hospital, said during his presentation at the NIH conference.
Dr. Bauer provided an update on the BCL11A research that seeks to block what amounts to a genetic “off switch” for production of fetal hemoglobin. It’s long been known that erythrocytes of newborns with sickle cell disease are protected from sickling by high levels of fetal hemoglobin. Clinical manifestations of sickle cell disease then emerge in the first year of life as fetal hemoglobin levels decline.
“A main goal in hematology has been to understand how is it that these alternative fetal hemoglobin genes get silenced and how can we turn them back on,” said Dr. Bauer, a staff physician in pediatric hematology/oncology.
The gene BCL11A also plays key roles in the development of the central nervous system, B lymphatic lymphocyte maturation, and hematopoietic stem cell self-renewal. That led the researchers to hone in on targeting sequences around the BCL11A gene that act as erythroid enhancers, intending to limit potential complications by creating a very specific therapy for sickle cell disease.
In a related clinical trial, using lentiviral gene therapy rather than gene editing, researchers at Boston Children’s began an open-label, nonrandomized, single-center pilot study that involves a single infusion of autologous bone marrow derived CD34+ HSC cells transduced by a vector containing a short-hairpin segment of RNA targeting the gene BCL11A.
The study has a maximum accrual of seven evaluable patients, according to the NIH’s clinical trials website. The protocol is similar to bone marrow transplant, in that native blood stem cells are eliminated by myeloablative conditioning therapy. In this gene therapy, the patient’s own blood stem cells are then infused after the new genetic material has been added to counter the normal BCL11A off switch.
Swee Lay Thein, MBBS, an organizer of the NIH’s sickle cell conference, said in an interview that the “gene therapy side is really looking very optimistic.”
Dr. Thein, a senior investigator for sickle-cell genetics at the National Heart, Lung, and Blood Institute, earlier in her career discovered segments of DNA, including the BCL11A gene. She said that gaining greater understanding about genomic variation might someday aid in determining which people need more intense intervention for their sickle cell disease.
“You would be able to predict who will have more severe disease; we could monitor them more closely and perhaps even advocate for gene therapy or bone marrow transplant before complications have occurred rather than waiting for them to occur,” Dr. Thein said.
She referred to this as her “dream” for care of people with sickle cell disease. “This is still far off in the horizon.”
The NHLBI in September 2018 launched its Cure Sickle Cell Initiative. The agency estimates that it spends about $100 million on sickle cell disease research each year. The inherited blood disorder affects about 100,000 people in the United States and 20 million individuals worldwide. In sickle cell disease, a single genetic mutation causes red blood cells to form abnormal, sickle shapes that can clog the blood vessels and deprive cells of oxygen.
Dr. Thompson reported research funding and consulting agreements with Biomarin, Bluebird Bio, Celgene, Novartis, and Shire. Dr. Bauer reported patents related to BCL11A enhancer editing, consulting agreements with Merck and Pfizer, and research support from Bioverativ.
BETHESDA, MD. – Experimental gene therapies for sickle cell disease and thalassemia appear to be advancing, with BCL11A among the most promising targets in this field, researchers said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
Several highly anticipated presentations on the topic are expected for December meeting of the American Society of Hematology.
Alexis A. Thompson, MD, of Northwestern University, Chicago, reviewed highlights from a study in which the majority of patients given a gene therapy for transfusion dependent beta-thalassemia didn’t need subsequent blood transfusions. The New England Journal of Medicine in April published the results of this work done with Bluebird Bio’s LentiGlobin gene therapy (N Engl J Med. 2018; 378:1479-93).
Of the 22 patients in this trial, 15 have become transfusion independent, Dr. Thompson said in her presentation. Those patients that did not have this positive outcome still appear to have been helped by the gene therapy, she said. They had a median of 60% reduction in their transfusion volumes and nearly 60% in their number of transfusions.
“Whether it was transfusion independence or reduction in their transfusion volume or number, the vast majority of individuals in this first large-scale study had clinical benefit” from the therapy, said Dr. Thompson, who was the lead author of the study.
Dr. Thompson, the current president of the American Society of Hematology (ASH), said she’s looking forward to presentations on some of the most advanced gene therapies for sickle cell disease and thalassemia at the group’s annual meeting in December. The ASH presentations include those of John F. Tisdale, MD, who will report the latest data on LentiGlobin gene therapy in sickle cell disease, and Punam Malik, MD, of Cincinnati Children’s Hospital, who has developed a gamma globin lentivirus vector. There also will be a first readout on a particularly novel approach taken by researchers at Boston Children’s Hospital, led by David Williams, MD.
