User login
Medicare to cover HSCT in approved clinical trials for myeloma, myelofibrosis, sickle cell disease
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
NHSBT offers more precise blood typing

Photo by Juan D. Alfonso
NHS Blood and Transplant (NHSBT) has announced an initiative to provide more detailed blood-group typing for patients with hemoglobinopathies, with the goal of enabling better-matched and potentially safer transfusions.
The typing will detect Rh variant blood groups, which need to be considered when planning transfusions.
Previously, typing to this level was only possible through reference laboratories using complex genotyping methods.
NHSBT is offering the testing at no extra cost to hospitals in England until the end of June 2016.
The initiative involves routinely testing for the RHD and RHCE variants most commonly found in patients with hemoglobinopathies. NHSBT will also test genes for the blood groups K, k, Kpa, Kpb, Jsa, Jsb, Jka, Jkb, Fya, Fyb, Fy (GATA), M, N, S, s, U, Doa, and Dob.
Unlike older methods, this testing can be performed in patients who have recently received blood.
NHSBT said this initiative will enable the creation of a database of genotyped blood details for patients with hemoglobinopathies.
Extended blood type information and fast access to the database could potentially enable safer blood transfusions for these patients, who may need numerous transfusions during their lifetime and may move between hospitals.
NHSBT said it has received more than 2500 blood samples thus far. The results are processed centrally by NHSBT at the International Blood Group Reference Laboratory in Filton and are securely stored.
Patients’ test results will be accessible to the teams involved in the patients’ care.
“Patients taking part can now potentially receive more finely matched blood if we know not just their blood group but whether they have a variant Rh type,” said Sara Trompeter, MB ChB, a consultant hematologist for NHSBT.
“And there will also be greater safety and likelihood of getting matched blood in an emergency, as their records will be held centrally and can be accessed by blood banks in local hospitals. We would urge all patients with hemoglobin disorders such as sickle cell disease or thalassemia to speak to their medical or nursing team about providing a blood sample to NHS Blood and Transplant via their local transfusion laboratories to be genotyped.”
Additional information on this initiative can be found at www.nhsbt.nhs.uk/extendedbloodgrouptesting. ![]()

Photo by Juan D. Alfonso
NHS Blood and Transplant (NHSBT) has announced an initiative to provide more detailed blood-group typing for patients with hemoglobinopathies, with the goal of enabling better-matched and potentially safer transfusions.
The typing will detect Rh variant blood groups, which need to be considered when planning transfusions.
Previously, typing to this level was only possible through reference laboratories using complex genotyping methods.
NHSBT is offering the testing at no extra cost to hospitals in England until the end of June 2016.
The initiative involves routinely testing for the RHD and RHCE variants most commonly found in patients with hemoglobinopathies. NHSBT will also test genes for the blood groups K, k, Kpa, Kpb, Jsa, Jsb, Jka, Jkb, Fya, Fyb, Fy (GATA), M, N, S, s, U, Doa, and Dob.
Unlike older methods, this testing can be performed in patients who have recently received blood.
NHSBT said this initiative will enable the creation of a database of genotyped blood details for patients with hemoglobinopathies.
Extended blood type information and fast access to the database could potentially enable safer blood transfusions for these patients, who may need numerous transfusions during their lifetime and may move between hospitals.
NHSBT said it has received more than 2500 blood samples thus far. The results are processed centrally by NHSBT at the International Blood Group Reference Laboratory in Filton and are securely stored.
Patients’ test results will be accessible to the teams involved in the patients’ care.
“Patients taking part can now potentially receive more finely matched blood if we know not just their blood group but whether they have a variant Rh type,” said Sara Trompeter, MB ChB, a consultant hematologist for NHSBT.
“And there will also be greater safety and likelihood of getting matched blood in an emergency, as their records will be held centrally and can be accessed by blood banks in local hospitals. We would urge all patients with hemoglobin disorders such as sickle cell disease or thalassemia to speak to their medical or nursing team about providing a blood sample to NHS Blood and Transplant via their local transfusion laboratories to be genotyped.”
Additional information on this initiative can be found at www.nhsbt.nhs.uk/extendedbloodgrouptesting. ![]()

