User login
Drug appears feasible for hard-to-treat myelofibrosis
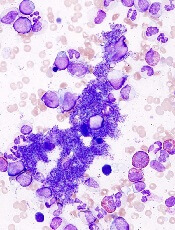
myelofibrosis
Results of a phase 2 study suggest the JAK2/FLT3 inhibitor pacritinib is a feasible treatment option for patients with myelofibrosis who cannot receive or do not respond well to standard therapies.
The drug reduced patients’ spleen volume and improved disease-related symptoms without causing clinically significant myelosuppression.
And pacritinib was considered well-tolerated, even in patients with disease-related anemia and thrombocytopenia.
“Currently, myelofibrosis patients with anemia and thrombocytopenia have limited treatment options for splenomegaly and constitutional symptoms, and
these data show that pacritinib has potential to help patients that are sub-optimally managed on currently available treatments,” said study author Rami S. Komrokji, MD, of the Moffitt Cancer Center in Tampa, Florida.
Dr Komrokji and his colleagues reported these results in Blood. The study was sponsored by CTI Biopharma, the company developing pacritinib.
The researchers evaluated the safety and efficacy of pacritinib in myelofibrosis patients who had clinical splenomegaly that was poorly controlled with standard therapies or who were newly diagnosed with intermediate- or high-risk disease and not considered candidates for standard therapy.
Patients were allowed to enroll irrespective of their degree of thrombocytopenia or anemia. At study entry, 40% of patients had hemoglobin levels below 10 g/dL, and 43% had platelet counts less than 100,000/µL.
A total of 35 patients were enrolled and treated with pacritinib administered at 400 mg once daily in 28-day cycles. The patients’ median age was 69 years.
The primary endpoint was assessment of the spleen response rate, defined as the proportion of subjects achieving 35% or greater reduction in spleen volume from baseline up to week 24, measured by MRI or CT.
A secondary endpoint was the proportion of patients with a 50% or greater reduction in spleen size as determined by physical exam.
The researchers also assessed the proportion of patients with a 50% or greater reduction in total symptom score, which included symptoms of abdominal pain,
bone pain, early satiety, fatigue, inactivity, night sweats, and pruritus, from baseline up to week 24.
Results showed that 30.8% of the evaluable patients (8/26) had a 35% or greater reduction in spleen volume by CT or MRI scan, with 42% of patients reaching a
35% or greater reduction by the end of treatment.
In addition, 42.4% of evaluable patients (14/33) achieved a 50% or greater reduction in spleen size by physical exam. And 48.4% of evaluable patients (15/31) achieved a 50% or greater reduction in total symptom score.
The most common treatment-emergent adverse events were grade 1-2 diarrhea (69%) and nausea (49%). Anemia and thrombocytopenia adverse events were reported in 12 (34.3%) and 8 (22.9%) patients, respectively.
Nine patients (26%) stopped taking pacritinib due to adverse events, but 3 of the events were deemed unrelated to the drug.
There were 5 deaths, 3 of which were due to serious adverse events. Of those, 1 (subdural hematoma) was considered possibly related to pacritinib treatment.
![]()
myelofibrosis
Results of a phase 2 study suggest the JAK2/FLT3 inhibitor pacritinib is a feasible treatment option for patients with myelofibrosis who cannot receive or do not respond well to standard therapies.
The drug reduced patients’ spleen volume and improved disease-related symptoms without causing clinically significant myelosuppression.
And pacritinib was considered well-tolerated, even in patients with disease-related anemia and thrombocytopenia.
“Currently, myelofibrosis patients with anemia and thrombocytopenia have limited treatment options for splenomegaly and constitutional symptoms, and
these data show that pacritinib has potential to help patients that are sub-optimally managed on currently available treatments,” said study author Rami S. Komrokji, MD, of the Moffitt Cancer Center in Tampa, Florida.
Dr Komrokji and his colleagues reported these results in Blood. The study was sponsored by CTI Biopharma, the company developing pacritinib.
The researchers evaluated the safety and efficacy of pacritinib in myelofibrosis patients who had clinical splenomegaly that was poorly controlled with standard therapies or who were newly diagnosed with intermediate- or high-risk disease and not considered candidates for standard therapy.
Patients were allowed to enroll irrespective of their degree of thrombocytopenia or anemia. At study entry, 40% of patients had hemoglobin levels below 10 g/dL, and 43% had platelet counts less than 100,000/µL.
A total of 35 patients were enrolled and treated with pacritinib administered at 400 mg once daily in 28-day cycles. The patients’ median age was 69 years.
The primary endpoint was assessment of the spleen response rate, defined as the proportion of subjects achieving 35% or greater reduction in spleen volume from baseline up to week 24, measured by MRI or CT.
A secondary endpoint was the proportion of patients with a 50% or greater reduction in spleen size as determined by physical exam.
The researchers also assessed the proportion of patients with a 50% or greater reduction in total symptom score, which included symptoms of abdominal pain,
bone pain, early satiety, fatigue, inactivity, night sweats, and pruritus, from baseline up to week 24.
Results showed that 30.8% of the evaluable patients (8/26) had a 35% or greater reduction in spleen volume by CT or MRI scan, with 42% of patients reaching a
35% or greater reduction by the end of treatment.
In addition, 42.4% of evaluable patients (14/33) achieved a 50% or greater reduction in spleen size by physical exam. And 48.4% of evaluable patients (15/31) achieved a 50% or greater reduction in total symptom score.
The most common treatment-emergent adverse events were grade 1-2 diarrhea (69%) and nausea (49%). Anemia and thrombocytopenia adverse events were reported in 12 (34.3%) and 8 (22.9%) patients, respectively.
Nine patients (26%) stopped taking pacritinib due to adverse events, but 3 of the events were deemed unrelated to the drug.
There were 5 deaths, 3 of which were due to serious adverse events. Of those, 1 (subdural hematoma) was considered possibly related to pacritinib treatment.
![]()
myelofibrosis
Results of a phase 2 study suggest the JAK2/FLT3 inhibitor pacritinib is a feasible treatment option for patients with myelofibrosis who cannot receive or do not respond well to standard therapies.
The drug reduced patients’ spleen volume and improved disease-related symptoms without causing clinically significant myelosuppression.
And pacritinib was considered well-tolerated, even in patients with disease-related anemia and thrombocytopenia.
“Currently, myelofibrosis patients with anemia and thrombocytopenia have limited treatment options for splenomegaly and constitutional symptoms, and
these data show that pacritinib has potential to help patients that are sub-optimally managed on currently available treatments,” said study author Rami S. Komrokji, MD, of the Moffitt Cancer Center in Tampa, Florida.
Dr Komrokji and his colleagues reported these results in Blood. The study was sponsored by CTI Biopharma, the company developing pacritinib.
The researchers evaluated the safety and efficacy of pacritinib in myelofibrosis patients who had clinical splenomegaly that was poorly controlled with standard therapies or who were newly diagnosed with intermediate- or high-risk disease and not considered candidates for standard therapy.
Patients were allowed to enroll irrespective of their degree of thrombocytopenia or anemia. At study entry, 40% of patients had hemoglobin levels below 10 g/dL, and 43% had platelet counts less than 100,000/µL.
A total of 35 patients were enrolled and treated with pacritinib administered at 400 mg once daily in 28-day cycles. The patients’ median age was 69 years.
The primary endpoint was assessment of the spleen response rate, defined as the proportion of subjects achieving 35% or greater reduction in spleen volume from baseline up to week 24, measured by MRI or CT.
A secondary endpoint was the proportion of patients with a 50% or greater reduction in spleen size as determined by physical exam.
The researchers also assessed the proportion of patients with a 50% or greater reduction in total symptom score, which included symptoms of abdominal pain,
bone pain, early satiety, fatigue, inactivity, night sweats, and pruritus, from baseline up to week 24.
Results showed that 30.8% of the evaluable patients (8/26) had a 35% or greater reduction in spleen volume by CT or MRI scan, with 42% of patients reaching a
35% or greater reduction by the end of treatment.
In addition, 42.4% of evaluable patients (14/33) achieved a 50% or greater reduction in spleen size by physical exam. And 48.4% of evaluable patients (15/31) achieved a 50% or greater reduction in total symptom score.
The most common treatment-emergent adverse events were grade 1-2 diarrhea (69%) and nausea (49%). Anemia and thrombocytopenia adverse events were reported in 12 (34.3%) and 8 (22.9%) patients, respectively.
Nine patients (26%) stopped taking pacritinib due to adverse events, but 3 of the events were deemed unrelated to the drug.
There were 5 deaths, 3 of which were due to serious adverse events. Of those, 1 (subdural hematoma) was considered possibly related to pacritinib treatment.
![]()
EC approves drug for polycythemia vera

