User login
Think beyond BMI to optimize bariatric patients presurgery
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
MBSAQIP data helped target problem areas to cut readmissions
NEW YORK – Targeted interventions aimed at reducing patient readmission after bariatric surgery at a high-volume academic medical center led to a 61% overall decrease year over year. The center also saw a substantial reduction in readmissions linked to the top three factors of readmission identified by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, as well as a precipitous drop in the revisional surgery readmission rate.
“Our center, like so many others, has quarterly meetings in accordance with the MBSAQIP to look at our data. And this led to recognition of some common reasons for readmission,” said Chetan V. Aher, MD, a general surgeon at the department of surgery at Vanderbilt University Medical Center in Nashville, Tenn. Oral (PO) intolerance, dehydration, and nonemergent abdominal pain were the top reasons flagged by the MBSAQIP registry data at the medical center. Dr. Aher and his colleagues moved to focus on postoperative diet, administration of medications, management of patients who return to the hospital after surgery, and optimal staffing.
“Notably, the readmission rate for revisional procedures decreased by a whopping 90%,” Dr. Aher said. “I think a lot of these targeted interventions just really helped these patients who were at a higher risk to begin with to be readmitted.”
New dietary dos and don’ts
“We changed our postoperative diet,” Dr. Aher said. Instead of a soft food diet a couple of days after surgery, the full liquid diet was extended to 3 weeks post surgery.
The clinicians also implemented what they called a ‘no MEALS’ policy, which stands for no Meat, Eggs And Leftovers. “We were having problems with meat, although tender fish was okay, and some other things that went down easily,” Dr. Aher said at the American College of Surgeons Quality and Safety Conference. “We had some complaints about no eggs after surgery. A lot of patients love eggs,” he added. But they recommended avoiding eggs for 1 month after bariatric surgery to avoid nausea.
“Avoiding leftovers was also a big deal for patients,” Dr. Aher said. But patients who microwaved leftovers would “then come into the hospital with problems.”
Medication modifications
Another frequent cause of nausea was a “terrible and off-putting” taste when crushed tablets or medication capsules were added to the patient’s diet. Changing how patients took their medication “was a big help.” At the same time, there was a large institutional effort at Vanderbilt to start providing discharge medications in the hospital to increase postoperative compliance. “Bariatric surgery was one of the pilot programs for this,” Dr. Aher said. Discharge medications were filled by the pharmacy at Vanderbilt and delivered to the patient’s room, and a pharmacist or pharmacy intern explained how to use them. Compliance on medications increased, which may in turn have had an impact on readmissions.
Changes to patient management
Dr. Aher and his colleagues also changed where they treated patients who returned with problems. “Previously, when patients called in, the clinic diverted them to the emergency room. We stopped doing that, and increased our capacity to see these patients in the clinic instead.” This led to an increase in use of IV hydration in the clinic.
A meeting attendee asked if providing this service led to any problems with clinic capacity.
“Sometimes,” Dr. Aher said. “We don’t have a huge number of patients coming in for IV hydration, but when we had two come in on the same day, it did take up a couple of exam rooms.” To address this, the clinicians found other space in the clinic that would offer privacy for patients while not tying up exam rooms.
In addition, the clinic expanded nurse practitioner availability to 5 days a week to make the discharge process more consistent. “Of course, as we rolled all these things out, we made sure our educational material was updated accordingly,” Dr. Aher said.
The study demonstrates that a collaborative team effort and targeted interventions can result in a significant reduction in readmissions, Dr. Aher said. “Regular quality focused meetings are really important to facilitate recognition of various areas for improvement, especially in a high-volume center. Introducing an MBSAQIP registry serves as an excellent tool to effect these changes,” he said.
Dr. Aher had no relevant financial disclosures.
NEW YORK – Targeted interventions aimed at reducing patient readmission after bariatric surgery at a high-volume academic medical center led to a 61% overall decrease year over year. The center also saw a substantial reduction in readmissions linked to the top three factors of readmission identified by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, as well as a precipitous drop in the revisional surgery readmission rate.
“Our center, like so many others, has quarterly meetings in accordance with the MBSAQIP to look at our data. And this led to recognition of some common reasons for readmission,” said Chetan V. Aher, MD, a general surgeon at the department of surgery at Vanderbilt University Medical Center in Nashville, Tenn. Oral (PO) intolerance, dehydration, and nonemergent abdominal pain were the top reasons flagged by the MBSAQIP registry data at the medical center. Dr. Aher and his colleagues moved to focus on postoperative diet, administration of medications, management of patients who return to the hospital after surgery, and optimal staffing.
“Notably, the readmission rate for revisional procedures decreased by a whopping 90%,” Dr. Aher said. “I think a lot of these targeted interventions just really helped these patients who were at a higher risk to begin with to be readmitted.”
New dietary dos and don’ts
“We changed our postoperative diet,” Dr. Aher said. Instead of a soft food diet a couple of days after surgery, the full liquid diet was extended to 3 weeks post surgery.
The clinicians also implemented what they called a ‘no MEALS’ policy, which stands for no Meat, Eggs And Leftovers. “We were having problems with meat, although tender fish was okay, and some other things that went down easily,” Dr. Aher said at the American College of Surgeons Quality and Safety Conference. “We had some complaints about no eggs after surgery. A lot of patients love eggs,” he added. But they recommended avoiding eggs for 1 month after bariatric surgery to avoid nausea.
“Avoiding leftovers was also a big deal for patients,” Dr. Aher said. But patients who microwaved leftovers would “then come into the hospital with problems.”
Medication modifications
Another frequent cause of nausea was a “terrible and off-putting” taste when crushed tablets or medication capsules were added to the patient’s diet. Changing how patients took their medication “was a big help.” At the same time, there was a large institutional effort at Vanderbilt to start providing discharge medications in the hospital to increase postoperative compliance. “Bariatric surgery was one of the pilot programs for this,” Dr. Aher said. Discharge medications were filled by the pharmacy at Vanderbilt and delivered to the patient’s room, and a pharmacist or pharmacy intern explained how to use them. Compliance on medications increased, which may in turn have had an impact on readmissions.
Changes to patient management
Dr. Aher and his colleagues also changed where they treated patients who returned with problems. “Previously, when patients called in, the clinic diverted them to the emergency room. We stopped doing that, and increased our capacity to see these patients in the clinic instead.” This led to an increase in use of IV hydration in the clinic.
A meeting attendee asked if providing this service led to any problems with clinic capacity.
“Sometimes,” Dr. Aher said. “We don’t have a huge number of patients coming in for IV hydration, but when we had two come in on the same day, it did take up a couple of exam rooms.” To address this, the clinicians found other space in the clinic that would offer privacy for patients while not tying up exam rooms.
In addition, the clinic expanded nurse practitioner availability to 5 days a week to make the discharge process more consistent. “Of course, as we rolled all these things out, we made sure our educational material was updated accordingly,” Dr. Aher said.
The study demonstrates that a collaborative team effort and targeted interventions can result in a significant reduction in readmissions, Dr. Aher said. “Regular quality focused meetings are really important to facilitate recognition of various areas for improvement, especially in a high-volume center. Introducing an MBSAQIP registry serves as an excellent tool to effect these changes,” he said.
Dr. Aher had no relevant financial disclosures.
NEW YORK – Targeted interventions aimed at reducing patient readmission after bariatric surgery at a high-volume academic medical center led to a 61% overall decrease year over year. The center also saw a substantial reduction in readmissions linked to the top three factors of readmission identified by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, as well as a precipitous drop in the revisional surgery readmission rate.
“Our center, like so many others, has quarterly meetings in accordance with the MBSAQIP to look at our data. And this led to recognition of some common reasons for readmission,” said Chetan V. Aher, MD, a general surgeon at the department of surgery at Vanderbilt University Medical Center in Nashville, Tenn. Oral (PO) intolerance, dehydration, and nonemergent abdominal pain were the top reasons flagged by the MBSAQIP registry data at the medical center. Dr. Aher and his colleagues moved to focus on postoperative diet, administration of medications, management of patients who return to the hospital after surgery, and optimal staffing.
“Notably, the readmission rate for revisional procedures decreased by a whopping 90%,” Dr. Aher said. “I think a lot of these targeted interventions just really helped these patients who were at a higher risk to begin with to be readmitted.”
New dietary dos and don’ts
“We changed our postoperative diet,” Dr. Aher said. Instead of a soft food diet a couple of days after surgery, the full liquid diet was extended to 3 weeks post surgery.
