User login
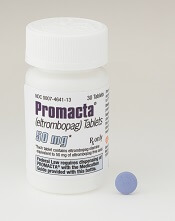
Eltrombopag can control ITP long-term, study suggests
Eltrombopag can provide long-term disease control for chronic/persistent immune thrombocytopenia (ITP), according to research published in Blood.
In the EXTEND study, investigators evaluated patients exposed to eltrombopag for a median of 2.4 years.
Most patients achieved a response to the drug, and more than half of them maintained that response for at least 25 weeks.
More than a third of patients were able to discontinue at least 1 concomitant ITP medication.
Most adverse events (AEs) were grade 1 or 2. However, 32% of patients had serious AEs, and 14% of patients withdrew from the study due to AEs.
This research was sponsored by GlaxoSmithKline, the company that previously owned eltrombopag. Now, the drug is a product of Novartis.
Patients
EXTEND is an open-label extension study of 4 trials (TRA100773A, TRA100773B, TRA102537/RAISE, and TRA108057/REPEAT), which enrolled 302 adults with chronic/persistent ITP.
Patients had completed the treatment and follow-up periods as defined in their previous study protocol and did not experience eltrombopag-related toxicity or other drug intolerance on a prior eltrombopag study. Patients who discontinued a previous study due to toxicity were only eligible if they had received a placebo.
The patients’ median time from diagnosis to enrollment in EXTEND was 58.8 months (range, 9-552). Their median age was 50 (range, 18-86), and 67% were female.
Most patients (70%) had a baseline platelet count below 30×109/L. Thirty-three percent of patients were using concomitant ITP medications, 53% had received at least 3 prior ITP treatments, and 38% had undergone splenectomy.
Treatment
Eltrombopag was started at a dose of 50 mg/day and titrated to 25-75 mg/day or less often based on platelet counts. Maintenance dosing continued after minimization of concomitant ITP medication and optimization of eltrombopag dosing.
The overall median duration of eltrombopag exposure was 2.37 years (range, 2 days to 8.76 years), and the mean average daily dose was 50.2 mg/day (range, 1-75).
One hundred and thirty-five patients (45%) completed the study, and 75 patients (25%) were treated for 4 or more years. The most common reasons for study withdrawal included AEs (n=41), patient decision (n=39), lack of efficacy (n=32), and “other” reasons (n=39).
Safety
AEs leading to study withdrawal (occurring at least twice) included hepatobiliary AEs (n=7), cataracts (n=4), deep vein thrombosis (n=3), cerebral infarction (n=2), headache (n=2), and myelofibrosis (n=2).
The overall incidence of AEs was 92%. The most frequent AEs were headache (28%), nasopharyngitis (25%), and upper respiratory tract infection (23%).
Twenty-six percent of patients had grade 3 AEs, 6% had grade 4 AEs, and 32% had serious AEs. Serious AEs included cataracts (5%), pneumonia (3%), anemia (2%), ALT increase (2%), epistaxis (1%), AST increase, (1%), bilirubin increase (1%), and deep vein thrombosis (1%).
Three percent of patients reported a malignancy while on study, including basal cell carcinoma, intramucosal adenocarcinoma, breast cancer, metastases to the lung, ovarian cancer, squamous cell carcinoma, transitional cell carcinoma, lymphoma, unclassifiable B-cell lymphoma (low grade), and Hodgkin lymphoma.
Efficacy
In all, 85.8% (259/302) of patients had a response to eltrombopag, which was defined as achieving a platelet count of at least 50×109/L at least once without rescue therapy.
Fifty-two percent (133/257) of patients achieved a continuous response lasting at least 25 weeks.
Thirty-four percent (34/101) of patients who were on concomitant ITP medication discontinued at least 1 medication. Thirty-nine percent (39/101) reduced or permanently stopped at least 1 ITP medication without receiving rescue therapy.
Fifty-seven percent of patients (171/302) had bleeding symptoms at baseline. This decreased to 16% (13/80) at 1 year.
“The EXTEND data published in Blood validate [eltrombopag] as an important oral treatment option that, by often increasing platelet counts, significantly decreased bleeding rates and reduced the need for concurrent therapies in certain patients with chronic/persistent immune thrombocytopenia,” said study author James Bussel, MD, of Weill Cornell Medicine in New York, New York.
“With this information, physicians can better optimize long-term disease management for appropriate patients living with this chronic disease.” ![]()
Eltrombopag can provide long-term disease control for chronic/persistent immune thrombocytopenia (ITP), according to research published in Blood.
In the EXTEND study, investigators evaluated patients exposed to eltrombopag for a median of 2.4 years.
Most patients achieved a response to the drug, and more than half of them maintained that response for at least 25 weeks.
More than a third of patients were able to discontinue at least 1 concomitant ITP medication.
Most adverse events (AEs) were grade 1 or 2. However, 32% of patients had serious AEs, and 14% of patients withdrew from the study due to AEs.
This research was sponsored by GlaxoSmithKline, the company that previously owned eltrombopag. Now, the drug is a product of Novartis.
Patients
EXTEND is an open-label extension study of 4 trials (TRA100773A, TRA100773B, TRA102537/RAISE, and TRA108057/REPEAT), which enrolled 302 adults with chronic/persistent ITP.
Patients had completed the treatment and follow-up periods as defined in their previous study protocol and did not experience eltrombopag-related toxicity or other drug intolerance on a prior eltrombopag study. Patients who discontinued a previous study due to toxicity were only eligible if they had received a placebo.
The patients’ median time from diagnosis to enrollment in EXTEND was 58.8 months (range, 9-552). Their median age was 50 (range, 18-86), and 67% were female.
Most patients (70%) had a baseline platelet count below 30×109/L. Thirty-three percent of patients were using concomitant ITP medications, 53% had received at least 3 prior ITP treatments, and 38% had undergone splenectomy.
Treatment
Eltrombopag was started at a dose of 50 mg/day and titrated to 25-75 mg/day or less often based on platelet counts. Maintenance dosing continued after minimization of concomitant ITP medication and optimization of eltrombopag dosing.
The overall median duration of eltrombopag exposure was 2.37 years (range, 2 days to 8.76 years), and the mean average daily dose was 50.2 mg/day (range, 1-75).
One hundred and thirty-five patients (45%) completed the study, and 75 patients (25%) were treated for 4 or more years. The most common reasons for study withdrawal included AEs (n=41), patient decision (n=39), lack of efficacy (n=32), and “other” reasons (n=39).
Safety
AEs leading to study withdrawal (occurring at least twice) included hepatobiliary AEs (n=7), cataracts (n=4), deep vein thrombosis (n=3), cerebral infarction (n=2), headache (n=2), and myelofibrosis (n=2).
The overall incidence of AEs was 92%. The most frequent AEs were headache (28%), nasopharyngitis (25%), and upper respiratory tract infection (23%).
Twenty-six percent of patients had grade 3 AEs, 6% had grade 4 AEs, and 32% had serious AEs. Serious AEs included cataracts (5%), pneumonia (3%), anemia (2%), ALT increase (2%), epistaxis (1%), AST increase, (1%), bilirubin increase (1%), and deep vein thrombosis (1%).
Three percent of patients reported a malignancy while on study, including basal cell carcinoma, intramucosal adenocarcinoma, breast cancer, metastases to the lung, ovarian cancer, squamous cell carcinoma, transitional cell carcinoma, lymphoma, unclassifiable B-cell lymphoma (low grade), and Hodgkin lymphoma.
Efficacy
In all, 85.8% (259/302) of patients had a response to eltrombopag, which was defined as achieving a platelet count of at least 50×109/L at least once without rescue therapy.
Fifty-two percent (133/257) of patients achieved a continuous response lasting at least 25 weeks.
Thirty-four percent (34/101) of patients who were on concomitant ITP medication discontinued at least 1 medication. Thirty-nine percent (39/101) reduced or permanently stopped at least 1 ITP medication without receiving rescue therapy.
Fifty-seven percent of patients (171/302) had bleeding symptoms at baseline. This decreased to 16% (13/80) at 1 year.
