User login
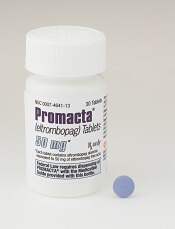
FDA expands approved use of ferumoxytol injection
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
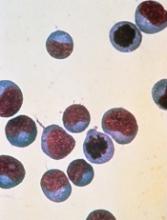
Children with sickle cell anemia fall short on antibiotic adherence
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
FROM PEDIATRICS
Key clinical point:
Major finding: A total of 18% of children with sickle cell anemia in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas received 300 days or more of prophylactic antibiotics.
Study details: A review of 2,821 children aged 3 months to 5 years with sickle cell anemia.
Disclosures: The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
Source: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Iron deficiency anemia: Disease heterogeneity and the rapid evolution of traditional diagnosis and treatment paradigms

Release Date: February 1, 2018
Expiration Date: January 31, 2019
Note: This activity is no longer available for credit
Agenda
Classification and Causes of Iron Deficiency and Iron Deficiency Anemia (duration 14:30)
Maureen M. Achebe, MD, MPH
Clinical Director, Non-Malignant Hematology Clinic
Dana-Farber Cancer Institute
Assistant Professor of Medicine
Harvard Medical School
Boston, MA
Diagnostic Approaches to Iron Deficiency Anemia:
Conventional Tests or Newer Assessments? (duration 13:00)
Thomas DeLoughery, MD, MACP
Professor of Medicine
OHSU School of Medicine
Portland, OR
Treatment: From Oral Iron Supplementation to Intravenous Therapy
(duration 21:00)
Michael Auerbach, MD, FACP
Clinical Professor of Medicine
Georgetown University School of Medicine
Washington, DC
Provided by:

Original activity supported by an educational grant from: Luitpold Pharmaceuticals, Inc.
Learning Objectives
After completing the activity, clinicians will be better able to:
- Describe iron metabolism and the mechanism of iron deficiency and iron deficiency anemia
- Differentiate the causes of iron deficiency and iron deficiency anemia and confounding factors
- Evaluate the different approaches to diagnose iron deficiency and iron deficiency anemia
- Discuss the indications for intravenous iron therapy, the various formulations, and the benefits and risk of each
Target Audience
Hematologists, oncologists, and allied healthcare professionals who manage patients with iron deficiency anemia
Statement of Need
Iron deficiency (ID) and iron deficiency anemia (IDA) are common conditions worldwide, with 1.6 billion people in both developing and developed countries affected by these conditions, which can have serious consequences. Clinicians can readily diagnose ID and IDA in a healthy individual with a single cause of anemia. However, “explosive knowledge” of iron metabolism over the last 20 years has made it increasingly more difficult for them to determine the correct diagnosis and treatment [Camaschella, Blood Rev 2017]. This leaves clinicians uncertain as to the appropriate tests to order, how to interpret the results, what treatment to use, and at what dose. This activity is designed to clarify these issues and help the healthcare team provide optimal care for patients.
Disclosures
Maureen Achebe, MD (Presenter)
Consulting fees: Luitpold Pharmaceuticals, Inc., AMAG Pharmaceuticals, Inc., Syros Pharmaceuticals, Inc.
Michael Auerbach, MD (Course Director and Presenter)
Consulting fee: AMAG Pharmaceuticals, Inc., American Regent Luitpold, Pharmacosmos
Contracted research (Data management only): AMAG Pharmaceuticals, Pharmacosmos
Thomas DeLoughery, MD (Presenter)
No relevant financial relationships with a commercial interest.
Permissions
Maureen Achebe presentation
- Slide 14: Functional Iron Deficiency
Republished with permission of the American Society of Hematology, from Bruganara C, et al. Red blood cell regeneration induced by subcutaneous recombinant erythropoietin: iron-deficient erythropoiesis in iron-replete subjects. Blood 1993; 81(4):956-64; permission conveyed through Copyright Clearance Center, Inc.
- Slide 22: Prevalence of Anemia by Cr and GFR in a Pre-dialysis Population
McClellan W, et al. The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 2004;20(9):1501-10, reprinted by permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com)
Michael Auerbach presentation
- Slide 9: Once vs Twice Daily Dosing
Reprinted from Lancet Haematol, Vol 4, No 11, Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials, e524-e533, © 2017, with permission from Elsevier.
- Slide 22: Iron Deficiency in Infancy Alters Neural Correlates of Recognition Memory at 10 Years: Key Study Results
Reprinted from J Pediatr, Vol 160, Congdon EL, Westerlund A, Algarin CR, et al. Iron deficiency in infancy is associated with altered neural correlates of recognition memory at 10 years, pp 1027-1033, © 2012, with permission from Elsevier.
Thomas DeLoughery presentation
- Slide 12: [No title]
From N Engl J Med, Lipschitz DA, Cook, JD, Finch CA, A clinical evaluation of serum ferritin as an index of iron stores, Vol 290, pages 1213-1216, © 1974 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
- Slide 15: Most Women Have Low Iron Stores
Reproduced with permission from JAMA, 1967, 199(12):897-900. Copyright© 1967 American Medical Association. All rights reserved
- Slide 16: Age and Ferritin
Reprinted from Am Heart J, Vol 140, Zacharski LR, Ornstein, DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data, pp 98-104, © 2000, with permission from Elsevier.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.

Release Date: February 1, 2018
Expiration Date: January 31, 2019
Note: This activity is no longer available for credit
Agenda
Classification and Causes of Iron Deficiency and Iron Deficiency Anemia (duration 14:30)
Maureen M. Achebe, MD, MPH
Clinical Director, Non-Malignant Hematology Clinic
Dana-Farber Cancer Institute
Assistant Professor of Medicine
Harvard Medical School
Boston, MA
Diagnostic Approaches to Iron Deficiency Anemia:
Conventional Tests or Newer Assessments? (duration 13:00)
Thomas DeLoughery, MD, MACP
Professor of Medicine
OHSU School of Medicine
Portland, OR
Treatment: From Oral Iron Supplementation to Intravenous Therapy
(duration 21:00)
Michael Auerbach, MD, FACP
Clinical Professor of Medicine
Georgetown University School of Medicine
Washington, DC
Provided by:

Original activity supported by an educational grant from: Luitpold Pharmaceuticals, Inc.
