User login
Ear-worn device helps Parkinson’s patients to improve their voice
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
PORTLAND, ORE. – A new device worn on one ear may help individuals with Parkinson’s disease to overcome speech deficits associated with the disease. When triggered by the wearer’s voice, the device, SpeechVive, provides a simulated room crowd noise or “babble” only when they are talking. Because it capitalizes on natural reflexes to this simulated background noise, improvement can occur independent of speech training.
Researchers led by Jessica Huber, PhD, a professor of speech, language, and hearing sciences at Purdue University in West Lafayette, Ind., investigated changes to speech after 3 months of daily use of the SpeechVive device by 16 individuals. The cohort had a mean age of 64.5 years (range: 56-78 years) and a mean disease duration of 8.1 years (range: 2-17 years). Six participants had previously had speech therapy (five with LSVT [Lee Silverman Voice Treatment] LOUD speech training exercises), and two had deep brain stimulation implants.
Similar to an earlier study of 39 participants, “We found a nice increase in loudness, that they just can wear the device, and they’re louder in their everyday communication,” Dr. Huber said in an interview during a poster session at the World Parkinson Congress. New to this study was a finding that the melody of speech was a little better, “so their questions are more like questions, and their statements are more like statements, so are the rising intonation on questions and the falling intonation on a statement.” Participants were also able to say more on one breath and to sound more natural with appropriate pauses because of the longer utterances.
After 3 months of use, participants as a group increased their sound pressure level (loudness) from 76.6 dB to 78.8 dB (a gain of 2.2 dB) from having the device OFF to ON. When it was then turned off, they had an intermediate sound pressure level of 77.7 dB (both P less than .0001 vs. pretest OFF). Intonation variability and intonation range also showed significant improvements for both statements and questions with the use of the device (all P less than or equal to .01). There were also improvements in a correct statement or question being produced, pausing patterns, and utterance length. No adverse events occurred in the study.
Dr. Huber said patients in the study were quite variable in their responses to SpeechVive for the different measures of speech. In general, she has found that about 75% of users get louder with the device, and some have clearer articulation or slower speech. Another 10%-15% have slower speech or better articulation without an increase in loudness.
A total of 50% of the users have a “carry-over” effect after using the device when they are not wearing it. “After about 8 weeks, they don’t need to keep wearing the device every day,” Dr. Huber noted. Others may wear it in the morning and have a lasting effect for the rest of the day, and some lose any benefit as soon as taking the device off. Not all patients reach a normal speech loudness, “but they’re going to get way better” than where they started, she said.
Available speech therapies
People with Parkinson’s disease (PD) often have reduced vocal loudness, increased speech rate, and slurred articulation. Available speech therapies have included adduction exercises, vocal function exercises, and LSVT LOUD speech training exercises. For some individuals with PD, these behavioral treatments may not carry over into daily life.
The SpeechVive consists of a piece placed into the ear canal and a piece that sits behind the ear, similar to a slightly larger version of a modern hearing aid. It is designed large enough that many patients, who have motor deficits, can don it themselves. Because it is on just one ear, users can hear other people talking and what is going on around them.
Dr. Huber noted several strengths of the device. First, it does not impose any cognitive load on the user because its effect is based on an automatic reflex. Second, little training is necessary. It is easy for the user to put on the device, and many of its beneficial effects occur as soon as it is activated. Third, compliance can be tracked using data stored by the device itself.
In a previous study, she saw that after using the device for 8 weeks, participants used more effective patterns with their respiratory and laryngeal mechanisms to produce louder speech. “It’s not like they’re working super hard after 8 weeks.” She thinks they are just not usually using their speech apparatus in the most efficient manner, and they become more efficient after using the device. They may also not sense how loud they are without it, so it helps patients “recalibrate” a sense of their own voices, something the LSVT LOUD training also does.
Jori Fleisher, MD, a movement disorders neurologist at the New York University Langone Medical Center, commented that the study shows an interesting approach to the common and difficult problem of hypophonia and dysphonia in people with Parkinson’s disease. “It can be very difficult to speak loud enough to be heard, and it often leads to people withdrawing socially and not speaking as much in conversation as they normally would,” she said. “LSVT LOUD works in practice when you’re actually doing the exercises, but often when people stop doing the exercises, their voice goes back toward their normal. So this is something that you can keep with you and sort of have constant prompting to overcome that tendency toward quieter voice. It has a lot of promise.”
She said she would like to see the data on compliance or adherence with using the device “because it seems like a great idea, but how much are people actually using it? ... Having more long-term follow-up to see whether this is something that people want to put into practice in their daily life would be very useful.” She also said she would like to see how long the carry-over effect lasts once people take off the device to be able to compare it with sessions of speech therapy or doing speech exercises.
SpeechVive is $2,495, which includes the device, a charger, and earpiece fittings. It is available only in the United States, but the company now has clearance to market it in Canada.
The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
AT WPC 2016
Key clinical point:
Major finding: Loudness increased 2.2 dB from 76.6 dB to 78.8 dB after 3 months of use. Intonation also improved.
Data source: A prospective study of 16 participants with hypophonia comparing speech parameters with and without the device after 3 months of use.
Disclosures: The research was funded by a grant from SpeechVive. Dr. Huber is the inventor of SpeechVive, has a patent on it, has a financial interest in the SpeechVive company, and sits on its board of directors. Dr. Fleisher reported having no financial conflicts.
Biopsy scalp area for alopecia diagnosis
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
Many overweight Parkinson’s patients have insulin resistance
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 84 nondiabetic, Parkinson’s patients, 58% had insulin resistance, although their blood glucose and insulin levels were not abnormal.
Data source: Prospective, observational study of a total of 93 Parkinson’s patients.
Disclosures: The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
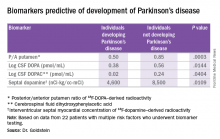
Biomarkers predict Parkinson’s among high-risk individuals
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 22 individuals followed for at least 3 years, biomarkers were 100% positively or negatively predictive of developing Parkinson’s disease.
Data source: A prospective cohort study of 3,176 individuals supplying risk factor data, of whom 31 had three or more risk factors and biomarkers testing, and of whom 22 were followed for at least 3 years.
