User login
Auto-HSCT linked to higher AML, MDS risk
Patients undergoing autologous hematopoietic stem cell transplant (auto-HSCT) for lymphoma or myeloma have an increased risk of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to a retrospective study.
The study suggested these patients have 10 to 100 times the risk of AML or MDS as the general population.
The elevated risk also exceeds that of similar lymphoma and myeloma patients largely untreated with auto-HSCT.
Tomas Radivoyevitch, PhD, of the Cleveland Clinic Foundation in Ohio, and his colleagues reported these findings in Leukemia Research.
The investigators noted that exposure to DNA-damaging drugs and ionizing radiation—both used in auto-HSCT—is known to increase the risk of AML and MDS.
With this in mind, the team analyzed data on auto-HSCT recipients reported to the Center for International Blood and Marrow Transplant Research (CIBMTR).
Analyses were based on 9028 patients undergoing auto-HSCT from 1995 to 2010 for Hodgkin lymphoma (n=916), non-Hodgkin lymphoma (NHL, n=3546), or plasma cell myeloma (n=4566). Their median duration of follow-up was 90 months, 110 months, and 97 months, respectively.
Overall, 3.7% of the cohort developed AML or MDS after their transplant.
More aggressive transplant protocols increased the likelihood of this outcome. The risk of developing AML or MDS was higher for:
- Hodgkin lymphoma patients who received conditioning with total body radiation versus chemotherapy alone (hazard ratio [HR], 4.0)
- NHL patients who received conditioning with total body radiation (HR, 1.7) or with busulfan and melphalan or cyclophosphamide (HR, 1.8) versus the BEAM regimen (bischloroethylnitrosourea, etoposide, cytarabine, and melphalan)
- NHL or myeloma patients who received 3 or more lines of chemotherapy versus 1 line (HR, 1.9 for NHL and 1.8 for myeloma)
- NHL patients who underwent transplant in 2005 to 2010 versus 1995 to 1999 (HR, 2.1).
Patients reported to the Surveillance, Epidemiology and End Results database with the same lymphoma and myeloma diagnoses, few of whom underwent auto-HSCT, had risks of AML and MDS that were 5 to 10 times higher than the background level in the population.
However, the study auto-HSCT cohort had a risk of AML that was 10 to 50 times higher and a relative risk of MDS that was roughly 100 times higher than the background level.
“These increases may be related to exposure to high doses of DNA-damaging drugs given for [auto-HSCT], but this hypothesis can only be tested in a prospective study,” Dr Radivoyevitch and his coinvestigators wrote.
The reason for the greater elevation of MDS risk, compared with AML risk, is unknown.
“One possible explanation is that many cases of MDS evolve to AML, and that earlier diagnosis from increased post-transplant surveillance resulted in a deficiency of AML,” the investigators wrote. “A second is based on steeper MDS versus AML incidences versus age . . . and the possibility that transplantation recipient marrow ages (ie, marrow biological ages) are perhaps decades older than calendar ages.”
The study authors said they had no relevant conflicts of interest. The CIBMTR is supported by several US government agencies and numerous pharmaceutical companies.
Patients undergoing autologous hematopoietic stem cell transplant (auto-HSCT) for lymphoma or myeloma have an increased risk of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to a retrospective study.
The study suggested these patients have 10 to 100 times the risk of AML or MDS as the general population.
The elevated risk also exceeds that of similar lymphoma and myeloma patients largely untreated with auto-HSCT.
Tomas Radivoyevitch, PhD, of the Cleveland Clinic Foundation in Ohio, and his colleagues reported these findings in Leukemia Research.
The investigators noted that exposure to DNA-damaging drugs and ionizing radiation—both used in auto-HSCT—is known to increase the risk of AML and MDS.
With this in mind, the team analyzed data on auto-HSCT recipients reported to the Center for International Blood and Marrow Transplant Research (CIBMTR).
Analyses were based on 9028 patients undergoing auto-HSCT from 1995 to 2010 for Hodgkin lymphoma (n=916), non-Hodgkin lymphoma (NHL, n=3546), or plasma cell myeloma (n=4566). Their median duration of follow-up was 90 months, 110 months, and 97 months, respectively.
Overall, 3.7% of the cohort developed AML or MDS after their transplant.
More aggressive transplant protocols increased the likelihood of this outcome. The risk of developing AML or MDS was higher for:
- Hodgkin lymphoma patients who received conditioning with total body radiation versus chemotherapy alone (hazard ratio [HR], 4.0)
- NHL patients who received conditioning with total body radiation (HR, 1.7) or with busulfan and melphalan or cyclophosphamide (HR, 1.8) versus the BEAM regimen (bischloroethylnitrosourea, etoposide, cytarabine, and melphalan)
- NHL or myeloma patients who received 3 or more lines of chemotherapy versus 1 line (HR, 1.9 for NHL and 1.8 for myeloma)
- NHL patients who underwent transplant in 2005 to 2010 versus 1995 to 1999 (HR, 2.1).
Patients reported to the Surveillance, Epidemiology and End Results database with the same lymphoma and myeloma diagnoses, few of whom underwent auto-HSCT, had risks of AML and MDS that were 5 to 10 times higher than the background level in the population.
However, the study auto-HSCT cohort had a risk of AML that was 10 to 50 times higher and a relative risk of MDS that was roughly 100 times higher than the background level.
“These increases may be related to exposure to high doses of DNA-damaging drugs given for [auto-HSCT], but this hypothesis can only be tested in a prospective study,” Dr Radivoyevitch and his coinvestigators wrote.
The reason for the greater elevation of MDS risk, compared with AML risk, is unknown.
“One possible explanation is that many cases of MDS evolve to AML, and that earlier diagnosis from increased post-transplant surveillance resulted in a deficiency of AML,” the investigators wrote. “A second is based on steeper MDS versus AML incidences versus age . . . and the possibility that transplantation recipient marrow ages (ie, marrow biological ages) are perhaps decades older than calendar ages.”
The study authors said they had no relevant conflicts of interest. The CIBMTR is supported by several US government agencies and numerous pharmaceutical companies.
Patients undergoing autologous hematopoietic stem cell transplant (auto-HSCT) for lymphoma or myeloma have an increased risk of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to a retrospective study.
The study suggested these patients have 10 to 100 times the risk of AML or MDS as the general population.
The elevated risk also exceeds that of similar lymphoma and myeloma patients largely untreated with auto-HSCT.
Tomas Radivoyevitch, PhD, of the Cleveland Clinic Foundation in Ohio, and his colleagues reported these findings in Leukemia Research.
The investigators noted that exposure to DNA-damaging drugs and ionizing radiation—both used in auto-HSCT—is known to increase the risk of AML and MDS.
With this in mind, the team analyzed data on auto-HSCT recipients reported to the Center for International Blood and Marrow Transplant Research (CIBMTR).