The clinicians also implemented what they called a ‘no MEALS’ policy, which stands for no Meat, Eggs And Leftovers. “We were having problems with meat, although tender fish was okay, and some other things that went down easily,” Dr. Aher said at the American College of Surgeons Quality and Safety Conference. “We had some complaints about no eggs after surgery. A lot of patients love eggs,” he added. But they recommended avoiding eggs for 1 month after bariatric surgery to avoid nausea.
“Avoiding leftovers was also a big deal for patients,” Dr. Aher said. But patients who microwaved leftovers would “then come into the hospital with problems.”
Medication modifications
Another frequent cause of nausea was a “terrible and off-putting” taste when crushed tablets or medication capsules were added to the patient’s diet. Changing how patients took their medication “was a big help.” At the same time, there was a large institutional effort at Vanderbilt to start providing discharge medications in the hospital to increase postoperative compliance. “Bariatric surgery was one of the pilot programs for this,” Dr. Aher said. Discharge medications were filled by the pharmacy at Vanderbilt and delivered to the patient’s room, and a pharmacist or pharmacy intern explained how to use them. Compliance on medications increased, which may in turn have had an impact on readmissions.
Changes to patient management
Dr. Aher and his colleagues also changed where they treated patients who returned with problems. “Previously, when patients called in, the clinic diverted them to the emergency room. We stopped doing that, and increased our capacity to see these patients in the clinic instead.” This led to an increase in use of IV hydration in the clinic.
A meeting attendee asked if providing this service led to any problems with clinic capacity.
“Sometimes,” Dr. Aher said. “We don’t have a huge number of patients coming in for IV hydration, but when we had two come in on the same day, it did take up a couple of exam rooms.” To address this, the clinicians found other space in the clinic that would offer privacy for patients while not tying up exam rooms.
In addition, the clinic expanded nurse practitioner availability to 5 days a week to make the discharge process more consistent. “Of course, as we rolled all these things out, we made sure our educational material was updated accordingly,” Dr. Aher said.
The study demonstrates that a collaborative team effort and targeted interventions can result in a significant reduction in readmissions, Dr. Aher said. “Regular quality focused meetings are really important to facilitate recognition of various areas for improvement, especially in a high-volume center. Introducing an MBSAQIP registry serves as an excellent tool to effect these changes,” he said.
Dr. Aher had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Key clinical point: A collaborative effort and target interventions can successfully reduce bariatric surgery readmissions.
Major finding: The overall bariatric surgery readmission rate dropped 61% in the year after intervention compared to the previous year.
Data source: Comparison of 471 bariatric procedures in 2015 to 539 others in 2016 at Vanderbilt University Medical Center.
Disclosures: Dr. Aher had no relevant financial disclosures.
Safety alert for intragastric balloon systems
The Food and Drug Administration announced a safety alert on Aug. 10, 2017, for liquid-filled intragastric balloon systems, as they have caused five reports of unanticipated deaths that occurred from 2016 to present in patients.
The cause or incidence of patient death is still unknown, and the FDA has not been able to definitively attribute the deaths to the devices or the insertion procedures for these devices. All five reports show that patient deaths occurred within a month or less of balloon placement. In three of the reports, death occurred as soon as 1-3 days after balloon placement. The FDA has also received two additional reports of deaths in the same time period related to potential complications associated with balloon treatment.
The FDA continues to recommend that health care providers closely monitor patients treated with these devices for complications. Any adverse events related to intragastric balloon systems should be reported through MedWatch. The FDA will keep the public informed as new information becomes available.
Read the full safety alert on the FDA’s website.
The Food and Drug Administration announced a safety alert on Aug. 10, 2017, for liquid-filled intragastric balloon systems, as they have caused five reports of unanticipated deaths that occurred from 2016 to present in patients.
The cause or incidence of patient death is still unknown, and the FDA has not been able to definitively attribute the deaths to the devices or the insertion procedures for these devices. All five reports show that patient deaths occurred within a month or less of balloon placement. In three of the reports, death occurred as soon as 1-3 days after balloon placement. The FDA has also received two additional reports of deaths in the same time period related to potential complications associated with balloon treatment.
The FDA continues to recommend that health care providers closely monitor patients treated with these devices for complications. Any adverse events related to intragastric balloon systems should be reported through MedWatch. The FDA will keep the public informed as new information becomes available.
Read the full safety alert on the FDA’s website.
The Food and Drug Administration announced a safety alert on Aug. 10, 2017, for liquid-filled intragastric balloon systems, as they have caused five reports of unanticipated deaths that occurred from 2016 to present in patients.
The cause or incidence of patient death is still unknown, and the FDA has not been able to definitively attribute the deaths to the devices or the insertion procedures for these devices. All five reports show that patient deaths occurred within a month or less of balloon placement. In three of the reports, death occurred as soon as 1-3 days after balloon placement. The FDA has also received two additional reports of deaths in the same time period related to potential complications associated with balloon treatment.
The FDA continues to recommend that health care providers closely monitor patients treated with these devices for complications. Any adverse events related to intragastric balloon systems should be reported through MedWatch. The FDA will keep the public informed as new information becomes available.
Read the full safety alert on the FDA’s website.
Fluid protocol takes aim at bariatric surgery readmissions
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
NEW YORK – With dehydration considered a contributor to hospital readmission after bariatric weight loss surgery, a multidisciplinary team of clinicians searched for a way to get patients to drink up. Specifically,
The project results were presented at a poster session at the American College of Surgeons Quality and Safety Conference.
“Our QI project was to streamline that process to ultimately eliminate or decrease those readmits,” Ms. Melei said.
They used 8-ounce water bottles. To track water consumption, they also numbered the bottles one through six for each patient. One-ounce cups were used during mealtimes. RNs, certified nursing assistants, and food service staff were educated about the fluid intake initiative. Only fluids provided by nursing were permitted and patients also received a clear message about fluid goals.
Another focus was standardizing communication with patients. They were not getting a consistent message from staff on what to expect before, during, and after surgery. “So we had to make sure [we] were all saying the same thing.”
The nurses and the other staff now ask the patients “Did you finish the bottle?” or “Where are you with the bottles?” Ms. Melei said. “At the end of a shift, the nurses document fluid consumption.”
During a 2-month baseline period, 12 patients drank an average 381.5 mL over 24 hours. Since the close of the project, the average daily fluid intake for patients undergoing bariatric surgery is 1,007 mL. In 12 months post implementation, average fluid intake for 39 patients jumped to 1,109.5 mL over 24 hours. “It was just such a hugely successful program. We had buy-in from every department, it worked really well, and we had great results,” said Cheryl Williams, the current bariatric program coordinator at Greenwich Hospital.
Sometimes dehydrated patients present to an emergency department complaining of vomiting, headache, and dizziness if they are not properly hydrated after surgery, Ms. Williams said. “Preventing dehydration helps to improve the patient’s recovery, as well as decrease emergency room visits and hospital admissions.”
Ashutosh Kaul, MD, FACS, medical director of the bariatric surgery program at Greenwich Hospital, said this study shows the importance of team building to improve patient care. “We built a core team that implemented a simple, low-cost, structured, and well-defined water distribution and documentation process, which resulted in better compliance of water intake. This reduced variability and improved postoperative intake progression, and we are presently studying its effect on reduction of readmissions and facilitating early discharge.”
Greenwich Hospital’s bariatric surgery center is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery. Ms. Williams and Ms. Melei had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Key clinical point: QI project to increase water intake after bariatric surgery could decrease hospital readmission rates.
Major finding: Multidisciplinary protocol increases 24-hour fluid intake from 382 mL to 1,110 mL on average.
Data source: Comparison of water consumed by 12 patients before versus 39 patients after implementation.
Disclosures: Ms. Williams and Ms. Melei had no relevant financial disclosures.
Better bariatric surgery outcomes with lower preoperative BMI
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
FROM JAMA SURGERY
Key clinical point: A BMI below 40 prior to undergoing bariatric surgery gives patients a significantly better chance of achieving a 1-year postoperative BMI under 30.
Major finding: Obese patients with a BMI less than 40 before undergoing bariatric surgery are more than 12 times more likely to achieve a postoperative BMI of under 30.
Data source: A retrospective study using prospectively gathered clinical data of 27, 320 adults who underwent bariatric surgery.
Disclosures: Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Imaging after bariatric surgery appears overdone
Nearly 70% of bariatric surgery patients received postoperative imaging, with more than one-third receiving CT imaging. This high level of screening resulted in symptom-related findings in only 23% of cases, and may be excessive, according to researchers who studied nearly 600 adults who underwent bariatric surgery.