Photo by Juan D. Alfonso
NHS Blood and Transplant (NHSBT) has announced an initiative to provide more detailed blood-group typing for patients with hemoglobinopathies, with the goal of enabling better-matched and potentially safer transfusions.
The typing will detect Rh variant blood groups, which need to be considered when planning transfusions.
Previously, typing to this level was only possible through reference laboratories using complex genotyping methods.
NHSBT is offering the testing at no extra cost to hospitals in England until the end of June 2016.
The initiative involves routinely testing for the RHD and RHCE variants most commonly found in patients with hemoglobinopathies. NHSBT will also test genes for the blood groups K, k, Kpa, Kpb, Jsa, Jsb, Jka, Jkb, Fya, Fyb, Fy (GATA), M, N, S, s, U, Doa, and Dob.
Unlike older methods, this testing can be performed in patients who have recently received blood.
NHSBT said this initiative will enable the creation of a database of genotyped blood details for patients with hemoglobinopathies.
Extended blood type information and fast access to the database could potentially enable safer blood transfusions for these patients, who may need numerous transfusions during their lifetime and may move between hospitals.
NHSBT said it has received more than 2500 blood samples thus far. The results are processed centrally by NHSBT at the International Blood Group Reference Laboratory in Filton and are securely stored.
Patients’ test results will be accessible to the teams involved in the patients’ care.
“Patients taking part can now potentially receive more finely matched blood if we know not just their blood group but whether they have a variant Rh type,” said Sara Trompeter, MB ChB, a consultant hematologist for NHSBT.
“And there will also be greater safety and likelihood of getting matched blood in an emergency, as their records will be held centrally and can be accessed by blood banks in local hospitals. We would urge all patients with hemoglobin disorders such as sickle cell disease or thalassemia to speak to their medical or nursing team about providing a blood sample to NHS Blood and Transplant via their local transfusion laboratories to be genotyped.”
Additional information on this initiative can be found at www.nhsbt.nhs.uk/extendedbloodgrouptesting. ![]()
Proper hydroxyurea dose tied to better survival in sickle cell anemia
Adults with sickle cell disease who received recommended doses of hydroxyurea had higher fetal hemoglobin (HbF) levels, less organ dysfunction, and improved survival, compared with those who did receive recommended hydroxyurea doses, according to researchers.
“Our data suggest that even moderate increases, and not necessarily maximum HbF induction, may improve survival in patients with sickle cell anemia,” wrote Dr. Courtney D. Fitzhugh, assistant clinical investigator in the Laboratory of Sickle Mortality Prevention at the National Heart, Lung, and Blood Institute, Bethesda, Md., and her colleagues (PLoS One. 2015 Nov 17; doi:10.1371/journal.pone.0141706).
From 2001 to 2010, 383 patients with sickle cell disease underwent data clinical, laboratory, and echocardiographic evaluations every 2 years during a median follow-up of 2.6 years (range, 0.1-11.7).
In total, 59 patients died, and the median age at death was 46 years for men and 44.5 for women. Deceased subjects had lower fetal hemoglobin (P = .0044), were less likely to have taken hydroxyurea (56% vs. 68%, P = .040), and had a smaller proportion who were prescribed hydroxyurea within the recommended dose range (29% vs. 46%, P = .0039). Study participants who received a dose between 15 and 35 mg/kg/day more likely survived than those who never took hydroxyurea (P = .005). To assess the impact of hydroxyurea-induced HbF on organ injury, the study compared laboratory values from the highest and lowest HbF quartiles. For the lowest HbF quartile, alkaline phosphatase, a marker of organ damage, was consistently lower. “Because organ dysfunction may limit dosing, and hydroxyurea may not reverse severe tissue injury, we recommend treatment before organ damage occurs,” the researchers wrote.
Dr. Fitzhugh reported having no disclosures.
Adults with sickle cell disease who received recommended doses of hydroxyurea had higher fetal hemoglobin (HbF) levels, less organ dysfunction, and improved survival, compared with those who did receive recommended hydroxyurea doses, according to researchers.
“Our data suggest that even moderate increases, and not necessarily maximum HbF induction, may improve survival in patients with sickle cell anemia,” wrote Dr. Courtney D. Fitzhugh, assistant clinical investigator in the Laboratory of Sickle Mortality Prevention at the National Heart, Lung, and Blood Institute, Bethesda, Md., and her colleagues (PLoS One. 2015 Nov 17; doi:10.1371/journal.pone.0141706).
From 2001 to 2010, 383 patients with sickle cell disease underwent data clinical, laboratory, and echocardiographic evaluations every 2 years during a median follow-up of 2.6 years (range, 0.1-11.7).
In total, 59 patients died, and the median age at death was 46 years for men and 44.5 for women. Deceased subjects had lower fetal hemoglobin (P = .0044), were less likely to have taken hydroxyurea (56% vs. 68%, P = .040), and had a smaller proportion who were prescribed hydroxyurea within the recommended dose range (29% vs. 46%, P = .0039). Study participants who received a dose between 15 and 35 mg/kg/day more likely survived than those who never took hydroxyurea (P = .005). To assess the impact of hydroxyurea-induced HbF on organ injury, the study compared laboratory values from the highest and lowest HbF quartiles. For the lowest HbF quartile, alkaline phosphatase, a marker of organ damage, was consistently lower. “Because organ dysfunction may limit dosing, and hydroxyurea may not reverse severe tissue injury, we recommend treatment before organ damage occurs,” the researchers wrote.
Dr. Fitzhugh reported having no disclosures.
Adults with sickle cell disease who received recommended doses of hydroxyurea had higher fetal hemoglobin (HbF) levels, less organ dysfunction, and improved survival, compared with those who did receive recommended hydroxyurea doses, according to researchers.
“Our data suggest that even moderate increases, and not necessarily maximum HbF induction, may improve survival in patients with sickle cell anemia,” wrote Dr. Courtney D. Fitzhugh, assistant clinical investigator in the Laboratory of Sickle Mortality Prevention at the National Heart, Lung, and Blood Institute, Bethesda, Md., and her colleagues (PLoS One. 2015 Nov 17; doi:10.1371/journal.pone.0141706).
From 2001 to 2010, 383 patients with sickle cell disease underwent data clinical, laboratory, and echocardiographic evaluations every 2 years during a median follow-up of 2.6 years (range, 0.1-11.7).
In total, 59 patients died, and the median age at death was 46 years for men and 44.5 for women. Deceased subjects had lower fetal hemoglobin (P = .0044), were less likely to have taken hydroxyurea (56% vs. 68%, P = .040), and had a smaller proportion who were prescribed hydroxyurea within the recommended dose range (29% vs. 46%, P = .0039). Study participants who received a dose between 15 and 35 mg/kg/day more likely survived than those who never took hydroxyurea (P = .005). To assess the impact of hydroxyurea-induced HbF on organ injury, the study compared laboratory values from the highest and lowest HbF quartiles. For the lowest HbF quartile, alkaline phosphatase, a marker of organ damage, was consistently lower. “Because organ dysfunction may limit dosing, and hydroxyurea may not reverse severe tissue injury, we recommend treatment before organ damage occurs,” the researchers wrote.
Dr. Fitzhugh reported having no disclosures.
FROM PLOS ONE
Key clinical point: Proper hydroxyurea dose in adults with sickle cell anemia was linked to higher fetal hemoglobin levels, less organ dysfunction, and improved survival.
Major finding: Patients in the highest fetal hemoglobin quartiles had higher rates of survival, and 75% of patients in the highest quartile received recommended hydroxyurea doses, compared with 18% in the lowest quartile.
Data source: From 2001 to 2010, 383 patients with sickle cell disease underwent data clinical, laboratory, and echocardiographic evaluations at enrollment and every two years subsequently.
Disclosures: Dr. Fitzhugh reported having no disclosures.
Converting hemoglobin to fetal-type state

A pair of transcription factors repress the expression of fetal hemoglobin and might therefore be targets for the treatment of hemoglobinopathies, according to research published in Science.
Previous studies have indicated that hemoglobinopathies may be treated by inducing fetal-type hemoglobin.
However, researchers have been unable to achieve this because they don’t fully understand the factors that influence adult hemoglobin, including those that repress fetal hemoglobin.
Takeshi Masuda, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues suspected that the transcription factor LRF might play a role in the differentiation between hemoglobin types.
To test this theory, the team knocked out the gene that encodes LRF, ZBTB7A, in mice.
This boosted the expression of genes known to play a role in the production of fetal-type hemoglobin but not adult-type hemoglobin. Knocking out ZBTB7A in human cells produced similar results.
The researchers said LRF/ZBTB7A occupies fetal γ-globin genes and maintains the nucleosome density necessary for γ-globin gene silencing in adults.
They also discovered that LRF represses the expression of fetal-type hemoglobin through a NuRD repressor complex independent of BCL11A, a transcription factor already known to repress fetal-type hemoglobin.
However, in mice with both ZBTB7A and BCL11A knocked out, fetal-type hemoglobin represented a greater percentage of total hemoglobin (91% to 94%) than when either gene was knocked out alone.
Therefore, the researchers believe that therapies targeting the 2 proteins these genes express—LRF and BCL11A—may offer a viable way to induce fetal-type hemoglobin in patients with hemoglobinopathies. ![]()

