User login
Statin may reduce vaso-occlusive pain in SCD

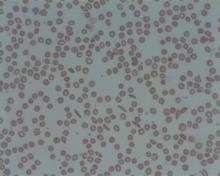
Photo courtesy of the CDC
ORLANDO, FL—In a small study, the cholesterol-lowering medication simvastatin reduced the frequency of vaso-occlusive pain in adults and children with sickle cell disease (SCD).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain after 3 months of treatment with simvastatin.
There was a slight overall decrease in the intensity of pain as well, but this was not statistically significant.
Still, investigators observed a decrease in biomarkers of inflammation and said the drug appeared to be safe for this patient population.
The team believes these preliminary data suggest the need to conduct a larger, randomized trial of simvastatin in SCD.
Carolyn C. Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California, presented the data at the 2015 ASH Annual Meeting (abstract 545).*
“Vaso-occlusive pain is a clinical hallmark and major cause of morbidity in sickle cell disease,” Dr Hoppe said. “Triggered by polymerization and hemolysis, vaso-occlusion involves multiple pathways.”
Similarly, although statins are best known for their cholesterol-inhibiting ability, they also inhibit oxidative stress and inflammation.
With this in mind, Dr Hoppe and her colleagues previously tested simvastatin in a phase 1 study of SCD patients who were 13 years of age or older.
The investigators found the safety profile to be acceptable, and they observed an improvement in biomarkers of inflammation. So they decided to carry out the current study.
This was a single-center, uncontrolled trial that enrolled SCD patients ages 10 and older. They received once-daily oral simvastatin (40 mg) for 3 months.
The primary outcome measure was the frequency and intensity of vaso-occlusive pain, as recorded by daily electronic pain diaries, before and after simvastatin treatment.
Clinical laboratory studies and plasma biomarkers were evaluated at baseline, at 0.5, 1, 2, and 3 months during treatment, as well as 1 month after the discontinuation of simvastatin.
Results
Nineteen patients completed the study. They had a mean age of 19 (range, 10-34), and 13 were female. Seventeen had HbSS genotype, and 2 had S/β0 thalassemia. Ten patients were receiving hydroxyurea.
The simvastatin adherence rate was 85%, and the adherence to using the daily pain diary was 73%.
Dr Hoppe said there were no new safety issues or drug-related adverse events in this trial. There was no myalgia or myopathy. One subject did experience transient facial swelling that may have been drug-related.
The patients’ total cholesterol decreased by 20% from baseline. There was a significant decrease in both LDL and HDL cholesterol (P<0.001 for both).
Creatinine kinase remained stable during treatment, as did hemoglobin levels.
Dr Hoppe noted that the study was not designed to include an assessment of fetal hemoglobin, so she and her colleagues did not have data on that measure for all the patients, but the team did observe an increase in fetal hemoglobin levels from baseline among the patients who were receiving hydroxyurea.
The investigators observed a decrease from baseline in markers of hemolysis—absolute reticulocyte count (P=0.006) and total bilirubin (P=0.02).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain from baseline (P=0.005) and a 10% decrease in the intensity of pain (which was not significant).
There was a 59% decrease in hsCRP (P=0.003), an 18% decrease in sE-selectin (P=0.01), a 5% decrease in sICAM (P=0.03), and a 17% decrease in VEGF (P=0.05). There was no significant effect on plasma nitric oxide metabolites, sVCAM1, or P-selectin levels.
“These results are basically preliminary data to give clinical support for a larger, randomized trial of simvastatin to assess its clinical efficacy in SCD,” Dr Hoppe concluded.
She reported receiving research funding and consultancy payments from Eli Lilly and Company, and another investigator involved in this study is an employee of Pharmacyclics LLC. ![]()
*Data in the abstract differ from the data presented.

Photo courtesy of the CDC
ORLANDO, FL—In a small study, the cholesterol-lowering medication simvastatin reduced the frequency of vaso-occlusive pain in adults and children with sickle cell disease (SCD).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain after 3 months of treatment with simvastatin.
There was a slight overall decrease in the intensity of pain as well, but this was not statistically significant.
Still, investigators observed a decrease in biomarkers of inflammation and said the drug appeared to be safe for this patient population.
The team believes these preliminary data suggest the need to conduct a larger, randomized trial of simvastatin in SCD.
Carolyn C. Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California, presented the data at the 2015 ASH Annual Meeting (abstract 545).*
“Vaso-occlusive pain is a clinical hallmark and major cause of morbidity in sickle cell disease,” Dr Hoppe said. “Triggered by polymerization and hemolysis, vaso-occlusion involves multiple pathways.”
Similarly, although statins are best known for their cholesterol-inhibiting ability, they also inhibit oxidative stress and inflammation.
With this in mind, Dr Hoppe and her colleagues previously tested simvastatin in a phase 1 study of SCD patients who were 13 years of age or older.
The investigators found the safety profile to be acceptable, and they observed an improvement in biomarkers of inflammation. So they decided to carry out the current study.
This was a single-center, uncontrolled trial that enrolled SCD patients ages 10 and older. They received once-daily oral simvastatin (40 mg) for 3 months.
The primary outcome measure was the frequency and intensity of vaso-occlusive pain, as recorded by daily electronic pain diaries, before and after simvastatin treatment.
Clinical laboratory studies and plasma biomarkers were evaluated at baseline, at 0.5, 1, 2, and 3 months during treatment, as well as 1 month after the discontinuation of simvastatin.
Results
Nineteen patients completed the study. They had a mean age of 19 (range, 10-34), and 13 were female. Seventeen had HbSS genotype, and 2 had S/β0 thalassemia. Ten patients were receiving hydroxyurea.
The simvastatin adherence rate was 85%, and the adherence to using the daily pain diary was 73%.
Dr Hoppe said there were no new safety issues or drug-related adverse events in this trial. There was no myalgia or myopathy. One subject did experience transient facial swelling that may have been drug-related.
The patients’ total cholesterol decreased by 20% from baseline. There was a significant decrease in both LDL and HDL cholesterol (P<0.001 for both).
Creatinine kinase remained stable during treatment, as did hemoglobin levels.
Dr Hoppe noted that the study was not designed to include an assessment of fetal hemoglobin, so she and her colleagues did not have data on that measure for all the patients, but the team did observe an increase in fetal hemoglobin levels from baseline among the patients who were receiving hydroxyurea.
The investigators observed a decrease from baseline in markers of hemolysis—absolute reticulocyte count (P=0.006) and total bilirubin (P=0.02).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain from baseline (P=0.005) and a 10% decrease in the intensity of pain (which was not significant).
There was a 59% decrease in hsCRP (P=0.003), an 18% decrease in sE-selectin (P=0.01), a 5% decrease in sICAM (P=0.03), and a 17% decrease in VEGF (P=0.05). There was no significant effect on plasma nitric oxide metabolites, sVCAM1, or P-selectin levels.
“These results are basically preliminary data to give clinical support for a larger, randomized trial of simvastatin to assess its clinical efficacy in SCD,” Dr Hoppe concluded.
She reported receiving research funding and consultancy payments from Eli Lilly and Company, and another investigator involved in this study is an employee of Pharmacyclics LLC. ![]()
*Data in the abstract differ from the data presented.

Photo courtesy of the CDC
ORLANDO, FL—In a small study, the cholesterol-lowering medication simvastatin reduced the frequency of vaso-occlusive pain in adults and children with sickle cell disease (SCD).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain after 3 months of treatment with simvastatin.
There was a slight overall decrease in the intensity of pain as well, but this was not statistically significant.
Still, investigators observed a decrease in biomarkers of inflammation and said the drug appeared to be safe for this patient population.
The team believes these preliminary data suggest the need to conduct a larger, randomized trial of simvastatin in SCD.
Carolyn C. Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California, presented the data at the 2015 ASH Annual Meeting (abstract 545).*
“Vaso-occlusive pain is a clinical hallmark and major cause of morbidity in sickle cell disease,” Dr Hoppe said. “Triggered by polymerization and hemolysis, vaso-occlusion involves multiple pathways.”
Similarly, although statins are best known for their cholesterol-inhibiting ability, they also inhibit oxidative stress and inflammation.
With this in mind, Dr Hoppe and her colleagues previously tested simvastatin in a phase 1 study of SCD patients who were 13 years of age or older.
The investigators found the safety profile to be acceptable, and they observed an improvement in biomarkers of inflammation. So they decided to carry out the current study.
This was a single-center, uncontrolled trial that enrolled SCD patients ages 10 and older. They received once-daily oral simvastatin (40 mg) for 3 months.
The primary outcome measure was the frequency and intensity of vaso-occlusive pain, as recorded by daily electronic pain diaries, before and after simvastatin treatment.
Clinical laboratory studies and plasma biomarkers were evaluated at baseline, at 0.5, 1, 2, and 3 months during treatment, as well as 1 month after the discontinuation of simvastatin.
Results
Nineteen patients completed the study. They had a mean age of 19 (range, 10-34), and 13 were female. Seventeen had HbSS genotype, and 2 had S/β0 thalassemia. Ten patients were receiving hydroxyurea.
The simvastatin adherence rate was 85%, and the adherence to using the daily pain diary was 73%.
Dr Hoppe said there were no new safety issues or drug-related adverse events in this trial. There was no myalgia or myopathy. One subject did experience transient facial swelling that may have been drug-related.
The patients’ total cholesterol decreased by 20% from baseline. There was a significant decrease in both LDL and HDL cholesterol (P<0.001 for both).
Creatinine kinase remained stable during treatment, as did hemoglobin levels.
Dr Hoppe noted that the study was not designed to include an assessment of fetal hemoglobin, so she and her colleagues did not have data on that measure for all the patients, but the team did observe an increase in fetal hemoglobin levels from baseline among the patients who were receiving hydroxyurea.
The investigators observed a decrease from baseline in markers of hemolysis—absolute reticulocyte count (P=0.006) and total bilirubin (P=0.02).
Overall, there was a 46% decrease in the frequency of vaso-occlusive pain from baseline (P=0.005) and a 10% decrease in the intensity of pain (which was not significant).
There was a 59% decrease in hsCRP (P=0.003), an 18% decrease in sE-selectin (P=0.01), a 5% decrease in sICAM (P=0.03), and a 17% decrease in VEGF (P=0.05). There was no significant effect on plasma nitric oxide metabolites, sVCAM1, or P-selectin levels.
“These results are basically preliminary data to give clinical support for a larger, randomized trial of simvastatin to assess its clinical efficacy in SCD,” Dr Hoppe concluded.
She reported receiving research funding and consultancy payments from Eli Lilly and Company, and another investigator involved in this study is an employee of Pharmacyclics LLC. ![]()
*Data in the abstract differ from the data presented.
Anemia tied to cognitive impairment

