User login
Imetelstat in MF: More research needed
The telomerase inhibitor imetelstat has exhibited unique activity in a pilot study of patients with intermediate- or high-risk myelofibrosis (MF), but more research is needed, according to investigators.
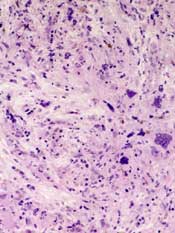
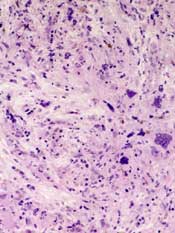
Imetelstat produced complete and partial responses in a minority of patients and reversed bone marrow fibrosis in complete responders.
However, imetelstat also prompted severe myelosuppression and liver-test abnormalities. And most patients ultimately discontinued treatment.
The investigators therefore concluded that additional research is needed to establish the most effective dosing of the drug, clarify its mechanism of action, and address concerns about toxicity.
Ayalew Tefferi, MD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues reported the results of this trial in NEJM.
A phase 2 trial of imetelstat in patients with essential thrombocythemia was published in NEJM simultaneously. Both trials were sponsored by Geron Corporation, the company developing imetelstat.
The MF study included 33 patients, 18 with primary MF, 10 with post-polycythemia vera MF, and 5 with post-essential thrombocythemia MF. About 52% had high-risk disease, and the rest had intermediate-2-risk MF.
The patients had a median age of 67. About 79% of patients had received prior therapy, and 48% had received a JAK inhibitor. Thirty-nine percent of patients were dependent on red cell transfusions, 64% had constitutional symptoms, 70% had palpable splenomegaly, and 55% had an abnormal karyotype, including 18% with an unfavorable karyotype.
Imetelstat was administered as a 2-hour intravenous infusion, at a starting dose of 9.4 mg per kilogram of body weight. There were 2 dosing schedules: (1) once every 3 weeks or (2) weekly for 4 weeks, followed by once every 3 weeks.
Responses
“We observed that imetelstat was active and induced morphologic and molecular remissions in some patients with myelofibrosis,” Dr Tefferi said. “We also observed that imetelstat demonstrated selective anticlonal activity, inhibiting the growth of cancer cells, which we had not previously documented with other drugs.”
Overall, 21% of patients (7/33) experienced a complete response (n=4) or partial response (n=3) to treatment. The median duration of complete response was 18 months (range, 13-20+), and the median duration of partial response was 10 months (range, 7-10+).
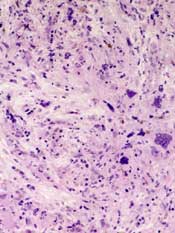
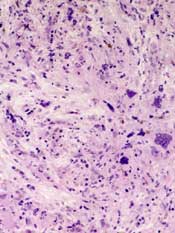
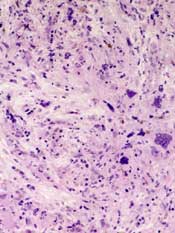
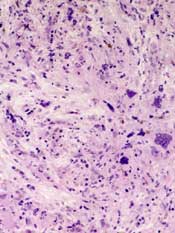
“Some patients treated with imetelstat have reverted back to normal bone marrow,” Dr Tefferi noted. “Typically, myelofibrosis is characterized by marrow scarring, and, although patients may derive symptomatic relief from other treatments, such as ruxolitinib, they usually do not revert back to normal bone marrow.”
Bone marrow fibrosis was reversed in all 4 patients with a complete response. A molecular response was documented in 3 of these patients.
Mutations and telomere length
“We noted a difference in response rates, especially in complete remission rates, in patients with and without certain specific gene mutations, such as ASXL1, SF3B1, and U2AF1,” Dr Tefferi noted. “This underscores the need for laboratory correlative studies in future clinical trials.”
Responses occurred in 27% of patients with a JAK2 mutation and 0% of patients without a JAK2 mutation (P=0.30). Alternatively, responses occurred in 32% of patients without an ASXL1 mutation and 0% of patients with an ASXL1 mutation (P=0.07).
The rate of complete response was 38% among patients with a mutation in SF3B1 or U2AF1, compared to 4% among patients without either mutation (P=0.04).
The investigators also found that responses were not correlated with baseline telomere length.
Toxicity
Dr Tefferi and his colleagues said the most clinically significant side effect of imetelstat was myelosuppression. It was the primary reason for a protocol-mandated dose reduction that occurred in 22 patients (67%).
Another “notable” side effect was the elevation of liver-enzyme levels. The investigators observed treatment-emergent (though not necessarily related) increases from baseline in total bilirubin (49%), alkaline phosphatase (58%), aspartate aminotransferase (58%), and alanine aminotransferase (27%).
None of these abnormalities were linked to clinically overt liver damage, and most patients ultimately saw their values return to baseline levels.
Adverse events that were considered at least possibly related to treatment and occurred in 3 or more patients included thrombocytopenia (45% grade 3/4), anemia (39% overall, 30% grade 3), neutropenia (27% grade 3/4), aspartate aminotransferase elevation (27% grade 1), alkaline phosphatase elevation (21% grade 1/2), elevation in total bilirubin (12% grade 1/2), infusion-related reactions (12% grade 1/2), diarrhea (9% grade 1/2), and epistaxis (9% grade 1/2).
Treatment discontinuation
At the data-cutoff date (December 5, 2014), 76% of patients had discontinued imetelstat (n=25). For all patients, the median duration of treatment was 8.6 months (range, 1.4 to 21.7).
Patients stopped treatment due to insufficient response (n=16), disease progression or relapse after response (n=3), death during the treatment period (n=2), adverse events (n=2), financial constraints (n=1), and pre-existing atrial fibrillation (n=1).
Both patients who discontinued imetelstat due to adverse events had persistent thrombocytopenia. Of the 2 deaths, 1 was considered treatment-related. That patient died of intracranial hemorrhage that was attributed to drug-induced, grade 4 thrombocytopenia after weekly dosing. The non-treatment-related death was the result of an upper gastrointestinal hemorrhage. ![]()
The telomerase inhibitor imetelstat has exhibited unique activity in a pilot study of patients with intermediate- or high-risk myelofibrosis (MF), but more research is needed, according to investigators.
Imetelstat produced complete and partial responses in a minority of patients and reversed bone marrow fibrosis in complete responders.
However, imetelstat also prompted severe myelosuppression and liver-test abnormalities. And most patients ultimately discontinued treatment.
The investigators therefore concluded that additional research is needed to establish the most effective dosing of the drug, clarify its mechanism of action, and address concerns about toxicity.
Ayalew Tefferi, MD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues reported the results of this trial in NEJM.
A phase 2 trial of imetelstat in patients with essential thrombocythemia was published in NEJM simultaneously. Both trials were sponsored by Geron Corporation, the company developing imetelstat.
The MF study included 33 patients, 18 with primary MF, 10 with post-polycythemia vera MF, and 5 with post-essential thrombocythemia MF. About 52% had high-risk disease, and the rest had intermediate-2-risk MF.
The patients had a median age of 67. About 79% of patients had received prior therapy, and 48% had received a JAK inhibitor. Thirty-nine percent of patients were dependent on red cell transfusions, 64% had constitutional symptoms, 70% had palpable splenomegaly, and 55% had an abnormal karyotype, including 18% with an unfavorable karyotype.
Imetelstat was administered as a 2-hour intravenous infusion, at a starting dose of 9.4 mg per kilogram of body weight. There were 2 dosing schedules: (1) once every 3 weeks or (2) weekly for 4 weeks, followed by once every 3 weeks.
Responses
“We observed that imetelstat was active and induced morphologic and molecular remissions in some patients with myelofibrosis,” Dr Tefferi said. “We also observed that imetelstat demonstrated selective anticlonal activity, inhibiting the growth of cancer cells, which we had not previously documented with other drugs.”
Overall, 21% of patients (7/33) experienced a complete response (n=4) or partial response (n=3) to treatment. The median duration of complete response was 18 months (range, 13-20+), and the median duration of partial response was 10 months (range, 7-10+).
“Some patients treated with imetelstat have reverted back to normal bone marrow,” Dr Tefferi noted. “Typically, myelofibrosis is characterized by marrow scarring, and, although patients may derive symptomatic relief from other treatments, such as ruxolitinib, they usually do not revert back to normal bone marrow.”
Bone marrow fibrosis was reversed in all 4 patients with a complete response. A molecular response was documented in 3 of these patients.
Mutations and telomere length
“We noted a difference in response rates, especially in complete remission rates, in patients with and without certain specific gene mutations, such as ASXL1, SF3B1, and U2AF1,” Dr Tefferi noted. “This underscores the need for laboratory correlative studies in future clinical trials.”
Responses occurred in 27% of patients with a JAK2 mutation and 0% of patients without a JAK2 mutation (P=0.30). Alternatively, responses occurred in 32% of patients without an ASXL1 mutation and 0% of patients with an ASXL1 mutation (P=0.07).
The rate of complete response was 38% among patients with a mutation in SF3B1 or U2AF1, compared to 4% among patients without either mutation (P=0.04).
The investigators also found that responses were not correlated with baseline telomere length.
Toxicity
Dr Tefferi and his colleagues said the most clinically significant side effect of imetelstat was myelosuppression. It was the primary reason for a protocol-mandated dose reduction that occurred in 22 patients (67%).
Another “notable” side effect was the elevation of liver-enzyme levels. The investigators observed treatment-emergent (though not necessarily related) increases from baseline in total bilirubin (49%), alkaline phosphatase (58%), aspartate aminotransferase (58%), and alanine aminotransferase (27%).
None of these abnormalities were linked to clinically overt liver damage, and most patients ultimately saw their values return to baseline levels.
Adverse events that were considered at least possibly related to treatment and occurred in 3 or more patients included thrombocytopenia (45% grade 3/4), anemia (39% overall, 30% grade 3), neutropenia (27% grade 3/4), aspartate aminotransferase elevation (27% grade 1), alkaline phosphatase elevation (21% grade 1/2), elevation in total bilirubin (12% grade 1/2), infusion-related reactions (12% grade 1/2), diarrhea (9% grade 1/2), and epistaxis (9% grade 1/2).
Treatment discontinuation
At the data-cutoff date (December 5, 2014), 76% of patients had discontinued imetelstat (n=25). For all patients, the median duration of treatment was 8.6 months (range, 1.4 to 21.7).
Patients stopped treatment due to insufficient response (n=16), disease progression or relapse after response (n=3), death during the treatment period (n=2), adverse events (n=2), financial constraints (n=1), and pre-existing atrial fibrillation (n=1).
Both patients who discontinued imetelstat due to adverse events had persistent thrombocytopenia. Of the 2 deaths, 1 was considered treatment-related. That patient died of intracranial hemorrhage that was attributed to drug-induced, grade 4 thrombocytopenia after weekly dosing. The non-treatment-related death was the result of an upper gastrointestinal hemorrhage. ![]()
The telomerase inhibitor imetelstat has exhibited unique activity in a pilot study of patients with intermediate- or high-risk myelofibrosis (MF), but more research is needed, according to investigators.
Imetelstat produced complete and partial responses in a minority of patients and reversed bone marrow fibrosis in complete responders.
However, imetelstat also prompted severe myelosuppression and liver-test abnormalities. And most patients ultimately discontinued treatment.
The investigators therefore concluded that additional research is needed to establish the most effective dosing of the drug, clarify its mechanism of action, and address concerns about toxicity.
Ayalew Tefferi, MD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues reported the results of this trial in NEJM.
A phase 2 trial of imetelstat in patients with essential thrombocythemia was published in NEJM simultaneously. Both trials were sponsored by Geron Corporation, the company developing imetelstat.
The MF study included 33 patients, 18 with primary MF, 10 with post-polycythemia vera MF, and 5 with post-essential thrombocythemia MF. About 52% had high-risk disease, and the rest had intermediate-2-risk MF.
The patients had a median age of 67. About 79% of patients had received prior therapy, and 48% had received a JAK inhibitor. Thirty-nine percent of patients were dependent on red cell transfusions, 64% had constitutional symptoms, 70% had palpable splenomegaly, and 55% had an abnormal karyotype, including 18% with an unfavorable karyotype.
Imetelstat was administered as a 2-hour intravenous infusion, at a starting dose of 9.4 mg per kilogram of body weight. There were 2 dosing schedules: (1) once every 3 weeks or (2) weekly for 4 weeks, followed by once every 3 weeks.
Responses
“We observed that imetelstat was active and induced morphologic and molecular remissions in some patients with myelofibrosis,” Dr Tefferi said. “We also observed that imetelstat demonstrated selective anticlonal activity, inhibiting the growth of cancer cells, which we had not previously documented with other drugs.”
Overall, 21% of patients (7/33) experienced a complete response (n=4) or partial response (n=3) to treatment. The median duration of complete response was 18 months (range, 13-20+), and the median duration of partial response was 10 months (range, 7-10+).
“Some patients treated with imetelstat have reverted back to normal bone marrow,” Dr Tefferi noted. “Typically, myelofibrosis is characterized by marrow scarring, and, although patients may derive symptomatic relief from other treatments, such as ruxolitinib, they usually do not revert back to normal bone marrow.”
Bone marrow fibrosis was reversed in all 4 patients with a complete response. A molecular response was documented in 3 of these patients.
Mutations and telomere length
“We noted a difference in response rates, especially in complete remission rates, in patients with and without certain specific gene mutations, such as ASXL1, SF3B1, and U2AF1,” Dr Tefferi noted. “This underscores the need for laboratory correlative studies in future clinical trials.”
Responses occurred in 27% of patients with a JAK2 mutation and 0% of patients without a JAK2 mutation (P=0.30). Alternatively, responses occurred in 32% of patients without an ASXL1 mutation and 0% of patients with an ASXL1 mutation (P=0.07).
The rate of complete response was 38% among patients with a mutation in SF3B1 or U2AF1, compared to 4% among patients without either mutation (P=0.04).
The investigators also found that responses were not correlated with baseline telomere length.
Toxicity
Dr Tefferi and his colleagues said the most clinically significant side effect of imetelstat was myelosuppression. It was the primary reason for a protocol-mandated dose reduction that occurred in 22 patients (67%).
Another “notable” side effect was the elevation of liver-enzyme levels. The investigators observed treatment-emergent (though not necessarily related) increases from baseline in total bilirubin (49%), alkaline phosphatase (58%), aspartate aminotransferase (58%), and alanine aminotransferase (27%).
None of these abnormalities were linked to clinically overt liver damage, and most patients ultimately saw their values return to baseline levels.
Adverse events that were considered at least possibly related to treatment and occurred in 3 or more patients included thrombocytopenia (45% grade 3/4), anemia (39% overall, 30% grade 3), neutropenia (27% grade 3/4), aspartate aminotransferase elevation (27% grade 1), alkaline phosphatase elevation (21% grade 1/2), elevation in total bilirubin (12% grade 1/2), infusion-related reactions (12% grade 1/2), diarrhea (9% grade 1/2), and epistaxis (9% grade 1/2).
Treatment discontinuation
At the data-cutoff date (December 5, 2014), 76% of patients had discontinued imetelstat (n=25). For all patients, the median duration of treatment was 8.6 months (range, 1.4 to 21.7).
Patients stopped treatment due to insufficient response (n=16), disease progression or relapse after response (n=3), death during the treatment period (n=2), adverse events (n=2), financial constraints (n=1), and pre-existing atrial fibrillation (n=1).
Both patients who discontinued imetelstat due to adverse events had persistent thrombocytopenia. Of the 2 deaths, 1 was considered treatment-related. That patient died of intracranial hemorrhage that was attributed to drug-induced, grade 4 thrombocytopenia after weekly dosing. The non-treatment-related death was the result of an upper gastrointestinal hemorrhage. ![]()
Drugs don’t play well together in MF

Photo courtesy of the CDC
Simultaneous administration of lenalidomide and ruxolitinib is not feasible in patients with myelofibrosis (MF), according to research published in haematologica.
Investigators said administering the drugs together proved difficult. Most patients had to stop taking lenalidomide at some point, and many did not restart the drug.
In addition, the study did not meet the predetermined efficacy criteria and was therefore terminated early.
Still, the investigators noted that 17 of 31 patients did respond to treatment, and 10 patients were still taking both drugs at the time of analysis.
The team therefore believes a sequential rather than concomitant treatment approach might work with this combination or for other agents to be combined with ruxolitinib.
Srdan Verstovsek, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, and his colleagues conducted this research. It was supported by Incyte Corporation (the company developing ruxolitinib) and MD Anderson.
The investigators initiated this study to determine if lenalidomide and ruxolitinib in combination would target distinct clinical and pathological manifestations of MF and prevent treatment-related decreases in blood counts.
They studied the combination in 31 patients with primary MF (n=15), post-polycythemia vera MF (n=12), or post-essential thrombocythemia MF (n=4). The patients’ median age was 66 (range, 37-82), and 21 had received prior treatments (range, 1-3).
The patients received ruxolitinib at 15 mg twice daily in continuous, 28-day cycles, plus 5 mg of lenalidomide once daily on days 1-21. The median follow-up was 28 months (range, 12-35+).
Dosing troubles
In all, 23 patients required dose interruptions of lenalidomide, with or without a dose decrease due to toxicity. Twenty of these interruptions occurred within the first 3 months of therapy, and 14 of the patients never restarted treatment with lenalidomide.
The reasons for dose interruption (or, ultimately, discontinuation) were low platelet count (n=8), low absolute neutrophil count (n=3), anemia (n=3), diarrhea (n=3), financial constraints (n=2), deep vein thrombosis (n=1), skin rash (n=1), transaminitis (n=1), and arthralgia/fever (n=1).
Conversely, 6 patients required an increased dose of ruxolitinib, 3 within the first 3 months. Doses were increased due to leukocytosis (n=2), suboptimal response (n=2), thrombocytosis (n=1), and progressive splenomegaly (n=1).
Discontinuation and early termination
At a median follow-up of 28 months, 25 patients (81%) were still alive, and 16 remained on study. Ten of these patients were taking both drugs, and 6 were taking ruxolitinib only.
For the 15 patients who came off the study, their reasons included concurrent disease (n=3), disease progression (n=2), myelosuppression (n=2), refractory disease (n=3), toxicities (n=2), persistent and severe lower-extremity cellulitis (n=1), non-compliance (n=1), and financial reasons (n=1).
The investigators noted that only 7 patients met the predetermined definition of efficacy—a response to combination treatment within 6 months of initiation without discontinuing either drug.
For the study to continue after the interim analysis, more than 10 patients would have to fulfill those criteria. As they did not, the study was terminated early.
Response
Seventeen patients (55%) achieved an IWG-MRT-defined response of clinical improvement in palpable spleen size. Seven patients had a 100% spleen reduction, and 10 had reduction of 50% or greater.
The median time to clinical improvement in spleen size was 1.8 months (range, 0.4-31), and the median duration of this response was 19 months (range, 3-32+). At last follow-up, 2 patients had lost their response.
One of the 17 spleen responders also achieved an IWG-MRT-defined clinical improvement in hemoglobin (increase of 2 g/dL or greater that was maintained for more than 8 weeks). The time to this response was 28 months, and the response lasted 6 months.
There were differences in response rate, response duration, time to response, and overall survival between patients who required dose interruptions and those who did not. However, none of these differences were statistically significant.
Toxicity
Grade 3/4 myelosuppression occurred in 16 patients, and there was 1 case of lower-extremity thrombosis. The most common non-hematologic adverse events (AEs) were diarrhea (n=8), nausea and vomiting (n=3), abdominal pain (n=3), and constipation (n=3).
Five patients had grade 3/4 non-hematologic AEs—diarrhea, edema, transaminitis, bilirubinemia, and acute kidney injury. Two patients discontinued treatment due to drug-related AEs—grade 2 persistent nausea and grade 3 diarrhea.
Three of the 6 deaths were documented (including 2 that occurred on-study). They were attributed to pneumonia, kidney failure, and possible stroke. ![]()

Photo courtesy of the CDC
Simultaneous administration of lenalidomide and ruxolitinib is not feasible in patients with myelofibrosis (MF), according to research published in haematologica.
Investigators said administering the drugs together proved difficult. Most patients had to stop taking lenalidomide at some point, and many did not restart the drug.
In addition, the study did not meet the predetermined efficacy criteria and was therefore terminated early.
Still, the investigators noted that 17 of 31 patients did respond to treatment, and 10 patients were still taking both drugs at the time of analysis.
The team therefore believes a sequential rather than concomitant treatment approach might work with this combination or for other agents to be combined with ruxolitinib.
Srdan Verstovsek, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, and his colleagues conducted this research. It was supported by Incyte Corporation (the company developing ruxolitinib) and MD Anderson.
The investigators initiated this study to determine if lenalidomide and ruxolitinib in combination would target distinct clinical and pathological manifestations of MF and prevent treatment-related decreases in blood counts.
They studied the combination in 31 patients with primary MF (n=15), post-polycythemia vera MF (n=12), or post-essential thrombocythemia MF (n=4). The patients’ median age was 66 (range, 37-82), and 21 had received prior treatments (range, 1-3).
The patients received ruxolitinib at 15 mg twice daily in continuous, 28-day cycles, plus 5 mg of lenalidomide once daily on days 1-21. The median follow-up was 28 months (range, 12-35+).
Dosing troubles
In all, 23 patients required dose interruptions of lenalidomide, with or without a dose decrease due to toxicity. Twenty of these interruptions occurred within the first 3 months of therapy, and 14 of the patients never restarted treatment with lenalidomide.
The reasons for dose interruption (or, ultimately, discontinuation) were low platelet count (n=8), low absolute neutrophil count (n=3), anemia (n=3), diarrhea (n=3), financial constraints (n=2), deep vein thrombosis (n=1), skin rash (n=1), transaminitis (n=1), and arthralgia/fever (n=1).
Conversely, 6 patients required an increased dose of ruxolitinib, 3 within the first 3 months. Doses were increased due to leukocytosis (n=2), suboptimal response (n=2), thrombocytosis (n=1), and progressive splenomegaly (n=1).
Discontinuation and early termination
At a median follow-up of 28 months, 25 patients (81%) were still alive, and 16 remained on study. Ten of these patients were taking both drugs, and 6 were taking ruxolitinib only.
For the 15 patients who came off the study, their reasons included concurrent disease (n=3), disease progression (n=2), myelosuppression (n=2), refractory disease (n=3), toxicities (n=2), persistent and severe lower-extremity cellulitis (n=1), non-compliance (n=1), and financial reasons (n=1).
The investigators noted that only 7 patients met the predetermined definition of efficacy—a response to combination treatment within 6 months of initiation without discontinuing either drug.
For the study to continue after the interim analysis, more than 10 patients would have to fulfill those criteria. As they did not, the study was terminated early.
Response
Seventeen patients (55%) achieved an IWG-MRT-defined response of clinical improvement in palpable spleen size. Seven patients had a 100% spleen reduction, and 10 had reduction of 50% or greater.
The median time to clinical improvement in spleen size was 1.8 months (range, 0.4-31), and the median duration of this response was 19 months (range, 3-32+). At last follow-up, 2 patients had lost their response.
One of the 17 spleen responders also achieved an IWG-MRT-defined clinical improvement in hemoglobin (increase of 2 g/dL or greater that was maintained for more than 8 weeks). The time to this response was 28 months, and the response lasted 6 months.
There were differences in response rate, response duration, time to response, and overall survival between patients who required dose interruptions and those who did not. However, none of these differences were statistically significant.
Toxicity
Grade 3/4 myelosuppression occurred in 16 patients, and there was 1 case of lower-extremity thrombosis. The most common non-hematologic adverse events (AEs) were diarrhea (n=8), nausea and vomiting (n=3), abdominal pain (n=3), and constipation (n=3).
Five patients had grade 3/4 non-hematologic AEs—diarrhea, edema, transaminitis, bilirubinemia, and acute kidney injury. Two patients discontinued treatment due to drug-related AEs—grade 2 persistent nausea and grade 3 diarrhea.
Three of the 6 deaths were documented (including 2 that occurred on-study). They were attributed to pneumonia, kidney failure, and possible stroke. ![]()