A pair of transcription factors repress the expression of fetal hemoglobin and might therefore be targets for the treatment of hemoglobinopathies, according to research published in Science.
Previous studies have indicated that hemoglobinopathies may be treated by inducing fetal-type hemoglobin.
However, researchers have been unable to achieve this because they don’t fully understand the factors that influence adult hemoglobin, including those that repress fetal hemoglobin.
Takeshi Masuda, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues suspected that the transcription factor LRF might play a role in the differentiation between hemoglobin types.
To test this theory, the team knocked out the gene that encodes LRF, ZBTB7A, in mice.
This boosted the expression of genes known to play a role in the production of fetal-type hemoglobin but not adult-type hemoglobin. Knocking out ZBTB7A in human cells produced similar results.
The researchers said LRF/ZBTB7A occupies fetal γ-globin genes and maintains the nucleosome density necessary for γ-globin gene silencing in adults.
They also discovered that LRF represses the expression of fetal-type hemoglobin through a NuRD repressor complex independent of BCL11A, a transcription factor already known to repress fetal-type hemoglobin.
However, in mice with both ZBTB7A and BCL11A knocked out, fetal-type hemoglobin represented a greater percentage of total hemoglobin (91% to 94%) than when either gene was knocked out alone.
Therefore, the researchers believe that therapies targeting the 2 proteins these genes express—LRF and BCL11A—may offer a viable way to induce fetal-type hemoglobin in patients with hemoglobinopathies. ![]()

A pair of transcription factors repress the expression of fetal hemoglobin and might therefore be targets for the treatment of hemoglobinopathies, according to research published in Science.
Previous studies have indicated that hemoglobinopathies may be treated by inducing fetal-type hemoglobin.
However, researchers have been unable to achieve this because they don’t fully understand the factors that influence adult hemoglobin, including those that repress fetal hemoglobin.
Takeshi Masuda, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues suspected that the transcription factor LRF might play a role in the differentiation between hemoglobin types.
To test this theory, the team knocked out the gene that encodes LRF, ZBTB7A, in mice.
This boosted the expression of genes known to play a role in the production of fetal-type hemoglobin but not adult-type hemoglobin. Knocking out ZBTB7A in human cells produced similar results.
The researchers said LRF/ZBTB7A occupies fetal γ-globin genes and maintains the nucleosome density necessary for γ-globin gene silencing in adults.
They also discovered that LRF represses the expression of fetal-type hemoglobin through a NuRD repressor complex independent of BCL11A, a transcription factor already known to repress fetal-type hemoglobin.
However, in mice with both ZBTB7A and BCL11A knocked out, fetal-type hemoglobin represented a greater percentage of total hemoglobin (91% to 94%) than when either gene was knocked out alone.
Therefore, the researchers believe that therapies targeting the 2 proteins these genes express—LRF and BCL11A—may offer a viable way to induce fetal-type hemoglobin in patients with hemoglobinopathies. ![]()
Blocking two targets boosted fetal hemoglobin expression
Two distinct proteins appear to control the switch from fetal to adult globin, based on studies performed in a humanized mouse model and human cells. The findings suggest therapies that target both proteins might induce a fetal-type globin state, which could prove therapeutically useful in individuals with human hemoglobinopathies such as sickle cell disease and thalassemia.
The leukemia/lymphoma-related factor (LRF) and B-cell lymphoma/leukemia 11A (BCL11A) are independently involved in the switch, and blocking their production may turn on fetal globin expression, Takeshi Masuda, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and his colleagues report (SCIENCE. 2015 Jan 15;351[6270]:285-9)
Using a humanized mouse model, the researchers knocked out the ZBTB7A gene, which is responsible for producing LRF. This action boosted the expression of genes that control fetal but not adult-type hemoglobin. Knocking out the gene in human cells also resulted in an increase in fetal hemoglobin proteins.
The researchers then examined BCL11A, which is involved with fetal hemoglobin but does not suppress it. When genes were knocked out for both ZBTB7A and BCL11A in the mice, fetal hemoglobin represented a 91%-94% greater percentage of total hemoglobin than when either gene alone was knocked out.
The research was supported by awards and/or grants from the National Institute of Diabetes and Digestive and Kidney Disease, the Doris Duke Charitable Foundation, the National Institutes of Health, and the American Society of Hematology. Dr. Masuda, along with two other study authors, is a contributor to a patent application filed on behalf of Brigham and Women’s Hospital related to therapeutic targeting of the pathways.
Click here to read the study at Science.
Two distinct proteins appear to control the switch from fetal to adult globin, based on studies performed in a humanized mouse model and human cells. The findings suggest therapies that target both proteins might induce a fetal-type globin state, which could prove therapeutically useful in individuals with human hemoglobinopathies such as sickle cell disease and thalassemia.
The leukemia/lymphoma-related factor (LRF) and B-cell lymphoma/leukemia 11A (BCL11A) are independently involved in the switch, and blocking their production may turn on fetal globin expression, Takeshi Masuda, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and his colleagues report (SCIENCE. 2015 Jan 15;351[6270]:285-9)
Using a humanized mouse model, the researchers knocked out the ZBTB7A gene, which is responsible for producing LRF. This action boosted the expression of genes that control fetal but not adult-type hemoglobin. Knocking out the gene in human cells also resulted in an increase in fetal hemoglobin proteins.
The researchers then examined BCL11A, which is involved with fetal hemoglobin but does not suppress it. When genes were knocked out for both ZBTB7A and BCL11A in the mice, fetal hemoglobin represented a 91%-94% greater percentage of total hemoglobin than when either gene alone was knocked out.
The research was supported by awards and/or grants from the National Institute of Diabetes and Digestive and Kidney Disease, the Doris Duke Charitable Foundation, the National Institutes of Health, and the American Society of Hematology. Dr. Masuda, along with two other study authors, is a contributor to a patent application filed on behalf of Brigham and Women’s Hospital related to therapeutic targeting of the pathways.
Click here to read the study at Science.
Two distinct proteins appear to control the switch from fetal to adult globin, based on studies performed in a humanized mouse model and human cells. The findings suggest therapies that target both proteins might induce a fetal-type globin state, which could prove therapeutically useful in individuals with human hemoglobinopathies such as sickle cell disease and thalassemia.
The leukemia/lymphoma-related factor (LRF) and B-cell lymphoma/leukemia 11A (BCL11A) are independently involved in the switch, and blocking their production may turn on fetal globin expression, Takeshi Masuda, Ph.D., of Brigham and Women’s Hospital and Harvard Medical School, Boston, and his colleagues report (SCIENCE. 2015 Jan 15;351[6270]:285-9)
Using a humanized mouse model, the researchers knocked out the ZBTB7A gene, which is responsible for producing LRF. This action boosted the expression of genes that control fetal but not adult-type hemoglobin. Knocking out the gene in human cells also resulted in an increase in fetal hemoglobin proteins.
The researchers then examined BCL11A, which is involved with fetal hemoglobin but does not suppress it. When genes were knocked out for both ZBTB7A and BCL11A in the mice, fetal hemoglobin represented a 91%-94% greater percentage of total hemoglobin than when either gene alone was knocked out.
The research was supported by awards and/or grants from the National Institute of Diabetes and Digestive and Kidney Disease, the Doris Duke Charitable Foundation, the National Institutes of Health, and the American Society of Hematology. Dr. Masuda, along with two other study authors, is a contributor to a patent application filed on behalf of Brigham and Women’s Hospital related to therapeutic targeting of the pathways.
Click here to read the study at Science.
FROM SCIENCE
Kinase could be therapeutic target for Fanconi anemia