“The EXTEND data published in Blood validate [eltrombopag] as an important oral treatment option that, by often increasing platelet counts, significantly decreased bleeding rates and reduced the need for concurrent therapies in certain patients with chronic/persistent immune thrombocytopenia,” said study author James Bussel, MD, of Weill Cornell Medicine in New York, New York.
“With this information, physicians can better optimize long-term disease management for appropriate patients living with this chronic disease.” ![]()
Eltrombopag can provide long-term disease control for chronic/persistent immune thrombocytopenia (ITP), according to research published in Blood.
In the EXTEND study, investigators evaluated patients exposed to eltrombopag for a median of 2.4 years.
Most patients achieved a response to the drug, and more than half of them maintained that response for at least 25 weeks.
More than a third of patients were able to discontinue at least 1 concomitant ITP medication.
Most adverse events (AEs) were grade 1 or 2. However, 32% of patients had serious AEs, and 14% of patients withdrew from the study due to AEs.
This research was sponsored by GlaxoSmithKline, the company that previously owned eltrombopag. Now, the drug is a product of Novartis.
Patients
EXTEND is an open-label extension study of 4 trials (TRA100773A, TRA100773B, TRA102537/RAISE, and TRA108057/REPEAT), which enrolled 302 adults with chronic/persistent ITP.
Patients had completed the treatment and follow-up periods as defined in their previous study protocol and did not experience eltrombopag-related toxicity or other drug intolerance on a prior eltrombopag study. Patients who discontinued a previous study due to toxicity were only eligible if they had received a placebo.
The patients’ median time from diagnosis to enrollment in EXTEND was 58.8 months (range, 9-552). Their median age was 50 (range, 18-86), and 67% were female.
Most patients (70%) had a baseline platelet count below 30×109/L. Thirty-three percent of patients were using concomitant ITP medications, 53% had received at least 3 prior ITP treatments, and 38% had undergone splenectomy.
Treatment
Eltrombopag was started at a dose of 50 mg/day and titrated to 25-75 mg/day or less often based on platelet counts. Maintenance dosing continued after minimization of concomitant ITP medication and optimization of eltrombopag dosing.
The overall median duration of eltrombopag exposure was 2.37 years (range, 2 days to 8.76 years), and the mean average daily dose was 50.2 mg/day (range, 1-75).
One hundred and thirty-five patients (45%) completed the study, and 75 patients (25%) were treated for 4 or more years. The most common reasons for study withdrawal included AEs (n=41), patient decision (n=39), lack of efficacy (n=32), and “other” reasons (n=39).
Safety
AEs leading to study withdrawal (occurring at least twice) included hepatobiliary AEs (n=7), cataracts (n=4), deep vein thrombosis (n=3), cerebral infarction (n=2), headache (n=2), and myelofibrosis (n=2).
The overall incidence of AEs was 92%. The most frequent AEs were headache (28%), nasopharyngitis (25%), and upper respiratory tract infection (23%).
Twenty-six percent of patients had grade 3 AEs, 6% had grade 4 AEs, and 32% had serious AEs. Serious AEs included cataracts (5%), pneumonia (3%), anemia (2%), ALT increase (2%), epistaxis (1%), AST increase, (1%), bilirubin increase (1%), and deep vein thrombosis (1%).
Three percent of patients reported a malignancy while on study, including basal cell carcinoma, intramucosal adenocarcinoma, breast cancer, metastases to the lung, ovarian cancer, squamous cell carcinoma, transitional cell carcinoma, lymphoma, unclassifiable B-cell lymphoma (low grade), and Hodgkin lymphoma.
Efficacy
In all, 85.8% (259/302) of patients had a response to eltrombopag, which was defined as achieving a platelet count of at least 50×109/L at least once without rescue therapy.
Fifty-two percent (133/257) of patients achieved a continuous response lasting at least 25 weeks.
Thirty-four percent (34/101) of patients who were on concomitant ITP medication discontinued at least 1 medication. Thirty-nine percent (39/101) reduced or permanently stopped at least 1 ITP medication without receiving rescue therapy.
Fifty-seven percent of patients (171/302) had bleeding symptoms at baseline. This decreased to 16% (13/80) at 1 year.
“The EXTEND data published in Blood validate [eltrombopag] as an important oral treatment option that, by often increasing platelet counts, significantly decreased bleeding rates and reduced the need for concurrent therapies in certain patients with chronic/persistent immune thrombocytopenia,” said study author James Bussel, MD, of Weill Cornell Medicine in New York, New York.
“With this information, physicians can better optimize long-term disease management for appropriate patients living with this chronic disease.” ![]()
Guidelines cut acute chest syndrome hospital returns in pediatric sickle cell
Children with sickle cell disease who experience acute chest syndrome benefit from the current guideline-recommended antibiotic regimen, based on data from more than 7,000 patients.
Although acute chest syndrome (ACS) is among the most common complications of sickle cell disease (SCD), data on the effectiveness of the recommended antibiotic therapies (macrolides and cephalosporins) are lacking, wrote David G. Bundy, MD, of the Medical University of South Carolina, Charleston, and colleagues. ACS often leads to intensive hospital care and 1%-2% morbidity, they noted.
The most recent guidelines from the National Heart, Lung, and Blood Institute call for “an intravenous cephalosporin and an oral macrolide antibiotic,” the researchers said.
To determine the impact of antibiotic use as directed on reducing hospital readmissions in young SCD patients, the researchers reviewed data from 14,480 hospitalizations for ACS involving 7,178 children and young adults aged 0-22 years seen at 41 hospitals in the United States (JAMA Pediatr. 2017 Sep 11. doi: 10.1001/jamapediatrics.2017.2526).
“This high level of interhospital variation also suggests possible clinician disagreement regarding the ideal antibiotic treatment for children with ACS,” the researchers wrote.
Rates of all-cause readmission and 30-day ACS-related readmission were significantly lower among patients who received the recommended antibiotics (odds ratio, 0.50 and 0.71, respectively). Children aged 5-9 years were most likely to receive the recommended antibiotics (80%), while young adults aged 19-22 years were the least likely (64%).
The findings were limited by several factors, including coding errors and incomplete clinical information, the researchers noted. But the results suggest that the guideline-recommended antibiotics are effective, “so more robust dissemination and implementation of existing treatment guidelines may reduce readmissions in this high-risk population,” they said.
The researchers had no financial conflicts to disclose. Study coauthor Staci Arnold, MD, was supported in part by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program.
Children with sickle cell disease who experience acute chest syndrome benefit from the current guideline-recommended antibiotic regimen, based on data from more than 7,000 patients.
Although acute chest syndrome (ACS) is among the most common complications of sickle cell disease (SCD), data on the effectiveness of the recommended antibiotic therapies (macrolides and cephalosporins) are lacking, wrote David G. Bundy, MD, of the Medical University of South Carolina, Charleston, and colleagues. ACS often leads to intensive hospital care and 1%-2% morbidity, they noted.
The most recent guidelines from the National Heart, Lung, and Blood Institute call for “an intravenous cephalosporin and an oral macrolide antibiotic,” the researchers said.
To determine the impact of antibiotic use as directed on reducing hospital readmissions in young SCD patients, the researchers reviewed data from 14,480 hospitalizations for ACS involving 7,178 children and young adults aged 0-22 years seen at 41 hospitals in the United States (JAMA Pediatr. 2017 Sep 11. doi: 10.1001/jamapediatrics.2017.2526).
“This high level of interhospital variation also suggests possible clinician disagreement regarding the ideal antibiotic treatment for children with ACS,” the researchers wrote.
Rates of all-cause readmission and 30-day ACS-related readmission were significantly lower among patients who received the recommended antibiotics (odds ratio, 0.50 and 0.71, respectively). Children aged 5-9 years were most likely to receive the recommended antibiotics (80%), while young adults aged 19-22 years were the least likely (64%).
The findings were limited by several factors, including coding errors and incomplete clinical information, the researchers noted. But the results suggest that the guideline-recommended antibiotics are effective, “so more robust dissemination and implementation of existing treatment guidelines may reduce readmissions in this high-risk population,” they said.
The researchers had no financial conflicts to disclose. Study coauthor Staci Arnold, MD, was supported in part by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program.
Children with sickle cell disease who experience acute chest syndrome benefit from the current guideline-recommended antibiotic regimen, based on data from more than 7,000 patients.
Although acute chest syndrome (ACS) is among the most common complications of sickle cell disease (SCD), data on the effectiveness of the recommended antibiotic therapies (macrolides and cephalosporins) are lacking, wrote David G. Bundy, MD, of the Medical University of South Carolina, Charleston, and colleagues. ACS often leads to intensive hospital care and 1%-2% morbidity, they noted.
The most recent guidelines from the National Heart, Lung, and Blood Institute call for “an intravenous cephalosporin and an oral macrolide antibiotic,” the researchers said.
To determine the impact of antibiotic use as directed on reducing hospital readmissions in young SCD patients, the researchers reviewed data from 14,480 hospitalizations for ACS involving 7,178 children and young adults aged 0-22 years seen at 41 hospitals in the United States (JAMA Pediatr. 2017 Sep 11. doi: 10.1001/jamapediatrics.2017.2526).
“This high level of interhospital variation also suggests possible clinician disagreement regarding the ideal antibiotic treatment for children with ACS,” the researchers wrote.
Rates of all-cause readmission and 30-day ACS-related readmission were significantly lower among patients who received the recommended antibiotics (odds ratio, 0.50 and 0.71, respectively). Children aged 5-9 years were most likely to receive the recommended antibiotics (80%), while young adults aged 19-22 years were the least likely (64%).
The findings were limited by several factors, including coding errors and incomplete clinical information, the researchers noted. But the results suggest that the guideline-recommended antibiotics are effective, “so more robust dissemination and implementation of existing treatment guidelines may reduce readmissions in this high-risk population,” they said.
The researchers had no financial conflicts to disclose. Study coauthor Staci Arnold, MD, was supported in part by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program.
FROM JAMA PEDIATRICS
Key clinical point: Treatment with the recommended antibiotics was effective in reducing hospital readmissions for acute chest syndrome in children and young adults up to age 22 years with sickle cell disease.
Major finding: Hospital readmission for 30-day acute chest syndrome and all-cause readmission were significantly lower (odds ratio, 0.71 and 0.50, respectively) among children with sickle cell disease who received antibiotics (macrolides and cephalosporins) according to current guidelines, compared with those who did not.
Data source: A retrospective, multicenter study of 14,480 hospitalizations at 41 locations involving 7,178 children and young adults aged 0-22 years.
Disclosures: The researchers had no financial conflicts to disclose. Study coauthor Staci Arnold, MD, was supported in part by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program.
Team devises new method to analyze cells
Biophysicists have developed a new method to determine a cell’s mechanical properties, and they believe this method could provide insights regarding cancers, sickle cell anemia, and other diseases.
The method allows researchers to make standardized measurements of single cells, determine each cell’s stiffness, and assign it a number, generally between 10 and 20,000, in pascals.
“Measuring cells with our calibrated instrument is like measuring time with a standardized clock,” said Amy Rowat, PhD, of the University of California Los Angeles.
“Our method can be used to obtain stiffness measurements of hundreds of cells per second.”
Dr Rowat and her colleagues described their method in Biophysical Journal.
The method is called quantitative deformability cytometry (q-DC). It involves a small device (about 1 inch by 2 inches) made of a soft, flexible rubber that has integrated circuit chips like those in computers.
The researchers use gel particles containing molecules derived from seaweed to force cells through tiny pores in the device. As the cells flow through the device, the researchers take videos at thousands of frames per second—more than 100 times faster than standard video.
Dr Rowat and her colleagues used the device to analyze promyelocytic leukemia cells (HL-60) and breast cancer cells.
The researchers believe this work will provide scientists with a more precise, standardized method to distinguish cancer cells from normal cells.
The team thinks that, in the future, their method could be used to track a cancer patient over time to see how a drug is affecting the patient’s cancer cells.
“By using q-DC, we can very rapidly assess how specific drug treatments affect physical properties of single cells—such as shape, size, and stiffness—and achieve calibrated, quantitative measurements,” Dr Rowat said.
She and her colleagues believe q-DC might also help predict how invasive a cancer cell could be and which drugs might be most effective in fighting the cancer, as well as revealing which proteins are important in regulating the invasion of a cancer cell.
The researchers are now applying q-DC to other types of cancer cells. The team would like to better understand the relationship between a cancer cell’s physical properties and how easily cancer cells can spread through the body.
Dr Rowat’s hypothesis is that properties such as stiffness, size, and a cell’s ability to change shape are important in enabling cancer cells to maneuver.
The researchers said they can also use q-DC to measure other types of cells, such as normal and sickled red blood cells. ![]()
Biophysicists have developed a new method to determine a cell’s mechanical properties, and they believe this method could provide insights regarding cancers, sickle cell anemia, and other diseases.
The method allows researchers to make standardized measurements of single cells, determine each cell’s stiffness, and assign it a number, generally between 10 and 20,000, in pascals.
“Measuring cells with our calibrated instrument is like measuring time with a standardized clock,” said Amy Rowat, PhD, of the University of California Los Angeles.
“Our method can be used to obtain stiffness measurements of hundreds of cells per second.”
Dr Rowat and her colleagues described their method in Biophysical Journal.
The method is called quantitative deformability cytometry (q-DC). It involves a small device (about 1 inch by 2 inches) made of a soft, flexible rubber that has integrated circuit chips like those in computers.
The researchers use gel particles containing molecules derived from seaweed to force cells through tiny pores in the device. As the cells flow through the device, the researchers take videos at thousands of frames per second—more than 100 times faster than standard video.
Dr Rowat and her colleagues used the device to analyze promyelocytic leukemia cells (HL-60) and breast cancer cells.
The researchers believe this work will provide scientists with a more precise, standardized method to distinguish cancer cells from normal cells.
The team thinks that, in the future, their method could be used to track a cancer patient over time to see how a drug is affecting the patient’s cancer cells.
“By using q-DC, we can very rapidly assess how specific drug treatments affect physical properties of single cells—such as shape, size, and stiffness—and achieve calibrated, quantitative measurements,” Dr Rowat said.
She and her colleagues believe q-DC might also help predict how invasive a cancer cell could be and which drugs might be most effective in fighting the cancer, as well as revealing which proteins are important in regulating the invasion of a cancer cell.
The researchers are now applying q-DC to other types of cancer cells. The team would like to better understand the relationship between a cancer cell’s physical properties and how easily cancer cells can spread through the body.
Dr Rowat’s hypothesis is that properties such as stiffness, size, and a cell’s ability to change shape are important in enabling cancer cells to maneuver.
The researchers said they can also use q-DC to measure other types of cells, such as normal and sickled red blood cells. ![]()
Biophysicists have developed a new method to determine a cell’s mechanical properties, and they believe this method could provide insights regarding cancers, sickle cell anemia, and other diseases.
The method allows researchers to make standardized measurements of single cells, determine each cell’s stiffness, and assign it a number, generally between 10 and 20,000, in pascals.
“Measuring cells with our calibrated instrument is like measuring time with a standardized clock,” said Amy Rowat, PhD, of the University of California Los Angeles.
“Our method can be used to obtain stiffness measurements of hundreds of cells per second.”
Dr Rowat and her colleagues described their method in Biophysical Journal.
The method is called quantitative deformability cytometry (q-DC). It involves a small device (about 1 inch by 2 inches) made of a soft, flexible rubber that has integrated circuit chips like those in computers.
The researchers use gel particles containing molecules derived from seaweed to force cells through tiny pores in the device. As the cells flow through the device, the researchers take videos at thousands of frames per second—more than 100 times faster than standard video.
Dr Rowat and her colleagues used the device to analyze promyelocytic leukemia cells (HL-60) and breast cancer cells.
The researchers believe this work will provide scientists with a more precise, standardized method to distinguish cancer cells from normal cells.
The team thinks that, in the future, their method could be used to track a cancer patient over time to see how a drug is affecting the patient’s cancer cells.
“By using q-DC, we can very rapidly assess how specific drug treatments affect physical properties of single cells—such as shape, size, and stiffness—and achieve calibrated, quantitative measurements,” Dr Rowat said.
She and her colleagues believe q-DC might also help predict how invasive a cancer cell could be and which drugs might be most effective in fighting the cancer, as well as revealing which proteins are important in regulating the invasion of a cancer cell.
The researchers are now applying q-DC to other types of cancer cells. The team would like to better understand the relationship between a cancer cell’s physical properties and how easily cancer cells can spread through the body.
Dr Rowat’s hypothesis is that properties such as stiffness, size, and a cell’s ability to change shape are important in enabling cancer cells to maneuver.
The researchers said they can also use q-DC to measure other types of cells, such as normal and sickled red blood cells. ![]()
FDA rejects pegfilgrastim biosimilar
The US Food and Drug Administration (FDA) has issued a complete response letter saying the agency cannot approve MYL-1401H, a proposed biosimilar of pegfilgrastim (Neulasta).
Biocon and Mylan are seeking approval of MYL-1401H to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving chemotherapy to treat non-myeloid malignancies.
Biocon and Mylan filed the biologics license application for MYL-1401H in February.
The FDA had planned to issue a decision on the application by October 9.
Biocon and Mylan said the FDA’s complete response letter relates to a pending update to the application. The update involves chemistry manufacturing and control data from facility requalification activities after recent plant modifications.
The complete response letter did not raise any questions on the biosimilarity of MYL-1401H, pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity. (Results of a phase 3 study presented at ESMO 2016 Congress suggested MYL-1401H is equivalent to Neulasta.)
Biocon and Mylan said they do not expect the complete response letter for MYL-1401H to impact the commercial launch timing of the drug in the US. The companies said they are committed to working with the FDA to resolve the issues outlined in the letter. ![]()
The US Food and Drug Administration (FDA) has issued a complete response letter saying the agency cannot approve MYL-1401H, a proposed biosimilar of pegfilgrastim (Neulasta).
Biocon and Mylan are seeking approval of MYL-1401H to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving chemotherapy to treat non-myeloid malignancies.
Biocon and Mylan filed the biologics license application for MYL-1401H in February.
The FDA had planned to issue a decision on the application by October 9.
Biocon and Mylan said the FDA’s complete response letter relates to a pending update to the application. The update involves chemistry manufacturing and control data from facility requalification activities after recent plant modifications.
The complete response letter did not raise any questions on the biosimilarity of MYL-1401H, pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity. (Results of a phase 3 study presented at ESMO 2016 Congress suggested MYL-1401H is equivalent to Neulasta.)
Biocon and Mylan said they do not expect the complete response letter for MYL-1401H to impact the commercial launch timing of the drug in the US. The companies said they are committed to working with the FDA to resolve the issues outlined in the letter. ![]()
The US Food and Drug Administration (FDA) has issued a complete response letter saying the agency cannot approve MYL-1401H, a proposed biosimilar of pegfilgrastim (Neulasta).
Biocon and Mylan are seeking approval of MYL-1401H to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving chemotherapy to treat non-myeloid malignancies.
Biocon and Mylan filed the biologics license application for MYL-1401H in February.
The FDA had planned to issue a decision on the application by October 9.
Biocon and Mylan said the FDA’s complete response letter relates to a pending update to the application. The update involves chemistry manufacturing and control data from facility requalification activities after recent plant modifications.
The complete response letter did not raise any questions on the biosimilarity of MYL-1401H, pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity. (Results of a phase 3 study presented at ESMO 2016 Congress suggested MYL-1401H is equivalent to Neulasta.)
Biocon and Mylan said they do not expect the complete response letter for MYL-1401H to impact the commercial launch timing of the drug in the US. The companies said they are committed to working with the FDA to resolve the issues outlined in the letter. ![]()
Drug receives orphan designation for treatment of MDS
The European Commission has granted orphan designation to asunercept (APG101) for the treatment of myelodysplastic syndromes (MDS).
Asunercept is a fully human fusion protein that consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG1 antibody.
Asunercept binds to the CD95 ligand and blocks activation of the CD95 receptor.
Excessive stimulation of the CD95 receptor on hematopoietic precursors inhibits erythropoiesis in MDS patients.
As a result, the patients develop transfusion-dependent anemia that is refractory to erythropoiesis-stimulating agents (ESAs).
Treatment with asunercept, by inhibiting the CD95 system, stimulates the production of red blood cells and decreases transfusion dependency.
Asunercept has been evaluated in a phase 1 trial, the results of which were presented at the 2016 ASH Annual Meeting.
The trial enrolled 20 patients with low- to intermediate-risk MDS. All patients had anemia resulting in a high transfusion burden, had hemoglobin levels of less than 10 g/dL, and were refractory to ESAs.
Patients received once-weekly asunercept infusions for 12 weeks. Eight of the 20 patients (40%) experienced a reduction in transfusion frequency for 6 months.
Asunercept was considered generally well tolerated, with no grade 3 or higher treatment-related adverse events reported. The most common treatment-emergent adverse events were peripheral edema (n=6), urinary tract infection (n=4), and oral herpes (n=3).
One patient developed acute myeloid leukemia, and 1 patient died from sepsis due to pre-existing neutropenia.
“We are highly encouraged by the data from our clinical phase 1 trial with asunercept in these patients and are currently preparing to initiate a clinical phase 2 proof-of-concept trial to further evaluate the efficacy of asunercept in MDS,” said Harald Fricke, chief medical officer of Apogenix AG, the company developing asunercept.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission has granted orphan designation to asunercept (APG101) for the treatment of myelodysplastic syndromes (MDS).
Asunercept is a fully human fusion protein that consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG1 antibody.
Asunercept binds to the CD95 ligand and blocks activation of the CD95 receptor.
Excessive stimulation of the CD95 receptor on hematopoietic precursors inhibits erythropoiesis in MDS patients.
As a result, the patients develop transfusion-dependent anemia that is refractory to erythropoiesis-stimulating agents (ESAs).
Treatment with asunercept, by inhibiting the CD95 system, stimulates the production of red blood cells and decreases transfusion dependency.
Asunercept has been evaluated in a phase 1 trial, the results of which were presented at the 2016 ASH Annual Meeting.
The trial enrolled 20 patients with low- to intermediate-risk MDS. All patients had anemia resulting in a high transfusion burden, had hemoglobin levels of less than 10 g/dL, and were refractory to ESAs.
Patients received once-weekly asunercept infusions for 12 weeks. Eight of the 20 patients (40%) experienced a reduction in transfusion frequency for 6 months.
Asunercept was considered generally well tolerated, with no grade 3 or higher treatment-related adverse events reported. The most common treatment-emergent adverse events were peripheral edema (n=6), urinary tract infection (n=4), and oral herpes (n=3).
One patient developed acute myeloid leukemia, and 1 patient died from sepsis due to pre-existing neutropenia.
“We are highly encouraged by the data from our clinical phase 1 trial with asunercept in these patients and are currently preparing to initiate a clinical phase 2 proof-of-concept trial to further evaluate the efficacy of asunercept in MDS,” said Harald Fricke, chief medical officer of Apogenix AG, the company developing asunercept.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
The European Commission has granted orphan designation to asunercept (APG101) for the treatment of myelodysplastic syndromes (MDS).
Asunercept is a fully human fusion protein that consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG1 antibody.
Asunercept binds to the CD95 ligand and blocks activation of the CD95 receptor.
Excessive stimulation of the CD95 receptor on hematopoietic precursors inhibits erythropoiesis in MDS patients.
As a result, the patients develop transfusion-dependent anemia that is refractory to erythropoiesis-stimulating agents (ESAs).
Treatment with asunercept, by inhibiting the CD95 system, stimulates the production of red blood cells and decreases transfusion dependency.
Asunercept has been evaluated in a phase 1 trial, the results of which were presented at the 2016 ASH Annual Meeting.
The trial enrolled 20 patients with low- to intermediate-risk MDS. All patients had anemia resulting in a high transfusion burden, had hemoglobin levels of less than 10 g/dL, and were refractory to ESAs.
Patients received once-weekly asunercept infusions for 12 weeks. Eight of the 20 patients (40%) experienced a reduction in transfusion frequency for 6 months.
Asunercept was considered generally well tolerated, with no grade 3 or higher treatment-related adverse events reported. The most common treatment-emergent adverse events were peripheral edema (n=6), urinary tract infection (n=4), and oral herpes (n=3).
One patient developed acute myeloid leukemia, and 1 patient died from sepsis due to pre-existing neutropenia.
“We are highly encouraged by the data from our clinical phase 1 trial with asunercept in these patients and are currently preparing to initiate a clinical phase 2 proof-of-concept trial to further evaluate the efficacy of asunercept in MDS,” said Harald Fricke, chief medical officer of Apogenix AG, the company developing asunercept.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
Device could improve anemia detection
A new microfluidic device could improve testing for anemia, according to researchers.
The team said the device can detect the level of hemoglobin in a whole blood sample using optical absorbance.
The device is portable, requires only a few drops of blood for analysis, and eliminates the need for chemical preparations.
In addition, researchers believe the device could be integrated with other microfluidic approaches to blood analysis.
The researchers described their device in AIP Advances.
The team noted that blood analyzers currently on the market measure hemoglobin via hemolysis. This requires hands-on expertise to prepare and run a sample, limiting the ability to monitor anemia in many parts of the world.
“The most exciting aspect to this analyzer is that it uses whole blood and does not require the additional steps and reagents to prepare a sample,” said study author Nathan Sniadecki, PhD, of the University of Washington in Seattle.
“You just run blood into the channel, and that’s it,” added Nikita Taparia, a doctoral candidate in Sniadecki’s lab. “It can be used anywhere.”
The analyzer takes advantage of the optical properties of blood, such as absorption and scattering, to measure hemoglobin concentration. Anemic blood transmits more light than normal blood, so the severity of anemia can be measured as a ratio of transmitted to original light intensity.
To simulate anemia, the researchers diluted blood samples with a buffer solution. The blood analyzer was effective at predicting cases of moderate to severe anemia, defined as less than 10 g/dL of hemoglobin in a sample. The analyzer did not produce any false-negative results.
The optical density of samples did not increase linearly, so a higher concentration of hemoglobin defines the upper limit of detection for the device.
The researchers said the device could be integrated with other microfluidic devices to analyze whole blood samples in parallel to diagnose anemia and other underlying factors that could contribute to the condition.
The team said such an integrated diagnostic tool would “aid the global health community in their continued surveillance of anemia and its etiology in high-risk subpopulations.” ![]()
A new microfluidic device could improve testing for anemia, according to researchers.
The team said the device can detect the level of hemoglobin in a whole blood sample using optical absorbance.
The device is portable, requires only a few drops of blood for analysis, and eliminates the need for chemical preparations.
In addition, researchers believe the device could be integrated with other microfluidic approaches to blood analysis.
The researchers described their device in AIP Advances.
The team noted that blood analyzers currently on the market measure hemoglobin via hemolysis. This requires hands-on expertise to prepare and run a sample, limiting the ability to monitor anemia in many parts of the world.
“The most exciting aspect to this analyzer is that it uses whole blood and does not require the additional steps and reagents to prepare a sample,” said study author Nathan Sniadecki, PhD, of the University of Washington in Seattle.
“You just run blood into the channel, and that’s it,” added Nikita Taparia, a doctoral candidate in Sniadecki’s lab. “It can be used anywhere.”
The analyzer takes advantage of the optical properties of blood, such as absorption and scattering, to measure hemoglobin concentration. Anemic blood transmits more light than normal blood, so the severity of anemia can be measured as a ratio of transmitted to original light intensity.
To simulate anemia, the researchers diluted blood samples with a buffer solution. The blood analyzer was effective at predicting cases of moderate to severe anemia, defined as less than 10 g/dL of hemoglobin in a sample. The analyzer did not produce any false-negative results.
The optical density of samples did not increase linearly, so a higher concentration of hemoglobin defines the upper limit of detection for the device.
The researchers said the device could be integrated with other microfluidic devices to analyze whole blood samples in parallel to diagnose anemia and other underlying factors that could contribute to the condition.
The team said such an integrated diagnostic tool would “aid the global health community in their continued surveillance of anemia and its etiology in high-risk subpopulations.” ![]()
A new microfluidic device could improve testing for anemia, according to researchers.
The team said the device can detect the level of hemoglobin in a whole blood sample using optical absorbance.
The device is portable, requires only a few drops of blood for analysis, and eliminates the need for chemical preparations.
In addition, researchers believe the device could be integrated with other microfluidic approaches to blood analysis.
The researchers described their device in AIP Advances.
The team noted that blood analyzers currently on the market measure hemoglobin via hemolysis. This requires hands-on expertise to prepare and run a sample, limiting the ability to monitor anemia in many parts of the world.
“The most exciting aspect to this analyzer is that it uses whole blood and does not require the additional steps and reagents to prepare a sample,” said study author Nathan Sniadecki, PhD, of the University of Washington in Seattle.
“You just run blood into the channel, and that’s it,” added Nikita Taparia, a doctoral candidate in Sniadecki’s lab. “It can be used anywhere.”
The analyzer takes advantage of the optical properties of blood, such as absorption and scattering, to measure hemoglobin concentration. Anemic blood transmits more light than normal blood, so the severity of anemia can be measured as a ratio of transmitted to original light intensity.
To simulate anemia, the researchers diluted blood samples with a buffer solution. The blood analyzer was effective at predicting cases of moderate to severe anemia, defined as less than 10 g/dL of hemoglobin in a sample. The analyzer did not produce any false-negative results.
The optical density of samples did not increase linearly, so a higher concentration of hemoglobin defines the upper limit of detection for the device.
The researchers said the device could be integrated with other microfluidic devices to analyze whole blood samples in parallel to diagnose anemia and other underlying factors that could contribute to the condition.
The team said such an integrated diagnostic tool would “aid the global health community in their continued surveillance of anemia and its etiology in high-risk subpopulations.” ![]()
Fostamatinib elicits responses in AIHA
The oral SYK inhibitor fostamatinib can produce responses in patients with warm antibody autoimmune hemolytic anemia (AIHA), according to Rigel Pharmaceuticals, Inc.
The company reported topline results from the first stage of the phase 2 SOAR study, which showed that fostamatinib produced a 35% response rate.
A response was defined as achieving a hemoglobin level of greater than 10 g/dL and at least a 2 g/dL increase from baseline.
“Many patients with AIHA suffer from severe, debilitating disease that negatively affects their quality of life,” said David J. Kuter, MD, the director for the Center of Hematology at Massachusetts General Hospital in Boston and the lead investigator of the SOAR study.
“There are no FDA-approved medications for the treatment of AIHA, which means that those living with the condition are in need of new and effective therapeutic options.”
In the SOAR study, Dr Kuter and his colleagues are evaluating fostamatinib in patients with warm antibody AIHA who previously received at least 1 treatment but did not have a meaningful benefit and are still anemic.
The study utilizes an open-label, Simon 2-stage design to evaluate fostamatinib given at 150 mg twice daily.
Stage 1 has enrolled 17 patients who have had at least 1 post-baseline hemoglobin measure.
Four of these patients responded to fostamatinib during the 12-week evaluation period, and an additional 2 patients met response criteria in the extension study after 12 weeks of dosing.
So the overall response rate was 35% (6/17), although Rigel Pharmaceuticals said these data are preliminary and require further verification.
Two patients withdrew from the study early due to non-safety-related reasons and will be replaced per the study protocol.
According to Rigel Pharmaceuticals, the treatment-emergent adverse events (AEs) in this trial were consistent with the prior clinical experience with fostamatinib.
Treatment-emergent AEs—which included diarrhea, elevated liver function tests, and hypertension—were manageable and mostly mild or moderate in nature.
There were 2 deaths reported during the trial. Both were due to non-treatment-related serious AEs, according to investigators. One patient had skin necrosis and infection. The other was an elderly patient who had pneumonia and was immunosuppressed due to prior chronic lymphocytic leukemia and steroid use.
A third patient experienced a non-treatment-related serious AE but recovered and continued on treatment.
Rigel Pharmaceuticals said a comprehensive analysis of the data will continue and will be presented at a future scientific conference.
The company also intends to begin enrollment for stage 2 of this study, in which 20 patients will be enrolled under the same protocol. ![]()
The oral SYK inhibitor fostamatinib can produce responses in patients with warm antibody autoimmune hemolytic anemia (AIHA), according to Rigel Pharmaceuticals, Inc.
The company reported topline results from the first stage of the phase 2 SOAR study, which showed that fostamatinib produced a 35% response rate.
A response was defined as achieving a hemoglobin level of greater than 10 g/dL and at least a 2 g/dL increase from baseline.
“Many patients with AIHA suffer from severe, debilitating disease that negatively affects their quality of life,” said David J. Kuter, MD, the director for the Center of Hematology at Massachusetts General Hospital in Boston and the lead investigator of the SOAR study.
“There are no FDA-approved medications for the treatment of AIHA, which means that those living with the condition are in need of new and effective therapeutic options.”
In the SOAR study, Dr Kuter and his colleagues are evaluating fostamatinib in patients with warm antibody AIHA who previously received at least 1 treatment but did not have a meaningful benefit and are still anemic.
The study utilizes an open-label, Simon 2-stage design to evaluate fostamatinib given at 150 mg twice daily.
Stage 1 has enrolled 17 patients who have had at least 1 post-baseline hemoglobin measure.
Four of these patients responded to fostamatinib during the 12-week evaluation period, and an additional 2 patients met response criteria in the extension study after 12 weeks of dosing.
So the overall response rate was 35% (6/17), although Rigel Pharmaceuticals said these data are preliminary and require further verification.
Two patients withdrew from the study early due to non-safety-related reasons and will be replaced per the study protocol.
According to Rigel Pharmaceuticals, the treatment-emergent adverse events (AEs) in this trial were consistent with the prior clinical experience with fostamatinib.
Treatment-emergent AEs—which included diarrhea, elevated liver function tests, and hypertension—were manageable and mostly mild or moderate in nature.
There were 2 deaths reported during the trial. Both were due to non-treatment-related serious AEs, according to investigators. One patient had skin necrosis and infection. The other was an elderly patient who had pneumonia and was immunosuppressed due to prior chronic lymphocytic leukemia and steroid use.
A third patient experienced a non-treatment-related serious AE but recovered and continued on treatment.
Rigel Pharmaceuticals said a comprehensive analysis of the data will continue and will be presented at a future scientific conference.
The company also intends to begin enrollment for stage 2 of this study, in which 20 patients will be enrolled under the same protocol. ![]()
The oral SYK inhibitor fostamatinib can produce responses in patients with warm antibody autoimmune hemolytic anemia (AIHA), according to Rigel Pharmaceuticals, Inc.
The company reported topline results from the first stage of the phase 2 SOAR study, which showed that fostamatinib produced a 35% response rate.
A response was defined as achieving a hemoglobin level of greater than 10 g/dL and at least a 2 g/dL increase from baseline.
“Many patients with AIHA suffer from severe, debilitating disease that negatively affects their quality of life,” said David J. Kuter, MD, the director for the Center of Hematology at Massachusetts General Hospital in Boston and the lead investigator of the SOAR study.
“There are no FDA-approved medications for the treatment of AIHA, which means that those living with the condition are in need of new and effective therapeutic options.”
In the SOAR study, Dr Kuter and his colleagues are evaluating fostamatinib in patients with warm antibody AIHA who previously received at least 1 treatment but did not have a meaningful benefit and are still anemic.
The study utilizes an open-label, Simon 2-stage design to evaluate fostamatinib given at 150 mg twice daily.
Stage 1 has enrolled 17 patients who have had at least 1 post-baseline hemoglobin measure.
Four of these patients responded to fostamatinib during the 12-week evaluation period, and an additional 2 patients met response criteria in the extension study after 12 weeks of dosing.
So the overall response rate was 35% (6/17), although Rigel Pharmaceuticals said these data are preliminary and require further verification.
Two patients withdrew from the study early due to non-safety-related reasons and will be replaced per the study protocol.
According to Rigel Pharmaceuticals, the treatment-emergent adverse events (AEs) in this trial were consistent with the prior clinical experience with fostamatinib.
Treatment-emergent AEs—which included diarrhea, elevated liver function tests, and hypertension—were manageable and mostly mild or moderate in nature.
There were 2 deaths reported during the trial. Both were due to non-treatment-related serious AEs, according to investigators. One patient had skin necrosis and infection. The other was an elderly patient who had pneumonia and was immunosuppressed due to prior chronic lymphocytic leukemia and steroid use.
A third patient experienced a non-treatment-related serious AE but recovered and continued on treatment.
Rigel Pharmaceuticals said a comprehensive analysis of the data will continue and will be presented at a future scientific conference.
The company also intends to begin enrollment for stage 2 of this study, in which 20 patients will be enrolled under the same protocol. ![]()
Caplacizumab may enhance treatment of aTTP
Caplacizumab can improve upon standard care for patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to results reported by Ablynx, the company developing caplacizumab.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab had a significant reduction in time to platelet count response.
In addition, they were significantly less likely than patients who received placebo to achieve the combined endpoint of aTTP-related death, aTTP recurrence, and experiencing at least 1 major thromboembolic event during the treatment period.
The safety profile of caplacizumab in this trial was said to be consistent with results from the phase 2 TITAN trial.
“The results of this landmark trial constitute a complete game-changer for patients with aTTP,” said HERCULES investigator Marie Scully, MBBS, of the University College Hospital in London, UK.
“They will revolutionize how we manage the acute phase of the disease, which is when patients are at highest risk for organ damage, recurrence, and death.”
Treatment
The HERCULES trial included 145 patients with an acute episode of aTTP. They were randomized 1:1 to receive either caplacizumab or placebo in addition to daily plasma exchange and immunosuppression (standard of care).
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange.
If, at the end of this treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, the treatment could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment.
Baseline characteristics
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. A majority of patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to confirmed normalization of platelet count response. There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A key secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
Another key secondary endpoint was the incidence of aTTP recurrence during the overall study period, which was 12.7% (n=9) in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
The incidence of aTTP recurrence during the follow-up period alone was 9.1% (n=6) in the caplacizumab arm and 0% (n=0) in the placebo arm.
A third key secondary endpoint was the percentage of patients with refractory aTTP, which was 0% (n=0) in the caplacizumab arm and 4.2% (n=3) in the placebo arm (P=0.0572).
Safety
The number and nature of treatment-emergent adverse events (AEs) were similar between the treatment arms, according to Ablynx. The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm than the placebo arm—66.2% and 49.3%, respectively. However, most bleeding-related events were mild or moderate in severity.
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
Caplacizumab can improve upon standard care for patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to results reported by Ablynx, the company developing caplacizumab.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab had a significant reduction in time to platelet count response.
In addition, they were significantly less likely than patients who received placebo to achieve the combined endpoint of aTTP-related death, aTTP recurrence, and experiencing at least 1 major thromboembolic event during the treatment period.
The safety profile of caplacizumab in this trial was said to be consistent with results from the phase 2 TITAN trial.
“The results of this landmark trial constitute a complete game-changer for patients with aTTP,” said HERCULES investigator Marie Scully, MBBS, of the University College Hospital in London, UK.
“They will revolutionize how we manage the acute phase of the disease, which is when patients are at highest risk for organ damage, recurrence, and death.”
Treatment
The HERCULES trial included 145 patients with an acute episode of aTTP. They were randomized 1:1 to receive either caplacizumab or placebo in addition to daily plasma exchange and immunosuppression (standard of care).
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange.
If, at the end of this treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, the treatment could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment.
Baseline characteristics
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. A majority of patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to confirmed normalization of platelet count response. There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A key secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
Another key secondary endpoint was the incidence of aTTP recurrence during the overall study period, which was 12.7% (n=9) in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
The incidence of aTTP recurrence during the follow-up period alone was 9.1% (n=6) in the caplacizumab arm and 0% (n=0) in the placebo arm.
A third key secondary endpoint was the percentage of patients with refractory aTTP, which was 0% (n=0) in the caplacizumab arm and 4.2% (n=3) in the placebo arm (P=0.0572).
Safety
The number and nature of treatment-emergent adverse events (AEs) were similar between the treatment arms, according to Ablynx. The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm than the placebo arm—66.2% and 49.3%, respectively. However, most bleeding-related events were mild or moderate in severity.