As the volume of bariatric surgery has increased, so has the role of postoperative imaging, wrote Dana Haddad, MD, and her colleagues at Harlem Hospital Center, New York.
“However, there is a lack of well-defined postoperative imaging guidelines,” they said. “Detrimental aspects of postoperative imaging include the potential for false-positive findings leading to further and often unnecessary investigations, radiation exposure, and additional cost,” they added.
The primary outcomes were the numbers of initial postimaging studies and whether the findings supported subsequent studies.
The study population included 399 adults who underwent laparoscopic bypass and 144 who underwent sleeve gastrectomy. The average age of the patients was 41 years and 90% were women.
The researchers identified 907 imaging studies performed in 400 patients (69% of the study population). Of these, 38% were ultrasound, 36% were CT, 15% were x-ray, 6.6% were fluoroscopy, 3.3% were MRI, and .6% were nuclear medicine.
On review of the imaging findings, the researchers found that half (50%) were unremarkable, while 13% were either surgery related or symptom related, 6.8% were not related to surgery but might have explained patients’ symptoms, 4.3% were surgery-related but not likely to explain symptoms, and 26% were incidental. “Interestingly, no incidental findings were found to be of major clinical importance; all were benign,” according to the researchers.
However, incidental findings led to a total of 71 additional studies, and to 5 laparoscopic cholecystectomies.
A univariate analysis showed that the factors with a significant impact a patient’s odds of undergoing postoperative abdominal imaging included having a bypass procedure vs. a sleeve procedure, older age, and lower baseline body mass index. In addition, patients with a history of abdominal surgery or dyspepsia or those who had a routine postoperative upper gastrointestinal series were significantly more likely to undergo CT scans. Patients with history of ulcer or reflux were significantly less likely to undergo CT scans.
Although the study was limited by the retrospective design and lack of information about possible imaging of patients at other centers, “results suggest that nonroutine postoperative abdominal imaging in the bariatric population is common and requires streamlined protocols, with almost 70% of patients undergoing imaging and greater than 70% of findings being unrelated to symptoms or negative,” the researchers said.
A clinical algorithm for imaging of bariatric patients should be based on clinical parameters collected during a physical exam. “Once an algorithm is in place, further studies will be needed to validate its accuracy and efficiency,” the researchers stated.
Dr. Haddad and her colleagues had no financial conflicts to disclose.
Nearly 70% of bariatric surgery patients received postoperative imaging, with more than one-third receiving CT imaging. This high level of screening resulted in symptom-related findings in only 23% of cases, and may be excessive, according to researchers who studied nearly 600 adults who underwent bariatric surgery.
As the volume of bariatric surgery has increased, so has the role of postoperative imaging, wrote Dana Haddad, MD, and her colleagues at Harlem Hospital Center, New York.
“However, there is a lack of well-defined postoperative imaging guidelines,” they said. “Detrimental aspects of postoperative imaging include the potential for false-positive findings leading to further and often unnecessary investigations, radiation exposure, and additional cost,” they added.
The primary outcomes were the numbers of initial postimaging studies and whether the findings supported subsequent studies.
The study population included 399 adults who underwent laparoscopic bypass and 144 who underwent sleeve gastrectomy. The average age of the patients was 41 years and 90% were women.
The researchers identified 907 imaging studies performed in 400 patients (69% of the study population). Of these, 38% were ultrasound, 36% were CT, 15% were x-ray, 6.6% were fluoroscopy, 3.3% were MRI, and .6% were nuclear medicine.
On review of the imaging findings, the researchers found that half (50%) were unremarkable, while 13% were either surgery related or symptom related, 6.8% were not related to surgery but might have explained patients’ symptoms, 4.3% were surgery-related but not likely to explain symptoms, and 26% were incidental. “Interestingly, no incidental findings were found to be of major clinical importance; all were benign,” according to the researchers.
However, incidental findings led to a total of 71 additional studies, and to 5 laparoscopic cholecystectomies.
A univariate analysis showed that the factors with a significant impact a patient’s odds of undergoing postoperative abdominal imaging included having a bypass procedure vs. a sleeve procedure, older age, and lower baseline body mass index. In addition, patients with a history of abdominal surgery or dyspepsia or those who had a routine postoperative upper gastrointestinal series were significantly more likely to undergo CT scans. Patients with history of ulcer or reflux were significantly less likely to undergo CT scans.
Although the study was limited by the retrospective design and lack of information about possible imaging of patients at other centers, “results suggest that nonroutine postoperative abdominal imaging in the bariatric population is common and requires streamlined protocols, with almost 70% of patients undergoing imaging and greater than 70% of findings being unrelated to symptoms or negative,” the researchers said.
A clinical algorithm for imaging of bariatric patients should be based on clinical parameters collected during a physical exam. “Once an algorithm is in place, further studies will be needed to validate its accuracy and efficiency,” the researchers stated.
Dr. Haddad and her colleagues had no financial conflicts to disclose.
Nearly 70% of bariatric surgery patients received postoperative imaging, with more than one-third receiving CT imaging. This high level of screening resulted in symptom-related findings in only 23% of cases, and may be excessive, according to researchers who studied nearly 600 adults who underwent bariatric surgery.
As the volume of bariatric surgery has increased, so has the role of postoperative imaging, wrote Dana Haddad, MD, and her colleagues at Harlem Hospital Center, New York.
“However, there is a lack of well-defined postoperative imaging guidelines,” they said. “Detrimental aspects of postoperative imaging include the potential for false-positive findings leading to further and often unnecessary investigations, radiation exposure, and additional cost,” they added.
The primary outcomes were the numbers of initial postimaging studies and whether the findings supported subsequent studies.
The study population included 399 adults who underwent laparoscopic bypass and 144 who underwent sleeve gastrectomy. The average age of the patients was 41 years and 90% were women.
The researchers identified 907 imaging studies performed in 400 patients (69% of the study population). Of these, 38% were ultrasound, 36% were CT, 15% were x-ray, 6.6% were fluoroscopy, 3.3% were MRI, and .6% were nuclear medicine.
On review of the imaging findings, the researchers found that half (50%) were unremarkable, while 13% were either surgery related or symptom related, 6.8% were not related to surgery but might have explained patients’ symptoms, 4.3% were surgery-related but not likely to explain symptoms, and 26% were incidental. “Interestingly, no incidental findings were found to be of major clinical importance; all were benign,” according to the researchers.
However, incidental findings led to a total of 71 additional studies, and to 5 laparoscopic cholecystectomies.
A univariate analysis showed that the factors with a significant impact a patient’s odds of undergoing postoperative abdominal imaging included having a bypass procedure vs. a sleeve procedure, older age, and lower baseline body mass index. In addition, patients with a history of abdominal surgery or dyspepsia or those who had a routine postoperative upper gastrointestinal series were significantly more likely to undergo CT scans. Patients with history of ulcer or reflux were significantly less likely to undergo CT scans.
Although the study was limited by the retrospective design and lack of information about possible imaging of patients at other centers, “results suggest that nonroutine postoperative abdominal imaging in the bariatric population is common and requires streamlined protocols, with almost 70% of patients undergoing imaging and greater than 70% of findings being unrelated to symptoms or negative,” the researchers said.
A clinical algorithm for imaging of bariatric patients should be based on clinical parameters collected during a physical exam. “Once an algorithm is in place, further studies will be needed to validate its accuracy and efficiency,” the researchers stated.
Dr. Haddad and her colleagues had no financial conflicts to disclose.
FROM SURGERY FOR OBESITY AND RELATED DISEASES
Key clinical point: No well-defined guidelines exist for when to use postoperative imaging in bariatric surgery patients.
Major finding: Approximately 70% of postoperative imaging findings were not symptom related, and incidental findings led to 71 additional studies.
Data source: A review of 578 patients who underwent gastric bypass or sleeve gastrectomy.
Disclosures: The researchers had no financial conflicts to disclose.
Rural patients less likely to have bariatric surgery
Obese patients living in rural areas of West Virginia were substantially less likely than were their urban and suburban counterparts to have bariatric surgery, according to findings from a study comparing outcomes in two patient groups.