A population-based study conducted in Germany has suggested a link between anemia and mild cognitive impairment (MCI).
Researchers found that subjects with anemia, defined as hemoglobin <13 g/dL in men and <12 g/dL in women, performed worse on cognitive tests than their nonanemic peers.
And MCI occurred almost twice as often in subjects with anemia than in subjects with normal hemoglobin levels.
This study was published in the Journal of Alzheimer’s Disease.
About MCI
MCI represents an intermediate and possibly modifiable stage between normal cognitive aging and dementia. Although individuals with MCI have an increased risk of developing dementia or Alzheimer’s disease, they can also remain stable for many years or even revert to a cognitively normal state over time. This modifiable characteristic makes the concept of MCI a promising target in the prevention of dementia.
The following 4 criteria are used to diagnose MCI. First, subjects must report a decline in cognitive performance over the past 2 years. Second, they must show a cognitive impairment in objective cognitive tasks that is greater than one would expect taking their age and education into consideration.
Third, the impairment must not be as pronounced as in demented individuals since people with MCI can perform normal daily living activities or are only slightly impaired in carrying out complex instrumental functions. Fourth, the cognitive impairment has to be insufficient to fulfil criteria for dementia.
The concept of MCI distinguishes between amnestic MCI (aMCI) and non-amnestic MCI (naMCI). In the former, impairment in the memory domain is evident, most likely reflecting Alzheimer’s disease pathology. In the latter, impairment in non-memory domains is present, mainly reflecting vascular pathology but also frontotemporal dementia or dementia with Lewy bodies.
Study details
The Heinz Nixdorf Recall study is an observational, population-based, prospective study in which researchers examined 4814 subjects between 2000 and 2003. Subjects were 50 to 80 years of age and lived in the metropolitan Ruhr Area. Both genders were equally represented.
After 5 years, the researchers conducted a second examination with 92% of the subjects taking part. The publication includes cross-sectional results of the second examination.
First, 163 subjects with anemia and 3870 without anemia were included to compare their performance in all cognitive subtests.
The subjects took verbal memory tests, which were used to gauge immediate recall and delayed recall. They were also tested on executive functioning, which included problem-solving/speed of processing, verbal fluency, visual spatial organization, and the clock drawing test.
In the initial analysis, anemic subjects showed more pronounced cardiovascular risk profiles and lower cognitive performance in all administered cognitive subtests. After adjusting for age, anemic subjects showed a significantly lower performance in the immediate recall task (P=0.009) and the verbal fluency task (P=0.004).
Next, the researchers compared 579 subjects diagnosed with MCI—299 with aMCI and 280 with naMCI—to 1438 cognitively normal subjects to determine the association between anemia at follow-up and MCI.
The team found that MCI occurred more often in anemic than non-anemic subjects. The unadjusted odds ratio (OR) was 2.59 (P<0.001). The OR after adjustment for age, gender, and years of education was 2.15 (P=0.002).
In a third analysis, the researchers adjusted for the aforementioned variables as well as body mass index, high-sensitivity C-reactive protein, glomerular filtration rate, cholesterol, serum iron, hypertension, diabetes mellitus, history of coronary heart disease, history of stroke, history of cancer, APOE4, smoking, severe depressive symptoms, and use of antidepressants. The OR after adjustment for these factors was 1.92 (P=0.04).
Similar results were found for aMCI and naMCI. The researchers said this suggests that having a low hemoglobin level may contribute to cognitive impairment via different pathways.
The team believes that, overall, their study results indicate that anemia is associated with an increased risk of MCI independent of traditional cardiovascular risk factors. They said the association between anemia and MCI has important clinical relevance because—depending on etiology—anemia can be treated effectively, and this might provide means to prevent or delay cognitive decline. ![]()

A population-based study conducted in Germany has suggested a link between anemia and mild cognitive impairment (MCI).
Researchers found that subjects with anemia, defined as hemoglobin <13 g/dL in men and <12 g/dL in women, performed worse on cognitive tests than their nonanemic peers.
And MCI occurred almost twice as often in subjects with anemia than in subjects with normal hemoglobin levels.
This study was published in the Journal of Alzheimer’s Disease.
About MCI
MCI represents an intermediate and possibly modifiable stage between normal cognitive aging and dementia. Although individuals with MCI have an increased risk of developing dementia or Alzheimer’s disease, they can also remain stable for many years or even revert to a cognitively normal state over time. This modifiable characteristic makes the concept of MCI a promising target in the prevention of dementia.
The following 4 criteria are used to diagnose MCI. First, subjects must report a decline in cognitive performance over the past 2 years. Second, they must show a cognitive impairment in objective cognitive tasks that is greater than one would expect taking their age and education into consideration.
Third, the impairment must not be as pronounced as in demented individuals since people with MCI can perform normal daily living activities or are only slightly impaired in carrying out complex instrumental functions. Fourth, the cognitive impairment has to be insufficient to fulfil criteria for dementia.
The concept of MCI distinguishes between amnestic MCI (aMCI) and non-amnestic MCI (naMCI). In the former, impairment in the memory domain is evident, most likely reflecting Alzheimer’s disease pathology. In the latter, impairment in non-memory domains is present, mainly reflecting vascular pathology but also frontotemporal dementia or dementia with Lewy bodies.
Study details
The Heinz Nixdorf Recall study is an observational, population-based, prospective study in which researchers examined 4814 subjects between 2000 and 2003. Subjects were 50 to 80 years of age and lived in the metropolitan Ruhr Area. Both genders were equally represented.
After 5 years, the researchers conducted a second examination with 92% of the subjects taking part. The publication includes cross-sectional results of the second examination.
First, 163 subjects with anemia and 3870 without anemia were included to compare their performance in all cognitive subtests.
The subjects took verbal memory tests, which were used to gauge immediate recall and delayed recall. They were also tested on executive functioning, which included problem-solving/speed of processing, verbal fluency, visual spatial organization, and the clock drawing test.
In the initial analysis, anemic subjects showed more pronounced cardiovascular risk profiles and lower cognitive performance in all administered cognitive subtests. After adjusting for age, anemic subjects showed a significantly lower performance in the immediate recall task (P=0.009) and the verbal fluency task (P=0.004).
Next, the researchers compared 579 subjects diagnosed with MCI—299 with aMCI and 280 with naMCI—to 1438 cognitively normal subjects to determine the association between anemia at follow-up and MCI.
The team found that MCI occurred more often in anemic than non-anemic subjects. The unadjusted odds ratio (OR) was 2.59 (P<0.001). The OR after adjustment for age, gender, and years of education was 2.15 (P=0.002).
In a third analysis, the researchers adjusted for the aforementioned variables as well as body mass index, high-sensitivity C-reactive protein, glomerular filtration rate, cholesterol, serum iron, hypertension, diabetes mellitus, history of coronary heart disease, history of stroke, history of cancer, APOE4, smoking, severe depressive symptoms, and use of antidepressants. The OR after adjustment for these factors was 1.92 (P=0.04).
Similar results were found for aMCI and naMCI. The researchers said this suggests that having a low hemoglobin level may contribute to cognitive impairment via different pathways.
The team believes that, overall, their study results indicate that anemia is associated with an increased risk of MCI independent of traditional cardiovascular risk factors. They said the association between anemia and MCI has important clinical relevance because—depending on etiology—anemia can be treated effectively, and this might provide means to prevent or delay cognitive decline. ![]()

A population-based study conducted in Germany has suggested a link between anemia and mild cognitive impairment (MCI).
Researchers found that subjects with anemia, defined as hemoglobin <13 g/dL in men and <12 g/dL in women, performed worse on cognitive tests than their nonanemic peers.
And MCI occurred almost twice as often in subjects with anemia than in subjects with normal hemoglobin levels.
This study was published in the Journal of Alzheimer’s Disease.
About MCI
MCI represents an intermediate and possibly modifiable stage between normal cognitive aging and dementia. Although individuals with MCI have an increased risk of developing dementia or Alzheimer’s disease, they can also remain stable for many years or even revert to a cognitively normal state over time. This modifiable characteristic makes the concept of MCI a promising target in the prevention of dementia.
The following 4 criteria are used to diagnose MCI. First, subjects must report a decline in cognitive performance over the past 2 years. Second, they must show a cognitive impairment in objective cognitive tasks that is greater than one would expect taking their age and education into consideration.
Third, the impairment must not be as pronounced as in demented individuals since people with MCI can perform normal daily living activities or are only slightly impaired in carrying out complex instrumental functions. Fourth, the cognitive impairment has to be insufficient to fulfil criteria for dementia.
The concept of MCI distinguishes between amnestic MCI (aMCI) and non-amnestic MCI (naMCI). In the former, impairment in the memory domain is evident, most likely reflecting Alzheimer’s disease pathology. In the latter, impairment in non-memory domains is present, mainly reflecting vascular pathology but also frontotemporal dementia or dementia with Lewy bodies.
Study details
The Heinz Nixdorf Recall study is an observational, population-based, prospective study in which researchers examined 4814 subjects between 2000 and 2003. Subjects were 50 to 80 years of age and lived in the metropolitan Ruhr Area. Both genders were equally represented.
After 5 years, the researchers conducted a second examination with 92% of the subjects taking part. The publication includes cross-sectional results of the second examination.
First, 163 subjects with anemia and 3870 without anemia were included to compare their performance in all cognitive subtests.
The subjects took verbal memory tests, which were used to gauge immediate recall and delayed recall. They were also tested on executive functioning, which included problem-solving/speed of processing, verbal fluency, visual spatial organization, and the clock drawing test.
In the initial analysis, anemic subjects showed more pronounced cardiovascular risk profiles and lower cognitive performance in all administered cognitive subtests. After adjusting for age, anemic subjects showed a significantly lower performance in the immediate recall task (P=0.009) and the verbal fluency task (P=0.004).
Next, the researchers compared 579 subjects diagnosed with MCI—299 with aMCI and 280 with naMCI—to 1438 cognitively normal subjects to determine the association between anemia at follow-up and MCI.
The team found that MCI occurred more often in anemic than non-anemic subjects. The unadjusted odds ratio (OR) was 2.59 (P<0.001). The OR after adjustment for age, gender, and years of education was 2.15 (P=0.002).
In a third analysis, the researchers adjusted for the aforementioned variables as well as body mass index, high-sensitivity C-reactive protein, glomerular filtration rate, cholesterol, serum iron, hypertension, diabetes mellitus, history of coronary heart disease, history of stroke, history of cancer, APOE4, smoking, severe depressive symptoms, and use of antidepressants. The OR after adjustment for these factors was 1.92 (P=0.04).
Similar results were found for aMCI and naMCI. The researchers said this suggests that having a low hemoglobin level may contribute to cognitive impairment via different pathways.
The team believes that, overall, their study results indicate that anemia is associated with an increased risk of MCI independent of traditional cardiovascular risk factors. They said the association between anemia and MCI has important clinical relevance because—depending on etiology—anemia can be treated effectively, and this might provide means to prevent or delay cognitive decline. ![]()
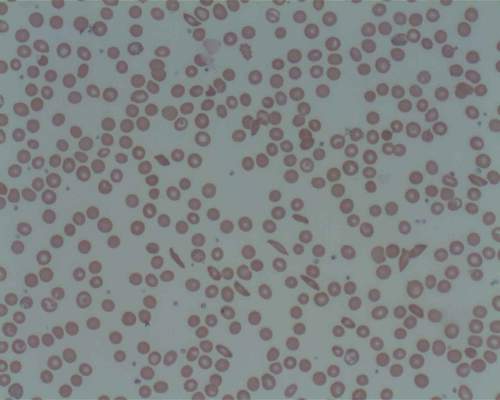
Myeloma drug could treat sickle cell disease, team says