The protein kinase CHK1 may be a therapeutic target for Fanconi anemia (FA), according to researchers.
They studied induced pluripotent stem cells (iPSCs) derived from FA patients and found the FA DNA repair pathway was essential for the cells’ proliferation and survival.
The team also discovered that CHK1 played a “crucial” role in iPSCs’ sensitivity to accrued DNA damage, and inhibiting CHK1 allowed FA-deficient iPSCs to grow
normally.
The team relayed these findings in Stem Cell Reports.
“This study provides an experimental platform to test new therapies that could prevent pre- and post-natal Fanconi anemia conditions, which have no cure and limited treatment options,” said study author Susanne Wells, PhD, of the Cincinnati Children’s Hospital Medical Center in Ohio.
“Our findings also raise a number of important questions, so there is a lot more to be done.”
For this study, Dr Wells and her colleagues used iPSCs reprogrammed from mature skin and connective tissue cells donated by FA patients. The cells had a defective FA DNA repair pathway.
The researchers studied the iPSCs in culture and injected them into humanized mouse models, monitoring their genetic, molecular, and developmental progression.
Even with defective FA DNA repair, the iPSCs retained their ability to transform into different tissues, and humanized mice injected with the defective cells started to form teratomas.
However, the DNA repair defect started to kill off the iPSCs by blocking cell division and causing apoptosis.
The researchers noticed that CHK1, which serves as a DNA regulatory checkpoint during cell division, was hyperactive in the iPSCs, which hastened their death.
So the team used pharmacologic inhibitors of CHK1 to block the hyperactive enzyme at a critical stage of the stem cell cycle. This allowed them to override what are usually unfixable errors in the FA repair pathway.
After targeted treatment, FA-pathway-deficient iPSCs resumed dividing and expanding normally.
The researchers said that, to their surprise, the resumption of cell growth occurred without what they had expected to be massive chromosome abnormalities. Because of this, they speculate that a compensating DNA repair process is engaged in the reinvigorated cells.
Because this unidentified repair process may also rescue the DNA repair defect in the different tissue types affected by FA, Dr Wells and her colleagues believe their study may point to an approach that treats all clinical manifestations of the disease, including anemia and cancer.
“A key question for us is, ‘What type of DNA repair kicks in under these conditions, and is it error-free or error-prone?’” Dr Wells explained. “A novel mode of emergency DNA repair might indeed be discovered in the [iPSCs]. We believe some type of compensatory DNA repair must be driven by CHK1 inhibition when cells have FA pathway loss. Otherwise, the cells would have died off very quickly.”
The researchers plan to follow up this study with additional testing in humanized and genetic mouse models. They said they will attempt to improve embryonic development and post-birth fitness in FA-pathway-deficient mice with timed application of a CHK1 inhibitor.
The team will monitor the mice as they age and use genetic sequencing to screen for disease-causing mutations. And they will look for evidence of a DNA repair process (either novel or existing) in the FA-deficient mice. ![]()

The protein kinase CHK1 may be a therapeutic target for Fanconi anemia (FA), according to researchers.
They studied induced pluripotent stem cells (iPSCs) derived from FA patients and found the FA DNA repair pathway was essential for the cells’ proliferation and survival.
The team also discovered that CHK1 played a “crucial” role in iPSCs’ sensitivity to accrued DNA damage, and inhibiting CHK1 allowed FA-deficient iPSCs to grow
normally.
The team relayed these findings in Stem Cell Reports.
“This study provides an experimental platform to test new therapies that could prevent pre- and post-natal Fanconi anemia conditions, which have no cure and limited treatment options,” said study author Susanne Wells, PhD, of the Cincinnati Children’s Hospital Medical Center in Ohio.
“Our findings also raise a number of important questions, so there is a lot more to be done.”
For this study, Dr Wells and her colleagues used iPSCs reprogrammed from mature skin and connective tissue cells donated by FA patients. The cells had a defective FA DNA repair pathway.
The researchers studied the iPSCs in culture and injected them into humanized mouse models, monitoring their genetic, molecular, and developmental progression.
Even with defective FA DNA repair, the iPSCs retained their ability to transform into different tissues, and humanized mice injected with the defective cells started to form teratomas.
However, the DNA repair defect started to kill off the iPSCs by blocking cell division and causing apoptosis.
The researchers noticed that CHK1, which serves as a DNA regulatory checkpoint during cell division, was hyperactive in the iPSCs, which hastened their death.
So the team used pharmacologic inhibitors of CHK1 to block the hyperactive enzyme at a critical stage of the stem cell cycle. This allowed them to override what are usually unfixable errors in the FA repair pathway.
After targeted treatment, FA-pathway-deficient iPSCs resumed dividing and expanding normally.
The researchers said that, to their surprise, the resumption of cell growth occurred without what they had expected to be massive chromosome abnormalities. Because of this, they speculate that a compensating DNA repair process is engaged in the reinvigorated cells.
Because this unidentified repair process may also rescue the DNA repair defect in the different tissue types affected by FA, Dr Wells and her colleagues believe their study may point to an approach that treats all clinical manifestations of the disease, including anemia and cancer.
“A key question for us is, ‘What type of DNA repair kicks in under these conditions, and is it error-free or error-prone?’” Dr Wells explained. “A novel mode of emergency DNA repair might indeed be discovered in the [iPSCs]. We believe some type of compensatory DNA repair must be driven by CHK1 inhibition when cells have FA pathway loss. Otherwise, the cells would have died off very quickly.”
The researchers plan to follow up this study with additional testing in humanized and genetic mouse models. They said they will attempt to improve embryonic development and post-birth fitness in FA-pathway-deficient mice with timed application of a CHK1 inhibitor.
The team will monitor the mice as they age and use genetic sequencing to screen for disease-causing mutations. And they will look for evidence of a DNA repair process (either novel or existing) in the FA-deficient mice. ![]()

The protein kinase CHK1 may be a therapeutic target for Fanconi anemia (FA), according to researchers.
They studied induced pluripotent stem cells (iPSCs) derived from FA patients and found the FA DNA repair pathway was essential for the cells’ proliferation and survival.
The team also discovered that CHK1 played a “crucial” role in iPSCs’ sensitivity to accrued DNA damage, and inhibiting CHK1 allowed FA-deficient iPSCs to grow
normally.
The team relayed these findings in Stem Cell Reports.
“This study provides an experimental platform to test new therapies that could prevent pre- and post-natal Fanconi anemia conditions, which have no cure and limited treatment options,” said study author Susanne Wells, PhD, of the Cincinnati Children’s Hospital Medical Center in Ohio.
“Our findings also raise a number of important questions, so there is a lot more to be done.”
For this study, Dr Wells and her colleagues used iPSCs reprogrammed from mature skin and connective tissue cells donated by FA patients. The cells had a defective FA DNA repair pathway.
The researchers studied the iPSCs in culture and injected them into humanized mouse models, monitoring their genetic, molecular, and developmental progression.
Even with defective FA DNA repair, the iPSCs retained their ability to transform into different tissues, and humanized mice injected with the defective cells started to form teratomas.
However, the DNA repair defect started to kill off the iPSCs by blocking cell division and causing apoptosis.
The researchers noticed that CHK1, which serves as a DNA regulatory checkpoint during cell division, was hyperactive in the iPSCs, which hastened their death.
So the team used pharmacologic inhibitors of CHK1 to block the hyperactive enzyme at a critical stage of the stem cell cycle. This allowed them to override what are usually unfixable errors in the FA repair pathway.
After targeted treatment, FA-pathway-deficient iPSCs resumed dividing and expanding normally.
The researchers said that, to their surprise, the resumption of cell growth occurred without what they had expected to be massive chromosome abnormalities. Because of this, they speculate that a compensating DNA repair process is engaged in the reinvigorated cells.
Because this unidentified repair process may also rescue the DNA repair defect in the different tissue types affected by FA, Dr Wells and her colleagues believe their study may point to an approach that treats all clinical manifestations of the disease, including anemia and cancer.
“A key question for us is, ‘What type of DNA repair kicks in under these conditions, and is it error-free or error-prone?’” Dr Wells explained. “A novel mode of emergency DNA repair might indeed be discovered in the [iPSCs]. We believe some type of compensatory DNA repair must be driven by CHK1 inhibition when cells have FA pathway loss. Otherwise, the cells would have died off very quickly.”
The researchers plan to follow up this study with additional testing in humanized and genetic mouse models. They said they will attempt to improve embryonic development and post-birth fitness in FA-pathway-deficient mice with timed application of a CHK1 inhibitor.
The team will monitor the mice as they age and use genetic sequencing to screen for disease-causing mutations. And they will look for evidence of a DNA repair process (either novel or existing) in the FA-deficient mice. ![]()
Predicting transformation from MDS to AML

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()
HSPCs shape their own environment, team says

in the bone marrow
New research has revealed a mechanism through which hematopoietic stem and progenitor cells (HSPCs) control both their own proliferation and the characteristics of the niche that houses them.
Researchers detected high expression of the protein E-selectin ligand-1 (ESL-1) in HSPCs and also found that ESL-1 controls HSPCs’ production of the cytokine TGF-β.
The team said this is important because TGF-β has antiproliferative properties and is essential for impeding the loss of HSPCs in some diseases, such as some types of anemia.
The researchers also showed that HSPCs lacking ESL-1 are resistant to chemotherapeutic and cytotoxic agents.
These results suggest ESL-1 is a potential target for therapies aimed at improving bone marrow regeneration after chemotherapy or for expanding the HSPC population in preparation for donation.
Magdalena Leiva, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues reported these findings in Nature Communications.
The researchers first found that ESL-1 deficiency causes HSPC quiescence and expansion, and elevated TGF-β causes quiescence in the absence of ESL-1. In addition, ESL-1 controls HSPC proliferation independently of E-selectin, and HSPCs are a relevant source of TGF-β.
The team also discovered that ESL-1 exerts local effects on distinct cell populations in the stromal niche. They found that hematopoietic-borne ESL-1 can control HSPC proliferation directly through cytokine secretion, and/or indirectly through repressive effects on supportive niche cells.
According to Dr Leiva, this finding opens the path to new therapies “that use genetically modified stem cells to treat hematological diseases, such as certain types of leukemia, in which the hematopoietic niche and HSPCs are very affected.”
The researchers made these discoveries by analyzing the bone marrow of mice deficient in ESL-1. In the absence of ESL-1, HSPCs proliferated less and were therefore of superior quality and more suitable for potential therapeutic applications, the team found.
“We see that these cells are resistant to processes associated with bone marrow damage, such as cell death triggered by cytotoxic agents,” Dr Leiva said.
She and her colleagues found that stem cells lacking ESL-1 were resistant to the deleterious effects of 5-fluorouracil and hydroxyurea. They said this suggests ESL-1 is a possible therapeutic target for improved regeneration of the bone marrow during chemotherapy. ![]()

in the bone marrow
New research has revealed a mechanism through which hematopoietic stem and progenitor cells (HSPCs) control both their own proliferation and the characteristics of the niche that houses them.
Researchers detected high expression of the protein E-selectin ligand-1 (ESL-1) in HSPCs and also found that ESL-1 controls HSPCs’ production of the cytokine TGF-β.
The team said this is important because TGF-β has antiproliferative properties and is essential for impeding the loss of HSPCs in some diseases, such as some types of anemia.
The researchers also showed that HSPCs lacking ESL-1 are resistant to chemotherapeutic and cytotoxic agents.
These results suggest ESL-1 is a potential target for therapies aimed at improving bone marrow regeneration after chemotherapy or for expanding the HSPC population in preparation for donation.
Magdalena Leiva, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues reported these findings in Nature Communications.
The researchers first found that ESL-1 deficiency causes HSPC quiescence and expansion, and elevated TGF-β causes quiescence in the absence of ESL-1. In addition, ESL-1 controls HSPC proliferation independently of E-selectin, and HSPCs are a relevant source of TGF-β.
The team also discovered that ESL-1 exerts local effects on distinct cell populations in the stromal niche. They found that hematopoietic-borne ESL-1 can control HSPC proliferation directly through cytokine secretion, and/or indirectly through repressive effects on supportive niche cells.
According to Dr Leiva, this finding opens the path to new therapies “that use genetically modified stem cells to treat hematological diseases, such as certain types of leukemia, in which the hematopoietic niche and HSPCs are very affected.”
The researchers made these discoveries by analyzing the bone marrow of mice deficient in ESL-1. In the absence of ESL-1, HSPCs proliferated less and were therefore of superior quality and more suitable for potential therapeutic applications, the team found.
“We see that these cells are resistant to processes associated with bone marrow damage, such as cell death triggered by cytotoxic agents,” Dr Leiva said.
She and her colleagues found that stem cells lacking ESL-1 were resistant to the deleterious effects of 5-fluorouracil and hydroxyurea. They said this suggests ESL-1 is a possible therapeutic target for improved regeneration of the bone marrow during chemotherapy. ![]()