Image courtesy of AFIP
The European Commission (EC) has approved ruxolitinib (Jakavi) to treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
This is the first targeted treatment the EC has approved for these patients.
The approval applies to all 28 member states of the European Union (EU), plus Iceland, Norway, and Liechtenstein.
Ruxolitinib is already approved to treat PV in the US, and additional regulatory applications for ruxolitinib in PV are ongoing worldwide.
The drug is also approved to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF in more than 70 countries, including EU member states and the US.
“The European Commission’s approval of Jakavi [for PV] is encouraging news for patients,” said Claire Harrison, MD, a consultant hematologist at Guy’s and St Thomas’ NHS Foundation Trust in London, England.
“Jakavi will fill an unmet need as the first treatment shown to significantly improve hematocrit, as well as symptom control and reduce spleen size in patients with polycythemia vera resistant to or intolerant of hydroxyurea.”
RESPONSE trial
The EC’s approval is based on data from the phase 3 RESPONSE trial. The study included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had splenomegaly.
Patients were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study’s primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
Twenty-one percent of ruxolitinib-treated patients met this endpoint (achieving hematocrit control and spleen reduction), compared to 1% of patients who received BAT (P<0.001).
And the researchers said ruxolitinib was well-tolerated. Common adverse events included headache, diarrhea, and fatigue.
Grade 3/4 anemia, grade 3/4 thrombocytopenia, and herpes zoster infections of all grades were more common in the ruxolitinib arm than the BAT arm. But thromboembolic events were more common with BAT than ruxolitinib.
This trial was funded by the Incyte Corporation, which markets ruxolitinib in the US. Novartis licensed ruxolitinib from Incyte for development and commercialization outside the US.
For more details on ruxolitinib, see the full prescribing information, available at www.jakavi.com. ![]()

Image courtesy of AFIP
The European Commission (EC) has approved ruxolitinib (Jakavi) to treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
This is the first targeted treatment the EC has approved for these patients.
The approval applies to all 28 member states of the European Union (EU), plus Iceland, Norway, and Liechtenstein.
Ruxolitinib is already approved to treat PV in the US, and additional regulatory applications for ruxolitinib in PV are ongoing worldwide.
The drug is also approved to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF in more than 70 countries, including EU member states and the US.
“The European Commission’s approval of Jakavi [for PV] is encouraging news for patients,” said Claire Harrison, MD, a consultant hematologist at Guy’s and St Thomas’ NHS Foundation Trust in London, England.
“Jakavi will fill an unmet need as the first treatment shown to significantly improve hematocrit, as well as symptom control and reduce spleen size in patients with polycythemia vera resistant to or intolerant of hydroxyurea.”
RESPONSE trial
The EC’s approval is based on data from the phase 3 RESPONSE trial. The study included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had splenomegaly.
Patients were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study’s primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
Twenty-one percent of ruxolitinib-treated patients met this endpoint (achieving hematocrit control and spleen reduction), compared to 1% of patients who received BAT (P<0.001).
And the researchers said ruxolitinib was well-tolerated. Common adverse events included headache, diarrhea, and fatigue.
Grade 3/4 anemia, grade 3/4 thrombocytopenia, and herpes zoster infections of all grades were more common in the ruxolitinib arm than the BAT arm. But thromboembolic events were more common with BAT than ruxolitinib.
This trial was funded by the Incyte Corporation, which markets ruxolitinib in the US. Novartis licensed ruxolitinib from Incyte for development and commercialization outside the US.
For more details on ruxolitinib, see the full prescribing information, available at www.jakavi.com. ![]()

Image courtesy of AFIP
The European Commission (EC) has approved ruxolitinib (Jakavi) to treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
This is the first targeted treatment the EC has approved for these patients.
The approval applies to all 28 member states of the European Union (EU), plus Iceland, Norway, and Liechtenstein.
Ruxolitinib is already approved to treat PV in the US, and additional regulatory applications for ruxolitinib in PV are ongoing worldwide.
The drug is also approved to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF in more than 70 countries, including EU member states and the US.
“The European Commission’s approval of Jakavi [for PV] is encouraging news for patients,” said Claire Harrison, MD, a consultant hematologist at Guy’s and St Thomas’ NHS Foundation Trust in London, England.
“Jakavi will fill an unmet need as the first treatment shown to significantly improve hematocrit, as well as symptom control and reduce spleen size in patients with polycythemia vera resistant to or intolerant of hydroxyurea.”
RESPONSE trial
The EC’s approval is based on data from the phase 3 RESPONSE trial. The study included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had splenomegaly.
Patients were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study’s primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
Twenty-one percent of ruxolitinib-treated patients met this endpoint (achieving hematocrit control and spleen reduction), compared to 1% of patients who received BAT (P<0.001).
And the researchers said ruxolitinib was well-tolerated. Common adverse events included headache, diarrhea, and fatigue.
Grade 3/4 anemia, grade 3/4 thrombocytopenia, and herpes zoster infections of all grades were more common in the ruxolitinib arm than the BAT arm. But thromboembolic events were more common with BAT than ruxolitinib.
This trial was funded by the Incyte Corporation, which markets ruxolitinib in the US. Novartis licensed ruxolitinib from Incyte for development and commercialization outside the US.
For more details on ruxolitinib, see the full prescribing information, available at www.jakavi.com. ![]()
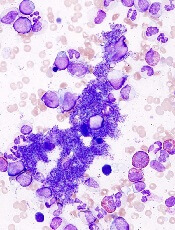
Inhibitor outperforms BAT in myelofibrosis trial

Image by Peter Anderson
Results of a phase 3 trial suggest the JAK2/FLT3 inhibitor pacritinib may be more effective for patients with myelofibrosis (MF) than best available therapy (BAT), excluding JAK inhibitors.
Patients who received pacritinib were more likely than those who received BAT to see a reduction in spleen volume and to become transfusion-independent,
regardless of their platelet counts.
In fact, pacritinib proved particularly effective among patients with severe thrombocytopenia.
CTI Biopharma and Baxter International, Inc., the companies developing pacritinib, announced these results from the PERSIST-1 trial yesterday.
“Despite the introduction of JAK2 inhibitors as effective therapies for patients with myelofibrosis, there remains a treatment gap for patients with disease-related or treatment-emergent thrombocytopenia,” said study investigator Claire Harrison, MD, of Guy’s Hospital in London, UK.
“The currently approved drug [ruxolitinib] may require dose titration to less effective doses in this patient population, thus limiting our ability to effectively treat them. Results from the PERSIST-1 randomized trial demonstrate that pacritinib could address this unmet medical need.”
PERSIST-1 is a randomized (2:1), phase 3 trial comparing the safety and efficacy of pacritinib to BAT, other than JAK inhibitors. Investigators enrolled 327 patients with primary and secondary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The study’s primary endpoint was the proportion of patients achieving a 35% or greater reduction in spleen volume from baseline to week 24, as measured by MRI or CT, when compared with BAT. Once patients completed 24 weeks of treatment, or if their disease progressed, they could cross over from the BAT arm to the pacritinib arm.
Investigators found that PERSIST-1 met its primary endpoint in the intent-to-treat population. Pacritinib produced a significantly better rate of spleen volume reduction (P=0.0003) when compared to BAT.
The same was true among patients with platelet counts of less than 100,000/μL and less than 50,000/μL, both subgroups that were stratified at randomization.
The magnitude of treatment effect was consistent with previously reported phase 2 results, with the greatest reduction observed among the sickest patients (platelet counts <50,000/μL).
Fifty patients were transfusion-dependent at study entry (receiving ≥ 6 units of red blood cells over 90 days pre-entry). And, compared to BAT, pacritinib resulted in a clinically meaningful percentage of patients becoming transfusion-independent.
Ultimately, 79% of patients in the BAT arm crossed over to the pacritinib arm.
Investigators said the safety profile in the PERSIST-1 trial was consistent with prior phase 2 trials, as the most common treatment-emergent adverse events were diarrhea, nausea, and vomiting. However, the incidence of grade 3 events was lower than previously observed in phase 2 trials. And no grade 4 gastrointestinal adverse events were reported.
Three patients discontinued treatment with pacritinib, and 9 required dose reductions for diarrhea. A preliminary analysis suggested that few patients discontinued pacritinib or required a dose reduction due to treatment-related anemia or thrombocytopenia.
Additional data from ongoing analyses will be submitted for presentation at an upcoming scientific meeting, according to Baxter and CTI Biopharma. ![]()

