User login
Rapid venetoclax dose escalation aids relapsed CLL
STOCKHOLM – Patients with chronic lymphocytic leukemia (CLL) who experience relapse after therapy with a B-cell receptor signaling inhibitor tend to have a swiftly progressive disease course that requires immediate intervention. For these patients, a rapid venetoclax dose-escalation protocol may be a safe way to quickly regain disease control, and possibly bridge to salvage therapies, investigators reported.
Of 15 patients with CLL who relapsed after treatment with a B-cell receptor inhibitor (BCRi), all were able to get to their target dose of venetoclax under close inpatient monitoring at a median of 12 days, compared with the 35 days usually required for venetoclax dose escalation, reported Farrukh T. Awan, MD, of Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues.
Only two patients developed clinical tumor lysis syndrome (TLS), a common occurrence with venetoclax therapy, and this adverse event was manageable, Dr. Awan said at the annual congress of the European Hematology Association.
“The reason why we have been doing a slow ramp up on venetoclax is the original toxicity issues that we saw early on,” he said in an interview. “But unfortunately, a lot of patients are progressing on these new agents and have very rapid disease progression, and what we have seen is that if you stop the ibrutinib, the disease progresses very quickly, and by the time they can get up to the effective dose of venetoclax, they’re too sick to continue, or they might even die from disease progression.”
To combat this problem, Dr. Awan and his colleagues developed a rapid dose escalation protocol that would ramp up from 20 mg to 400 mg, with increases every 1 or 2 days depending on tolerability and incident TLS. Lab tests for TLS were evaluated every 4-8 hours.
All patients were closely monitored in the hospital, and all were started on allopurinol or other uric acid–lowering agents before starting on venetoclax.
The investigators reported safety and efficacy outcomes for the patients in a retrospective analysis.
The median age of the patients, 12 men and 3 women, was 65 years (range, 58-86 years). Seven patients had Eastern Cooperative Oncology Group Performance Status of 0, seven had an ECOG score of 1, and one had a score of 2-4.
Ten patients had most recently been treated with a BCRi, either a Bruton’s tyrosine kinase inhibitor (ibrutinib or acalabrutinib), idelalisib, or entospletinib. Three patients received ibrutinib plus chemotherapy, and two received rituximab and dexamethasone followed by rituximab maintenance.
The median time to full venetoclax dose was 12 days (range, 5-21 days) and all 15 patients reached the target dose. The mean length of stay during the ramp-up period was 9.5 days (range, 6-22 days).
The incidence of clinical TLS was 13.2%, occurring in two patients, one at the initial 20-mg dose, and one at the 200-mg dose level. Another five patients had asymptomatic TLS. Other treatment-related adverse events were anemia in seven patients, neutropenia in six patients, thrombocytopenia in five patients, and lung infection in one patient.
Twelve patients had a partial response, one had stable disease, and two had progressive disease. The mean time to best response was 71 days.
One-year progression-free survival was 49%, and 1-year overall survival was 68%.
The investigators found that for patients who still have some disease control with a BCRi, it may be possible to keep them on that drug while transitioning to venetoclax. The rapid dose escalation protocol should only be attempted in highly experience comprehensive cancer centers, Dr. Awan said.
“Under very close monitoring in an experienced inpatient setting, where the nurses are very used to doing this on a weekly basis in a very high volume center, I think that our data show that we could do this without affecting toxicity significantly or mortality,” he said.
Venetoclax therapy could buy enough time for patients to bridge to other options, such as chimeric antigen receptor (CAR) T-cell therapy or allogeneic stem cell transplant, he noted.
“But if we had waited 4 weeks, most of these patients would not have made it,” he said.
The study was internally funded. Dr. Awan reported research funding from Gilead, Pharmacyclics, AbbVie, and Janssen.
SOURCE: Koenig K et al. EHA Congress, Abstract PF357.
STOCKHOLM – Patients with chronic lymphocytic leukemia (CLL) who experience relapse after therapy with a B-cell receptor signaling inhibitor tend to have a swiftly progressive disease course that requires immediate intervention. For these patients, a rapid venetoclax dose-escalation protocol may be a safe way to quickly regain disease control, and possibly bridge to salvage therapies, investigators reported.
Of 15 patients with CLL who relapsed after treatment with a B-cell receptor inhibitor (BCRi), all were able to get to their target dose of venetoclax under close inpatient monitoring at a median of 12 days, compared with the 35 days usually required for venetoclax dose escalation, reported Farrukh T. Awan, MD, of Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues.
Only two patients developed clinical tumor lysis syndrome (TLS), a common occurrence with venetoclax therapy, and this adverse event was manageable, Dr. Awan said at the annual congress of the European Hematology Association.
“The reason why we have been doing a slow ramp up on venetoclax is the original toxicity issues that we saw early on,” he said in an interview. “But unfortunately, a lot of patients are progressing on these new agents and have very rapid disease progression, and what we have seen is that if you stop the ibrutinib, the disease progresses very quickly, and by the time they can get up to the effective dose of venetoclax, they’re too sick to continue, or they might even die from disease progression.”
To combat this problem, Dr. Awan and his colleagues developed a rapid dose escalation protocol that would ramp up from 20 mg to 400 mg, with increases every 1 or 2 days depending on tolerability and incident TLS. Lab tests for TLS were evaluated every 4-8 hours.
All patients were closely monitored in the hospital, and all were started on allopurinol or other uric acid–lowering agents before starting on venetoclax.
The investigators reported safety and efficacy outcomes for the patients in a retrospective analysis.
The median age of the patients, 12 men and 3 women, was 65 years (range, 58-86 years). Seven patients had Eastern Cooperative Oncology Group Performance Status of 0, seven had an ECOG score of 1, and one had a score of 2-4.
Ten patients had most recently been treated with a BCRi, either a Bruton’s tyrosine kinase inhibitor (ibrutinib or acalabrutinib), idelalisib, or entospletinib. Three patients received ibrutinib plus chemotherapy, and two received rituximab and dexamethasone followed by rituximab maintenance.
The median time to full venetoclax dose was 12 days (range, 5-21 days) and all 15 patients reached the target dose. The mean length of stay during the ramp-up period was 9.5 days (range, 6-22 days).
The incidence of clinical TLS was 13.2%, occurring in two patients, one at the initial 20-mg dose, and one at the 200-mg dose level. Another five patients had asymptomatic TLS. Other treatment-related adverse events were anemia in seven patients, neutropenia in six patients, thrombocytopenia in five patients, and lung infection in one patient.
Twelve patients had a partial response, one had stable disease, and two had progressive disease. The mean time to best response was 71 days.
One-year progression-free survival was 49%, and 1-year overall survival was 68%.
The investigators found that for patients who still have some disease control with a BCRi, it may be possible to keep them on that drug while transitioning to venetoclax. The rapid dose escalation protocol should only be attempted in highly experience comprehensive cancer centers, Dr. Awan said.
“Under very close monitoring in an experienced inpatient setting, where the nurses are very used to doing this on a weekly basis in a very high volume center, I think that our data show that we could do this without affecting toxicity significantly or mortality,” he said.
Venetoclax therapy could buy enough time for patients to bridge to other options, such as chimeric antigen receptor (CAR) T-cell therapy or allogeneic stem cell transplant, he noted.
“But if we had waited 4 weeks, most of these patients would not have made it,” he said.
The study was internally funded. Dr. Awan reported research funding from Gilead, Pharmacyclics, AbbVie, and Janssen.
SOURCE: Koenig K et al. EHA Congress, Abstract PF357.
STOCKHOLM – Patients with chronic lymphocytic leukemia (CLL) who experience relapse after therapy with a B-cell receptor signaling inhibitor tend to have a swiftly progressive disease course that requires immediate intervention. For these patients, a rapid venetoclax dose-escalation protocol may be a safe way to quickly regain disease control, and possibly bridge to salvage therapies, investigators reported.
Of 15 patients with CLL who relapsed after treatment with a B-cell receptor inhibitor (BCRi), all were able to get to their target dose of venetoclax under close inpatient monitoring at a median of 12 days, compared with the 35 days usually required for venetoclax dose escalation, reported Farrukh T. Awan, MD, of Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues.
Only two patients developed clinical tumor lysis syndrome (TLS), a common occurrence with venetoclax therapy, and this adverse event was manageable, Dr. Awan said at the annual congress of the European Hematology Association.
“The reason why we have been doing a slow ramp up on venetoclax is the original toxicity issues that we saw early on,” he said in an interview. “But unfortunately, a lot of patients are progressing on these new agents and have very rapid disease progression, and what we have seen is that if you stop the ibrutinib, the disease progresses very quickly, and by the time they can get up to the effective dose of venetoclax, they’re too sick to continue, or they might even die from disease progression.”
To combat this problem, Dr. Awan and his colleagues developed a rapid dose escalation protocol that would ramp up from 20 mg to 400 mg, with increases every 1 or 2 days depending on tolerability and incident TLS. Lab tests for TLS were evaluated every 4-8 hours.
All patients were closely monitored in the hospital, and all were started on allopurinol or other uric acid–lowering agents before starting on venetoclax.
The investigators reported safety and efficacy outcomes for the patients in a retrospective analysis.
The median age of the patients, 12 men and 3 women, was 65 years (range, 58-86 years). Seven patients had Eastern Cooperative Oncology Group Performance Status of 0, seven had an ECOG score of 1, and one had a score of 2-4.
Ten patients had most recently been treated with a BCRi, either a Bruton’s tyrosine kinase inhibitor (ibrutinib or acalabrutinib), idelalisib, or entospletinib. Three patients received ibrutinib plus chemotherapy, and two received rituximab and dexamethasone followed by rituximab maintenance.
The median time to full venetoclax dose was 12 days (range, 5-21 days) and all 15 patients reached the target dose. The mean length of stay during the ramp-up period was 9.5 days (range, 6-22 days).