Disclosures: The study was run by the National Institute of Neurological Disorders and Stroke and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
Asleep deep brain stimulation placement offers advantages in Parkinson’s
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – Performing deep brain stimulation surgery for Parkinson’s disease using intraoperative CT imaging while the patient is under general anesthesia had clinical advantages and no disadvantages over surgery using microelectrode recording for lead placement with the patient awake, in a prospective, open-label study of 64 patients.
Regarding motor outcomes after asleep surgery, “We found that it was noninferior, so in other words, the change in scores following surgery were the same for asleep and awake patients,” physician assistant and study coauthor Shannon Anderson said during a poster session at the World Parkinson Congress. “What was surprising to us was that verbal fluency ... the ability to come up with the right word, actually improved in our asleep DBS [deep brain stimulation] group, which is a huge complication for patients [and] has a really negative impact on their life.”
Patients with Parkinson’s disease and motor complications (n = 64) were enrolled prospectively at the Oregon Health & Science University in Portland. Thirty received asleep procedures under general anesthesia with ICT guidance for lead targeting to the globus pallidus pars interna (GPi; n = 21) or to the subthalamic nucleus (STN; n = 9). Thirty-four patients received DBS devices with MER guidance (15 STN; 19 GPi). At baseline, the two groups were similar in age (mean 61.1-62.7 years) and off-medication motor subscale scores of the Unified Parkinson’s Disease Rating Scale (mUPDRS; mean 43.0-43.5). The university investigators optimized the DBS parameters at 1, 2, 3, and 6 months after implantation. The same surgeon performed all the procedures at the same medical center.
Motor improvements were similar between the asleep and awake cohorts. At 6 months, the ICT (asleep) group experienced a mean improvement in motor abilities of 14.3 (plus or minus 10.88) on the mUPDRS off-medication and on DBS, compared with an improvement of 17.6 (plus or minus 12.26) for the MER (awake) group (P = .25).
Better language measures with asleep DBS
Asleep DBS with ICT resulted in improvements in aspects of language, whereas awake patients lost language abilities. The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Although both cohorts showed significant improvements on the 39-item Parkinson’s Disease Questionnaire at 6 months, the cohorts did not differ in their degrees of improvement. Similarly, both had improvements on scores of activities of daily living, and both cohorts had a 4-4.5 hours/day increase in “on” time without dyskinesia and a 2.6-3.5 hours/day decrease in “on” time with dyskinesia.
Patients tolerated asleep DBS well, and there were no serious complications.
The sleep surgery is much shorter, “so it’s about 2 hours long as opposed to 4, 5, sometimes 8, 10 hours with the awake. There [are fewer] complications, so less risk of hemorrhage or seizures or things like that,” Ms. Anderson said. “In a separate study, we found that it’s a much more accurate placement of the electrodes so the target is much more accurate. So, all of those things considered, we feel the asleep version is definitely the superior choice between the two.”
Being asleep is much more comfortable for the patient, added study leader Matthew Brodsky, MD. “But the biggest advantage is that it’s a single pass into the brain as opposed to multiple passes.” The average number of passes using MER is two to three per side of the brain, and in some centers, four or more. “Problems such as speech prosody are related to pokes in the brain, if you will, rather than stimulation,” he said.
Ms. Anderson said MER “is a fantastic research tool, and it gives us a lot of information on the electrophysiology, but really, there’s no need for it in the clinical application of DBS.”
Based on the asleep procedure’s accuracy, lower rate of complications, shorter operating room time, and noninferiority in terms of motor outcomes, she said, “Our recommendation is that more centers, more neurosurgeons be trained in this technique ... We’d like to see the clinical field move toward that area and really reserve microelectrode recording for the research side of things.”
“If you talk to folks who are considering brain surgery for their Parkinson’s, for some of them, the idea of being awake in the operating room and undergoing this is a barrier that they can’t quite overcome,” Dr. Brodsky said. “So, having this as an option makes it easier for them to sign up for the process.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, said that the asleep procedure is the newer one and can target either the GPi or the STN. “The asleep DBS seems to have a little bit better improvement on speech afterwards than the awake DBS, and there could be several causes of this,” he said. “Some might be operative in that you can make smaller holes, you can get really nice guidance, you don’t have to sort of move around as in the awake DBS.”
In addition, CT scanning with the patients asleep in the operating room allows more time in the scanner and greater precision in anatomical placement of the DBS leads.
“If I had to choose, looking at this particular study, it would suggest that the asleep DBS is actually a better overall way to go,” Dr. Smeyne said. However, he had no objection to awake procedures “if the neurosurgeon has a record of good results with it ... But if you have the option ... that becomes an individual choice that you should discuss with the neurosurgeon.”
Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: The asleep group showed a 0.8-point increase in phonemic fluency and a 1.0-point increase in semantic fluency at 6 months versus a worsening on both language measures (–3.5 points and –4.7 points, respectively; both P less than .001) if DBS was performed via MER on awake patients.
Data source: Prospective, open-label study of 64 patients receiving either awake or asleep deep brain stimulation placement.
Disclosures: Some of the work presented in the study was supported by a research grant from Medtronic. Ms. Anderson and Dr. Brodsky reported having no other financial disclosures. Dr. Smeyne reported having no financial disclosures.
Acne and diet: Still no solid basis for dietary recommendations
BOSTON – For years, much of the information that has circulated about the relationship of diet to acne has been inconsistent. And while recent studies have pointed to two aggravating factors – foods with a high glycemic index and skim milk – whether dietary changes can help control acne remains up in the air, according to Andrea Zaenglein, MD.
At the American Academy of Dermatology summer meeting, Dr. Zaenglein, professor of dermatology and pediatrics, Penn State University, Hershey, reviewed information about diet and acne dating back to the early 1930s, when reports suggested an increased risk of acne in people who were glucose intolerant. Subsequent studies looked at the role of dairy, carbohydrate, chloride, saturated and total fats, sugar, and chocolate in acne. Researchers found no acne in a study of natives of Kitava, an island in Papua New Guinea, whose diet consisted mostly of roots, coconut, fruit, and fish (Arch Dermatol. 2002;138[12]:1584-90). But genetics certainly appears to play a dominant role in acne, Dr. Zaenglein said, referring to a large twin study that found that in 81% of the population with acne, it was due to genetic factors, and in 19% it was due to environmental factors (J Invest Dermatol. 2002 Dec;119[6]:1317-22).