Image by Peter Anderson
Results of a phase 3 trial suggest the JAK2/FLT3 inhibitor pacritinib may be more effective for patients with myelofibrosis (MF) than best available therapy (BAT), excluding JAK inhibitors.
Patients who received pacritinib were more likely than those who received BAT to see a reduction in spleen volume and to become transfusion-independent,
regardless of their platelet counts.
In fact, pacritinib proved particularly effective among patients with severe thrombocytopenia.
CTI Biopharma and Baxter International, Inc., the companies developing pacritinib, announced these results from the PERSIST-1 trial yesterday.
“Despite the introduction of JAK2 inhibitors as effective therapies for patients with myelofibrosis, there remains a treatment gap for patients with disease-related or treatment-emergent thrombocytopenia,” said study investigator Claire Harrison, MD, of Guy’s Hospital in London, UK.
“The currently approved drug [ruxolitinib] may require dose titration to less effective doses in this patient population, thus limiting our ability to effectively treat them. Results from the PERSIST-1 randomized trial demonstrate that pacritinib could address this unmet medical need.”
PERSIST-1 is a randomized (2:1), phase 3 trial comparing the safety and efficacy of pacritinib to BAT, other than JAK inhibitors. Investigators enrolled 327 patients with primary and secondary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The study’s primary endpoint was the proportion of patients achieving a 35% or greater reduction in spleen volume from baseline to week 24, as measured by MRI or CT, when compared with BAT. Once patients completed 24 weeks of treatment, or if their disease progressed, they could cross over from the BAT arm to the pacritinib arm.
Investigators found that PERSIST-1 met its primary endpoint in the intent-to-treat population. Pacritinib produced a significantly better rate of spleen volume reduction (P=0.0003) when compared to BAT.
The same was true among patients with platelet counts of less than 100,000/μL and less than 50,000/μL, both subgroups that were stratified at randomization.
The magnitude of treatment effect was consistent with previously reported phase 2 results, with the greatest reduction observed among the sickest patients (platelet counts <50,000/μL).
Fifty patients were transfusion-dependent at study entry (receiving ≥ 6 units of red blood cells over 90 days pre-entry). And, compared to BAT, pacritinib resulted in a clinically meaningful percentage of patients becoming transfusion-independent.
Ultimately, 79% of patients in the BAT arm crossed over to the pacritinib arm.
Investigators said the safety profile in the PERSIST-1 trial was consistent with prior phase 2 trials, as the most common treatment-emergent adverse events were diarrhea, nausea, and vomiting. However, the incidence of grade 3 events was lower than previously observed in phase 2 trials. And no grade 4 gastrointestinal adverse events were reported.
Three patients discontinued treatment with pacritinib, and 9 required dose reductions for diarrhea. A preliminary analysis suggested that few patients discontinued pacritinib or required a dose reduction due to treatment-related anemia or thrombocytopenia.
Additional data from ongoing analyses will be submitted for presentation at an upcoming scientific meeting, according to Baxter and CTI Biopharma. ![]()

Image by Peter Anderson
Results of a phase 3 trial suggest the JAK2/FLT3 inhibitor pacritinib may be more effective for patients with myelofibrosis (MF) than best available therapy (BAT), excluding JAK inhibitors.
Patients who received pacritinib were more likely than those who received BAT to see a reduction in spleen volume and to become transfusion-independent,
regardless of their platelet counts.
In fact, pacritinib proved particularly effective among patients with severe thrombocytopenia.
CTI Biopharma and Baxter International, Inc., the companies developing pacritinib, announced these results from the PERSIST-1 trial yesterday.
“Despite the introduction of JAK2 inhibitors as effective therapies for patients with myelofibrosis, there remains a treatment gap for patients with disease-related or treatment-emergent thrombocytopenia,” said study investigator Claire Harrison, MD, of Guy’s Hospital in London, UK.
“The currently approved drug [ruxolitinib] may require dose titration to less effective doses in this patient population, thus limiting our ability to effectively treat them. Results from the PERSIST-1 randomized trial demonstrate that pacritinib could address this unmet medical need.”
PERSIST-1 is a randomized (2:1), phase 3 trial comparing the safety and efficacy of pacritinib to BAT, other than JAK inhibitors. Investigators enrolled 327 patients with primary and secondary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The study’s primary endpoint was the proportion of patients achieving a 35% or greater reduction in spleen volume from baseline to week 24, as measured by MRI or CT, when compared with BAT. Once patients completed 24 weeks of treatment, or if their disease progressed, they could cross over from the BAT arm to the pacritinib arm.
Investigators found that PERSIST-1 met its primary endpoint in the intent-to-treat population. Pacritinib produced a significantly better rate of spleen volume reduction (P=0.0003) when compared to BAT.
The same was true among patients with platelet counts of less than 100,000/μL and less than 50,000/μL, both subgroups that were stratified at randomization.
The magnitude of treatment effect was consistent with previously reported phase 2 results, with the greatest reduction observed among the sickest patients (platelet counts <50,000/μL).
Fifty patients were transfusion-dependent at study entry (receiving ≥ 6 units of red blood cells over 90 days pre-entry). And, compared to BAT, pacritinib resulted in a clinically meaningful percentage of patients becoming transfusion-independent.
Ultimately, 79% of patients in the BAT arm crossed over to the pacritinib arm.
Investigators said the safety profile in the PERSIST-1 trial was consistent with prior phase 2 trials, as the most common treatment-emergent adverse events were diarrhea, nausea, and vomiting. However, the incidence of grade 3 events was lower than previously observed in phase 2 trials. And no grade 4 gastrointestinal adverse events were reported.
Three patients discontinued treatment with pacritinib, and 9 required dose reductions for diarrhea. A preliminary analysis suggested that few patients discontinued pacritinib or required a dose reduction due to treatment-related anemia or thrombocytopenia.
Additional data from ongoing analyses will be submitted for presentation at an upcoming scientific meeting, according to Baxter and CTI Biopharma. ![]()
Order of mutations impacts MPN behavior
essential thrombocythemia
The order in which genetic mutations are acquired determines how myeloproliferative neoplasms (MPNs) behave, according to research published in NEJM.
Investigators found that mutation order impacts everything from the type of MPN a patient develops to how the disease responds to treatment.
“This surprising finding could help us offer more accurate prognoses to MPN patients based on their mutation order and tailor potential therapies towards them,” said study author David Kent, PhD, of the University of Cambridge in the UK.
“For example, our results predict that targeted JAK2 therapy would be more effective in patients with one mutation order but not the other.”
To uncover this finding, Dr Kent and his colleagues screened 246 MPN patients for mutations in JAK2 and TET2. By studying patients who carried both mutations, the team was able to determine which mutation came first and study the effect of mutation order on the behavior of hematopoietic stem cells.
The investigators found that patients who acquired mutations in JAK2 prior to those in TET2 displayed aberrant blood counts more than a decade earlier.
These patients were more likely to present with polycythemia vera than with essential thrombocythemia, and they were more likely to develop thromboses.
At the same time, JAK2-mutant progenitors from these patients exhibited increased sensitivity to the JAK1/2 inhibitor ruxolitinib in vitro.
“This is the first time that mutation order has been shown to affect any cancer, and it is likely that this phenomenon occurs in many types of malignancy,” said study author Tony Green, MD, PhD, of the University of Cambridge.
“These results show how the study of MPNs provides unparalleled access to the earliest stages of tumor development (inaccessible in other cancers, which usually cannot be detected until many mutations have accumulated). This should give us powerful insights into the origins of cancer.” ![]()
essential thrombocythemia
The order in which genetic mutations are acquired determines how myeloproliferative neoplasms (MPNs) behave, according to research published in NEJM.
Investigators found that mutation order impacts everything from the type of MPN a patient develops to how the disease responds to treatment.
“This surprising finding could help us offer more accurate prognoses to MPN patients based on their mutation order and tailor potential therapies towards them,” said study author David Kent, PhD, of the University of Cambridge in the UK.
“For example, our results predict that targeted JAK2 therapy would be more effective in patients with one mutation order but not the other.”
To uncover this finding, Dr Kent and his colleagues screened 246 MPN patients for mutations in JAK2 and TET2. By studying patients who carried both mutations, the team was able to determine which mutation came first and study the effect of mutation order on the behavior of hematopoietic stem cells.
The investigators found that patients who acquired mutations in JAK2 prior to those in TET2 displayed aberrant blood counts more than a decade earlier.
These patients were more likely to present with polycythemia vera than with essential thrombocythemia, and they were more likely to develop thromboses.
At the same time, JAK2-mutant progenitors from these patients exhibited increased sensitivity to the JAK1/2 inhibitor ruxolitinib in vitro.
“This is the first time that mutation order has been shown to affect any cancer, and it is likely that this phenomenon occurs in many types of malignancy,” said study author Tony Green, MD, PhD, of the University of Cambridge.
“These results show how the study of MPNs provides unparalleled access to the earliest stages of tumor development (inaccessible in other cancers, which usually cannot be detected until many mutations have accumulated). This should give us powerful insights into the origins of cancer.” ![]()
essential thrombocythemia
The order in which genetic mutations are acquired determines how myeloproliferative neoplasms (MPNs) behave, according to research published in NEJM.
Investigators found that mutation order impacts everything from the type of MPN a patient develops to how the disease responds to treatment.
“This surprising finding could help us offer more accurate prognoses to MPN patients based on their mutation order and tailor potential therapies towards them,” said study author David Kent, PhD, of the University of Cambridge in the UK.
“For example, our results predict that targeted JAK2 therapy would be more effective in patients with one mutation order but not the other.”
To uncover this finding, Dr Kent and his colleagues screened 246 MPN patients for mutations in JAK2 and TET2. By studying patients who carried both mutations, the team was able to determine which mutation came first and study the effect of mutation order on the behavior of hematopoietic stem cells.
The investigators found that patients who acquired mutations in JAK2 prior to those in TET2 displayed aberrant blood counts more than a decade earlier.
These patients were more likely to present with polycythemia vera than with essential thrombocythemia, and they were more likely to develop thromboses.
At the same time, JAK2-mutant progenitors from these patients exhibited increased sensitivity to the JAK1/2 inhibitor ruxolitinib in vitro.
“This is the first time that mutation order has been shown to affect any cancer, and it is likely that this phenomenon occurs in many types of malignancy,” said study author Tony Green, MD, PhD, of the University of Cambridge.
“These results show how the study of MPNs provides unparalleled access to the earliest stages of tumor development (inaccessible in other cancers, which usually cannot be detected until many mutations have accumulated). This should give us powerful insights into the origins of cancer.” ![]()
Ruxolitinib bests standard treatment for PV
The JAK1/2 inhibitor ruxolitinib can outperform standard therapy in patients with polycythemia vera (PV), results of the RESPONSE trial suggest.
In patients who could not tolerate or were resistant to hydroxyurea, ruxolitinib proved superior to standard therapy for controlling hematocrit levels and reducing spleen volume
“This study indicates that ruxolitinib may represent an important advance for this population of patients with PV,” said Alessandro M. Vannucchi, MD, of the University of Florence in Italy.
Dr Vannucchi and his colleagues reported these findings in NEJM. The trial was funded by Incyte Corporation, the company developing ruxolitinib.
The phase 3 study included 222 patients. They were phlebotomy-dependent, had splenomegaly, and could not tolerate or were resistant to hydroxyurea.
The patients were randomized 1:1 to receive either ruxolitinib (starting dose of 10 mg twice daily) or standard therapy, which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the study.
The primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
So 21% of patients in the ruxolitinib group met the primary endpoint, achieving both hematocrit control and spleen reduction. But only 1% of patients in the standard-therapy group did the same (P<0.001).
In all, 60% of patients in the ruxolitinib arm achieved hematocrit control, compared to 20% of those receiving standard therapy. And 38% of patients in the ruxolitinib arm had at least a 35% spleen reduction, compared to 1% of patients in the standard-therapy arm.
The rate of complete hematologic remission was significantly higher in the ruxolitinib group than in the standard-therapy group, at 24% and 9%, respectively (P=0.003).
And ruxolitinib-treated patients had a greater reduction in overall symptoms. Forty-nine percent of ruxolitinib-treated patients had at least a 50% reduction in their total symptom score at week 32 (as measured by the MPN-SAF 14-item total symptom score), compared to 5% of patients on standard therapy.
Based on these results, most patients in the standard-therapy arm crossed over to receive ruxolitinib immediately after week 32. So the researchers could only compare rates of adverse events through week 32.
They found that grade 3/4 anemia was more common with ruxolitinib than with standard therapy (2% and 0%, respectively). The same was true of grade 3/4 thrombocytopenia (5% and 4%, respectively) and herpes zoster infections of all grades (6% and 0%, respectively).
However, thromboembolic events were more common with standard therapy. They occurred in 6 patients who received standard therapy and 1 ruxolitinib-treated patient.
The most common non-hematologic adverse events in the ruxolitinib arm were headache (16%), diarrhea (15%), and fatigue (15%), which were mainly grade 1 or 2. The rates of these events in the standard therapy arm were 19%, 7%, and 15%, respectively.
The researchers also noted that nearly 85% of patients randomized to ruxolitinib were still receiving treatment at a median follow-up of 81 weeks. ![]()
The JAK1/2 inhibitor ruxolitinib can outperform standard therapy in patients with polycythemia vera (PV), results of the RESPONSE trial suggest.
In patients who could not tolerate or were resistant to hydroxyurea, ruxolitinib proved superior to standard therapy for controlling hematocrit levels and reducing spleen volume
“This study indicates that ruxolitinib may represent an important advance for this population of patients with PV,” said Alessandro M. Vannucchi, MD, of the University of Florence in Italy.
Dr Vannucchi and his colleagues reported these findings in NEJM. The trial was funded by Incyte Corporation, the company developing ruxolitinib.
The phase 3 study included 222 patients. They were phlebotomy-dependent, had splenomegaly, and could not tolerate or were resistant to hydroxyurea.
The patients were randomized 1:1 to receive either ruxolitinib (starting dose of 10 mg twice daily) or standard therapy, which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the study.
The primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
So 21% of patients in the ruxolitinib group met the primary endpoint, achieving both hematocrit control and spleen reduction. But only 1% of patients in the standard-therapy group did the same (P<0.001).
In all, 60% of patients in the ruxolitinib arm achieved hematocrit control, compared to 20% of those receiving standard therapy. And 38% of patients in the ruxolitinib arm had at least a 35% spleen reduction, compared to 1% of patients in the standard-therapy arm.
The rate of complete hematologic remission was significantly higher in the ruxolitinib group than in the standard-therapy group, at 24% and 9%, respectively (P=0.003).
And ruxolitinib-treated patients had a greater reduction in overall symptoms. Forty-nine percent of ruxolitinib-treated patients had at least a 50% reduction in their total symptom score at week 32 (as measured by the MPN-SAF 14-item total symptom score), compared to 5% of patients on standard therapy.
Based on these results, most patients in the standard-therapy arm crossed over to receive ruxolitinib immediately after week 32. So the researchers could only compare rates of adverse events through week 32.
They found that grade 3/4 anemia was more common with ruxolitinib than with standard therapy (2% and 0%, respectively). The same was true of grade 3/4 thrombocytopenia (5% and 4%, respectively) and herpes zoster infections of all grades (6% and 0%, respectively).
However, thromboembolic events were more common with standard therapy. They occurred in 6 patients who received standard therapy and 1 ruxolitinib-treated patient.
The most common non-hematologic adverse events in the ruxolitinib arm were headache (16%), diarrhea (15%), and fatigue (15%), which were mainly grade 1 or 2. The rates of these events in the standard therapy arm were 19%, 7%, and 15%, respectively.
The researchers also noted that nearly 85% of patients randomized to ruxolitinib were still receiving treatment at a median follow-up of 81 weeks. ![]()
The JAK1/2 inhibitor ruxolitinib can outperform standard therapy in patients with polycythemia vera (PV), results of the RESPONSE trial suggest.
In patients who could not tolerate or were resistant to hydroxyurea, ruxolitinib proved superior to standard therapy for controlling hematocrit levels and reducing spleen volume
“This study indicates that ruxolitinib may represent an important advance for this population of patients with PV,” said Alessandro M. Vannucchi, MD, of the University of Florence in Italy.
Dr Vannucchi and his colleagues reported these findings in NEJM. The trial was funded by Incyte Corporation, the company developing ruxolitinib.
The phase 3 study included 222 patients. They were phlebotomy-dependent, had splenomegaly, and could not tolerate or were resistant to hydroxyurea.
The patients were randomized 1:1 to receive either ruxolitinib (starting dose of 10 mg twice daily) or standard therapy, which was defined as investigator-selected monotherapy or observation only. The ruxolitinib dose was adjusted as needed throughout the study.
The primary endpoint was a composite of hematocrit control and spleen reduction. To meet the endpoint, patients had to experience a 35% or greater reduction in spleen volume from baseline, as assessed by imaging at week 32.
And a patient’s hematocrit was considered under control if he was not eligible for phlebotomy from week 8 through 32 (and had no more than one instance of phlebotomy eligibility between randomization and week 8). Patients who were deemed eligible for phlebotomy had hematocrit that was greater than 45% or had increased 3 or more percentage points from the time they entered the study.
So 21% of patients in the ruxolitinib group met the primary endpoint, achieving both hematocrit control and spleen reduction. But only 1% of patients in the standard-therapy group did the same (P<0.001).
In all, 60% of patients in the ruxolitinib arm achieved hematocrit control, compared to 20% of those receiving standard therapy. And 38% of patients in the ruxolitinib arm had at least a 35% spleen reduction, compared to 1% of patients in the standard-therapy arm.
The rate of complete hematologic remission was significantly higher in the ruxolitinib group than in the standard-therapy group, at 24% and 9%, respectively (P=0.003).
And ruxolitinib-treated patients had a greater reduction in overall symptoms. Forty-nine percent of ruxolitinib-treated patients had at least a 50% reduction in their total symptom score at week 32 (as measured by the MPN-SAF 14-item total symptom score), compared to 5% of patients on standard therapy.
Based on these results, most patients in the standard-therapy arm crossed over to receive ruxolitinib immediately after week 32. So the researchers could only compare rates of adverse events through week 32.
They found that grade 3/4 anemia was more common with ruxolitinib than with standard therapy (2% and 0%, respectively). The same was true of grade 3/4 thrombocytopenia (5% and 4%, respectively) and herpes zoster infections of all grades (6% and 0%, respectively).
However, thromboembolic events were more common with standard therapy. They occurred in 6 patients who received standard therapy and 1 ruxolitinib-treated patient.
The most common non-hematologic adverse events in the ruxolitinib arm were headache (16%), diarrhea (15%), and fatigue (15%), which were mainly grade 1 or 2. The rates of these events in the standard therapy arm were 19%, 7%, and 15%, respectively.
The researchers also noted that nearly 85% of patients randomized to ruxolitinib were still receiving treatment at a median follow-up of 81 weeks. ![]()
CHMP recommends ruxolitinib for PV

Credit: Zak Hubbard
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending the approval of ruxolitinib (Jakavi) to
treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
The European Commission generally follows the CHMP’s advice and delivers its final decision within 3 months of the CHMP recommendation.
If approved, ruxolitinib would be the first targeted treatment option for PV patients in Europe.
The European Commission’s decision will be applicable to all 28 member states of the European Union, plus Iceland, Norway, and Liechtenstein.
About ruxolitinib
Ruxolitinib is an oral inhibitor of the JAK 1 and JAK 2 tyrosine kinases. It was approved by the European Commission in August 2012 to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF. The drug is approved to treat MF in more than 70 countries.
Novartis licensed ruxolitinib from Incyte Corporation (which markets the drug as Jakafi in the US) for development and commercialization outside the US. Ruxolitinib is approved in the US to treat patients with MF and those with PV.
Ruxolitinib in PV: The RESPONSE trial
The CHMP’s recommendation to approve ruxolitinib for PV was based on results from the phase 3 RESPONSE trial, which was funded by Incyte.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had an enlarged spleen.
They were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common hematologic adverse events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles. ![]()

Credit: Zak Hubbard
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending the approval of ruxolitinib (Jakavi) to
treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
The European Commission generally follows the CHMP’s advice and delivers its final decision within 3 months of the CHMP recommendation.
If approved, ruxolitinib would be the first targeted treatment option for PV patients in Europe.
The European Commission’s decision will be applicable to all 28 member states of the European Union, plus Iceland, Norway, and Liechtenstein.
About ruxolitinib
Ruxolitinib is an oral inhibitor of the JAK 1 and JAK 2 tyrosine kinases. It was approved by the European Commission in August 2012 to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF. The drug is approved to treat MF in more than 70 countries.
Novartis licensed ruxolitinib from Incyte Corporation (which markets the drug as Jakafi in the US) for development and commercialization outside the US. Ruxolitinib is approved in the US to treat patients with MF and those with PV.
Ruxolitinib in PV: The RESPONSE trial
The CHMP’s recommendation to approve ruxolitinib for PV was based on results from the phase 3 RESPONSE trial, which was funded by Incyte.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had an enlarged spleen.
They were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common hematologic adverse events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles. ![]()

Credit: Zak Hubbard
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending the approval of ruxolitinib (Jakavi) to
treat adults with polycythemia vera (PV) who are resistant to or cannot tolerate hydroxyurea.
The European Commission generally follows the CHMP’s advice and delivers its final decision within 3 months of the CHMP recommendation.
If approved, ruxolitinib would be the first targeted treatment option for PV patients in Europe.
The European Commission’s decision will be applicable to all 28 member states of the European Union, plus Iceland, Norway, and Liechtenstein.
About ruxolitinib
Ruxolitinib is an oral inhibitor of the JAK 1 and JAK 2 tyrosine kinases. It was approved by the European Commission in August 2012 to treat adults with primary myelofibrosis (MF), post-PV MF, or post-essential thrombocythemia MF. The drug is approved to treat MF in more than 70 countries.
Novartis licensed ruxolitinib from Incyte Corporation (which markets the drug as Jakafi in the US) for development and commercialization outside the US. Ruxolitinib is approved in the US to treat patients with MF and those with PV.
Ruxolitinib in PV: The RESPONSE trial
The CHMP’s recommendation to approve ruxolitinib for PV was based on results from the phase 3 RESPONSE trial, which was funded by Incyte.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy, and had an enlarged spleen.
They were randomized to receive ruxolitinib starting at 10 mg twice daily or best available therapy (BAT) as determined by the investigator. The ruxolitinib dose was adjusted as needed.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common hematologic adverse events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles. ![]()
Iron overload aids potentially deadly bacteria
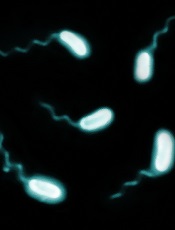
Credit: Paul A. Gulig
Researchers say they’ve determined why patients with hereditary hemochromatosis are so vulnerable to severe illness from Vibrio vulnificus infection.
Patients with hereditary hemochromatosis have a deficiency of the iron-regulating hormone hepcidin and therefore develop excess iron in their blood and tissue, providing prime growth conditions for Vibrio vulnificus.
The researchers also showed that minihepcidin, a medicinal form of the hormone hepcidin that lowers iron levels in blood, could cure the infection by restricting bacterial growth.
The findings appear in Cell Host and Microbe.
“This is the first time that the association of hepcidin deficiency and susceptibility to Vibrio vulnificus infection was tested,” said study author Yonca Bulut, MD, of the David Geffen School of Medicine at UCLA in Los Angeles.
“The dramatic effectiveness of the new treatment, even after the infection was established, was impressive.”
To conduct this study, Dr Bulut and her colleagues compared the fatality of Vibrio vulnificus infection in healthy mice with mice that lacked hepcidin, modeling human hereditary hemochromatosis.
The infection was much more lethal in hepcidin-deficient mice because their bodies could not decrease iron levels in the blood in response to infection, a process mediated by hepcidin in healthy mice.
Giving minihepcidin to hepcidin-deficient mice prevented infection if the hormone was given before Vibrio vulnificus was introduced. And mice given minihepcidin 3 hours after the bacterium was introduced were cured of any infection.
“We found that hepcidin is required for resistance to a Vibrio vulnificus infection,” said study author Joao Arezes, a graduate student from the University of Porto in Portugal.
“The development of the treatment tested in mouse models could reduce the high mortality rate of this disease.”
The next stage of this research is to investigate why Vibrio vulnificus bacteria become so lethal when iron levels are high, and to learn which other microbes respond similarly to excess iron. ![]()
Credit: Paul A. Gulig
Researchers say they’ve determined why patients with hereditary hemochromatosis are so vulnerable to severe illness from Vibrio vulnificus infection.
Patients with hereditary hemochromatosis have a deficiency of the iron-regulating hormone hepcidin and therefore develop excess iron in their blood and tissue, providing prime growth conditions for Vibrio vulnificus.
The researchers also showed that minihepcidin, a medicinal form of the hormone hepcidin that lowers iron levels in blood, could cure the infection by restricting bacterial growth.
The findings appear in Cell Host and Microbe.
“This is the first time that the association of hepcidin deficiency and susceptibility to Vibrio vulnificus infection was tested,” said study author Yonca Bulut, MD, of the David Geffen School of Medicine at UCLA in Los Angeles.
“The dramatic effectiveness of the new treatment, even after the infection was established, was impressive.”
To conduct this study, Dr Bulut and her colleagues compared the fatality of Vibrio vulnificus infection in healthy mice with mice that lacked hepcidin, modeling human hereditary hemochromatosis.
The infection was much more lethal in hepcidin-deficient mice because their bodies could not decrease iron levels in the blood in response to infection, a process mediated by hepcidin in healthy mice.
Giving minihepcidin to hepcidin-deficient mice prevented infection if the hormone was given before Vibrio vulnificus was introduced. And mice given minihepcidin 3 hours after the bacterium was introduced were cured of any infection.
“We found that hepcidin is required for resistance to a Vibrio vulnificus infection,” said study author Joao Arezes, a graduate student from the University of Porto in Portugal.
“The development of the treatment tested in mouse models could reduce the high mortality rate of this disease.”
The next stage of this research is to investigate why Vibrio vulnificus bacteria become so lethal when iron levels are high, and to learn which other microbes respond similarly to excess iron. ![]()
Credit: Paul A. Gulig
Researchers say they’ve determined why patients with hereditary hemochromatosis are so vulnerable to severe illness from Vibrio vulnificus infection.
Patients with hereditary hemochromatosis have a deficiency of the iron-regulating hormone hepcidin and therefore develop excess iron in their blood and tissue, providing prime growth conditions for Vibrio vulnificus.
The researchers also showed that minihepcidin, a medicinal form of the hormone hepcidin that lowers iron levels in blood, could cure the infection by restricting bacterial growth.
The findings appear in Cell Host and Microbe.
“This is the first time that the association of hepcidin deficiency and susceptibility to Vibrio vulnificus infection was tested,” said study author Yonca Bulut, MD, of the David Geffen School of Medicine at UCLA in Los Angeles.
“The dramatic effectiveness of the new treatment, even after the infection was established, was impressive.”
To conduct this study, Dr Bulut and her colleagues compared the fatality of Vibrio vulnificus infection in healthy mice with mice that lacked hepcidin, modeling human hereditary hemochromatosis.
The infection was much more lethal in hepcidin-deficient mice because their bodies could not decrease iron levels in the blood in response to infection, a process mediated by hepcidin in healthy mice.
Giving minihepcidin to hepcidin-deficient mice prevented infection if the hormone was given before Vibrio vulnificus was introduced. And mice given minihepcidin 3 hours after the bacterium was introduced were cured of any infection.
“We found that hepcidin is required for resistance to a Vibrio vulnificus infection,” said study author Joao Arezes, a graduate student from the University of Porto in Portugal.
“The development of the treatment tested in mouse models could reduce the high mortality rate of this disease.”
The next stage of this research is to investigate why Vibrio vulnificus bacteria become so lethal when iron levels are high, and to learn which other microbes respond similarly to excess iron.
CRISPR bests TALEN in iPSCs