Analyses were based on 9028 patients undergoing auto-HSCT from 1995 to 2010 for Hodgkin lymphoma (n=916), non-Hodgkin lymphoma (NHL, n=3546), or plasma cell myeloma (n=4566). Their median duration of follow-up was 90 months, 110 months, and 97 months, respectively.
Overall, 3.7% of the cohort developed AML or MDS after their transplant.
More aggressive transplant protocols increased the likelihood of this outcome. The risk of developing AML or MDS was higher for:
- Hodgkin lymphoma patients who received conditioning with total body radiation versus chemotherapy alone (hazard ratio [HR], 4.0)
- NHL patients who received conditioning with total body radiation (HR, 1.7) or with busulfan and melphalan or cyclophosphamide (HR, 1.8) versus the BEAM regimen (bischloroethylnitrosourea, etoposide, cytarabine, and melphalan)
- NHL or myeloma patients who received 3 or more lines of chemotherapy versus 1 line (HR, 1.9 for NHL and 1.8 for myeloma)
- NHL patients who underwent transplant in 2005 to 2010 versus 1995 to 1999 (HR, 2.1).
Patients reported to the Surveillance, Epidemiology and End Results database with the same lymphoma and myeloma diagnoses, few of whom underwent auto-HSCT, had risks of AML and MDS that were 5 to 10 times higher than the background level in the population.
However, the study auto-HSCT cohort had a risk of AML that was 10 to 50 times higher and a relative risk of MDS that was roughly 100 times higher than the background level.
“These increases may be related to exposure to high doses of DNA-damaging drugs given for [auto-HSCT], but this hypothesis can only be tested in a prospective study,” Dr Radivoyevitch and his coinvestigators wrote.
The reason for the greater elevation of MDS risk, compared with AML risk, is unknown.
“One possible explanation is that many cases of MDS evolve to AML, and that earlier diagnosis from increased post-transplant surveillance resulted in a deficiency of AML,” the investigators wrote. “A second is based on steeper MDS versus AML incidences versus age . . . and the possibility that transplantation recipient marrow ages (ie, marrow biological ages) are perhaps decades older than calendar ages.”
The study authors said they had no relevant conflicts of interest. The CIBMTR is supported by several US government agencies and numerous pharmaceutical companies.
Familial risk of myeloid malignancies
A large study has revealed “the strongest evidence yet” supporting genetic susceptibility to myeloid malignancies, according to a researcher.
The study showed that first-degree relatives of patients with myeloid malignancies had double the risk of developing a myeloid malignancy themselves, when compared to the general population.
The researchers observed significant risks for developing acute myeloid leukemia (AML), myelodysplastic syndromes (MDS), essential thrombocythemia (ET), and polycythemia vera (PV).
“Our study provides the strongest evidence yet for inherited risk for these diseases—evidence that has proved evasive before, in part, because these cancers are relatively uncommon, and our ability to characterize these diseases has, until recently, been limited,” said Amit Sud, MBChB, PhD, of The Institute of Cancer Research in London, UK.
Dr Sud and his colleagues described their research in a letter to Blood.
The researchers analyzed data from the Swedish Family-Cancer Database, which included 93,199 first-degree relatives of 35,037 patients with myeloid malignancies. The patients had been diagnosed between 1958 and 2015.
First-degree relatives of the patients had an increased risk of all myeloid malignancies, with a standardized incidence ratio (SIR) of 1.99 (95% CI 1.12-2.04).
For individual diseases, there was a significant association between family history and increased risk for:
- AML—SIR=1.53 (95% CI 1.21-2.17)
- ET—SIR=6.30 (95% CI 3.95-9.54)
- MDS—SIR=6.87 (95% CI 4.07-10.86)
- PV—SIR=7.66 (95% CI 5.74-10.02).
Dr Sud and his colleagues noted that the strongest familial relative risks tended to occur for the same disease, but there were significant associations between different myeloid malignancies as well.
Risk by age group
The researchers also looked at familial relative risk for the same disease by patients’ age at diagnosis and observed a significantly increased risk for younger cases for all myeloproliferative neoplasms (MPNs) combined, PV, and MDS.
The SIRs for MPNs were 6.46 (95% CI 5.12-8.04) for patients age 59 or younger and 4.15 (95% CI 3.38-5.04) for patients older than 59.
The SIRs for PV were 10.90 (95% CI 7.12-15.97) for patients age 59 or younger and 5.96 (95% CI 3.93-8.67) for patients older than 59.
The SIRs for MDS were 11.95 (95% CI 6.36-20.43) for patients age 68 or younger and 3.27 (95% CI 1.06-7.63) for patients older than 68.
Risk by number of relatives
Dr Sud and his colleagues also discovered that familial relative risks of all myeloid malignancies and MPNs were significantly associated with the number of first-degree relatives affected by myeloid malignancies or MPNs.
The SIRs for first-degree relatives with 2 or more affected relatives were 4.55 (95% CI 2.08-8.64) for all myeloid malignancies and 17.82 (95% CI 5.79-24.89) for MPNs.
The SIRs for first-degree relatives with 1 affected relative were 1.96 (95% CI 1.79-2.15) for all myeloid malignancies and 4.83 (95% CI 4.14-5.60) for MPNs.
The researchers said these results suggest inherited genetic changes increase the risk of myeloid malignancies, although environmental factors shared in families could also play a role.
“In the future, our findings could help identify people at higher risk than normal because of their family background who could be prioritized for medical help like screening to catch the disease earlier if it arises,” Dr Sud said.
This study was funded by German Cancer Aid, the Swedish Research Council, ALF funding from Region Skåne, DKFZ, and Bloodwise.
A large study has revealed “the strongest evidence yet” supporting genetic susceptibility to myeloid malignancies, according to a researcher.
The study showed that first-degree relatives of patients with myeloid malignancies had double the risk of developing a myeloid malignancy themselves, when compared to the general population.
The researchers observed significant risks for developing acute myeloid leukemia (AML), myelodysplastic syndromes (MDS), essential thrombocythemia (ET), and polycythemia vera (PV).
“Our study provides the strongest evidence yet for inherited risk for these diseases—evidence that has proved evasive before, in part, because these cancers are relatively uncommon, and our ability to characterize these diseases has, until recently, been limited,” said Amit Sud, MBChB, PhD, of The Institute of Cancer Research in London, UK.
Dr Sud and his colleagues described their research in a letter to Blood.
The researchers analyzed data from the Swedish Family-Cancer Database, which included 93,199 first-degree relatives of 35,037 patients with myeloid malignancies. The patients had been diagnosed between 1958 and 2015.
First-degree relatives of the patients had an increased risk of all myeloid malignancies, with a standardized incidence ratio (SIR) of 1.99 (95% CI 1.12-2.04).