For now, Dr. Zaenglein’s advice is to recommend a low glycemic index diet mainly of fruits and vegetables and low in saturated fats and sugars, which may ameliorate acne by decreasing weight and insulin resistance – especially in patients who already have abnormal metabolic parameters. Patients should also be advised to limit processed foods, meat, and dairy, she added.
As far as dairy and acne, it is too early to say what the impact of intervention would be “because we don’t have any great interventional studies that have been done,” she said. Moreover, it is unclear how early dietary interventions would need to be started to reduce an individual’s risk of acne, she added.“It could go all the way back to things that happened when you were born that influence your outcome,” Dr. Zaenglein said. For example, babies born prematurely are at greater risk for endocrine stressors, which lead to premature adrenarche, increasing their risk for acne, she noted.
“We really need new, better intervention studies to be able to give advice to our patients,” she said. However, conducting such studies is challenging because it is difficult for people to eliminate dairy or other types of food from their diets for a prolonged period. To date, the majority of dietary studies have been observational and have relied on subjects’ recall of what they consumed, so these studies have their own inherent problems, she added.Dr. Zaenglein’s disclosures include serving as an adviser to Anacor Pharmaceuticals and Valeant Pharmaceuticals International, and serving as an investigator and receiving grants/research funding from Anacor, Astellas Pharma US, Ranbaxy Laboratories Limited, and Stiefel, a GSK company.
BOSTON – For years, much of the information that has circulated about the relationship of diet to acne has been inconsistent. And while recent studies have pointed to two aggravating factors – foods with a high glycemic index and skim milk – whether dietary changes can help control acne remains up in the air, according to Andrea Zaenglein, MD.
At the American Academy of Dermatology summer meeting, Dr. Zaenglein, professor of dermatology and pediatrics, Penn State University, Hershey, reviewed information about diet and acne dating back to the early 1930s, when reports suggested an increased risk of acne in people who were glucose intolerant. Subsequent studies looked at the role of dairy, carbohydrate, chloride, saturated and total fats, sugar, and chocolate in acne. Researchers found no acne in a study of natives of Kitava, an island in Papua New Guinea, whose diet consisted mostly of roots, coconut, fruit, and fish (Arch Dermatol. 2002;138[12]:1584-90). But genetics certainly appears to play a dominant role in acne, Dr. Zaenglein said, referring to a large twin study that found that in 81% of the population with acne, it was due to genetic factors, and in 19% it was due to environmental factors (J Invest Dermatol. 2002 Dec;119[6]:1317-22).
For now, Dr. Zaenglein’s advice is to recommend a low glycemic index diet mainly of fruits and vegetables and low in saturated fats and sugars, which may ameliorate acne by decreasing weight and insulin resistance – especially in patients who already have abnormal metabolic parameters. Patients should also be advised to limit processed foods, meat, and dairy, she added.
As far as dairy and acne, it is too early to say what the impact of intervention would be “because we don’t have any great interventional studies that have been done,” she said. Moreover, it is unclear how early dietary interventions would need to be started to reduce an individual’s risk of acne, she added.“It could go all the way back to things that happened when you were born that influence your outcome,” Dr. Zaenglein said. For example, babies born prematurely are at greater risk for endocrine stressors, which lead to premature adrenarche, increasing their risk for acne, she noted.
“We really need new, better intervention studies to be able to give advice to our patients,” she said. However, conducting such studies is challenging because it is difficult for people to eliminate dairy or other types of food from their diets for a prolonged period. To date, the majority of dietary studies have been observational and have relied on subjects’ recall of what they consumed, so these studies have their own inherent problems, she added.Dr. Zaenglein’s disclosures include serving as an adviser to Anacor Pharmaceuticals and Valeant Pharmaceuticals International, and serving as an investigator and receiving grants/research funding from Anacor, Astellas Pharma US, Ranbaxy Laboratories Limited, and Stiefel, a GSK company.
BOSTON – For years, much of the information that has circulated about the relationship of diet to acne has been inconsistent. And while recent studies have pointed to two aggravating factors – foods with a high glycemic index and skim milk – whether dietary changes can help control acne remains up in the air, according to Andrea Zaenglein, MD.
At the American Academy of Dermatology summer meeting, Dr. Zaenglein, professor of dermatology and pediatrics, Penn State University, Hershey, reviewed information about diet and acne dating back to the early 1930s, when reports suggested an increased risk of acne in people who were glucose intolerant. Subsequent studies looked at the role of dairy, carbohydrate, chloride, saturated and total fats, sugar, and chocolate in acne. Researchers found no acne in a study of natives of Kitava, an island in Papua New Guinea, whose diet consisted mostly of roots, coconut, fruit, and fish (Arch Dermatol. 2002;138[12]:1584-90). But genetics certainly appears to play a dominant role in acne, Dr. Zaenglein said, referring to a large twin study that found that in 81% of the population with acne, it was due to genetic factors, and in 19% it was due to environmental factors (J Invest Dermatol. 2002 Dec;119[6]:1317-22).
For now, Dr. Zaenglein’s advice is to recommend a low glycemic index diet mainly of fruits and vegetables and low in saturated fats and sugars, which may ameliorate acne by decreasing weight and insulin resistance – especially in patients who already have abnormal metabolic parameters. Patients should also be advised to limit processed foods, meat, and dairy, she added.
As far as dairy and acne, it is too early to say what the impact of intervention would be “because we don’t have any great interventional studies that have been done,” she said. Moreover, it is unclear how early dietary interventions would need to be started to reduce an individual’s risk of acne, she added.“It could go all the way back to things that happened when you were born that influence your outcome,” Dr. Zaenglein said. For example, babies born prematurely are at greater risk for endocrine stressors, which lead to premature adrenarche, increasing their risk for acne, she noted.
“We really need new, better intervention studies to be able to give advice to our patients,” she said. However, conducting such studies is challenging because it is difficult for people to eliminate dairy or other types of food from their diets for a prolonged period. To date, the majority of dietary studies have been observational and have relied on subjects’ recall of what they consumed, so these studies have their own inherent problems, she added.Dr. Zaenglein’s disclosures include serving as an adviser to Anacor Pharmaceuticals and Valeant Pharmaceuticals International, and serving as an investigator and receiving grants/research funding from Anacor, Astellas Pharma US, Ranbaxy Laboratories Limited, and Stiefel, a GSK company.
Transcranial direct current stimulation enhances cognitive training in Parkinson’s
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
PORTLAND, ORE. – Combining transcranial direct current stimulation and cognitive training resulted in an improvement in a greater number of cognitive outcomes than either intervention alone in a small, randomized, controlled trial of patients with Parkinson’s disease and mild cognitive impairment.
Researchers at Curtin University in Perth, Western Australia, conducted the trial comparing the effects of standard (not individualized) cognitive training (SCT), tailored (individualized) cognitive training (TCT), transcranial direct current stimulation (tDCS), and a combination of tDCS with either form of cognitive training on cognitive outcomes, activities of daily living, and quality of life in such Parkinson’s patients with mild cognitive impairment. Previously, it was not known whether either form of cognitive training or tDCS or a combination of the two would be most efficacious in improving cognition in such patients.
Patients had cognitive deficits that did not interfere with functional independence and were responding to stable doses of antiparkinsonian medication. Forty-two eligible participants underwent neuropsychological testing at baseline and were randomly and equally assigned to one of six groups: SCT, TCT, tDCS, SCT+tDCS, TCT+tDCS, or control.
Cognitive training consisted of three 45-minute sessions per week for 4 weeks using Smartbrain Pro software in participants’ homes. tDCS involved constant 1.5 mA stimulation for 20 minutes in one session per week for 4 weeks at the university, with the anode placed over area F3 to stimulate the left dorsal lateral prefrontal cortex. Follow-up evaluations were at 12 weeks.
The following tests were used to evaluate each outcome: executive function – Stockings of Cambridge; attention/working memory – Stroop test; memory – paragraph recall; quality of life – PDQ-39; activities of daily living – Unified Parkinson’s Disease Rating Scale-II; and language – similarities test.
In general, combining tDCS with either form of cognitive training resulted in significantly greater improvements in more outcomes than any of the modalities alone. SCT showed positive results when compared against the control group in memory improvement at follow-up (effect size, 1.30), as well as quality of life and activities of daily living postintervention (effect sizes, 0.24 and 0.33, respectively). TCT showed benefits on quality of life at both time points (effect sizes 0.26 at postintervention and 0.12 at follow-up, respectively).
When combined with tDCS, SCT produced improvements in attention/working memory both postintervention and at 12-week follow-up (effect sizes, 0.60 and 0.24, respectively) as well as executive function at postintervention and follow-up (0.41 and 0.23). Improvement in activities of daily living and language were statistically significant only immediately postintervention.
Combining tDCS with TCT resulted in improvements postintervention and at follow-up on measures of memory (1.36 and 1.75) and executive function (0.19 and 0.92), as well as in language postintervention (1.06).
“The main takeaway was that the groups that completed both cognitive training and brain stimulation improved to a greater extent and in more outcomes than the groups that just completed the brain training or the stimulation individually,” Mr. Lawrence said. “The majority of the effects were shown immediately after the intervention, but some of the promising results ... actually maintained improvement at the 12-week follow-up, so that was after about 8 weeks, when they didn’t complete any intervention whatsoever.”
The improvements are probably clinically meaningful to patients since they themselves reported the outcomes on quality of life and activities of daily living scales, he said. He added that studies are coming out that look at the effect of brain stimulation and brain training at the same time, and they have shown improvement, but not many such studies have yet been done in Parkinson’s disease.
Key clinical point:
Major finding: tDCS adds cognitive benefit when combined with cognitive training alone.
Data source: Randomized, controlled trial of 42 patients with Parkinson’s disease and mild cognitive impairment.
Disclosures: There was no commercial funding of the study. Mr. Lawrence reported he had no financial disclosures.
Gait predicts cognitive decline in early Parkinson’s
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
PORTLAND, ORE. – Gait characteristics, rather than cognition, in early Parkinson’s disease predicted cognitive decline 3 years later in a small longitudinal study, suggesting that gait measures may provide a low cost clinical biomarker when combined with other predictors of cognitive decline in Parkinson’s disease.
Cognitive decline and dementia take a significant toll on patients’ personal, social, and economic affairs. Being able to identify at-risk individuals may allow for early behavioral and possibly pharmacological interventions. Gait has been shown to be a sensitive measure of cognitive decline in older adults, and the investigators here tested it as a predictor of cognitive decline in Parkinson’s disease (PD).
Led by Rosie Morris, PhD, of Newcastle University, Newcastle upon Tyne, England, researchers assessed gait characteristics and cognition in 119 patients within 4-6 months of a diagnosis of idiopathic PD and then 18 and 36 months later. The patients were recruited from the Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation – Parkinson’s Disease (ICICLE-PD) study.
In this ICICLE-Gait substudy, participants walked for 2 minutes around a circuit that included a 7-meter instrumented walkway (GaitRite) that recorded 16 gait characteristics in the five independent domains of pace, variability, rhythm, asymmetry, and posture control. The investigators used the Montreal Cognitive Assessment (MoCA) battery of tests to assess global cognition, attention, fluctuating attention, executive function, working memory, visual memory, and visuospatial ability. They adjusted the results for covariates of age, education, gender, depression, and levodopa equivalent daily doses.
“We found that seven characteristics of gait were able to predict changes in measures of attention,” Dr. Morris said during a poster session at the World Parkinson Congress. The characteristics of gait were “mainly pace and variability and at diagnosis were sensitive to decline in tests of attention.”
With the multiple measures used in this study, a P value of less than or equal to .01 was considered statistically significant.
There were significant cognitive declines in the areas of attention, fluctuating attention, executive function, and visual memory. Fluctuating attention was predicted by measures of gait pace (step velocity, step length, and step swing: all P less than or equal to .007), gait variability (step stance and step length: both P less than or equal to .01), and postural control (P = .004). The pace measure of step length also predicted a decline in visual memory (P = .01).
Baseline MoCA predicted a decline in attention (P less than .001) but not in fluctuating attention or in visual memory.
The authors said that this study is the first “to demonstrate that discrete gait characteristics can predict measures of cognitive decline in early PD.” Asked why gait may predict cognitive decline, Dr. Morris postulated that certain characteristics of gait, such as speed and postural control, are related to cognition more so than other characteristics such as asymmetry.
These techniques may have clinical utility and not be merely of research interest. The parameters of gait may be measurable in the community using wearable sensors such as accelerometers “to measure discrete characteristics of gait ... So, ideally, it will be a possible future biomarker, and then we can measure them in the clinic and then identify risks from there,” she said, adding that she is planning research to explore the association of gait and cognition. Confounding factors yet to be examined are the effects of being on or off different medications and different medication cycles when patients are free-living in the community.
If researchers can validate that gait is a sensitive predictor of dementia, then the question becomes what to do about it. Dr. Morris suggested that physical therapy should incorporate more cognitive tasks.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center, said that the study is “really interesting because right now there’s a huge search underway for biomarkers” to reliably predict progression of Parkinson’s disease or predict who is at risk for the disease.
“These investigators looked at whether something as seemingly simple as gait – so the way that someone walks, the way that their balance is, the pace of their walking – could predict decline in cognition. And that’s something of great interest to clinicians and to researchers: How do we figure out which of our patients are going to experience cognitive decline and in what different domains?” she said.
Although the researchers in this study used sophisticated and sensitive measures of several aspects of gait not generally available to clinicians, Dr. Fleisher predicted that it may be possible to extrapolate the findings to look for specific aspects of gait variability (possibly through the use of wearable devices) so the technique may become widely useful.
Once a patient is seen to be at high risk for cognitive decline, she said, exercise may be an appropriate intervention. “We know huge benefits of exercise, which have been shown in various aspects of cognitive decline ... [to] slow the decline in cognitive function.” Dr. Fleisher said the best exercise is any one that a patient will continue to do, whether it is walking, dancing, or any other exercise that the person will stick with.
The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris reported having no financial disclosures. Dr. Fleisher had no financial disclosures.
AT WPC 2016
Key clinical point: Gait characteristics, not cognition, predict cognitive decline in early Parkinson’s.
Major finding: Gait pace, variability, and postural control predict cognitive decline.
Data source: Observational study of 119 patients with early idiopathic Parkinson’s disease assessed at baseline and at 36 months.
Disclosures: The study was supported in the United Kingdom by the National Institute for Health Research, the National Health Service, and Parkinson’s UK. There was no commercial funding. Dr. Morris and Dr. Fleisher had no financial disclosures.
Parkinson’s cell transplant trials require better standardization
PORTLAND, ORE. – Implantation of dopamine-producing cells to replace those lost in the substantia nigra has been seen as the cure for Parkinson’s disease, with many attempts in patients over the years. Along the way, a few successes have occurred, but in general, cell-based therapies have produced mixed results.
“When it works well, it works very well with fetal dopamine cells, but it does not always work well,” said Roger Barker, MBBS, PhD, of the department of clinical neurosciences at the University of Cambridge (England). In his lecture to a large, capacity crowd at the World Parkinson Congress, he reviewed the field going back more than three decades and drew “lessons learned” from the results of animal experiments and human trials.
He said dopamine-producing cell therapy will never cure the disease, although it works well early in the disease “but creates problems later,” with off-target and nonphysiologic effects in other parts of the brain, such as overstimulation. One exception was the use of fetal dopamine cells in an animal model, showing that cells could survive long-term, connect and integrate into the brain, release dopamine, and restore behaviors to normal if cells from the same species were used at the right developmental stage of the animal and implanted where dopamine normally works, that is, in the striatum.
Other problems reported from human trials using embryonic dopamine neurons or fetal nigral transplants have been graft-induced dyskinesias, but without clinical benefit, as well as Lewy bodies in grafted neurons, suggesting host-to-graft disease propagation. However, in another report, a patient had a clinical benefit and showed extensive graft-derived dopaminergic innervation 24 years after transplantation, at which time the patient died.
Lessons learned over time
Dr. Barker explained that the variable results that have been achieved in various trials using different protocols and nonstandardized approaches over the years make it “extremely difficult to make any conclusions.” These variations included performing tests on different kinds of patients and using different doses of cells, delivery approaches, immunosuppression, primary endpoints of the trials, and levels of follow-up.
The age of the patient, disease stage, and graft technique emerged as key issues in data gathered from the trials, he said. The best chance of success occurred in younger patients with less advanced disease, when grafting occurred across the whole striatum evenly, and when contamination with 5-hydroxytryptamine (serotonin) neurons was avoided.
Going forward, trials in Parkinson’s disease are planned or underway using embryonic/fetal stem cells or adult stem cells. Such cells provide logistical advantages in that their differentiation can be controlled more easily and they are a defined product. Nigral dopaminergic cells can be produced from human embryonic stem cells that behave like human fetal ventral midbrain dopamine cells in vitro and in vivo in rats and show similar efficacy and potency.
The Center for iPS Cell Research and Application in Kyoto, Japan, will conduct a trial using induced pluripotent stem (iPS) cells beginning next year, the New York State Stem Cell Science Consortia (NYSTEM) will use human embryonic stem cells beginning in 2018, and around the same time the European Union’s NeuroStemCellRepair network will also use human embryonic stem cells. In addition, the European TRANSEURO trial, coordinated by Dr. Barker, is planning a single-arm, multicenter, dose-escalation trial for 2018/2019 using intracerebral neurotransplantation of dopaminergic neurons derived from human embryonic stem cells. Participating patients will be younger than 65 years with less than 10 years disease duration, no significant levodopa-induced dyskinesia, and no cognitive or psychiatric problems.
From these trials, scientists hope to eventually produce a human embryonic stem cell–derived dopaminergic cell product made under GMP (good manufacturing practice) conditions that can be tested for safety and efficacy and put into clinical trials, with an ultimate goal of production and commercialization.
Finally, Dr. Barker alerted physicians to published guidance from the International Society for Stem Cell Research that can help them critically evaluate any cell-based clinical trial that they may be asked to run. And for patients, large numbers of whom attended the conference, he advised avoiding any “trial” that would charge them to participate because legitimate research trials do not charge for experimental therapies.
Asked to comment on the field, Peter LeWitt, MD, director of the Parkinson’s Disease and Movement Disorders Program at Henry Ford Hospital, West Bloomfield, Mich., and professor of neurology at Wayne State University, Detroit, said, “The jury is out and is coming back on stem cells and its alternative, such as fetal tissue. It’s pointing to the bright future of restoring the brain and not just using drugs to mask symptoms.”