Credit: Salk Institute
The gene-editing technology CRISPR can precisely and efficiently alter human stem cells, according to research published in Molecular Therapy.
Using JAK2 and other genes as models, researchers showed that CRISPR offers advantages over TALEN, another gene-editing technique, for manipulating induced pluripotent stem cells (iPSCs).
And, unlike in a previous study, CRISPR did not produce any off-target effects.
The team believes their findings could streamline and speed up efforts to modify human iPSCs for use as treatments or in the development of model systems to study diseases and test drugs.
“Stem cell technology is quickly advancing, and we think that the days when we can use iPSCs for human therapy aren’t that far away,” said study author Zhaohui Ye, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“This is one of the first studies to detail the use of CRISPR in human iPSCs, showcasing its potential in these cells.”
CRISPR originated from a microbial immune system that contains DNA segments known as “clustered regularly interspaced short palindromic repeats.” The system makes use of an enzyme that nicks together DNA with a piece of small RNA that guides the tool to where researchers want to introduce cuts or other changes in the genome.
Previous research has shown that CRISPR can generate genomic changes or mutations through these interventions more efficiently than other gene-editing techniques, such as TALEN, which is short for “transcription activator-like effector nuclease.”
Despite CRISPR’s advantages, a recent study suggested it might also produce a large number of off-target effects in human cancer cell lines; specifically, modification of genes that researchers didn’t mean to change.
To see if this unwanted effect occurred in other human cell types, Dr Ye and his colleagues pitted CRISPR against TALEN in human iPSCs. The researchers compared the ability of both techniques to either cut out pieces of known genes in iPSCs or cut out a piece of these genes and replace it with another.
As model genes, the researchers used JAK2, a gene that, when mutated, causes myeloproliferative neoplasms; SERPINA1, a gene that, when mutated, causes alpha1-antitrypsin deficiency, an inherited disorder that may cause lung and liver disease; and AAVS1, a gene that’s been recently discovered to be a “safe harbor” in the human genome for inserting foreign genes.
The comparison showed that, when simply cutting out portions of genes, the CRISPR system was significantly more efficient than TALEN in all 3 gene systems, inducing up to 100 times more cuts.
However, when using these genome-editing tools for replacing portions of the genes, such as the disease-causing mutations in JAK2 and SERPINA1 genes, CRISPR and TALEN showed about the same efficiency in patient-derived iPSCs.
Contrary to results of the human cancer cell line study, both CRISPR and TALEN had the same targeting specificity in human iPSCs, hitting only the genes they were designed to affect.
The researchers also found that the CRISPR system has a second advantage over TALEN. It can be designed to target only the mutation-containing gene without affecting the healthy gene in patients where only one copy of a gene is affected.
These findings, according to the researchers, offer reassurance that CRISPR will be a useful tool for editing the genes of human iPSCs with little risk of off-target effects.

Credit: Salk Institute
The gene-editing technology CRISPR can precisely and efficiently alter human stem cells, according to research published in Molecular Therapy.
Using JAK2 and other genes as models, researchers showed that CRISPR offers advantages over TALEN, another gene-editing technique, for manipulating induced pluripotent stem cells (iPSCs).
And, unlike in a previous study, CRISPR did not produce any off-target effects.
The team believes their findings could streamline and speed up efforts to modify human iPSCs for use as treatments or in the development of model systems to study diseases and test drugs.
“Stem cell technology is quickly advancing, and we think that the days when we can use iPSCs for human therapy aren’t that far away,” said study author Zhaohui Ye, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“This is one of the first studies to detail the use of CRISPR in human iPSCs, showcasing its potential in these cells.”
CRISPR originated from a microbial immune system that contains DNA segments known as “clustered regularly interspaced short palindromic repeats.” The system makes use of an enzyme that nicks together DNA with a piece of small RNA that guides the tool to where researchers want to introduce cuts or other changes in the genome.
Previous research has shown that CRISPR can generate genomic changes or mutations through these interventions more efficiently than other gene-editing techniques, such as TALEN, which is short for “transcription activator-like effector nuclease.”
Despite CRISPR’s advantages, a recent study suggested it might also produce a large number of off-target effects in human cancer cell lines; specifically, modification of genes that researchers didn’t mean to change.
To see if this unwanted effect occurred in other human cell types, Dr Ye and his colleagues pitted CRISPR against TALEN in human iPSCs. The researchers compared the ability of both techniques to either cut out pieces of known genes in iPSCs or cut out a piece of these genes and replace it with another.
As model genes, the researchers used JAK2, a gene that, when mutated, causes myeloproliferative neoplasms; SERPINA1, a gene that, when mutated, causes alpha1-antitrypsin deficiency, an inherited disorder that may cause lung and liver disease; and AAVS1, a gene that’s been recently discovered to be a “safe harbor” in the human genome for inserting foreign genes.
The comparison showed that, when simply cutting out portions of genes, the CRISPR system was significantly more efficient than TALEN in all 3 gene systems, inducing up to 100 times more cuts.
However, when using these genome-editing tools for replacing portions of the genes, such as the disease-causing mutations in JAK2 and SERPINA1 genes, CRISPR and TALEN showed about the same efficiency in patient-derived iPSCs.
Contrary to results of the human cancer cell line study, both CRISPR and TALEN had the same targeting specificity in human iPSCs, hitting only the genes they were designed to affect.
The researchers also found that the CRISPR system has a second advantage over TALEN. It can be designed to target only the mutation-containing gene without affecting the healthy gene in patients where only one copy of a gene is affected.
These findings, according to the researchers, offer reassurance that CRISPR will be a useful tool for editing the genes of human iPSCs with little risk of off-target effects.

