User login
Biomarker-driven targeted therapy feasible for NSCLC
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic NSCLC.
Major finding: The primary endpoint – disease control rate at 8 weeks – was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4.
Data source: A randomized open-label phase II study involving 200 patients with heavily pretreated, metastatic NSCLC.
Disclosures: This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
Early results positive for nivolumab as first-line therapy in advanced NSCLC
The PD-1 immune checkpoint inhibitor nivolumab may be safe and effective as a first-line therapy in adult patients with non–small cell lung cancer (NSCLC), according to the results of the phase I CheckMate 012 trial.
Of 52 adult patients with advanced NSCLC who received nivolumab, 19% experienced grade three or four adverse events, and the overall response rate was 23% with four ongoing complete responses, reported Scott Gettinger, MD, of the Yale Cancer Center, New Haven, Conn., and his associates (J Clin Oncol. 2016 June. doi: 10.1200/JCO.2016.66.9929).
In the study cohort, 94% had stage IV NSCLC, 79% were former or current smokers, and 65% had received either radiotherapy, adjuvant or neoadjuvant chemotherapy.
Treatment-related adverse events were reported in 71% of patients, the most common being fatigue (29%), rash (19%), and nausea (14%). Grade 3 or 4 adverse events including rash, cardiac failure, and lung infection occurred in 10 patients (19%). There were no treatment-related deaths, but adverse events led to the discontinuation of the drug treatment in six patients.
Responses to nivolumab (overall response rate, 23%) were durable with duration of responses ranging from 4.2 to 25.8 months. In addition, the median overall survival was 19.4 months, median progression-free survival was 3.5 months, and the 24-week progression-free survival rate was 31% (95% confidence interval, 28%-60%).
Forty-six patients had tumor specimens evaluable for PD-L1 expression. Clinical activity was observed regardless of PD-L1 expression, the investigators reported. However, the overall response rate was higher in patients with tumors that expressed PD-L1, compared with non-PD-L1-expressing tumors.
All investigators reported serving in advisory roles for, receiving financial compensation or honoraria from, or having ownership or stock in multiple companies including Bristol-Myers Squibb, which funded the study.
On Twitter @jessnicolecraig
The PD-1 immune checkpoint inhibitor nivolumab may be safe and effective as a first-line therapy in adult patients with non–small cell lung cancer (NSCLC), according to the results of the phase I CheckMate 012 trial.
Of 52 adult patients with advanced NSCLC who received nivolumab, 19% experienced grade three or four adverse events, and the overall response rate was 23% with four ongoing complete responses, reported Scott Gettinger, MD, of the Yale Cancer Center, New Haven, Conn., and his associates (J Clin Oncol. 2016 June. doi: 10.1200/JCO.2016.66.9929).
In the study cohort, 94% had stage IV NSCLC, 79% were former or current smokers, and 65% had received either radiotherapy, adjuvant or neoadjuvant chemotherapy.
Treatment-related adverse events were reported in 71% of patients, the most common being fatigue (29%), rash (19%), and nausea (14%). Grade 3 or 4 adverse events including rash, cardiac failure, and lung infection occurred in 10 patients (19%). There were no treatment-related deaths, but adverse events led to the discontinuation of the drug treatment in six patients.
Responses to nivolumab (overall response rate, 23%) were durable with duration of responses ranging from 4.2 to 25.8 months. In addition, the median overall survival was 19.4 months, median progression-free survival was 3.5 months, and the 24-week progression-free survival rate was 31% (95% confidence interval, 28%-60%).
Forty-six patients had tumor specimens evaluable for PD-L1 expression. Clinical activity was observed regardless of PD-L1 expression, the investigators reported. However, the overall response rate was higher in patients with tumors that expressed PD-L1, compared with non-PD-L1-expressing tumors.
All investigators reported serving in advisory roles for, receiving financial compensation or honoraria from, or having ownership or stock in multiple companies including Bristol-Myers Squibb, which funded the study.
On Twitter @jessnicolecraig
The PD-1 immune checkpoint inhibitor nivolumab may be safe and effective as a first-line therapy in adult patients with non–small cell lung cancer (NSCLC), according to the results of the phase I CheckMate 012 trial.
Of 52 adult patients with advanced NSCLC who received nivolumab, 19% experienced grade three or four adverse events, and the overall response rate was 23% with four ongoing complete responses, reported Scott Gettinger, MD, of the Yale Cancer Center, New Haven, Conn., and his associates (J Clin Oncol. 2016 June. doi: 10.1200/JCO.2016.66.9929).
In the study cohort, 94% had stage IV NSCLC, 79% were former or current smokers, and 65% had received either radiotherapy, adjuvant or neoadjuvant chemotherapy.