Learning Objectives
After completing the activity, clinicians will be better able to:
- Describe iron metabolism and the mechanism of iron deficiency and iron deficiency anemia
- Differentiate the causes of iron deficiency and iron deficiency anemia and confounding factors
- Evaluate the different approaches to diagnose iron deficiency and iron deficiency anemia
- Discuss the indications for intravenous iron therapy, the various formulations, and the benefits and risk of each
Target Audience
Hematologists, oncologists, and allied healthcare professionals who manage patients with iron deficiency anemia
Statement of Need
Iron deficiency (ID) and iron deficiency anemia (IDA) are common conditions worldwide, with 1.6 billion people in both developing and developed countries affected by these conditions, which can have serious consequences. Clinicians can readily diagnose ID and IDA in a healthy individual with a single cause of anemia. However, “explosive knowledge” of iron metabolism over the last 20 years has made it increasingly more difficult for them to determine the correct diagnosis and treatment [Camaschella, Blood Rev 2017]. This leaves clinicians uncertain as to the appropriate tests to order, how to interpret the results, what treatment to use, and at what dose. This activity is designed to clarify these issues and help the healthcare team provide optimal care for patients.
Disclosures
Maureen Achebe, MD (Presenter)
Consulting fees: Luitpold Pharmaceuticals, Inc., AMAG Pharmaceuticals, Inc., Syros Pharmaceuticals, Inc.
Michael Auerbach, MD (Course Director and Presenter)
Consulting fee: AMAG Pharmaceuticals, Inc., American Regent Luitpold, Pharmacosmos
Contracted research (Data management only): AMAG Pharmaceuticals, Pharmacosmos
Thomas DeLoughery, MD (Presenter)
No relevant financial relationships with a commercial interest.
Permissions
Maureen Achebe presentation
- Slide 14: Functional Iron Deficiency
Republished with permission of the American Society of Hematology, from Bruganara C, et al. Red blood cell regeneration induced by subcutaneous recombinant erythropoietin: iron-deficient erythropoiesis in iron-replete subjects. Blood 1993; 81(4):956-64; permission conveyed through Copyright Clearance Center, Inc.
- Slide 22: Prevalence of Anemia by Cr and GFR in a Pre-dialysis Population
McClellan W, et al. The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 2004;20(9):1501-10, reprinted by permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com)
Michael Auerbach presentation
- Slide 9: Once vs Twice Daily Dosing
Reprinted from Lancet Haematol, Vol 4, No 11, Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials, e524-e533, © 2017, with permission from Elsevier.
- Slide 22: Iron Deficiency in Infancy Alters Neural Correlates of Recognition Memory at 10 Years: Key Study Results
Reprinted from J Pediatr, Vol 160, Congdon EL, Westerlund A, Algarin CR, et al. Iron deficiency in infancy is associated with altered neural correlates of recognition memory at 10 years, pp 1027-1033, © 2012, with permission from Elsevier.
Thomas DeLoughery presentation
- Slide 12: [No title]
From N Engl J Med, Lipschitz DA, Cook, JD, Finch CA, A clinical evaluation of serum ferritin as an index of iron stores, Vol 290, pages 1213-1216, © 1974 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
- Slide 15: Most Women Have Low Iron Stores
Reproduced with permission from JAMA, 1967, 199(12):897-900. Copyright© 1967 American Medical Association. All rights reserved
- Slide 16: Age and Ferritin
Reprinted from Am Heart J, Vol 140, Zacharski LR, Ornstein, DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data, pp 98-104, © 2000, with permission from Elsevier.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.

Release Date: February 1, 2018
Expiration Date: January 31, 2019
Note: This activity is no longer available for credit
Agenda
Classification and Causes of Iron Deficiency and Iron Deficiency Anemia (duration 14:30)
Maureen M. Achebe, MD, MPH
Clinical Director, Non-Malignant Hematology Clinic
Dana-Farber Cancer Institute
Assistant Professor of Medicine
Harvard Medical School
Boston, MA
Diagnostic Approaches to Iron Deficiency Anemia:
Conventional Tests or Newer Assessments? (duration 13:00)
Thomas DeLoughery, MD, MACP
Professor of Medicine
OHSU School of Medicine
Portland, OR
Treatment: From Oral Iron Supplementation to Intravenous Therapy
(duration 21:00)
Michael Auerbach, MD, FACP
Clinical Professor of Medicine
Georgetown University School of Medicine
Washington, DC
Provided by:

Original activity supported by an educational grant from: Luitpold Pharmaceuticals, Inc.
Learning Objectives
After completing the activity, clinicians will be better able to:
- Describe iron metabolism and the mechanism of iron deficiency and iron deficiency anemia
- Differentiate the causes of iron deficiency and iron deficiency anemia and confounding factors
- Evaluate the different approaches to diagnose iron deficiency and iron deficiency anemia
- Discuss the indications for intravenous iron therapy, the various formulations, and the benefits and risk of each
Target Audience
Hematologists, oncologists, and allied healthcare professionals who manage patients with iron deficiency anemia
Statement of Need
Iron deficiency (ID) and iron deficiency anemia (IDA) are common conditions worldwide, with 1.6 billion people in both developing and developed countries affected by these conditions, which can have serious consequences. Clinicians can readily diagnose ID and IDA in a healthy individual with a single cause of anemia. However, “explosive knowledge” of iron metabolism over the last 20 years has made it increasingly more difficult for them to determine the correct diagnosis and treatment [Camaschella, Blood Rev 2017]. This leaves clinicians uncertain as to the appropriate tests to order, how to interpret the results, what treatment to use, and at what dose. This activity is designed to clarify these issues and help the healthcare team provide optimal care for patients.
Disclosures
Maureen Achebe, MD (Presenter)
Consulting fees: Luitpold Pharmaceuticals, Inc., AMAG Pharmaceuticals, Inc., Syros Pharmaceuticals, Inc.
Michael Auerbach, MD (Course Director and Presenter)
Consulting fee: AMAG Pharmaceuticals, Inc., American Regent Luitpold, Pharmacosmos
Contracted research (Data management only): AMAG Pharmaceuticals, Pharmacosmos
Thomas DeLoughery, MD (Presenter)
No relevant financial relationships with a commercial interest.
Permissions
Maureen Achebe presentation
- Slide 14: Functional Iron Deficiency
Republished with permission of the American Society of Hematology, from Bruganara C, et al. Red blood cell regeneration induced by subcutaneous recombinant erythropoietin: iron-deficient erythropoiesis in iron-replete subjects. Blood 1993; 81(4):956-64; permission conveyed through Copyright Clearance Center, Inc.
- Slide 22: Prevalence of Anemia by Cr and GFR in a Pre-dialysis Population
McClellan W, et al. The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 2004;20(9):1501-10, reprinted by permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com)
Michael Auerbach presentation
- Slide 9: Once vs Twice Daily Dosing
Reprinted from Lancet Haematol, Vol 4, No 11, Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials, e524-e533, © 2017, with permission from Elsevier.
- Slide 22: Iron Deficiency in Infancy Alters Neural Correlates of Recognition Memory at 10 Years: Key Study Results
Reprinted from J Pediatr, Vol 160, Congdon EL, Westerlund A, Algarin CR, et al. Iron deficiency in infancy is associated with altered neural correlates of recognition memory at 10 years, pp 1027-1033, © 2012, with permission from Elsevier.
Thomas DeLoughery presentation
- Slide 12: [No title]
From N Engl J Med, Lipschitz DA, Cook, JD, Finch CA, A clinical evaluation of serum ferritin as an index of iron stores, Vol 290, pages 1213-1216, © 1974 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
- Slide 15: Most Women Have Low Iron Stores
Reproduced with permission from JAMA, 1967, 199(12):897-900. Copyright© 1967 American Medical Association. All rights reserved
- Slide 16: Age and Ferritin
Reprinted from Am Heart J, Vol 140, Zacharski LR, Ornstein, DL, Woloshin S, et al. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data, pp 98-104, © 2000, with permission from Elsevier.
Disclaimer
The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Hemedicus, the supporter, or Frontline Medical Communications. This material is prepared based upon a review of multiple sources of information, but it is not exhaustive of the subject matter. Therefore, healthcare professionals and other individuals should review and consider other publications and materials on the subject matter before relying solely upon the information contained within this educational activity.
FDA places T-cell therapy on clinical hold
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501. ![]()
* Data in the abstract were updated in the oral presentation and reported on the company’s website.
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501. ![]()
* Data in the abstract were updated in the oral presentation and reported on the company’s website.
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501. ![]()
* Data in the abstract were updated in the oral presentation and reported on the company’s website.
Sotatercept promising for treatment of anemia in MDS
A novel agent holds promise as a treatment option for anemia in patients with lower-risk myelodysplastic syndromes who are not helped by erythropoiesis-stimulating agents (ESAs), according to results from a phase 2 trial.
Sotatercept (ACE-011) is a first-in-class novel recombinant fusion protein, and was found to be effective and well tolerated, increasing hemoglobin concentrations and decreasing the transfusion burden in this patient population.
Nearly half (29, 47%) of 62 patients with a high transfusion burden achieved hematologic improvement–erythroid (HI-E), which for them was a reduction in red blood cell transfusion from baseline of 4 U or more for at least 56 days. Additionally, 7 of 12 patients (58%) with a low transfusion burden also achieved HI-E, defined as an increase in hemoglobin of 1.5 g/dL or more that was sustained for at least 56 days without a transfusion.
“Taken together, these findings provide proof of principle that the recombinant protein sotatercept can restore ineffective erythropoiesis in patients with lower-risk myelodysplastic syndromes, with an acceptable safety profile,” Rami Komrokji, MD, of Moffitt Cancer Center and Research Institute, Tampa, and his colleagues, wrote in the Lancet Haematology.
There are few effective treatment options available for patients with lower-risk myelodysplastic syndromes who have anemia, especially after they fail primary or secondary treatment with ESAs, or for those who are not likely to benefit from ESA therapy.
In this phase 2 trial, the researchers sought to establish a safe and effective dose of sotatercept in a cohort of 74 patients. Of this group, 7 received 0.1 mg/kg sotatercept, 6 got 0.3 mg/kg, 21 received 0.5 mg/kg, 35 got 1.0 mg/kg, and 5 patients received doses up to 2.0 mg/kg. The primary efficacy endpoint of the study was the proportion of patients who achieved HI-E.
All of the patients were pretreated, having received prior therapy for myelodysplastic syndromes, including ESAs, hypomethylating agents (azacitidine or decitabine), lenalidomide, and other agents including corticosteroids and immunomodulators.
Within this cohort, 36 patients (49%; 95% confidence intervaI, 38-60) achieved HI-E while 20 patients (27%; 95% CI, 18-38) achieved independence from transfusion for at least 56 days.
Fatigue (26%) and peripheral edema (24%) were the most common adverse events reported, while grade 3-4 treatment-emergent adverse events (TEAEs) were reported in 34% of patients. Of these, 4 patients had grade 3-4 TEAEs that were probably related to the treatment. The most common grade 3-4 TEAEs were lipase increase and anemia, and each was reported in three patients. Additionally, 17 patients (23%) experienced at least one serious TEAE, including a death from a treatment-emergent subdural hematoma (which caused the patient to fall).
The study was funded by the Celgene. Dr. Komrokji reported financial relationships with Celgene and Novartis. Other study authors reported relationships with various pharmaceutical companies.
SOURCE: Komrokji R et al. Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026(18)30002-4.
Sotatercept appears to have promise in treating anemia in patients with lower-risk myelodysplastic syndromes, and has also demonstrated an acceptable safety profile, according to Valeria Santini, MD.
“Ameliorating anemia in myelodysplastic syndromes by reversing ineffective erythropoiesis secondary to aberrant TGF [transforming growth factor]-beta stimulation is indeed an interesting new therapeutic avenue for these patients,” she wrote.
Dr. Santini also pointed out that the “most intriguing aspect of sotatercept” is its unique mechanism of action. The current study demonstrated the agent’s erythroid-stimulating and antiosteoporotic activity, which should encourage continuing research into the mutifaceted and extremely complex TGF-beta pathway.
While important results were demonstrated in this study, several questions remain, Dr. Santini noted. For example, what are the clinical characteristics of the patients who were sensitive to and responded to treatment with sotatercept? Are these patients different from those who responded to a different agent, luspatercept?
Dr. Santini is with department of hematology at the University of Florence (Italy). She reported giving lectures in supported symposia for Celgene, Janssen, and Novartis and serving on the advisory boards for Abbvie, Otsuka, and Janssen. Her remarks were adapted from an accompanying editorial (Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026[18]30003-6).
Sotatercept appears to have promise in treating anemia in patients with lower-risk myelodysplastic syndromes, and has also demonstrated an acceptable safety profile, according to Valeria Santini, MD.
“Ameliorating anemia in myelodysplastic syndromes by reversing ineffective erythropoiesis secondary to aberrant TGF [transforming growth factor]-beta stimulation is indeed an interesting new therapeutic avenue for these patients,” she wrote.
Dr. Santini also pointed out that the “most intriguing aspect of sotatercept” is its unique mechanism of action. The current study demonstrated the agent’s erythroid-stimulating and antiosteoporotic activity, which should encourage continuing research into the mutifaceted and extremely complex TGF-beta pathway.
While important results were demonstrated in this study, several questions remain, Dr. Santini noted. For example, what are the clinical characteristics of the patients who were sensitive to and responded to treatment with sotatercept? Are these patients different from those who responded to a different agent, luspatercept?
Dr. Santini is with department of hematology at the University of Florence (Italy). She reported giving lectures in supported symposia for Celgene, Janssen, and Novartis and serving on the advisory boards for Abbvie, Otsuka, and Janssen. Her remarks were adapted from an accompanying editorial (Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026[18]30003-6).
Sotatercept appears to have promise in treating anemia in patients with lower-risk myelodysplastic syndromes, and has also demonstrated an acceptable safety profile, according to Valeria Santini, MD.
“Ameliorating anemia in myelodysplastic syndromes by reversing ineffective erythropoiesis secondary to aberrant TGF [transforming growth factor]-beta stimulation is indeed an interesting new therapeutic avenue for these patients,” she wrote.
Dr. Santini also pointed out that the “most intriguing aspect of sotatercept” is its unique mechanism of action. The current study demonstrated the agent’s erythroid-stimulating and antiosteoporotic activity, which should encourage continuing research into the mutifaceted and extremely complex TGF-beta pathway.
While important results were demonstrated in this study, several questions remain, Dr. Santini noted. For example, what are the clinical characteristics of the patients who were sensitive to and responded to treatment with sotatercept? Are these patients different from those who responded to a different agent, luspatercept?
Dr. Santini is with department of hematology at the University of Florence (Italy). She reported giving lectures in supported symposia for Celgene, Janssen, and Novartis and serving on the advisory boards for Abbvie, Otsuka, and Janssen. Her remarks were adapted from an accompanying editorial (Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026[18]30003-6).
A novel agent holds promise as a treatment option for anemia in patients with lower-risk myelodysplastic syndromes who are not helped by erythropoiesis-stimulating agents (ESAs), according to results from a phase 2 trial.
Sotatercept (ACE-011) is a first-in-class novel recombinant fusion protein, and was found to be effective and well tolerated, increasing hemoglobin concentrations and decreasing the transfusion burden in this patient population.
Nearly half (29, 47%) of 62 patients with a high transfusion burden achieved hematologic improvement–erythroid (HI-E), which for them was a reduction in red blood cell transfusion from baseline of 4 U or more for at least 56 days. Additionally, 7 of 12 patients (58%) with a low transfusion burden also achieved HI-E, defined as an increase in hemoglobin of 1.5 g/dL or more that was sustained for at least 56 days without a transfusion.
“Taken together, these findings provide proof of principle that the recombinant protein sotatercept can restore ineffective erythropoiesis in patients with lower-risk myelodysplastic syndromes, with an acceptable safety profile,” Rami Komrokji, MD, of Moffitt Cancer Center and Research Institute, Tampa, and his colleagues, wrote in the Lancet Haematology.
There are few effective treatment options available for patients with lower-risk myelodysplastic syndromes who have anemia, especially after they fail primary or secondary treatment with ESAs, or for those who are not likely to benefit from ESA therapy.
In this phase 2 trial, the researchers sought to establish a safe and effective dose of sotatercept in a cohort of 74 patients. Of this group, 7 received 0.1 mg/kg sotatercept, 6 got 0.3 mg/kg, 21 received 0.5 mg/kg, 35 got 1.0 mg/kg, and 5 patients received doses up to 2.0 mg/kg. The primary efficacy endpoint of the study was the proportion of patients who achieved HI-E.
All of the patients were pretreated, having received prior therapy for myelodysplastic syndromes, including ESAs, hypomethylating agents (azacitidine or decitabine), lenalidomide, and other agents including corticosteroids and immunomodulators.
Within this cohort, 36 patients (49%; 95% confidence intervaI, 38-60) achieved HI-E while 20 patients (27%; 95% CI, 18-38) achieved independence from transfusion for at least 56 days.
Fatigue (26%) and peripheral edema (24%) were the most common adverse events reported, while grade 3-4 treatment-emergent adverse events (TEAEs) were reported in 34% of patients. Of these, 4 patients had grade 3-4 TEAEs that were probably related to the treatment. The most common grade 3-4 TEAEs were lipase increase and anemia, and each was reported in three patients. Additionally, 17 patients (23%) experienced at least one serious TEAE, including a death from a treatment-emergent subdural hematoma (which caused the patient to fall).
The study was funded by the Celgene. Dr. Komrokji reported financial relationships with Celgene and Novartis. Other study authors reported relationships with various pharmaceutical companies.
SOURCE: Komrokji R et al. Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026(18)30002-4.
A novel agent holds promise as a treatment option for anemia in patients with lower-risk myelodysplastic syndromes who are not helped by erythropoiesis-stimulating agents (ESAs), according to results from a phase 2 trial.
Sotatercept (ACE-011) is a first-in-class novel recombinant fusion protein, and was found to be effective and well tolerated, increasing hemoglobin concentrations and decreasing the transfusion burden in this patient population.