For individual diseases, there was a significant association between family history and increased risk for:
- AML—SIR=1.53 (95% CI 1.21-2.17)
- ET—SIR=6.30 (95% CI 3.95-9.54)
- MDS—SIR=6.87 (95% CI 4.07-10.86)
- PV—SIR=7.66 (95% CI 5.74-10.02).
Dr Sud and his colleagues noted that the strongest familial relative risks tended to occur for the same disease, but there were significant associations between different myeloid malignancies as well.
Risk by age group
The researchers also looked at familial relative risk for the same disease by patients’ age at diagnosis and observed a significantly increased risk for younger cases for all myeloproliferative neoplasms (MPNs) combined, PV, and MDS.
The SIRs for MPNs were 6.46 (95% CI 5.12-8.04) for patients age 59 or younger and 4.15 (95% CI 3.38-5.04) for patients older than 59.
The SIRs for PV were 10.90 (95% CI 7.12-15.97) for patients age 59 or younger and 5.96 (95% CI 3.93-8.67) for patients older than 59.
The SIRs for MDS were 11.95 (95% CI 6.36-20.43) for patients age 68 or younger and 3.27 (95% CI 1.06-7.63) for patients older than 68.
Risk by number of relatives
Dr Sud and his colleagues also discovered that familial relative risks of all myeloid malignancies and MPNs were significantly associated with the number of first-degree relatives affected by myeloid malignancies or MPNs.
The SIRs for first-degree relatives with 2 or more affected relatives were 4.55 (95% CI 2.08-8.64) for all myeloid malignancies and 17.82 (95% CI 5.79-24.89) for MPNs.
The SIRs for first-degree relatives with 1 affected relative were 1.96 (95% CI 1.79-2.15) for all myeloid malignancies and 4.83 (95% CI 4.14-5.60) for MPNs.
The researchers said these results suggest inherited genetic changes increase the risk of myeloid malignancies, although environmental factors shared in families could also play a role.
“In the future, our findings could help identify people at higher risk than normal because of their family background who could be prioritized for medical help like screening to catch the disease earlier if it arises,” Dr Sud said.
This study was funded by German Cancer Aid, the Swedish Research Council, ALF funding from Region Skåne, DKFZ, and Bloodwise.
A large study has revealed “the strongest evidence yet” supporting genetic susceptibility to myeloid malignancies, according to a researcher.
The study showed that first-degree relatives of patients with myeloid malignancies had double the risk of developing a myeloid malignancy themselves, when compared to the general population.
The researchers observed significant risks for developing acute myeloid leukemia (AML), myelodysplastic syndromes (MDS), essential thrombocythemia (ET), and polycythemia vera (PV).
“Our study provides the strongest evidence yet for inherited risk for these diseases—evidence that has proved evasive before, in part, because these cancers are relatively uncommon, and our ability to characterize these diseases has, until recently, been limited,” said Amit Sud, MBChB, PhD, of The Institute of Cancer Research in London, UK.
Dr Sud and his colleagues described their research in a letter to Blood.
The researchers analyzed data from the Swedish Family-Cancer Database, which included 93,199 first-degree relatives of 35,037 patients with myeloid malignancies. The patients had been diagnosed between 1958 and 2015.
First-degree relatives of the patients had an increased risk of all myeloid malignancies, with a standardized incidence ratio (SIR) of 1.99 (95% CI 1.12-2.04).
For individual diseases, there was a significant association between family history and increased risk for:
- AML—SIR=1.53 (95% CI 1.21-2.17)
- ET—SIR=6.30 (95% CI 3.95-9.54)
- MDS—SIR=6.87 (95% CI 4.07-10.86)
- PV—SIR=7.66 (95% CI 5.74-10.02).
Dr Sud and his colleagues noted that the strongest familial relative risks tended to occur for the same disease, but there were significant associations between different myeloid malignancies as well.
Risk by age group
The researchers also looked at familial relative risk for the same disease by patients’ age at diagnosis and observed a significantly increased risk for younger cases for all myeloproliferative neoplasms (MPNs) combined, PV, and MDS.
The SIRs for MPNs were 6.46 (95% CI 5.12-8.04) for patients age 59 or younger and 4.15 (95% CI 3.38-5.04) for patients older than 59.
The SIRs for PV were 10.90 (95% CI 7.12-15.97) for patients age 59 or younger and 5.96 (95% CI 3.93-8.67) for patients older than 59.
The SIRs for MDS were 11.95 (95% CI 6.36-20.43) for patients age 68 or younger and 3.27 (95% CI 1.06-7.63) for patients older than 68.
Risk by number of relatives
Dr Sud and his colleagues also discovered that familial relative risks of all myeloid malignancies and MPNs were significantly associated with the number of first-degree relatives affected by myeloid malignancies or MPNs.
The SIRs for first-degree relatives with 2 or more affected relatives were 4.55 (95% CI 2.08-8.64) for all myeloid malignancies and 17.82 (95% CI 5.79-24.89) for MPNs.
The SIRs for first-degree relatives with 1 affected relative were 1.96 (95% CI 1.79-2.15) for all myeloid malignancies and 4.83 (95% CI 4.14-5.60) for MPNs.
The researchers said these results suggest inherited genetic changes increase the risk of myeloid malignancies, although environmental factors shared in families could also play a role.
“In the future, our findings could help identify people at higher risk than normal because of their family background who could be prioritized for medical help like screening to catch the disease earlier if it arises,” Dr Sud said.
This study was funded by German Cancer Aid, the Swedish Research Council, ALF funding from Region Skåne, DKFZ, and Bloodwise.
FA pathway key to DNA repair after CRISPR cutting
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
CHMP recommends generic deferiprone
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for Deferiprone Lipomed to treat iron overload in patients with thalassemia major.
Deferiprone Lipomed is a generic version of the iron chelating agent Ferriprox, which has been authorized in the European Union since August 1999.
According to the CHMP, studies have shown that Deferiprone Lipomed is of satisfactory quality and bioequivalent to Ferriprox.
The CHMP’s recommendation for Deferiprone Lipomed will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Deferiprone Lipomed will be available as 500-mg film-coated tablets.
The drug will be authorized for the following uses:
- As monotherapy to treat iron overload in patients with thalassemia major when current chelation therapy is contraindicated or inadequate
- In combination with another chelator in patients with thalassemia major when monotherapy with any iron chelator is ineffective or when prevention or treatment of life-threatening consequences of iron overload justifies rapid or intensive correction.
According to the prescribing information for Ferriprox, the combination of iron chelators should be considered on a case-by-case basis, and patients should be monitored for response and adverse events.
Fatalities and life-threatening situations (caused by agranulocytosis) have been reported with the combination of deferiprone and deferoxamine.
Combination therapy is not recommended when monotherapy with either chelator is adequate or when serum ferritin falls below 500 μg/l. Additionally, there are limited data on the combined use of Ferriprox and deferasirox.