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab. ![]()
Caplacizumab can improve upon standard care for patients with acquired thrombotic thrombocytopenic purpura (aTTP), according to results reported by Ablynx, the company developing caplacizumab.
In the phase 3 HERCULES trial, researchers compared caplacizumab, an anti-von Willebrand factor nanobody, plus standard care to placebo plus standard care in patients with aTTP.
Patients who received caplacizumab had a significant reduction in time to platelet count response.
In addition, they were significantly less likely than patients who received placebo to achieve the combined endpoint of aTTP-related death, aTTP recurrence, and experiencing at least 1 major thromboembolic event during the treatment period.
The safety profile of caplacizumab in this trial was said to be consistent with results from the phase 2 TITAN trial.
“The results of this landmark trial constitute a complete game-changer for patients with aTTP,” said HERCULES investigator Marie Scully, MBBS, of the University College Hospital in London, UK.
“They will revolutionize how we manage the acute phase of the disease, which is when patients are at highest risk for organ damage, recurrence, and death.”
Treatment
The HERCULES trial included 145 patients with an acute episode of aTTP. They were randomized 1:1 to receive either caplacizumab or placebo in addition to daily plasma exchange and immunosuppression (standard of care).
Patients received a single intravenous bolus of 10 mg of caplacizumab or placebo followed by a daily subcutaneous dose of 10 mg of caplacizumab or placebo until 30 days after the last daily plasma exchange.
If, at the end of this treatment period, there was evidence of persistent underlying disease activity indicative of an imminent risk for recurrence, the treatment could be extended for additional 7-day periods up to a maximum of 28 days. Patients were followed for a further 28 days after discontinuation of treatment.
In all, 71 patients received caplacizumab, and 58 (80.6%) of them completed the treatment. Seventy-three patients received placebo, and 50 of these patients (68.5%) completed treatment.
Baseline characteristics
At baseline, the mean age was 44.9 in the caplacizumab arm and 47.3 in the placebo arm. A majority of patients in both arms were female—68.1% and 69.9%, respectively.
The proportion of patients with an initial aTTP episode was 66.7% in the caplacizumab arm and 46.6% in the placebo arm. The proportion with a recurrent episode was 33.3% and 53.4%, respectively.
Most patients in both arms had ADAMTS13 activity below 10% at baseline—81.7% in the caplacizumab arm and 90.3% in the placebo arm.
The mean platelet count at baseline was 32.0 x 109/L in the caplacizumab arm and 39.1 x 109/L in the placebo arm.
Efficacy
The study’s primary endpoint was the time to confirmed normalization of platelet count response. There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A key secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
Another key secondary endpoint was the incidence of aTTP recurrence during the overall study period, which was 12.7% (n=9) in the caplacizumab arm and 38.4% (n=28) in the placebo arm (P<0.001).
The incidence of aTTP recurrence during the follow-up period alone was 9.1% (n=6) in the caplacizumab arm and 0% (n=0) in the placebo arm.
A third key secondary endpoint was the percentage of patients with refractory aTTP, which was 0% (n=0) in the caplacizumab arm and 4.2% (n=3) in the placebo arm (P=0.0572).
Safety
The number and nature of treatment-emergent adverse events (AEs) were similar between the treatment arms, according to Ablynx. The proportion of patients with at least 1 treatment-emergent AE was 97.2% in the caplacizumab arm and 97.3% in the placebo arm.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
The incidence of bleeding-related AEs was higher in the caplacizumab arm than the placebo arm—66.2% and 49.3%, respectively. However, most bleeding-related events were mild or moderate in severity.
The proportion of patients with at least 1 serious AE was 39.4% (n=28) in the caplacizumab arm and 53.4% (n=39) in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab.
Many years on metformin linked to anemia risk
LISBON – People with type 2 diabetes who take metformin for many years are more likely to develop anemia than are those who do not, according to the results of a large analysis of data from an observational, population-based study with 20 years of follow-up.
“Metformin treatment was associated with a 6% higher risk of anemia for every cumulative year of metformin exposure,” Louise Donnelly, PhD, and her associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes.
In an interview, Dr. Donnelly, a postdoctoral research assistant at the University of Dundee (Scotland), explained why they looked at the use of metformin and anemia risk in people with type 2 diabetes.
“The Diabetes Prevention Program (DPP) study showed that long-term metformin use in individuals with impaired glucose tolerance was associated with an increased risk of anemia, and this was independent of vitamin B12 status,” she said (J Clin Endocrinol Metab. 2016;101:1754-61). “Anemia is a common finding in people with type 2 diabetes, but the impact of long-term metformin use on anemia hasn’t been studied.”
Dr. Donnelly and her associates obtained detailed information on metformin prescribing and hematology measures from electronic patient medical records from the Genetics of Diabetes Audit and Research in Tayside and Scotland (GoDARTS) cohort, based in Scotland. This database contains information on individuals with type 2 diabetes and matching controls and is available to researchers worldwide.
For the analysis, the team looked for people diagnosed from 1996 onward who had a baseline hemoglobin measurement. Of 6,440 individuals with type 2 diabetes in the GoDARTS cohort, just over half had a hemoglobin measurement.
“We used a definition of ‘moderate’ anemia and we excluded patients with mild anemia or worse at diabetes diagnosis,” Dr. Donnelly observed. Anemia was considered to be a hemoglobin level of less than 12 g/dL in women and less than 13 g/dL in men. In all, 280 individuals with anemia were excluded from further analysis as the aim was to follow people until they developed anemia, died, left the area, or until the end of the follow-up period, which was set at September 30, 2015. A discrete-time failure analysis was used to model the effect of cumulative metformin exposure on anemia risk.
After a median follow-up of 8 years and a median number of 11 hemoglobin measurements per patient, 2,487 study subjects (71%) had some exposure to metformin and 1,458 of the whole sample (41.8%) had become anemic. Of those who developed anemia, 745 (51%) were current metformin users, 194 (13%) were former users, and 519 (36%) had never taken metformin.
“Cumulative metformin use was independently associated with an increased risk of anemia,” Dr. Donnelly noted (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.02-1.09; P = .0006). This association was not seen when they examined the data based on sulfonylurea use (OR 1.0; 95% CI 0.97-1.04, P = .8), she added.
“Anemia risk was higher with age at diagnosis, duration of diabetes, lower hemoglobin at baseline, and lower eGFR [estimated glomerular filtration rate],” she observed. ORs for first anemia event were 1.03 (95% CI, 1.02-1.04) for every year of increasing age, 1.05 (95% CI, 1.03-1.08) for every additional year since diabetes diagnosis, 0.70 (95% CI, 0.66-0.74) per 1 g/dL of hemoglobin at diagnosis, and eGFR 0.98 (95% CI, 0.98-1.01) per additional 1 mL/min per 1.732 (P less than .0001 for all).
Why cumulative metformin use is associated with an increased of anemia is unclear, however, and Dr. Donnelly noted that this needs further investigation. “We do have data from two other clinical trials now, showing similar results, and maybe through those data we might be able to untangle it.”
The team does not think the anemia is related to B12 deficiency, however, as people who developed anemia while taking metformin were more likely to develop microcytic (12% vs. 7.3%) than macrocytic (7.6% vs. 12.3%), anemia, compared with people with anemia who were not exposed to metformin (P less than .0001).
“In terms of mechanism, we can only conjecture,” Ewan Pearson, MB, senior author of the study and professor of medicine at the University of Dundee, said during a discussion at the poster presentation. “It is important to stress that metformin is a great drug and we shouldn’t stop it because of a potentially increased risk of anemia.”
The Medical Research Council supported the work. Dr. Donnelly reported having no financial disclosures.
LISBON – People with type 2 diabetes who take metformin for many years are more likely to develop anemia than are those who do not, according to the results of a large analysis of data from an observational, population-based study with 20 years of follow-up.
“Metformin treatment was associated with a 6% higher risk of anemia for every cumulative year of metformin exposure,” Louise Donnelly, PhD, and her associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes.
In an interview, Dr. Donnelly, a postdoctoral research assistant at the University of Dundee (Scotland), explained why they looked at the use of metformin and anemia risk in people with type 2 diabetes.