The development of CRISPR-Cas9 “has really opened up the field” of gene therapy, aiding researchers at Boston Children’s in their efforts to develop a treatment to maintain fetal hemoglobin production, Daniel E. Bauer, MD, PhD, of Boston Children’s Hospital, said during his presentation at the NIH conference.
Dr. Bauer provided an update on the BCL11A research that seeks to block what amounts to a genetic “off switch” for production of fetal hemoglobin. It’s long been known that erythrocytes of newborns with sickle cell disease are protected from sickling by high levels of fetal hemoglobin. Clinical manifestations of sickle cell disease then emerge in the first year of life as fetal hemoglobin levels decline.
“A main goal in hematology has been to understand how is it that these alternative fetal hemoglobin genes get silenced and how can we turn them back on,” said Dr. Bauer, a staff physician in pediatric hematology/oncology.
The gene BCL11A also plays key roles in the development of the central nervous system, B lymphatic lymphocyte maturation, and hematopoietic stem cell self-renewal. That led the researchers to hone in on targeting sequences around the BCL11A gene that act as erythroid enhancers, intending to limit potential complications by creating a very specific therapy for sickle cell disease.
In a related clinical trial, using lentiviral gene therapy rather than gene editing, researchers at Boston Children’s began an open-label, nonrandomized, single-center pilot study that involves a single infusion of autologous bone marrow derived CD34+ HSC cells transduced by a vector containing a short-hairpin segment of RNA targeting the gene BCL11A.
The study has a maximum accrual of seven evaluable patients, according to the NIH’s clinical trials website. The protocol is similar to bone marrow transplant, in that native blood stem cells are eliminated by myeloablative conditioning therapy. In this gene therapy, the patient’s own blood stem cells are then infused after the new genetic material has been added to counter the normal BCL11A off switch.
Swee Lay Thein, MBBS, an organizer of the NIH’s sickle cell conference, said in an interview that the “gene therapy side is really looking very optimistic.”
Dr. Thein, a senior investigator for sickle-cell genetics at the National Heart, Lung, and Blood Institute, earlier in her career discovered segments of DNA, including the BCL11A gene. She said that gaining greater understanding about genomic variation might someday aid in determining which people need more intense intervention for their sickle cell disease.
“You would be able to predict who will have more severe disease; we could monitor them more closely and perhaps even advocate for gene therapy or bone marrow transplant before complications have occurred rather than waiting for them to occur,” Dr. Thein said.
She referred to this as her “dream” for care of people with sickle cell disease. “This is still far off in the horizon.”
The NHLBI in September 2018 launched its Cure Sickle Cell Initiative. The agency estimates that it spends about $100 million on sickle cell disease research each year. The inherited blood disorder affects about 100,000 people in the United States and 20 million individuals worldwide. In sickle cell disease, a single genetic mutation causes red blood cells to form abnormal, sickle shapes that can clog the blood vessels and deprive cells of oxygen.
Dr. Thompson reported research funding and consulting agreements with Biomarin, Bluebird Bio, Celgene, Novartis, and Shire. Dr. Bauer reported patents related to BCL11A enhancer editing, consulting agreements with Merck and Pfizer, and research support from Bioverativ.
REPORTING FROM SICKLE CELL IN FOCUS
Links between SCT and adverse outcomes
Although sickle cell trait (SCT) has been linked to adverse clinical outcomes in multiple studies, only a handful of associations have strong evidence supporting them, according to a systematic review.
Evidence was strongest for the association between SCT and venous and renal complications.
There was low-strength evidence supporting a link between SCT and exertion-related sudden death and moderate-strength evidence supporting a link between SCT and exertion-related rhabdomyolysis.
Most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link.
Rakhi P. Naik, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues reported these findings in Annals of Internal Medicine.
The researchers’ systematic review was focused on 41 studies, most of which were population-based cohort or case-control studies.
The team rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, mortality, and renal, vascular, pediatric, surgery-, and trauma-related outcomes.
The researchers found low-strength evidence for a link between SCT and hematuria, end-stage renal disease, hypertension, myocardial infarction, retinopathy, diabetic vasculopathy, sudden infant death syndrome, surgery- and trauma-related injury, and overall mortality.
There was moderate-strength evidence for a link between SCT and pediatric height/weight, stroke, and heart failure/cardiomyopathy.
Exertion-related injury/death
The strength of evidence for a link between SCT and exertion-related death was low in this analysis, which included two studies of this outcome.
However, Dr. Naik and her colleagues did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions, such as highly strenuous athletic training or the military.
There was moderate-strength evidence supporting the link between SCT and exertional rhabdomyolysis, based on two studies.
However, the researchers said the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” the researchers wrote.
Venous and renal outcomes
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was moderate-strength evidence showing no increased risk of isolated deep-vein thrombosis in individuals with SCT.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” the researchers wrote.
Renal outcomes were often attributed to SCT, and the researchers said there was high-strength evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease (CKD).
Out of six studies of proteinuria, the one high-quality study showed a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without. The other studies “showed a consistent direction of increased risk for proteinuria with SCT,” according to the researchers.
Out of four CKD studies, the two high-quality studies showed a 1.57- and 1.89-fold increased risk of CKD in African Americans with SCT.
Support for this review came, in part, from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Although sickle cell trait (SCT) has been linked to adverse clinical outcomes in multiple studies, only a handful of associations have strong evidence supporting them, according to a systematic review.
Evidence was strongest for the association between SCT and venous and renal complications.
There was low-strength evidence supporting a link between SCT and exertion-related sudden death and moderate-strength evidence supporting a link between SCT and exertion-related rhabdomyolysis.
Most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link.
Rakhi P. Naik, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues reported these findings in Annals of Internal Medicine.
The researchers’ systematic review was focused on 41 studies, most of which were population-based cohort or case-control studies.
The team rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, mortality, and renal, vascular, pediatric, surgery-, and trauma-related outcomes.
The researchers found low-strength evidence for a link between SCT and hematuria, end-stage renal disease, hypertension, myocardial infarction, retinopathy, diabetic vasculopathy, sudden infant death syndrome, surgery- and trauma-related injury, and overall mortality.
There was moderate-strength evidence for a link between SCT and pediatric height/weight, stroke, and heart failure/cardiomyopathy.
Exertion-related injury/death
The strength of evidence for a link between SCT and exertion-related death was low in this analysis, which included two studies of this outcome.
However, Dr. Naik and her colleagues did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions, such as highly strenuous athletic training or the military.
There was moderate-strength evidence supporting the link between SCT and exertional rhabdomyolysis, based on two studies.
However, the researchers said the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” the researchers wrote.
Venous and renal outcomes
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was moderate-strength evidence showing no increased risk of isolated deep-vein thrombosis in individuals with SCT.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” the researchers wrote.
Renal outcomes were often attributed to SCT, and the researchers said there was high-strength evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease (CKD).
Out of six studies of proteinuria, the one high-quality study showed a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without. The other studies “showed a consistent direction of increased risk for proteinuria with SCT,” according to the researchers.
Out of four CKD studies, the two high-quality studies showed a 1.57- and 1.89-fold increased risk of CKD in African Americans with SCT.
Support for this review came, in part, from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Although sickle cell trait (SCT) has been linked to adverse clinical outcomes in multiple studies, only a handful of associations have strong evidence supporting them, according to a systematic review.
Evidence was strongest for the association between SCT and venous and renal complications.
There was low-strength evidence supporting a link between SCT and exertion-related sudden death and moderate-strength evidence supporting a link between SCT and exertion-related rhabdomyolysis.
Most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link.
Rakhi P. Naik, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues reported these findings in Annals of Internal Medicine.
The researchers’ systematic review was focused on 41 studies, most of which were population-based cohort or case-control studies.
The team rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, mortality, and renal, vascular, pediatric, surgery-, and trauma-related outcomes.
The researchers found low-strength evidence for a link between SCT and hematuria, end-stage renal disease, hypertension, myocardial infarction, retinopathy, diabetic vasculopathy, sudden infant death syndrome, surgery- and trauma-related injury, and overall mortality.
There was moderate-strength evidence for a link between SCT and pediatric height/weight, stroke, and heart failure/cardiomyopathy.
Exertion-related injury/death
The strength of evidence for a link between SCT and exertion-related death was low in this analysis, which included two studies of this outcome.
However, Dr. Naik and her colleagues did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions, such as highly strenuous athletic training or the military.
There was moderate-strength evidence supporting the link between SCT and exertional rhabdomyolysis, based on two studies.
However, the researchers said the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” the researchers wrote.
Venous and renal outcomes
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was moderate-strength evidence showing no increased risk of isolated deep-vein thrombosis in individuals with SCT.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” the researchers wrote.
Renal outcomes were often attributed to SCT, and the researchers said there was high-strength evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease (CKD).
Out of six studies of proteinuria, the one high-quality study showed a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without. The other studies “showed a consistent direction of increased risk for proteinuria with SCT,” according to the researchers.
Out of four CKD studies, the two high-quality studies showed a 1.57- and 1.89-fold increased risk of CKD in African Americans with SCT.
Support for this review came, in part, from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Few clinical outcomes convincingly linked to sickle cell trait
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: Risks of 1.57-fold and higher were seen in high-quality studies linking SCT to venous and renal complications, while studies of moderate quality suggested small absolute risks of exertion-related mortality or rhabdomyolysis.
Study details: A systematic review including 41 mostly population-based cohort or case-control studies looking at 24 clinical outcomes of interest.
Disclosures: Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Source: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Lnk deficiency boosts HSC replication in Fanconi anemia
A novel approach can restore hematopoietic stem cell (HSC) function in Fanconi anemia (FA), according to preclinical research published in Nature Communications.
The investigators showed that Lnk (Sh2b3) deficiency restores HSC proliferation and survival in Fancd2-deficient mice.
And it does so, in part, by alleviating blocks to cytokine-mediated JAK2 signaling.
These findings, the researchers wrote, “highlight a new role for cytokine/JAK signaling” and have therapeutic implications for FA.
The investigators noted that FA is caused by mutations in genes that are essential for DNA interstrand crosslink repair and replication stress tolerance.
Allogeneic transplant can replace defective HSCs in patients with FA, the researchers said, but there are no interventions that mitigate defects in HSCs. So the investigators decided to test whether Lnk deficiency ameliorates HSC defects in FA.
Using a model of FA in which mice lacked Fancd2, the researchers inhibited the regulatory protein Sh2b3/Lnk.
The investigators said Lnk deficiency restored the proliferation and survival of Fancd2−/− HSCs while also reducing replication stress and genomic instability. Lnk deficiency did not, however, affect DNA interstrand crosslink repair.
“We expected that inhibiting Lnk would restore the ability of FA cells to repair DNA damage, but this was not the case,” said study author Wei Tong, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Instead, inhibiting Lnk stabilized the stalled replication machinery, allowing affected cells to continue to copy DNA, and to prevent small errors from cascading into a catastrophic failure. The most exciting aspect of this discovery is that Lnk is part of a well-known growth pathway that can be manipulated by existing drugs in other diseases.”
That pathway is the TPO/MPL/JAK2 pathway, which is already targeted by eltrombopag and romiplostin for immune thrombocytopenia and eltrombopag for aplastic anemia.
The researchers plan to continue their work with animal models of FA and Lnk.
“Our ultimate goal is to translate our knowledge into treatments for both Fanconi anemia and for the broader problem of bone marrow failure,” Dr. Tong said.
This research was supported by the National Institutes of Health, the Fanconi Anemia Research Fund, the Department of Defense, the Basser Center for BRCA Team Science Grant, the Leukemia Lymphoma Society Scholar Award, and the Patel Family Award.
The researchers declared no competing interests.
A novel approach can restore hematopoietic stem cell (HSC) function in Fanconi anemia (FA), according to preclinical research published in Nature Communications.
The investigators showed that Lnk (Sh2b3) deficiency restores HSC proliferation and survival in Fancd2-deficient mice.
And it does so, in part, by alleviating blocks to cytokine-mediated JAK2 signaling.
These findings, the researchers wrote, “highlight a new role for cytokine/JAK signaling” and have therapeutic implications for FA.
The investigators noted that FA is caused by mutations in genes that are essential for DNA interstrand crosslink repair and replication stress tolerance.
Allogeneic transplant can replace defective HSCs in patients with FA, the researchers said, but there are no interventions that mitigate defects in HSCs. So the investigators decided to test whether Lnk deficiency ameliorates HSC defects in FA.
Using a model of FA in which mice lacked Fancd2, the researchers inhibited the regulatory protein Sh2b3/Lnk.
The investigators said Lnk deficiency restored the proliferation and survival of Fancd2−/− HSCs while also reducing replication stress and genomic instability. Lnk deficiency did not, however, affect DNA interstrand crosslink repair.
“We expected that inhibiting Lnk would restore the ability of FA cells to repair DNA damage, but this was not the case,” said study author Wei Tong, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Instead, inhibiting Lnk stabilized the stalled replication machinery, allowing affected cells to continue to copy DNA, and to prevent small errors from cascading into a catastrophic failure. The most exciting aspect of this discovery is that Lnk is part of a well-known growth pathway that can be manipulated by existing drugs in other diseases.”
That pathway is the TPO/MPL/JAK2 pathway, which is already targeted by eltrombopag and romiplostin for immune thrombocytopenia and eltrombopag for aplastic anemia.
The researchers plan to continue their work with animal models of FA and Lnk.
“Our ultimate goal is to translate our knowledge into treatments for both Fanconi anemia and for the broader problem of bone marrow failure,” Dr. Tong said.
This research was supported by the National Institutes of Health, the Fanconi Anemia Research Fund, the Department of Defense, the Basser Center for BRCA Team Science Grant, the Leukemia Lymphoma Society Scholar Award, and the Patel Family Award.
The researchers declared no competing interests.
A novel approach can restore hematopoietic stem cell (HSC) function in Fanconi anemia (FA), according to preclinical research published in Nature Communications.
The investigators showed that Lnk (Sh2b3) deficiency restores HSC proliferation and survival in Fancd2-deficient mice.
And it does so, in part, by alleviating blocks to cytokine-mediated JAK2 signaling.
These findings, the researchers wrote, “highlight a new role for cytokine/JAK signaling” and have therapeutic implications for FA.
The investigators noted that FA is caused by mutations in genes that are essential for DNA interstrand crosslink repair and replication stress tolerance.
Allogeneic transplant can replace defective HSCs in patients with FA, the researchers said, but there are no interventions that mitigate defects in HSCs. So the investigators decided to test whether Lnk deficiency ameliorates HSC defects in FA.
Using a model of FA in which mice lacked Fancd2, the researchers inhibited the regulatory protein Sh2b3/Lnk.
The investigators said Lnk deficiency restored the proliferation and survival of Fancd2−/− HSCs while also reducing replication stress and genomic instability. Lnk deficiency did not, however, affect DNA interstrand crosslink repair.
“We expected that inhibiting Lnk would restore the ability of FA cells to repair DNA damage, but this was not the case,” said study author Wei Tong, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Instead, inhibiting Lnk stabilized the stalled replication machinery, allowing affected cells to continue to copy DNA, and to prevent small errors from cascading into a catastrophic failure. The most exciting aspect of this discovery is that Lnk is part of a well-known growth pathway that can be manipulated by existing drugs in other diseases.”
That pathway is the TPO/MPL/JAK2 pathway, which is already targeted by eltrombopag and romiplostin for immune thrombocytopenia and eltrombopag for aplastic anemia.
The researchers plan to continue their work with animal models of FA and Lnk.
“Our ultimate goal is to translate our knowledge into treatments for both Fanconi anemia and for the broader problem of bone marrow failure,” Dr. Tong said.
This research was supported by the National Institutes of Health, the Fanconi Anemia Research Fund, the Department of Defense, the Basser Center for BRCA Team Science Grant, the Leukemia Lymphoma Society Scholar Award, and the Patel Family Award.
The researchers declared no competing interests.
Inhibitor receives orphan designation for ITP
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to PRN1008 for the treatment of patients with immune thrombocytopenia (ITP).
PRN1008 is an oral, reversible, covalent Bruton’s tyrosine kinase (BTK) inhibitor being developed by Principia Biopharma, Inc.
Principia is conducting a phase 1/2 trial (NCT03395210) to evaluate the safety and efficacy of PRN1008 in patients with ITP.
Results of preclinical research with PRN1008 in ITP were presented at the 2017 ASH Annual Meeting.
There, researchers reported that PRN1008 significantly reduced platelet loss in a mouse model of ITP.
The team found the BTK inhibitor could diminish platelet loss in two ways:
- By reducing platelet destruction via inhibition of autoantibody/FcγR signaling in splenic macrophages
- By reducing autoantibody generation through inhibition of B-cell activation and maturation.
The researchers also assessed the effects of PRN1008 and ibrutinib on platelet function in samples from healthy volunteers and ITP patients.
Samples were treated with one of the two BTK inhibitors, and platelet aggregation was induced by platelet agonists.
Unlike ibrutinib, PRN1008 did not impact platelet aggregation in healthy volunteer or ITP patient samples.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
‘Intense’ end-of-life care may be common in HSCT recipients
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
Patients who die within a year of allogeneic hematopoietic stem cell transplant (HSCT) tend to receive “medically intense” end-of-life care, an analysis suggests.
Researchers studied more than 2,000 patients who died within a year of allogeneic HSCT and found that a majority of the patients died in the hospital, and about half of them were admitted to the intensive care unit (ICU).
However, patient age, underlying diagnosis, and other factors influenced the likelihood of receiving intense end-of-life care.
For example, patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) were less likely than patients with acute lymphoblastic leukemia (ALL) to receive medically intense care.
Emily Johnston, MD, of the University of Alabama at Birmingham, and her colleagues reported these findings in the Journal of Clinical Oncology.
The researchers studied 2,135 patients in California who underwent inpatient HSCT and died within a year of the transplant (not as a result of peripartum events or trauma) between 2000 and 2013.
Fifty-three percent of the patients received some type of medically intense intervention, and 57% had at least two types of intense interventions.
Eighty-three percent of patients died in hospital, and 43% spent all of their last 30 days in the hospital.
Forty-nine percent of patients were admitted to the ICU, 45% were intubated, 22% underwent hemodialysis, and 8% received cardiopulmonary resuscitation.
Factors associated with intense care
The researchers said receipt of a medically intense intervention varied by age at death, underlying diagnosis, year of HSCT, location of care, and comorbidities. However, use of intense interventions did not vary according to sex, race/ethnicity, insurance type, or income.
Compared to patients age 60 and older, patients in the following age groups were more likely to receive medically intense interventions:
- Ages 15 to 21—odds ratio (OR)=2.6 (P<0.001)
- Ages 30 to 39—OR=1.8 (P<0.01)
- Ages 40 to 49—OR=1.4 (P<0.05).
Patients with comorbidities were more likely to receive intense interventions as well. The OR was 1.6 (P<0.01) for patients with one comorbidity and 2.5 (P<0.001) for patients with two or more comorbidities.
Patients with AML or MDS were less likely than patients with ALL to receive a medically intense intervention—OR=0.7 (P<0.05).
Patients who were transplanted between 2000 and 2004 were less likely to receive an intense intervention than patients transplanted between 2010 and 2013—OR=0.7 (P<0.01).
Patients who changed hospitals between HSCT and death were less likely to receive an intense intervention than patients who stayed at the same hospital. The OR was 0.3 if they transferred to a community hospital and 0.4 if they transferred to a specialty hospital (P<0.001 for both).
Patients living in rural areas were less likely than urban patients to receive a medically intense intervention—OR=0.6 (P<0.05).
“From our data, we understand there is a correlation with high-intensity end-of-life care in patients who die within one year after receiving a stem cell transplant, but we are still unsure if that was the care they wanted,” Dr. Johnston said.
“The findings suggest that, as oncologists, we need to start having end-of-life care conversations earlier with patients to determine if a high-intensity treatment plan is consistent with their goals or if a lower-intensity treatment plan is best. It’s not a one-size-fits-all approach in end-of-life care.”
This research was supported by Stanford University. One study author reported relationships with Corvus Pharmaceuticals, Shire Pharmaceuticals, and Adaptive Biotechnologies. All other authors reported no conflicts.
FDA approves DNA-based blood type test
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.
The for use in transfusion.
It’s the second molecular test for blood compatibility but the first to report genotype in its results, according to an announcement from the agency.
The test is important because it evaluates patients – especially those who receive repeated blood transfusions for conditions such as sickle cell anemia – for non-ABO antigens, but it does so without using antisera, which is sometimes unavailable.
A study found comparable performance between the ID CORE XT, licensed serologic reagents, and DNA sequencing tests, according to the FDA.
The ID CORE XT test is marketed by Progenika Biopharma, a Grifols company.
More information can be found in the full FDA press announcement.