The applicant for Deferiprone Lipomed is Lipomed GmbH.
CHMP supports expanded approval for epoetin alfa products
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a change to the terms of marketing authorization for 3 versions of epoetin alfa—Abseamed, Binocrit, and Epoetin alfa Hexal.
The CHMP is recommending that all 3 products be approved to treat symptomatic anemia (hemoglobin concentration of ≤ 10 g/dL) in adults with low- or intermediate-1-risk primary myelodysplastic syndromes who have low serum erythropoietin (< 200 mU/mL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Abseamed, Binocrit, and Epoetin alfa Hexal are already EC-approved for the following indications:
- To treat symptomatic anemia associated with chronic renal failure in adults and children ages 1 to 18 on hemodialysis and adults on peritoneal dialysis
- To treat symptomatic anemia associated with chronic renal failure in adults with renal insufficiency not yet undergoing dialysis for the treatment of severe anemia of renal origin accompanied by clinical symptoms in patients
- For adults receiving chemotherapy for solid tumors, malignant lymphoma, or multiple myeloma who are at risk of transfusion as assessed by the patient’s general status (eg, cardiovascular status, pre-existing anemia at the start of chemotherapy) for the treatment of anemia and reduction of transfusion requirements
- For adults in a predonation program to increase the yield of autologous blood; treatment should only be given to patients with moderate anemia (hemoglobin concentration range between 10 to 13 g/dL [6.2 to 8.1 mmol/L], no iron deficiency) if blood-saving procedures are not available or insufficient when the scheduled major elective surgery requires a large volume of blood (4 or more units for females or 5 or more units for males)
- For non-iron-deficient adults set to undergo major elective orthopedic surgery who have a high perceived risk for transfusion complications to reduce exposure to allogeneic blood transfusions; use should be restricted to patients with moderate anemia (eg, hemoglobin concentration range between 10 to 13 g/dL or 6.2 to 8.1 mmol/L) who do not have an autologous predonation program available and with expected moderate blood loss (900 to 1800 mL).
The marketing authorization holders are Medice Arzneimittel Pütter GmbH & Co. KG for Abseamed, Sandoz GmbH for Binocrit, and Hexal AG for Epoetin alfa Hexal.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a change to the terms of marketing authorization for 3 versions of epoetin alfa—Abseamed, Binocrit, and Epoetin alfa Hexal.
The CHMP is recommending that all 3 products be approved to treat symptomatic anemia (hemoglobin concentration of ≤ 10 g/dL) in adults with low- or intermediate-1-risk primary myelodysplastic syndromes who have low serum erythropoietin (< 200 mU/mL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Abseamed, Binocrit, and Epoetin alfa Hexal are already EC-approved for the following indications:
- To treat symptomatic anemia associated with chronic renal failure in adults and children ages 1 to 18 on hemodialysis and adults on peritoneal dialysis
- To treat symptomatic anemia associated with chronic renal failure in adults with renal insufficiency not yet undergoing dialysis for the treatment of severe anemia of renal origin accompanied by clinical symptoms in patients
- For adults receiving chemotherapy for solid tumors, malignant lymphoma, or multiple myeloma who are at risk of transfusion as assessed by the patient’s general status (eg, cardiovascular status, pre-existing anemia at the start of chemotherapy) for the treatment of anemia and reduction of transfusion requirements
- For adults in a predonation program to increase the yield of autologous blood; treatment should only be given to patients with moderate anemia (hemoglobin concentration range between 10 to 13 g/dL [6.2 to 8.1 mmol/L], no iron deficiency) if blood-saving procedures are not available or insufficient when the scheduled major elective surgery requires a large volume of blood (4 or more units for females or 5 or more units for males)
- For non-iron-deficient adults set to undergo major elective orthopedic surgery who have a high perceived risk for transfusion complications to reduce exposure to allogeneic blood transfusions; use should be restricted to patients with moderate anemia (eg, hemoglobin concentration range between 10 to 13 g/dL or 6.2 to 8.1 mmol/L) who do not have an autologous predonation program available and with expected moderate blood loss (900 to 1800 mL).
The marketing authorization holders are Medice Arzneimittel Pütter GmbH & Co. KG for Abseamed, Sandoz GmbH for Binocrit, and Hexal AG for Epoetin alfa Hexal.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a change to the terms of marketing authorization for 3 versions of epoetin alfa—Abseamed, Binocrit, and Epoetin alfa Hexal.
The CHMP is recommending that all 3 products be approved to treat symptomatic anemia (hemoglobin concentration of ≤ 10 g/dL) in adults with low- or intermediate-1-risk primary myelodysplastic syndromes who have low serum erythropoietin (< 200 mU/mL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of the CHMP’s recommendation.
Abseamed, Binocrit, and Epoetin alfa Hexal are already EC-approved for the following indications:
- To treat symptomatic anemia associated with chronic renal failure in adults and children ages 1 to 18 on hemodialysis and adults on peritoneal dialysis
- To treat symptomatic anemia associated with chronic renal failure in adults with renal insufficiency not yet undergoing dialysis for the treatment of severe anemia of renal origin accompanied by clinical symptoms in patients
- For adults receiving chemotherapy for solid tumors, malignant lymphoma, or multiple myeloma who are at risk of transfusion as assessed by the patient’s general status (eg, cardiovascular status, pre-existing anemia at the start of chemotherapy) for the treatment of anemia and reduction of transfusion requirements
- For adults in a predonation program to increase the yield of autologous blood; treatment should only be given to patients with moderate anemia (hemoglobin concentration range between 10 to 13 g/dL [6.2 to 8.1 mmol/L], no iron deficiency) if blood-saving procedures are not available or insufficient when the scheduled major elective surgery requires a large volume of blood (4 or more units for females or 5 or more units for males)
- For non-iron-deficient adults set to undergo major elective orthopedic surgery who have a high perceived risk for transfusion complications to reduce exposure to allogeneic blood transfusions; use should be restricted to patients with moderate anemia (eg, hemoglobin concentration range between 10 to 13 g/dL or 6.2 to 8.1 mmol/L) who do not have an autologous predonation program available and with expected moderate blood loss (900 to 1800 mL).
The marketing authorization holders are Medice Arzneimittel Pütter GmbH & Co. KG for Abseamed, Sandoz GmbH for Binocrit, and Hexal AG for Epoetin alfa Hexal.
CHMP backs 2 biosimilar pegfilgrastim products
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for 2 pegfilgrastim biosimilar candidates—Udenyca and Pelgraz.
Both products have been deemed highly similar to the reference product, Neulasta, a growth-colony-stimulating factor intended to reduce the duration of neutropenia and the incidence of febrile neutropenia due to chemotherapy.
The CHMP’s recommendations for Pelgraz and Udenyca will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Udenyca and Pelgraz will be available as 6 mg solutions for injection.
The full indication for both products will be to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies, except chronic myeloid leukemia and myelodysplastic syndromes.
The CHMP said data have shown that Pelgraz and Udenyca both have comparable quality, safety, and efficacy to Neulasta.
Pelgraz’s marketing authorization application is supported by data from a phase 1 pharmacokinetic (PK) and pharmacodynamic (PD) study in healthy volunteers and a phase 3 study of breast cancer patients receiving docetaxel, doxorubicin, and cyclophosphamide.
Results from the phase 1 study were published in Clinical Pharmacology in Drug Development in 2016.
Udenyca’s marketing authorization application is supported by data from an immunogenicity study as well as a PK/PD study comparing Udenyca (formerly CHS-1701) and Neulasta in healthy subjects.
Results from the PK/PD trial were presented at the 2017 ASCO Annual Meeting.
The applicant for Udenyca is ERA Consulting GmbH. The applicant for Pelgraz is Accord Healthcare Limited (the international arm of Intas Pharmaceuticals Ltd).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for 2 pegfilgrastim biosimilar candidates—Udenyca and Pelgraz.
Both products have been deemed highly similar to the reference product, Neulasta, a growth-colony-stimulating factor intended to reduce the duration of neutropenia and the incidence of febrile neutropenia due to chemotherapy.
The CHMP’s recommendations for Pelgraz and Udenyca will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Udenyca and Pelgraz will be available as 6 mg solutions for injection.
The full indication for both products will be to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies, except chronic myeloid leukemia and myelodysplastic syndromes.
The CHMP said data have shown that Pelgraz and Udenyca both have comparable quality, safety, and efficacy to Neulasta.
Pelgraz’s marketing authorization application is supported by data from a phase 1 pharmacokinetic (PK) and pharmacodynamic (PD) study in healthy volunteers and a phase 3 study of breast cancer patients receiving docetaxel, doxorubicin, and cyclophosphamide.
Results from the phase 1 study were published in Clinical Pharmacology in Drug Development in 2016.
Udenyca’s marketing authorization application is supported by data from an immunogenicity study as well as a PK/PD study comparing Udenyca (formerly CHS-1701) and Neulasta in healthy subjects.
Results from the PK/PD trial were presented at the 2017 ASCO Annual Meeting.
The applicant for Udenyca is ERA Consulting GmbH. The applicant for Pelgraz is Accord Healthcare Limited (the international arm of Intas Pharmaceuticals Ltd).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for 2 pegfilgrastim biosimilar candidates—Udenyca and Pelgraz.
Both products have been deemed highly similar to the reference product, Neulasta, a growth-colony-stimulating factor intended to reduce the duration of neutropenia and the incidence of febrile neutropenia due to chemotherapy.
The CHMP’s recommendations for Pelgraz and Udenyca will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
If approved, Udenyca and Pelgraz will be available as 6 mg solutions for injection.
The full indication for both products will be to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic chemotherapy for malignancies, except chronic myeloid leukemia and myelodysplastic syndromes.
The CHMP said data have shown that Pelgraz and Udenyca both have comparable quality, safety, and efficacy to Neulasta.
Pelgraz’s marketing authorization application is supported by data from a phase 1 pharmacokinetic (PK) and pharmacodynamic (PD) study in healthy volunteers and a phase 3 study of breast cancer patients receiving docetaxel, doxorubicin, and cyclophosphamide.
Results from the phase 1 study were published in Clinical Pharmacology in Drug Development in 2016.
Udenyca’s marketing authorization application is supported by data from an immunogenicity study as well as a PK/PD study comparing Udenyca (formerly CHS-1701) and Neulasta in healthy subjects.
Results from the PK/PD trial were presented at the 2017 ASCO Annual Meeting.
The applicant for Udenyca is ERA Consulting GmbH. The applicant for Pelgraz is Accord Healthcare Limited (the international arm of Intas Pharmaceuticals Ltd).
Study could change treatment of MLSM7
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
Gene therapy granted accelerated assessment
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use has granted accelerated assessment for the upcoming marketing authorization application (MAA) for LentiGlobin™.
LentiGlobin is a gene therapy intended for the treatment of adolescents and adults with transfusion-dependent β-thalassemia (TDT) and a non-β0/β0 genotype.
bluebird bio intends to file an MAA for LentiGlobin with the EMA this year.
Accelerated assessment can reduce the active review time of an MAA from 210 days to 150 days once it has been validated by the EMA.
An accelerated assessment is granted to products deemed to be of major interest for public health and represent therapeutic innovation.
The accelerated assessment for LentiGlobin is supported by data from clinical studies, including the phase 1/2 Northstar (HGB-204) study, phase 1/2 HGB-205 study, phase 3 Northstar-2 (HGB-207) study, and the long-term follow-up study LTF-303.
The EMA previously granted PRIME (Priority Medicines) eligibility and orphan designation to LentiGlobin for the treatment of TDT.
LentiGlobin is also part of the EMA’s Adaptive Pathways pilot program, which is part of the EMA’s effort to improve timely access to new medicines.
Phase 1/2 trials
Results from the phase 1/2 trials of LentiGlobin—HGB-204 and HGB-205—were published in NEJM in April.
HGB-204 is a completed study that included 18 patients with TDT. Eight patients had a β0/β0 genotype, 6 had a βE/β0 genotype, and 4 had other genotypes.
HGB-205 is an ongoing study, and results were reported for 4 patients with TDT. Three patients had a βE/β0 genotype. The remaining patient was homozygous for the IVS1-110 mutation and had a severe clinical presentation similar to that seen in β0/β0 genotypes.
For both studies, the researchers harvested hematopoietic stem and progenitor cells (mobilized with filgrastim and plerixafor) from the patients. CD34+ cells were transduced ex vivo with LentiGlobin BB305 vector, which encodes adult hemoglobin (HbA) with a T87Q amino acid substitution (HbAT87Q).
The patients underwent myeloablative conditioning with busulfan, and the final LentiGlobin product was infused into patients after a 72-hour washout period.
In HGB-205 only, patients received enhanced red blood cell (RBC) transfusions for at least 3 months before stem cell mobilization and harvest to maintain a hemoglobin level of more than 11.0 g/dL.
Safety
In HGB-204, there were 5 grade 1 adverse events (AEs) considered possibly or probably related to LentiGlobin—abdominal pain (n=2), dyspnea (n=1), hot flush (n=1), and non-cardiac chest pain (n=1).
There were 9 serious AEs. Grade 3 serious AEs included 2 episodes of veno-occlusive liver disease that were attributed to busulfan, Klebsiella infection, cardiac ventricular thrombosis, cellulitis, hyperglycemia, and gastroenteritis. Grade 2 serious AEs included device-related thrombosis and infectious diarrhea.