The incidence of clinical TLS was 13.2%, occurring in two patients, one at the initial 20-mg dose, and one at the 200-mg dose level. Another five patients had asymptomatic TLS. Other treatment-related adverse events were anemia in seven patients, neutropenia in six patients, thrombocytopenia in five patients, and lung infection in one patient.
Twelve patients had a partial response, one had stable disease, and two had progressive disease. The mean time to best response was 71 days.
One-year progression-free survival was 49%, and 1-year overall survival was 68%.
The investigators found that for patients who still have some disease control with a BCRi, it may be possible to keep them on that drug while transitioning to venetoclax. The rapid dose escalation protocol should only be attempted in highly experience comprehensive cancer centers, Dr. Awan said.
“Under very close monitoring in an experienced inpatient setting, where the nurses are very used to doing this on a weekly basis in a very high volume center, I think that our data show that we could do this without affecting toxicity significantly or mortality,” he said.
Venetoclax therapy could buy enough time for patients to bridge to other options, such as chimeric antigen receptor (CAR) T-cell therapy or allogeneic stem cell transplant, he noted.
“But if we had waited 4 weeks, most of these patients would not have made it,” he said.
The study was internally funded. Dr. Awan reported research funding from Gilead, Pharmacyclics, AbbVie, and Janssen.
SOURCE: Koenig K et al. EHA Congress, Abstract PF357.
REPORTING FROM THE EHA CONGRESS
Key clinical point:
Major finding: All patients reached the target dose of venetoclax, with only two cases of manageable clinical tumor lysis syndrome.
Study details: Retrospective analysis of outcomes for 15 patients with CLL who relapsed after treatment with a B-cell receptor signaling inhibitor.
Disclosures: The study was internally funded. Dr. Awan reported research funding from Gilead, Pharmacyclics, AbbVie, and Janssen.
Source: Koenig K et al. EHA Congress, Abstract PF357.
Is CLL chemoimmunotherapy dead? Not yet
CHICAGO – Chemoimmunotherapy for chronic lymphocytic leukemia is on the way out, but there’s one scenario where it still plays a key role, according to one leukemia expert.
That scenario is not in relapsed or refractory chronic lymphocytic leukemia (CLL), where the use of fludarabine, cyclophosphamide, and rituximab (FCR) may be hard to justify today. Data supporting use of FCR in relapsed CLL show a median progression-free survival (PFS) of about 21 months, Susan M. O’Brien, MD, of the University of California, Irvine, said at the annual meeting of the American Society of Clinical Oncology. There is also data for bendamustine-rituximab retreatment showing a median event-free survival of about 15 months, she added.
By contrast, the 5-year follow-up data for the Bruton tyrosine kinase inhibitor ibrutinib in the relapsed/refractory setting shows a median PFS of 52 months, which is “extraordinary,” given that the patients had a median of four prior regimens, Dr. O’Brien said.
Similarly, recently published results from the randomized, phase 3 MURANO study of venetoclax plus rituximab in relapsed/refractory CLL showed that median PFS was not reached at a median follow-up of 23.8 months, versus a median of 17 months for the bendamustine-rituximab comparison arm (N Engl J Med. 2018;378[12]:1107-20).
“Thanks to the MURANO study, we likely will have an expanded label for venetoclax that includes the combination of venetoclax and rituximab,” Dr. O’Brien said. “I think it’s quite clear that either of these is dramatically better than what you get with retreatment with chemotherapy, so I personally don’t think there is a role for chemoimmunotherapy in the relapsed patient.”
On June 8, 2018, the Food and Drug Administration granted regular approval for venetoclax for patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who have received at least one prior therapy. The FDA also approved its use in combination with rituximab.*
But frontline CLL treatment is currently a little bit more complicated, Dr. O’Brien said.
Recent studies show favorable long-term outcomes with FCR frontline therapy in the immunoglobulin heavy chain variable gene (IgHV) –mutated subgroup of patients, she noted.
The longest follow-up comes from a study from investigators at the University of Texas MD Anderson Cancer Center, Houston, published in 2016. In that study, the 12.8-year PFS was 53.9% for IgHV-mutated patients, versus just 8.7% for patients with unmutated IgHV. Of the IgHV-mutated group, more than half achieved minimal residual disease (MRD) negativity after treatment (Blood. 2016 Jan 21; 127[3]: 303-9).
“I’m going to go out on a limb and I’m going to suggest that I think there is a cure fraction here,” Dr. O’Brien said. “On the other hand, if there’s not a cure fraction and they’re going to relapse after 17 years, that’s a pretty attractive endpoint, even if it’s not a cure fraction.”
Clinical practice guidelines now recognize IgHV mutation status as an important marker that should be obtained when deciding on treatment, Dr. O’Brien noted.
For unmutated patients, the RESONATE-2 trial showed that ibrutinib was superior to chlorambucil in older patients, many of whom had comorbid conditions. In the 3-year update, median PFS was approximately 15 months for chlorambucil, while for ibrutinib the median PFS was “nowhere near” being reached, Dr. O’Brien said.
Those data may not be so relevant for fit, unmutated patients, and two randomized trials comparing FCR with bendamustine and rituximab have yet to report data. However, one recent cross-trial comparison found fairly overlapping survival curves for the two chemoimmunotherapy approaches.
Dr. O’Brien said she would put older patients with comorbidities on ibrutinib if a clinical trial was not available, and for fit, unmutated patients, while more data are needed, she would also use ibrutinib. However, patient preference sometimes tips the scale in favor of FCR.
“The discussions sometimes are quite long about whether the patient should opt to take ibrutinib or FCR,” Dr. O’Brien said. “The last patient I had that discussion with elected to take FCR. When I asked him why, he said because he liked the idea of being finished in six cycles, off all therapy, and hopefully in remission.”
While Dr. O’Brien said she views chemoimmunotherapy as still relevant in IgHV-mutated patients, eventually it will go away, she concluded. Toward that end, there is considerable interest in venetoclax plus ibrutinib, a combination that, in early reports, has yielded very encouraging MRD results in first-line CLL.
“We have no long-term data, but very, very exciting MRD negativity data,” Dr. O’Brien said.
Dr. O’Brien reported relationships with Abbvie, Amgen, Celgene, Gilead Sciences, Janssen, Pfizer, Pharmacyclics, Sunesis Pharmaceuticals, and others.
*This story was updated 6/25/2018.
CHICAGO – Chemoimmunotherapy for chronic lymphocytic leukemia is on the way out, but there’s one scenario where it still plays a key role, according to one leukemia expert.
That scenario is not in relapsed or refractory chronic lymphocytic leukemia (CLL), where the use of fludarabine, cyclophosphamide, and rituximab (FCR) may be hard to justify today. Data supporting use of FCR in relapsed CLL show a median progression-free survival (PFS) of about 21 months, Susan M. O’Brien, MD, of the University of California, Irvine, said at the annual meeting of the American Society of Clinical Oncology. There is also data for bendamustine-rituximab retreatment showing a median event-free survival of about 15 months, she added.
By contrast, the 5-year follow-up data for the Bruton tyrosine kinase inhibitor ibrutinib in the relapsed/refractory setting shows a median PFS of 52 months, which is “extraordinary,” given that the patients had a median of four prior regimens, Dr. O’Brien said.
Similarly, recently published results from the randomized, phase 3 MURANO study of venetoclax plus rituximab in relapsed/refractory CLL showed that median PFS was not reached at a median follow-up of 23.8 months, versus a median of 17 months for the bendamustine-rituximab comparison arm (N Engl J Med. 2018;378[12]:1107-20).
“Thanks to the MURANO study, we likely will have an expanded label for venetoclax that includes the combination of venetoclax and rituximab,” Dr. O’Brien said. “I think it’s quite clear that either of these is dramatically better than what you get with retreatment with chemotherapy, so I personally don’t think there is a role for chemoimmunotherapy in the relapsed patient.”
On June 8, 2018, the Food and Drug Administration granted regular approval for venetoclax for patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who have received at least one prior therapy. The FDA also approved its use in combination with rituximab.*
But frontline CLL treatment is currently a little bit more complicated, Dr. O’Brien said.
Recent studies show favorable long-term outcomes with FCR frontline therapy in the immunoglobulin heavy chain variable gene (IgHV) –mutated subgroup of patients, she noted.
The longest follow-up comes from a study from investigators at the University of Texas MD Anderson Cancer Center, Houston, published in 2016. In that study, the 12.8-year PFS was 53.9% for IgHV-mutated patients, versus just 8.7% for patients with unmutated IgHV. Of the IgHV-mutated group, more than half achieved minimal residual disease (MRD) negativity after treatment (Blood. 2016 Jan 21; 127[3]: 303-9).
“I’m going to go out on a limb and I’m going to suggest that I think there is a cure fraction here,” Dr. O’Brien said. “On the other hand, if there’s not a cure fraction and they’re going to relapse after 17 years, that’s a pretty attractive endpoint, even if it’s not a cure fraction.”
Clinical practice guidelines now recognize IgHV mutation status as an important marker that should be obtained when deciding on treatment, Dr. O’Brien noted.
For unmutated patients, the RESONATE-2 trial showed that ibrutinib was superior to chlorambucil in older patients, many of whom had comorbid conditions. In the 3-year update, median PFS was approximately 15 months for chlorambucil, while for ibrutinib the median PFS was “nowhere near” being reached, Dr. O’Brien said.
Those data may not be so relevant for fit, unmutated patients, and two randomized trials comparing FCR with bendamustine and rituximab have yet to report data. However, one recent cross-trial comparison found fairly overlapping survival curves for the two chemoimmunotherapy approaches.
Dr. O’Brien said she would put older patients with comorbidities on ibrutinib if a clinical trial was not available, and for fit, unmutated patients, while more data are needed, she would also use ibrutinib. However, patient preference sometimes tips the scale in favor of FCR.
“The discussions sometimes are quite long about whether the patient should opt to take ibrutinib or FCR,” Dr. O’Brien said. “The last patient I had that discussion with elected to take FCR. When I asked him why, he said because he liked the idea of being finished in six cycles, off all therapy, and hopefully in remission.”