He said the critical review of evidence from past trials “sounds like it’s heading towards a more focused view of how to enhance the successes that have occurred already – the 24-year outcomes [of] the patients who have met all biological plausibility improvements at this point. ... The science has moved along to improve their techniques of judging success and failure and sorting out partial benefits.”
Dr. Barker reported that he sits on an advisory board of Teva-Lundbeck and has advised and received honoraria from Solvay, GSK, Eli Lilly, and Pfizer, receives royalties from Springer, Wiley, and Cambridge University Press, and receives grant support from various institutes and foundations, Dr. LeWitt reported no relevant conflicts of interest.
PORTLAND, ORE. – Implantation of dopamine-producing cells to replace those lost in the substantia nigra has been seen as the cure for Parkinson’s disease, with many attempts in patients over the years. Along the way, a few successes have occurred, but in general, cell-based therapies have produced mixed results.
“When it works well, it works very well with fetal dopamine cells, but it does not always work well,” said Roger Barker, MBBS, PhD, of the department of clinical neurosciences at the University of Cambridge (England). In his lecture to a large, capacity crowd at the World Parkinson Congress, he reviewed the field going back more than three decades and drew “lessons learned” from the results of animal experiments and human trials.
He said dopamine-producing cell therapy will never cure the disease, although it works well early in the disease “but creates problems later,” with off-target and nonphysiologic effects in other parts of the brain, such as overstimulation. One exception was the use of fetal dopamine cells in an animal model, showing that cells could survive long-term, connect and integrate into the brain, release dopamine, and restore behaviors to normal if cells from the same species were used at the right developmental stage of the animal and implanted where dopamine normally works, that is, in the striatum.
Other problems reported from human trials using embryonic dopamine neurons or fetal nigral transplants have been graft-induced dyskinesias, but without clinical benefit, as well as Lewy bodies in grafted neurons, suggesting host-to-graft disease propagation. However, in another report, a patient had a clinical benefit and showed extensive graft-derived dopaminergic innervation 24 years after transplantation, at which time the patient died.
Lessons learned over time
Dr. Barker explained that the variable results that have been achieved in various trials using different protocols and nonstandardized approaches over the years make it “extremely difficult to make any conclusions.” These variations included performing tests on different kinds of patients and using different doses of cells, delivery approaches, immunosuppression, primary endpoints of the trials, and levels of follow-up.
The age of the patient, disease stage, and graft technique emerged as key issues in data gathered from the trials, he said. The best chance of success occurred in younger patients with less advanced disease, when grafting occurred across the whole striatum evenly, and when contamination with 5-hydroxytryptamine (serotonin) neurons was avoided.
Going forward, trials in Parkinson’s disease are planned or underway using embryonic/fetal stem cells or adult stem cells. Such cells provide logistical advantages in that their differentiation can be controlled more easily and they are a defined product. Nigral dopaminergic cells can be produced from human embryonic stem cells that behave like human fetal ventral midbrain dopamine cells in vitro and in vivo in rats and show similar efficacy and potency.
The Center for iPS Cell Research and Application in Kyoto, Japan, will conduct a trial using induced pluripotent stem (iPS) cells beginning next year, the New York State Stem Cell Science Consortia (NYSTEM) will use human embryonic stem cells beginning in 2018, and around the same time the European Union’s NeuroStemCellRepair network will also use human embryonic stem cells. In addition, the European TRANSEURO trial, coordinated by Dr. Barker, is planning a single-arm, multicenter, dose-escalation trial for 2018/2019 using intracerebral neurotransplantation of dopaminergic neurons derived from human embryonic stem cells. Participating patients will be younger than 65 years with less than 10 years disease duration, no significant levodopa-induced dyskinesia, and no cognitive or psychiatric problems.
From these trials, scientists hope to eventually produce a human embryonic stem cell–derived dopaminergic cell product made under GMP (good manufacturing practice) conditions that can be tested for safety and efficacy and put into clinical trials, with an ultimate goal of production and commercialization.
Finally, Dr. Barker alerted physicians to published guidance from the International Society for Stem Cell Research that can help them critically evaluate any cell-based clinical trial that they may be asked to run. And for patients, large numbers of whom attended the conference, he advised avoiding any “trial” that would charge them to participate because legitimate research trials do not charge for experimental therapies.
Asked to comment on the field, Peter LeWitt, MD, director of the Parkinson’s Disease and Movement Disorders Program at Henry Ford Hospital, West Bloomfield, Mich., and professor of neurology at Wayne State University, Detroit, said, “The jury is out and is coming back on stem cells and its alternative, such as fetal tissue. It’s pointing to the bright future of restoring the brain and not just using drugs to mask symptoms.”
He said the critical review of evidence from past trials “sounds like it’s heading towards a more focused view of how to enhance the successes that have occurred already – the 24-year outcomes [of] the patients who have met all biological plausibility improvements at this point. ... The science has moved along to improve their techniques of judging success and failure and sorting out partial benefits.”
Dr. Barker reported that he sits on an advisory board of Teva-Lundbeck and has advised and received honoraria from Solvay, GSK, Eli Lilly, and Pfizer, receives royalties from Springer, Wiley, and Cambridge University Press, and receives grant support from various institutes and foundations, Dr. LeWitt reported no relevant conflicts of interest.
PORTLAND, ORE. – Implantation of dopamine-producing cells to replace those lost in the substantia nigra has been seen as the cure for Parkinson’s disease, with many attempts in patients over the years. Along the way, a few successes have occurred, but in general, cell-based therapies have produced mixed results.
“When it works well, it works very well with fetal dopamine cells, but it does not always work well,” said Roger Barker, MBBS, PhD, of the department of clinical neurosciences at the University of Cambridge (England). In his lecture to a large, capacity crowd at the World Parkinson Congress, he reviewed the field going back more than three decades and drew “lessons learned” from the results of animal experiments and human trials.
He said dopamine-producing cell therapy will never cure the disease, although it works well early in the disease “but creates problems later,” with off-target and nonphysiologic effects in other parts of the brain, such as overstimulation. One exception was the use of fetal dopamine cells in an animal model, showing that cells could survive long-term, connect and integrate into the brain, release dopamine, and restore behaviors to normal if cells from the same species were used at the right developmental stage of the animal and implanted where dopamine normally works, that is, in the striatum.