and a normal one
Image by Betty Pace
Preclinical research suggests a drug used to treat multiple myeloma (MM) might also prove effective in the treatment of sickle cell disease (SCD).
Researchers say this study is the first to reveal how the drug, pomalidomide, increases the production of fetal hemoglobin, which is known to interfere with the sickling of red blood cells.
“We knew the drug would make fetal hemoglobin, but we didn’t know to what extent or how,” said Lionel Blanc, PhD, of the Feinstein Institute for Medical Research in Manhasset, New York.
He and his colleagues reported their findings in Blood.
The researchers’ in vitro experiments revealed that pomalidomide reverses γ-globin silencing during adult erythropoiesis, and the drug delays the maturation of early erythroid precursors without impairing terminal differentiation.
The team also found that pomalidomide selectively targets BCL11A and SOX6 to induce γ-globin synthesis, the drug’s mechanism of action during erythropoiesis is independent of IKZF1 degradation, and pomalidomide partially reprograms adult erythroid progenitors to a fetal-like state.
Finally, the researchers discovered that pomalidomide’s mechanism of action is conserved in cells from SCD patients, and treatment with pomalidomide leads to γ-globin production in MM patients.
“We can also say something else—that hydroxyurea, the only FDA-approved drug for sickle cell anemia, was less effective than pomalidomide and appeared to act through a different mechanism of action,” Dr Blanc said.
“The current therapy is good, but not everyone responds equally to hydroxyurea, and what we hope with pomalidomide is to improve this.”
Dr Blanc and his colleagues plan to launch a clinical trial in the near future to test pomalidomide in young adults with SCD. ![]()

and a normal one
Image by Betty Pace
Preclinical research suggests a drug used to treat multiple myeloma (MM) might also prove effective in the treatment of sickle cell disease (SCD).
Researchers say this study is the first to reveal how the drug, pomalidomide, increases the production of fetal hemoglobin, which is known to interfere with the sickling of red blood cells.
“We knew the drug would make fetal hemoglobin, but we didn’t know to what extent or how,” said Lionel Blanc, PhD, of the Feinstein Institute for Medical Research in Manhasset, New York.
He and his colleagues reported their findings in Blood.
The researchers’ in vitro experiments revealed that pomalidomide reverses γ-globin silencing during adult erythropoiesis, and the drug delays the maturation of early erythroid precursors without impairing terminal differentiation.
The team also found that pomalidomide selectively targets BCL11A and SOX6 to induce γ-globin synthesis, the drug’s mechanism of action during erythropoiesis is independent of IKZF1 degradation, and pomalidomide partially reprograms adult erythroid progenitors to a fetal-like state.
Finally, the researchers discovered that pomalidomide’s mechanism of action is conserved in cells from SCD patients, and treatment with pomalidomide leads to γ-globin production in MM patients.
“We can also say something else—that hydroxyurea, the only FDA-approved drug for sickle cell anemia, was less effective than pomalidomide and appeared to act through a different mechanism of action,” Dr Blanc said.
“The current therapy is good, but not everyone responds equally to hydroxyurea, and what we hope with pomalidomide is to improve this.”
Dr Blanc and his colleagues plan to launch a clinical trial in the near future to test pomalidomide in young adults with SCD. ![]()

and a normal one
Image by Betty Pace
Preclinical research suggests a drug used to treat multiple myeloma (MM) might also prove effective in the treatment of sickle cell disease (SCD).
Researchers say this study is the first to reveal how the drug, pomalidomide, increases the production of fetal hemoglobin, which is known to interfere with the sickling of red blood cells.
“We knew the drug would make fetal hemoglobin, but we didn’t know to what extent or how,” said Lionel Blanc, PhD, of the Feinstein Institute for Medical Research in Manhasset, New York.
He and his colleagues reported their findings in Blood.
The researchers’ in vitro experiments revealed that pomalidomide reverses γ-globin silencing during adult erythropoiesis, and the drug delays the maturation of early erythroid precursors without impairing terminal differentiation.
The team also found that pomalidomide selectively targets BCL11A and SOX6 to induce γ-globin synthesis, the drug’s mechanism of action during erythropoiesis is independent of IKZF1 degradation, and pomalidomide partially reprograms adult erythroid progenitors to a fetal-like state.
Finally, the researchers discovered that pomalidomide’s mechanism of action is conserved in cells from SCD patients, and treatment with pomalidomide leads to γ-globin production in MM patients.
“We can also say something else—that hydroxyurea, the only FDA-approved drug for sickle cell anemia, was less effective than pomalidomide and appeared to act through a different mechanism of action,” Dr Blanc said.
“The current therapy is good, but not everyone responds equally to hydroxyurea, and what we hope with pomalidomide is to improve this.”
Dr Blanc and his colleagues plan to launch a clinical trial in the near future to test pomalidomide in young adults with SCD. ![]()
Graft source and timing of HSCT affect survival in SCD

Photo by Chad McNeeley
ORLANDO, FL—In a large, registry-based study, transplants from human leukocyte antigen (HLA)-identical sibling donors proved successful in more than 90% of children and adults with severe sickle cell disease (SCD).
However, younger patients and those who received bone marrow (BM) or cord blood (CB) transplants fared the best.
Patient age and stem cell source were both independently associated with event-free and overall survival.
These results suggest SCD patients should be referred for transplant early but should not receive peripheral blood stem cell (PBSC) transplants, said Barbara Cappelli, MD, of the Eurocord International Registry in Paris, France.
Dr Cappelli presented the results of this study at the 2015 ASH Annual Meeting (abstract 541*).
The study included 1000 SCD patients who received HLA-identical sibling transplants from 1986 through 2013. The transplants took place at 88 centers in 23 countries and were reported to the Eurocord-Monacord/European Group for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
The patients’ median age was 9 (range, 1-54), and most (85%) were younger than 16. Most patients (94%) were homozygotes for hemoglobin S. Most had received red blood cell transfusions (94%), and a little more than half had received hydroxyurea (56%).
About half of HSCTs (53%) were performed after 2007, 29% from 2000 to 2006, 16% from 1991 to 1999, and 2% before 1999.
The most common indication for HSCT was recurrent vaso-occlusive crisis (77%), followed by stroke or central nervous system event (48%), and recurrent chest syndrome (32%), among other indications.
Most patients received BM transplants (84%), although a minority received CB (9%) or PBSC (7%) transplants.
A majority of patients received myeloablative conditioning regimens (n=873, 87%), largely based on the combination of busulfan and cyclophosphamide (n=719). Among the patients who received reduced-intensity conditioning (n=127, 13%), fludarabine with cyclophosphamide was the predominant regimen (n=48).
Most regimens included in vivo T-cell depletion (70%) with anti-thymocyte globulin (n=630) or alemtuzumab (n=76). The most common regimen for graft-vs-host disease (GVHD) prophylaxis was cyclosporine plus methotrexate (56%).
Results
The median follow-up was 45 months (range, 1-325).
At 60 days, the cumulative incidence of neutrophil engraftment was 98%, and the median time to neutrophil engraftment was 19 days. The cumulative incidence of platelet engraftment was 96%, and the median time to platelet engraftment was 25 days.
Acute GVHD occurred in 14.4% of patients, and chronic GVHD occurred 13.3%.
Multivariate analysis showed that the risk of acute GVHD was significantly higher in older patients, but none of the variables the researchers tested (T-cell depletion, conditioning regimen, etc.) were associated with chronic GVHD.
Younger age at HSCT and receiving a BM or CB transplant were independently associated with better event-free survival and overall survival. Undergoing HSCT after the year 2000 was associated with better overall survival.
The 3-year event-free survival was 90% overall, 90% for patients who received BM transplants, 78% for those who received PBSCs, and 97% for those who received CB transplants.
The 3-year overall survival was 94% overall, 94% for patients who received BM transplants, 80% for those who received PBSCs, and 99% for those who received CB transplants.
Seventy-one patients (7%) had autologous reconstitution (45 with late graft failure), 31 (3%) underwent a second HSCT, and 67 (7%) died—6% in the BM group, 21% in the PBSC group, and 1% in the CB group.
Death was related to transplant in 59 cases—14 due to infection, 12 due to toxicity, 9 due to GVHD, and 24 were of an unknown (but presumably HSCT-related) cause.
Three patients died from disease recurrence or persistence, 2 died from secondary malignancies, and 3 had unknown causes of death.
“This study shows excellent 3-year overall and event-free survival, with limited toxicity, despite the use of myeloablative conditioning regimens,” Dr Cappelli noted. “This should increase the early referral to transplant for patients with severe sickle cell disease, as age is an independent predictor for event-free survival and overall survival.”
She added that PBSC transplants “are not recommended,” as they were associated with higher mortality. And novel strategies are needed for lowing rates of graft failure and GVHD in SCD patients. ![]()
*Data in the abstract differ from the presentation.