Treatment-related adverse events were reported in 71% of patients, the most common being fatigue (29%), rash (19%), and nausea (14%). Grade 3 or 4 adverse events including rash, cardiac failure, and lung infection occurred in 10 patients (19%). There were no treatment-related deaths, but adverse events led to the discontinuation of the drug treatment in six patients.
Responses to nivolumab (overall response rate, 23%) were durable with duration of responses ranging from 4.2 to 25.8 months. In addition, the median overall survival was 19.4 months, median progression-free survival was 3.5 months, and the 24-week progression-free survival rate was 31% (95% confidence interval, 28%-60%).
Forty-six patients had tumor specimens evaluable for PD-L1 expression. Clinical activity was observed regardless of PD-L1 expression, the investigators reported. However, the overall response rate was higher in patients with tumors that expressed PD-L1, compared with non-PD-L1-expressing tumors.
All investigators reported serving in advisory roles for, receiving financial compensation or honoraria from, or having ownership or stock in multiple companies including Bristol-Myers Squibb, which funded the study.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A phase I trial indicates that nivolumab is safe and shows durable activity as a first-line therapy in treating patients with advanced NSCLC.
Major finding: Grade 3 or 4 adverse events were reported in 19% of patients. The overall response rate was 23% with four ongoing complete responses.
Data source: A phase I trial of 52 patients with stage 3 or 4 non–small-cell lung cancer.
Disclosures: All investigators reported serving in advisory roles for, receiving financial compensation or honoraria from, or having ownership or stock interest in multiple companies including Bristol-Myers Squibb, which funded the study.
Wedge resection showed improved survival over SBRT for early-stage NSCLC
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Wedge resection outperformed SBRT in terms of mortality for early-stage NSCLC.
Major finding: In matched groups, SBRT was associated with significantly lower 5-year overall survival than was wedge resection (32% vs. 50%).
Data source: The study assessed more than 8.000 patients with early stage NSCLC who had either wedge resection or SBRT from the National Cancer Database from 2003 to 2011.
Disclosures: Dr. Yerokun had no relevant disclosures.
Esophagectomy 30-day readmission rate pegged at 19%
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Operative length, perioperative blood transfusions, and postoperative ICU admission were significant risk factors for readmission after esophagectomy.
Major finding: The rate of unplanned 30-day readmission was 19%.
Data source: The study assessed 86 patients who underwent esophagectomy at the Mayo Clinic between August 2012 and July 2014.
Disclosures: Dr. Dickinson and her colleagues reported having no relevant disclosures.
Hospital-acquired respiratory viruses cause significant morbidity, mortality
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
AT ASM MICROBE 2016
Key clinical point: Hospital-acquired respiratory viral illnesses had a 39% mortality rate.
Major finding: Of 44 symptomatic patients with positive respiratory virus panel screens, 17 died and 2/3 of the survivors went to advanced care settings on discharge.
Data source: Retrospective multisite chart review of 44 patients with HA-RVIs and positive RVP screens.
Disclosures: No external funding source was reported, and the study authors had no disclosures.
IASLC lung cancer staging project proposes changes for new TNM classification
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
FROM THE JOURNAL OF THORACIC ONCOLOGY
Key clinical point: New lung cancer classification to become effective January 2017.
Major finding: Size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed dividing stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm.
Data source: The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer.
Disclosures: The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
Web app boosts lung cancer survival
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
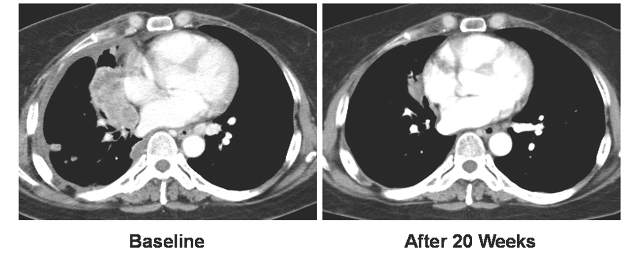
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: A Web-based app improves survival for advanced lung cancer patients.
Major finding: Survival improved by 26% for web-app patients vs. controls.
Data source: Multicenter, prospective, phase III, randomized trial of 121 patients.
Disclosures: Dr. Denis has received honoraria and expenses from several pharmaceutical companies and has received institutional research funding from Sivan. Dr. Patricia Ganz reported stock and other ownership interest in Abbott Laboratories, GlaxoSmithKline, Johnson & Johnson, Merck, Novartis, Pfizer, and Teva.
Vandetanib shows variable response, toxicity in RET-positive NSCLC
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Vandetanib shows marked yet variable anti-tumor activity and toxicity in patients with RET-rearranged NSCLC.
Major finding: The overall response rates were 53% and 61% in two independent trials.
Data source: Two independently-conducted multicenter phase II trials of patients with RET-rearranged non-small cell lung cancer.
Disclosures: The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea Ltd. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
VIDEO: Lobectomy quality requires linking outcomes to process change
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Surgical quality measures boost survival in cancer patients
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING