User login
DiaRem score predicts remission of type 2 diabetes after sleeve gastrectomy
SAN DIEGO – The DiaRem score was effective in predicting remission of type 2 diabetes following laparoscopic sleeve gastrectomy, results from a single-center study showed.
Developed by clinicians at Geisinger Clinic, the DiaRem is a simple score that helps predict remission of type 2 diabetes in severely obese subjects with metabolic syndrome who undergo Roux-en-Y gastric bypass surgery (Lancet Diabetes Endocrinol 2014;2[1]:38-45). The DiaRem score spans from 0 to 22 and is divided into five groups corresponding to five probability ranges for type 2 diabetes remission: 0-2 (88%-99%), 3-7 (64%-88%), 8-12 (23%-49%), 13-17 (11%-33%), 18-22 (2%-16%). In an effort to assess the feasibility of using the DiaRem score to predict remission of type 2 diabetes after laparoscopic sleeve gastrectomy, Raul J. Rosenthal, MD, FACS, and his associates conducted a 4-year retrospective review of 162 patients at the Cleveland Clinic Florida, Weston. “This is the first report that uses the DiaRem score for similar subjects that underwent sleeve gastrectomy instead,” Dr. Rosenthal said in an interview in advance of the annual clinical congress of the American College of Surgeons.
The mean age of the 162 patients was 55 years, 61% were women, 74% were non-Hispanic, their mean body mass index was 43.2 kg/m2, 33% had a preoperative hemoglobin A1c level between 7% and 8.9%, and 22% had an HbA1c of 9%. All had a minimum follow-up of 1 year after their laparoscopic sleeve gastrectomy and 67% had follow-up of 3 years or more, said Dr. Rosenthal, professor and chairman of the department of general surgery at Cleveland Clinic Florida.
Based on results of the DiaRem scores, 58% of patients achieved complete remission of type 2 diabetes, 6% achieved partial remission, and 36% had no remission. Specifically, 96% had DiaRem scores between 0 and 2; 92% had scores between 3 and 7; 50% had scores between 8 and 12, 20% had scores between 13 and 17, and 24% had scores between 18 and 22. “We were pleased to find out that 58% of patients that underwent sleeve gastrectomy achieved complete remission of type 2 diabetes mellitus,” said Dr. Rosenthal, who also directs the clinic’s bariatric and metabolic institute. “This compares favorably to previous reports in which patients achieved 33% of complete remission after gastric bypass.” The researchers also found that 84% of patients achieved remission in 12 months and the rest in 3 years. They observed medication reduction in 93% of the patients.
“Sleeve gastrectomy is a valid bariatric-metabolic procedure in patients with type 2 diabetes,” Dr. Rosenthal concluded. “The main limitation of this study is that is it a retrospective one, and we do not have a control group of patients that underwent gastric bypass or medical treatment to compare.”
The findings were presented at the meeting by Emanuele Lo Menzo, MD. Dr. Rosenthal disclosed that he is a consultant for Medtronic. Dr. Lo Menzo reported having no financial disclosures.
SAN DIEGO – The DiaRem score was effective in predicting remission of type 2 diabetes following laparoscopic sleeve gastrectomy, results from a single-center study showed.
Developed by clinicians at Geisinger Clinic, the DiaRem is a simple score that helps predict remission of type 2 diabetes in severely obese subjects with metabolic syndrome who undergo Roux-en-Y gastric bypass surgery (Lancet Diabetes Endocrinol 2014;2[1]:38-45). The DiaRem score spans from 0 to 22 and is divided into five groups corresponding to five probability ranges for type 2 diabetes remission: 0-2 (88%-99%), 3-7 (64%-88%), 8-12 (23%-49%), 13-17 (11%-33%), 18-22 (2%-16%). In an effort to assess the feasibility of using the DiaRem score to predict remission of type 2 diabetes after laparoscopic sleeve gastrectomy, Raul J. Rosenthal, MD, FACS, and his associates conducted a 4-year retrospective review of 162 patients at the Cleveland Clinic Florida, Weston. “This is the first report that uses the DiaRem score for similar subjects that underwent sleeve gastrectomy instead,” Dr. Rosenthal said in an interview in advance of the annual clinical congress of the American College of Surgeons.
The mean age of the 162 patients was 55 years, 61% were women, 74% were non-Hispanic, their mean body mass index was 43.2 kg/m2, 33% had a preoperative hemoglobin A1c level between 7% and 8.9%, and 22% had an HbA1c of 9%. All had a minimum follow-up of 1 year after their laparoscopic sleeve gastrectomy and 67% had follow-up of 3 years or more, said Dr. Rosenthal, professor and chairman of the department of general surgery at Cleveland Clinic Florida.
Based on results of the DiaRem scores, 58% of patients achieved complete remission of type 2 diabetes, 6% achieved partial remission, and 36% had no remission. Specifically, 96% had DiaRem scores between 0 and 2; 92% had scores between 3 and 7; 50% had scores between 8 and 12, 20% had scores between 13 and 17, and 24% had scores between 18 and 22. “We were pleased to find out that 58% of patients that underwent sleeve gastrectomy achieved complete remission of type 2 diabetes mellitus,” said Dr. Rosenthal, who also directs the clinic’s bariatric and metabolic institute. “This compares favorably to previous reports in which patients achieved 33% of complete remission after gastric bypass.” The researchers also found that 84% of patients achieved remission in 12 months and the rest in 3 years. They observed medication reduction in 93% of the patients.
“Sleeve gastrectomy is a valid bariatric-metabolic procedure in patients with type 2 diabetes,” Dr. Rosenthal concluded. “The main limitation of this study is that is it a retrospective one, and we do not have a control group of patients that underwent gastric bypass or medical treatment to compare.”
The findings were presented at the meeting by Emanuele Lo Menzo, MD. Dr. Rosenthal disclosed that he is a consultant for Medtronic. Dr. Lo Menzo reported having no financial disclosures.
SAN DIEGO – The DiaRem score was effective in predicting remission of type 2 diabetes following laparoscopic sleeve gastrectomy, results from a single-center study showed.
Developed by clinicians at Geisinger Clinic, the DiaRem is a simple score that helps predict remission of type 2 diabetes in severely obese subjects with metabolic syndrome who undergo Roux-en-Y gastric bypass surgery (Lancet Diabetes Endocrinol 2014;2[1]:38-45). The DiaRem score spans from 0 to 22 and is divided into five groups corresponding to five probability ranges for type 2 diabetes remission: 0-2 (88%-99%), 3-7 (64%-88%), 8-12 (23%-49%), 13-17 (11%-33%), 18-22 (2%-16%). In an effort to assess the feasibility of using the DiaRem score to predict remission of type 2 diabetes after laparoscopic sleeve gastrectomy, Raul J. Rosenthal, MD, FACS, and his associates conducted a 4-year retrospective review of 162 patients at the Cleveland Clinic Florida, Weston. “This is the first report that uses the DiaRem score for similar subjects that underwent sleeve gastrectomy instead,” Dr. Rosenthal said in an interview in advance of the annual clinical congress of the American College of Surgeons.
The mean age of the 162 patients was 55 years, 61% were women, 74% were non-Hispanic, their mean body mass index was 43.2 kg/m2, 33% had a preoperative hemoglobin A1c level between 7% and 8.9%, and 22% had an HbA1c of 9%. All had a minimum follow-up of 1 year after their laparoscopic sleeve gastrectomy and 67% had follow-up of 3 years or more, said Dr. Rosenthal, professor and chairman of the department of general surgery at Cleveland Clinic Florida.