Photo by Chad McNeeley
ORLANDO, FL—In a large, registry-based study, transplants from human leukocyte antigen (HLA)-identical sibling donors proved successful in more than 90% of children and adults with severe sickle cell disease (SCD).
However, younger patients and those who received bone marrow (BM) or cord blood (CB) transplants fared the best.
Patient age and stem cell source were both independently associated with event-free and overall survival.
These results suggest SCD patients should be referred for transplant early but should not receive peripheral blood stem cell (PBSC) transplants, said Barbara Cappelli, MD, of the Eurocord International Registry in Paris, France.
Dr Cappelli presented the results of this study at the 2015 ASH Annual Meeting (abstract 541*).
The study included 1000 SCD patients who received HLA-identical sibling transplants from 1986 through 2013. The transplants took place at 88 centers in 23 countries and were reported to the Eurocord-Monacord/European Group for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
The patients’ median age was 9 (range, 1-54), and most (85%) were younger than 16. Most patients (94%) were homozygotes for hemoglobin S. Most had received red blood cell transfusions (94%), and a little more than half had received hydroxyurea (56%).
About half of HSCTs (53%) were performed after 2007, 29% from 2000 to 2006, 16% from 1991 to 1999, and 2% before 1999.
The most common indication for HSCT was recurrent vaso-occlusive crisis (77%), followed by stroke or central nervous system event (48%), and recurrent chest syndrome (32%), among other indications.
Most patients received BM transplants (84%), although a minority received CB (9%) or PBSC (7%) transplants.
A majority of patients received myeloablative conditioning regimens (n=873, 87%), largely based on the combination of busulfan and cyclophosphamide (n=719). Among the patients who received reduced-intensity conditioning (n=127, 13%), fludarabine with cyclophosphamide was the predominant regimen (n=48).
Most regimens included in vivo T-cell depletion (70%) with anti-thymocyte globulin (n=630) or alemtuzumab (n=76). The most common regimen for graft-vs-host disease (GVHD) prophylaxis was cyclosporine plus methotrexate (56%).
Results
The median follow-up was 45 months (range, 1-325).
At 60 days, the cumulative incidence of neutrophil engraftment was 98%, and the median time to neutrophil engraftment was 19 days. The cumulative incidence of platelet engraftment was 96%, and the median time to platelet engraftment was 25 days.
Acute GVHD occurred in 14.4% of patients, and chronic GVHD occurred 13.3%.
Multivariate analysis showed that the risk of acute GVHD was significantly higher in older patients, but none of the variables the researchers tested (T-cell depletion, conditioning regimen, etc.) were associated with chronic GVHD.
Younger age at HSCT and receiving a BM or CB transplant were independently associated with better event-free survival and overall survival. Undergoing HSCT after the year 2000 was associated with better overall survival.
The 3-year event-free survival was 90% overall, 90% for patients who received BM transplants, 78% for those who received PBSCs, and 97% for those who received CB transplants.
The 3-year overall survival was 94% overall, 94% for patients who received BM transplants, 80% for those who received PBSCs, and 99% for those who received CB transplants.
Seventy-one patients (7%) had autologous reconstitution (45 with late graft failure), 31 (3%) underwent a second HSCT, and 67 (7%) died—6% in the BM group, 21% in the PBSC group, and 1% in the CB group.
Death was related to transplant in 59 cases—14 due to infection, 12 due to toxicity, 9 due to GVHD, and 24 were of an unknown (but presumably HSCT-related) cause.
Three patients died from disease recurrence or persistence, 2 died from secondary malignancies, and 3 had unknown causes of death.
“This study shows excellent 3-year overall and event-free survival, with limited toxicity, despite the use of myeloablative conditioning regimens,” Dr Cappelli noted. “This should increase the early referral to transplant for patients with severe sickle cell disease, as age is an independent predictor for event-free survival and overall survival.”
She added that PBSC transplants “are not recommended,” as they were associated with higher mortality. And novel strategies are needed for lowing rates of graft failure and GVHD in SCD patients. ![]()
*Data in the abstract differ from the presentation.

Photo by Chad McNeeley
ORLANDO, FL—In a large, registry-based study, transplants from human leukocyte antigen (HLA)-identical sibling donors proved successful in more than 90% of children and adults with severe sickle cell disease (SCD).
However, younger patients and those who received bone marrow (BM) or cord blood (CB) transplants fared the best.
Patient age and stem cell source were both independently associated with event-free and overall survival.
These results suggest SCD patients should be referred for transplant early but should not receive peripheral blood stem cell (PBSC) transplants, said Barbara Cappelli, MD, of the Eurocord International Registry in Paris, France.
Dr Cappelli presented the results of this study at the 2015 ASH Annual Meeting (abstract 541*).
The study included 1000 SCD patients who received HLA-identical sibling transplants from 1986 through 2013. The transplants took place at 88 centers in 23 countries and were reported to the Eurocord-Monacord/European Group for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
The patients’ median age was 9 (range, 1-54), and most (85%) were younger than 16. Most patients (94%) were homozygotes for hemoglobin S. Most had received red blood cell transfusions (94%), and a little more than half had received hydroxyurea (56%).
About half of HSCTs (53%) were performed after 2007, 29% from 2000 to 2006, 16% from 1991 to 1999, and 2% before 1999.
The most common indication for HSCT was recurrent vaso-occlusive crisis (77%), followed by stroke or central nervous system event (48%), and recurrent chest syndrome (32%), among other indications.
Most patients received BM transplants (84%), although a minority received CB (9%) or PBSC (7%) transplants.
A majority of patients received myeloablative conditioning regimens (n=873, 87%), largely based on the combination of busulfan and cyclophosphamide (n=719). Among the patients who received reduced-intensity conditioning (n=127, 13%), fludarabine with cyclophosphamide was the predominant regimen (n=48).
Most regimens included in vivo T-cell depletion (70%) with anti-thymocyte globulin (n=630) or alemtuzumab (n=76). The most common regimen for graft-vs-host disease (GVHD) prophylaxis was cyclosporine plus methotrexate (56%).
Results
The median follow-up was 45 months (range, 1-325).
At 60 days, the cumulative incidence of neutrophil engraftment was 98%, and the median time to neutrophil engraftment was 19 days. The cumulative incidence of platelet engraftment was 96%, and the median time to platelet engraftment was 25 days.
Acute GVHD occurred in 14.4% of patients, and chronic GVHD occurred 13.3%.
Multivariate analysis showed that the risk of acute GVHD was significantly higher in older patients, but none of the variables the researchers tested (T-cell depletion, conditioning regimen, etc.) were associated with chronic GVHD.
Younger age at HSCT and receiving a BM or CB transplant were independently associated with better event-free survival and overall survival. Undergoing HSCT after the year 2000 was associated with better overall survival.
The 3-year event-free survival was 90% overall, 90% for patients who received BM transplants, 78% for those who received PBSCs, and 97% for those who received CB transplants.
The 3-year overall survival was 94% overall, 94% for patients who received BM transplants, 80% for those who received PBSCs, and 99% for those who received CB transplants.
Seventy-one patients (7%) had autologous reconstitution (45 with late graft failure), 31 (3%) underwent a second HSCT, and 67 (7%) died—6% in the BM group, 21% in the PBSC group, and 1% in the CB group.
Death was related to transplant in 59 cases—14 due to infection, 12 due to toxicity, 9 due to GVHD, and 24 were of an unknown (but presumably HSCT-related) cause.
Three patients died from disease recurrence or persistence, 2 died from secondary malignancies, and 3 had unknown causes of death.
“This study shows excellent 3-year overall and event-free survival, with limited toxicity, despite the use of myeloablative conditioning regimens,” Dr Cappelli noted. “This should increase the early referral to transplant for patients with severe sickle cell disease, as age is an independent predictor for event-free survival and overall survival.”
She added that PBSC transplants “are not recommended,” as they were associated with higher mortality. And novel strategies are needed for lowing rates of graft failure and GVHD in SCD patients. ![]()
*Data in the abstract differ from the presentation.
SAA patients benefit from upfront eltrombopag combo

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.
HU noninferior to transfusion for stroke prevention in SCD

Photo courtesy of ASH
ORLANDO, FL—Hydroxyurea (HU) is noninferior to chronic blood transfusions for reducing the risk of stroke in children with sickle cell disease (SCD), results of the TWiTCH trial suggest.
The trial showed that daily doses of HU lower the transcranial Doppler (TCD) blood velocity in children with SCD to a similar degree as blood transfusions, thereby decreasing the risk of stroke.
Because of these findings, the trial was terminated early, in November of last year.
Last week, results from TWiTCH were presented at the 2015 ASH Annual Meeting (abstract 3*) and published in The Lancet. The study was funded by the National Heart Lung and Blood Institute.
“Stroke . . . is one of the most severe and catastrophic clinical events that occurs in children with sickle cell, with serious motor and cognitive sequelae,” said study investigator and ASH presenter Russell E. Ware, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“With the advent of TCD, we now have the ability to identify high-risk children and use chronic transfusion therapy to prevent primary stroke.”
Dr Ware noted that results of the STOP trial showed that chronic transfusion reduced the risk of stroke in high-risk children with SCD, but the transfusions could not be stopped. The STOP 2 trial confirmed this, showing that stopping transfusions led to an increase in TCD blood velocity and stroke risk.
Because transfusions must be continued indefinitely and are associated with morbidity, an alternative stroke prevention strategy is needed, Dr Ware said. He and his colleagues conducted the TWiTCH trial to determine if HU would fit the bill.
Study design
For this phase 3 study, the researchers compared 24 months of transfusions to HU in children with SCD and abnormal TCD velocities. Study enrollment began in September 2011 and ended in April 2013.
All eligible children had received at least 12 months of transfusions prior to enrollment. They were randomized 1:1 to continue receiving transfusions or to receive the maximum-tolerated dose (MTD) of HU.
In the transfusion arm, the goal was to keep hemoglobin S levels below 30%, and iron overload was managed with daily oral chelation.
In the HU arm, the drug was escalated to the MTD, and children continued receiving transfusions until the MTD was achieved. Iron overload was managed with monthly phlebotomy.
The study had a noninferiority design, and the primary endpoint was the 24-month TCD velocity (with a noninferiority margin of 15 cm/sec). TCD velocities were obtained every 12 weeks and reviewed centrally. Local researchers were masked to the results.
Results
In all, 121 children were randomized—61 to transfusions and 60 to HU. Patient characteristics—baseline TCD velocities, age, duration of transfusion, etc.—were well balanced between the treatment arms.
“The average age of the patients was 9 or 10 years old, with about 3 or 4 years of transfusions coming in to the study,” Dr Ware noted.
In the transfusion arm, the children maintained a hemoglobin level of about 9 g/dL and hemoglobin S levels of less than 30%. Most patients received chelation with deferasirox at 26 ±6 mg/kg/day.
In the HU arm, 57 of 60 patients reached the MTD, which was 27 ± 4 mg/kg/day, on average. The median transfusion overlap was 6 months, the average absolute neutrophil count was 3.5 ± 1.6 x 109/L, the average hemoglobin was about 9 g/dL, and fetal hemoglobin rose to about 25%. There were 756 phlebotomy procedures performed in 54 children.
“[In the HU arm,] very quickly after enrollment, the sickle hemoglobin rises, as the transfusions are weaned,” Dr Ware noted.
“Commensurately, the hemoglobin F rises as a protection. The neutrophil count and reticulocyte count drops, and those curves [counts in the HU and transfusion arms] diverge fairly quickly. The serum ferritin [curves] diverged as well.”
Early termination and noninferiority
Interim data analyses were scheduled to take place after one-third of the patients had exited the study and after two-thirds had exited. The first interim analysis demonstrated noninferiority, and the trial was closed early. An analysis was repeated after half of the patients had exited the study, and the trial was terminated.
At that point, 42 children had completed 24 months of treatment in the transfusion arm, 11 patients had truncated treatment, and 8 had early exits. Forty-one patients had completed 24 months of therapy in the HU arm, 13 had truncated treatment, and 6 had early exits.
The final TCD velocity (mean ± standard error) was 143 ± 1.6 cm/sec in the transfusion arm and 138 ± 1.6 cm/sec in the HU arm. The P value for noninferiority (in the intent-to-treat population) was 8.82 x 10-16. By post-hoc analysis, the P value for superiority was 0.023.
Secondary endpoints
There were 29 new neurological events during the trial—12 in the transfusion arm and 17 in the HU arm. There were no new strokes, but there were 6 new transient ischemic attacks—3 in each arm.
There were no new cerebral infarcts in either arm. But there was 1 new progressive vasculopathy in the transfusion arm. And 1 child in the transfusion arm was withdrawn from the study for increasing TCD (>240 cm/sec).
Iron overload improved more in the HU arm than the transfusion arm, with a greater average change in both serum ferritin (P<0.001) and liver iron concentration (P=0.001).
Serious adverse events were more common in the HU arm than the transfusion arm—23 events in 9 patients and 10 events in 6 patients, respectively. But none of these events were thought to be related to study treatment or procedures.
The most common serious adverse event in both groups was vaso-occlusive pain—11 events in 5 HU-treated patients and 3 events in 1 transfusion-treated patient.
Dr Ware noted that there were no secondary leukemias associated with HU in this trial, and there is “a cumulative body of evidence” spanning 20 years that suggests the drug is not carcinogenic in this patient population. ![]()
*Data in the abstract differ from data presented at the meeting.