in the bone marrow
New research has revealed a mechanism through which hematopoietic stem and progenitor cells (HSPCs) control both their own proliferation and the characteristics of the niche that houses them.
Researchers detected high expression of the protein E-selectin ligand-1 (ESL-1) in HSPCs and also found that ESL-1 controls HSPCs’ production of the cytokine TGF-β.
The team said this is important because TGF-β has antiproliferative properties and is essential for impeding the loss of HSPCs in some diseases, such as some types of anemia.
The researchers also showed that HSPCs lacking ESL-1 are resistant to chemotherapeutic and cytotoxic agents.
These results suggest ESL-1 is a potential target for therapies aimed at improving bone marrow regeneration after chemotherapy or for expanding the HSPC population in preparation for donation.
Magdalena Leiva, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues reported these findings in Nature Communications.
The researchers first found that ESL-1 deficiency causes HSPC quiescence and expansion, and elevated TGF-β causes quiescence in the absence of ESL-1. In addition, ESL-1 controls HSPC proliferation independently of E-selectin, and HSPCs are a relevant source of TGF-β.
The team also discovered that ESL-1 exerts local effects on distinct cell populations in the stromal niche. They found that hematopoietic-borne ESL-1 can control HSPC proliferation directly through cytokine secretion, and/or indirectly through repressive effects on supportive niche cells.
According to Dr Leiva, this finding opens the path to new therapies “that use genetically modified stem cells to treat hematological diseases, such as certain types of leukemia, in which the hematopoietic niche and HSPCs are very affected.”
The researchers made these discoveries by analyzing the bone marrow of mice deficient in ESL-1. In the absence of ESL-1, HSPCs proliferated less and were therefore of superior quality and more suitable for potential therapeutic applications, the team found.
“We see that these cells are resistant to processes associated with bone marrow damage, such as cell death triggered by cytotoxic agents,” Dr Leiva said.
She and her colleagues found that stem cells lacking ESL-1 were resistant to the deleterious effects of 5-fluorouracil and hydroxyurea. They said this suggests ESL-1 is a possible therapeutic target for improved regeneration of the bone marrow during chemotherapy. ![]()
Drug granted orphan designation for SCD

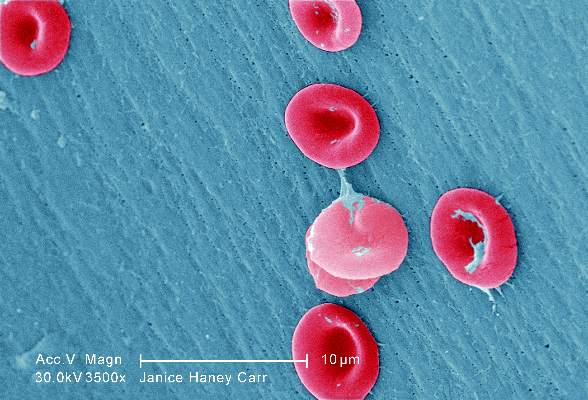
red blood cells
Image by Graham Beards
The US Food and Drug Administration (FDA) has granted orphan drug designation for the small molecule GBT440 to treat patients with sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
“Receiving orphan drug designation, along with the previously announced fast track designation, are important milestones in our regulatory strategy for GBT440 and highlight the FDA’s agreement that the SCD community faces a critical need for new treatments,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc., the company developing GBT440.
The FDA grants orphan designation to drugs that are intended to treat diseases or conditions affecting fewer than 200,000 patients in the US. The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
The FDA grants fast track designation to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need. Through the fast track program, a drug may be eligible for priority review and rolling review, and the company developing the drug may receive additional help from the FDA to expedite development.
GBT440 trial
Early results from an ongoing phase 1/2 study of GBT440 were presented at the 2015 ASH Annual Meeting last month (abstract 542*).
The trial, which includes healthy subjects and patients with SCD, is being conducted in 2 parts: part A (single-dose administration) and part B (multiple-dose administration, daily for 15 days in healthy subjects and 28 days in SCD patients).
As of November 20, 2015, 8 SCD patients completed part A, and 30 SCD patients had either completed or were ongoing in part B.
Of the 30 SCD patients, 16 patients completed 700 mg daily dosing and follow-up (12 on GBT440 and 4 on placebo), and 14 patients completed or were ongoing at 500 mg daily dosing and follow-up (10 on GBT440 and 4 on placebo). A cohort of SCD patients on 1000 mg per day for 28 days is currently enrolling.
Thus far, GBT440 treatment has conferred several improvements from baseline to day 28.
Hemoglobin increases were evident by day 4 of treatment. And the researchers observed absolute hemoglobin increases of 0.5 and 0.7 g/dL with GBT440 at 500 and 700 mg, respectively, compared with a 0.1 g/dL decrease with placebo.
The median reticulocyte count decreased by 31% and 37% with GBT440 at 500 and 700 mg, respectively, compared with a 7% increase with placebo, indicating that the hemoglobin rise is due to decreased hemolysis.
Median erythropoietin levels decreased by 9 and 18 mU/mL with GBT440 at 500 and 700 mg, respectively, compared with an increase of 28 mU/mL with placebo.
Median unconjugated bilirubin levels decrease by 31% and 43% with GBT440 at 500 mg and 700 mg, respectively, compared with an increase of 2% with placebo.
Median lactate dehydrogenase levels decreased by 20% and 12% with GBT440 at 500 and 700 mg, respectively, compared with a decrease of 7% with placebo.
Median sickle cell counts decreased by 56% and 46% with GBT440 at 500 and 700 mg, respectively, compared with a 14% increase with placebo.
The researchers noted high inter- and intra-patient variability in circulating sickle cell counts.
They said inflammatory soluble adhesion molecules for the 700 mg dose cohort showed promising trends in improvement. The median P-selectin decreased 19%, compared with an increase of 20% with placebo. And the median ICAM-1 decreased 6%, compared with an increase of 33% in placebo. Data for the 500 mg dose cohort has not yet been analyzed.
The researchers said pharmacokinetic data demonstrated linear and dose-proportional properties, with a half-life amenable to once-daily dosing.
And GBT440 was well tolerated over the 28 days of dosing. None of the SCD patients discontinued GBT440. The most common adverse event was headache, and there have been no serious adverse events thought to be drug-related.
“We continue to believe that GBT440 has the potential to become the first mechanism-based and disease-modifying therapeutic for this grievous disease and look forward to sharing full results from our phase 1/2 trial and potentially initiating a pivotal trial in adult patients with SCD in 2016,” Dr Love said. ![]()
*Data in the abstract differ from the presentation.