Nearly half (29, 47%) of 62 patients with a high transfusion burden achieved hematologic improvement–erythroid (HI-E), which for them was a reduction in red blood cell transfusion from baseline of 4 U or more for at least 56 days. Additionally, 7 of 12 patients (58%) with a low transfusion burden also achieved HI-E, defined as an increase in hemoglobin of 1.5 g/dL or more that was sustained for at least 56 days without a transfusion.
“Taken together, these findings provide proof of principle that the recombinant protein sotatercept can restore ineffective erythropoiesis in patients with lower-risk myelodysplastic syndromes, with an acceptable safety profile,” Rami Komrokji, MD, of Moffitt Cancer Center and Research Institute, Tampa, and his colleagues, wrote in the Lancet Haematology.
There are few effective treatment options available for patients with lower-risk myelodysplastic syndromes who have anemia, especially after they fail primary or secondary treatment with ESAs, or for those who are not likely to benefit from ESA therapy.
In this phase 2 trial, the researchers sought to establish a safe and effective dose of sotatercept in a cohort of 74 patients. Of this group, 7 received 0.1 mg/kg sotatercept, 6 got 0.3 mg/kg, 21 received 0.5 mg/kg, 35 got 1.0 mg/kg, and 5 patients received doses up to 2.0 mg/kg. The primary efficacy endpoint of the study was the proportion of patients who achieved HI-E.
All of the patients were pretreated, having received prior therapy for myelodysplastic syndromes, including ESAs, hypomethylating agents (azacitidine or decitabine), lenalidomide, and other agents including corticosteroids and immunomodulators.
Within this cohort, 36 patients (49%; 95% confidence intervaI, 38-60) achieved HI-E while 20 patients (27%; 95% CI, 18-38) achieved independence from transfusion for at least 56 days.
Fatigue (26%) and peripheral edema (24%) were the most common adverse events reported, while grade 3-4 treatment-emergent adverse events (TEAEs) were reported in 34% of patients. Of these, 4 patients had grade 3-4 TEAEs that were probably related to the treatment. The most common grade 3-4 TEAEs were lipase increase and anemia, and each was reported in three patients. Additionally, 17 patients (23%) experienced at least one serious TEAE, including a death from a treatment-emergent subdural hematoma (which caused the patient to fall).
The study was funded by the Celgene. Dr. Komrokji reported financial relationships with Celgene and Novartis. Other study authors reported relationships with various pharmaceutical companies.
SOURCE: Komrokji R et al. Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026(18)30002-4.
FROM LANCET HAEMATOLOGY
Key clinical point:
Major finding: In all, 36 patients (49%) achieved hematologic improvement–erythroid and 20 patients (27%) achieved independence from transfusion for at least 56 days.
Data source: A phase 2 trial that included 74 patients with lower-risk myelodysplastic syndromes who did not respond to erythropoiesis-stimulating agents.
Disclosures: Celgene funded the study. Dr. Komrokji reported financial relationships with Celgene and Novartis. Other study authors reported relationships with various pharmaceutical companies.
Source: Komrokji R et al. Lancet Haematol. 2018 Jan 10. doi: 10.1016/S2352-3026(18)30002-4.
Predicting response to AZA in MDS, CMML
Researchers have developed a technique that may help predict whether patients with myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) will respond to treatment with azacytidine (AZA).
“The new method, called AZA-MS, utilizes a cutting-edge technique known as mass spectrometry to measure the different forms of AZA inside blood cells of patients—such as the AZA molecules that are incorporated into the DNA or RNA,” said Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
With this method, Dr Unnikrishnan and his colleagues found that patients who do not respond to AZA may incorporate fewer AZA molecules in their DNA and have lower DNA demethylation than responders. However, this is not always the case.
The researchers reported these findings in Leukemia.
The team initially tested AZA-MS in AZA-treated RKO cells and found that AZA-MS could quantify the ribonucleoside (5-AZA-cR) and deoxyribonucleoside (5-AZA-CdR) forms of AZA in RNA, DNA, and the cytoplasm—all in the same sample.
The researchers also found that AZA induced dose-dependent DNA demethylation but did not have an effect on RNA methylation.
The team then used AZA-MS to analyze bone marrow samples from patients with MDS (n=4) or CMML (n=4) who were undergoing treatment with AZA. All of the patients had received at least 6 cycles of the drug.
Each patient had 3 bone marrow samples collected—one immediately before starting treatment; one on day 8 of cycle 1 (C1d8); and one on day 28 of cycle 1 (C1d28), when they had spent 20 days off the drug.
Four of the patients were complete responders, and 4 were nonresponders. In each group, 2 patients had MDS, and 2 had CMML.
At C1d8, DNA-5-AZA-CdR was significantly greater in responders than nonresponders. And, overall, responders had increased DNA demethylation compared to nonresponders.
However, the researchers also observed differences among the nonresponders. Two nonresponders had very low levels of DNA-5-AZA-CdR at C1d8 and no demethylation. The other 2 nonresponders had much higher DNA-5-AZA-CdR and DNA demethylation levels, which were comparable to levels in responders.
The researchers said they could detect AZA and DNA-5-AZA-CdR intracellularly, as well as RNA-AZA, in the nonresponders with minimal DNA-5-AZA-CdR and DNA demethylation.
The team said this suggests that neither cellular uptake nor intracellular metabolism explain the low DNA-5-AZA-CdR in these patients. Instead, the researchers believe these patients may have a greater proportion of bone marrow cells that are quiescent and not undergoing DNA replication.
The researchers also believe the nonresponders with higher DNA-5-AZA-CdR may be explained by a failure to induce an interferon response, which is necessary for a clinical response.
On the other hand, these nonresponders could have defective immune cell-mediated clearance of dysplastic cells or increased tolerance to this clearance, the researchers said.
The team also noted that, at C1d28, DNA-5-AZA-CdR levels dropped (but were still detectable) in all 8 patients, and DNA methylation had nearly returned to pretreatment levels in all patients. ![]()
Researchers have developed a technique that may help predict whether patients with myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) will respond to treatment with azacytidine (AZA).
“The new method, called AZA-MS, utilizes a cutting-edge technique known as mass spectrometry to measure the different forms of AZA inside blood cells of patients—such as the AZA molecules that are incorporated into the DNA or RNA,” said Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
With this method, Dr Unnikrishnan and his colleagues found that patients who do not respond to AZA may incorporate fewer AZA molecules in their DNA and have lower DNA demethylation than responders. However, this is not always the case.