In HGB-205, there were no AEs considered possibly or probably related to LentiGlobin. The 3 serious AEs were tooth infection (grade 3), major depression (grade 3), and pneumonia (grade 2).
Efficacy
The median time to neutrophil engraftment was 18.5 days (range, 14.0 to 30.0) in HGB-204 and 16.5 days (range, 14.0 to 29.0) in HGB-205.
The median time to platelet engraftment was 39.5 days (range, 19.0 to 191.0) and 23.0 days (range, 20.0 to 26.0), respectively.
In both studies, the median follow-up was 26 months (range, 15 to 42) after LentiGlobin infusion.
At last follow-up, all but 1 of the 13 patients with a non-β0/β0 genotype had stopped receiving RBC transfusions.
In the 8 patients with a β0/β0 genotype and the 1 patient with 2 copies of the IVS1-110 mutation, the median annualized transfusion volume decreased by 73% after LentiGlobin administration.
Two patients with a β0/β0 genotype were able to stop receiving RBC transfusions, as was the patient with 2 copies of the IVS1-110 mutation.
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use has granted accelerated assessment for the upcoming marketing authorization application (MAA) for LentiGlobin™.
LentiGlobin is a gene therapy intended for the treatment of adolescents and adults with transfusion-dependent β-thalassemia (TDT) and a non-β0/β0 genotype.
bluebird bio intends to file an MAA for LentiGlobin with the EMA this year.
Accelerated assessment can reduce the active review time of an MAA from 210 days to 150 days once it has been validated by the EMA.
An accelerated assessment is granted to products deemed to be of major interest for public health and represent therapeutic innovation.
The accelerated assessment for LentiGlobin is supported by data from clinical studies, including the phase 1/2 Northstar (HGB-204) study, phase 1/2 HGB-205 study, phase 3 Northstar-2 (HGB-207) study, and the long-term follow-up study LTF-303.
The EMA previously granted PRIME (Priority Medicines) eligibility and orphan designation to LentiGlobin for the treatment of TDT.
LentiGlobin is also part of the EMA’s Adaptive Pathways pilot program, which is part of the EMA’s effort to improve timely access to new medicines.
Phase 1/2 trials
Results from the phase 1/2 trials of LentiGlobin—HGB-204 and HGB-205—were published in NEJM in April.
HGB-204 is a completed study that included 18 patients with TDT. Eight patients had a β0/β0 genotype, 6 had a βE/β0 genotype, and 4 had other genotypes.
HGB-205 is an ongoing study, and results were reported for 4 patients with TDT. Three patients had a βE/β0 genotype. The remaining patient was homozygous for the IVS1-110 mutation and had a severe clinical presentation similar to that seen in β0/β0 genotypes.
For both studies, the researchers harvested hematopoietic stem and progenitor cells (mobilized with filgrastim and plerixafor) from the patients. CD34+ cells were transduced ex vivo with LentiGlobin BB305 vector, which encodes adult hemoglobin (HbA) with a T87Q amino acid substitution (HbAT87Q).
The patients underwent myeloablative conditioning with busulfan, and the final LentiGlobin product was infused into patients after a 72-hour washout period.
In HGB-205 only, patients received enhanced red blood cell (RBC) transfusions for at least 3 months before stem cell mobilization and harvest to maintain a hemoglobin level of more than 11.0 g/dL.
Safety
In HGB-204, there were 5 grade 1 adverse events (AEs) considered possibly or probably related to LentiGlobin—abdominal pain (n=2), dyspnea (n=1), hot flush (n=1), and non-cardiac chest pain (n=1).
There were 9 serious AEs. Grade 3 serious AEs included 2 episodes of veno-occlusive liver disease that were attributed to busulfan, Klebsiella infection, cardiac ventricular thrombosis, cellulitis, hyperglycemia, and gastroenteritis. Grade 2 serious AEs included device-related thrombosis and infectious diarrhea.
In HGB-205, there were no AEs considered possibly or probably related to LentiGlobin. The 3 serious AEs were tooth infection (grade 3), major depression (grade 3), and pneumonia (grade 2).
Efficacy
The median time to neutrophil engraftment was 18.5 days (range, 14.0 to 30.0) in HGB-204 and 16.5 days (range, 14.0 to 29.0) in HGB-205.
The median time to platelet engraftment was 39.5 days (range, 19.0 to 191.0) and 23.0 days (range, 20.0 to 26.0), respectively.
In both studies, the median follow-up was 26 months (range, 15 to 42) after LentiGlobin infusion.
At last follow-up, all but 1 of the 13 patients with a non-β0/β0 genotype had stopped receiving RBC transfusions.
In the 8 patients with a β0/β0 genotype and the 1 patient with 2 copies of the IVS1-110 mutation, the median annualized transfusion volume decreased by 73% after LentiGlobin administration.
Two patients with a β0/β0 genotype were able to stop receiving RBC transfusions, as was the patient with 2 copies of the IVS1-110 mutation.
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use has granted accelerated assessment for the upcoming marketing authorization application (MAA) for LentiGlobin™.
LentiGlobin is a gene therapy intended for the treatment of adolescents and adults with transfusion-dependent β-thalassemia (TDT) and a non-β0/β0 genotype.
bluebird bio intends to file an MAA for LentiGlobin with the EMA this year.
Accelerated assessment can reduce the active review time of an MAA from 210 days to 150 days once it has been validated by the EMA.
An accelerated assessment is granted to products deemed to be of major interest for public health and represent therapeutic innovation.
The accelerated assessment for LentiGlobin is supported by data from clinical studies, including the phase 1/2 Northstar (HGB-204) study, phase 1/2 HGB-205 study, phase 3 Northstar-2 (HGB-207) study, and the long-term follow-up study LTF-303.
The EMA previously granted PRIME (Priority Medicines) eligibility and orphan designation to LentiGlobin for the treatment of TDT.
LentiGlobin is also part of the EMA’s Adaptive Pathways pilot program, which is part of the EMA’s effort to improve timely access to new medicines.
Phase 1/2 trials
Results from the phase 1/2 trials of LentiGlobin—HGB-204 and HGB-205—were published in NEJM in April.
HGB-204 is a completed study that included 18 patients with TDT. Eight patients had a β0/β0 genotype, 6 had a βE/β0 genotype, and 4 had other genotypes.
HGB-205 is an ongoing study, and results were reported for 4 patients with TDT. Three patients had a βE/β0 genotype. The remaining patient was homozygous for the IVS1-110 mutation and had a severe clinical presentation similar to that seen in β0/β0 genotypes.
For both studies, the researchers harvested hematopoietic stem and progenitor cells (mobilized with filgrastim and plerixafor) from the patients. CD34+ cells were transduced ex vivo with LentiGlobin BB305 vector, which encodes adult hemoglobin (HbA) with a T87Q amino acid substitution (HbAT87Q).