red blood cells
Image by Graham Beards
The US Food and Drug Administration (FDA) has granted orphan drug designation for the small molecule GBT440 to treat patients with sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
“Receiving orphan drug designation, along with the previously announced fast track designation, are important milestones in our regulatory strategy for GBT440 and highlight the FDA’s agreement that the SCD community faces a critical need for new treatments,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc., the company developing GBT440.
The FDA grants orphan designation to drugs that are intended to treat diseases or conditions affecting fewer than 200,000 patients in the US. The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
The FDA grants fast track designation to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need. Through the fast track program, a drug may be eligible for priority review and rolling review, and the company developing the drug may receive additional help from the FDA to expedite development.
GBT440 trial
Early results from an ongoing phase 1/2 study of GBT440 were presented at the 2015 ASH Annual Meeting last month (abstract 542*).
The trial, which includes healthy subjects and patients with SCD, is being conducted in 2 parts: part A (single-dose administration) and part B (multiple-dose administration, daily for 15 days in healthy subjects and 28 days in SCD patients).
As of November 20, 2015, 8 SCD patients completed part A, and 30 SCD patients had either completed or were ongoing in part B.
Of the 30 SCD patients, 16 patients completed 700 mg daily dosing and follow-up (12 on GBT440 and 4 on placebo), and 14 patients completed or were ongoing at 500 mg daily dosing and follow-up (10 on GBT440 and 4 on placebo). A cohort of SCD patients on 1000 mg per day for 28 days is currently enrolling.
Thus far, GBT440 treatment has conferred several improvements from baseline to day 28.
Hemoglobin increases were evident by day 4 of treatment. And the researchers observed absolute hemoglobin increases of 0.5 and 0.7 g/dL with GBT440 at 500 and 700 mg, respectively, compared with a 0.1 g/dL decrease with placebo.
The median reticulocyte count decreased by 31% and 37% with GBT440 at 500 and 700 mg, respectively, compared with a 7% increase with placebo, indicating that the hemoglobin rise is due to decreased hemolysis.
Median erythropoietin levels decreased by 9 and 18 mU/mL with GBT440 at 500 and 700 mg, respectively, compared with an increase of 28 mU/mL with placebo.
Median unconjugated bilirubin levels decrease by 31% and 43% with GBT440 at 500 mg and 700 mg, respectively, compared with an increase of 2% with placebo.
Median lactate dehydrogenase levels decreased by 20% and 12% with GBT440 at 500 and 700 mg, respectively, compared with a decrease of 7% with placebo.
Median sickle cell counts decreased by 56% and 46% with GBT440 at 500 and 700 mg, respectively, compared with a 14% increase with placebo.
The researchers noted high inter- and intra-patient variability in circulating sickle cell counts.
They said inflammatory soluble adhesion molecules for the 700 mg dose cohort showed promising trends in improvement. The median P-selectin decreased 19%, compared with an increase of 20% with placebo. And the median ICAM-1 decreased 6%, compared with an increase of 33% in placebo. Data for the 500 mg dose cohort has not yet been analyzed.
The researchers said pharmacokinetic data demonstrated linear and dose-proportional properties, with a half-life amenable to once-daily dosing.
And GBT440 was well tolerated over the 28 days of dosing. None of the SCD patients discontinued GBT440. The most common adverse event was headache, and there have been no serious adverse events thought to be drug-related.
“We continue to believe that GBT440 has the potential to become the first mechanism-based and disease-modifying therapeutic for this grievous disease and look forward to sharing full results from our phase 1/2 trial and potentially initiating a pivotal trial in adult patients with SCD in 2016,” Dr Love said. ![]()
*Data in the abstract differ from the presentation.

red blood cells
Image by Graham Beards
The US Food and Drug Administration (FDA) has granted orphan drug designation for the small molecule GBT440 to treat patients with sickle cell disease (SCD).
GBT440 is being developed as a potentially disease-modifying therapy for SCD. The drug works by increasing hemoglobin’s affinity for oxygen.
Since oxygenated sickle hemoglobin does not polymerize, it is believed that GBT440 blocks polymerization and the resultant sickling of red blood cells.
If GBT440 can restore normal hemoglobin function and improve oxygen delivery, the drug may be capable of modifying the progression of SCD.
“Receiving orphan drug designation, along with the previously announced fast track designation, are important milestones in our regulatory strategy for GBT440 and highlight the FDA’s agreement that the SCD community faces a critical need for new treatments,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc., the company developing GBT440.
The FDA grants orphan designation to drugs that are intended to treat diseases or conditions affecting fewer than 200,000 patients in the US. The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
The FDA grants fast track designation to facilitate and expedite the development and review of new drugs intended to treat serious or life-threatening conditions and address unmet medical need. Through the fast track program, a drug may be eligible for priority review and rolling review, and the company developing the drug may receive additional help from the FDA to expedite development.
GBT440 trial
Early results from an ongoing phase 1/2 study of GBT440 were presented at the 2015 ASH Annual Meeting last month (abstract 542*).
The trial, which includes healthy subjects and patients with SCD, is being conducted in 2 parts: part A (single-dose administration) and part B (multiple-dose administration, daily for 15 days in healthy subjects and 28 days in SCD patients).
As of November 20, 2015, 8 SCD patients completed part A, and 30 SCD patients had either completed or were ongoing in part B.
Of the 30 SCD patients, 16 patients completed 700 mg daily dosing and follow-up (12 on GBT440 and 4 on placebo), and 14 patients completed or were ongoing at 500 mg daily dosing and follow-up (10 on GBT440 and 4 on placebo). A cohort of SCD patients on 1000 mg per day for 28 days is currently enrolling.
Thus far, GBT440 treatment has conferred several improvements from baseline to day 28.
Hemoglobin increases were evident by day 4 of treatment. And the researchers observed absolute hemoglobin increases of 0.5 and 0.7 g/dL with GBT440 at 500 and 700 mg, respectively, compared with a 0.1 g/dL decrease with placebo.
The median reticulocyte count decreased by 31% and 37% with GBT440 at 500 and 700 mg, respectively, compared with a 7% increase with placebo, indicating that the hemoglobin rise is due to decreased hemolysis.
Median erythropoietin levels decreased by 9 and 18 mU/mL with GBT440 at 500 and 700 mg, respectively, compared with an increase of 28 mU/mL with placebo.
Median unconjugated bilirubin levels decrease by 31% and 43% with GBT440 at 500 mg and 700 mg, respectively, compared with an increase of 2% with placebo.
Median lactate dehydrogenase levels decreased by 20% and 12% with GBT440 at 500 and 700 mg, respectively, compared with a decrease of 7% with placebo.
Median sickle cell counts decreased by 56% and 46% with GBT440 at 500 and 700 mg, respectively, compared with a 14% increase with placebo.
The researchers noted high inter- and intra-patient variability in circulating sickle cell counts.
They said inflammatory soluble adhesion molecules for the 700 mg dose cohort showed promising trends in improvement. The median P-selectin decreased 19%, compared with an increase of 20% with placebo. And the median ICAM-1 decreased 6%, compared with an increase of 33% in placebo. Data for the 500 mg dose cohort has not yet been analyzed.
The researchers said pharmacokinetic data demonstrated linear and dose-proportional properties, with a half-life amenable to once-daily dosing.
And GBT440 was well tolerated over the 28 days of dosing. None of the SCD patients discontinued GBT440. The most common adverse event was headache, and there have been no serious adverse events thought to be drug-related.
“We continue to believe that GBT440 has the potential to become the first mechanism-based and disease-modifying therapeutic for this grievous disease and look forward to sharing full results from our phase 1/2 trial and potentially initiating a pivotal trial in adult patients with SCD in 2016,” Dr Love said. ![]()
*Data in the abstract differ from the presentation.
De novo mutation linked to FA subtype