Other problems reported from human trials using embryonic dopamine neurons or fetal nigral transplants have been graft-induced dyskinesias, but without clinical benefit, as well as Lewy bodies in grafted neurons, suggesting host-to-graft disease propagation. However, in another report, a patient had a clinical benefit and showed extensive graft-derived dopaminergic innervation 24 years after transplantation, at which time the patient died.
Lessons learned over time
Dr. Barker explained that the variable results that have been achieved in various trials using different protocols and nonstandardized approaches over the years make it “extremely difficult to make any conclusions.” These variations included performing tests on different kinds of patients and using different doses of cells, delivery approaches, immunosuppression, primary endpoints of the trials, and levels of follow-up.
The age of the patient, disease stage, and graft technique emerged as key issues in data gathered from the trials, he said. The best chance of success occurred in younger patients with less advanced disease, when grafting occurred across the whole striatum evenly, and when contamination with 5-hydroxytryptamine (serotonin) neurons was avoided.
Going forward, trials in Parkinson’s disease are planned or underway using embryonic/fetal stem cells or adult stem cells. Such cells provide logistical advantages in that their differentiation can be controlled more easily and they are a defined product. Nigral dopaminergic cells can be produced from human embryonic stem cells that behave like human fetal ventral midbrain dopamine cells in vitro and in vivo in rats and show similar efficacy and potency.
The Center for iPS Cell Research and Application in Kyoto, Japan, will conduct a trial using induced pluripotent stem (iPS) cells beginning next year, the New York State Stem Cell Science Consortia (NYSTEM) will use human embryonic stem cells beginning in 2018, and around the same time the European Union’s NeuroStemCellRepair network will also use human embryonic stem cells. In addition, the European TRANSEURO trial, coordinated by Dr. Barker, is planning a single-arm, multicenter, dose-escalation trial for 2018/2019 using intracerebral neurotransplantation of dopaminergic neurons derived from human embryonic stem cells. Participating patients will be younger than 65 years with less than 10 years disease duration, no significant levodopa-induced dyskinesia, and no cognitive or psychiatric problems.
From these trials, scientists hope to eventually produce a human embryonic stem cell–derived dopaminergic cell product made under GMP (good manufacturing practice) conditions that can be tested for safety and efficacy and put into clinical trials, with an ultimate goal of production and commercialization.
Finally, Dr. Barker alerted physicians to published guidance from the International Society for Stem Cell Research that can help them critically evaluate any cell-based clinical trial that they may be asked to run. And for patients, large numbers of whom attended the conference, he advised avoiding any “trial” that would charge them to participate because legitimate research trials do not charge for experimental therapies.
Asked to comment on the field, Peter LeWitt, MD, director of the Parkinson’s Disease and Movement Disorders Program at Henry Ford Hospital, West Bloomfield, Mich., and professor of neurology at Wayne State University, Detroit, said, “The jury is out and is coming back on stem cells and its alternative, such as fetal tissue. It’s pointing to the bright future of restoring the brain and not just using drugs to mask symptoms.”
He said the critical review of evidence from past trials “sounds like it’s heading towards a more focused view of how to enhance the successes that have occurred already – the 24-year outcomes [of] the patients who have met all biological plausibility improvements at this point. ... The science has moved along to improve their techniques of judging success and failure and sorting out partial benefits.”
Dr. Barker reported that he sits on an advisory board of Teva-Lundbeck and has advised and received honoraria from Solvay, GSK, Eli Lilly, and Pfizer, receives royalties from Springer, Wiley, and Cambridge University Press, and receives grant support from various institutes and foundations, Dr. LeWitt reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM WPC 2016
Transplant recipients need dermatologists both pre- and post-transplant
Boston – Shared medical appointments can work well for patients undergoing solid organ transplants and for the clinical staff treating them – serving as an efficient way to educate several patients in a common setting and giving them the opportunity to interact with others going through a similar experience.
“Having those shared medical appointments where they’re sitting next to somebody who’s going through the same thought process and information gathering ... and the ability to talk with similar folks is a huge benefit for those patients,” said Allison Vidimos, MD, chair of the department of dermatology at the Cleveland Clinic. Dr. Vidimos and her colleagues have been so focused on skin cancer diagnosis and treatment in this group of patients that “we’ve kind of lost sight of the human aspect of it and the fear that these patients have,” she added.
These shared medical appointments at the Cleveland Clinic also provide the dermatology staff an efficient means to educate a group of patients about the risks of developing skin cancers and benign conditions associated with immunosuppressive treatments. They also discuss sun protection and avoidance practices, and how to perform skin self exams, all of which are “really important for their well being after their transplant,” Dr. Vidimos said during an interview at the American Academy of Dermatology summer meeting.
Patients learn how frequently they will need a clinical skin exam post-transplant, depending on the occurrence of skin cancers, and that biopsies may be necessary at times.
Dr. Vidimos said it is up to the transplant surgeons to discuss with patients the very low risk of transmission of malignancies from the donor to the recipient. In her presentation at the meeting, she cited a 1.4% risk of an undetected skin or internal malignancy in a donor being transmitted to the recipient.
Because of changes in criteria, patients who have relatively low risk skin cancers or higher risk skin cancers and have been treated, and are at “a defined interval post-treatment where we feel it’s safe to do that transplant,” may be considered a transplant candidate, she said noting that previously, such patients would be excluded from a transplant.
The appropriate time intervals to wait for a transplant for candidates with a history of cutaneous squamous cell carcinoma, malignant melanoma, or Merkel cell carcinoma are spelled out in a recently published consensus paper Dr. Vidimos coauthored with other members of the International Transplant Skin Cancer Collaborative (Am J Transplant. 2016 Feb;16[2]:407-13).
Dr. Vidimos said she is sometimes called to the bedside to perform a skin exam in a pretransplant patient who is very ill. The most common scenario is a liver transplant candidate awaiting transport to the operating room, who has not had a skin exam and needs to be cleared by a dermatologist to rule out a melanoma or another type of skin cancer that could be “fertilized” by postoperative immunosuppressant therapy.
After a transplant, patients need to be seen frequently enough to detect malignant transformation of precancerous skin lesions. Dermatologists should have a low threshold for biopsying any suspicious lesions early. “A lot of times we get biopsies back of skin cancer that do not match ... the clinical picture,” Dr. Vidimos said. Patients should be referred when the dermatologist feels that he or she can not deliver the appropriate treatment.