Photo courtesy of ASH
ORLANDO, FL—Hydroxyurea (HU) is noninferior to chronic blood transfusions for reducing the risk of stroke in children with sickle cell disease (SCD), results of the TWiTCH trial suggest.
The trial showed that daily doses of HU lower the transcranial Doppler (TCD) blood velocity in children with SCD to a similar degree as blood transfusions, thereby decreasing the risk of stroke.
Because of these findings, the trial was terminated early, in November of last year.
Last week, results from TWiTCH were presented at the 2015 ASH Annual Meeting (abstract 3*) and published in The Lancet. The study was funded by the National Heart Lung and Blood Institute.
“Stroke . . . is one of the most severe and catastrophic clinical events that occurs in children with sickle cell, with serious motor and cognitive sequelae,” said study investigator and ASH presenter Russell E. Ware, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“With the advent of TCD, we now have the ability to identify high-risk children and use chronic transfusion therapy to prevent primary stroke.”
Dr Ware noted that results of the STOP trial showed that chronic transfusion reduced the risk of stroke in high-risk children with SCD, but the transfusions could not be stopped. The STOP 2 trial confirmed this, showing that stopping transfusions led to an increase in TCD blood velocity and stroke risk.
Because transfusions must be continued indefinitely and are associated with morbidity, an alternative stroke prevention strategy is needed, Dr Ware said. He and his colleagues conducted the TWiTCH trial to determine if HU would fit the bill.
Study design
For this phase 3 study, the researchers compared 24 months of transfusions to HU in children with SCD and abnormal TCD velocities. Study enrollment began in September 2011 and ended in April 2013.
All eligible children had received at least 12 months of transfusions prior to enrollment. They were randomized 1:1 to continue receiving transfusions or to receive the maximum-tolerated dose (MTD) of HU.
In the transfusion arm, the goal was to keep hemoglobin S levels below 30%, and iron overload was managed with daily oral chelation.
In the HU arm, the drug was escalated to the MTD, and children continued receiving transfusions until the MTD was achieved. Iron overload was managed with monthly phlebotomy.
The study had a noninferiority design, and the primary endpoint was the 24-month TCD velocity (with a noninferiority margin of 15 cm/sec). TCD velocities were obtained every 12 weeks and reviewed centrally. Local researchers were masked to the results.
Results
In all, 121 children were randomized—61 to transfusions and 60 to HU. Patient characteristics—baseline TCD velocities, age, duration of transfusion, etc.—were well balanced between the treatment arms.
“The average age of the patients was 9 or 10 years old, with about 3 or 4 years of transfusions coming in to the study,” Dr Ware noted.
In the transfusion arm, the children maintained a hemoglobin level of about 9 g/dL and hemoglobin S levels of less than 30%. Most patients received chelation with deferasirox at 26 ±6 mg/kg/day.
In the HU arm, 57 of 60 patients reached the MTD, which was 27 ± 4 mg/kg/day, on average. The median transfusion overlap was 6 months, the average absolute neutrophil count was 3.5 ± 1.6 x 109/L, the average hemoglobin was about 9 g/dL, and fetal hemoglobin rose to about 25%. There were 756 phlebotomy procedures performed in 54 children.
“[In the HU arm,] very quickly after enrollment, the sickle hemoglobin rises, as the transfusions are weaned,” Dr Ware noted.
“Commensurately, the hemoglobin F rises as a protection. The neutrophil count and reticulocyte count drops, and those curves [counts in the HU and transfusion arms] diverge fairly quickly. The serum ferritin [curves] diverged as well.”
Early termination and noninferiority
Interim data analyses were scheduled to take place after one-third of the patients had exited the study and after two-thirds had exited. The first interim analysis demonstrated noninferiority, and the trial was closed early. An analysis was repeated after half of the patients had exited the study, and the trial was terminated.
At that point, 42 children had completed 24 months of treatment in the transfusion arm, 11 patients had truncated treatment, and 8 had early exits. Forty-one patients had completed 24 months of therapy in the HU arm, 13 had truncated treatment, and 6 had early exits.
The final TCD velocity (mean ± standard error) was 143 ± 1.6 cm/sec in the transfusion arm and 138 ± 1.6 cm/sec in the HU arm. The P value for noninferiority (in the intent-to-treat population) was 8.82 x 10-16. By post-hoc analysis, the P value for superiority was 0.023.
Secondary endpoints
There were 29 new neurological events during the trial—12 in the transfusion arm and 17 in the HU arm. There were no new strokes, but there were 6 new transient ischemic attacks—3 in each arm.
There were no new cerebral infarcts in either arm. But there was 1 new progressive vasculopathy in the transfusion arm. And 1 child in the transfusion arm was withdrawn from the study for increasing TCD (>240 cm/sec).
Iron overload improved more in the HU arm than the transfusion arm, with a greater average change in both serum ferritin (P<0.001) and liver iron concentration (P=0.001).
Serious adverse events were more common in the HU arm than the transfusion arm—23 events in 9 patients and 10 events in 6 patients, respectively. But none of these events were thought to be related to study treatment or procedures.
The most common serious adverse event in both groups was vaso-occlusive pain—11 events in 5 HU-treated patients and 3 events in 1 transfusion-treated patient.
Dr Ware noted that there were no secondary leukemias associated with HU in this trial, and there is “a cumulative body of evidence” spanning 20 years that suggests the drug is not carcinogenic in this patient population. ![]()
*Data in the abstract differ from data presented at the meeting.

Photo courtesy of ASH
ORLANDO, FL—Hydroxyurea (HU) is noninferior to chronic blood transfusions for reducing the risk of stroke in children with sickle cell disease (SCD), results of the TWiTCH trial suggest.
The trial showed that daily doses of HU lower the transcranial Doppler (TCD) blood velocity in children with SCD to a similar degree as blood transfusions, thereby decreasing the risk of stroke.
Because of these findings, the trial was terminated early, in November of last year.
Last week, results from TWiTCH were presented at the 2015 ASH Annual Meeting (abstract 3*) and published in The Lancet. The study was funded by the National Heart Lung and Blood Institute.
“Stroke . . . is one of the most severe and catastrophic clinical events that occurs in children with sickle cell, with serious motor and cognitive sequelae,” said study investigator and ASH presenter Russell E. Ware, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“With the advent of TCD, we now have the ability to identify high-risk children and use chronic transfusion therapy to prevent primary stroke.”
Dr Ware noted that results of the STOP trial showed that chronic transfusion reduced the risk of stroke in high-risk children with SCD, but the transfusions could not be stopped. The STOP 2 trial confirmed this, showing that stopping transfusions led to an increase in TCD blood velocity and stroke risk.
Because transfusions must be continued indefinitely and are associated with morbidity, an alternative stroke prevention strategy is needed, Dr Ware said. He and his colleagues conducted the TWiTCH trial to determine if HU would fit the bill.
Study design
For this phase 3 study, the researchers compared 24 months of transfusions to HU in children with SCD and abnormal TCD velocities. Study enrollment began in September 2011 and ended in April 2013.
All eligible children had received at least 12 months of transfusions prior to enrollment. They were randomized 1:1 to continue receiving transfusions or to receive the maximum-tolerated dose (MTD) of HU.
In the transfusion arm, the goal was to keep hemoglobin S levels below 30%, and iron overload was managed with daily oral chelation.
In the HU arm, the drug was escalated to the MTD, and children continued receiving transfusions until the MTD was achieved. Iron overload was managed with monthly phlebotomy.
The study had a noninferiority design, and the primary endpoint was the 24-month TCD velocity (with a noninferiority margin of 15 cm/sec). TCD velocities were obtained every 12 weeks and reviewed centrally. Local researchers were masked to the results.
Results
In all, 121 children were randomized—61 to transfusions and 60 to HU. Patient characteristics—baseline TCD velocities, age, duration of transfusion, etc.—were well balanced between the treatment arms.
“The average age of the patients was 9 or 10 years old, with about 3 or 4 years of transfusions coming in to the study,” Dr Ware noted.
In the transfusion arm, the children maintained a hemoglobin level of about 9 g/dL and hemoglobin S levels of less than 30%. Most patients received chelation with deferasirox at 26 ±6 mg/kg/day.
In the HU arm, 57 of 60 patients reached the MTD, which was 27 ± 4 mg/kg/day, on average. The median transfusion overlap was 6 months, the average absolute neutrophil count was 3.5 ± 1.6 x 109/L, the average hemoglobin was about 9 g/dL, and fetal hemoglobin rose to about 25%. There were 756 phlebotomy procedures performed in 54 children.
“[In the HU arm,] very quickly after enrollment, the sickle hemoglobin rises, as the transfusions are weaned,” Dr Ware noted.
“Commensurately, the hemoglobin F rises as a protection. The neutrophil count and reticulocyte count drops, and those curves [counts in the HU and transfusion arms] diverge fairly quickly. The serum ferritin [curves] diverged as well.”
Early termination and noninferiority
Interim data analyses were scheduled to take place after one-third of the patients had exited the study and after two-thirds had exited. The first interim analysis demonstrated noninferiority, and the trial was closed early. An analysis was repeated after half of the patients had exited the study, and the trial was terminated.
At that point, 42 children had completed 24 months of treatment in the transfusion arm, 11 patients had truncated treatment, and 8 had early exits. Forty-one patients had completed 24 months of therapy in the HU arm, 13 had truncated treatment, and 6 had early exits.
The final TCD velocity (mean ± standard error) was 143 ± 1.6 cm/sec in the transfusion arm and 138 ± 1.6 cm/sec in the HU arm. The P value for noninferiority (in the intent-to-treat population) was 8.82 x 10-16. By post-hoc analysis, the P value for superiority was 0.023.
Secondary endpoints
There were 29 new neurological events during the trial—12 in the transfusion arm and 17 in the HU arm. There were no new strokes, but there were 6 new transient ischemic attacks—3 in each arm.
There were no new cerebral infarcts in either arm. But there was 1 new progressive vasculopathy in the transfusion arm. And 1 child in the transfusion arm was withdrawn from the study for increasing TCD (>240 cm/sec).
Iron overload improved more in the HU arm than the transfusion arm, with a greater average change in both serum ferritin (P<0.001) and liver iron concentration (P=0.001).
Serious adverse events were more common in the HU arm than the transfusion arm—23 events in 9 patients and 10 events in 6 patients, respectively. But none of these events were thought to be related to study treatment or procedures.
The most common serious adverse event in both groups was vaso-occlusive pain—11 events in 5 HU-treated patients and 3 events in 1 transfusion-treated patient.
Dr Ware noted that there were no secondary leukemias associated with HU in this trial, and there is “a cumulative body of evidence” spanning 20 years that suggests the drug is not carcinogenic in this patient population. ![]()
*Data in the abstract differ from data presented at the meeting.
mAb could provide targeted approach to HLH treatment