This discrepancy is attributed to a difference between rural and nonrural patients in type of insurance coverage. In this 2-year study, rural patients were nearly five times more likely to be covered by West Virginia Medicaid than were patients living in nonrural areas of the state, said Kristie L. Bergmann, PhD, of the department of behavioral medicine and psychiatry, West Virginia University, Morgantown, and her associates. The findings were published in Surgery for Obesity and Related Diseases (2017;13[4]:632-6), the journal of the American Society for Metabolic and Bariatric Surgery.
Previous research has identified rural patients’ lack of insurance as a barrier to health care. “Our results suggest that insurance denial represents a successive barrier. Despite being insured, rural individuals may be barred from surgery if insurance carriers do not offer it as a covered benefit, deny approval, or require indomitable prerequisites for surgery,” Dr. Bergmann and her associates said.
They examined the associations among rural status, access to bariatric surgery, and surgical outcomes in West Virginia in part because the state’s residents “have been consistently ranked as the most obese population in the United States, with approximately 35.1% of residents meeting criteria for obesity.” West Virginia also has the highest rates of diabetes (13%) and hypertension (41%) in the United States.
At the same time, rural populations are known to have decreased access to all forms of health care and specifically to bariatric surgery. This makes rural West Virginians “a particularly vulnerable population of interest,” the investigators said.
They performed a retrospective cohort study involving 122 obese patients seeking bariatric surgery at their university’s medical center during 2012-2014. A total of 97% of these patients were white, 83% were women, and the mean age was 47 years. Only 82 of the 122 study participants underwent bariatric surgery: 77 had Roux-en-Y gastric bypass and 5 had sleeve gastrectomy.
Rural residents were significantly less likely to undergo bariatric surgery than were nonrural patients, but coverage by West Virginia Medicaid explained 83.6% of this difference. When Medicaid patients were excluded from the analysis, nonrural status no longer predicted the use of bariatric surgery.
Moreover, when Medicaid coverage was controlled for, rural status had no effect on the effectiveness of bariatric surgery. Patients residing in rural areas had the same attendance at follow-up visits and the same reduction in body mass index at 6 months and at 12 months as did nonrural patients.
In addition, patients who had higher levels of education and who worked full-time were more likely to undergo bariatric surgery, but overall, rural patients were more likely to have comorbidities, disability, and lower rates of full-time work. “An argument can be made that rural individuals may have a greater medical need for bariatric surgery, as obesity and associated health conditions may contribute to lower rates of employment. Unfortunately, barring these patients from receiving care may reinforce a cycle of disability and declining health status,” Dr. Bergmann and her associates noted.
This study was limited in that it had a relatively small sample size, particularly in analyses that excluded Medicaid recipients. It also had a follow-up of only 1 year, so longer-term outcomes of bariatric surgery could not be assessed. “Our sample is also predominantly Caucasian and may have unique culturally-based characteristics” that limit the generalizability of the study findings, they added.
No specific sponsor was cited for this study. Dr. Bergmann and her associates reported having no relevant financial disclosures.
Obese patients living in rural areas of West Virginia were substantially less likely than were their urban and suburban counterparts to have bariatric surgery, according to findings from a study comparing outcomes in two patient groups.
This discrepancy is attributed to a difference between rural and nonrural patients in type of insurance coverage. In this 2-year study, rural patients were nearly five times more likely to be covered by West Virginia Medicaid than were patients living in nonrural areas of the state, said Kristie L. Bergmann, PhD, of the department of behavioral medicine and psychiatry, West Virginia University, Morgantown, and her associates. The findings were published in Surgery for Obesity and Related Diseases (2017;13[4]:632-6), the journal of the American Society for Metabolic and Bariatric Surgery.
Previous research has identified rural patients’ lack of insurance as a barrier to health care. “Our results suggest that insurance denial represents a successive barrier. Despite being insured, rural individuals may be barred from surgery if insurance carriers do not offer it as a covered benefit, deny approval, or require indomitable prerequisites for surgery,” Dr. Bergmann and her associates said.
They examined the associations among rural status, access to bariatric surgery, and surgical outcomes in West Virginia in part because the state’s residents “have been consistently ranked as the most obese population in the United States, with approximately 35.1% of residents meeting criteria for obesity.” West Virginia also has the highest rates of diabetes (13%) and hypertension (41%) in the United States.
At the same time, rural populations are known to have decreased access to all forms of health care and specifically to bariatric surgery. This makes rural West Virginians “a particularly vulnerable population of interest,” the investigators said.
They performed a retrospective cohort study involving 122 obese patients seeking bariatric surgery at their university’s medical center during 2012-2014. A total of 97% of these patients were white, 83% were women, and the mean age was 47 years. Only 82 of the 122 study participants underwent bariatric surgery: 77 had Roux-en-Y gastric bypass and 5 had sleeve gastrectomy.
Rural residents were significantly less likely to undergo bariatric surgery than were nonrural patients, but coverage by West Virginia Medicaid explained 83.6% of this difference. When Medicaid patients were excluded from the analysis, nonrural status no longer predicted the use of bariatric surgery.
Moreover, when Medicaid coverage was controlled for, rural status had no effect on the effectiveness of bariatric surgery. Patients residing in rural areas had the same attendance at follow-up visits and the same reduction in body mass index at 6 months and at 12 months as did nonrural patients.
In addition, patients who had higher levels of education and who worked full-time were more likely to undergo bariatric surgery, but overall, rural patients were more likely to have comorbidities, disability, and lower rates of full-time work. “An argument can be made that rural individuals may have a greater medical need for bariatric surgery, as obesity and associated health conditions may contribute to lower rates of employment. Unfortunately, barring these patients from receiving care may reinforce a cycle of disability and declining health status,” Dr. Bergmann and her associates noted.
This study was limited in that it had a relatively small sample size, particularly in analyses that excluded Medicaid recipients. It also had a follow-up of only 1 year, so longer-term outcomes of bariatric surgery could not be assessed. “Our sample is also predominantly Caucasian and may have unique culturally-based characteristics” that limit the generalizability of the study findings, they added.
No specific sponsor was cited for this study. Dr. Bergmann and her associates reported having no relevant financial disclosures.
Obese patients living in rural areas of West Virginia were substantially less likely than were their urban and suburban counterparts to have bariatric surgery, according to findings from a study comparing outcomes in two patient groups.
This discrepancy is attributed to a difference between rural and nonrural patients in type of insurance coverage. In this 2-year study, rural patients were nearly five times more likely to be covered by West Virginia Medicaid than were patients living in nonrural areas of the state, said Kristie L. Bergmann, PhD, of the department of behavioral medicine and psychiatry, West Virginia University, Morgantown, and her associates. The findings were published in Surgery for Obesity and Related Diseases (2017;13[4]:632-6), the journal of the American Society for Metabolic and Bariatric Surgery.
Previous research has identified rural patients’ lack of insurance as a barrier to health care. “Our results suggest that insurance denial represents a successive barrier. Despite being insured, rural individuals may be barred from surgery if insurance carriers do not offer it as a covered benefit, deny approval, or require indomitable prerequisites for surgery,” Dr. Bergmann and her associates said.
They examined the associations among rural status, access to bariatric surgery, and surgical outcomes in West Virginia in part because the state’s residents “have been consistently ranked as the most obese population in the United States, with approximately 35.1% of residents meeting criteria for obesity.” West Virginia also has the highest rates of diabetes (13%) and hypertension (41%) in the United States.
At the same time, rural populations are known to have decreased access to all forms of health care and specifically to bariatric surgery. This makes rural West Virginians “a particularly vulnerable population of interest,” the investigators said.
They performed a retrospective cohort study involving 122 obese patients seeking bariatric surgery at their university’s medical center during 2012-2014. A total of 97% of these patients were white, 83% were women, and the mean age was 47 years. Only 82 of the 122 study participants underwent bariatric surgery: 77 had Roux-en-Y gastric bypass and 5 had sleeve gastrectomy.
Rural residents were significantly less likely to undergo bariatric surgery than were nonrural patients, but coverage by West Virginia Medicaid explained 83.6% of this difference. When Medicaid patients were excluded from the analysis, nonrural status no longer predicted the use of bariatric surgery.
Moreover, when Medicaid coverage was controlled for, rural status had no effect on the effectiveness of bariatric surgery. Patients residing in rural areas had the same attendance at follow-up visits and the same reduction in body mass index at 6 months and at 12 months as did nonrural patients.
In addition, patients who had higher levels of education and who worked full-time were more likely to undergo bariatric surgery, but overall, rural patients were more likely to have comorbidities, disability, and lower rates of full-time work. “An argument can be made that rural individuals may have a greater medical need for bariatric surgery, as obesity and associated health conditions may contribute to lower rates of employment. Unfortunately, barring these patients from receiving care may reinforce a cycle of disability and declining health status,” Dr. Bergmann and her associates noted.