While Dr. O’Brien said she views chemoimmunotherapy as still relevant in IgHV-mutated patients, eventually it will go away, she concluded. Toward that end, there is considerable interest in venetoclax plus ibrutinib, a combination that, in early reports, has yielded very encouraging MRD results in first-line CLL.
“We have no long-term data, but very, very exciting MRD negativity data,” Dr. O’Brien said.
Dr. O’Brien reported relationships with Abbvie, Amgen, Celgene, Gilead Sciences, Janssen, Pfizer, Pharmacyclics, Sunesis Pharmaceuticals, and others.
*This story was updated 6/25/2018.
CHICAGO – Chemoimmunotherapy for chronic lymphocytic leukemia is on the way out, but there’s one scenario where it still plays a key role, according to one leukemia expert.
That scenario is not in relapsed or refractory chronic lymphocytic leukemia (CLL), where the use of fludarabine, cyclophosphamide, and rituximab (FCR) may be hard to justify today. Data supporting use of FCR in relapsed CLL show a median progression-free survival (PFS) of about 21 months, Susan M. O’Brien, MD, of the University of California, Irvine, said at the annual meeting of the American Society of Clinical Oncology. There is also data for bendamustine-rituximab retreatment showing a median event-free survival of about 15 months, she added.
By contrast, the 5-year follow-up data for the Bruton tyrosine kinase inhibitor ibrutinib in the relapsed/refractory setting shows a median PFS of 52 months, which is “extraordinary,” given that the patients had a median of four prior regimens, Dr. O’Brien said.
Similarly, recently published results from the randomized, phase 3 MURANO study of venetoclax plus rituximab in relapsed/refractory CLL showed that median PFS was not reached at a median follow-up of 23.8 months, versus a median of 17 months for the bendamustine-rituximab comparison arm (N Engl J Med. 2018;378[12]:1107-20).
“Thanks to the MURANO study, we likely will have an expanded label for venetoclax that includes the combination of venetoclax and rituximab,” Dr. O’Brien said. “I think it’s quite clear that either of these is dramatically better than what you get with retreatment with chemotherapy, so I personally don’t think there is a role for chemoimmunotherapy in the relapsed patient.”
On June 8, 2018, the Food and Drug Administration granted regular approval for venetoclax for patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who have received at least one prior therapy. The FDA also approved its use in combination with rituximab.*
But frontline CLL treatment is currently a little bit more complicated, Dr. O’Brien said.
Recent studies show favorable long-term outcomes with FCR frontline therapy in the immunoglobulin heavy chain variable gene (IgHV) –mutated subgroup of patients, she noted.
The longest follow-up comes from a study from investigators at the University of Texas MD Anderson Cancer Center, Houston, published in 2016. In that study, the 12.8-year PFS was 53.9% for IgHV-mutated patients, versus just 8.7% for patients with unmutated IgHV. Of the IgHV-mutated group, more than half achieved minimal residual disease (MRD) negativity after treatment (Blood. 2016 Jan 21; 127[3]: 303-9).
“I’m going to go out on a limb and I’m going to suggest that I think there is a cure fraction here,” Dr. O’Brien said. “On the other hand, if there’s not a cure fraction and they’re going to relapse after 17 years, that’s a pretty attractive endpoint, even if it’s not a cure fraction.”
Clinical practice guidelines now recognize IgHV mutation status as an important marker that should be obtained when deciding on treatment, Dr. O’Brien noted.
For unmutated patients, the RESONATE-2 trial showed that ibrutinib was superior to chlorambucil in older patients, many of whom had comorbid conditions. In the 3-year update, median PFS was approximately 15 months for chlorambucil, while for ibrutinib the median PFS was “nowhere near” being reached, Dr. O’Brien said.
Those data may not be so relevant for fit, unmutated patients, and two randomized trials comparing FCR with bendamustine and rituximab have yet to report data. However, one recent cross-trial comparison found fairly overlapping survival curves for the two chemoimmunotherapy approaches.
Dr. O’Brien said she would put older patients with comorbidities on ibrutinib if a clinical trial was not available, and for fit, unmutated patients, while more data are needed, she would also use ibrutinib. However, patient preference sometimes tips the scale in favor of FCR.
“The discussions sometimes are quite long about whether the patient should opt to take ibrutinib or FCR,” Dr. O’Brien said. “The last patient I had that discussion with elected to take FCR. When I asked him why, he said because he liked the idea of being finished in six cycles, off all therapy, and hopefully in remission.”
While Dr. O’Brien said she views chemoimmunotherapy as still relevant in IgHV-mutated patients, eventually it will go away, she concluded. Toward that end, there is considerable interest in venetoclax plus ibrutinib, a combination that, in early reports, has yielded very encouraging MRD results in first-line CLL.
“We have no long-term data, but very, very exciting MRD negativity data,” Dr. O’Brien said.
Dr. O’Brien reported relationships with Abbvie, Amgen, Celgene, Gilead Sciences, Janssen, Pfizer, Pharmacyclics, Sunesis Pharmaceuticals, and others.
*This story was updated 6/25/2018.
EXPERT ANALYSIS FROM ASCO 2018
FDA grants regular approval to venetoclax for CLL/SLL
Venetoclax (Venclexta) has received regular approval from the Food and Drug Administration for the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), with or without 17p deletion, who have received at least one prior therapy.
The approval was based results from the MURANO trial of 389 patients, which was a randomized, multicenter, open-label trial of venetoclax plus rituximab versus bendamustine plus rituximab.
Neutropenia, diarrhea, upper respiratory tract infection, fatigue, cough, and nausea were the most common adverse events seen in the venetoclax arm. Grade 3 or 4 neutropenia developed in 64% of those patients, and grade 4 in 31%. The most common infection in venetoclax patients was pneumonia, but overall, 21% of patients in that arm experienced some kind of infection.
Because of the rapid reduction in tumor size, tumor lysis syndrome is possible with venetoclax treatment, the FDA noted.
In 2016, the FDA granted accelerated approval to venetoclax for treatment of patients with CLL with 17d deletion who had received at least one prior line of therapy.
Venetoclax (Venclexta) has received regular approval from the Food and Drug Administration for the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), with or without 17p deletion, who have received at least one prior therapy.
The approval was based results from the MURANO trial of 389 patients, which was a randomized, multicenter, open-label trial of venetoclax plus rituximab versus bendamustine plus rituximab.
Neutropenia, diarrhea, upper respiratory tract infection, fatigue, cough, and nausea were the most common adverse events seen in the venetoclax arm. Grade 3 or 4 neutropenia developed in 64% of those patients, and grade 4 in 31%. The most common infection in venetoclax patients was pneumonia, but overall, 21% of patients in that arm experienced some kind of infection.
Because of the rapid reduction in tumor size, tumor lysis syndrome is possible with venetoclax treatment, the FDA noted.
In 2016, the FDA granted accelerated approval to venetoclax for treatment of patients with CLL with 17d deletion who had received at least one prior line of therapy.
Venetoclax (Venclexta) has received regular approval from the Food and Drug Administration for the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), with or without 17p deletion, who have received at least one prior therapy.
The approval was based results from the MURANO trial of 389 patients, which was a randomized, multicenter, open-label trial of venetoclax plus rituximab versus bendamustine plus rituximab.
Neutropenia, diarrhea, upper respiratory tract infection, fatigue, cough, and nausea were the most common adverse events seen in the venetoclax arm. Grade 3 or 4 neutropenia developed in 64% of those patients, and grade 4 in 31%. The most common infection in venetoclax patients was pneumonia, but overall, 21% of patients in that arm experienced some kind of infection.
Because of the rapid reduction in tumor size, tumor lysis syndrome is possible with venetoclax treatment, the FDA noted.
In 2016, the FDA granted accelerated approval to venetoclax for treatment of patients with CLL with 17d deletion who had received at least one prior line of therapy.
Venetoclax plus ibrutinib yields encouraging MRD results in first-line CLL
CHICAGO – The combination of ibrutinib plus venetoclax yielded a high rate of undetectable minimal residual disease (MRD) when used as first-line treatment for chronic lymphocytic leukemia (CLL), according to preliminary results of the CAPTIVATE trial.
Of the first 30 patients in the trial, 23 (77%) had undetectable blood MRD after just six cycles of combined treatment, said investigator William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” Dr. Wierda said in a presentation of the CAPTIVATE results at the annual meeting of the American Society of Clinical Oncology.
Those MRD results are “at least as good as we can achieve with chemoimmunotherapy,” Bruce D. Cheson, MD, head of hematology at Georgetown University, Washington, said during a discussion of the CAPTIVATE study results.
Dr. Cheson referenced MRD results from a 2016 analysis of the CLL8 and CLL10 trials, which included patients treated with fludarabine, cyclophosphamide, and rituximab (FCR) and bendamustine plus rituximab (BR). In that analysis, 33.6% of patients achieved MRD-negative complete response and 29.1% achieved MRD-negative partial response.
In CAPTIVATE, by contrast, all of the complete remissions were MRD negative, as were a majority of the partial responders, Dr. Cheson noted.
Venetoclax and ibrutinib have “clinically complimentary activity” that provided a rationale for combining the two, Dr. Wierda said at ASCO. Ibrutinib is a BTK inhibitor that has a high rate of response and durable disease control, though continuous treatment is indicated, he said, because most patients achieve partial remissions as best response and continue to have residual disease in blood or bone marrow. Venetoclax, he added, is a BCL-2 inhibitor that produces durable partial remissions, though “residual disease is typically present in the form of persistently enlarged lymph nodes,” he said. “Venetoclax is highly effective at clearing disease from blood and bone marrow.”
The phase 2 CAPTIVATE trial includes a total of 164 patients younger than 70 years of age who receive a 3-cycle ibrutinib lead-in, followed by ibrutinib plus venetoclax for 12 cycles. At that point, patients are randomized according to MRD status. Patients with confirmed undetectable MRD are randomized to further treatment with ibrutinib or placebo, and those with undetectable MRD not confirmed are randomized to ibrutinib versus ibrutinib plus venetoclax.
In addition to early efficacy data, Dr. Wierda also reported some safety data. Compared with the single-agent ibrutinib lead-in period, combined ibrutinib plus venetoclax treatment had more gastrointestinal-associated events and neutropenia. Almost half of patients (45%) have had a treatment-related grade 3-4 adverse event, though just 18 (11%) have had treatment-related adverse events classified as serious, and there have been no adverse event-related deaths on study.
The high activity of ibrutinib plus venetoclax in CAPTIVATE supports further study of the combination, Dr. Wierda said. A randomized, open-label phase 3 trial of ibrutinib plus venetoclax versus chlorambucil plus obinutuzumab as first-line treatment for CLL is currently recruiting.
The study was sponsored by Pharmacyclics, an AbbVie company. Dr. Wierda reported consulting and research funding from Pharmacyclics, AbbVie, and several other companies.
SOURCE: Wierda WG et al. ASCO 2018, Abstract 7502.
CHICAGO – The combination of ibrutinib plus venetoclax yielded a high rate of undetectable minimal residual disease (MRD) when used as first-line treatment for chronic lymphocytic leukemia (CLL), according to preliminary results of the CAPTIVATE trial.
Of the first 30 patients in the trial, 23 (77%) had undetectable blood MRD after just six cycles of combined treatment, said investigator William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” Dr. Wierda said in a presentation of the CAPTIVATE results at the annual meeting of the American Society of Clinical Oncology.
Those MRD results are “at least as good as we can achieve with chemoimmunotherapy,” Bruce D. Cheson, MD, head of hematology at Georgetown University, Washington, said during a discussion of the CAPTIVATE study results.
Dr. Cheson referenced MRD results from a 2016 analysis of the CLL8 and CLL10 trials, which included patients treated with fludarabine, cyclophosphamide, and rituximab (FCR) and bendamustine plus rituximab (BR). In that analysis, 33.6% of patients achieved MRD-negative complete response and 29.1% achieved MRD-negative partial response.
In CAPTIVATE, by contrast, all of the complete remissions were MRD negative, as were a majority of the partial responders, Dr. Cheson noted.
Venetoclax and ibrutinib have “clinically complimentary activity” that provided a rationale for combining the two, Dr. Wierda said at ASCO. Ibrutinib is a BTK inhibitor that has a high rate of response and durable disease control, though continuous treatment is indicated, he said, because most patients achieve partial remissions as best response and continue to have residual disease in blood or bone marrow. Venetoclax, he added, is a BCL-2 inhibitor that produces durable partial remissions, though “residual disease is typically present in the form of persistently enlarged lymph nodes,” he said. “Venetoclax is highly effective at clearing disease from blood and bone marrow.”
The phase 2 CAPTIVATE trial includes a total of 164 patients younger than 70 years of age who receive a 3-cycle ibrutinib lead-in, followed by ibrutinib plus venetoclax for 12 cycles. At that point, patients are randomized according to MRD status. Patients with confirmed undetectable MRD are randomized to further treatment with ibrutinib or placebo, and those with undetectable MRD not confirmed are randomized to ibrutinib versus ibrutinib plus venetoclax.
In addition to early efficacy data, Dr. Wierda also reported some safety data. Compared with the single-agent ibrutinib lead-in period, combined ibrutinib plus venetoclax treatment had more gastrointestinal-associated events and neutropenia. Almost half of patients (45%) have had a treatment-related grade 3-4 adverse event, though just 18 (11%) have had treatment-related adverse events classified as serious, and there have been no adverse event-related deaths on study.
The high activity of ibrutinib plus venetoclax in CAPTIVATE supports further study of the combination, Dr. Wierda said. A randomized, open-label phase 3 trial of ibrutinib plus venetoclax versus chlorambucil plus obinutuzumab as first-line treatment for CLL is currently recruiting.
The study was sponsored by Pharmacyclics, an AbbVie company. Dr. Wierda reported consulting and research funding from Pharmacyclics, AbbVie, and several other companies.
SOURCE: Wierda WG et al. ASCO 2018, Abstract 7502.
CHICAGO – The combination of ibrutinib plus venetoclax yielded a high rate of undetectable minimal residual disease (MRD) when used as first-line treatment for chronic lymphocytic leukemia (CLL), according to preliminary results of the CAPTIVATE trial.
Of the first 30 patients in the trial, 23 (77%) had undetectable blood MRD after just six cycles of combined treatment, said investigator William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“These early results show a highly active and safe treatment with 12 cycles of combined treatment with ibrutinib and venetoclax,” Dr. Wierda said in a presentation of the CAPTIVATE results at the annual meeting of the American Society of Clinical Oncology.
Those MRD results are “at least as good as we can achieve with chemoimmunotherapy,” Bruce D. Cheson, MD, head of hematology at Georgetown University, Washington, said during a discussion of the CAPTIVATE study results.
Dr. Cheson referenced MRD results from a 2016 analysis of the CLL8 and CLL10 trials, which included patients treated with fludarabine, cyclophosphamide, and rituximab (FCR) and bendamustine plus rituximab (BR). In that analysis, 33.6% of patients achieved MRD-negative complete response and 29.1% achieved MRD-negative partial response.
In CAPTIVATE, by contrast, all of the complete remissions were MRD negative, as were a majority of the partial responders, Dr. Cheson noted.
Venetoclax and ibrutinib have “clinically complimentary activity” that provided a rationale for combining the two, Dr. Wierda said at ASCO. Ibrutinib is a BTK inhibitor that has a high rate of response and durable disease control, though continuous treatment is indicated, he said, because most patients achieve partial remissions as best response and continue to have residual disease in blood or bone marrow. Venetoclax, he added, is a BCL-2 inhibitor that produces durable partial remissions, though “residual disease is typically present in the form of persistently enlarged lymph nodes,” he said. “Venetoclax is highly effective at clearing disease from blood and bone marrow.”
The phase 2 CAPTIVATE trial includes a total of 164 patients younger than 70 years of age who receive a 3-cycle ibrutinib lead-in, followed by ibrutinib plus venetoclax for 12 cycles. At that point, patients are randomized according to MRD status. Patients with confirmed undetectable MRD are randomized to further treatment with ibrutinib or placebo, and those with undetectable MRD not confirmed are randomized to ibrutinib versus ibrutinib plus venetoclax.
In addition to early efficacy data, Dr. Wierda also reported some safety data. Compared with the single-agent ibrutinib lead-in period, combined ibrutinib plus venetoclax treatment had more gastrointestinal-associated events and neutropenia. Almost half of patients (45%) have had a treatment-related grade 3-4 adverse event, though just 18 (11%) have had treatment-related adverse events classified as serious, and there have been no adverse event-related deaths on study.
The high activity of ibrutinib plus venetoclax in CAPTIVATE supports further study of the combination, Dr. Wierda said. A randomized, open-label phase 3 trial of ibrutinib plus venetoclax versus chlorambucil plus obinutuzumab as first-line treatment for CLL is currently recruiting.
The study was sponsored by Pharmacyclics, an AbbVie company. Dr. Wierda reported consulting and research funding from Pharmacyclics, AbbVie, and several other companies.
SOURCE: Wierda WG et al. ASCO 2018, Abstract 7502.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: Of 14 patients, 12 (86%) who completed 12 cycles of treatment had undetectable bone marrow MRD.
Study details: Early results of the phase 2 CAPTIVATE trial including 164 patients younger than 70 years of age with previously untreated CLL.
Disclosures: The study was sponsored by Pharmacyclics, an Abbvie company. Dr. Wierda reported consulting and research funding from Pharmacyclics, AbbVie, and several other companies.
Source: Wierda WG et al. ASCO 2018, Abstract 7502.
Older CLL and NHL patients are more vulnerable to toxicities
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Key clinical point:
Major finding: Older CLL patients had significantly higher odds of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI 1.39-1.55).
Study details: An analysis of data from 1,199 CLL and NHL patients in the Alliance for Clinical Trials in Oncology.
Disclosures: The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
Source: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
5-year data show deepening response with ibrutinib in CLL
Single-agent ibrutinib has had sustained efficacy and a rate of complete response that has increased over time, according to a 5-year follow-up report including 132 patients with chronic lymphocytic leukemia (CLL).
Efficacy has been maintained in both treatment-naive and relapsed/refractory CLL, despite the presence of high-risk genomic features in many patients, investigators reported in Blood.
Treatment has been well tolerated, and the occurrence of severe adverse events has diminished over time, according to Susan M. O’Brien, MD, of the Chao Family Comprehensive Cancer Center, University of California, Irvine, and her colleagues.
“The safety profile of ibrutinib over time remains acceptable and manageable, allowing almost one-half of the patients (48%) to be treated for more than 4 years and thus maximize response,” the investigators wrote.
The report was based on 5-year follow-up of patients with CLL who had been enrolled in a phase 1b/2 study (PCYC-1102) and an extension study (PCYC-1103). A total of 132 patients were evaluated, including 101 with relapsed/refractory disease and 31 who were treatment naive.
The overall response rate remained high, at 89% in this 5-year follow-up. Complete response rates increased over time, reaching 29% in treatment-naive patients and 10% in relapsed/refractory patients. In a previous report on 3-year follow-up for these patients, investigators reported complete response rates of 23% in the previously untreated group and 7% in the relapsed/refractory group. The new findings demonstrate “deepening of responses” with continued ibrutinib therapy, Dr. O’Brien and her coauthors wrote.
The 5-year rate of progression-free survival was 44% for relapsed/refractory patients and 92% for treatment-naive patients in this study. Median progression-free survival was 51 months for the relapsed/refractory cohort. “[Progression-free survival] with single-agent ibrutinib in [treatment-naive] patients appears particularly favorable, because the median has not been reached,” investigators wrote.
Adverse events that limited treatment were more frequent during the first year of treatment than in subsequent years, data show, while new onset of neutropenia and thrombocytopenia decreased over time.
The overall response rate was high even in patients with high-risk genetic features. Rates of overall response ranged from 79% to 97%, depending on genomic subgroup. That held true for relapsed/refractory CLL patients with del(17p), a significant negative prognostic factor for survival. In that group, the overall response rate was 79% and the duration of response was 31 months, representing “promising single-agent efficacy” in that group, investigators said.
Pharmacyclics, an AbbVie Company, provided funding for the study and writing support. The study was also supported by grants from the National Institutes of Health and a private foundation. Dr. O’Brien reported ties to AbbVie, Janssen, and Pharmacyclics. Other investigators reported financial relationships with various pharmaceutical companies.
SOURCE: O’Brien S et al. Blood. 2018;131(17):1910-9.
This report on the 5-year experience with single-agent ibrutinib in chronic lymphocytic leukemia (CLL) is a step forward in knowledge of the drug’s natural history, according to Jennifer R. Brown, MD, PhD.
“Ibrutinib data are starting to mature, but much opportunity for growth remains,” Dr. Brown said in an editorial.
One notable update in the report is that a median, progression-free survival has been reached in patients with relapsed/refractory CLL. The reported 51-month median progression-free survival is “strikingly good” in this cohort of patients with high-risk disease, and compares favorably to older regimens in similar patient populations, she said.
Regarding previously untreated CLL patients, it is notable that 45% of this cohort discontinued treatment, many apparently after year 4, Dr. Brown said. The finding that median duration on therapy was just about 5.5 years in the cohort could be “potentially quite useful” in counseling patients, if confirmed in a larger cohort, she added.
Given the discontinuation data, one unanswered question is the durability of remission after stopping ibrutinib in a “deep but probably not complete remission” versus continuing therapy.
“Further follow-up of patients who discontinue without disease progression, as well as systematic investigation of time-limited therapy, including novel likely combination approaches, is clearly warranted,” Dr. Brown said in her editorial.
Dr. Jennifer R. Brown is with the Dana-Farber Cancer Institute in Boston. These comments are adapted an accompanying editorial ( Blood. 2018;131:1880-2 ). Dr. Brown reported ties to Janssen, Pharmacyclics, AstraZeneca, Sun, Redx, Sunesis, Loxo, Gilead, TG Therapeutics, Verastem, and AbbVie.
This report on the 5-year experience with single-agent ibrutinib in chronic lymphocytic leukemia (CLL) is a step forward in knowledge of the drug’s natural history, according to Jennifer R. Brown, MD, PhD.
“Ibrutinib data are starting to mature, but much opportunity for growth remains,” Dr. Brown said in an editorial.
One notable update in the report is that a median, progression-free survival has been reached in patients with relapsed/refractory CLL. The reported 51-month median progression-free survival is “strikingly good” in this cohort of patients with high-risk disease, and compares favorably to older regimens in similar patient populations, she said.
Regarding previously untreated CLL patients, it is notable that 45% of this cohort discontinued treatment, many apparently after year 4, Dr. Brown said. The finding that median duration on therapy was just about 5.5 years in the cohort could be “potentially quite useful” in counseling patients, if confirmed in a larger cohort, she added.
Given the discontinuation data, one unanswered question is the durability of remission after stopping ibrutinib in a “deep but probably not complete remission” versus continuing therapy.
“Further follow-up of patients who discontinue without disease progression, as well as systematic investigation of time-limited therapy, including novel likely combination approaches, is clearly warranted,” Dr. Brown said in her editorial.
Dr. Jennifer R. Brown is with the Dana-Farber Cancer Institute in Boston. These comments are adapted an accompanying editorial ( Blood. 2018;131:1880-2 ). Dr. Brown reported ties to Janssen, Pharmacyclics, AstraZeneca, Sun, Redx, Sunesis, Loxo, Gilead, TG Therapeutics, Verastem, and AbbVie.
This report on the 5-year experience with single-agent ibrutinib in chronic lymphocytic leukemia (CLL) is a step forward in knowledge of the drug’s natural history, according to Jennifer R. Brown, MD, PhD.
“Ibrutinib data are starting to mature, but much opportunity for growth remains,” Dr. Brown said in an editorial.
One notable update in the report is that a median, progression-free survival has been reached in patients with relapsed/refractory CLL. The reported 51-month median progression-free survival is “strikingly good” in this cohort of patients with high-risk disease, and compares favorably to older regimens in similar patient populations, she said.
Regarding previously untreated CLL patients, it is notable that 45% of this cohort discontinued treatment, many apparently after year 4, Dr. Brown said. The finding that median duration on therapy was just about 5.5 years in the cohort could be “potentially quite useful” in counseling patients, if confirmed in a larger cohort, she added.
Given the discontinuation data, one unanswered question is the durability of remission after stopping ibrutinib in a “deep but probably not complete remission” versus continuing therapy.
“Further follow-up of patients who discontinue without disease progression, as well as systematic investigation of time-limited therapy, including novel likely combination approaches, is clearly warranted,” Dr. Brown said in her editorial.
Dr. Jennifer R. Brown is with the Dana-Farber Cancer Institute in Boston. These comments are adapted an accompanying editorial ( Blood. 2018;131:1880-2 ). Dr. Brown reported ties to Janssen, Pharmacyclics, AstraZeneca, Sun, Redx, Sunesis, Loxo, Gilead, TG Therapeutics, Verastem, and AbbVie.
Single-agent ibrutinib has had sustained efficacy and a rate of complete response that has increased over time, according to a 5-year follow-up report including 132 patients with chronic lymphocytic leukemia (CLL).
Efficacy has been maintained in both treatment-naive and relapsed/refractory CLL, despite the presence of high-risk genomic features in many patients, investigators reported in Blood.
Treatment has been well tolerated, and the occurrence of severe adverse events has diminished over time, according to Susan M. O’Brien, MD, of the Chao Family Comprehensive Cancer Center, University of California, Irvine, and her colleagues.
“The safety profile of ibrutinib over time remains acceptable and manageable, allowing almost one-half of the patients (48%) to be treated for more than 4 years and thus maximize response,” the investigators wrote.
The report was based on 5-year follow-up of patients with CLL who had been enrolled in a phase 1b/2 study (PCYC-1102) and an extension study (PCYC-1103). A total of 132 patients were evaluated, including 101 with relapsed/refractory disease and 31 who were treatment naive.
The overall response rate remained high, at 89% in this 5-year follow-up. Complete response rates increased over time, reaching 29% in treatment-naive patients and 10% in relapsed/refractory patients. In a previous report on 3-year follow-up for these patients, investigators reported complete response rates of 23% in the previously untreated group and 7% in the relapsed/refractory group. The new findings demonstrate “deepening of responses” with continued ibrutinib therapy, Dr. O’Brien and her coauthors wrote.
The 5-year rate of progression-free survival was 44% for relapsed/refractory patients and 92% for treatment-naive patients in this study. Median progression-free survival was 51 months for the relapsed/refractory cohort. “[Progression-free survival] with single-agent ibrutinib in [treatment-naive] patients appears particularly favorable, because the median has not been reached,” investigators wrote.
Adverse events that limited treatment were more frequent during the first year of treatment than in subsequent years, data show, while new onset of neutropenia and thrombocytopenia decreased over time.
The overall response rate was high even in patients with high-risk genetic features. Rates of overall response ranged from 79% to 97%, depending on genomic subgroup. That held true for relapsed/refractory CLL patients with del(17p), a significant negative prognostic factor for survival. In that group, the overall response rate was 79% and the duration of response was 31 months, representing “promising single-agent efficacy” in that group, investigators said.
Pharmacyclics, an AbbVie Company, provided funding for the study and writing support. The study was also supported by grants from the National Institutes of Health and a private foundation. Dr. O’Brien reported ties to AbbVie, Janssen, and Pharmacyclics. Other investigators reported financial relationships with various pharmaceutical companies.
SOURCE: O’Brien S et al. Blood. 2018;131(17):1910-9.
Single-agent ibrutinib has had sustained efficacy and a rate of complete response that has increased over time, according to a 5-year follow-up report including 132 patients with chronic lymphocytic leukemia (CLL).
Efficacy has been maintained in both treatment-naive and relapsed/refractory CLL, despite the presence of high-risk genomic features in many patients, investigators reported in Blood.
Treatment has been well tolerated, and the occurrence of severe adverse events has diminished over time, according to Susan M. O’Brien, MD, of the Chao Family Comprehensive Cancer Center, University of California, Irvine, and her colleagues.
“The safety profile of ibrutinib over time remains acceptable and manageable, allowing almost one-half of the patients (48%) to be treated for more than 4 years and thus maximize response,” the investigators wrote.
The report was based on 5-year follow-up of patients with CLL who had been enrolled in a phase 1b/2 study (PCYC-1102) and an extension study (PCYC-1103). A total of 132 patients were evaluated, including 101 with relapsed/refractory disease and 31 who were treatment naive.
The overall response rate remained high, at 89% in this 5-year follow-up. Complete response rates increased over time, reaching 29% in treatment-naive patients and 10% in relapsed/refractory patients. In a previous report on 3-year follow-up for these patients, investigators reported complete response rates of 23% in the previously untreated group and 7% in the relapsed/refractory group. The new findings demonstrate “deepening of responses” with continued ibrutinib therapy, Dr. O’Brien and her coauthors wrote.
The 5-year rate of progression-free survival was 44% for relapsed/refractory patients and 92% for treatment-naive patients in this study. Median progression-free survival was 51 months for the relapsed/refractory cohort. “[Progression-free survival] with single-agent ibrutinib in [treatment-naive] patients appears particularly favorable, because the median has not been reached,” investigators wrote.
Adverse events that limited treatment were more frequent during the first year of treatment than in subsequent years, data show, while new onset of neutropenia and thrombocytopenia decreased over time.
The overall response rate was high even in patients with high-risk genetic features. Rates of overall response ranged from 79% to 97%, depending on genomic subgroup. That held true for relapsed/refractory CLL patients with del(17p), a significant negative prognostic factor for survival. In that group, the overall response rate was 79% and the duration of response was 31 months, representing “promising single-agent efficacy” in that group, investigators said.
Pharmacyclics, an AbbVie Company, provided funding for the study and writing support. The study was also supported by grants from the National Institutes of Health and a private foundation. Dr. O’Brien reported ties to AbbVie, Janssen, and Pharmacyclics. Other investigators reported financial relationships with various pharmaceutical companies.
SOURCE: O’Brien S et al. Blood. 2018;131(17):1910-9.
FROM BLOOD
Key clinical point:
Major finding: The 5-year rate of progression-free survival was 44% for relapsed/refractory patients and 92% for treatment-naive patients.
Study details: Report on 5-year follow-up of 132 patients with CLL enrolled in a phase 1b/2 study (PCYC-1102) and an extension study (PCYC-1103).
Disclosures: Pharmacyclics, an AbbVie Company, provided funding for the study and writing support. The study was also supported by grants from the National Institutes of Health and a private foundation. The authors reported ties to Pharmacyclics and other companies.
Source: O’Brien S et al. Blood. 2018;131(17):1910-9.
Venetoclax shows muscle against CLL relapsed after idelalisib
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
For patients with relapsed or refractory chronic lymphocytic leukemia despite therapy with idelalisib (Zydelig), venetoclax (Venclexta) was associated with relatively high overall response and progression-free survival rates, results of a phase 2 study show.
Among 36 patients with relapsed/refractory CLL who had received idelalisib as their most recent B-cell receptor pathway inhibitor (BCRi), the overall response rate (ORR) was 67%, and median progression-free and overall survival (PFS and OS) had not been reached after 14 months of follow-up, reported Steven Coutre, MD, of Stanford (Calif.) University, and his colleagues.
“[V]enetoclax monotherapy is active and well-tolerated in patients with CLL progression after therapy with idelalisib, including a significant number of patients who also received prior therapy with ibrutinib [Imbruvica]. These results from the first prospective trial in this high-risk population provide evidence that venetoclax should be considered as a treatment option for such patients,” the investigators wrote. The report was published in Blood.
In clinical trials with idelalisib, approximately one-third of patients with CLL experienced disease progression on therapy, and other patients had to discontinue the drug, an inhibitor of the delta isoform of phosphoinositide 3-kinase (PI3K), because of toxicities, the investigators noted.
“The optimal treatment of patients with CLL progressing after idelalisib has not been well characterized,” they wrote. “Outcomes in patients who discontinued idelalisib treatment early are poor, with one retrospective analysis reporting a median overall survival (OS) after idelalisib discontinuation of approximately 2 months (range, 0-10 months).”
Venetoclax, an inhibitor of the apoptotic BCL-2 protein, has been shown to have activity against CLL, including in patients with high-risk features such as the chromosome 17p deletion (del17p), prompting the investigators to evaluate it as a follow-on in patients with relapsed/refractory CLL treated with a B-cell receptor pathway inhibitor.
They reported on the idelalisib cohort in a phase 2 trial in which patients with CLL that progressed on either idelalisib or ibrutinib were subsequently treated with venetoclax. The patients in this analysis included those treated with idelalisib in the main study cohort or an expansion cohort.
Patients were started on venetoclax 20 mg daily, followed by weekly dose escalations to a target of 400 mg daily by week 5, or to a maximum of 600 mg for patients who did not have a response by the week 12 assessment.
The overall response rate – the primary efficacy endpoint – was 67%. There were two complete remissions (CR) and one CR with incomplete bone marrow recovery. The remaining 21 patients with responses had partial responses.
At a median of 14 months of follow-up, neither median PFS, duration of response, or OS had been reached.
The investigator-estimated 12-month PFS rate was 79%.
The most common grade 3 or 4 adverse events were neutropenia in 50% of patients, thrombocytopenia in 25%, and anemia in 17%. There were no cases of clinical tumor lysis syndrome, which has been known to occur when venetoclax is initiated at full dose without a ramp-up.
The most common adverse events of any grade included neutropenia, diarrhea, upper respiratory tract infection, thrombocytopenia, nausea, fatigue, cough, rash, and anemia.
“The low number of CRs reported at the time of analysis may be a result of the follow-up time, particularly for patients in the expansion cohort, as other clinical studies with venetoclax report CR occurring after 1 year on therapy. Patients with prior ibrutinib exposure who had progressed on idelalisib as their most recent therapy before study entry had similar efficacy results,” the investigators wrote.
Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
SOURCE: Coutre S et al. Blood. 2018;131(15):1704-11.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 67%, including two complete responses (CRs) and one CR with incomplete bone marrow recovery.
Study details: Cohort of 36 patients with relapsed/refractory CLL previously treated with idelalisib.
Disclosures: Genentech and AbbVie funded the study. Dr. Coutre is an advisory board member for both companies and others, and receives institutional funding from AbbVie and others. Multiple coauthors disclosed financial relationships with AbbVie, Genentech, or both, as well as other companies.
Source: Coutre S et al. Blood. 2018;131(15):1704-11.
Updated CLL guidelines incorporate a decade of advances
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
FROM BLOOD
Experimental voxtalisib shows mixed results in phase 2 study
Voxtalisib, an investigational agent that targets both mTOR and multiple isoforms of PI3K, showed “promising” efficacy with acceptable safety in patients with relapsed or refractory follicular lymphoma (FL), results of a phase 2 trial indicate.
Among 46 patients with FL, the overall response rate was 41.3%, including five (10.9%) complete responses. The median progression-free survival in this group was 58 weeks, reported Jennifer R. Brown, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and her colleagues.
“The observed activity of voxtalisib in relapsed or refractory follicular lymphoma, notable for inducing complete responses in 10.9% of patients, warrants further study,” the investigators wrote in a study published in the Lancet Haematology.
Efficacy of the drug was limited, however, against aggressive malignancies, including mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), or chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
Voxtalisib (XL765) is a potent inhibitor of all four class I PI3Ks, as well as a less robust inhibitor of the mammalian target of rapamycin (mTOR). In contrast, idelalisib (Zydelig) – which is approved by the Food and Drug Administration for treatment of relapsed/refractory FL or for CLL, in combination with rituximab – inhibits only the delta isoform of PI3K, and does not have marked anti–mTOR properties.
The investigators conducted an open-label, nonrandomized trial of voxtalisib in 30 centers in the United States, Belgium, France, Germany, the Netherlands, and Australia.
Adults 18 years or older with relapsed or refractory MCL, FL, DLBCL or CLL/SLL with Eastern Cooperative Oncology Group performance status of 2 or less were enrolled. All patients received voxtalisib 50 mg orally twice daily in 28-day continuous dosing cycles until progression or unacceptable toxicity.
All patients who received more the 4 weeks of treatment and had both a baseline and one or more on-treatment tumor assessments were included in the efficacy analysis. Patients with lymphoma had received a median of three prior lines of therapy, and those with CLL had received a median of four prior lines.
The overall response rate in the entire study population was 18.3% (30 patients), including 22 partial and 8 complete responses. ORR rates were as follows:
- FL: 41.3% (19 of 46 patients).
- MCL: 11.9% (5 of 42 patients).
- DLBCL: 4.9% (2 of 41 patients).
- CLL/SLL: 11.4% (4 of 35 patients).
The safety analysis, which included all 167 patients enrolled, was consistent with that of previous studies of voxtalisib, the investigators said. The most frequently reported adverse events of any grade or type were diarrhea in 35% of patients, fatigue in 32%, nausea in 27%, pyrexia in 26%, cough 24%, and decreased appetite in 21%.
Grade 3 or greater adverse events include anemia in 12%, and pneumonia and thrombocytopenia in 8% each. Slightly more than half of all patients (58.1%) had a serious adverse event.
The investigators noted that voxtalisib’s short plasma half-life may explain the drug’s lack of efficacy against the aggressive lymphomas and CLL/SLL. Longer-acting formulations of the drug or more frequent dosing might address this problem, although the latter solution could be challenging for patients to follow, the investigators acknowledged.
In light of the results, no further studies of voxtalisib in CLL are planned, thought investigation of the drug alone or in combination with chemoimmunotherapy is warranted for patients with follicular lymphoma, the investigators wrote.
The study was funded by Sanofi. Dr. Brown reported consulting for Janssen, Gilead, Celgene, Sun BioPharma, Novartis, AbbVie, Pfizer, AstraZeneca, Astellas, RedX, Pharmacyclics, Genentech/Roche, Verastem, and TG Therapeutics, and grants from Gilead and Sun BioPharma.
SOURCE: Brown J et al. Lancet Haematol. 2018 Mar 14. doi: 10.1016/S2352-3026(18)30030-9.
Voxtalisib, an investigational agent that targets both mTOR and multiple isoforms of PI3K, showed “promising” efficacy with acceptable safety in patients with relapsed or refractory follicular lymphoma (FL), results of a phase 2 trial indicate.
Among 46 patients with FL, the overall response rate was 41.3%, including five (10.9%) complete responses. The median progression-free survival in this group was 58 weeks, reported Jennifer R. Brown, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and her colleagues.
“The observed activity of voxtalisib in relapsed or refractory follicular lymphoma, notable for inducing complete responses in 10.9% of patients, warrants further study,” the investigators wrote in a study published in the Lancet Haematology.
Efficacy of the drug was limited, however, against aggressive malignancies, including mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), or chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
Voxtalisib (XL765) is a potent inhibitor of all four class I PI3Ks, as well as a less robust inhibitor of the mammalian target of rapamycin (mTOR). In contrast, idelalisib (Zydelig) – which is approved by the Food and Drug Administration for treatment of relapsed/refractory FL or for CLL, in combination with rituximab – inhibits only the delta isoform of PI3K, and does not have marked anti–mTOR properties.
The investigators conducted an open-label, nonrandomized trial of voxtalisib in 30 centers in the United States, Belgium, France, Germany, the Netherlands, and Australia.
Adults 18 years or older with relapsed or refractory MCL, FL, DLBCL or CLL/SLL with Eastern Cooperative Oncology Group performance status of 2 or less were enrolled. All patients received voxtalisib 50 mg orally twice daily in 28-day continuous dosing cycles until progression or unacceptable toxicity.
All patients who received more the 4 weeks of treatment and had both a baseline and one or more on-treatment tumor assessments were included in the efficacy analysis. Patients with lymphoma had received a median of three prior lines of therapy, and those with CLL had received a median of four prior lines.
The overall response rate in the entire study population was 18.3% (30 patients), including 22 partial and 8 complete responses. ORR rates were as follows:
- FL: 41.3% (19 of 46 patients).
- MCL: 11.9% (5 of 42 patients).
- DLBCL: 4.9% (2 of 41 patients).
- CLL/SLL: 11.4% (4 of 35 patients).
The safety analysis, which included all 167 patients enrolled, was consistent with that of previous studies of voxtalisib, the investigators said. The most frequently reported adverse events of any grade or type were diarrhea in 35% of patients, fatigue in 32%, nausea in 27%, pyrexia in 26%, cough 24%, and decreased appetite in 21%.
Grade 3 or greater adverse events include anemia in 12%, and pneumonia and thrombocytopenia in 8% each. Slightly more than half of all patients (58.1%) had a serious adverse event.
The investigators noted that voxtalisib’s short plasma half-life may explain the drug’s lack of efficacy against the aggressive lymphomas and CLL/SLL. Longer-acting formulations of the drug or more frequent dosing might address this problem, although the latter solution could be challenging for patients to follow, the investigators acknowledged.
In light of the results, no further studies of voxtalisib in CLL are planned, thought investigation of the drug alone or in combination with chemoimmunotherapy is warranted for patients with follicular lymphoma, the investigators wrote.
The study was funded by Sanofi. Dr. Brown reported consulting for Janssen, Gilead, Celgene, Sun BioPharma, Novartis, AbbVie, Pfizer, AstraZeneca, Astellas, RedX, Pharmacyclics, Genentech/Roche, Verastem, and TG Therapeutics, and grants from Gilead and Sun BioPharma.
SOURCE: Brown J et al. Lancet Haematol. 2018 Mar 14. doi: 10.1016/S2352-3026(18)30030-9.
Voxtalisib, an investigational agent that targets both mTOR and multiple isoforms of PI3K, showed “promising” efficacy with acceptable safety in patients with relapsed or refractory follicular lymphoma (FL), results of a phase 2 trial indicate.
Among 46 patients with FL, the overall response rate was 41.3%, including five (10.9%) complete responses. The median progression-free survival in this group was 58 weeks, reported Jennifer R. Brown, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and her colleagues.
“The observed activity of voxtalisib in relapsed or refractory follicular lymphoma, notable for inducing complete responses in 10.9% of patients, warrants further study,” the investigators wrote in a study published in the Lancet Haematology.
Efficacy of the drug was limited, however, against aggressive malignancies, including mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), or chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
Voxtalisib (XL765) is a potent inhibitor of all four class I PI3Ks, as well as a less robust inhibitor of the mammalian target of rapamycin (mTOR). In contrast, idelalisib (Zydelig) – which is approved by the Food and Drug Administration for treatment of relapsed/refractory FL or for CLL, in combination with rituximab – inhibits only the delta isoform of PI3K, and does not have marked anti–mTOR properties.
The investigators conducted an open-label, nonrandomized trial of voxtalisib in 30 centers in the United States, Belgium, France, Germany, the Netherlands, and Australia.
Adults 18 years or older with relapsed or refractory MCL, FL, DLBCL or CLL/SLL with Eastern Cooperative Oncology Group performance status of 2 or less were enrolled. All patients received voxtalisib 50 mg orally twice daily in 28-day continuous dosing cycles until progression or unacceptable toxicity.
All patients who received more the 4 weeks of treatment and had both a baseline and one or more on-treatment tumor assessments were included in the efficacy analysis. Patients with lymphoma had received a median of three prior lines of therapy, and those with CLL had received a median of four prior lines.
The overall response rate in the entire study population was 18.3% (30 patients), including 22 partial and 8 complete responses. ORR rates were as follows:
- FL: 41.3% (19 of 46 patients).
- MCL: 11.9% (5 of 42 patients).
- DLBCL: 4.9% (2 of 41 patients).
- CLL/SLL: 11.4% (4 of 35 patients).
The safety analysis, which included all 167 patients enrolled, was consistent with that of previous studies of voxtalisib, the investigators said. The most frequently reported adverse events of any grade or type were diarrhea in 35% of patients, fatigue in 32%, nausea in 27%, pyrexia in 26%, cough 24%, and decreased appetite in 21%.
Grade 3 or greater adverse events include anemia in 12%, and pneumonia and thrombocytopenia in 8% each. Slightly more than half of all patients (58.1%) had a serious adverse event.
The investigators noted that voxtalisib’s short plasma half-life may explain the drug’s lack of efficacy against the aggressive lymphomas and CLL/SLL. Longer-acting formulations of the drug or more frequent dosing might address this problem, although the latter solution could be challenging for patients to follow, the investigators acknowledged.
In light of the results, no further studies of voxtalisib in CLL are planned, thought investigation of the drug alone or in combination with chemoimmunotherapy is warranted for patients with follicular lymphoma, the investigators wrote.
The study was funded by Sanofi. Dr. Brown reported consulting for Janssen, Gilead, Celgene, Sun BioPharma, Novartis, AbbVie, Pfizer, AstraZeneca, Astellas, RedX, Pharmacyclics, Genentech/Roche, Verastem, and TG Therapeutics, and grants from Gilead and Sun BioPharma.
SOURCE: Brown J et al. Lancet Haematol. 2018 Mar 14. doi: 10.1016/S2352-3026(18)30030-9.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: The overall response rate in patients with relapsed/refractory FL was 41.3%.
Study details: Open-label, nonrandomized trial in 167 patients from 30 centers in six countries.
Disclosures: The study was funded by Sanofi. Dr. Brown disclosed consulting for Janssen, Gilead, Celgene, Sun BioPharma, Novartis, AbbVie, Pfizer, AstraZeneca, Astellas, RedX, Pharmacyclics, Genentech/Roche, Verastem, and TG Therapeutics, and grants from Gilead and Sun BioPharma.
Source: Brown J et al. Lancet Haematol. 2018 Mar 14. doi: 10.1016/S2352-3026(18)30030-9.
A global snapshot of leukemia incidence
, according to an analysis of World Health Organization cancer databases.
Incidence also is generally higher in males, with a global male to female ratio of 1.4. For men, the highest regional leukemia rate – estimated at 11.3 per 100,000 population for 2012 – was found in Australia and New Zealand, with northern America (the United States and Canada) next at 10.5 per 100,000. Australia/New Zealand and northern America had the highest rate for women at 7.2 per 100,000, followed by western Europe and northern Europe at 6.0 per 100,000, reported Adalberto Miranda-Filho, PhD, of the WHO’s International Agency for Research on Cancer in Lyon, France, and his associates.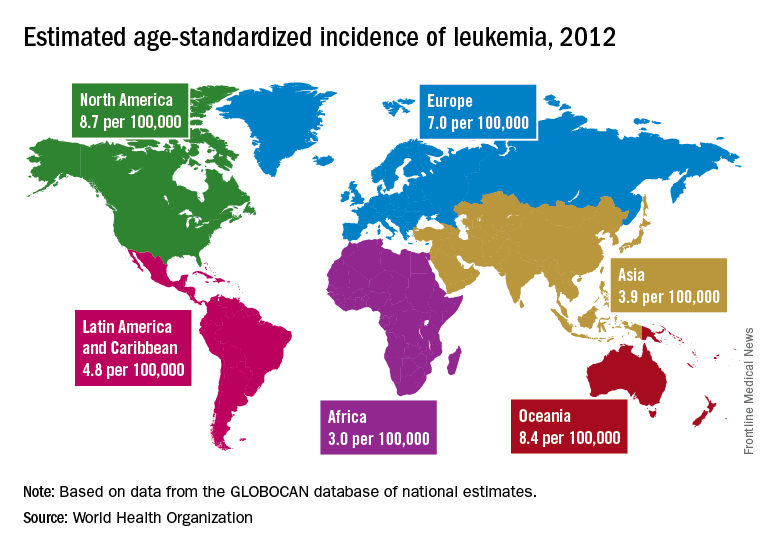
The lowest regional rates for women were found in western Africa (1.2 per 100,000), middle Africa (1.8), and Micronesia/Polynesia (2.1). For men, leukemia incidence was lowest in western Africa (1.4 per 100,000), middle Africa (2.6), and south-central Asia (3.4), according to data from the WHO’s GLOBOCAN database. The report was published in The Lancet Haematology.
Estimates for leukemia subtypes in 2003-2007 – calculated for 54 countries, not regions – also showed a great deal of variation. For acute lymphoblastic leukemia, Ecuador had the highest rates for both males (2.8 per 100,000) and females (3.3), with high rates seen in Costa Rica, Columbia, and Cyprus. Rates in the United States were near the top: 2.1 for males and 1.6 for females. Rates were lowest for men in Jamaica (0.4) and Serbia (0.6) and for women in India (0.5) and Serbia and Cuba (0.6), Dr. Miranda-Filho and his associates said.
Incidence rates for acute myeloid leukemia were highest in Australia for men (2.8 per 100,000) and Austria for women (2.2), with the United States near the top for both men (2.6) and women (1.9). The lowest rates occurred in Cuba and Egypt for men (0.9 per 100,000) and Cuba for women (0.4), data from the WHO’s Cancer Incidence in Five Continents Volume X show.
Chronic lymphocytic leukemia incidence was highest for men in Canada (4.5 per 100,000), Ireland and Lithuania (4.4), and Slovakia (4.3). The incidence was highest for women in Lithuania (2.5), Canada (2.3), and Slovakia and Denmark (2.1). Incidence in the United States was 3.5 for men and 1.8 for women. At the other end of the scale, the lowest rates for both men and women were in Japan and Malaysia (0.1), the investigators’ analysis showed.