Credit: Salk Institute
The gene-editing technology CRISPR can precisely and efficiently alter human stem cells, according to research published in Molecular Therapy.
Using JAK2 and other genes as models, researchers showed that CRISPR offers advantages over TALEN, another gene-editing technique, for manipulating induced pluripotent stem cells (iPSCs).
And, unlike in a previous study, CRISPR did not produce any off-target effects.
The team believes their findings could streamline and speed up efforts to modify human iPSCs for use as treatments or in the development of model systems to study diseases and test drugs.
“Stem cell technology is quickly advancing, and we think that the days when we can use iPSCs for human therapy aren’t that far away,” said study author Zhaohui Ye, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“This is one of the first studies to detail the use of CRISPR in human iPSCs, showcasing its potential in these cells.”
CRISPR originated from a microbial immune system that contains DNA segments known as “clustered regularly interspaced short palindromic repeats.” The system makes use of an enzyme that nicks together DNA with a piece of small RNA that guides the tool to where researchers want to introduce cuts or other changes in the genome.
Previous research has shown that CRISPR can generate genomic changes or mutations through these interventions more efficiently than other gene-editing techniques, such as TALEN, which is short for “transcription activator-like effector nuclease.”
Despite CRISPR’s advantages, a recent study suggested it might also produce a large number of off-target effects in human cancer cell lines; specifically, modification of genes that researchers didn’t mean to change.
To see if this unwanted effect occurred in other human cell types, Dr Ye and his colleagues pitted CRISPR against TALEN in human iPSCs. The researchers compared the ability of both techniques to either cut out pieces of known genes in iPSCs or cut out a piece of these genes and replace it with another.
As model genes, the researchers used JAK2, a gene that, when mutated, causes myeloproliferative neoplasms; SERPINA1, a gene that, when mutated, causes alpha1-antitrypsin deficiency, an inherited disorder that may cause lung and liver disease; and AAVS1, a gene that’s been recently discovered to be a “safe harbor” in the human genome for inserting foreign genes.
The comparison showed that, when simply cutting out portions of genes, the CRISPR system was significantly more efficient than TALEN in all 3 gene systems, inducing up to 100 times more cuts.
However, when using these genome-editing tools for replacing portions of the genes, such as the disease-causing mutations in JAK2 and SERPINA1 genes, CRISPR and TALEN showed about the same efficiency in patient-derived iPSCs.
Contrary to results of the human cancer cell line study, both CRISPR and TALEN had the same targeting specificity in human iPSCs, hitting only the genes they were designed to affect.
The researchers also found that the CRISPR system has a second advantage over TALEN. It can be designed to target only the mutation-containing gene without affecting the healthy gene in patients where only one copy of a gene is affected.
These findings, according to the researchers, offer reassurance that CRISPR will be a useful tool for editing the genes of human iPSCs with little risk of off-target effects.
Teams map paths to drug resistance in cancers, MPNs
Researchers say they’ve discovered key events that prompt drug resistance in myeloproliferative neoplasms (MPNs) and certain solid tumor malignancies.
By mapping the steps that myelofibrosis, melanoma, and breast cancer cells use to become resistant to drugs, the investigators believe they have identified better targets for blocking those pathways to ensure current therapies are effective.
The groups reported these findings in two papers published in Science Signaling.
“In our studies, we developed a screening technology that allows us to quickly identify the routes cells can use to become resistant, and, using that information, we were able to show that these mechanisms seen in the laboratory are actually also occurring in patients’ tumors,” said Kris Wood, PhD, an assistant professor at Duke University in Durham, North Carolina, and senior author of both studies.
In the first study, Dr Wood and his colleagues conducted a broad survey of the known cell-signaling pathways that, when activated, have the potential to trigger drug resistance.
Using this screening technology, the researchers were able to corroborate the results of earlier drug-resistance studies, while also finding pathways that had not previously been described.
The team identified the MAPK and PI3K pathways, which are known to mediate drug resistance. But they also found that activation of the Notch1 pathway caused drug resistance, and inhibiting Notch1 signaling restored drug efficacy.
“Interestingly, the mechanisms are quite similar among all 3 of the cancer types,” Dr Wood noted. “In breast cancer and melanoma, our findings suggest the same Notch1 pathway as a potential driver of resistance to a wide array of targeted therapies—a role that has not been widely acknowledged previously.”
The investigators found that Notch signaling mediated drug resistance to an estrogen receptor-targeted therapy used in breast cancer and to a kinase-targeted therapy used in melanoma. And tumors from some patients with relapsed breast cancer or melanoma had increased markers of Notch1 signaling.
In the second study, the researchers used the aforementioned pathway-centric screen to track a pair of separate signaling pathways downstream of RAS, a protein frequently activated in MPNs.
The team found the pathway mediated by RAS promoted drug resistance in hematopoietic cell lines containing an activating mutation in JAK2. And RAS signaling led to the phosphorylation-mediated inactivation of the pro-apoptotic protein BAD, which enabled cell survival.
Combining JAK inhibitors with inhibitors of kinases downstream of RAS signaling prompted apoptosis in cell lines that were resistant to JAK inhibitors. This suggests such combinations may be effective for treating drug-resistant MPNs.
“Together, these findings improve our ability to stratify patients into groups more and less likely to respond to therapy and design drug combinations that work together to block or delay resistance,” Dr Wood concluded.
Researchers say they’ve discovered key events that prompt drug resistance in myeloproliferative neoplasms (MPNs) and certain solid tumor malignancies.
By mapping the steps that myelofibrosis, melanoma, and breast cancer cells use to become resistant to drugs, the investigators believe they have identified better targets for blocking those pathways to ensure current therapies are effective.
The groups reported these findings in two papers published in Science Signaling.
“In our studies, we developed a screening technology that allows us to quickly identify the routes cells can use to become resistant, and, using that information, we were able to show that these mechanisms seen in the laboratory are actually also occurring in patients’ tumors,” said Kris Wood, PhD, an assistant professor at Duke University in Durham, North Carolina, and senior author of both studies.
In the first study, Dr Wood and his colleagues conducted a broad survey of the known cell-signaling pathways that, when activated, have the potential to trigger drug resistance.
Using this screening technology, the researchers were able to corroborate the results of earlier drug-resistance studies, while also finding pathways that had not previously been described.
The team identified the MAPK and PI3K pathways, which are known to mediate drug resistance. But they also found that activation of the Notch1 pathway caused drug resistance, and inhibiting Notch1 signaling restored drug efficacy.
“Interestingly, the mechanisms are quite similar among all 3 of the cancer types,” Dr Wood noted. “In breast cancer and melanoma, our findings suggest the same Notch1 pathway as a potential driver of resistance to a wide array of targeted therapies—a role that has not been widely acknowledged previously.”
The investigators found that Notch signaling mediated drug resistance to an estrogen receptor-targeted therapy used in breast cancer and to a kinase-targeted therapy used in melanoma. And tumors from some patients with relapsed breast cancer or melanoma had increased markers of Notch1 signaling.
In the second study, the researchers used the aforementioned pathway-centric screen to track a pair of separate signaling pathways downstream of RAS, a protein frequently activated in MPNs.
The team found the pathway mediated by RAS promoted drug resistance in hematopoietic cell lines containing an activating mutation in JAK2. And RAS signaling led to the phosphorylation-mediated inactivation of the pro-apoptotic protein BAD, which enabled cell survival.
Combining JAK inhibitors with inhibitors of kinases downstream of RAS signaling prompted apoptosis in cell lines that were resistant to JAK inhibitors. This suggests such combinations may be effective for treating drug-resistant MPNs.
“Together, these findings improve our ability to stratify patients into groups more and less likely to respond to therapy and design drug combinations that work together to block or delay resistance,” Dr Wood concluded.
Researchers say they’ve discovered key events that prompt drug resistance in myeloproliferative neoplasms (MPNs) and certain solid tumor malignancies.
By mapping the steps that myelofibrosis, melanoma, and breast cancer cells use to become resistant to drugs, the investigators believe they have identified better targets for blocking those pathways to ensure current therapies are effective.
The groups reported these findings in two papers published in Science Signaling.
“In our studies, we developed a screening technology that allows us to quickly identify the routes cells can use to become resistant, and, using that information, we were able to show that these mechanisms seen in the laboratory are actually also occurring in patients’ tumors,” said Kris Wood, PhD, an assistant professor at Duke University in Durham, North Carolina, and senior author of both studies.
In the first study, Dr Wood and his colleagues conducted a broad survey of the known cell-signaling pathways that, when activated, have the potential to trigger drug resistance.
Using this screening technology, the researchers were able to corroborate the results of earlier drug-resistance studies, while also finding pathways that had not previously been described.
The team identified the MAPK and PI3K pathways, which are known to mediate drug resistance. But they also found that activation of the Notch1 pathway caused drug resistance, and inhibiting Notch1 signaling restored drug efficacy.
“Interestingly, the mechanisms are quite similar among all 3 of the cancer types,” Dr Wood noted. “In breast cancer and melanoma, our findings suggest the same Notch1 pathway as a potential driver of resistance to a wide array of targeted therapies—a role that has not been widely acknowledged previously.”
The investigators found that Notch signaling mediated drug resistance to an estrogen receptor-targeted therapy used in breast cancer and to a kinase-targeted therapy used in melanoma. And tumors from some patients with relapsed breast cancer or melanoma had increased markers of Notch1 signaling.
In the second study, the researchers used the aforementioned pathway-centric screen to track a pair of separate signaling pathways downstream of RAS, a protein frequently activated in MPNs.
The team found the pathway mediated by RAS promoted drug resistance in hematopoietic cell lines containing an activating mutation in JAK2. And RAS signaling led to the phosphorylation-mediated inactivation of the pro-apoptotic protein BAD, which enabled cell survival.
Combining JAK inhibitors with inhibitors of kinases downstream of RAS signaling prompted apoptosis in cell lines that were resistant to JAK inhibitors. This suggests such combinations may be effective for treating drug-resistant MPNs.
“Together, these findings improve our ability to stratify patients into groups more and less likely to respond to therapy and design drug combinations that work together to block or delay resistance,” Dr Wood concluded.
Combo may enhance spleen reductions in MF