Photo courtesy of the CDC
Simultaneous administration of lenalidomide and ruxolitinib is not feasible in patients with myelofibrosis (MF), according to research published in haematologica.
Investigators said administering the drugs together proved difficult. Most patients had to stop taking lenalidomide at some point, and many did not restart the drug.
In addition, the study did not meet the predetermined efficacy criteria and was therefore terminated early.
Still, the investigators noted that 17 of 31 patients did respond to treatment, and 10 patients were still taking both drugs at the time of analysis.
The team therefore believes a sequential rather than concomitant treatment approach might work with this combination or for other agents to be combined with ruxolitinib.
Srdan Verstovsek, MD, PhD, of the MD Anderson Cancer Center in Houston, Texas, and his colleagues conducted this research. It was supported by Incyte Corporation (the company developing ruxolitinib) and MD Anderson.
The investigators initiated this study to determine if lenalidomide and ruxolitinib in combination would target distinct clinical and pathological manifestations of MF and prevent treatment-related decreases in blood counts.
They studied the combination in 31 patients with primary MF (n=15), post-polycythemia vera MF (n=12), or post-essential thrombocythemia MF (n=4). The patients’ median age was 66 (range, 37-82), and 21 had received prior treatments (range, 1-3).
The patients received ruxolitinib at 15 mg twice daily in continuous, 28-day cycles, plus 5 mg of lenalidomide once daily on days 1-21. The median follow-up was 28 months (range, 12-35+).
Dosing troubles
In all, 23 patients required dose interruptions of lenalidomide, with or without a dose decrease due to toxicity. Twenty of these interruptions occurred within the first 3 months of therapy, and 14 of the patients never restarted treatment with lenalidomide.
The reasons for dose interruption (or, ultimately, discontinuation) were low platelet count (n=8), low absolute neutrophil count (n=3), anemia (n=3), diarrhea (n=3), financial constraints (n=2), deep vein thrombosis (n=1), skin rash (n=1), transaminitis (n=1), and arthralgia/fever (n=1).
Conversely, 6 patients required an increased dose of ruxolitinib, 3 within the first 3 months. Doses were increased due to leukocytosis (n=2), suboptimal response (n=2), thrombocytosis (n=1), and progressive splenomegaly (n=1).
Discontinuation and early termination
At a median follow-up of 28 months, 25 patients (81%) were still alive, and 16 remained on study. Ten of these patients were taking both drugs, and 6 were taking ruxolitinib only.
For the 15 patients who came off the study, their reasons included concurrent disease (n=3), disease progression (n=2), myelosuppression (n=2), refractory disease (n=3), toxicities (n=2), persistent and severe lower-extremity cellulitis (n=1), non-compliance (n=1), and financial reasons (n=1).
The investigators noted that only 7 patients met the predetermined definition of efficacy—a response to combination treatment within 6 months of initiation without discontinuing either drug.
For the study to continue after the interim analysis, more than 10 patients would have to fulfill those criteria. As they did not, the study was terminated early.
Response
Seventeen patients (55%) achieved an IWG-MRT-defined response of clinical improvement in palpable spleen size. Seven patients had a 100% spleen reduction, and 10 had reduction of 50% or greater.
The median time to clinical improvement in spleen size was 1.8 months (range, 0.4-31), and the median duration of this response was 19 months (range, 3-32+). At last follow-up, 2 patients had lost their response.
One of the 17 spleen responders also achieved an IWG-MRT-defined clinical improvement in hemoglobin (increase of 2 g/dL or greater that was maintained for more than 8 weeks). The time to this response was 28 months, and the response lasted 6 months.
There were differences in response rate, response duration, time to response, and overall survival between patients who required dose interruptions and those who did not. However, none of these differences were statistically significant.
Toxicity
Grade 3/4 myelosuppression occurred in 16 patients, and there was 1 case of lower-extremity thrombosis. The most common non-hematologic adverse events (AEs) were diarrhea (n=8), nausea and vomiting (n=3), abdominal pain (n=3), and constipation (n=3).
Five patients had grade 3/4 non-hematologic AEs—diarrhea, edema, transaminitis, bilirubinemia, and acute kidney injury. Two patients discontinued treatment due to drug-related AEs—grade 2 persistent nausea and grade 3 diarrhea.
Three of the 6 deaths were documented (including 2 that occurred on-study). They were attributed to pneumonia, kidney failure, and possible stroke. ![]()
Team reports phase 3 results with abandoned MPN drug
Researchers have reported results of the phase 3 JAKARTA trial, in which they evaluated the selective JAK2 inhibitor fedratinib in patients with myelofibrosis (MF).
Fedratinib was being developed as a treatment for myeloproliferative neoplasms (MPNs), but Sanofi Oncology stopped clinical development of the drug in 2013, after it was linked to a neurological condition known as Wernicke encephalopathy.
There were 4 confirmed cases of Wernicke encephalopathy in the JAKARTA trial, in addition to other adverse events (AEs). However, fedratinib also lessened the severity of MF symptoms in about 35% to 40% of patients.
These results have been published in JAMA Oncology alongside an invited commentary. The study was sponsored by Sanofi.
Treatment and response
The study enrolled 289 adult patients with intermediate-2 or high-risk primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF. Patients were randomized to receive fedratinib at 400 mg once a day, fedratinib at 500 mg once a day, or placebo for at least 6 consecutive, 4-week cycles.
The study’s primary endpoint was spleen response, or a 35% or greater reduction in spleen volume from baseline (determined by MRI or CT) at week 24 and confirmed 4 weeks later.
Thirty-six percent (35/96) of patients in the 400 mg arm and 40% (39/97) in the 500 mg arm achieved the primary endpoint, compared to 1% (1/96) of patients in the placebo arm (P<0.001).
The main secondary endpoint was symptom response, or a 50% or greater reduction in total symptom score (assessed using the modified Myelofibrosis Symptom Assessment Form).
At week 24, symptom response rates were 36% (33/91) in the 400 mg arm, 34% (31/91) in the 500 mg arm, and 7% (6/85) in the placebo arm (P<0.001).
Safety data
Treatment-emergent AEs occurred in 100% of patients in the 400 mg arm, 98% in the 500 mg arm, and 94% in the placebo arm. Serious AEs occurred in 27%, 31%, and 23%, respectively. AEs leading to discontinuation occurred in 14%, 25%, and 8%, respectively.
Infections occurred in 42% of patients in the 400 mg arm, 39% of patients in the 500 mg arm, and 27% of patients of patients in the placebo arm.
Nonhematologic AEs occurring in at least 10% of patients in any group were diarrhea (66%, 56%, and 16%, respectively), vomiting (42%, 55%, and 5%, respectively), nausea (64%, 51%, and 15%, respectively), constipation (10%, 18%, and 7%, respectively), asthenia (9%, 16%, and 6%, respectively), abdominal pain (15%, 12%, and 16%, respectively), fatigue (16%, 10%, and 10%, respectively), dyspnea (8%, 10%, and 6%, respectively), and weight loss (4%, 10%, and 5%, respectively).
Hematologic AEs occurring in at least 10% of patients in any group were anemia (99%, 98%, and 91%, respectively), thrombocytopenia (63%, 57%, and 51%, respectively), lymphopenia (57%, 66%, and 54%, respectively), leukopenia (47%, 53%, and 19%, respectively), and neutropenia (28%, 44%, and 15%, respectively).
One patient in each fedratinib arm and 2 in the placebo arm transformed to acute myeloid leukemia.
There were 24 deaths during the first 24 weeks of the study—4 in the 400 mg arm, 10 in the 500 mg arm, and 10 in the placebo arm. Nine of the deaths were attributed to AEs—1, 4, and 4, respectively.
Wernicke encephalopathy
There were 4 cases of Wernicke encephalopathy, all in women who received fedratinib at 500 mg. All of these cases were confirmed by an independent expert safety panel, 3 on the basis of clinical features and MRI results, and 1 on the basis of clinical symptoms alone.
The patients developed symptoms 6 weeks to 44 weeks after beginning fedratinib treatment, and all discontinued treatment permanently.
Cognitive symptoms manifested in the context of persistent vomiting, malnutrition, and cachexia in 1 patient, vomiting and hyponatremia in 1 patient, and renal failure with mild hyponatremia in 1 patient.
All of the patients received intravenous thiamine and showed responses to the treatment, but all had persistent cognitive defects at last follow-up. ![]()
Researchers have reported results of the phase 3 JAKARTA trial, in which they evaluated the selective JAK2 inhibitor fedratinib in patients with myelofibrosis (MF).
Fedratinib was being developed as a treatment for myeloproliferative neoplasms (MPNs), but Sanofi Oncology stopped clinical development of the drug in 2013, after it was linked to a neurological condition known as Wernicke encephalopathy.
There were 4 confirmed cases of Wernicke encephalopathy in the JAKARTA trial, in addition to other adverse events (AEs). However, fedratinib also lessened the severity of MF symptoms in about 35% to 40% of patients.
These results have been published in JAMA Oncology alongside an invited commentary. The study was sponsored by Sanofi.
Treatment and response
The study enrolled 289 adult patients with intermediate-2 or high-risk primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF. Patients were randomized to receive fedratinib at 400 mg once a day, fedratinib at 500 mg once a day, or placebo for at least 6 consecutive, 4-week cycles.
The study’s primary endpoint was spleen response, or a 35% or greater reduction in spleen volume from baseline (determined by MRI or CT) at week 24 and confirmed 4 weeks later.
Thirty-six percent (35/96) of patients in the 400 mg arm and 40% (39/97) in the 500 mg arm achieved the primary endpoint, compared to 1% (1/96) of patients in the placebo arm (P<0.001).
The main secondary endpoint was symptom response, or a 50% or greater reduction in total symptom score (assessed using the modified Myelofibrosis Symptom Assessment Form).
At week 24, symptom response rates were 36% (33/91) in the 400 mg arm, 34% (31/91) in the 500 mg arm, and 7% (6/85) in the placebo arm (P<0.001).
Safety data
Treatment-emergent AEs occurred in 100% of patients in the 400 mg arm, 98% in the 500 mg arm, and 94% in the placebo arm. Serious AEs occurred in 27%, 31%, and 23%, respectively. AEs leading to discontinuation occurred in 14%, 25%, and 8%, respectively.
Infections occurred in 42% of patients in the 400 mg arm, 39% of patients in the 500 mg arm, and 27% of patients of patients in the placebo arm.
Nonhematologic AEs occurring in at least 10% of patients in any group were diarrhea (66%, 56%, and 16%, respectively), vomiting (42%, 55%, and 5%, respectively), nausea (64%, 51%, and 15%, respectively), constipation (10%, 18%, and 7%, respectively), asthenia (9%, 16%, and 6%, respectively), abdominal pain (15%, 12%, and 16%, respectively), fatigue (16%, 10%, and 10%, respectively), dyspnea (8%, 10%, and 6%, respectively), and weight loss (4%, 10%, and 5%, respectively).
Hematologic AEs occurring in at least 10% of patients in any group were anemia (99%, 98%, and 91%, respectively), thrombocytopenia (63%, 57%, and 51%, respectively), lymphopenia (57%, 66%, and 54%, respectively), leukopenia (47%, 53%, and 19%, respectively), and neutropenia (28%, 44%, and 15%, respectively).
One patient in each fedratinib arm and 2 in the placebo arm transformed to acute myeloid leukemia.
There were 24 deaths during the first 24 weeks of the study—4 in the 400 mg arm, 10 in the 500 mg arm, and 10 in the placebo arm. Nine of the deaths were attributed to AEs—1, 4, and 4, respectively.
Wernicke encephalopathy
There were 4 cases of Wernicke encephalopathy, all in women who received fedratinib at 500 mg. All of these cases were confirmed by an independent expert safety panel, 3 on the basis of clinical features and MRI results, and 1 on the basis of clinical symptoms alone.
The patients developed symptoms 6 weeks to 44 weeks after beginning fedratinib treatment, and all discontinued treatment permanently.
Cognitive symptoms manifested in the context of persistent vomiting, malnutrition, and cachexia in 1 patient, vomiting and hyponatremia in 1 patient, and renal failure with mild hyponatremia in 1 patient.
All of the patients received intravenous thiamine and showed responses to the treatment, but all had persistent cognitive defects at last follow-up. ![]()
Researchers have reported results of the phase 3 JAKARTA trial, in which they evaluated the selective JAK2 inhibitor fedratinib in patients with myelofibrosis (MF).
Fedratinib was being developed as a treatment for myeloproliferative neoplasms (MPNs), but Sanofi Oncology stopped clinical development of the drug in 2013, after it was linked to a neurological condition known as Wernicke encephalopathy.
There were 4 confirmed cases of Wernicke encephalopathy in the JAKARTA trial, in addition to other adverse events (AEs). However, fedratinib also lessened the severity of MF symptoms in about 35% to 40% of patients.
These results have been published in JAMA Oncology alongside an invited commentary. The study was sponsored by Sanofi.
Treatment and response
The study enrolled 289 adult patients with intermediate-2 or high-risk primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF. Patients were randomized to receive fedratinib at 400 mg once a day, fedratinib at 500 mg once a day, or placebo for at least 6 consecutive, 4-week cycles.
The study’s primary endpoint was spleen response, or a 35% or greater reduction in spleen volume from baseline (determined by MRI or CT) at week 24 and confirmed 4 weeks later.
Thirty-six percent (35/96) of patients in the 400 mg arm and 40% (39/97) in the 500 mg arm achieved the primary endpoint, compared to 1% (1/96) of patients in the placebo arm (P<0.001).
The main secondary endpoint was symptom response, or a 50% or greater reduction in total symptom score (assessed using the modified Myelofibrosis Symptom Assessment Form).
At week 24, symptom response rates were 36% (33/91) in the 400 mg arm, 34% (31/91) in the 500 mg arm, and 7% (6/85) in the placebo arm (P<0.001).
Safety data
Treatment-emergent AEs occurred in 100% of patients in the 400 mg arm, 98% in the 500 mg arm, and 94% in the placebo arm. Serious AEs occurred in 27%, 31%, and 23%, respectively. AEs leading to discontinuation occurred in 14%, 25%, and 8%, respectively.
Infections occurred in 42% of patients in the 400 mg arm, 39% of patients in the 500 mg arm, and 27% of patients of patients in the placebo arm.
Nonhematologic AEs occurring in at least 10% of patients in any group were diarrhea (66%, 56%, and 16%, respectively), vomiting (42%, 55%, and 5%, respectively), nausea (64%, 51%, and 15%, respectively), constipation (10%, 18%, and 7%, respectively), asthenia (9%, 16%, and 6%, respectively), abdominal pain (15%, 12%, and 16%, respectively), fatigue (16%, 10%, and 10%, respectively), dyspnea (8%, 10%, and 6%, respectively), and weight loss (4%, 10%, and 5%, respectively).
Hematologic AEs occurring in at least 10% of patients in any group were anemia (99%, 98%, and 91%, respectively), thrombocytopenia (63%, 57%, and 51%, respectively), lymphopenia (57%, 66%, and 54%, respectively), leukopenia (47%, 53%, and 19%, respectively), and neutropenia (28%, 44%, and 15%, respectively).
One patient in each fedratinib arm and 2 in the placebo arm transformed to acute myeloid leukemia.
There were 24 deaths during the first 24 weeks of the study—4 in the 400 mg arm, 10 in the 500 mg arm, and 10 in the placebo arm. Nine of the deaths were attributed to AEs—1, 4, and 4, respectively.
Wernicke encephalopathy
There were 4 cases of Wernicke encephalopathy, all in women who received fedratinib at 500 mg. All of these cases were confirmed by an independent expert safety panel, 3 on the basis of clinical features and MRI results, and 1 on the basis of clinical symptoms alone.
The patients developed symptoms 6 weeks to 44 weeks after beginning fedratinib treatment, and all discontinued treatment permanently.
Cognitive symptoms manifested in the context of persistent vomiting, malnutrition, and cachexia in 1 patient, vomiting and hyponatremia in 1 patient, and renal failure with mild hyponatremia in 1 patient.
All of the patients received intravenous thiamine and showed responses to the treatment, but all had persistent cognitive defects at last follow-up. ![]()
Inhibitor could treat range of hematologic disorders
A small molecule that targets the sonic Hedgehog signaling pathway has advanced to phase 2 trials in a range of hematologic disorders.
In a phase 1 study, the inhibitor, PF-04449913, exhibited activity in adults with leukemias, myelodysplastic syndromes (MDS), and myelofibrosis (MF).
Sixty percent of the patients studied experienced treatment-related adverse events (AEs), but there were no treatment-related deaths. Most deaths were disease-related.
Researchers detailed the results of this trial in The Lancet Haematology. The study was funded by Pfizer, the company developing PF-04449913, as well as the California Institute for Regenerative Medicine and European Leukemia Net.
Preclinical research showed that PF-04449913 forces dormant cancer stem cells in the bone marrow to begin differentiating and exit into the blood stream where they can be destroyed by chemotherapy agents targeting dividing cells.
“This drug gets that unwanted house guests to leave and never come back,” said Catriona Jamieson, MD, PhD, of University of California, San Diego School of Medicine.
“It’s a significant step forward in treating people with refractory or resistant myeloid leukemia, myelodysplastic syndrome, and myelofibrosis. It’s a bonus that the drug can be administered as easily as an aspirin, in a single, daily, oral tablet.”
For the first-in-human study, Dr Jamieson and her colleagues evaluated PF-04449913 in 47 adult patients. Twenty-eight of them had acute myeloid leukemia (AML), 6 had MDS, 5 had chronic myeloid leukemia (CML), 1 had chronic myelomonocytic leukemia (CMML), and 7 had MF.
Eighty-five percent of patients (n=40) had an ECOG performance status of 0-1. Eighty-one percent (n=38) had received previous systemic treatment, and 47% (n=22) had received 3 or more previous treatment regimens.
Patients received escalating daily doses of PF-04449913 in 28-day cycles. Treatment cycles were repeated until a patient experienced unacceptable AEs without evidence of clinical improvement. Patients who showed clinical activity without experiencing serious AEs received additional treatment cycles.
Dosing and AEs
Patients received PF-04449913 once daily at 5 mg (n=3), 10 mg (n=3), 20 mg (n=4), 40 mg (n=4), 80 mg (n=8), 120 mg (n=3), 180 mg (n=3), 270 mg (n=5), 400 mg (n=9), or 600 mg (n=5).
The researchers found the maximum-tolerated dose to be 400 mg once daily. The mean half-life was 23.9 hours in this dose group, and pharmacokinetics seemed to be dose-proportional.
Two patients experienced dose-limiting toxicities, 1 in the 80 mg group (grade 3 hypoxia and grade 3 pleural effusion), and 1 in the 600 mg group (grade 3 peripheral edema).
In all, 60% of patients (n=28) experienced treatment-related AEs. The most common were dysgeusia (28%), decreased appetite (19%), and alopecia (15%). There were 3 grade 4 AEs—1 case of neutropenia and 2 cases of thrombocytopenia.
There were 15 deaths, none of which were treatment-related. Eleven deaths were disease-related, and the remaining 4 were related to infection.
Clinical activity
The researchers said there was “some suggestion of clinical activity” in 23 patients (49%).
Of the 5 patients with CML (2 chronic phase and 3 blast phase), 1 patient with blast phase CML had a partial cytogenetic response to PF-04449913.
Of the 6 patients with MDS and 1 with CMML, 4 had stable disease after treatment. Two of these patients had hematologic improvement.
Two of the 7 patients with MF had clinical improvement.
Of the 28 patients with AML, 16 showed evidence of possible biological activity. One patient had a complete response and 4 had a partial response with incomplete hematologic recovery. Four AML patients had minor responses, and 7 had stable disease.
Given these results, PF-04449913 is now being investigated in 5 phase 2 trials of hematologic disorders, 4 of which are recruiting participants.
“Our hope is that this drug will enable more effective treatment to begin earlier and that, with earlier intervention, we can alter the course of disease and remove the need for, or improve the chances of success with, bone marrow transplantation,” Dr Jamieson said. “It’s all about reducing the burden of disease by intervening early.” ![]()
A small molecule that targets the sonic Hedgehog signaling pathway has advanced to phase 2 trials in a range of hematologic disorders.
In a phase 1 study, the inhibitor, PF-04449913, exhibited activity in adults with leukemias, myelodysplastic syndromes (MDS), and myelofibrosis (MF).
Sixty percent of the patients studied experienced treatment-related adverse events (AEs), but there were no treatment-related deaths. Most deaths were disease-related.
Researchers detailed the results of this trial in The Lancet Haematology. The study was funded by Pfizer, the company developing PF-04449913, as well as the California Institute for Regenerative Medicine and European Leukemia Net.
Preclinical research showed that PF-04449913 forces dormant cancer stem cells in the bone marrow to begin differentiating and exit into the blood stream where they can be destroyed by chemotherapy agents targeting dividing cells.
“This drug gets that unwanted house guests to leave and never come back,” said Catriona Jamieson, MD, PhD, of University of California, San Diego School of Medicine.
“It’s a significant step forward in treating people with refractory or resistant myeloid leukemia, myelodysplastic syndrome, and myelofibrosis. It’s a bonus that the drug can be administered as easily as an aspirin, in a single, daily, oral tablet.”
For the first-in-human study, Dr Jamieson and her colleagues evaluated PF-04449913 in 47 adult patients. Twenty-eight of them had acute myeloid leukemia (AML), 6 had MDS, 5 had chronic myeloid leukemia (CML), 1 had chronic myelomonocytic leukemia (CMML), and 7 had MF.
Eighty-five percent of patients (n=40) had an ECOG performance status of 0-1. Eighty-one percent (n=38) had received previous systemic treatment, and 47% (n=22) had received 3 or more previous treatment regimens.
Patients received escalating daily doses of PF-04449913 in 28-day cycles. Treatment cycles were repeated until a patient experienced unacceptable AEs without evidence of clinical improvement. Patients who showed clinical activity without experiencing serious AEs received additional treatment cycles.
Dosing and AEs
Patients received PF-04449913 once daily at 5 mg (n=3), 10 mg (n=3), 20 mg (n=4), 40 mg (n=4), 80 mg (n=8), 120 mg (n=3), 180 mg (n=3), 270 mg (n=5), 400 mg (n=9), or 600 mg (n=5).
The researchers found the maximum-tolerated dose to be 400 mg once daily. The mean half-life was 23.9 hours in this dose group, and pharmacokinetics seemed to be dose-proportional.
Two patients experienced dose-limiting toxicities, 1 in the 80 mg group (grade 3 hypoxia and grade 3 pleural effusion), and 1 in the 600 mg group (grade 3 peripheral edema).
In all, 60% of patients (n=28) experienced treatment-related AEs. The most common were dysgeusia (28%), decreased appetite (19%), and alopecia (15%). There were 3 grade 4 AEs—1 case of neutropenia and 2 cases of thrombocytopenia.
There were 15 deaths, none of which were treatment-related. Eleven deaths were disease-related, and the remaining 4 were related to infection.
Clinical activity
The researchers said there was “some suggestion of clinical activity” in 23 patients (49%).
Of the 5 patients with CML (2 chronic phase and 3 blast phase), 1 patient with blast phase CML had a partial cytogenetic response to PF-04449913.
Of the 6 patients with MDS and 1 with CMML, 4 had stable disease after treatment. Two of these patients had hematologic improvement.
Two of the 7 patients with MF had clinical improvement.
Of the 28 patients with AML, 16 showed evidence of possible biological activity. One patient had a complete response and 4 had a partial response with incomplete hematologic recovery. Four AML patients had minor responses, and 7 had stable disease.
Given these results, PF-04449913 is now being investigated in 5 phase 2 trials of hematologic disorders, 4 of which are recruiting participants.
“Our hope is that this drug will enable more effective treatment to begin earlier and that, with earlier intervention, we can alter the course of disease and remove the need for, or improve the chances of success with, bone marrow transplantation,” Dr Jamieson said. “It’s all about reducing the burden of disease by intervening early.” ![]()
A small molecule that targets the sonic Hedgehog signaling pathway has advanced to phase 2 trials in a range of hematologic disorders.
In a phase 1 study, the inhibitor, PF-04449913, exhibited activity in adults with leukemias, myelodysplastic syndromes (MDS), and myelofibrosis (MF).
Sixty percent of the patients studied experienced treatment-related adverse events (AEs), but there were no treatment-related deaths. Most deaths were disease-related.
Researchers detailed the results of this trial in The Lancet Haematology. The study was funded by Pfizer, the company developing PF-04449913, as well as the California Institute for Regenerative Medicine and European Leukemia Net.
Preclinical research showed that PF-04449913 forces dormant cancer stem cells in the bone marrow to begin differentiating and exit into the blood stream where they can be destroyed by chemotherapy agents targeting dividing cells.
“This drug gets that unwanted house guests to leave and never come back,” said Catriona Jamieson, MD, PhD, of University of California, San Diego School of Medicine.
“It’s a significant step forward in treating people with refractory or resistant myeloid leukemia, myelodysplastic syndrome, and myelofibrosis. It’s a bonus that the drug can be administered as easily as an aspirin, in a single, daily, oral tablet.”
For the first-in-human study, Dr Jamieson and her colleagues evaluated PF-04449913 in 47 adult patients. Twenty-eight of them had acute myeloid leukemia (AML), 6 had MDS, 5 had chronic myeloid leukemia (CML), 1 had chronic myelomonocytic leukemia (CMML), and 7 had MF.
Eighty-five percent of patients (n=40) had an ECOG performance status of 0-1. Eighty-one percent (n=38) had received previous systemic treatment, and 47% (n=22) had received 3 or more previous treatment regimens.
Patients received escalating daily doses of PF-04449913 in 28-day cycles. Treatment cycles were repeated until a patient experienced unacceptable AEs without evidence of clinical improvement. Patients who showed clinical activity without experiencing serious AEs received additional treatment cycles.
Dosing and AEs
Patients received PF-04449913 once daily at 5 mg (n=3), 10 mg (n=3), 20 mg (n=4), 40 mg (n=4), 80 mg (n=8), 120 mg (n=3), 180 mg (n=3), 270 mg (n=5), 400 mg (n=9), or 600 mg (n=5).
The researchers found the maximum-tolerated dose to be 400 mg once daily. The mean half-life was 23.9 hours in this dose group, and pharmacokinetics seemed to be dose-proportional.
Two patients experienced dose-limiting toxicities, 1 in the 80 mg group (grade 3 hypoxia and grade 3 pleural effusion), and 1 in the 600 mg group (grade 3 peripheral edema).
In all, 60% of patients (n=28) experienced treatment-related AEs. The most common were dysgeusia (28%), decreased appetite (19%), and alopecia (15%). There were 3 grade 4 AEs—1 case of neutropenia and 2 cases of thrombocytopenia.
There were 15 deaths, none of which were treatment-related. Eleven deaths were disease-related, and the remaining 4 were related to infection.
Clinical activity
The researchers said there was “some suggestion of clinical activity” in 23 patients (49%).
Of the 5 patients with CML (2 chronic phase and 3 blast phase), 1 patient with blast phase CML had a partial cytogenetic response to PF-04449913.
Of the 6 patients with MDS and 1 with CMML, 4 had stable disease after treatment. Two of these patients had hematologic improvement.
Two of the 7 patients with MF had clinical improvement.
Of the 28 patients with AML, 16 showed evidence of possible biological activity. One patient had a complete response and 4 had a partial response with incomplete hematologic recovery. Four AML patients had minor responses, and 7 had stable disease.
Given these results, PF-04449913 is now being investigated in 5 phase 2 trials of hematologic disorders, 4 of which are recruiting participants.
“Our hope is that this drug will enable more effective treatment to begin earlier and that, with earlier intervention, we can alter the course of disease and remove the need for, or improve the chances of success with, bone marrow transplantation,” Dr Jamieson said. “It’s all about reducing the burden of disease by intervening early.” ![]()
Methotrexate could treat MPNs cheaply, team says

Photo courtesy of the
National Cancer Institute
Preclinical research suggests the antineoplastic agent methotrexate (MTX) could be used to treat patients with myeloproliferative neoplasms (MPNs).
Experiments in Drosophila and human cell lines showed that MTX reduces JAK/STAT pathway activity and MPN-associated pathway signaling.
Researchers therefore speculated that low doses of MTX might treat MPNs as effectively as the JAK1/2 inhibitor ruxolitinib, but for a lower cost.
“Given that a year’s course of low-dose MTX costs around £30, the potential to repurpose MTX could provide thousands of patients with a much-needed treatment option and also generate substantial savings for healthcare systems,” said study author Martin Zeidler, DPhil, of The University of Sheffield in the UK.
He and his colleagues noted that, in comparison, ruxolitinib costs more than £40,000 per year per patient.
The researchers made this comparison and described their work with MTX in PLOS ONE.
The team used cells from the fruit fly Drosophila to screen for small molecules that suppress the JAK/STAT signaling pathway, which is central to the development of MPNs in humans. The screen suggested that MTX and a related molecule, aminopterin, suppress STAT activation.
So the researchers conducted experiments in human cell lines and found that MTX suppresses human JAK/STAT signaling without affecting other phosphorylation-dependent pathways.
The team also found that MTX significantly reduces STAT5 phosphorylation in cells expressing JAK2 V617F. However, MTX-treated cells can still respond to physiological levels of erythropoietin.
The researchers are now looking to undertake clinical trials to examine the possibility of repurposing low-dose MTX for the treatment of MPNs.
“We have the potential to revolutionize the treatment of this group of chronic diseases—a breakthrough that may ultimately represent a new treatment option able to bring relief to both patients and health funders,” Dr Zeidler said. ![]()