Based on results of the DiaRem scores, 58% of patients achieved complete remission of type 2 diabetes, 6% achieved partial remission, and 36% had no remission. Specifically, 96% had DiaRem scores between 0 and 2; 92% had scores between 3 and 7; 50% had scores between 8 and 12, 20% had scores between 13 and 17, and 24% had scores between 18 and 22. “We were pleased to find out that 58% of patients that underwent sleeve gastrectomy achieved complete remission of type 2 diabetes mellitus,” said Dr. Rosenthal, who also directs the clinic’s bariatric and metabolic institute. “This compares favorably to previous reports in which patients achieved 33% of complete remission after gastric bypass.” The researchers also found that 84% of patients achieved remission in 12 months and the rest in 3 years. They observed medication reduction in 93% of the patients.
“Sleeve gastrectomy is a valid bariatric-metabolic procedure in patients with type 2 diabetes,” Dr. Rosenthal concluded. “The main limitation of this study is that is it a retrospective one, and we do not have a control group of patients that underwent gastric bypass or medical treatment to compare.”
The findings were presented at the meeting by Emanuele Lo Menzo, MD. Dr. Rosenthal disclosed that he is a consultant for Medtronic. Dr. Lo Menzo reported having no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: The DiaRem score is useful in predicting remission of type 2 diabetes following laparoscopic sleeve gastrectomy.
Major finding: Results of the DiaRem scores indicated that 58% of patients achieved complete remission of type 2 diabetes.
Study details: A retrospective analysis of 162 patients who underwent laparoscopic sleeve gastrectomy.
Disclosures: Dr. Rosenthal disclosed that he is a consultant for Medtronic. Dr. Lo Menzo reported having no financial disclosures.
VIDEO: SBO in bariatric patient can mean internal herniation
SAN DIEGO – You get a call from the emergency department at 3 a.m. A 48-year-old woman is presenting with fever, nausea, vomiting, and left upper quadrant pain. And the patient says she had a gastric bypass procedure 3 years ago.
Time to panic? Not necessarily, but things can, and occasionally do, go bad for these patients, even if they have had a long-stable bypass, Jennifer Choi, MD, FACS, said in a video interview at the annual clinical congress of the American College of Surgeons.
“We do have to remember that our bariatric surgery patients can develop all of the same kinds of problems that anyone else can,” said Dr. Choi, a general surgeon at Indiana University, Indianapolis. “Appendicitis, diverticulitis, abdominal wall hernias, and other common things do happen.”
In her book, though, a patient with a gastric bypass who presents with a combination of small-bowel obstruction and pain has an internal herniation until proven otherwise.
“The symptoms can be subtle, and they can either have been building for several weeks or have an acute onset,” Dr. Choi said. These can include nausea, dry heaves, bloating, or nonbilious vomiting. Pain is typically located in the left upper quadrant or mid-back, especially if the hernia is located at one of the two most common spots: Petersen’s defect. This is the point where the biliopancreatic loop tends to slip under the alimentary loop and become trapped. Imaging will show a typical swirling of blood vessels around the herniation, accompanied by dilated small bowel at the point of obstruction.
At the other common herniation point, the site of the jejunojejunostomy, the alimentary loop can slip under the biliopancreatic loop. On imaging, jejunum will be seen in the upper right quadrant.
Both of these can be surgical emergencies, Dr. Choi said. “This needs an operation sooner, rather than later. It needs to be reduced and repaired.”
She typically performs this laparoscopically, but said that some surgeons prefer an open approach, which is a perfectly sound option.
“The key to a successful repair is to start at the ileocecal valve, because it is consistent and fixed, and run the bowel from distal to proximal to reduce the internal hernia. Then close the defect with a permanent suture,” she said.
Chylous ascites is almost always present in these cases because the herniation traumatizes the lymphatic system, Dr. Choi added. “It doesn’t all always have to be removed at the time of surgery, but just be aware that this is definitely something we do see, almost all the time in bariatric patients with these internal hernias.”
Dr. Choi had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
SAN DIEGO – You get a call from the emergency department at 3 a.m. A 48-year-old woman is presenting with fever, nausea, vomiting, and left upper quadrant pain. And the patient says she had a gastric bypass procedure 3 years ago.
Time to panic? Not necessarily, but things can, and occasionally do, go bad for these patients, even if they have had a long-stable bypass, Jennifer Choi, MD, FACS, said in a video interview at the annual clinical congress of the American College of Surgeons.
“We do have to remember that our bariatric surgery patients can develop all of the same kinds of problems that anyone else can,” said Dr. Choi, a general surgeon at Indiana University, Indianapolis. “Appendicitis, diverticulitis, abdominal wall hernias, and other common things do happen.”
In her book, though, a patient with a gastric bypass who presents with a combination of small-bowel obstruction and pain has an internal herniation until proven otherwise.
“The symptoms can be subtle, and they can either have been building for several weeks or have an acute onset,” Dr. Choi said. These can include nausea, dry heaves, bloating, or nonbilious vomiting. Pain is typically located in the left upper quadrant or mid-back, especially if the hernia is located at one of the two most common spots: Petersen’s defect. This is the point where the biliopancreatic loop tends to slip under the alimentary loop and become trapped. Imaging will show a typical swirling of blood vessels around the herniation, accompanied by dilated small bowel at the point of obstruction.
At the other common herniation point, the site of the jejunojejunostomy, the alimentary loop can slip under the biliopancreatic loop. On imaging, jejunum will be seen in the upper right quadrant.
Both of these can be surgical emergencies, Dr. Choi said. “This needs an operation sooner, rather than later. It needs to be reduced and repaired.”
She typically performs this laparoscopically, but said that some surgeons prefer an open approach, which is a perfectly sound option.
“The key to a successful repair is to start at the ileocecal valve, because it is consistent and fixed, and run the bowel from distal to proximal to reduce the internal hernia. Then close the defect with a permanent suture,” she said.
Chylous ascites is almost always present in these cases because the herniation traumatizes the lymphatic system, Dr. Choi added. “It doesn’t all always have to be removed at the time of surgery, but just be aware that this is definitely something we do see, almost all the time in bariatric patients with these internal hernias.”
Dr. Choi had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
SAN DIEGO – You get a call from the emergency department at 3 a.m. A 48-year-old woman is presenting with fever, nausea, vomiting, and left upper quadrant pain. And the patient says she had a gastric bypass procedure 3 years ago.
Time to panic? Not necessarily, but things can, and occasionally do, go bad for these patients, even if they have had a long-stable bypass, Jennifer Choi, MD, FACS, said in a video interview at the annual clinical congress of the American College of Surgeons.
“We do have to remember that our bariatric surgery patients can develop all of the same kinds of problems that anyone else can,” said Dr. Choi, a general surgeon at Indiana University, Indianapolis. “Appendicitis, diverticulitis, abdominal wall hernias, and other common things do happen.”
In her book, though, a patient with a gastric bypass who presents with a combination of small-bowel obstruction and pain has an internal herniation until proven otherwise.
“The symptoms can be subtle, and they can either have been building for several weeks or have an acute onset,” Dr. Choi said. These can include nausea, dry heaves, bloating, or nonbilious vomiting. Pain is typically located in the left upper quadrant or mid-back, especially if the hernia is located at one of the two most common spots: Petersen’s defect. This is the point where the biliopancreatic loop tends to slip under the alimentary loop and become trapped. Imaging will show a typical swirling of blood vessels around the herniation, accompanied by dilated small bowel at the point of obstruction.
At the other common herniation point, the site of the jejunojejunostomy, the alimentary loop can slip under the biliopancreatic loop. On imaging, jejunum will be seen in the upper right quadrant.
Both of these can be surgical emergencies, Dr. Choi said. “This needs an operation sooner, rather than later. It needs to be reduced and repaired.”
She typically performs this laparoscopically, but said that some surgeons prefer an open approach, which is a perfectly sound option.
“The key to a successful repair is to start at the ileocecal valve, because it is consistent and fixed, and run the bowel from distal to proximal to reduce the internal hernia. Then close the defect with a permanent suture,” she said.
Chylous ascites is almost always present in these cases because the herniation traumatizes the lymphatic system, Dr. Choi added. “It doesn’t all always have to be removed at the time of surgery, but just be aware that this is definitely something we do see, almost all the time in bariatric patients with these internal hernias.”
Dr. Choi had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
AT THE ACS Clinical Congress
Antibiotic exposure blunted metabolic improvement following vertical sleeve gastrectomy
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
SAN DIEGO – results from a mouse study demonstrated.
The finding raises the question of whether patients with suboptimal outcomes following vertical sleeve gastrectomy may benefit from microbial modulation.
According to Dr. Jahansouz of the University of Minnesota Microbiota Transplantation Program, mechanisms mediating metabolic improvement following bariatric surgery remain incompletely understood. “Outcomes are also somewhat variable: As many as 40%-75% of patients regain weight in the years following nadir of weight loss,” he said. “Human studies have shown an acute and sustained shift in the gut microbiota, and an altered bile acid profile. Bile acids increase following surgery.”
Meanwhile, mice deficient in Farnesoid X-receptor (FXR) and Takeda G protein–coupled Receptor 5 (TGR5) do not experience metabolic improvement following bariatric surgery; the composition of the microbiome can significantly impact the composition of bile acids.
“By altering the postsurgical composition of mice following bariatric surgery, we eliminate the metabolic benefits of surgery, possibly by altering bile acid profiles,” Dr. Jahansouz said.
For the trial, diet-induced obese mice were randomized to vertical sleeve gastrectomy (VSG) or sham surgery, with or without exposure to antibiotics that selectively suppress mainly gram-positive (fidaxomicin, streptomycin) or gram-negative (ceftriaxone) bacteria on postoperative days 1-4. The researchers characterized fecal microbiota before surgery and on postoperative days 7 and 28. Mice were metabolically characterized on postoperative days 30-32 and euthanized on postoperative day 35.
Mice in the VSG group experienced weight loss and shifts in the intestinal microbiota composition, compared with those in the sham surgery group.
“Antibiotic exposure resulted in sustained reductions in alpha (within sample) diversity of microbiota and shifts in its composition,” the researchers wrote in their abstract. “Different antimicrobial specificity of antibiotics led to functionally distinct physiologic effects. Specifically, fidaxomicin and streptomycin markedly altered hepatic bile acid signaling and lipid metabolism, while ceftriaxone resulted in greater reduction in the expression of key antimicrobial peptides.
“However, VSG mice exposed to antibiotics, regardless of their specificity, had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, relative to control mice,” the investigators noted.
Dr. Jahansouz said that he was surprised by the fact that all three antibiotics tested, no matter their specificity in gut bacteria eliminated, resulted in significantly diminished weight loss and metabolic improvement following vertical sleeve gastrectomy in the mouse model. He acknowledged that translating the findings from mice to humans is a key limitation of the analysis.
“There are fundamental physiologic differences between mice and humans that need consideration in all murine models of metabolic disorders,” he said. “Therefore, it is critical that insights gained from these models are followed up in human studies.”
The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Postsurgical disruption of intestinal microbiota composition attenuates the metabolic efficacy of vertical sleeve gastrectomy.
Major finding: VSG mice exposed to antibiotics had significantly increased subcutaneous adiposity and impaired glucose homeostasis without changes in food intake, compared with control mice.
Study details: A study of diet-induced obese mice that were randomized to VSG or sham surgery, with or without exposure to antibiotics.
Disclosures: The study was funded by the American Diabetes Association and a Minnesota Discovery, Research and InnoVation Economy grant from the University of Minnesota. Dr. Jahansouz reported having no financial disclosures.
Low risk of bariatric surgery complications in IBD
Bariatric surgery is safe and feasible in patients with inflammatory bowel disease (IBD), with a low risk of postoperative complications vs. controls, according to results of a recent cohort study.
Besides a significantly higher risk of perioperative small-bowel obstruction and a 1-day increase in hospital stay, outcomes were comparable between patients with IBD and controls (Obes Surg. 2017 Oct 10. doi: 10.1007/s11695-017-2955-4).
Limitations of the retrospective study, according to the authors, included a potential underestimation of short-term postoperative complications, since the data set used in the study was limited to in-hospital stays and would not include events occurring after discharge.
Nevertheless, “our data show that it is reasonable to carefully proceed with bariatric interventions in obese IBD patients, especially those who are at higher risk of cardiovascular mortality and drastic need for weight reduction, to accrue benefits of weight loss,” wrote Fateh Bazerbachi, MD, of the Mayo Clinic, Rochester, Minn. and his coauthors.
Bariatric surgery is the “most effective solution” for obesity, and “appropriate candidates should not be deprived of this important, potentially life-saving procedure, if the intervention is deemed acceptably safe,” Dr. Bazerbachi and his colleagues noted.
Their cohort study included data for 314,864 adult patients in the Nationwide Inpatient Sample who underwent bariatric surgery between 2011 and 2013. Of that group, 790 patients had underlying IBD (459 Crohn’s disease, 331 ulcerative colitis). Remaining patients made up the comparator group.
The primary outcomes evaluated in the study included risks of systemic and technical complications. Risk of perioperative small-bowel obstruction was significantly higher in the IBD group (adjusted odds ratio, 4.0; 95% confidence interval, 2.2-7.4). However, the rates of other complications were similar between the two groups, data show.
Secondary outcomes in the study included length of hospital stay and mortality. Mean length of hospital stay was 3.4 days for IBD patients, vs. 2.5 days for the comparison group (P = .01), according to the report. Mortality was 0.25% for controls, while no deaths were reported in the IBD group.
In the future, bariatric surgeons may face increasing demand to treat IBD patients, given the increasing prevalence of obesity in the IBD patient population, Dr. Bazerbachi and his colleagues said.
Some surgeons may believe that bariatric intervention is more challenging in IBD patients, in part because of the underlying inflammatory state that might interfere with healing of wounds and recovery of bowel motility, they said. Bariatric surgery, however, can reduce body mass index, which in turn might make future IBD surgeries less challenging.
Another potential advantage is reduction in cardiovascular risk, which is elevated in IBD patients both due to obesity as well as the IBD condition, they added.
“Further studies are certainly needed to examine long-term outcomes of bariatric surgery on IBD and to determine whether cardiovascular mortality is reduced from these interventions in this susceptible cohort of obese IBD patients,” Dr. Bazerbachi and his colleagues wrote.
The authors declared that they had no conflicts of interest.
Bariatric surgery is safe and feasible in patients with inflammatory bowel disease (IBD), with a low risk of postoperative complications vs. controls, according to results of a recent cohort study.
Besides a significantly higher risk of perioperative small-bowel obstruction and a 1-day increase in hospital stay, outcomes were comparable between patients with IBD and controls (Obes Surg. 2017 Oct 10. doi: 10.1007/s11695-017-2955-4).
Limitations of the retrospective study, according to the authors, included a potential underestimation of short-term postoperative complications, since the data set used in the study was limited to in-hospital stays and would not include events occurring after discharge.
Nevertheless, “our data show that it is reasonable to carefully proceed with bariatric interventions in obese IBD patients, especially those who are at higher risk of cardiovascular mortality and drastic need for weight reduction, to accrue benefits of weight loss,” wrote Fateh Bazerbachi, MD, of the Mayo Clinic, Rochester, Minn. and his coauthors.
Bariatric surgery is the “most effective solution” for obesity, and “appropriate candidates should not be deprived of this important, potentially life-saving procedure, if the intervention is deemed acceptably safe,” Dr. Bazerbachi and his colleagues noted.
Their cohort study included data for 314,864 adult patients in the Nationwide Inpatient Sample who underwent bariatric surgery between 2011 and 2013. Of that group, 790 patients had underlying IBD (459 Crohn’s disease, 331 ulcerative colitis). Remaining patients made up the comparator group.
The primary outcomes evaluated in the study included risks of systemic and technical complications. Risk of perioperative small-bowel obstruction was significantly higher in the IBD group (adjusted odds ratio, 4.0; 95% confidence interval, 2.2-7.4). However, the rates of other complications were similar between the two groups, data show.
Secondary outcomes in the study included length of hospital stay and mortality. Mean length of hospital stay was 3.4 days for IBD patients, vs. 2.5 days for the comparison group (P = .01), according to the report. Mortality was 0.25% for controls, while no deaths were reported in the IBD group.
In the future, bariatric surgeons may face increasing demand to treat IBD patients, given the increasing prevalence of obesity in the IBD patient population, Dr. Bazerbachi and his colleagues said.
Some surgeons may believe that bariatric intervention is more challenging in IBD patients, in part because of the underlying inflammatory state that might interfere with healing of wounds and recovery of bowel motility, they said. Bariatric surgery, however, can reduce body mass index, which in turn might make future IBD surgeries less challenging.
Another potential advantage is reduction in cardiovascular risk, which is elevated in IBD patients both due to obesity as well as the IBD condition, they added.
“Further studies are certainly needed to examine long-term outcomes of bariatric surgery on IBD and to determine whether cardiovascular mortality is reduced from these interventions in this susceptible cohort of obese IBD patients,” Dr. Bazerbachi and his colleagues wrote.
The authors declared that they had no conflicts of interest.
Bariatric surgery is safe and feasible in patients with inflammatory bowel disease (IBD), with a low risk of postoperative complications vs. controls, according to results of a recent cohort study.
Besides a significantly higher risk of perioperative small-bowel obstruction and a 1-day increase in hospital stay, outcomes were comparable between patients with IBD and controls (Obes Surg. 2017 Oct 10. doi: 10.1007/s11695-017-2955-4).
Limitations of the retrospective study, according to the authors, included a potential underestimation of short-term postoperative complications, since the data set used in the study was limited to in-hospital stays and would not include events occurring after discharge.
Nevertheless, “our data show that it is reasonable to carefully proceed with bariatric interventions in obese IBD patients, especially those who are at higher risk of cardiovascular mortality and drastic need for weight reduction, to accrue benefits of weight loss,” wrote Fateh Bazerbachi, MD, of the Mayo Clinic, Rochester, Minn. and his coauthors.
Bariatric surgery is the “most effective solution” for obesity, and “appropriate candidates should not be deprived of this important, potentially life-saving procedure, if the intervention is deemed acceptably safe,” Dr. Bazerbachi and his colleagues noted.
Their cohort study included data for 314,864 adult patients in the Nationwide Inpatient Sample who underwent bariatric surgery between 2011 and 2013. Of that group, 790 patients had underlying IBD (459 Crohn’s disease, 331 ulcerative colitis). Remaining patients made up the comparator group.
The primary outcomes evaluated in the study included risks of systemic and technical complications. Risk of perioperative small-bowel obstruction was significantly higher in the IBD group (adjusted odds ratio, 4.0; 95% confidence interval, 2.2-7.4). However, the rates of other complications were similar between the two groups, data show.
Secondary outcomes in the study included length of hospital stay and mortality. Mean length of hospital stay was 3.4 days for IBD patients, vs. 2.5 days for the comparison group (P = .01), according to the report. Mortality was 0.25% for controls, while no deaths were reported in the IBD group.
In the future, bariatric surgeons may face increasing demand to treat IBD patients, given the increasing prevalence of obesity in the IBD patient population, Dr. Bazerbachi and his colleagues said.
Some surgeons may believe that bariatric intervention is more challenging in IBD patients, in part because of the underlying inflammatory state that might interfere with healing of wounds and recovery of bowel motility, they said. Bariatric surgery, however, can reduce body mass index, which in turn might make future IBD surgeries less challenging.
Another potential advantage is reduction in cardiovascular risk, which is elevated in IBD patients both due to obesity as well as the IBD condition, they added.
“Further studies are certainly needed to examine long-term outcomes of bariatric surgery on IBD and to determine whether cardiovascular mortality is reduced from these interventions in this susceptible cohort of obese IBD patients,” Dr. Bazerbachi and his colleagues wrote.
The authors declared that they had no conflicts of interest.
FROM OBESITY SURGERY
Key clinical point: Watch for perioperative small-bowel obstruction in IBD patients undergoing bariatric surgery.
Major finding: IBD patients had a higher risk of perioperative small bowel obstruction (adjusted odds ratio, 4.0; 95% confidence interval, 2.2-7.4) and a 1-day increase in hospital stay (P = .01), compared with controls.
Data source: Retrospective cohort study of Nationwide Inpatient Sample data including 790 patients with underlying IBD.
Disclosures: The authors declared that they had no conflicts of interest.
Many women have unprotected sex in year after bariatric surgery
More than 40% of reproductive-age women reported having unprotected sex in the year after undergoing bariatric surgery, despite recommendations to avoid pregnancy for at least a year, a new study finds. Another 4% of women reported trying to conceive in the 12 months after surgery.
“We were surprised to find such a large percentage of women were not using contraception, and we were also surprised to find so many were actively trying to conceive,” the study’s lead author Marie N. Menke, MD, MPH, of the University of Pittsburgh, said in an interview. “Reproductive-age women who are considering bariatric surgery should be counseled that they should plan to use contraceptives after surgery for about 12-18 months.”
Pregnancy isn’t recommended over that period mainly because of the risks to the fetus, Dr. Menke said. “These risks are different from obesity in general. We don’t know exactly why surgery causes these risks, but ideally, patients would be weight-stable prior to conception.”
In 2013, the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic & Bariatric Surgery provided a Grade D recommendation for a 12-18 month delay in conception (Obesity [Silver Spring] 2013;21[suppl 1]:S1-27). A recent study provided more insight into the potential risks of pregnancy soon after weight-loss procedures. It reported that, compared with those who gave birth more than 4 years later, women who gave birth within 2 years of bariatric surgery had higher risks of premature birth, admission to neonatal intensive care units, and small-for-gestational-age infants (JAMA Surg. 2017 Feb 1;152[2]:1-8).
The current prospective cohort study included women who underwent bariatric surgery for the first time during 2005-2009 at 10 U.S. hospitals. The women, all aged 18-44 years, answered questions for as long as 7 years, until January 2015 (Obstet Gynecol. 2017 Oct 6. doi: 10.1097/AOG.0000000000002323).
The analysis included 710 women who provided conception data. The median body mass index of the women was 46.3 kg/m2. Most patients underwent Roux-en-Y gastric bypass (73%), followed by laparoscopic adjustable gastric banding (23%).
Researchers found that 4.3% of the women tried to conceive in the first year after surgery (95% confidence interval, 2.4-6.3), and 13.1% did so in the second year (95% CI, 9.3-17.0; P less than .001).