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—A monoclonal antibody (mAb) targeting interferon-gamma (IFNγ) has shown promise for treating hemophagocytic lymphohistiocytosis (HLH), according to a late-breaking abstract presented at the 2015 ASH Annual Meeting.
Results of an ongoing phase 2 study suggest the mAb, NI-0501, may be a feasible treatment option for patients with HLH who have demonstrated an unsatisfactory response to, or cannot tolerate, conventional therapy.
Nine of 13 evaluable patients achieved a “satisfactory response” to NI-0501, and no safety concerns were identified, said Michael Jordan, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
Dr Jordan presented these results at ASH as LBA-3.* The trial was sponsored by Novimmune.
“Treatment of HLH remains very challenging,” Dr Jordan noted. “Initial therapy is directed at trying to suppress the out-of-control immune response. In children that are at risk for recurrent episodes of HLH, they proceed to hematopoietic cell transplantation and, hopefully, this allows long-term survival.”
“First-line therapy has been defined in international trials and involves etoposide and dexamethasone. This regimen, as you might imagine, in children that present already with cytopenias, is myelosuppressive. It’s also broadly immune-suppressive. And although this does allow long-term survival in these children, there’s plenty of room for improvement in results.”
“[T]here is no standard of care for second-line therapy. Though there are no prospective data, children are increasingly treated with T-cell-depleting agents such as alemtuzumab and ATG, but this produces profound and long-lasting immune suppression. Though survival is not well-defined in these patients, it’s thought to be poor.”
In hopes of finding a new treatment option for HLH, Dr Jordan and his colleagues attempted to determine what drives the disease process. In preclinical studies, they identified IFNγ as a rational target in HLH. Blockade of IFNγ led to improved survival in mouse models.
The researchers also found elevated levels of IFNγ in patients with HLH. These preclinical and clinical data led to the development of NI-0501, a fully human, high affinity, anti-IFNγ mAb that binds to and neutralizes IFNγ.
Patients and treatment
In their phase 2 trial, Dr Jordan and his colleagues assessed NI-0501 in 16 patients—8 males and 8 females. Their median age was 1.2 years (range, 0.2-13). Twelve patients had causative mutations—FHL2 (n=4), FHL3 (n=2), FHL4 (n=1), GS-2 (n=3), XLP-1 (n=1), and XLP-2 (n=1). And 4 patients had central nervous system (CNS) involvement.
Two patients were receiving NI-0501 as first-line treatment, and the rest were receiving the mAb as second-line treatment. Patients had previously received dexamethasone (n=13), methylprednisone (n=2), etoposide (n=13), ATG (n=4), cyclosporine A (n=6), and “other” therapy (n=4).
NI-0501 was given at a starting dose of 1 mg/kg every 3 days, with possible dose increases guided by pharmacokinetic data and/or clinical response in each patient. The mAb was administered with dexamethasone at a dose of 5mg/m2 to 10 mg/m2, but dexamethasone could be tapered during the treatment course.
The treatment duration ranged from 4 weeks to 8 weeks, and the follow-up period was 4 weeks.
Response and survival
One patient was excluded from the analysis due to a lymphoma diagnosis after enrollment. Two patients are still receiving treatment, and 13 have completed treatment.
Among the patients who completed therapy, 4 had an insufficient response. Two of these patients died, and 2 proceeded to allogeneic hematopoietic stem cell transplant (HSCT) after receiving additional agents to control their disease.
Nine patients achieved a favorable response to NI-0501. Seven of these patients proceeded to HSCT, and 2 are awaiting HSCT with their disease well-controlled.
Post-transplant follow-up is still early for most patients, but 2 patients have follow-up greater than 1 year. One child died of graft-vs-host disease around day 45, but the remaining patients who went on to HSCT are still alive.
Characteristics of response
For some patients, response to NI-0501 included a significant improvement in neutrophil count (8/10, P<0.001), platelet count (7/12, P<0.001), and ferritin level (P=0.0025). The median serum ferritin level was 4142 ng/mL at baseline and 1648 ng/mL at the end of treatment.
Both patients who were febrile at the start of treatment experienced rapid normalization of fever. Six of 7 patients with palpable spleen or liver at the start of treatment had an improvement in organomegaly. And 3 of 4 patients had resolution or improvement of CNS involvement.
Overall, there was a significant decrease in glucocorticoid dose. The median dose at baseline was 10.0 mg/m2. At the end of treatment, the median dose was 4.0 mg/m2 (P=0.023).
“One pharmacodynamic readout that’s useful for understanding IFNγ biology in vivo is CXCL9,” Dr Jordan noted. “This is secreted by mononuclear phagocytes in response to IFNγ. And most patients had a very clear fall in CXCL9 while receiving NI-0501.”
Adverse events and death
No off-target effects of NI-0501 have been observed, and none of the patients have withdrawn from the study for safety reasons.
There have been 14 serious adverse events in 8 patients, but only 1 of these events was considered treatment-related. The patient had necrotizing fasciitis following P aeruginosa skin infection, which resolved. This event was considered treatment-related by an investigator but not by the data monitoring committee or the sponsor.
In all, 3 patients have died, but none of the deaths were related to NI-0501. Two patients died of HLH/multi-organ failure, and 1 died of graft-vs-host disease.
Infections
“[NI-0501 provides] a targeted form of immune suppression, so we can expect that most concerns will be related to infection,” Dr Jordan said. “The effects of IFNγ on immune defense are actually predictable, and they’re predictable because of 2 patient populations.”
“First are the rare patients who are born with IFNγ-receptor deficiency, and second are individuals that develop neutralizing autoantibodies against IFNγ. Both patient populations experience infections with atypical mycobacteria, tuberculosis, Salmonella, and so forth.”
There were 10 infections already present at the start of the study—St epidermidis (n=1), C difficile (n=1), E coli (n=1, gram-positive), cytomegalovirus (n=1), Epstein-Barr virus (n=4), and parvovirus (n=1). All of these infections resolved with treatment.
Fourteen infections arose during the study course—St epidermidis (n=1), C difficile (n=1), P aeruginosa (n=1), K pneumoniae (n=1), E coli (1 gram-positive, 1 gram-negative), adenovirus (n=1), cytomegalovirus (n=2), Epstein-Barr virus (1 reactivation), parvovirus (1 reactivation), parainfluenza T3 (n=1), influenza A (n=1), and Candida (n=1).
Most of these infections resolved. The exceptions were the case of adenovirus, 1 case of cytomegalovirus (although there was improvement), the Epstein-Barr virus reactivation, the parvovirus reactivation (though improved), and the case of influenza A.
The researchers did not know if the parainfluenza T3 infection resolved. The patient’s viral status was not reassessed prior to death.
“So, in conclusion, NI-0501 has shown the potential to improve or resolve clinical and laboratory abnormalities of HLH, including CNS signs and symptoms,” Dr Jordan said. “The response to this agent appears to be independent of the underlying causative mutation. It’s also independent of the presence and type of infectious trigger.”
“NI-0501 was very well-tolerated. No safety concerns have emerged to date, and no infections known to be caused by deficiency of IFNγ have been observed. The neutralization of IFNγ by NI-0501 can offer an innovative and targeted approach to the management of HLH.” ![]()
*Data in the abstract differ from data presented at the meeting.