Chronic myeloid leukemia rates were the lowest of the subtypes, and Tunisia was the lowest for men at 0.4 per 100,000 and tied for lowest with Serbia, Slovenia, and Puerto Rico for women at 0.3. Incidence was highest for men in Australia at 1.8 per 100,000 and highest for women in Uruguay at 1.1. Rates in the United States were 1.3 for men and 0.8 for women, Dr. Miranda-Filho and his associates said.
“The higher incidence of acute lymphoblastic leukaemia in parts of South America, as well as of chronic lymphocytic leukaemia in populations across North America and Oceania, alongside a lower incidence in Asia, might be important markers for further epidemiological study, and a means to better understand the underlying factors to support future cancer prevention strategies,” the investigators wrote.
SOURCE: Miranda-Filho A et al. Lancet Haematol. 2018;5:e14-24.
, according to an analysis of World Health Organization cancer databases.
Incidence also is generally higher in males, with a global male to female ratio of 1.4. For men, the highest regional leukemia rate – estimated at 11.3 per 100,000 population for 2012 – was found in Australia and New Zealand, with northern America (the United States and Canada) next at 10.5 per 100,000. Australia/New Zealand and northern America had the highest rate for women at 7.2 per 100,000, followed by western Europe and northern Europe at 6.0 per 100,000, reported Adalberto Miranda-Filho, PhD, of the WHO’s International Agency for Research on Cancer in Lyon, France, and his associates.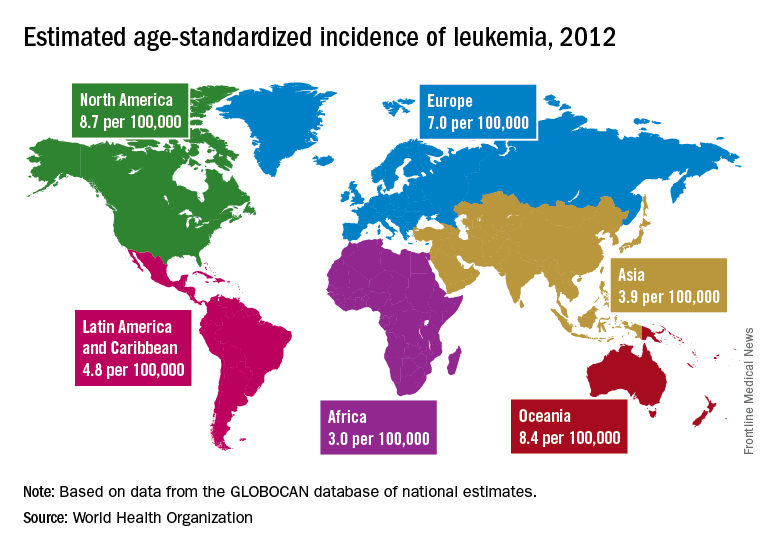
The lowest regional rates for women were found in western Africa (1.2 per 100,000), middle Africa (1.8), and Micronesia/Polynesia (2.1). For men, leukemia incidence was lowest in western Africa (1.4 per 100,000), middle Africa (2.6), and south-central Asia (3.4), according to data from the WHO’s GLOBOCAN database. The report was published in The Lancet Haematology.
Estimates for leukemia subtypes in 2003-2007 – calculated for 54 countries, not regions – also showed a great deal of variation. For acute lymphoblastic leukemia, Ecuador had the highest rates for both males (2.8 per 100,000) and females (3.3), with high rates seen in Costa Rica, Columbia, and Cyprus. Rates in the United States were near the top: 2.1 for males and 1.6 for females. Rates were lowest for men in Jamaica (0.4) and Serbia (0.6) and for women in India (0.5) and Serbia and Cuba (0.6), Dr. Miranda-Filho and his associates said.
Incidence rates for acute myeloid leukemia were highest in Australia for men (2.8 per 100,000) and Austria for women (2.2), with the United States near the top for both men (2.6) and women (1.9). The lowest rates occurred in Cuba and Egypt for men (0.9 per 100,000) and Cuba for women (0.4), data from the WHO’s Cancer Incidence in Five Continents Volume X show.
Chronic lymphocytic leukemia incidence was highest for men in Canada (4.5 per 100,000), Ireland and Lithuania (4.4), and Slovakia (4.3). The incidence was highest for women in Lithuania (2.5), Canada (2.3), and Slovakia and Denmark (2.1). Incidence in the United States was 3.5 for men and 1.8 for women. At the other end of the scale, the lowest rates for both men and women were in Japan and Malaysia (0.1), the investigators’ analysis showed.
Chronic myeloid leukemia rates were the lowest of the subtypes, and Tunisia was the lowest for men at 0.4 per 100,000 and tied for lowest with Serbia, Slovenia, and Puerto Rico for women at 0.3. Incidence was highest for men in Australia at 1.8 per 100,000 and highest for women in Uruguay at 1.1. Rates in the United States were 1.3 for men and 0.8 for women, Dr. Miranda-Filho and his associates said.
“The higher incidence of acute lymphoblastic leukaemia in parts of South America, as well as of chronic lymphocytic leukaemia in populations across North America and Oceania, alongside a lower incidence in Asia, might be important markers for further epidemiological study, and a means to better understand the underlying factors to support future cancer prevention strategies,” the investigators wrote.
SOURCE: Miranda-Filho A et al. Lancet Haematol. 2018;5:e14-24.
, according to an analysis of World Health Organization cancer databases.
Incidence also is generally higher in males, with a global male to female ratio of 1.4. For men, the highest regional leukemia rate – estimated at 11.3 per 100,000 population for 2012 – was found in Australia and New Zealand, with northern America (the United States and Canada) next at 10.5 per 100,000. Australia/New Zealand and northern America had the highest rate for women at 7.2 per 100,000, followed by western Europe and northern Europe at 6.0 per 100,000, reported Adalberto Miranda-Filho, PhD, of the WHO’s International Agency for Research on Cancer in Lyon, France, and his associates.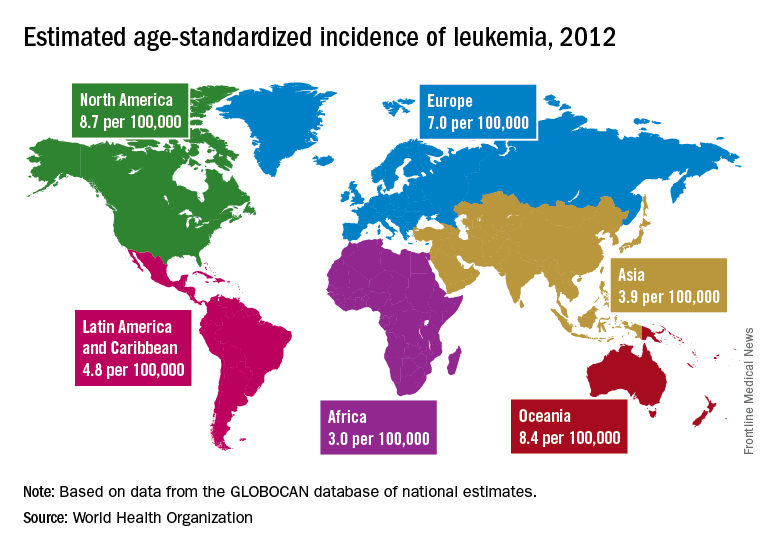
The lowest regional rates for women were found in western Africa (1.2 per 100,000), middle Africa (1.8), and Micronesia/Polynesia (2.1). For men, leukemia incidence was lowest in western Africa (1.4 per 100,000), middle Africa (2.6), and south-central Asia (3.4), according to data from the WHO’s GLOBOCAN database. The report was published in The Lancet Haematology.
Estimates for leukemia subtypes in 2003-2007 – calculated for 54 countries, not regions – also showed a great deal of variation. For acute lymphoblastic leukemia, Ecuador had the highest rates for both males (2.8 per 100,000) and females (3.3), with high rates seen in Costa Rica, Columbia, and Cyprus. Rates in the United States were near the top: 2.1 for males and 1.6 for females. Rates were lowest for men in Jamaica (0.4) and Serbia (0.6) and for women in India (0.5) and Serbia and Cuba (0.6), Dr. Miranda-Filho and his associates said.
Incidence rates for acute myeloid leukemia were highest in Australia for men (2.8 per 100,000) and Austria for women (2.2), with the United States near the top for both men (2.6) and women (1.9). The lowest rates occurred in Cuba and Egypt for men (0.9 per 100,000) and Cuba for women (0.4), data from the WHO’s Cancer Incidence in Five Continents Volume X show.
Chronic lymphocytic leukemia incidence was highest for men in Canada (4.5 per 100,000), Ireland and Lithuania (4.4), and Slovakia (4.3). The incidence was highest for women in Lithuania (2.5), Canada (2.3), and Slovakia and Denmark (2.1). Incidence in the United States was 3.5 for men and 1.8 for women. At the other end of the scale, the lowest rates for both men and women were in Japan and Malaysia (0.1), the investigators’ analysis showed.
Chronic myeloid leukemia rates were the lowest of the subtypes, and Tunisia was the lowest for men at 0.4 per 100,000 and tied for lowest with Serbia, Slovenia, and Puerto Rico for women at 0.3. Incidence was highest for men in Australia at 1.8 per 100,000 and highest for women in Uruguay at 1.1. Rates in the United States were 1.3 for men and 0.8 for women, Dr. Miranda-Filho and his associates said.
“The higher incidence of acute lymphoblastic leukaemia in parts of South America, as well as of chronic lymphocytic leukaemia in populations across North America and Oceania, alongside a lower incidence in Asia, might be important markers for further epidemiological study, and a means to better understand the underlying factors to support future cancer prevention strategies,” the investigators wrote.
SOURCE: Miranda-Filho A et al. Lancet Haematol. 2018;5:e14-24.
FROM THE LANCET HAEMATOLOGY