During the first year after surgery, 12.7% of women had no intercourse (95% CI, 9.4-16.0), 40.5% had only protected intercourse (95% CI, 35.6-45.4), and 41.5% (95% CI, 36.4-46.6) had unprotected intercourse while not trying to conceive.
Why are the unprotected sex numbers so high? “We wonder if some women simply feel that they cannot get pregnant,” Dr. Menke said. “Our group has previously reported that 42% of women who had attempted to conceive prior to bariatric surgery had a history of infertility. Some of these women went on to deliver a live birth, but many did not.”
The study reports that 183 of the 710 women did ultimately conceive and that the number may be as high as 237 because data were missing for 54 women who may have not wanted to report a nonlive birth. Of the women who reported conceiving, 68.9% had live births, 1.1% had stillbirths, 1.1% had ectopic pregnancies, 21.9% miscarried and 7.1% had abortions.
“We’d really like this research to be a reason to consider presurgical contraceptive counseling as one of the steps prior to bariatric surgery,” Dr. Menke said. “This may include a referral by the bariatric surgeon to a physician would who provide counseling, prescribe, or both.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Menke reported having no relevant disclosures. Her coauthors reported financial relationships with pharmaceutical and medical device companies with products to treat metabolic diseases.
More than 40% of reproductive-age women reported having unprotected sex in the year after undergoing bariatric surgery, despite recommendations to avoid pregnancy for at least a year, a new study finds. Another 4% of women reported trying to conceive in the 12 months after surgery.
“We were surprised to find such a large percentage of women were not using contraception, and we were also surprised to find so many were actively trying to conceive,” the study’s lead author Marie N. Menke, MD, MPH, of the University of Pittsburgh, said in an interview. “Reproductive-age women who are considering bariatric surgery should be counseled that they should plan to use contraceptives after surgery for about 12-18 months.”
Pregnancy isn’t recommended over that period mainly because of the risks to the fetus, Dr. Menke said. “These risks are different from obesity in general. We don’t know exactly why surgery causes these risks, but ideally, patients would be weight-stable prior to conception.”
In 2013, the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic & Bariatric Surgery provided a Grade D recommendation for a 12-18 month delay in conception (Obesity [Silver Spring] 2013;21[suppl 1]:S1-27). A recent study provided more insight into the potential risks of pregnancy soon after weight-loss procedures. It reported that, compared with those who gave birth more than 4 years later, women who gave birth within 2 years of bariatric surgery had higher risks of premature birth, admission to neonatal intensive care units, and small-for-gestational-age infants (JAMA Surg. 2017 Feb 1;152[2]:1-8).
The current prospective cohort study included women who underwent bariatric surgery for the first time during 2005-2009 at 10 U.S. hospitals. The women, all aged 18-44 years, answered questions for as long as 7 years, until January 2015 (Obstet Gynecol. 2017 Oct 6. doi: 10.1097/AOG.0000000000002323).
The analysis included 710 women who provided conception data. The median body mass index of the women was 46.3 kg/m2. Most patients underwent Roux-en-Y gastric bypass (73%), followed by laparoscopic adjustable gastric banding (23%).
Researchers found that 4.3% of the women tried to conceive in the first year after surgery (95% confidence interval, 2.4-6.3), and 13.1% did so in the second year (95% CI, 9.3-17.0; P less than .001).
During the first year after surgery, 12.7% of women had no intercourse (95% CI, 9.4-16.0), 40.5% had only protected intercourse (95% CI, 35.6-45.4), and 41.5% (95% CI, 36.4-46.6) had unprotected intercourse while not trying to conceive.
Why are the unprotected sex numbers so high? “We wonder if some women simply feel that they cannot get pregnant,” Dr. Menke said. “Our group has previously reported that 42% of women who had attempted to conceive prior to bariatric surgery had a history of infertility. Some of these women went on to deliver a live birth, but many did not.”
The study reports that 183 of the 710 women did ultimately conceive and that the number may be as high as 237 because data were missing for 54 women who may have not wanted to report a nonlive birth. Of the women who reported conceiving, 68.9% had live births, 1.1% had stillbirths, 1.1% had ectopic pregnancies, 21.9% miscarried and 7.1% had abortions.
“We’d really like this research to be a reason to consider presurgical contraceptive counseling as one of the steps prior to bariatric surgery,” Dr. Menke said. “This may include a referral by the bariatric surgeon to a physician would who provide counseling, prescribe, or both.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Menke reported having no relevant disclosures. Her coauthors reported financial relationships with pharmaceutical and medical device companies with products to treat metabolic diseases.
More than 40% of reproductive-age women reported having unprotected sex in the year after undergoing bariatric surgery, despite recommendations to avoid pregnancy for at least a year, a new study finds. Another 4% of women reported trying to conceive in the 12 months after surgery.
“We were surprised to find such a large percentage of women were not using contraception, and we were also surprised to find so many were actively trying to conceive,” the study’s lead author Marie N. Menke, MD, MPH, of the University of Pittsburgh, said in an interview. “Reproductive-age women who are considering bariatric surgery should be counseled that they should plan to use contraceptives after surgery for about 12-18 months.”
Pregnancy isn’t recommended over that period mainly because of the risks to the fetus, Dr. Menke said. “These risks are different from obesity in general. We don’t know exactly why surgery causes these risks, but ideally, patients would be weight-stable prior to conception.”
In 2013, the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic & Bariatric Surgery provided a Grade D recommendation for a 12-18 month delay in conception (Obesity [Silver Spring] 2013;21[suppl 1]:S1-27). A recent study provided more insight into the potential risks of pregnancy soon after weight-loss procedures. It reported that, compared with those who gave birth more than 4 years later, women who gave birth within 2 years of bariatric surgery had higher risks of premature birth, admission to neonatal intensive care units, and small-for-gestational-age infants (JAMA Surg. 2017 Feb 1;152[2]:1-8).
The current prospective cohort study included women who underwent bariatric surgery for the first time during 2005-2009 at 10 U.S. hospitals. The women, all aged 18-44 years, answered questions for as long as 7 years, until January 2015 (Obstet Gynecol. 2017 Oct 6. doi: 10.1097/AOG.0000000000002323).
The analysis included 710 women who provided conception data. The median body mass index of the women was 46.3 kg/m2. Most patients underwent Roux-en-Y gastric bypass (73%), followed by laparoscopic adjustable gastric banding (23%).
Researchers found that 4.3% of the women tried to conceive in the first year after surgery (95% confidence interval, 2.4-6.3), and 13.1% did so in the second year (95% CI, 9.3-17.0; P less than .001).
During the first year after surgery, 12.7% of women had no intercourse (95% CI, 9.4-16.0), 40.5% had only protected intercourse (95% CI, 35.6-45.4), and 41.5% (95% CI, 36.4-46.6) had unprotected intercourse while not trying to conceive.
Why are the unprotected sex numbers so high? “We wonder if some women simply feel that they cannot get pregnant,” Dr. Menke said. “Our group has previously reported that 42% of women who had attempted to conceive prior to bariatric surgery had a history of infertility. Some of these women went on to deliver a live birth, but many did not.”
The study reports that 183 of the 710 women did ultimately conceive and that the number may be as high as 237 because data were missing for 54 women who may have not wanted to report a nonlive birth. Of the women who reported conceiving, 68.9% had live births, 1.1% had stillbirths, 1.1% had ectopic pregnancies, 21.9% miscarried and 7.1% had abortions.