the 2014 ASH Annual Meeting
SAN FRANCISCO—Combination therapy with ruxolitinib and panobinostat shows signs of efficacy in myelofibrosis (MF), according to research
presented at the 2014 ASH Annual Meeting.
“Targeting multiple components of the JAK/STAT pathway, as well as parallel signaling pathways that may also be involved in the pathogenesis of myelofibrosis, has the potential to have a synergistic therapeutic effect on the underlying disease,” said Jean-Jacques Kiladjian MD, PhD, of the Hôpital Saint-Louis and Université Paris Diderot in Paris, France.
Ruxolitinib, a potent JAK1/JAK2 inhibitor, demonstrated rapid and durable reductions in splenomegaly and MF-related symptoms, improved quality of life, and provided a survival advantage in the phase 3 COMFORT studies.
Panobinostat, a potent oral pan-deacetylase inhibitor, reduced spleen size, symptoms, and JAK2V617F allele burden in patients with MF in phase 1 and phase 2 studies.
The combination of ruxolitinib and panobinostat demonstrated synergistic anti-MF activity in a phase 1b study.
At ASH, Dr Kiladjian presented updated results from the expansion phase of this trial (abstract 711). This study was sponsored by Novartis, the company developing ruxolitinib.
The treatment schedule was ruxolitinib at 5 mg to 15 mg twice daily and panobinostat at 10 mg to 25 mg once daily 3 times per week on days 2, 4, and 6 every other week in a 28-day cycle.
A dose-escalation phase included 38 patients with a median age of 63 years, and an expansion phase included 23 patients with a median age of 67 years.
The recommended phase 2 dose was 15 mg of ruxolitinib twice daily and 25 mg of panobinostat twice weekly, every other week.
“Changes in spleen size were seen in the escalation phase, even at low doses,” Dr Kiladjian said. “Some patients completely eliminated splenomegaly.”
The expansion phase showed similar results. At 24 weeks, more than 85% of patients had a 50% or greater reduction in splenomegaly. Some 59% of patients achieved a 50% or greater reduction in palpable spleen length.
“We saw some JAK2 inhibition and reduction in bone marrow fibrosis, as well as significant reduction in several cytokines related to inflammation,” Dr Kiladjian said.
The most common hematologic adverse events were anemia and thrombocytopenia. There were few neutropenias.
“We saw quite remarkably stable levels of hemoglobin and platelets,” Dr Kiladjian said.
Non-hematologic adverse events were primarily gastrointestinal toxicity associated with panobinostat, including grade 3 or 4 diarrhea and asthenia.
“The rates of adverse events observed in this trial are in line with the expected and known adverse events of these 2 agents when used as monotherapies,” Dr Kiladjian said.
“The combination of ruxolitinib and panobinostat was well-tolerated and resulted in substantial reductions in splenomegaly. Most patients treated at the [recommended phase 2 dose] of combination therapy achieved a spleen response.”
Dr Kiladjian therefore encouraged further exploration of this “favorable” combination. ![]()

the 2014 ASH Annual Meeting
SAN FRANCISCO—Combination therapy with ruxolitinib and panobinostat shows signs of efficacy in myelofibrosis (MF), according to research
presented at the 2014 ASH Annual Meeting.
“Targeting multiple components of the JAK/STAT pathway, as well as parallel signaling pathways that may also be involved in the pathogenesis of myelofibrosis, has the potential to have a synergistic therapeutic effect on the underlying disease,” said Jean-Jacques Kiladjian MD, PhD, of the Hôpital Saint-Louis and Université Paris Diderot in Paris, France.
Ruxolitinib, a potent JAK1/JAK2 inhibitor, demonstrated rapid and durable reductions in splenomegaly and MF-related symptoms, improved quality of life, and provided a survival advantage in the phase 3 COMFORT studies.
Panobinostat, a potent oral pan-deacetylase inhibitor, reduced spleen size, symptoms, and JAK2V617F allele burden in patients with MF in phase 1 and phase 2 studies.
The combination of ruxolitinib and panobinostat demonstrated synergistic anti-MF activity in a phase 1b study.
At ASH, Dr Kiladjian presented updated results from the expansion phase of this trial (abstract 711). This study was sponsored by Novartis, the company developing ruxolitinib.
The treatment schedule was ruxolitinib at 5 mg to 15 mg twice daily and panobinostat at 10 mg to 25 mg once daily 3 times per week on days 2, 4, and 6 every other week in a 28-day cycle.
A dose-escalation phase included 38 patients with a median age of 63 years, and an expansion phase included 23 patients with a median age of 67 years.
The recommended phase 2 dose was 15 mg of ruxolitinib twice daily and 25 mg of panobinostat twice weekly, every other week.
“Changes in spleen size were seen in the escalation phase, even at low doses,” Dr Kiladjian said. “Some patients completely eliminated splenomegaly.”
The expansion phase showed similar results. At 24 weeks, more than 85% of patients had a 50% or greater reduction in splenomegaly. Some 59% of patients achieved a 50% or greater reduction in palpable spleen length.
“We saw some JAK2 inhibition and reduction in bone marrow fibrosis, as well as significant reduction in several cytokines related to inflammation,” Dr Kiladjian said.
The most common hematologic adverse events were anemia and thrombocytopenia. There were few neutropenias.
“We saw quite remarkably stable levels of hemoglobin and platelets,” Dr Kiladjian said.
Non-hematologic adverse events were primarily gastrointestinal toxicity associated with panobinostat, including grade 3 or 4 diarrhea and asthenia.
“The rates of adverse events observed in this trial are in line with the expected and known adverse events of these 2 agents when used as monotherapies,” Dr Kiladjian said.
“The combination of ruxolitinib and panobinostat was well-tolerated and resulted in substantial reductions in splenomegaly. Most patients treated at the [recommended phase 2 dose] of combination therapy achieved a spleen response.”
Dr Kiladjian therefore encouraged further exploration of this “favorable” combination. ![]()

the 2014 ASH Annual Meeting
SAN FRANCISCO—Combination therapy with ruxolitinib and panobinostat shows signs of efficacy in myelofibrosis (MF), according to research
presented at the 2014 ASH Annual Meeting.
“Targeting multiple components of the JAK/STAT pathway, as well as parallel signaling pathways that may also be involved in the pathogenesis of myelofibrosis, has the potential to have a synergistic therapeutic effect on the underlying disease,” said Jean-Jacques Kiladjian MD, PhD, of the Hôpital Saint-Louis and Université Paris Diderot in Paris, France.
Ruxolitinib, a potent JAK1/JAK2 inhibitor, demonstrated rapid and durable reductions in splenomegaly and MF-related symptoms, improved quality of life, and provided a survival advantage in the phase 3 COMFORT studies.
Panobinostat, a potent oral pan-deacetylase inhibitor, reduced spleen size, symptoms, and JAK2V617F allele burden in patients with MF in phase 1 and phase 2 studies.
The combination of ruxolitinib and panobinostat demonstrated synergistic anti-MF activity in a phase 1b study.
At ASH, Dr Kiladjian presented updated results from the expansion phase of this trial (abstract 711). This study was sponsored by Novartis, the company developing ruxolitinib.
The treatment schedule was ruxolitinib at 5 mg to 15 mg twice daily and panobinostat at 10 mg to 25 mg once daily 3 times per week on days 2, 4, and 6 every other week in a 28-day cycle.
A dose-escalation phase included 38 patients with a median age of 63 years, and an expansion phase included 23 patients with a median age of 67 years.
The recommended phase 2 dose was 15 mg of ruxolitinib twice daily and 25 mg of panobinostat twice weekly, every other week.
“Changes in spleen size were seen in the escalation phase, even at low doses,” Dr Kiladjian said. “Some patients completely eliminated splenomegaly.”
The expansion phase showed similar results. At 24 weeks, more than 85% of patients had a 50% or greater reduction in splenomegaly. Some 59% of patients achieved a 50% or greater reduction in palpable spleen length.
“We saw some JAK2 inhibition and reduction in bone marrow fibrosis, as well as significant reduction in several cytokines related to inflammation,” Dr Kiladjian said.
The most common hematologic adverse events were anemia and thrombocytopenia. There were few neutropenias.
“We saw quite remarkably stable levels of hemoglobin and platelets,” Dr Kiladjian said.
Non-hematologic adverse events were primarily gastrointestinal toxicity associated with panobinostat, including grade 3 or 4 diarrhea and asthenia.
“The rates of adverse events observed in this trial are in line with the expected and known adverse events of these 2 agents when used as monotherapies,” Dr Kiladjian said.
“The combination of ruxolitinib and panobinostat was well-tolerated and resulted in substantial reductions in splenomegaly. Most patients treated at the [recommended phase 2 dose] of combination therapy achieved a spleen response.”
Dr Kiladjian therefore encouraged further exploration of this “favorable” combination. ![]()