As transplants have become fairly routine and patients are living longer, community dermatologists will most likely be seeing solid organ transplant recipients more frequently. With longer lifespans, those patients will have more opportunity to develop more skin cancers.
Dr. Vidimos disclosed having received grants and research funding from Genentech.
Boston – Shared medical appointments can work well for patients undergoing solid organ transplants and for the clinical staff treating them – serving as an efficient way to educate several patients in a common setting and giving them the opportunity to interact with others going through a similar experience.
“Having those shared medical appointments where they’re sitting next to somebody who’s going through the same thought process and information gathering ... and the ability to talk with similar folks is a huge benefit for those patients,” said Allison Vidimos, MD, chair of the department of dermatology at the Cleveland Clinic. Dr. Vidimos and her colleagues have been so focused on skin cancer diagnosis and treatment in this group of patients that “we’ve kind of lost sight of the human aspect of it and the fear that these patients have,” she added.
These shared medical appointments at the Cleveland Clinic also provide the dermatology staff an efficient means to educate a group of patients about the risks of developing skin cancers and benign conditions associated with immunosuppressive treatments. They also discuss sun protection and avoidance practices, and how to perform skin self exams, all of which are “really important for their well being after their transplant,” Dr. Vidimos said during an interview at the American Academy of Dermatology summer meeting.
Patients learn how frequently they will need a clinical skin exam post-transplant, depending on the occurrence of skin cancers, and that biopsies may be necessary at times.
Dr. Vidimos said it is up to the transplant surgeons to discuss with patients the very low risk of transmission of malignancies from the donor to the recipient. In her presentation at the meeting, she cited a 1.4% risk of an undetected skin or internal malignancy in a donor being transmitted to the recipient.
Because of changes in criteria, patients who have relatively low risk skin cancers or higher risk skin cancers and have been treated, and are at “a defined interval post-treatment where we feel it’s safe to do that transplant,” may be considered a transplant candidate, she said noting that previously, such patients would be excluded from a transplant.
The appropriate time intervals to wait for a transplant for candidates with a history of cutaneous squamous cell carcinoma, malignant melanoma, or Merkel cell carcinoma are spelled out in a recently published consensus paper Dr. Vidimos coauthored with other members of the International Transplant Skin Cancer Collaborative (Am J Transplant. 2016 Feb;16[2]:407-13).
Dr. Vidimos said she is sometimes called to the bedside to perform a skin exam in a pretransplant patient who is very ill. The most common scenario is a liver transplant candidate awaiting transport to the operating room, who has not had a skin exam and needs to be cleared by a dermatologist to rule out a melanoma or another type of skin cancer that could be “fertilized” by postoperative immunosuppressant therapy.
After a transplant, patients need to be seen frequently enough to detect malignant transformation of precancerous skin lesions. Dermatologists should have a low threshold for biopsying any suspicious lesions early. “A lot of times we get biopsies back of skin cancer that do not match ... the clinical picture,” Dr. Vidimos said. Patients should be referred when the dermatologist feels that he or she can not deliver the appropriate treatment.
As transplants have become fairly routine and patients are living longer, community dermatologists will most likely be seeing solid organ transplant recipients more frequently. With longer lifespans, those patients will have more opportunity to develop more skin cancers.
Dr. Vidimos disclosed having received grants and research funding from Genentech.
Boston – Shared medical appointments can work well for patients undergoing solid organ transplants and for the clinical staff treating them – serving as an efficient way to educate several patients in a common setting and giving them the opportunity to interact with others going through a similar experience.
“Having those shared medical appointments where they’re sitting next to somebody who’s going through the same thought process and information gathering ... and the ability to talk with similar folks is a huge benefit for those patients,” said Allison Vidimos, MD, chair of the department of dermatology at the Cleveland Clinic. Dr. Vidimos and her colleagues have been so focused on skin cancer diagnosis and treatment in this group of patients that “we’ve kind of lost sight of the human aspect of it and the fear that these patients have,” she added.
These shared medical appointments at the Cleveland Clinic also provide the dermatology staff an efficient means to educate a group of patients about the risks of developing skin cancers and benign conditions associated with immunosuppressive treatments. They also discuss sun protection and avoidance practices, and how to perform skin self exams, all of which are “really important for their well being after their transplant,” Dr. Vidimos said during an interview at the American Academy of Dermatology summer meeting.
Patients learn how frequently they will need a clinical skin exam post-transplant, depending on the occurrence of skin cancers, and that biopsies may be necessary at times.
Dr. Vidimos said it is up to the transplant surgeons to discuss with patients the very low risk of transmission of malignancies from the donor to the recipient. In her presentation at the meeting, she cited a 1.4% risk of an undetected skin or internal malignancy in a donor being transmitted to the recipient.
Because of changes in criteria, patients who have relatively low risk skin cancers or higher risk skin cancers and have been treated, and are at “a defined interval post-treatment where we feel it’s safe to do that transplant,” may be considered a transplant candidate, she said noting that previously, such patients would be excluded from a transplant.
The appropriate time intervals to wait for a transplant for candidates with a history of cutaneous squamous cell carcinoma, malignant melanoma, or Merkel cell carcinoma are spelled out in a recently published consensus paper Dr. Vidimos coauthored with other members of the International Transplant Skin Cancer Collaborative (Am J Transplant. 2016 Feb;16[2]:407-13).
Dr. Vidimos said she is sometimes called to the bedside to perform a skin exam in a pretransplant patient who is very ill. The most common scenario is a liver transplant candidate awaiting transport to the operating room, who has not had a skin exam and needs to be cleared by a dermatologist to rule out a melanoma or another type of skin cancer that could be “fertilized” by postoperative immunosuppressant therapy.
After a transplant, patients need to be seen frequently enough to detect malignant transformation of precancerous skin lesions. Dermatologists should have a low threshold for biopsying any suspicious lesions early. “A lot of times we get biopsies back of skin cancer that do not match ... the clinical picture,” Dr. Vidimos said. Patients should be referred when the dermatologist feels that he or she can not deliver the appropriate treatment.
As transplants have become fairly routine and patients are living longer, community dermatologists will most likely be seeing solid organ transplant recipients more frequently. With longer lifespans, those patients will have more opportunity to develop more skin cancers.
Dr. Vidimos disclosed having received grants and research funding from Genentech.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016