with Fanconi anemia
Researchers say they have established the cause of a subtype of Fanconi anemia (FA)—a de novo mutation in 1 allele of RAD51, a gene responsible for repairing DNA damage.
The team made this discovery in a child with an FA-like syndrome who has healthy parents and a healthy sister.
“The particular mutation in this patient was a surprise to us,” said Patrick May, PhD, of the University of Luxembourg.
“It occurred only in 1 of the 2 RAD51 gene copies, which every person carries in the genome, but every RAD51 gene copy was normal in the child’s parents.”
Dr May and his colleagues described the mutation in Nature Communications.
Specifically, the researchers found a de novo g.41022153G>A; p.Ala293Thr (NM_002875) missense mutation in 1 allele of RAD51.
They said this heterozygous mutation causes a novel FA subtype, dubbed “FA-R,” which appears to be the first subtype of FA caused by a dominant-negative mutation.
The patient the researchers analyzed has microcephaly and mental retardation but has reached adulthood without the bone marrow failure and pediatric cancers typically observed in patients with FA.
Until this case, researchers believed that mutations leading to FA showed recessive inheritance and therefore had to be derived from both parents to lead to FA. Spontaneous mutations of the RAD51 gene like in this case had not been observed.
Dr May and his colleagues said their finding has implications for genetic counseling of families with a high risk for FA. Previously, people who wanted to have children but had relatives suffering from FA were screened for mutations in 1 of the 17 genes connected with the disease. Now, the risk of having a child with FA has to be recalculated.
“Furthermore, understanding this mutation teaches us more about how the RAD51 gene product protects the DNA and how disruptions of DNA repair may lead to leukemia and solid tumors,” Dr May said. “Of course, understanding the origins of human cancer will help us diagnose it with more confidence earlier and devise new therapies to prevent or mitigate it.” ![]()

with Fanconi anemia
Researchers say they have established the cause of a subtype of Fanconi anemia (FA)—a de novo mutation in 1 allele of RAD51, a gene responsible for repairing DNA damage.
The team made this discovery in a child with an FA-like syndrome who has healthy parents and a healthy sister.
“The particular mutation in this patient was a surprise to us,” said Patrick May, PhD, of the University of Luxembourg.
“It occurred only in 1 of the 2 RAD51 gene copies, which every person carries in the genome, but every RAD51 gene copy was normal in the child’s parents.”
Dr May and his colleagues described the mutation in Nature Communications.
Specifically, the researchers found a de novo g.41022153G>A; p.Ala293Thr (NM_002875) missense mutation in 1 allele of RAD51.
They said this heterozygous mutation causes a novel FA subtype, dubbed “FA-R,” which appears to be the first subtype of FA caused by a dominant-negative mutation.
The patient the researchers analyzed has microcephaly and mental retardation but has reached adulthood without the bone marrow failure and pediatric cancers typically observed in patients with FA.
Until this case, researchers believed that mutations leading to FA showed recessive inheritance and therefore had to be derived from both parents to lead to FA. Spontaneous mutations of the RAD51 gene like in this case had not been observed.
Dr May and his colleagues said their finding has implications for genetic counseling of families with a high risk for FA. Previously, people who wanted to have children but had relatives suffering from FA were screened for mutations in 1 of the 17 genes connected with the disease. Now, the risk of having a child with FA has to be recalculated.
“Furthermore, understanding this mutation teaches us more about how the RAD51 gene product protects the DNA and how disruptions of DNA repair may lead to leukemia and solid tumors,” Dr May said. “Of course, understanding the origins of human cancer will help us diagnose it with more confidence earlier and devise new therapies to prevent or mitigate it.” ![]()

with Fanconi anemia
Researchers say they have established the cause of a subtype of Fanconi anemia (FA)—a de novo mutation in 1 allele of RAD51, a gene responsible for repairing DNA damage.
The team made this discovery in a child with an FA-like syndrome who has healthy parents and a healthy sister.
“The particular mutation in this patient was a surprise to us,” said Patrick May, PhD, of the University of Luxembourg.
“It occurred only in 1 of the 2 RAD51 gene copies, which every person carries in the genome, but every RAD51 gene copy was normal in the child’s parents.”
Dr May and his colleagues described the mutation in Nature Communications.
Specifically, the researchers found a de novo g.41022153G>A; p.Ala293Thr (NM_002875) missense mutation in 1 allele of RAD51.
They said this heterozygous mutation causes a novel FA subtype, dubbed “FA-R,” which appears to be the first subtype of FA caused by a dominant-negative mutation.
The patient the researchers analyzed has microcephaly and mental retardation but has reached adulthood without the bone marrow failure and pediatric cancers typically observed in patients with FA.
Until this case, researchers believed that mutations leading to FA showed recessive inheritance and therefore had to be derived from both parents to lead to FA. Spontaneous mutations of the RAD51 gene like in this case had not been observed.
Dr May and his colleagues said their finding has implications for genetic counseling of families with a high risk for FA. Previously, people who wanted to have children but had relatives suffering from FA were screened for mutations in 1 of the 17 genes connected with the disease. Now, the risk of having a child with FA has to be recalculated.
“Furthermore, understanding this mutation teaches us more about how the RAD51 gene product protects the DNA and how disruptions of DNA repair may lead to leukemia and solid tumors,” Dr May said. “Of course, understanding the origins of human cancer will help us diagnose it with more confidence earlier and devise new therapies to prevent or mitigate it.”