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—A monoclonal antibody (mAb) targeting interferon-gamma (IFNγ) has shown promise for treating hemophagocytic lymphohistiocytosis (HLH), according to a late-breaking abstract presented at the 2015 ASH Annual Meeting.
Results of an ongoing phase 2 study suggest the mAb, NI-0501, may be a feasible treatment option for patients with HLH who have demonstrated an unsatisfactory response to, or cannot tolerate, conventional therapy.
Nine of 13 evaluable patients achieved a “satisfactory response” to NI-0501, and no safety concerns were identified, said Michael Jordan, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
Dr Jordan presented these results at ASH as LBA-3.* The trial was sponsored by Novimmune.
“Treatment of HLH remains very challenging,” Dr Jordan noted. “Initial therapy is directed at trying to suppress the out-of-control immune response. In children that are at risk for recurrent episodes of HLH, they proceed to hematopoietic cell transplantation and, hopefully, this allows long-term survival.”
“First-line therapy has been defined in international trials and involves etoposide and dexamethasone. This regimen, as you might imagine, in children that present already with cytopenias, is myelosuppressive. It’s also broadly immune-suppressive. And although this does allow long-term survival in these children, there’s plenty of room for improvement in results.”
“[T]here is no standard of care for second-line therapy. Though there are no prospective data, children are increasingly treated with T-cell-depleting agents such as alemtuzumab and ATG, but this produces profound and long-lasting immune suppression. Though survival is not well-defined in these patients, it’s thought to be poor.”
In hopes of finding a new treatment option for HLH, Dr Jordan and his colleagues attempted to determine what drives the disease process. In preclinical studies, they identified IFNγ as a rational target in HLH. Blockade of IFNγ led to improved survival in mouse models.
The researchers also found elevated levels of IFNγ in patients with HLH. These preclinical and clinical data led to the development of NI-0501, a fully human, high affinity, anti-IFNγ mAb that binds to and neutralizes IFNγ.
Patients and treatment
In their phase 2 trial, Dr Jordan and his colleagues assessed NI-0501 in 16 patients—8 males and 8 females. Their median age was 1.2 years (range, 0.2-13). Twelve patients had causative mutations—FHL2 (n=4), FHL3 (n=2), FHL4 (n=1), GS-2 (n=3), XLP-1 (n=1), and XLP-2 (n=1). And 4 patients had central nervous system (CNS) involvement.
Two patients were receiving NI-0501 as first-line treatment, and the rest were receiving the mAb as second-line treatment. Patients had previously received dexamethasone (n=13), methylprednisone (n=2), etoposide (n=13), ATG (n=4), cyclosporine A (n=6), and “other” therapy (n=4).
NI-0501 was given at a starting dose of 1 mg/kg every 3 days, with possible dose increases guided by pharmacokinetic data and/or clinical response in each patient. The mAb was administered with dexamethasone at a dose of 5mg/m2 to 10 mg/m2, but dexamethasone could be tapered during the treatment course.
The treatment duration ranged from 4 weeks to 8 weeks, and the follow-up period was 4 weeks.
Response and survival
One patient was excluded from the analysis due to a lymphoma diagnosis after enrollment. Two patients are still receiving treatment, and 13 have completed treatment.
Among the patients who completed therapy, 4 had an insufficient response. Two of these patients died, and 2 proceeded to allogeneic hematopoietic stem cell transplant (HSCT) after receiving additional agents to control their disease.
Nine patients achieved a favorable response to NI-0501. Seven of these patients proceeded to HSCT, and 2 are awaiting HSCT with their disease well-controlled.
Post-transplant follow-up is still early for most patients, but 2 patients have follow-up greater than 1 year. One child died of graft-vs-host disease around day 45, but the remaining patients who went on to HSCT are still alive.
Characteristics of response
For some patients, response to NI-0501 included a significant improvement in neutrophil count (8/10, P<0.001), platelet count (7/12, P<0.001), and ferritin level (P=0.0025). The median serum ferritin level was 4142 ng/mL at baseline and 1648 ng/mL at the end of treatment.
Both patients who were febrile at the start of treatment experienced rapid normalization of fever. Six of 7 patients with palpable spleen or liver at the start of treatment had an improvement in organomegaly. And 3 of 4 patients had resolution or improvement of CNS involvement.
Overall, there was a significant decrease in glucocorticoid dose. The median dose at baseline was 10.0 mg/m2. At the end of treatment, the median dose was 4.0 mg/m2 (P=0.023).
“One pharmacodynamic readout that’s useful for understanding IFNγ biology in vivo is CXCL9,” Dr Jordan noted. “This is secreted by mononuclear phagocytes in response to IFNγ. And most patients had a very clear fall in CXCL9 while receiving NI-0501.”
Adverse events and death
No off-target effects of NI-0501 have been observed, and none of the patients have withdrawn from the study for safety reasons.
There have been 14 serious adverse events in 8 patients, but only 1 of these events was considered treatment-related. The patient had necrotizing fasciitis following P aeruginosa skin infection, which resolved. This event was considered treatment-related by an investigator but not by the data monitoring committee or the sponsor.
In all, 3 patients have died, but none of the deaths were related to NI-0501. Two patients died of HLH/multi-organ failure, and 1 died of graft-vs-host disease.
Infections
“[NI-0501 provides] a targeted form of immune suppression, so we can expect that most concerns will be related to infection,” Dr Jordan said. “The effects of IFNγ on immune defense are actually predictable, and they’re predictable because of 2 patient populations.”
“First are the rare patients who are born with IFNγ-receptor deficiency, and second are individuals that develop neutralizing autoantibodies against IFNγ. Both patient populations experience infections with atypical mycobacteria, tuberculosis, Salmonella, and so forth.”
There were 10 infections already present at the start of the study—St epidermidis (n=1), C difficile (n=1), E coli (n=1, gram-positive), cytomegalovirus (n=1), Epstein-Barr virus (n=4), and parvovirus (n=1). All of these infections resolved with treatment.
Fourteen infections arose during the study course—St epidermidis (n=1), C difficile (n=1), P aeruginosa (n=1), K pneumoniae (n=1), E coli (1 gram-positive, 1 gram-negative), adenovirus (n=1), cytomegalovirus (n=2), Epstein-Barr virus (1 reactivation), parvovirus (1 reactivation), parainfluenza T3 (n=1), influenza A (n=1), and Candida (n=1).
Most of these infections resolved. The exceptions were the case of adenovirus, 1 case of cytomegalovirus (although there was improvement), the Epstein-Barr virus reactivation, the parvovirus reactivation (though improved), and the case of influenza A.
The researchers did not know if the parainfluenza T3 infection resolved. The patient’s viral status was not reassessed prior to death.
“So, in conclusion, NI-0501 has shown the potential to improve or resolve clinical and laboratory abnormalities of HLH, including CNS signs and symptoms,” Dr Jordan said. “The response to this agent appears to be independent of the underlying causative mutation. It’s also independent of the presence and type of infectious trigger.”
“NI-0501 was very well-tolerated. No safety concerns have emerged to date, and no infections known to be caused by deficiency of IFNγ have been observed. The neutralization of IFNγ by NI-0501 can offer an innovative and targeted approach to the management of HLH.” ![]()
*Data in the abstract differ from data presented at the meeting.

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—A monoclonal antibody (mAb) targeting interferon-gamma (IFNγ) has shown promise for treating hemophagocytic lymphohistiocytosis (HLH), according to a late-breaking abstract presented at the 2015 ASH Annual Meeting.
Results of an ongoing phase 2 study suggest the mAb, NI-0501, may be a feasible treatment option for patients with HLH who have demonstrated an unsatisfactory response to, or cannot tolerate, conventional therapy.
Nine of 13 evaluable patients achieved a “satisfactory response” to NI-0501, and no safety concerns were identified, said Michael Jordan, MD, of Cincinnati Children’s Hospital Medical Center in Ohio.
Dr Jordan presented these results at ASH as LBA-3.* The trial was sponsored by Novimmune.
“Treatment of HLH remains very challenging,” Dr Jordan noted. “Initial therapy is directed at trying to suppress the out-of-control immune response. In children that are at risk for recurrent episodes of HLH, they proceed to hematopoietic cell transplantation and, hopefully, this allows long-term survival.”
“First-line therapy has been defined in international trials and involves etoposide and dexamethasone. This regimen, as you might imagine, in children that present already with cytopenias, is myelosuppressive. It’s also broadly immune-suppressive. And although this does allow long-term survival in these children, there’s plenty of room for improvement in results.”
“[T]here is no standard of care for second-line therapy. Though there are no prospective data, children are increasingly treated with T-cell-depleting agents such as alemtuzumab and ATG, but this produces profound and long-lasting immune suppression. Though survival is not well-defined in these patients, it’s thought to be poor.”
In hopes of finding a new treatment option for HLH, Dr Jordan and his colleagues attempted to determine what drives the disease process. In preclinical studies, they identified IFNγ as a rational target in HLH. Blockade of IFNγ led to improved survival in mouse models.
The researchers also found elevated levels of IFNγ in patients with HLH. These preclinical and clinical data led to the development of NI-0501, a fully human, high affinity, anti-IFNγ mAb that binds to and neutralizes IFNγ.
Patients and treatment
In their phase 2 trial, Dr Jordan and his colleagues assessed NI-0501 in 16 patients—8 males and 8 females. Their median age was 1.2 years (range, 0.2-13). Twelve patients had causative mutations—FHL2 (n=4), FHL3 (n=2), FHL4 (n=1), GS-2 (n=3), XLP-1 (n=1), and XLP-2 (n=1). And 4 patients had central nervous system (CNS) involvement.
Two patients were receiving NI-0501 as first-line treatment, and the rest were receiving the mAb as second-line treatment. Patients had previously received dexamethasone (n=13), methylprednisone (n=2), etoposide (n=13), ATG (n=4), cyclosporine A (n=6), and “other” therapy (n=4).
NI-0501 was given at a starting dose of 1 mg/kg every 3 days, with possible dose increases guided by pharmacokinetic data and/or clinical response in each patient. The mAb was administered with dexamethasone at a dose of 5mg/m2 to 10 mg/m2, but dexamethasone could be tapered during the treatment course.
The treatment duration ranged from 4 weeks to 8 weeks, and the follow-up period was 4 weeks.
Response and survival
One patient was excluded from the analysis due to a lymphoma diagnosis after enrollment. Two patients are still receiving treatment, and 13 have completed treatment.
Among the patients who completed therapy, 4 had an insufficient response. Two of these patients died, and 2 proceeded to allogeneic hematopoietic stem cell transplant (HSCT) after receiving additional agents to control their disease.
Nine patients achieved a favorable response to NI-0501. Seven of these patients proceeded to HSCT, and 2 are awaiting HSCT with their disease well-controlled.
Post-transplant follow-up is still early for most patients, but 2 patients have follow-up greater than 1 year. One child died of graft-vs-host disease around day 45, but the remaining patients who went on to HSCT are still alive.
Characteristics of response
For some patients, response to NI-0501 included a significant improvement in neutrophil count (8/10, P<0.001), platelet count (7/12, P<0.001), and ferritin level (P=0.0025). The median serum ferritin level was 4142 ng/mL at baseline and 1648 ng/mL at the end of treatment.
Both patients who were febrile at the start of treatment experienced rapid normalization of fever. Six of 7 patients with palpable spleen or liver at the start of treatment had an improvement in organomegaly. And 3 of 4 patients had resolution or improvement of CNS involvement.
Overall, there was a significant decrease in glucocorticoid dose. The median dose at baseline was 10.0 mg/m2. At the end of treatment, the median dose was 4.0 mg/m2 (P=0.023).
“One pharmacodynamic readout that’s useful for understanding IFNγ biology in vivo is CXCL9,” Dr Jordan noted. “This is secreted by mononuclear phagocytes in response to IFNγ. And most patients had a very clear fall in CXCL9 while receiving NI-0501.”
Adverse events and death
No off-target effects of NI-0501 have been observed, and none of the patients have withdrawn from the study for safety reasons.
There have been 14 serious adverse events in 8 patients, but only 1 of these events was considered treatment-related. The patient had necrotizing fasciitis following P aeruginosa skin infection, which resolved. This event was considered treatment-related by an investigator but not by the data monitoring committee or the sponsor.
In all, 3 patients have died, but none of the deaths were related to NI-0501. Two patients died of HLH/multi-organ failure, and 1 died of graft-vs-host disease.
Infections
“[NI-0501 provides] a targeted form of immune suppression, so we can expect that most concerns will be related to infection,” Dr Jordan said. “The effects of IFNγ on immune defense are actually predictable, and they’re predictable because of 2 patient populations.”
“First are the rare patients who are born with IFNγ-receptor deficiency, and second are individuals that develop neutralizing autoantibodies against IFNγ. Both patient populations experience infections with atypical mycobacteria, tuberculosis, Salmonella, and so forth.”
There were 10 infections already present at the start of the study—St epidermidis (n=1), C difficile (n=1), E coli (n=1, gram-positive), cytomegalovirus (n=1), Epstein-Barr virus (n=4), and parvovirus (n=1). All of these infections resolved with treatment.
Fourteen infections arose during the study course—St epidermidis (n=1), C difficile (n=1), P aeruginosa (n=1), K pneumoniae (n=1), E coli (1 gram-positive, 1 gram-negative), adenovirus (n=1), cytomegalovirus (n=2), Epstein-Barr virus (1 reactivation), parvovirus (1 reactivation), parainfluenza T3 (n=1), influenza A (n=1), and Candida (n=1).
Most of these infections resolved. The exceptions were the case of adenovirus, 1 case of cytomegalovirus (although there was improvement), the Epstein-Barr virus reactivation, the parvovirus reactivation (though improved), and the case of influenza A.
The researchers did not know if the parainfluenza T3 infection resolved. The patient’s viral status was not reassessed prior to death.
“So, in conclusion, NI-0501 has shown the potential to improve or resolve clinical and laboratory abnormalities of HLH, including CNS signs and symptoms,” Dr Jordan said. “The response to this agent appears to be independent of the underlying causative mutation. It’s also independent of the presence and type of infectious trigger.”
“NI-0501 was very well-tolerated. No safety concerns have emerged to date, and no infections known to be caused by deficiency of IFNγ have been observed. The neutralization of IFNγ by NI-0501 can offer an innovative and targeted approach to the management of HLH.”
*Data in the abstract differ from data presented at the meeting.
Antiplatelet agent proves ineffective in SCD