Photo courtesy of the
National Cancer Institute
Preclinical research suggests the antineoplastic agent methotrexate (MTX) could be used to treat patients with myeloproliferative neoplasms (MPNs).
Experiments in Drosophila and human cell lines showed that MTX reduces JAK/STAT pathway activity and MPN-associated pathway signaling.
Researchers therefore speculated that low doses of MTX might treat MPNs as effectively as the JAK1/2 inhibitor ruxolitinib, but for a lower cost.
“Given that a year’s course of low-dose MTX costs around £30, the potential to repurpose MTX could provide thousands of patients with a much-needed treatment option and also generate substantial savings for healthcare systems,” said study author Martin Zeidler, DPhil, of The University of Sheffield in the UK.
He and his colleagues noted that, in comparison, ruxolitinib costs more than £40,000 per year per patient.
The researchers made this comparison and described their work with MTX in PLOS ONE.
The team used cells from the fruit fly Drosophila to screen for small molecules that suppress the JAK/STAT signaling pathway, which is central to the development of MPNs in humans. The screen suggested that MTX and a related molecule, aminopterin, suppress STAT activation.
So the researchers conducted experiments in human cell lines and found that MTX suppresses human JAK/STAT signaling without affecting other phosphorylation-dependent pathways.
The team also found that MTX significantly reduces STAT5 phosphorylation in cells expressing JAK2 V617F. However, MTX-treated cells can still respond to physiological levels of erythropoietin.
The researchers are now looking to undertake clinical trials to examine the possibility of repurposing low-dose MTX for the treatment of MPNs.
“We have the potential to revolutionize the treatment of this group of chronic diseases—a breakthrough that may ultimately represent a new treatment option able to bring relief to both patients and health funders,” Dr Zeidler said. ![]()

Photo courtesy of the
National Cancer Institute
Preclinical research suggests the antineoplastic agent methotrexate (MTX) could be used to treat patients with myeloproliferative neoplasms (MPNs).
Experiments in Drosophila and human cell lines showed that MTX reduces JAK/STAT pathway activity and MPN-associated pathway signaling.
Researchers therefore speculated that low doses of MTX might treat MPNs as effectively as the JAK1/2 inhibitor ruxolitinib, but for a lower cost.
“Given that a year’s course of low-dose MTX costs around £30, the potential to repurpose MTX could provide thousands of patients with a much-needed treatment option and also generate substantial savings for healthcare systems,” said study author Martin Zeidler, DPhil, of The University of Sheffield in the UK.
He and his colleagues noted that, in comparison, ruxolitinib costs more than £40,000 per year per patient.
The researchers made this comparison and described their work with MTX in PLOS ONE.
The team used cells from the fruit fly Drosophila to screen for small molecules that suppress the JAK/STAT signaling pathway, which is central to the development of MPNs in humans. The screen suggested that MTX and a related molecule, aminopterin, suppress STAT activation.
So the researchers conducted experiments in human cell lines and found that MTX suppresses human JAK/STAT signaling without affecting other phosphorylation-dependent pathways.
The team also found that MTX significantly reduces STAT5 phosphorylation in cells expressing JAK2 V617F. However, MTX-treated cells can still respond to physiological levels of erythropoietin.
The researchers are now looking to undertake clinical trials to examine the possibility of repurposing low-dose MTX for the treatment of MPNs.
“We have the potential to revolutionize the treatment of this group of chronic diseases—a breakthrough that may ultimately represent a new treatment option able to bring relief to both patients and health funders,” Dr Zeidler said. ![]()
HSCT outcomes ‘encouraging’ in JAKi responders