This study was limited in that it had a relatively small sample size, particularly in analyses that excluded Medicaid recipients. It also had a follow-up of only 1 year, so longer-term outcomes of bariatric surgery could not be assessed. “Our sample is also predominantly Caucasian and may have unique culturally-based characteristics” that limit the generalizability of the study findings, they added.
No specific sponsor was cited for this study. Dr. Bergmann and her associates reported having no relevant financial disclosures.
FROM SURGERY FOR OBESITY AND RELATED DISEASES
Key clinical point: Obese patients living in rural areas of West Virginia are substantially less likely than are their urban and suburban counterparts to have bariatric surgery.
Major finding: Rural residents were significantly less likely to undergo bariatric surgery than were nonrural patients, but coverage by West Virginia Medicaid explained 83.6% of this difference.
Data source: A retrospective single-center cohort study involving 122 obese West Virginians seeking bariatric surgery in 2012-2014.
Disclosures: No specific sponsor was cited for this study. Dr. Bergmann and her associates reported having no relevant financial disclosures.
Gastric bands hit with high reoperation rates, rising costs
About one in five laparoscopic gastric band surgeries result in device-related reoperations and reoperations account for almost half of all Medicare expenditures for gastric band surgery, a large retrospective study has found.
The laparoscopic adjustable gastric band for treatment of morbid obesity, approved in 2001 by the Food and Drug Administration, was once a common choice for bariatric patients. Although its use has declined from in recent years, the American Society for Metabolic and Bariatric Surgery estimated that 11,000 bands were placed in 2015 and many others remain in place (ASMBS, Estimate of bariatric surgery numbers, 2011-2015, https://goo.gl/f8iByl). Many of these gastric bands will need to be removed, replaced, or revised in a series of procedures over the coming years.
Of the 24,042 gastric band patients in this study group, 4,636 (18.5%) underwent reoperation, defined as band removal, band replacement, or revision to a different bariatric procedure, but not including band size adjustment. Patients who had reoperations were more likely to be women, to be white, and to have slightly lower rates of hypertension and diabetes. But they were also more likely to have received a psychiatric, anemia, or electrolyte disorder diagnosis at the time of their index operations.
Among the 4,636 patients who had reoperations, 17,539 such procedures were performed, an average of 3.8 procedures per patient, in addition to the index operation, over an average follow-up of 4.5 years. The most common reoperation was for band removal (41.8%). Other reasons included conversion to laparoscopic Roux-en-Y gastric bypass (13.1%) or laparoscopic sleeve gastrectomy (5.3%).
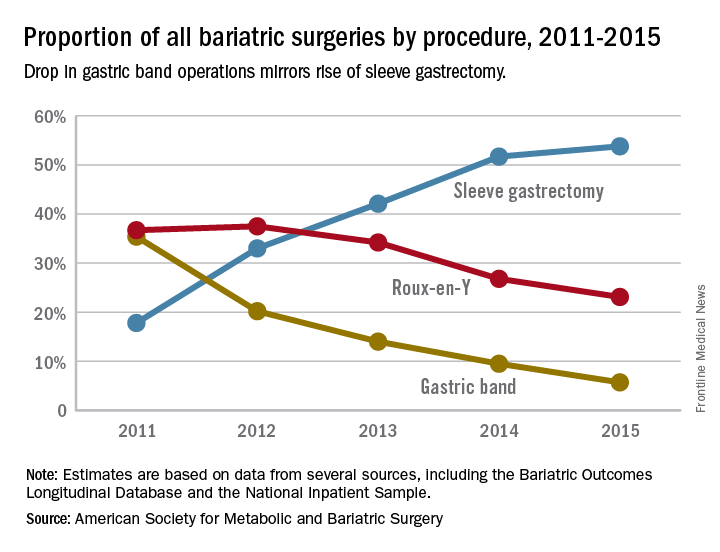
The study also looked at the regional differences, reflecting the comparative success of some programs in managing laparoscopic gastric band placement. Reoperation rates across the referral hospitals ranged from 5% to 95.5%, The study found a nearly a threefold variation in reoperation rates across geographic regions. The bottom quartile of hospital referral regions had an average reoperation rate of 13.3% (0.3 standard deviation) and the top quartile had an average reoperation rate of 39.1% (0.21 SD). Top-quartile regions were concentrated in the West, but were otherwise distributed throughout the country.
Most reoperations were elective admissions (79.9%), while 10% were classified as urgent and another 10.1% as emergency. So although previous studies have documented complications such as band slippage and gastric erosion, the preponderance of elective admissions suggests patient and clinician preferences, or weight loss failure, rather than emergency situations, may be the driving force in the reoperation trend.
The investigators concluded that patients should be fully informed about the likelihood of reoperation with the gastric band. In addition, the wide range of reoperation rates across regions and institutions suggests that more training or better patient selection may be needed to improve outcomes. However, they suggested that “taken together, these findings indicate that the gastric band is associated with high reoperation rates and considerable costs to the payers, which raises concerns about its safety, effectiveness, and value.” They added that “payers should reconsider their coverage of the gastric band device.”
Coauthor Justin B. Dimick, MD, disclosed a financial interest in ArborMetrix. The other coauthors reported having no financial disclosures. The Robert Wood Johnson Foundation, U.S. Department of Veterans Affairs, National Institute on Aging, and National Institute of Diabetes and Digestive and Kidney Diseases provided funding.
Dr. Ibrahim and his colleagues have suggested that payers reconsider covering the adjustable laparoscopic gastric band. I disagree and feel that this device still has a role, albeit limited in the modern bariatric surgical program. Many patients do well for a long period. A committed surgeon and program, and the ideal patient with a similar level of commitment, are needed to achieve these best outcomes. Now that patients and surgeons are better informed of the drawbacks to the device, use has decreased without external regulations or policies to drive this change. No single bariatric procedure is appropriate for all patients. Patients need options, and we need better data to help guide their decisions. Do not throw the baby out with the bathwater.
Jon C. Gould, MD, FACS, is with the Medical College of Wisconsin, Milwaukee. Dr. Gould made these comments in an editorial (JAMA Surg. 2017 May 17; doi: 10.1001/jamasurg.2017.1082) that accompanied the study. He has no disclosures.
Dr. Ibrahim and his colleagues have suggested that payers reconsider covering the adjustable laparoscopic gastric band. I disagree and feel that this device still has a role, albeit limited in the modern bariatric surgical program. Many patients do well for a long period. A committed surgeon and program, and the ideal patient with a similar level of commitment, are needed to achieve these best outcomes. Now that patients and surgeons are better informed of the drawbacks to the device, use has decreased without external regulations or policies to drive this change. No single bariatric procedure is appropriate for all patients. Patients need options, and we need better data to help guide their decisions. Do not throw the baby out with the bathwater.
Jon C. Gould, MD, FACS, is with the Medical College of Wisconsin, Milwaukee. Dr. Gould made these comments in an editorial (JAMA Surg. 2017 May 17; doi: 10.1001/jamasurg.2017.1082) that accompanied the study. He has no disclosures.
Dr. Ibrahim and his colleagues have suggested that payers reconsider covering the adjustable laparoscopic gastric band. I disagree and feel that this device still has a role, albeit limited in the modern bariatric surgical program. Many patients do well for a long period. A committed surgeon and program, and the ideal patient with a similar level of commitment, are needed to achieve these best outcomes. Now that patients and surgeons are better informed of the drawbacks to the device, use has decreased without external regulations or policies to drive this change. No single bariatric procedure is appropriate for all patients. Patients need options, and we need better data to help guide their decisions. Do not throw the baby out with the bathwater.
Jon C. Gould, MD, FACS, is with the Medical College of Wisconsin, Milwaukee. Dr. Gould made these comments in an editorial (JAMA Surg. 2017 May 17; doi: 10.1001/jamasurg.2017.1082) that accompanied the study. He has no disclosures.
About one in five laparoscopic gastric band surgeries result in device-related reoperations and reoperations account for almost half of all Medicare expenditures for gastric band surgery, a large retrospective study has found.
The laparoscopic adjustable gastric band for treatment of morbid obesity, approved in 2001 by the Food and Drug Administration, was once a common choice for bariatric patients. Although its use has declined from in recent years, the American Society for Metabolic and Bariatric Surgery estimated that 11,000 bands were placed in 2015 and many others remain in place (ASMBS, Estimate of bariatric surgery numbers, 2011-2015, https://goo.gl/f8iByl). Many of these gastric bands will need to be removed, replaced, or revised in a series of procedures over the coming years.