Photo courtesy of St. Jude
Children’s Research Hospital
Treatment with the antiplatelet agent prasugrel does not significantly reduce the rate of pain crises or severe lung complications in children with sickle cell disease (SCD), according to one of the largest and most geographically diverse international trials on SCD to date.
The DOVE trial was a double blind, randomized, placebo-controlled phase 3 study conducted at 51 sites across 13 nations in the Americas, Europe, the Middle East, Asia, and Africa.
“Although we were disappointed that prasugrel does not appear to ease the suffering of children with sickle cell disease, the fact that this study incorporated patients in the wide range of countries where the disease occurs is hugely significant,” said Carolyn Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California.
“The logistical challenges that we addressed in designing and implementing the study can serve as a model for future research.”
The results of the study were published in NEJM. The research was sponsored by Daiichi Sankyo Company, Ltd. and Eli Lilly and Company.
The goal of the DOVE trial was to determine whether prasugrel could significantly reduce the rate of vaso-occlusive crises (VOCs)—defined as pain crises or acute chest syndrome—in children with SCD.
The trial enrolled 341 patients. About half of them (n=170) received daily oral prasugrel for between 9 and 24 months at individualized, blinded doses intended to maintain a selected target range of platelet activity. The remaining patients received a placebo.
All patients were monitored for VOCs prompting medical visits and for any increased risk of bleeding due to reduced platelet activity. In addition, patients 4 years old and older kept a daily electronic pain diary to aid in the reporting of painful events between visits.
At the end of the study period, there was no significant difference between the treatment arms in the overall rate of VOCs. The rate was 2.3 episodes per person-year in the prasugrel arm and 2.8 episodes per person-year in the placebo arm (P=0.12).
Similarly, prasugrel did not have a significant effect on the trial’s secondary outcome measures—VOC-related hospitalization rate, duration of hospitalization, time between VOCs, incidence of ischemic attack or ischemic stroke, transfusion rate, rate of pain, intensity of pain, use of analgesics, or missed school due to SCD-related pain.
The data did reveal a trend toward reduced VOC rates among patients ages 12 to 18 (P=0.06) and among patients who were not taking hydroxyurea (P=0.06). However, these trends were not statistically significant and require further research to determine their validity.
The investigators noted no adverse events related to prasugrel.
“Even though prasugrel did not achieve significant results, the findings should not detract from the fact that this team successfully completed a rigorous, sophisticated trial in a disease where the barriers to conducting large-scale international, patient-focused research are quite high,” said Matthew M. Heeney, MD, of the Dana–Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts.
To conduct the study successfully on such a broad geographical scale, the investigators had to address several obstacles, such as varying standards of care, local technological resources, and infrastructure challenges, such as a lack of reliable electrical power.

Photo courtesy of St. Jude
Children’s Research Hospital
Treatment with the antiplatelet agent prasugrel does not significantly reduce the rate of pain crises or severe lung complications in children with sickle cell disease (SCD), according to one of the largest and most geographically diverse international trials on SCD to date.
The DOVE trial was a double blind, randomized, placebo-controlled phase 3 study conducted at 51 sites across 13 nations in the Americas, Europe, the Middle East, Asia, and Africa.
“Although we were disappointed that prasugrel does not appear to ease the suffering of children with sickle cell disease, the fact that this study incorporated patients in the wide range of countries where the disease occurs is hugely significant,” said Carolyn Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California.
“The logistical challenges that we addressed in designing and implementing the study can serve as a model for future research.”
The results of the study were published in NEJM. The research was sponsored by Daiichi Sankyo Company, Ltd. and Eli Lilly and Company.
The goal of the DOVE trial was to determine whether prasugrel could significantly reduce the rate of vaso-occlusive crises (VOCs)—defined as pain crises or acute chest syndrome—in children with SCD.
The trial enrolled 341 patients. About half of them (n=170) received daily oral prasugrel for between 9 and 24 months at individualized, blinded doses intended to maintain a selected target range of platelet activity. The remaining patients received a placebo.
All patients were monitored for VOCs prompting medical visits and for any increased risk of bleeding due to reduced platelet activity. In addition, patients 4 years old and older kept a daily electronic pain diary to aid in the reporting of painful events between visits.
At the end of the study period, there was no significant difference between the treatment arms in the overall rate of VOCs. The rate was 2.3 episodes per person-year in the prasugrel arm and 2.8 episodes per person-year in the placebo arm (P=0.12).
Similarly, prasugrel did not have a significant effect on the trial’s secondary outcome measures—VOC-related hospitalization rate, duration of hospitalization, time between VOCs, incidence of ischemic attack or ischemic stroke, transfusion rate, rate of pain, intensity of pain, use of analgesics, or missed school due to SCD-related pain.
The data did reveal a trend toward reduced VOC rates among patients ages 12 to 18 (P=0.06) and among patients who were not taking hydroxyurea (P=0.06). However, these trends were not statistically significant and require further research to determine their validity.
The investigators noted no adverse events related to prasugrel.
“Even though prasugrel did not achieve significant results, the findings should not detract from the fact that this team successfully completed a rigorous, sophisticated trial in a disease where the barriers to conducting large-scale international, patient-focused research are quite high,” said Matthew M. Heeney, MD, of the Dana–Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts.
To conduct the study successfully on such a broad geographical scale, the investigators had to address several obstacles, such as varying standards of care, local technological resources, and infrastructure challenges, such as a lack of reliable electrical power.

Photo courtesy of St. Jude
Children’s Research Hospital
Treatment with the antiplatelet agent prasugrel does not significantly reduce the rate of pain crises or severe lung complications in children with sickle cell disease (SCD), according to one of the largest and most geographically diverse international trials on SCD to date.
The DOVE trial was a double blind, randomized, placebo-controlled phase 3 study conducted at 51 sites across 13 nations in the Americas, Europe, the Middle East, Asia, and Africa.
“Although we were disappointed that prasugrel does not appear to ease the suffering of children with sickle cell disease, the fact that this study incorporated patients in the wide range of countries where the disease occurs is hugely significant,” said Carolyn Hoppe, MD, of UCSF Benioff Children’s Hospital Oakland in California.
“The logistical challenges that we addressed in designing and implementing the study can serve as a model for future research.”
The results of the study were published in NEJM. The research was sponsored by Daiichi Sankyo Company, Ltd. and Eli Lilly and Company.
The goal of the DOVE trial was to determine whether prasugrel could significantly reduce the rate of vaso-occlusive crises (VOCs)—defined as pain crises or acute chest syndrome—in children with SCD.
The trial enrolled 341 patients. About half of them (n=170) received daily oral prasugrel for between 9 and 24 months at individualized, blinded doses intended to maintain a selected target range of platelet activity. The remaining patients received a placebo.
All patients were monitored for VOCs prompting medical visits and for any increased risk of bleeding due to reduced platelet activity. In addition, patients 4 years old and older kept a daily electronic pain diary to aid in the reporting of painful events between visits.
At the end of the study period, there was no significant difference between the treatment arms in the overall rate of VOCs. The rate was 2.3 episodes per person-year in the prasugrel arm and 2.8 episodes per person-year in the placebo arm (P=0.12).
Similarly, prasugrel did not have a significant effect on the trial’s secondary outcome measures—VOC-related hospitalization rate, duration of hospitalization, time between VOCs, incidence of ischemic attack or ischemic stroke, transfusion rate, rate of pain, intensity of pain, use of analgesics, or missed school due to SCD-related pain.
The data did reveal a trend toward reduced VOC rates among patients ages 12 to 18 (P=0.06) and among patients who were not taking hydroxyurea (P=0.06). However, these trends were not statistically significant and require further research to determine their validity.
The investigators noted no adverse events related to prasugrel.
“Even though prasugrel did not achieve significant results, the findings should not detract from the fact that this team successfully completed a rigorous, sophisticated trial in a disease where the barriers to conducting large-scale international, patient-focused research are quite high,” said Matthew M. Heeney, MD, of the Dana–Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts.
To conduct the study successfully on such a broad geographical scale, the investigators had to address several obstacles, such as varying standards of care, local technological resources, and infrastructure challenges, such as a lack of reliable electrical power.
Video: Eltrombopag boosted standard therapy in severe, newly-diagnosed aplastic anemia
ORLANDO – Adding eltrombopag to standard immunosuppressive treatment for newly-diagnosed severe aplastic anemia boosted overall response rates from around 65% to over 90%, based on a late-breaker study presented by Dr. Danielle M. Townsley at the annual meeting of the American Society of Hematology.
Dr. Townsley said that starting the combination treatment immediately at diagnosis, rather than waiting to introduce eltrombopag at either 2 weeks or 3 months after initiating standard immunosuppressive therapy, was associated with better outcomes. As a result of the findings, a cohort extension of the trial will continue and is enrolling patients.
In our video interview, Dr. Townsley discusses the top-level results and says that it’s too early to introduce the protocol into practice outside a clinical trial. She urges hematologists to enroll their patients in the ongoing cohort study.
On Twitter @maryjodales
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Adding eltrombopag to standard immunosuppressive treatment for newly-diagnosed severe aplastic anemia boosted overall response rates from around 65% to over 90%, based on a late-breaker study presented by Dr. Danielle M. Townsley at the annual meeting of the American Society of Hematology.
Dr. Townsley said that starting the combination treatment immediately at diagnosis, rather than waiting to introduce eltrombopag at either 2 weeks or 3 months after initiating standard immunosuppressive therapy, was associated with better outcomes. As a result of the findings, a cohort extension of the trial will continue and is enrolling patients.
In our video interview, Dr. Townsley discusses the top-level results and says that it’s too early to introduce the protocol into practice outside a clinical trial. She urges hematologists to enroll their patients in the ongoing cohort study.
On Twitter @maryjodales
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Adding eltrombopag to standard immunosuppressive treatment for newly-diagnosed severe aplastic anemia boosted overall response rates from around 65% to over 90%, based on a late-breaker study presented by Dr. Danielle M. Townsley at the annual meeting of the American Society of Hematology.
Dr. Townsley said that starting the combination treatment immediately at diagnosis, rather than waiting to introduce eltrombopag at either 2 weeks or 3 months after initiating standard immunosuppressive therapy, was associated with better outcomes. As a result of the findings, a cohort extension of the trial will continue and is enrolling patients.
In our video interview, Dr. Townsley discusses the top-level results and says that it’s too early to introduce the protocol into practice outside a clinical trial. She urges hematologists to enroll their patients in the ongoing cohort study.
On Twitter @maryjodales
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
ASH: Prasugrel does not reduce vaso-occlusive crises in sickle cell anemia
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
FROM ASH 2015
Key clinical point: Platelet inhibitor prasugrel does not reduce the rate of vaso-occlusive crises events in young patients with sickle cell anemia.
Major finding: Prasugrel did not achieve a significant reduction in vaso-occlusive crises, compared with placebo.
Data source: A phase III randomized placebo-controlled trial of 341 children and adolescents with sickle cell anemia.
Disclosures: Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.