“The Diabetes Prevention Program (DPP) study showed that long-term metformin use in individuals with impaired glucose tolerance was associated with an increased risk of anemia, and this was independent of vitamin B12 status,” she said (J Clin Endocrinol Metab. 2016;101:1754-61). “Anemia is a common finding in people with type 2 diabetes, but the impact of long-term metformin use on anemia hasn’t been studied.”
Dr. Donnelly and her associates obtained detailed information on metformin prescribing and hematology measures from electronic patient medical records from the Genetics of Diabetes Audit and Research in Tayside and Scotland (GoDARTS) cohort, based in Scotland. This database contains information on individuals with type 2 diabetes and matching controls and is available to researchers worldwide.
For the analysis, the team looked for people diagnosed from 1996 onward who had a baseline hemoglobin measurement. Of 6,440 individuals with type 2 diabetes in the GoDARTS cohort, just over half had a hemoglobin measurement.
“We used a definition of ‘moderate’ anemia and we excluded patients with mild anemia or worse at diabetes diagnosis,” Dr. Donnelly observed. Anemia was considered to be a hemoglobin level of less than 12 g/dL in women and less than 13 g/dL in men. In all, 280 individuals with anemia were excluded from further analysis as the aim was to follow people until they developed anemia, died, left the area, or until the end of the follow-up period, which was set at September 30, 2015. A discrete-time failure analysis was used to model the effect of cumulative metformin exposure on anemia risk.
After a median follow-up of 8 years and a median number of 11 hemoglobin measurements per patient, 2,487 study subjects (71%) had some exposure to metformin and 1,458 of the whole sample (41.8%) had become anemic. Of those who developed anemia, 745 (51%) were current metformin users, 194 (13%) were former users, and 519 (36%) had never taken metformin.
“Cumulative metformin use was independently associated with an increased risk of anemia,” Dr. Donnelly noted (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.02-1.09; P = .0006). This association was not seen when they examined the data based on sulfonylurea use (OR 1.0; 95% CI 0.97-1.04, P = .8), she added.
“Anemia risk was higher with age at diagnosis, duration of diabetes, lower hemoglobin at baseline, and lower eGFR [estimated glomerular filtration rate],” she observed. ORs for first anemia event were 1.03 (95% CI, 1.02-1.04) for every year of increasing age, 1.05 (95% CI, 1.03-1.08) for every additional year since diabetes diagnosis, 0.70 (95% CI, 0.66-0.74) per 1 g/dL of hemoglobin at diagnosis, and eGFR 0.98 (95% CI, 0.98-1.01) per additional 1 mL/min per 1.732 (P less than .0001 for all).
Why cumulative metformin use is associated with an increased of anemia is unclear, however, and Dr. Donnelly noted that this needs further investigation. “We do have data from two other clinical trials now, showing similar results, and maybe through those data we might be able to untangle it.”
The team does not think the anemia is related to B12 deficiency, however, as people who developed anemia while taking metformin were more likely to develop microcytic (12% vs. 7.3%) than macrocytic (7.6% vs. 12.3%), anemia, compared with people with anemia who were not exposed to metformin (P less than .0001).
“In terms of mechanism, we can only conjecture,” Ewan Pearson, MB, senior author of the study and professor of medicine at the University of Dundee, said during a discussion at the poster presentation. “It is important to stress that metformin is a great drug and we shouldn’t stop it because of a potentially increased risk of anemia.”
The Medical Research Council supported the work. Dr. Donnelly reported having no financial disclosures.
LISBON – People with type 2 diabetes who take metformin for many years are more likely to develop anemia than are those who do not, according to the results of a large analysis of data from an observational, population-based study with 20 years of follow-up.
“Metformin treatment was associated with a 6% higher risk of anemia for every cumulative year of metformin exposure,” Louise Donnelly, PhD, and her associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes.
In an interview, Dr. Donnelly, a postdoctoral research assistant at the University of Dundee (Scotland), explained why they looked at the use of metformin and anemia risk in people with type 2 diabetes.
“The Diabetes Prevention Program (DPP) study showed that long-term metformin use in individuals with impaired glucose tolerance was associated with an increased risk of anemia, and this was independent of vitamin B12 status,” she said (J Clin Endocrinol Metab. 2016;101:1754-61). “Anemia is a common finding in people with type 2 diabetes, but the impact of long-term metformin use on anemia hasn’t been studied.”
Dr. Donnelly and her associates obtained detailed information on metformin prescribing and hematology measures from electronic patient medical records from the Genetics of Diabetes Audit and Research in Tayside and Scotland (GoDARTS) cohort, based in Scotland. This database contains information on individuals with type 2 diabetes and matching controls and is available to researchers worldwide.
For the analysis, the team looked for people diagnosed from 1996 onward who had a baseline hemoglobin measurement. Of 6,440 individuals with type 2 diabetes in the GoDARTS cohort, just over half had a hemoglobin measurement.
“We used a definition of ‘moderate’ anemia and we excluded patients with mild anemia or worse at diabetes diagnosis,” Dr. Donnelly observed. Anemia was considered to be a hemoglobin level of less than 12 g/dL in women and less than 13 g/dL in men. In all, 280 individuals with anemia were excluded from further analysis as the aim was to follow people until they developed anemia, died, left the area, or until the end of the follow-up period, which was set at September 30, 2015. A discrete-time failure analysis was used to model the effect of cumulative metformin exposure on anemia risk.
After a median follow-up of 8 years and a median number of 11 hemoglobin measurements per patient, 2,487 study subjects (71%) had some exposure to metformin and 1,458 of the whole sample (41.8%) had become anemic. Of those who developed anemia, 745 (51%) were current metformin users, 194 (13%) were former users, and 519 (36%) had never taken metformin.
“Cumulative metformin use was independently associated with an increased risk of anemia,” Dr. Donnelly noted (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.02-1.09; P = .0006). This association was not seen when they examined the data based on sulfonylurea use (OR 1.0; 95% CI 0.97-1.04, P = .8), she added.
“Anemia risk was higher with age at diagnosis, duration of diabetes, lower hemoglobin at baseline, and lower eGFR [estimated glomerular filtration rate],” she observed. ORs for first anemia event were 1.03 (95% CI, 1.02-1.04) for every year of increasing age, 1.05 (95% CI, 1.03-1.08) for every additional year since diabetes diagnosis, 0.70 (95% CI, 0.66-0.74) per 1 g/dL of hemoglobin at diagnosis, and eGFR 0.98 (95% CI, 0.98-1.01) per additional 1 mL/min per 1.732 (P less than .0001 for all).
Why cumulative metformin use is associated with an increased of anemia is unclear, however, and Dr. Donnelly noted that this needs further investigation. “We do have data from two other clinical trials now, showing similar results, and maybe through those data we might be able to untangle it.”
The team does not think the anemia is related to B12 deficiency, however, as people who developed anemia while taking metformin were more likely to develop microcytic (12% vs. 7.3%) than macrocytic (7.6% vs. 12.3%), anemia, compared with people with anemia who were not exposed to metformin (P less than .0001).
“In terms of mechanism, we can only conjecture,” Ewan Pearson, MB, senior author of the study and professor of medicine at the University of Dundee, said during a discussion at the poster presentation. “It is important to stress that metformin is a great drug and we shouldn’t stop it because of a potentially increased risk of anemia.”
The Medical Research Council supported the work. Dr. Donnelly reported having no financial disclosures.
AT EASD 2017
Key clinical point: Cumulative metformin use was associated with an increased risk for anemia in patients with type 2 diabetes.
Major finding: For every additional year of metformin use, there was a 6% increase in the risk for anemia.
Data source: Data analysis of 3,435 individuals with type 2 diabetes who participated in a large observational, population-based study with almost 20 years of follow-up.
Disclosures: The Medical Research Council supported the work. Dr. Donnelly reported having no financial disclosures.
Long-term specialist care reduces post-RYGB anemia risk
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
FROM JAMA SURGERY
Key clinical point:
Major finding: RYGB patients without specialist follow-up had significantly higher odds of anemia at 10 years (adjusted odds ratio, 6.1).
Data source: A retrospective review of 74 patients from a prospective 10-year database.
Disclosures: The authors reported having no disclosures.