The patients underwent myeloablative conditioning with busulfan, and the final LentiGlobin product was infused into patients after a 72-hour washout period.
In HGB-205 only, patients received enhanced red blood cell (RBC) transfusions for at least 3 months before stem cell mobilization and harvest to maintain a hemoglobin level of more than 11.0 g/dL.
Safety
In HGB-204, there were 5 grade 1 adverse events (AEs) considered possibly or probably related to LentiGlobin—abdominal pain (n=2), dyspnea (n=1), hot flush (n=1), and non-cardiac chest pain (n=1).
There were 9 serious AEs. Grade 3 serious AEs included 2 episodes of veno-occlusive liver disease that were attributed to busulfan, Klebsiella infection, cardiac ventricular thrombosis, cellulitis, hyperglycemia, and gastroenteritis. Grade 2 serious AEs included device-related thrombosis and infectious diarrhea.
In HGB-205, there were no AEs considered possibly or probably related to LentiGlobin. The 3 serious AEs were tooth infection (grade 3), major depression (grade 3), and pneumonia (grade 2).
Efficacy
The median time to neutrophil engraftment was 18.5 days (range, 14.0 to 30.0) in HGB-204 and 16.5 days (range, 14.0 to 29.0) in HGB-205.
The median time to platelet engraftment was 39.5 days (range, 19.0 to 191.0) and 23.0 days (range, 20.0 to 26.0), respectively.
In both studies, the median follow-up was 26 months (range, 15 to 42) after LentiGlobin infusion.
At last follow-up, all but 1 of the 13 patients with a non-β0/β0 genotype had stopped receiving RBC transfusions.
In the 8 patients with a β0/β0 genotype and the 1 patient with 2 copies of the IVS1-110 mutation, the median annualized transfusion volume decreased by 73% after LentiGlobin administration.
Two patients with a β0/β0 genotype were able to stop receiving RBC transfusions, as was the patient with 2 copies of the IVS1-110 mutation.
In Ghana, SCD research is meeting patients on home turf
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
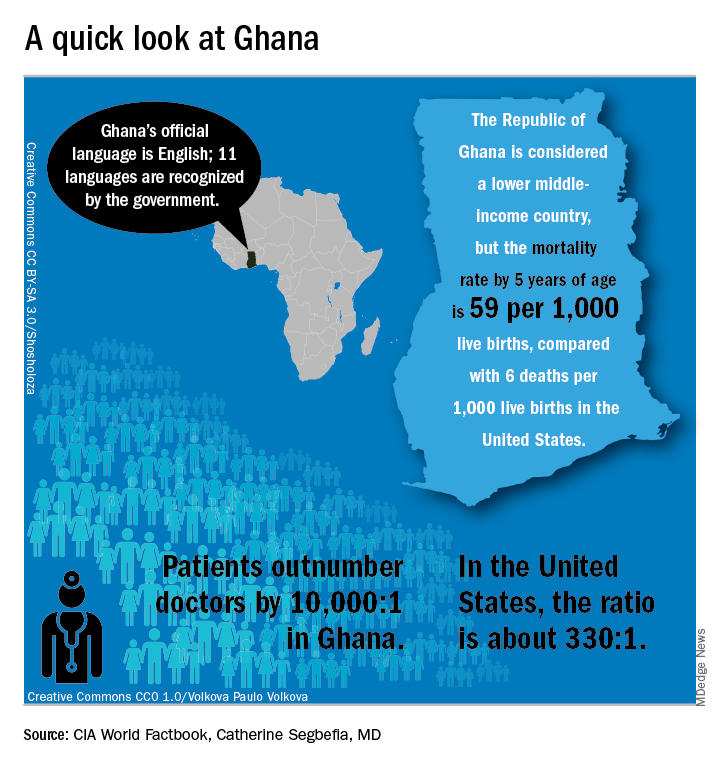
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
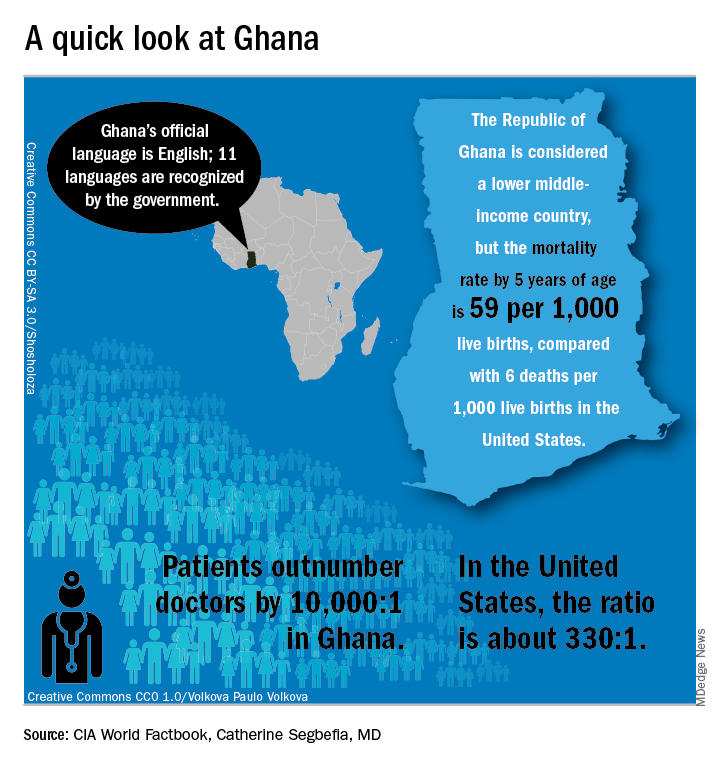
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
WASHINGTON – Sometimes, the hardest part of solving a problem is figuring out how to work around misaligned resources, and so it has been with sickle cell disease research.