Photo by Chad McNeeley
VIENNA—Outcomes of hematopoietic stem cell transplant (HSCT) are encouraging in myelofibrosis (MF) patients who respond well to JAK inhibitors, according to researchers.
The group found that patients with the best response to JAK inhibition had a 2-year survival probability of 91% after HSCT, compared to 32% for patients with
leukemic transformation while on a JAK inhibitor.
In addition, receiving a JAK inhibitor until HSCT could prevent the return of MF-related symptoms.
Mohamed Shanavas, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, presented these findings at the 20th Congress of the European Hematology Association (abstract S450*).
The decision to undergo HSCT is a complex one in MF, particularly for those patients who are responding to JAK inhibitors. So Dr Shanavas and his colleagues undertook a retrospective, multicenter analysis to determine if there is an association between response to JAK inhibition and HSCT outcome.
The investigators analyzed the outcomes of 100 patients who had a first HSCT for primary MF, post-essential thrombocythemia MF, or post-polycythemia vera MF. Patients had to have exposure to a JAK inhibitor but no history of leukemic transformation prior to taking a JAK inhibitor.
Response criteria
The researchers stratified patients’ JAK1/2 response according to the following criteria:
- Group A: Clinical improvement: Fifty percent or greater reduction in palpable spleen length for spleen palpable by ≥ 10 cm, or complete resolution of splenomegaly for spleen < 10 cm
- Group B: Stable disease: Spleen response not meeting the criteria of clinical improvement
- Group C: A 10% to 19% increase in blasts, new onset of anemia requiring transfusions, or intolerance to treatment due to side effects
- Group D: Progressive disease: New splenomegaly > 5 cm, 100% increase in spleen 5-10 cm, or 50% increase in spleen > 10 cm
- Group E: Leukemic transformation: Bone marrow or circulating blasts ≥ 20%.
Patient and treatment characteristics
Patients were a median age of 59 (range, 32–72). Fifty-seven had primary MF, 21 had post-essential thrombocythemia MF, and 22 had post-polycythemia vera MF. Sixty-two patients had JAK2V617F-mutated disease, 37 were wild-type, and 1 had unknown JAK status.
The majority of patients had intermediate-2 or high-risk disease according to their DIPSS scores, and 42 had a transplant comorbidity index score of 3 or greater.
Most patients (n=91) had ruxolitinib as their JAK inhibitor, 6 had momelotinib, and 3 had another inhibitor.
The median duration of JAK inhibitor therapy was 5 months (range, 1–36), and 66 patients were on treatment at the time of transplant. Thirty patients had previously discontinued JAK therapy, and the status of 4 was unknown.
In terms of their response to JAK inhibitors, 23 patients were in group A (clinical improvement), 31 in group B (stable disease), 15 in group C (increased blasts/transfusion need/intolerance), 18 in group D (progressive disease), and 13 in group E (leukemic transformation).
Fifty patients received a matched unrelated donor transplant, 36 had a matched sibling donor, and 14 had either a mismatched unrelated donor or a haploidentical transplant.
Fifty-six patients had a reduced-intensity conditioning regimen, and 44 had full intensity. Fifty percent of patients had T-cell depletion prior to transplant.
Outcomes
Patients who stopped JAK inhibitor therapy 6 or more days prior to transplant (n=20) experienced more “withdrawal symptoms”—the return of MF-related symptoms—than patients in whom the interval was less than 6 days (n=46). For the most part, withdrawal symptoms were non-severe in nature.
Two patients had fatal HSCT-related toxicity of venoocclusive disease, 4 had primary graft failure, and 4 had secondary graft failure. Forty-three percent of cytomegalovirus-seropositive patients had reactivation, 6 patients had Epstein-Barr virus reactivation, 6 had adenovirus or human polyomavirus BK infections, and 7 had invasive fungal infections.
Grade 2-4 acute graft-vs-host disease (GVHD) occurred in 37% of patients at day 100, and grade 3-4 occurred in 16%. Chronic GVHD of all grades occurred in 48% of patients, and extensive chronic GVHD occurred in 23%.
The cumulative incidence of relapse at 2 years was 17%, and non-relapse mortality was 28%. Overall survival (OS) was 61%.
“We analyzed this outcome based upon the response to JAK inhibitors,” Dr Shanavas said. “Patients who were deriving clinical improvement, group A, had a superior outcome, with a probability of survival of 91% at 2 years. Patients who had leukemic transformation, group E, had an inferior OS of 32% at 2 years.”
He noted that the outcomes appeared similar in the other 3 groups, so the researchers combined them for further analysis.
“As expected,” he said, “patients who had leukemic transformation had a significantly higher relapse rate than the other groups.”
The researchers then performed a multivariate analysis and found that response to JAK inhibitors, DIPSS score prior to JAK therapy, and donor type had a significant effect on OS.
The team concluded that prior exposure to JAK inhibitors does not have a negative effect on early HSCT outcomes. And actually, patients who undergo HSCT while responding to JAK inhibitors have encouraging outcomes. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo by Chad McNeeley
VIENNA—Outcomes of hematopoietic stem cell transplant (HSCT) are encouraging in myelofibrosis (MF) patients who respond well to JAK inhibitors, according to researchers.
The group found that patients with the best response to JAK inhibition had a 2-year survival probability of 91% after HSCT, compared to 32% for patients with
leukemic transformation while on a JAK inhibitor.
In addition, receiving a JAK inhibitor until HSCT could prevent the return of MF-related symptoms.
Mohamed Shanavas, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, presented these findings at the 20th Congress of the European Hematology Association (abstract S450*).
The decision to undergo HSCT is a complex one in MF, particularly for those patients who are responding to JAK inhibitors. So Dr Shanavas and his colleagues undertook a retrospective, multicenter analysis to determine if there is an association between response to JAK inhibition and HSCT outcome.
The investigators analyzed the outcomes of 100 patients who had a first HSCT for primary MF, post-essential thrombocythemia MF, or post-polycythemia vera MF. Patients had to have exposure to a JAK inhibitor but no history of leukemic transformation prior to taking a JAK inhibitor.
Response criteria
The researchers stratified patients’ JAK1/2 response according to the following criteria:
- Group A: Clinical improvement: Fifty percent or greater reduction in palpable spleen length for spleen palpable by ≥ 10 cm, or complete resolution of splenomegaly for spleen < 10 cm
- Group B: Stable disease: Spleen response not meeting the criteria of clinical improvement
- Group C: A 10% to 19% increase in blasts, new onset of anemia requiring transfusions, or intolerance to treatment due to side effects
- Group D: Progressive disease: New splenomegaly > 5 cm, 100% increase in spleen 5-10 cm, or 50% increase in spleen > 10 cm
- Group E: Leukemic transformation: Bone marrow or circulating blasts ≥ 20%.
Patient and treatment characteristics
Patients were a median age of 59 (range, 32–72). Fifty-seven had primary MF, 21 had post-essential thrombocythemia MF, and 22 had post-polycythemia vera MF. Sixty-two patients had JAK2V617F-mutated disease, 37 were wild-type, and 1 had unknown JAK status.
The majority of patients had intermediate-2 or high-risk disease according to their DIPSS scores, and 42 had a transplant comorbidity index score of 3 or greater.
Most patients (n=91) had ruxolitinib as their JAK inhibitor, 6 had momelotinib, and 3 had another inhibitor.
The median duration of JAK inhibitor therapy was 5 months (range, 1–36), and 66 patients were on treatment at the time of transplant. Thirty patients had previously discontinued JAK therapy, and the status of 4 was unknown.
In terms of their response to JAK inhibitors, 23 patients were in group A (clinical improvement), 31 in group B (stable disease), 15 in group C (increased blasts/transfusion need/intolerance), 18 in group D (progressive disease), and 13 in group E (leukemic transformation).
Fifty patients received a matched unrelated donor transplant, 36 had a matched sibling donor, and 14 had either a mismatched unrelated donor or a haploidentical transplant.
Fifty-six patients had a reduced-intensity conditioning regimen, and 44 had full intensity. Fifty percent of patients had T-cell depletion prior to transplant.
Outcomes
Patients who stopped JAK inhibitor therapy 6 or more days prior to transplant (n=20) experienced more “withdrawal symptoms”—the return of MF-related symptoms—than patients in whom the interval was less than 6 days (n=46). For the most part, withdrawal symptoms were non-severe in nature.
Two patients had fatal HSCT-related toxicity of venoocclusive disease, 4 had primary graft failure, and 4 had secondary graft failure. Forty-three percent of cytomegalovirus-seropositive patients had reactivation, 6 patients had Epstein-Barr virus reactivation, 6 had adenovirus or human polyomavirus BK infections, and 7 had invasive fungal infections.
Grade 2-4 acute graft-vs-host disease (GVHD) occurred in 37% of patients at day 100, and grade 3-4 occurred in 16%. Chronic GVHD of all grades occurred in 48% of patients, and extensive chronic GVHD occurred in 23%.
The cumulative incidence of relapse at 2 years was 17%, and non-relapse mortality was 28%. Overall survival (OS) was 61%.
“We analyzed this outcome based upon the response to JAK inhibitors,” Dr Shanavas said. “Patients who were deriving clinical improvement, group A, had a superior outcome, with a probability of survival of 91% at 2 years. Patients who had leukemic transformation, group E, had an inferior OS of 32% at 2 years.”
He noted that the outcomes appeared similar in the other 3 groups, so the researchers combined them for further analysis.
“As expected,” he said, “patients who had leukemic transformation had a significantly higher relapse rate than the other groups.”
The researchers then performed a multivariate analysis and found that response to JAK inhibitors, DIPSS score prior to JAK therapy, and donor type had a significant effect on OS.
The team concluded that prior exposure to JAK inhibitors does not have a negative effect on early HSCT outcomes. And actually, patients who undergo HSCT while responding to JAK inhibitors have encouraging outcomes. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo by Chad McNeeley
VIENNA—Outcomes of hematopoietic stem cell transplant (HSCT) are encouraging in myelofibrosis (MF) patients who respond well to JAK inhibitors, according to researchers.
The group found that patients with the best response to JAK inhibition had a 2-year survival probability of 91% after HSCT, compared to 32% for patients with
leukemic transformation while on a JAK inhibitor.
In addition, receiving a JAK inhibitor until HSCT could prevent the return of MF-related symptoms.
Mohamed Shanavas, MD, of Princess Margaret Cancer Centre in Toronto, Ontario, Canada, presented these findings at the 20th Congress of the European Hematology Association (abstract S450*).
The decision to undergo HSCT is a complex one in MF, particularly for those patients who are responding to JAK inhibitors. So Dr Shanavas and his colleagues undertook a retrospective, multicenter analysis to determine if there is an association between response to JAK inhibition and HSCT outcome.
The investigators analyzed the outcomes of 100 patients who had a first HSCT for primary MF, post-essential thrombocythemia MF, or post-polycythemia vera MF. Patients had to have exposure to a JAK inhibitor but no history of leukemic transformation prior to taking a JAK inhibitor.
Response criteria
The researchers stratified patients’ JAK1/2 response according to the following criteria:
- Group A: Clinical improvement: Fifty percent or greater reduction in palpable spleen length for spleen palpable by ≥ 10 cm, or complete resolution of splenomegaly for spleen < 10 cm
- Group B: Stable disease: Spleen response not meeting the criteria of clinical improvement
- Group C: A 10% to 19% increase in blasts, new onset of anemia requiring transfusions, or intolerance to treatment due to side effects
- Group D: Progressive disease: New splenomegaly > 5 cm, 100% increase in spleen 5-10 cm, or 50% increase in spleen > 10 cm
- Group E: Leukemic transformation: Bone marrow or circulating blasts ≥ 20%.
Patient and treatment characteristics
Patients were a median age of 59 (range, 32–72). Fifty-seven had primary MF, 21 had post-essential thrombocythemia MF, and 22 had post-polycythemia vera MF. Sixty-two patients had JAK2V617F-mutated disease, 37 were wild-type, and 1 had unknown JAK status.
The majority of patients had intermediate-2 or high-risk disease according to their DIPSS scores, and 42 had a transplant comorbidity index score of 3 or greater.
Most patients (n=91) had ruxolitinib as their JAK inhibitor, 6 had momelotinib, and 3 had another inhibitor.
The median duration of JAK inhibitor therapy was 5 months (range, 1–36), and 66 patients were on treatment at the time of transplant. Thirty patients had previously discontinued JAK therapy, and the status of 4 was unknown.
In terms of their response to JAK inhibitors, 23 patients were in group A (clinical improvement), 31 in group B (stable disease), 15 in group C (increased blasts/transfusion need/intolerance), 18 in group D (progressive disease), and 13 in group E (leukemic transformation).
Fifty patients received a matched unrelated donor transplant, 36 had a matched sibling donor, and 14 had either a mismatched unrelated donor or a haploidentical transplant.
Fifty-six patients had a reduced-intensity conditioning regimen, and 44 had full intensity. Fifty percent of patients had T-cell depletion prior to transplant.
Outcomes
Patients who stopped JAK inhibitor therapy 6 or more days prior to transplant (n=20) experienced more “withdrawal symptoms”—the return of MF-related symptoms—than patients in whom the interval was less than 6 days (n=46). For the most part, withdrawal symptoms were non-severe in nature.
Two patients had fatal HSCT-related toxicity of venoocclusive disease, 4 had primary graft failure, and 4 had secondary graft failure. Forty-three percent of cytomegalovirus-seropositive patients had reactivation, 6 patients had Epstein-Barr virus reactivation, 6 had adenovirus or human polyomavirus BK infections, and 7 had invasive fungal infections.
Grade 2-4 acute graft-vs-host disease (GVHD) occurred in 37% of patients at day 100, and grade 3-4 occurred in 16%. Chronic GVHD of all grades occurred in 48% of patients, and extensive chronic GVHD occurred in 23%.
The cumulative incidence of relapse at 2 years was 17%, and non-relapse mortality was 28%. Overall survival (OS) was 61%.
“We analyzed this outcome based upon the response to JAK inhibitors,” Dr Shanavas said. “Patients who were deriving clinical improvement, group A, had a superior outcome, with a probability of survival of 91% at 2 years. Patients who had leukemic transformation, group E, had an inferior OS of 32% at 2 years.”
He noted that the outcomes appeared similar in the other 3 groups, so the researchers combined them for further analysis.
“As expected,” he said, “patients who had leukemic transformation had a significantly higher relapse rate than the other groups.”
The researchers then performed a multivariate analysis and found that response to JAK inhibitors, DIPSS score prior to JAK therapy, and donor type had a significant effect on OS.
The team concluded that prior exposure to JAK inhibitors does not have a negative effect on early HSCT outcomes. And actually, patients who undergo HSCT while responding to JAK inhibitors have encouraging outcomes. ![]()
*Information in the abstract differs from that presented at the meeting.
Agent reduces fibrosis, improves platelet counts in MF
VIENNA—The immunotherapeutic agent PRM-151, when given alone or in combination with ruxolitinib, can reduce bone marrow fibrosis and improve platelet counts in patients with myelofibrosis (MF), results of a phase 2 trial suggest.
Using a novel assessment technique known as computer-assisted image analysis (CIA), researchers found that PRM-151, with or without ruxolitinib, prompted fibrosis responses in nearly three-quarters of patients studied.
And nearly 60% of thrombocytopenic patients saw improvements in their platelet counts.
“Thrombocytopenia remains a significant problem for many patients with myelofibrosis, and a new treatment that is not myelosuppressive and actually increases platelet counts would be of great benefit to patients,” said Srdan Verstovsek, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
He and his colleagues presented this research—the first part of a 2-stage study—at the 20th Congress of the European Hematology Association (abstract P677*). The trial is sponsored by Promedior, the company developing PRM-151.
Stage 1 of the study included 27 patients with a median age of 67 (range, 51-85). They had been diagnosed with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The patients received PRM-151 at 10 mg/kg IV dosed weekly (n=8) or monthly (n=7), or ruxolitinib plus PRM-151 at 10 mg/kg IV dosed weekly (n=6) or monthly (n=6). The patients who received ruxolitinib were already taking the drug, and doses varied. The mean duration of ruxolitinib treatment was 1.6 years (range, 0.6-3 years).
Patients were set to receive study treatment for 24 weeks but could continue beyond that if they experienced clinical improvement.
Response assessment: Using CIA
Hematopathologists who were blinded to the patient, treatment, and time point performed morphologic analysis on bone marrow specimens taken at baseline and at 12, 24, and 36 weeks (if available).
The pathologists also performed CIA on whole-slide scans from specimens taken at the same time points. The idea to use CIA came after morphologic analyses revealed some surprising findings.
“[The pathologists] were really struck by the fact that, in the patients who had reductions in fibrosis, there were other elements in the bone marrow that showed improvements,” said Beth Trehu, MD, Chief Medical Officer at Promedior. “There were trends toward normalization of the red cells and of the megakaryocytes.”
“They also remarked that, whereas the baseline samples were totally homogeneous—a grade 3 was a grade 3 throughout the bone marrow—after treatment, the samples became very heterogeneous. There were areas of grade 3, grade 2, grade 1, and 0, all in one sample.”
To solve this problem, the pathologists decided that a sample’s WHO grade would be defined as whatever grade was present in at least 50% of the sample. But the team still thought these grades weren’t accurately quantifying the effects of PRM-151.
So they turned to CIA, which allowed them to quantify the volume of collagen or reticulin fibers in the bone marrow.
Fibrosis and platelet responses
According to CIA, 73% of evaluable patients (19/26) experienced reductions in bone marrow fibrosis at any time during the trial.
Of the 23 evaluable patients who had grade 2 or 3 fibrosis at baseline, 11 patients had a reduction of 1 grade or more during the study period, according to morphologic analysis. Nine patients had a fibrosis response by morphology at the last time point they were assessed.
Reductions in fibrosis correlated with increased platelet counts in thrombocytopenic patients. Fifty-seven percent of thrombocytopenic patients (8/14) saw an improvement in platelet counts after treatment.
Results across treatment groups were as follows:
| Treatment group (n) | WHO fibrosis
response at any time |
CIA fibrosis
response at any time |
Platelet
improvement |
| PRM-151 QW (7) | 3 | 4 | 2 |
| PRM-151 Q4W (7) | 3 | 6 | 4 |
| PRM-151 QW + RUX (6) | 2 | 4 | 1 |
| PRM-151 Q4W + RUX (6) | 3 | 5 | 1 |
“The responses we saw with single-agent PRM-151, in particular, give us a lot of confidence that this drug is absolutely reversing fibrosis in the bone marrow,” Dr Trehu said. “And that is very nicely correlated with improvements in platelets, which are much harder to see in patients who are getting ruxolitinib because it’s a myelosuppressive agent.”
Dr Trehu added that these data suggest a monthly dose of PRM-151 is sufficient to treat MF patients, and there is a path forward for PRM-151 both alone and in combination with ruxolitinib.
Hemoglobin and spleen responses
The researchers also observed some improvements in hemoglobin levels and spleen size after treatment.
Of the 15 patients who had hemoglobin levels below 100 g/L at baseline, 3 met criteria for hemoglobin improvement. This included becoming transfusion independent, having a 50% reduction in the need for transfusion, or experiencing a 2 g/L increase in hemoglobin.
“Other patients had a nice trend toward hemoglobin improvement,” Dr Trehu noted.
Of the 20 patients with palpable spleen at baseline, reductions occurred in all but 1 patient. Four patients had a 50% or greater reduction in spleen size, but this response did not last beyond 12 weeks.
Adverse events
Forty-eight percent of patients (13/27) had at least 1 treatment-related adverse event (AE). Grade 1 AEs included diarrhea (n=3), fatigue (n=2), bruising at the infusion site (n=2), oral herpes (n=1), joint swelling (n=2), and headache (n=2). One patient had grade 2 oral herpes.
There were 5 serious AEs that were possibly treatment-related. Three events, from which patients recovered, were abdominal pain, sialadenitis, and pneumonia. The other 2 serious AEs were gastroenteritis and pneumonia, which resulted in death in an 85-year-old patient.
There were 2 deaths unrelated to treatment. One was due to pneumonia, and the other was a result of multi-organ failure and cardiac arrest. ![]()
*Information in the abstract differs from that presented at the meeting.
VIENNA—The immunotherapeutic agent PRM-151, when given alone or in combination with ruxolitinib, can reduce bone marrow fibrosis and improve platelet counts in patients with myelofibrosis (MF), results of a phase 2 trial suggest.
Using a novel assessment technique known as computer-assisted image analysis (CIA), researchers found that PRM-151, with or without ruxolitinib, prompted fibrosis responses in nearly three-quarters of patients studied.
And nearly 60% of thrombocytopenic patients saw improvements in their platelet counts.
“Thrombocytopenia remains a significant problem for many patients with myelofibrosis, and a new treatment that is not myelosuppressive and actually increases platelet counts would be of great benefit to patients,” said Srdan Verstovsek, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
He and his colleagues presented this research—the first part of a 2-stage study—at the 20th Congress of the European Hematology Association (abstract P677*). The trial is sponsored by Promedior, the company developing PRM-151.
Stage 1 of the study included 27 patients with a median age of 67 (range, 51-85). They had been diagnosed with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The patients received PRM-151 at 10 mg/kg IV dosed weekly (n=8) or monthly (n=7), or ruxolitinib plus PRM-151 at 10 mg/kg IV dosed weekly (n=6) or monthly (n=6). The patients who received ruxolitinib were already taking the drug, and doses varied. The mean duration of ruxolitinib treatment was 1.6 years (range, 0.6-3 years).
Patients were set to receive study treatment for 24 weeks but could continue beyond that if they experienced clinical improvement.
Response assessment: Using CIA
Hematopathologists who were blinded to the patient, treatment, and time point performed morphologic analysis on bone marrow specimens taken at baseline and at 12, 24, and 36 weeks (if available).
The pathologists also performed CIA on whole-slide scans from specimens taken at the same time points. The idea to use CIA came after morphologic analyses revealed some surprising findings.
“[The pathologists] were really struck by the fact that, in the patients who had reductions in fibrosis, there were other elements in the bone marrow that showed improvements,” said Beth Trehu, MD, Chief Medical Officer at Promedior. “There were trends toward normalization of the red cells and of the megakaryocytes.”
“They also remarked that, whereas the baseline samples were totally homogeneous—a grade 3 was a grade 3 throughout the bone marrow—after treatment, the samples became very heterogeneous. There were areas of grade 3, grade 2, grade 1, and 0, all in one sample.”
To solve this problem, the pathologists decided that a sample’s WHO grade would be defined as whatever grade was present in at least 50% of the sample. But the team still thought these grades weren’t accurately quantifying the effects of PRM-151.
So they turned to CIA, which allowed them to quantify the volume of collagen or reticulin fibers in the bone marrow.
Fibrosis and platelet responses
According to CIA, 73% of evaluable patients (19/26) experienced reductions in bone marrow fibrosis at any time during the trial.
Of the 23 evaluable patients who had grade 2 or 3 fibrosis at baseline, 11 patients had a reduction of 1 grade or more during the study period, according to morphologic analysis. Nine patients had a fibrosis response by morphology at the last time point they were assessed.
Reductions in fibrosis correlated with increased platelet counts in thrombocytopenic patients. Fifty-seven percent of thrombocytopenic patients (8/14) saw an improvement in platelet counts after treatment.
Results across treatment groups were as follows:
| Treatment group (n) | WHO fibrosis
response at any time |
CIA fibrosis
response at any time |
Platelet
improvement |
| PRM-151 QW (7) | 3 | 4 | 2 |
| PRM-151 Q4W (7) | 3 | 6 | 4 |
| PRM-151 QW + RUX (6) | 2 | 4 | 1 |
| PRM-151 Q4W + RUX (6) | 3 | 5 | 1 |
“The responses we saw with single-agent PRM-151, in particular, give us a lot of confidence that this drug is absolutely reversing fibrosis in the bone marrow,” Dr Trehu said. “And that is very nicely correlated with improvements in platelets, which are much harder to see in patients who are getting ruxolitinib because it’s a myelosuppressive agent.”
Dr Trehu added that these data suggest a monthly dose of PRM-151 is sufficient to treat MF patients, and there is a path forward for PRM-151 both alone and in combination with ruxolitinib.
Hemoglobin and spleen responses
The researchers also observed some improvements in hemoglobin levels and spleen size after treatment.
Of the 15 patients who had hemoglobin levels below 100 g/L at baseline, 3 met criteria for hemoglobin improvement. This included becoming transfusion independent, having a 50% reduction in the need for transfusion, or experiencing a 2 g/L increase in hemoglobin.
“Other patients had a nice trend toward hemoglobin improvement,” Dr Trehu noted.
Of the 20 patients with palpable spleen at baseline, reductions occurred in all but 1 patient. Four patients had a 50% or greater reduction in spleen size, but this response did not last beyond 12 weeks.
Adverse events
Forty-eight percent of patients (13/27) had at least 1 treatment-related adverse event (AE). Grade 1 AEs included diarrhea (n=3), fatigue (n=2), bruising at the infusion site (n=2), oral herpes (n=1), joint swelling (n=2), and headache (n=2). One patient had grade 2 oral herpes.
There were 5 serious AEs that were possibly treatment-related. Three events, from which patients recovered, were abdominal pain, sialadenitis, and pneumonia. The other 2 serious AEs were gastroenteritis and pneumonia, which resulted in death in an 85-year-old patient.
There were 2 deaths unrelated to treatment. One was due to pneumonia, and the other was a result of multi-organ failure and cardiac arrest. ![]()
*Information in the abstract differs from that presented at the meeting.
VIENNA—The immunotherapeutic agent PRM-151, when given alone or in combination with ruxolitinib, can reduce bone marrow fibrosis and improve platelet counts in patients with myelofibrosis (MF), results of a phase 2 trial suggest.
Using a novel assessment technique known as computer-assisted image analysis (CIA), researchers found that PRM-151, with or without ruxolitinib, prompted fibrosis responses in nearly three-quarters of patients studied.
And nearly 60% of thrombocytopenic patients saw improvements in their platelet counts.
“Thrombocytopenia remains a significant problem for many patients with myelofibrosis, and a new treatment that is not myelosuppressive and actually increases platelet counts would be of great benefit to patients,” said Srdan Verstovsek, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
He and his colleagues presented this research—the first part of a 2-stage study—at the 20th Congress of the European Hematology Association (abstract P677*). The trial is sponsored by Promedior, the company developing PRM-151.
Stage 1 of the study included 27 patients with a median age of 67 (range, 51-85). They had been diagnosed with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The patients received PRM-151 at 10 mg/kg IV dosed weekly (n=8) or monthly (n=7), or ruxolitinib plus PRM-151 at 10 mg/kg IV dosed weekly (n=6) or monthly (n=6). The patients who received ruxolitinib were already taking the drug, and doses varied. The mean duration of ruxolitinib treatment was 1.6 years (range, 0.6-3 years).
Patients were set to receive study treatment for 24 weeks but could continue beyond that if they experienced clinical improvement.
Response assessment: Using CIA
Hematopathologists who were blinded to the patient, treatment, and time point performed morphologic analysis on bone marrow specimens taken at baseline and at 12, 24, and 36 weeks (if available).
The pathologists also performed CIA on whole-slide scans from specimens taken at the same time points. The idea to use CIA came after morphologic analyses revealed some surprising findings.
“[The pathologists] were really struck by the fact that, in the patients who had reductions in fibrosis, there were other elements in the bone marrow that showed improvements,” said Beth Trehu, MD, Chief Medical Officer at Promedior. “There were trends toward normalization of the red cells and of the megakaryocytes.”
“They also remarked that, whereas the baseline samples were totally homogeneous—a grade 3 was a grade 3 throughout the bone marrow—after treatment, the samples became very heterogeneous. There were areas of grade 3, grade 2, grade 1, and 0, all in one sample.”
To solve this problem, the pathologists decided that a sample’s WHO grade would be defined as whatever grade was present in at least 50% of the sample. But the team still thought these grades weren’t accurately quantifying the effects of PRM-151.
So they turned to CIA, which allowed them to quantify the volume of collagen or reticulin fibers in the bone marrow.
Fibrosis and platelet responses
According to CIA, 73% of evaluable patients (19/26) experienced reductions in bone marrow fibrosis at any time during the trial.
Of the 23 evaluable patients who had grade 2 or 3 fibrosis at baseline, 11 patients had a reduction of 1 grade or more during the study period, according to morphologic analysis. Nine patients had a fibrosis response by morphology at the last time point they were assessed.
Reductions in fibrosis correlated with increased platelet counts in thrombocytopenic patients. Fifty-seven percent of thrombocytopenic patients (8/14) saw an improvement in platelet counts after treatment.
Results across treatment groups were as follows:
| Treatment group (n) | WHO fibrosis
response at any time |
CIA fibrosis
response at any time |
Platelet
improvement |
| PRM-151 QW (7) | 3 | 4 | 2 |
| PRM-151 Q4W (7) | 3 | 6 | 4 |
| PRM-151 QW + RUX (6) | 2 | 4 | 1 |
| PRM-151 Q4W + RUX (6) | 3 | 5 | 1 |
“The responses we saw with single-agent PRM-151, in particular, give us a lot of confidence that this drug is absolutely reversing fibrosis in the bone marrow,” Dr Trehu said. “And that is very nicely correlated with improvements in platelets, which are much harder to see in patients who are getting ruxolitinib because it’s a myelosuppressive agent.”
Dr Trehu added that these data suggest a monthly dose of PRM-151 is sufficient to treat MF patients, and there is a path forward for PRM-151 both alone and in combination with ruxolitinib.
Hemoglobin and spleen responses
The researchers also observed some improvements in hemoglobin levels and spleen size after treatment.
Of the 15 patients who had hemoglobin levels below 100 g/L at baseline, 3 met criteria for hemoglobin improvement. This included becoming transfusion independent, having a 50% reduction in the need for transfusion, or experiencing a 2 g/L increase in hemoglobin.
“Other patients had a nice trend toward hemoglobin improvement,” Dr Trehu noted.
Of the 20 patients with palpable spleen at baseline, reductions occurred in all but 1 patient. Four patients had a 50% or greater reduction in spleen size, but this response did not last beyond 12 weeks.
Adverse events
Forty-eight percent of patients (13/27) had at least 1 treatment-related adverse event (AE). Grade 1 AEs included diarrhea (n=3), fatigue (n=2), bruising at the infusion site (n=2), oral herpes (n=1), joint swelling (n=2), and headache (n=2). One patient had grade 2 oral herpes.
There were 5 serious AEs that were possibly treatment-related. Three events, from which patients recovered, were abdominal pain, sialadenitis, and pneumonia. The other 2 serious AEs were gastroenteritis and pneumonia, which resulted in death in an 85-year-old patient.
There were 2 deaths unrelated to treatment. One was due to pneumonia, and the other was a result of multi-organ failure and cardiac arrest.
*Information in the abstract differs from that presented at the meeting.
JAK inhibitor can provide long-term disease control in PV