The researchers reported these findings in Leukemia.
The team initially tested AZA-MS in AZA-treated RKO cells and found that AZA-MS could quantify the ribonucleoside (5-AZA-cR) and deoxyribonucleoside (5-AZA-CdR) forms of AZA in RNA, DNA, and the cytoplasm—all in the same sample.
The researchers also found that AZA induced dose-dependent DNA demethylation but did not have an effect on RNA methylation.
The team then used AZA-MS to analyze bone marrow samples from patients with MDS (n=4) or CMML (n=4) who were undergoing treatment with AZA. All of the patients had received at least 6 cycles of the drug.
Each patient had 3 bone marrow samples collected—one immediately before starting treatment; one on day 8 of cycle 1 (C1d8); and one on day 28 of cycle 1 (C1d28), when they had spent 20 days off the drug.
Four of the patients were complete responders, and 4 were nonresponders. In each group, 2 patients had MDS, and 2 had CMML.
At C1d8, DNA-5-AZA-CdR was significantly greater in responders than nonresponders. And, overall, responders had increased DNA demethylation compared to nonresponders.
However, the researchers also observed differences among the nonresponders. Two nonresponders had very low levels of DNA-5-AZA-CdR at C1d8 and no demethylation. The other 2 nonresponders had much higher DNA-5-AZA-CdR and DNA demethylation levels, which were comparable to levels in responders.
The researchers said they could detect AZA and DNA-5-AZA-CdR intracellularly, as well as RNA-AZA, in the nonresponders with minimal DNA-5-AZA-CdR and DNA demethylation.
The team said this suggests that neither cellular uptake nor intracellular metabolism explain the low DNA-5-AZA-CdR in these patients. Instead, the researchers believe these patients may have a greater proportion of bone marrow cells that are quiescent and not undergoing DNA replication.
The researchers also believe the nonresponders with higher DNA-5-AZA-CdR may be explained by a failure to induce an interferon response, which is necessary for a clinical response.
On the other hand, these nonresponders could have defective immune cell-mediated clearance of dysplastic cells or increased tolerance to this clearance, the researchers said.
The team also noted that, at C1d28, DNA-5-AZA-CdR levels dropped (but were still detectable) in all 8 patients, and DNA methylation had nearly returned to pretreatment levels in all patients. ![]()
Researchers have developed a technique that may help predict whether patients with myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) will respond to treatment with azacytidine (AZA).
“The new method, called AZA-MS, utilizes a cutting-edge technique known as mass spectrometry to measure the different forms of AZA inside blood cells of patients—such as the AZA molecules that are incorporated into the DNA or RNA,” said Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
With this method, Dr Unnikrishnan and his colleagues found that patients who do not respond to AZA may incorporate fewer AZA molecules in their DNA and have lower DNA demethylation than responders. However, this is not always the case.
The researchers reported these findings in Leukemia.
The team initially tested AZA-MS in AZA-treated RKO cells and found that AZA-MS could quantify the ribonucleoside (5-AZA-cR) and deoxyribonucleoside (5-AZA-CdR) forms of AZA in RNA, DNA, and the cytoplasm—all in the same sample.
The researchers also found that AZA induced dose-dependent DNA demethylation but did not have an effect on RNA methylation.
The team then used AZA-MS to analyze bone marrow samples from patients with MDS (n=4) or CMML (n=4) who were undergoing treatment with AZA. All of the patients had received at least 6 cycles of the drug.
Each patient had 3 bone marrow samples collected—one immediately before starting treatment; one on day 8 of cycle 1 (C1d8); and one on day 28 of cycle 1 (C1d28), when they had spent 20 days off the drug.
Four of the patients were complete responders, and 4 were nonresponders. In each group, 2 patients had MDS, and 2 had CMML.
At C1d8, DNA-5-AZA-CdR was significantly greater in responders than nonresponders. And, overall, responders had increased DNA demethylation compared to nonresponders.
However, the researchers also observed differences among the nonresponders. Two nonresponders had very low levels of DNA-5-AZA-CdR at C1d8 and no demethylation. The other 2 nonresponders had much higher DNA-5-AZA-CdR and DNA demethylation levels, which were comparable to levels in responders.
The researchers said they could detect AZA and DNA-5-AZA-CdR intracellularly, as well as RNA-AZA, in the nonresponders with minimal DNA-5-AZA-CdR and DNA demethylation.
The team said this suggests that neither cellular uptake nor intracellular metabolism explain the low DNA-5-AZA-CdR in these patients. Instead, the researchers believe these patients may have a greater proportion of bone marrow cells that are quiescent and not undergoing DNA replication.
The researchers also believe the nonresponders with higher DNA-5-AZA-CdR may be explained by a failure to induce an interferon response, which is necessary for a clinical response.
On the other hand, these nonresponders could have defective immune cell-mediated clearance of dysplastic cells or increased tolerance to this clearance, the researchers said.
The team also noted that, at C1d28, DNA-5-AZA-CdR levels dropped (but were still detectable) in all 8 patients, and DNA methylation had nearly returned to pretreatment levels in all patients. ![]()
Drug receives breakthrough designation for SCD
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to voxelotor (previously GBT440) for the treatment of sickle cell disease (SCD).
Voxelotor is being developed by Global Blood Therapeutics, Inc., as a potentially disease-modifying therapy for SCD.
The drug works by increasing hemoglobin’s affinity for oxygen. Since oxygenated sickle hemoglobin does not polymerize, it is believed that voxelotor blocks polymerization and the resultant sickling of red blood cells.
If voxelotor can restore normal hemoglobin function and improve oxygen delivery, the therapy may be capable of modifying the progression of SCD.
The FDA previously granted voxelotor fast track designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s decision to grant breakthrough therapy designation to voxelotor was based on clinical data submitted from the following studies:
- Part A of the phase 3 HOPE study (GBT440-031)
- A phase 1/2 study and open-label extension in adults (GBT440-001/GBT440-024), which was presented at the 2016 ASH Annual Meeting
- The ongoing phase 2 HOPE-KIDS 1 study in children age 6 to 17 (GBT440-007), which was presented at the 2017 ASH Annual Meeting (abstract 689)
- The compassionate access experience in adults with severe SCD who were not eligible for the HOPE study, which was presented at the 2017 ASH Annual Meeting (abstract 3545).