“We’d really like this research to be a reason to consider presurgical contraceptive counseling as one of the steps prior to bariatric surgery,” Dr. Menke said. “This may include a referral by the bariatric surgeon to a physician would who provide counseling, prescribe, or both.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Menke reported having no relevant disclosures. Her coauthors reported financial relationships with pharmaceutical and medical device companies with products to treat metabolic diseases.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: In the first year after surgery, 4.3% of women surveyed tried to conceive (95% CI, 2.4-6.3), and another 41.5% had unprotected intercourse (95% CI, 36.4-46.6).
Data source: Prospective cohort study of 710 women, aged 18-44 years, who underwent bariatric surgery for the first time during 2005-2009 at 10 U.S. hospitals.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Menke reported having no relevant disclosures. Her coauthors reported financial relationships with pharmaceutical and medical device companies with products to treat metabolic diseases.
Swedish study finds low risk of developing psoriasis in bariatric surgery patients
Obese patients who undergo bariatric surgery have a lower risk of later developing psoriasis, according to results of nonrandomized, longitudinal intervention trial.
Cristina Maglio, MD, of the University of Gothenburg, Sweden, and her associates found that over a 26-year follow-up period, the adjusted hazard ratio (HR) of developing psoriasis was 0.65 (95% confidence interval [CI], 0.47-0.89; P = .008) for patients who underwent bariatric surgery, compared with those who received conventional, nonsurgical obesity treatments. Psoriasis developed in 3.6% of 1,991 patients in the surgery group during follow-up and in 5.1% of 2,018 control patients during follow-up.
Conversely, the difference in the risk of developing psoriatic arthritis (PsA), experienced by up to one-third of patients with psoriasis, was not statistically significant (HR, 0.77; 95% CI, 0.43-1.37; P = .287). PsA developed in 1% of subjects from the surgery group and 1.3% from the control group.
To understand how surgery affected the development of psoriasis or psoriatic arthritis, the researchers conducted a trial with a control group and surgery group. In the control group, 2,018 patients received standard obesity treatments that included recommendations on eating behavior, food selection, and physical activity. The 1,991 patients in the surgery group underwent gastric banding (375), vertical banded gastroplasty (1,354), or gastric bypass (262). At the start of the study, patients were evaluated for baseline measurements, then again at 6 months. After the 6-month mark, patients were reevaluated at 1, 2, 3, 4, 6, 8, 10, 15, and 20 years, respectively. All study participants, regardless of trial group, were examined and presented patient health questionnaires at each follow-up. The endpoint for this study was the first diagnosis of either psoriasis or PsA. Body mass index decreased significantly in the surgery group, compared with virtually no change in the control group.
Vertical banded gastroplasty was found to significantly lower the incidence of psoriasis, compared with usual treatment. But using gastric banding as a reference, vertical banded gastroplasty (HR, 0.80; 95% CI, 0.46-1.39; P = .418) and gastric bypass (HR, 0.71; 95% CI, 0.29-1.71; P = 0.439) were found to have similar effects on the prevention of psoriasis.
The researchers also identified several risk factors that significantly increased the risk of developing psoriasis. Smoking (HR, 1.75; 95% CI, 1.26-2.42; P = .001), a known risk factor in the development of psoriasis, and the length of time a patient had been obese (HR, 1.28; 95% CI, 1.05-1.55; P = .014) were found to be independently associated with an increased risk of psoriasis.
As part of their risk analysis, Dr. Maglio and her colleagues analyzed the interactions of baseline risk factors such as BMI and obesity duration with the bariatric surgery. This analysis found no significant interactions between baseline risk factors and bariatric surgery. It did reveal that patients who were older at baseline evaluation had slightly better responses to bariatric surgery with lower incidences of psoriasis, compared with younger patients, but the differences were not statistically significant.
“The preventive role of bariatric surgery on the risk of psoriasis has been recently highlighted by a retrospective Danish study (JAMA Surg. 2017 Apr 1;152[4]:344-9),” noted Dr. Maglio and her colleagues. “However, we lent strength to the previous results by confirming this association in a large prospective intervention trial designed to examine the effect of bariatric surgery on obesity-related comorbidities in comparison with usual obesity care.
This study was funded in part by the National Institutes of Diabetes and Digestive and Kidney Diseases, the Swedish Rheumatism association, the Swedish Research Council, the University of Gothenburg, and the Swedish federal government. Dr. Anna Rudin reported that part of her salary at Sahlgrenska University is supported by a grant from AstraZeneca. Dr. Lena M.S. Carlsson has received lecture fees from AstraZeneca, Johnson & Johnson, and Merck Sharp and Dohme. Dr. Maglio and Dr. Markku Peltonen had no relevant financial disclosures.
SOURCE: Maglio et al. Obesity. 2017. Dec; 25[12]:2068-73.
Obese patients who undergo bariatric surgery have a lower risk of later developing psoriasis, according to results of nonrandomized, longitudinal intervention trial.
Cristina Maglio, MD, of the University of Gothenburg, Sweden, and her associates found that over a 26-year follow-up period, the adjusted hazard ratio (HR) of developing psoriasis was 0.65 (95% confidence interval [CI], 0.47-0.89; P = .008) for patients who underwent bariatric surgery, compared with those who received conventional, nonsurgical obesity treatments. Psoriasis developed in 3.6% of 1,991 patients in the surgery group during follow-up and in 5.1% of 2,018 control patients during follow-up.
Conversely, the difference in the risk of developing psoriatic arthritis (PsA), experienced by up to one-third of patients with psoriasis, was not statistically significant (HR, 0.77; 95% CI, 0.43-1.37; P = .287). PsA developed in 1% of subjects from the surgery group and 1.3% from the control group.
To understand how surgery affected the development of psoriasis or psoriatic arthritis, the researchers conducted a trial with a control group and surgery group. In the control group, 2,018 patients received standard obesity treatments that included recommendations on eating behavior, food selection, and physical activity. The 1,991 patients in the surgery group underwent gastric banding (375), vertical banded gastroplasty (1,354), or gastric bypass (262). At the start of the study, patients were evaluated for baseline measurements, then again at 6 months. After the 6-month mark, patients were reevaluated at 1, 2, 3, 4, 6, 8, 10, 15, and 20 years, respectively. All study participants, regardless of trial group, were examined and presented patient health questionnaires at each follow-up. The endpoint for this study was the first diagnosis of either psoriasis or PsA. Body mass index decreased significantly in the surgery group, compared with virtually no change in the control group.
Vertical banded gastroplasty was found to significantly lower the incidence of psoriasis, compared with usual treatment. But using gastric banding as a reference, vertical banded gastroplasty (HR, 0.80; 95% CI, 0.46-1.39; P = .418) and gastric bypass (HR, 0.71; 95% CI, 0.29-1.71; P = 0.439) were found to have similar effects on the prevention of psoriasis.
The researchers also identified several risk factors that significantly increased the risk of developing psoriasis. Smoking (HR, 1.75; 95% CI, 1.26-2.42; P = .001), a known risk factor in the development of psoriasis, and the length of time a patient had been obese (HR, 1.28; 95% CI, 1.05-1.55; P = .014) were found to be independently associated with an increased risk of psoriasis.
As part of their risk analysis, Dr. Maglio and her colleagues analyzed the interactions of baseline risk factors such as BMI and obesity duration with the bariatric surgery. This analysis found no significant interactions between baseline risk factors and bariatric surgery. It did reveal that patients who were older at baseline evaluation had slightly better responses to bariatric surgery with lower incidences of psoriasis, compared with younger patients, but the differences were not statistically significant.
“The preventive role of bariatric surgery on the risk of psoriasis has been recently highlighted by a retrospective Danish study (JAMA Surg. 2017 Apr 1;152[4]:344-9),” noted Dr. Maglio and her colleagues. “However, we lent strength to the previous results by confirming this association in a large prospective intervention trial designed to examine the effect of bariatric surgery on obesity-related comorbidities in comparison with usual obesity care.
This study was funded in part by the National Institutes of Diabetes and Digestive and Kidney Diseases, the Swedish Rheumatism association, the Swedish Research Council, the University of Gothenburg, and the Swedish federal government. Dr. Anna Rudin reported that part of her salary at Sahlgrenska University is supported by a grant from AstraZeneca. Dr. Lena M.S. Carlsson has received lecture fees from AstraZeneca, Johnson & Johnson, and Merck Sharp and Dohme. Dr. Maglio and Dr. Markku Peltonen had no relevant financial disclosures.
SOURCE: Maglio et al. Obesity. 2017. Dec; 25[12]:2068-73.
Obese patients who undergo bariatric surgery have a lower risk of later developing psoriasis, according to results of nonrandomized, longitudinal intervention trial.
Cristina Maglio, MD, of the University of Gothenburg, Sweden, and her associates found that over a 26-year follow-up period, the adjusted hazard ratio (HR) of developing psoriasis was 0.65 (95% confidence interval [CI], 0.47-0.89; P = .008) for patients who underwent bariatric surgery, compared with those who received conventional, nonsurgical obesity treatments. Psoriasis developed in 3.6% of 1,991 patients in the surgery group during follow-up and in 5.1% of 2,018 control patients during follow-up.
Conversely, the difference in the risk of developing psoriatic arthritis (PsA), experienced by up to one-third of patients with psoriasis, was not statistically significant (HR, 0.77; 95% CI, 0.43-1.37; P = .287). PsA developed in 1% of subjects from the surgery group and 1.3% from the control group.
To understand how surgery affected the development of psoriasis or psoriatic arthritis, the researchers conducted a trial with a control group and surgery group. In the control group, 2,018 patients received standard obesity treatments that included recommendations on eating behavior, food selection, and physical activity. The 1,991 patients in the surgery group underwent gastric banding (375), vertical banded gastroplasty (1,354), or gastric bypass (262). At the start of the study, patients were evaluated for baseline measurements, then again at 6 months. After the 6-month mark, patients were reevaluated at 1, 2, 3, 4, 6, 8, 10, 15, and 20 years, respectively. All study participants, regardless of trial group, were examined and presented patient health questionnaires at each follow-up. The endpoint for this study was the first diagnosis of either psoriasis or PsA. Body mass index decreased significantly in the surgery group, compared with virtually no change in the control group.
Vertical banded gastroplasty was found to significantly lower the incidence of psoriasis, compared with usual treatment. But using gastric banding as a reference, vertical banded gastroplasty (HR, 0.80; 95% CI, 0.46-1.39; P = .418) and gastric bypass (HR, 0.71; 95% CI, 0.29-1.71; P = 0.439) were found to have similar effects on the prevention of psoriasis.
The researchers also identified several risk factors that significantly increased the risk of developing psoriasis. Smoking (HR, 1.75; 95% CI, 1.26-2.42; P = .001), a known risk factor in the development of psoriasis, and the length of time a patient had been obese (HR, 1.28; 95% CI, 1.05-1.55; P = .014) were found to be independently associated with an increased risk of psoriasis.
As part of their risk analysis, Dr. Maglio and her colleagues analyzed the interactions of baseline risk factors such as BMI and obesity duration with the bariatric surgery. This analysis found no significant interactions between baseline risk factors and bariatric surgery. It did reveal that patients who were older at baseline evaluation had slightly better responses to bariatric surgery with lower incidences of psoriasis, compared with younger patients, but the differences were not statistically significant.
“The preventive role of bariatric surgery on the risk of psoriasis has been recently highlighted by a retrospective Danish study (JAMA Surg. 2017 Apr 1;152[4]:344-9),” noted Dr. Maglio and her colleagues. “However, we lent strength to the previous results by confirming this association in a large prospective intervention trial designed to examine the effect of bariatric surgery on obesity-related comorbidities in comparison with usual obesity care.
This study was funded in part by the National Institutes of Diabetes and Digestive and Kidney Diseases, the Swedish Rheumatism association, the Swedish Research Council, the University of Gothenburg, and the Swedish federal government. Dr. Anna Rudin reported that part of her salary at Sahlgrenska University is supported by a grant from AstraZeneca. Dr. Lena M.S. Carlsson has received lecture fees from AstraZeneca, Johnson & Johnson, and Merck Sharp and Dohme. Dr. Maglio and Dr. Markku Peltonen had no relevant financial disclosures.
SOURCE: Maglio et al. Obesity. 2017. Dec; 25[12]:2068-73.
FROM OBESITY
Key clinical point:
Major finding: Obese patients who underwent bariatric surgery had a lower incidence of psoriasis over a 26-year period (HR, 0.65; 95% CI: 0.47-0.89; P = .008), compared with usual care.
Study details: Swedish Obese Subjects study, a longitudinal, nonrandomized intervention trial comprising 1,991 surgery group patients and 2,018 control patients.
Disclosures: This study was funded in part by the National Institutes of Diabetes and Digestive and Kidney Diseases, the Swedish Rheumatism association, the Swedish Research Council, the University of Gothenburg, and the Swedish federal government. Dr. Anna Rudin reported that part of her salary at Sahlgrenska University is supported by a grant from AstraZeneca. Dr. Lena M.S. Carlsson has received lecture fees from AstraZeneca, Johnson & Johnson, and Merck Sharp and Dohme. Dr. Maglio and Dr. Markku Peltonen had no relevant financial disclosures.
Source: Maglio et al. Obesity. 2017. Dec; 25[12]:2068-2073.
Long-term specialist care reduces post-RYGB anemia risk
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
Patients who underwent Roux-en-Y gastric bypass surgery (RYGB) without long-term bariatric specialist follow-up experienced a significantly higher rate of anemia at 10 years than did patients who had such specialist follow-up, according to findings from a database review.
Among 74 patients available for analysis – 58 men and 16 women with a mean age of 51 years who underwent RYGB at a single Veterans Affairs medical center between 2002 and 2006 – the mean rate of preoperative anemia was 20% (15 patients). The rate increased to 28% (21 patients) at 1 year, 31% (23 patients) at 5 years, and 47% (35 patients) at 10 years, according to a research letter by Gao Linda Chen, MD, and her colleagues in the surgical service of the VA Palo Alto (Calif.) Health Care System (JAMA Surg. 2017. Sep 20. doi: 10.1001/jamasurg.2017.3158).
Among 58 patients with no bariatric specialist follow-up after 5 years, the anemia rate increased from 22% (13 patients) before surgery to 57% (33 patients) at 10 years, while the corresponding rates for those with specialty follow-up were 19% (3 patients) and 13% (2 patients). After adjustment for preoperative anemia, those without specialist follow-up had significantly higher odds of anemia at 10 years (odds ratio, 6.1).
“Long-term complications of RYGB, such as anemia, may go unrecognized by nonbariatric specialists,” the investigators wrote, noting that the high rates of anemia at 10 years “may reflect a mixed vitamin and mineral deficiency, because patients had normocytic anemia.
“Our study suggests that follow-up with bariatric specialists more than 5 years after surgery, rather than with specialists with no bariatric expertise, can decrease long-term anemia risk,” they continued. “This finding may demonstrate the bariatric specialist’s specific understanding of the long-term risk for nutritional deficiency after RYGB and the importance of vitamin and mineral supplementation.”
The findings suggest a bariatric team approach with planning for long-term follow-up. “We implemented a hub-and-spoke model for bariatric care, including health care specialist education, in which the bariatric team communicates regularly with the patient’s primary care clinician before and after surgery.”
Although the study is limited by small sample size, the findings nevertheless underscore that “long-term follow-up should be an integral part of bariatric programs, and additional studies are needed to identify potential barriers to successful follow-up,” they concluded.
The authors reported having no disclosures.
FROM JAMA SURGERY
Key clinical point:
Major finding: RYGB patients without specialist follow-up had significantly higher odds of anemia at 10 years (adjusted odds ratio, 6.1).
Data source: A retrospective review of 74 patients from a prospective 10-year database.
Disclosures: The authors reported having no disclosures.
Diagnostic laparoscopy pinpoints postop abdominal pain in bariatric patients
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
The etiology of chronic pain after bariatric surgery can be difficult to pinpoint, but diagnostic laparoscopy can detect causes in about half of patients, findings from a small study have shown.
In an investigation conducted by Mohammed Alsulaimy, MD, a surgeon at the Bariatric and Metabolic Institute at the Cleveland Clinic, and his colleagues, 35 patients underwent diagnostic laparoscopy (DL) to identify the causes of their chronic abdominal pain after bariatric surgery. Patients included in the study had a history of abdominal pain lasting longer than 30 days after their bariatric procedure, a negative CT scan of their abdomen and pelvis, a gallstone-negative abdominal ultrasound, and an upper GI endoscopy with no abnormalities. Researchers collected patient data including age, gender, body, weight, and body mass index, type of previous bariatric procedure, and time between surgery and onset of pain.
The results of DL were either positive (presence detected of pathology or injury) or negative (no disease or injury detected).
Twenty patients (57%) had positive findings on DL including the presence of adhesions, chronic cholecystitis, mesenteric defect, internal hernia, and necrotic omentum, and of this group, 43% had treatment that led to improvement of pain symptoms. Only 1 of the 15 patients with negative DL findings had eventual improvement of their pain symptoms. Most patients with negative DL findings had persistent abdominal pain, possibly because of nonorganic causes and were referred to the chronic pain management service, the investigators wrote.
“About 40% of patients who undergo DL and 70% of patients with positive findings on DL experience significant symptom improvement,” the investigators said. “This study highlights the importance of offering DL as both a diagnostic and therapeutic tool in post–bariatric surgery patients with chronic abdominal of unknown etiology.”
The investigators had no relevant financial disclosures to report.
FROM OBESITY SURGERY
Key clinical point:
Major finding: In the study group, 57% of patients had a positive diagnostic laparoscopy results identifying the source of their chronic abdominal pain.
Data source: Retrospective review of post–bariatric surgery patients who underwent diagnostic laparoscopy (DL) during 2003-2015.
Disclosures: The investigators had no relevant financial disclosures to report.
Roux-en-Y gastric bypass produced durable clinical improvements at 12 years
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Severely obese individuals in the United States who underwent Roux-en-Y gastric bypass (RYGB) averaged a 27% weight loss 12 years later, with only a 3% incidence of type 2 diabetes mellitus and a 51% rate of diabetes remission, according to the results of a large multicenter observational prospective study.
In striking contrast, patients who did not undergo bariatric surgery averaged a 1%-2% weight loss at 12 years, a 26% incidence of diabetes, and only a 5%-10% rate of diabetes remission, said Ted D. Adams, PhD, of the University of Utah, Salt Lake City, and his associates. RYGB surgery also conferred substantial and statistically significant improvements long-term improvements in systolic hypertension and lipid levels, the researchers reported in the New England Journal of Medicine (2017 Sep 20. doi: 10.1056/NEJMoa1700459).
“The follow-up rate exceeded 90% at 12 years,” the researchers wrote. Two years after undergoing Roux-en-Y gastric bypass, patients had lost an average of 45 kg (95% confidence interval, 43-47 kg). By postoperative year 6, they had regained an average of 9 kg (average loss from baseline, 36 kg; 95% CI, 34-39 kg). But they typically gained only about 1.3 kg more between years 6 and 12, and they had about a 92% lower odds of developing diabetes mellitus, compared with individuals who did not undergo bariatric surgery (odds ratio, 0.08; P less than .001). “Remission of type 2 diabetes was much more likely if the Roux-en-Y gastric bypass occurred before [patients began] treatment with insulin, presumably owing to the ability of partially viable beta cells to improve their function,” the researchers noted.
Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Roux-en-Y gastric bypass produced durable results on numerous clinical outcome measures.
Major finding: Twelve years after surgery, RYGB patients averaged a 27% weight loss from baseline, with a 51% rate of remission and a 3% incidence of type 2 diabetes mellitus.
Data source: A prospective study of 1,156 severely obese individuals, of whom 418 underwent Roux-en-Y gastric bypass.
Disclosures: Funders included the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, Weill Cornell Medicine, and Intermountain Healthcare. Dr. Adams reported having no relevant conflicts of interest. One coinvestigator disclosed royalties from licensing a questionnaire on weight loss and the quality of life, and another coinvestigator disclosed fees for services rendered during a trial of an intragastric balloon. The remaining researchers had no relevant disclosures.
Immobility implicated in increased complications after bariatric surgery
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
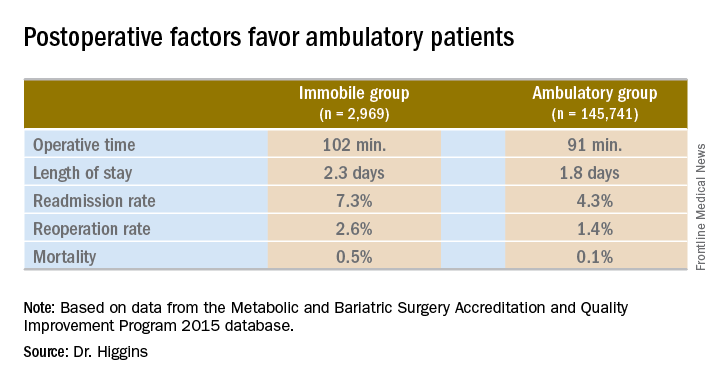
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
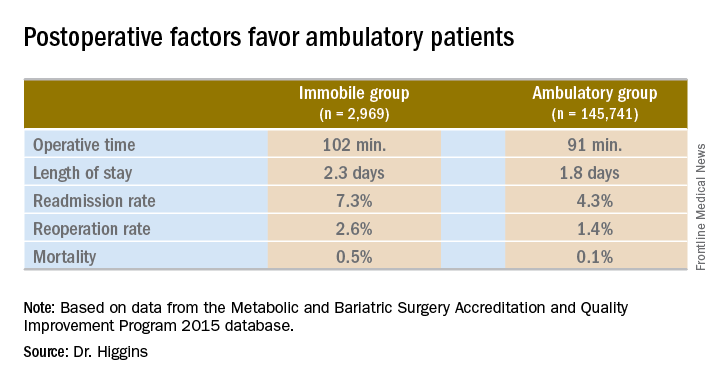
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Key clinical point: Patients immobile before bariatric surgery could require closer monitoring for postoperative complications.
Major finding: Thirty-day mortality after bariatric surgery in immobile patients was 0.5%, vs. 0.1% for an ambulatory group (P less than .0001).
Data source: A comparison of 2015 MBSAQIP data for 145,741 ambulatory patients and 2,969 immobile patients before bariatric surgery.
Disclosures: Dr. Higgins had no relevant financial disclosures.