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”

Image courtesy of AFIP
VIENNA—Updated results from the phase 3 RESPONSE trial suggest the JAK1/2 inhibitor ruxolitinib can provide long-term disease control in patients with polycythemia vera (PV) who are resistant to or intolerant of hydroxyurea.
At 18 months of follow-up, 80% of patients had achieved a durable response to ruxolitinib, sustaining hematocrit levels below 45% without the use of phlebotomy and experiencing reductions in spleen size.
In addition, 83% of patients were still receiving ruxolitinib at last follow-up.
“Polycythemia vera can lead to serious complications if inadequately controlled, and these data demonstrate the ability of [ruxolitinib] to provide a durable and comprehensive clinical benefit in this patient population,” said Jean-Jacques Kiladjian, MD, PhD, of Hôpital Saint-Louis et Université Paris Diderot in France.
Dr Kiladjian presented these results at the 20th Congress of the European Hematology Association (abstract S447). The RESPONSE trial was sponsored by Incyte Corporation and Novartis Pharmaceuticals, the companies developing ruxolitinib.
The study included 222 patients with PV whose were resistant to or could not tolerate hydroxyurea. They were randomized 1:1 to receive either ruxolitinib (at a starting dose of 10 mg twice daily) or best available therapy (BAT), which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the trial.
The study’s primary endpoint was the proportion of patients who achieved hematocrit control and were not eligible for phlebotomy from week 8 through 32 (with no more than 1 instance of phlebotomy eligibility between randomization and week 8) and who saw a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
Patients were deemed eligible for phlebotomy if they had hematocrit that was greater than 45% and had increased 3 or more percentage points from the time they entered the trial or if they had hematocrit greater than 48%.
The researchers performed a second, preplanned analysis at 80 weeks (18 months), evaluating the durability of primary response, hematocrit control, spleen size reduction, complete hematologic remission, and safety. The team also conducted a separate analysis evaluating hematologic parameters.
Results at 32 and 80 weeks
Twenty-one percent of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved the primary endpoint (P<0.0001). All but 1 of the responders in the ruxolitinib arm maintained this response at 80 weeks.
Sixty percent of patients in the ruxolitinib arm and 20% in the BAT arm achieved hematocrit control without phlebotomy through week 32. Patients in the ruxolitinib arm had an 89% probability of maintaining this response for 80 weeks from the time of initial response. Of the 98 patients on ruxolitinib at week 32, 90% did not have a phlebotomy between weeks 32 and 80.
At week 32, 38% of patients in the ruxolitinib arm and 1% of patients in the BAT arm achieved a 35% or greater reduction in spleen volume. All of the ruxolitinib-treated patients maintained this response at 80 weeks.
At week 32, 24% of patients in the ruxolitinib arm had a complete hematologic remission, as did 9% of patients in the BAT arm. Patients in the ruxolitinib arm had a 69% probability of maintaining this response for 80 weeks.
A separate analysis of the data at 18 months demonstrated that ruxolitinib treatment also led to sustained control of white blood cell and platelet levels, with the largest reductions occurring in patients who had the most elevated values at baseline.
At week 80, 83% of patients in the ruxolitinib arm remained on treatment (median exposure of 111 weeks), but none of the patients in the BAT arm were still receiving their assigned therapy.
At 80 weeks, the most common adverse events in the ruxolitinib arm were headache (22%), diarrhea (20%), pruritus (20%), and fatigue (17%). Grade 3 or 4 anemia and thrombocytopenia occurred in 2% and 6% of patients, respectively. Five percent of patients discontinued treatment due to adverse events.
“There is currently a significant unmet need for patients with polycythemia vera who are unable to tolerate or control their disease on other treatments,” Dr Kiladjian said. “For these patients, [ruxolitinib] represents a valuable new option, as confirmed by results from the long-term, phase 3 study.”
Inhibitor may fulfill unmet need in MF

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded.

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded.

© ASCO/Zach Boyden-Holmes
CHICAGO—The JAK2/FLT3 inhibitor pacritinib may fulfill an unmet need in the treatment of myelofibrosis (MF), according to a speaker at the 2015 ASCO Annual Meeting.
Results of the phase 3 PERSIST-1 trial indicate that pacritinib is safe and effective for MF patients with thrombocytopenia.
“Thrombocytopenia is a common feature in people with advanced [MF], and current treatment options have not been able to concurrently improve splenomegaly symptoms and cytopenias in these patients,” said study investigator Ruben A. Mesa, MD, of the Mayo Clinic Cancer Center in Scottsdale, Arizona.
But PERSIST-1 showed that pacritinib can accomplish this. And the drug proved more effective than best available therapy (BAT), excluding JAK inhibitors, in reducing spleen volume and alleviating MF symptoms in the entire cohort of MF patients.
Dr Mesa presented these results at ASCO as abstract LBA7006. The study was funded by CTI BioPharma Corp., the company developing pacritinib.
The trial included 327 patients who were randomized to receive pacritinib (n=220) or BAT (n=107).
Patients in the BAT arm received therapies that are routinely prescribed off-label for MF, such as erythropoietin-stimulating agents, immunomodulatory drugs, and hydroxyurea. Ruxolitinib was intentionally excluded from this trial because the study included patients with thrombocytopenia.
Dr Mesa said the patients’ baseline characteristics “demonstrate a group of individuals with advanced myelofibrosis, a heavy percentage of those with primary myelofibrosis, the vast majority having intermediate-2 or high-risk disease, with very significant splenomegaly, and the vast majority having the JAK2 mutation.”
“About half the individuals were anemic or transfusion-dependent,” he noted. “And a full third were thrombocytopenic, under 100,000 [platelets/µL], with 16% under 50,000 [platelets/µL]. This was the first phase 3 study of myelofibrosis that allowed individuals with a platelet count of less than 100,000 to be enrolled.”
Fifty-six percent of patients remained on pacritinib at the time of analysis, as did 8% of patients on BAT. Seventy-nine percent of patients crossed over from the BAT arm to the pacritinib arm.
Spleen reduction
The study’s primary endpoint was a reduction in spleen volume of 35% or greater.
In the intent-to-treat (ITT) population, 19.1% of patients in the pacritinib arm met this endpoint, as did 4.7% of patients in the BAT arm (P=0.0003). In the evaluable population—165 patients in the pacritinib arm and 85 patients in the BAT arm—the rates were 25% and 5.9%, respectively (P=0.0001).
Dr Mesa noted that pacritinib was able to reduce spleen volume in all subgroups of patients, including those with thrombocytopenia.
“Both the group [with platelet counts] under 100,000 as well as under 50,000 uniquely responded only on the pacritinib arm, with no responses on the BAT arm,” he said.
In the ITT population, 16.7% of patients with platelet counts under 100,000/µL and 22.9% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values, in the comparison with the BAT arm, were 0.0451 and 0.0086, respectively.
In the evaluable population, 23.5% of patients with platelet counts under 100,000/µL and 33.3% of patients with platelet counts under 50,000/µL met the primary endpoint. The P values were 0.0370 and 0.0072, respectively.
“It is too early to know if pacritinib has an impact on survival, but that is clearly our expectation [based on the spleen responses observed],” Dr Mesa said.
TSS and transfusion
The study’s secondary endpoint was the proportion of patients with a 50% or greater reduction in Total Symptom Score (TSS) from baseline to week 24. TSS was measured by patient responses on the Myeloproliferative Neoplasm Symptom Assessment Form.
In the ITT population, 24.5% of pacritinib-treated patients and 6.5% of BAT-treated patients had a 50% or greater reduction in TSS score (P<0.0001). In the evaluable population, 40.9% and 9.9% of patients, respectively (P<0.0001), met this endpoint.
Dr Mesa also pointed out that 25.7% of pacritinib-treated patients who were severely anemic and transfusion-dependent—requiring at least 6 units of blood in the 90 days prior to study entry—became transfusion independent. But none of the BAT-treated patients did so (P<0.043).
Adverse events
“The most common adverse events [in the pacritinib arm] were consistent with the earlier studies,” Dr Mesa said. “Gastrointestinal toxicities were most common, although typically at low grades.”
“As expected, we saw very few individuals with any significant thrombocytopenia or anemia as drug-emergent. There were individuals who enrolled in the study as a grade 4, so some of those remained.”
The most common adverse events of any grade were diarrhea (53.2% in the pacritinib arm and 12.3% in the BAT arm), nausea (26.8% vs 6.6%), anemia (22.3% vs 19.8%), thrombocytopenia (16.8% vs 13.2%), and vomiting (15.9% vs 5.7%).
Ten percent of patients in the pacritinib arm required dose reductions due to adverse events. Diarrhea prompted dose interruptions in 13 patients and discontinuation in 3 patients. But pacritinib-associated diarrhea typically resolved in a little over a week.
“Based on these preliminary results, pacritinib may represent a very important agent for individuals with advanced disease and may have an impact on the disease course,” Dr Mesa concluded.
Team reports new method to identify immune cells

Photo by Graham Colm
A new method for identifying immune cells could pave the way for rapid detection of hematologic malignancies from a small blood sample, according to researchers.
The team found they could use wavelength modulated Raman spectroscopy (WMRS) to identify subsets of T cells, natural killer cells, and dendritic cells.
Traditional methods of identifying these cells usually involve labeling them with fluorescent or magnetically labeled antibodies.
Using WMRS, the researchers were able to identify immune cells with no labeling at all, thus permitting rapid identification and further analysis to take place with no potential alteration to the cells.
Simon Powis, PhD, of the University of St Andrews in Fife, Scotland, and his colleagues described this work in PLOS ONE.
Raman scattering refers to light scattering from molecules in a sample where the light energy can be shifted up or down and recorded as a “molecular fingerprint” that can be used for identification. Normally, this process is very weak and further hampered by other background light (eg, fluorescence).
WMRS subtly changes the incident laser light that, in turn, results in a modulation of the Raman signal, allowing it to be extracted from any (stationary) interfering signal.
Using WMRS, Dr Powis and his colleagues found they could identify CD4+ T cells, CD8+ T cells, CD56+ natural killer cells, CD303+ lymphoid/plasmacytoid dendritic cells, and CD1c+ myeloid dendritic cells.
“Under a normal light microscope, these immune cells essentially all look identical,” Dr Powis said. “With this new method, we can identify key cell types without any labeling.”
“Our next goal is to make a full catalogue of all the normal cell types of the immune system that can be detected in the bloodstream. Once we have this completed, we can then collaborate with our clinical colleagues to start identifying when these immune cells are altered, in conditions such as leukemia and lymphoma, potentially providing a rapid detection system from just a small blood sample.”

Photo by Graham Colm
A new method for identifying immune cells could pave the way for rapid detection of hematologic malignancies from a small blood sample, according to researchers.
The team found they could use wavelength modulated Raman spectroscopy (WMRS) to identify subsets of T cells, natural killer cells, and dendritic cells.
Traditional methods of identifying these cells usually involve labeling them with fluorescent or magnetically labeled antibodies.
Using WMRS, the researchers were able to identify immune cells with no labeling at all, thus permitting rapid identification and further analysis to take place with no potential alteration to the cells.
Simon Powis, PhD, of the University of St Andrews in Fife, Scotland, and his colleagues described this work in PLOS ONE.
Raman scattering refers to light scattering from molecules in a sample where the light energy can be shifted up or down and recorded as a “molecular fingerprint” that can be used for identification. Normally, this process is very weak and further hampered by other background light (eg, fluorescence).
WMRS subtly changes the incident laser light that, in turn, results in a modulation of the Raman signal, allowing it to be extracted from any (stationary) interfering signal.
Using WMRS, Dr Powis and his colleagues found they could identify CD4+ T cells, CD8+ T cells, CD56+ natural killer cells, CD303+ lymphoid/plasmacytoid dendritic cells, and CD1c+ myeloid dendritic cells.
“Under a normal light microscope, these immune cells essentially all look identical,” Dr Powis said. “With this new method, we can identify key cell types without any labeling.”
“Our next goal is to make a full catalogue of all the normal cell types of the immune system that can be detected in the bloodstream. Once we have this completed, we can then collaborate with our clinical colleagues to start identifying when these immune cells are altered, in conditions such as leukemia and lymphoma, potentially providing a rapid detection system from just a small blood sample.”

Photo by Graham Colm
A new method for identifying immune cells could pave the way for rapid detection of hematologic malignancies from a small blood sample, according to researchers.
The team found they could use wavelength modulated Raman spectroscopy (WMRS) to identify subsets of T cells, natural killer cells, and dendritic cells.
Traditional methods of identifying these cells usually involve labeling them with fluorescent or magnetically labeled antibodies.
Using WMRS, the researchers were able to identify immune cells with no labeling at all, thus permitting rapid identification and further analysis to take place with no potential alteration to the cells.
Simon Powis, PhD, of the University of St Andrews in Fife, Scotland, and his colleagues described this work in PLOS ONE.
Raman scattering refers to light scattering from molecules in a sample where the light energy can be shifted up or down and recorded as a “molecular fingerprint” that can be used for identification. Normally, this process is very weak and further hampered by other background light (eg, fluorescence).
WMRS subtly changes the incident laser light that, in turn, results in a modulation of the Raman signal, allowing it to be extracted from any (stationary) interfering signal.
Using WMRS, Dr Powis and his colleagues found they could identify CD4+ T cells, CD8+ T cells, CD56+ natural killer cells, CD303+ lymphoid/plasmacytoid dendritic cells, and CD1c+ myeloid dendritic cells.
“Under a normal light microscope, these immune cells essentially all look identical,” Dr Powis said. “With this new method, we can identify key cell types without any labeling.”
“Our next goal is to make a full catalogue of all the normal cell types of the immune system that can be detected in the bloodstream. Once we have this completed, we can then collaborate with our clinical colleagues to start identifying when these immune cells are altered, in conditions such as leukemia and lymphoma, potentially providing a rapid detection system from just a small blood sample.”