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to voxelotor (previously GBT440) for the treatment of sickle cell disease (SCD).
Voxelotor is being developed by Global Blood Therapeutics, Inc., as a potentially disease-modifying therapy for SCD.
The drug works by increasing hemoglobin’s affinity for oxygen. Since oxygenated sickle hemoglobin does not polymerize, it is believed that voxelotor blocks polymerization and the resultant sickling of red blood cells.
If voxelotor can restore normal hemoglobin function and improve oxygen delivery, the therapy may be capable of modifying the progression of SCD.
The FDA previously granted voxelotor fast track designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s decision to grant breakthrough therapy designation to voxelotor was based on clinical data submitted from the following studies:
- Part A of the phase 3 HOPE study (GBT440-031)
- A phase 1/2 study and open-label extension in adults (GBT440-001/GBT440-024), which was presented at the 2016 ASH Annual Meeting
- The ongoing phase 2 HOPE-KIDS 1 study in children age 6 to 17 (GBT440-007), which was presented at the 2017 ASH Annual Meeting (abstract 689)
- The compassionate access experience in adults with severe SCD who were not eligible for the HOPE study, which was presented at the 2017 ASH Annual Meeting (abstract 3545).
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to voxelotor (previously GBT440) for the treatment of sickle cell disease (SCD).
Voxelotor is being developed by Global Blood Therapeutics, Inc., as a potentially disease-modifying therapy for SCD.
The drug works by increasing hemoglobin’s affinity for oxygen. Since oxygenated sickle hemoglobin does not polymerize, it is believed that voxelotor blocks polymerization and the resultant sickling of red blood cells.
If voxelotor can restore normal hemoglobin function and improve oxygen delivery, the therapy may be capable of modifying the progression of SCD.
The FDA previously granted voxelotor fast track designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s decision to grant breakthrough therapy designation to voxelotor was based on clinical data submitted from the following studies:
- Part A of the phase 3 HOPE study (GBT440-031)
- A phase 1/2 study and open-label extension in adults (GBT440-001/GBT440-024), which was presented at the 2016 ASH Annual Meeting
- The ongoing phase 2 HOPE-KIDS 1 study in children age 6 to 17 (GBT440-007), which was presented at the 2017 ASH Annual Meeting (abstract 689)
- The compassionate access experience in adults with severe SCD who were not eligible for the HOPE study, which was presented at the 2017 ASH Annual Meeting (abstract 3545).
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
Caplacizumab improves outcomes in aTTP
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
ATLANTA—Caplacizumab can improve outcomes in patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to research presented at the 2017 ASH Annual Meeting.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care (plasma exchange and immunosuppression) to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab were significantly more likely to achieve platelet normalization and significantly less likely to experience aTTP-related death, aTTP recurrence, and major thromboembolic events.
Patients in the caplacizumab arm also required plasma exchange less frequently and spent less time in the hospital and intensive care unit (ICU).
Bleeding-related adverse events (AEs) were more common among patients who received caplacizumab than those who received placebo.
Marie Scully, MD, of the University College London Hospitals in London, UK, presented these results from HERCULES as a late-breaking abstract at the ASH Annual Meeting (abstract LBA-1). HERCULES was supported by Ablynx.
Patients and treatment
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange. If patients had a recurrence during the 30-day treatment period, they could go on to receive open-label caplacizumab.
If, at the end of the 30-day treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, caplacizumab or placebo could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment. Twenty-six patients in the placebo arm and 2 patients in the caplacizumab arm received open-label caplacizumab.
“If we look at the demographics, they’re relatively comparable to any data we normally see in patients with immune-mediated TTP,” Dr Scully said.
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. Most patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
“Patients were 55% more likely to achieve normalization of their platelet count at any time in the caplacizumab group, and this was highly significant,” Dr Scully said.
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The researchers also assessed aTTP recurrence during the overall study period, which occurred in 12.7% (n=9) of patients in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
During the follow-up period, there were 6 relapses (9.1%) in the caplacizumab arm but none in the placebo arm.
“This tells us something about the pathophysiology of TTP and the role of caplacizumab,” Dr Scully said. “All of these patients, on stopping caplacizumab, had ADAMTS13 levels less than 5%. Therefore, it was important that their treatment was continued to ensure removal of antibody.”
According to the International TTP Working Group consensus definition, none of the patients in the caplacizumab arm and 7.0% (n=5) of patients in the placebo arm had refractory aTTP (P=0.018).
The mean number of days of plasma exchange during the overall treatment period was 5.8 days in the caplacizumab arm and 9.4 days in the placebo arm (a 38% relative reduction). The mean volume of plasma used was 21.3L and 35.9L, respectively (a 41% relative reduction).
The mean duration of hospital stay was 9.9 days in the caplacizumab arm and 14.4 days in the placebo arm (a 31% relative reduction).
For patients admitted to the ICU (28 in the caplacizumab arm and 27 in the placebo arm), the mean number of days in the ICU was 3.4 days in the caplacizumab arm and 9.7 days in the placebo arm (a 65% relative reduction).
Safety
“The safety profile [of caplacizumab] was comparable to previous results and in keeping with the mechanism of action,” Dr Scully said.
The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm (45.6%) than the placebo arm (23.3%).
Bleeding-related AEs (in the caplacizumab and placebo arms, respectively) included epistaxis (23.9% and 1.4%), gingival bleeding (11.3% and 0%), bruising (7.0% and 4.1%), hematuria (5.6% and 1.4%), vaginal hemorrhage (4.2% and 1.4%), menorrhagia (2.8% and 1.4%), catheter site hemorrhage (2.8% and 4.1%), injection site bruising (2.8% and 2.7%), hematochezia (2.8% and 0%), and hematoma (2.8% and 0%).
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
Drug granted breakthrough status as first-line SAA therapy
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to eltrombopag (Promacta®) for use in combination with standard immunosuppressive therapy as first-line treatment for patients with severe aplastic anemia (SAA).
Novartis plans to submit an application to the FDA for this indication later this year.