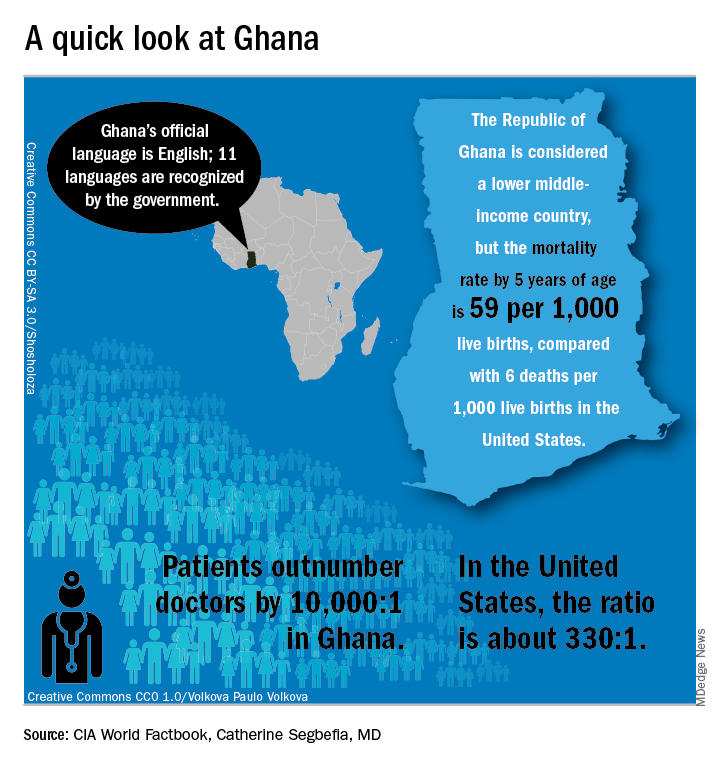
“From my point of view, what I call the geographical disparity in sickle cell disease research can be explained by the fact that the majority of affected individuals are living in the East, and the overwhelming majority of the research takes place in the West,” said Solomon Ofori-Acquah, PhD. He and three physician collaborators from Ghana shared their roadmap to conducting clinical trials in West Africa during an “East Meets West” session of the annual symposium of the Foundation for Sickle Cell Disease Research.
In Ghana, not far from where scientists now believe the hemoglobin sickling mutation originated, fully 2% of newborns have SCD; this translates into 16,000 new cases per year in a population of just 28 million, compared with the 2,000 new SCD cases seen annually in the entire United States. And access even to proven therapies can be limited; historically, little to no clinical drug development work has been conducted in this part of the world.
In the United States, half of the SCD trials that were withdrawn or terminated listed recruitment and retention of study participants as a factor in the study’s discontinuation, said Amma Owusu-Ansah, MD. “I see what we are doing as a very feasible solution to the problem of inadequate accrual to studies in the U.S.,” said Dr. Owusu-Ansah, a hematologist at the University of Pittsburgh’s Center for Translational and International Hematology (CTIH), where she serves as clinical director.
From the African perspective, hosting clinical trials – and building a robust infrastructure to do so – may help alleviate the delay in translation of disease-modifying therapies for SCD to Africa, where most people with the disease live, she said.
An existing example of resource sharing is the Human Heredity & Health in Africa (H3Africa) initiative, said Dr. Ofori-Acquah, who directs the CTIH and also holds an appointment at the University of Ghana. The project, funded by the National Institutes of Health and the Wellcome Trust, “aims to facilitate a contemporary research approach to the study of genomics and environmental determinants of common diseases with the goal of improving the health of African populations,” according to the H3Africa website. Within this framework of 40 research centers conducting genomics research and biobanking, several discrete projects aim to expand knowledge of sickle cell disease.
“All of these networks are going to study thousands of patients,” said Dr. Ofori-Acquah. “I see the H3 as a mechanism to accelerate genomics research in sickle cell disease.”
“We created a research team and built capacity for future work…. Ghana, and Africa, are capable of conducting clinical trials to global standards and producing quality data,” she said.
The story of one clinical trial is illustrative of the challenges and strengths of the multinational approach.
The phase 1b trial of a novel treatment for sickle cell disease, NVX-508, began with an initial hurdle of lack of access to emergency care at the study site, said Dr. Owusu-Ansah, a study investigator. Her first reaction, she said, was, “Well, we can’t do this, because we don’t have access to a big staff and emergency facilities.”
But after consulting with colleagues, she realized a shift in mindset was needed: “Rather than focus on what we don’t have, what do we actually have available? We have relationships we have built with institutions,” including the oldest SCD clinic in Ghana, the Ghana Institute of Clinical Genetics (GICG). This facility sits next door to a hospital with 24-hour care, Korle Bu Teaching Hospital (KBTH), a major tertiary care and referral center.
Open since 1974, the KBTH-allied GICG provides comprehensive outpatient health care to teens and adult with SCD. Currently, more than 25,000 SCD patients are registered at GICG; about half have the HbSS genotype, and another 40% have the HbSC genotype, said Yvonne Dei-Adomakoh, MD. Dr. Dei-Adomakoh of the University of Ghana is an investigator for an upcoming phase 3 trial to test voxelotor against placebo in SCD.
The GICG is working hard to become a site where clinical trials, as well as research and development, are embedded into clinic functions. In this way, not only will research be advanced for all those with SCD, but advances will be more easily incorporated into clinical care, said Dr. Dei-Adomakoh.
Dr. Owusu-Ansah noted that the facility offers a pharmacy, a laboratory, exam rooms, and information technology and medical record resources. Importantly, GICG is already staffed with physicians and allied health personnel with SCD expertise.
The University of Ghana campus is home to one of Africa’s leading biomedical research facilities, a sophisticated 11,000-square-foot laboratory that can perform testing ranging from polymerase chain reactions to DNA sequencing to genotyping and flow cytometry; it also houses a laboratory animal facility. This laboratory, the Noguchi Memorial Institute for Medical Research, also offers administrative, scientific, and research support, and houses an institutional review board.
The problem of the Noguchi laboratory site’s distance from the 24-hour support of KBTH has been solved by arranging to have an ambulance with paramedics available on site during the clinical trials.
Some other challenges the investigators discovered highlighted less-obvious infrastructure deficits; keeping a refrigerated chain of custody for biological samples, for example, can be difficult. In preparation for the trials, much basic laboratory and clinical equipment has been updated.
Conducting a U.S.-registered clinical trial in Ghana doesn’t obviate the need to meet that country’s considerable regulatory hurdles, said Dr. Owusu-Ansah. Requirements include a full regulatory submission to, and physical inspection by, Ghana’s FDA. Ghana also requires that the principal investigator must live in Ghana for the duration of the trial and that key study personnel complete Ghanaian good clinical practices training, she said.
The University of Pittsburgh is a U.S. partner in the NVX-508 study, and it was non-negotiable for that institution that a clinical trial monitor visit the African study sites. The institution’s institutional review board was sensitive to the importance of protecting vulnerable populations, and needed to hear complete plans for risk assessment, data protection, and compensation for Ghanaian study participants, Dr. Owusu-Ansah said.
But, in a turn of events typical of the ups and downs of drug development, the phase 1 trial had passed most of the administrative hurdles when in July the drug’s sponsor, NuvOx Pharma, suspended the NVX-508 trial to focus on other areas. For now, the trial registration has been withdrawn on clinicaltrials.gov and the new drug application is inactive. But Dr. Owusu-Ansah said study preparations could resume in the future, if the drug is made available to investigators.
Dr. Owusu-Ansah reported that she has received salary support from NuvOx Pharma. Dr. Segbefia reported that she has received support from Daiichi-Sankyo and Eli Lilly and Company.
EXPERT ANALYSIS FROM FSCDR 2018
Treatments, disease affect spermatogonia in boys
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.