Of the 24,042 gastric band patients in this study group, 4,636 (18.5%) underwent reoperation, defined as band removal, band replacement, or revision to a different bariatric procedure, but not including band size adjustment. Patients who had reoperations were more likely to be women, to be white, and to have slightly lower rates of hypertension and diabetes. But they were also more likely to have received a psychiatric, anemia, or electrolyte disorder diagnosis at the time of their index operations.
Among the 4,636 patients who had reoperations, 17,539 such procedures were performed, an average of 3.8 procedures per patient, in addition to the index operation, over an average follow-up of 4.5 years. The most common reoperation was for band removal (41.8%). Other reasons included conversion to laparoscopic Roux-en-Y gastric bypass (13.1%) or laparoscopic sleeve gastrectomy (5.3%).
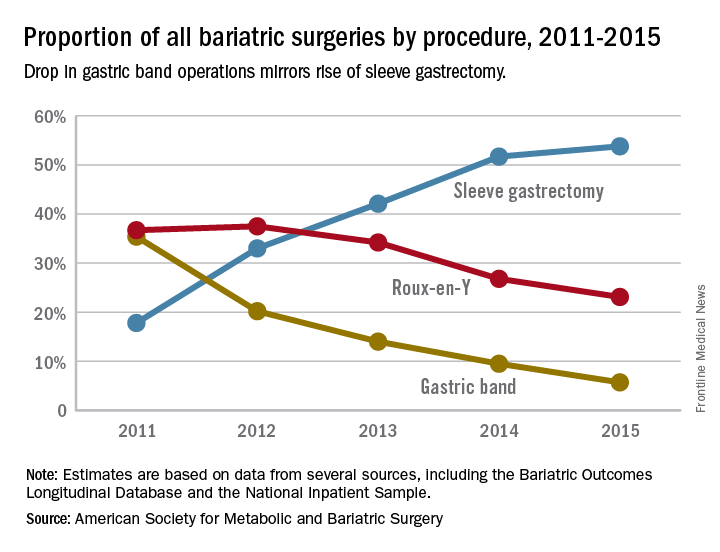
The study also looked at the regional differences, reflecting the comparative success of some programs in managing laparoscopic gastric band placement. Reoperation rates across the referral hospitals ranged from 5% to 95.5%, The study found a nearly a threefold variation in reoperation rates across geographic regions. The bottom quartile of hospital referral regions had an average reoperation rate of 13.3% (0.3 standard deviation) and the top quartile had an average reoperation rate of 39.1% (0.21 SD). Top-quartile regions were concentrated in the West, but were otherwise distributed throughout the country.
Most reoperations were elective admissions (79.9%), while 10% were classified as urgent and another 10.1% as emergency. So although previous studies have documented complications such as band slippage and gastric erosion, the preponderance of elective admissions suggests patient and clinician preferences, or weight loss failure, rather than emergency situations, may be the driving force in the reoperation trend.
The investigators concluded that patients should be fully informed about the likelihood of reoperation with the gastric band. In addition, the wide range of reoperation rates across regions and institutions suggests that more training or better patient selection may be needed to improve outcomes. However, they suggested that “taken together, these findings indicate that the gastric band is associated with high reoperation rates and considerable costs to the payers, which raises concerns about its safety, effectiveness, and value.” They added that “payers should reconsider their coverage of the gastric band device.”
Coauthor Justin B. Dimick, MD, disclosed a financial interest in ArborMetrix. The other coauthors reported having no financial disclosures. The Robert Wood Johnson Foundation, U.S. Department of Veterans Affairs, National Institute on Aging, and National Institute of Diabetes and Digestive and Kidney Diseases provided funding.
About one in five laparoscopic gastric band surgeries result in device-related reoperations and reoperations account for almost half of all Medicare expenditures for gastric band surgery, a large retrospective study has found.
The laparoscopic adjustable gastric band for treatment of morbid obesity, approved in 2001 by the Food and Drug Administration, was once a common choice for bariatric patients. Although its use has declined from in recent years, the American Society for Metabolic and Bariatric Surgery estimated that 11,000 bands were placed in 2015 and many others remain in place (ASMBS, Estimate of bariatric surgery numbers, 2011-2015, https://goo.gl/f8iByl). Many of these gastric bands will need to be removed, replaced, or revised in a series of procedures over the coming years.
Of the 24,042 gastric band patients in this study group, 4,636 (18.5%) underwent reoperation, defined as band removal, band replacement, or revision to a different bariatric procedure, but not including band size adjustment. Patients who had reoperations were more likely to be women, to be white, and to have slightly lower rates of hypertension and diabetes. But they were also more likely to have received a psychiatric, anemia, or electrolyte disorder diagnosis at the time of their index operations.
Among the 4,636 patients who had reoperations, 17,539 such procedures were performed, an average of 3.8 procedures per patient, in addition to the index operation, over an average follow-up of 4.5 years. The most common reoperation was for band removal (41.8%). Other reasons included conversion to laparoscopic Roux-en-Y gastric bypass (13.1%) or laparoscopic sleeve gastrectomy (5.3%).
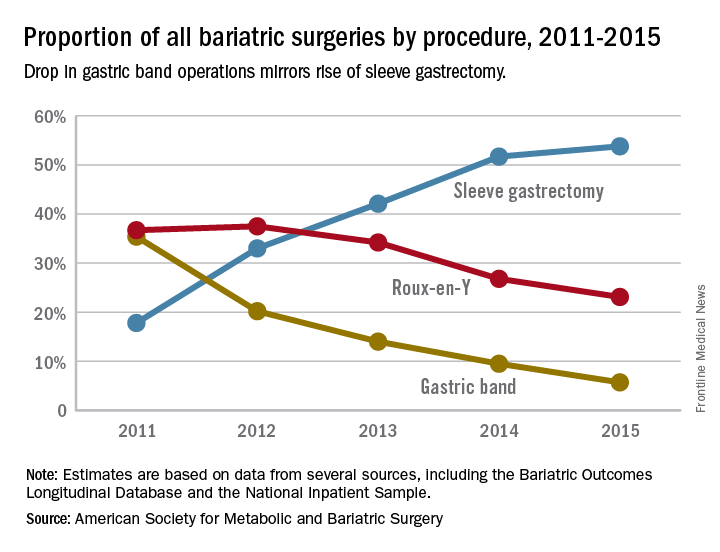
The study also looked at the regional differences, reflecting the comparative success of some programs in managing laparoscopic gastric band placement. Reoperation rates across the referral hospitals ranged from 5% to 95.5%, The study found a nearly a threefold variation in reoperation rates across geographic regions. The bottom quartile of hospital referral regions had an average reoperation rate of 13.3% (0.3 standard deviation) and the top quartile had an average reoperation rate of 39.1% (0.21 SD). Top-quartile regions were concentrated in the West, but were otherwise distributed throughout the country.
Most reoperations were elective admissions (79.9%), while 10% were classified as urgent and another 10.1% as emergency. So although previous studies have documented complications such as band slippage and gastric erosion, the preponderance of elective admissions suggests patient and clinician preferences, or weight loss failure, rather than emergency situations, may be the driving force in the reoperation trend.
The investigators concluded that patients should be fully informed about the likelihood of reoperation with the gastric band. In addition, the wide range of reoperation rates across regions and institutions suggests that more training or better patient selection may be needed to improve outcomes. However, they suggested that “taken together, these findings indicate that the gastric band is associated with high reoperation rates and considerable costs to the payers, which raises concerns about its safety, effectiveness, and value.” They added that “payers should reconsider their coverage of the gastric band device.”
Coauthor Justin B. Dimick, MD, disclosed a financial interest in ArborMetrix. The other coauthors reported having no financial disclosures. The Robert Wood Johnson Foundation, U.S. Department of Veterans Affairs, National Institute on Aging, and National Institute of Diabetes and Digestive and Kidney Diseases provided funding.
FROM JAMA SURGERY
Key clinical point: Reoperations after gastric band placement are common and raise concerns about the safety, effectiveness, and value of the device.
Major finding: During the study period, reoperations accounted for 47.6% of Medicare payments for laparoscopic gastric band procedures.
Data source: Medicare Provider Analysis and Review file of 25,042 beneficiaries who had gastric band procedures between 2006 and 2013.
Disclosures: Coauthor Justin B. Dimick, MD, disclosed a financial interest in ArborMetrix. The other coauthors reported having no financial disclosures. The Robert Wood Johnson Foundation, U.S. Department of Veterans Affairs, National Institute on Aging, and National Institute of Diabetes and Digestive and Kidney Diseases provided funding.
Bariatric patients can conquer obesity, but few achieve BMI < 25
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Around one-quarter of obese individuals who undergo Roux-en-Y gastric bypass had sustained, long-term remission of obesity, but far fewer achieved body mass index of under 25 kg/m2 or maintained it over 5 years, new research suggests.
Researchers reported on the outcomes of a retrospective cohort study of 219 patients who underwent Roux-en-Y gastric bypass surgery at a single center between 2008 and 2010 and were followed for up to 7 years after the procedure.
Only 16.9% of female patients achieved a BMI of under 25 kg/m2 – during the study period, and only 2.7% reached this BMI by year 2 and sustained it at least to year 5 of follow-up.
Two males in the study achieved BMI of under 25 during follow-up. One was recorded as having maintained this weight at year 1 and the other at year 4, but no further measurements were available for either.
“Given the low number of patients achieving BMI of less than 25 kg/m2, we also wanted to focus on another important clinical goal of obesity remission (BMI less than 30),” wrote Corey J. Lager, MD, of the University of Michigan, Brehm Center for Diabetes, Ann Arbor, and his coauthors. “Taking into account that the mean BMI prior to surgery in our cohort was 47.1 kg/m2, this target is associated with significant estimated health benefits and likely brings a mortality benefit for patients undergoing gastric bypass.”
The authors said that a conservative estimate of the probability of achieving and sustaining BMI 25 or less after Roux-en-Y gastric bypass was just 2.3%. However, they offered a more liberal estimate – based on the number of patients who were at BMI 25 or under at the last available data point – of 6.8%.
Achieving weight loss to a BMI less than 30 was significantly influenced by age. The group who achieved this weight were on average 3 years younger at baseline than those who did not.
Similarly, initial BMI played a role in outcomes. The women who achieved a BMI below 30 had an initial mean BMI of 43.5, compared with 50.4 in the women who did not achieve this weight (P less than .0001). In males, the mean baseline BMI in those who got their weight below 30 was 44.6, compared with 48.1 in those who did not (P = .18).
Roux-en-Y gastric bypass was also associated with significant and sustained decreases in both systolic and diastolic blood pressure that was similar for both sexes. The maximum mean decrease of 14 ± 7 mm Hg was achieved at 1 year after surgery, and, at 5 years, the mean decrease was 11 ± 3 mm Hg.
The authors commented that, despite “excellent” weight loss being achieved by a majority of patients, the findings show the challenge of weight loss and maintenance in patients with a very high BMI. However, they also pointed to the encouragingly low rates of significant weight regain and the fact that fewer than 1% of patients returned to a weight greater than their preoperative weight. Higher preoperative BMI was correlated with greater weight loss but also negatively correlated with achieving BMI under 30.
The authors concluded with two takeaway messages. First, realistic goals should be set for patients undergoing gastric bypass surgery, with an emphasis on remission of obesity and with a reduced expectation of achievement of BMI under 25 over the long run. In addition, because the higher the initial BMI, the less likely that weight loss will not be maintained, “we should also carefully examine the option of pursuing surgery at lower BMI cutoffs, at which point patients have a greater likelihood of obesity remission.”
The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
FROM OBESITY SURGERY
Key clinical point: Roux-en-Y gastric bypass is associated with sustained, long-term remission of obesity in around one-quarter of patients.
Major finding: Nearly one-quarter of patients who underwent Roux-en-Y gastric bypass achieved a BMI below 30 kg/m2 that was sustained at their last follow-up, but healthy weight was sustained at 5 years’ follow-up in far fewer patients.
Data source: Retrospective cohort study of 219 patients.
Disclosures: The study was supported by the University of Michigan Health System, the National Institutes of Health, and the Nutrition Obesity Research Centers. One author declared grant support and advisory positions with pharmaceutical companies and intellectual property unrelated to the study. Another author is an investigator on a sponsored clinical study. No other conflicts of interest were declared.
Roux-en-Y bests sleeve gastrectomy for weight loss
AT ENDO 2017
ORLANDO – Roux-en-Y gastric bypass resulted in greater weight loss than sleeve gastrectomy in a study that followed more than 700 patients, an effect that was sustained over time.
However, surgical complications were more common than with sleeve gastrectomy, and patients were more likely to have an extended hospital stay.
The study, conducted by Corey Lager, MD, and his collaborators at the University of Michigan Medical Center, Ann Arbor, looked at 5-year outcomes for 380 patients who had Roux-en-Y gastric bypass (RYGB), compared with those for 336 patients who received sleeve gastrectomy (SG).
Specific outcomes examined included the amount of absolute weight loss and excess body weight loss over the 5-year study period, whether obesity-related comorbidities resolved, and the type and number of complications seen with each procedure.
Sleeve gastrectomy is becoming increasingly popular, even as RYGB and adjustable gastric banding procedures have become more and more rare, Dr. Lager said at the annual meeting of the Endocrine Society. Duodenal switch procedures have continued to represent a very small proportion of surgical weight loss surgeries. Of the four, SG accounted for nearly 80% of the procedures performed in 2013; RYGB, which accounted for about 60% of procedures in 2006, fell to about 30% of procedures by 2013.
The investigators conducted a retrospective analysis of patients undergoing RYGB or SG from January 2008 to November 2013. Patients were seen annually in postoperative follow-up, so the study was able to track body mass index (BMI), weight, excess body weight loss, hemoglobin A1c levels, blood pressure, and serum lipid and vitamin levels over the 5-year period. Additionally, the study captured 30-day postoperative complications for each procedure.
Although about 80% of patients undergoing each procedure were female and baseline lab values and characteristics were similar in many respects, patients undergoing sleeve gastrectomy had higher body weight (mean, 143 kg) and BMI (mean, 50 kg/m2), compared with those who received RYGB (weight, 133 kg; BMI, 47; P less than .001 for both). The average age in both groups was about 45 years.
Sleeve gastrectomy patients were less likely to continue for the full 5 years of follow-up. Of 336 SG patients originally enrolled, 93 had 5-year data. Of the 380 RYGB patients, 188 returned for the 5-year follow-up.
At all time points, the RYGB patients had significantly more total weight loss than the SG patients (P less than .05); the initial weight loss for RYGB patients approached 28% of body weight at year 1, compared with about 23% for the SG patients. By the end of the 5-year period, RYGB patients had maintained about a 24% weight loss, compared with almost 20% for the SG group.
This pattern was mirrored for BMI in each cohort: At year 1, the RYGB patients were down about 14 points, compared with about 12 points for the SG group. By year 5, the difference had narrowed so that each group had lost a mean of between 11 and 12 points from their original BMI, but the difference was still statistically significant (P less than .05).
The final measure of weight loss was excess body weight lost, and again, RYGB patients lost significantly more of their excess body weight at all time points than did the SG patients. At the end of the first year, RYGB had lost more than 65% of their excess body weight, compared with about 48% for the SG patients. By 5 years, the SG patients had regained enough weight that their net excess weight loss was a little less than 40%, while the RYGB patients’ regain put them at about 55% excess weight loss by the end of the study period.
In terms of biomarkers, systolic blood pressure did not differ significantly between the three groups except at study year 3, though the RYGB group had numerically slightly lower systolic blood pressures at all time points. Total cholesterol was lower at 1, 2, 4, and 5 years after surgery for the RYGB group.
Sleeve gastrectomy, as expected, had lower rates of grade I surgical complications, including hemorrhage and infection. Also, the SG patients had fewer postsurgical emergency department visits and a shorter length of stay.
The study results were consistent with those of a 2016 meta-analysis that favored RYGB in terms of excess weight lost, readmission for diabetes-related complications, and resolution of hypertension (Obes Surg. 2016 Feb;26[2]:429-42).
Although this was a large study, it was limited by its retrospective nature and by the lack of randomization, said Dr. Lager. Retaining patients for long-term follow-up was also an issue: Of the original 719 patients, 507 were followed at 3 years and 281 at 5 years, so a significant number weren’t tracked for the full 5 years.
Dr. Lager reported no conflicts of interest, and the study had no outside sources of funding.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO – Roux-en-Y gastric bypass resulted in greater weight loss than sleeve gastrectomy in a study that followed more than 700 patients, an effect that was sustained over time.
However, surgical complications were more common than with sleeve gastrectomy, and patients were more likely to have an extended hospital stay.
The study, conducted by Corey Lager, MD, and his collaborators at the University of Michigan Medical Center, Ann Arbor, looked at 5-year outcomes for 380 patients who had Roux-en-Y gastric bypass (RYGB), compared with those for 336 patients who received sleeve gastrectomy (SG).
Specific outcomes examined included the amount of absolute weight loss and excess body weight loss over the 5-year study period, whether obesity-related comorbidities resolved, and the type and number of complications seen with each procedure.
Sleeve gastrectomy is becoming increasingly popular, even as RYGB and adjustable gastric banding procedures have become more and more rare, Dr. Lager said at the annual meeting of the Endocrine Society. Duodenal switch procedures have continued to represent a very small proportion of surgical weight loss surgeries. Of the four, SG accounted for nearly 80% of the procedures performed in 2013; RYGB, which accounted for about 60% of procedures in 2006, fell to about 30% of procedures by 2013.
The investigators conducted a retrospective analysis of patients undergoing RYGB or SG from January 2008 to November 2013. Patients were seen annually in postoperative follow-up, so the study was able to track body mass index (BMI), weight, excess body weight loss, hemoglobin A1c levels, blood pressure, and serum lipid and vitamin levels over the 5-year period. Additionally, the study captured 30-day postoperative complications for each procedure.
Although about 80% of patients undergoing each procedure were female and baseline lab values and characteristics were similar in many respects, patients undergoing sleeve gastrectomy had higher body weight (mean, 143 kg) and BMI (mean, 50 kg/m2), compared with those who received RYGB (weight, 133 kg; BMI, 47; P less than .001 for both). The average age in both groups was about 45 years.
Sleeve gastrectomy patients were less likely to continue for the full 5 years of follow-up. Of 336 SG patients originally enrolled, 93 had 5-year data. Of the 380 RYGB patients, 188 returned for the 5-year follow-up.
At all time points, the RYGB patients had significantly more total weight loss than the SG patients (P less than .05); the initial weight loss for RYGB patients approached 28% of body weight at year 1, compared with about 23% for the SG patients. By the end of the 5-year period, RYGB patients had maintained about a 24% weight loss, compared with almost 20% for the SG group.
This pattern was mirrored for BMI in each cohort: At year 1, the RYGB patients were down about 14 points, compared with about 12 points for the SG group. By year 5, the difference had narrowed so that each group had lost a mean of between 11 and 12 points from their original BMI, but the difference was still statistically significant (P less than .05).
The final measure of weight loss was excess body weight lost, and again, RYGB patients lost significantly more of their excess body weight at all time points than did the SG patients. At the end of the first year, RYGB had lost more than 65% of their excess body weight, compared with about 48% for the SG patients. By 5 years, the SG patients had regained enough weight that their net excess weight loss was a little less than 40%, while the RYGB patients’ regain put them at about 55% excess weight loss by the end of the study period.
In terms of biomarkers, systolic blood pressure did not differ significantly between the three groups except at study year 3, though the RYGB group had numerically slightly lower systolic blood pressures at all time points. Total cholesterol was lower at 1, 2, 4, and 5 years after surgery for the RYGB group.
Sleeve gastrectomy, as expected, had lower rates of grade I surgical complications, including hemorrhage and infection. Also, the SG patients had fewer postsurgical emergency department visits and a shorter length of stay.
The study results were consistent with those of a 2016 meta-analysis that favored RYGB in terms of excess weight lost, readmission for diabetes-related complications, and resolution of hypertension (Obes Surg. 2016 Feb;26[2]:429-42).
Although this was a large study, it was limited by its retrospective nature and by the lack of randomization, said Dr. Lager. Retaining patients for long-term follow-up was also an issue: Of the original 719 patients, 507 were followed at 3 years and 281 at 5 years, so a significant number weren’t tracked for the full 5 years.
Dr. Lager reported no conflicts of interest, and the study had no outside sources of funding.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO – Roux-en-Y gastric bypass resulted in greater weight loss than sleeve gastrectomy in a study that followed more than 700 patients, an effect that was sustained over time.
However, surgical complications were more common than with sleeve gastrectomy, and patients were more likely to have an extended hospital stay.
The study, conducted by Corey Lager, MD, and his collaborators at the University of Michigan Medical Center, Ann Arbor, looked at 5-year outcomes for 380 patients who had Roux-en-Y gastric bypass (RYGB), compared with those for 336 patients who received sleeve gastrectomy (SG).
Specific outcomes examined included the amount of absolute weight loss and excess body weight loss over the 5-year study period, whether obesity-related comorbidities resolved, and the type and number of complications seen with each procedure.
Sleeve gastrectomy is becoming increasingly popular, even as RYGB and adjustable gastric banding procedures have become more and more rare, Dr. Lager said at the annual meeting of the Endocrine Society. Duodenal switch procedures have continued to represent a very small proportion of surgical weight loss surgeries. Of the four, SG accounted for nearly 80% of the procedures performed in 2013; RYGB, which accounted for about 60% of procedures in 2006, fell to about 30% of procedures by 2013.
The investigators conducted a retrospective analysis of patients undergoing RYGB or SG from January 2008 to November 2013. Patients were seen annually in postoperative follow-up, so the study was able to track body mass index (BMI), weight, excess body weight loss, hemoglobin A1c levels, blood pressure, and serum lipid and vitamin levels over the 5-year period. Additionally, the study captured 30-day postoperative complications for each procedure.
Although about 80% of patients undergoing each procedure were female and baseline lab values and characteristics were similar in many respects, patients undergoing sleeve gastrectomy had higher body weight (mean, 143 kg) and BMI (mean, 50 kg/m2), compared with those who received RYGB (weight, 133 kg; BMI, 47; P less than .001 for both). The average age in both groups was about 45 years.
Sleeve gastrectomy patients were less likely to continue for the full 5 years of follow-up. Of 336 SG patients originally enrolled, 93 had 5-year data. Of the 380 RYGB patients, 188 returned for the 5-year follow-up.
At all time points, the RYGB patients had significantly more total weight loss than the SG patients (P less than .05); the initial weight loss for RYGB patients approached 28% of body weight at year 1, compared with about 23% for the SG patients. By the end of the 5-year period, RYGB patients had maintained about a 24% weight loss, compared with almost 20% for the SG group.
This pattern was mirrored for BMI in each cohort: At year 1, the RYGB patients were down about 14 points, compared with about 12 points for the SG group. By year 5, the difference had narrowed so that each group had lost a mean of between 11 and 12 points from their original BMI, but the difference was still statistically significant (P less than .05).
The final measure of weight loss was excess body weight lost, and again, RYGB patients lost significantly more of their excess body weight at all time points than did the SG patients. At the end of the first year, RYGB had lost more than 65% of their excess body weight, compared with about 48% for the SG patients. By 5 years, the SG patients had regained enough weight that their net excess weight loss was a little less than 40%, while the RYGB patients’ regain put them at about 55% excess weight loss by the end of the study period.
In terms of biomarkers, systolic blood pressure did not differ significantly between the three groups except at study year 3, though the RYGB group had numerically slightly lower systolic blood pressures at all time points. Total cholesterol was lower at 1, 2, 4, and 5 years after surgery for the RYGB group.
Sleeve gastrectomy, as expected, had lower rates of grade I surgical complications, including hemorrhage and infection. Also, the SG patients had fewer postsurgical emergency department visits and a shorter length of stay.
The study results were consistent with those of a 2016 meta-analysis that favored RYGB in terms of excess weight lost, readmission for diabetes-related complications, and resolution of hypertension (Obes Surg. 2016 Feb;26[2]:429-42).
Although this was a large study, it was limited by its retrospective nature and by the lack of randomization, said Dr. Lager. Retaining patients for long-term follow-up was also an issue: Of the original 719 patients, 507 were followed at 3 years and 281 at 5 years, so a significant number weren’t tracked for the full 5 years.
Dr. Lager reported no conflicts of interest, and the study had no outside sources of funding.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: At 5 years post surgery, Roux-en-Y recipients had kept off 25% of their body weight, compared with 20% for sleeve gastrectomy patients (P less than .05).
Data source: Longitudinal follow-up of 716 patients who had one of two surgical procedures for weight loss.
Disclosures: None of the study authors reported relevant disclosures, and no external source of funding was reported.