Eltrombopag is already FDA-approved to treat SAA patients who have had an insufficient response to immunosuppressive therapy.
The drug is also approved to treat patients with chronic immune thrombocytopenia who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
And eltrombopag is approved to treat thrombocytopenia in patients with chronic hepatitis C to allow for the initiation and maintenance of interferon-based therapy.
Trial data
The breakthrough designation for eltrombopag as first-line treatment in SAA is supported by data from a phase 1/2 trial, which were published in NEJM in April 2017.
The trial included 92 patients with previously untreated SAA. They received immunosuppressive therapy and eltrombopag in 3 different cohorts.
Patients in cohort 1 received eltrombopag from day 14 to 6 months. Patients in cohort 2 received the drug from day 14 to 3 months. And patients in cohort 3 received eltrombopag from day 1 to 6 months.
At 6 months, the overall response rate was 80% in cohort 1, 87% in cohort 2, and 94% in cohort 3. The rate of complete response at 6 months was 33%, 26%, and 58%, respectively.
At a median follow-up of 2 years, the overall survival rate was 97%.
Seven patients briefly stopped taking eltrombopag during the first 2 weeks due to transient elevations in liver-enzyme levels.
There were 2 severe adverse events that were related to eltrombopag and resulted in patients stopping the drug. These were a grade 2 and grade 3 cutaneous eruption.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to eltrombopag (Promacta®) for use in combination with standard immunosuppressive therapy as first-line treatment for patients with severe aplastic anemia (SAA).
Novartis plans to submit an application to the FDA for this indication later this year.
Eltrombopag is already FDA-approved to treat SAA patients who have had an insufficient response to immunosuppressive therapy.
The drug is also approved to treat patients with chronic immune thrombocytopenia who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
And eltrombopag is approved to treat thrombocytopenia in patients with chronic hepatitis C to allow for the initiation and maintenance of interferon-based therapy.
Trial data
The breakthrough designation for eltrombopag as first-line treatment in SAA is supported by data from a phase 1/2 trial, which were published in NEJM in April 2017.
The trial included 92 patients with previously untreated SAA. They received immunosuppressive therapy and eltrombopag in 3 different cohorts.
Patients in cohort 1 received eltrombopag from day 14 to 6 months. Patients in cohort 2 received the drug from day 14 to 3 months. And patients in cohort 3 received eltrombopag from day 1 to 6 months.
At 6 months, the overall response rate was 80% in cohort 1, 87% in cohort 2, and 94% in cohort 3. The rate of complete response at 6 months was 33%, 26%, and 58%, respectively.
At a median follow-up of 2 years, the overall survival rate was 97%.
Seven patients briefly stopped taking eltrombopag during the first 2 weeks due to transient elevations in liver-enzyme levels.
There were 2 severe adverse events that were related to eltrombopag and resulted in patients stopping the drug. These were a grade 2 and grade 3 cutaneous eruption.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to eltrombopag (Promacta®) for use in combination with standard immunosuppressive therapy as first-line treatment for patients with severe aplastic anemia (SAA).
Novartis plans to submit an application to the FDA for this indication later this year.
Eltrombopag is already FDA-approved to treat SAA patients who have had an insufficient response to immunosuppressive therapy.
The drug is also approved to treat patients with chronic immune thrombocytopenia who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
And eltrombopag is approved to treat thrombocytopenia in patients with chronic hepatitis C to allow for the initiation and maintenance of interferon-based therapy.
Trial data
The breakthrough designation for eltrombopag as first-line treatment in SAA is supported by data from a phase 1/2 trial, which were published in NEJM in April 2017.
The trial included 92 patients with previously untreated SAA. They received immunosuppressive therapy and eltrombopag in 3 different cohorts.
Patients in cohort 1 received eltrombopag from day 14 to 6 months. Patients in cohort 2 received the drug from day 14 to 3 months. And patients in cohort 3 received eltrombopag from day 1 to 6 months.
At 6 months, the overall response rate was 80% in cohort 1, 87% in cohort 2, and 94% in cohort 3. The rate of complete response at 6 months was 33%, 26%, and 58%, respectively.
At a median follow-up of 2 years, the overall survival rate was 97%.
Seven patients briefly stopped taking eltrombopag during the first 2 weeks due to transient elevations in liver-enzyme levels.
There were 2 severe adverse events that were related to eltrombopag and resulted in patients stopping the drug. These were a grade 2 and grade 3 cutaneous eruption.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
FDA grants breakthrough therapy designation for severe aplastic anemia drug
The Food and Drug Administration has granted breakthrough therapy designation to eltrombopag (Promacta) for use in combination with standard immunosuppressive therapy as a first-line treatment for patients with severe aplastic anemia (SAA).
Eltrombopag already is approved as a second-line therapy in patients with refractory SAA and is approved for adults and children with refractory chronic immune thrombocytopenia (ITP).
“Promacta is a promising medicine that, if approved for first-line use in severe aplastic anemia, may redefine the standard of care for patients with this rare and serious bone marrow condition,” Samit Hirawat, MD, head of Novartis Oncology Global Drug Development, said in a statement.
The Food and Drug Administration has granted breakthrough therapy designation to eltrombopag (Promacta) for use in combination with standard immunosuppressive therapy as a first-line treatment for patients with severe aplastic anemia (SAA).
Eltrombopag already is approved as a second-line therapy in patients with refractory SAA and is approved for adults and children with refractory chronic immune thrombocytopenia (ITP).
“Promacta is a promising medicine that, if approved for first-line use in severe aplastic anemia, may redefine the standard of care for patients with this rare and serious bone marrow condition,” Samit Hirawat, MD, head of Novartis Oncology Global Drug Development, said in a statement.
The Food and Drug Administration has granted breakthrough therapy designation to eltrombopag (Promacta) for use in combination with standard immunosuppressive therapy as a first-line treatment for patients with severe aplastic anemia (SAA).
Eltrombopag already is approved as a second-line therapy in patients with refractory SAA and is approved for adults and children with refractory chronic immune thrombocytopenia (ITP).
“Promacta is a promising medicine that, if approved for first-line use in severe aplastic anemia, may redefine the standard of care for patients with this rare and serious bone marrow condition,” Samit Hirawat, MD, head of Novartis Oncology Global Drug Development, said in a statement.